- Department of Urology, Shengzhou People’s Hospital (Shengzhou Branch of the First Affiliated Hospital of Zhejiang University School of Medicine, The Shengzhou People’s Hospital of Shaoxing University), Shengzhou, Zhejiang, China
Objective: The adherence to plant-based diets has been shown to positively impact longevity by reducing the incidence and severity of lifestyle-related diseases. Previous studies on the association of plant-based dietary pattern, as evaluated by plant-based dietary index (PDI), healthy plant-based dietary index (hPDI) and unhealthy plant-based dietary index (uPDI), with mortality risk have reported inconsistent results. We performed the present meta-analysis to summarize evidence on this association and to quantify the potential dose–response relationship based on all available cohort studies.
Methods: A comprehensive literature search and systematic review of relevant articles up to October 2024 was performed in PubMed and Scopus. The summary risk estimates (RR) with 95% confidence interval (CI) for the highest versus the lowest category of PDIs, hPDIs and uPDIs were calculated. Dose–response meta-analysis was also performed for studies reporting categorical risk estimates for at least three quantitative levels of PDIs, hPDIs and uPDIs.
Results: A total of 11 eligible cohort studies (13 datasets) were eventually included in this meta-analysis. Participants in the highest quintile of both the PDI and hPDI had a significantly decreased risk of all-cause mortality (pooled HRPDI = 0.85; 95% CI: 0.80–0.90; pooled HRhPDI = 0.86; 95% CI: 0.81–0.92) compared to participants in the lowest quintile. In contrast, the highest uPDI was associated with an increased risk of mortality (pooled HRuPDI = 1.20; 95% CI: 1.11–1.31). Dose–response meta-analysis showed that there was a non-linear relationship between PDI or hPDI level and all-cause mortality (p = 0.001 and p < 0.001 for non-linearity, respectively). No evidence of a non-linear relationship was observed for uPDI (p = 0.596 for non-linearity).
Conclusion: Greater adherence to PDI or hPDI dietary pattern was associated with a lower risk of mortality, whereas uPDI dietary pattern was positively associated with mortality risk. Thus, promoting a plant-based dietary pattern may be a key strategy in improving public health and reducing the burden of diet-related mortality.
Introduction
In recent years, life expectancy has generally increased worldwide, driven by advances in healthcare, improved living conditions, and vaccination efforts. However, significant disparities persist between high-income and low-income regions (1). While non-communicable diseases (NCDs) such as cardiovascular disease (CVD), cancer, and diabetes are the leading causes of death globally, low-income countries still face high mortality rates due to infectious diseases, malnutrition, and inadequate healthcare infrastructure (2, 3). Additionally, emerging challenges, including climate change, pandemics, and an aging population, continue to influence mortality patterns and present ongoing public health concerns (4–6).
Dietary patterns play a critical role in determining mortality risk, influencing both all-cause and cause-specific outcomes (7). Understanding the long-term effects of various dietary patterns on health outcomes is essential for developing effective nutritional guidelines that promote public health and reduce preventable mortality. Diets rich in fruits, vegetables, whole grains, and nuts have been consistently associated with reduced risks of CVD, cancer, and other NCDs, thereby contributing to lower mortality rates (8). Conversely, dietary patterns high in processed foods, red and processed meats, added sugars, and unhealthy fats are linked to increased morbidity and mortality due to their association with obesity, hypertension, dyslipidemia, and chronic inflammation (9).
The adherence to plant-based diets or those emphasizing nutrient-dense, minimally processed foods has been shown to positively impact longevity by reducing the incidence of lifestyle-related diseases (9). In recognition of its significance, plant-based dietary indexes (PDIs) were introduced in 2016 as a tool to link a plant-based dietary pattern to health outcomes (10). These indexes use a graded scoring system for various food items and include three categories: (1) plant-based diet index (PDI), which assesses the consumption of plant-based foods while reducing intake of animal-based foods; (2) healthful plant-based diet index (hPDI), which assigns positive scores to nutritious plant foods (like whole grains, fruits, vegetables, nuts, and legumes) and negative scores to less healthy plant foods (such as refined grains and potatoes), as well as to animal-based foods; (3) unhealthful plant-based diet index (uPDI), which gives positive scores to less healthy plant foods and negative scores to healthy plant foods and animal foods. Recently, various studies (11–14) have attempted to assess the associations between PDIs and mortality risk with inconclusive results. Due to this inconstancy, our objective was to conduct a systematic review and meta-analysis of prospective studies to investigate whether adherence to the PDIs is associated with the risk of mortality.
Methods
Publication search
A comprehensive literature search was conducted in the PubMed and Scopus databases for articles published up to October 2024. The search algorithm included terms such as (“plant-based diet” or “plant based diet”) and (“mortality” or “survival” or “death”). Relevant publications were initially screened based on their titles and abstracts, and all studies meeting the eligibility criteria were retrieved. Reference lists from selected articles and reviews were also checked to identify additional relevant studies. No language restrictions were applied. This systematic review and meta-analysis was conducted following established quality standards for reporting meta-analyses (15, 16).
