- 1School of Public Health, College of Health Science and Medicine, Wolaita Sodo University, Sodo, Ethiopia
- 2Department of Human Nutrition, Wolaita Zone Health Office, Sodo, Ethiopia
- 3Data Quality Office, Nifas Silk Lafto Worda 11, Addis Ababa, Ethiopia
Overweight and obesity are body mass index (BMI) for age Z-score > +1SD and > +2SD, respectively. Despite its largest contribution to overweight/obesity, there is little attention in our country about fast-food consumption. Hence, this study aimed to assess the prevalence of overweight/obesity and its association with fast-food consumption among adolescents in Southern Ethiopia. From 14 June 2022 to 15 July 2022, a cross-sectional study design was conducted using a structured questionnaire and anthropometric measurements, with a sample size of 563. The data were coded, cleaned, and imported into EPI-INF version 7.2 before being exported to SPSS version 25 for analysis. All variables with p-values less than or equal to 0.25 in bivariate logistic regression were candidate variables for multivariable logistic regression. The response rate of this study was 97%. Based on BMI, the combined prevalence of overweight/obesity was 6.0% (95% CI: 4.2–8.4%). Adolescents who are female, come from high-income families, and eat fast-food frequently are more likely to be overweight or obese. Future health initiatives aimed at lowering the prevalence of overweight and obesity in adolescents should pay special attention to female adolescents and those from high-income families.
Introduction
Overweight and obesity are described by body mass index (BMI) for age Z-score > +1SD and > +2SD above the WHO Growth Reference median, respectively. Overweight is BMI ≥ 85th to <95th percentile for age and sex, and obesity is BMI ≥ 95th percentile for age and sex (1). Overweight/obesity among adolescents is dramatically increasing and becoming a global concern. In 2022, more than 390 million children and adolescents between the age of 5 and 19 years were overweight, with 160 million of them suffering from obesity (2). In addition, overweight and obesity are the main contributors to type 2 diabetes mellitus, insulin resistance, cardiovascular disease, and cancer-related consequences. Previously, overweight and obesity were an issue in high-income countries, but currently, it is expanding to low-income and middle-income countries, especially in metropolitan areas (3, 4). Ethiopia is also experiencing a spike in both overweight and obesity. Therefore, a combined pooled prevalence of overweight and obesity among children and adolescents in Ethiopia suggested 11.30% (95% CI: 8.71, 13.88), whereas the individual pooled prevalence was 8.92 and 2.39%, respectively (5). Recent research suggested that increased availability to fast-food restaurants and a higher intake of ultra-processed food might increase the prevalence of metabolic syndrome, particularly abdominal obesity and diabetes mellitus (6, 7). Several studies have also shown that increased fast-food consumption of adolescents is associated with a rise in overweight and obesity (8–10).
Even though the causes of obesity are thought to be numerous, fast food has been related to the issue in many nations due to its rising popularity, high-calorie content, and large serving sizes (11). A study in college students found that frequent fast-food consumption raised the prevalence of obesity from 3.6 to 35.4% for those who ate fast food less than four times per week and more than four times per week, respectively (12). Fast food is a mass-produced food designed for commercial resale, with a strong priority placed on service speed and consumption outside of the home (13). It is calorie-dense, lacks micronutrients, has a high glycemic index and low fiber content, and is served in large quantities (14). Additionally, it contains a lot of saturated and trans fatty acids (15).
People’s eating habits of people are changing in Ethiopia, with more urban dwellers preferring ready-to-eat (quick) foods accessible in open markets and low-cost eateries (16). Cheap, nutrient-poor, and energy-dense foods are currently simpler to find than nutritious foods. In metropolitan areas, the intake of processed meats, sweetened beverages, saturated fats, cholesterol, and sodium is increasing, according to a recent study (17).
A number of studies carried out abroad show an adverse association between fast food and overweight or obesity. In Indonesia, a study suggested both waist circumference and BMI have a significantly negative association with increased fast food consumption (18). Another study, in the UK, indicated participants who consumed fast food on a weekly basis had ~20% lower odds of being overweight than those who consumed it rarely or never (19).
One might expect that youth who are more educated would make better choices regarding nutrition; however, regardless of their level of education, adolescents are becoming increasingly overweight or obese. Studies in Ethiopia, however, have ignored young, preschoolers concentrating on adolescent students instead. In Ethiopia, the economy is growing fast, facing rural–urban migration problems. Due to this transition, the food habits of people are changing with more people in urban areas eating outside the home and giving preference to fast foods (16). Wolaita Sodo is one of the fastest growing cities in the country, with new urban region developments growing largely in all directions of the town (20).
Despite being the main cause of overweight and obesity, fast-food consumption has received little attention in our country. The goal of this study was to concentrate more on fast-food consumption as a primary covariate, in Sodo town, at the community level.
In addition, conducting this study at the community level enabled us to include both in-school and out-of-school adolescents. Moreover, investigating the prevalence of overweight/obesity and its associated factors is so essential to stimulating action before the onset of chronic disease. It can also serve as a piece of evidence for the development of national food policies, programs, and dietary guidelines as this is the first community-based study in a study area.
The hypothesis of the study is, ‘Adolescents who eat fast food frequently have a higher likelihood of being overweight or obese than those who eat fast food less frequently, in Sodo town.’
Methods
Study setting, design, and period
From the 14th of June up to the 15th of July 2022, a community-based cross-sectional study was carried out in Wolaita Sodo town, southern Ethiopia. The town has 6°54′ N latitude, 39°45′ E longitude, and an altitude of roughly 1900 m; it is situated 320 kilometers southwest of capital city of Ethiopia of Addis Ababa and 160 kilometers west of the regional town of Hawasa. The Federal Democratic Republic of Central Statistics Agency of Ethiopia reported in 2018 that the town had a total population of 132,271 (62,340 men and 69,931 women), of whom 3,263 were young people (aged 15–24 years) (21). According to recent demographic data in the administrative office of town, the town is divided into seven sub-cities, which have 46,956 households (HH) and a population of 286,566.
Population
Adolescents in Wolaita Sodo town were the source population, whereas those in three selected subcities of Wolaita Sodo town were the study population. Individual adolescents from selected households were included in the study. However, adolescents who had a physical disability (unable to stand erect), mental disability, pregnancy, or edema due to some other pathological causes were excluded.
Sample size determination and sampling procedure
Using a single population proportion formula, the sample size was calculated under the following assumptions: a 95% confidence level, a margin of error of 4%, a design effect of 1.5, and a non-response rate of 5%. We used the outcome variable overweight/obesity, which has a combined prevalence of 18.2% among school-aged adolescents in Addis Ababa, to calculate the size of our sample (22). Our final sample was 563.
