- 1Department of Pediatrics and Child Health Nursing, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
- 2Department of Emergency and Critical Care Nursing, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
Introduction: Lactation is the critical time for meeting the nutritional demands of mothers and infants. Mothers from low-income countries, including Ethiopia, are considered nutritionally vulnerable. Good dietary practices for mothers during lactation are therefore important for the good health of their children. The main objective of this study was to assess dietary practice and associated factors of lactating mothers in Dangila Zuria District, Amhara region, Ethiopia, 2022.
Methods: A community-based cross-sectional study was conducted among 609 lactating women from March 1st to May 1st 2022. The study participants were selected using a straightforward simple random sampling techniques. Data was collected by using structured questionnaires. The data was entered in Epi-data and exported to SPSS version 23 for analysis. Bi-variable and multi-variable logistic regression analyses were used to see the relevant associations. The variable significantly associated with dietary practice was identified based on a P-value ≤ 0.05.
Results: This study revealed that only one-third 204 lactating mothers, demonstrated good dietary practices. Notably, several factors were significantly associated with poor dietary practices: mothers with a family size greater than four had 3.01 times higher odds of inadequate dietary habits (AOR = 3.01; 95% CI: 1.56, 9.28), while those with birth intervals of <2 years faced 2.31 times greater odds (AOR = 2.31; 95% CI: 1.49, 3.56). Additionally, daily laborers exhibited a striking 9.35 times higher likelihood of poor dietary practices (AOR = 9.35; 95% CI: 8.02, 19.96), and food-insecure mothers had 4.93 times higher odds of inadequate nutrition (AOR = 4.93; 95% CI: 3.40, 7.16).
Conclusion: In conclusion, the dietary practices of lactating mothers were found to be suboptimal, falling below WHO and FAO recommendations. Factors such as family size, birth intervals, maternal occupation (especially daily laborers), and food insecurity were identified as significant contributors. Addressing these issues is crucial. Key stakeholders, including the Ministry of Health (MOH), Regional Health Bureaus (RHB), and health professionals, must work together to alleviate food insecurity, promote optimal family planning, and educate mothers on proper nutrition. Addressing these challenges is essential to achieving global objectives such as reducing malnutrition, improving maternal health, and ensuring healthy child development.
1 Introduction
1.1 Background
The lactation period refers to the time during which the mammalian produces milk to feed their young (1). Lactation itself is the physiological process of milk production, which is stimulated by hormones such as prolactin and oxytocin (2). During the lactation time, the mother's body changes to produce milk in response to the baby's suckling. Proper nutrition and hydration are required to maintain the milk supply of the mothers. Access to good dietary practices is fundamental to the survival of lactating mothers as well as the newborn's good growth and development (1). Maternal health during lactation is crucial, not just for individual women but also for their newborns and families (3). In low and middle-income countries like Ethiopia, women of reproductive age often face nutritional vulnerabilities that can adversely affect their wellbeing and that of their newborns (4). Lactating mothers' dietary practices are influenced by a variety of factors, including cultural beliefs, socio-economic conditions, and access to healthcare, with significant global variation (5). While international guidelines recommend specific nutritional intake for lactating women, adherence to these recommendations often varies due to economic constraints, lack of education, and limited access to healthcare, especially in low-resource settings (6, 7). There are gaps in research regarding the impact of culturally specific dietary practices, the effectiveness of nutritional interventions, and the long-term effects of maternal diet on both maternal and infant health (8).
Good dietary practice is not simply two or more additional feedings than usual (9), but it includes a variety of food groups in the daily patterns, and women in low and middle-income countries, especially in our country Ethiopia, have a limited intake of animal sources foods, fruits, and vegetables, and their intake of micronutrients is less than the recommended values, which can increase women's risk of micronutrient deficiencies and their child's for poor growth and development with inadequate breast milk (10, 11). In general, good nutrition (good dietary practice) during pregnancy and lactation is the cornerstone for the survival, health, and development of current and succeeding generations. However, almost more than half of the lactating mothers do not consume the recommended dietary practice during this period and they face protein-energy malnutrition, nutritional anemia, vitamin A deficiency, and iodine deficiency disorders (IDD) (12, 13).
Dietary practices before and during pregnancy and lactation periods have been shown to induce long-term effects on the later health of the child, including the risk of common non-communicable diseases such as obesity, diabetes, and cardiovascular disease (14). Poor dietary practices and poor health from preventable causes disproportionately affect the wellbeing of millions of people in the developing world.
Poor dietary practices affect over 850 million people worldwide and 200 million adults in Sub-Saharan Africa (SSA), especially affecting children and their mothers Worldwide (15, 16).
More than 3.5 million women and children under the age of five in developing countries die each year due to the underlying cause of under-nutrition which is caused by poor dietary practices (17, 18). Studies show that lactating women from developing countries are vulnerable to poor dietary practices. This is true in our country: poor dietary practice is the leading cause of maternal and child malnutrition, which leads to poor secretion of nutrients in breast milk, and this can have a long-term impact on the child's growth and development (19–21). In general, to improve maternal health and their child's growth and development, it is important to know the burden of poor dietary practice and its associated factors. A study conducted in Tigray, Moyale District, Borena Zone, and Gondar showed that most lactating mother's dietary practices are below WHO and FAO recommendations (8, 22–24).
Despite the efforts of the government to improve nutrition, few studies done on maternal nutrition in the country revealed sub-optimal nutrient intakes of pregnant lactating women compared with the standard recommended by the WHO (25, 26). Only about few lactating women who attend antenatal care at public hospitals reported good dietary practices (27). Similarly, studies also identified education, monthly income, attitude, and gravidity as factors associated with the dietary practices of lactating women (28, 29).
According to current evidence, exclusive breastfeeding mothers are advised to consume an additional 300–500 calories per day or include 1–2 extra snacks to meet the increased nutritional demands of lactation, which are significantly higher than those during pregnancy or for non-pregnant women. However, in Ethiopia, many lactating mothers lack training or awareness about the importance of increasing meal frequency during this period (30, 31). The challenge to ensure consistent quality dietary practice for lactating mothers in Ethiopia is because half of the population is living below the food poverty line and cannot meet their daily minimum nutritional requirement (20, 32). Taking this into consideration, the Ethiopian government continuously showed its commitment to averting nutritional problems by developing food and nutrition policies, strategies, and programs targeted at improving the nutritional status of pregnant and lactating women and interventions had been going on through the routine health care services (33). Therefore, this study aimed to assess the dietary practices and associated factors among lactating women in the Awi Zone Dangila Zuria Woreda.
2 Methods
2.1 Study area and design
A community-based cross-sectional study was employed to assess dietary practice and associated factors among lactating mothers in Dangila Zuria Woreda, Awi Zone Ethiopia. The study was conducted in Dangila Zuria Woreda Northwest Ethiopia, from March 1st to May 1st in 2022.
