- 1Department of General Surgery, Nanfang Hospital, Southern Medical University, Guangzhou, China
- 2School of Nursing, Southern Medical University, Guangzhou, China
- 3Department of Thoracic Surgery, Nanfang Hospital, Southern Medical University, Guangzhou, China
Background: Globally, diet low in milk is the third greatest risk factor for colorectal cancer (CRC). However, there has been a lack of detailed worldwide analysis of the burden and trends of CRC attributable to diet low in milk.
Objective: We aim to assess the spatiotemporal trends of CRC-related mortality and disability-adjusted life-years (DALYs) attributable to diet low in milk at the global, regional, and national levels from 1990 to 2019.
Methods: Data of mortality, DALYs, age-standardized mortality rate (ASMR), and age-standardized DALY rate (ASDR) of CRC attributable to diet low in milk were extracted from the Global Burden of Disease (GBD) 2019 study. The burden of CRC attributable to diet low in milk was estimated using the ASMR and ASDR, while accounting for sex, age, country, and socio-demographic index (SDI). From 1990 to 2019, the estimated annual percentage change (EAPC) was calculated to clarify the temporal trends in the ASMR and ASDR attributable to diet low in milk.
Results: In 2019, there were 166,456 (95% UI = 107,221–226,027) deaths and 3,799,297 (95% UI = 2,457,768–5,124,453) DALYs attributable to diet low in milk, accounting for 15.3 and 15.6% of CRC-related deaths and DALYs in 2019. CRC-related deaths and DALYs attributed to diet low in milk increased by 130.5 and 115.4%, from 1990 to 2019. The burden of CRC attributable to diet low in milk varied notably among regions and nations. High-middle SDI regions had the highest ASDR and ASMR of CRC linked to diet low in milk, while there was a slight downward trend high SDI regions. Among geographical regions, East Asia had the highest number of CRC-related deaths and DALYs attributable to diet low in milk. Notably, the burden of CRC was highest in males and the elderly. With coefficients of −0.36 and −0.36, the EAPC in ASMR and ASDR was significantly inversely correlated with the Human Development Index in 2019.
Conclusion: Globally, the number of CRC deaths attributable to diet low in milk has continued to increase over the last 30 years. Therefore, government and authorities should conduct education campaigns to encourage individuals to increase daily milk intake.
1 Introduction
As the second most common malignancy and the third most common cause of cancer-related death globally, colorectal cancer (CRC) accounted for more than 2.1 million (7%) of all new cancer cases and 1.0 million (11%) of all cancer-related deaths worldwide in 2019 (1). There are considerable geographic variations in the burden of CRC, which is strongly associated with socioeconomic status (2). Traditionally, the incidence and mortality rates of CRC are highest in Europe, Oceania, and North America (3, 4). However, the incidence rates are rising in high-middle socio-demographic index (SDI) regions, notably in East Asia, Eastern Europe, Asia, and South America, as a result of economic improvements and shifts in dietary patterns and lifestyles (5, 6). Consequently, CRC remains a significant economic and medical challenge globally.
Multiple risk factors would promote the malignant development of CRC, such as genetic, age, environmental, lifestyle (dietary habits and activities) and metabolic risks (7). However, the exact cause of CRC is still unknown, and these risk factors may lead to potential confounders that could lead to spurious relationships in the observed data. In the GBD study, the three highest attributable proportions of risk factors of CRC in 2019 were diet low in whole grain diet (15.8%), diet low in milk (15.3%), and smoking (12.9%) (8). The risk attributable to diet low in milk have exceeded the risk attributable to diet high in processed meat. Meanwhile, the proportion of CRC attributable risk attributable to diet high in processed meat diet decreased (9). Milk, as a cheap and commonly consumed food worldwide, can provides a variety of macronutrients, micronutrients, and bioactive components that are crucial to growth and development (10). In addition, milk conveys various potential health advantages, including anti-cancer, anti-inflammatory, antioxidant, anti-fat, anti-hypertension, anti-hyperglycemia, and anti-osteoporosis activities (11). A recent meta-analysis of 15 cohort studies involving 11,733 individuals found that higher consumption of total dairy products and milk may be associated with a decreased risk of CRC (12). Moreover, the American Institute for Cancer Research and the World Cancer Research Fund found that drinking milk may reduce the incidence of CRC (13). However, the majority of the population does not reach the recommended daily milk intake, and there is a lack of updated epidemiological research analyzing colorectal cancer due to low dietary milk levels from a global perspective. Therefore, it is necessary to systematically explore the burden of colorectal cancer attributable to diet low in milk.
The Global Burden of Disease (GBD) 2019 study provides comprehensive and up-to-date data of 369 diseases and injuries, as well as 87 risk factors, from more than 204 countries and territories worldwide (14). Several recent studies have utilized the GBD database to investigate the global, regional, and national burdens of CRC and identify associated risk factors. The results of these studies revealed that the primary risk factors for disability-adjusted life years (DALYs) associated with CRC across all countries and regions were diet low in milk, smoking, low calcium diets, and alcohol intake (7–9). A prior study (15) was conducted to analyze the burden and trend of CRC attributable to diet low in milk in China from 1990 to 2017, but this investigation only focused on a single country. To the best of our knowledge, there has not yet been any detailed worldwide analysis of the burden and trends of CRC attributable to diet low in milk.
Therefore, the aim of this comprehensive review was to quantified the global, regional, and national disease burden associated with CRC attributable to a low milk diet in reference to the most recent data from the GBD 2019 study. In addition, potential correlations among the human development index (HDI), sociodemographic index (SDI), and CRC burden were assessed. Moreover, the estimated annual percentage change (EAPC) was calculated in order to quantify the trend of the age-standardized rate (ASR) over time. The results of this study will help to better understand the impact of diet low in milk in order to decrease the incidence and burden of CRC.
2 Materials and methods
2.1 Data source
All data were derived from the GBD 2019 study, which was a cooperative international research project to estimate the burden of 286 causes of death, 369 diseases and injuries, and 87 risk factors in 204 countries or territories, 21 regions, and 5 SDI regions from 1990 to 2019 (16). The GBD 2019 research team collected raw data from civil registration, vital statistics, hospital records, and household surveys in each country, providing reliable estimates about the burden of colorectal cancer. DisMod-MR version 2.1 was used to adjust for bias in the raw data to provide internally consistent estimates of prevalence by age, gender, location, and year (17). With the use of the Global Health Data Exchange website,1 the number of CRC deaths and DALYs attributable to diet low in milk, as well as additional age-standardized mortality rates (ASMRs) and age-standardized DALY rates (ASDRs) of 204 countries and territories between January 1, 1990 and December 31, 2019 were obtained from the GBD 2019 study and stratified by sex, age, GBD region, and SDI quintile. The detailed methods for data input, mortality estimation, and modelling of the GBD 2019 study were obtained from earlier published articles (18). The searched terms included “colorectal cancer,” “diet low in milk,” “death” and “DALYs,” in addition to the years “1990–2010,” “1990–2019,” and “2010–2019,” as well as the metrics “number,” “percent,” and “rate.” The HDI values were retrieved from the United Nations Development Programme database.2
2.2 Definitions
The GBD 2019 study defined diet low in milk as an average daily intake of less than 360–500 g of whole, skim, and semiskim milk, excluding soy milk and other plant-based products (7). DALY is the sum of all healthy life-years lost between the onset of disease and mortality. The ASR was calculated based on age groups of the standard population. Because the total population mortality and DALY rate are influenced not only by the level of mortality and DALY rate of each age group, as well as the age composition of the population, the ASR provides the ability to eliminate the effect of the age composition of the population to enable more accurate comparisons of total mortality and DALY rates of different regions and time periods.
In addition, the correlation between the burden of disease and the SDI was analyzed. The SDI is a composite indicator of the average per capita income, fertility, and educational level of each country and region. The 204 countries and regions were divided into five categories based on the SDI: low (<0.45), low-middle (≥0.45 and <0.61), middle (≥0.61 and <0.69), high-middle (≥0.69 and <0.80), and high (≥0.80).
2.3 Statistical analysis
The burden of CRC attributable to diet low in milk was assessed by SDI, region, country, sex, and age group based on the number of deaths, DALYs, ASDR, and ASMR. The following formula was used to calculate the ASR:
where ai is the age-specific rate in the ith age group, w is the number of people (or the weight) in the respective ith age group from the chosen standard population, and A is the number of age groups. All rates are provided as per 100,000 persons in order to avoid effects due to the age composition of the populations. Rather than using the global population size in 2019, the weight was based on the global standard population (GBD 2019 study). Moreover, linear regression was used to calculate the EAPC, as linear regression research predicts the value of unknown data by using another relevant known data value. EAPC is approximately equal to the annual change over a specified time period, to evaluate trends in the ASR. The regression model used to assess trends in the ASR was y = α + βx + ε, where x is the calendar year, y is the ln(ASMR or ASDR), ε is the error term, and β is the positive or negative trend of the ASR. The exact calculation was EAPC = 100 (exp(β) − 1). The 95% confidence interval (CI) was obtained from the linear regression model. If the EAPC and 95% CI were >0, the ASR was considered an increasing trend or <0 as a decreasing trend. Otherwise, the ASR was considered stable. The 204 countries or territories were divided into four groups based on temporal trends using hierarchical cluster analysis: remained stable, minor increase, significant increase, or decrease. Finally, to identify variables influencing the EAPC, Pearson’s correlation analysis was performed to analyze the relationship between the EAPCs and ASR in 1990, as well as the relationship between the EAPCs and HDI in 2019. The reason for choosing Pearson’s correlation analysis is that it can effectively measure linear correlation in continuous data. All statistical analyses were performed using R software version 4.2.3.3 A probability (p) value <0.05 was considered statistically significant.