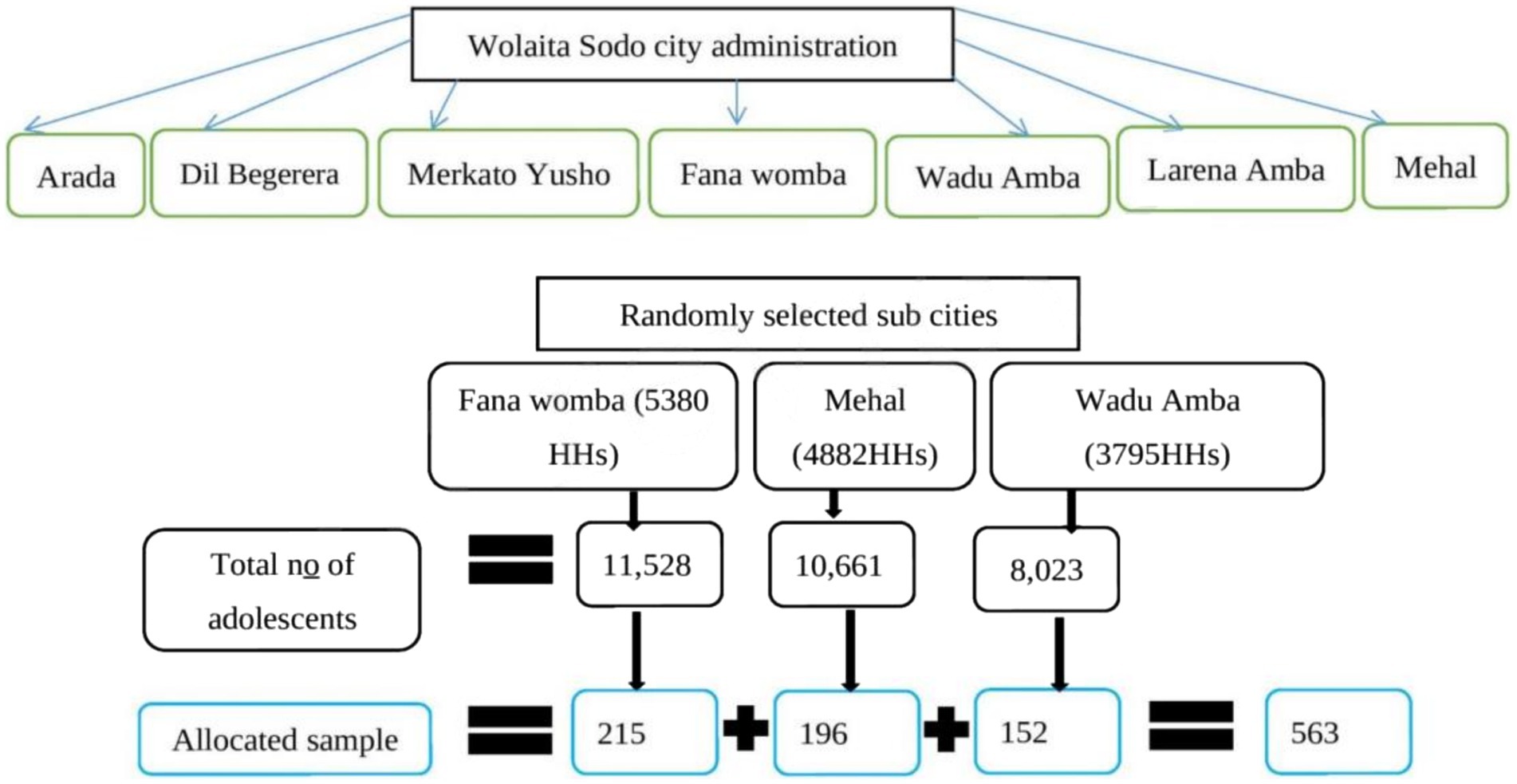
Currently, there are seven (7) sub-cities in Wolaita Sodo town administration. Initially, three sub-cities (Wadu Amba, Fana Womba, and Mehal) were randomly selected, and the census was conducted to determine the total number of adolescents in each sub-city. During the process of the census, the households with one or more adolescents were given a new consecutive code, and the number of adolescents was recorded.
Using the new codes, labeling was done, and the total number of adolescents in each sub-city was calculated. Then, the total sample size was allocated to each sub-city proportionally to the total number of households with adolescents within the sub-city. Finally, study units were selected by the systematic random sampling method. The sampling procedure is shown in Figure 1.
Study measures/variables
Overweight/obesity was the outcome variable, whereas socio-demographic variables, fast-food consumption, physical activity, alcohol intake, and sedentary lifestyle characteristics were the independent variables in this study.
Operational definition
Overweight: BMI-for-age z-score is greater than +1 SD above the WHO growth reference median.
Obesity: BMI-for-age z-score is greater than +2 SD above the WHO growth reference media.
Fast food: Foods that are packaged, easily accessible from vending machines, simply prepared, and served quickly (such as pizza, burgers, chocolate, ice cream, cookies/cake, chips, soft drinks, and biscuits).
Frequent fast-food consumers: Those adolescents who took fast food two or more times in the last 1 week.
Lack of cooking skills: Lack of ability to perform tasks related to the preparation of food at home.
Alcohol intake: Intake of alcoholic beverages (beer, wine, whiskey, Areke, Tela, Tej, etc.) for a non-medicinal purpose within the last 1 month.
Sometimes take alcohol: Intake of alcoholic beverages less than or equal to one time a week.
Rarely take alcohol: Intake of alcoholic beverages less than or equal to one time a month.
Data collection procedures
Data associated with socio-demographic variables, dietary information, habits of fast-food consumption, and the like were collected using face-to-face interviews using a questionnaire developed after a thorough review of literature. Obesity index data such as waist and hip circumferences for calculating waist–hip ratio (WHR), and height and weight for computing BMI, were collected. Waist and hip circumference were measured by an anthropometric tape meter; the height of subjects was measured by a standard meter stick; and the weight of study subjects was taken to the nearest 0.1 kg using a calibrated digital balance in standing position by trained health professionals.
Height was measured to the nearest 0.5 cm after participants removed their heavy clothing and shoes, and waist and hip circumference measurements were taken at the narrowest and widest areas, respectively. Data were collected on weekend days (Saturday and Sunday) in order to address school-going adolescents.
Data quality assurance
Two days of training for data collectors and supervisors was given prior to the actual survey. Standardization was done among 10 adolescents before the actual survey and systematized based on the result of anthropometric measurements. All three data collectors were degree holders in public health. Three assistants (one for each data collector) were assigned. All six of them speak local as well as Amharic language. A pretest was conducted on 5% of the questionnaire in the Merkato Yusho sub-city, which was not included in actual data collection. Appropriate modifications were made after analyzing the pretest results before the actual data collection. The reliability test results obtained Cronbach’s alpha value of 0.89; then, the instrument was declared reliable.
Data processing and analysis
Data were cleaned, coded, and entered into EPI-INFO version 7.2 before being exported and analyzed in SPSS version 25. Anthropometric data and other crucial variables were imported into WHO Anthro-plus software, which uses WHO 2007 population references to convert anthropometric data into body mass index for age z-score (BAZ) while taking age and sex into account. We calculated WHR using an open waist-to-hip ratio calculator and used the WHO cutoff points of 0.94 cm for men and 0.85 cm for women to determine central obesity. Frequency tables, proportions, and texts were used to present the descriptive statistics.
Pearson correlation was used to ascertain the correlation and strength of the association between consuming fast food and being overweight or obese. Bivariate logistic regression analyses were also conducted to evaluate the relationship between other independent variables and the dependent variable. In the multivariable logistic regression model, variables that exhibited an association (p-value of 0.25 in the bivariate analysis) were included. Outputs with p-values of ≤0.05 were deemed statistically significant. Before the data analysis, normality was checked for continuous variables using the Shapiro–Wilk normality test and visualized using Q-Q plots.
We found that they were derived from a population with a normal distribution (p-value >0.05). The Hosmer–Lemshow and variance inflation factor (VIF) tests were used to determine the model fitness and multicollinearity, respectively.
Results
Socio-demographic characteristics of the study subjects
A total of 546 adolescents participated in this study, with a response rate of 97%; 259 (47.4%) were early adolescents aged 10–14 years, and 287 (52.6%) were late adolescents aged 15–19 years. 325 (59.5%) of the respondents were females, and 221 (40.5%) were males. More than two-thirds 380 (69.6%) of them were protestant Christians, followed by Orthodox Tewahedo 140 (25.6%) and Muslim 20 (3.7%) and 64.7% had primary education (Table 1).
