
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 05 June 2024
Sec. Nutritional Epidemiology
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1407454
Background: Previous findings imply a potential positive association between BMI and all-cause mortality in individuals with psoriasis, yet direct evidence remains absent. This study aimed to fill this gap.
Methods: We utilized data from the National Health and Nutrition Examination Survey (NHANES) for the periods 2003–2006 and 2009–2014. Participants’ BMI was categorized as lean (<25), overweight (25 ≤ BMI < 30), and obese (BMI ≥ 30). Psoriasis status was determined through self-reporting. The main outcome measured was all-cause mortality up to December 2019. We accounted for multiple covariates, such as sociodemographic factors and histories of smoking and alcohol consumption. Our statistical analyses mainly included Kaplan–Meier survival analysis, Restricted Cubic Spline (RCS) and Multivariate Cox Regression (MCR). We also applied propensity score matching (PSM) to verify the robustness of our findings.
Results: Among 22,876 participants, 618 (2.70%) reported a history of psoriasis. An overall effect from the MCR analysis showed that, among individuals with psoriasis, a higher baseline BMI was independently associated with an increased risk of all-cause mortality, noting a 5.5% rise in mortality risk per BMI unit [hazard ratio (HR) = 1.055, 95% CI: 1.004–1.110, p = 0.035]. This significant relationship persisted after PSM. A statistically significant positive correlation was consistent among males, smokers, and individuals younger than 60. However, no such association was found in individuals without a history of psoriasis. Additionally, no significant difference in mortality risk was found between lean and overweight groups with psoriasis, according to the RCS regression and stratified analysis.
Conclusion: Our findings indicated a trend that, higher BMIs significantly correlated with increased risks of all-cause mortality in people with psoriasis, particularly among obese ones. However, the impact of being overweight on this relationship remains underexplored. Moreover, the necessity to employ alternative metrics beyond BMI for body fat assessment to further investigate these associations is critical.
Psoriasis, a chronic and immune-mediated inflammatory skin disorder with no cure, is characterized by red, scaly plaques. These plaques most frequently appear on the elbows, knees, scalp, and lower back, but can affect any skin surface (1). It impacts millions worldwide, with a notably higher prevalence in Western countries characterized by older populations and higher income levels (2). The rate of psoriasis varies significantly by region, from 0.14% in East Asia to 1.99% in Australasia, with also substantial prevalence in Western Europe (1.92%), Central Europe (1.83%), and North America (1.50%) (1). Considered now as a serious non-communicable systemic disease, psoriasis is linked with a wide range of co-morbidities, including psychological, metabolic, arthritic, and cardiovascular issues (1). Prior research has indicated that psoriasis can be independently linked to a higher risk of mortality (3), presenting complex challenges for both dermatological and systemic health care, especially in individuals with more severe forms of the disease (1, 2).
The relationship between psoriasis and obesity has been a subject of increasing interest within the medical research community (4–6), given the growing evidence suggesting that obesity, as a prevalent and potentially modifiable risk factor, can exacerbate the clinical trajectory of psoriasis and vice versa (4, 6, 7). It was found that the inflammatory pathways shared between obesity and psoriasis, which involve cytokines such as TNF-α and IL-6, may suggest a biological plausibility for their bidirectional correlations (8–10). Both conditions are associated with a heightened risk of mortality (3, 11).
Body mass index (BMI) serves as a convenient and reliable approach for evaluating obesity in most people most of the time (12). Aune et al. identified a dose–response relationship between BMI and the risk of psoriasis onset, noting the lowest risk at a BMI of 20 and a significant risk increase starting from a BMI of 22.5–24 (13, 14). However, the association between BMI and mortality remains elusive. A US retrospective cohort study, spanning recent two decades, revealed a U-shaped relationship relating weight to mortality, indicating highest death rates at two extreme sides of BMI. Interestingly, being overweight (BMI 25–30) did not correlate with increased mortality (15). Contrarily, a meta-analysis suggested that both overweight and obesity are linked to a higher risk of all-cause mortality (16). Tobias et al. provided additional evidence to support a strong association between escalating BMI and increased mortality starting from a BMI of 25 kg/m2 (17). Despite the well-documented relationship between psoriasis, obesity, and increased risks of morbidity and mortality, the role of BMI, especially in the categories considered underweight or overweight, in affecting mortality is still unclear. The mediating effects of factors such as smoking, income and educational level can further complicate this association (18, 19).
A study suggested that higher BMIs are associated with more severe psoriasis among individuals who are lean or overweight (20). Another study showed that more severe psoriasis could be related to an increased risk of mortality (21). Based on these prior findings, one may speculate that, among non-obese individuals with psoriasis, a lower BMI can be associated with a reduced psoriasis severity, and thus a reduced risk of mortality. However, no current study provides direct evidence about this. Additionally, the influence of potentially confounding factors such as sex, age, previous smoking history, and comorbidities on such relationship is uncertain.
The National Health and Nutrition Examination Survey (NHANES) can provide invaluable resource for studying these associations, based on a large, nationally representative sample of the U.S. population. Therefore, through analyzing its data, we aimed to provide evidence about the impact of BMI on the risk of all-cause mortality in individuals with a history of psoriasis. We also extended our investigation to ascertain if this link persists in those without psoriasis. In addition, we aimed scrutinize the influence of various factors, such as age, sex, prior smoking history, on this critical association, aiming to inform clinical management and intervention strategies effectively.