3 Results
3.1 Global trends of CRC attributable to diet low in milk
In 2019, the global number of CRC-related deaths and DALYs attributable to diet low in milk were estimated at 166,456 [95% uncertainty interval (UI) = 107,221–226,027] and 3,799,297 (95% UI = 2,457,768–5,124,453), representing 15.3 and 15.6% of all CRC-related deaths and DALYs, respectively (Figure 1). Between 1990 and 2019, the number of global deaths from CRC associated with diet low in milk increased by 130.5%, from 72,199 (95% UI = 44,384–99,966) to 166,456 (95% UI = 107,221–226,027), respectively. Similarly, the number of DALYs increased by 115.4%, from 1,764,172 (95% UI = 1,115,033–2,420,485) to 3,799,297 (95% UI = 2,457,768–5,124,453), respectively. In 2019, the ASDR and ASMR were 46.09 (95% UI = 29.83–62.18) and 2.09 (95% UI = 1.34–2.84) per 100,000, respectively. Both the global CRC-associated ASMR and ASDR due to diet low milk had modestly increased, with EAPCs of 0.19% [95% Confidence Interval (CI) = 0.16–0.23] and 0.19% (95% CI = 0.16–0.22), respectively (Table 1; Figure 2).
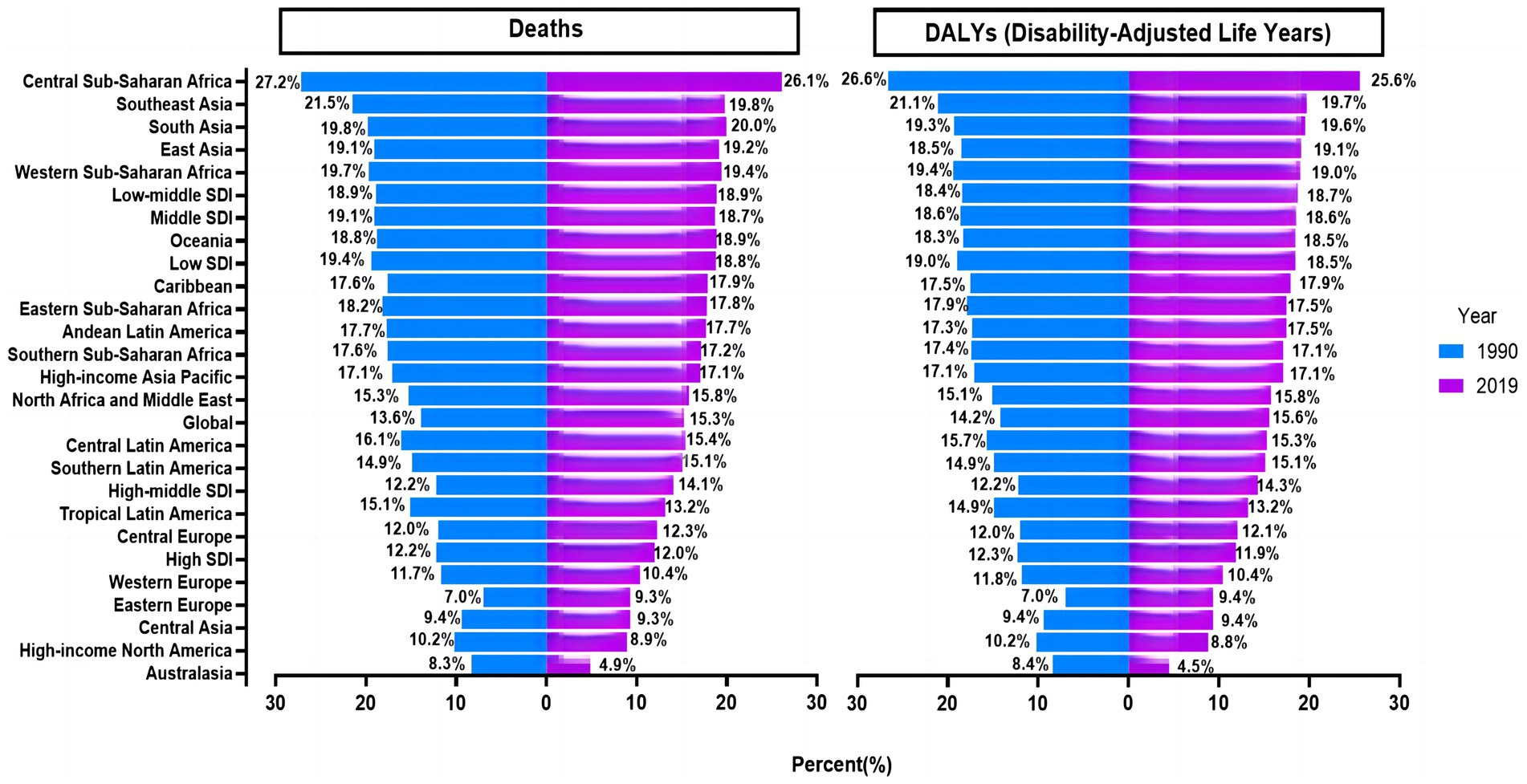
Figure 1. Proportion of colorectal cancer deaths and DALYs attributable to diet low in milk globally and in 26 GBD regions in 1990 and 2019. DALYs, disability-adjusted life-years; GBD, Global Burden of Disease Study.
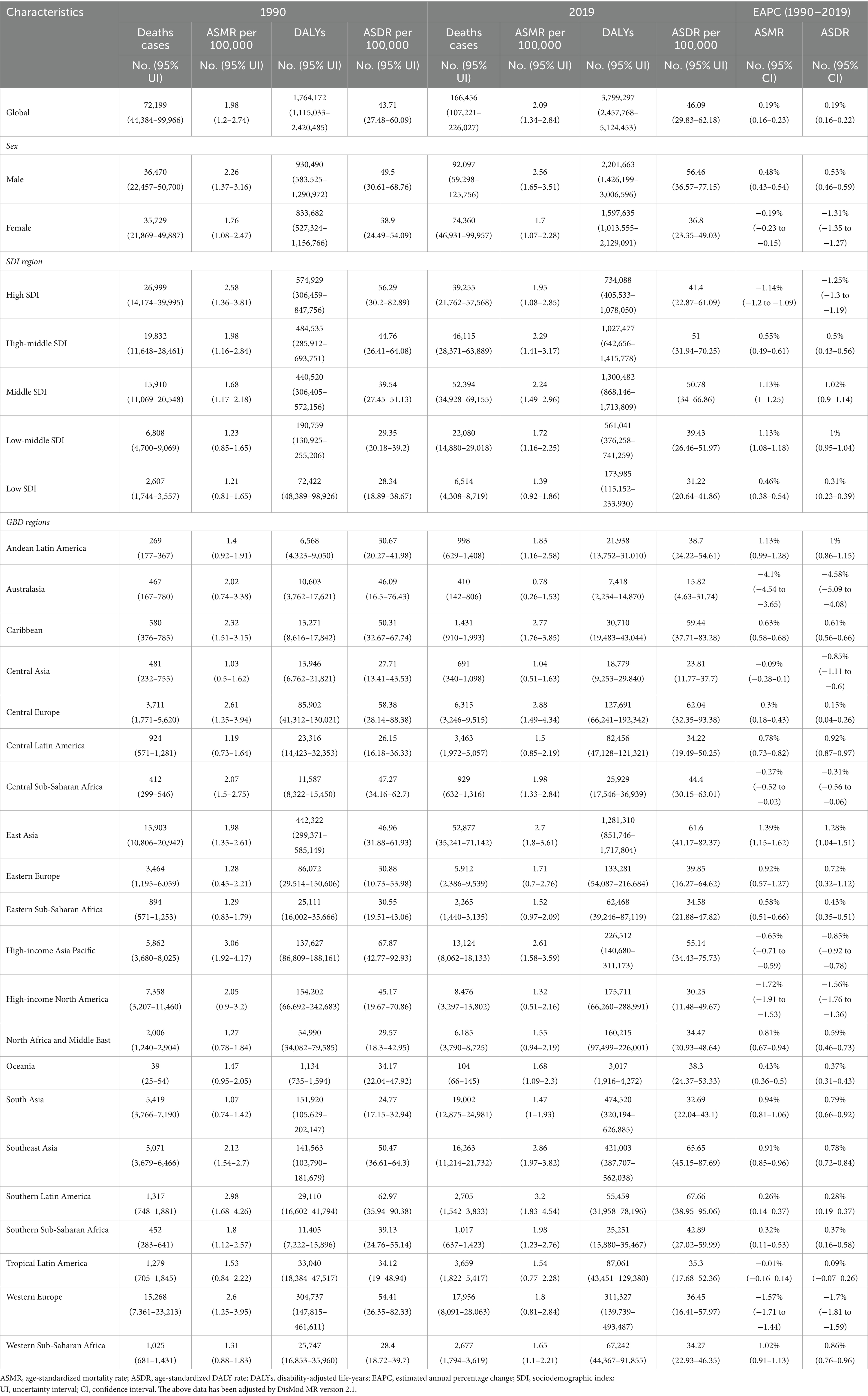
Table 1. Global burden of colon and rectum cancer in 1990 and 2019 for both sexes and all locations, with EAPC.
