- 1Department of Gynecologic Oncology, Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing Maternal and Child Health Care Hospital, Beijing, China
- 2Department of Obstetrics and Gynecology, China-Japan Friendship Hospital, Beijing, China
- 3Graduate School, Capital Medical University, Beijing, China
Aim: This study aims to understand the association between body roundness index (BRI) and female infertility prevalence. Infertility is a public health concern with significant implications for individuals’ well-being and rights.
Methods: All individuals who completed the National Health and Nutrition Examination Survey (NHANES) between 2013 and 2018 were initially included in this cross-sectional study. Following the screening, 2,777 eligible participants were selected for analysis from the original pool of 10,375 participants. Trained operators conducted anthropometric measurements, including height, weight, and waist circumference. The BRI was then calculated based on established research. Data from infertility status questionnaires were gathered from the NHANES database for all participants, with self-reported infertility serving as the study outcome. Multivariable logistic regression and restricted cubic splines (RCS) were employed to investigate the relationship between BRI and infertility. Subgroup analyses were also conducted to further explore the association between BRI and infertility.
Results: Upon analyzing the baseline characteristics of all women in the study, notable distinctions were identified in the clinical and demographic features between fertile and infertile women. Our investigation revealed a positive correlation between BRI and the likelihood of infertility in both weighted and unweighted multiple logistic regression models. Additionally, BRI exhibited a significant association with infertility in both continuous and categorical forms. Utilizing RCS curves, we noted a linear escalation in the prevalence of infertility with rising BRI values. Subgroup analyses provided further clarity on these observations.
Conclusion: Our study demonstrates a statistically significant positive correlation between BRI and the prevalence of infertility across diverse populations, suggesting potential implications for infertility prevention and treatment. Future prospective cohort studies will explore this association and understand the underlying mechanisms.
Introduction
Infertility is a global health concern with significant implications for individuals’ well-being and rights (1–3). Around 48.5 million people worldwide are affected by infertility, leading to psychological, social, and reproductive health challenges, especially in underdeveloped regions (4). The condition is influenced by genetic, endocrine, and environmental factors (5). Hence, the prevention and management of infertility are imperative for the overall health and psychological welfare of women.
Abdominal obesity, characterized by fat accumulation around visceral organs in the abdominal cavity, is a prevalent issue linked to infertility (6, 7). Studies have shown a strong association between abdominal obesity and conditions like ovulation disorders, Polycystic Ovary Syndrome (PCOS), insulin resistance, abnormal estrogen levels, and disruptions in the reproductive cycle (8–12). Body mass index (BMI) is often used to assess obesity, still it may not accurately predict infertility prevalence due to its limitations in distinguishing between fat and muscle mass, and not considering fat distribution, particularly in cases of abdominal obesity (11).
In recent years, the body roundness index (BRI) has been recognized as a new anthropometric index that combines height and waist circumference measurements to provide a detailed picture of body shape and fat distribution (13). Higher BRI values indicate more abdominal fat, which can lead to health issues. Studies have linked high BRI levels to metabolic syndrome, fatty liver, cardiovascular disease, and psychological distress, providing a new tool for health assessment (14–20). Nevertheless, the relationship between BRI and infertility remains uncertain.
Further research on the relationship between BRI and infertility issues, along with an exploration of the physiological and pathological mechanisms involved, is crucial for enhancing the prevention and treatment of infertility and advancing reproductive health. In this study, we utilized data from the National Health and Nutrition Examination Survey (NHANES) to conduct a significant cross-sectional study, for the first time, examining the link between BRI and infertility among women in the United States. The results of this study could provide valuable insights into the prevention and treatment of infertility.
Methods
Study population
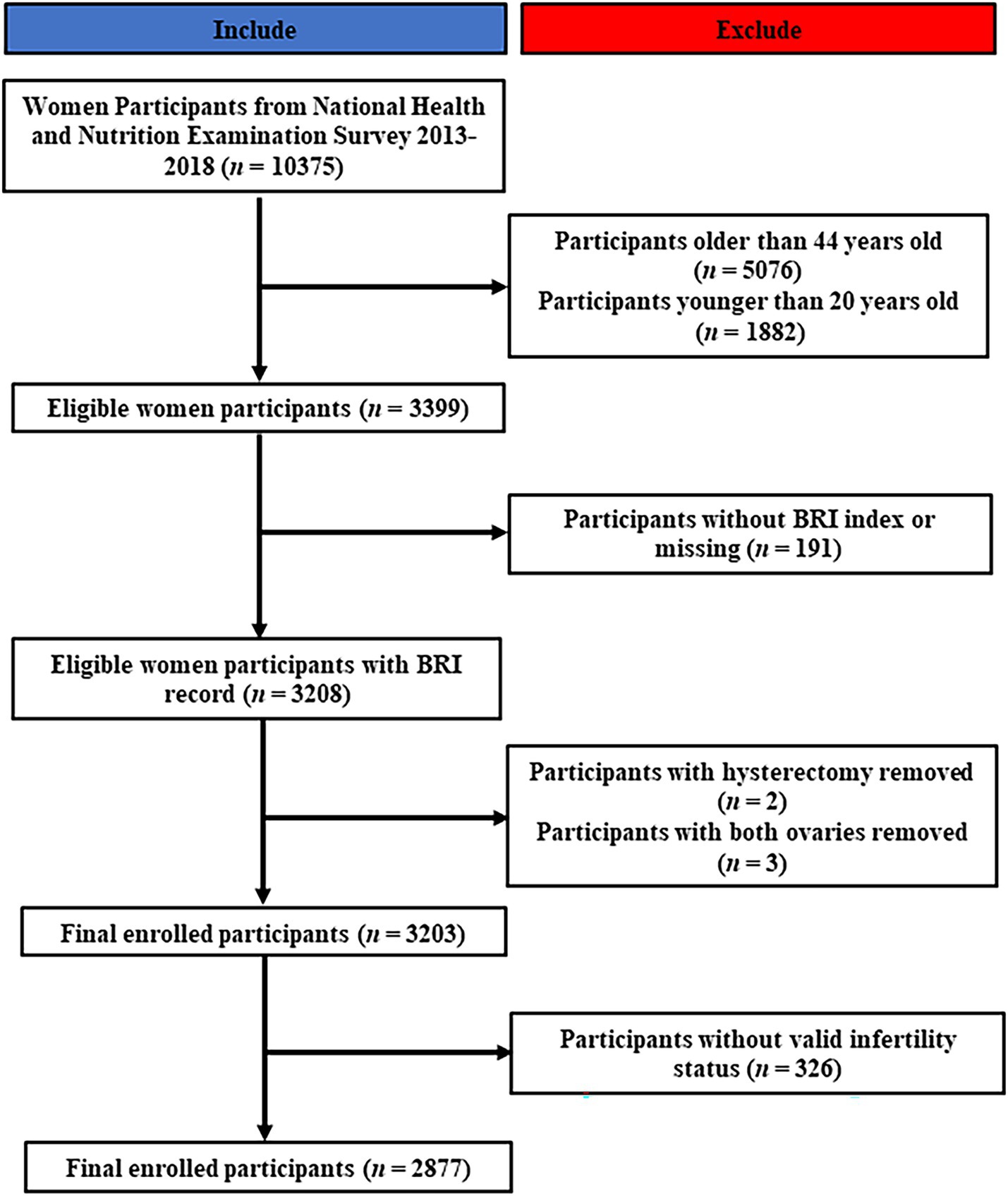
The NHANES study, a comprehensive cross-sectional investigation conducted on a national scale in the United States, is designed to assess the health and dietary patterns of the entire population, encompassing both adults and children (21, 22). This study has played a pivotal role in informing health policy decisions (23). Given the limited availability of infertility-related data from 2013 to 2018, our study initially focused on analyzing data from the 10,375 female participants in NHANES during this time period, applying rigorous inclusion and exclusion criteria. Initially, women who did not fall within the reproductive age range were excluded from the study, comprising 5,076 individuals over the age of 44 and 1882 individuals under the age of 20. Subsequently, participants with incomplete or absent BRI data (n = 191) were excluded, as well as those who had undergone hysterectomy or oophorectomy procedures (N = 5). Furthermore, 326 women were found to be lacking essential infertility-related data. Ultimately, a total of 2,877 participants were included in the study. The recruitment process is visually represented in Figure 1.