The NHANES database, an ongoing program conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC), offers information into the nutritional and health statuses of adults and children in the U.S. through population estimates. This survey employs a stratified, multistage probability design for selecting a representative sample of the U.S. population, gathering data through personal structured interviews at participants’ homes, health examinations at mobile examination centers, and laboratory analyses of specimens (22). The protocols for NHANES received approval from the Research Ethics Review Board at NCHS (23). Informed written consent was obtained from all participants involved in NHANES. The datasets produced and analyzed in this study can be accessed on the NHANES website.1
In the current study, we downloaded and analyzed the continuous NHANES data from 2003–2006 and 2009–2014, which encompass extensive details, including BMI values and the presence of psoriasis. The 2007–2008 NHANES cycle was not included due to the lack of psoriasis-related data.
Participants’ BMI baseline data were determined by the formula: weight/height2 (kg/m2). The height and weight of participants were measured by professional surveyors. They were categorized into three groups based on their BMI: a lean group (BMI < 25), an overweight group (25 ≤ BMI < 30), and an obese group (BMI ≥ 30) (24). Follow-up data regarding BMI among these participants were not available.
All participants provided self-reported information on their dermatological conditions related to psoriasis. History of psoriasis was identified though a positive response to the question, “Have you ever been told by a health care provider that you have psoriasis?” The severity of psoriasis was assessed based on responses to the question, “What is the current severity of your psoriasis?” Participants could indicate their condition as (1). little or no psoriasis; (2). only a few patches; (3). scattered patches; or (4). extensive psoriasis.
This study’s main outcome was all-cause mortality, which includes all deaths occurring during the follow-up period extending through December 2019. Confirmation of deaths was obtained through linkage with the National Death Index records (25).
We extracted the data pertaining participants’ sociodemographic details, as well as their histories of smoking and alcohol use, the severity of their current psoriasis, and the presence of diabetes, hypertension, and dyslipidemia. Individuals who had smoked fewer than 100 cigarettes in their lifetime were categorized as non-smokers, whereas those who had smoked 100 or more cigarettes were classified as smokers (22). Alcohol consumers were identified in participants who reported consuming at least 12 alcoholic drinks in their lifetime (26). We subjectively categorized the severity of current psoriasis among participants, including none (i.e., indicating little or no psoriasis), mild (i.e., indicating only a few patches), moderate (i.e., indicating scattered patches), and severe (i.e., indicating extensive psoriasis). Diabetes was determined by a glycosylated hemoglobin level of 6.5% or higher, a self-reported physician diagnosis, or the use of insulin (27). Hypertension was identified by a blood pressure reading of 140/90 mmHg or higher, a self-reported physician diagnosis, or the use of medication for hypertension (28). Dyslipidemia was defined by a serum total cholesterol level greater than 6.2 mmol/L or a self-reported physician diagnosis of dyslipidemia (29).
Continuous variables were reported as mean ± SD (standard deviation) or median and interquartile ranges, while categorical variables were presented as percentages. To compare continuous variables, we utilized the t-test or Mann–Whitney U test as appropriate. Categorical variables were compared using the chi-square test or Fisher’s exact test. Kaplan–Meier method was used to analyze survival probability of psoriatic individuals over time, based on BMI category. Restricted cubic spline (RCS) regression was employed to investigate the non-linear association between BMI (as a continuous variable) and all-cause mortality risk among psoriatic individuals. Multivariate Cox proportional hazards regression was also employed, in order to estimate hazard ratios (HRs) for all-cause mortality in relation to BMI in individuals with or without psoriasis (the latter one serves as an extra analysis), as well as for psoriatic severity based on BMI among psoriatic individuals. Stratified analyses were performed based on sex (men or women), age (≤60 or > 60 years old), and previous smoking status to explore their potential modifying effects, which were assessed by testing multiplicative interaction terms. Fisher’s exact test was employed to analyze the differing mortality rates among individuals with mild psoriasis and those with moderate-to-severe psoriasis based on BMI category groups.
In multivariate Cox regression models, we developed two statistical models for analyses. Model 1 adjusted for age (as a continuous variable), sex (male or female), and race/ethnicity (non-Hispanic White or other). Model 2 included adjustments for age, sex, race/ethnicity, education level (less than high school, high school or equivalent, or college or above), family income-to-poverty ratio (PIR) (as a continuous variable), previous alcohol consumption, previous smoking status, and the presence of diabetes, hypertension, dyslipidemia, and current severity of psoriasis (mild or moderate-to-severe).
Sensitivity analyses including several inclusion criteria for psoriatic participants were conducted to assess the stability of our results. Firstly, to mitigate potential biases arising from underlying confounding factors that may accelerate the dying process of psoriatic participants, those who died within the first 2 years of follow-up were excluded (n = 12). Secondly, we used the propensity score matching (PSM) approach to balance baseline characteristics between obese (BMI ≥ 30) and non-obese (BMI < 30) groups at a 1:2 ratio. The predefined factors employed for these adjustments included: age, sex, race/ethnicity, educational level, PIR, previous alcohol consumption, previous smoking status, the presence of hypertension, diabetes and dyslipidemia, and the current severity of psoriasis. Finally, we conducted a third sensitivity analysis based on the combined inclusion criteria from the previous two analyses.
