- The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, China
Cataract is a common eye disease characterized by lens opacity, leading to blurred vision and progressive blindness of the eye. Factors affecting the development of cataracts include nutrition, oxidative stress, micronutrients and inflammatory factors, and also include genetics, toxicity, infrared exposure, hyperuricemia, and mechanical injuries. Among the nutritional factors, a balanced diet, vegetarian diet, dairy products and vegetables are protective against cataracts; high-sodium diet, high intake of carbohydrates and polyunsaturated fatty acids may increase the risk of cataracts; and increased intake of proteins, especially animal proteins, may prevent nuclear cataracts. Intake of antioxidants such as β-carotene, lutein, or zeaxanthin is associated with a reduced risk of cataracts. Minerals such as zinc, selenium, calcium and sodium have also been associated with cataract development. Oxidative stress plays an important role in the development of cataracts and is associated with several antioxidative enzymes and biomarkers such as glutathione (GSH), superoxide dismutase (SOD), malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE). Insulin resistance is also an essential risk factor for cataracts, especially in diabetic patients. In conclusion, understanding these influencing factors helps us to better prevent cataracts. And in this article, we will focus on the important factor of diet and nutrition for a detailed discussion.
1 Introduction
Cataract is a common eye disease whose typical symptom is the opacity of the lens, which causes blurred vision and even progressive blindness. According to the World Health Organization (WHO), cataracts affect more than 94 million people worldwide (1), indicating that cataracts have become one of the major causes of global vision impairment. Therefore, exploring the risk factors affecting cataract formation is crucial for the prevention and mitigation of this disease. The object of this study is to comprehensively analyze all known influencing factors, including dietary structure, chronic diseases, to deepen the understanding of the pathogenesis of cataract and providing scientific evidences for the development of effective preventive measures. At the same time, this study will also examine some generally proposed influencing factors, such as nutrient intake, oxidative stress, insulin resistance, etc., in order to expand our knowledge in cataract formation. By systematically analyzing these factors, this study hopes to facilitate preventive intervention and mitigation of early cataract formation and provide new thoughts and solutions for clinical practice.
2 Correlation of dietary mode and intakes with cataract
2.1 Dietary mode
Falkowska et al. (2) pointed out that a balanced diet (mainly based on calorie restriction of vegetables, grains, legumes and fish, and a nutrient pattern of low animal fats), a vegetables diet, “dairy and vegetables,” “traditional diet,” “antioxidants” and “Omega-3 (polyunsaturated fatty acids)” have a significant protective effect on age-related cataracts. A large hospital cohort study conducted by Jee and Park (3) assessed lifestyle-related risk factors. Metabolic syndrome (MS) was positively associated with age-related cataract (ARC). In addition, they found that individuals with hyperglycemia and low density lipoprotein (LDL) cholesterolemia were more prone to ARC, and plasma glucose and HbA1c concentrations increased 1.50 and 1.92-fold, in patients with MS exhibiting ARC risk. High carbohydrate intake increased the risk of ARC by 1.4-fold, and high fat (≥15%), protein and calcium intake reduced the risk of ARC by 0.74-fold. Movahedian (4) et al. found a significant and direct relationship between dietary glycemic index, glycemic load, insulin load and cataracts, and speculated that improving the quality of the diet is a key approach to reduce the risk of cataracts.
2.2 Carbohydrate intake
Several studies have shown (5, 6) that carbohydrate intake is positively associated with cataract development. The specific mechanism of the reaction is unknown, and it may be that the slow absorption and utilization of glucose by the ocular aqueous humor leads to prolonged exposure of lens proteins to higher concentrations of glucose, causing the occurrence of protein cross-linking, aggregation, and precipitation, which leads to lens opacity and the development of cataracts (7). In addition, carbohydrates can elevate blood glucose concentrations, increasing the risk of cataract development (8).
2.3 High fat diet
Lu et al. (9) found that intake of large amounts of linoleic or linolenic acid increases the risk of lens opacity, which may ultimately lead to cataracts, because of the susceptibility of unsaturated fatty acids to lipid peroxidation, which results in the susceptibility of lens epithelial cells to oxidative stress, causing cell damage.
3 Correlation of glucose metabolism with cataract
3.1 Association of insulin resistance with cataract
Guo (10) found that in patients with diabetic cataract, high levels of fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), and insulin resistance index (HOMA-IR) were negatively correlated with visual acuity, and positively correlated with intraocular pressure (IOP) serum levels of interleukin-6 (IL-6), insulin-like growth factor (IGF-1), and vascular endothelial growth factor (VEGF) levels. This suggests that IL-6, IGF-1, and VEGF are important inflammatory factors promoting insulin resistance, and glucose fluctuations in diabetic cataracts and these factors are closely related to oxidative stress injury. It has been noted (11, 12) that NADPH oxidase-mediated oxidative stress and P53 (p53 is a tumor suppressor protein that regulates the expression of a variety of genes that are involved in apoptosis, growth arrest, inhibition of cell cycle progression, differentiation and accelerated DNA repair or senescence in response to genotoxicity or cell stress.) and Bax/Bcl2-mediated apoptosis signaling pathways are involved in the pathogenesis of cataracts in diabetic rats, and Puerarin may exert a therapeutic effect on diabetic cataract rats by improving the state of insulin resistance and downregulating the level of P53 protein (12).
3.2 The pathogenesis of diabetic cataract
In diabetic patients, prolonged hyperglycemia leads to excessive accumulation of sorbitol in the lens, increased osmotic pressure, influx of aqueous humor, leading to intracellular edema and fiber breakage, ultimately leading to lens turbidity and further worsening the extent of oxidative stress. It has been proposed (13) that cataract formation usually occurs in the several weeks or months after the initiation of insulin treatment in type I diabetes, and insulin autoantibodies are positive within 3 months of the initiation of insulin therapy, which coincided with cataract formation. Martina et al. (14) found that the development of cataracts in type II diabetes mellitus was closely related to the course of diabetes and various metabolic risk factors, especially the coexistence of poor glycemic control, hypercholesterolemia, diastolic blood pressure and diabetic nephropathy.
Decrease in insulin level or inhibition of galactokinase activity in the patients results in increased blood glucose content and the osmotic pressure within the lens. Lens fibers will be swelling and contain fractures, with increased opacity due to excessive osmotic pressure elevation. Early and timely diagnose is mandatory under this situation (15). After testing the serum levels of HbA1c, FPG, and fasting insulin (FINS) in patients with diabetic cataracts and other cataracts, calculating HOMA-IR, and testing the levels of IGF-1 and IL-6, Tang et al. (15) found that the other cataract patients had lower levels of HbA1c, FPG, HOMA-IR, IGF-1, and IL-6 than the patients with diabetic cataracts. Therefore, they believed that these indicators can assist in determining the condition. Guo et al. (10) yielded similar results and also mentioned that the IOP of diabetic cataract patients was higher than other cataract patients. Cai et al. (16) analyzed the relationship between postoperative insulin resistance and changes in inflammatory factor levels and quality of vision in cataract patients with glaucoma. It was mentioned that the patient’s preoperative objective scatter index (OSI) was negatively correlated with insulin sensitivity index, that is, the degree of insulin resistance correlated with the degree of lens opacity. Suryanarayana et al. (17) showed that impaired glucose tolerance (IGT), which is suggestive of insulin resistance, affects cataract development in rat model experiments.
