- 1Department of Acupuncture and Tuina, Changchun University of Chinese Medicine, Changchun, China
- 2School of Basic Medical Sciences, Hubei University of Chinese Medicine, Wuhan, China
- 3Department of Traditional Chinese Medicine, China-Japan Union Hospital of Jilin University, Changchun, China
- 4Department of Tuina,Affiliated Hospital of Changchun University of Traditional Chinese Medicine, Changchun, China
Background: Many previous studies explored the relationship between diabetes and insulin resistance (IR); however, addressing the research gap where no bibliometric analysis had been conducted to summarize and analyze these publications, we will undertake a comprehensive bibliometric analysis to investigate the current status and emerging trends in publications examining the association between diabetes and IR.
Methods: We retrieved publications related to the interaction between diabetes and IR from the Web of Science Core Collection (WoSCC). By utilizing software such as CiteSpace, VOSviewer, and Excel 2019, we analyzed and extracted relevant information from the literature to identify and delineate the research hotspots and directions in the study of diabetes and IR.
Results: From 1900 to 2024, a total of 2,698 publications were included in the bibliometric analysis, showing a steady annual increase in the number of publications. The USA led in this research field, with the Harvard University being a key research institution. The author Olefsky JM, published the most papers;Defronzo RA was the most cited author. DIABETES was the journal with the highest number of published papers and was also the most cited journal. The main discipline in the field of diabetes and IR research was Endocrinology and Metabolism. The most cited article was “Mechanisms linking obesity to insulin resistance and type 2 diabetes (2006)”;“The IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045(2018)” was the most cited reference. “insulin resistance” was the most frequently occurring keyword. The main research hotspots and frontier areas in diabetes and IR research were as follows: (1) The association between IR, diabetes, and obesity was a popular research topic; (2) Cardiovascular diseases secondary to diabetes and IR were another hot topic among researchers; (3) As a core pathological change in diabetes, IR was a major therapeutic target for improving diabetes.
Conclusion: This study summarized the research trends and hotspots in the field of diabetes and IR, provided valuable information and insights for scholars who focused on diabetes and IR scientific research, and offered a reference for future research directions.
1 Introduction
Diabetes has emerged as a global public health issue, currently affecting 463 million adults worldwide and accounting for 10% of global healthcare expenditures; the prevalence of diabetes was projected to rise to 700 million by 2045 (1–3). Diabetes was a chronic metabolic disorder characterized by persistent hyperglycemia, with its etiology involving IR and reduced insulin secretion from β-cells, where IR was considered a precursor to diabetes, as individuals with IR require higher levels of insulin to facilitate glucose uptake into cells (4–6). The concept of IR was initially proposed by Fatu (1931) and Himsworth (1936), and later gained widespread attention after the development of the radioimmunoassay by Yalow and Berson (7, 8). IR referred to the reduced sensitivity of insulin target tissues, such as adipose tissue, skeletal muscle, and the liver. In the early stages, pancreatic β-cells could compensate by increasing insulin secretion to offset the deficiency; however, over time, their function gradually deteriorated, leading to impaired glucose tolerance, prediabetes, and the onset of type 2 diabetes (9, 10). Therefore, as a primary pathogenic factor in diabetes, improving IR was crucial for the prevention of diabetes (11). To effectively improve IR, it was essential first to understand its underlying mechanisms. Although the mechanisms of IR were not yet fully elucidated, several key mechanisms had been proposed, including inflammation, oxidative stress, insulin receptor mutations, endoplasmic reticulum stress, and mitochondrial dysfunction (12). Previous bibliometric analyses have primarily focused on other complications of diabetes, such as diabetic foot, diabetic kidney disease, and gestational diabetes, which are also significant contributors to the global disease burden (13–15). However, insulin resistance, as a common precursor to many of these complications, remains a key therapeutic target. As a primary and common cause of metabolic disorders, IR is regarded as one of the core therapeutic targets for metabolic diseases, including diabetes. As a primary and common cause of metabolic disorders, IR was regarded as one of the core therapeutic targets for metabolic diseases, including diabetes. The primary therapeutic strategies for IR involved using diabetes medications (such as insulin, sulfonylureas, biguanides, and incretins) that stimulated insulin secretion or enhanced insulin sensitivity. Additionally, agents that inhibited hepatic fat synthesis and stimulate the oxidation of skeletal muscle and adipose tissue (such as adipose and anti-obesity agents) could reduce ectopic lipid accumulation, improve insulin sensitivity, and ultimately prevent or delay the onset of diabetes (16, 17). In addition to pharmacological treatments, lifestyle interventions, such as regular physical activity, a balanced diet, and weight control, have been shown to improve insulin sensitivity and are essential components of managing diabetes (18).
Bibliometrics served as a crucial quantitative measurement method for research in a specific field, facilitating the analysis and summarization of the research status, future trends, and global scientific competitiveness of a particular topic by filtering published data in databases according to research objectives and employing statistical methods as well as graphical and tabular representations (19). Despite the numerous publications on diabetes and IR within the WOSCC, there had yet to be a bibliometric and visualization analysis conducted on this specific topic. Therefore, this study aimed to review articles related to diabetes and IR published in the WOSCC from 1900 to 2024, to assist scholars and researchers in the field of endocrinology in better understanding the research hotspots and frontiers in this domain.
2 Methods
2.1 Data sources and search strategy
In the literature search conducted by our team (Figure 1), we used the WoSCC database on July 31, 2024. The time span was set from “1900 to 2024” and the search formula was TI = (diabetes) AND TI = (insulin resistance), with the language limited to “English” and document types set to “articles” and “reviews.”
2.2 Data analysis
In bibliometric research, CiteSpace was one of the popular tools based on Java program information, used for literature data analysis and visualization in specific fields (20). VOSviewer was a literature analysis software tool developed by Nees Jan van Eck and Ludo Waltman from Leiden University in 2010 for creating and exploring maps based on network data (21). Depending on the research objectives and plotting requirements, we selected the appropriate software and set relevant parameters to complete the plotting and analysis. Additionally, Microsoft Office Excel 2019 was used for quantitative analysis of the publications.
3 Results
3.1 Analysis of annual publications and trends
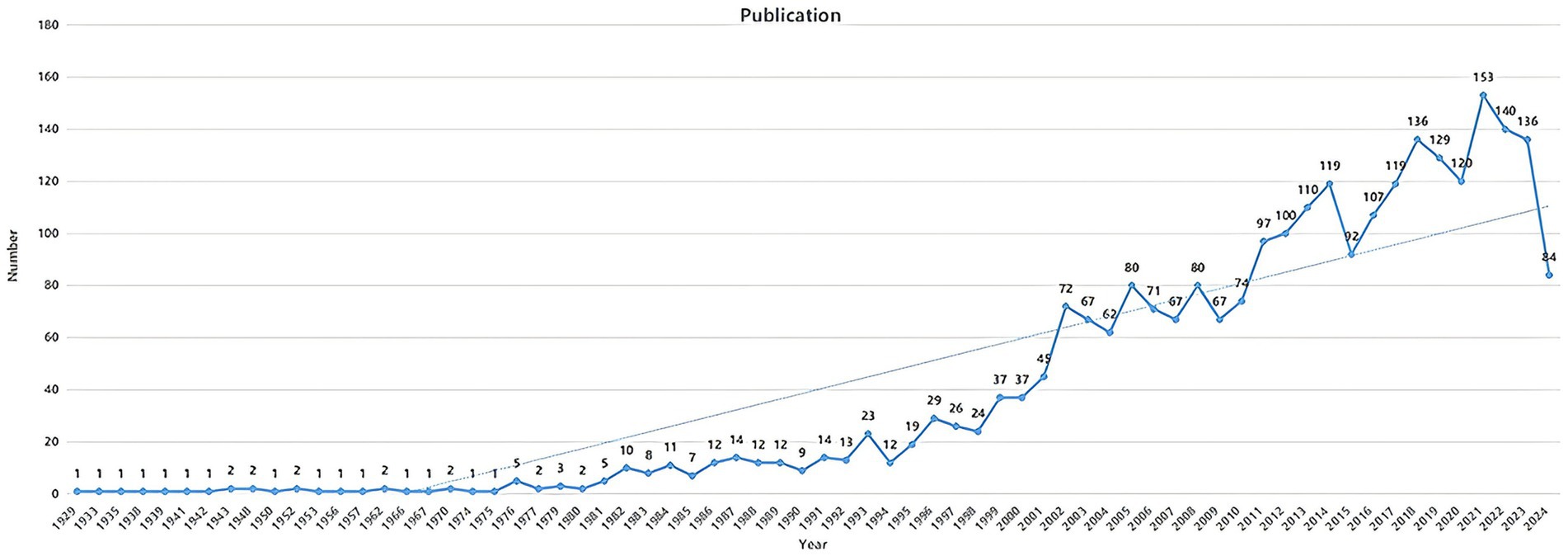
In the annual publication trend, the publication count served as an indicator of the trends and current status in a specific research field (Figure 2) (22). From 1900 to 2024, this trend reflected the research focus related to diabetes and IR. In this study, a total of 2,698 publications were retrieved, including 2,343 articles and 355 reviews. The overall trend in the annual publication volume related to diabetes and IR showed a steady increase.