All statistical analyses were conducted using IBM SPSS Statistics 27 and R software version 4.3.1. A two-sided p-value of <0.05 was deemed to indicate statistical significance.
A total of 22,876 individuals, with or without a history of psoriasis, aged 20 years old and above were included in the final analysis. 618 (2.7%) were identified as having a history of psoriasis (see Figure 1 for participant selection details). The lowest recorded baseline BMI among all participants was 16.56, and the highest was 63. Among individuals with histories of psoriasis, only 3 participants had a baseline BMI below 18.5, and 26 participants had a baseline BMI exceeding 45.
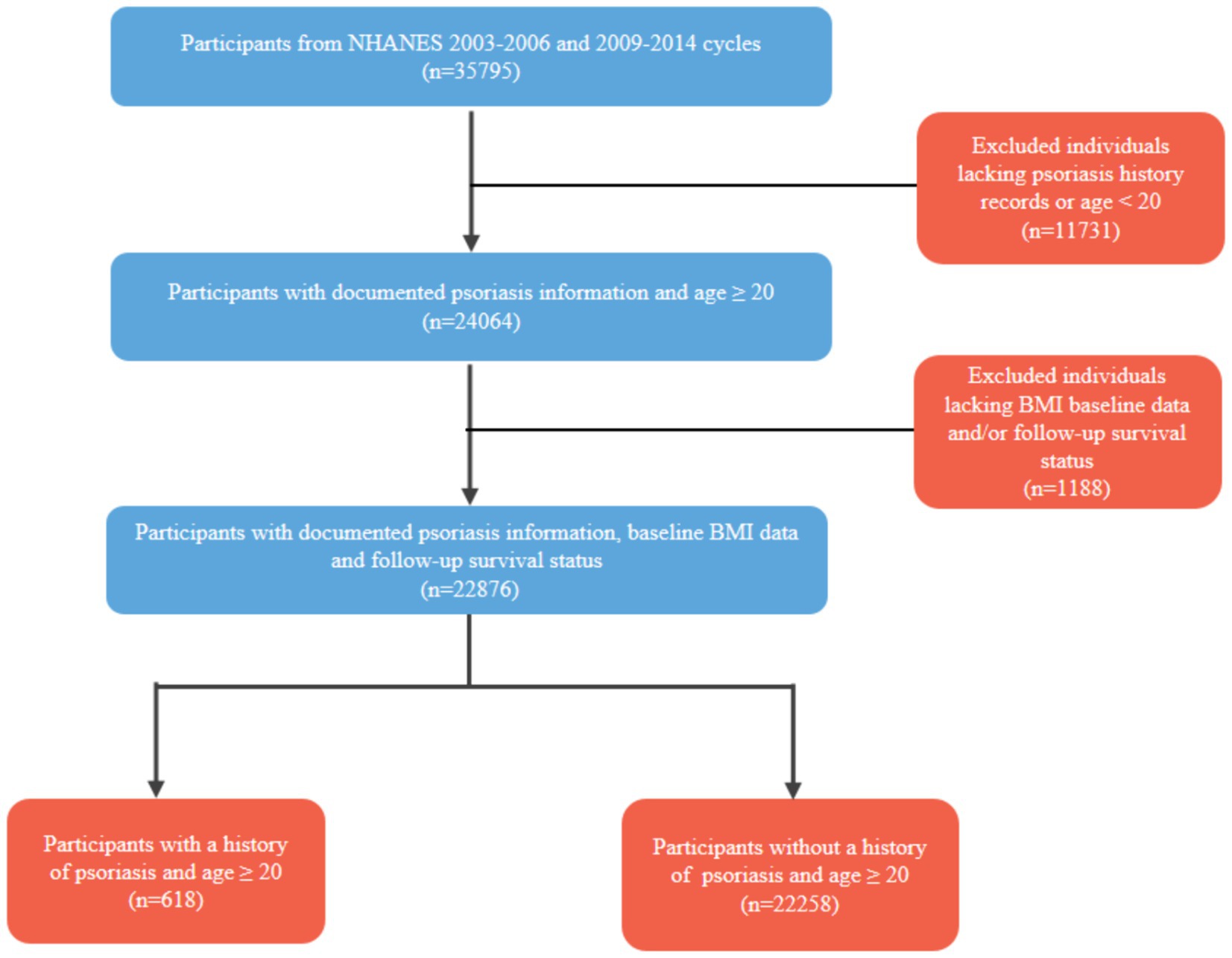
Figure 1. Flow-chart of participant selection process. BMI, body mass index; NHANES, National Health and Nutrition Examination Survey.