4 Correlation of fat metabolism with cataract
4.1 Correlation of hyperlipidemia and cataract
Yin et al. (18) proposed that hyperlipidemia is the main factor for increased lens density in patients with age-related nuclear cataract. They found that serum total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDLC) levels in age-related nuclear cataract were correlated with lens density. Zhang et al. (19) suggested that hyperlipidemia promotes the development of galactose cataract to some extent based on data derived from rats experiments and suggested that cataract formation may be involved in the oxidative stress response. The hyperlipidemic cataract group had reduced GSH and higher malondialdehyde contents than the normal cataract group, reflecting reduction of antioxidative capacity and increase of damages caused by free radicals under a hyperlipidemic status (20). This reflects the reduced activity of the antioxidant system in the lens of rats in the hyperlipidemic cataract group, and the increased malondialdehyde content suggests an increased severity of cell attacked by free radicals. Similar results were obtained by Tsutsumi et al. (20) in rats experiments, leading to a conclusion that hyperlipidemia that hyperlipidemia and LDLC are risk factors for the development of diabetic cataracts. In a case–control study conducted by Galeone et al. (21), cataract occurrence was found to associate with hyperlipidemia, central obesity, hypertension and diabetes. Zhang et al. (22) also concluded that age-related cataract patients are often afflicted with hyperlipidemia, hypertension and hyperglycemia. They found that oxidized low-density lipoprotein (oxLDL) can effectively affect lens epithelial cell transcription, leading to differential expression of Rho signaling and ATP1B1, which may be involved in cataract formation.
However, Jiang et al. (23) proposed a different viewpoint, with data showing that only the decrease in HDLC content increased the risk of age-related cataracts in middle-aged and elderly people, and there was no correlation between TC and TG, and they did not discuss LDL. This is inconsistent with the previous view. However, at present, there is not enough research to support the inevitable relationship between hyperuricemia and the development of cataract.
4.2 The relationship between MAFLD and cataract
In a Korean study (24), it was found that metabolism-associated fatty liver disease (MAFLD) was more closely associated with cataracts than non-alcoholic fatty liver disease (NAFLD). MAFLD may be a combined risk factor for cataracts, with significant correlations with all cataract subtypes because cataracts can be caused by various metabolic and inflammatory conditions, and MAFLD covers alcohol-induced cirrhosis and various metabolic diseases. In addition, hepatic factors and the signaling proteins secreted by the liver can reach the eye and cause oxidative stress and inflammation.
5 Correlation of mineral metabolism and cataract
Minerals are also closely related to cataracts, and nutritional dystrophy (lack of macroelement and microelement, insufficient oxygen supply, and reduced hemoglobin) can lead to the development of nuclear cataracts (25).
5.1 Zinc
The content of zinc in ocular tissues, especially in retina, is significantly higher than in other tissues. One study found that combining zinc and vitamin A as a nutrient supplement reduced the incidence of cataracts (26). It can be assumed that oxidative damages cause alterations in the structure of lens proteins, while antioxidant metalloenzymes relied by zinc, such as SOD, protect the lens (27).
5.2 Selenium
Selenium acts as a functional heteroatom in peroxidases and plays an important role in the metabolism of H2O2 and other peroxides, effectively preventing free radical production and damages to tissues. If the amount of selenium exceeds the amount required for the synthesis of proteins containing selenium, a redox cycle is initiated, which promotes oxidative damage and ultimately induces cataract development in laboratory animals (28). In addition, Dawczynski (29) et al. found that the amount of selenium in the lens increases with increasing lens opacity, and the amount of selenium in the lens is higher in the mature stage of cataract than in other stages, whereas serum selenium shows the opposite change. But the exact mechanism is still unknown.
5.3 Calcium
When the concentration of calcium ions in the aqueous humor deviates from the normal value, either too high or too low, it will lead to the development of lens opacity, which is named as hypercalcemic cataract and hypocalcemic cataract, respectively. Delamere et al. (30) constructed a model of hypocalcemic cataract in rabbits by feeding a low-calcium diet and divided the hypocalcemic cataracts into three stages, including posterior subcapsule punctate opacity, dense opacity, and extension to the superficial anterior cortical layer, and suggested that aqueous humor calcium can be inferred from the serum calcium. Yang et al. (31) incubated rabbit lens in different concentrations of CaCl2 solution for 36H and found that all the rabbit lenses could develop hypercalcemic cataracts with complete cortical turbidity when the CaCl2 concentration in the culture solution was ≥30 mmol/L. The homeostasis of calcium ions plays an important role in maintaining lens transparency. When the cell membrane is damaged, large amounts of calcium ions from the aqueous humor move in to the lens and activate calpain, leading to the degradation of numerous important structural proteins (31).
5.4 Sodium
High intake of sodium is also a factor affecting cataracts (32). When the lens cell membranes are damaged by oxidative stress, the function of Sodium-Potassium Pump that maintains the normal low Na + and high K+ concentrations is altered in the cells, which increases the permeability of sodium ions and the concentration of sodium ions in the lens, exacerbating lens opacity.
6 Correlation of vitamins with cataract
Vitamin A, vitamin C, and vitamin E have been associated with a reduced risk of ARC too. Vitamin C, also named as ascorbic acid, is a strong antioxidant in the body. Its remarkable antioxidant properties have been negatively correlated with the development of cataracts. It can react rapidly with free radicals such as O-, HOO-, and OH- to generate semi-dehydroascorbic acid and be beneficial to the scavenging of single oxygen (33). Ge et al. (34) suggested that the antioxidant efficacy of vitamin C in organisms far exceeds that of the in vitro. It may be attributed to its action in vivo through a range of indirect mechanisms rather than direct scavenging oxygen radicals. So, increasing the intake of vitamin C can be considered as an effective strategy to improve the antioxidant capacity of the organism and help to prevent cataracts.
In a streptozotocin (STZ)-induced oxidative stress model in senile diabetic rats (35), dietary vitamin C and E supplementation alleviated oxidative stress and increased the antioxidant levels of the lens. The mechanism may be that reduced GSH synergises with antioxidant vitamins to resist oxidative stress. Vitamin E transfers its hydrogen to superoxide radical of polyunsaturated fatty acids, breaking the radical chain reaction and preventing the peroxidation of polyunsaturated fatty acids in the cellular and subcellular membranes. These vitamins can also directly scavenge ROS and increase the activity of antioxidant enzymes.