Dangila Zuria Woreda is one of the eleventh Woreda in the Awi Zone of Amhara Regional State, which is located 485 km away from the capital, Addis Ababa, in the North West Ethiopia, and 78 km away from Bahir Dar the capital city of the region and 40 kms from the Zonal Capital city Injibara. Administratively, the district is structured into six clusters and according to the Ethiopian statistical service the population size of towns by sex, region, zone and woreda as of July 2021, the district, has a total population of 53,225 out of which 25,813 are females and 27,412 are males. The estimated number of lactating mothers in the district is 3,520. The district census which was obtained from the Woreda health office used as a baseline. The Woreda currently has one district hospital & 6 health centers, and 27 health posts. The major agricultural products are Teff, Dagussa, Maize, Potato, Sorghum, peas and beans, and some vegetables like cabbage, carrots tomatoes.
2.2 Source and study population
The source population for this study comprised all lactating mothers residing in the Dangila Zuria Woreda, with the study population specifically including those living in selected kebeles. The study unit consisted of mothers who were selected as samples and interviewed. Lactating mothers paired with a child under 2 years old who had lived in the Woreda for at least 6 months were included in the study, while lactating mothers who were critically ill and those whose children with critical illnesses were excluded from participation in the study.
2.3 Sample size determination
A single population proportion formula was used to determine the sample size, allowing for the estimation of a sufficient number of participants. The sample was calculated for both the dependent and independent variables taking the prevalence of poor dietary practices among lactating mothers as 71.2% for lactating mothers (8), by considering 5% marginal error, 95% CI, and 2 as the design effect, Based on this, the actual sample size were calculated using the formula for single population proportion.
Therefore;
Where Z = level of confidence at (1.96)2 95% CI
P = Single Population Proportion (71.2%).
d = Margin of error 5% (0.05).
n = Sample Size
When we considered the design effect of 2 for the assumption of multistage sampling, across the clusters, the total sample was 316 × 2 = 632.
2.4 Sampling procedures
We employed a multi-stage sampling technique to systematically select kebeles, households, and lactating mothers for our study. First, we focused on the Dangila District, which comprises 27 rural kebeles. To ensure a representative sample, we randomly selected six kebeles from the total kebeles using a lottery method, which helps eliminate bias in the selection process.
Once the kebeles were chosen, we allocated lactating mothers to each kebele based on the population size of the kebele, ensuring the representation was proportional and used to capture a diverse range of experiences and perspectives across different community sizes. Within each selected kebele, we then identified individual lactating mothers using simple random sampling.
2.5 Operational definition
Dietary practice: is an observable action or behavior of eating habits, food choices, and nutritional behaviors of women who are breastfeeding.
Poor dietary practice: lactating women who score below 50% for dietary practice-related questions in 24 h. Unhealthy eating habits can include inadequate caloric and nutrient intake (11).
Good dietary practice: lactating women who score above 50% for dietary practice-related questions in 24 h (11).
Adequate dietary diversity: refers to households consuming at least four different food groups within the 24 h before the survey.
Inadequate dietary diversity: when households consumed less than four food groups within 24 h before the survey.
Food insecurity: the limited or uncertain access to sufficient and nutritious food among lactating mothers, insufficient availability of food in the household, or disruptions in food supply.
2.6 Data collection procedures
A structured questionnaire that was given by an interviewer was used to collect data, which made it easier to compile information in an organized manner. Which comprised; socio-demographic characteristics, source of food, feeding practice and other individual-related factors; dietary diversity, and food security-related questions.
The questionnaire designed to assess the eating habits of lactating mothers was adapted from existing studies to better suit our local context. We included 11 questions to evaluate the dietary practices of lactating mothers. The dietary practice was assessed by using open-ended surveys such as dietary recalls or records, or using closed-ended surveys including food frequency questionnaires and we assessed the dietary practice by using the modified form of the nine-item scales taken from previous literature (23, 34). The items were focused on the short-term dietary practices of lactating mothers. The score of the respondents was taken and respondents were classified as having good or poor dietary practices by taking their responses ≥50% and <50%, respectively (8, 32).
The items had “Yes” or “No” responses. Lactating mothers who scored ≥50% for the responses were classified as having good dietary practice and poor dietary practice otherwise. The rest questioner was adapted and modified from WHO and other similar studies (8, 35). Five diploma nurses' data collectors and two BSc nurse supervisors participated in the data collection. The 2-day training was given to the data collectors and supervisors on the approach of data collection.
2.7 Data quality control
To ensure the integrity and accuracy of the data, all data collectors and supervisors underwent comprehensive orientation and training on the processes for reviewing and recording information, which aimed to minimize potential biases during the data collection. A pretest was conducted in Fagita Lokoma Woreda with a sample of 20 lactating mothers to evaluate the consistency and completeness of the data collection tools, allowing us to identify and address any issues before the main data collection commenced.
During the data collection period, close supervision and monitoring were implemented by both supervisors and the perinatal investigator. This involved regular check-ins and feedback sessions to reinforce proper data collection techniques and address any challenges that arose in real-time. After data collection, a thorough review was conducted by both the supervisor and the investigator to check for completeness and accuracy.
Any discrepancies or missing data were addressed promptly. Furthermore, data entry procedures were standardized, and validation checks were applied to identify potential errors.
2.8 Data processing and analysis
The data was coded and entered Epi-data then exported to SPSS software package version 23 for analysis. Percentages, frequency distributions, proportions, mean and range were done and used for describing descriptive data. Then bi-variable logistic regression was made to see the crude significant relation of each independent variable with dependent variables.
Finally, independent variables with P-value < 0.2 were entered into a multi-variable logistic regression to control the effect of confounding. An odds ratio with a 95% confidence interval to ascertain the association between the independent and dependent variables was used. A p-value of less than 5% was used to declare the association between factors and the dependent variable.
2.9 Ethical approval
The research was approved by the Institutional Review Board (IRB) at Bahir Dar University College of Medicine and Health Sciences. Ethical approval was granted on 6 September 2021, under protocol number 280/2021. The IRB thoroughly reviewed the study design to ensure it adhered to ethical standards, safeguarding the rights and wellbeing of all participants. All experiments were conducted in strict accordance with relevant national and international ethical guidelines, including the Declaration of Helsinki and the Ethiopian National Guidelines for Biomedical Research. These guidelines were followed to minimize harm to participants and maintain the integrity of the research. Informed consent was obtained from all participants prior to the start of the study. Participants were provided with detailed information about the study's objectives, procedures, potential risks, and their rights. Written informed consent was obtained from all participants, ensuring their participation was voluntary and based on a clear understanding of the study.
3 Results
3.1 Socio-demographic characteristics
In this comprehensive study of 609 lactating mothers aged 15–49 years, an impressive response rate of 96.36% was recorded. A significant majority, of lactating mothers (79.8%) identified as part of the Amhara ethnic group. Nearly half (47.8%) of lactating mothers were aged 25–34 years, and a substantial 61.9% were unable to read or write.
