- 1Department of Ophthalmology, The Second Hospital of Jilin University, Jilin University, Changchun, China
- 2The First Hospital of Jilin University, Jilin University, Changchun, China
Objective: Although numerous studies have substantiated the neuroprotective effects of vitamin B6 on the optic nerve and its enhancement of visual function, comprehensive data delineating the correlation between vitamin B6 and glaucoma at a national demographic scale remain insufficient. This study is designed to explore the link between the dietary consumption of vitamin B6 and glaucoma.
Methods: This study included 3,850 individuals aged 40 and older from the National Health and Nutrition Examination Survey (NHANES), spanning 2005–2008. Dietary consumption of vitamin B6 was calculated from the average of two 24-h dietary recall interviews. Glaucoma was diagnosed in accordance with the established Rotterdam criteria. To evaluate the relationship between vitamin B6 dietary consumption and the risk of glaucoma, we employed Restricted Cubic Splines and weighted multivariable logistic regression analysis. We employed stratified and three other sensitivity analyses to confirm the robustness of our results, and conducted a preliminary exploration of the potential association between vitamin B6 supplement consumption and glaucoma risk.
Results: After adjusting for covariates, we found a significant inverse correlation between dietary consumption of vitamin B6 and glaucoma risk (pnon-linearity = 0.18; p for trend = 0.02). Stratified analysis and three other sensitivity analyses revealed stability in the outcomes (all p for interaction>0.05). Compared to the lowest quartile of consumption (≤1.23 mg/day), individuals in the highest quartile of vitamin B6 consumption (>2.34 mg/day) experienced a 75% reduction in glaucoma risk (OR = 0.25, 95% CI 0.07–0.92). However, the effect of vitamin B6 supplements on glaucoma was inconclusive.
Conclusion: A diet high in vitamin B6 inversely correlates with glaucoma risk, suggesting that increasing dietary intake of vitamin B6 could be a viable preventative strategy against glaucoma among adults in the United States.
1 Introduction
Glaucoma, a leading global cause of irreversible vision loss, affects over 80 million individuals worldwide (1, 2). This condition is characterized by the progressive degeneration of retinal ganglion cells (RGCs) and their axons. Key risk factors for glaucoma include advanced age and elevated intraocular pressure (IOP) (3). The prevailing treatment strategy for glaucoma primarily revolves around the reduction of IOP. However, a significant subset of patients who effectively manage their IOP continue to experience progressive visual impairment. This phenomenon has sparked intense scientific investigation into alternative therapeutic approaches.
In glaucoma, RGC death occurs through apoptosis, triggered by various mechanisms such as mechanical damage and ischemic changes due to high IOP, both contributing to oxidative stress. Additional glaucoma risk factors, such as advanced age, genetic predispositions, and inflammatory processes, also precipitate oxidative stress through distinct biological pathways (4–7). RGCs, with their high energy demands, are particularly vulnerable to fluctuations in cellular fuel supply (8). Oxidative stress can lead to mitochondrial dysfunction and compromised ATP synthesis, causing irreparable cellular damage and ultimately resulting in the loss of RGCs (9–13). Furthermore, research suggests that oxidative stress may exacerbate damage to the trabecular meshwork (TM) in the eye, thereby increasing IOP and perpetuating a vicious cycle (14). Hence, oxidative stress is instrumental in the pathogenesis of glaucoma, constituting a crucial element of the alterations associated with glaucoma.
Emerging evidence suggests that antioxidant-rich diets, serving as an alternative therapy, can play a minimally invasive role in managing disease progression and significantly prevent glaucoma (15, 16). Specifically, vitamin B6, known for its antioxidant properties, shows potential in neuroprotection and improving visual function (15, 17). For instance, animal model experiments by Wang et al. (18) have revealed that vitamin B6 can counteract neuronal death in adult primate retinas following ischemia. Meanwhile, clinical trials by Mallone et al. (19) indicate that high-dose administration of vitamins B1, B6, and B12 significantly enhances visual function metrics in cases of chronic visual impairment associated with multiple sclerosis. Furthermore, Ruamviboonsuk et al. (20) have proposed that a 6-month regimen combining vitamins B6, B9, and B12 significantly enhances retinal sensitivity and thickness in patients with mild to moderate non-proliferative diabetic retinopathy Additionally, a case report by Xuan Cui et al. suggests that supplementation with vitamin B6 positively affects the delay of Gyrate atrophy (21).
Concurrently, the relationship between vitamin B6 and the broader group of B vitamins with glaucoma is increasingly being studied and discussed at various levels. Li et al. (22) conducted a meta-analysis to examine the association between serum levels of vitamins B6, B12, and D across various types of glaucoma. Their findings indicated no significant link between serum vitamin B6 levels and glaucoma. Similarly, meta-analyses by Xu et al. (23) and Li et al. (24) on non-ocular risk factors for primary glaucoma corroborated these results. In contrast, clinical research led by Rolle et al. (25) demonstrated that supplements containing vitamins B2, B6, and folic acid could decelerate the progression of functional impairment in patients with primary open-angle glaucoma and enhance visual function. Additionally, a recent cross-sectional study by Lee et al. (26) exploring the relationship between niacin intake and glaucoma incorporated the intake of vitamins B2 and B6 as covariates in their model. However, direct research linking dietary intake of vitamin B6 to glaucoma is relatively scarce and tends to focus on specific types of the condition (27), such as the prospective study by Walter Willet and others on exfoliative glaucoma and its suspected cases in relation to folic acid, vitamin B6, and B12 (27). As a nationally representative cross-sectional study, this research aims to utilize NHANES data to explore the potential relationship between dietary vitamin B6 intake and glaucoma in the U.S. population.