3.2 Analysis of the trend of countries/regions, institutions, and authors
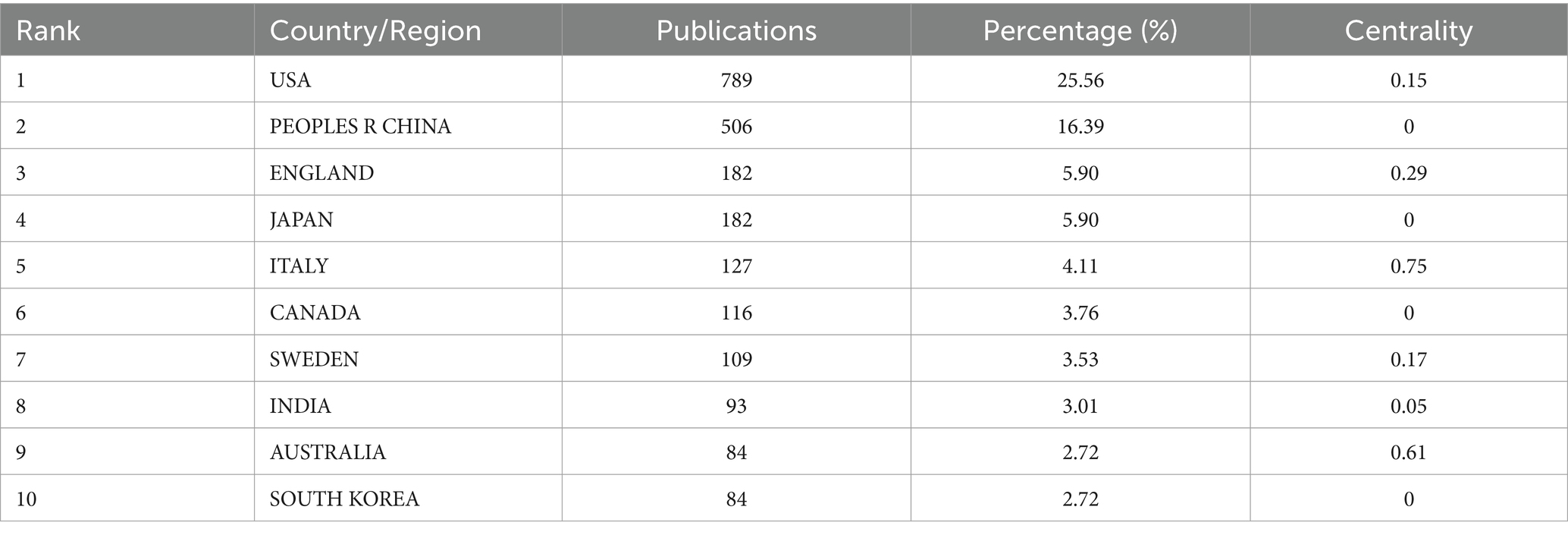
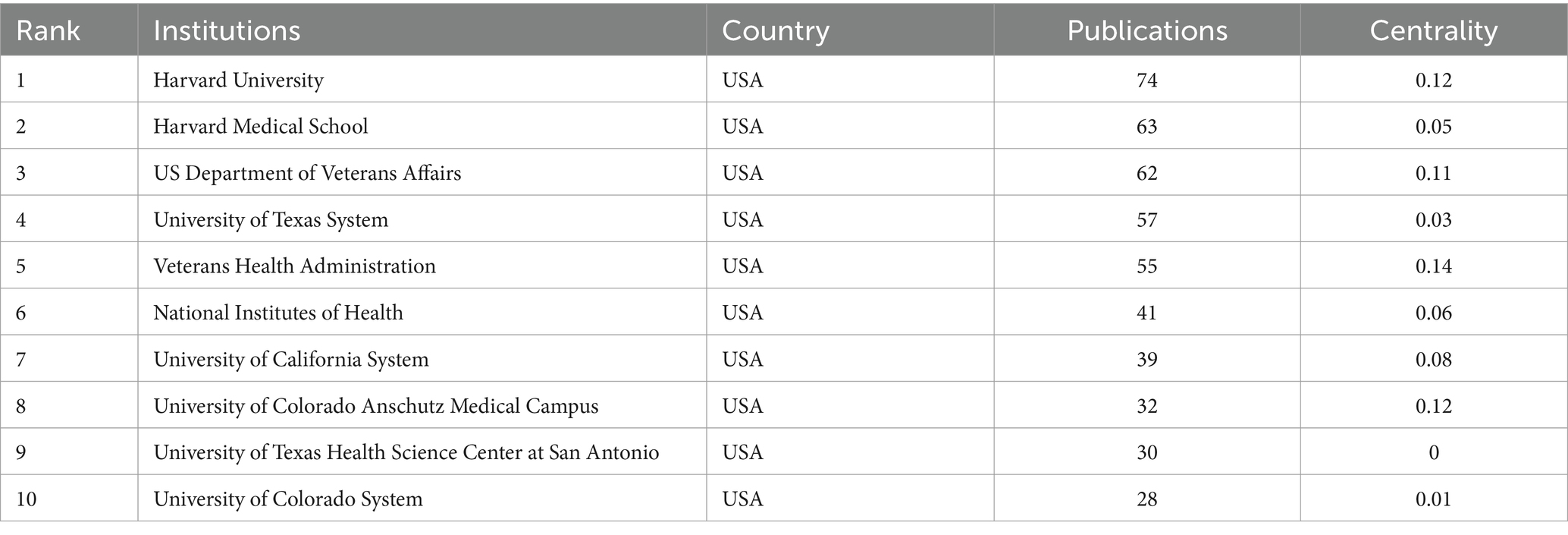
A total of 64 countries and regions contributed to the body of research on diabetes and IR. Table 1 highlighted the top 10 countries ranked by publication volume. The United States topped the list with 789 publications (25.56%), followed by China with 506 publications (16.39%). England and Japan shared the same publication count, each contributing 182 articles (5.90%). In the co-authorship network (Figure 3A), nodes represented individual countries, and the links between them indicated collaborative relationships. A country’s node size correlates with its publication output in this field, with larger nodes indicating higher productivity. The gray inner circles signified earlier publications, while the red outer circles denoted more recent work. The United States, China, Italy, Australia, and England emerged as the most prolific contributors. The centrality of a country or region reflects its significance within the network, with a positive correlation observed between collaboration and centrality. Italy boasted a centrality of 0.75, followed by Australia (0.61) and England (0.29).
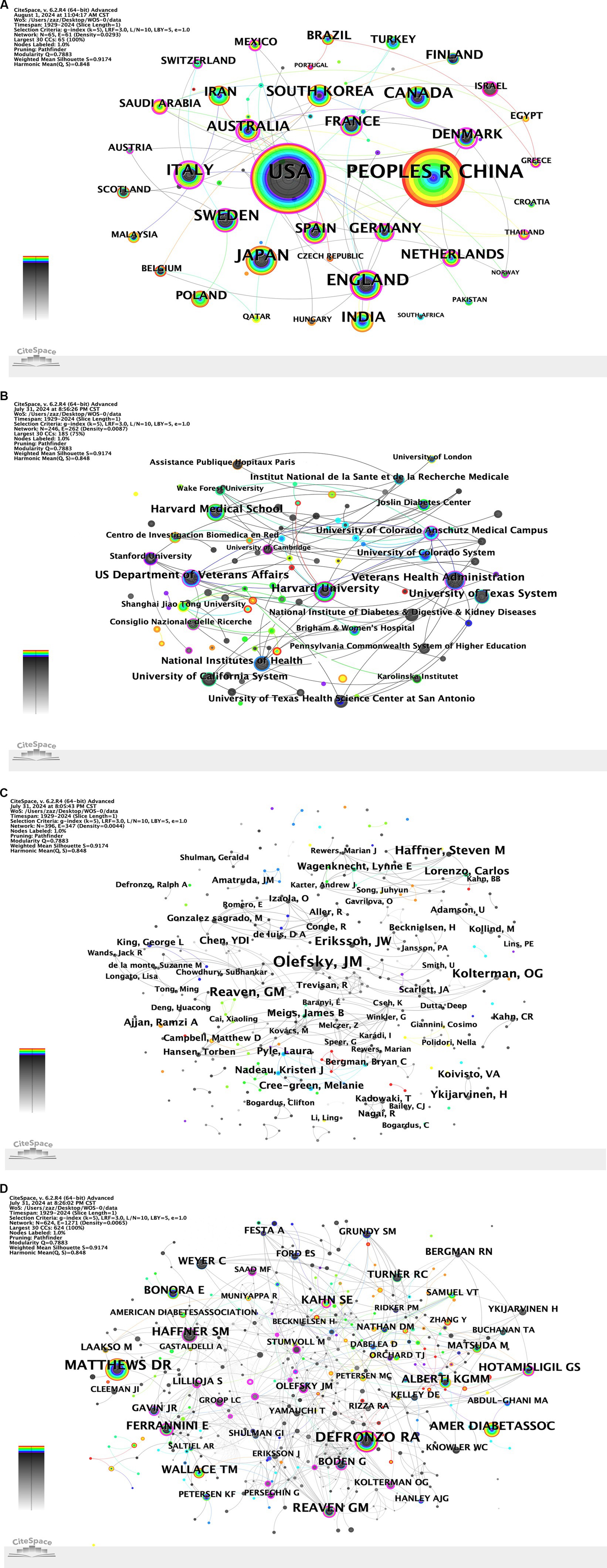
Figure 3. (A) Country co-occurrence map. (B) Institution co-occurrence map. (C) Author co-occurrence map. (D) Cited author co-occurrence map.
A total of 246 academic institutions published research findings related to diabetes and IR. Table 2 listed the top 10 institutions by the number of publications. The top three institutions were Harvard University (74 papers), Harvard Medical School (63 papers), and the US Department of Veterans Affairs (62 papers). In the collaboration network (Figure 3B), the collaboration relationships and publication volumes among these institutions were illustrated, showing close connections across all institutions. The Veterans Health Administration (0.14), Harvard University (0.12), and the University of Colorado Anschutz Medical Campus (0.12) ranked as the top three in centrality, reflecting their significant roles in the collaborative network.
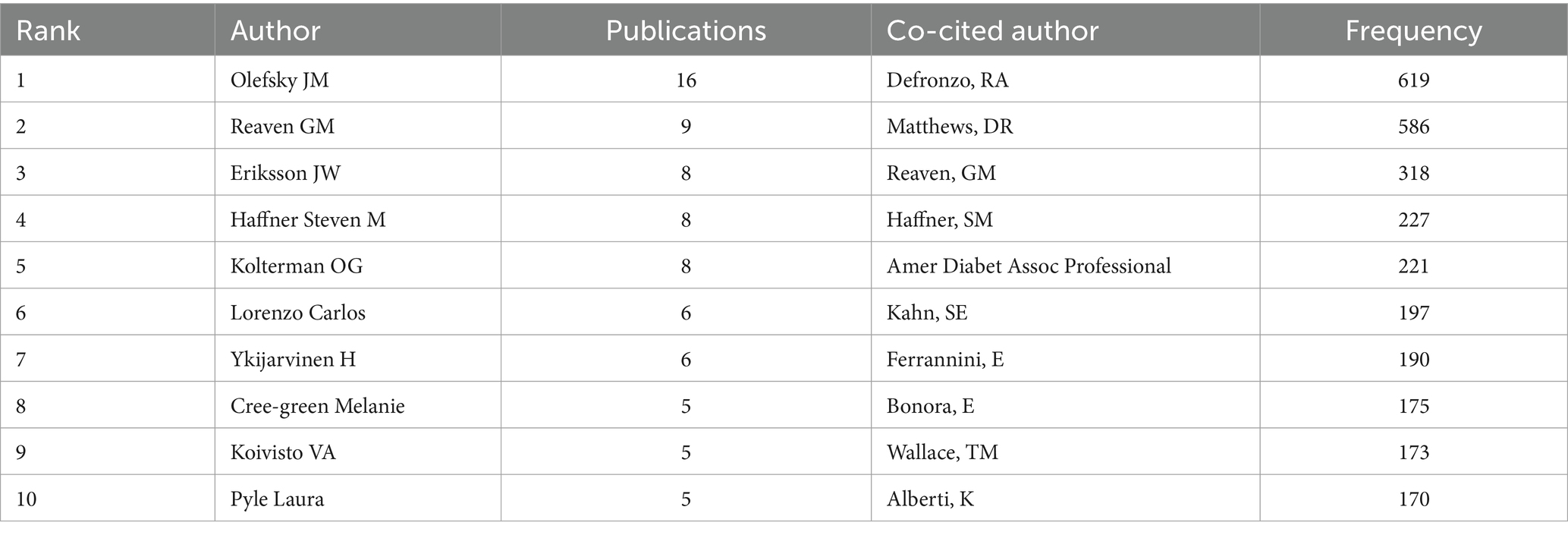
A total of 395 authors have published papers on diabetes and IR, with their publication volumes (Figure 3C). Table 3 listed the top 10 authors and co-cited author by the number of publications or frequency. Olefsky JM published 16 papers, making Olefsky the most prolific author, followed by Reaven GM (9 papers) and Eriksson JW (8 papers). These 10 authors played significant roles in the field of diabetes and IR research. Among the top 10 authors, 7 were from the United States. The centrality of all the authors retrieved in this study was 0, indicating that collaboration among authors remained an area for improvement. The top three co-cited authors were Defronzo RA, Matthews DR, and Reaven GM. The cited author co-occurrence map (Figure 3D) presents the co-occurrence network of cited authors in the field.
