
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr., 18 June 2024
Sec. Clinical Nutrition
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1423305
Background: Cumulative evidence has suggested that vitamin D deficiency is related with an increased susceptibility to various types of cancers. However, the association between vitamin D and thyroid cancer (TC) has remained to be unknown. Thus, there has been an urgent need for a meta-analysis to summarize existing evidence on vitamin D levels and the risk of TC.
Objective: This meta-analysis aimed to figure out the association between vitamin D level and the risk of TC.
Methods: A systematic search was performed for eligible articles on the association between vitamin D and TC based on PubMed, Embase, Web of Science, Cochrane, and ClinicalTrials.gov. Outcomes were the vitamin D level of cases with TC and the incidence of vitamin D deficiency in cases with TC comparing with the controls. The effect measures included standardized mean difference (SMD), ratio of means (RoM), and odds ratio (OR). A dose-response meta-analysis was performed to assess the correlation between vitamin D level and the risk of TC. Subgroup analyses and meta-regressions were conducted to explore the source of heterogeneity. And publication bias was evaluated through Begg's and Egger's tests.
Results: Results of the meta-analysis revealed lower levels of vitamin D in TC cases comparing with those in control [SMD = −0.25, 95% CI: (−0.38, −0.12); RoM = 0.87, 95% CI: (0.81, 0.94)] and the levels of 1,25 (OH)D in cases with TC were also lower than controls [SMD = −0.49, 95% CI: (−0.80, −0.19); RoM = 0.90, 95% CI: (0.85, 0.96)]. And vitamin D deficiency was associated with the increased risk of TC [OR = 1.49, 95% CI: (1.23, 1.80)]. Additionally, results from the dose-response meta-analysis showed that there is a 6% increase in the risk of TC for each 10 ng/ml decrease in 25 (OH)D levels [OR = 0.94; 95% CI: (0.89, 0.99)].
Conclusions: Individuals with TC had lower levels of vitamin D compared to controls, and vitamin D deficiency was correlated with an increase risk of TC.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=504417, identifier: CRD42024504417.
Thyroid cancer (TC) is the most common malignancy of the endocrine system, encompassing three overarching histological classifications: differentiated, medullary and anaplastic thyroid cancer (1, 2). Extensive research indicates a consistent upward trend in the worldwide prevalence of TC over the past few decades, while its mortality rates have remained relatively stable (3–9). The global age-standardized incidence rates of TC in 2020 were found to reached 3.1 per 100,000 person-years in males and 10.1 per 100,000 person-years in females. However, the mortality rates have remained to be 0.5 per 100,000 person-years worldwide over the past four decades (10, 11). GLOBOCAN 2020 database, compiled by the World Health Organization, has speculated that TC would become the second most prevalent cancer in women and the ninth in men by 2030, severely aggravate the burden of economic and health for society. (3). Thus, the prevention, diagnosis and management of TC have been an emerging problem (10, 12–16).
Vitamin D is a versatile steroid pro-hormone that is predominantly synthesized in the skin through the sunlight exposure and partly obtained from dietary sources (17). Both cutaneous and dietary vitamin D will be metabolized into 25-hydroxyvitamin D [25 (OH)D] in the liver and further converted into 1, 25-hydroxyvitamin D [1,25 (OH)D], the bio-active form of vitamin D, in the kidneys (18). The classical roles of 1,25 (OH)D include mediating calcium absorption in the intestine, regulating bone metabolism and so on (18). Recently, accumulating evidence has highlighted the potential anticancer action of vitamin D through its ability to hinder the proliferation, invasiveness and metastatic potential of malignant cells and promoting cell differentiation. In light of those mechanisms above, it is widely believed that the deficiency of vitamin D may be closely associated with an increased susceptibility to various types of cancers.
Also, the relationship between TC and vitamin D levels has been a topic of debate (19). Numerous clinical and experimental studies have suggested that individuals with TC tend to exhibit lower levels of vitamin D compared to both healthy individuals and those with benign thyroid nodules, while findings in some other studies have presented contrasting results (20–22). As a result, the association between vitamin D deficiency and the risk of TC has also remained inconclusive so far (23).
Given those aforementioned circumstances, there is an urgent need for a meta-analysis to summarize existing evidence quantitatively on vitamin D levels and the risk of TC. Although a few related meta-analyses have discussed the elevated risks of TC in individuals with vitamin D deficiency compared to those with sufficient vitamin D levels, whether these risks differ by the severity of the deficiency and how different forms of vitamin D are associated with TC still remained unclear (24, 25). Consequently, we performed this meta-analysis to address these uncertainties in more comprehensive precise manners.
A systematic search was conducted for relevant published articles from five databases (PubMed, Embase, Web of Science, Cochrane, and ClinicalTrials.gov) based on medical subjects heading terms, key words and word variants for “thyroid cancer,” “thyroid carcinoma,” “thyroid neoplasm,” “vitamin D,” “25-hydroxyvitamin D,” “25 (OH)D,” “25 OHD” and “cholecalciferol”. Additional published studies were retrieved by screening the references of the relevant original reports. A further search in preprint servers including Biorxiv and Medrxiv for preprint articles were conducted in order to identify eligible unpublished literature. All searches were performed on November 29th, 2023 and a more specific search strategy is shown in Table 1.
Inclusion criteria were as follows: (1) study type: prospective or retrospective observational designs including case-control studies, cohort studies and cross-sectional studies (2) population: patients diagnosed with thyroid cancer and health controls or cases with benign thyroid disease (3) study content: articles assessing the association between vitamin D and thyroid cancer which are published or unpublished (4) outcome: the levels of vitamin D in TC groups and control groups (healthy cases or those with benign thyroid diseases), the link between vitamin D deficiency and the risk of TC which was always expressed as odds ratios with 95% confidence intervals (CIs).
The exclusion criteria were defined as follows: (1) case reports, reviews, letters, conference records (2) studies conducted on animals (3) studies based on public databases or other non-original data.
Two investigators independently performed the three-step selection process consisting of title-screening, abstract-screening and full-text screening. Disagreement between investigators (Yue Hu and Shumeng Ren) were solved by consensus with a third person (Lishuo Dong).
The following characteristics were extracted from eligible studies: title, the name of the first author, year of publication, country where the study was conducted, study design, the type of thyroid cancer, the source of control, sample size of patients and controls, age, sex, body mass index, dietary habits, and tobacco use of participants, timing of vitamin D exposure measurement, methods of vitamin D measurement and the type of vitamin D measured. The following outcomes of studies were also extracted: levels of vitamin D in both TC cases and controls, adjusted odds ratios (OR) with 95% confidence intervals (CIs) for every category of vitamin D levels, the distribution of cases and controls in each category, variables adjusted for in the analysis, and the number of patients and controls with sufficient vitamin D levels, as well as the number of participants with vitamin D deficiency in each group. Data were extracted by two investigators independently using a standardized data extraction form, and any discrepancy was resolved by a cross-check.