Study selection
The included studies met the following criteria: (i) the primary exposure was the PDIs (i.e., PDI, hPDI and uPDI); (ii) the outcome of interest was all-cause and cause-specific mortality; (iii) the study used a prospective cohort design; and (iv) relative risk (RRs) with corresponding 95% confidence intervals (CIs) were reported or could be calculated. Studies were excluded if they were reviews, meta-analyses, case reports, or non-human studies. Additionally, studies focusing on other exposures or diseases were not considered. If multiple studies reported data based on the same population, the publication with the largest sample size and longest follow-up was included in our meta-analysis.
Data extraction
Data extraction was conducted independently by two authors (Q.M. and X.Z.) using a predefined extraction form. From each study, the following information was collected: first author’s name, publication year, study location, study name, study population, sample size (number of participants and cases), participants’ age, dietary assessment, adjusted effect estimates for all exposure categories, and covariates considered in study design or data analysis.
Quality assessment
The quality of each study was independently evaluated by two authors (Q.M. and X.Z.) using the Newcastle-Ottawa Scale (NOS)1. Any disagreements were resolved through a joint review with a third author. The NOS assigns up to nine points per study, with scores of less than 8 indicating lower quality and scores of 8 or higher indicating high quality.
Statistical methods
The main outcome of our study was all-cause mortality. We also included information on CVD and cancer, which were the leading causes of death worldwide. The strength of the relationship between PDIs and mortality risk was measured using a pooled adjusted RR and its 95% CI estimated by a DerSimonian and Laird random effects model (17). Comparisons were made between the highest and lowest PDI score categories to assess the all-cause and cause-specific mortality risk.