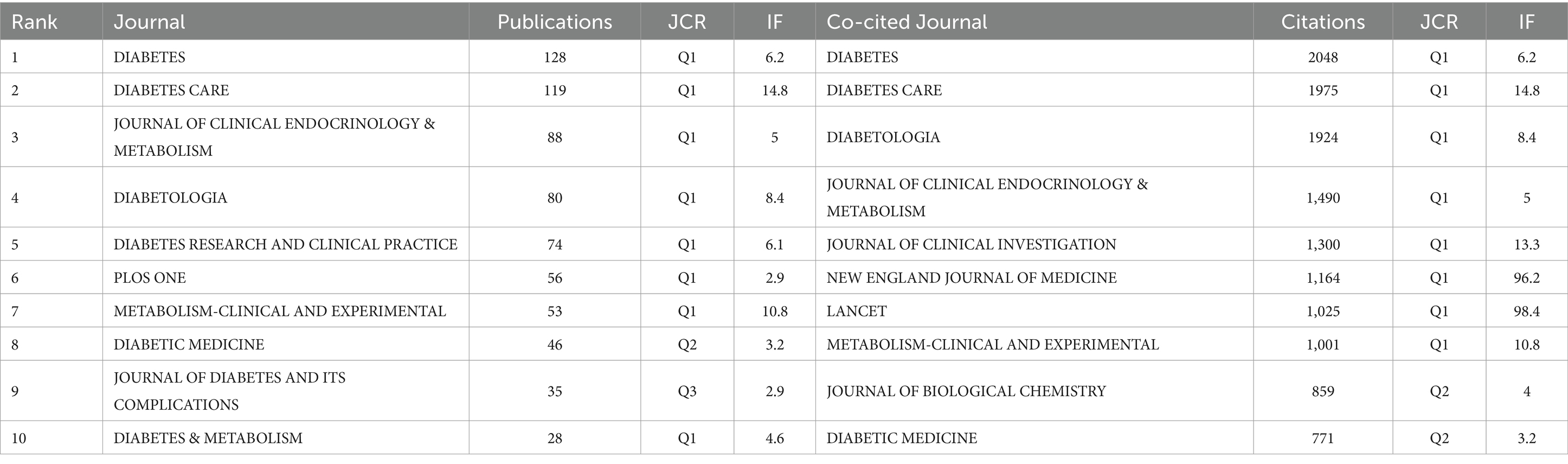
3.3 Journals and subjects analysis
The journals publishing articles on diabetes and IR and the collaborative relationships among them were illustrated using VOSviewer (Figure 4A). Table 4 listed the top 10 journals by the number of diabetes and IR-related publications, as well as the top 10 journals by citation frequency, including their JCR rankings and impact factors (IF). The network analysis view of the co-cited journals was shown (Figure 4B). DIABETES and DIABETES CARE ranked first and second in terms of both publication volume and citation frequency. DIABETES (Q1, IF = 6.2) had the highest number of publications (128) and was cited 2,048 times. It was followed by DIABETES CARE (Q1, IF = 14.8) with 119 publications and 1,975 citations. Among the top 10 journals by publication volume, 8 were in the Q1 quartile. DIABETES CARE had the highest impact factor among the top 10 by publication volume, at 14.8; among the highly cited journals, LANCET had the highest impact factor, at 98.4.In addition to publication volume and citation frequency, the total link strength (TLS) of the top journals was analyzed using VOSviewer, which reflects the degree of connectivity between journals in the citation network. DIABETES had the highest TLS of 744, followed by DIABETES CARE with a TLS of 639, and Journal of Clinical Endocrinology & Metabolism with a TLS of 496. These results indicate that DIABETES and DIABETES CARE not only lead in publication volume and citation frequency but are also highly interconnected with other journals, suggesting their central role in disseminating knowledge and facilitating collaboration in diabetes research.
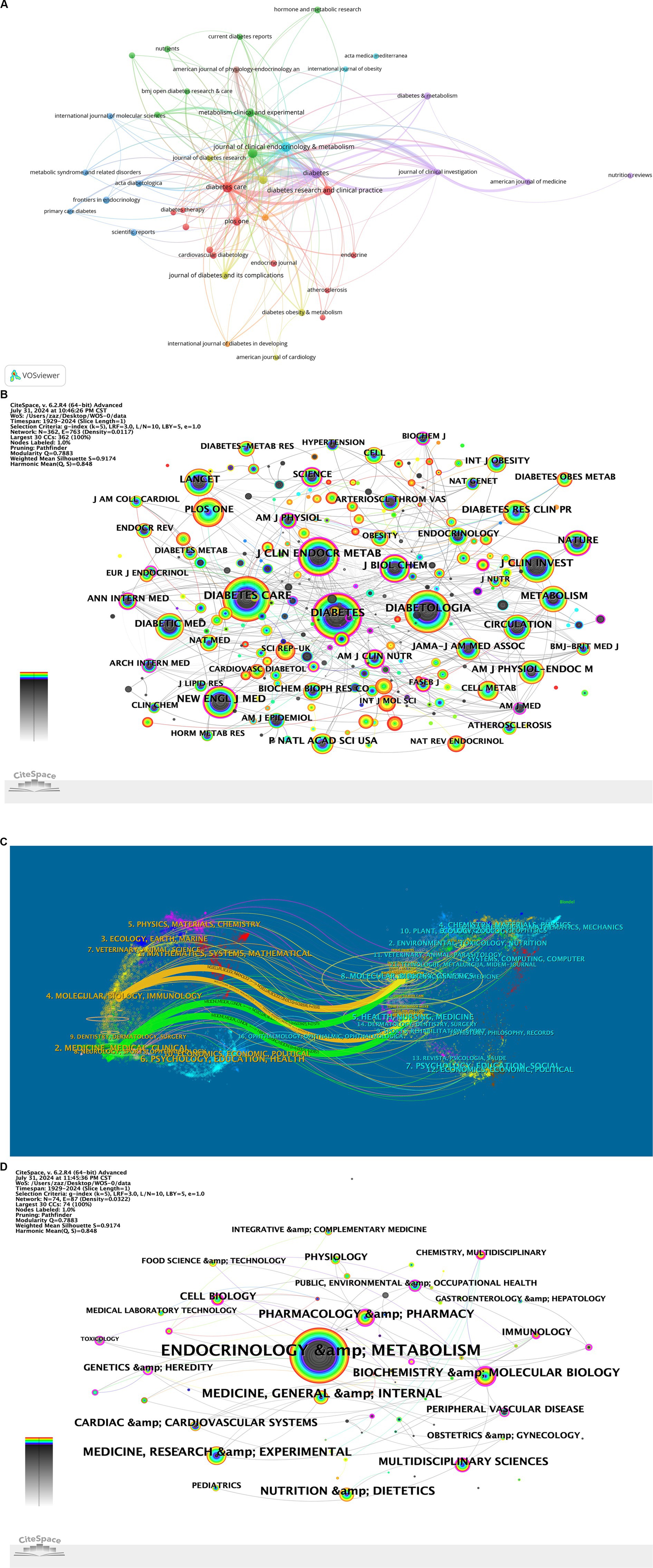
Figure 4. (A) Journal collaboration diagram. (B) Journal co-occurrence network. (C) Journal dual-map overlay. (D) Subject co-occurrence network.
The journal dual-map overlay was presented, showing the distribution of topics, with labels representing the covered subjects and colored paths indicating citation relationships (Figure 4C). The connections and collaborations between different disciplines were illustrated (Figure 4D). In the field of diabetes and IR research, the primary discipline was Endocrinology & Metabolism, which frequently collaborated closely with several other disciplines.
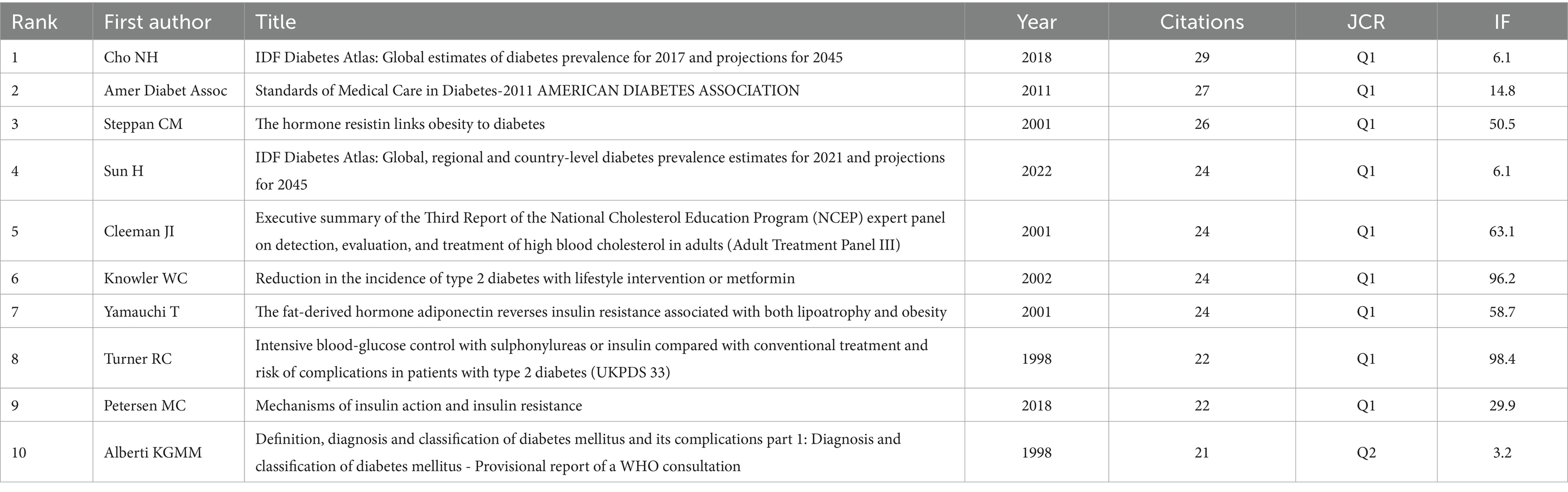
3.4 Analysis of articles and references
Table 5 listed the top 10 highly cited articles. “Mechanisms linking obesity to insulin resistance and type 2 diabetes” published in NATURE (Q1, IF = 50.5) was cited 3,616 times. This was followed by “Hypoadiponectinemia in obesity and type 2 diabetes: Close association with insulin resistance and hyperinsulinemia” published in JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM (Q1, IF = 5), with 2,855 citations, and “Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome” published in JOURNAL OF CLINICAL INVESTIGATION (Q1, IF = 13.3), which had 2,175 citations. All of the top 10 highly cited articles belonged to Q1 journals, indicating their significant academic impact. Notably, Guilherme A’s paper titled “Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes,” published in the renowned journal NATURE REVIEWS MOLECULAR CELL BIOLOGY, had an exceptionally high impact factor of 81.3.