Compared to those without histories of psoriasis, individuals with histories of the condition were generally older, predominantly non-Hispanic White, had higher BMI levels, and were more likely to smoke (refer to Supplementary Table S1, all p-values <0.05). The distribution of these characteristics among participants with psoriasis, based on BMI categories, was detailed in Table 1. Notably, the overweight group (25 ≤ BMI < 30) had the highest percentages of male participants, non-Hispanic Whites, and individuals with the highest Poverty Income Ratio (PIR), with significant differences observed (p < 0.05). However, no significant differences were noted in other characteristics across BMI groups (p > 0.05). Furthermore, Supplementary Tables S2, S3 display the baseline characteristics of individuals with psoriasis, categorized by obesity status, after sole Propensity Score Matching (PSM), and after PSM combined with the exclusion of participants who died within the first two years of follow-up. In these PSM data, no statistically significant differences were found between obese and non-obese groups with histories of psoriasis. In addition, Supplementary Table S4 shows that, in the psoriatic individuals, among various causes of death, the incidence of cardiovascular-related death events was significantly higher in the obese group compared to the lean and overweight groups (p = 0.005).
The initial analysis explored the impact of BMI categories (i.e., lean, overweight, and obese) on all-cause mortality among those with a history of psoriasis. Out of 2,098 deceased participants over a median follow-up of 8.9 years (IQR = 6.4), 81 (3.9%) had psoriasis, and 2,017 (96.1%) did not.
After adjusting for multiple covariates, the stratified analysis revealed a significantly higher all-cause mortality in the obese group (BMI ≥ 30) (HR: 4.239, 95% CI: 1.442–12.458, p = 0.020), but not in the overweight group (HR: 0.238, 95% CI: 0.052–1.092), compared to the lean group (see Table 2). The obese group was also significantly associated with higher mortality risks in the subgroups of men, women, age ≤ 60, age > 60, smokers, non-smokers, individuals with mild psoriasis, and individuals with moderate-to-severe psoriasis. However, insignificant differences were observed in all these subgroups between the lean and overweight groups. Additionally, no significant interactions were observed in the stratified analyses (all p > 0.05).
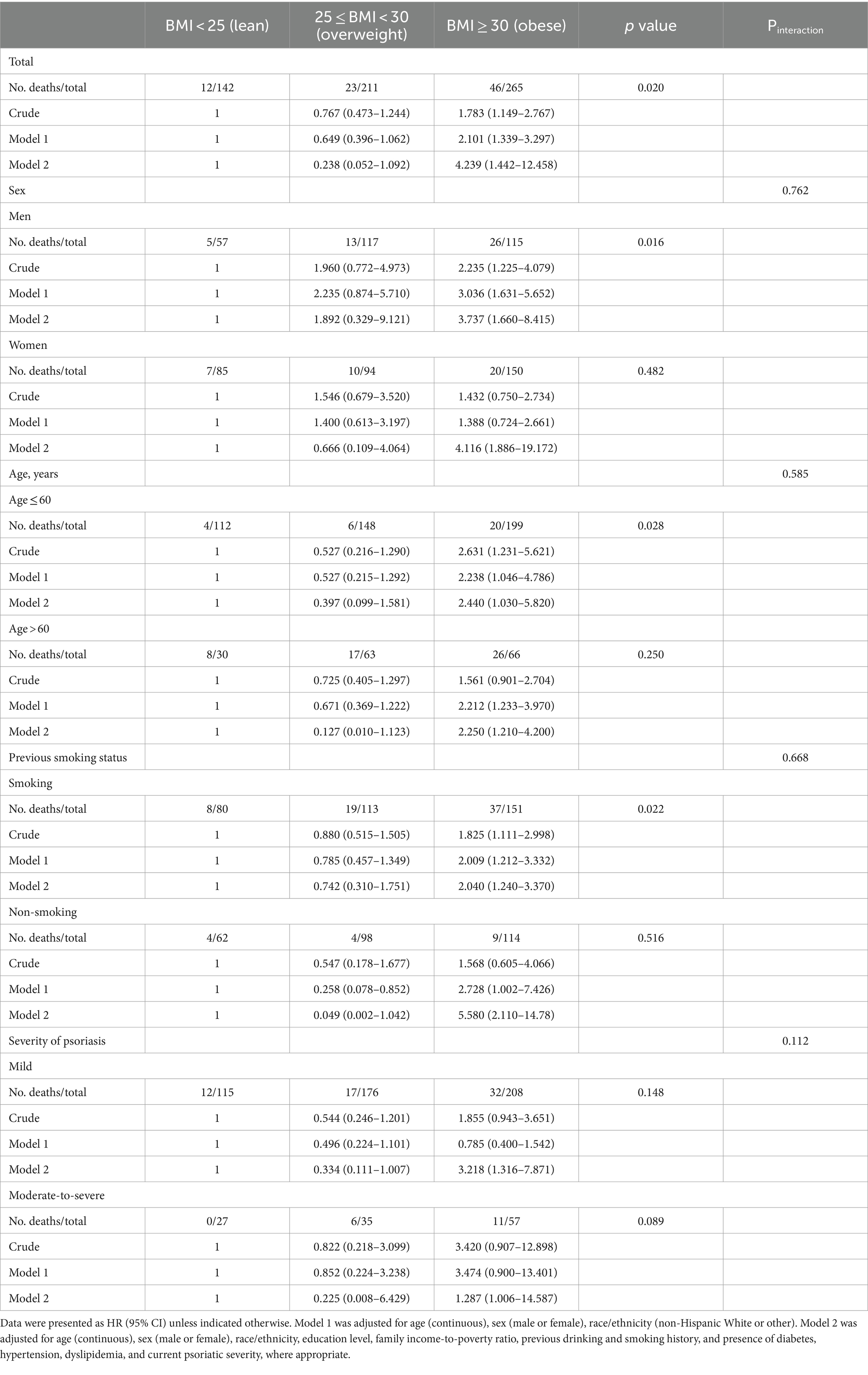
Table 2. Stratified analysis of the risk of all-cause mortality based on BMI category of psoriatic individuals.