Most participants (77.8%) of lactating mothers were housewives in their occupational status, while over two-thirds (69.8%) of their husbands were engaged in farming and nearly half (47.6%) of the husbands were also illiterate. Financially, a large portion of the lactating mothers (88.2%) reported a monthly income between 1,000 and 2,000 Ethiopian Birr, and more than two-thirds (65.2%) lived in households with 4–6 family members. Of the total two-thirds (64.9%) of lactating mothers practiced Orthodox Christianity. Additionally, over half (54.4%) of the lactating mothers reported that a birth interval >2 years (Table 1).
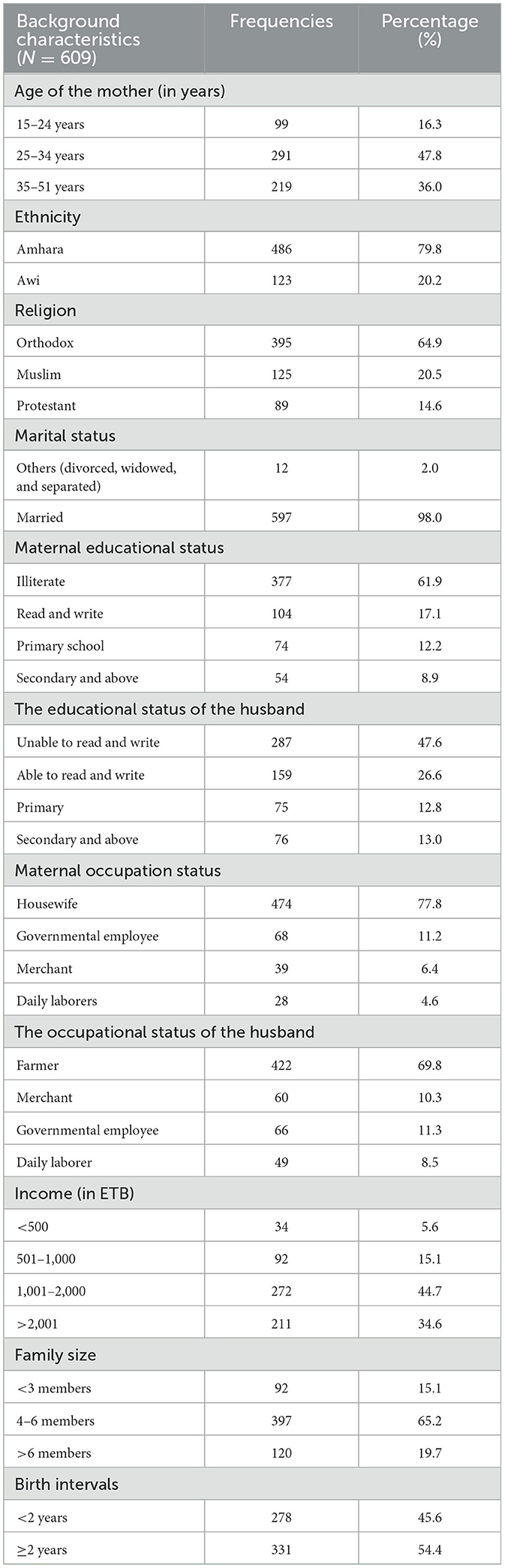
Table 1. Socio-demographic and economic-related characteristics of lactating mothers at Dangila Zuria District Awi Zone, Amhara region, Ethiopia, 2022.
3.2 Health service utilization and child feeding
Six hundred eight (99.8%) study participants had ANC follow-up. Of them majority of mothers had more than three follow-up visits in the last pregnancy. Almost all lactating mothers didn't suffer from any chronic illnesses during their breastfeeding period.
However, 21 (3.4%) mothers had a history of illness in the last 2 weeks. Nearly all (98.7%) study participants reported that they gave birth at a health facility. All mothers also reported that they have practiced exclusive breastfeeding (Table 2).
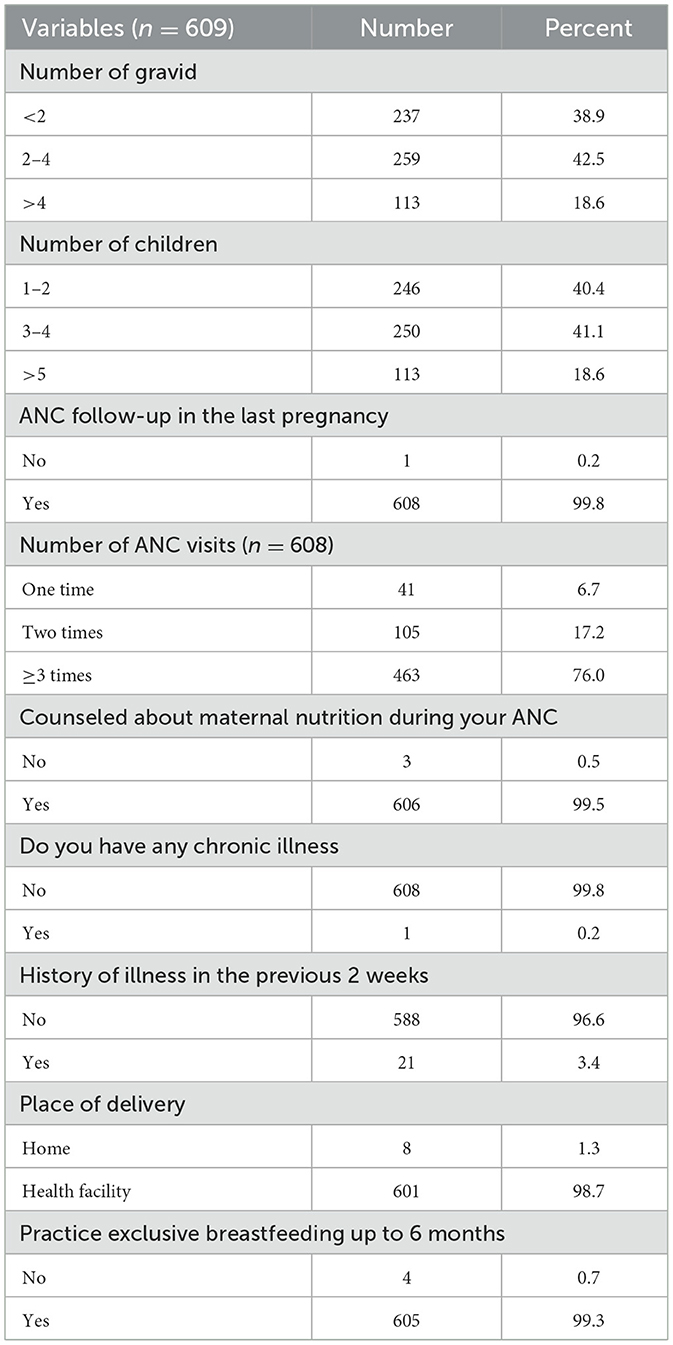
Table 2. Health service utilization and child feeding of lactating mothers at Dangila Zuria District Awi Zone, Amhara region, Ethiopia, 2022.
3.3 Dietary practices
The majority of lactating women (83.1%) reported that the main source of their food was their production. Similarly, 502 (82.4%) respondents practice home gardening. The majority of the respondents (71.1%) had a habit of jumping their usual feeding practices. Most of the respondents (88.7%) have eaten additional foods during their lactation period. More than half of the participants (52.1%) reported that they feed more than three times per day.