BRI measurement
Anthropometric measurements, such as body height (BH), body weight, and waist circumference (WC), were collected by trained examiners at a mobile examination center equipped with standardized tools. Participants’ body mass was evaluated using calibrated platform scales with a precision of 0.1 kg, and their height was measured with stadiometers while standing, accurate to 0.1 cm. These measurements were taken with participants wearing light clothing and no shoes. Consistent with prior research, BRI was calculated using the formula developed by Thomas et al. (20):
Self-reported infertility
Consistent with previous research, infertility is defined as the failure to achieve pregnancy after 1 year of unprotected intercourse, as self-reported by individuals (24–26). The presence of infertility was determined through responses to a questionnaire, with women indicating a positive response to either of two questions: “Have you attempted to conceive for at least 1 year without success?” or “Have you sought medical assistance for infertility?” being classified as ever infertile.
Covariates
Demographic information, including age, gender, race/ethnicity, educational level, marital status, household income, smoking, and alcohol consumption habits, was collected through standardized questionnaires and in-person interviews. Furthermore, data on menstrual regularity, pelvic infections, use of female hormones, and contraceptive pill usage was obtained through face-to-face interviews. Ethnicity was classified into five distinct categories: non-Hispanic White, non-Hispanic Black, other Hispanic, Mexican American, and other racial groups. Academic achievement was categorized into three tiers: below high school, high school, and above high school. The BMI, calculated by dividing weight in kilograms (kg) by height in meters squared (m2), was utilized as the principal measure for assessing overweight and obesity, with BMI values surpassing 25 kg/m2 and 30 kg/m2 denoting overweight and obesity, respectively.
Statistical methods
The NHANES study employed a sophisticated weighted sampling technique to collect data, requiring the weighting of all analyses to ensure the sample’s representativeness. Data was presented using percentages and 95% confidence intervals. T-tests and chi-square tests were applied in the baseline characteristics table to compare variables across different groups. The BRI variable was analyzed both as a continuous variable and divided into four groups for further statistical explanations. Weighted and unweighted multivariable logistic regression analyses were conducted to consider covariates related to infertility. Additionally, the RCS method was used to investigate the relationship between BRI and infertility. Subgroup analyses were performed to explore how BRI and infertility are linked in diverse populations. Statistical analyses were carried out using R software version 4.1.6, with statistical significance set at a two-tailed p-value <0.05.
Results
Demographical and clinical characteristics of the study population
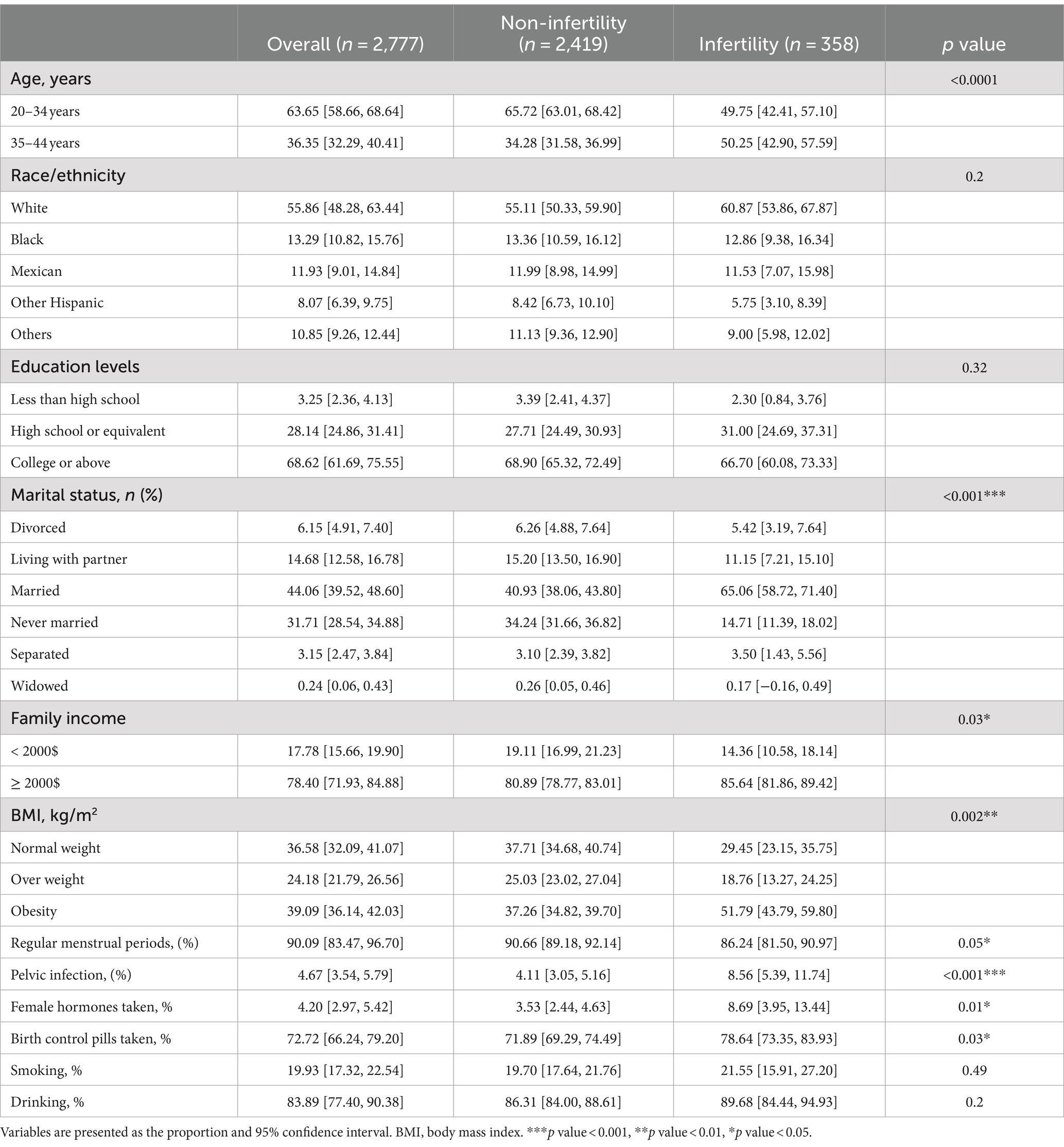
In this study, strict criteria for participant selection were applied, including of 2,777 eligible female participants from the NHANES. Among the cohort, 63.7% were females aged 20–34, while 36.3% were females aged 35–44. Of the total participants, 358 were identified as having infertility conditions, with this subgroup generally being older than those without infertility. Analysis of baseline data highlighted differences in marital status and family income between the two groups. Specifically, women with infertility had higher family incomes, higher rates of obesity based on BMI measurements, irregular menstrual periods, and a higher prevalence of pelvic infections. They also reported more frequent past use of female hormones and birth control pills. No significant differences were found in race, education level, smoking and alcohol consumption between the groups, as indicated in Table 1. Furthermore, participants were divided into four groups based on BRI, with detailed comparisons of baseline demographic and clinical characteristics provided in Supplementary Table S1.
