
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 22 January 2025
Sec. Nutrition and Metabolism
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1414930
This article is part of the Research Topic Holistic Approaches to Understanding Obesity and Metabolic Diseases in Urban Environments View all 9 articles
Introduction: A widely recognized public health issue affecting people worldwide is central obesity. Numerous chronic conditions, such as type 2 diabetes mellitus, cardiovascular disease, and malignancies are linked to this syndrome. There is limited information about waist circumference (WC) and its related variables among urban bank workers in Ethiopia. Therefore, the purpose of this study was to evaluate waist circumference and the factors associated with it among bank workers in Northeast Ethiopia.
Methods: An institution-based cross-sectional study was carried out in Dessie, Northeast Ethiopia, between 2 October 2023 and 24 October 2023. A random selection method was employed to select 363 bank workers. STATA version 17 was used for analysis after the data were imported into EpiData version 4.4.2.0. Univariate and multivariate linear regression analyzes were performed to identify factors related to waist circumference. Normality, homoscedasticity, significant outliers, and multicollinearity were assessed, and a p-value of less than 0.05, along with a 95% confidence interval, was considered statistically significant.
Results: A total of 345 participants were included in the final analysis, with a 95% response rate. The overall mean ± standard deviation (SD) of the waist circumference of the employees was 81.7 ± 6.8 cm, with 82.4 ± 6.5 cm for men and 80.7 ± 7.2 cm for women. The overall prevalence of central obesity was 57.7%, with 48.2% for the men and 70.3% for the women. The overall mean ± SD of the waist-to-hip ratio (WHR) was 0.90 ± 0.05, with 0.91 ± 0.04 for men and 0.89 ± 0.05 for women. The average waist circumference was significantly associated with the participants’ age (0.2 cm per year (SE: 0.1)) and MET hours (0.2 cm (SE: 0.1)). The mean waist circumference was 2.7 cm (SE:0.8) higher in the married women, 4.6 cm (SE:1.9) higher in the participants with non-communicable diseases (NCDs), and 1.7 cm (SE:0.8) higher in the participants who consumed discretionary calories for 4 days/week.
Conclusion: The mean waist circumference among bank employees was higher, with more than half of the participants having central obesity. Age, marital status, discretionary calorie intake, non-communicable diseases, and metabolic equivalence task hours were the significant factors of waist circumference. Therefore, promoting activities aimed at preventing non-communicable diseases, such as leisure-time physical activity, and reducing discretionary calorie intake are essential for reducing high waist circumference measurements.
Obesity, defined by waist circumference (WC) and measured midway between the lowest rib cage at the mid-clavicular line and the anterior superior iliac spine, is the most practical indicator of fat distribution and central obesity (1). It is the most common condition that causes disability, disease, and premature death and is measured using body mass index (2). The National Cholesterol Education Program Third Adult Treatment Panel (NCEP-ATP III) defines central obesity as a waist circumference of ≥102 cm for men and ≥88 cm for women, while the International Diabetes Federation (IDF) establishes cut-off points of ≥94 cm for men and ≥80 cm for women (3, 4). Additionally, specific cut-off points for Ethiopians are 83.7 cm for men and 78 cm for women (5).
A complex combination of behavioral, environmental, social, and hereditary factors contribute to obesity (3, 6). Being overweight or obese has been estimated to cause 35.8 million (2.3%) disability-adjusted life years and 2.8 million deaths worldwide each year (7). Sub-Saharan Africa has been facing the double burden of communicable and non-communicable diseases in recent years (8). Compared to BMI, central obesity is more strongly correlated with diabetes mellitus (DM) and cerebrovascular disease (CVD) (9). According to a linear dose–response analysis, the incidence of CVD increased by 3.4% for women and 4.0% for men with every 10 cm rise in waist circumference (WC) (10). The World Health Organization lists obesity as the fifth and seventeenth major risk factor contributing to the overall burden of disease in emerging nations with low and high death rates, respectively (11). Obesity has been linked to approximately 44% of diabetes cases, 23% of ischemic heart disease cases, and 7–41% of certain cancer cases (12).
Chronic health issues such as type 2 diabetes and cardiovascular diseases have been on the rise in many developing and underdeveloped nations, including Ethiopia, as a result of obesity and overweight. In Ethiopia, central obesity and overweight have become serious public health concerns, particularly among urban residents (13, 14). Ethiopia is currently facing the fallout from epidemiologic, demographic, economic, and nutritional shifts that continue to drive the spread of chronic non-communicable disease (NCD) epidemics (15). The burden of chronic disease morbidity and mortality is still rising despite government efforts to reduce risk factors for chronic diseases, such as central obesity (16).
There have been very few studies conducted on the prevalence of obesity based on body mass index in our country (17). Work environments that require limited physical activity (18), such as banks, are major employers. Thus, the purpose of this study was to evaluate obesity among urban bank employees in the study area. The results of this study can serve as a guide, especially for individuals who are at high risk.
An institution-based cross-sectional study was conducted from 2 October to 24 October 2023 among urban bank employees in Dessie. Dessie is a city located 400 km to the north of the capital, Addis Ababa. It has a population of more than 230,733 people across five sub-cities (19). The city has 23 banks, with a total of 1,870 permanent employees, of whom 1,174 are men and the remaining 696 are women.
The study population consisted of individuals aged ≥18 years, randomly selected from among the bank employees during the data collection period.
All permanent bank employees were included in the study, whereas pregnant women, mothers with <6 months postpartum, individuals with deformities on their backs, individuals unable to stand in an erect position, those with chronic edema, and non-permanent employees (employees with less than 6 months of work experience and outsourced security workers) were excluded from the study.
The sample size was calculated using the mean waist circumference formula, as the single population proportion formula and the double population proportion formula had lower sample sizes compared to using the mean. Therefore, with a standard deviation (SD) of 13.9 cm, a maximum accepted margin of error of 1.5 cm [taken from a previous study (20)], and a 95% CI, the final sample size, allowing for a 10% non-response rate, was 363.
