
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Nutr., 04 March 2025
Sec. Food Policy and Economics
Volume 12 - 2025 | https://doi.org/10.3389/fnut.2025.1524580
 Vitowe Batch1,2
Vitowe Batch1,2 Martina Kress1
Martina Kress1 Aggrey Pemba Gama3
Aggrey Pemba Gama3 Tinna Ng’ong’ola-Manani3
Tinna Ng’ong’ola-Manani3 Gabriella Chiutsi-Phiri4
Gabriella Chiutsi-Phiri4 Ponyadira Leah Corner5
Ponyadira Leah Corner5 Save Kumwenda2
Save Kumwenda2 Chikumbusko Kaonga2
Chikumbusko Kaonga2 Mphatso Kamndaya2
Mphatso Kamndaya2 Maurice Monjerezi6
Maurice Monjerezi6 John F. Leslie7
John F. Leslie7 Limbikani Matumba4*
Limbikani Matumba4*Food contamination is a critical global health issue, with the WHO estimating millions of deaths and Disability-adjusted life years (DALYs) lost annually due to foodborne diseases, particularly in developing countries. To address this, the WHO introduced the Five Keys to Safer Food (WHO-FKSF) to promote essential food safety practices. We analyzed the limitations of the WHO-FKSF for use in developing countries. We explore contextually relevant adaptations, such as community engagement, infrastructure improvements, and innovations like durable, child-resistant tippy taps (simple, low-cost handwashing devices that dispense water when tipped) for handwashing, required to make the WHO-FKSF applicable in rural portions of developing countries. Addressing cultural norms and involving men in water-related tasks can further align food safety practices with everyday realities. We recommend providing a specific rationale for each actionable step, beyond the general reasoning provided for the five keys themselves. This additional information will improve comprehension and adherence to the practices. We also recommend revising Key 4, “Keep food at safe temperatures,” to “Store food safely” to better accommodate the lack of refrigeration and to promote low-cost food preservation methods. Adapting the WHO-FKSF to the specific needs of these communities could significantly reduce foodborne illnesses and improve public health outcomes across sub-Saharan Africa.
Food contamination is a major global health challenge, resulting in significant morbidity and mortality, with WHO’s 2010 Foodborne Disease Burden Epidemiology Reference Group (FERG) estimates indicating millions of deaths and Disability-adjusted life years (DALYs) from foodborne diseases, comparable to malaria and tuberculosis (1, 2). This burden is especially high in Asia and Africa, where tropical climates facilitate pathogen growth particularly affecting children (3, 4). The true impact may be even greater, and updated estimates are anticipated in 2025 (5).
To combat foodborne diseases, WHO introduced the Five Keys to Safer Food (WHO-FKSF) in 2001, outlining essential food safety practices: (1) Keep clean, (2) Separate raw and cooked foods, (3) Cook thoroughly, (4) Keep food at safe temperatures, and (5) Use safe water and raw materials (6). These guidelines, translated into various languages, offer a foundational framework for improving food safety. Adherence to the WHO-FKSF depends on access to resources and the ability to integrate these practices into daily routines, which are influenced by cultural norms, social dynamics, and household responsibilities.
The WHO Five Keys to Safer Food Manual (6) provides implementation guidelines applicable primarily in urban and developed areas, where refrigeration, electricity, water and sanitation facilities are commonly available. Yet these guidelines are even more important in rural areas of developing countries, where food safety risks are significantly higher due to inadequate infrastructure, limited access to clean water, poor sanitation, and lack of refrigeration (3). Some local customs promote unhygienic activities, e.g., limited handwashing, and common utensils and surfaces for kitchen and non-kitchen purposes, that need non-scientific efforts to change (7). The reliance on traditional food preparation methods can further increase the risk of contamination. Unlike urban settings, where modern facilities and regulations may mitigate foodborne threats, rural communities experience a disproportionately higher burden of foodborne diseases (8, 9). Adhering to the WHO-FKSF and identifying functional adaptations for rural developing situations can help mitigate these risks by promoting hygiene, safe food handling, and proper storage, thereby reducing illness and improving public health.