There is a considerable controversy regarding the effect of vitamin E on cataract formation. Increasing dietary intake of food rich in vitamin E and supplying vitamin E pill to the population may reduce the risk of nuclear cataract development (36), but most studies do not show results in agreement with this hypothesis, especially in studies regarding the role of vitamin E in cortical cataracts (37).
The literature published by Spector et al. (38) mentioned that nutrient interventions may be a solution to reduce cataract risk. They showed that increasing intake of vitamin C, lutein, xanthines and dietary fruit can reduce the incidence of age-related cataracts. Lawrenson and Grzybowski (39) have also shown that a diet containing antioxidants can delay the progression of cataracts. Nutrient factors, particularly vitamins with antioxidant properties, are thought to play a protective role in cataract development and progression. Vitamin A, niacin, riboflavin, thiamin, folic acid and vitamin B12 appear to have a protective effect, either alone or as components of multi-vitamin preparations (26, 40).
7 Analysis of other nutritional factors related to cataract
7.1 The relationship between oxidative stress and cataract
Oxidative stress is a state of imbalance between oxidative and antioxidative effects in the body, with more oxidative stress due to higher oxidative effects. Oxidative stress plays an important role in the pathogenesis of all types of cataracts. The lens derives its energy mainly from the glycolysis, so the lens inevitably generates a large number of oxygen radicals, such as superoxide anion (O2-), hydroxyl radical (OH-), and hydrogen peroxide (H2O2) during metabolism, causing oxidative stress on the membranes and proteins in the lens, affecting lens transparency in different degrees. If the degree of oxidation exceeds the regulatory capacity of the antioxidant system, lens damage occurs, leading to cataract.
7.1.1 Mechanisms of oxidative stress-induced cataract
In almost all types of cataract lens, the amount of GSH decreases with increasing lens opacity, so deficiency of GSH is thought to be one of the causes of cataract. Antioxidant enzyme systems, such as SOD, facilitate to scavenge O2-, protect cells from oxidative stress damage, and maintain redox balance in the lens. Zhou et al. (41) have shown that H2O2 can impair the antioxidant system of the lens, reducing GSH content and decreasing SOD viability to promote the occurrence of cataract.
7.1.2 Methods to mitigate the oxidative damage
The extract of concha haliotidis significantly reduced H2O2-induced cataract formation, and its mechanism is to protect lens SOD activity, maintain GSH content, and reduce lens epithelial cell damage (42). In addition, it was found (43) that quercetin improved selenite-induced cataract in rats by enhancing the Nrf-2/HO-1 signaling pathway, through inhibition of oxidative stress. Kang et al. (44) pointed out that nitric oxide synthase (NOS) mRNA was positively correlated with the representative level of oxidative stress in the organism, SOD, in the lens of cortical cataract patients. They further proposed that NOS mRNA is also a factor involved in the process of oxidative stress in patients with cortical cataracts and has a certain effect on the progression of cataracts. It has been shown in the literature (45, 46) that nuclear factor erythroid 2-related factor 2/Kelch-like ECH-associated protein 1 (Nrf2-keap1) is the main mechanism of resistance to oxidative stress, and demethylation of keap1 promoter activates the expression of Keap1 protein, which promotes the degradation of Nrf2 proteasome and attenuates Nrf2 activity, leading to the reduction of resistance to oxidative stress and ultimately causing the cataract occurrence. In addition to Nrf2-keap1, Song et al. (47) proposed that blood suppressor II (BDS-II) inhibits oxidative stress-induced cataract by suppressing oxidative stress-induced reduction of GSH levels and lens epithelial cell death. BDS-II is a blocker of Kv3 channel (voltage gated potassium ion channels), which mainly blocks the oxidation-sensitive channel Kv3.4 to resist oxidative stress.
In normal conditions, Nrf2 is in the cytoplasm, and keap1 protein can maintain the stability of Nrf2 in the cytoplasm. When oxidative stress causes excessive generation of oxygen free radicals, keap1 protein releases Nrf2 through the release of zinc ions, followed by the entrance of Nrf2 into the nucleus to bind to the ARE anti-oxidative stress element sequence, and activates gene transcription downstream of the ARE region, which then initiates the oxidative stress response and reduces the oxidative stress.
Antioxidants have been promoted to delay or prevent cataracts due to their ability to reduce oxidative damage. In a dose–response meta-analysis (48), increasing 5 mg β-carotene daily reduced 10% risk of ARC, and increasing 10 mg lutein or zeaxanthin daily reduced 19% risk of ARC. Lutein and zeaxanthin concentrate in the eye more than any other nutrients and are the only nutrients that have the ability to block blue light and ultraviolet like sunglasses. Blue light and ultraviolet are the primary factors to eye fatigue, blurred vision, and eventually cataracts. Lutein and zeaxanthin are also potent natural antioxidants that resist the destruction of free radical to the eyes. Ma (49) pointed that dietary intake of flavonols (quercetin and isorhamnetin) is associated with the development of age-related cataracts, and increasing dietary intake of quercetin and isorhamnetin may result in a lower risk of age-related cataracts.
8 Dietary inflammation index
Shivappa et al. (50) found that eating red meat, sugary drinks, and high-fat dairy products increased the dietary inflammatory index (DII), and higher DII is more likely to be inflammatory. However, the mechanism between DII and the development of cataracts is unclear. One of the possible mechanisms is that pro-inflammatory foods can increase the effects of pro-inflammatory factors (IL-1, IL-6, TNFα) on the transcription of acute-phase proteins, which leads to increased mitosis and collagen synthesis in lens epithelial cells, triggering cataracts. Studies (51) found differences in the expression of inflammatory factors at different ages, which may be related to the development of immune cells in the uvea stroma. This hypothesis can explain that EGF, IL-3, IL-8, and MCP-1 are positively corrective with age. Among the various pro-inflammatory factors, TNFα can promote the production of extracellular matrix (ECM) and regulate the proliferation and differentiation of lens epithelial cells, but the roles of other factors in cataract formation need to be further investigated.