The nine-star Newcastle-Ottawa quality assessment scales were used to assess the quality of case-control and cohort studies, while the scale of Agency for Healthcare Research and Quality (AHQR) were applied to cross-sectional studies. Two investigators (Yue Hu and Shumeng Ren) assessed the quality of studies independently, any discrepancy were resolved by consensus with a third person (Lishuo Dong).
The primary outcome was the level of vitamin D in patients with thyroid cancer, whose effect size was reported in terms of standardized mean difference (SMD) with 95% CIs, calculated from the mean value and standard deviation (SD). Methods by Luo et al., and Wan et al. were used to optimally estimate the mean and SD from the sample size, median, mid-range and mid-quartile range when only five-number summary was provided by included articles (26, 27). And a subgroup analysis were conducted based on the methods of vitamin D measurement, the timing of measurement, the countries, the sample source of vitamin D and the source of controls. Meta-regressions were performed on the basis of the methods of vitamin D measurement, the timing of measurement, the countries, the sample source of vitamin D, the source of controls, the publication year, the sex ratio of participants and the age of participants. To provide clinicians with more intuitive clinical interpretation of the differences of vitamin D levels between case group and control group, the ratio of means (RoM) with 95% CIs, defined by the mean value in the case group divided by the mean value in the control group, was also introduced as another effect size. The second outcome was the incidence of vitamin D deficiency in patients with TC presented by odds ratio (OR) with 95% CIs. Random effects models were used to ensure the robustness of these results. A subgroup analysis and a meta-regression were conducted based on the timing of measurement and the source of the controls.
A dose-response meta-analysis for a deeper explanation of correlation between the vitamin D level and the risk of TC was also conducted. Firstly, we tested the potential non-linearity in the correlation between vitamin D level and the risk of TC through a fixed-effect restricted cubic spline model with four knots at the percentiles of 5, 35, 65, and 95% of the distribution. Then we estimated the linear trend from the correlated ORs and 95% CIs across categories of vitamin D using generalized least squares regression.
Heterogeneity was estimated using I2 statistics indicating the percentage of heterogeneity that is beyond chance (low heterogeneity: I2 < 25%; moderate heterogeneity: I2 = 25–50%; strong heterogeneity: I2 > 50%). Sensitivity analysis was conducted to evaluated the stability of the results. Finally, we assessed the publication bias through Beggs test and Eggers test.
Results were considered statistically significant when p-value was < 0.05, and all statistic analysis were conducted using STATA 14.0 software.
Two thousand one hundred thirty-two articles were yielded through databases searching. After the removal of reduplicates, 2,082 articles remained for the screening of titles. The abstracts of 135 articles were assessed, and finally 28 articles went through full-text screening. Eventually, 21 eligible published articles were included according to the inclusion and exclusion criteria. A flow diagram of study selection is presented in Figure 1.
The included articles were published from 1982 to 2020 and involved 2,434 patients and 7,398 controls, with six of them conducted in China, three from Iran, two from Turkey, and others from Brazil, the United States, Poland, German, Korea, Canada, Romania, Thailand, Japan and Denmark. Sixteen Studies reported the level of vitamin D in cases and controls, 9 reported the OR and 95% CIs, and three reported the dose-response data of vitamin D level and the risk of thyroid cancer. Among all eligible studies, 16 of them were case-control studies, four were cross-sectional studies and one was cohort study. The main characteristics of included studies are shown in Table 2.
All case-control studies got no < 6 stars and the cohort study got full stars. The results suggested a relatively high quality (Tables 3, 4).
Twelve studies had evaluated the blood levels of 25 (OH)D in patients with thyroid cancer and controls. The pooled standardized mean difference between the 25 (OH)D levels in TC patients and the controls was −0.25 (95% CI: −0.38, −0.12; P < 0.05) with a moderate heterogeneity (I2 = 46.0%, P < 0.05), which indicated that the blood levels of 25 (OH)D in TC patients were significantly lower than those in the control group (Figure 2). To explore the source of heterogeneity, several subgroup analyses were conducted. Table 5 show the results of subgroup analyses based on the testing method of 25 (OH)D, the timing of measurement of 25 (OH)D, the sample source, the countries where the included studies were conducted and the source of controls. The outcomes suggested that the results of this meta-analysis were significant regardless of these factors. Moreover, the heterogeneity of the subgroups using health individuals and individuals with benign thyroid diseases as control groups were 0.0% (P = 0.448) and 21.5% (P = 0.272), respectively, indicating that the source of controls was a prominent cause of heterogeneity. The results of the meta-regression for each covariate are presented in Table 6, demonstrating that the source of controls (P = 0.02) and the age of participants (P = 0.009) were the source of the heterogeneity. The results of sensitivity analysis showed that the removal of any single trial did not affect the significance of the outcome (Figure 3). The funnel plot is shown in Figure 4, and the Eggers' and Beggs' tests did not reveal any significant publication bias (P = 0.205, P = 0.451). And the pooled RoM for level of 25 (OH)D was 0.87 (95% CI: 0.81,0.94; P < 0.05; I2 = 74.7%), which indicated that the 25 (OH)D level in TC cases was 13% lower than that in controls (Figure 5).
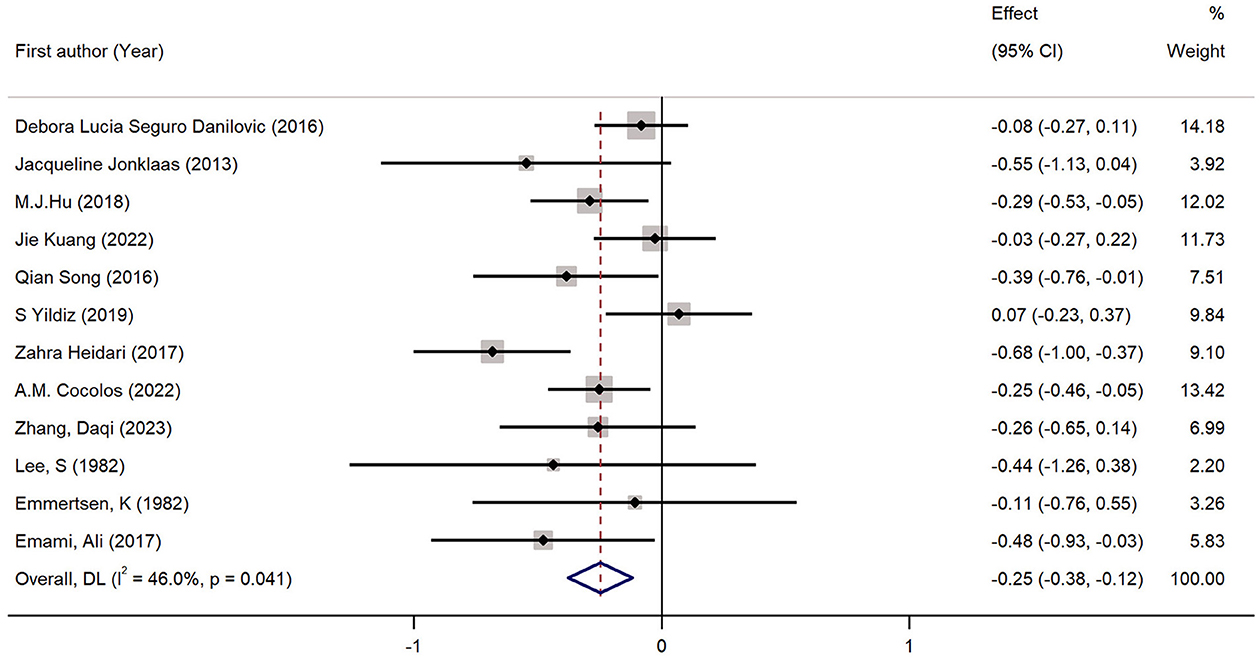
Figure 2. Forest plots and pooled estimates of the effect for the meta-analysis of the standardized mean difference between the 25 (OH)D levels in the patients with thyroid cancer and the controls.