2 Materials and methods
2.1 Study population
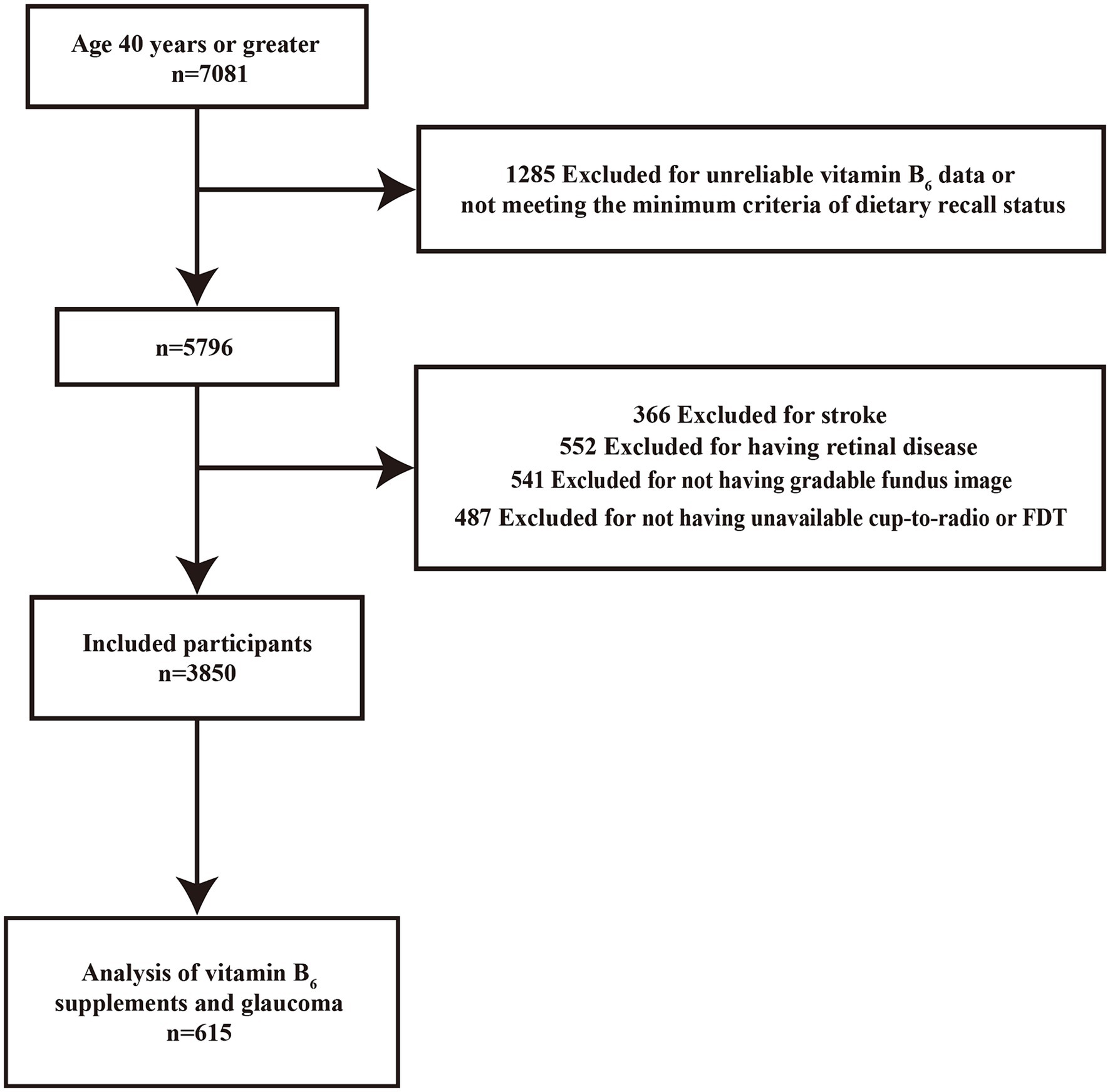
The National Health and Nutrition Examination Survey (NHANES), conducted biennially, is a national epidemiological cross-sectional study that utilizes a stratified multistage cluster sampling design to collect health and nutrition data from the U.S. population (28). Additional information about this survey is available on its official website (29). This study adheres to strict ethical standards, ensuring that all participants voluntarily provided informed consent. Our research utilized data collected from 2005 to 2008 by NHANES, involving 7,081 individuals aged 40 and older who underwent eye examinations. We excluded participants who did not attend two dietary interviews or lacked vitamin B6 dietary data (n = 1,285), those without gradable fundus photographs (n = 541), participants with unavailable or unusable frequency doubling technology (FDT) visual field test results or cup-to-disc ratio data (n = 487), and those with abnormal FDT results or cup-to-disc ratios likely due to alternative causes such as cerebrovascular disease (n = 366) or various retinal diseases (n = 552). After these exclusions, 3,850 participants were included in the final analysis. Given that the missing values in all confounding variables were less than 5% of the final sample size, based on existing literature (30), we considered such a small proportion of missing data unlikely to introduce significant bias into our results. Therefore, we did not exclude these participants from our analysis. Baseline characteristics of included and excluded participants are detailed in Supplementary Table S1. Of the final sample, data on vitamin B6 supplement intake was available for 615 participants; this data was analyzed to investigate the association between vitamin B6 supplement intake and the incidence of glaucoma (Figure 1).
2.2 Exposure and outcome variables
The principal exposure in this study is the intake of vitamin B6 in daily diets, derived from the Dietary Interview component of the dataset. This dataset focuses on collecting and analyzing dietary habits and nutrient intake across the U.S. population (31, 32). In our study, all eligible participants underwent two 24-h dietary recall interviews. These interviews detailed the types and quantities of food consumed in the 24 h preceding each interview. The initial interview was conducted at the Mobile Examination Center (MEC) (32), followed by a second interview via telephone 3 to 10 days later (33). We calculated the average of two interview sessions to estimate the final intake of vitamin B6, which potentially provides a closer approximation of the participants’ usual dietary intake compared to using data from a single interview.
