- 1Department of Oncology Surgery, Fuzhou Hospital of Traditional Chinese Medicine Affiliated to Fujian University of Traditional Chinese Medicine, Fuzhou, Fujian, China
- 2Department of Clinical Medicine, School of Medicine, Shihezi University, Shihezi, China
- 3Department of Physiology, College of Medicine, Chosun University, Gwangju, Republic of Korea
Background: The relationship between CDAI and suicidal ideation is unclear. This study investigates the relationship between CDAI and suicidal ideation and examines the association between CDAI and all-cause mortality (ACM) or cardiovascular disease mortality (CVM) among participants with and without suicidal ideation.
Methods: Data from seven NHANES cycles (2005–2018) were analyzed using cross-sectional and prospective cohort studies. Weighted multivariable logistic regression models, restricted cubic spline (RCS) plots, and subgroup analyses explored the association between CDAI and suicidal ideation. Kaplan–Meier (KM) curves, weighted multivariable Cox proportional hazards models, and RCS assessed the relationship between CDAI and CVM or ACM.
Results: Among 30,976 participants aged over 20, 1,154 (3.72%) had suicidal ideation. Higher CDAI levels (Quartile 4) were associated with a 28% reduction in suicidal ideation compared to lower levels (Quartile 1). Over an average follow-up of 89 months, 3,267 participants (7.6%) died, including 808 (1.8%) from cardiovascular causes. Higher CDAI levels were linked to a 30, 68, and 28% reduction in ACM in the total population, those with suicidal ideation, and those without, respectively. CVM was reduced by 40% in the total population and by 41% in those without suicidal ideation.
Conclusion: CDAI is negatively associated with suicidal ideation and correlated with reduced ACM and CVM among participants with and without suicidal ideation.
1 Introduction
Suicide stands as a significant global concern in both public health and society, ranking as the second highest cause of mortality among individuals aged 15 to 29 (1). Gustavo Turecki and colleagues reported a suicide rate of nearly 11.4 per 100,000 individuals, equating to roughly 1 million global suicides annually (2). The ramifications of suicide extend far beyond the individual, affecting families, communities, and even nations, leaving lasting emotional and societal scars (3). Suicidal ideation, as an early psychological activity preceding suicide, is considered a strong predictor of suicidal behavior (4). Therefore, identifying modifiable factors linked to suicidal thoughts at an early stage is imperative.
CDAI is a simple, cost-effective measure for evaluating an individual’s intake of dietary antioxidants. It has been associated with various chronic diseases, such as coronary heart disease (5), stroke (6), chronic respiratory diseases (7), and hyperlipidemia (8). Additionally, research by Juanjuan Luo and Xiying Xu has shown that CDAI is linearly and negatively associated with depression (OR = 0.77, 95% CI [0.67, 0.89]) (9). Roughly 90% of individuals experiencing suicidal thoughts have been reported to contend with mental disorders like depression (10). Therefore, we hypothesize that CDAI is negatively correlated with the odds of suicidal ideation.
Therefore, this study seeks to explore the correlation between CDAI and suicidal thoughts, as well as assess the connection between CDAI ACM and CVM in both individuals with and without suicidal ideation. The study population is derived from data spanning seven cycles of the NHANES from 2005 to 2018.
2 Methods
2.1 Study participants
The NHANES is an ongoing, stratified, multistage sampling program designed to assess the health and nutritional status of adults and children in the United States. It encompasses a variety of health outcomes and nutritional indicators (11). The NHANES study has been approved by the Research Ethics Review Board of the NCHS, and all participants provided written informed consent (12).
Among the 70,190 participants in the seven NHANES cycles from 2005 to 2018, 39,749 were aged 20 years or older. Following the exclusion of participants with incomplete CDAI data (n = 6,739), missing suicidal ideation data (n = 1,980), and missing follow-up data (n = 54), the study comprised a total of 30,976 participants (Supplementary Figure S1).
2.2 Exposure and outcome variables
The main exposure variable in this study is CDAI. Based on previous research (9, 13), six dietary minerals and vitamins (manganese, selenium, zinc, and vitamins A, C, and E) were used to calculate CDAI for all participants. The detailed calculation formula is provided in Supplementary Table S1. The primary outcomes were suicidal ideation and mortality (ACM and CVM). Suicidal ideation was assessed using the PHQ-9. Data on ACM and CVM were obtained from the National Death Index (NDI) up to December 31, 2019.1 Specific definitions of these variables are provided in Supplementary Table S1.
2.3 Covariables
According to previous studies (14, 15), the covariates considered in the study encompass age, sex, race, marital status, education level, PIR, obesity, smoking, alcohol consumption, hypertension, and diabetes. For comprehensive details on these covariates, kindly consult Supplementary Table S1.
2.4 Statistical analysis
Sampling weights were used in all statistical analyses to ensure that the estimated data were nationally representative. In our study, the two-day dietary sample weight (WTDR2D) was used as the weighting variable, with the new weights (for 2005–2018) calculated as 1/7 × WTDR2D. Baseline characteristics were stratified into two groups based on the presence or absence of suicidal ideation and into quartiles based on CDAI. Continuous variables are expressed as mean (SD), whereas categorical variables are depicted as frequencies (9). Differences between the non-suicidal ideation group and the suicidal ideation group were assessed using weighted t-tests for continuous variables and weighted chi-square tests for categorical variables (9).