There are 23 banks in Dessie city. Of these, five banks (Hibret, CBE, Amhara, Oromia, and Abay banks) were randomly selected. Then, an exhaustive list of permanent employees from the selected banks was prepared, and the number of the included participants from each bank was allocated proportionally. Finally, the participants were selected through systematic random sampling with a k-value of 2 (N/n = 761/363 ≈ 2). The first participant was selected using simple random sampling (lottery method), and the subsequent participants were selected at every second interval (Figure 1).
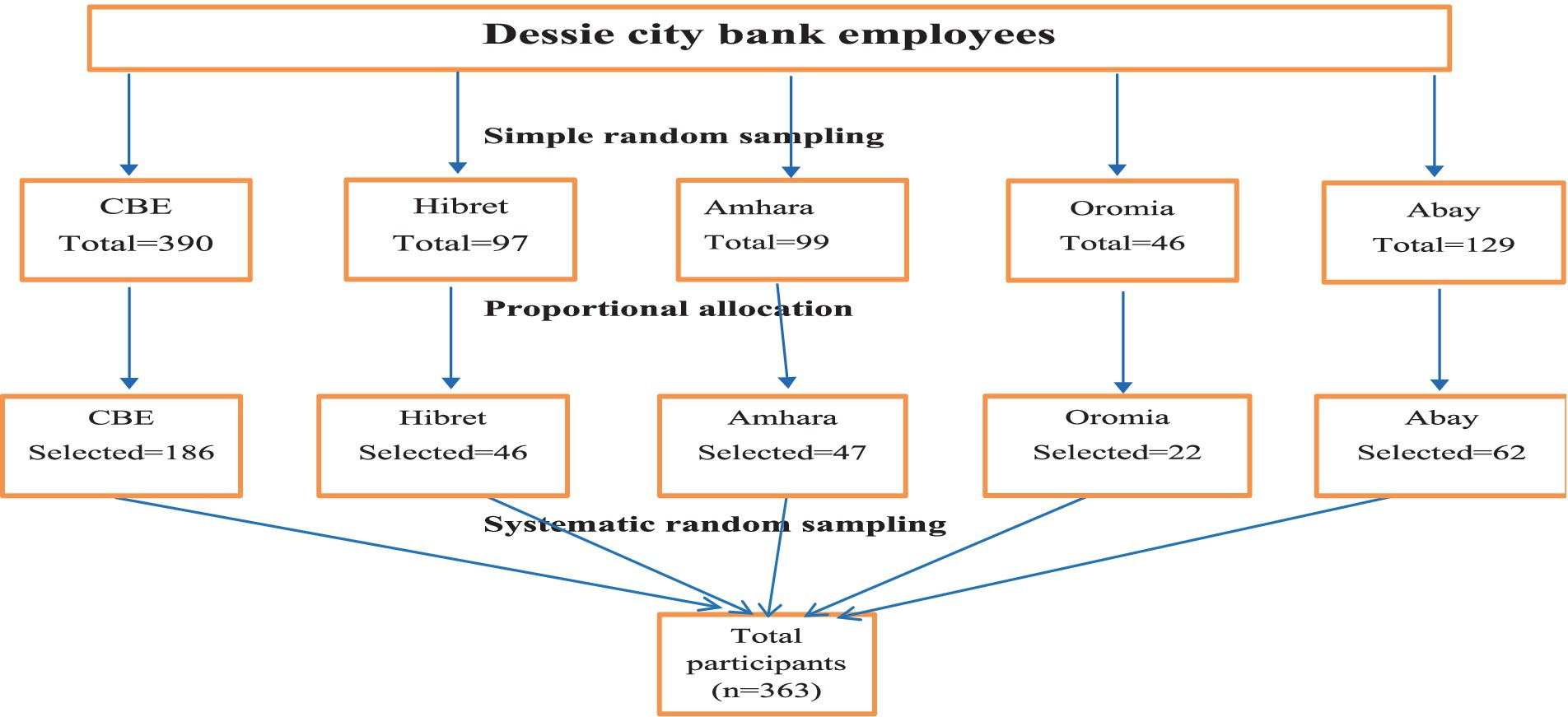
Figure 1. Schematic representation of the sampling procedure for waist circumference and the associated factors among the bank employees in Northeast Ethiopia, 2023.
For Ethiopian adults, it was defined as a waist circumference of 83.7 cm for men and 78 cm for women (21). Another cut-off point for Ethiopian adults was a waist-to-hip ratio (WHR) of 0.88 for men and 0.82 for women (5).
The dietary intake of the study participants was evaluated using a 24-h dietary recall. From the morning of the previous day to the morning of the current day, the participants were asked to list everything they had eaten, including snacks and food consumed outside their houses. The FAO’s nine food groups were used to classify these foods. Based on the number of food groups consumed, the participants were scored as being in the low, medium, or high range, with low being equal to or less than 3, medium being equal to or less than 4–5, and high being equal to or more than 6 (20).
After calculating the average daily consumption of fruits and vegetables, two groups were created, with the cut-off point being the mean consumption value of 0.95 servings/day (22).
The frequency of alcohol consumption was recorded, ranging from daily to less than once per month, based on the subjects’ consumption over the previous 12 months (23).
Discretionary foods include items such as soft drinks, cakes, Chocolate, and other high-sugar, low-nutrient food items that are also high in saturated fat, added sugars, and added salt (24).
The data collection tool was designed according to the WHO STEP-wise approach to non-communicable disease surveillance and the Food and Agriculture Organization assessment guidelines (25). The questionnaires regarding demographic data, behavioral assessments, and physical assessments in the survey were completed. Four trained clinical nurses, two men and two women, collected the data under the direction of a healthcare professional holding a Master of Public Health degree. Using a constant tension tape, the waist circumference was measured to the nearest 0.1 cm at the midpoint between the top of the iliac crest and the lower edge of the last perceptible rib. Similarly, the hip circumference was measured at the level of the greater trochanter, or the widest part of the gluteal muscle, recorded to the nearest 0.1 cm.