Associations between BRI and prevalence of infertility
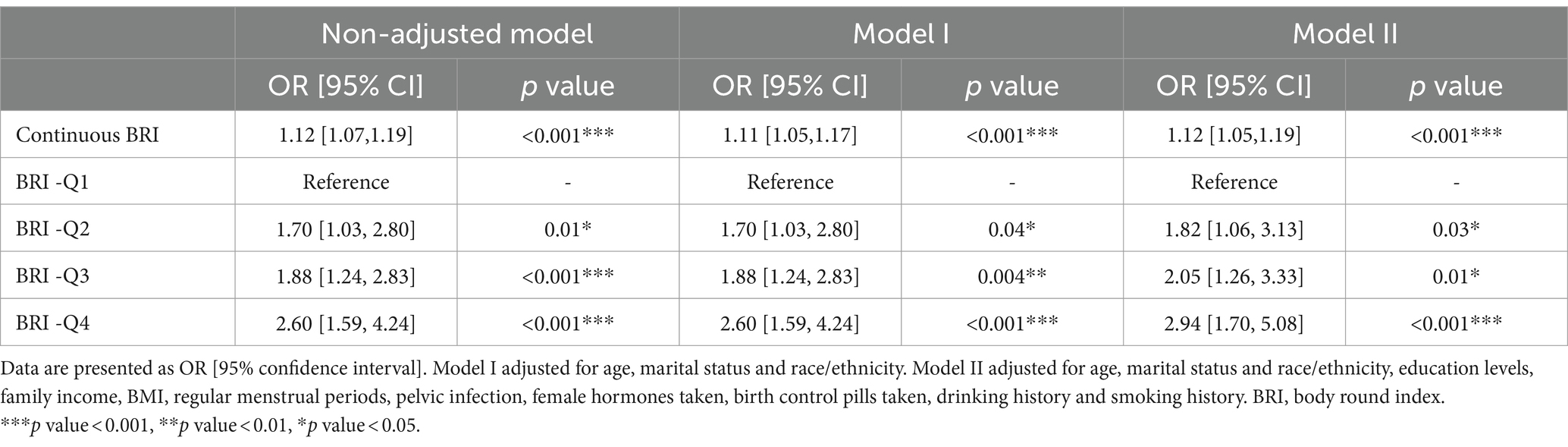
A comprehensive weighted multivariable logistic regression analysis was conducted to investigate the relationship between BRI and infertility prevalence. Covariates such as age, marital status, ethnicity, education level, income, BMI, menstrual regularity, pelvic infection, hormone and birth control pill usage, alcohol consumption, and smoking history were adjusted to account for potential confounding factors. The results indicated a statistically significant relationship between BRI and infertility, regardless of whether BRI was treated as a continuous or categorical variable. In the fully adjusted model, the odds ratio (OR) for BRI as a continuous variable was 1.12 (95%CI: 1.05–1.19). When BRI was treated as a categorical variable with Q1 as the reference, the ORs were as follows: Q2 (OR: 1.82; 95%CI: 1.06–3.13), Q3 (OR: 2.05; 95%CI: 1.26–3.33), Q4 (OR: 2.94; 95%CI: 1.70–5.08; Table 2). While weighting methods may improve sample representativeness, some studies suggest that weighted and unweighted results can vary. In this study, an unweighted multivariable regression analysis was performed to examine the association between BRI and infertility. The findings of the unweighted analysis were found to align with those of the weighted analysis (Table 3). Furthermore, the RCS method was utilized to explore the correlation between BRI and infertility, revealing a notable linear rise in infertility rates with increasing BRI (Figure 2).
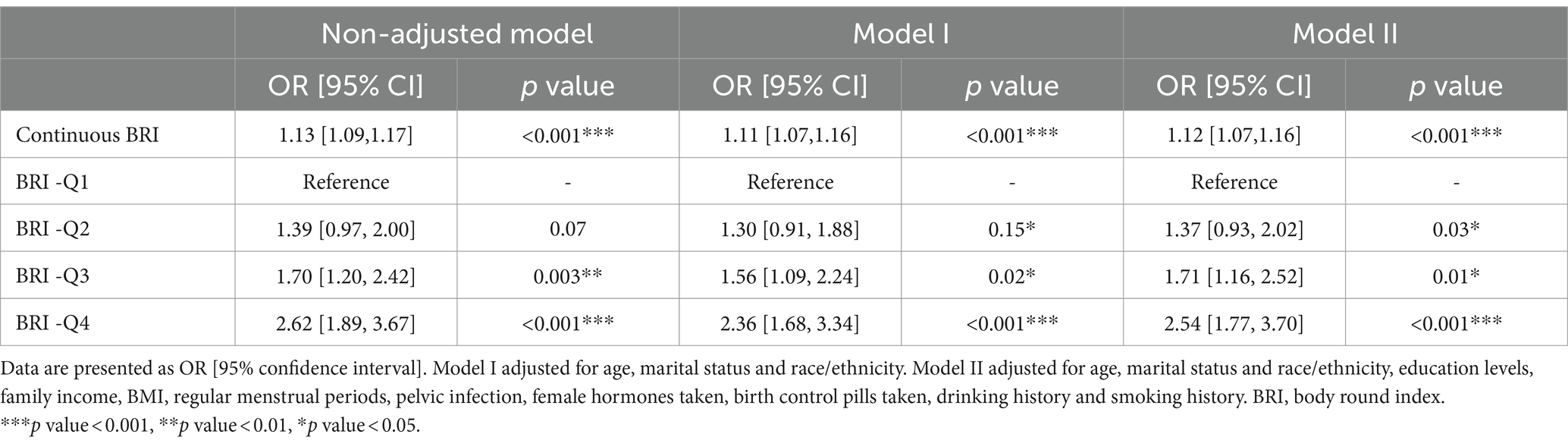
Table 3. Unweighted multivariate logistic regression of the association between BRI and infertility.