The main result was the identification of glaucoma according to the Rotterdam Criteria, which considered the participants’ abnormalities in the visual field and the appearance of the optic nerve. In NHANES, optic nerve morphology was evaluated by optic nerve imaging, and FDT was used to measure glaucoma visual field defects. Glaucoma was clinically diagnosed if at least one eye exhibited a positive FDT result, combined with a CDR in one eye or CDR asymmetry across both eyes, meeting or exceeding 97.5% of the average NHANES population’s threshold (34–36).
In NHANES, trained technicians performed the FDT examination under dark conditions. Each eye underwent testing at 19 visual field locations, ensuring comprehensive assessment. The FDT outcome was classified as positive (using the 2–2-1 algorithm) if a minimum of two locations fell beneath the 1% threshold level in both initial and subsequent tests, with at least one identical failed location in both assessments (37). The CDR was ascertained through the analysis of two 45° non-mydriatic retinal digital images, captured by proficient technicians. Each image underwent review by a minimum of three trained graders. If the CDR scores from at least two of the three graders deviated by no more than 0.1, the outcome was established based on the median score. If the score difference between any two graders is greater than 2.2, the image was reviewed again with all graders present to reach a consensus (38).
2.3 Covariates
We conducted an extensive review of existing clinical research and practices related to glaucoma, including 20 potential confounding variables in our model to ensure reliability. These variables include age, sex, race, marital status, education level, household income, total caloric intake, Body Mass Index (BMI), alcohol consumption, waist circumference, diabetes, hypertension, cardiovascular disease (CVD), serum total cholesterol, C-reactive protein (CRP) levels, and dietary consumption of vitamins B1, B2, B3, B9, and B12 (26, 27, 35, 39, 40). The first six of these variables, pertaining to sociodemographic information, were gathered through personal interviews (41). The intake levels of these vitamins were obtained from dietary interviews, which also accounted for total energy and alcohol consumption (32, 33). For our study, CVD was defined to include any heart-related conditions, such as congestive heart failure, coronary artery disease, angina, or myocardial infarction. Diabetes was classified based on a physician’s diagnosis, the use of insulin or oral hypoglycemic agents, fasting plasma glucose levels ≥7.0 mmol/L, or glycated hemoglobin values ≥6.5%. Additionally, hypertension was characterized by a systolic blood pressure ≥ 130 mmHg or a diastolic blood pressure ≥ 80 mmHg, ascertained by the mean of three consecutive readings, a self-disclosed history of hypertension, or the administration of antihypertensive medication (42, 43). Waist circumference measurements and BMI were obtained in the MEC (44), and non-fasting blood samples collected there were sent to laboratory for analysis to obtain total serum cholesterol levels and CRP (45–47). Due to the missing values of the covariate “smoking” reaching 47% of the study population, it could introduce significant bias to the statistical results. Therefore, this variable was not included in the adjusted covariates in this study.
2.4 Exploratory analysis of supplemental consumption of vitamin B6
Vitamin B6 supplements were introduced as exploratory variables to evaluate the potential influence of different sources of vitamin B6 on the risk of glaucoma. The consumption of supplemental vitamin B6 was determined by averaging data from two 24-h dietary recall interviews with participants.
2.5 Statistical analysis
We conducted weighted analyses using dietary sample weights from NHANES, adapting these to its complex survey sampling design and multilevel clustering. Continuous variables were described using weighted means with accompanying standard errors (SE), and categorical variables were presented as frequencies. The aim was to compare the distribution of potential confounding factors between participants with and without glaucoma. To assess the impact of the distribution of variables, the continuous exposure variables of dietary and supplemental intake of vitamin B6 were converted into quartiles. This process involves arranging the data in ascending order based on the values of the exposure variables, and then determining the quartiles’ cutoff values at the 25th, 50th, and 75th percentiles. These cutoff values divide the dataset into four approximately equal groups, allowing evaluation of the impact of varying levels of exposure variables on the outcome. Similarly, the division into quintiles follows a similar method, with cutoff values at the 20th, 40th, 60th, and 80th percentiles.
Three analytical models were constructed: a base model without adjustment, Model 1 with adjustments for age and sex, and Model 2, which extended these adjustments to include all relevant confounders. Building on Model 2, we first analyzed vitamin B6 dietary consumption as a continuous variable using Restricted Cubic Splines (RCS) method. By positioning three knots at the 10th, 50th, and 90th percentiles, we used the likelihood ratio test to assess its association with glaucoma risk. Subsequently, we utilized the quartiles of dietary intake and supplemental intake of vitamin B6, exploring their association with the risk of glaucoma using a weighted logistic regression model.
To bolster the validity of our research outcomes, we used subgroup analysis, accounting for various dimensions including age, race, sex, marital status, household income, education level, diabetes, CVD, and hypertension. This was to assess the consistency and stability of the results across different population groups. Additionally, we conducted three types of sensitivity analyses: (1) an unweighted logistic regression analysis of the sample; (2) an analysis of vitamin B6 dietary intake divided into quintiles; and (3) an analysis excluding all participants with missing values in the confounding variables.
All statistical tests were conducted as two-tailed, with a significance level set at p < 0.05. Analytical procedures were executed using R 4.3.1.