Weighted logistic regression was used to investigate the correlation between CDAI and suicidal ideation. Kaplan–Meier curves were utilized to depict mortality rates among different quartiles of CDAI, with comparisons conducted via log-rank tests. Weighted Cox proportional hazard models were employed to examine the association between CDAI and mortality rates among participants, stratified by the presence or absence of suicidal ideation. Three logistic regression models and three Cox proportional hazards models were constructed: In model 1, no adjustment was made for any confounding factors. Model 2 was adjusted for age, sex, race, marital status, education level, and PIR. Model 3 additionally accounted for obesity, smoking status, alcohol status, hypertension, and diabetes. Additionally, in Model 3, CDAI was treated as a continuous variable, and RCS curves were employed to elucidate the dose–response relationship between CDAI and the odds of suicidal ideation or all-cause mortality.
To further explore the relationships mentioned above, we conducted subgroup analyses by the variables in Model 3. Interaction analyses were performed to examine whether there were differential associations between subgroups. Statistical analyses were performed using R software (version 4.3.1). A significance level of p < 0.05 (two-sided) was considered statistically significant.
3 Result
3.1 Baseline characteristics
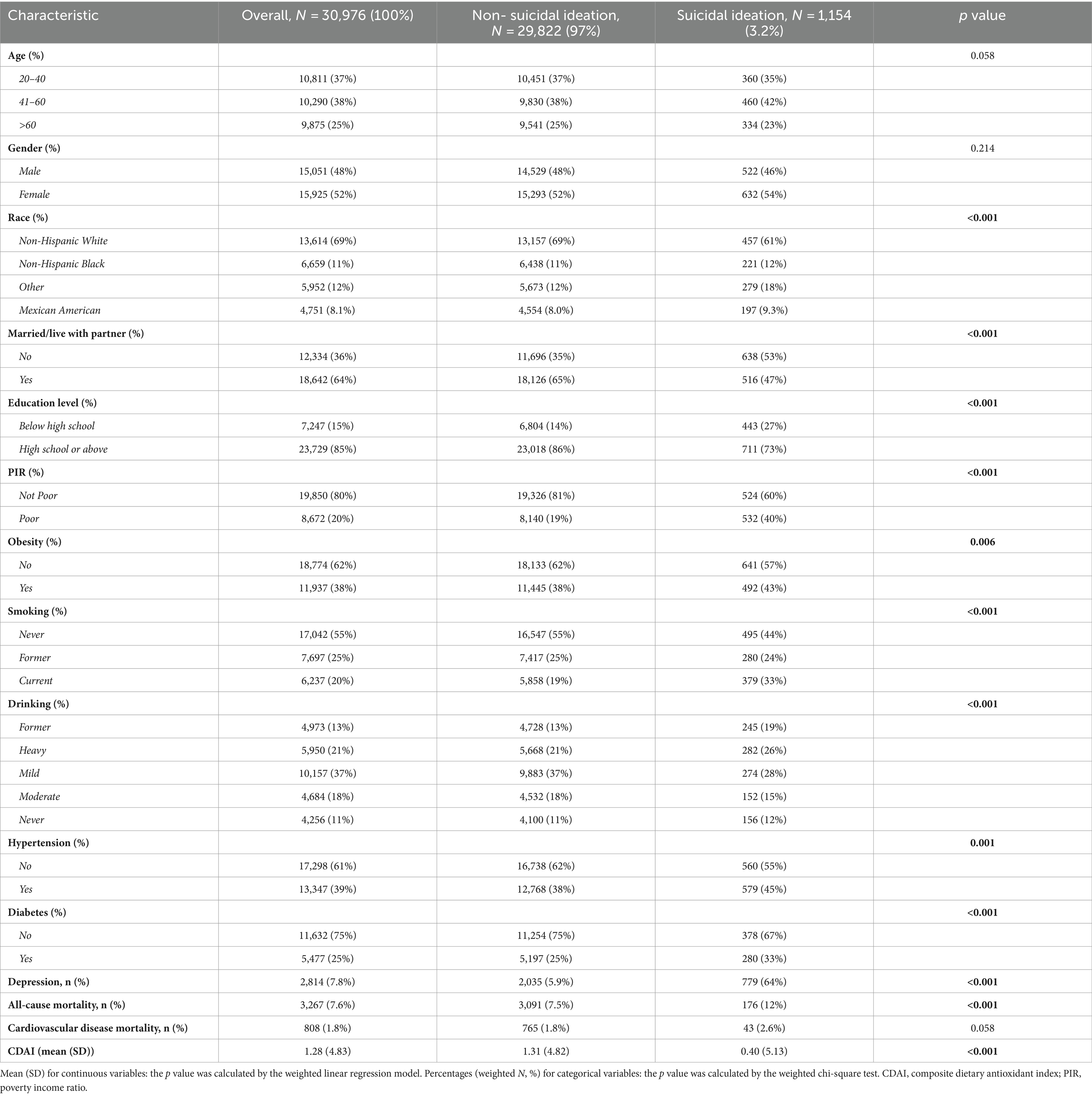
In this study, a total of 30,976 participants aged 20 years or older were included, consisting of 15,051 males and 15,925 females. Baseline characteristics of participants with and without suicidal ideation are shown in Table 1. The mean (SD) CDAI was 1.28 (4.83), and the prevalence of suicidal ideation was 3.2% (equivalent to 5.92 million of the U.S. population). Over an average follow-up period of 89 months, a total of 3,267 participants (7.6%) died from all causes, with 808 (1.8%) deaths attributed to cardiovascular causes. Preliminary assessment revealed that a larger proportion of participants with suicidal ideation were female, younger in age, White, unmarried, of higher socioeconomic status, and current or former smokers. Additionally, participants with suicidal ideation were more likely to have lower CDAI. Baseline characteristics of participants stratified by the presence or absence of suicidal ideation based on CDAI are presented in Supplementary Tables S2–S4.