The majority of the study participants had no history of fasting in the last 24 h. The majority (92.8%) of participants had a habit of eating snacks in the previous 24 h. In general, 204 (33.5%) lactating mothers have good dietary practices (Table 3).
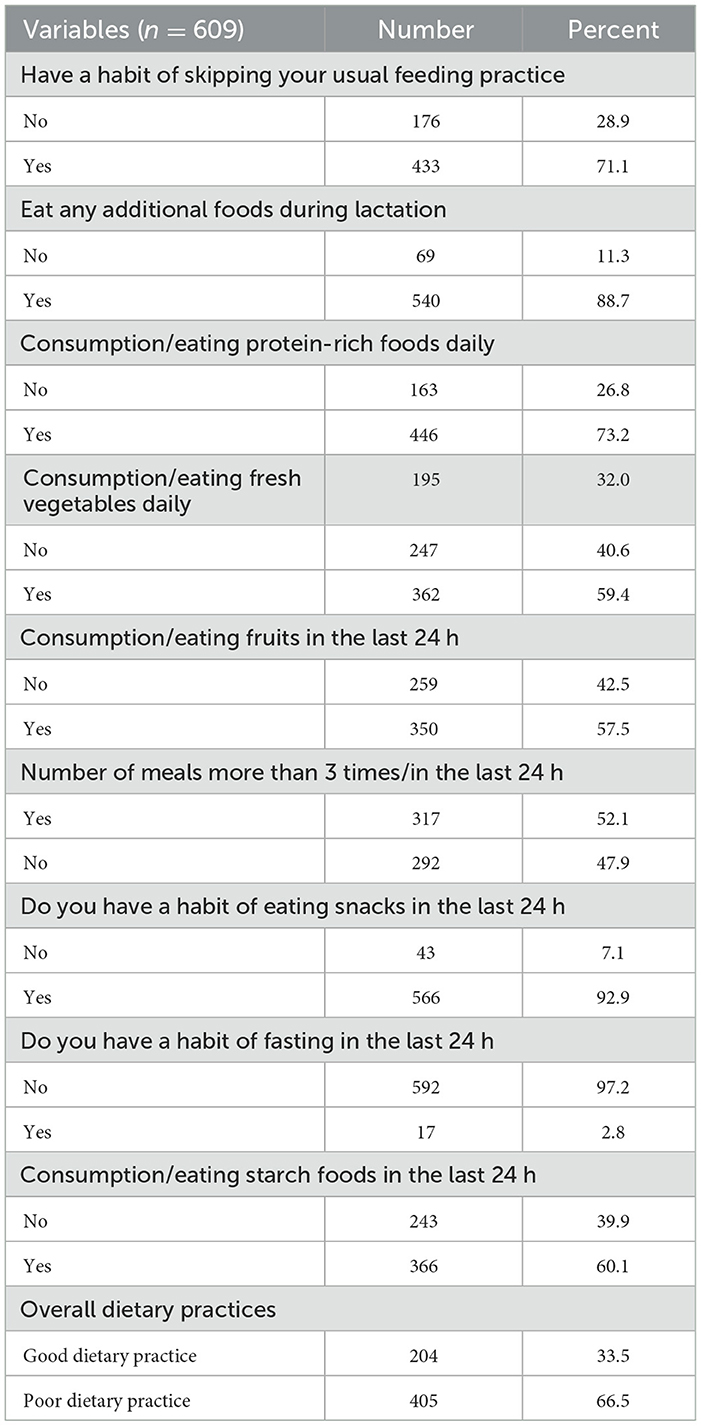
Table 3. Source of food and dietary practices among lactating mothers at Dangila Zuria District Awi Zone, Amhara region, Ethiopia, 2022.
3.4 Dietary diversity
Based on the dietary diversity score of lactating mothers, about three-fourths of the lactating women (73.2%) reported that they consumed grains, white roots and tubers, and plantains in the previous 24 h. Three-hundred sixty-six (60.1%) respondents reported that they consumed pulses (beans, peas, and lentils) in the last 24 h. Similarly, more than half of the lactating mothers consume vitamin A-rich fruits and vegetables in 24 h. Only 139 (22.8%) of the respondents consumed meat, poultry, and fish in the 24 h. In general, 455 (74.7%) lactating mothers have good dietary diversity scores in the previous 24 h (Table 4).
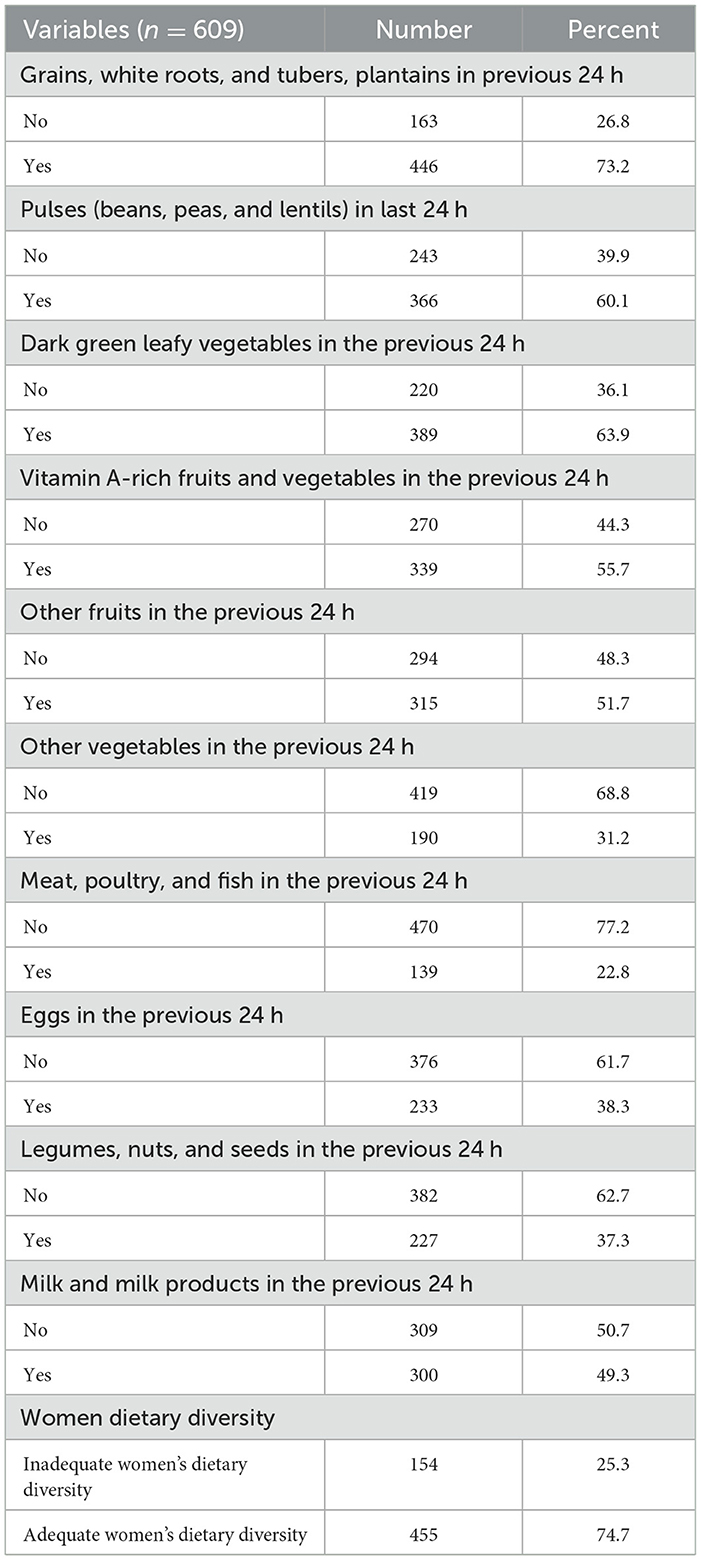
Table 4. Dietary diversity among lactating mothers at Dangila Zuria District Awi Zone, Amhara region, Ethiopia, 2022.