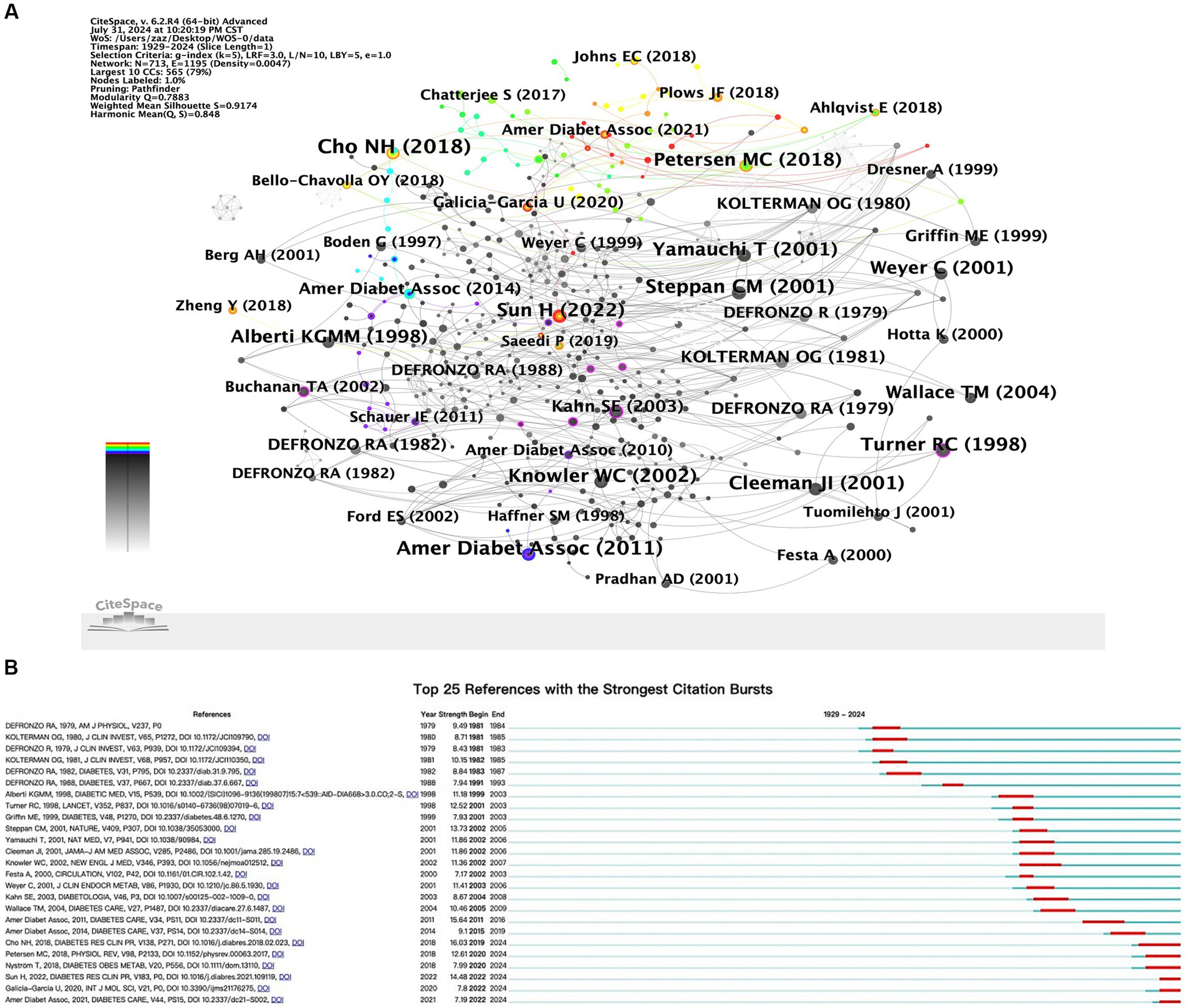
When multiple references were cited repeatedly by different documents, co-citation relationships were formed. These relationships were often used to determine the degree of association between different references (23). Table 6 listed the top 10 most frequently cited references, and the network view of the co-occurrence analysis of these references was presented (Figure 5A) “Mechanisms linking obesity to insulin resistance and type 2 diabetes” was the most cited, with 29 citations, followed by “Standards of Medical Care in Diabetes-2011 American Diabetes Association” with 27 citations. The third most frequently cited article was “The hormone resistin links obesity to diabetes,” with 26 citations. The top 25 references with the highest burst strength were shown (Figure 5B). Among them, Cho NH et al.’s article “IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045,” published in DIABETES RESEARCH AND CLINICAL PRACTICE (Strength = 16.03), was identified as the reference with the strongest citation burst.
3.5 Analysis of keywords
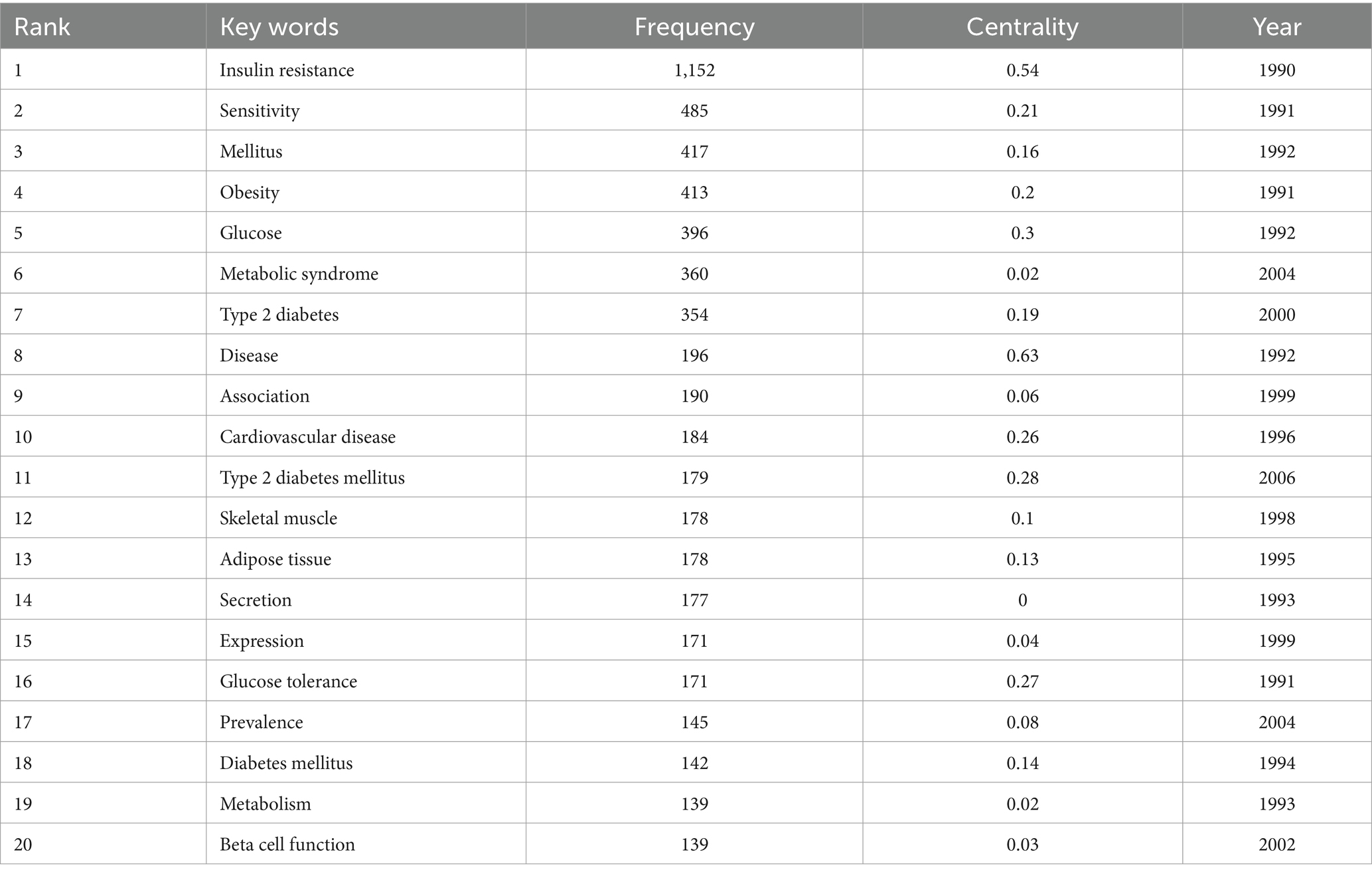
3.5.1 High frequency keywords analysis
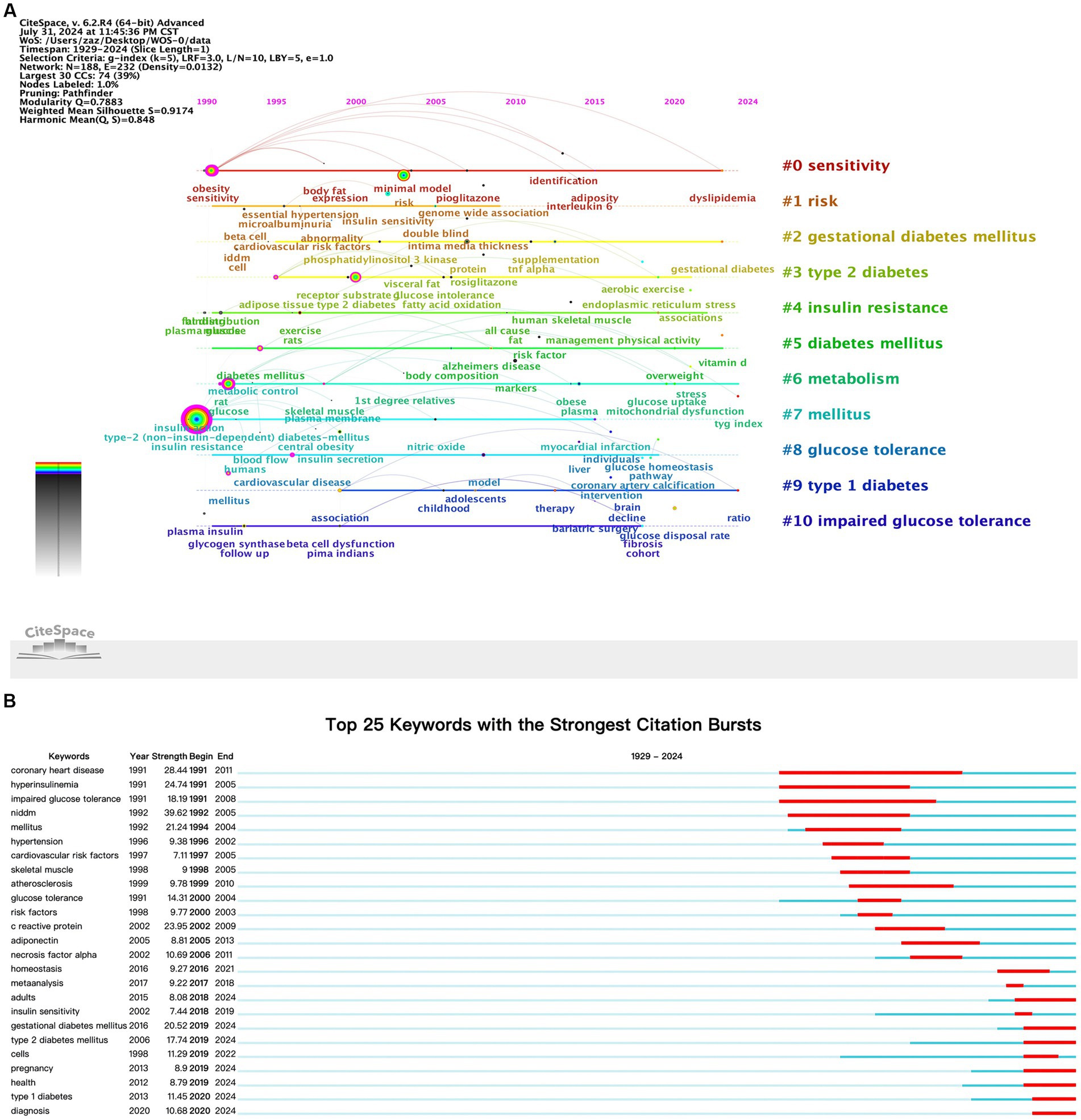
High frequency keywords reflected the focus of researchers over a certain period, indicating research hotspots and frontier areas (24). This study identified a total of 187 keywords. Table 7 lists the top 20 most frequently occurring keywords. The co-occurrence of these keywords was shown (Figure 6A). The keyword “insulin resistance” (n = 1,152, centrality: 0.54) appeared most frequently, with closely related keywords including “sensitivity” (n = 485, centrality: 0.21), “mellitus” (n = 417, centrality: 0.16), “obesity” (n = 413, centrality: 0.2), and “glucose” (n = 396, centrality: 0.3). To better understand the research hotspots and current status of diabetes and IR, we set a threshold of at least five occurrences for keywords, resulting in a keyword density map (Figure 6C). The density map shows that the main research hotspots in IR are focused on its associations with diabetes, obesity, and cardiovascular disease, as well as its biological mechanisms, clinical treatments, and impacts on specific populations.
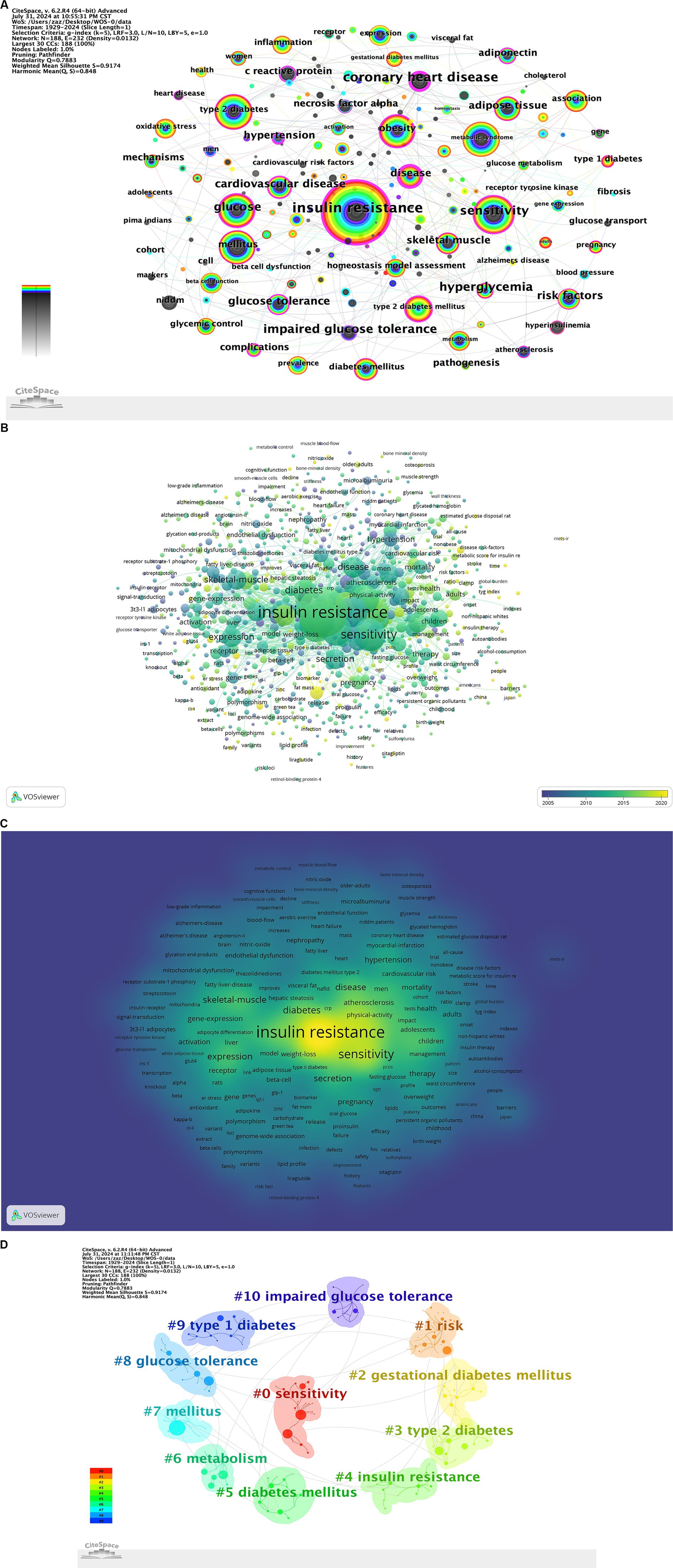
Figure 6. (A) Keyword co-occurrence map. (B) Keyword time zone map. (C) Keyword density map. (D) Keyword clustering map.
3.5.2 Keyword clustering
To understand the research frontiers of diabetes and IR since 1900, we employed CiteSpace to cluster diabetes and IR-related keywords. The keyword clustering results were shown (Figure 6D), identifying 11 clusters: #0 sensitivity, #1 risk, #2 gestational diabetes mellitus, #3 type 2 diabetes, #4 insulin resistance, #5 diabetes mellitus, #6 metabolism, #7 mellitus, #8 glucose tolerance, #9 type 1 diabetes, and #10 impaired glucose tolerance. These clusters highlight major research topics, with “sensitivity” as the largest cluster, indicating a strong research focus on insulin sensitivity. Other prominent clusters, such as “risk,” “gestational diabetes mellitus,” and “type 2 diabetes,” reflect additional critical areas of study within diabetes and IR research.