Before the data were collected, the questionnaire was written in English, translated into Amharic, and then back into English using a different translator to maintain the questionnaire’s consistency. Training for supervisors and data collectors lasted 2 days. Before the actual data collection, 5% (19) of the final sample size had the questionnaire pretested on bank workers.
EpiData version 4.4.2.0 was used to enter the obtained data, and the data were exported to STATA version 17 for analysis. Tables and figures were used to present the results of the computation of descriptive statistics. For each explanatory variable, univariate linear regression analysis was performed first, and multivariate linear regression analysis was then performed for variables with p-values less than 0.20. Multicollinearity in the multivariate linear regression model was assessed using the variance inflation factor (VIF) (values <10 for individual variables and <5 for the global value). The level of significance was set at a p-value of < 0.05.
A total of 345 participants were included in the analysis, with a 95.0% response rate. The mean age of the study participants was 34.4 ± 6.7 years. The majority of respondents (216) were in the age category of 30–44 years. Only 27 (7.8%) participants had a tertiary education, and 42 (12.2%) held managerial positions (Table 1).
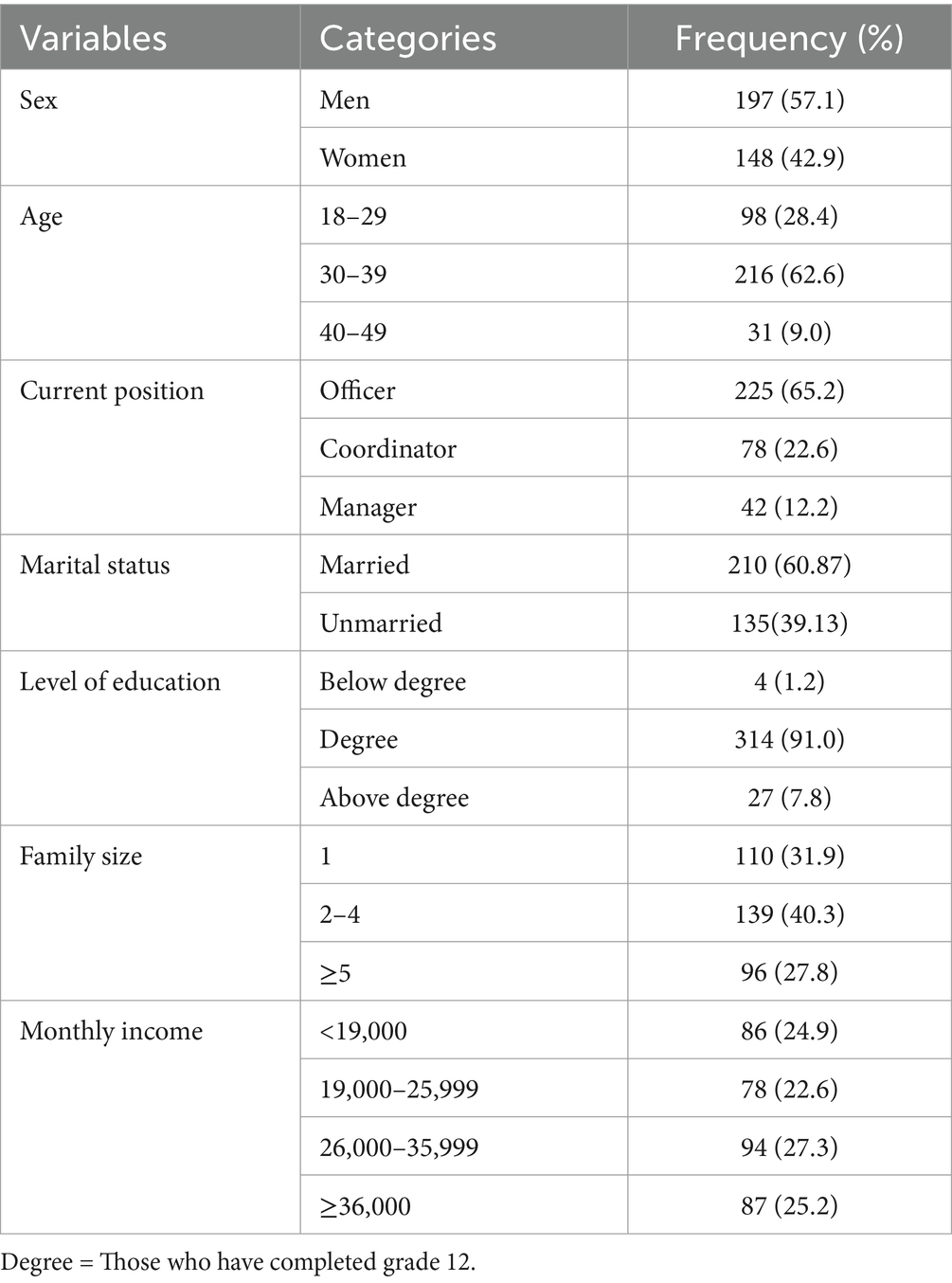
Table 1. Sociodemographic characteristics of the study participants among the bank employees in Northeast Ethiopia, 2023 (n = 345).
Nearly all (99.4%) participants were non-smokers, and 204 (59.1%) had never consumed alcohol. The mean metabolic equivalent of task (MET)-min ± standard deviation (SD) was 203 ± 211, with only 18 (5.2%) participants meeting the target of 600 MET-min/week. Nearly all (99%) participants were non-smokers and 92.7%of the participants slept for 8 h/day. Only 13 (3.8%) of the participants had been diagnosed with non-communicable diseases (NCDs) (Table 2).