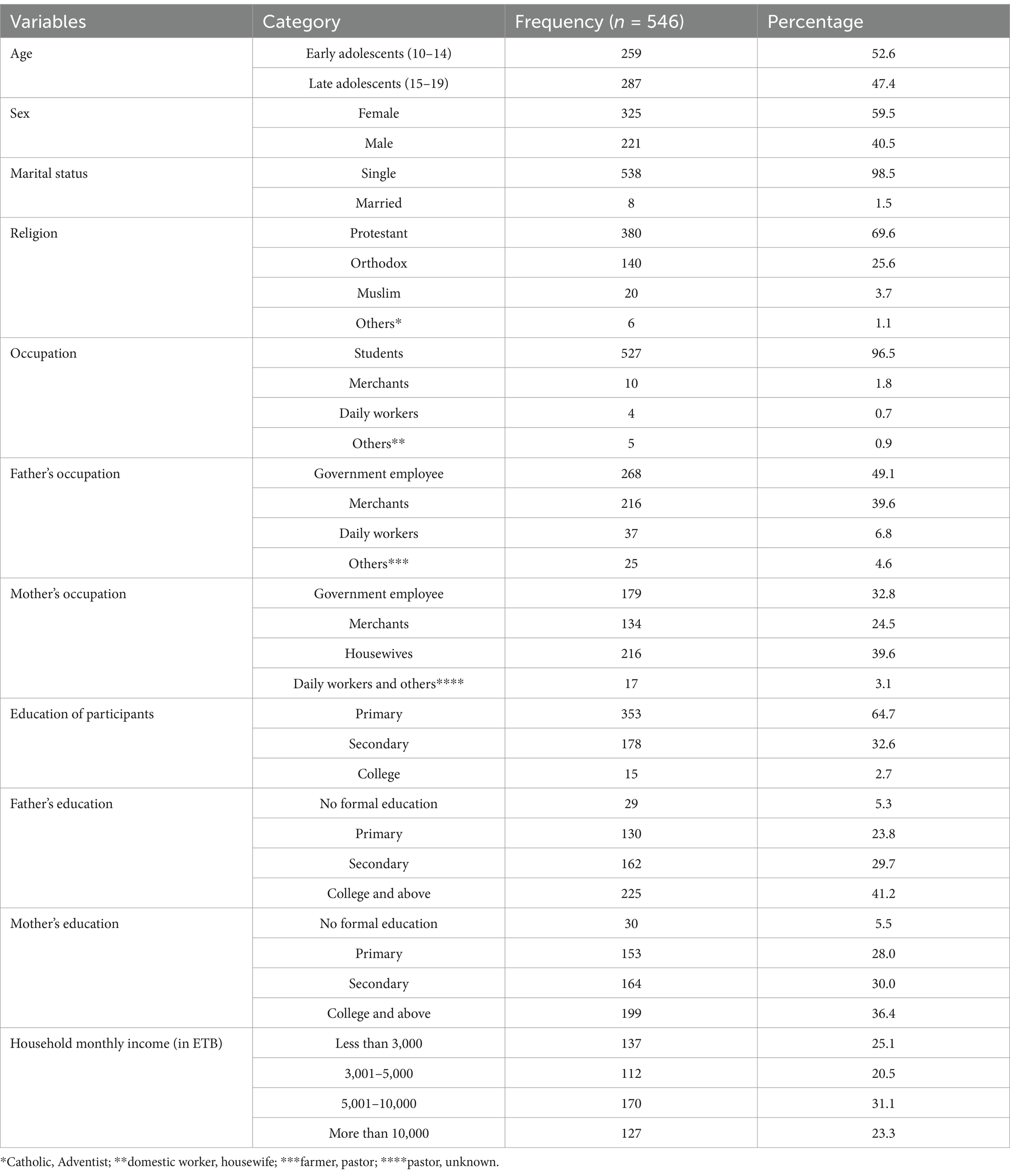
Table 1. Demographic and socioeconomic characteristics of adolescents in Wolaita Sodo town, Southern Ethiopia, 2022.
Habits and patterns of fast-food consumption of the respondents
Regarding fast-food consumption, 176 (32.2%) of the respondents were frequent (>2 times) consumers, of which 103 (58.5%) were females and 73 (41.5% were males); 130 (23.8%) of the respondents did not eat any kind of fast food in the past 7 days, and the remaining 416 (76.2%) ate fast food at least one time in the past 7 days. Of the 416 who ate fast food at least one time a week, approximately 115 (27.9%) consumed it from home, restaurants, and streets, 90 (21.6%) consumed it from restaurants and streets, and 77 (18.5%) ate only from their home. Most of the fast-food consumers, 132 (31.7%), preferred it because of its tasty nature, cheap price, recreational purpose, and convincing advertisements, followed by 102 (24.5%), who preferred it because of its tasty nature and convincing advertisements only (Table 2).
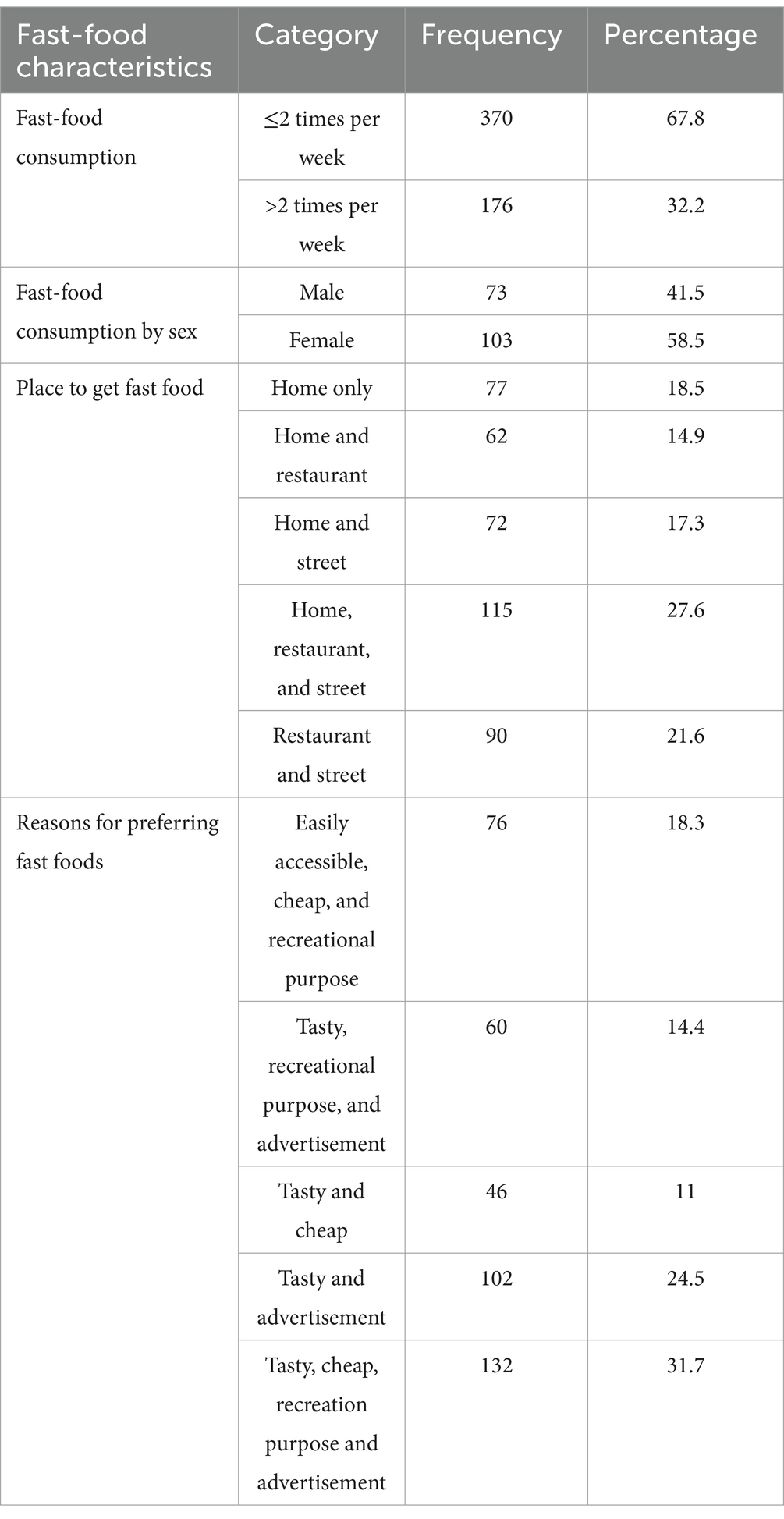
Table 2. Habits and patterns of fast-food consumption among adolescents in Wolaita Sodo town, Southern Ethiopia, 2022.