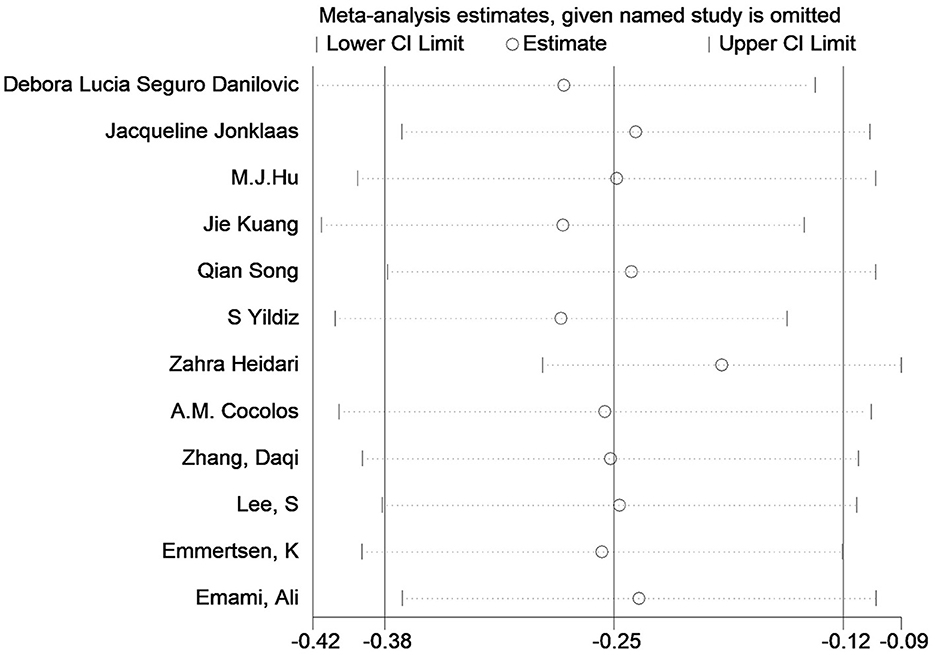
Figure 3. Sensitivity analysis of the standardized mean difference between the 25 (OH)D levels in the patients with thyroid cancer and the controls.
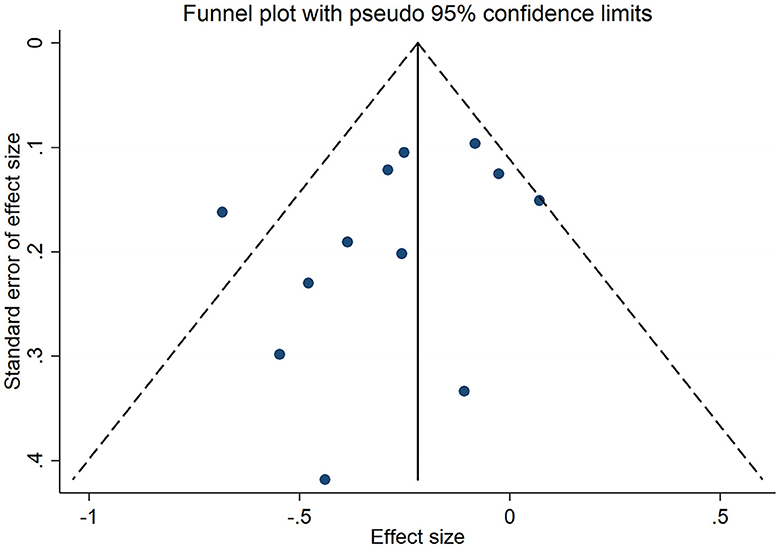
Figure 4. Funnel plot of the studies included in the meta-analysis of the standardized mean difference between the 25 (OH)D levels in the patients with thyroid cancer and the controls.
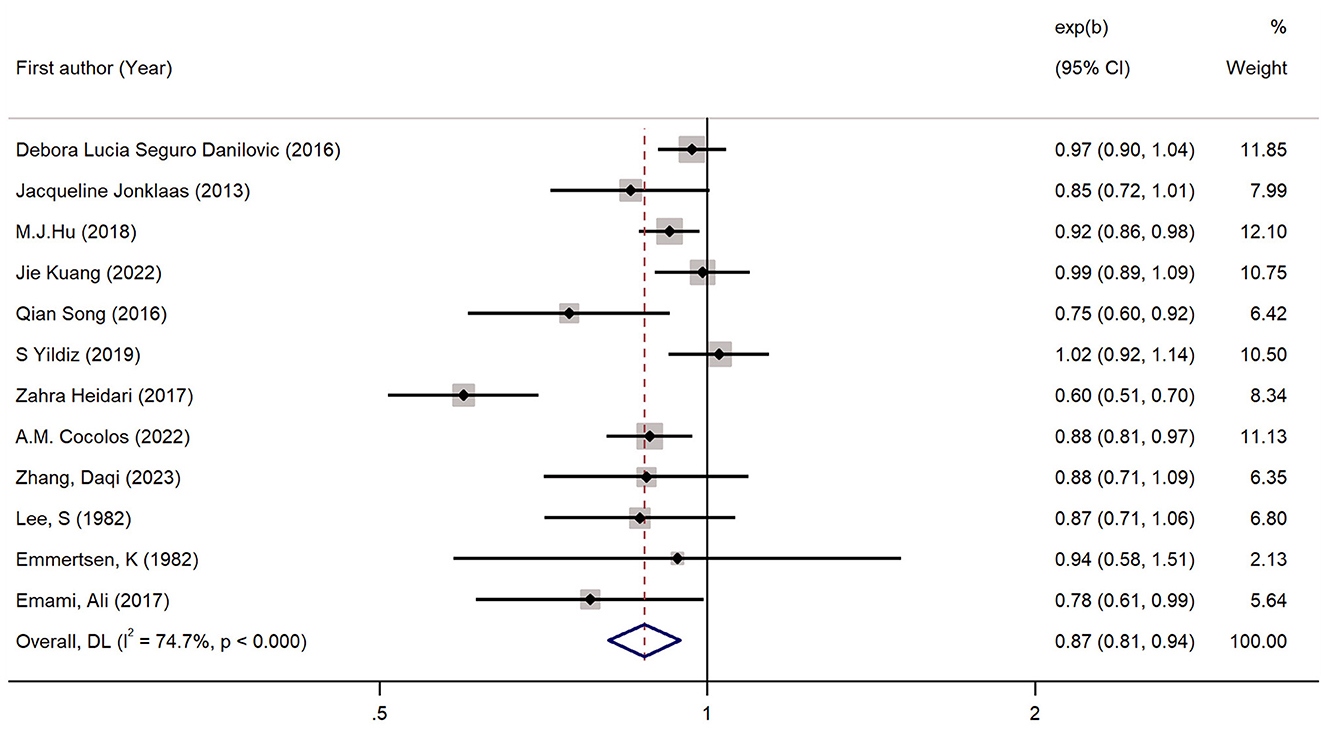
Figure 5. Forest plots and pooled estimates of the effect for the meta-analysis of the ratio of means between the 25 (OH)D levels in the patients with thyroid cancer and the controls.