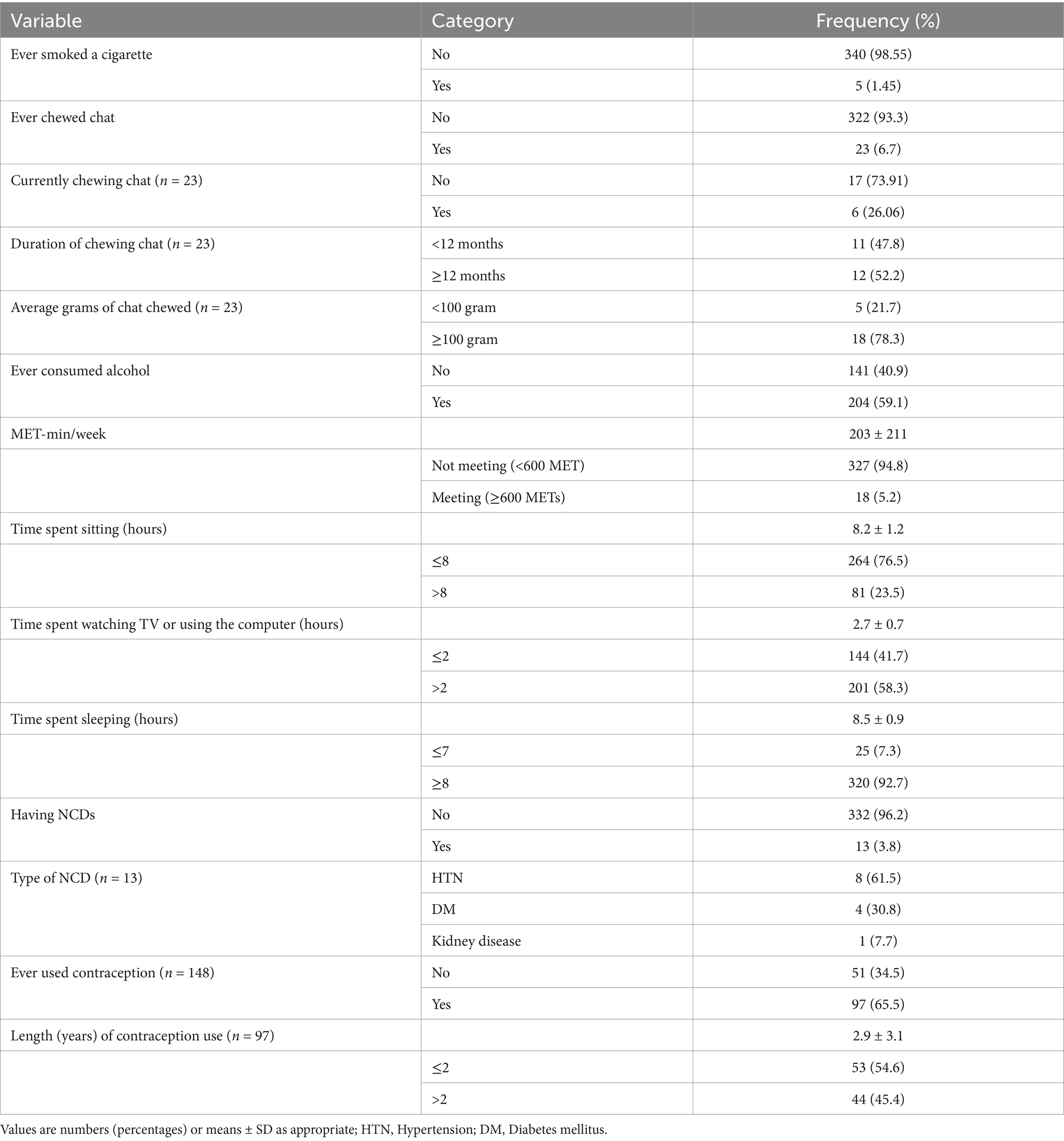
Table 2. Behavioral and personal health-related characteristics of the bank employees in Northeast Ethiopia, 2023 (n = 345).
The mean ± SD of the servings of fruit and vegetables consumed per day was 0.95 ± 0.69, with 57.1% of the participants exceeding the mean value. The majority, 286 (91.0%), of participants had a medium DDS value, and 94 (27.3%) reported being currently fasting (Table 3).
The overall mean ± SD of the waist circumference of the bank employees was 81.7 ± 6.8 cm. The mean WC was higher among men (82.4 ± 6.5 cm) than women (80.7 ± 7.2 cm). Accordingly, the overall mean ± SD of the WHR was 0.90 ± 0.05, with men having a value of 0.91 ± 0.04 and women having a value of 0.89 ± 0.05. The prevalence of central obesity was 57.7% (95% CI, 52.4–62.8%) (Figure 2).
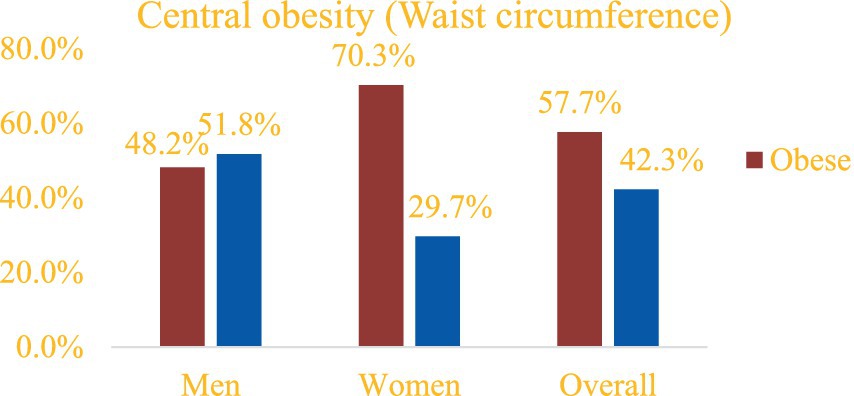
Figure 2. Prevalence of central obesity among bank employees in Northeast Ethiopia based on WC, 2023 (n = 345).