WHO-FKSF guidelines are scientifically robust, but implementing them in rural, resource-limited settings present unique and complex challenges. These challenges are influenced by a combination of cultural norms, societal structures, and resource constraints that affect food safety practices and attitudes toward them. This perspective explores known barriers to adherence to the Five Keys in resource-limited communities in developing countries. As a result, we propose adapting WHO’s food safety strategies to better align with the everyday realities and constraints of rural life in these regions—Five Keys to Safer Food in Developing Countries (FKSF-DC).
In many households, limited access to running water forces communities to rely on alternatives like tippy taps (10) for handwashing. These simple devices, typically consisting of containers that dispense water when tipped via a foot lever, are frequently damaged by children and livestock, making them difficult to maintain. A recent study found that only 10.5% of households had functional tippy taps, all located near toilets, with none placed near kitchens where food is prepared (7). The scarcity and specific placement of these stations likely increase their novelty, making them attractive as playthings for children, leading to frequent misuse and damage. The lack of adequate household water exacerbates these problems. Many households rely on water drawn from distant sources that is carried home in jugs or pails carried by women on their heads. Bringing water is time-consuming and is only one of many responsibilities that women bear, e.g., hygiene, farming, child care, etc. (11). Thus, clean household water is at a premium, very limited in quantity and its use restricted to essential activities with drinking and cooking usually prioritized over hygiene practices such as handwashing, and cleaning of utensils and work surfaces (12).
Soap also is perceived as a luxury due to competing household priorities (13), and its cost often renders it inaccessible in many communities. From a recent focus group, “We lack soap for bathing, so how can we afford the luxury of frequent hand washing with soap?” (Batch et al., unpublished). Inadequate knowledge of the health benefits of handwashing and social norms hinder compliance even further, as deeply rooted beliefs and behaviors can undermine the adoption of consistent hand hygiene practices. For example, from a focus group participant, “If you insist on proper hand washing in public such as at a funeral, church, wedding or in the company of your in-laws, they will ridicule you and say you are selfish and pompous” (Batch et al., unpublished). The improper use and handling of kitchen cloths also compounds hygiene risks, as cloths are often reused without adequate washing or drying, creating a breeding ground for pathogens. The necessity of safeguarding livestock from theft leads many households to keep animals within close proximity, further complicating food safety practices (14).
Economic constraints prevent families from purchasing enough utensils to separate raw and cooked foods, a challenge worsened by the scarcity of potable water and soap, which renders washing between uses ineffective if it occurs at all (15). Home-slaughtered livestock, especially chickens, are desirable, but less common, and the same utensils are frequently used for both raw and cooked meats or other dishes leading to frequent cross-contamination. Furthermore, cultural priorities often place the importance of dish and utensil purchases below other household expenses such as food, school fees, and medical costs, and duplicate sets of bowls, plates and serving utensils are often viewed as a luxury that is unaffordable and perhaps even unnecessary.
Thermometers are unavailable or are too expensive, which leads to reliance on visual cues such as clear juices or browning, which may not suffice to ensure safety. Limited access to affordable fuel restricts cooking time, particularly for large cuts of meat. Many households lack electricity, much less devices such as microwaves. Using only wood or charcoal fires makes it difficult to reheat food evenly and safely (16).
Most households in developing countries lack refrigerators and ice boxes for cooling, forcing reliance on unsafe food preservation methods. While solar-powered refrigeration can serve as an alternative, its high cost makes it too expensive for many (17). Further, the cold chain is not always available during distribution and retail sale of fresh and highly perishable foods in informal markets which are the main sources of these foods for most households. Meat usually is boiled, although it may also be fried or grilled over an open fire. Cooked food often is kept warm by simmering, which commonly requires wood or charcoal to keep a fire going and may not evenly distribute the heat across the pot or pan. In general, other than dried grains and similar products, food, whether raw or cooked, is not preserved and must be consumed the day it is acquired and processed.