3.2 Association of CDAI and suicidal ideation
As illustrated in Table 2, three distinct models were employed to evaluate the relationship between CDAI and suicidal ideation. In the model adjusting for all covariates, an increase of 1 unit in CDAI was associated with a 3% decrease in the odds of suicidal ideation (OR: 0.97, 95% CI: 0.94, 1.00). Furthermore, compared to the lowest quartile (Q1) of CDAI, the odds of suicidal ideation in the highest quartile (Q4) were 0.72 (95% CI, 0.53, 0.98). RCS analysis (Figure 1) further demonstrated a significant negative correlation between CDAI and the odds of suicidal ideation. The results of the subgroup analysis (Figure 2) also confirmed the consistency of the findings.
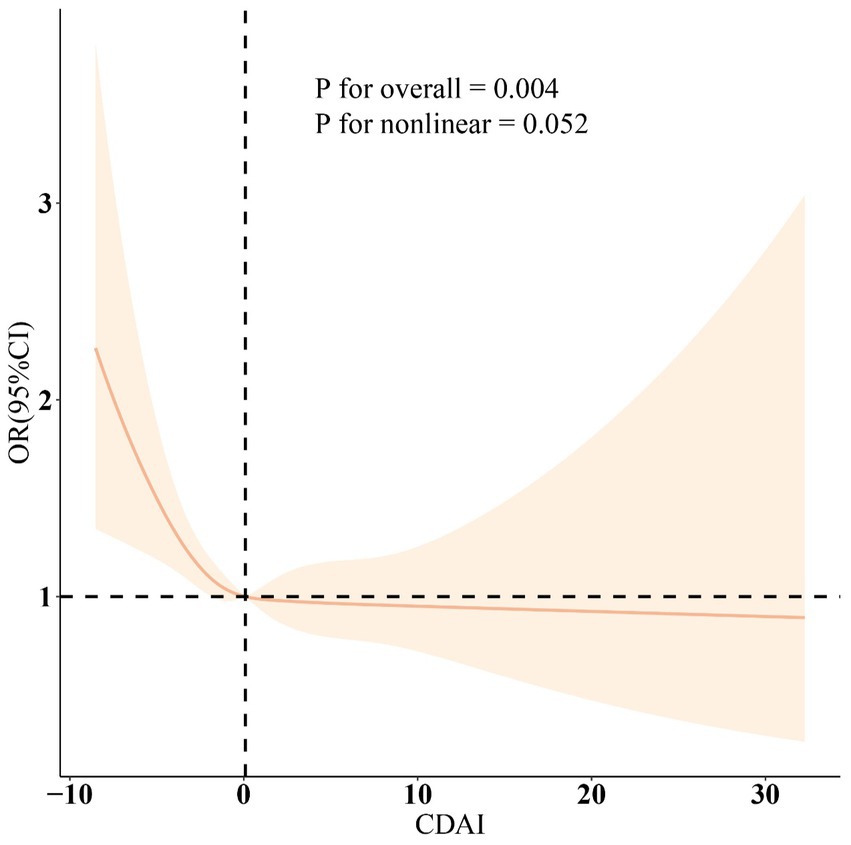
Figure 1. The smooth curve fitting analysis of CDAI and suicidal ideation. OR (solid lines) and 95% confidence levels (shaded areas) were adjusted for age, gender, education level, marital status, PIR, race, obesity, smoking, drinking, hypertension, and diabetes. PIR, poverty income ratio; CDAI, composite dietary antioxidant index; OR, odds ratio; CI, confidence interval.