Similarly, the prevalence of central obesity based on the WHR was 62.0% (95% CI, 56.8–67.0%) (Figure 3).
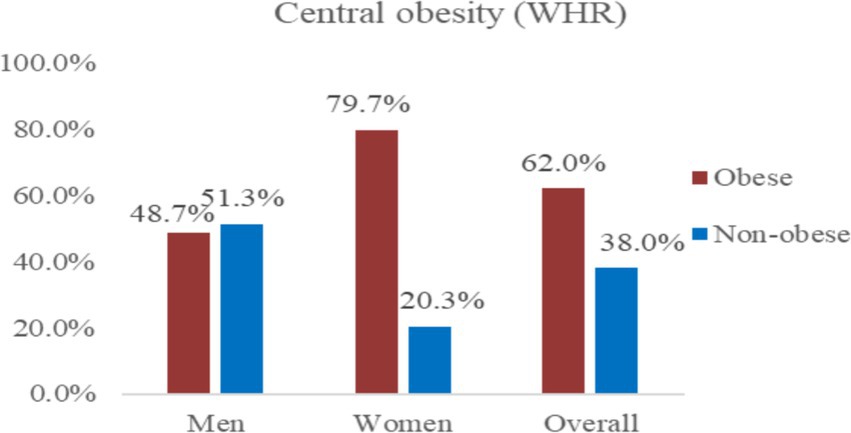
Figure 3. Prevalence of central obesity among bank employees in Northeast Ethiopia based on the WHR, 2023 (n = 345).
In the univariate linear regression analysis, age, sex, position, marital status, family income, khat chewing, discretionary calorie intake, time spent sleeping, having NCDs, number of meals eaten outside the home/week, meal-skipping habits, and MET-hours were considered. The variables with p-values less than 0.2 were then included in the multivariate linear regression analysis (Table 4).

Table 4. Univariate and multivariate linear regression of factors associated with waist circumference among bank employees in Northeast Ethiopia, 2023 (n = 345).
Thus, a one-year increase in age was associated with Intermediate increase of 0.2 cm (Standard error (SE): 0.1) in WC. In addition, the mean WC was 2.7 cm (SE:0.8) higher in married women compared to unmarried women. Similarly, the participants who consumed discretionary calories for 4 days/week had Intermediate WC increase of 1.7 cm (SE:0.8) compared to those who consumed discretionary calories for 3 days/week. Moreover, participants with NCDs had Intermediate WC value of 4.6 cm (SE:1.9) higher than their counterparts. A one-unit increase in MET-hours was associated with Intermediate decrease of 0.2 cm in the WC (SE:0.1).
Regarding the standardized beta coefficient, marital status and age had a greater effect on the waist circumference compared to the other significant variables. Accordingly, a change of one standard deviation in age resulted in a 0.18 standard deviation increase in the waist circumference. Similarly, on average, the married participants had a 0.19 standard deviation increase in the waist circumference compared to the unmarried participants.
The mean ± SD values of the WHR and WC were found to be 0.90 ± 0.05 cm and 82.4 ± 6.5 cm, respectively, based on the results. The prevalence of central obesity was 57.7% based on WC and 62.0% based on the WHR. The average waist circumference was 81.7 ± 6.8 cm (95% CI: 81.0–82.4 cm). Compared to women [80.7 ± 7.2 cm (95%CI, 79.5–81.9)], men reported higher WC values [82.4 ± 6.5 cm (95%CI, 81.5–83.3 cm)]. In comparison to studies conducted in Australia, Costa Rica, and Indonesia, the mean waist circumference (WC) in this study was lower. In Australia, the mean WC was 97.5 cm for men and 87.5 cm for women (26); in Costa Rica, it was 86.4 cm for women and 88.1 cm for men (27); and in Indonesia, it was 92.4 ± 1.3 cm for men and 89.5 ± 3.2 cm for women (28). This discrepancy may be attributed to the higher intake of processed foods, sugar-sweetened beverages, and sedentary lifestyle in developed countries (29, 30). However, a lower mean WC was reported in Mozambique, with values of 75.2 cm for women and 76.1 cm for men (31). This disparity could be explained by differences in the study time, study environment (urban vs. both urban and rural), and study design (community-based vs. institution-based). Furthermore, the main causes for the various WC reports are national variations in sociocultural, economic, and behavioral norms. Conversely, similar results were found in a survey conducted in Addis Ababa, Ethiopia (81.8 cm for men and 80.7 for women) (20). This could be a result of the research’s comparable metropolitan settings and similar study periods. Based on the study’s findings, each additional year of age was linked to an average increase of 0.2 cm. Scientific data indicate that aging is linked to an increase in abdominal obesity, with a mean rise of 2.43–2.68 cm in visceral adipose tissue (32). In addition, metabolic rate, muscle mass, and bone mass decrease as age increases (33, 34). These findings are supported by related similar studies from South Africa (35), Korea (36), Iran (37), Benin (38), Southwest Ethiopia (39), Western Ethiopia (40), Eastern Ethiopia (41), and Adama town, Ethiopia (42), which reported a positive association between age and central obesity.
Married participants had a significantly higher average waist circumference value than the unmarried participants. This result is in line with studies conducted in China among twins (43), Greece (44), Western Ethiopia (31), Eastern Ethiopia (20), and Adama town, Ethiopia (45). This may be due to changes in behavior and lifestyle that occur after marriage, which affect energy consumption and expenditure. Moreover, married individuals may engage in less daily activities and exercises as parents often have less time for such activities (46, 47). The level of physical activity, computed as MET-hours, had a significant association with WC. This finding is supported by studies conducted in Ethiopia (14), Sri Lanka (48), Benin (49), Iran (50), Southwest Ethiopia (39), and Eastern Ethiopia (41). This may be because physical activity helps in reducing belly fat and increases total energy expenditure. The most changeable aspect of energy expenditure is leisure-time physical activity, and workplace physical activity may lower the risk of obesity in adults (51).