Many households in developing countries must fetch water from distant sources, a task predominantly carried out by women. Due to their numerous other responsibilities, such as childcare, cooking, and farming, women often cannot fetch sufficient water to meet all household needs, such as cooking, hygiene and sanitation. Water treatment chemicals either are unavailable or too expensive. Boiling water may change its taste, requires more firewood, and increases expense and deforestation. In many locations, it is all but impossible to obtain safe raw materials as hygiene is neither prioritized nor viewed as important. Local marketplaces commonly are unkempt at best (Figure 1), yet consumers continue to patronize them without questioning the safety of the products they purchase. Foods in these markets are normally not refrigerated. They commonly are open to the air and may be stored on the ground where they can be easily mixed with soil, animal dung, food waste and other debris and acquire microbial contaminants from the air or other sources.
Implementation of stringent food safety guidelines in developing countries is critical. The high ambient temperatures in many of these countries are conducive to the proliferation of foodborne pathogens, significantly elevating the risk of foodborne illnesses. Paradoxically, despite the heightened need, the implementation of WHO-FKSF faces considerable challenges in these regions. These obstacles are rooted in a combination of cultural norms and infrastructural, educational, and resource limitations, which hinder effective adherence to these essential food safety measures.
The WHO-FKSF are premised on the assumption that communities have relatively easy access to essential resources such as clean running water, soap, refrigeration, and proper cooking utensils, each of which is critical for preventing food contamination and ensuring food safety (3, 4). Unfortunately, in many rural areas of developing countries, these fundamental resources are lacking, or are not present at all. Most rural residents lack access to safe drinking water, and may have limited access to water for other purposes. Only a small proportion of rural households are connected to electricity, which makes refrigeration all but unobtainable. These shortages, compounded by inadequate sanitation facilities and insufficient cooking tools, undermine the practical implementation of the WHO-FKSF guidelines. The gap between the premise of available resources and the reality on the ground highlights the need for food safety strategies that are adapted to these local constraints.
Cultural norms and societal structures also present additional barriers. In many rural areas, deeply entrenched gender roles dictate that women are solely responsible for water collection, cooking, and other household tasks, giving them the primary responsibility for food safety. These roles limit their time and capacity to consistently follow the WHO-FKSF guidelines. Involving men and boys in water-related tasks can alleviate some of these burdens. For example, in India when men participate in water-fetching, they often use technology or transport methods that increases efficiency, reduces physical strain, and enables more sustainable approaches to meeting household water needs (18).
The omission of traditional preservation methods, e.g., drying, smoking, and fermenting, and the lack of guidance on microbial and mycotoxin contamination control, reveal a bias in the guidelines for resource-advantaged settings. The omission of these methods means that subsistence communities that rely on these methods lack guidance for contamination control, as highlighted under key number 5 (19). For example, integrating procedures specifically focused on mycotoxin control, such as those proposed by Matumba et al. (20), could increase the applicability of the WHO-FKSF in these settings. Such changes also align with the recommendations of Langsrud et al. (21), who advocate a revision of the WHO-FKSF that adopts a multidisciplinary, consumer-centered approach. Effective food safety communication addresses consumer motivations, cultural contexts, and practical challenges, including resource limitations and local practices. Such revisions would make the WHO-FKSF more adaptable, relevant, and applicable to food safety outcomes across diverse environments.
To increase the applicability of the WHO-FKSF in rural, resource-limited settings, these guidelines need to address local cultural practices, resource constraints, and societal structures. Engaging community leaders in promoting context-specific adaptations can make these hygiene practices more relevant. Child-resistant, durable designs for tippy taps can minimize misuse and prolong functionality, supporting consistent hand washing practices. Encouraging men’s involvement in water-related tasks could distribute some household tasks more equitably and promote innovative water solutions. Integrating affordable, well-established food preservation alternatives, e.g., fermentation and drying, can reduce the demand for refrigeration, while specific strategies for mycotoxin management and livestock containment can mitigate contamination risks in subsistence farming communities. Further, consumers should be taught to consider the hygienic conditions in open markets and to select food only from hygienic stalls.