9 Prospects and outlook
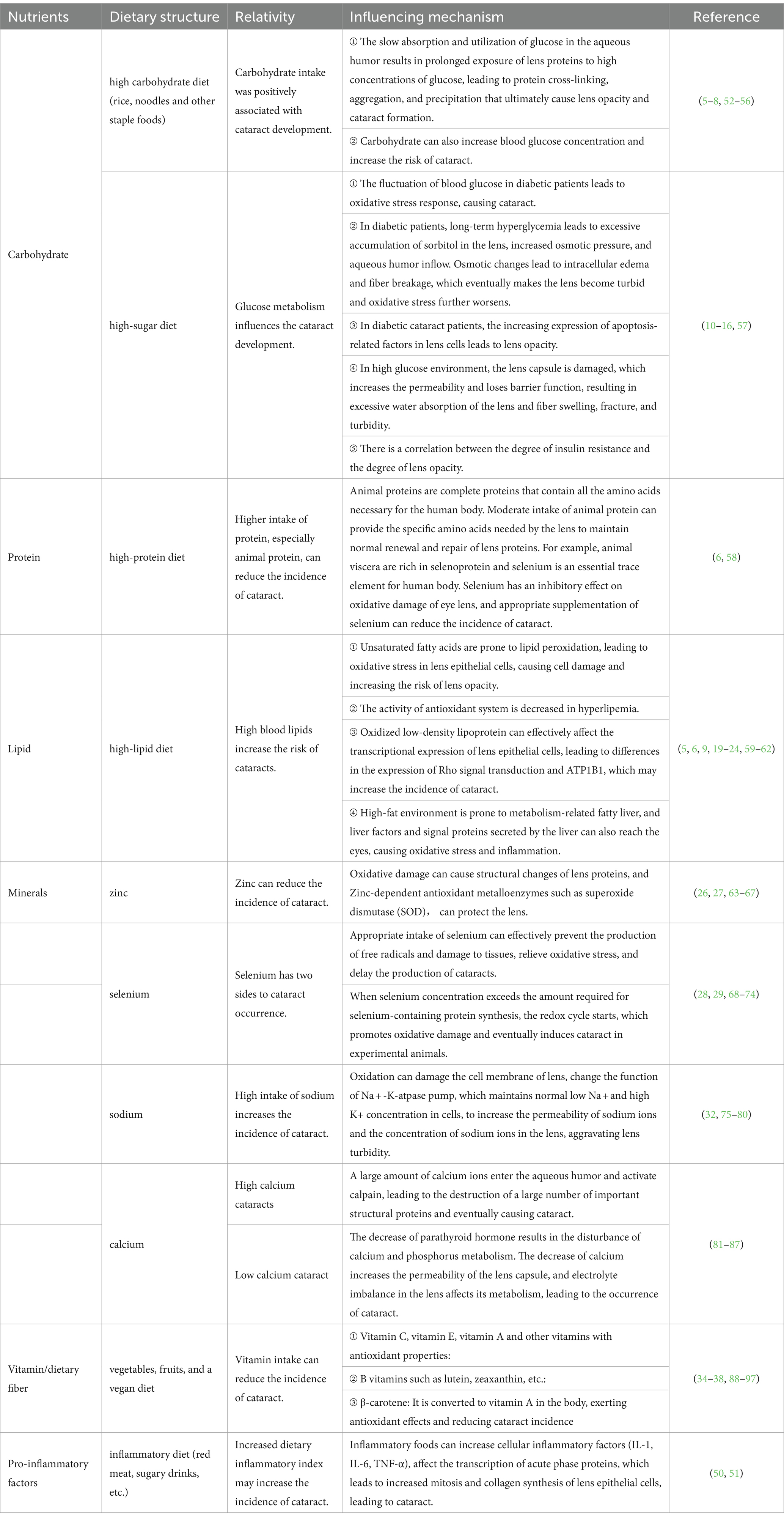
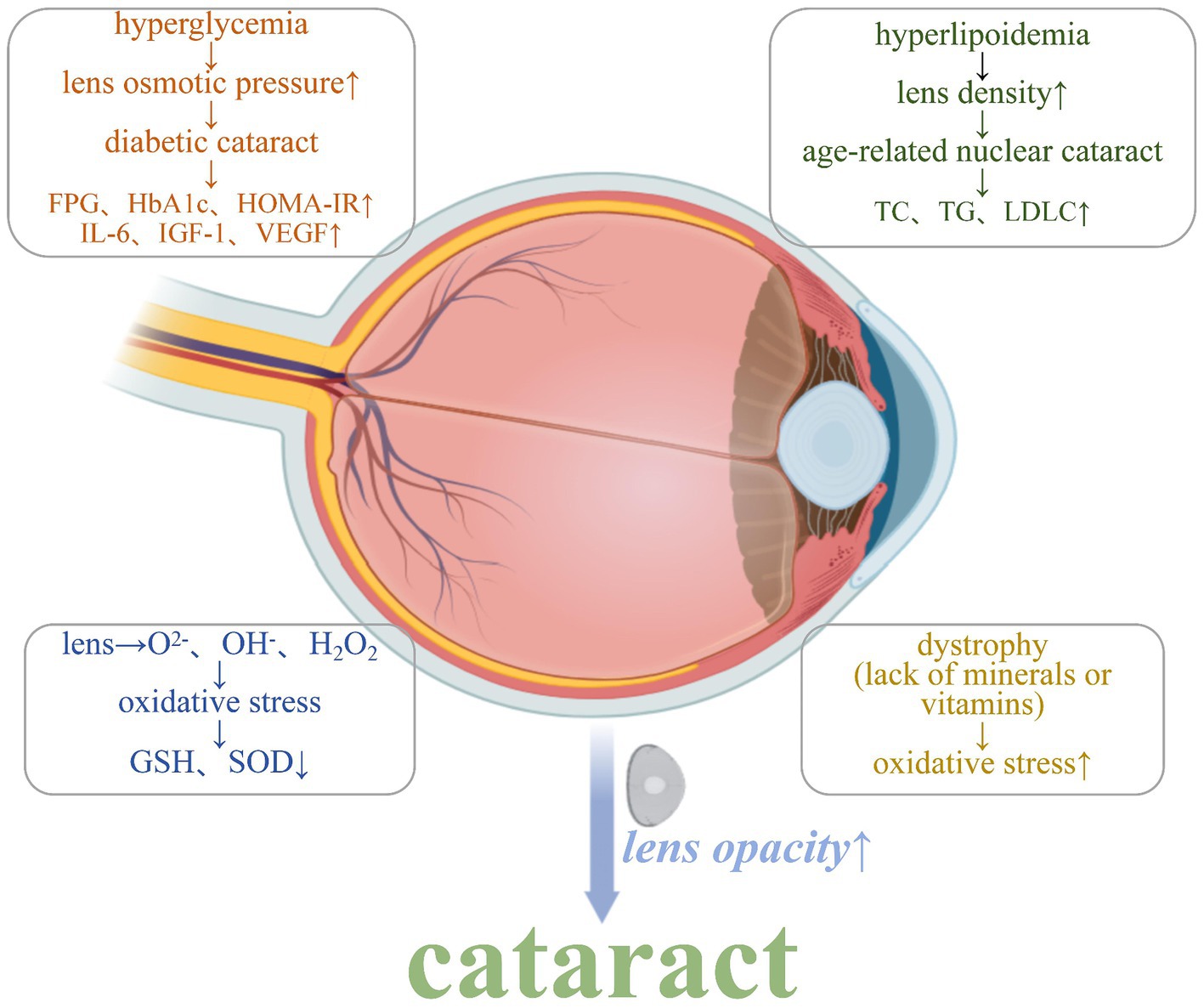
Cataracts have a serious impact on people’s quality of life and need to be treated early, but the occurrence is associated with various factors that make it difficult to prevent. Therefore, continuing and deep studies are necessary to better prevent and to develop novel treat regimen for cataracts. In studying the relationship between dietary nutrition and cataract development, Table 1 highlights key nutrients associated with cataract risk. Understanding their roles in maintaining ocular health provides insights into potential preventative measures. Figure 1 illustrates the mechanisms that lead to cataract formation, including oxidative stress, inflammation, and apoptosis. The followings are some suggested actions that can be taken to fight against cataract formation.