A dose–response meta-analysis followed the methods of Greenland and Longnecker (18) and Orsini et al. (19). We included studies that provided at least three quantitative categories with the number of cases and person-years for each. For studies that only reported overall person-years, we estimated the distribution using the approach of Aune et al. (20). Median or midpoint values for each category were used to represent the dose. If the upper boundary of the highest category was unavailable, we estimated it based on the nearest category. To explore a potential non-linear dose–response relationship between PDIs and mortality, we used restricted cubic splines, with knots placed at the 25th, 50th, and 75th percentiles of the distribution (21). Non-linearity was tested by checking if the second spline’s coefficient was zero.
We assessed study heterogeneity using the Q statistic and the I2 score (22), with heterogeneity defined as low (I2 < 25%), moderate (I2 = 25–50%), or high (I2 > 50%). Meta-regression analysis explored possible sources of heterogeneity, and subgroup analyses were performed based on study region, sample size, and follow-up duration. Sensitivity analysis involved repeating the meta-analysis, excluding each study one by one. Potential publication bias was checked using Begg’s test (rank correlation method) (23) and Egger’s test (linear regression method) (24). All statistical analyses were conducted in STATA 12.0 (StataCorp, College Station, TX), with two-sided p-values.
Results
Literature search and study characteristics
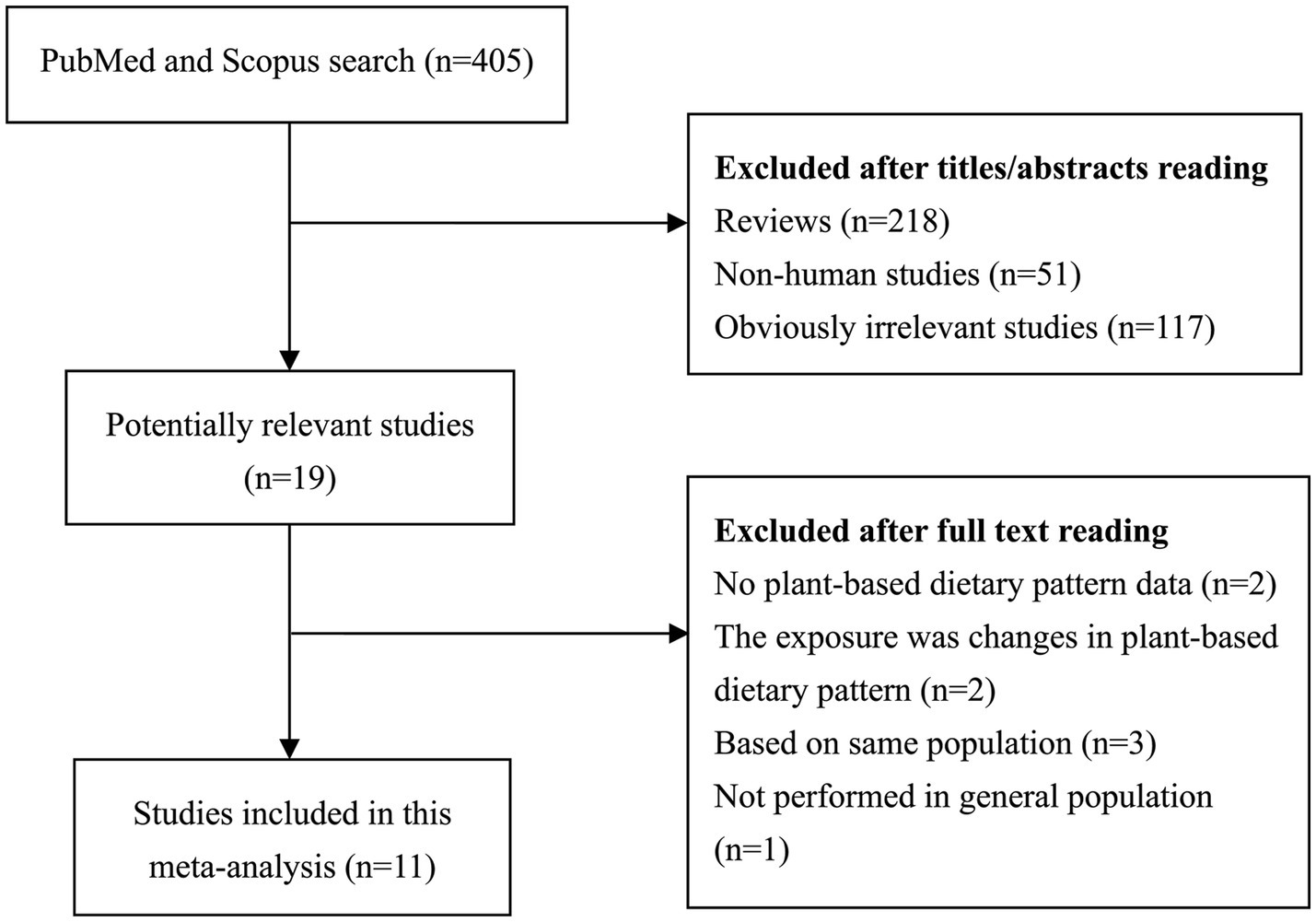
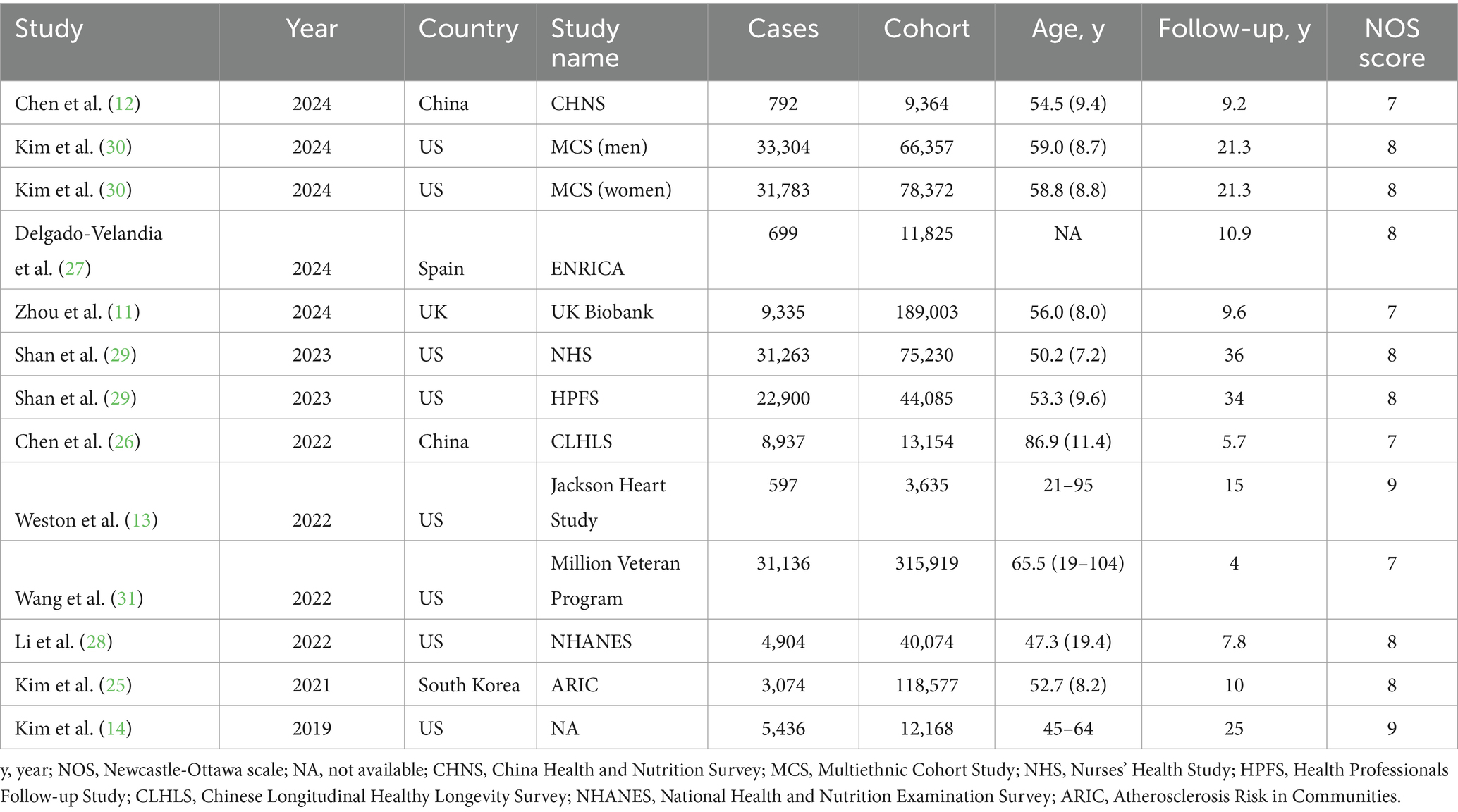
Figure 1 presents the detailed process of literature review. A total of 11 eligible cohort studies (13 datasets) (11–14, 25–31) were eventually included in this meta-analysis aimed to comprehensively evaluate the relationship between PDIs and mortality risk. These studies were performed in Asia (n = 3), North America (n = 6), and Europe (n = 2). 977,763 participants were included in these studies published between 2019 and 2024. There were 184,160 death events, which was mainly confirmed by linking to National Death Index. Table 1 summaries the main characteristics of all included studies analyzed in this meta-analysis. NOS scores ranged from 7 to 9, with a median value of 8 (Supplementary Table S1).