The Kaplan–Meier survival analysis curves suggested significant differences in mortality rates across BMI groups among psoriatic individuals by the end of the follow-up period (Lean: 8.4% vs. Overweight: 10.9% vs. Obese: 17.4%, log-rank p = 0.026, see Supplementary Figure S1A). This pattern was also significant among participants aged ≤60 (Lean: 3.5% vs. Overweight: 4.1% vs. Obese: 16.8%, log-rank p = 0.033, see Supplementary Figure S1C), and those considered as smokers (Lean: 10.0% vs. Overweight: 16.8% vs. Obese: 24.5%, log-rank p = 0.024, see Supplementary Figure S1D), but not among those aged >60 (log-rank p = 0.276, see Supplementary Figure S1B) or those considered as non-smokers (log-rank p = 0.534, see Supplementary Figure S1E).
Multivariate Cox regression analyses indicated that a higher BMI was associated with an increased risk of all-cause mortality in individuals with a history of psoriasis, even after adjusting for age, sex, race/ethnicity, education level, family income-to-poverty ratio, previous alcohol consumption, previous smoking status, the presence of diabetes, hypertension, and dyslipidemia, and current psoriatic severity. The risk of death increased by 5.5% per BMI unit increase (HR: 1.055, 95% CI: 1.004–1.110, p = 0.035, see Table 3). However, the association between a higher BMI value and an increased all-cause mortality risk was not significantly observed in those without a history of psoriasis (Supplementary Table S5, p = 0.553).
Figure 2, via an RCS regression model, suggests an overall trend of linear relationship between BMI value and the risk of all-cause mortality among individuals with a history of psoriasis (p for nonlinearity = 0.715). According to the RCS model, when a BMI of 28.1 served as a reference for an HR of 1, the overall association was statistically significant (p = 0.003). On one hand, we found that that individuals with baseline BMI values below 28.1 tended to exhibit a slight reduction in HR (i.e., less than 1). Nonetheless, this trend lacks statistical significance. On the other hand, when BMI exceeds 28.1, there was a potentially linear significant correlation between BMI and the risk of all-cause mortality in this population.
Supplementary Table S6 indicates that an elevated BMI in psoriatic individuals was correlated with an increased probability of having severe psoriasis (HR = 1.057, 95% CI 1.003–1.113, p = 0.038). Also, those who had a BMI ≥30 were 6.369 times more likely to have more severe psoriasis compared to those with a BMI <30.
Supplementary Table S7 shows significant mortality rate differences between overweight individuals with mild psoriasis and obese individuals with moderate-to-severe (MtS) psoriasis (p = 0.032), as well as between lean individuals with mild psoriasis and obese individuals with MtS psoriasis (p = 0.045). However, we did not find such difference between lean individuals with mild psoriasis and overweight individuals with moderate-to-severe psoriasis (p = 0.371).
In our sensitivity analyses, the positive association between higher BMI and increased all-cause mortality risk among individuals with psoriasis was not materially altered when excluding participants who died within the first two years of follow-up (adjusted HR = 1.082, 95% CI 1.045–1.228, p < 0.001). Similar results were observed with the use of propensity score matching (PSM) (adjusted HR = 1.040, 95% CI 1.010–1.070, p = 0.004). The results remained substantially unchanged even after combining both criteria (adjusted HR = 1.050, 95% CI 1.020–1.080, p = 0.002). Refer to Supplementary Table S8.
The sensitivity analyses, conditioned on balancing the baseline variables, confirmed the robustness of the association between higher BMI and increased all-cause mortality in individuals with psoriasis in our study.
To the best of our knowledge, the present study was the first to explore the relationship between BMI and the risk of all-cause mortality among individuals with psoriasis. More specifically, we analyzed data from the NHANES database collected between 2003 and 2006, as well as between 2009 and 2014, encompassing a total of 22,876 individuals aged 20 years and above, with or without a history of psoriasis. Our primary finding suggested a positive correlation between BMI and the risk of all-cause mortality among individuals (≥20) with a history of psoriasis. After adjusting for multiple potential confounders, BMI was found to independently increase all-cause mortality risk in this population, showing a trend where mortality risk increased by 5.5% for each unit rise in BMI. These results remained consistent even when utilizing a propensity score matching (PSM) approach. However, similar associations were not observed among individuals without histories of psoriasis in our study.