3.5.3 Keyword timeline analysis
The VOSviewer keyword time evolution overlay visualization was shown (Figure 6B). In the figure, the purple cluster represented the earliest keywords, the green cluster indicated earlier keywords, and the yellow cluster represented the most recent keywords. Keywords in the green cluster, such as “insulin resistance,” “sensitivity,” “skeletal muscle,” “diabetes,” and “expression,” were particularly prominent. A timeline visualization of keywords was created using CiteSpace, resulting in a clear representation of keyword trends over time (Figure 7A). The timeline view structure included the X-axis representing the publication year and the Y-axis corresponding to the keyword cluster names. Red (#0) represented the theme of “sensitivity,” which was prevalent in the earlier years of research (around the 1990s) and gradually decreased in relevance. Orange (#1) related to “risk” with keywords becoming more prominent starting in the early 2000s and continuing through to recent years. Yellow (#2) corresponded to “gestational diabetes mellitus” a theme that emerged in the 2010s and showed increasing relevance up to 2024. Green clusters (#3, #4, #5, and #6), which included themes like “type 2 diabetes,” “insulin resistance,” and “metabolism,” showed steady importance and dominated in research from the 2000s through the 2020s, indicating the sustained focus on these topics. Blue (#7 to #10) included themes like “glucose tolerance” and “type 1 diabetes,” which emerged more recently and represented growing areas of interest as research evolved. This provided a clear depiction of the stage-specific hotspots and development trajectory of keywords in diabetes and IR research over time.
3.5.4 Keyword burst analysis
The emergence of keywords can indicated a sudden increase in research interest over a certain period, which may suggest future research trends. The top 25 keywords with the highest burst intensity within the research topics of diabetes and IR were presented (Figure 7B). In the figure, the blue line represented the start time of the research, while the red line indicated the duration of the keyword burst. Recently, researchers had been focusing on “diagnosis” “type 2 diabetes” “gestational diabetes” and “health.” This shift in focus highlights a growing interest in more specific aspects of diabetes and insulin resistance, particularly around diagnostics, subtype classification, and public health implications. The recent emphasis on these keywords suggests that the research community is increasingly prioritizing early detection, management strategies tailored to diabetes subtypes, and a broader consideration of overall health outcomes. This trend may indicate an evolving research landscape where prevention, personalized treatment, and population health perspectives are gaining prominence. These insights not only reflect current research priorities but may also guide future studies towards more targeted interventions and holistic approaches in diabetes and IR management.
