Editorial on the Research Topic
Vitamin D: from pathophysiology to clinical impact, volume II
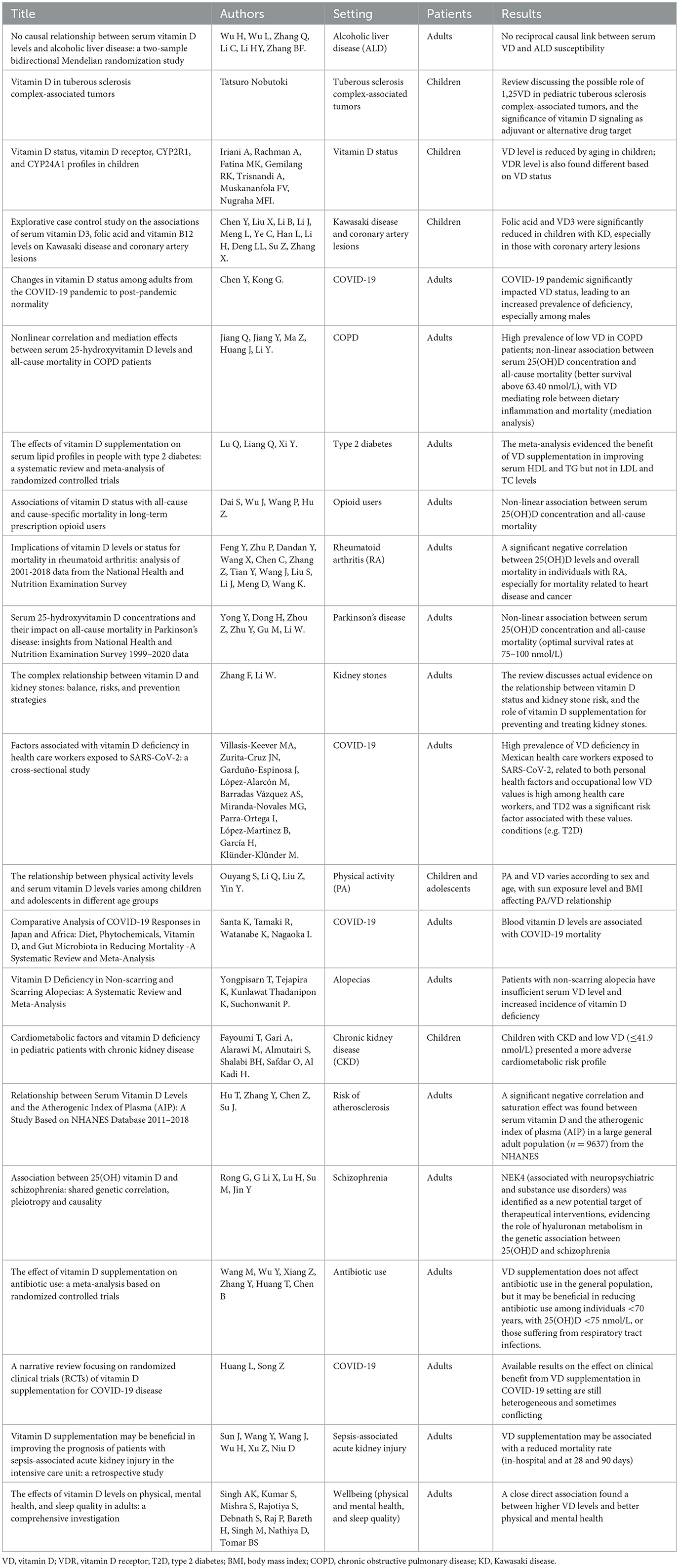
Besides the well-known positive effects on skeletal homeostasis and bone metabolism, growing evidence highlights the importance of vitamin D also in other many extra-skeletal districts; the articles published in this Research Topic confirm this observation in both adult and pediatric populations, spanning different conditions from inflammation and infectious diseases, obesity, and diabetes, to neurological disorders, gastrointestinal conditions, neurological disorders, cardiovascular health, and malignancies (see Table 1). This fact contributes to the increasing attention toward the measurement of serum 25(OH)D (main circulating form and recognized biomarker of vitamin D status) in laboratory medicine as well as the requirements of accuracy and speed of testing. However, despite the growth and refinement of analytical methods, the measurement of vitamin D still represents a challenge; immunoanalytical techniques still retain great variability in inter-laboratory comparisons, whereas mass spectrometry presents many different difficulties (e.g., costs, time, and complexity, matrix effects, derivatization step) (1). Interestingly, other vitamin D metabolites may have biological roles, and are expected to be assessed in the serum in the future (2).