Main analyses
Participants in the highest quintile of both the PDI and hPDI had a significantly decreased risk of all-cause mortality (Figure 2, pooled HRPDI = 0.85; 95% CI: 0.80–0.90; pooled HRhPDI = 0.86; 95% CI: 0.81–0.92) compared to participants in the lowest quintile. In contrast, the highest uPDI was associated with an increased risk of mortality (pooled HRuPDI = 1.20; 95% CI: 1.11–1.31). In terms of the cause-specific mortality, comparing the highest versus lowest quintiles of the scores, greater adherence to PDI and hPDI was associated with a 19% (Table 2, HR = 0.81, 95% CI: 0.76–0.86) and 17% (HR = 0.83, 95% CI: 0.75–0.92) lower risk of CVD mortality, respectively. In contrast, an increased risk of CVD mortality was observed for uPDI (HR = 1.19, 95% CI: 1.07–1.32). A higher PDI was also associated with a lower risk of death from cancer (HR = 0.86, 95% CI: 0.77–0.96). However, the associations of cancer mortality with hPDI and uPDI were not statistically significant (Table 2).
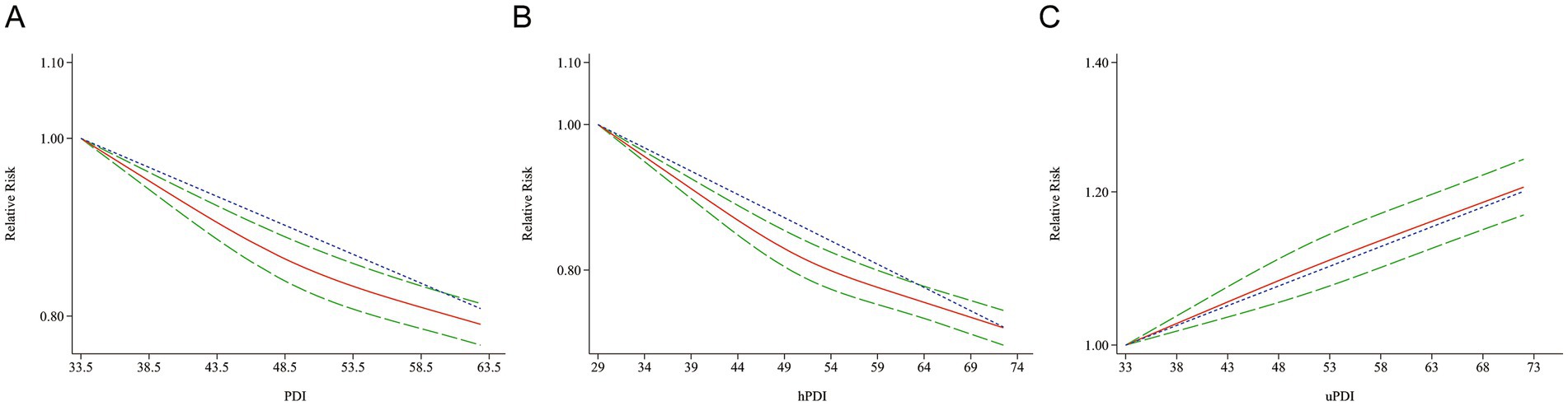
Figure 2. Risk of PDI (A), hPDI (B), and uPDI (C) associated with all-cause mortality. Weights are from random effects analysis. RR, relative risk; CI, confidence interval.
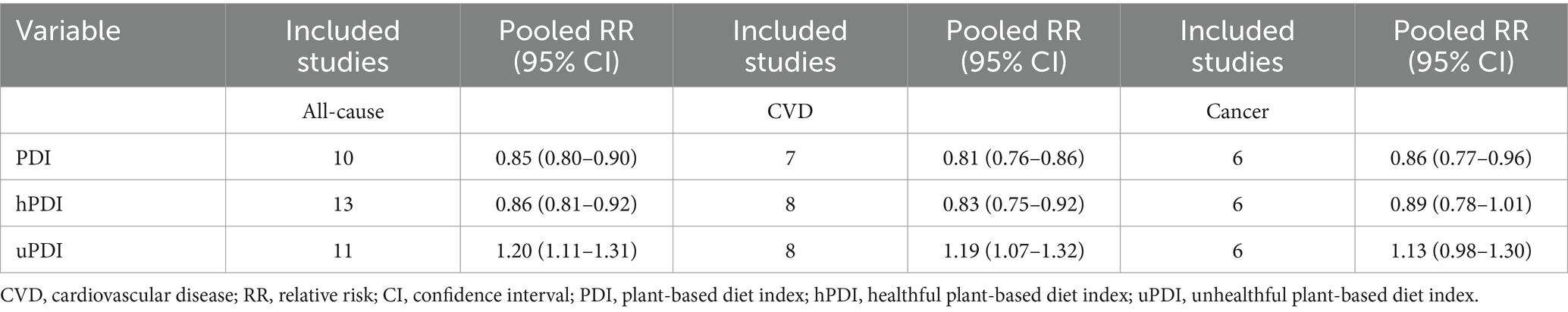
Table 2. Associations between plant-based diet pattern and all-cause and cause-specific mortality risk.