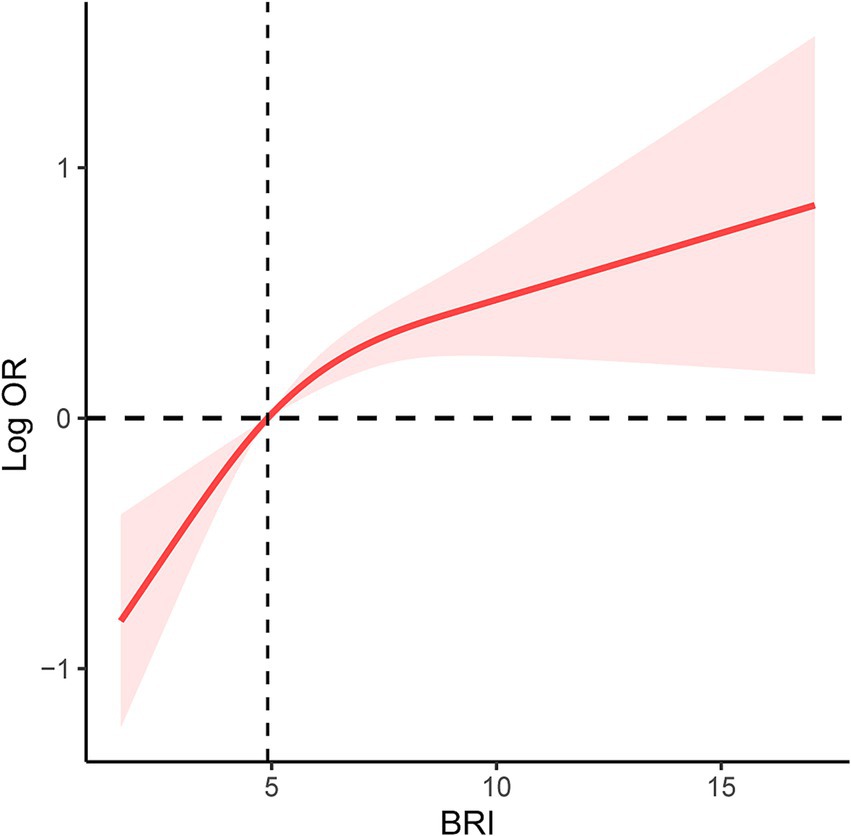
Figure 2. RCS curve of the association between BRI and prevalence of infertility among all participants. It was adjusted for age, marital status and race/ethnicity, education levels, family income, BMI, regular menstrual periods, pelvic infection, female hormones taken, birth control pills taken, drinking history and smoking history. RCS, restricted cubic spline; BRI, body round index; BMI, body mass index; OR, odds ratio.
Subgroup analysis on the associations between BRI and prevalence of infertility
In this study, detailed subgroup analyses to explore the relationship between BRI and infertility across various demographics. The findings revealed a positive correlation between BRI and infertility occurrence rates in several subgroups. However, this correlation did not reach statistical significance among older adult patients, overweight individuals, those with an educational level below high school, and non-drinkers. Conversely, statistically significant positive correlations between BRI and infertility were observed in other demographic groups, as illustrated in Figure 3. Furthermore, RCS spline analyses were performed on diverse populations characterized by varying ages, races, smoking and drinking habits, and income levels. The results indicated a significant positive correlation between BRI and infertility across a range of demographic variables. Specifically, as BRI levels increased, there was a consistent trend of rising infertility rates observed among different population subsets (Figure 4).
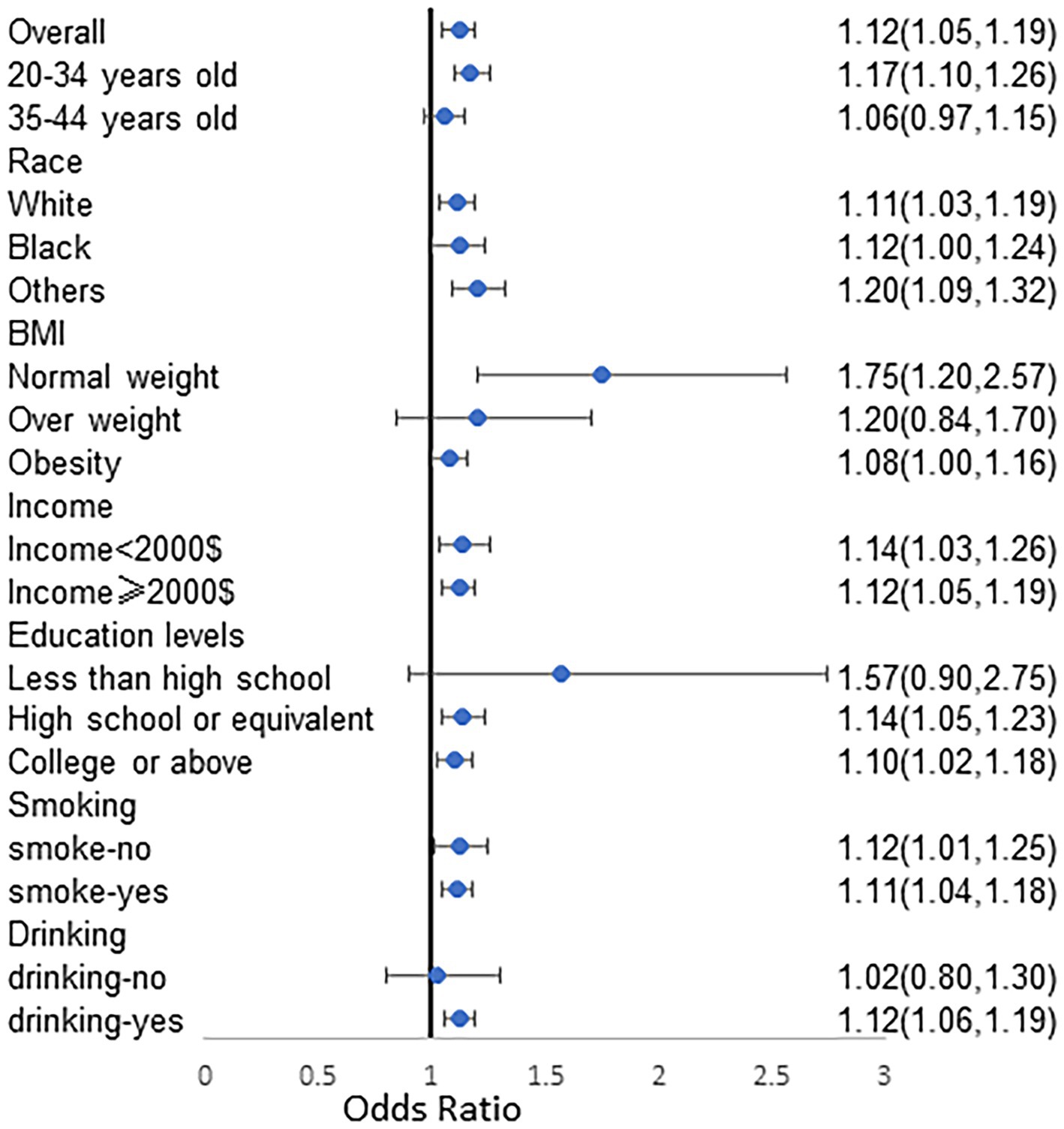
Figure 3. Subgroups analyzes stratified by age, race, family income, education levels, smoking and drinking for the association between BRI and prevalence of infertility. Analyses were adjusted for age, marital status and race/ethnicity, education levels, family income, BMI, regular menstrual periods, pelvic infection, female hormones taken, birth control pills taken, drinking history and smoking history. BRI, body round index; BMI, body mass index; OR, odds ratio.