3.5 Food security characteristics
From the 9 HFIAS items; the most frequently reported experience of food insecurity was skipping meals (27.4%) followed by worrying about running out of food (25.8%), and being unable to eat preferred foods (25.1%). Overall, nearly one-third (29.7%) of the lactating mothers were food secure (Table 5).

Table 5. HFIAS items among lactating mothers at Dangila Zuria District Awi Zone, Amhara region, Ethiopia, 2022.
3.6 Factors associated with lactating women's dietary practice
Table 6 shows a bi-variable and multivariate analysis of factors associated with the dietary practice of lactating mothers. In the Bi-variable level analysis, the mother's occupation, being a daily laborer, was nine times more likely to have low dietary practice than the counterparts (AOR 9.35, 95% CI [8.02, 19.96]). Lactating mothers whose birth interval was <2 years, with family size greater than four members, and food insecure mothers were 2.3, 2.8, and 4.0 times more likely to have low dietary practice than those whose birth interval >24 months, whose family size less than four members and who were food secure, respectively (AOR = 2.3, 95% CI [1.49, 3.56]), (AOR = 2.8, 95% CI [1.65, 4.80]), and (AOR = 4.0, 95% CI [2.63, 6.12]), respectively (Table 6).
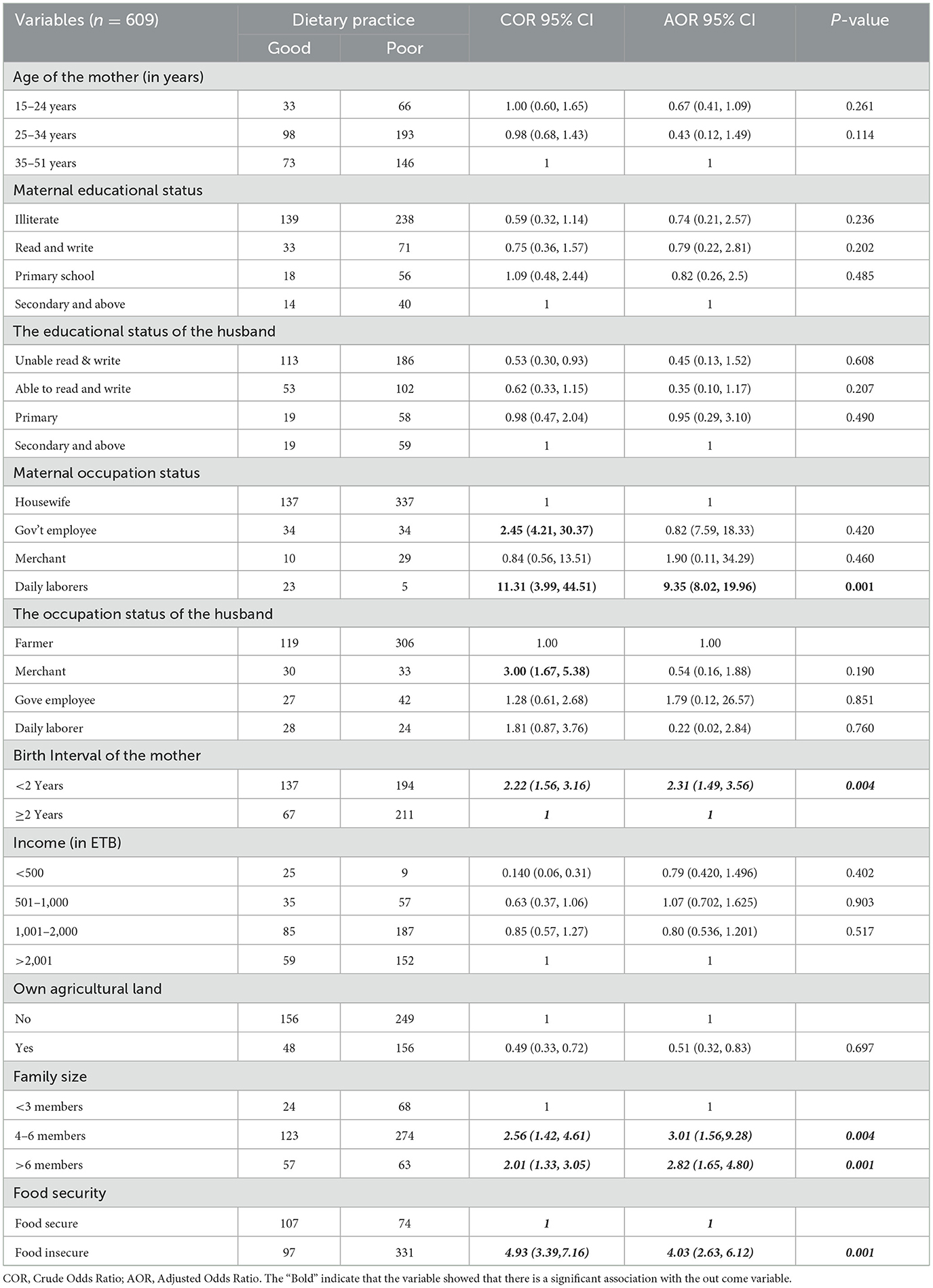
Table 6. Factors associated with dietary practice among lactating mothers at Dangila Zuria District Awi Zone, Amhara region, Ethiopia, 2022.
4 Discussion
Effective dietary practices during lactation are crucial for both maternal health and infant wellbeing. The Essential Nutrition Action (ENA) framework, along with numerous studies, emphasizes the importance of optimal nutrition for lactating women. Adhering to recommended dietary guidelines can enhance maternal health outcomes and support healthy growth and development in children (23). In this community-based cross-sectional study, we measured the proportion of good dietary practices among lactating mothers in the Dangila Zuria Woreda. The findings revealed that 33.5% [95% CI] of lactating mothers practiced good dietary habits during their lactation periods. The finding is consistent with studies conducted in other regions.