Four studies had reported the blood levels of 1,25 (OH)D in cases with TC and controls. As shown in Figure 6, the pooled standardized mean difference was −0.49 (95% CI: −0.80, −0.19; P < 0.05) with a heterogeneity of 37.3% (P = 0.188). The pooled RoM was 0.90 (95% CI: 0.85, 0.96; P < 0.05; I2 = 79.0%), demonstrating that the 1,25 (OH)D level in TC cases were 10% lower than in controls (Figure 7).
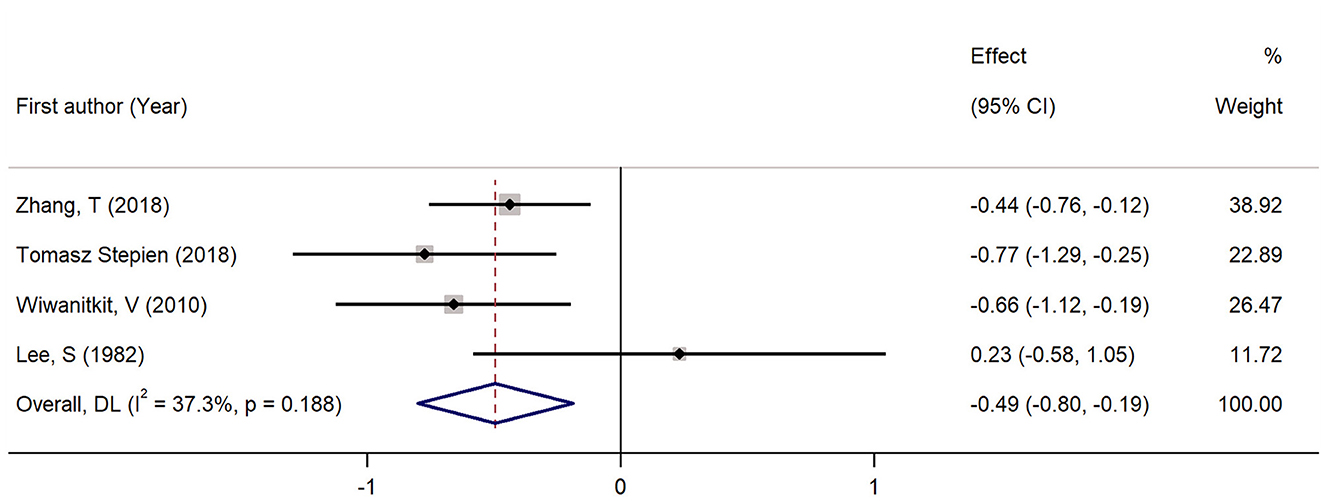
Figure 6. Forest plots and pooled estimates of the effect for the meta-analysis of the standardized mean difference between the 1, 25 (OH)D levels in the patients with thyroid cancer and the controls.
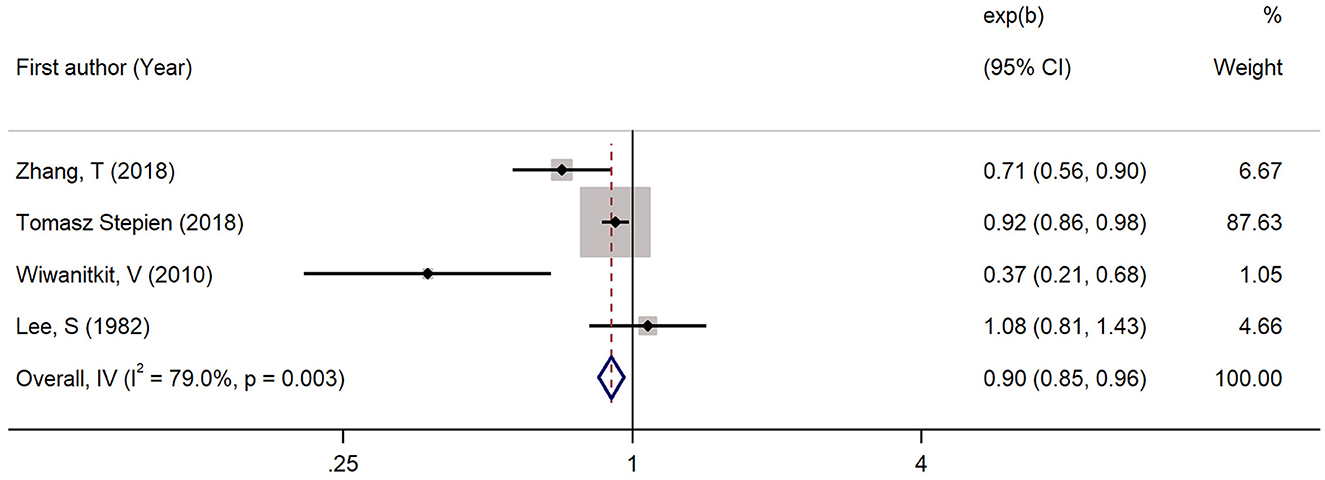
Figure 7. Forest plots and pooled estimates of the effect for the meta-analysis of the ratio of means between the 1, 25 (OH)D levels in the patients with thyroid cancer and the controls.