The mechanisms of action of various risk factors need to be further clarified. For example, the specific mechanism of the inflammatory factors TNF-α and IL-6 in cataract development remains to be revealed. By resolving these signaling pathways, new targets can be provided for therapy.
Explore MAFLD and other areas that have received less attention, change the research thinking, and explore the occurrence and mechanism of cataract formation from other perspectives.
Enhance nutrient intervention research. Dietary components, such as the antioxidants vitamin C, E and flavonoids, have a protective effect against cataract formation, and personalized diet can be developed for different populations in the future.
In conclusion, cataract is a complex and multi-factorial disease that requires multidisciplinary cooperation to study pathogenesis deeply. With the advancement of science and technology, it is believed that more effective prevention and therapy can be found in the future to reduce the burden of cataract on human beings.
Author contributions
YZ: Writing – original draft, Writing – review & editing. XQ: Writing – original draft, Writing – review & editing. TX: Writing – review & editing, Writing – original draft. FC: Writing – review & editing, Writing – original draft. BH: Writing – review & editing, Project administration, Supervision.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study is supported by the Promotion Plan for High Quality Development of Disciplines of Zhejiang Provincial Hospital of Chinese Medicine-ophthalmology (No. 2D02320).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group volume number 14 and page 29 volume number 39 and page range 4 range 1 Medicine and Health of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the global burden of disease study. Lancet Glob Health. (2021) 9:e144–60. doi: 10.1016/S2214-109X(20)30489-7
2. Falkowska, M, Młynarczyk, M, Micun, Z, Konopińska, J, and Socha, K. Influence of diet, dietary products and vitamins on age-related cataract incidence: a systematic review. Nutrients. (2023) 15:4585. doi: 10.3390/nu15214585
3. Jee, D, and Park, S. Hyperglycemia and hypo-HDL-cholesterolemia are primary risk factors for age-related cataract, and a Korean-style balanced diet has a negative association, based on the Korean genome and epidemiology study. J Korean Med Sci. (2021) 36:e155. doi: 10.3346/jkms.2021.36.e155
4. Movahedian, M, Thomas, J, Rahmani, J, Clark, CCT, Rashidkhani, B, and Ghanavati, M. Association between dietary glycemic index and glycemic load, insulin index and load with incidence of age-related cataract: results from a case-control study. Diabetes Metab Syndr. (2020) 14:199–204. doi: 10.1016/j.dsx.2020.02.013
5. Yan, J, Zhang, L, Sun, W, Zhang, D, Jiang, T, Zhai, S, et al. Relation between dietary carbohydrate and fat intake and the risk of age-related cataract. Int Eye Sci. (2011) 11:1928–31. doi: 10.3969/j.issn.1672-5123.2011.11.017
6. Yan, J. (2013). Association of dietary factors with age-related cataract. [master’s thesis]. [Jinzhou(Liaoning)]: Liaoning Medical College.
7. Franke, S, Dawczynski, J, Strobel, J, Niwa, T, Stahl, P, and Stein, G. Increased levels of advanced glycation end products in human cataractous lenses. J Cataract Refract Surg. (2003) 29:998–1004. doi: 10.1016/s0886-3350(02)01841-2
8. Huang, X, and Song, L. Risk factors of cataract formation. Int Eye Sci. (2010) 10:1128–30. doi: 10.3969/j.issn.1672-5123.2010.06.034
9. Lu, M, Taylor, A, Chylack, LT Jr, Rogers, G, Hankinson, SE, Willett, WC, et al. Dietary fat intake and early age-related lens opacities. Am J Clin Nutr. (2005) 81:773–9. doi: 10.1093/ajcn/81.4.773
10. Guo, J . Blood glucose levels in patients with diabetes cataract. Jilin Medical J. (2022) 43:2961–3. doi: 10.3969/j.issn.1004-0412.2022.11.024
11. Wan, L, Liu, W, Shen, Y, Yu, Q, and Zhang, J. Oxidative stress-apoptosis mediated STZ-induced diabetic cataract and the interventions of puerarin. Int Eye Sci. (2014) 14:1773–5. doi: 10.3980/j.issn.1672-5123.2014.10.08
12. Zhang, J, and Han, F. Effect of puerarin on disease progression in diabetic cataract rat model. Chin J Gerontol. (2018) 38:2195–6. doi: 10.3969/j.issn.1005-9202.2018.09.057
13. Papadimitriou, DT, Bothou, C, Skarmoutsos, F, Alexandrides, TK, Papaevangelou, V, and Papadimitriou, A. The autoimmune hypothesis for acute bilateral cataract in type 1 diabetes. Diabetes Metab. (2016) 42:386–7. doi: 10.1016/j.diabet.2016.04.006
14. Martina, T, Romano, V, Petar, R, Spomenka, L, Tomislav, B, and Dario, R. Hypertension and hypercholesterolemia are associated with cataract development in patients with type 2 diabetes. High Blood Pressure & Cardiovascular Prevent. (2021) 28:475–81. doi: 10.1007/s40292-021-00472-8
15. Tang, Z, Lu, Y, and Chen, X. Correlation of abnormal glucose metabolism, insulin resistance and inflammatory factors in aqueous humor and serum in diabetic cataract patients. Int Eye Sci. (2019) 19:32–4. doi: 10.3980/j.issn.1672-5123.2019.1.06
16. Cai, Y, Liu, W, Zhuo, Y, and Huang, L. Relationship between postoperative insulin resistance and inflammatory factor levels and visual quality in patients with cataract and glaucoma. Medical Sci J Central South China. (2023) 51:242–5. doi: 10.15972/j.cnki.43-1509/r.2023.02.021
17. Suryanarayana, P, Patil, MA, and Reddy, GB. Insulin resistance mediated biochemical alterations in eye lens of neonatal streptozotocin-induced diabetic rat. Indian J Exp Biol. (2011) 49:749–55.