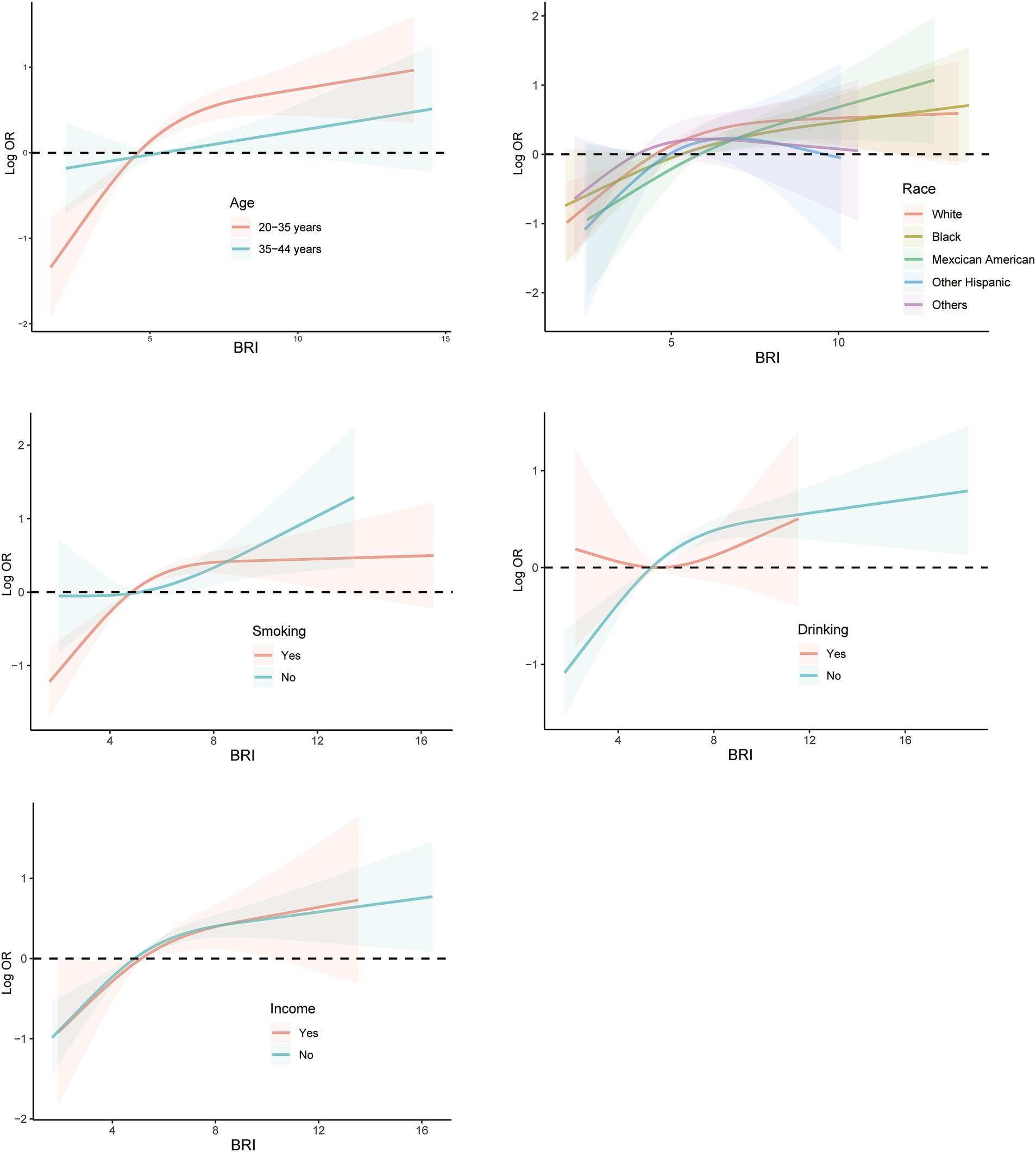
Figure 4. Subgroups RCS curves for the association between BRI and prevalence of infertility among populations with different characteristics. Analyses were stratified by age, race, smoking, drinking, and family income. RCS analyses were adjusted for age, marital status and race/ethnicity, education levels, family income, BMI, regular menstrual periods, pelvic infection, female hormones taken, birth control pills taken, drinking history and smoking history. RCS, restricted cubic spline; BRI, body round index; BMI, body mass index; OR, odds ratio.
Predictive value of BRI on the prevalence of infertility
In addition, an examination was conducted to assess the predictive capacity of BRI in relation to infertility through the utilization of ROC curves. It was determined that BRI demonstrates a favorable predictive capability for fertility, as evidenced by an area under the curve (AUC) of 60.5% (57.3%—63.7%). The optimal cutoff value was identified as 5.6, yielding a sensitivity of 61.8% and a specificity of 63.7% (Figure 5).
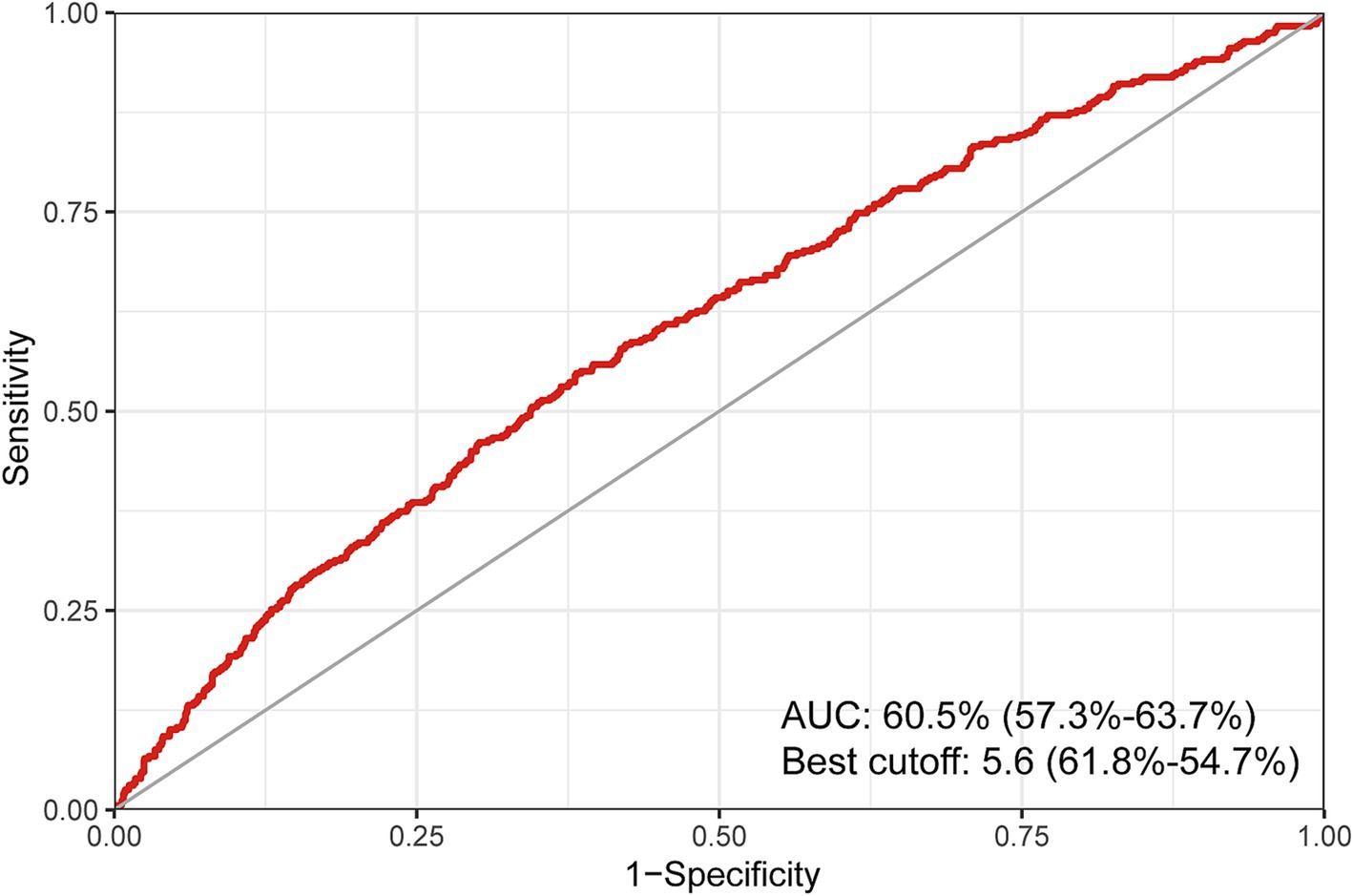
Figure 5. ROC curve of the predictive value for BRI on the prevalence of infertility. ROC, restricted cubic spline; BRI, body round index.