This meta-analysis included nine studies, demonstrating that vitamin D deficiency was associated with a higher risk of TC (pooled OR: 1.49, 95% CI: 1.23, 1.80; P < 0.05) (Figure 8). And the heterogeneity was not significant (I2 = 21.6%, P = 0.251). Subgroup analyses demonstrated that the result of the meta-analysis was significant regardless of whether the source of controls were healthy individuals or patients with benign thyroid disease (Table 7). However, the subgroup whose vitamin D levels were measured before the diagnosis of TC showed an insignificant results, which might be due to the limited number of trials included in the subgroup (Table 7). The results of meta regression are shown in Table 8, and the sensitivity analysis confirmed the stability of this meta-analysis (Figure 9). The publication bias was not significant according to the results of Eggers and Beggs tests (P = 0.394, P = 0.917).
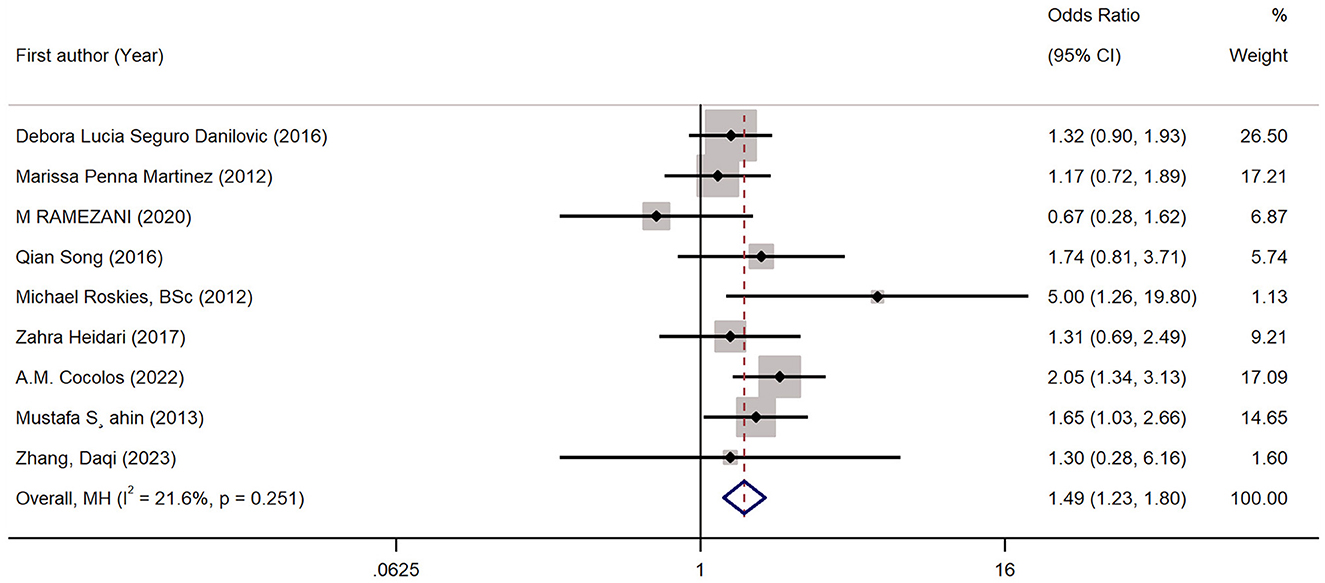
Figure 8. Forest plots and pooled estimates of the effect for the meta-analysis of the association between vitamin D deficiency and the risk of thyroid cancer.
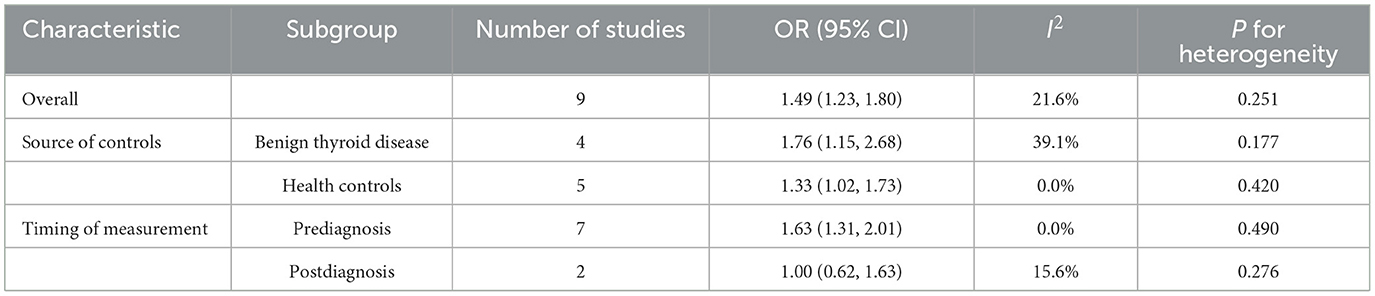
Table 7. Results of subgroup analysis for the association between vitamin D deficiency and the risk of thyroid cancer.
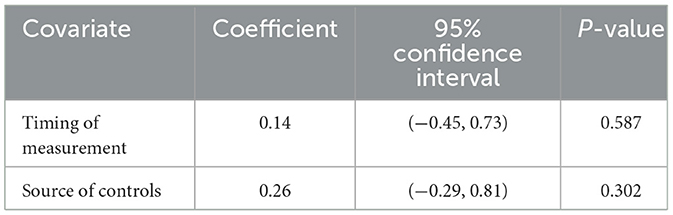
Table 8. Results of the meta-regression for the association between vitamin D deficiency and the risk of thyroid cancer.
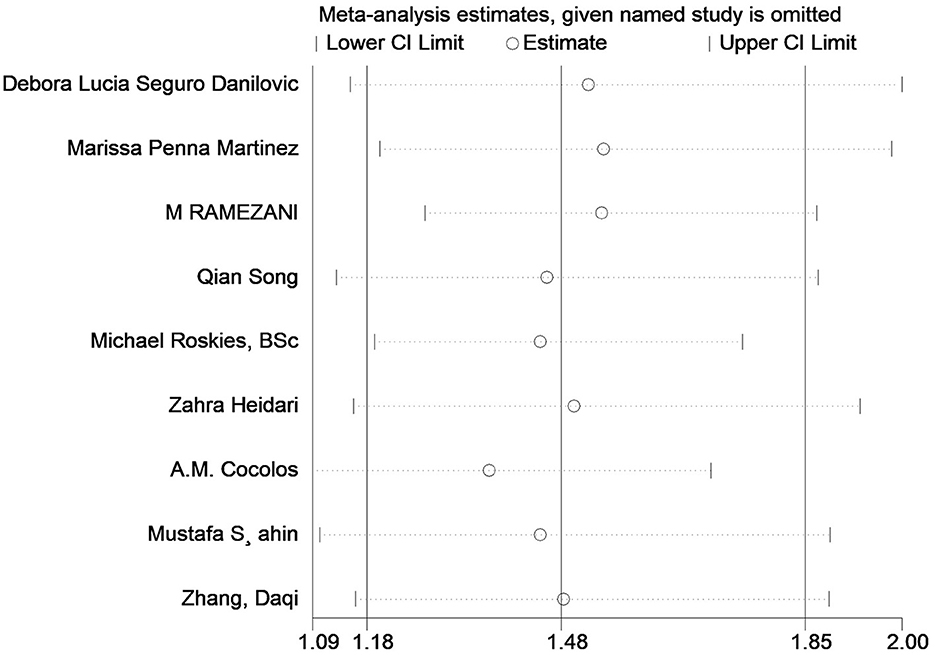
Figure 9. Sensitivity analysis of the association between vitamin D deficiency and the risk of thyroid cancer.