We propose modifying the WHO-FKSF guidelines to better align with the realities of resource-limited settings. In particular, we recommend revising Key 4, “Keep food at safe temperatures,” to “Store food safely” (Table 1). This change expands the guideline to include alternatives to refrigeration, that are more readily implemented in resource-constrained developing countries, where refrigeration infrastructure is limited or non-existent. Additionally, we suggest providing a clear, evidence-based rationale for each overarching key and its specific actions. For example, as part of the “Keep clean” key (Key no. 1), the rationale for using running water during handwashing should clearly explain why washing in running water is more effective than is washing in stagnant water. By offering clear, scientifically supported explanations for each key action, the guidelines will be easier to understand, and more likely to be adopted, as individuals will more easily see the practical benefits of these food safety practices.
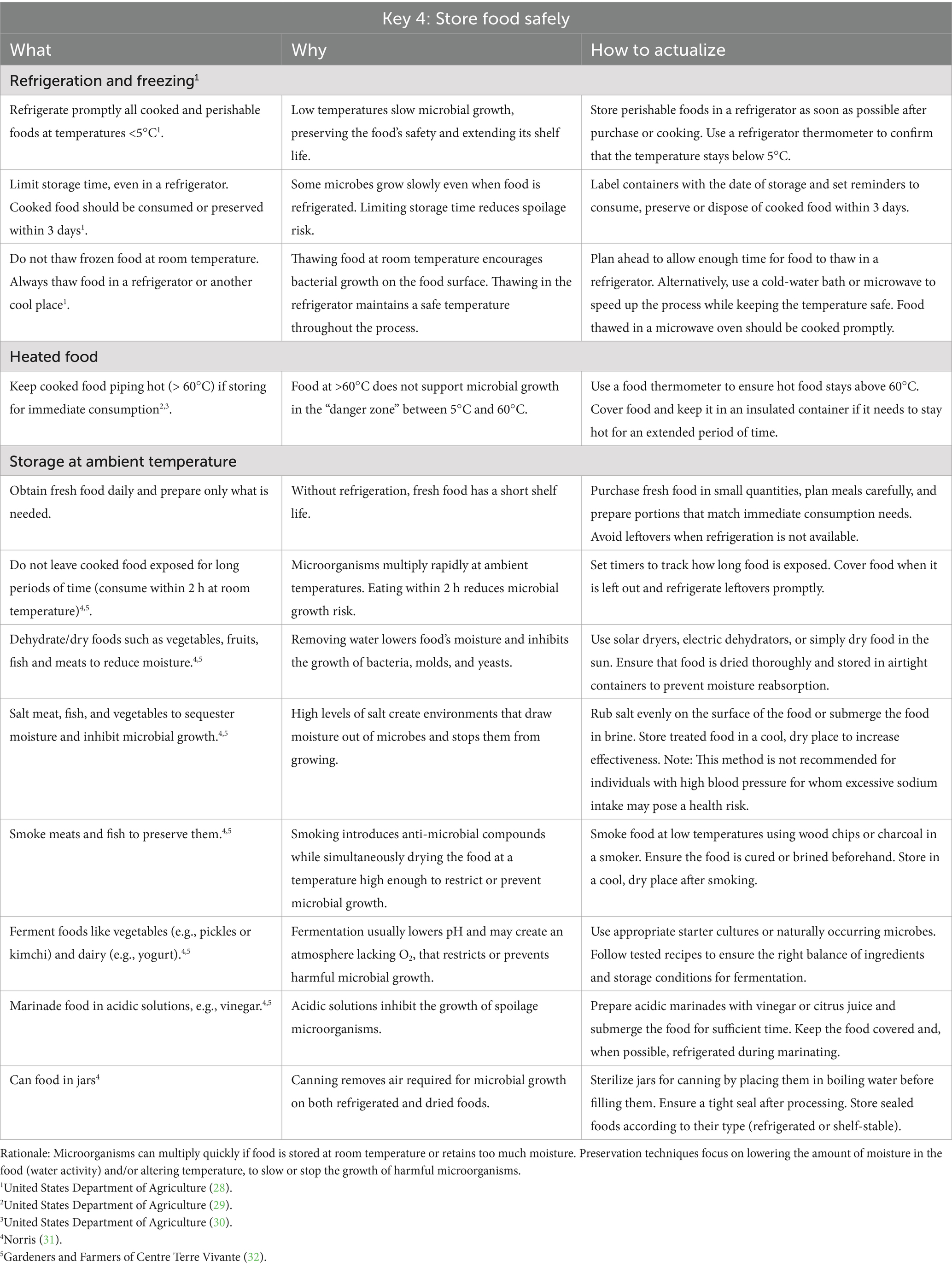
Table 1. Proposed modification of the WHO five keys to safer food’s fourth key, from “Keep food at safe temperatures” to “Store food safely” for regions with limited refrigeration.