Additional analyses
We performed subgroup analyses for all-cause mortality based on geographical region (Europe vs. North America vs. Asia), number of participants (≥50,000 vs. <50,000), and duration of follow-up (≥10 years vs. <10 years). No significant interactions were observed for these factors in most analyses based on meta-regression models, except for follow-up year in uPDI analysis (Table 3). Sensitivity analysis was performed by ruling out each study in turn and repeating the meta-analysis for all-cause mortality. The association remained statistically significant after omitting any individual studies (Supplementary Figure S1). There was no obvious evidence of publication bias as shown in Begg’s funnel plot (Supplementary Figure S2). Dose–response meta-analysis showed that there was a non-linear relationship between PDI or hPDI level and all-cause mortality (Figure 3, p = 0.001 and p < 0.001 for non-linearity, respectively). No evidence of a non-linear relationship was observed for uPDI (p = 0.596 for non-linearity).
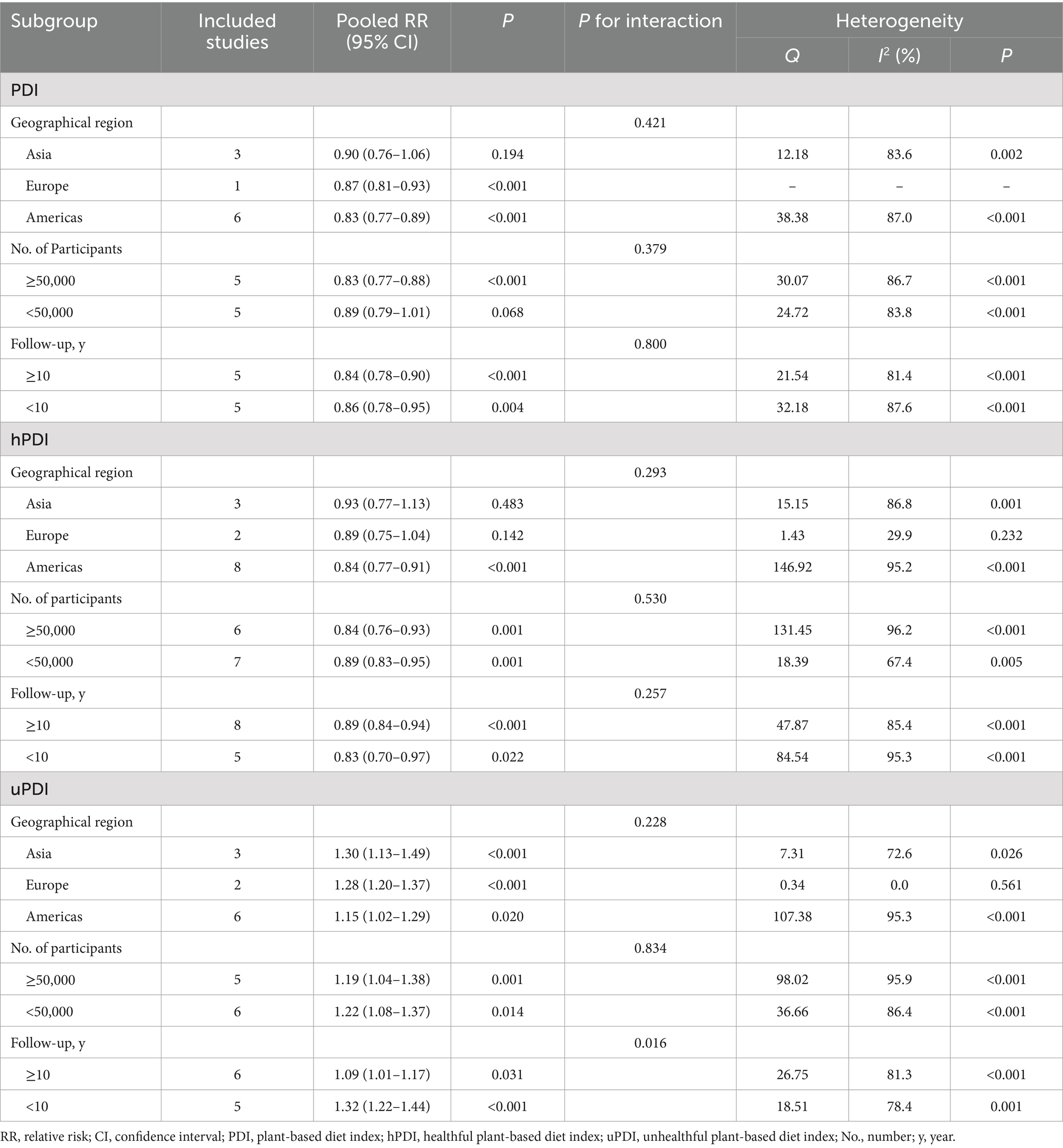
Table 3. Subgroup analyses of the association between plant-based diet pattern and all-cause mortality risk.