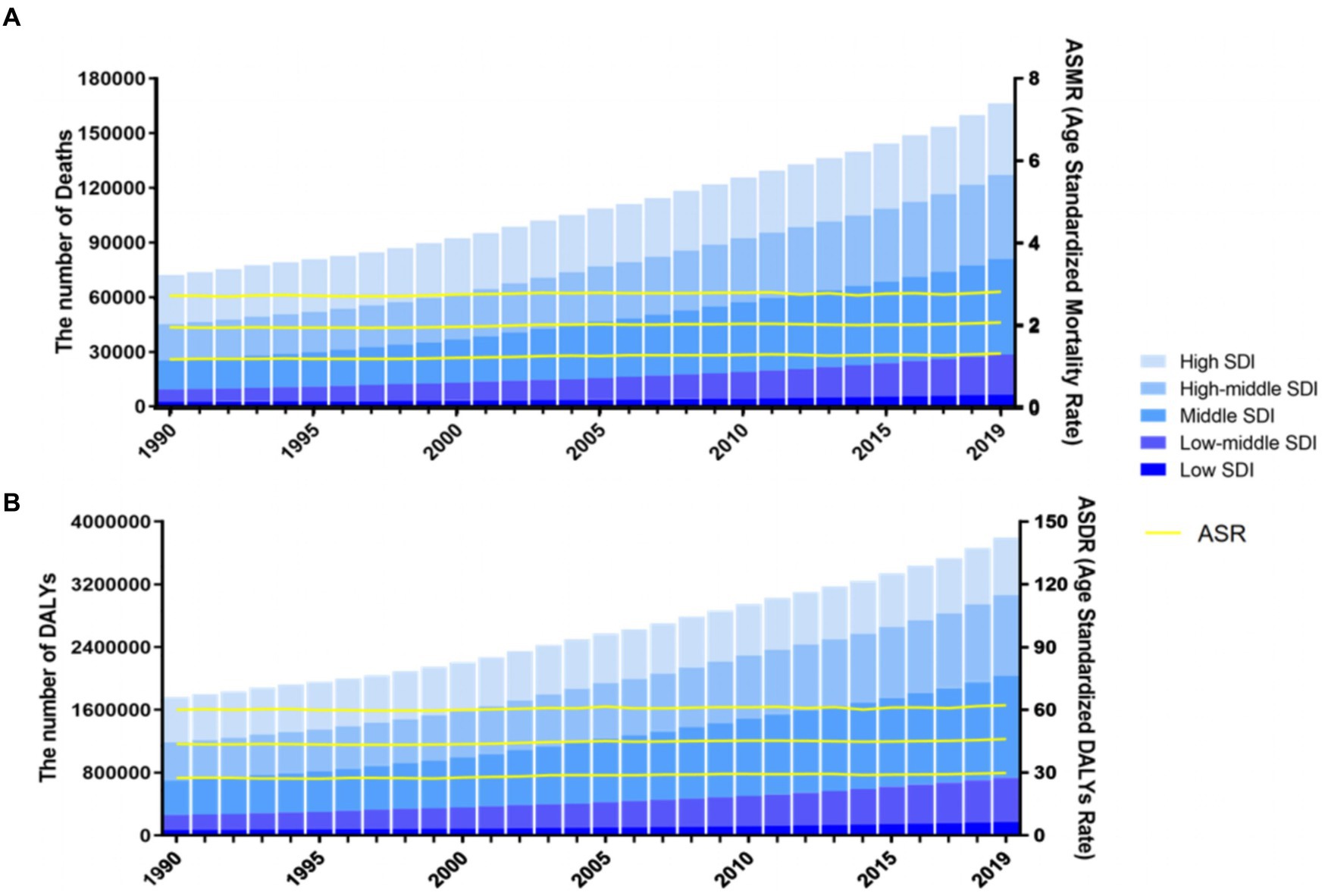
Figure 2. Number and rate of colorectal cancer deaths (A) and DALYS (B) attributable to diet low in milk from 1990 to 2019 by SDI level. The bars represent the number of colorectal cancer deaths (A) and DALYS (B) attributable to diet low in milk from 1990 to 2019 colored by SDI level. The line represents the mean ASMR (A) and ASDR (B) (per 100,000) attributable to diet low in milk at the global level. The shaded area represents the 95% UI for the mean rate. ASMR, age-standardized mortality rate; ASDR, age-standardized DALY rate; DALYs, disability-adjusted life-years; SDI, socio-demographic index; UI, uncertainty interval.
3.2 Geographical variations in CRC attributable to diet low in milk
In 2019, the middle SDI regions had the highest number of CRC-related deaths [52,394 (95% UI = 34,928–69,155)] and DALYs [1,300,482 (95% UI = 868,146–1,713,809)] due to diet low in milk. Conversely, the lowest SDI regions had the low number of CRC-related deaths [6,514 (95% UI = 4,308–8,719)] and DALYs [173,985 (95% UI = 115,152–233,930)]. At the same time, high-middle SDI regions had the greatest ASMR [2.29 (95% CI = 1.41–3.17)] and ASDR [51 (95% CI = 31.94–70.25)] per 100,000, respectively. From 1990 to 2019, the ASMR and ASDR of the low, low-middle, middle, and high-middle SDI regions had gradually increased, whereas those of the high SDI regions had decreased (Table 1).
Geographically, East Asia had the highest number of CRC-related deaths [52,877 (95% UI = 35,241–71,142)] and DALYs [1,281,310 (95% UI = 851,746–1,717,804)] in 2019 associated with diet low in milk. Also in 2019, Australasia had the lowest and Southern Latin America had the highest ASMR and ASDR (0.78 and 3.2 deaths vs. 15.82 and 67.66 DALYs per 100,000, respectively). Between 1990 and 2019, Australasia had the largest decreases and East Asia had the largest increases in ASMR and ASDR [−4.1 (95% CI = −4.54 to −3.65) vs. 1.39 (95% CI = 1.15–1.62) and −4.58 (95% CI = −5.09 to −4.08) vs. 1.28 (95% CI = 1.04–1.51), respectively] (Table 1). Central Sub-Saharan Africa, Southeast Asia, and South Asia had the largest percentage of CRC deaths and DALYs linked to low milk consumption in 1990, while Eastern Europe, Australasia, Central Asia and High-income North America had the lowest percentages. This disparity was roughly three times larger in 1990. Similar trends were observed in the proportion attributable to diet low in milk in 2019 (Figure 1).
3.3 Country-level burden of CRC attributable to diet low in milk
In 2019, at the nation level, China had the highest number of CRC deaths and DALYs associated with diet low in milk [50,310 (95% UI = 33,195–67,665) and 1,222,433 (95% UI = 804,709–1,648,733), respectively], followed by India [16,394 (95% UI = 11,214–21,686) and 406,643 (95% UI = 276,849–542,329), respectively], and Japan [10,794 (95% UI = 6,541–1,5,041) and 178,533 (95% UI = 109,415–248,995), respectively]. Also in 2019, Albania, Finland, and Kyrgyzstan had the greatest ASMR owing to diet low in milk, whereas Seychelles, Brunei Darussalam, and Taiwan (Province of China) had the highest ASDR (Figures 3A,B). Equatorial Guinea, Latvia, and Vietnam had the highest increases in ASMR, with EAPCs of 3.67 (95% CI = 3.37–3.96), 2.68 (95% CI = 1.89–3.48), and 2.65 (95% CI = 2.42–2.67), respectively. Similarly, Equatorial Guinea, Lesotho, and Vietnam had the highest increases in ASDR, with EAPCs of 3.22 (95% CI = 2.95–3.49), 2.64% (95% CI = 2.41–2.87), and 2.57 (95% CI = 2.42–2.72), respectively. Meanwhile, Albania experienced the fastest decline in ASMR and ASDR, with EAPCs of −8.06 (95% CI = −8.74 to −7.38) and −8.74 (95% CI = −9.56 to −7.91), respectively (Figures 3C,D; Supplementary Tables S1–S6). The percentage change in the fraction of all CRC deaths and DALYs attributable to diet low in milk is shown in Supplementary Tables S7, S8.