4 Discussion
4.1 General information
Research on diabetes and IR dates back to 1929, though annual publication output remained below 10 until 1981. Starting in 1991, research articles on these topics stabilized above 10 per year, with a notable surge between 2001 and 2002, likely reflecting growing global recognition of diabetes as a major public health issue. Annual publication numbers reached 100 for the first time in 2013. Although there was a slight decline in 2015, the trend quickly rebounded, leading to a peak of 153 articles in 2021. This consistent growth indicates that diabetes and IR remain key areas of research focus, driven by advancements in diagnostic and therapeutic technologies and an increasing emphasis on metabolic health. These trends suggest that future research will likely continue to explore novel treatment approaches, prevention strategies, and the broader implications of diabetes and IR on public health.
Research on diabetes and IR was primarily concentrated in the Northern Hemisphere, with strong connections between North America, Europe, Oceania, and Asia. Oceania maintained especially close ties with North America and Europe. The United States and China had the highest publication volumes in this field, but collaboration between the two countries remained limited. Among the top 10 countries, some with a heavier burden of diabetes had lower research productivity, possibly due to a lack of funding and infrastructure. Exploring these disparities could be a valuable direction for future research. Meanwhile, China, with 114 million people with diabetes, faces significant challenges. Over the past decade, China has expanded health insurance and launched strategies to promote health and strengthen primary care. In addition, innovations in artificial intelligence and Big Data are aiding diabetes management (25). Although the U.S. and China collaborate less frequently, both have made substantial contributions to diabetes research.
The top 10 institutions by publication volume were all world-renowned universities and research institutions from the United States, closely connected to Harvard University, which demonstrated Harvard’s significant academic influence. These leading institutions included universities, research institutes, medical schools, national institutions, health science centers, and the Department of Veterans Affairs. Notably, due to the high prevalence of diabetes among veterans and the fact that the Department of Veterans Affairs operated the largest integrated healthcare system in the U.S., it provided extensive clinical data and abundant research resources (26, 27). Additionally, U.S. healthcare policies supported such research (28, 29). Institutions such as the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC) have established extensive research networks that focus on diabetes, contributing to the prominence of US institutions in this field (30, 31). The multi-center institutional model developed in the U.S. for diabetes and IR research enabled multi-dimensional studies and exploration of diabetes, IR, and related diseases, making significant contributions to the advancement of this field.
Co-citation analysis identified cases where two authors’ works were cited together by a third author (Figure 3D), reflecting both their academic achievements and contributions to advancing scientific knowledge. Analysis of the most frequently cited authors in diabetes and IR research highlighted their impact and key research areas. The top three most cited authors were Defronzo RA (619 citations), Matthews DR (586 citations), and Reaven GM (318 citations).
The analysis revealed that eight of the top 10 journals were high-quality Q1-ranked, highlighting the significant scientific and clinical value of diabetes and IR research. Frequent citations in these journals underscored their critical role in advancing the field and their profound impact on subsequent research. The presence of numerous high-impact journals confirmed that insulin resistance research had become a major focus in biomedicine, particularly within Endocrinology & Metabolism, which was closely linked to disciplines like Biochemistry, Pharmacology, Cardiovascular Science, Nutrition, and Medicine.
Keyword bursts indicated a sharp increase in research interest, signaling potential future trends. Figure 7B showed the top 25 keywords with the highest burst strength in diabetes and IR research. From 1990 to 2000, keywords like “coronary heart disease,” “hyperinsulinemia,” and “impaired glucose tolerance” reflected the focus on the relationship between diabetes, IR, and metabolic diseases. From 2000 to 2010, keywords such as “C-reactive protein” and “adiponectin” highlighted research on inflammatory factors. From 2010 to 2020, keywords like “homeostasis” and “insulin sensitivity” indicated growing diversity in research topics, with a focus on systemic metabolic balance. From 2021 to 2024, emphasis shifted towards applications, as terms like “diagnosis” and “health” surged, reflecting a growing focus on clinical diagnostics and health management, alongside increased attention to cellular-level mechanistic studies.
4.2 Hotspots and frontiers
Based on a comprehensive analysis from multiple perspectives, including keywords, highly cited articles, highly referenced literature, and authors, the primary research trends and hot topics in the field of diabetes and IR research could be broadly categorized into three key areas.
Firstly, the relationship between IR, diabetes, and obesity has emerged as one of the key focal points of interest among researchers. Diabetes was a chronic hyperglycemic disease that occurred when the pancreas failed to produce sufficient insulin or when the body was unable to effectively utilize the insulin it produced. Type 1 diabetes mellitus was considered an autoimmune disease that developed in genetically predisposed individuals due to T-cell-mediated destruction of pancreatic β-cells. In contrast, type 2 diabetes mellitus (T2DM), which accounted for 90% of all diabetes cases and was the most extensively studied type, was characterized by an imbalance in blood glucose levels, with its pathogenesis rooted in IR and secretion abnormalities (32, 33). IR was a prominent characteristic of diabetes (34), serving not only as the most powerful predictor of future development of T2DM but also as a critical therapeutic target once hyperglycemia occurred (35). Defects in insulin signaling could lead to IR in key insulin target organs, including muscle, liver, and adipose tissue (36). β-cell dysfunction, inflammation, and adipocyte dysfunction were the key factors that linked obesity to IR and diabetes (37–39). Obesity were closely associated with an increased risk of IR and the development of T2DM. In obese individuals, adipose tissue released elevated levels of non-esterified fatty acids, glycerol, hormones, and pro-inflammatory cytokines, all of which contributed to the development of IR. When IR was coupled with dysfunction of pancreatic β-cells, the cells responsible for insulin secretion, it led to the onset and progression of diabetes (37). In the context of insulin resistance associated with obesity and T2DM, chronic nutritional excess leads to oxidative stress and inflammatory changes. Adipose tissue, beyond serving as a fat reservoir, was demonstrated to function as an endocrine organ that produced inflammatory cytokines. The increased concentrations of TNF-α and IL-6 could interfere with the anti-inflammatory effects of insulin by inhibiting insulin signaling, potentially exacerbating the inflammatory response (38, 40). Additionally, gestational diabetes mellitus (GDM) has emerged as a key area of interest due to its close association with insulin resistance, particularly in the context of obesity (41). GDM occurs when the body’s insulin resistance increases during pregnancy, often in women who are already predisposed to IR (42). It is not only a predictor of future T2DM in affected women but also represents a significant metabolic stressor during pregnancy, contributing to complications for both mother and child (43). The elevated risk of developing T2DM after experiencing GDM highlights the long-term metabolic consequences of insulin resistance during pregnancy (44). In summary, obesity played a crucial role in the development of IR (40), which was one of the most typical and common pathological changes observed in diabetes (36).
Secondly, cardiovascular diseases secondary to diabetes and IR have emerged as another focal point of interest among researchers. IR in diabetes was recognized as one of the risk factors for cardiovascular diseases and was closely associated with conditions such as coronary heart disease, hypertension, and atherosclerosis. T2DM was fundamentally a vascular disease, commonly associated with hypertension, macrovascular events, and microvascular complications. It often progressed to hypertension, which was a major determinant of cardiovascular morbidity and mortality in this patient population (45). When IR increased, the risk of coronary heart disease in non-diabetic individuals was higher than in those with diabetes, indicating that IR posed a greater risk for coronary heart disease than T2DM itself (46). IR, blood glucose levels, and inflammatory cytokines were significant risk factors for cardiovascular events in patients with diabetes complicated by coronary heart disease. Additionally, inflammation mediated by hyperglycemia and IR was considered a significant risk factor in the development of atherosclerosis, with C-reactive protein (CRP) often serving as a predictor of cardiovascular events (47, 48). Serum adiponectin levels, IR, and inflammatory cytokines were closely linked to diabetes complicated by coronary heart disease. Factors such as reduced insulin sensitivity, diminished blood pressure regulation, dysfunction of the fibrinolytic system, and heightened inflammatory responses could all affect the severity of vascular endothelial injury (47, 49). IR also played a crucial role in the pathogenesis and progression of target organ damage induced by hypertension, such as left ventricular hypertrophy, atherosclerosis, and chronic kidney disease (50). Therefore, focusing on the treatment of diabetes and IR was fundamental and essential for the prevention and management of cardiovascular diseases.
Thirdly, as the central pathological change in diabetes, IR was a primary therapeutic target in the treatment of patients with diabetes. Obesity and lack of physical activity were the main contributing factors to IR (51). The treatment strategies for IR primarily involved inhibiting fat synthesis in the liver, stimulating fat oxidation, and increasing muscle mass. These approaches aimed to reduce ectopic lipid accumulation, enhance insulin sensitivity, and ultimately prevent or delay the onset and progression of T2DM (16). Non-pharmacological management, including exercise, dietary changes, and behavioral modification, also plays a key role in managing insulin resistance and diabetes (52). Regular physical activity helps with weight reduction, improves skeletal muscle mass and VO2peak, and enhances insulin sensitivity (53–55). Additionally, dietary adjustments and behavioral strategies contribute to lowering HbA1c levels and improving overall metabolic control (56). Following these lifestyle interventions, pharmacological treatments are often necessary to further target the underlying mechanisms of insulin resistance and improve glycemic control. A variety of drugs were employed in the prevention and treatment of IR, including insulin, sulfonylureas (such as carbutamide and tolbutamide), biguanides (such as metformin, phenformin, and buformin), thiazolidinediones, incretins, sodium/glucose co-transporter-2 inhibitors, and adipose and anti-obesity agents aimed at reducing weight (17). These drugs worked through different mechanisms to improve insulin sensitivity and regulate blood glucose levels. Insulin facilitated glucose uptake into cells, while sulfonylureas stimulated pancreatic beta cells to increase insulin secretion (57, 58). Biguanides reduced hepatic glucose production and enhanced insulin sensitivity in peripheral tissues (59). Thiazolidinediones activated PPAR-γ receptors, promoting glucose uptake in adipocytes and reducing inflammation (60). Incretins, such as GLP-1 receptor agonists, increased insulin secretion and suppressed glucagon, thus improving postprandial glucose control (61). SGLT-2 inhibitors decreased glucose reabsorption in the kidneys, leading to increased glucose excretion in the urine (62). Additionally, anti-obesity agents targeted body weight reduction and fat accumulation, improving insulin sensitivity by modulating appetite and fat metabolism (63). Acupuncture, originating from China, was increasingly utilized worldwide for the treatment of diseases related to IR (64, 65). Acupuncture has the ability to correct metabolic dysregulation (65), lower hyperglycemia (66), improve body weight (67), suppress appetite (68), reduce lipids (69), exert anti-inflammatory effects (70), improve changes in sympathetic nervous system activity (71), and address insulin signaling deficits (72), as well as enhance insulin sensitivity (73).