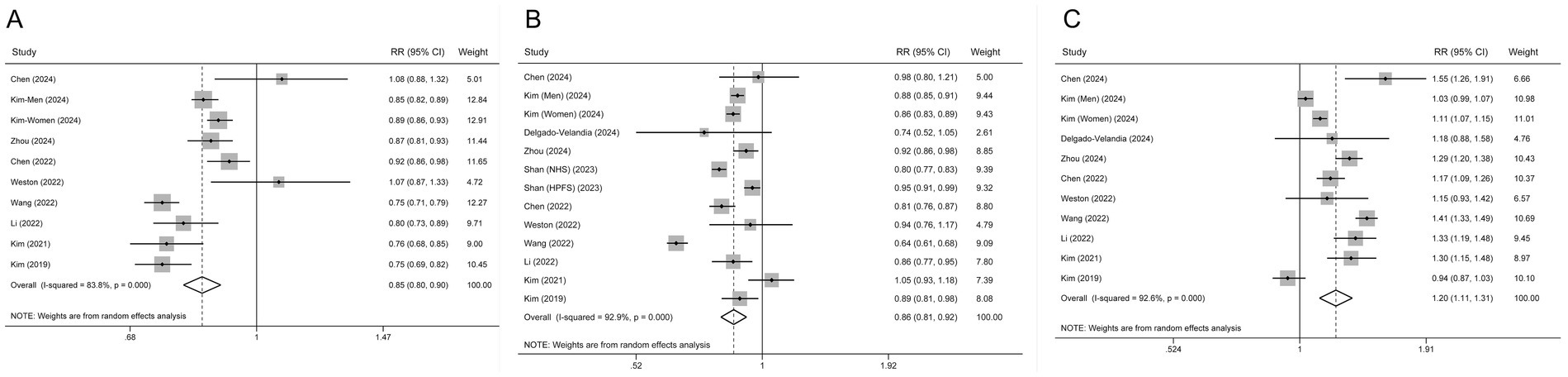
Figure 3. Dose–response associations between PDI (A), hPDI (B) and uPDI (C) and relative risk for all-cause mortality. Red solid line and green dash lines represent point estimates and 95% confidence intervals for non-linear analysis; blue dash line represents point estimates for linear analysis.
Discussion
This comprehensive meta-analysis of cohort studies showed that higher adherence to a PDI and hPDI dietary pattern was linked to a reduced risk of overall mortality. In contrast, greater adherence to an uPDI was associated with an increased risk of all-cause mortality. A similar pattern emerged for CVD mortality. Our findings suggest that a plant-based diet-low in animal foods, sugary drinks, refined grains, and fruit juices-correlates with lower risks of both all-cause and CVD mortality. To our knowledge, this is the first meta-analysis to evaluate the impact of PDIs on mortality risk.
Our study strengthens the evidence supporting a beneficial link between plant-based diets, including healthful plant-based foods, and reduced mortality. We also highlight the increased risk of mortality associated with frequent consumption of unhealthful plant-based foods. A plant-based diet refers to an eating pattern that prioritizes foods derived from plants. It can vary in its degree of restriction and may not necessarily exclude animal products completely. Healthful plant-based foods refer specifically to the quality and nutritional value of the foods within the plant-based spectrum. Our findings emphasize that the quality of plant foods is just as important as the quantity of plant-based foods.
Several mechanisms may explain the potential associations between adherence to a plant-based diet or a healthy plant-based pattern and lower risk of mortality. Diets emphasizing whole plant foods, including fruits, vegetables, legumes, whole grains, nuts, and seeds, are rich in essential nutrients, antioxidants, and dietary fiber, which collectively contribute to a lower risk of chronic diseases such as CVD, diabetes, and certain cancers (32–34). Moreover, plant-based diets are associated with improved metabolic markers, reduced inflammatory markers, and healthier lipid profiles, all of which are critical in reducing the risk of premature death (35–37). On the other hand, diets low in plant-based components and high in animal products, particularly red and processed meats, have been correlated with higher mortality risk (38, 39).
A non-significant association between both the hPDI and uPDI and cancer mortality was observed in our study. This was unexpected, as previous research has linked high fiber intake and reduced consumption of red and processed meats with a lower risk of cancer mortality (40, 41). One explanation for this null association could be inaccuracies in the cause-of-death information on death certificates, especially concerning cancer. Another possibility is that participants diagnosed with cancer may have changed their dietary habits after their diagnosis. Furthermore, the presence of associations may vary depending on the specific type of cancer mortality being studied (42).
Our meta-analysis has several strengths. First, it included a large sample size and had substantial statistical power, with only prospective studies considered. Second, the methodological quality of the included studies was generally high, as assessed by the NOS. Third, we conducted both categorical and dose–response analyses, which enhanced the robustness and reliability of the results. Lastly, the PDI scores in each study were calculated using a consistent methodology, enhancing the comparability of the studies.
However, some limitations should be noted. First, while no significant publication bias was detected through Begg’s and Egger’s tests, there is still the possibility of bias, as smaller studies with null results may be less likely to be published. Second, variations in dietary assessment methods and cut-off points across the included studies could have affected the pooled results. Third, significant heterogeneity among the studies may reduce the overall strength of our conclusions. Lastly, meta-analyses may not fully address confounding factors that are present in the studies they include. The potential for unmeasured or residual confounding remains, which could influence the outcomes and limit the ability to draw definitive conclusions.