3 Results
3.1 Baseline characteristics
The research included 3,850 unweighted participants and 96,323,492 weighted participants, all aged 40 or above, who participated in dietary interviews and had accessible fundus imaging and FDT test data. Out of these, 151 were identified as having glaucoma as per the study’s definition, making up 3.9% of the unweighted population. In the weighted population, the proportion of glaucoma was 2.6% (n = 2,463,459). The findings indicated that among those with glaucoma, there was a significantly higher proportion of participants who were older, non-Hispanic black, not married, and had diabetes, hypertension, CVD, lower CRP, larger waist circumference, and lower total serum cholesterol levels, along with lower intake of vitamins B3 and B12 (all p < 0.05). No notable differences were detected among participants in sex, household income, education level, total energy consumption, BMI, alcohol consumption, vitamin B1, B2 and B9 intake, irrespective of their glaucoma status (all p > 0.05) (Supplementary Table S2).
3.2 Vitamin B6 dietary consumption and glaucoma
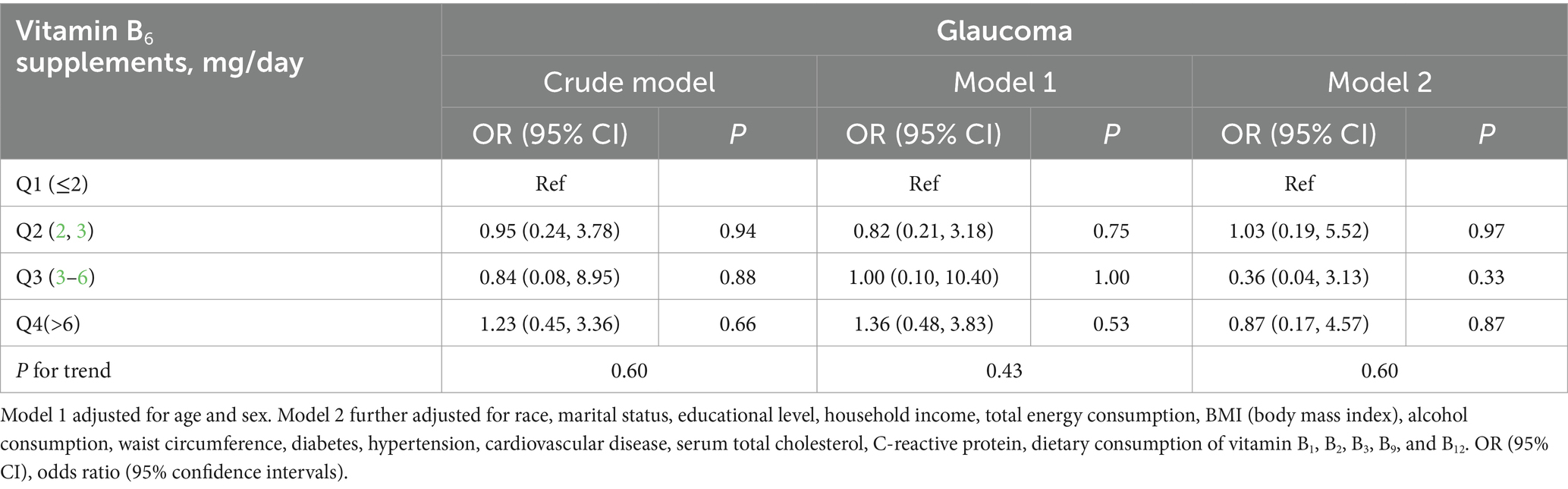
The average dietary consumption of vitamin B6 among all eligible participants was 1.96 mg/day (SE 0.02). Notably, the average vitamin B6 dietary consumption in the glaucoma group [1.82 (SE 0.10) mg/day] was markedly inferior to that in the non-glaucoma group [2.04 (SE 0.03) mg/day] (p = 0.02). Based on the fully adjusted Model 2, the RCS analysis indicated no significant non-linear correlation between dietary vitamin B6 consumption and glaucoma risk (p overall = 0.02, p non-linearity = 0.18) (Figure 2).