Discussion
In this cross-sectional study with a nationally representative sample, we investigated the relationship between BRI and infertility in women aged 20 to 45. Our findings reveal a notable link between BRI and the likelihood of infertility, even after accounting for potential confounding factors. BRI has the potential to serve as a predictive marker for infertility prevalence, which could inform strategies for prevention and treatment. Managing weight, decreasing abdominal circumference, and subsequently lowering BRI levels may potentially mitigate the prevalence of infertility.
This study is the first to directly investigate the relationship between the BRI and female infertility. Previous research has suggested that obesity can lead to hormonal imbalances and endocrine dysfunction, which may affect infertility (27, 28). However, the mechanism of increased BRI levels causing infertility prevalence in women remains unclear, and there exist several possible explanations. Excessive fat tissue, especially in the abdominal area, can raise estrogen levels in obese women, disrupting hormonal balance and causing changes in ovulation and menstrual cycles (29–33). Additionally, obesity can worsen ovulation problems, especially in cases of abdominal obesity, which are associated with hormonal imbalances such as PCOS (34). This form of obesity is also linked to insulin resistance and high blood sugar levels (35). Furthermore, inflammatory substances released by abdominal fat can negatively impact fertility and the receptivity of the endometrium to support a pregnancy. Moreover, obesity and excess fat can contribute to psychological issues like low self-esteem and anxiety in women, which can subsequently affect fertility (36).
BRI is a novel measurement index that offers advantages over the traditional BMI by specifically addressing the crucial health issue of abdominal obesity (37). Unlike BMI, which solely relies on height and weight, the BRI takes into account waist circumference, providing a more holistic perspective on body shape (38). This feature enhances the accuracy of the BRI in identifying abdominal obesity, particularly in individuals with excess abdominal fat, leading to a more precise evaluation of this condition (39). Moreover, the BRI is less influenced by muscle mass, making it a more dependable indicator of the relationship between fat content and health risks in individuals with higher muscle mass (40–43). Besides, the advantage of the BRI over WC is its incorporation of height information. This dual consideration enables the BRI to more comprehensively reflect an individual’s body shape characteristics and fat distribution. Consequently, the BRI is better suited for assessing diseases closely linked to abdominal obesity. Numerous studies have demonstrated that BRI is more strongly associated with the risk of metabolic disorders like diabetes and cardiovascular disease compared to BMI (13, 44). Furthermore, studies have shown that BRI can significantly determine the presence of insulin resistance (45). These results suggest that the BRI may offer a more precise reflection of the connection between body fat distribution and health risks (23).
Our study investigated the association between female infertility and BRI, revealing a positive correlation between BRI and a higher prevalence of infertility in both unadjusted and adjusted models. It is widely acknowledged that BRI serves as an indicator for obesity and reproductive issues. Our findings were consistent with anticipated outcomes. However, the precise mechanism through which elevated BRI levels contribute to the prevalence of female infertility remains unclear. Potential explanations include disruptions in fatty acid metabolism in visceral adipose tissue due to obesity, leading to excessive accumulation of fatty acids in various tissues. This accumulation can result in insulin resistance, fatty acid peroxidation, hormonal imbalances, and ultimately impact ovulation and ovum quality. Moreover, visceral adipose tissue, being an active endocrine tissue, can generate inflammatory mediators such as tumor necrosis factor α and interleukin-6. The excessive release of these mediators may trigger a chronic inflammatory response, causing damage to vascular endothelial cells and reducing endometrial receptivity (46, 47). Should further evidence emerge, it would be beneficial for individuals to identify the optimal control range for managing body size.
This study has various strengths. Firstly, the research utilized data from the NHANES database, including all eligible participants available. With a large number of participants included, the conclusions drawn can be considered more reliable. Secondly, the NHANES database employs complex stratified sampling methods, and all data analyses in the study were conducted using weighted analysis, enhancing the representativeness of the findings. Thirdly, detailed stratified analyses in subgroups revealed significant relationships between BRI and infertility across different populations, further bolstering the reliability of the research. Finally, both weighted and unweighted analyses were employed to validate the conclusions, and the results from both analyses were consistent.
This study also has some limitations. Firstly, it was only a cross-sectional study, limiting the ability to infer causal relationships. Secondly, the self-reported nature of the outcome measure, infertility, may introduce reporting bias. Thirdly, the study was conducted solely within the United States, and while it included multiple ethnicities, the generalizability of the findings to other countries and regions requires further confirmation through large-scale prospective cohort studies.
Conclusion
Participants in this study were recruited from NHANES, specifically targeting women of childbearing age. The study results indicated a significant positive correlation between BRI and the prevalence of infertility. As the BRI level increased, the prevalence of infertility also increased linearly. This correlation was consistent across demographic characteristics. Additionally, BRI may serve as a valuable predictor of infertility prevalence. In order to improve fertility, it is recommended that women prioritize the maintenance of a balanced diet, regular physical activity, and the management of a healthy weight and waist circumference. Should further research corroborate these conclusions, it would be advantageous for individuals to ascertain the optimal BRI for the regulation of body size. Future prospective cohort studies should delve into the association and elucidate the underlying mechanisms.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The NHANES protocol adheres to the Policy for the Protection of Human Research Subjects set forth by the U.S. Department of Health and Human Services. The protocol numbers for NCHS IRB/ERC are #2011-17 and #2018-01. All participants provided informed consent for their involvement in the NHANES survey.