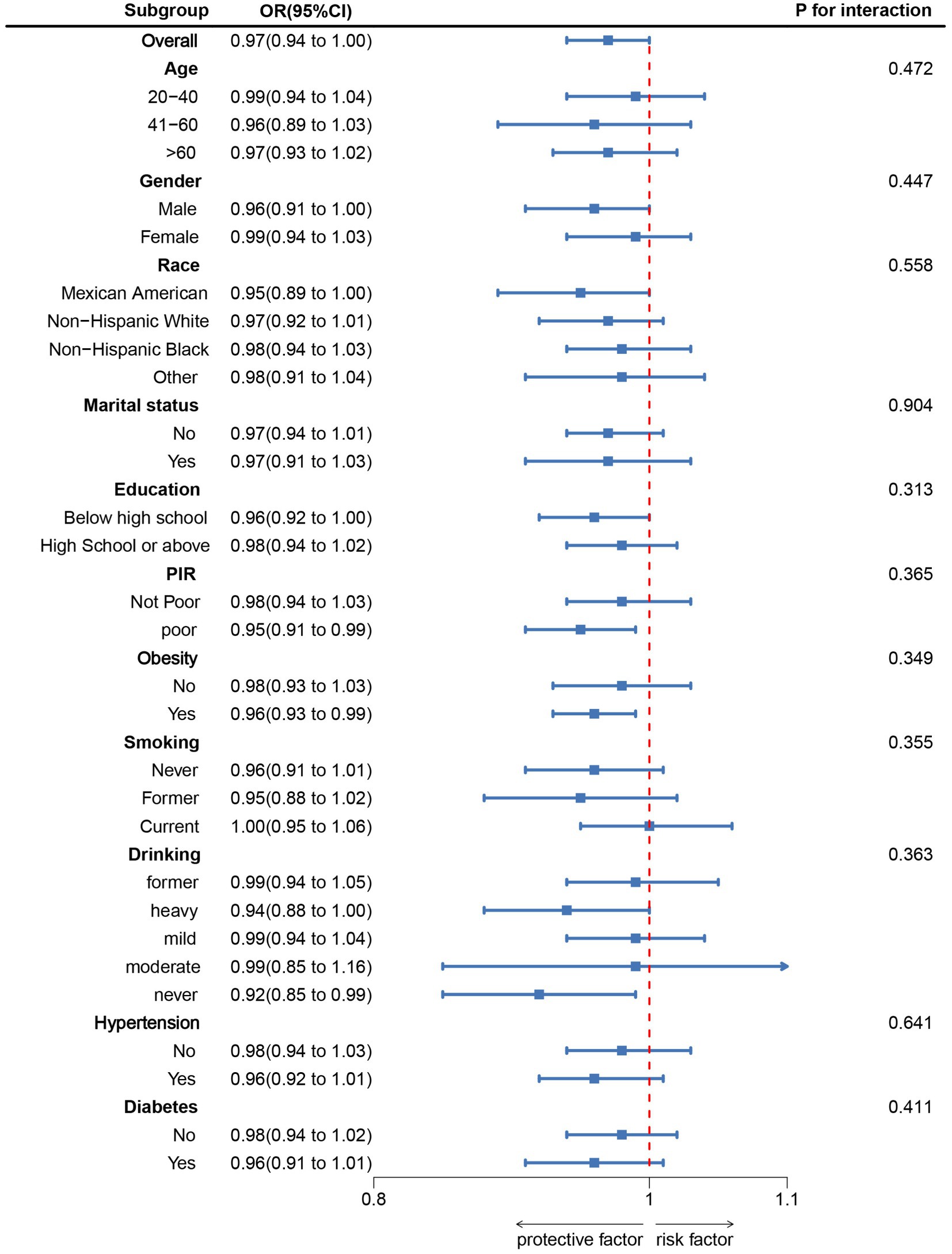
Figure 2. Subgroup analysis between CDAI and suicidal ideation. ORs were calculated as each unit increased in CDAI. Analyses were adjusted for age, gender, education level, marital status, PIR, race, obesity, smoking, drinking, hypertension, and diabetes. PIR, poverty income ratio; CDAI, composite dietary antioxidant index; OR, odds ratio; CI, confidence interval.
3.3 Correlation between CDAI and mortality in participants with or without suicidal ideation
Among all participants, 3,267 individuals died. K-M survival curves showed that higher CDAI was correlated with lower ACM in all participants, regardless of their suicidal ideation status (all p-values <0.05, as shown in Figure 3). Multivariable Cox regression models in Table 3 indicated that compared to participants with lower CDAI, those with higher CDAI had a 30% reduction in ACM (HR = 0.70, 95% CI: 0.60, 0.83), a 68% reduction in ACM among participants with suicidal ideation (HR = 0.32, 95% CI: 0.13, 0.78), and a 28% reduction in ACM among participants without suicidal ideation (HR = 0.72, 95% CI: 0.61, 0.85). CVM decreased by 40% in the total population (HR = 0.60, 95% CI: 0.42, 0.85) and by 41% in participants without suicidal ideation (HR = 0.59, 95% CI: 0.41, 0.86). RCS analysis (Supplementary Figure S2) and subgroup analyses also supported these findings (Supplementary Figures S3–S5).