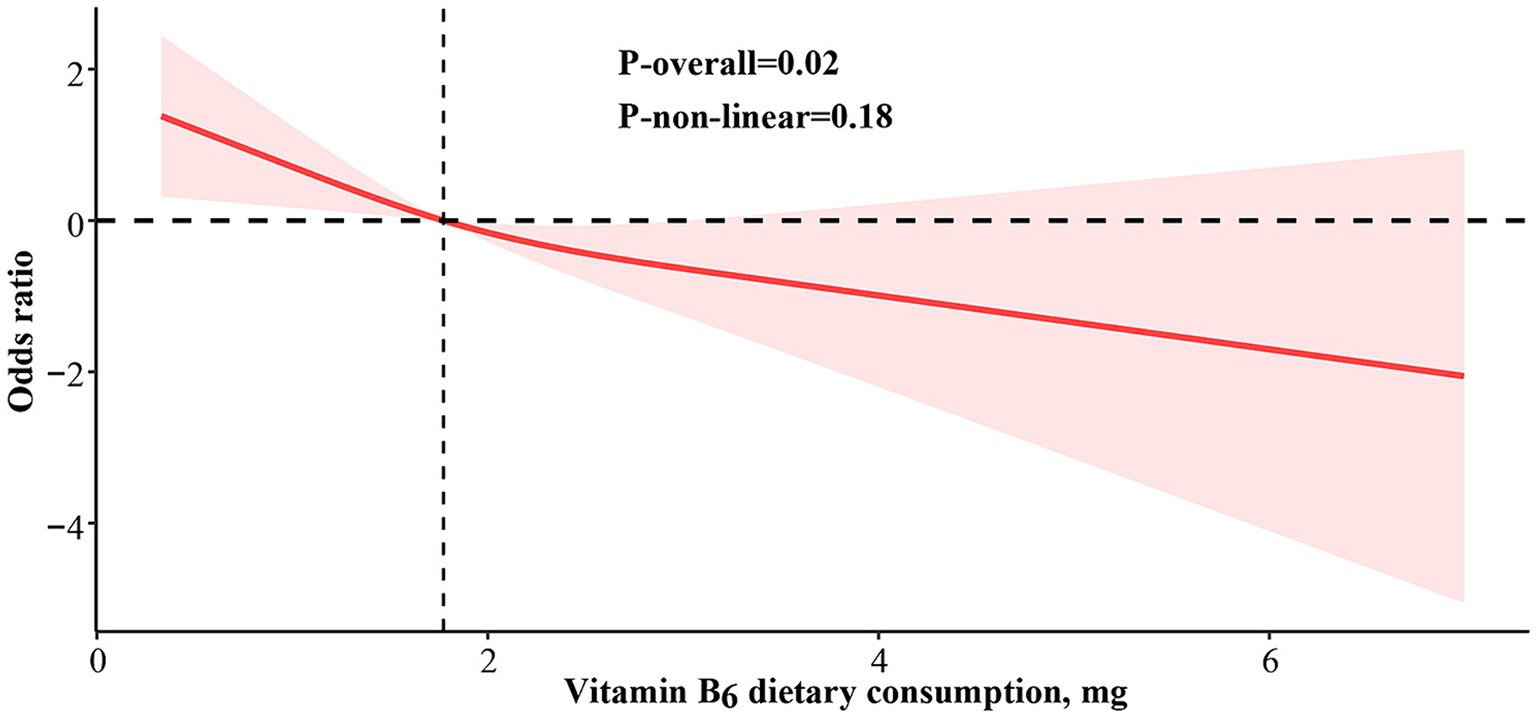
Figure 2. Restricted cubic spline analysis of vitamin B6 dietary consumption and odds ratio of glaucoma based on Model 2, which was adjusted for age, sex, race, marital status, educational level, household income, total energy consumption, BMI (body mass index), alcohol consumption, waist circumference, diabetes, hypertension, cardiovascular disease, serum total cholesterol, C-reactive protein, dietary consumption of vitamin B1, B2, B3, B9 and B12.
To delve deeper into the potential linear correlation between the consumption of dietary vitamin B6 and glaucoma, we divided vitamin B6 dietary consumption into four quartiles: Q1 (first) (≤1.23 mg/day), Q2 (second) (>1.23 to ≤1.70 mg/day), Q3 (third) (>1.70 to ≤2.34 mg/day), and Q4 (fourth) (>2.34 mg/day). The outcomes from the logistic regression model revealed a substantial negative linear correlation between glaucoma and vitamin B6 dietary consumption in the crude model (p for trend = 0.003), with a notable reduction in glaucoma proportion in the higher quartiles of vitamin B6 dietary consumption compared to the lowest quartile (Q3: OR 0.53, 95% CI 0.32–0.88; Q4: OR 0.42, 95% CI 0.24–0.75). This inverse linear correlation persisted even after controlling for covariates. (Model 1: Q3: OR = 0.50, 95% CI 0.29–0.84; Q4: OR = 0.38, 95% CI 0.20–0.73; p for trend = 0.004; Model 2: Q3: OR = 0.43, 95% CI 0.21–0.86; Q4: OR = 0.25, 95% CI 0.07–0.92 p for trend = 0.02). (Table 1).
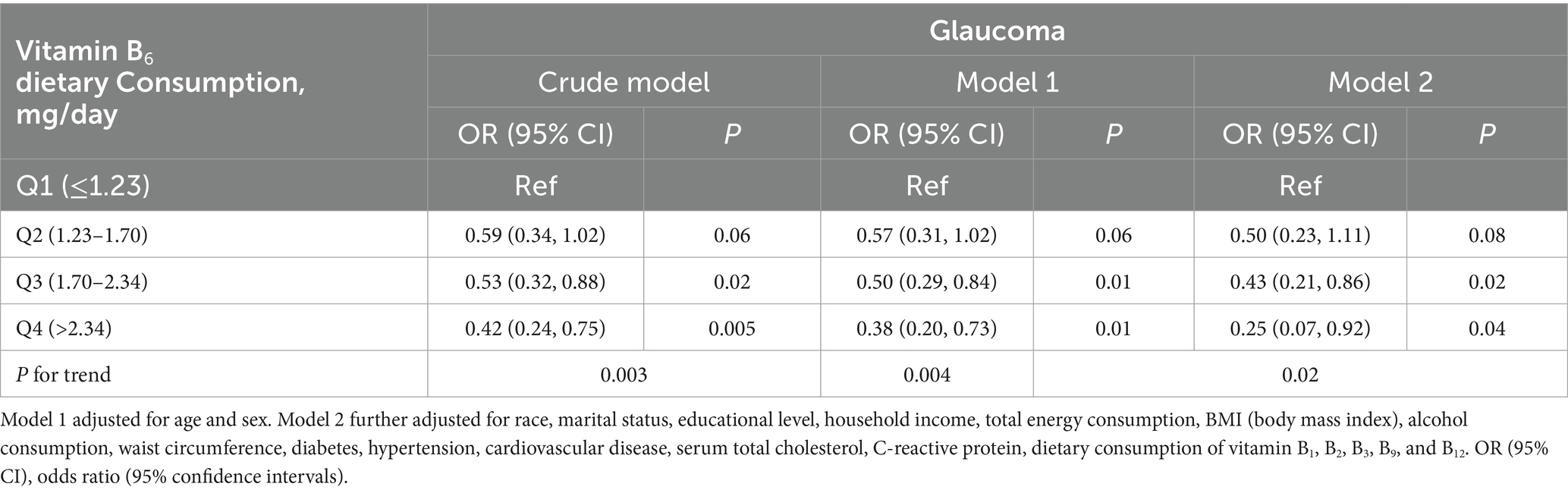
Table 1. Results of weighted logistic regressions between vitamin B6 dietary consumption and risk of glaucoma.