Finally, we evaluated the dose-response relationship between the level of blood 25 (OH)D and the risk of TC. As shown in Figure 10, a significant linear correlation between blood 25 (OH)D level and the risk of TC. For each 10 ng/ml decrease in 25 (OH)D levels, there is a 6% increase in the risk of TC (OR: 0.94; 95% CI: 0.89, 0.99).
In the past few years, vitamin D has attracted clinical interest for its association with cancers. Several observational studies have demonstrated a correlation between vitamin D deficiency and the occurrence and fatality of various types of cancer (28–35). Additionally, laboratory investigations have provided substantial evidence supporting the anticancer properties of vitamin D through vitamin D receptor binding or indirect interaction with transcriptional regulators and cell signally systems (36–38). Specifically, vitamin D has demonstrated the ability to impede the expression of proto-oncogene c-MYC, while concurrently promoting the accumulation of p27. Consequently, this regulation of the cell cycle ultimately leads to the inhibition of cellular proliferation (39–41). Furthermore, vitamin D has been observed to enhance the expression of fibronectin via the PTEN/PI3 kinase pathway, as well as reverse the cadherin switch. As a result, this leads to a reduction in the invasion and metastasis of cancer cells (42, 43). In addition, the potential of vitamin D to improve the inflammatory micro-environment in TC by inhibiting the proliferation of Th1 and Th17 as well as the expression of cytokines such as IL-1, IL-17 and IL-21 has been reported (44, 45). Although preclinical trials have revealed the potential anticancer effect of vitamin D and that vitamin D receptor polymorphisms are likely to be closely correlated with the risk of TC, data from human remain to be inconsistent (6). A number of studies have suggested that vitamin D level is unreliable as a risk and prognostic factor for TC, while others have linked vitamin D status to the risk of TC (46–49). Thus, a meta-analysis is necessary to comprehensively analyze existing clinical evidence and draw a conclusion. Despite 2 relative meta-analyses published, new clinical evidence has been published in the last few years (24, 25). Thus, we updated the included literature and performed a completely new meta-analysis. Our analysis reported the difference between the levels of 1,25 (OH)D in TC cases and controls for the first time. Additionally, we introduced RoM, a new effect size, to determine the difference between vitamin levels in TC cases and the controls, so that the disparity in vitamin D levels between groups can be easily demonstrated in percentage terms, which was easier to clinically interpret compared to SMD, a classical effect size of meta-analysis for continuous data. (50). As far as we know, our study was the first to conduct a dose-response meta-analysis to reveal the relationship between the status of vitamin D and the risk of TC.
Based on 21 trials involving 2,434 patients with TC and 7,398 controls, our meta-analysis indicated that the blood level of 25 (OH)D in TC cases was significantly lower than that in healthy individuals or those with benign thyroid diseases. This outcome did not differ by the testing methods of 25 (OH)D, countries where the studies conducted, the timing of 25 (OH)D measurement, the source of samples, and the source of the controls, which was consistent with the results of the previous meta-analysis. Subgroup analysis and meta regression indicated that the source of controls were the major source of the heterogeneity, which was noteworthy. Actually, we found a few articles regarding relatively low vitamin D status in patients with benign thyroid disease such as thyroid nodules (51, 52). Regrettably, studies on the mechanism linking vitamin D and thyroid disease are still primarily focused on autoimmune thyroiditis and thyroid cancer, with other benign thyroid diseases receiving inadequate attention. Thus, more experimental evidence is urgently needed to clarify the mechanism lying behind the results of our subgroup analysis. Nevertheless, we still found the level of 25 (OH)D in TC cases significant lower than cases with benign thyroid disease, which make the level of 25 (OH)D still a potential and valuable risk factor for TC. Moreover, according to the results of meta-regression, the age of participants was another source of the heterogeneity, which was not surprising since cumulative studies had reported the effect of age on serum vitamin D level and on the capacity of human skin to produce vitamin D (53, 54).
We first reported that the level of 25 (OH)D in cases with TC was likely to be 13% lower than in controls. And our study was the first meta-analysis reporting the level of 1, 25 (OH)D, the hormonally active form of vitamin D, in TC cases. As shown in our article, the blood level of 1,25 (OH)D was relatively low and might be 10% lower than that in controls, which was not mentioned in any previous meta-analysis. The outcome of our meta-analysis had also demonstrated that vitamin D deficiency might potentially increase the risk of TC by 49%. This association was significant in subgroups of both healthy controls and benign thyroid disease. Although it was not significant in the subgroup whose vitamin D levels were measured before the diagnosis of TC, we considered the reliability of this result to be limited. Because only two trials were included in this subgroup which could lead to a false negative outcome from a statistic standpoint. Finally, our study firstly conducted a dose-response meta-analysis between the level of vitamin D and the risk of TC. Our results showed an inverse linear association between 25 (OH)D level and the TC risk and 10 ng/ml of increase in 25 (OH)D level was correlated with 6% lower risk of TC.
Several limitations of this meta-analysis warrant attention. First, the majority of the included studies were case-control studies, thereby posing challenges in establishing a definitive causal relationship between vitamin D levels and the risk of TC. Therefore, more prospective cohort studies on a larger scale were expected to improve the reliability of our analysis. Secondly, the standards of vitamin D deficiency were inconsistent, which was likely to influence the results of meta-analysis adopting OR as the effect size. Third, several studies included cases with multiple pathological TC types and lacked the necessary data of cases with each kind of TC, which created a barrier to performing a subgroup analysis based on types of TC. Forth, we failed to explore the impact of multiple factors including body-mass index, dietary habits and smoking on the results of the meta-analyses due to the absence of data. Thus, more articles published with complete data would be needed in the future to address these issues.
The findings of our study indicate that individuals with TC have lower blood levels of 25 (OH)D and 1,25 (OH)D compared to controls. Additionally, an inverse linear correlation between 25 (OH)D level and the risk of TC is existed. Thus, although numerous negative results have been published, we still propose vitamin D deficiency as a potential risk factor for TC. Furthermore, robust clinical and preclinical evidence is needed for a large, well-executed and more inclusive systematic review with meta-analysis on this topic.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
YH: Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. CX: Conceptualization, Supervision, Validation, Writing – original draft, Writing – review & editing. SR: Data curation, Methodology, Writing – review & editing. LD: Data curation, Methodology, Writing – review & editing. JG: Data curation, Software, Writing – review & editing. XL: Data curation, Investigation, Software, Supervision, Writing – original draft, Writing – review & editing.