Dietary habits and meal patterns of adolescents
Three hundred twenty-five (59.5%) of the respondents said that they used fruits two to four times in the past 7 days, and 81 (14.8%) used them once per day. Regarding the intake of vegetables, 218 (39.9%) ate the vegetables two to four times in the past 1 week, followed by 129 (23.6%) who used more than two times per day. One hundred and eighty (33%) ate bread and cereals two to four times per week; 117 (21.4%) used them once a day, and 100 (18.3) ate more than two times per day. Regarding the animal source foods, 188 (34.4%), 133 (24.4%), 123 (22.5%), and 80 (14.7%) of the respondents ate meat and eggs one time a week, two to four times per week, less than once a week, and once per day, respectively. The majority of the adolescents (474) (86.8%) consumed snacks, with 201 (42.4%) taking them sometimes, 170 (35.6%) were daily users, and 103 (21.7%) use them rarely (Table 3).
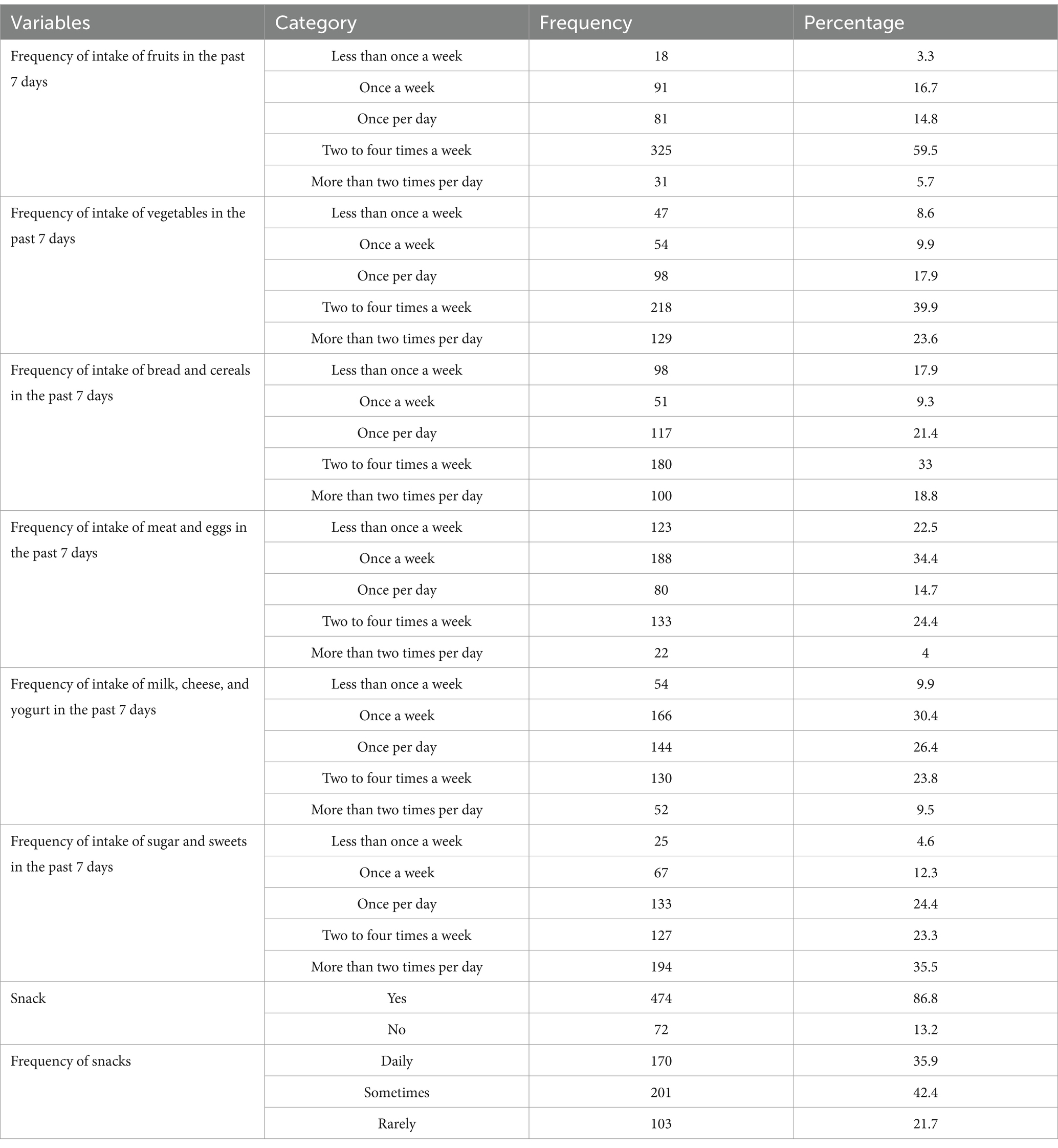
Table 3. Dietary habits and meal patterns of adolescents in Wolaita Sodo town, Southern Ethiopia, 2022.
Physical activity, alcohol intake, and sedentary lifestyle
The participants’ physical activity statuses related to sport and recreation revealed that only 23 (4.2%) participated in vigorous (high intensity) physical activity, whereas the majority (409, 74.9%) participated in moderate physical activity, and 114 (20.9%) of the participants had only low-intensity physical activity. Regarding the alcohol intake of the respondents, nearly all (530 [97.1%]) had no habits of taking any kind of alcoholic beverages. Moreover, the remaining 16 (2.9%) had habits of taking alcohol, of which seven (7) consumed sometimes and nine (9) took rarely. The sedentary behavior of the respondents showed that 269 (49.3%) of the adolescents spent watching TV programs, playing video games, or browsing the internet less than or equal to 120 min a day, whereas 277 (50.7%) spent more than 120 min a day. Regarding sleep duration, 94 (17.2%) spent short (< 8 h), 407 (74.5%) spent normal (8–10 h), and 45 (8.2%) spent long (>10 h) sleeping (Table 4).
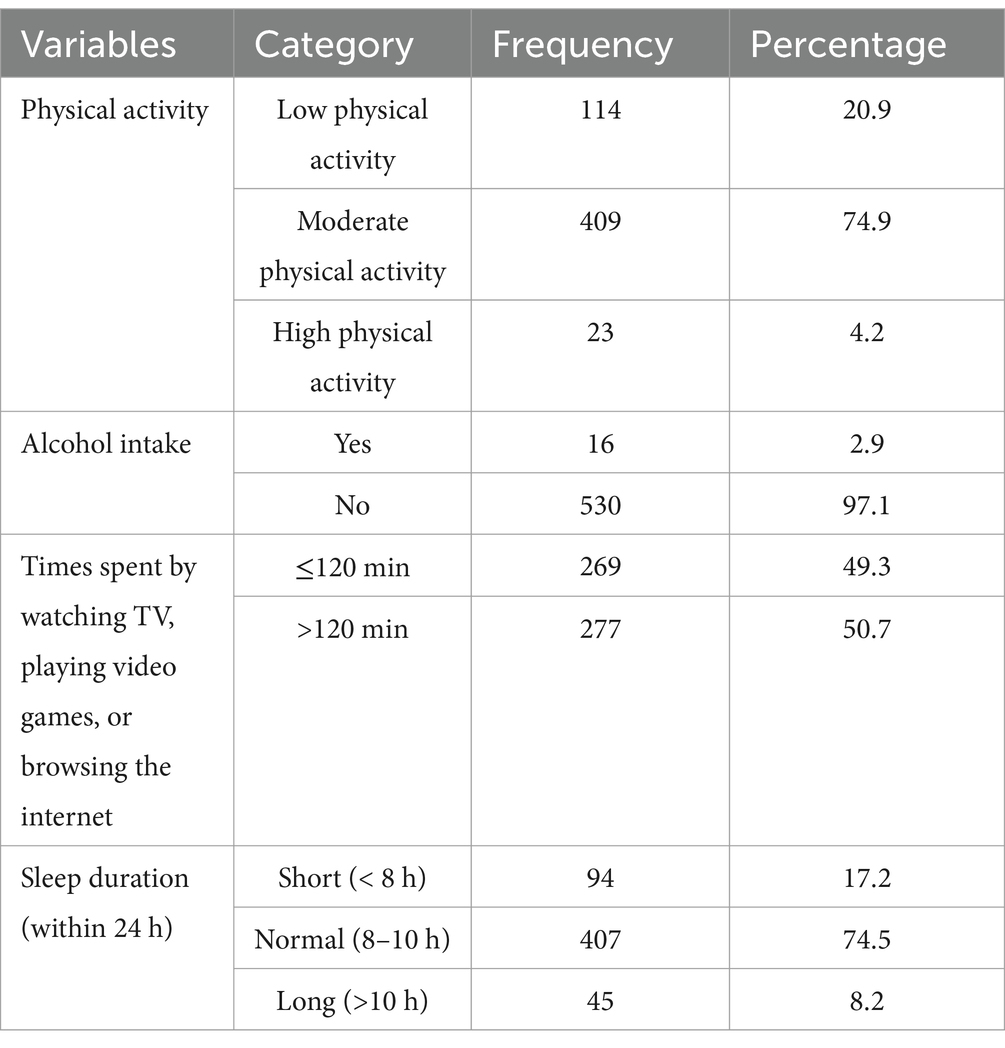
Table 4. Physical activity, alcohol intake, and sedentary behavior of adolescents in Wolaita Sodo town, southern Ethiopia, 2022.