5 Advantages and shortcomings
As far as we knew, this was the first time to conduct a comprehensive analysis of research in the field of diabetes and insulin resistance had been conducted, with special attention to its trends and hot spots, which would be very useful for scholars and researchers interested in this topic. Firstly, given the authority and comprehensiveness of the WOSCC, we only searched this database and may have overlooked the important value and information in other important database literature (e.g., PubMed, Scopus, Google Scholar, CrossRef). Secondly, we only included papers primarily written in English in our analysis, which may have resulted in a significant omission of excellent literature published in other languages. Finally, due to the continuous updates of the database and publication time, some recently published excellent papers with potential value may not have been fully researched and cited, which may lead to underestimation of the value and quality of the latest publications in bibliometric analysis results.
6 Conclusion
Using bibliometric methods, it was discovered that research in the fields of diabetes and IR was receiving increasing attention, with trends and hotspots being summarized into the following three key points. The association between IR, diabetes, and obesity has emerged as a popular research topic. Cardiovascular diseases secondary to diabetes and IR constitute another focal point of interest among researchers. As the core pathological change in diabetes, IR improvement was the primary therapeutic target in diabetes management. In the future, further in-depth research on the relationship between diabetes and IR, as well as its underlying mechanisms, held significant importance for the treatment and prevention of these diseases.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
SZ: Writing – original draft, Resources. HY: Writing – review & editing, Resources. WS: Writing – review & editing. JL: Writing – review & editing. JX: Writing – review & editing. DC: Resources, Writing – review & editing. BS: Writing – review & editing, Conceptualization. XW: Writing – review & editing, Conceptualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Key Research and Development Program of China (No. 2019YFC1709900) and Jilin Provincial Natural Science Foundation Project (No. YDZJ202301ZYTS140).
Acknowledgments
We extend our gratitude to all authors involved in the bibliometric and visualization studies on diabetes and IR.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Du, Y, Dennis, B, Rhodes, SL, Sia, M, Ko, J, Jiwani, R, et al. Technology-assisted self-monitoring of lifestyle behaviors and health indicators in diabetes: qualitative study. JMIR Diabetes. (2020) 5:e21183. doi: 10.2196/21183
2. Zarora, R, Immanuel, J, Chivese, T, MacMillan, F, and Simmons, D. Effectiveness of integrated diabetes care interventions involving diabetes specialists working in primary and community care settings: A systematic review and Meta-analysis. Int J Integr Care. (2022) 22:11. doi: 10.5334/ijic.6025
3. Sun, H, Saeedi, P, Karuranga, S, Pinkepank, M, Ogurtsova, K, Duncan, BB, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
4. Majjad, A, Errahali, Y, Toufik, H, Djossou, JH, Ghassem, MA, Kasouati, J, et al. Musculoskeletal disorders in patients with diabetes mellitus: a cross-sectional study. Int J Rheumatol. (2018) 2018:3839872. doi: 10.1155/2018/3839872
5. Hu, L, He, F, Huang, M, Zhao, Q, Cheng, L, Said, N, et al. SPARC promotes insulin secretion through down-regulation of RGS4 protein in pancreatic β cells. Sci Rep. (2020) 10:17581. doi: 10.1038/s41598-020-74593-w
6. Niemann, MJ, Tucker, LA, Bailey, BW, and Davidson, LE. Strength training and insulin resistance: the mediating role of body composition. J Diabetes Res. (2020) 2020:7694825–11. doi: 10.1155/2020/7694825
7. Chockalingam, A, Natarajan, P, Thanikachalam, P, and Pandiyan, R. Insulin resistance: the inconvenient truth. Mo Med. (2021) 118:119–21.
8. Thornton, PS, Stanley, CA, and De Leon, DD. Congenital Hyperinsulinism: an historical perspective. Horm Res Paediatr. (2022) 95:631–7. doi: 10.1159/000526442
9. Xiong, Q-Y, Xiong, C-Q, Wang, L-Z, and Gao, J-L. Effect of sidt2 gene on cell insulin resistance and its molecular mechanism. J Diabetes Res. (2020) 2020:4217607–8. doi: 10.1155/2020/4217607
10. Bungau, S, Behl, T, Tit, DM, Banica, F, Bratu, OG, Diaconu, CC, et al. Interactions between leptin and insulin resistance in patients with prediabetes, with and without NAFLD. Exp Ther Med. (2020) 20:1. doi: 10.3892/etm.2020.9327
11. Urakaze, M, Kobashi, C, Satou, Y, Shigeta, K, Toshima, M, Takagi, M, et al. The beneficial effects of Astaxanthin on glucose metabolism and modified low-density lipoprotein in healthy volunteers and subjects with prediabetes. Nutrients. (2021) 13:4381. doi: 10.3390/nu13124381
12. Yaribeygi, H, Farrokhi, FR, Butler, AE, and Sahebkar, A. Insulin resistance: review of the underlying molecular mechanisms. J Cell Physiol. (2019) 234:8152–61. doi: 10.1002/jcp.27603
13. Zhao, X-P, Li, D, Li, C-L, Zhang, Y-N, Zhao, N-R, and Xu, J-X. Knowledge mapping of diabetic foot research based on web of science database: A bibliometric analysis. Medicine. (2023) 102:e34053. doi: 10.1097/MD.0000000000034053
14. Shi, L, Li, C, Wang, J, Zhong, H, Wei, T, Fan, W, et al. The intellectual base and global trends in inflammation of diabetic kidney disease: a bibliometric analysis. Ren Fail. (2023) 45:2270061. doi: 10.1080/0886022X.2023.2270061
15. Chen, H, Wei, F, Chen, X, and Chen, K. Global research trends in gestational diabetes mellitus from 2000 to 2020: A bibliometric study. Z Geburtshilfe Neonatol. (2022) 226:197–204. doi: 10.1055/a-1756-5518
16. Lee, S-H, Park, S-Y, and Choi, CS. Insulin resistance: from mechanisms to therapeutic strategies. Diabetes Metab J. (2022) 46:15–37. doi: 10.4093/dmj.2021.0280
17. Bailey, CJ. Insulin resistance: impact on therapeutic developments in diabetes. Diab Vasc Dis Res. (2019) 16:128–32. doi: 10.1177/1479164119827570
18. Chen, K, Wang, Y, Li, D, Li, J, Huang, Y, Huang, M, et al. Impact of diverse aerobic exercise plans on glycemic control, lipid levels, and functional activity in stroke patients with type 2 diabetes mellitus. Front Endocrinol. (2024) 15:1389538. doi: 10.3389/fendo.2024.1389538
19. Zheng, S, Wang, Y, Geng, J, Liu, X, and Huo, L. Global trends in research on MOG antibody-associated disease: bibliometrics and visualization analysis. Front Immunol. (2024) 15:1278867. doi: 10.3389/fimmu.2024.1278867
20. Sun, W, Wu, W, Dong, X, and Yu, G. Frontier and hot topics in the application of hydrogel in the biomedical field: a bibliometric analysis based on CiteSpace. J Biol Eng. (2024) 18:40. doi: 10.1186/s13036-024-00435-2
21. Arruda, H, Silva, ER, Lessa, M, Proença, D, and Bartholo, R. VOSviewer and Bibliometrix. J Med Libr Assoc. (2022) 110:392–5. doi: 10.5195/jmla.2022.1434
22. Tang, F, Jiang, C, Chen, J, Wang, L, and Zhao, F. Global hotspots and trends in myofascial pain syndrome research from 1956 to 2022: a bibliometric analysis. Medicine. (2023) 102:e33347. doi: 10.1097/MD.0000000000033347
23. Jiang, R, Cong, Z, Zheng, L, Zhang, L, Guan, Q, Wang, S, et al. Global research trends in regulating gut microbiome to improve type 2 diabetes mellitus: bibliometrics and visual analysis. Front Endocrinol. (2024) 15:1401070. doi: 10.3389/fendo.2024.1401070
24. Zhang, R, Ge, Y, Xia, L, and Cheng, Y. Bibliometric analysis of development trends and research hotspots in the study of data mining in nursing based on CiteSpace. J Multidiscip Healthc. (2024) 17:1561–75. doi: 10.2147/JMDH.S459079
25. Luo, Z, Fabre, G, and Rodwin, VG. Meeting the challenge of diabetes in China. Int J Health Policy Manag. (2020) 9:47–52. doi: 10.15171/ijhpm.2019.80
26. Conlin, PR, Burke, BV, Hobbs, C, Hurren, KM, Lang, AE, Morrison, JW, et al. Management of type 2 diabetes mellitus: synopsis of the department of veterans affairs and department of defense clinical practice guideline. Mayo Clin Proc. (2024). doi: 10.1016/j.mayocp.2024.04.014
27. Litkowski, EM, Logue, MW, Zhang, R, Charest, BR, Lange, EM, Hokanson, JE, et al. Mendelian randomization study of diabetes and dementia in the million veteran program. Alzheimers Dement. (2023) 19:4367–76. doi: 10.1002/alz.13373
28. Fleming, BB, Greenfield, S, Engelgau, MM, Pogach, LM, Clauser, SB, and Parrott, MA. The diabetes quality improvement project: moving science into health policy to gain an edge on the diabetes epidemic. Diabetes Care. (2001) 24:1815–20. doi: 10.2337/diacare.24.10.1815
29. Desai, J, Geiss, L, Mukhtar, Q, Harwell, T, Benjamin, S, Bell, R, et al. Public health surveillance of diabetes in the United States. J Public Health Manage Pract. (2003) 9:S44–51. doi: 10.1097/00124784-200311001-00008
30. Oklahoma State Medical Association. National Institutes of Health, Patient Page 48: 50 ways to prevent diabetes. J Okla State Med Assoc. (2004) 97:205–6.
31. Vinicor, F, and Jack, L. 25 years and counting: Centers for Disease Control and Prevention identifies opportunities and challenges for diabetes prevention and control. Ann Intern Med. (2004) 140:943–4. doi: 10.7326/0003-4819-140-11-200406010-00034
32. Ternák, G, Németh, M, Rozanovic, M, and Bogár, L. Antibiotic consumption patterns in European countries might be associated with the prevalence of type 1 and 2 diabetes. Front Endocrinol. (2022) 13:870465. doi: 10.3389/fendo.2022.870465
33. Saini, V. Molecular mechanisms of insulin resistance in type 2 diabetes mellitus. World J Diabetes. (2010) 1:68–75. doi: 10.4239/wjd.v1.i3.68
34. DeFronzo, RA, Hendler, R, and Simonson, D. Insulin resistance is a prominent feature of insulin-dependent diabetes. Diabetes. (1982) 31:795–801. doi: 10.2337/diab.31.9.795
35. Taylor, R. Insulin resistance and type 2 diabetes. Diabetes. (2012) 61:778–9. doi: 10.2337/db12-0073
36. Yu, T, Gao, M, Yang, P, Pei, Q, Liu, D, Wang, D, et al. Topical insulin accelerates cutaneous wound healing in insulin-resistant diabetic rats. Am J Transl Res. (2017) 9:4682–93.