Author contributions
WW: Writing – original draft, Writing – review & editing. SH: Writing – original draft. KW: Writing – original draft. BL: Writing – review & editing. HY: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by Capital’ s Funds for Health Improvement and Research (No. 2022-2-406), the National High Level Hospital Clinical Research Funding (No. 2022-NHLHCRF-PY-02) and the Funds of the China-Japan Friendship Hospital (No. 2017-RC-4).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1416637/full#supplementary-material
References
1. Eisenberg, ML, Esteves, SC, Lamb, DJ, Hotaling, JM, Giwercman, A, Hwang, K, et al. Male infertility. Nat Rev Dis Primers. (2023):9. doi: 10.1038/s41572-023-00459-w
2. Sadri-Ardekani, H, and Atala, A. Regenerative medicine for the treatment of reproductive system disorders: current and potential options. Adv Drug Deliv Rev. (2015) 82-83:145–52. doi: 10.1016/j.addr.2014.10.019
3. Ennab, F, and Atiomo, W. Obesity and female infertility. Best Pract Res Clin Obstet Gynaecol. (2023) 89:102336. doi: 10.1016/j.bpobgyn.2023.102336
4. Mascarenhas, MN, Flaxman, SR, Boerma, T, Vanderpoel, S, and Stevens, GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. (2012) 9:e1001356. doi: 10.1371/journal.pmed.1001356
5. Woodward, JT, Cirino, NH, Copland, S, and Davoudian, T. Integrated behavioral health Care in Reproductive Medicine: how and why to include mental health professionals in infertility care teams. Clin Obstet Gynecol. (2024) 67:222–32. doi: 10.1097/GRF.0000000000000829
6. Mansour, S, Alkhaaldi, S, Sammanasunathan, AF, Ibrahim, S, Farhat, J, and Al-Omari, B. Precision nutrition unveiled: gene-nutrient interactions, microbiota dynamics, and lifestyle factors in obesity management. Nutrients. (2024) 16:581. doi: 10.3390/nu16050581
7. Després, J, and Lemieux, I. Abdominal obesity and metabolic syndrome. Nature. (2006) 444:881–7. doi: 10.1038/nature05488
8. Kobori, T, Iwabu, M, Okada-Iwabu, M, Ohuchi, N, Kikuchi, A, Yamauchi, N, et al. Decreased AdipoR1 signaling and its implications for obesity-induced male infertility. Sci Rep. (2024) 14:5701. doi: 10.1038/s41598-024-56290-0
9. Liu, X, Zhang, J, and Wang, S. Global, regional, and national burden of infertility attributable to PCOS, 1990-2019. Hum Reprod. (2024) 39:108–18. doi: 10.1093/humrep/dead241
10. Jiang, NX, Zhao, WJ, Shen, HR, Du, DF, and Li, XL. Hyperinsulinemia impairs decidualization via AKT-NR4A1 signaling: new insight into polycystic ovary syndrome (PCOS)-related infertility. J Ovarian Res. (2024) 17:31. doi: 10.1186/s13048-023-01334-8
11. Li, M, Mínguez-Alarcón, L, Arvizu, M, Chiu, Y, Ford, JB, Williams, PL, et al. Waist circumference in relation to outcomes of infertility treatment with assisted reproductive technologies. Am J Obstet Gynecol. (2019) 220:578.e1–578.e13. doi: 10.1016/j.ajog.2019.02.013
12. Jiang, N, Zhang, S, Chu, J, Yang, N, and Lu, M. Association between body roundness index and non-alcoholic fatty liver disease detected by Fibroscan in America. J Clin Lab Anal. (2023) 37:37. doi: 10.1002/jcla.24973
13. Li, Z, Fan, C, Huang, J, Chen, Z, Yu, X, and Qian, J. Non-linear relationship between the body roundness index and metabolic syndrome: data from National Health and nutrition examination survey (NHANES) 1999-2018. Br J Nutr. (2024) 131:1852–9. doi: 10.1017/S0007114524000357
14. Zhao, E, Wen, X, Qiu, W, and Zhang, C. Association between body roundness index and risk of ultrasound-defined non-alcoholic fatty liver disease. Heliyon. (2024) 10:e23429. doi: 10.1016/j.heliyon.2023.e23429
15. Lotfi, K, Hassanzadeh Keshteli, A, Saneei, P, Afshar, H, Esmaillzadeh, A, and Adibi, P. A body shape index and body roundness index in relation to anxiety, depression, and psychological distress in adults. Front Nutr. (2022) 9:9. doi: 10.3389/fnut.2022.843155
16. Ding, J, Chen, X, Shi, Z, Bai, K, and Shi, S. Association of body roundness index and its trajectories with all-cause and cardiovascular mortality among a Chinese middle-aged and older population: a retrospective cohort study. Front Public Health. (2023) 11:11. doi: 10.3389/fpubh.2023.1107158
17. Wu, M, Yu, X, Xu, L, Wu, S, and Tian, Y. Associations of longitudinal trajectories in body roundness index with mortality and cardiovascular outcomes: a cohort study. Am J Clin Nutr. (2022) 115:671–8. doi: 10.1093/ajcn/nqab412
18. Feng, J, He, S, and Chen, X. Body adiposity index and body roundness index in identifying insulin resistance among adults without diabetes. Am J Med Sci. (2019) 357:116–23. doi: 10.1016/j.amjms.2018.11.006
19. Liu, Y, Liu, X, Guan, H, Zhang, S, Zhu, Q, Fu, X, et al. Body roundness index is a superior obesity index in predicting diabetes risk among hypertensive patients: a prospective cohort study in China. Front Cardiovasc Med. (2021) 8:736073. doi: 10.3389/fcvm.2021.736073
20. Thomas, DM, Bredlau, C, Bosy-Westphal, A, Mueller, M, Shen, W, Gallagher, D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring). (2013) 21:2264–71. doi: 10.1002/oby.20408
21. Tao, L, Miao, L, Guo, YJ, Liu, YL, Xiao, LH, and Yang, ZJ. Associations of body roundness index with cardiovascular and all-cause mortality: NHANES 2001-2018. J Hum Hypertens. (2024) 38:120–7. doi: 10.1038/s41371-023-00864-4
22. Lin, W, and Lin, ME. Novel anthropometric measures are positively associated with erectile dysfunction: a cross-sectional study. Int Urol Nephrol. (2024) 56:855–65. doi: 10.1007/s11255-023-03840-6
23. Wu, LD, Kong, CH, Shi, Y, Zhang, JX, and Chen, SL. Associations between novel anthropometric measures and the prevalence of hypertension among 45,853 adults: a cross-sectional study. Front Cardiovasc Med. (2022) 9:1050654. doi: 10.3389/fcvm.2022.1050654
24. Zhuang, J, Xi, K, Yu, L, and Li, X. Non-linear Association of Serum sex Hormone Binding Globulin Concentration with female infertility. Clin Lab. (2024) 70:70. doi: 10.7754/Clin.Lab.2023.230638
25. Torrone, E, Papp, J, and Weinstock, H. Prevalence of Chlamydia trachomatis genital infection among persons aged 14-39 years--United States, 2007-2012. MMWR Morb Mortal Wkly Rep. (2014) 63:834–8.