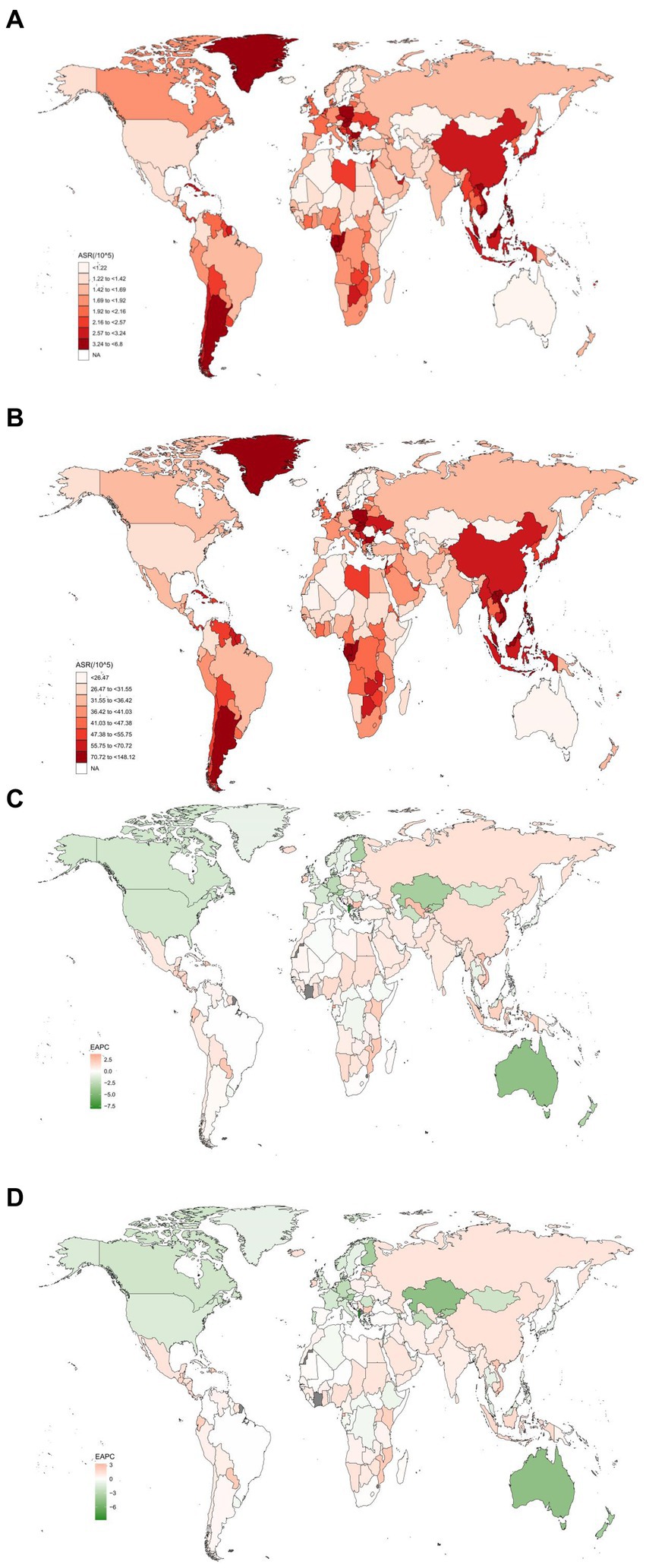
Figure 3. The spatial distribution of the colorectal cancer ASMR (A) and ASDR (B) attributable to diet low in milk in 2019, and the EAPC in colorectal cancer ASMR (C) and ASDR (D) attributable to diet low in milk. ASMR, age-standardized mortality rate; ASDR, age-standardized DALY rate; EAPC, estimated annual percentage change.
3.4 Global CRC burden attributable to diet low in milk by sex and age
Globally, sex inequality continues to influence the burden of CRC attributable to diet low in milk, with a greater impact on males, which increased with age. In 2019, CRC-related deaths and DALYs were more common in males than females [92,097 (95% UI = 59,298–125,756) vs. 74,360 (95% UI = 46,931–99,957) and 2,201,663 (95% UI = 1,426,199–3,006,596) vs. 1,597,635 (95% UI = 1,013,555–2,129,091), respectively] (Table 1). In 2019, the ASMR per 100,000 of CRC linked to diet low in milk was greater in males than females [2.56 (95% UI = 1.65–3.51) vs. 1.7 (95% UI = 1.07–2.28), respectively]. Similarly, ASDR was greater in males than females [56.46 (95% UI = 36.57–77.15) vs. 36.8 (95% UI = 23.35–49.03), respectively]. From 1990 to 2019, the average annual increase in ASMR and ASDR of CRC attributable to diet low in milk was 0.48 (95% CI = 0.43–0.54) and 0.53 (95% CI = 0.46–0.59) for males, while the average annual decrease was −0.19 (95% CI = −0.23 to −0.15) and −1.31 (95% CI = −1.35 to −1.27) for females.
In 2019, the ASMR of CRC attributable to diet low in milk increased with age, with the largest number of deaths occurring in those aged 70–74 years (Figure 4A). Meanwhile, the ASDR decreased progressively after peaking in the group aged 90–94 years, and the largest number of DALYs in the group aged 65–69 years (Figure 4B). From 1990 to 2019, ASMR increased globally in almost all age groups, except for a decrease in groups aged 25–29 and 35–39 years. The group aged >95 years experienced the greatest growth, while the group aged 25–29 had the greatest decline. The ASMR increased in low, low-middle, middle and high-middle SDI regions from 1990 to 2019, with higher EAPCs in mortality in low-middle SDI regions (Figure 5A). The age-standardized DALY rates were similar for EAPCs and ASMR (Figure 5B). The distribution of deaths and DALYs remained stable over time in each of the four age subgroups (Supplementary Figure S1).
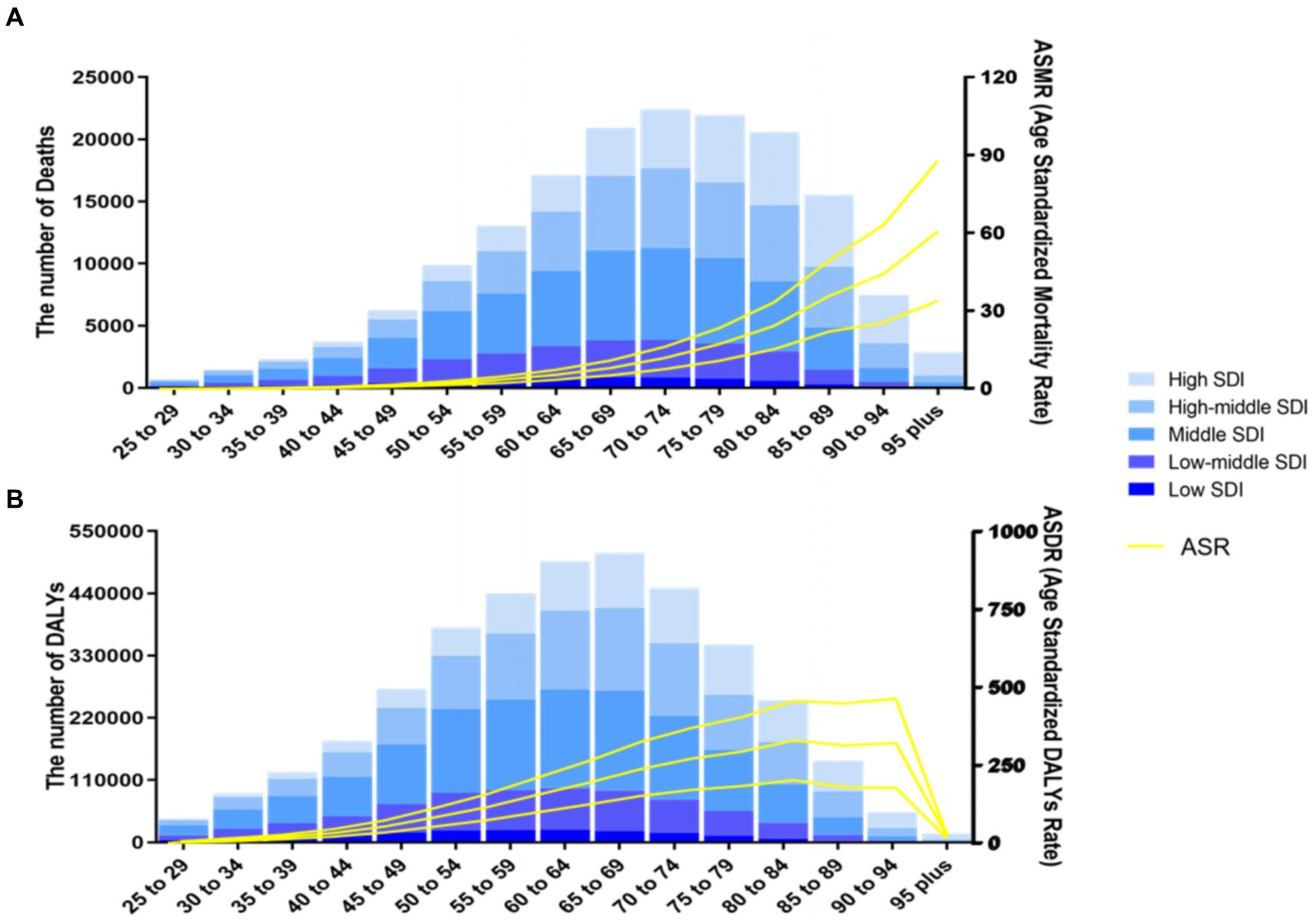
Figure 4. Number and rate of colorectal cancer deaths (A) and DALYs (B) attributable to diet low in milk by age group and SDI level in 2019. The bars represent the number of colorectal cancer deaths (A) and DALYs (B) attributable to diet low in milk colored by SDI level. The line represents the mean ASMR (A) and ASDR (B) (per 100,000) attributable to diet low in milk at the global level. The shaded area represents the 95% UI for the mean rate. DALYs, disability-adjusted life-years; ASMR, age-standardized mortality rate; ASDR, age-standardized DALY rate; UI, uncertainty interval; SDI, socio-demographic index.