37. Kahn, SE, Hull, RL, and Utzschneider, KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. (2006) 444:840–6. doi: 10.1038/nature05482
38. Dandona, P, Aljada, A, and Bandyopadhyay, A. Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol. (2004) 25:4–7. doi: 10.1016/j.it.2003.10.013
39. Weyer, C, Funahashi, T, Tanaka, S, Hotta, K, Matsuzawa, Y, Pratley, RE, et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab. (2001) 86:1930–5. doi: 10.1210/jcem.86.5.7463
40. Gallagher, EJ, Leroith, D, and Karnieli, E. The metabolic syndrome--from insulin resistance to obesity and diabetes. Med Clin North Am. (2011) 95:855–73. doi: 10.1016/j.mcna.2011.06.001
41. Mihai, M, Vladut, S, Sonia-Teodora, L, Laura Mihaela, S, Victoria, N, Irina Elena, M, et al. Correlation between overweight, obesity, gestational diabetes mellitus, Adipokines (Adipolin and adiponectin), and adverse pregnancy outcomes: A pilot study. Medicina (Kaunas). (2024) 60:1544. doi: 10.3390/medicina60091544
42. Mogensen, CS, Nygaard, M, Kampmann, U, Mølgaard, C, Magkos, F, and Geiker, NRW. Maternal glucose homeostasis during pregnancy in women with overweight or obesity and offspring metabolic health. Sci Rep. (2024) 14:21398. doi: 10.1038/s41598-024-72223-3
43. Dj, H, and Tg, H. Maternal diet during pregnancy and adaptive changes in the maternal and fetal pancreas have implications for future metabolic health. Front Endocrinol. (2024) 15:1456629. doi: 10.3389/fendo.2024.1456629
44. Maor-Sagie, E, Hallak, M, Haggiag, N, Naeh, A, Toledano, Y, and Gabbay-Benziv, R. Timing of gestational diabetes diagnosis and progression to type 2 diabetes: A comparative analysis. Diabetes Res Clin Pract. (2024) 214:111782. doi: 10.1016/j.diabres.2024.111782
45. Ko, S-H, Cao, W, and Liu, Z. Hypertension management and microvascular insulin resistance in diabetes. Curr Hypertens Rep. (2010) 12:243–51. doi: 10.1007/s11906-010-0114-6
46. Kim, J, Chae, YK, and Chernoff, A. The risk for coronary heart disease according to insulin resistance with and without type 2 diabetes. Endocr Res. (2013) 38:195–205. doi: 10.3109/07435800.2013.766800
47. Festa, A, D’Agostino, R, Howard, G, Mykkänen, L, Tracy, RP, and Haffner, SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: the insulin resistance atherosclerosis study (IRAS). Circulation. (2000) 102:42–7. doi: 10.1161/01.cir.102.1.42
48. Wang, C, Li, F, Guo, J, Li, C, Xu, D, and Wang, B. Insulin resistance, blood glucose and inflammatory cytokine levels are risk factors for cardiovascular events in diabetic patients complicated with coronary heart disease. Exp Ther Med. (2018) 15:1515–9. doi: 10.3892/etm.2017.5584
49. Xu, W, Tian, M, and Zhou, Y. The relationship between insulin resistance, adiponectin and C-reactive protein and vascular endothelial injury in diabetic patients with coronary heart disease. Exp Ther Med. (2018) 16:2022–6. doi: 10.3892/etm.2018.6407
50. Mancusi, C, Izzo, R, di Gioia, G, Losi, MA, Barbato, E, and Morisco, C. Insulin resistance the hinge between hypertension and type 2 diabetes. High Blood Press Cardiovasc Prevent. (2020) 27:515–26. doi: 10.1007/s40292-020-00408-8
51. Altaf, Q-A, Barnett, AH, and Tahrani, AA. Novel therapeutics for type 2 diabetes: insulin resistance. Diabetes Obes Metab. (2015) 17:319–34. doi: 10.1111/dom.12400
52. Khursheed, R, Singh, SK, Wadhwa, S, Kapoor, B, Gulati, M, Kumar, R, et al. Treatment strategies against diabetes: success so far and challenges ahead. Eur J Pharmacol. (2019) 862:172625. doi: 10.1016/j.ejphar.2019.172625
53. Bushey, E, Wu, Y, Wright, A, and Pescatello, L. The influence of physical activity and diet Mobile apps on cardiovascular disease risk factors: Meta-review. J Med Internet Res. (2024) 26:e51321. doi: 10.2196/51321
54. Calcaterra, V, Magenes, VC, Bianchi, A, Rossi, V, Gatti, A, Marin, L, et al. How can promoting skeletal muscle health and exercise in children and adolescents prevent insulin resistance and type 2 diabetes? Life. (2024) 14:1198. doi: 10.3390/life14091198
55. Kindlovits, R, Sousa, AC, Viana, JL, Milheiro, J, Oliveira, BM, Marques, F, et al. Eight weeks of intermittent exercise in hypoxia, with or without a low-carbohydrate diet, improves bone mass and functional and physiological capacity in older adults with type 2 diabetes. Nutrients. (2024) 16:1624. doi: 10.3390/nu16111624
56. Manoogian, ENC, Wilkinson, MJ, O'Neal, M, Laing, K, Nguyen, J, van, D, et al. Time-restricted eating in adults with metabolic syndrome: a randomized controlled trial. Ann Intern Med. (2024) 177:1462–70. doi: 10.7326/M24-0859
57. Wang, J, Yu, J, Zhang, Y, Kahkoska, AR, Wang, Z, Fang, J, et al. Glucose transporter inhibitor-conjugated insulin mitigates hypoglycemia. Proc Natl Acad Sci USA. (2019) 116:10744–8. doi: 10.1073/pnas.1901967116
58. Jc, H. Misunderstandings and controversies about the insulin-secreting properties of antidiabetic sulfonylureas. Biochimie. (2017) 143:3–9. doi: 10.1016/j.biochi.2017.07.002
59. L H,. Metformin and systemic metabolism. Trends Pharmacol Sci. (2020) 41:868–81. doi: 10.1016/j.tips.2020.09.001
60. Ahsan, W. The journey of Thiazolidinediones as modulators of PPARs for the management of diabetes: a current perspective. Curr Pharm Des. (2019) 25:2540–54. doi: 10.2174/1381612825666190716094852
61. Müller, TD, Finan, B, Bloom, SR, D'Alessio, D, Drucker, DJ, Flatt, PR, et al. Glucagon-like peptide 1 (GLP-1). Mol Metab. (2019) 30:72–130. doi: 10.1016/j.molmet.2019.09.010
62. Si, T, Je, B, Ki, R, and Al, B. SGLT2 inhibitors as adjunctive therapy for type 1 diabetes: balancing benefits and risks. Lancet Diab Endocrinol. (2019) 7:949–58. doi: 10.1016/S2213-8587(19)30154-8
63. Tong, Y, Xu, S, Huang, L, and Chen, C. Obesity and insulin resistance: pathophysiology and treatment. Drug Discov Today. (2022) 27:822–30. doi: 10.1016/j.drudis.2021.11.001
64. Peplow, PV. Electroacupuncture treatment of insulin resistance in diabetes mellitus. Acupunct Med. (2015) 33:347–9. doi: 10.1136/acupmed-2015-010942
65. Liang, F, and Koya, D. Acupuncture: is it effective for treatment of insulin resistance? Diabetes Obes Metab. (2010) 12:555–69. doi: 10.1111/j.1463-1326.2009.01192.x
66. Yc, C, Yi, C, Cm, L, Sw, C, Th, H, Wj, H, et al. Electroacupuncture combined with acarbose improves insulin sensitivity via peroxisome proliferator-activated receptor γ activation and produces a stronger glucose-lowering effect than acarbose alone in a rat model of steroid-induced insulin resistance. Acupunct Med. (2020) 38:335–42. doi: 10.1177/0964528419901135
67. Rerksuppaphol, L, and Rerksuppaphol, S. Efficacy of short duration versus conventional electroacupuncture in the treatment of obesity: a randomized crossover study. J Trad Chinese Med. (2022) 42:256–63. doi: 10.19852/j.cnki.jtcm.2022.02.006
68. Cabýoglu, MT, Ergene, N, and Tan, U. The treatment of obesity by acupuncture. Int J Neurosci. (2006) 116:165–75. doi: 10.1080/00207450500341522
69. Yin, Y, Zhao, Q, Li, S, Jiang, H, Yin, C, Chen, H, et al. Efficacy of acupuncture and moxibustion therapy for simple obesity in adults: a meta-analysis of randomized controlled trials. Medicine. (2022) 101:e31148. doi: 10.1097/MD.0000000000031148
70. Xu, T, Yu, Z, Liu, Y, Lu, M, Gong, M, Li, Q, et al. Hypoglycemic effect of electroacupuncture at ST25 through neural regulation of the pancreatic intrinsic nervous system. Mol Neurobiol. (2022) 59:703–16. doi: 10.1007/s12035-021-02609-1
71. Lansdown, A, and Rees, DA. The sympathetic nervous system in polycystic ovary syndrome: a novel therapeutic target? Clin Endocrinol. (2012) 77:791–801. doi: 10.1111/cen.12003
72. Benrick, A, Maliqueo, M, Johansson, J, Sun, M, Wu, X, Mannerås-Holm, L, et al. Enhanced insulin sensitivity and acute regulation of metabolic genes and signaling pathways after a single electrical or manual acupuncture session in female insulin-resistant rats. Acta Diabetol. (2014) 51:963–72. doi: 10.1007/s00592-014-0645-4
Keywords: diabetes, insulin resistance, bibliometric, visual analysis, CiteSpace, VOSviewer
Citation: Zhang S, Yan H, Cao D, Sun W, Li J, Xu J, Song B and Wu X (2024) Research hotspots and trends in diabetes and insulin resistance: a bibliometric analysis. Front. Nutr. 11:1480491. doi: 10.3389/fnut.2024.1480491
Edited by:
Ourlad Alzeus G. Tantengco, University of the Philippines Manila, PhilippinesReviewed by:
Manuel Vidal Jr, San Beda University, PhilippinesSridhar R. Gumpeny, Endocrine and Diabetes Centre, India
Copyright © 2024 Zhang, Yan, Cao, Sun, Li, Xu, Song and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bailin Song, Y3pkc29uZ2JhaWxpbkAxMjYuY29t; Xingquan Wu, d3V4aW5ncXVhbjIwMDVAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Shaobo Zhang
Shaobo Zhang Huixin Yan
Huixin Yan Di Cao
Di Cao Weichen Sun1,3
Weichen Sun1,3 Bailin Song
Bailin Song Xingquan Wu
Xingquan Wu