Despite these novel findings, our results from the restricted cubic splines (RCS) analysis and Multivariate Cox Regression model revealed nuanced results within the population of individuals with psoriasis. The RCS analysis indicated a potential dose–response relationship between baseline BMI and the risk of all-cause mortality. For BMIs ranging from 20 to 28.1, no significant correlation with mortality risk was identified, partially aligning with the results of our stratified analysis when considering BMI as a categorical variable. This stratified analysis suggested no difference in mortality risk between the lean and overweight groups. However, notably, from a BMI of 28.1 onwards, an evident increase in mortality risk was observed in the RCS analysis as BMI values climbed, suggesting a potential linear relationship within this higher BMI spectrum. By contrast, the Multivariate Cox Regression analysis indicated a continuous elevation in mortality risk, with a hazard ratio (HR) of 1.055 per unit increase in BMI across the entire BMI spectrum. This discrepancy between analyses may be attributed to methodological disparities. Compared to the RCS approach, which allowed for exploring such relationship across distinct BMI segments and offered insights into the behavior of this association at a more granular level, the Cox regression model provided an average effect size across the entire BMI range. This approach potentially overshadows subtleties within individual segments. Therefore, although we suggested a positive association between BMI and all-cause mortality risk, evidenced by significant results even after propensity score matching, the interaction between a BMI below 28.1 and mortality risk may be more complex than initially indicated. Further evidence is needed to investigate the impact of a BMI below the obesity threshold on mortality risk. Furthermore, where possible, future prospective studies are encouraged to include larger populations with psoriasis and conduct extended follow-ups to document dynamic changes in BMI, thereby providing comprehensive evidence to better explain and understand the current findings.
Although the impact of overweight on mortality risk is still debated, factors such as a BMI exceeding 30 (i.e., obesity), cigarette smoking, and being male consistently emerge as risk factors for higher all-cause mortality, irrespective of participants having psoriasis or not (16, 30–32). These associations persist in our study even after adjusting for multiple potential confounding covariates, including race/ethnicity, education level, family income-to-poverty ratio, and comorbidities, highlighting the protective effects of being non-obese, non-smoking, and female. Furthermore, in line with previous studies (30, 33), our results also indicated that overweight in older adults aged over 60 was not associated with increased mortality compared to a BMI < 25 group. This finding could be attributed to many elderly individuals having a relatively lower BMI due to unintentional weight loss from illness, potentially exacerbating illness due to sarcopenia (34). Conversely, higher weight increases the risk of developing multiple conditions such as diabetes, arthritis, fatty liver, hypertension, heart failure, and kidney disease (17).
Excessive adiposity (body fatness), a well-established risk factor for premature mortality, is primarily linked to various chronic diseases (14, 16). However, excess weight reflected by a higher BMI could not directly reflect excess body fat. It was suggested that BMI is a relatively poor indicator of body fat percentage and does not account for fat mass distribution across different body sites (35). The observation that there was no change in mortality within the BMI range of 22.5 to 30 in a previous study and below 28.1 in our study may be due to the weak association between BMI and adiposity within this range (15, 35). For example, prior research has shown that among individuals with a BMI of 25 kg/m2, body fat percentage in men ranged from 14 to 35%, and in women, it ranged from 26 to 43% (35), suggesting the instability of utilizing BMI to reflect one’s body fat.
Previous studies suggested an indirect correlation between BMI and mortality among non-obese individuals with psoriasis, indicating that a higher BMI may lead to a higher risk of severe psoriasis and subsequently to a higher risk of all-cause mortality (20, 21). In our study, we did observe a notably positive correlation between BMI and the risk of more severe psoriasis in non-obese group. However, we did not find a significant difference in mortality rate between lean individuals with mild psoriasis and overweight individuals with moderate-to-severe psoriasis. These results may indicate that the relationship between BMI and mortality between lean and overweight groups of individuals with psoriasis is far more complicated than what could be inferred indirectly based on prior findings (20, 21). For future studies, exploring alternative metrics to assess body fat mass and their impacts on these associations is encouraged, especially between lean weight and overweight groups. Moreover, in clinical practice, it is advisable to comprehensively consider the specific condition of a person with psoriasis when assessing their all-cause mortality risk based on BMI.
Overall, our study has several strengths. Firstly, the nationally representative sample size is commendable. Secondly, we adjusted for multiple potential confounding factors using the propensity score matching (PSM). Before PSM, the overweight group had the highest percentages of male participants, non-Hispanic Whites, and individuals with the highest Poverty Income Ratio (PIR), with significant differences noted. The post-PSM comparison increased the validity of our analysis by compensating for these baseline differences, thus ensuring a more balanced and unbiased assessment across the groups. Interestingly, the results remained consistent with those obtained before PSM, enhancing the reliability and stability of our findings. Thirdly, while prior findings indirectly suggest a positive association between BMI and all-cause mortality in non-obese psoriatic individuals, our study provided direct evidence that did not support this relationship. Lastly, our study contributed additional evidence regarding the insignificant association between BMI and all-cause mortality among the general population, consistent with findings from previous studies.
However, there are several limitations to our study. First, we relied on single baseline measures of BMI, precluding evaluation of the time-varying association of interest. Second, the questionnaire format of the psoriasis profile may introduce recall bias. Third, our results are based solely on U.S. adults, limiting generalizability to other populations. Finally, due to the limitations of using BMI to reflect body fat mass and the possibility of residual and unknown confounding factors, our results should be interpreted with caution.