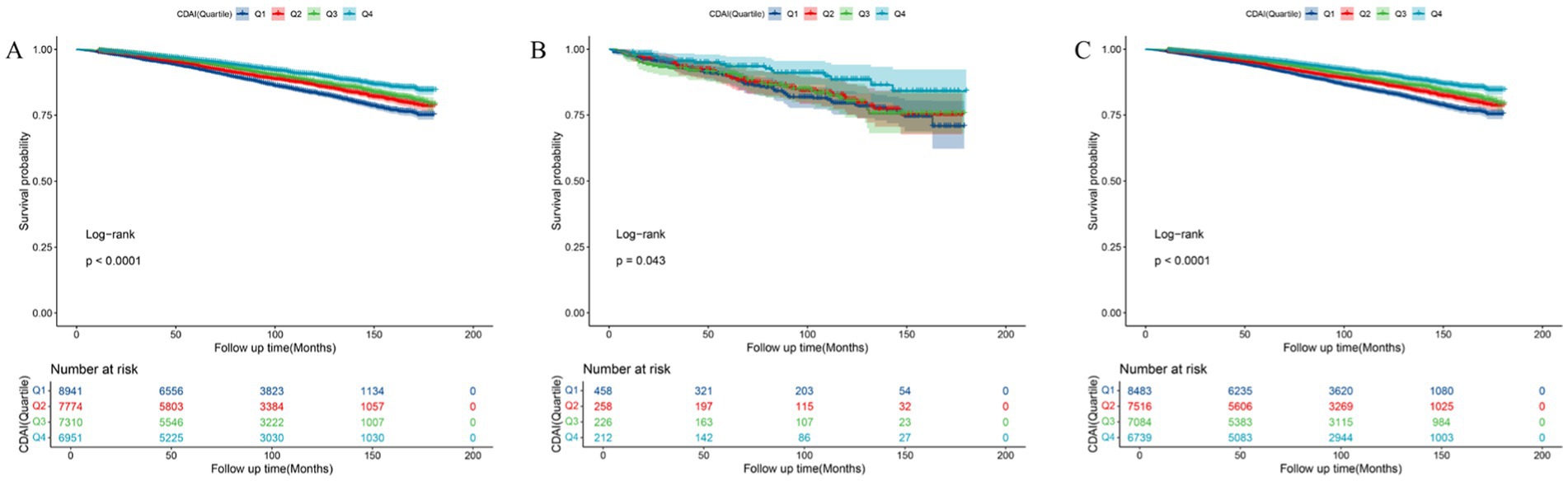
Figure 3. Kaplan–Meier analysis of all-cause mortality in (A) total participants, (B) participants with suicidal ideation, and (C) participants without suicidal ideation.
4 Discussion
In this nationally representative sample study of American adults, a notable negative correlation was observed between CDAI and the likelihood of experiencing suicidal ideation. Furthermore, it is noteworthy that higher CDAI was correlated with reduced mortality in both participants with and without suicidal ideation. These findings underscore the potential impact of CDAI on the incidence of suicidal ideation and mortality rates in these patients, emphasizing the importance of dietary antioxidants in monitoring and reducing the incidence of suicidal ideation and mortality rates.
To the best of our knowledge, this study represents the first examination of the relationship between CDAI and the prevalence of suicidal ideation. In recent years, there has been increasing scholarly attention to the role of dietary antioxidants in suicidal ideation. Findings from a randomized placebo-controlled clinical trial by Sahraian et al. (16) suggest that vitamin C may serve as an adjunctive agent in the treatment of suicidal behaviors. A study by Strumila et al. (17) indicates that patients with low selenium levels have a higher risk of suicide, accompanied by a more frequent history of suicide attempts. Additionally, research by Sher (18) suggests that selenium deficiency plays a significant role in the pathophysiology of suicidal behavior in alcohol abusers.
In a cross-sectional study based on a national survey involving 4,561 American participants, Dong Huang et al. found (14) that, after adjusting for potential confounding factors, the second quartile (compared to the highest quartile) of serum zinc levels had a higher risk of suicidal ideation [OR = 2.63; 95% CI: (1.53, 4.53)]. In this study, we observed similar results when applying the CDAI calculated based on manganese, selenium, zinc, and vitamins A, C, and E, indicating a negative association between CDAI and the odds of suicidal ideation. Furthermore, CDAI was also negatively correlated with the mortality rate in the population with suicidal ideation.
Although the mechanisms underlying the negative relationship between CDAI and the prevalence and mortality of suicidal ideation are extensive and complex, some studies have provided potential molecular mechanisms for these associations, primarily oxidative stress. Research by Koweszko et al. (19) found that levels of oxidative stress biomarkers (NADPH oxidase, advanced oxidative protein products, and oxidative stress index) were significantly higher in subjects with a history of suicidal ideation in the past three months. Additionally, a study by Loo et al. (20) demonstrated that compared to the group without suicidal ideation, those with a lifetime history of suicidal ideation had higher levels of oxidative stress (i.e., DNA damage). DNA damage can lead to dysfunction in DNA repair mechanisms, subsequently resulting in abnormal neurotransmission, impaired neuroplasticity, and dysfunctional energy metabolism in the brain (21). The consumption of foods abundant in antioxidants can mitigate oxidative stress, safeguarding cells and tissues from damage induced by free radicals. This may consequently reduce the occurrence of suicidal ideation (14, 16). Based on previous research, antioxidants such as vitamins C and E have been shown to counteract oxidative damage, protecting cell membranes from harm caused by free radicals, thereby reducing the risk of various chronic diseases (such as diabetes (22), cardiovascular diseases (23, 24), etc.) and lowering the risk of ACM and CHD death in the elderly (25).