26. Kreisel, K, Torrone, E, Bernstein, K, Hong, J, and Gorwitz, R. Prevalence of pelvic inflammatory disease in sexually experienced women of reproductive age - United States, 2013-2014. MMWR Morb Mortal Wkly Rep. (2017) 66:80–3. doi: 10.15585/mmwr.mm6603a3
27. Patel, JA, Colella, JJ, Esaka, E, Patel, NA, and Thomas, RL. Improvement in infertility and pregnancy outcomes after weight loss surgery. Med Clin North Am. (2007) 91:515–28. doi: 10.1016/j.mcna.2007.01.002
28. Pasquali, R. Obesity, fat distribution and infertility. Maturitas. (2006) 54:363–71. doi: 10.1016/j.maturitas.2006.04.018
29. Jurczewska, J, Ostrowska, J, Chelchowska, M, Panczyk, M, Rudnicka, E, Kucharski, M, et al. Abdominal obesity in women with polycystic ovary syndrome and its relationship with diet, physical activity and insulin resistance: a pilot study. Nutrients. (2023) 15:15. doi: 10.3390/nu15163652
30. Dondi, E, Tufano, M, Vigone, MC, Lucaccioni, L, Pozzobon, G, Ubertini, G, et al. Polycystic ovary syndrome in pediatric obesity and diabetes. Minerva Pediatr (Torino). (2021) 73:523–36. doi: 10.23736/S2724-5276.21.06542-3
31. Tan, O, and Carr, BR. The impact of bariatric surgery on obesity-related infertility and in vitro fertilization outcomes. Semin Reprod Med. (2012) 30:517–28. doi: 10.1055/s-0032-1328880
32. Pasdar, Y, Rezaeian, S, Mohammadi, E, Khosravi Shadmani, F, Shahnazi, N, Najafi, F, et al. The interaction between general or abdominal obesity and hypertension on the risk of type 2 diabetes mellitus: a cross-sectional analysis in Iranian adults from the RaNCD cohort study. BMC Public Health. (2024) 24:752. doi: 10.1186/s12889-024-18290-7
33. Incedal Irgat, S, and Bakirhan, H. The effect of obesity on human reproductive health and foetal life. Hum Fertil (Camb). (2022) 25:860–71. doi: 10.1080/14647273.2021.1928774
34. Tatarchuk, T, Todurov, I, Anagnostis, P, Tutchenko, T, Pedachenko, N, Glamazda, M, et al. The effect of gastric sleeve resection on menstrual pattern and ovulation in premenopausal women with classes III-IV obesity. Obes Surg. (2022) 32:599–606. doi: 10.1007/s11695-021-05820-0
35. Hsu, MC, Chen, CH, Wang, MC, Chen, WH, Hu, PA, Guo, BC, et al. Apigenin targets fetuin-a to ameliorate obesity-induced insulin resistance. Int J Biol Sci. (2024) 20:1563–77. doi: 10.7150/ijbs.91695
36. Brennan, L, Murphy, KD, de la Piedad, GX, Ellis, ME, Metzendorf, M, and McKenzie, JE. Psychological interventions for adults who are overweight or obese. Cochrane Database Syst Rev. (2018) 2018:CD012114. doi: 10.1002/14651858.CD012114.pub2
37. Lin, G, Zhan, F, Ren, W, Pan, Y, and Wei, W. Association between novel anthropometric indices and prevalence of kidney stones in US adults. World J Urol. (2023) 41:3105–11. doi: 10.1007/s00345-023-04582-x
38. Zhou, D, Liu, X, Huang, Y, and Feng, Y. A nonlinear association between body roundness index and all-cause mortality and cardiovascular mortality in general population. Public Health Nutr. (2022) 25:3008–15. doi: 10.1017/S1368980022001768
39. Li, M, Cui, M, Li, G, Liu, Y, Xu, Y, Eftekhar, SP, et al. The pathophysiological associations between obesity, NAFLD, and atherosclerotic cardiovascular diseases. Horm Metab Res. (2024) 56:683–96. doi: 10.1055/a-2266-1503
40. Tian, X, Ding, N, Su, Y, and Qin, J. Comparison of obesity-related indicators for nonalcoholic fatty liver disease diagnosed by transient Elastography. Turk J Gastroenterol. (2023) 34:1078–87. doi: 10.5152/tjg.2023.23101
41. Sun, Z, Wang, K, Yun, C, Bai, F, Yuan, X, Lee, Y, et al. Correlation between the variability of different obesity indices and diabetic kidney disease: a retrospective cohort study based on populations in Taiwan. Diabetes Metab Syndr Obes. (2023) 16:2791–802. doi: 10.2147/DMSO.S425198
42. Alkhatib, B, Agraib, LM, Al-Shami, I, and Al-Dalaeen, A. The novelty of using obesity indices as blood pressure predictors. Curr Hypertens Rev. (2023) 20:36–43. doi: 10.2174/0115734021277171231114103758
43. Tian, S, Zhang, X, Xu, Y, and Dong, H. Feasibility of body roundness index for identifying a clustering of cardiometabolic abnormalities compared to BMI, waist circumference and other anthropometric indices. Medicine (Baltimore). (2016) 95:e4642. doi: 10.1097/MD.0000000000004642
44. Sisay, BG, Jima, BR, Habtamu, M, Gebru, NW, and Hassen, HY. Predictive ability of anthropometric indices in identifying metabolic syndrome among US adolescents 10 to 19 years old: analysis from the National Health and nutrition examination survey 2011 to 2018 data set. Nutrition. (2023) 113:112081. doi: 10.1016/j.nut.2023.112081
45. Zhang, S, Han, S, Zheng, L, Sun, Y, and Sun, Z. Associations of trajectories in body roundness index with incident cardiovascular disease: a prospective cohort study in rural China. Front Nutr. (2024) 11:11. doi: 10.3389/fnut.2024.1291093
46. Cai, X, Song, S, Hu, J, Zhu, Q, Yang, W, Hong, J, et al. Body roundness index improves the predictive value of cardiovascular disease risk in hypertensive patients with obstructive sleep apnea: a cohort study. Clin Exp Hypertens. (2023) 45:2259132. doi: 10.1080/10641963.2023.2259132
Keywords: BRI, infertility, cross-sectional study, NHANES, women health
Citation: Wang W, Hou S, Wang K, Ling B and Yu H (2024) Association of body roundness index with female infertility: 2013–2018 NHANES. Front. Nutr. 11:1416637. doi: 10.3389/fnut.2024.1416637
Edited by:
Roberto Fernandes Da Costa, Autonomous University of Chile, ChileReviewed by:
Iolanda Karla Santana dos Santos, Federal University of ABC, BrazilBo Liu, Guangdong Provincial Academy of Chinese Medical Sciences, China
Copyright © 2024 Wang, Hou, Wang, Ling and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huan Yu, eXVodWFuMjAwMEBzaW5hLmNvbQ==
 Wenhui Wang
Wenhui Wang Shengdi Hou2,3
Shengdi Hou2,3 Bin Ling
Bin Ling Huan Yu
Huan Yu