In a nationally representative sample of U.S. adults, we observed a trend wherein a higher BMI was linked to an increased risk of all-cause mortality among individuals with psoriasis, but not among those without the condition. However, the definitive impact of overweight compared to normal weight or underweight remains inadequately explored. Further studies are needed to provide additional evidence on these relationships. Additionally, exploring alternative metrics for assessing body fat to investigate these associations is also urgent.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by National Health and Nutrition Examination Survey. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
ZW: Writing – original draft, Conceptualization, Data curation, Formal analysis, Methodology. GN: Writing – original draft, Conceptualization, Data curation, Investigation, Methodology. CS: Writing – review & editing, Conceptualization, Formal analysis, Methodology. DS: Writing – review & editing, Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Visualization, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1407454/full#supplementary-material
1. Parisi, R, Iskandar, IYK, Kontopantelis, E, Augustin, M, Griffiths, CEM, and Ashcroft, DM. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. (2020) 369:m1590. doi: 10.1136/bmj.m1590
2. Gelfand, JM, and Wang, S. Expanding the global perspective on psoriasis. JAMA Netw Open. (2023) 6:e236802. doi: 10.1001/jamanetworkopen.2023.6802
3. Dhana, A, Yen, H, Yen, H, and Cho, E. All-cause and cause-specific mortality in psoriasis: a systematic review and meta-analysis. J Am Acad Dermatol. (2019) 80:1332–43. doi: 10.1016/j.jaad.2018.12.037
4. Jensen, P, and Skov, L. Psoriasis and obesity. Dermatology. (2017) 232:633–9. doi: 10.1159/000455840
5. Paroutoglou, K, Papadavid, E, Christodoulatos, GS, and Dalamaga, M. Deciphering the association between psoriasis and obesity: current evidence and treatment considerations. Curr Obes Rep. (2020) 9:165–78. doi: 10.1007/s13679-020-00380-3
6. Barros, G, Duran, P, Vera, I, and Bermúdez, V. Exploring the links between obesity and psoriasis: a comprehensive review. Int J Mol Sci. (2022) 23:7499. doi: 10.3390/ijms23147499
7. Vata, D, Tarcau, BM, Popescu, IA, Halip, IA, Patrascu, AI, Gheuca Solovastru, DF, et al. Update on obesity in psoriasis patients. Life (Basel). (2023) 13:1947. doi: 10.3390/life13101947
8. Ellulu, MS, Patimah, I, Khaza'ai, H, Rahmat, A, and Abed, Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. (2017) 13:851–63. doi: 10.5114/aoms.2016.58928
9. Man, AM, Orăsan, MS, Hoteiuc, OA, Olănescu-Vaida-Voevod, MC, and Mocan, T. Inflammation and psoriasis: a comprehensive review. Int J Mol Sci. (2023) 24:16095. doi: 10.3390/ijms242216095
10. Lønnberg, AS, Skov, L, Skytthe, A, Kyvik, KO, Pedersen, OB, and Thomsen, SF. Association of Psoriasis with the risk for type 2 diabetes mellitus and obesity. JAMA Dermatol. (2016) 152:761–7. doi: 10.1001/jamadermatol.2015.6262
11. Abdelaal, M, le Roux, CW, and Docherty, NG. Morbidity and mortality associated with obesity. Ann Transl Med. (2017) 5:161. doi: 10.21037/atm.2017.03.107
12. Adab, P, Pallan, M, and Whincup, PH. Is BMI the best measure of obesity? BMJ. (2018) 360:k1274. doi: 10.1136/bmj.k1274
13. Aune, D, Snekvik, I, Schlesinger, S, Norat, T, Riboli, E, and Vatten, LJ. Body mass index, abdominal fatness, weight gain and the risk of psoriasis: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. (2018) 33:1163–78. doi: 10.1007/s10654-018-0366-z
14. Budu-Aggrey, A, Brumpton, B, Tyrrell, J, Watkins, S, Modalsli, EH, Celis-Morales, C, et al. Evidence of a causal relationship between body mass index and psoriasis: a mendelian randomization study. PLoS Med. (2019) 16:e1002739. doi: 10.1371/journal.pmed.1002739
15. Visaria, A, and Setoguchi, S. Body mass index and all-cause mortality in a 21st century U.S. population: a National Health Interview Survey analysis. PLoS One. (2023) 18:e0287218. doi: 10.1371/journal.pone.0287218
16. Aune, D, Sen, A, Prasad, M, Norat, T, Janszky, I, Tonstad, S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. (2016) 353:i2156. doi: 10.1136/bmj.i2156
17. Tobias, DK, and Hu, FB. The association between BMI and mortality: implications for obesity prevention. Lancet Diabetes Endocrinol. (2018) 6:916–7. doi: 10.1016/S2213-8587(18)30309-7
18. Li, Y, Zhang, J, Wen, J, Liu, M, Liu, W, and Li, Y. Large-scale genome-wide association study to identify causal relationships and potential mediators between education and autoimmune diseases. Front Immunol. (2023) 14:1249017. doi: 10.3389/fimmu.2023.1249017