In addition to individual responsibilities, the government must play a crucial role (22) by providing educational resources and in creating an enabling environment for compliance with the WHO-FKSK guidelines. In this role, four key areas must be addressed: (i) access to safe water, (ii) reliable electricity infrastructure, (iii) public education, and (iv) the affordability of hygiene essentials (23–27). Safe water is fundamental for cooking, cleaning, and handwashing, preventing contamination and foodborne illnesses. A stable electricity supply supports refrigeration, reducing spoilage and extending the shelf life of perishable foods. Public education initiatives should enhance awareness of proper hygiene practices and safe food handling. Finally, ensuring that hygiene products, e.g., hand and dish soap, and water dispensers, remain affordable will encourage their widespread, consistent use and help minimize microbial contamination during food preparation. By prioritizing these four areas, the government can strengthen public health and food security, and foster a safer and healthier society.
In rural portions of developing countries the stark reality is that unless food safety guidelines are adapted to local conditions, the most vulnerable communities may be left behind. The WHO-FKSF must evolve beyond its current framework to incorporate cultural understanding and resource-adaptive strategies to create meaningful change. As a first step in this evolution, we suggest that the WHO Five Keys to Safer Food (WHO-FKSF)—(1) Keep clean, (2) Separate raw and cooked foods, (3) Cook thoroughly, (4) Keep food at safe temperatures, and (5) Use safe water and raw materials—be changed to FKSF-DC—(1) Keep clean, (2) Separate raw and cooked foods, (3) Cook thoroughly, (4) Store food safely , and (5) Use safe water and raw materials. Further, guidelines should be developed to address particular regions’ socio-economic realities. By making this change, these guidelines will impact situations in developing countries that are in greatest need of improvement in food safety.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
VB: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing, Data curation. MaK: Project administration, Writing – original draft, Writing – review & editing, Funding acquisition. AG: Writing – original draft, Writing – review & editing, Conceptualization. TN: Conceptualization, Writing – original draft, Writing – review & editing. GC-P: Writing – original draft, Writing – review & editing. PC: Writing – original draft, Writing – review & editing. SK: Writing – original draft, Writing – review & editing. CK: Writing – original draft, Writing – review & editing. MpK: Writing – original draft, Writing – review & editing. MM: Writing – original draft, Writing – review & editing. JL: Writing – original draft, Writing – review & editing, Conceptualization. LM: Conceptualization, Writing – original draft, Writing – review & editing, Formal analysis, Investigation, Methodology, Project administration, Supervision.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Malawi Food and Nutrition Security Programme (FNSP) under the Special Initiative “Transformation of Agricultural and Food Systems” (SI AGER), which is funded by the German Ministry for Economic Cooperation and Development and implemented by the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) GmbH between February 2015 and March 2025. The funder supported the salaries of the first and second authors as research personnel and facilitated manuscript preparation. The funder had no direct influence on the study design, data interpretation, or conclusions presented. The authors are solely responsible for the content and views expressed in this publication.
Manuscript no. 25-090-J from the Kansas Agricultural Experiment Station, Manhattan.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The authors declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Havelaar, AH, Kirk, MD, Torgerson, PR, and Gibb, HJWorld Health Organization Foodborne Disease Burden Epidemiology Reference Group. World Health Organization global estimates and regional comparisons of the burden of foodborne disease in 2010. PLoS Med. (2015) 12:e1001923. doi: 10.1371/journal.pmed.1001923
2. Pires, SM, and Devleesschauwer, B. Estimates of global disease burden associated with foodborne pathogens In: JG Morris Jr and DJ Vugia, editors. Foodborne infections and intoxications. Cambridge, MA, USA: Academic Press (2021). 3–17.