The author (s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (grant numbers ZYYCXTD-D-202001), Scientific and Technological innovation project of China Academy of Chinese Medical Sciences (grant numbers CI2021A01602), and Special Project for the Construction of Clinical Medical Research Centre of Guang'anmen Hospital, China Academy of Traditional Chinese Medicine (grant numbers 2022LYJSZX08).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Filetti S, Durante C, Hartl D, Leboulleux S, Locati LD, Newbold K, et al. Thyroid cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up†. Ann Oncol. (2019) 30:1856–83. doi: 10.1093/annonc/mdz400
2. Raue F, Frank-Raue K. Thyroid cancer: risk-stratified management and individualized therapy. Clin Cancer Res. (2016) 22:5012–21. doi: 10.1158/1078-0432.CCR-16-0484
3. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
4. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA. (2017) 317:1338–48. doi: 10.1001/jama.2017.2719
5. Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol. (2016) 12:646–53. doi: 10.1038/nrendo.2016.110
6. Penna-Martinez M, Ramos-Lopez E, Stern J, Hinsch N, Hansmann ML, Selkinski I, et al. Vitamin d receptor polymorphisms in differentiated thyroid carcinoma. Thyroid. (2009) 19:623–28. doi: 10.1089/thy.2008.0388
7. Pizzato M, Li M, Vignat J, Laversanne M, Singh D, La Vecchia C, et al. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. (2022) 10:264–72. doi: 10.1016/S2213-8587(22)00035-3
8. Li M, Dal Maso L, Vaccarella S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. (2020) 8:468–70. doi: 10.1016/S2213-8587(20)30115-7
9. Miranda-Filho A, Lortet-Tieulent J, Bray F, Cao B, Franceschi S, Vaccarella S, et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. (2021) 9:225–34. doi: 10.1016/S2213-8587(21)00027-9
10. Chen DW, Lang B, McLeod D, Newbold K, Haymart MR. Thyroid cancer. Lancet. (2023) 401:1531–44. doi: 10.1016/S0140-6736(23)00020-X
11. Chen J, Wang C, Shao B. Global, regional, and national thyroid cancer age-period-cohort modeling and BAYESIAN predictive modeling studies: a systematic analysis of the Global Burden of Disease Study 2019. Heliyon. (2023) 9:e22490. doi: 10.1016/j.heliyon.2023.e22490
12. Laha D, Nilubol N, Boufraqech M. New therapies for advanced thyroid cancer. Front Endocrinol. (2020) 11:82. doi: 10.3389/fendo.2020.00082
13. Alexander EK, Cibas ES. Diagnosis of thyroid nodules. Lancet Diabetes Endocrinol. (2022) 10:533–39. doi: 10.1016/S2213-8587(22)00101-2
14. Xing M. Molecular pathogenesis and mechanisms of thyroid cancer. Nat Rev Cancer. (2013) 13:184–99. doi: 10.1038/nrc3431
15. Nikiforov YE, Nikiforova MN. Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol. (2011) 7:569–80. doi: 10.1038/nrendo.2011.142
16. Schlumberger M, Leboulleux S. Current practice in patients with differentiated thyroid cancer. Nat Rev Endocrinol. (2021) 17:176–88. doi: 10.1038/s41574-020-00448-z
17. Gallagher JC, Rosen CJ. Vitamin D: 100 years of discoveries, yet controversy continues. Lancet Diabetes Endocrinol. (2023) 11:362–74. doi: 10.1016/S2213-8587(23)00060-8
18. Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G. Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev. (2016) 96:365–408. doi: 10.1152/physrev.00014.2015
19. Palanca A, Ampudia-Blasco FJ, Real JT. The controversial role of vitamin D in thyroid cancer prevention. Nutrients. (2022) 14:2593. doi: 10.3390/nu14132593
20. Bains A, Mur T, Wallace N, Noordzij JP. The role of vitamin D as a prognostic marker in papillary thyroid cancer. Cancers. (2021) 13:143516. doi: 10.3390/cancers13143516
21. Hu MJ, Niu QS, Wu HB, Lu XL, Wang L, Tong XR, et al. Association of thyroid cancer risk with plasma 25-hydroxyvitamin D and vitamin D binding protein: a case-control study in china. J Endocrinol Invest. (2020) 43:799–808. doi: 10.1007/s40618-019-01167-7
22. Jonklaas J, Danielsen M, Wang H. A pilot study of serum selenium, vitamin D, and thyrotropin concentrations in patients with thyroid cancer. Thyroid. (2013) 23:1079–86. doi: 10.1089/thy.2012.0548
23. Barrea L, Gallo M, Ruggeri RM, Giacinto PD, Sesti F, Prinzi N, et al. Nutritional status and follicular-derived thyroid cancer: an update. Crit Rev Food Sci Nutr. (2021) 61:25–59. doi: 10.1080/10408398.2020.1714542
24. Hu MJ, Zhang Q, Liang L, Wang SY, Zheng XC, Zhou MM, et al. Association between vitamin d deficiency and risk of thyroid cancer: a case-control study and a meta-analysis. J Endocrinol Invest. (2018) 41:1199–210. doi: 10.1007/s40618-018-0853-9
25. Zhao J, Wang H, Zhang Z, Zhou X, Yao J, Zhang R, et al. Vitamin D deficiency as a risk factor for thyroid cancer: a meta-analysis of case-control studies. Nutrition. (2019) 57:5–11. doi: 10.1016/j.nut.2018.04.015
26. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. Bmc Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
27. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
28. Kim Y, Chang Y, Cho Y, Chang J, Kim K, Park DI, et al. Serum 25-hydroxyvitamin d levels and risk of colorectal cancer: an age-stratified analysis. Gastroenterology. (2023) 165:920–31. doi: 10.1053/j.gastro.2023.06.029
29. Lawler T, Warren AS. Serum 25-hydroxyvitamin D and cancer risk: a systematic review of Mendelian randomization studies. Nutrients. (2023) 15:422. doi: 10.3390/nu15020422
30. Wang QL, Ma C, Yuan C, Shi Q, Wolpin BM, Zhang Y, et al. Plasma 25-hydroxyvitamin d levels and survival in stage III colon cancer: findings from CALGB/SWOG 80702 (alliance). Clin Cancer Res. (2023) 29:2621–30. doi: 10.1158/1078-0432.CCR-23-0447