18. Yin, R, Du, L, and Wang, H. Study on the lens density of age-related nuclear cataract patients affected by hyperlipidemia. Chinese J Practical Ophthalmol. (2010) 28:1218–21. doi: 10.3760/cma.j.issn.1006-4443.2010.011.017
19. Dong, D, Lu, J, and Zhang, W. Effect of hyperlipemia on galactose induced. J Lanzhou University (Med Sci). (2010) 36:23. doi: 10.3969/j.issn.1000-2812.2010.01.005
20. Tsutsumi, K, Inoue, Y, and Yoshida, C. Acceleration of development of diabetic cataract by hyperlipidemia and low high-density lipoprotein in rats. Biol Pharm Bull. (1999) 22:37–41. doi: 10.1248/bpb.22.37
21. Galeone, C, Petracci, E, Pelucchi, C, Zucchetto, A, La Vecchia, C, and Tavani, A. Metabolic syndrome, its components and risk of age-related cataract extraction: a case-control study in Italy. Ann Epidemiol. (2010) 20:380–4. doi: 10.1016/j.annepidem.2010.01.009
22. Zhang, R, Fang, Y, Bai, S, Gao, H, Chen, H, Zhang, Z, et al. Effect of oxLDL on transcriptional expression of human lens epithelial cells. Int J Clin Exp Pathol. (2020) 13:655–63.
23. Jiang, T, Zhai, S, Yan, J, Li, Y, and Lu, Z. Association between hyperlipidemia, diabetes and age-related cataract. Int Eye Sci. (2012) 12:2098–101. doi: 10.3969/j.issn.1672-5123.2012.11.16
24. Kang, KH, Shin, D, Ryu, IH, Kim, JK, Lee, IS, Koh, K, et al. Association between cataract and fatty liver diseases from a nationwide cross-sectional study in South Korea. Sci Rep. (2024) 14:77. doi: 10.1038/s41598-023-50582-7
25. Li, T . Talk about the types, clinical symptoms and treatment methods of cataracts. Med Health. (2023) 40:15.
26. Cumming, RG, Mitchell, P, and Smith, W. Diet and cataract: the Blue Mountains eye study. Ophthalmology. (2000) 107:450–6. doi: 10.1016/s0161-6420(99)00024-x
27. Schaal, S, Beiran, I, Rozner, H, Rubinstein, I, Chevion, M, Miller, B, et al. Desferrioxamine and zinc-desferrioxamine reduce lens oxidative damage. Exp Eye Res. (2007) 84:561–8. doi: 10.1016/j.exer.2006.11.010
28. Leopold, F . Selenium, selenoproteins and vision. Dev Ophthalmol. (2005) 38:89–102. doi: 10.1159/000082770
29. Yan, J, Zhang, L, Sun, W, Zhang, D, Jiang, T, Zhai, S, et al. Relationship between dietary sodium intake, body mass index and age-related cataract. Chin J Gerontol. (2012) 32:1458–60. doi: 10.3969/j.issn.1005-9202.2012.07.061
30. Delamere, NA, Paterson, CA, and Holmes, DL. Hypocalcemic cataract. I. An animal model and cation distribution study. Metab Pediatr Ophthalmol. (1981) 5:77–82.
31. Yang, Y, Lu, J, Zhang, W, and Zhang, D. Protective effect of E-64d on calcium-induced cataract. Int Eye Sci. (2015) 15:972–5. doi: 10.3980/j.issn.1672-5123.2015.6.08
32. Dawczynski, J, Winnefeld, K, Königsdörffer, E, Augsten, R, Blum, M, and Strobel, J. Selenium and cataract--risk factor or useful dietary supplement? KLINISCHE MONATSBLATTER FUR AUGENHEILKUNDE. (2006) 223:675–80. doi: 10.1055/s-2006-926695
33. Feng, J. (2013) Effect of antioxidant nutrients on the occurrence and development of senile cataract. [dissertation’s thesis]. [Taiyuan (Shanxi)]:Shanxi Medical University.
34. Ge, Y, and Zhong, X. Progress on the antioxidant mechanisms of vitamin C and vitamin E and their applications. Jilin Medical J. (2007) 50:707–8. doi: 10.3969/j.issn.1004-0412.2007.05.066
35. Dilek, Ö, Mustafa, N, Abdullah, A, Alpay, D, Banu Kale, K, Neriman, Ç, et al. Dietary vitamin C and E modulates oxidative stress induced-kidney and lens injury in diabetic aged male rats through modulating glucose homeostasis and antioxidant systems. Cell Biochem Funct. (2011) 29:287–93. doi: 10.1002/cbf.1749
36. Maria, P . Fruit and vegetable intake and vitamins C and E are associated with a reduced prevalence of cataract in a Spanish Mediterranean population. BMC Ophthalmol. (2013) 13:52. doi: 10.1186/1471-2415-13-52
37. McNeil, JJ, Robman, L, Tikellis, G, Sinclair, MI, McCarty, CA, and Taylor, HR. Vitamin E supplementation and cataract: randomized controlled trial. Ophthalmology. (2004) 111:75–84. doi: 10.1016/j.ophtha.2003.04.009
38. Karen, AW, Caren, G, Alyssa, B, and Allen, T. Nutritional modulation of cataract. Nutr Rev. (2014) 72:30–47. doi: 10.1111/nure.12077
39. Lawrenson, JG, and Grzybowski, A. Controversies in the use of nutritional supplements in ophthalmology. Curr Pharm Des. (2015) 21:4667–72. doi: 10.2174/1381612821666150909095916
40. Christen, WG, Glynn, RJ, Chew, EY, Albert, CM, and Manson, JE. Folic acid, vitamin B6, and vitamin B12 in combination and age-related cataract in a randomized trial of women. Ophthalmic Epidemiol. (2016) 23:32–9. doi: 10.3109/09286586.2015.1130845
41. Zhou, Y, Jin, X, Qi, L, Wang, Y, Qu, Q, Zheng, M, et al. Experimental study of the abalone Shell on cataract induced by oxidative stress. Guangming J Chinese Med. (2016) 31:650–5. doi: 10.3969/j.issn.1003-8914.2016.05.021
42. Xu, GX, Cui, LJ, Lin, Y, and Wu, YB. Protective effect of haliotidis on the oxidative damage in the human lens epithelial cells. Zhonghua Yan Ke Za Zhi. (2013) 49:817–21.