3.3 Sensitivity analysis
Subgroup analysis revealed no significant interactions between dietary vitamin B6 consumption and variables such as age, race, sex, marital status, family income, educational level, diabetes, CVD, and hypertension (all p for interaction >0.05) (Figure 3). Additionally, in our three sensitivity analyses, the results remained robust: (1) unweighted logistic regression analysis was conducted on the sample; (2) dietary intake of vitamin B6 was analyzed by dividing it into quintiles; (3) analysis was performed after excluding all participants who had missing values in the confounding variables (Supplementary Tables S3–S6).
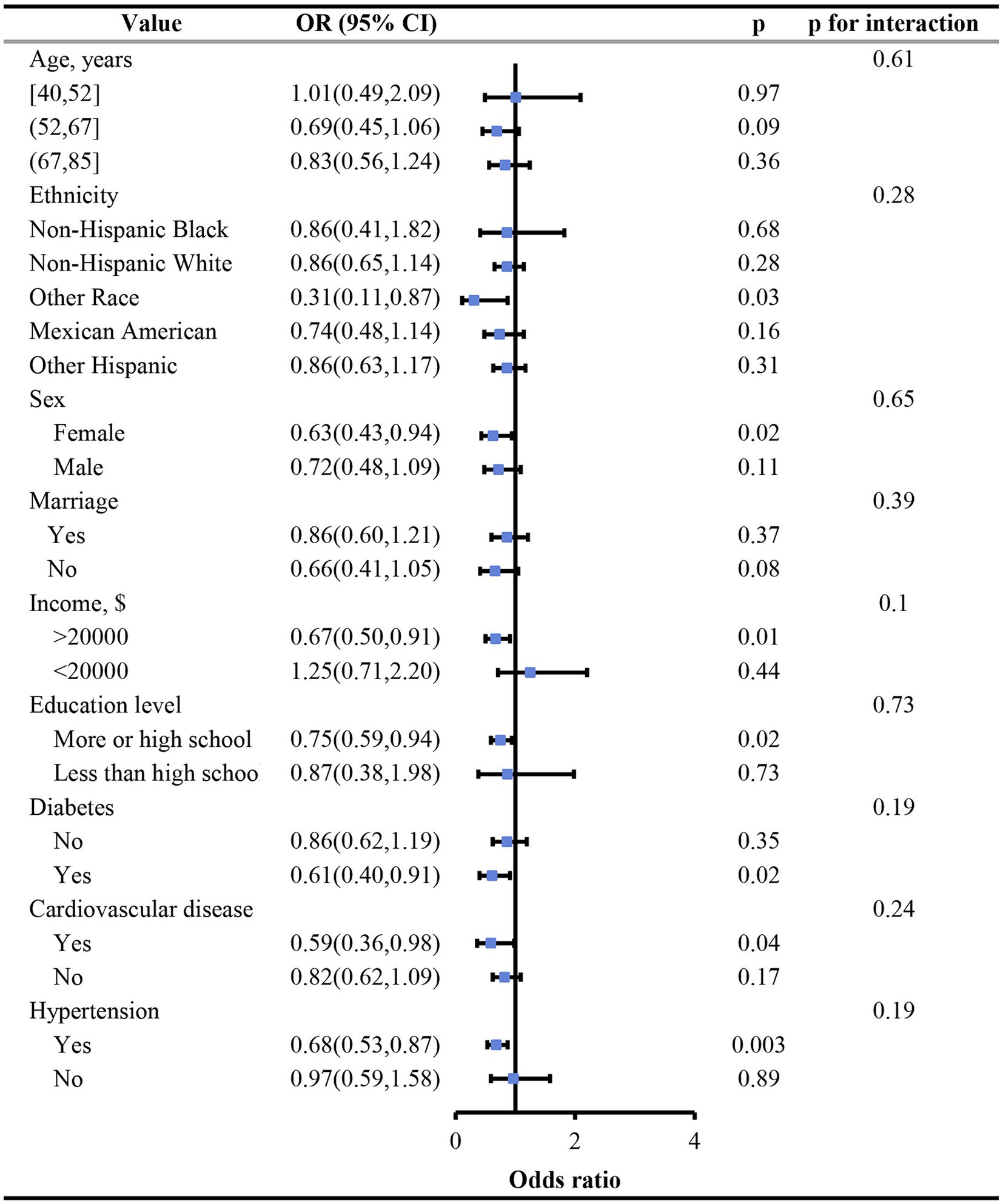
Figure 3. Subgroup analysis of correlation between vitamin B6 dietary consumption and glaucoma stratified by age, race, sex, marital status, household income, education level, diabetes, cardiovascular disease and hypertension.
3.4 Vitamin B6 supplements shows no negative correlation with glaucoma
To investigate the impact of vitamin B6 supplement consumption on glaucoma, we conducted a multivariate regression analysis examining the association between vitamin B6 supplement intake and glaucoma incidence. The results indicated that the vitamin B6 supplements consumption exhibited no association with glaucoma (Table 2).
4 Discussion
In our study involving 3,850 Americans aged 40 and older, we discovered a significant independent linear negative correlation between dietary intake of vitamin B6 and the risk of glaucoma. This relationship remained robust even after adjusting for multiple potential confounders. Relative to the first quartile of vitamin B6 dietary consumption, which falls below the Recommended Dietary Allowance (RDA) of 1.6 mg/day for men and 1.4 mg/day for women, the odds of developing glaucoma dropped by 75% for individuals in the fourth quartile (>2.34 mg/day) (OR = 0.25, 95% CI 0.07–0.92). Additionally, we found no significant correlation between consumption of vitamin B6 supplements and glaucoma risk.