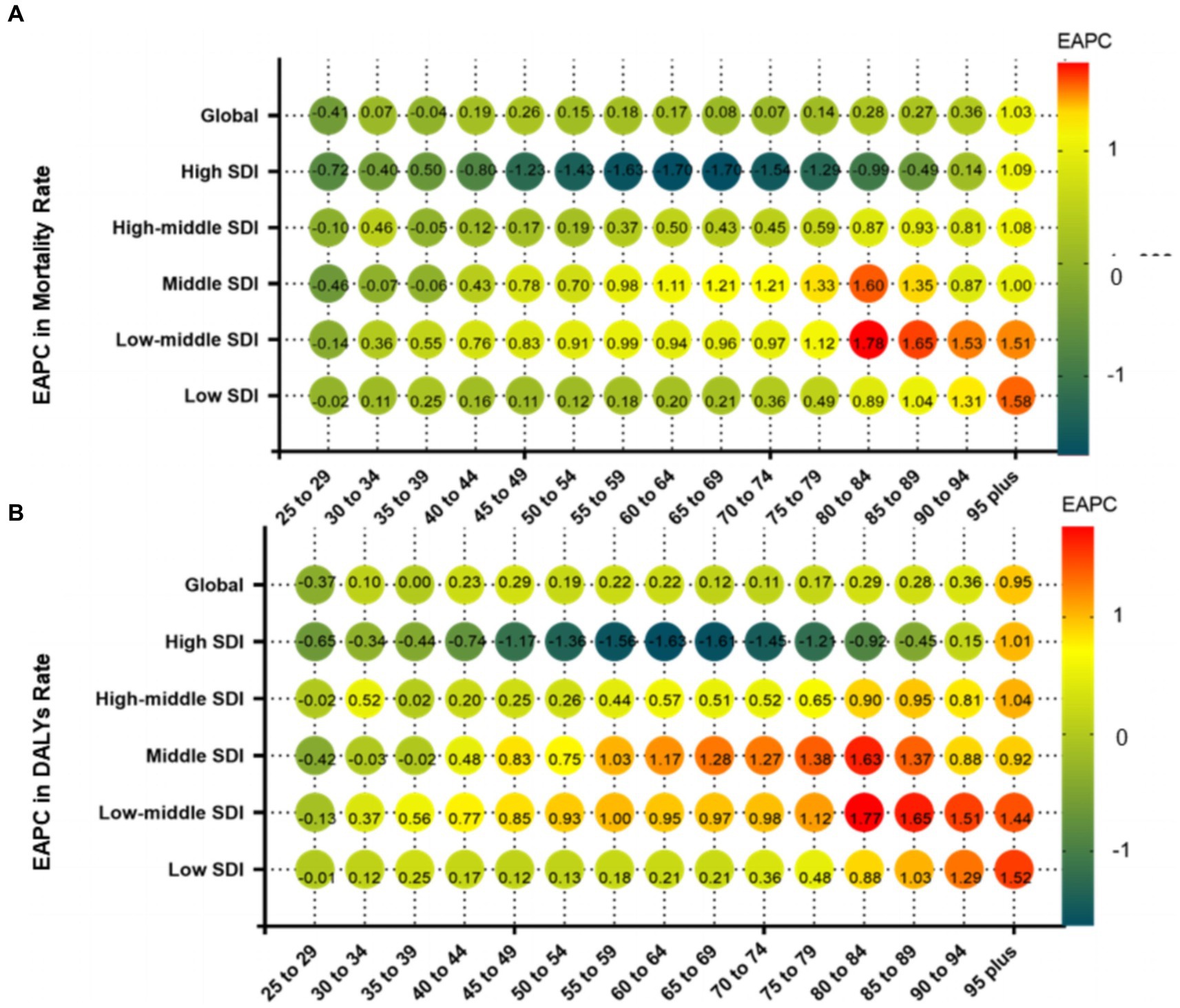
Figure 5. Annual percentage change in mortality (A) and DALYs (B) between 1990 and 2019 by age group and region. EAPC, estimated annual percentage change; SDI, socio-demographic index; DALYs, disability-adjusted life-years.
Cluster analysis revealed that 121 countries or territories, most notably North Macedonia, Benin, and Burkina Faso, were classified as having “remained stable,” while 20 countries or territories were classified as “minor increase,” which included Singapore, Israel, and Portugal. Additionally, 56 countries or territories, including Paraguay, the Dominican Republic, and Mozambique, were classified as “increase.” Albania was the only country to be classified as “significant decrease.” The remaining six nations or territories, including Finland, Kazakhstan, and Australia, were classified as “decrease” (Supplementary Figure S2).
3.5 Factors associated with the burden of CRC burden attributable to diet low in milk
Overall, there was a nonlinear “S”-shaped association between the overall ASMR and SDI, with the ASMR rapidly increasing when the SDI was greater than 0.75 and progressively decreasing at less than 0.45. Among the different regions, the highest ASMR related to diet low in milk were observed in Southern Latin America, followed by high-income Asia Pacific and Central Europe, while the lowest ASMR and ASDR related to diet low in milk occurred in Australasia and Central Asia (Figure 6A). A similar association occurred between ASDR and SDI (Figure 6B). In 2019, across 204 countries and territories globally, the relationships between ASMR and ASDR attributable to CRC and SDI initially increased and then decreased as SDI increased (Figures 7A,B).
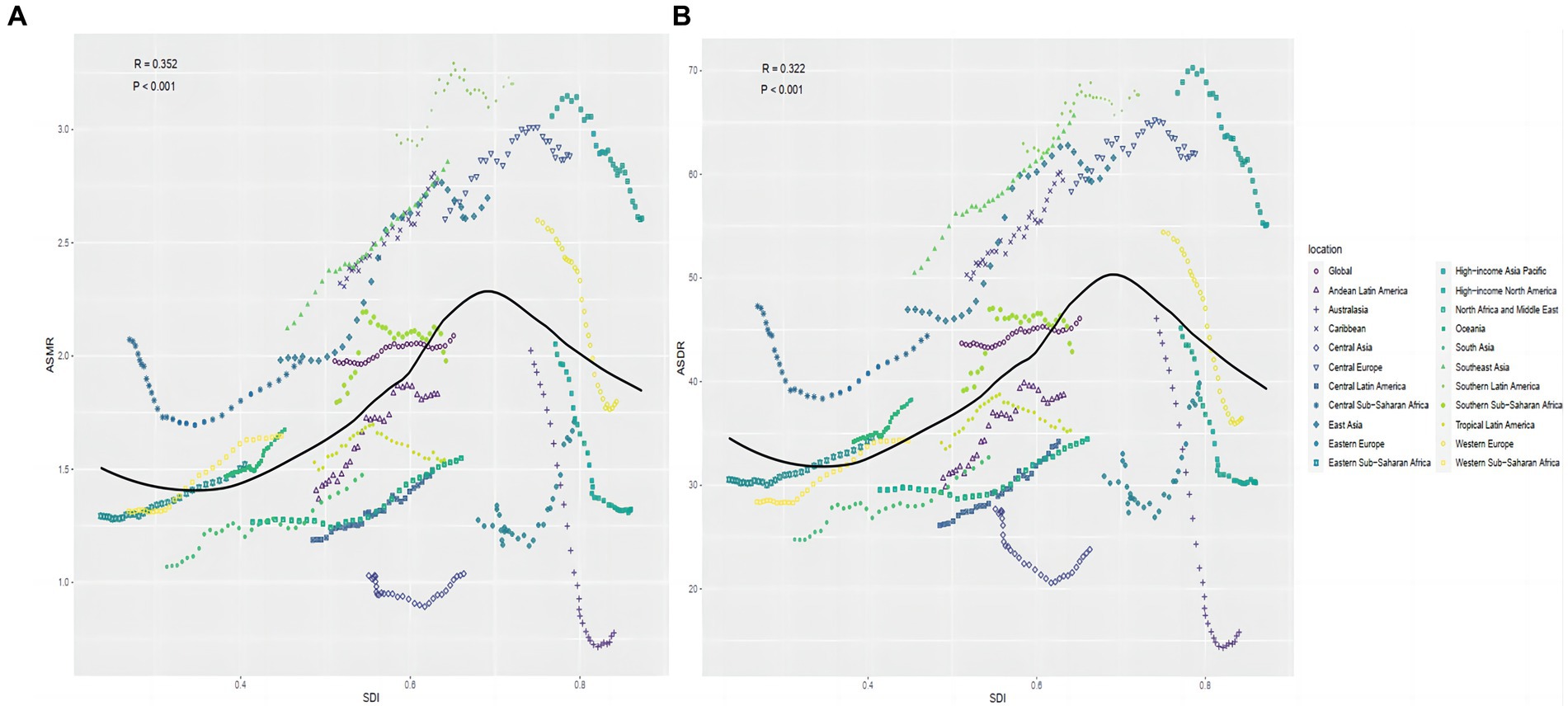
Figure 6. Correlation between diet low in milk-attributable colorectal cancer in ASMR (A) or ASDR (B) and SDI globally in 21 GBD regions between 1990 and 2019. ASMR, age-standardized mortality rate; ASDR, age-standardized DALY rate; GBD, global burden of disease study.