3. Kirk, MD, Pires, SM, Black, RE, Caipo, M, Crump, JA, Devleesschauwer, B, et al. World health organization estimates of the global and regional disease burden of 22 foodborne bacterial, protozoal, and viral diseases, 2010: a data synthesis. PLoS Med. (2015) 12:e1001921. doi: 10.1371/journal.pmed.1001921
4. Oduoye, MO, Akilimali, A, Karim, KA, Moradeyo, AA, Abdullahi, ZZ, Muzata, D, et al. Diseases transmitted to humans through foodborne microbes in the global south In: MC Ogwu, SC Izah, and NR Ntuli, editors. Food safety and quality in the global south. Singapore: Springer Nature (2024). 561–97.
5. WHO. (2021). WHO steps up action to improve food safety and protect people from disease. Available online at: https://www.who.int/news/item/07-06-2021-who-steps-up-action-to-improve-food-safety-and-protect-people-from-disease (Accessed on 13 January 2025).
6. WHO. (2006). Five keys to food safer manual. Available online at: https://iris.who.int/bitstream/10665/43546/1/9789241594639_eng.pdf (Accessed on 10 February 2025).
7. Batch, V, Kress, M, Luhanga, E, Monjerezi, M, Pfaff, D, Phiri, H, et al. Knowledge, attitude, and practices of food hygiene among mothers from rural communities in Malawi. Hygie. (2024) 4:361–73. doi: 10.3390/hygiene4030028
8. Hoffmann, V, Moser, C, and Saak, A. Food safety in low and middle-income countries: the evidence through an economic lens. World Dev. (2019) 123:104611. doi: 10.1016/j.worlddev.2019.104611
9. Ortega, DL, and Tschirley, DL. Demand for food safety in emerging and developing countries: a research agenda for Asia and sub-Saharan Africa. J Agribusiness Develop Emerg Econ. (2017) 7:21–34. doi: 10.1108/JADEE-12-2014-0045
10. Bensen, D. (2023). What is a tippy-tap hand-washing device? Available online at: https://healingwaters.org/what-is-a-tippy-tap-hand-washing-device/ (Accessed on 13 January 2025)
11. Ezezika, O, Heng, J, Fatima, K, Mohamed, A, and Barrett, K. What are the barriers and facilitators to community handwashing with water and soap? A systematic review. PLOS Global Public Health. (2023) 3:e0001720. doi: 10.1371/journal.pgph.0001720
12. Howard, G., Bartram, J., Williams, A., Overbo, A., and Geere, J. (2020). Domestic water quantity, service level and health. World Health Organization. Available online at: https://apps.who.int/iris/bitstream/handle/10665/338044/9789240015241-eng.pdf. (Accessed on 13 January 2025)
13. Bowen, A, Agboatwalla, M, and Ayers, T. Sustained improvements in handwashing indicators more than 5 years after a cluster-randomized, community-based trial of handwashing promotion in Karachi, Pakistan. Trop Med Int Health. (2013) 18:259–67. doi: 10.1111/tmi.12046
14. Amissah-Reynolds, PK. Zoonotic risks from domestic animals in Ghana. Int J Pathog Res. (2020) 4:17–31. doi: 10.9734/ijpr/2020/v4i330113
15. Grace, D. Burden of foodborne disease in low-income and middle-income countries and opportunities for scaling food safety interventions. Food Secur. (2023) 15:1475–88. doi: 10.1007/s12571-023-01391-3
16. Rubinstein, F, Mbatchou Ngahane, BH, Nilsson, M, Esong, MB, Betang, E, Goura, AP, et al. Adoption of electricity for clean cooking in Cameroon: a mixed-methods field evaluation of current cooking practices and scale-up potential. Energy Sustain Dev. (2022) 71:118–31. doi: 10.1016/j.esd.2022.09.010
17. Aworh, OC. Food safety issues in fresh produce supply chain with particular reference to sub-Saharan Africa. Food Control. (2021) 123:107737. doi: 10.1016/j.foodcont.2020.107737
18. Brewis, A, Choudhary, N, and Wutich, A. Men’s household water fetching in India: gender inequity is associated with greater responsibility and related risks. Am J Hum Biol. (2024) 36:e23990. doi: 10.1002/ajhb.23990