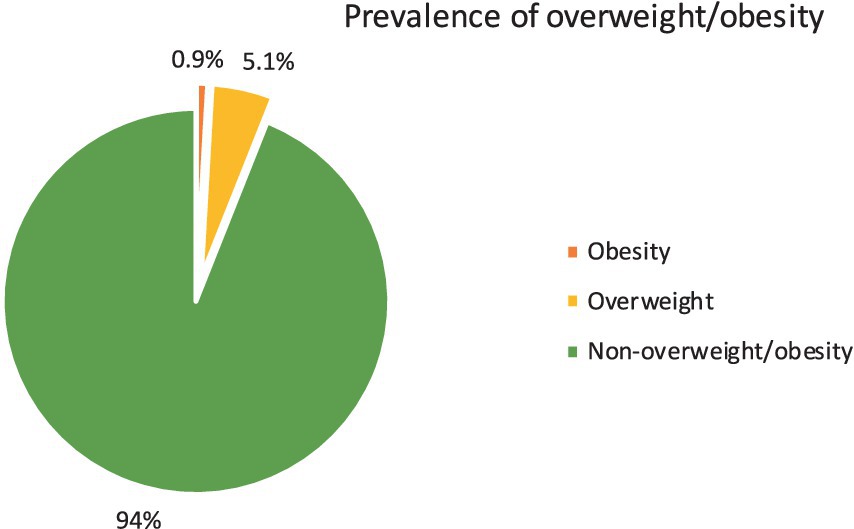
The prevalence of overweight/obesity
The combined prevalence of overweight/obesity was 6.0% (95% CI: 4.2–8.4%) based on BMI-for-age categorization. The separated prevalence of overweight and obesity was 5.1% (95% CI: 3.4–7.3%) and 0.9% (95% CI: 0.3–2.1%), respectively. In addition, the prevalence of overweight/obesity was 7.9% based on WHR. Overweight/obesity was found to be 4.7% among females and 1.3% among males, respectively, and 4.2% among late adolescents and 1.8% among early adolescents. The prevalence of overweight/obesity is 10.2% among frequent (>2 times) fast-food eaters and 4.1% among non-frequent consumers (Figure 2). There is a substantial correlation between the frequency of fast-food consumption and overweight/obesity.
The frequency of fast-food consumption and BMI-for-age Z-score level was shown to be a statistically significant correlation (p < 0.01), with a moderately strong positive association (Pearson r = 0.56) between the frequency of fast-food consumption and BMI-for-age Z-score (as shown in Table 5).
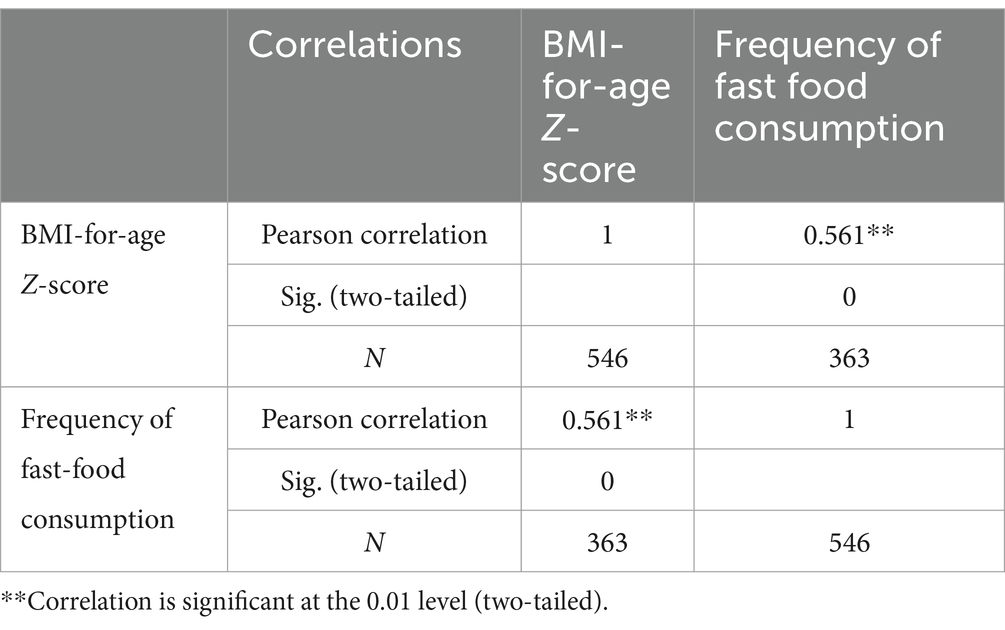
Table 5. The linear correlation between BAZ and frequency of fast-food consumption among adolescents in Wolaita Sodo town, Southern Ethiopia, 2022.
Sex of participants, age group of the respondents, mother’s occupation, household monthly income, frequency of fast-food consumption, frequency of meat and egg consumption, and physical activity level were variables having a p-value of less than 0.25 in bivariate analysis. Therefore, these variables were fitted in the multivariate logistic regression to get the adjusted effect of each covariate. After adjusting, the sex of participants, household monthly income, and frequency of fast-food consumption were significantly associated with overweight/obesity at a 95% confidence level and a p-value of ≤0.05.
Adolescent girls were 1.75 times more at risk of becoming overweight and obese than adolescent males (AOR = 1.75 [95%CI: 1.03–3.40]). Adolescents from households with monthly incomes greater than 10,000 EBT were 3.2 times at higher risk for becoming overweight or obese as compared to adolescents whose family income was less than 3,000 EBT per month (AOR = 3.21 [95%CI: 1.22–5.42]). Prevalence for overweight/obesity was almost three times higher for those who frequently consumed fast food, than those adolescents consuming fast foods two times or less than two times within a week (AOR = 2.98 [95%CI: 1.89–4.76]) (Table 6).