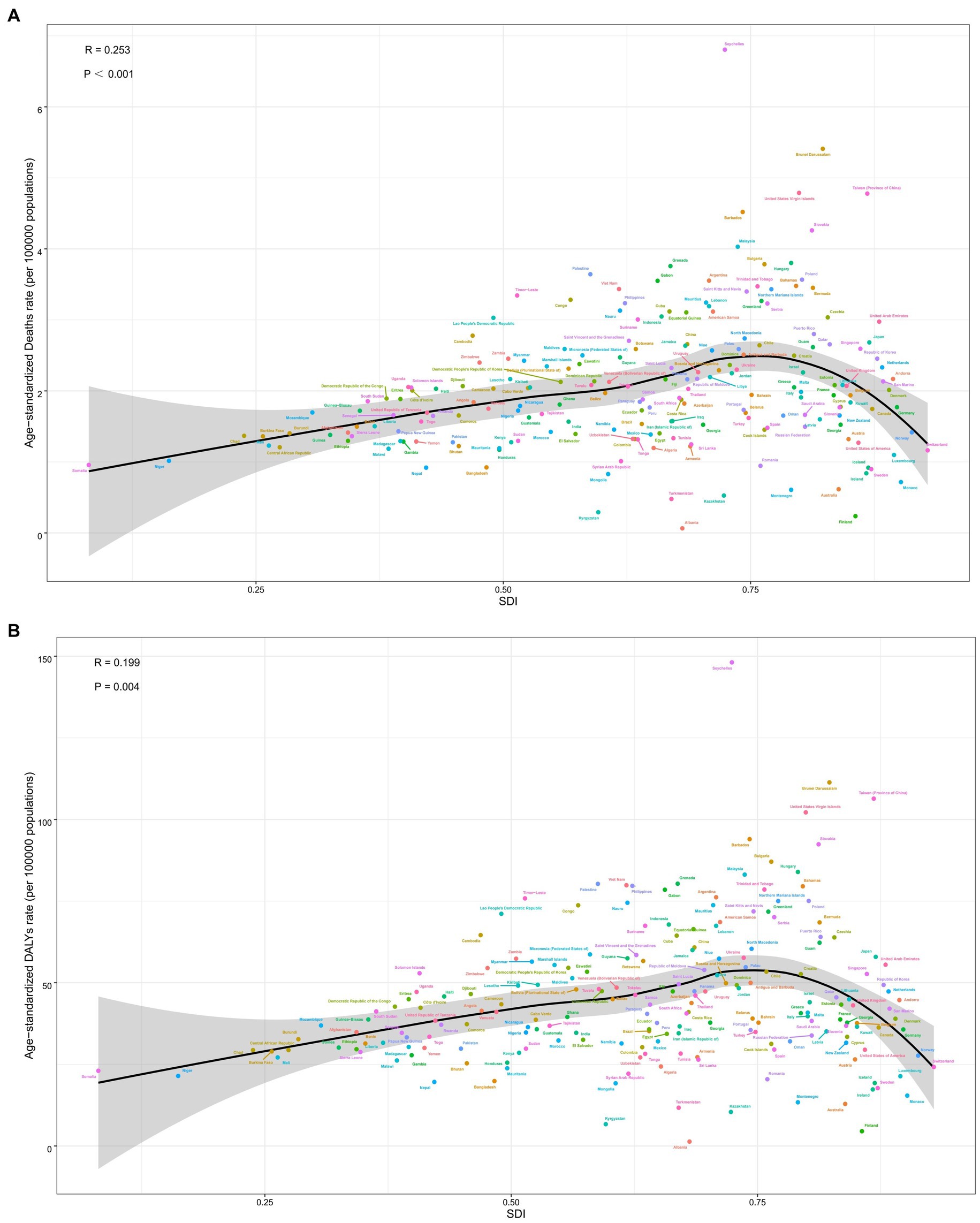
Figure 7. Correlation between diet low in milk attributable to colorectal cancer in ASMR (A), ASDR (B) and SDI globally in 204 nations. ASMR, age-standardized mortality rate; ASDR, age-standardized DALY rate; SDI, socio-demographic index.
A noteworthy negative correlation (R = −0.362, p < 0.001) was observed in 2019 between the EAPC in ASMR and HDI (Figure 8A). Similarly, an inverse relationship (R = −0.36, p < 0.001) occurred between the EAPC in ASDR and HDI in 2019 across various countries (Figure 8B). The same pattern occurred with the EAPC in ASMR and ASMR in 1990 (R = −0.27, p < 0.001) (Figure 8C), as well as the EAPC in ASDR and ASDR in 1990 (R = −0.229, p < 0.001) (Figure 8D).
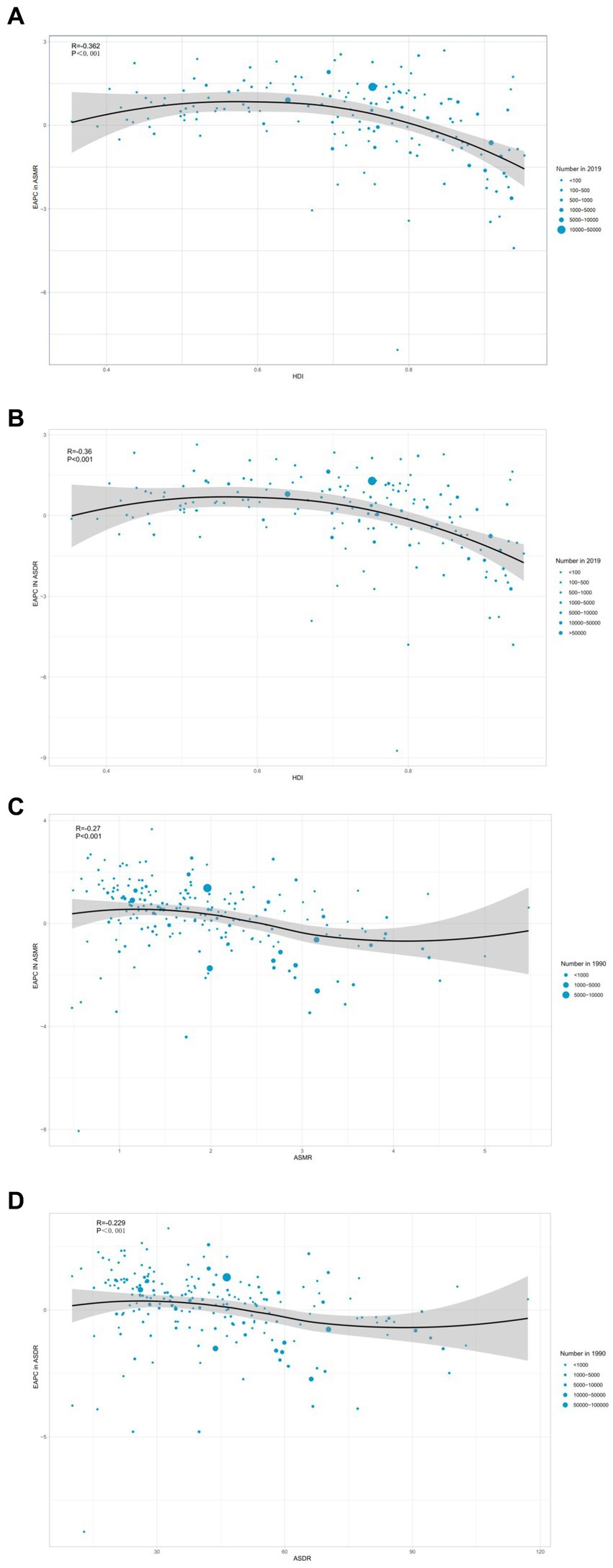
Figure 8. Correlation between EAPC in ASMR (A), ASDR (B) and HDI in 2019. Correlation between EAPC in ASMR and ASMR in 1990 (C). Correlation between EAPC in ASDR and ASDR in 1990 (D). EAPC, estimated annual percentage change; ASMR, age-standardized mortality rate; HDI, human development index; ASDR, age-standardized DALY rate.
4 Discussion
This analysis comprehensively summarized the global epidemiological trends of CRC attributable to diet low in milk. The findings showed that incidences of deaths and DALYs attributable to CRC were 15.3 and 18.6%, respectively. On a global scale, the number of CRC-related deaths and DALYs attributable to diet low in milk increased by 130.5 and 115.4% from 1990 to 2019, respectively. The spatial distribution of the burden of CRC varied significantly among different countries and regions. The ASMR and ASDR associated with CRC attributable to diet low in milk were more significant in high-middle SDI regions. East Asia, especially China, had the highest number of CRC-related deaths and DALYs attributable to diet low in milk. The burden of CRC was higher in males than females and the elderly than younger populations. These findings filled the gap in the global burden of CRC attributable to diet low in milk, help raise awareness of the importance of increasing milk intake, and provided evidence for policy makers to adapt appropriate dietary strategies to better manage CRC patients.
Diet low in milk is the leading risk factor for the burden of CRC worldwide. A prior study indicated that individuals who consumed ≥250 g of milk per day had a 15% lower risk of CRC as compared to those who consumed <70 g, and each increase of 500 g per day in milk intake reduced the risk of CRC by 12% (19). However, the mechanism underlying the reduced risk of CRC associated with increased milk consumption remains unclear. As a possible explanation, milk contains a large amount of calcium, which may be responsible for the reported inverse association between milk intake and CRC. Through colonic sequestration of secondary bile acids, including deoxycholic acid and phospholipids, calcium could provide protection against CRC (20, 21). Moreover, additional nutrients or bioactive substances found in milk, such as vitamin D, lactoferrin, and the short-chain fatty acid butyrate, might also act to prevent CRC (22, 23). Alarmingly, the number of individuals who consume an insufficient amount of milk has increased significantly (24). Globally, there was a substantial disparity between the current and optimal milk intake in 2017, with an average optimal consumption of 16% (25). The 2020–2025 Dietary Guidelines for Americans recommend 3 cup equivalent servings of skim or semiskim milk daily for all adults. However, adults aged ≥20 years consume only 1.5 cup-equivalents of dairy products daily (26). The major reasons for this are rapid economic development and changing dietary patterns, as milk consumption has decreased in favor of sweetened beverages and fruit juices. Sweetened beverages include regular sweetened carbonated soda, sports drinks, energy drinks, and non-pure fruit drinks. Sugar beverages and fruit juices often contain high levels of added sugars, which could potentially contribute to weight gain, inflammation, and metabolic dysregulation, all of which are implicated in CRC development (27). Due to the complexity of diet, these substitutes may confound or interact with the relationship between milk consumption and colorectal cancer risk. It is necessary to conduct further in-depth research on the complex interactions of dietary risks in the future. In addition, education and food security have also been associated with insufficient milk intake. So, education and awareness campaigns should be launched to encourage daily consumption of milk and other dairy products. Variable correlations may exist between the risk of CRC and the consumption of whole, skim, and semiskim milk and related fat components (28). The consumption of whole milk was positively linked with CRC mortality, while consumption of skim milk was negatively associated with CRC mortality, possibly due to fat-induced inhibition of other bioactive components in skim milk (29, 30). However, the GBD database did not further classify milk types, so the impact of different types of milk deficiency on the burden of CRC remains unclear.