19. Shan, D, Wang, Y, Tousey-Pfarrer, M, Guo, C, Wan, M, Wang, P, et al. Association between patterns of biological rhythm and self-harm: evidence from the baoxing youth mental health (BYMH) cohort. Child Adolesc Psychiatry Ment Health. (2024) 18:3. doi: 10.1186/s13034-023-00685-w
20. Alizadeh, N, Azimi, SZ, and Hoseinzadeh, S. Body mass index and severity of psoriasis: a cross-sectional study. Iran J Dermatol. (2021) 24:46–52. doi: 10.22034/ijd.2020.232580.1107
21. Danielsen, K . Increased risk of death in patients with psoriasis: disease or lifestyle? Br J Dermatol. (2019) 180:3–4. doi: 10.1111/bjd.17141
22. Qiu, Z, Chen, X, Geng, T, Wan, Z, Lu, Q, Li, L, et al. Associations of serum carotenoids with risk of cardiovascular mortality among individuals with type 2 diabetes: results from NHANES. Diabetes Care. (2022) 45:1453–61. doi: 10.2337/dc21-2371
23. National Center for Health Statistics . Centers for Disease Control and Prevention NCHS research ethics review board (ERB) approval NHANES (2024). Hyattsville: National Center for Health Statistics. Available online at: https://www.cdc.gov/nchs/nhanes/index.htm
24. Fiorentino, TV, de Vito, F, Suraci, E, Marasco, R, Hribal, ML, Luzza, F, et al. Obesity and overweight are linked to increased sodium-glucose cotransporter 1 and glucose transporter 5 levels in duodenum. Obesity (Silver Spring). (2023) 31:724–31. doi: 10.1002/oby.23653
25. The Linkage of National Center for Health Statistics . Survey data to the National Death Index – 2015 linked mortality file (LMF): Methodology overview and analytic considerations National Center for Health Statistics, Centers for Disease Control and Prevention (2019). Hyattsville: National Center for Health Statistics. Available online at: https://www.cdc.gov/nchs/nhanes/index.htm
26. National Center for Health Statistics . (2018). National Health and Nutrition Examination Survey. Available online at: https://www.cdc.gov/nchs/nhanes/index.htm
27. Chandrasekar, EK, Ali, MK, Wei, J, Narayan, KMV, Owens-Gary, MD, and Bullard, KMK. Trends in depression by glycemic status: serial cross-sectional analyses of the National Health and nutrition examination surveys, 2005-2016. Prim Care Diabetes. (2022) 16:404–10. doi: 10.1016/j.pcd.2022.03.001
28. Foti, K, Hardy, ST, Chang, AR, Selvin, E, Coresh, J, and Muntner, P. BMI and blood pressure control among United States adults with hypertension. J Hypertens. (2022) 40:741–8. doi: 10.1097/HJH.0000000000003072
29. Huang, C, Zhang, WQ, Tang, WW, Liu, Y, Liu, JX, Xu, RH, et al. Prevalence and related factors of dyslipidemia among urban adults aged 35 to 79 years in southwestern China. Sci Rep. (2021) 11:17579. doi: 10.1038/s41598-021-96864-w
30. Prospective Studies CollaborationWhitlock, G, Lewington, S, Sherliker, P, Clarke, R, Emberson, J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. (2009) 373:1083–96. doi: 10.1016/S0140-6736(09)60318-4
31. Lim, KH, Cheong, YL, Lim, HL, Kee, CC, Mohd Ghazali, S, Pradmahan Singh, BSG, et al. Assessment of association between smoking and all-cause mortality among Malaysian adult population: findings from a retrospective cohort study. Tob Induc Dis. (2022) 20:1–10. doi: 10.18332/tid/147656
32. Rosella, LC, Calzavara, A, Frank, JW, Fitzpatrick, T, Donnelly, PD, and Henry, D. Narrowing mortality gap between men and women over two decades: a registry-based study in Ontario, Canada. BMJ Open. (2016) 6:e012564. doi: 10.1136/bmjopen-2016-012564
33. Winter, JE, MacInnis, RJ, Wattanapenpaiboon, N, and Nowson, CA. BMI and all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. (2014) 99:875–90. doi: 10.3945/ajcn.113.068122
34. Arango-Lopera, VE, Arroyo, P, Gutiérrez-Robledo, LM, Pérez-Zepeda, MU, and Cesari, M. Mortality as an adverse outcome of sarcopenia. J Nutr Health Aging. (2013) 17:259–62. doi: 10.1007/s12603-012-0434-0
Keywords: psoriasis, body mass index, BMI, all-cause mortality, obesity, NHANES, overweight
Citation: Wei Z, Nie G, Sadik CD and Shan D (2024) Associations between body mass index and all-cause mortality among individuals with psoriasis: results from the NHANES database retrospective cohort study. Front. Nutr. 11:1407454. doi: 10.3389/fnut.2024.1407454
Received: 28 March 2024; Accepted: 14 May 2024;
Published: 05 June 2024.
Edited by:
Yejun Tan, University of Minnesota Health Twin Cities, United StatesReviewed by:
Helen Booth, Medicines and Healthcare Products Regulatory Agency, United KingdomCopyright © 2024 Wei, Nie, Sadik and Shan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Shan, ZC5zaGFuQGxhbmNhc3Rlci5hYy51aw==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.