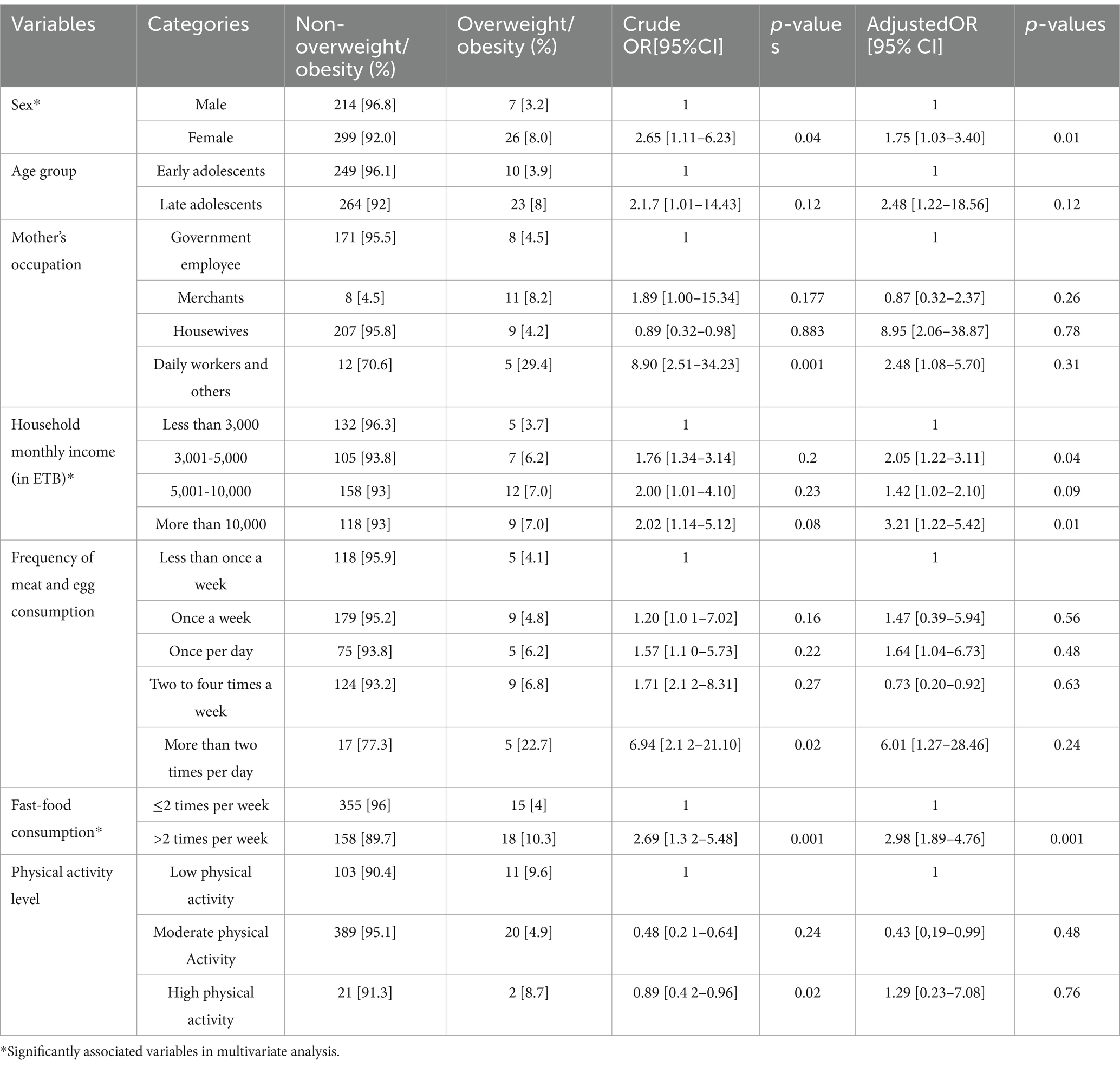
Table 6. Odds ratios of overweight/obesity for significantly associated factors (logistic regression analysis) for adolescents in Wolaita Sodo town, Southern Ethiopia, 2022.
Discussion
Based on BMI-for-age classification, the combined prevalence of overweight/obesity was 6.0% (95% CI: 4.2–8.4%), and a statistically significant association (p < 0.01) was found between the frequency of fast-food consumption and BMI for the age Z-score level, with a positive correlation and moderate strength, with a Pearson’s r value of 0.56. The prevalence of overweight/obesity in our study is consistent with previous findings in the same location 5 years ago, which is 5.1% (23). However, the prevalence of obesity alone (0.9%) is higher than the previous finding, which is 0.3%. This could be because of a shift in lifestyle that involves less physical exercise, the impact of technology, intermittent economic volatility, and the adoption of Western diets (fast foods); and a difference in methods as this study was community-based.
However, the magnitude of overweight/obesity in this study is lower than results from South Africa, which was 16.9% (24), and Ghana and Uganda, where the prevalence of overweight/obesity was 15.9% (25). It is lower than the findings from South Wollo, which revealed the magnitude of overweight/obesity as 8.2% (26), and Bahr Dar town, which is 7.7 and 10.7% for overweight and obesity, respectively (27).
The socioeconomic background of the research population may be the cause of this; in Africa, being overweight is a sign of wealth, and the prevalence may vary depending on the economic standing of community.
The findings revealed a considerable sex difference in overweight (males: 0.9%; females: 4.2%) and obesity (males: 0.4%; females: 0.5%). Moreover, female adolescents were 1.75 times more likely to be overweight or obese than males. According to a Nepalese study, female adolescents were more likely to become overweight than male adolescents (28). This study is aligned with a study from Mekele, which suggested similar results; the odds of overweight and obesity among females were two times higher as compared to males (29). This finding also agrees with the result from meta-analysis, which showed that female adolescents were 3.23 times more likely to be overweight/obese than their male counterparts (5). This is again in line with findings from Hawasa town, in which girls were 5.14 times more likely to be overweight or obese compared with boys (30). Similar results were documented in studies from Dessie Town (26) and Dire Dawa (31). This discrepancy may result from women engaging in less physical activity than men, spending more time at home, and having more limited mobility as a result of cultural factors. It is also highly likely to be associated with general physiological differences between the sexes. In Ethiopia, due to some cultural constraints, girls were spending their free time doing sedentary things such as sitting and watching TV shows and movies, as well as assisting their mothers with home chores, whereas boys could have the opportunity to participate in outdoor games (32).
In this study, household monthly income had a statistically significant relationship with overweight and obesity. Adolescents from families with a monthly income of more than 10,000 ETB were 3.2 times more likely to become overweight/obese than adolescents from families with a monthly income of less than 3,000 ETB. Several reports revealed consistent findings. A study in Morocco found that the prevalence of overweight and obesity increases with higher household wealth (33). Meta-analysis in Ethiopia suggests adolescents from high-income families were 3.16 times more likely to be overweight/obese as compared to those from middle and low-income families (5). A substantial relationship between household income and overweight/obesity was also found in the study from Bahir Dar; adolescents from higher income families had a higher likelihood of being overweight/obese than those from lower income families (27).
In addition to this, a study from Addis Ababa reported that adolescents whose family’s income was more than 22,727 ETB per month were 4.1 times more likely to be overweight/obese (AOR = 4.1, 95% CI: 1.1, 15.8) than those families’ incomes less than or equal to 1,864 ETB per month (22) and a study from Hawasa town also showed a similar association (30). This may be due to the Western-style eating habits of adolescents from higher socioeconomic groups, which consume more high-fat, high-calorie foods in place of the wholesome, traditional diet of cereals, fruit, and vegetables.
In addition, they are even more exposed to a sedentary way of life. However, a cohort study from Taipei showed that children from low-income households had a significantly higher risk of becoming overweight/obesity than those from middle-and high-income households (34). Another qualitative study, from Hong Kong, reveals that adolescents from low-income families are more likely to engage in unhealthy dietary behaviors and, as a result, are more vulnerable to diet-related health problems (35). One possible explanation for this could be that adolescents from industrialized countries, while likely more aware of healthy diets, consume fast food because it is cheap and convenient.
About 32.2% of the respondents were frequent (>2 times) fast-food consumers, of which 105 (59%) were females and 73 (41% were males). This result is lower than the findings from Bangladesh (36) and Sri Lanka (37). Moreover, this finding is even lower than reports from Saudi Arabia (38). This could be related to differences in socioeconomic status, lifestyle, and easy access to junk and processed foods among the research population. According to one Italian survey, over 80% of kids have visited a fast-food restaurant at least once in their lives, yet just 15.5% of the sample said they frequented the establishment more than once a week (39). This is significantly less than what we found. Moreover, this might be because of a government plan that includes a number of programs designed to encourage pupils in that particular area to consume more fruits and veggies. A study in Saudi Arabia identified there was no significant relationship between BMI categories and father’s education level and mother’s education. However, the same study results show that while the fathers of most of the overweight and obese children were employed, the mothers of most of the overweight and obese children were not employed (40). However, our research showed no significant association between adolescents’ overweight/obesity and their parents’ career or level of education. This discrepancy may be due to the difference in type of study design and sample size.
In terms of frequency of fast-food intake, frequent fast-food users were almost three times more overweight/obese than those who consumed fast foods two times or less than two times per week, which is similar to data from Sri Lanka (37) and Saudi Arabia (38).