In any case, at present the high prevalence of vitamin D deficiency is a worldwide major public sanitary issue in every stage of life, including children and adolescents, where an inadequate status can have implications on future health and wellbeing (3, 4). In this regard, as many as five contributions focusing on different children issues are included in this Research Topic (see Table 1). Moreover, available dosing recommendations for vitamin D supplementation may considerably vary in the literature depending on the clinical setting and specific cohort evaluated. Importantly, there is still no international general consensus on how to define an optimal vitamin D status, mainly defined based on the inverse relationship of parathyroid hormone and 25(OH)D. For it concerns bone health, the Endocrine Society defines as adequate serum 25(OH)D levels higher than 75 nmol/L (30 ng/mL) and values higher than 50 nmol/L (20 ng/mL) as deficient (5); instead, the Institute of Medicine (IOM, now National Academy of Medicine) definition suggests vitamin D sufficiency for values higher than 50 nmol/L (20 ng/mL), insufficiency between 30 and 50 nmol/L (12–20 ng/mL); deficiency for levels lower than 30 nmol/L (12 ng/mL) (6). In addition, differences may also be due to methodological issues (e.g., seasonal sampling, variability in the vitamin D assays), characteristics of the studied populations, (e.g., age, sex, and calcium intake), and life-style habits (physical activity, outdoor activities, and sun exposure) (1). Moreover, the majority of evidence derived from studies conducted in adults, and even the threshold used to define vitamin D deficiency or insufficiency may not be appropriate when applied to children and/or adolescents. Indeed, currently, there are no specific guidelines and no clear consensus on targets for optimal vitamin D status and supplementation in most extra-skeletal conditions (1). Thus, for non-classical actions, more research is needed concerning the optimal 25(OH)D levels to maintain and clarify the suitability of 25(OH)D reference levels (in turn useful to decide the recommended vitamin D intake to maintain most people above this threshold, providing adequacy) and the role of vitamin D as key indicator of health in different clinical settings. We hope that manuscripts included in this Research Topic, which highlight the role and levels of vitamin D in different pathophysiological conditions, may contribute to the actual discussion in this field and may be appreciated by readers of Frontiers in Nutrition, facilitating further studies stimulated by the data reported and by the many challenges still to be solved in this important research area.
Author contributions
CV: Conceptualization, Writing – original draft.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Della Nera G, Sabatino L, Gaggini M, Gorini F, Vassalle C. Vitamin D determinants, status, and antioxidant/anti-inflammatory-related effects in cardiovascular risk and disease: not the last word in the controversy. Antioxidants (Basel). (2023) 12:948. doi: 10.3390/antiox12040948
2. Slominski AT, Tuckey RC, Jetten AM, Holick MF. Recent advances in vitamin D biology: something new under the sun. J Investig Dermatol. (2023) 143:2340–2. doi: 10.1016/j.jid.2023.07.003
3. Cui A, Zhang T, Xiao P, Fan Z, Wang H, Zhuang Y. Global and regional prevalence of vitamin D deficiency in population-based studies from 2000 to 2022: a pooled analysis of 7.9 million participants. Front Nutr. (2023) 10:1070808. doi: 10.3389/fnut.2023.1070808
4. Huh SY, Gordon CM. Vitamin D deficiency in children and adolescents: epidemiology, impact and treatment. Rev Endocr Metab Disord. (2008) 9:161–70. doi: 10.1007/s11154-007-9072-y
5. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:1911–30. doi: 10.1210/jc.2011-0385
Keywords: 25(OH)D, extraskeletal districts, reference levels, threshold, vitamin D
Citation: Vassalle C (2024) Editorial: Vitamin D: from pathophysiology to clinical impact, volume II. Front. Nutr. 11:1506137. doi: 10.3389/fnut.2024.1506137
Received: 04 October 2024; Accepted: 11 October 2024;
Published: 29 October 2024.
Edited and reviewed by: Paula Ravasco, Catholic University of Portugal, Portugal
Copyright © 2024 Vassalle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cristina Vassalle, Y3Jpc3RpbmEudmFzc2FsbGVAZnRnbS5pdA==
 Cristina Vassalle
Cristina Vassalle