This study investigated sex differences in the incidence of CRC attributable to diet low in milk. Since 1990, the increases in ASDR and ASMR were more pronounced in males than females with a notable difference in the contribution of diet low in milk to CRC (11.1% vs. 4.6%, respectively) (31). As a potential explanation for this finding, women are more likely to receive recommendations to increase milk intake than men because of the greater risk of osteoporosis (32, 33). Furthermore, women tend to be more concerned and consciousness of health status. Sex hormones have been recognized as a factor in sex differences in the incidence and mortality of CRC (34). Furthermore, risk behaviors, including drinking alcohol and smoking, are more common in men (35). Milk consumption decreases in the elderly due to various factors, such as decreased concern for personal health, higher rates of milk intolerance and digestion problems, changes in dietary preferences attributable to taste and palatability, and efforts to reduce fat intake (36). Therefore, initiatives are needed to increase awareness of milk intake to reduce sex-based disparities and decrease the incidence of preventable cancers.
There was an “S”-shaped correlation between ASMR or ASDR attributable to diet low in milk and SDI worldwide. The study revealed that diet low in milk remained common in Central sub-Saharan Africa, Southeast Asia, and South Asia. Conversely, milk intake has dramatically increased in North America, Central Asia, and Australasia, especially Australia (7). The primary factors contributing to these geographical disparities include behaviors related to lifestyle and diet, levels of socioeconomic development, and local medical conditions (37, 38). With the regional development, increased household income, and improvements in education, the consumption frequency and daily intake of milk have increased (39). For example, daily milk intake ranged from <200 g to >600 g in Western populations and from <42.4 g to >82.6 g in Asian populations (40). Notably, lactose intolerance is the major cause of milk restriction globally (41). The prevalence of lactose intolerance exhibits racial variation, from 64% in Asia to as low as 28% in Northern Europe (42). Even though it is difficult to encourage immediate change to dietary habits, education and propaganda campaigns are recommended to gradually increase daily milk intake.
China is the most populous nation globally and also has the highest number of CRC-related deaths and DALYs attributable to diet low in milk (43). Consumption of milk and dairy products continues to increase in China, but remains relatively low due to traditional dietary habits (44). A comprehensive prospective study reported that the average daily intake of milk and dairy products in China has increased from 2.06 g in 1989 to 26.47 g in 2011, which is still significantly lower than in European and North American countries (39). The recommended intake of milk and dairy products was revised in the latest version of the Chinese Dietary Guidelines for Residents (2022), from no less than 300 g per day to 300–500 g per day. Colonoscopy is considered the gold standard for CRC screening. However, due to a lack of a comprehensive national screening program and health resource restrictions, population-based screening of CRC has not yet been implemented in China (45).
As this study is a longitudinal observational study, although the modeling approach used estimates risk based on available dietary risk data but does not establish causation and should be regarded as approximations of risk (46). The GBD study had some deficiencies. Primarily, underdeveloped countries lack adequate cancer registries, thus estimates were based on predictive covariates or trends in neighboring countries, which likely biased the results. Second, the impact of different types of milk deficiencies on the burden of CRC remain unclear due to the lack of relevant data. Furthermore, the interrelationship between diets may have influenced the estimated burden of CRC attributable to diet low in milk. Although many of these dietary relative risks have been adjusted for the major confounders (e.g., age, sex), the possibility of residual confounding cannot be excluded.
5 Conclusion
This study comprehensively analyzed the association between the global burden of CRC and diet low in milk. The results indicated that the number of CRC-related deaths and DALYs due to diet low in milk continued to increase globally. There were significant differences in the burden of CRC linked to diet low in milk among countries and regions. Notably, high-middle SDI regions had the highest ASDR and ASMR of CRC attributable to diet low in milk. East Asia, especially China, had the highest number of CRC-related deaths and DALYs attributable to diet low in milk. In addition, diet low in milk has been associated with a greater burden of CRC in males and older individuals. These findings provided critical temporal and geographic data to assist policymakers to develop targeted dietary strategies for CRC patients, as well as raise public awareness regarding the necessity of increasing milk intake. Due to the interrelationships between diets and potential confounding factors that may affect the estimated burden of CRC attributed to diet low in milk, further research is needed in the future to understand the complexity of dietary alternatives.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Author contributions
XgZ: Writing – original draft, Writing – review & editing, Data curation, Methodology, Project administration, Supervision. XrZ: Data curation, Writing – original draft, Writing – review & editing. RL: Data curation, Writing – original draft, Writing – review & editing. ML: Data curation, Writing – original draft, Writing – review & editing. TO: Data curation, Writing – original draft, Writing – review & editing. HZ: Data curation, Writing – original draft, Writing – review & editing. ZC: Project administration, Writing – original draft, Writing – review & editing, Supervision. LZ: Project administration, Writing – original draft, Writing – review & editing, Supervision.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the President Foundation of Nanfang Hospital, Southern Medical University (Nos. 2023H002 and 2023H005) and the Guangdong Medical Research Foundation (No. A2024705).
Acknowledgments
Thanks to the Institute for Health Metrics and Evaluation and the Global Burden of Disease study collaborations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1431962/full#supplementary-material
SUPPLEMENTARY FIGURE S1 | Age composition ratio of colorectal cancer deaths and DALYs attributable to diet low in milk, 1990–2019.
SUPPLEMENTARY FIGURE S2 | Hierarchical cluster analysis based on national and regional temporal trends in the ASMR and ASDR.
SUPPLEMENTARY TABLE S1 | Top 10 countries or territories with the highest number of colorectal cancer deaths attributable to diet low in milk in 2019.
SUPPLEMENTARY TABLE S2 | Top 10 countries or territories with the highest number of colorectal cancer DALYs related to diet low in milk in 2019.
SUPPLEMENTARY TABLE S3 | Top 10 countries or territories with the highest colorectal cancer ASMR (per 100,000) attributable to diet low in milk in 2019.
SUPPLEMENTARY TABLE S4 | Top 10 countries or territories with the highest colorectal cancer ASDR (per 100,000) attributable to diet low in milk in 2019.
SUPPLEMENTARY TABLE S5 | Top 10 countries or territories with the highest or lowest EAPC in the ASMR (per 100,000) attributable to diet low in milk, 1990–2019.
SUPPLEMENTARY TABLE S6 | Top 10 countries or territories with the highest or lowest EAPC in the ASDR (per 100,000) attributable to diet low in milk, 1990–2019.
SUPPLEMENTARY TABLE S7 | Percentage change across countries of the fraction of all colorectal cancer deaths attributable to diet low in milk (95% CI).
SUPPLEMENTARY TABLE S8 | Percentage change across countries of the fraction of all colorectal cancer DALYs attributable to diet low in milk (95% CI).