19. Kebede, H, Liu, X, Jin, J, and Xing, F. Current status of major mycotoxins contamination in food and feed in Africa. Food Control. (2020) 110:106975. doi: 10.1016/j.foodcont.2019.106975
20. Matumba, L, Namaumbo, S, Ngoma, T, Meleke, N, De Boevre, M, Logrieco, AF, et al. Five keys to prevention and control of mycotoxins in grains: a proposal. Glob Food Sec. (2021) 30:100562. doi: 10.1016/j.gfs.2021.100562
21. Langsrud, S, Veflen, N, Allison, R, Crawford, B, Izsó, T, Kasza, G, et al. A trans disciplinary and multi actor approach to develop high impact food safety messages to consumers: time for a revision of the WHO-five keys to safer food? Trends Food Sci Technol. (2023) 133:87–98. doi: 10.1016/j.tifs.2023.01.018
22. Reilly, A, Ellard, R, and O’Connor, J. Food safety at the national level In: B-P Mansourian, A Wojtzak, and SM Mahfouz, editors. Medical sciences, vol II. Encyclopedia of life support systems. Oxford, UK: UNESCO-EOLSS Publications (2010). 383–93.
23. Grace, D. Food safety in low and middle-income countries. Int J Environ Res Public Health. (2015) 12:10490–507. doi: 10.3390/ijerph120910490
24. Hutton, G, and Chase, C. The knowledge base for achieving the sustainable development goal targets on water supply, sanitation, and hygiene. Int J Environ Res Public Health. (2016) 13:536. doi: 10.3390/ijerph13060536
25. Lelieveld, H, Holah, J, and Gabric, D. Handbook of hygiene control in the food industry. Cambridge, UK: Woodhead Publishing (2016).
26. Soon, JM, Baines, R, and Seaman, P. Meta-analysis of food safety training on hand hygiene knowledge and attitudes among food handlers. J Food Prot. (2012) 75:793–804. doi: 10.4315/0362-028X.JFP-11-502
27. WHO. Guidelines for drinking-water quality: Incorporating the first and second addenda. Geneva: World Health Organization (2022).
28. United States Department of Agriculture (2023). Cold food storage charts. Available online at: https://www.foodsafety.gov/food-safety-charts/cold-food-storage-charts (Accessed on 23 Jan. 2025).
29. United States Department of Agriculture. (2024). Food safety during a power outage. Available online at: https://www.foodsafety.gov/food-safety-charts/food-safety-during-power-outage (Accessed on 23 Jan. 2025).
30. United States Department of Agriculture. (2024). Safe Minimum Internal Temperatures. Available online at: https://www.foodsafety.gov/food-safety-charts/safe-minimum-internal-temperatures (Accessed on 23 Jan. 2025).
31. Norris, MK. Everything worth preserving: The complete guide for food preservation at home. Stillwater, Minnesota, USA: Homestead Living (2023).
Keywords: cooking, food safety guidelines, food storage, hand washing, microbial contamination, mycotoxin, refrigeration, resource constrained household
Citation: Batch V, Kress M, Gama AP, Ng’ong’ola-Manani T, Chiutsi-Phiri G, Corner PL, Kumwenda S, Kaonga C, Kamndaya M, Monjerezi M, Leslie JF and Matumba L (2025) Perspectives on barriers to implementing WHO’s five keys to safer food in resource-limited rural areas of developing countries. Front. Nutr. 12:1524580. doi: 10.3389/fnut.2025.1524580
Received: 11 November 2024; Accepted: 19 February 2025;
Published: 04 March 2025.
Edited by:
Ricardo Assunção, Egas Moniz - Cooperativa de Ensino Superior, PortugalReviewed by:
Ana Rita Henriques, Egas Moniz School of Health and Science, PortugalCopyright © 2025 Batch, Kress, Gama, Ng’ong’ola-Manani, Chiutsi-Phiri, Corner, Kumwenda, Kaonga, Kamndaya, Monjerezi, Leslie and Matumba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Limbikani Matumba, bG1hdHVtYmFAbHVhbmFyLmFjLm13
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.