In conclusion, greater adherence to a PDI or hPDI dietary pattern was associated with a lower risk of all-cause and CVD mortality, whereas uPDI dietary pattern was negatively associated with mortality risk. Thus, promoting a plant-based dietary pattern may be a key strategy in improving public health and reducing the burden of diet-related mortality.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
QM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft. JW: Formal analysis, Investigation, Methodology, Writing – original draft. YL: Data curation, Formal analysis, Investigation, Writing – review & editing. XZ: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1518519/full#supplementary-material
Footnotes
References
1. Galvani-Townsend, S, Martinez, I, and Pandey, A. Is life expectancy higher in countries and territories with publicly funded health care? Global analysis of health care access and the social determinants of health. J Glob Health. (2022) 12:04091. doi: 10.7189/jogh.12.04091
2. Gowshall, M, and Taylor-Robinson, SD. The increasing prevalence of non-communicable diseases in low-middle income countries: the view from Malawi. Int J Gen Med. (2018) 11:255–64. doi: 10.2147/ijgm.s157987
3. Boutayeb, A, and Boutayeb, S. The burden of non-communicable diseases in developing countries. Int J Equity Health. (2005) 4:2. doi: 10.1186/1475-9276-4-2
4. Liao, H, Lyon, CJ, Ying, B, and Hu, T. Climate change, its impact on emerging infectious diseases and new technologies to combat the challenge. Emerg Microbes Infect. (2024) 13:2356143. doi: 10.1080/22221751.2024.2356143
5. Sarkar, SM, Dhar, BK, Fahlevi, M, Ahmed, S, Hossain, MJ, Rahman, MM, et al. Climate change and aging health in developing countries. Glob Chall. (2023) 7:2200246. doi: 10.1002/gch2.202200246
6. Global age-sex-specific mortality. Life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950-2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the global burden of disease study 2021. Lancet. (2024) 403:1989–2056. doi: 10.1016/s0140-6736(24)00476-8
7. English, LK, Ard, JD, Bailey, RL, Bates, M, Bazzano, LA, Boushey, CJ, et al. Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open. (2021) 4:e2122277. doi: 10.1001/jamanetworkopen.2021.22277
8. Aune, D. Plant foods, antioxidant biomarkers, and the risk of cardiovascular disease, cancer, and mortality: a review of the evidence. Adv Nutr. (2019) 10:S404–21. doi: 10.1093/advances/nmz042
9. Dicken, SJ, and Batterham, RL. The role of diet quality in mediating the association between ultra-processed food intake, obesity and health-related outcomes: a review of prospective cohort studies. Nutrients. (2021) 14:23. doi: 10.3390/nu14010023
10. Satija, A, Bhupathiraju, SN, Rimm, EB, Spiegelman, D, Chiuve, SE, Borgi, L, et al. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med. (2016) 13:e1002039. doi: 10.1371/journal.pmed.1002039
11. Zhou, L, Zhang, R, Yang, H, Zhang, S, Zhang, Y, Li, H, et al. Association of plant-based diets with total and cause-specific mortality across socioeconomic deprivation level: a large prospective cohort. Eur J Nutr. (2024) 63:835–46. doi: 10.1007/s00394-023-03317-3
12. Chen, H, Wang, X, Ji, JS, Huang, L, Qi, Y, Wu, Y, et al. Plant-based and planetary-health diets, environmental burden, and risk of mortality: a prospective cohort study of middle-aged and older adults in China. Lancet Planet Health. (2024) 8:e545–53. doi: 10.1016/s2542-5196(24)00143-8
13. Weston, LJ, Kim, H, Talegawkar, SA, Tucker, KL, Correa, A, and Rebholz, CM. Plant-based diets and incident cardiovascular disease and all-cause mortality in African Americans: a cohort study. PLoS Med. (2022) 19:e1003863. doi: 10.1371/journal.pmed.1003863
14. Kim, H, Caulfield, LE, Garcia-Larsen, V, Steffen, LM, Coresh, J, and Rebholz, CM. Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. J Am Heart Assoc. (2019) 8:e012865. doi: 10.1161/jaha.119.012865
15. McShane, LM, Altman, DG, Sauerbrei, W, Taube, SE, Gion, M, and Clark, GM. REporting recommendations for tumour MARKer prognostic studies (REMARK). Br J Cancer. (2005) 93:387–91. doi: 10.1038/sj.bjc.6602678
16. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
17. DerSimonian, R, and Laird, N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
18. Greenland, S, and Longnecker, MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. (1992) 135:1301–9. doi: 10.1093/oxfordjournals.aje.a116237
19. Orsini, N, Li, R, Wolk, A, Khudyakov, P, and Spiegelman, D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. (2012) 175:66–73. doi: 10.1093/aje/kwr265
20. Aune, D, Greenwood, DC, Chan, DS, Vieira, R, Vieira, AR, Navarro, DA, et al. Body mass index, abdominal fatness and pancreatic cancer risk: a systematic review and non-linear dose-response meta-analysis of prospective studies. Ann Oncol. (2012) 23:843–52. doi: 10.1093/annonc/mdr398