43. Huang, G, Du, Q, Han, D, Yang, F, and Zhang, Y. Quercitrin alleviates selenite-induced cataract in rats by enhancing Nrf-2/HO-1 signaling pathway. Chin J Mod Appl Pharm. (2022) 39:352–7. doi: 10.13748/j.cnki.issn1007-7693.2022.03.011
44. Gu, G, Yang, W, Liang, C, and Yao, J. Correlation between NOS and SIRT1 mRNA levels in lens and oxidative stress in patients with cortical cataract and its diagnostic value. Med Health. (2023) 33:587–91.
45. Liu, XF, Hao, JL, Xie, T, Malik, TH, Lu, CB, Liu, C, et al. Nrf2 as a target for prevention of age-related and diabetic cataracts by against oxidative stress. Aging Cell. (2017) 16:934–42. doi: 10.1111/acel.12645
46. Gao, Y, Yan, Y, and Huang, T. Human age-related cataracts: epigenetic suppression of the nuclear factor erythroid 2-related factor 2-mediated antioxidant system. Mol Med Rep. (2015) 11:1442–7. doi: 10.3892/mmr.2014.2849
47. Song, MS, Sim, HJ, Kang, S, Park, S, Seo, K, and Lee, SY. Pharmacological inhibition of Kv3 on oxidative stress-induced cataract progression. Biochem Biophys Res Commun. (2020) 533:1255–61. doi: 10.1016/j.bbrc.2020.09.138
48. Jiang, H, Yin, Y, Wu, C, Liu, Y, Guo, F, Li, M, et al. Dietary vitamin and carotenoid intake and risk of age-related cataract. Am J Clin Nutr. (2019) 109:43–54. doi: 10.1093/ajcn/nqy270
49. Ma, YN . (2019). Relationship between dietary flavonoid intake and age-related cataract [dissertation’s thesis]. [Harbin (Heilongjiang)]:Harbin Medical University.
50. Shivappa, N, Hebert, JR, Assadi, M, Rashidkhani, B, and Ghanavati, M. Inflammatory potential of diet is associated with increased odds of cataract in a case-control study from Iran. Int J Vitamin and Nutrition Res: Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. (2017) 87:17–24. doi: 10.1024/0300-9831/a000420
51. Wu, X, Liu, Z, Wang, D, Lin, D, Long, E, Lin, Z, et al. Preoperative profile of inflammatory factors in aqueous humor correlates with postoperative inflammatory response in patients with congenital cataract. Mol Vis. (2018) 24:414–24.
52. Liu, Y, Yin, X, Chen, Y, Shi, R, and Dong, Y. Changes of inflammatory related factors in aqueous humor and serum of patients with diabetes cataract and their correlation with glucose metabolism. J Clin Experimental Med. (2023) 22:2300–3. doi: 10.3969/j.issn.1671-4695.2023.21.016
53. Chen, Y, Luo, J, Zhu, J, Meng, Y, Ji, M, and Guan, H. Advances in the role of glycosylation in the pathogenesis of diabetic cataract. Recent Advan Ophthalmol. (2023) 43:819–22. doi: 10.13389/j.cnki.rao.2023.0165
54. Zhuo, Y. (2023) Correlation of oxidative stress-induced E2F1 nuclear entry mediating increased THBS 1 expression with apoptosis in lens epithelial cells and diabetic cataract. [master’s thesis]. [Hefei(Anhui)]:Anhui Medical University.
55. Chen, Y, and Peng, J. Effect of miR-124 on apoptosis of Lens epithelial cells in diabetic Cataractous patients and its mechanism. J Nanchang University:Medical Sci. (2022) 62:9–15. doi: 10.13764/j.cnki.ncdm.2022.01.002
56. Gao, C, and Wu, J. Research progress on pathogenesis and drug treatment of diabetic cataract. Eye Sci. (2020) 35:234–42. doi: 10.3978/j.issn.1000-4432.2020.09.01
57. Xie, Q, Xue, L, Cao, X, Huang, L, and Song, Y. Apoptosis of Lens epithelial cells and expression of NLRP3-related proteins in patients with diabetes and cataract. Ocul Immunol Inflamm. (2023) 31:1103–10. doi: 10.1080/09273948.2022.2079537
58. Townend, BS, Townend, ME, Flood, V, Burlutsky, G, Rochtchina, E, Wang, JJ, et al. Dietary macronutrient intake and five-year incident cataract: the blue mountains eye study. Am J Ophthalmol. (2007) 143:932–939.e1. doi: 10.1016/j.ajo.2007.03.006
59. Yuan, J, Yu, Z, Gao, J, Luo, K, Shen, X, Cui, B, et al. Inhibition of GCN2 alleviates hepatic steatosis and oxidative stress in obese mice: involvement of NRF2 regulation. Redox Biol. (2022) 49:102224. doi: 10.1016/j.redox.2021.102224
60. Chen, H. (2021) Analysis of factors related to posterior recurrent cataract in patients with age-related cataract. [master’s thesis]. [Nanning(Guangxi)]: Guangxi Medical College.
61. Altomare, E, Vendemiale, G, Grattagliano, I, Angelini, P, Micelli-Ferrari, T, and Cardia, L. Human diabetic cataract: role of lipid peroxidation. Diabetes Metab. (1995) 21:173–9.
62. Spiteller, G . Lipid peroxidation in aging and age-dependent diseases. Exp Gerontol. (2001) 36:1425–57. doi: 10.1016/s0531-5565(01)00131-0
63. Jia, Y, Song, P, Zhou, J, and Zhong, N. Effects of zinc on expression and activity of cu/Zn-SOD in human lens epithelial cells induced by SIN-1. Recent Advan Ophthalmol. (2017) 37:24–7. doi: 10.13389/j.cnki.rao.2017.0006
64. Song, N, and Gao, Q. An experimental research of the relationship between cataract and zinc contents in blood and eyeballtissue. J Hubei Medical Staff College. (2001) 14:1–3.
65. Philip, AJP, Fjelldal, PG, Remø, S, Silva, M, Holme, M, Lock, E, et al. Dietary zinc, selenium and water temperature during early seawater phase influences the development of vertebral deformities and cataract in adult Atlantic salmon. Aquaculture. (2023) 572:739529. doi: 10.1016/j.aquaculture.2023.739529
66. Rose, R, and Kartadinata, E. Decreased erythrocyte superoxide dismutase in elderly men with early nuclear cataract. Universa Medicina. (2014) 33:65–72. doi: 10.18051/Univ
67. Olofsson, EM, Marklund, SL, and Behndig, A. Enhanced diabetes-induced cataract in copper-zinc superoxide dismutase-null mice. Invest Ophthalmol Vis Sci. (2009) 50:2913–8. doi: 10.1167/iovs.09-3510
68. Yin, N. (2016) Inhibition of the 15kDa selenoprotein (Sep15) on Chitlamycin-induced lens cell differentiation disorder. [dissertation’s thesis]. [Wuhan(Hubei)]: Huazhong University of Science and Technology.