The study found a strong correlation between waist circumference and discretionary calorie intake each week. This result is consistent with other research findings, which reported that adults who consumed fewer discretionary calories had noticeably smaller waist circumference compared to adults who consumed more calories (52). This may be because discretionary foods are high in calories, low in nutrients, and high in saturated fat, added sugars, added salt, and cholesterol (48, 53). In addition, compared to their counterparts, individuals with NCDs had a noticeably higher average WC value (54, 55).
The study addresses an important gap by investigating central obesity in a specific occupational group (bank employees) in Ethiopia, a setting with limited prior research. The inclusion of diverse variables (e.g., dietary diversity, physical activity, and discretionary calorie intake) allowed for a robust multivariate analysis of central obesity determinants. The lack of detailed hip circumference analysis may have diminished the validity of the WHR findings. In addition, establishing causal inference was not possible due to the cross-sectional nature of the study. Furthermore, causal inferences could not be established due to the cross-sectional design of the study. Furthermore, height and weight data were not collected for the study group, allowing us to assess the limits of their influence on our findings.
Because bank personnel had a high mean waist circumference value, almost half of the participants were classified as centrally obese. Significant variables that influenced the waist circumference included age, marital status, discretionary calorie intake, the presence of NCDs, and MET-hours. These results highlight the necessity of implementing initiatives specifically designed to prevent non-communicable diseases by encouraging physical activity, promoting exercise during leisure time, building physical fitness facilities, and raising awareness of the importance of a healthy diet. All of these efforts can contribute to reducing the burden of obesity in the general population.
The original contributions presented in the study are included in the article and further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Ethical clearance and approval were obtained from Wollo University College of Medicine and Health Sciences ethical review committee. Official letters were written to each selected bank and permission was obtained from the responsible managers. Oral informed consent was obtained from study participant and confidentiality and anonymity was secured. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
WY: Methodology, Writing – review & editing, Investigation, Supervision, Writing – original draft. LA: Data curation, Methodology, Writing – review & editing. FG: Methodology, Writing – original draft. TA: Methodology, Writing – review & editing. AM: Investigation, Methodology, Writing – original draft. FY: Formal analysis, Methodology, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to thank the Ethical Review Committee of Wollo University, School of Public Health, for their ethical evaluation and approval. The authors appreciate the respective study institutions and all respondents, data collectors, and supervisors, for providing valuable time and necessary information for this research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
BMI, Body mass index; CAD, Cerebrovascular disease; DM, Diabetes mellitus; METs, Metabolic equivalent of tasks; NCD, Non-communicable diseases; WC, Waist circumference; WHR, Waist to hip ratio.
1. Yoo, MC, Won, CW, and Soh, Y. Association of high body mass index, waist circumference, and body fat percentage with sarcopenia in older women. BMC Geriatr. (2022) 22:937. doi: 10.1186/s12877-022-03643-x
2. Dai, H, Alsalhe, TA, Chalghaf, N, Riccò, M, Bragazzi, NL, and Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the global burden of disease study. PLoS Med. (2020) 17:e1003198. doi: 10.1371/journal.pmed.1003198
3. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III): the program. Circulation. (2002) 285:2486–97. doi: 10.1001/jama.285.19.2486
4. Alberti, KG, Eckel, RH, Grundy, SM, Zimmet, PZ, Cleeman, JI, Donato, KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. (2009) 120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644
5. Sinaga, M, Worku, M, Yemane, T, Tegene, E, Wakayo, T, Girma, T, et al. Optimal cut-off for obesity and markers of metabolic syndrome for Ethiopian adults. Nutr J. (2018) 17:1–12. doi: 10.1186/s12937-018-0416-0
6. Albuquerque, D, Nóbrega, C, Manco, L, and Padez, C. The contribution of genetics and environment to obesity. Br Med Bull. (2017) 123:159–73. doi: 10.1093/bmb/ldx022
7. Wong, MC, Huang, J, Wang, J, Chan, PS, Lok, V, Chen, X, et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. (2020) 35:673–83. doi: 10.1007/s10654-020-00650-3
8. Seidell, JC, and Halberstadt, J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab. (2015) 66:7–12. doi: 10.1159/000375143
9. Li, Z, Shi, J, Li, N, Wang, M, Jin, Y, and Zheng, Z-j. Temporal trends in the burden of non-communicable diseases in countries with the highest malaria burden, 1990–2019: evaluating the double burden of non-communicable and communicable diseases in epidemiological transition. Glob Health. (2022) 18:90. doi: 10.1186/s12992-022-00882-w
10. Balkau, B, Deanfield, JE, Després, J-P, Bassand, J-P, Fox, K, Smith, SC, et al. Idea: a study of waist circumference, cardiovascular disease and diabetes in 168,000 primary care patients in 63 countries. Circulation. (2007) 116:1942–51. doi: 10.1161/CIRCULATIONAHA.106.676379
11. Pischon, T, Boeing, H, Hoffmann, K, Bergmann, M, Schulze, MB, Overvad, K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. (2008) 359:2105–20. doi: 10.1056/NEJMoa0801891
12. Tesfaye, TS, Zeleke, TM, Alemu, W, Argaw, D, and Bedane, TK. Dietary diversity and physical activity as risk factors of abdominal obesity among adults in Dilla town, Ethiopia. PLoS One. (2020) 15:e0236671. doi: 10.1371/journal.pone.0236671
13. Kassie, AM, Abate, BB, and Kassaw, MW. Prevalence of overweight/obesity among the adult population in Ethiopia: a systematic review and meta-analysis. BMJ Open. (2020) 10:e039200. doi: 10.1136/bmjopen-2020-039200
14. Tegegne, KD, Wagaw, GB, Gebeyehu, NA, Yirdaw, LT, Shewangashaw, NE, Mekonen, NA, et al. Prevalence of central obesity and associated factors in Ethiopia: a systematic review and meta-analysis. Front Endocrinol. (2022) 13:983180. doi: 10.3389/fendo.2022.983180
15. Alamnia, TT, Sargent, GM, and Kelly, M. Patterns of non-communicable disease, multimorbidity, and population awareness in Bahir Dar, Northwest Ethiopia: a cross-sectional study. Int J Gen Med. (2023) 16:3013–31. doi: 10.2147/IJGM.S421749
16. Hu, F, Liu, Y, and Willett, W. Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev. (2011) 12:552–9. doi: 10.1111/j.1467-789X.2011.00863.x
17. Molla, MD, Wolde, HF, and Atnafu, A. Magnitude of central obesity and its associated factors among adults in urban areas of Northwest Ethiopia. Diabetes Metab Syndr Obes. (2020) 13:4169–78. doi: 10.2147/DMSO.S279837
18. Zubery, D, Kimiywe, J, and Martin, HD. Prevalence of overweight and obesity, and its associated factors among health-care workers, teachers, and bankers in Arusha City, Tanzania. Diabetes Metab Syndr Obes. (2021) 14:455–65. doi: 10.2147/DMSO.S283595
19. Abebe, F. Determinants of income inequality in urban Ethiopia: a study of south wollo administrative zone, Amhara national and regional state. Int J Appl Res. (2016) 2:550–63.