A study in Bag Lung District, Nepal, found that 31.8% of lactating mothers had good dietary practices (21), while a study in Wollega showed 33.9%. In Bahir Dar town, 35.9% of mothers demonstrated good dietary habits. Two systematic reviews in Ethiopia reported that 34.3% of lactating mothers c another study in Bahir Dar found that 39.3% of respondents had good dietary practices (10, 12, 20, 36, 37). The similarity may be because of cultural influences, such as shared beliefs about nutrition during lactation, socioeconomic conditions that limit access to diverse foods, common public health initiatives, and educational programs, the use of similar research methodologies, including sampling techniques and dietary assessment tools, and adherence to established nutritional guidelines, like those from the Essential Nutrition Action (ENA), may uniformly influence the dietary habits of mothers in these regions was with this low and similar prevalence.
However, this finding is lower than the study conducted in South Eastern Zone of Tigray 46.7%, in Gondar town 40.1%, rural community of Tigray 43.8%, Addis Ababa 48.6%, and in Dessie town, 45.2% (8, 29, 32–34). This discrepancy may be attributed to variations in regional dietary practices, access to resources, and differences in educational outreach related to nutrition during lactation. Additionally, the studies in these locations may have benefited from more robust health promotion initiatives or differing socioeconomic conditions that support better dietary practices among lactating mothers.
On the other hand, the finding of this study is higher than the study conducted in Samre Woreda, Tigray 28.8%, Finote selam 23.7%, and West Gojjam Zone 19.9%, Mizan Aman Town, Southwest Ethiopia 25.1% (8, 10, 38, 39). This difference may be attributed to geographical variations in agricultural productivity and dietary resources. For instance, the study conducted in Tigray occurred in an area less productive than our study site, which could impact the availability and diversity of food. Additionally, the smaller sample size in the second study may have influenced its findings. Central Ethiopia primarily produces Teff, Dagussa, and cereals, while the northern regions depend more on cereal crops, leading to significant differences in the dietary practices of lactating mothers.
Furthermore, our study found a statistically significant association between mothers' dietary practices and various associated factors, including the mother's occupation, which was specifically linked to the dietary practices of lactating mothers. Lactating mothers who were daily laborers had higher odds of poor dietary practice compared to those who were housewives (AOR = 9.35, 95% CI: [8.02, 19.960]).
This is supported by the studies mountains of Nepal (40), Ambo district Ethiopia (11), and Misha Woreda, South Ethiopia (41). The increased likelihood of poor dietary practices among daily laborer mothers may be attributed to their lower economic status and the demands of their work, which often leave them with limited time and resources to consume the recommended types of nutritious foods. In contrast, housewives may have more opportunities to focus on meal preparation and dietary quality for themselves and their children.
In this study, family size was found to have a statistical association with the dietary practices of lactating mothers. Mothers with a family size greater than four had higher odds of poor dietary practices compared to those with smaller families (AOR = 2.821, 95% CI: 1.656, 4.804). This is supported by studies conducted in Wollega, Guto Gido woreda, and Nekemte referral hospitals (42), East Wollega Zone, Ethiopia (12), as well as a systematic review in Ethiopia (37). The possible explanation for this trend is that women with larger family sizes may become less focused on their dietary practices due to competing demands. When food supply is limited, mothers may prioritize feeding their children or other family members over their own nutritional needs, which can negatively impact both their health and that of their infants.
The finding of this study identified that a mother's birth interval has a strong statistical association with the dietary practices of lactating mothers. Mothers whose birth interval <2 years was had higher odds of poor dietary practice as compared to their counterparts.
This may be due to the increased demands placed on mothers with closely spaced births, as they often prioritize the care of their younger child while managing the needs of the family. Consequently, this can lead to limited time and resources for self-care, making it challenging for them to meet their nutritional needs and those of the entire family. As a result, the focus on immediate child care can significantly hinder their ability to improve their nutritional status.
In this study food security of the mothers has a strong statistical association with dietary practices of lactating mothers. Mothers who had food insecurity had higher odds of poor dietary practice as compared to mothers who were food-secured (AOR = 4.030, 95% CI: 2.653, 6.123). This may have been explained as, when a woman had food security, she became more concerned about good dietary practices and immediately put it into practice. This is supported by a study which was conducted in Boston (43), West Gojam Zone (10), a systematic review in Ethiopia (37), Mizan Aman Town, Southwest Ethiopia (39), food insecurity may worsen diet quality and health of women's in their life.
5 Conclusion
In conclusion, this study highlights a concerning prevalence of poor dietary practices among lactating mothers, which is notably lower than findings from other research. The analysis revealed significant associations between dietary diversity and several key factors, including family size exceeding four members, short birth intervals, maternal occupation, and food insecurity. These insights underscore the need for targeted interventions that address these critical areas to improve the nutritional wellbeing of lactating mothers. By focusing on enhancing good dietary practices and addressing economic and social barriers, we can better support mothers in meeting their nutritional needs, ultimately benefiting both their health and that of their children.
5.1 Recommendation
Ministry of Health (MOH), Regional Health Bureaus (RHB), and health professionals, should play a critical role in improving maternal nutrition. Specifically, the MOH and RHB should integrate dietary counseling into existing maternal health programs, ensuring that healthcare providers are trained to offer personalized nutrition guidance during antenatal and postnatal visits. This could include incorporating nutrition-focused education into routine health check-ups for lactating mothers, with an emphasis on practical, culturally appropriate dietary practices.
Health professionals, including clinicians, and community health workers, can provide ongoing support through home visits and local health outreach programs. Additionally, these stakeholders should work to strengthen community-based interventions, such as organizing local nutrition workshops and peer support groups, where lactating mothers can learn about balanced diets, food security, and breastfeeding support.
To address food insecurity, the MOH should collaborate with agricultural and social welfare sectors to enhance access to nutritious food in vulnerable areas. Furthermore, promoting women's occupational opportunities and strengthening family planning initiatives, including appropriate birth spacing, will contribute to better maternal health outcomes and allow mothers to focus on optimal nutrition. In general, all stakeholders can significantly enhance maternal dietary practices, improve health outcomes for mothers and children, and foster a healthier future for families and communities.
5.2 Limitation of the study
The main limitation of this study is the reliance on maternal self-report through a 24-h dietary recall to assess dietary practices. This method is subject to recall bias, as mothers may not accurately remember or report all foods consumed within the previous 24 h. Factors such as forgetfulness, misunderstanding of portion sizes, or social desirability bias could influence the accuracy of the reported data. Additionally, the dietary assessment does not account for variations in long-term eating patterns or seasonal changes in dietary practices. Future studies could benefit from using more objective measures, such as food diaries or biomarkers, to complement self-reported data and reduce these biases. Furthermore, the cross-sectional design of the study limits the ability to draw causal inferences.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical clearance was obtained from Bahir Dar University, the College of Medical and Health Sciences, and the Institutional Health Research Ethics Review Committee (IHRERC). A formal letter for permission and support was written to the Dangila Zuria District and the ethical clearance was submitted to the Dangila Zuria Woreda Health Office. An official permission letter from the office was obtained for the next steps. The written permission letter from the district health office was submitted to each Kebeles administrative office, which is where the actual data collection was conducted. All lactating mothers were informed about the objective of the study. Then after the study objectives were explained, all mothers' ages were>18, and informed verbal consent from every LW was obtained. The right to participate or withdraw from the study at any time without any requirement was disclosed to the participant. Furthermore, the confidentiality of the information obtained from participants was guaranteed by all data collectors and investigators by using code numbers and keeping the questionnaires locked.