Furthermore, chronic inflammation is another factor. Research by Lee et al. (26) suggests that brain inflammation can promote the occurrence of depression, a condition often accompanied by suicidal ideation (27). A diet rich in antioxidants can reduce neuroinflammation by modulating various inflammatory factors. Studies by Xu et al. (28) indicate that dietary vitamins A and E, along with the trace element zinc, can lower levels of various inflammatory factors (such as IL-6, TNF-α, and IFN-γ), thus mitigating the impact of brain inflammation on depression. Additionally, chronic inflammation is associated with the occurrence of various diseases (such as hypertension, diabetes, kidney disease, etc. (29–31)) and increased risk of mortality (32, 33). Consuming antioxidant-rich foods can reduce inflammatory factors and lower the risk of mortality (9).
Thirdly, improving gut microbiota is crucial. Research indicates that dysbiosis of gut microbiota is associated with depression (34) and poor prognosis for various chronic diseases (35, 36). A study by Ogdur et al. (37) revealed significant differences in the gut microbiota composition of suicide victims compared to controls, particularly in genera such as Bacteroides, Clostridium, Lactobacillus, and Bifidobacterium. Therefore, supplementing probiotics to individuals with gut microbiota imbalance may help reduce the risk of suicide death. Moreover, consuming antioxidant-rich foods can regulate gut microbiota to alleviate depressive symptoms and prolong patients’ lives (38, 39).
The findings from this study could provide valuable insights for the management and prevention of suicide risk. Firstly, this study represents the pioneering use of CDAI in predicting the risk of suicidal ideation, thus holding substantial clinical significance. Secondly, we meticulously considered appropriate sampling weights in our analysis to mitigate biases stemming from oversampling, thereby enhancing the reliability of our conclusions. Lastly, due to the nationally representative sample of American adults, these findings can be extrapolated to a wider population (40). However, the study also has several limitations: (1) The cross-sectional design hinders establishing causality, thus the causal relationship between CDAI and suicidal ideation cannot be determined. (2) Diagnosis of suicidal ideation primarily relies on questionnaire formats, which may entail measurement errors. (3) Despite adjustments for many other confounding factors, limitations of the NHANES database prevent the complete elimination of all potential confounders’ final impact on the study outcomes (40). (4) It is important to acknowledge that factors such as treatment for suicidal patients, experiences with substance addiction, and the presence of gastrointestinal disorders or food allergies may influence the results of this study. Future research should account for these factors and their potentially confounding effects to provide a more comprehensive understanding of the relationship between CDAI and suicidal ideation. (5) Furthermore, individuals frequently use psychotropic medications and counseling interventions to prevent or alleviate psychological symptoms without a doctor’s prescription. These factors may influence the study’s results, and we urge a careful interpretation of the findings.
5 Conclusion
In conclusion, our study indicates a negative relationship between CDAI and the occurrence of suicidal ideation as well as all-cause mortality. These findings may aid public health officials and mental health professionals in formulating relevant policies to prevent the occurrence of suicide tragedies.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Publicly available datasets were analyzed in this study. The data can be found here: https://www.cdc.gov/nchs/nhanes/.
Ethics statement
The studies involving humans were approved by the NHANES and the Research Ethics Review Board of the NCHS, and all participants provided written informed consent. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SH: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. WZ: Conceptualization, Data curation, Formal analysis, Investigation, Software, Writing – original draft, Writing – review & editing. SC: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. HG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are very grateful to the NHANES database for all the data provided.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1457244/full#supplementary-material
Abbreviations
NHANES, National Health and Nutrition Examination Survey; CDAI, Composite Dietary Antioxidant Index; RCS, Restricted cubic spline; ACM, All-cause mortality; CVM, Cardiovascular disease mortality; PHQ-9, Patient Health Questionnaire 9; K-M, curves Kaplan–Meier curves; CHD, coronary heart disease.