20. Gebremedhin, S, Mekonene, M, Hagos, S, Baye, K, Shikur, B, Berhane, A, et al. Association between normal-weight obesity and cardiometabolic risk factors among adults in Addis Ababa, Ethiopia. Sci Rep. (2023) 13:22772. doi: 10.1038/s41598-023-49039-8
21. Teklemariam, W. Magnitude of central obesity and associated factors among adults in Addis Ababa Ethiopia. (2020).
22. Olaya, B, Essau, CA, Moneta, MV, Lara, E, Miret, M, Martín-María, N, et al. Fruit and vegetable consumption and potential moderators associated with all-cause mortality in a representative sample of Spanish older adults. Nutrients. (2019) 11:1794. doi: 10.3390/nu11081794
23. Organization WH. WHO guidelines on physical activity and sedentary behaviour World Health Organization. Geneva, Switzerland: WHO guidelines on physical activity and sedentary behaviour. (2020).
24. National Health and Medical Research Council. Australian dietary guidelines National Health and Medical Research Council, National Resource Management Ministerial Council. Canberra, Australia: Australian Dietary Guidelines. (2013).
25. Mwenda, V, Mwangi, M, Nyanjau, L, Gichu, M, Kyobutungi, C, and Kibachio, J. Dietary risk factors for non-communicable diseases in Kenya: findings of the STEPS survey, 2015. BMC Public Health. (2018) 18:1–8. doi: 10.1186/s12889-018-6060-y
27. Aráuz-Hernández, AG, Guzmán-Padilla, S, and Roselló-Araya, M. Waist circumference as indicator of cardiovascular risk. Acta Med Costarric. (2013) 55:122–7.
28. Astuti, Y, and Jenie, IM. Correlation of body mass index on waist circumference and blood pressure. Int J Public Health. (2020) 9:373–8. doi: 10.11591/ijphs.v9i4.20443
29. Swinburn, BA, Sacks, G, Hall, KD, McPherson, K, Finegood, DT, Moodie, ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. (2011) 378:804–14. doi: 10.1016/S0140-6736(11)60813-1
30. Malik, VS, Popkin, BM, Bray, GA, Després, J-P, Willett, WC, and Hu, FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. (2010) 33:2477–83. doi: 10.2337/dc10-1079
31. Gomes, A, Damasceno, A, Azevedo, A, Prista, A, Silva-Matos, C, Saranga, S, et al. Body mass index and waist circumference in Mozambique: urban/rural gap during epidemiological transition. Obes Rev. (2010) 11:627–34. doi: 10.1111/j.1467-789X.2010.00739.x
32. Boneva-Asiova, Z, and Boyanov, M. Age-related changes of body composition and abdominal adipose tissue assessed by bio-electrical impedance analysis and computed tomography. Endocrinol Nutr. (2011) 58:472–7. doi: 10.1016/j.endonu.2011.07.004
33. St-Onge, M-P, and Gallagher, D. Body composition changes with aging: the cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition. (2010) 26:152–5. doi: 10.1016/j.nut.2009.07.004
34. Jiang, Y, Zhang, Y, Jin, M, Gu, Z, Pei, Y, and Meng, P. Aged-related changes in body composition and association between body composition with bone mass density by body mass index in Chinese Han men over 50-year-old. PLoS One. (2015) 10:e0130400. doi: 10.1371/journal.pone.0130400
35. Owolabi, EO, Ter Goon, D, and Adeniyi, OV. Central obesity and normal-weight central obesity among adults attending healthcare facilities in Buffalo City metropolitan municipality, South Africa: a cross-sectional study. J Health Popul Nutr. (2017) 36:1–10. doi: 10.1186/s41043-017-0133-x
36. Kim, HY, Kim, JK, Shin, GG, Han, JA, and Kim, JW. Association between abdominal obesity and cardiovascular risk factors in adults with normal body mass index: based on the sixth Korea National Health and nutrition examination survey. J Obes Metab Syndr. (2019) 28:262–70. doi: 10.7570/jomes.2019.28.4.262
37. Tabrizi, JS, Sadeghi-Bazargani, H, Farahbakhsh, M, Nikniaz, L, and Nikniaz, Z. Prevalence and associated factors of overweight or obesity and abdominal obesity in Iranian population: a population-based study of northwestern Iran. Iran J Public Health. (2018) 47:1583–92. doi: 10.18502/ijph.v47i11.1465
38. Gbary, AR, Kpozehouen, A, Houehanou, YC, Djrolo, F, Amoussou, MP, Tchabi, Y, et al. Prevalence and risk factors of overweight and obesity: findings from a cross-sectional community-based survey in Benin. Glob Epidemic Obes. (2014) 2:3. doi: 10.7243/2052-5966-2-3
39. Tefera, W, Shuremu, M, Tadelle, A, Abdissa, D, and Banjaw, Z. Magnitude of central obesity and associated factors among adults working in government offices in Bedele town, Buno Bedele zone, Southwest Ethiopia. SAGE Open Med. (2022) 10:20503121221105993. doi: 10.1177/20503121221105993