69. JiTao, S . Research of selenium in preventing and treating eye disease. Trace Elements Sci. (2011) 18:22–5. doi: 10.3969/j.issn.1006-446X.2011.10.002
70. Liu, X . Current status of selenium-induced cataract research. Stud Trace Elements and Health. (2000) 17:68–79.
71. Li, S . Progress on clinical application of selenium. Trace Elements Sci. (2009) 16:8–12. doi: 10.3969/j.issn.1006-446X.2009.07.002
72. Tan, S, Yang, Y, Wu, F, and Shi, K. Exploring the therapeutic effect of selenium on cataract. Chinese J Practical Ophthalmol. (1995) 13:3.
73. Gao, X, and Jin, Z. Micro elements and senile cataract. Stud Trace Elements and Health. (2003) 20:51–3. doi: 10.3969/j.issn.1005-5320.2003.04.025
74. Chen, Y, Wang, D, Deng, R, and Li, X. Trace element selenium and health. Trace Elements Sci. (2001) 8:6–9. doi: 10.3969/j.issn.1006-446X.2001.02.002
75. Mao, L, Xu, X, Chen, P, Gu, Y, and Zhen, M. Analysis of the concentrations of three inorganic ions in the aqueous humor and serum of patients with age-related cataract. Modern Practical Med. (2012) 24:1180–2. doi: 10.3969/j.issn.1671-0800.2012.10.055
76. Ren, X, Zhao, H, Hu, S, Sun, L, and Gu, Y. A study of dynamic changes on +, K+~, Mg2+ and Zn2+ in sugar Cataractous rat lenses. Chin Ophthalmic Res. (1991) 12:203.
77. Tabassum, R, Syed Sadaf, A, Shabhat, R, Rabiya, I, Sabia, R, Sabhiya, M, et al. Impact of clinico-biochemical variations on the etiopathogenesis of cataract: a case-control study. J circulating biomarkers. (2023) 12:1–11. doi: 10.33393/jcb.2023.2479
78. Chowdary, CC, V, S, and Y, JR. Study of changes in serum electrolytes and its risk in development of senile cortical cataract. J Evol Med Dent Sci. (2018) 7:3115–8. doi: 10.14260/JEMDS/2018/700
79. Gaurav, M, and Vijaya, P. Comparison of serum sodium and potassium levels in patients with senile cataract and age-matched individuals without cataract. Indian J Ophthalmol. (2016) 64:446–7. doi: 10.4103/0301-4738.99837
80. Pakhomova, NA, Borisenko, TE, Roshchin, SV, Bursov, AI, Kravchik, MV, Novikov, IA, et al. Features of accumulation of chemical elements in the volume of the lens in senile cataract. Vestn oftalmol. (2023) 139:35–45. doi: 10.17116/oftalma202313901135
81. Yao, Y. (2014) Study of the effects of changes in extracellular Ca2 + concentration on ER stress in human lens epithelial cells. [master’s thesis]. [Fuzhou(Fujian)]: Fujian Medical College.
82. Wang, X, Wu, K, and Zeng, J. Effects of calcium on glucocorticoid-induced cataract in chicken embryo. Chin Ophthalmic Res. (2005) 23:125–7. doi: 10.3760/cma.j.issn.2095-0160.2005.02.004
83. Wei, Y. (2013) Effects of intracellular Ca2 + concentration changes in lens epithelial cells on AQP 1 expression and cellular activity. [master’s thesis]. [Fuzhou(Fujian)]: Fujian Medical College.
84. Cui, H, Wang, J, and Yang, Q. Analysis of calcium ion changes in aqueous humor in patients with senile cataract. Zhejiang Medical J. (1999) 21:2.
85. Liu, X, Fang, Q, Yan, M, and Wu, Z. Study on the regulation of calcium in the human Normal and senile Cataractous lenses. Chin Ophthalmic Res. (1996) 28:2–7.
86. Wen, X. (2002) Role of calpain in the mechanism of hydrogen peroxide-induced cataracts ogenesis and the prevention of oxidative cataract. [dissertation’s thesis]. [Hangzhou(Zhejiang)]:Zhejiang University.
87. Duan, S, and Feng, R. Hypoparathyroidism cataract. Chinese J Practical Ophthalmol. (2004) 22:10. doi: 10.3760/cma.j.issn.1006-4443.2004.01.024
88. Feng, J. (2012) Effect of antioxidant nutrients on the occurrence and development of senile cataract. [master’s thesis]. [Taiyuan(Shanxi)]: Shanxi Medical College.
89. Zhang, R, Tong, Y, Cheng, L, Mou, Y, and Wen, S. Clinical applications and research advances of natural antioxidants. Shandong Chemical Industry. (2020) 49:48–52. doi: 10.3969/j.issn.1008-021X.2020.22.018
90. Lian, J . Food that is conducive to eye health care. Family & Traditional Chinese Med. (2021) 29:28–9.
91. Li, X, Liu, X, Lu, L, He, Y, and Wang, L. Research progress of oxidative stress and diabetic cataract. Medical J National Defending Forces in Northwest China. (2020) 41:457–62. doi: 10.16021/j.cnki.1007-8622.2020.07.014
93. Li, G, and Chen, C. The mechanism and efficacy of antioxidant treatment for cataract. Foreign Medical Sci(Section of Ophthalmol). (1992) 16:110–4.
94. Wang, J . The relationship between oxidation and cataract and antioxidants in the treatment of cataract. Recent Advan Ophthalmol. (1995) 15:2.
95. Zhu, Z, Du, J, Zhang, Q, Guo, F, and Ma, L. Effects of lutein on the prevention and treatment of age-related cataract. Modern Prevent Med. (2014) 41:3.
96. Jiang, H, Li, R, and Ma, L. Correlation between dietary antioxidant intake and the development of age-related cataract. Medicine and Health (2017)
Keywords: cataract, nutrition, oxidative stress, insulin resistance, micronutrients, inflammatory factors
Citation: Zhang Y, Qin X, Xu T, Chu F and He B (2024) Research progress on the correlation between cataract occurrence and nutrition. Front. Nutr. 11:1405033. doi: 10.3389/fnut.2024.1405033
Edited by:
Arunkumar Ranganathan, The University of Utah, United StatesReviewed by:
David Pei-Cheng Lin, Chung Shan Medical University, TaiwanCopyright © 2024 Zhang, Qin, Xu, Chu and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beihui He, Z3JhZjMwM0BzaW5hLmNvbQ==
†These authors have contributed equally to this work
 Yi Zhang
Yi Zhang Xiang Qin
Xiang Qin Tianyu Xu†
Tianyu Xu† Beihui He
Beihui He