Another recent study, in the UK, found that increased visits to fast-food outlets were associated with higher BMI SD scores in adolescents (41), which is again in line with these findings. This might be due to the fact that fast foods are energy dense and high calories. However, there is one contrary finding from Hawasa town, among the adult community, in which no significant associations were found for frequency of consumption of fast foods and overweight/obesity (42). This may be due to differences in the study population and study period. Compared to states in the European Union, where the prevalence varies from 12% in the Netherlands to 36% in Malta, the prevalence of overweight and obesity in our study is significantly lower (43). This could be due to adolescents in developing nations still adjusting to a Western-style diet.
Recommendation
WHO published the six implementation plans for the prevention and interventions of childhood and adolescents’ obesity in 2017. First, there is a need to implement comprehensive programs that promote the intake of healthy foods and reduce the intake of unhealthy foods and sugary beverages by children and adolescents. Second, comprehensive programs must promote physical activity and reduce sedentary behaviors in children and adolescents. Third, the program must integrate and strengthen guidance for non-communicable disease prevention with current guidance for preconception and antenatal care to reduce the risk of childhood obesity. Fourth, it is imperative to provide guidance on and support for healthy diet, sleep, and physical activity in early childhood to ensure children grow appropriately and develop healthy habits. Fifth, the comprehensive programs must promote healthy school environments, health and nutrition literacy, and physical activity among schoolage children and adolescents. Finally, it is important to provide family-based, multicomponent, lifestyle weight management services for children and young people who are obese.
Specifically for our study area, the federal government of Ethiopia should influence the food industry to lower the fat, sugar, and salt content of processed foods; guarantee that all consumers have access to and can afford healthy and nutritious options; limit the marketing of foods high in sugar, salt, and fat, particularly those targeted at children and teenagers; and promote regular physical activity in the workplace (44).
As a public health priority, the health sector of the town should concentrate on preventing overweight and obesity. Health officials should also work with the education sector of school district to mitigate problems among school-age adolescents by setting up play areas for physical activity and raising awareness through health professionals.
Adolescents should consume less sugar and fast food, eat more fruits, vegetables, and whole grains, and be physically active on a regular basis.
Limitations
The shortcoming of the study was that it did not take genetic factors or parental BMI into account. Another problem could be recollection bias, which affects outcomes as participants may forget what they ate in the previous 7 days, and food portion size was not taken into account. In addition, both nutritional consumption and physical activity were self-reported data; therefore, overreporting or underreporting could be a significant issue in this study. Finally, only a sample of three chosen sub-cities was included in the study. Consequently, statistics from the omitted sub-cities may have produced a different result.
Conclusion
Findings of this study revealed that the overall prevalence of overweight/obesity was 6.0%. Adolescents who are female, come from high-income families, and eat fast food frequently are more likely to be overweight or obese. Future health initiatives aimed at lowering the prevalence of overweight and obesity in adolescents should pay special attention to female adolescents and those from high-income families.
Additionally, more studies in this area should be conducted with a larger sample size, taking into account the portion size of food.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethical clearance was obtained from the institutional review board of Wolaita Sodo University, College of Health Sciences and Medicine. The official letter of permission was written to Wolaita Sodo city administration mayor office. And again, an official letter from the mayor’s office was written to the administrative offices of three selected sub-cities. The data collectors’ team approached each study unit identified for the study and explained the study objectives, confidentiality issues, data use and handling, and their right to withdraw from the study at any time without requiring a reason. Informed verbal consent was obtained from the parents for those aged 10–12, and adolescents above 12 years old gave the consent by themselves. And the interview was carried out in the privacy of their home or in other private locations where they felt comfortable being interviewed. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
CE: Methodology, Resources, Writing – original draft, Writing – review & editing, Formal analysis. AA: Conceptualization, Investigation, Writing – review & editing. CA: Formal analysis, Investigation, Supervision, Writing – original draft. TY: Data curation, Formal analysis, Software, Writing – review & editing. DG: Data curation, Formal Analysis, Supervision, Validation, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
First, we would like to thank the Almighty God who keeps us alive and became our strength. Our heartfelt gratitude goes to Wolaita Sodo University College of Health Science and Medicine, Department of Human Nutrition and Reproductive Health. Finally, we would like to thank data collectors, supervisors, and respondents.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; BAZ, body mass index for age z-score; BMI, body mass index; C OR, crude odds ratio; DALYs, disability-adjusted life years; DM, diabetes mellitus; HHs, households; LMICs, low-income and middle-income countries; NCDs, non-communicable diseases; NRR, non-response rate; OR, odds ratio; SNNPR, South Nation, Nationalities and Peoples’ Region; SPSS, Statistical Package for Social Students; UNICEF United Nations Children’s Fund; US, United States; WHR, waist-to-hip ratio; WHO, World Health Organization.
References
1. WHO. (2021). Obesity and Overweight. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
2. WHO. Obesity rising in Africa. Regional Office for Africa (2022). Available at: https://www.afro.who.int/news/obesity-rising-africa-who-analysis-finds (Accessed March 02, 2022).
3. Chandrasekaran, P, and Weiskirchen, R (2024). The role of obesity in type 2 diabetes mellitus—an overview. Int J Mol Sci 25:1882. doi: 10.3390/ijms25031882
4. Addis, E, Dessie, Y, and Assefa, N (2024). Burden of overweight and obesity among adolescents in Ethiopia: a systematic review and meta-analysis. Int Health. doi: 10.1093/inthealth/ihae041
5. Gebrie, A, Alebel, A, Zegeye, A, Tesfaye, B, and Ferede, A (2018). Prevalence and associated factors of overweight/obesity among children and adolescents in Ethiopia: A systematic review and meta-analysis BMC Obes. 5:1–12. doi: 10.1186/s40608-018-0198-0,
6. Hsieh, S, Klassen, AC, Curriero, FC, Caulfield, LE, Cheskin, LJ, Davis, JN, et al. (2018). Fast-food restaurants, park access, and insulin resistance among Hispanic youth. Am J Prev Med 46:378–87. doi: 10.1016/j.amepre.2013.12.007
7. Tavares, LF, Fonseca, SC, and Garcia Rosa, ML (2019). Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian family doctor program. Public Heal Nutr 15:82–7. doi: 10.1017/S1368980011001571
8. Mohammadbeigi, A, Asgarian, A, Moshir, E, Heidari, H, Afrashteh, S, Khazaei, S, et al. (2018). Fast food consumption and overweight/obesity prevalence in students and its association with general and abdominal obesity. J Prev Med Hyg 59:E236–40. doi: 10.15167/2421-4248/jpmh2018.59.3.830
9. Kansra, AR, Lakkunarajah, S, and Jay, MS (2021). Childhood and adolescent obesity. Review 8:1–16. doi: 10.3389/fped.2020.581461
10. Fraser, LKL, Clarke, GP, and EK, CJE (2016). Fast food and obesity: a spatial analysis in a large United Kingdom population of children aged 13-15. Am J Prev Med 42:e77–85. doi: 10.1016/j.amepre.2012.02.007
11. Maria, EN (2022). Worldwide relation between fast food availability and obesity rates. Int J Res Innov Soc Sci 6:336–341.
12. Ulfah Mahardika, PP, Yuhan, Z, Ying, Z, Saiying, C, and Lina, Y (2024). The association between fast food consumption and obesity among college students in Indonesia. Int J Appl Res Sustain Sci :2. doi: 10.59890/ijarss.v2i2.1402
13. Wiki fast-food-definition. Available at: https://en.wikipedia.org/
14. Kumar, NS, and Raina, NDA (2024). To study the relation between fast food and obesity in the teenagers. Int J Res Public Seminars 15:252–8. doi: 10.36676/jrps.v15.i2.1419
15. Shridhar, G, Rajendra, N, Murigendra, H, Shridevi, P, Prasad, M, Mujeeb, MA, et al. (2015). Modern diet and its impact on human health. J Nutr Food Sci 5:430–3. doi: 10.4172/2155-9600.1000430
16. IFPRI. Food Systems for Healthier Diets in Ethiopia: Towards a research agenda. (2018). Available at: https://a4nh.cgiar.org/files/2018/04/DP1050_Formatted.pdf (Accessed April 17, 2018).