Author contributions
SM: Conceptualization, Data curation, Formal analysis, Investigation, Resources, Software, Validation, Visualization, Writing – original draft. GM: Conceptualization, Formal analysis, Methodology, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. AG: Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We authors would like to forward our heartfelt gratitude to the study subjects and data collectors for their willingness to participate in our study. In addition, we are adding our unlimited thanks to the health office and the Bahir Dar University College of Medicine and Health Science for securing the ethical issues of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, Ante Natal Care; AOR, Adjusted Odds Ratio; BMI, Body Mass Index; DDS, Dietary Diversity Score; EBF, Exclusive Breast Feeding; ENA, Essential Nutrition Action; FAO, Food and Agriculture Organization; FANTA, Food and Nutrition Technical Assistance; IDD, Iodine Deficiency Disorder; MDDS, Women's Minimum Dietary Diversity Score; MUAC, Mid Upper Arm Circumference; PNC, Post Natal Care; SDG, Sustainable Development Goals; SNNP, South Nation Nationality People; SPSS, Statistical Package for Social Science; SSA, Sub-Saharan Africa; UNICEF, United Nation International Children's Emergency Fund; WHO, World Health Organization.
References
1. Blaxter K. Lactation and the growth of the young. Milk. (1961) 2:305–61. doi: 10.1016/B978-1-4832-3225-6.50011-9
2. Lawrence RA. Physiology of Lactation. In: Breastfeeding (Ninth Edition) A Guide for the Medical Profession. New York, NY: University of Rochester School of Medicine and Dentistry Rochester (2022). p. 58–92. doi: 10.1016/B978-0-323-68013-4.00003-1
3. Von Salmuth V, Brennan E, Kerac M, McGrath M, Frison S, Lelijveld N. Maternal-focused interventions to improve infant growth and nutritional status in low-middle income countries: a systematic review of reviews. PLoS ONE. (2021) 16:e0256188. doi: 10.1371/journal.pone.0256188
4. Abera SF, Kantelhardt EJ, Bezabih AM, Tsadik M, Lauvai J, Ejeta G, et al. What factors are associated with maternal undernutrition in eastern zone of Tigray, Ethiopia? Evidence for nutritional well-being of lactating mothers. BMC Pub Health. (2020) 20:1214. doi: 10.1186/s12889-020-09313-0
5. Chakona G. Social circumstances and cultural beliefs influence maternal nutrition, breastfeeding and child feeding practices in South Africa. Nutr J. (2020) 19:1–15. doi: 10.1186/s12937-020-00566-4
6. Hall Moran V, Lowe N, Crossland N, Berti C, Cetin I, Hermoso M, et al. Nutritional requirements during lactation. Towards European alignment of reference values: the EURRECA network. Matern Child Nutr. (2010) 6:39–54. doi: 10.1111/j.1740-8709.2010.00276.x
7. Jouanne M, Oddoux S, Noël A, Voisin-Chiret AS. Nutrient requirements during pregnancy and lactation. Nutrients. (2021) 13:692. doi: 10.3390/nu13020692
8. Haileslassie K, Mulugeta A, Girma M. Feeding practices, nutritional status and associated factors of lactating women in Samre Woreda, South Eastern Zone of Tigray, Ethiopia. Nutr J. (2013) 12:28. doi: 10.1186/1475-2891-12-28
9. Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, et al. Complementary feeding: a commentary by the ESPGHAN committee on nutrition. J Pediatr Gastroenterol Nutr. (2008) 46:99–110. doi: 10.1097/01.mpg.0000304464.60788.bd
10. Demilew YM, Alem AT, Emiru AA. Dietary practice and associated factors among type 2 diabetic patients in Felege Hiwot Regional Referral Hospital, Bahir Dar, Ethiopia. BMC Res Notes. (2018) 11:434. doi: 10.1186/s13104-018-3531-2
11. Tolera B, Mideksa S, Dida N. Assessment of dietary practice and associated factors among pregnant mother in Ambo District, West Shoa, Oromia, Ethiopia, 2018. Ethiop J. Reprod Health. (2018) 10:4. doi: 10.69614/ejrh.v10i4.205
12. Daba G, Beyene F, Garoma W, Fekadu H. Assessment of nutritional practices of pregnant mothers on maternal nutrition and associated factors in Guto Gida Woreda, east Wollega zone, Ethiopia. Sci Technol Arts Res J. (2013) 2:105–13. doi: 10.4314/star.v2i3.98748
13. Comerford KB, Ayoob KT, Murray RD, Atkinson SA. The role of avocados in maternal diets during the periconceptional period, pregnancy, and lactation. Nutrients. (2016) 8:313. doi: 10.3390/nu8050313
14. Alabduljabbar S, Zaidan SA, Lakshmanan AP, Terranegra A. Personalized nutrition approach in pregnancy and early life to tackle childhood and adult non-communicable diseases. Life. (2021) 11:467. doi: 10.3390/life11060467