31. Virtanen JK, Nurmi T, Aro A, Bertone-Johnson ER, Hyppönen E, Kröger H, et al. Vitamin D supplementation and prevention of cardiovascular disease and cancer in the finnish vitamin D trial: a randomized controlled trial. Am J Clin Nutr. (2022) 115:1300–10. doi: 10.1093/ajcn/nqab419
32. Trummer O, Langsenlehner U, Krenn-Pilko S, Pieber TR, Obermayer-Pietsch B, Gerger A, et al. Vitamin D and prostate cancer prognosis: a Mendelian Randomization Study. World J Urol. (2016) 34:607–11. doi: 10.1007/s00345-015-1646-9
33. Limonte CP, Zelnick LR, Hoofnagle AN, Thadhani R, Melamed ML, Mora S, et al. Effects of vitamin D(3) supplementation on cardiovascular and cancer outcomes by EGFR in vital. Kidney360. (2022) 3:2095–105. doi: 10.34067/KID.0006472022
34. Chandler PD, Buring JE, Manson JE, Giovannucci EL, Moorthy MV, Zhang S, et al. Circulating vitamin D levels and risk of colorectal cancer in women. Cancer Prev Res. (2015) 8:675–82. doi: 10.1158/1940-6207.CAPR-14-0470
35. Feldman D, Krishnan AV, Swami S, Giovannucci E, Feldman BJ. The role of vitamin D in reducing cancer risk and progression. Nat Rev Cancer. (2014) 14:342–57. doi: 10.1038/nrc3691
36. Manson JE, Bassuk SS, Buring JE. Vitamin D, calcium, and cancer: approaching daylight? JAMA. (2017) 317:1217–18. doi: 10.1001/jama.2017.2155
37. Rozmus D, Ciesielska A, Płomiński J, Grzybowski R, Fiedorowicz E, Kordulewska N, et al. Vitamin D binding protein (VDBP) and its gene polymorphisms-the risk of malignant tumors and other diseases. Int J Mol Sci. (2020) 21:217822. doi: 10.3390/ijms21217822
38. Roehlen N, Doering C, Hansmann ML, Gruenwald F, Vorlaender C, Bechstein WO, et al. Vitamin D, FOXO3A, and Sirtuin1 in Hashimoto's thyroiditis and differentiated thyroid cancer. Front Endocrinol. (2018) 9:527. doi: 10.3389/fendo.2018.00527
39. Kim D. The role of vitamin D in thyroid diseases. Int J Mol Sci. (2017) 18:91949. doi: 10.3390/ijms18091949
40. Salehi-Tabar R, Nguyen-Yamamoto L, Tavera-Mendoza LE, Quail T, Dimitrov V, An BS, et al. Vitamin D receptor as a master regulator of the c-MYC/MXD1 network. Proc Natl Acad Sci USA. (2012) 109:18827–32. doi: 10.1073/pnas.1210037109
41. Chiang KC, Kuo SF, Chen CH, Ng S, Lin SF, Yeh CN, et al. MART-10, the vitamin d analog, is a potent drug to inhibit anaplastic thyroid cancer cell metastatic potential. Cancer Lett. (2015) 369:76–85. doi: 10.1016/j.canlet.2015.07.024
42. Liu W, Asa SL, Fantus IG, Walfish PG, Ezzat S. Vitamin d arrests thyroid carcinoma cell growth and induces p27 dephosphorylation and accumulation through PTEN/Akt-dependent and -independent pathways. Am J Pathol. (2002) 160:511–19. doi: 10.1016/S0002-9440(10)64870-5
43. Liu W, Asa SL, Ezzat S. 1alpha,25-Dihydroxyvitamin D3 targets pten-dependent fibronectin expression to restore thyroid cancer cell adhesiveness. Mol Endocrinol. (2005) 19:2349–57. doi: 10.1210/me.2005-0117
44. Mele C, Caputo M, Bisceglia A, Samà MT, Zavattaro M, Aimaretti G, et al. Immunomodulatory effects of vitamin D in thyroid diseases. Nutrients. (2020) 12:1444. doi: 10.3390/nu12051444
45. Xi C, Zhang GQ, Sun ZK, Song HJ, Shen CT, Chen XY, et al. Interleukins in thyroid cancer: from basic researches to applications in clinical practice. Front Immunol. (2020) 11:1124. doi: 10.3389/fimmu.2020.01124
46. Kuang J, Jin Z, Chen L, Zhao Q, Huang H, Liu Z, et al. Serum 25-hydroxyvitamin D level is unreliable as a risk factor and prognostic marker in papillary thyroid cancer. Ann Transl Med. (2022) 10:193. doi: 10.21037/atm-22-10
47. Demircioglu ZG, Aygun N, Demircioglu MK, Ozguven BY, Uludag M. Low vitamin D status is not associated with the aggressive pathological features of papillary thyroid cancer. Sisli Etfal Hastan Tip Bul. (2022) 56:132–36. doi: 10.14744/SEMB.2022.36048
48. Choi YM, Kim WG, Kim TY, Bae SJ, Kim HK, Jang EK, et al. Serum vitamin D3 levels are not associated with thyroid cancer prevalence in euthyroid subjects without autoimmune thyroid disease. Korean J Intern Med. (2017) 32:102–08. doi: 10.3904/kjim.2015.090
49. Ahn HY, Chung YJ, Park KY, Cho BY. Serum 25-hydroxyvitamin D level does not affect the aggressiveness and prognosis of papillary thyroid cancer. Thyroid. (2016) 26:429–33. doi: 10.1089/thy.2015.0516
50. Friedrich JO, Adhikari NK, Beyene J. Ratio of means for analyzing continuous outcomes in meta-analysis performed as well as mean difference methods. J Clin Epidemiol. (2011) 64:556–64. doi: 10.1016/j.jclinepi.2010.09.016
51. Bolat H, Erdogan A. Benign nodules of the thyroid gland and 25-hydroxy-vitamin D levels in euthyroid patients. Ann Saudi Med. (2022) 42:83–8. doi: 10.5144/0256-4947.2022.83
52. Laney N, Meza J, Lyden E, Erickson J, Treude K, Goldner W. The prevalence of vitamin d deficiency is similar between thyroid nodule and thyroid cancer patients. Int J Endocrinol. (2010) 2010:805716. doi: 10.1155/2010/805716
53. van der Wielen RP, Löwik MR, van den Berg H, de Groot LC, Haller J, Moreiras O, et al. Serum vitamin D concentrations among elderly people in Europe. Lancet. (1995) 346:207–10. doi: 10.1016/S0140-6736(95)91266-5
Keywords: vitamin D, meta-analysis, thyroid cancer, vitamin D deficiency, 25 (OH)D, 1, 25 (OH)D
Citation: Hu Y, Xue C, Ren S, Dong L, Gao J and Li X (2024) Association between vitamin D status and thyroid cancer: a meta-analysis. Front. Nutr. 11:1423305. doi: 10.3389/fnut.2024.1423305
Received: 25 April 2024; Accepted: 31 May 2024;
Published: 18 June 2024.
Edited by:
Rhitajit Sarkar, National Institute of Diabetes and Digestive and Kidney Diseases (NIH), United StatesReviewed by:
Ying Lu, Shenzhen Second People's Hospital, ChinaCopyright © 2024 Hu, Xue, Ren, Dong, Gao and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuyang Li, bGVleGl1eWFuZ0AxMjYuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.