17. Elizabeth, L, Machado, P, Zinöcker, M, Baker, P, and Lawrence, M (2020). Ultra-processed foods and health outcomes: a narrative review. Nutrients 12:1955. doi: 10.3390/nu12071955
18. Andriyani, A, Lee, Y, Win, K, Tan, C, Amini, F, Tan, E, et al. (2024). Fast food consumption, obesity and nutrient intake among adults in Indonesia. Food Res 8:55–65. doi: 10.26656/fr.2017.8(s3).5
19. Green, MA, Hobbs, M, Ding, D, Widener, M, Murray, J, Reece, L, et al. (2021). The association between fast food outlets and overweight in adolescents is confounded by Neighbourhood deprivation: a longitudinal analysis of the millennium cohort study. Int J Environ Res Public Health 18:13212. doi: 10.3390/ijerph182413212
20. Teshome, M (2019). The role of geoinformation technology for predicting and mapping urban change detection: Wolaita Sodo town case study. Ethiopia Int J Curr Res AcaRev 7:23–33. doi: 10.20546/ijcrar.2019.710.004
21. Federal democratic republic of Ethiopia central statically agency. Ethiopian Household Consumption-Expenditure Survey Southern Nations Nationalities Region Report (2018)
22. Dereje, D, and Yirgu, RTC (2018). Magnitude of overweight/obesity and associated factors among high school students in Addis Ababa. J Nutr Disord 8:1–10. doi: 10.4172/2161-0509.1000231
23. Teferi, DY, Atomssa, GE, and Mekonnen, TC (2018). Overweight and undernutrition in the cases of school-going adolescents in Wolaita Sodo town, Southern Ethiopia. Cross-Sectional Study 2018:1–10. doi: 10.1155/2018/8678561
24. Otitoola, O, Oldewage-Theron, W, and Egal, A (2021). Prevalence of overweight and obesity among selected schoolchildren and adolescents in Cofimvaba, South Africa. South African J Clin Nutr 34:97–102. doi: 10.1080/16070658.2020.1733305
25. Peltzer, K, and Pengpid, S (2016). Overweight and obesity and associated factors among school-aged adolescents in Ghana and Uganda. Int J Environ Res Public Health 8:3859–70. doi: 10.3390/ijerph8103859
26. Mulu Birru, G, Eshete Tadesse, S, Hassen Abate, K, Mekonnen, TC, and Genetu, CM (2021). Malnutrition in school-going adolescents in Dessie town, south Wollo, Ethiopia. J Nutr Metab 2021:1–8. doi: 10.1155/2021/4898970
27. Worku, M, Gizaw, Z, Belew, AK, Wagnew, A, and Hunegnaw, MT. Prevalence and associated factors of overweight and obesity among high school adolescents in Bahir Dar City, Ethiopia: A Cross-Sectional Study. (2021), 2021, 1–8
28. Chaulagain, K (2021). The burden of overweight and its risk factors in urban Nepalese school adolescents: a cross-sectional study. J Qual Heal Care Econ 4. doi: 10.23880/jqhe-16000230
29. Andargie, M, Gebremariam, K, Hailu, T, Addisu, A, and Zereabruk, K (2021). Magnitude of overweightand obesity and associated factors among public and private secondary school adolescent students in Mekelle City, Tigray region, Ethiopia, 2019: comparative cross-sectional study. Diabetes Metab Syndr Obes Targets Ther 14:901–15. doi: 10.2147/DMSO.S262480
30. Singh, P. Prevalence and associated factors of overweight and obesity among high school adolescents in urban communities of Hawassa. Southern Ethiopia: (2016).
31. Belay, M, Oumer, A, Abdureshid, N, and Ale, A (2022). Overnutrition and associated factors among high school adolescents in mid COVID-19 pandemic in Ethiopia: neglected public health concern. Adolesc Health Med Ther 13:1–14. doi: 10.2147/AHMT.S349189
32. Abera, M, Hardy-Johnson, P, Abdissa, A, Workicho, A, Ali, R, Weller, S, et al. (2021). Social, economic and cultural influences on adolescent nutrition and physical activity in Jimma, Ethiopia: perspectives from adolescents and their caregivers. Public Health Nutr 24:5218–26. doi: 10.1017/S1368980020001664
33. El Kabbaoui, M, Chda, A, Bousfiha, A, Aarab, L, Bencheikh, R, and Tazi, A (2018). Prevalence of and risk factors for overweight and obesity among adolescents in Morocco. East Mediterr Heal J 24:512–21. doi: 10.26719/2018.24.6.512
34. Chou, YC, Cheng, FS, Weng, SH, Yen, YF, and Hu, HY (2024). Impact of household income on the risk of overweight and obesity over time among preschool-aged children: a population-based cohort study. BMC Public Health 24:549. doi: 10.1186/s12889-024-18010-1
35. Siu, JY, Chan, K, and Lee, A (2019). Adolescents from low-income families in Hong Kong and unhealthy eating behaviours: implications for health and social care practitioners. Health Soc Care Community 27:366–74. doi: 10.1111/hsc.12654
36. Tareq, AM, Mahmud, MH, Billah, MM, Hasan, MN, Jahan, S, Hossain, MM, et al. (2022). Fast-food and obesity: status among the young adult population in Bangladesh. Narra J 2:e86. doi: 10.52225/narra.v2i3.86
37. Priyanath, HM, and Dasanayaka, P (2022). Impact of fast-food consumption on overweight among young adults in Sri Lanka. Int J Educ Teach Soc Sci 2:10–21. doi: 10.47747/ijets.v2i3.728
38. Al-otaibi, HH, and Basuny, AM (2015). Fast food consumption associated with obesity/overweight risk among university female student in Saudi Arabia fast food consumption associated with obesity/overweight risk among university female student in Saudi Arabia Pak J Nutr. 14:511–6. doi: 10.3923/pjn.2015.511.516,
39. Acito, M, Cangelosi, G, Petrelli, F, Moretti, M, Villarini, M, Celestino, A, et al. (2024). Eating and lifestyle habits and primary school health-related pro-grams: a survey involving Italian children and teachers. Ann Ig 36:123–43. doi: 10.7416/ai.2024.2599
40. Alqarni, F, Alariefy, M, Albishri, A, Bajubair, A, Almuzaini, A, Alzahrani, E, et al. (2017). Do parental education and occupation affects children’s body mass index (BMI)? Int J Adv Res 5:1381–8. doi: 10.21474/ijar01/6097
41. Jiang, J, Lau, PWC, Li, Y, Gao, D, Chen, L, Chen, M, et al. (2022). Association of fast-food restaurants with overweight and obesity in school-aged children and adolescents: a systematic review and meta-analysis. Obes Rev 24:e13536. doi: 10.1111/obr.13536
42. Darebo, T, Mesfin, A, and Gebremedhin, S (2019). Prevalence and factors associated with overweight and obesity among adults in Hawassa city, southern Ethiopia: A community based cross-sectional study. BMC Obes. 6:1–10. doi: 10.1186/s40608-019-0227-7
43. OECD/European Union. Health at a glance: Europe 2020: state of health in the EU cycle. Paris: OECD Publishing (2020).
Keywords: fast food, overweight/obesity, prevalence, adolescent, urban
Citation: Elias C, Abraham A, Asrat C, Yakob T and Girma D (2025) Prevalence of overweight/obesity and its association with fast food consumption among adolescents in Southern Ethiopia, 2022: a community-based cross-sectional study. Front. Nutr. 11:1475116. doi: 10.3389/fnut.2024.1475116
Edited by:
Haleama Al Sabbah, Abu Dhabi University, United Arab EmiratesReviewed by:
Jeff Bolles, Francis Marion University, United StatesGiulio Nittari, University of Camerino, Italy
Diana Nur Afifah, Diponegoro University, Indonesia
Iolanda Grappasonni, University of Camerino, Italy
Copyright © 2025 Elias, Abraham, Asrat, Yakob and Girma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chernet Elias, Y2hlcm5ldGVsaWFzQGdtYWlsLmNvbQ==
 Chernet Elias
Chernet Elias Awoke Abraham
Awoke Abraham Chernet Asrat
Chernet Asrat Tagese Yakob
Tagese Yakob Daniel Girma3
Daniel Girma3