Footnotes
References
1. Parekh, A, and Phillips, M. Preventing suicide: a global imperative. World Health Organization (2014). Available at: https://www.who.int/publications/i/item/9789241564779
2. Turecki, G, and Brent, DA. Suicide and suicidal behaviour. Lancet. (2016) 387:1227–39. doi: 10.1016/S0140-6736(15)00234-2
3. Kukoyi, O, Orok, E, Oluwafemi, F, Oni, O, Oluwadare, T, Ojo, T, et al. Factors influencing suicidal ideation and self-harm among undergraduate students in a Nigerian private university. Middle East Curr Psychiatry. (2023) 30:1. doi: 10.1186/s43045-022-00274-1
4. Klonsky, ED, Dixon-Luinenburg, T, and May, AM. The critical distinction between suicidal ideation and suicide attempts. World Psychiatry. (2021) 20:439–41. doi: 10.1002/wps.20909
5. Ma, R, Zhou, X, Zhang, G, Wu, H, Lu, Y, Liu, F, et al. Association between composite dietary antioxidant index and coronary heart disease among US adults: a cross-sectional analysis. BMC Public Health. (2023) 23:2426. doi: 10.1186/s12889-023-17373-1
6. Teng, T-Q, Liu, J, Hu, F-F, Li, Q-Q, Hu, Z-Z, and Shi, Y. Association of composite dietary antioxidant index with prevalence of stroke: insights from NHANES 1999-2018. Front Immunol. (2024) 15:1306059. doi: 10.3389/fimmu.2024.1306059
7. Wang, S, Teng, H, Zhang, L, and Wu, L. Association between dietary antioxidant intakes and chronic respiratory diseases in adults. World Allergy Organ J. (2024) 17:100851. doi: 10.1016/j.waojou.2023.100851
8. Zhou, H, Li, T, Li, J, Zheng, D, Yang, J, and Zhuang, X. Linear association of compound dietary antioxidant index with hyperlipidemia: a cross-sectional study. Front Nutr. (2024) 11:1365580. doi: 10.3389/fnut.2024.1365580
9. Luo, J, Xu, X, Sun, Y, Lu, X, and Zhao, L. Association of composite dietary antioxidant index with depression and all-cause mortality in middle-aged and elderly population. Sci Rep. (2024) 14:9809. doi: 10.1038/s41598-024-60322-0
10. Cavanagh, JTO, Carson, AJ, Sharpe, M, and Lawrie, SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. (2003) 33:395–405. doi: 10.1017/s0033291702006943
11. Huang, S, He, Q, Wang, X, Choi, S, and Gong, H. Associations of the planetary health diet index (PHDI) with asthma: the mediating role of body mass index. BMC Public Health. (2024) 24:2305. doi: 10.1186/s12889-024-19856-1
12. NHANES – NCHS Research Ethics Review Board Approval. (2022) https://www.cdc.gov/nchs/nhanes/irba98.htm (accessed April 23, 2024).
13. He, H, Chen, X, Ding, Y, Chen, X, and He, X. Composite dietary antioxidant index associated with delayed biological aging: a population-based study. Aging (Albany NY). (2024) 16:15–27. doi: 10.18632/aging.205232
14. Huang, D, Zhong, S, Yan, H, Lai, S, Lam, M, and Jia, Y. Association between serum zinc levels and suicidal ideation in US adults: A population-based cross-sectional study. J Affect Disord. (2023) 329:359–68. doi: 10.1016/j.jad.2023.02.039
15. Liang, J-H, Ge, W-X, Jin, Z-G, Wang, C, Liu, M-L, Pu, Y-Q, et al. Sexual orientation disparities in the prevalence of suicidal ideation among U.S adults aged 20 to 59 years: results from NHANES 2005-2016. Psychiatry Res. (2024) 331:115639. doi: 10.1016/j.psychres.2023.115639
16. Sahraian, A, Ghanizadeh, A, and Kazemeini, F. Vitamin C as an adjuvant for treating major depressive disorder and suicidal behavior, a randomized placebo-controlled clinical trial. Trials. (2015) 16:94. doi: 10.1186/s13063-015-0609-1
17. Strumila, R, Lengvenyte, A, Olie, E, Seneque, M, Dupuis-Maurin, K, Alacreu-Crespo, A, et al. Selenium deficiency is associated with disease severity, disrupted reward processing, and increased suicide risk in patients with anorexia nervosa. Psychoneuroendocrinology. (2022) 140:105723. doi: 10.1016/j.psyneuen.2022.105723
18. Sher, L . Possible role of selenium deficiency in the neurobiology of depression and suicidal behavior in patients with alcohol use disorders. Int J Disabil Hum Dev. (2007) 6:227–30. doi: 10.1515/IJDHD.2007.6.3.227
19. Koweszko, T, Gierus, J, Zalewska, A, Maciejczyk, M, Waszkiewicz, N, and Szulc, A. The relationship between suicide and oxidative stress in a Group of Psychiatric Inpatients. J Clin Med. (2020) 9:3462. doi: 10.3390/jcm9113462
20. Loo, JL, Mohamad Kamal, NA, Goon, JA, Ahmad Damanhuri, H, Tan, JAC, Abdul Murad, NA, et al. The role of oxidative stress in suicidal behaviour among bipolar patients: A cross-sectional study in a Malaysian sample. Front Psych. (2021) 12:698911. doi: 10.3389/fpsyt.2021.698911
21. Raza, MU, Tufan, T, Wang, Y, Hill, C, and Zhu, M-Y. DNA damage in major psychiatric diseases. Neurotox Res. (2016) 30:251–67. doi: 10.1007/s12640-016-9621-9