In light of these results, our review of existing research indicates that there is still debate over whether vitamins from natural dietary sources and synthetic supplements are equivalent in terms of bioavailability and metabolic effects (48). While studies by Nelson et al. (49) suggest that vitamin B6 from supplements has a higher absorption efficiency, research by Meinrad Lindschinger shows that natural and synthetic B vitamins are roughly equivalent in bioavailability. However, natural vitamin B6 not only improves serum vitamin B6 concentrations more effectively compared to its synthetic counterpart but also has a stronger impact on metabolic parameters like homocysteine levels and total antioxidant capacity (48). Additionally, there is currently no evidence to suggest that consuming large amounts of vitamin B6 from food leads to adverse effects (50). However, multiple reports indicate that long-term excessive use of vitamin B6 supplements can cause adverse reactions (50–53). Additionally, the discrepancy in our findings might be attributed to significant data loss among supplement users, reducing the sample size from 3,850 to 615, potentially introducing substantial bias into the results. Given the limitations of NHANES data, we could not further explore the relationship between these variables. Considering the controversies in existing research, we believe that comparing the efficacy of different sources of vitamin B6 is a crucial direction for future studies.
Contrarily, our study findings diverge from those reported by JaeH Kang and his colleagues, who conducted a thorough cohort study identifying no significant link between vitamin B6 intake and the risk of exfoliative glaucoma or its suspected cases. We hold their work in high regard for its rigor and evidential strength (27). The variations in our results likely stem from several key factors: Firstly, our research included all types of glaucoma, not just exfoliative glaucoma, which is estimated to constitute about 25% of all open-angle glaucoma cases (54). Secondly, our method for assessing vitamin B6 intake, based on 24-h dietary recall interviews, differed from Kang’s team, who used a long-term average intake method. Additionally, in the study populations, Kang and colleagues included female registered nurses and male health professionals, whereas our study population is based on NHANES data and broadly involves non-institutionalized civilians across the United States. There may be some degree of demographic and sociological differences between the two study populations. These factors highlight the diversity of research designs, which may explain differences in study outcomes. These key elements are worthy of further exploration and discussion in future research.
Given the discrepancies in existing research findings, a deep understanding of the biochemical roles and mechanisms of vitamin B6 is particularly crucial. Vitamin B6, a coenzyme essential for countless biochemical reactions, comprises six compounds (55). These include pyridoxal, pyridoxamine, pyridoxine, and their 5′-phosphate esters (56). Pyridoxal-5′-phosphate (PLP), known as the biologically active form of vitamin B6 in humans, is often used interchangeably with the term “Vitamin B6” (57, 58).
One potential protective mechanism of vitamin B6 against glaucoma may be its antioxidant activity. Pioneering work by Margaret Daub’s team has shown that vitamins are highly effective in quenching reactive oxygen species (ROS), with potential comparable to carotenoids and tocopherols (58, 59). Vitamin B6, by quenching excess ROS, can reduce damage to ocular structures such as RGCs in the eye mitochondria caused by ROS imbalance, and play a certain role in the prevention of glaucoma and intervention in disease progression (13). On the other hand, vitamin B6 has also been found to be involved in maintaining normal homocysteine (Hcy) levels, and its circulating levels often decrease concurrently with hyperhomocysteinemia (60). High levels of Hcy can promote the progression of glaucoma by stimulating cytochrome c release and ROS production, and by inducing mitochondrial dysfunction and oxidative stress through the ERK1/2 signaling pathway (60). Emerging research increasingly substantiates that hyperhomocysteinemia is a substantial risk factor in the progression of glaucoma (60, 61). A study carried out in Russia involving participants with glaucoma and early-stage cataracts has demonstrated that a 20-day course of low-dose pyridoxine hydrochloride eye drops can impact visual parameters, such as changes in visual acuity and expansion of the visual field. This regimen also showed a reduction in intraocular pressure and the Becker’s coefficient (62).
Another potential protective mechanism of vitamin B6 against glaucoma may be its role in promoting the synthesis of myelin phospholipids, which have been shown to play a significant role in nourishing axons (63, 64). PLP, as a coenzyme in myelin synthesis, plays a positive role in slowing disease progression (63). Considering these potential mechanisms, it’s plausible that boosting vitamin B6 consumption could strengthen the resilience of RGCs against glaucomatous neurodegeneration.
This study’s strength lies in its use of stringent inclusion and exclusion criteria to enroll a large, nationally representative sample of American adults, which enhances the reliability of the results to a certain extent. Additionally, we validated the robustness of our conclusions through various sensitivity analyses, including subgroup analyses. On another note, our analysis of the relationship between vitamin B6 supplements and glaucoma offers a preliminary exploration of the equivalence in efficacy between different sources of vitamin B6.
This study presents several limitations that warrant consideration. First, to mitigate the impact of confounding factors, we implemented stricter inclusion and exclusion criteria that excluded individuals with stroke and retinal diseases. This approach limited the generalizability of our findings to the excluded groups and potentially introduced selection bias. Moreover, due to the cross-sectional nature of NHANES data, we could not explore causal or temporal associations between dietary vitamin B6 consumption and glaucoma risk. Dietary intake data, based on self-reporting, may be subject to recall bias. Additionally, given the potential variability in daily food consumption, using data from only two interviews may not accurately reflect participants’ regular dietary habits. Furthermore, we defined glaucoma using the Rotterdam criteria, which, despite being internationally validated, have inherent false positive and negative rates (34). The lack of comprehensive eye examinations to differentiate among the various subtypes of glaucoma also limited our understanding of the correlation between vitamin B6 dietary consumption and various subtypes of the condition.