Footnotes
References
1. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Aarts, MJ, Lemmens, VE, Louwman, MW, Kunst, AE, and Coebergh, JW. Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer. (2010) 46:2681–95. doi: 10.1016/j.ejca.2010.04.026
3. Morgan, E, Arnold, M, Gini, A, Lorenzoni, V, Cabasag, CJ, Laversanne, M, et al. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Gut. (2023) 72:338–44. doi: 10.1136/gutjnl-2022-327736
4. Hu, S, Li, Y, Zhu, W, Liu, J, and Wei, S. Global, region and national trends and age-period-cohort effects in colorectal cancer burden from 1990 to 2019, with predictions to 2039. Environ Sci Pollut Res Int. (2023) 30:83245–59. doi: 10.1007/s11356-023-28223-3
5. Keum, N, and Giovannucci, E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. (2019) 16:713–32. doi: 10.1038/s41575-019-0189-8
6. Awedew, AF, Asefa, Z, and Belay, WB. Burden and trend of colorectal cancer in 54 countries of Africa 2010–2019: a systematic examination for Global Burden of Disease. BMC Gastroenterol. (2022) 22:204. doi: 10.1186/s12876-022-02275-0
7. Deng, Y, Wei, B, Zhai, Z, Zheng, Y, Yao, J, Wang, S, et al. Dietary risk-related colorectal cancer burden: estimates from 1990 to 2019. Front Nutr. (2021) 8:690663. doi: 10.3389/fnut.2021.690663
8. Liu, Y, Zhang, C, Wang, Q, Wu, K, Sun, Z, Tang, Z, et al. Temporal trends in the disease burden of colorectal cancer with its risk factors at the global and national level from 1990 to 2019, and projections until 2044. Clin Epidemiol. (2023) 15:55–71. doi: 10.2147/CLEP.S388323
9. GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. (2022) 7:627–47. doi: 10.1016/s2468-1253(22)00044-9
10. Michaëlsson, K, Wolk, A, Langenskiöld, S, Basu, S, Warensjö Lemming, E, Melhus, H, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. (2014) 349:g6015. doi: 10.1136/bmj.g6015
11. Zhang, X, Chen, X, Xu, Y, Yang, J, Du, L, Li, K, et al. Milk consumption and multiple health outcomes: umbrella review of systematic reviews and meta-analyses in humans. Nutr Metab. (2021) 18:7. doi: 10.1186/s12986-020-00527-y
12. Barrubés, L, Babio, N, Becerra-Tomás, N, Rosique-Esteban, N, and Salas-Salvadó, J. Association between dairy product consumption and colorectal cancer risk in adults: a systematic review and meta-analysis of epidemiologic studies. Adv Nutr. (2019) 10:S190–s211. doi: 10.1093/advances/nmy114
13. Malcomson, FC, Wiggins, C, Parra-Soto, S, Ho, FK, Celis-Morales, C, Sharp, L, et al. Adherence to the 2018 World Cancer Research Fund/American Institute for Cancer Research Cancer Prevention Recommendations and cancer risk: a systematic review and meta-analysis. Cancer. (2023) 129:2655–70. doi: 10.1002/cncr.34842
14. Murray, CJL, Aravkin, AY, Zheng, P, Abbafati, C, Abbas, KM, Abbasi-Kangevari, M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
15. Wang, ZQ, Zhang, L, Guo, WB, Gao, Y, Li, XJ, Zhao, YF, et al. Burden of colorectal cancer attributable to diet low in milk in China, 1990–2017: findings from the global burden of disease study 2017. J Hum Nutr Diet. (2020) 34:233–42. doi: 10.1111/jhn.12836
16. GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. (2020) 5:17–30. doi: 10.1016/S2468-1253(19)30333-4
17. Kieling, C, Buchweitz, C, Caye, A, Silvani, J, Ameis, SH, Brunoni, AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the Global Burden of Disease Study. JAMA Psychiatry. (2024) 81:347–56. doi: 10.1001/jamapsychiatry.2023.5051
18. Wang, FX, Kong, XH, Guo, Z, Li, LX, and Zhang, S. Global, regional, and national burden of diet high in processed meat from 1990 to 2019: a systematic analysis from the Global Burden of Disease Study 2019. Front Nutr. (2024) 11:1354287. doi: 10.3389/fnut.2024.1354287
19. Pufulete, M. Intake of dairy products and risk of colorectal neoplasia. Nutr Res Rev. (2008) 21:56–67. doi: 10.1017/s0954422408035920
20. Aune, D, Lau, R, Chan, DSM, Vieira, R, Greenwood, DC, Kampman, E, et al. Dairy products and colorectal cancer risk: a systematic review and meta-analysis of cohort studies. Ann Oncol. (2012) 23:37–45. doi: 10.1093/annonc/mdr269
21. Kim, H, Hur, J, Wu, K, Song, M, Wang, M, Smith-Warner, SA, et al. Total calcium, dairy foods and risk of colorectal cancer: a prospective cohort study of younger US women. Int J Epidemiol. (2023) 52:87–95. doi: 10.1093/ije/dyac202
22. Song, M, Garrett, WS, and Chan, AT. Nutrients, foods, and colorectal cancer prevention. Gastroenterology. (2015) 148:1244–1260.e16. doi: 10.1053/j.gastro.2014.12.035
23. Cruz-Pierard, SM, Nestares, T, and Amaro-Gahete, FJ. Vitamin D and calcium as key potential factors related to colorectal cancer prevention and treatment: a systematic review. Nutrients. (2022) 14:4934. doi: 10.3390/nu14224934
24. Ricklefs-Johnson, K, and Pikosky, MA. Perspective: the benefits of including flavored Milk in healthy dietary patterns. Adv Nutr. (2023) 14:959–72. doi: 10.1016/j.advnut.2023.06.002
25. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
26. Hess, JM, Cifelli, CJ, and Fulgoni Iii, VL. Energy and nutrient intake of Americans according to meeting current dairy recommendations. Nutrients. (2020) 12:3006. doi: 10.3390/nu12103006
27. Liu, C, Zheng, S, Gao, H, Yuan, X, Zhang, Z, Xie, J, et al. Causal relationship of sugar-sweetened and sweet beverages with colorectal cancer: a Mendelian randomization study. Eur J Nutr. (2023) 62:379–83. doi: 10.1007/s00394-022-02993-x
28. Barrubés, L, Babio, NA-O, Mena-Sánchez, G, Toledo, E, Ramírez-Sabio, JB, Estruch, R, et al. Dairy product consumption and risk of colorectal cancer in an older Mediterranean population at high cardiovascular risk. Int J Cancer. (2018) 143:1356–66. doi: 10.1002/ijc.31540
29. Um, CA-O, Prizment, A, Hong, CP, Lazovich, D, and Bostick, RM. Associations of calcium and dairy product intakes with all-cause, all-cancer, colorectal cancer and CHD mortality among older women in the Iowa Women's Health Study. Br J Nutr. (2019) 121:1188–200. doi: 10.1017/S000711451900045X
30. Vargas, AJ, and Thompson, PA. Diet and nutrient factors in colorectal cancer risk. Nutr Clin Pract. (2012) 27:613–23. doi: 10.1177/0884533612454885
31. Liang, Y, Zhang, N, Wang, M, Liu, Y, Ma, L, Wang, Q, et al. Distributions and trends of the global burden of colorectal cancer attributable to dietary risk factors over the past 30 years. Nutrients. (2023) 16:132. doi: 10.3390/nu16010132
32. Zingone, F, Bucci, C, Iovino, P, and Ciacci, C. Consumption of milk and dairy products: facts and figures. Nutrition. (2017) 33:322–5. doi: 10.1016/j.nut.2016.07.019
33. Pellay, H, Marmonier, C, Samieri, C, and Feart, C. Socio-demographic characteristics, dietary, and nutritional intakes of French elderly community dwellers according to their dairy product consumption: data from the three-city cohort. Nutrients. (2020) 12:3418. doi: 10.3390/nu12113418
34. Hang, D, and Shen, H. Sex hormone and colorectal cancer: the knowns and unknowns. Cancer Epidemiol Biomarkers Prev. (2021) 30:1302–4. doi: 10.1158/1055-9965.EPI-21-0472
35. Dekker, E, Tanis, PJ, Vleugels, JLA, Kasi, PM, and Wallace, MB. Colorectal cancer. Lancet. (2019) 394:1467–80. doi: 10.1016/S0140-6736(19)32319-0
36. Ribeiro, IGM, Figueiredo, D, Lourenço, J, Paúl, C, and Costa, E. Dairy product intake in older adults across Europe based on the SHARE database. J Nutr Gerontol Geriatr. (2019) 38:297–306. doi: 10.1080/21551197.2019.1627972
37. Prentice, AM. Dairy products in global public health. Am J Clin Nutr. (2014) 99:1212S–6S. doi: 10.3945/ajcn.113.073437
38. Touvier, M, Méjean, C, Kesse-Guyot, E, Vergnaud, AC, Hercberg, S, and Castetbon, K. Sociodemographic and economic characteristics associated with dairy intake vary across genders. J Hum Nutr Diet. (2011) 24:74–85. doi: 10.1111/j.1365-277X.2010.01113.x
39. Xu, PP, Yang, TT, Xu, J, Li, L, Cao, W, Gan, Q, et al. Dairy consumption and associations with nutritional status of Chinese children and adolescents. Biomed Environ Sci. (2019) 32:393–405. doi: 10.3967/bes2019.054
40. Wang, XJ, Jiang, CQ, Zhang, WS, Zhu, F, Jin, YL, Woo, J, et al. Milk consumption and risk of mortality from all-cause, cardiovascular disease and cancer in older people. Clin Nutr. (2020) 39:3442–51. doi: 10.1016/j.clnu.2020.03.003
41. Bayless, TM, Brown, E, and Paige, DM. Lactase non-persistence and lactose intolerance. Curr Gastroenterol Rep. (2017) 19:23. doi: 10.1007/s11894-017-0558-9
42. Storhaug, CL, Fosse, SK, and Fadnes, LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. (2017) 2:738–46. doi: 10.1016/S2468-1253(17)30154-1
43. Sharma, RA-O, and Rakshit, B. Spatial and temporal patterns of colorectal cancer in Asia, 1990–2019. Int J Clin Oncol. (2023) 28:255–67. doi: 10.1007/s10147-022-02274-x
44. Dehghan, M, Mente, A, Rangarajan, S, Sheridan, P, Mohan, V, Iqbal, R, et al. Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study. Lancet. (2018) 392:2288–97. doi: 10.1016/S0140-6736(18)31812-9
45. Zhang, X, Yang, L, Liu, S, Li, H, Li, Q, Li, H, et al. Performance of different colorectal cancer screening strategies: a long-term passive follow-up population-based screening program in Beijing, China. BMC Public Health. (2023) 23:1640. doi: 10.1186/s12889-023-16564-0
Keywords: colorectal cancer, diet low in milk, Global Burden of Disease, disability-adjusted life year, GBD 2019
Citation: Zhang X, Zhang X, Li R, Lin M, Ou T, Zhou H, Chen Z and Zhen L (2024) Global, regional, and national analyses of the burden of colorectal cancer attributable to diet low in milk from 1990 to 2019: longitudinal observational study. Front. Nutr. 11:1431962. doi: 10.3389/fnut.2024.1431962
Edited by:
Lucilla Crudele, University of Bari Aldo Moro, ItalyReviewed by:
Leigh A. Frame, George Washington University, United StatesMohammad Ali Mohsenpour, Shiraz University of Medical Sciences, Iran
Copyright © 2024 Zhang, Zhang, Li, Lin, Ou, Zhou, Chen and Zhen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiming Chen, Y2hlbnpoaW1pbmdzbXVAMTYzLmNvbQ==; Li Zhen, emhlbmxpNTE2OEAxMjYuY29t
 Xingxing Zhang
Xingxing Zhang Xinru Zhang2
Xinru Zhang2 Meiyan Lin
Meiyan Lin Zhiming Chen
Zhiming Chen