40. Biru, B, Tamiru, D, Taye, A, and Regassa, FB. Central obesity and its predictors among adults in Nekemte town, West Ethiopia. SAGE Open Med. (2021) 9:20503121211054988. doi: 10.1177/20503121211054988
41. Israel, E, Hassen, K, Markos, M, Wolde, K, and Hawulte, B. Central obesity and associated factors among urban adults in Dire Dawa administrative city, Eastern Ethiopia. Diabetes Metab Syndr Obes. (2022) 15:601–14. doi: 10.2147/DMSO.S348098
42. Getahun, MS, Deybasso, HA, Komicha, MA, and Gurara, AM. Magnitude of central obesity and associated factors among adult patients attending public health facilities in Adama town, Oromia region, Ethiopia, 2022. J Health Popul Nutr. (2023) 42:57. doi: 10.1186/s41043-023-00397-z
43. Zhang, P, Wang, R, Gao, C, Jiang, L, Lv, X, Song, Y, et al. Prevalence of central obesity among adults with normal BMI and its association with metabolic diseases in Northeast China. PLoS One. (2016) 11:e0160402. doi: 10.1371/journal.pone.0160402
44. Sousa, TF, Nahas, MV, Silva, DAS, Del Duca, GF, and Peres, MA. Factors associated with central obesity in adults from Florianópolis, Santa Catarina: a population based-study. Rev Bras Epidemiol. (2011) 14:296–309. doi: 10.1590/S1415-790X2011000200011
45. Omar, SM, Taha, Z, Hassan, AA, Al-Wutayd, O, and Adam, I. Prevalence and factors associated with overweight and central obesity among adults in the eastern Sudan. PLoS One. (2020) 15:e0232624. doi: 10.1371/journal.pone.0232624
46. Janghorbani, M, Amini, M, Rezvanian, H, Mm, G, Ar, D, Alikhani, S, et al. Association of body mass index and abdominal obesity with marital status in adults. Arch Iran Med. (2008) 11:3.. doi: 10.47176/aim.11.3.274
47. Cisse, K, Samadoulougou, S, Ouedraogo, M, Kouanda, S, and Kirakoya-Samadoulougou, F. Prevalence of abdominal obesity and its association with cardiovascular risk among the adult population in Burkina Faso: findings from a nationwide cross-sectional study. BMJ Open. (2021) 11:e049496. doi: 10.1136/bmjopen-2021-049496
48. Rathnayake, KM, Roopasingam, T, and Dibley, MJ. High carbohydrate diet and physical inactivity associated with central obesity among premenopausal housewives in Sri Lanka. BMC Res Notes. (2014) 7:564. doi: 10.1186/1756-0500-7-564
49. Ntandou, G, Delisle, H, Agueh, V, and Fayomi, B. Abdominal obesity explains the positive rural-urban gradient in the prevalence of the metabolic syndrome in Benin. West Africa Nutr Res. (2009) 29:180–9. doi: 10.1016/j.nutres.2009.02.001
50. Dalvand, S, Koohpayehzadeh, J, Karimlou, M, Asgari, F, Rafei, A, Seifi, B, et al. Assessing factors related to waist circumference and obesity: application of a latent variable model. J Environ Public Health. (2015) 2015:1–9. doi: 10.1155/2015/893198
51. Jakicic, JM, and Davis, KK. Obesity and physical activity. Psychiatr Clin North Am. (2011) 34:829–40. doi: 10.1016/j.psc.2011.08.009
52. Sumardilah, DS, Hasan, A, and Gunawan, TA. Factors affecting the central obesity (pot belly) risk in state attorney office. J Med Sci Res. (2018) 6, 3–8. doi: 10.18535/jmscr/v6i3.127
53. Astiarani, Y, Kedang, MG, Fitriah, N, and Chandra, FA. Prevalence and determinants of central obesity at urban slum dwellers in North Jakarta. Jurnal Ilmu Kesehatan Masyarakat. (2022) 13:14–25. doi: 10.26553/jikm.2022.13.1.14-25
54. Tekalegn, Y, Solomon, D, Sahiledengle, B, Assefa, T, Negash, W, Tahir, A, et al. Prevalence of central obesity and its associated risk factors among adults in Southeast Ethiopia: a community-based cross-sectional study. PLoS One. (2022) 17:e0265107. doi: 10.1371/journal.pone.0265107
55. WHO. Overweight and obesity. Available at: https://www.paho.org/en/enlace/overweight-and-obesity (2023).
Keywords: waist circumference, central obesity, factors, non-communicable disease, Eastern Ethiopia
Citation: Yimer W, Asmare L, Gebeyehu FB, Alemu T, Mehamed A and Yeshanew Ayele F (2025) Factors influencing waist circumference among urban bank employees in Northeast Ethiopia: a cross-sectional study. Front. Nutr. 11:1414930. doi: 10.3389/fnut.2024.1414930
Received: 09 April 2024; Accepted: 30 December 2024;
Published: 22 January 2025.
Edited by:
Emmanuel Cohen, UMR7206 Eco Anthropologie et Ethnobiologie (EAE), FranceReviewed by:
Jayashree Arcot, University of New South Wales, AustraliaCopyright © 2025 Yimer, Asmare, Gebeyehu, Alemu, Mehamed and Yeshanew Ayele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lakew Asmare, bGFrZXd0MDcxOTgxQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.