21. Harre, F, Lee, KL, and Pollock, BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. (1988) 80:1198–202. doi: 10.1093/jnci/80.15.1198
22. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
23. Begg, CB, and Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
24. Egger, M, Smith, G, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
25. Kim, J, Kim, H, and Giovannucci, EL. Plant-based diet quality and the risk of total and disease-specific mortality: a population-based prospective study. Clin Nutr. (2021) 40:5718–25. doi: 10.1016/j.clnu.2021.10.013
26. Chen, H, Shen, J, Xuan, J, Zhu, A, Ji, JS, Liu, X, et al. Plant-based dietary patterns in relation to mortality among older adults in China. Nat Aging. (2022) 2:224–30. doi: 10.1038/s43587-022-00180-5
27. Delgado-Velandia, M, Maroto-Rodríguez, J, Ortolá, R, García-Esquinas, E, Rodríguez-Artalejo, F, and Sotos-Prieto, M. Plant-based diets and all-cause and cardiovascular mortality in a Nationwide cohort in Spain: the ENRICA study. Mayo Clin Proc. (2022) 97:2005–15. doi: 10.1016/j.mayocp.2022.06.008
28. Li, H, Zeng, X, Wang, Y, Zhang, Z, Zhu, Y, Li, X, et al. A prospective study of healthful and unhealthful plant-based diet and risk of overall and cause-specific mortality. Eur J Nutr. (2022) 61:387–98. doi: 10.1007/s00394-021-02660-7
29. Shan, Z, Wang, F, Li, Y, Baden, MY, Bhupathiraju, SN, Wang, DD, et al. Healthy eating patterns and risk of Total and cause-specific mortality. JAMA Intern Med. (2023) 183:142–53. doi: 10.1001/jamainternmed.2022.6117
30. Kim, J, Wilkens, LR, Haiman, CA, Le Marchand, L, and Park, SY. Plant-based dietary patterns and mortality from all causes, cardiovascular disease, and cancer: the multiethnic cohort study. Clin Nutr. (2024) 43:1447–53. doi: 10.1016/j.clnu.2024.04.035
31. Wang, DD, Li, Y, Nguyen, XT, Song, RJ, Ho, YL, Hu, FB, et al. Degree of adherence to plant-based diet and total and cause-specific mortality: prospective cohort study in the million veteran program. Public Health Nutr. (2023) 26:381–92. doi: 10.1017/s1368980022000659
32. Goñi, I, and Hernández-Galiot, A. Intake of nutrient and non-nutrient dietary antioxidants. Contribution of macromolecular antioxidant polyphenols in an elderly Mediterranean population. Nutrients. (2019) 11:2165. doi: 10.3390/nu11092165
33. Threapleton, DE, Greenwood, DC, Evans, CE, Cleghorn, CL, Nykjaer, C, Woodhead, C, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. (2013) 347:f6879. doi: 10.1136/bmj.f6879
34. Lattimer, JM, and Haub, MD. Effects of dietary fiber and its components on metabolic health. Nutrients. (2010) 2:1266–89. doi: 10.3390/nu2121266
35. Munteanu, C, and Schwartz, B. Interactions between dietary antioxidants, dietary Fiber and the gut microbiome: their putative role in inflammation and Cancer. Int J Mol Sci. (2024) 25:8250. doi: 10.3390/ijms25158250
36. Wiśniewska, K, Okręglicka, KM, Nitsch-Osuch, A, and Oczkowski, M. Plant-based diets and metabolic syndrome components: the questions that still need to be answered-a narrative review. Nutrients. (2024) 16:165. doi: 10.3390/nu16010165
37. Thomas, MS, Calle, M, and Fernandez, ML. Healthy plant-based diets improve dyslipidemias, insulin resistance, and inflammation in metabolic syndrome. A narrative review. Adv Nutr. (2023) 14:44–54. doi: 10.1016/j.advnut.2022.10.002
38. Wang, X, Lin, X, Ouyang, YY, Liu, J, Zhao, G, Pan, A, et al. Red and processed meat consumption and mortality: dose-response meta-analysis of prospective cohort studies. Public Health Nutr. (2016) 19:893–905. doi: 10.1017/s1368980015002062
39. Zheng, Y, Li, Y, Satija, A, Pan, A, Sotos-Prieto, M, Rimm, E, et al. Association of changes in red meat consumption with total and cause specific mortality among US women and men: two prospective cohort studies. BMJ. (2019) 365:l2110. doi: 10.1136/bmj.l2110
40. Ramezani, F, Pourghazi, F, Eslami, M, Gholami, M, Mohammadian Khonsari, N, Ejtahed, HS, et al. Dietary fiber intake and all-cause and cause-specific mortality: an updated systematic review and meta-analysis of prospective cohort studies. Clin Nutr. (2024) 43:65–83. doi: 10.1016/j.clnu.2023.11.005
41. Huang, Y, Cao, D, Chen, Z, Chen, B, Li, J, Guo, J, et al. Red and processed meat consumption and cancer outcomes: umbrella review. Food Chem. (2021) 356:129697. doi: 10.1016/j.foodchem.2021.129697
Keywords: plant-based diet, mortality, cardiovascular disease, cancer, cohort, meta-analysis
Citation: Mo Q, Wu J, Lu Y and Zhang X (2025) Plant-based diets and total and cause-specific mortality: a meta-analysis of prospective studies. Front. Nutr. 12:1518519. doi: 10.3389/fnut.2025.1518519
Edited by:
José María Huerta, Carlos III Health Institute (ISCIII), SpainReviewed by:
Margherita Springer, Max Planck Institute of Psychiatry (MPI), GermanyDavid Goldman, University of Helsinki, Finland
Copyright © 2025 Mo, Wu, Lu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiao Zhang, emhhbmd4aWFvMjAyNDEwQHNpbmEuY29t
 Qiwang Mo
Qiwang Mo Xiao Zhang
Xiao Zhang