22. Rafighi, Z, Shiva, A, Arab, S, and Yusuf, RM. Association of Dietary Vitamin C and E Intake and antioxidant enzymes in type 2 diabetes mellitus patients. Glob J Health Sci. (2013) 5:183–7. doi: 10.5539/gjhs.v5n3p183
23. Sesso, HD, Buring, JE, Christen, WG, Kurth, T, Belanger, C, MacFadyen, J, et al. Vitamins E and C in the prevention of cardiovascular disease in men: the physicians’ health study II randomized trial. JAMA. (2008) 300:2123–33. doi: 10.1001/jama.2008.600
24. Dagenais, GR, Marchioli, R, Tognoni, G, and Yusuf, S. Beta-carotene, vitamin C, and vitamin E and cardiovascular diseases. Curr Cardiol Rep. (2000) 2:293–9. doi: 10.1007/s11886-000-0084-4
25. Losonczy, K, Harris, T, and Havlik, R. Vitamin E and vitamin C supplement use and risk of all-cause and coronary heart disease mortality in older persons: the established populations for epidemiologic studies of the elderly. Am J Clin Nutr. (1996) 64:190–6. doi: 10.1093/ajcn/64.2.190
26. Lee, C-H, and Giuliani, F. The role of inflammation in depression and fatigue. Front Immunol. (2019) 10:1696. doi: 10.3389/fimmu.2019.01696
27. Brådvik, L . Suicide risk and mental disorders. Int J Environ Res Public Health. (2018) 15:2028. doi: 10.3390/ijerph15092028
28. Xu, Y, Wang, C, Klabnik, JJ, and O’Donnell, JM. Novel therapeutic targets in depression and anxiety: antioxidants as a candidate treatment. Curr Neuropharmacol. (2014) 12:108–19. doi: 10.2174/1570159X11666131120231448
29. Shiraishi, FG, Stringuetta Belik, F, Oliveira e Silva, VR, Martin, LC, Hueb, JC, De S, GR, et al. Inflammation, diabetes, and chronic kidney disease: role of aerobic capacity. Exp Diabetes Res. (2012) 2012:750286:1–6. doi: 10.1155/2012/750286
30. Stenvinkel, P, Chertow, GM, Devarajan, P, Levin, A, Andreoli, SP, Bangalore, S, et al. Chronic inflammation in chronic kidney disease progression: role of Nrf2. Kidney Int Rep. (2021) 6:1775–87. doi: 10.1016/j.ekir.2021.04.023
31. Patrick, DM, Van Beusecum, JP, and Kirabo, A. The role of inflammation in hypertension: novel concepts. Curr Opin Physio. (2021) 19:92–8. doi: 10.1016/j.cophys.2020.09.016
32. Mason, JC, and Libby, P. Cardiovascular disease in patients with chronic inflammation: mechanisms underlying premature cardiovascular events in rheumatologic conditions. Eur Heart J. (2015) 36:482–9. doi: 10.1093/eurheartj/ehu403
33. Shah, NN, Wass, S, Hajjari, J, Heisler, AC, Malakooti, S, Janus, SE, et al. Proportionate cardiovascular mortality in chronic inflammatory disease in adults in the United States from 1999 to 2019. J Clin Rheumatol. (2022) 28:97–103. doi: 10.1097/RHU.0000000000001818
34. Liu, L, Wang, H, Chen, X, Zhang, Y, Zhang, H, and Xie, P. Gut microbiota and its metabolites in depression: from pathogenesis to treatment. EBioMedicine. (2023) 90:104527. doi: 10.1016/j.ebiom.2023.104527
35. Muñoz-Garach, A, Diaz-Perdigones, C, and Tinahones, FJ. Gut microbiota and type 2 diabetes mellitus. Endocrinol Nutr. (2016) 63:560–8. doi: 10.1016/j.endoen.2016.07.004
36. Gagnière, J, Raisch, J, Veziant, J, Barnich, N, Bonnet, R, Buc, E, et al. Gut microbiota imbalance and colorectal cancer. World J Gastroenterol. (2016) 22:501–18. doi: 10.3748/wjg.v22.i2.501
37. Öğdür, M, Cakan, H, and Evrensel, A. Investigation of gut microbiota in suicide cases instead of forensic sciences. Med Sci. (2022) 11:361–6. doi: 10.5455/medscience.2021.09.311
38. Bear, TLK, Dalziel, JE, Coad, J, Roy, NC, Butts, CA, and Gopal, PK. The role of the gut microbiota in dietary interventions for depression and anxiety. Adv Nutr. (2020) 11:890–907. doi: 10.1093/advances/nmaa016
39. Xiong, R-G, Li, J, Cheng, J, Zhou, D-D, Wu, S-X, Huang, S-Y, et al. The role of gut microbiota in anxiety, depression, and other mental disorders as well as the protective effects of dietary components. Nutrients. (2023) 15:3258. doi: 10.3390/nu15143258
Keywords: CDAI, suicidal ideation, all-cause mortality, NHANES, mortality
Citation: Huang S, Zhao W, Choi S and Gong H (2024) Associations of composite dietary antioxidant index with suicidal ideation incidence and mortality among the U.S. population. Front. Nutr. 11:1457244. doi: 10.3389/fnut.2024.1457244
Edited by:
Magdalena Sowa-Kućma, University of Rzeszow, PolandReviewed by:
Paulina Misztak, Louisiana State University, United StatesMassimo Tusconi, University of Cagliari, Italy
Copyright © 2024 Huang, Zhao, Choi and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyang Gong, aHlnb25nQGNob3N1bi5hYy5rcg==
 Shaoqun Huang1
Shaoqun Huang1 Hongyang Gong
Hongyang Gong