15. Cohen L, Chavez V, Chehimi S. Prevention is Primary: Strategies for Community Well-being. John Wiley & Sons. (2010).
16. Schickedanz A, Dreyer BP, Halfon N. Childhood poverty: understanding and preventing the adverse impacts of a most-prevalent risk to pediatric health and well-being. Pediatr Clin. (2015) 62:1111–35. doi: 10.1016/j.pcl.2015.05.008
17. Quisumbing AR, Haddad L, Peña C. Are women overrepresented among the poor? An analysis of poverty in 10 developing countries. J Dev Econ. (2001) 66:225–69. doi: 10.1016/S0304-3878(01)00152-3
18. Rutstein SO. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. Int J Gynecol Obstetr. (2005) 89:S7–24. doi: 10.1016/j.ijgo.2004.11.012
19. Lartey A. Maternal and child nutrition in Sub-Saharan Africa: challenges and interventions. Proc Nutr Soc. (2008) 67:105–8. doi: 10.1017/S0029665108006083
20. Zerfu TA, Biadgilign S. Pregnant mothers have limited knowledge and poor dietary diversity practices, but favorable attitude towards nutritional recommendations in rural Ethiopia: evidence from community-based study. BMC Nutr. (2018) 4:43. doi: 10.1186/s40795-018-0251-x
21. Nana A, Zema T. Dietary practices and associated factors during pregnancy in northwestern Ethiopia. BMC Preg Childbirth. (2018) 18:183. doi: 10.1186/s12884-018-1822-1
22. Forsido SF, Tadesse F, Belachew T, Hensel O. Maternal dietary practices, dietary diversity, and nutrient composition of diets of lactating mothers in Jimma Zone, Southwest Ethiopia. PLoS ONE. (2021) 16:e0254259. doi: 10.1371/journal.pone.0254259
23. Weldehaweria NB, Misgina KH, Weldu MG, Gebregiorgis YS, Gebrezgi BH, Zewdie BH, et al. Dietary diversity and related factors among lactating women visiting public health facilities in Aksum town, Tigray, Northern Ethiopia. BMC Nutr. (2016) 2:38. doi: 10.1186/s40795-016-0077-3
24. Bekele H, Jima GH, Regesu AH. Undernutrition and associated factors among lactating women: community-based cross-sectional study in Moyale District, Borena Zone, Southern Ethiopia. Adv Publ Health. (2020) 2020:4367145. doi: 10.1155/2020/4367145
25. Zerfu TA, Umeta M, Baye K. Dietary habits, food taboos, and perceptions towards weight gain during pregnancy in Arsi, rural central Ethiopia: a qualitative cross-sectional study. J Health Populat Nutr. (2016) 35:1–7. doi: 10.1186/s41043-016-0059-8
26. Asayehu TT, Lachat C, Henauw S, Gebreyesus SH. Dietary behaviour, food and nutrient intake of women do not change during pregnancy in Southern Ethiopia. Mater Child Nutr. (2017) 13:e12343. doi: 10.1111/mcn.12343
27. Tenaw Z, Arega M, Tachbele E. Nutritional knowledge, attitude and practices among pregnant women who attend antenatal care at public hospitals of Addis Ababa, Ethiopia. Int J Nurs Midwife. (2018) 10:81–9. doi: 10.5897/IJNM2017.0289
28. Kedir H, Berhane Y, Worku A. Magnitude and determinants of malnutrition among pregnant women in eastern Ethiopia: evidence from rural, community-based setting. Mater Child Nutr. (2016) 12:51–63. doi: 10.1111/mcn.12136
29. Alemayehu MS, Tesema EM. Dietary practice and associated factors among pregnant women in Gondar town north west, Ethiopia, 2014. Int J Nutr Food Sci. (2015) 4:707–12. doi: 10.11648/j.ijnfs.20150406.27
30. Habte A, Gizachew A, Ejajo T, Endale F. The uptake of key Essential Nutrition Action (ENA) messages and its predictors among mothers of children aged 6–24 months in Southern Ethiopia, 2021: a community-based crossectional study. PLoS ONE. (2022) 17:e0275208. doi: 10.1371/journal.pone.0275208
31. Beletew B, Gebremichael B, Tesfaye T, Mengesha A, Wudu M. The practice of key essential nutrition action messages and associated factors among mothers of children from birth up to 2 years old in Wereilu Wereda, south Wollo zone, Amhara, Northeast Ethiopia: a community based cross-sectional study. BMC Pediatr. (2019) 19:459. doi: 10.1186/s12887-019-1814-y
32. Beyene SA, Weldegerima L, Tela FG, Seid O, Brown AT, Bezabih AM. Barriers to utilize nutrition interventions among lactating women in rural communities of Tigray, northern Ethiopia: an exploratory study. PLoS ONE. (2021) 16:e0250696. doi: 10.1371/journal.pone.0250696
33. Diddana TZ. Factors associated with dietary practice and nutritional status of pregnant women in Dessie town, northeastern Ethiopia: a community-based cross-sectional study. BMC Preg Childbirth. (2019) 19:517. doi: 10.1186/s12884-019-2649-0
34. Worku A, Mekonnen Abebe S, Wassie MM. Dietary practice and associated factors among type 2 diabetic patients: a cross sectional hospital based study, Addis Ababa, Ethiopia. SpringerPlus. (2015) 4:1–8. doi: 10.1186/s40064-015-0785-1
35. Berihu A, Buruh Abera G, Berhe H, Kidanu K. Mother's knowledge on nutritional requirement of infant and young child feeding in Mekelle, Ethiopia, cross sectional study. Glob J Med Res. (2013) 13:13–24.
36. Bitew ZW, Alemu A, Ayele EG, Worku T. Dietary diversity and practice of pregnant and lactating women in Ethiopia: a systematic review and meta-analysis. Food Sci Nutr. (2021) 9:2686–702. doi: 10.1002/fsn3.2228
37. Bayked EM, Menelik MM, Toleha HN, Workneh BD, Wendie TF, Kahissay MH. Dietary knowledge, attitude, practice, and associated factors among pregnant mothers in Ethiopia: a systematic review and meta-analysis. Front Publ Health. (2024) 12:1393764. doi: 10.3389/fpubh.2024.1393764
38. Mekuria G, Wubneh Y, Tewabe T. Household dietary diversity and associated factors among residents of finote selam town, north west Ethiopia: a cross sectional study. BMC Nutr. (2017) 3:28. doi: 10.1186/s40795-017-0148-0
39. Girma Tilahun A, Molla Kebede A, Ejigu AG. Dietary practice and associated factors among pregnant women at public health institution in Mizan-Aman Town, Southwest Ethiopia. Nutr Metab Insights. (2021) 14:11786388211057796. doi: 10.1177/11786388211057796
40. Singh DR, Ghimire S, Upadhayay SR, Singh S, Ghimire U. Food insecurity and dietary diversity among lactating mothers in the urban municipality in the mountains of Nepal. PLoS ONE. (2020) 15:e0227873. doi: 10.1371/journal.pone.0227873
41. Abute L, Beyamo A, Erchafo B, Tadesse T, Sulamo D, Sadoro T. Dietary practice and associated factors among pregnant women in Misha Woreda, South Ethiopia: a community-based cross-sectional study. J Nutr Metab. (2020) 2020:5091318. doi: 10.1155/2020/5091318
42. Hundera TD, Wirtu D, Gemede HF, Kenie DN. Nutritional status and associated factors among lactating mothers in Nekemte Referral Hospital and Health Centers, Ethiopia. Int J Nutr Food Sci. (2015) 4:216–22. doi: 10.11648/j.ijnfs.20150402.23
Keywords: lactating mothers, dietary practice, dietary diversity, food security, Dangila, Ethiopia
Citation: Mulatu S, Mulatu G and Gedif A (2025) Dietary practice and associated factors among lactating mothers in Dangila District in the Awi Zone Amhara region Ethiopia, 2022: a cross-sectional study. Front. Nutr. 11:1506707. doi: 10.3389/fnut.2024.1506707
Received: 06 October 2024; Accepted: 10 December 2024;
Published: 06 January 2025.
Edited by:
Misganaw Asmamaw Mengstie, Debre Tabor University, EthiopiaReviewed by:
Chalachew Yenew, Debre Tabor University, EthiopiaAddisu Melake, University of Gondar, Ethiopia
Copyright © 2025 Mulatu, Mulatu and Gedif. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sileshi Mulatu, c2lsc2hpbXVsYXR1QGdtYWlsLmNvbQ==; U2lsZXNoLm11bGF0dUBiZHUuZWR1LmV0
 Sileshi Mulatu
Sileshi Mulatu Getasew Mulatu2
Getasew Mulatu2