To better understand the role of vitamin B6 in preventing and treating glaucoma, future research should employ less restrictive criteria to include a more diverse group of participants, thereby enhancing the generalizability of the findings. Additionally, more frequent dietary assessments or extended dietary tracking periods could enhance the accuracy of dietary intake estimates. It is also important to take into account other influencing factors such as genetics and environmental conditions, and to conduct further investigations through randomized controlled trials or epidemiological cohort studies. Furthermore, distinguishing between different types and stages of glaucoma will help identify the most effective ways to use vitamin B6 in prevention and treatment, offering more precise guidance for clinical practice.
5 Conclusion
Our findings indicate an inverse linear correlation between vitamin B6 dietary consumption and glaucoma risk. Thus, sufficient dietary consumption of vitamin B6 may serve as a preventive measure against glaucoma.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found a: https://www.jianguoyun.com/p/DagglMEQ_cmbDBjDrqgFIAA.
Ethics statement
The studies involving humans were approved by the NCHS Research Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The manuscript presents research on animals that do not require ethical approval for their study.
Author contributions
ZY: Formal analysis, Methodology, Writing – original draft. JZ: Conceptualization, Writing – original draft. YZ: Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the National Natural Science Foundation of China (No. 81271002), and the Jilin Health Science and Technology Capacity Improvement Project (No. 2022LC114).
Acknowledgments
Appreciation to every member of the NHANES team for their assistance.
Conflict of interest
The authors affirm that this research was conducted independently, with no commercial or financial affiliations that might be interpreted as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1363539/full#supplementary-material
References
1. Quigley, HA, and Broman, AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. (2006) 90:262–7. doi: 10.1136/bjo.2005.081224
2. Tribble, JR, Hui, F, Jöe, M, Bell, K, Chrysostomou, V, Crowston, JG, et al. Targeting diet and exercise for neuroprotection and Neurorecovery in Glaucoma. Cells. (2021) 10:295. doi: 10.3390/cells10020295
3. Weinreb, RN, Aung, T, and Medeiros, FA. The pathophysiology and treatment of glaucoma: a review. JAMA. (2014) 311:1901–11. doi: 10.1001/jama.2014.3192
4. Adornetto, A, Russo, R, and Parisi, V. Neuroinflammation as a target for glaucoma therapy. Neural Regen Res. (2019) 14:391–4. doi: 10.4103/1673-5374.245465
5. Tang, B, Li, S, Cao, W, and Sun, X. The Association of Oxidative Stress Status with open-angle Glaucoma and exfoliation Glaucoma: a systematic review and Meta-analysis. J Ophthalmol. (2019) 2019:1–14. doi: 10.1155/2019/1803619
6. Gupta, N, and Yücel, YH. Glaucoma as a neurodegenerative disease. Curr Opin Ophthalmol. (2007) 18:110–4. doi: 10.1097/ICU.0b013e3280895aea
7. Kaur, C, Foulds, WS, and Ling, EA. Hypoxia-ischemia and retinal ganglion cell damage. Clin Ophthalmol. (2008) 2:879–89. doi: 10.2147/OPTH.S3361
8. Yu, DY, Cringle, SJ, Balaratnasingam, C, Morgan, WH, Yu, PK, and Su, EN. Retinal ganglion cells: energetics, compartmentation, axonal transport, cytoskeletons and vulnerability. Prog Retin Eye Res. (2013) 36:217–46. doi: 10.1016/j.preteyeres.2013.07.001
9. Sanz-Morello, B, Ahmadi, H, Vohra, R, Saruhanian, S, Freude, KK, Hamann, S, et al. Oxidative stress in optic neuropathies. Antioxidants. (2021) 10:1538. doi: 10.3390/antiox10101538
10. Ruan, Y, Jiang, S, Musayeva, A, and Gericke, A. Oxidative stress and vascular dysfunction in the retina: therapeutic strategies. Antioxidants. (2020) 9:761. doi: 10.3390/antiox9080761
11. Langbøl, M, Saruhanian, S, Baskaran, T, Tiedemann, D, Mouhammad, ZA, Toft-Kehler, AK, et al. Increased antioxidant capacity and pro-homeostatic lipid mediators in ocular hypertension-a human experimental model. J Clin Med. (2020) 9:2979. doi: 10.3390/jcm9092979
12. Kang, EY, Liu, PK, Wen, YT, Quinn, PMJ, Levi, SR, Wang, NK, et al. Role of oxidative stress in ocular diseases associated with retinal ganglion cells degeneration. Antioxidants. (2021) 10:1948. doi: 10.3390/antiox10121948
13. Buonfiglio, F, Böhm, EW, Pfeiffer, N, and Gericke, A. Oxidative stress: a suitable therapeutic target for optic nerve diseases? Antioxidants. (2023) 12:1465. doi: 10.3390/antiox12071465
14. Saccà, SC, Izzotti, A, Rossi, P, and Traverso, C. Glaucomatous outflow pathway and oxidative stress. Exp Eye Res. (2007) 84:389–99. doi: 10.1016/j.exer.2006.10.008
15. Ford, TC, Downey, LA, Simpson, T, McPhee, G, Oliver, C, and Stough, C. The effect of a high-dose vitamin B multivitamin supplement on the relationship between brain metabolism and blood biomarkers of oxidative stress: a randomized control trial. Nutrients. (2018) 10:1860. doi: 10.3390/nu10121860
16. Kang, JH, Willett, WC, Rosner, BA, Buys, E, Wiggs, JL, and Pasquale, LR. Association of Dietary Nitrate Intake with Primary Open-Angle Glaucoma: a prospective analysis from the Nurses' health study and health professionals follow-up study. JAMA Ophthalmol. (2016) 134:294–303. doi: 10.1001/jamaophthalmol.2015.5601
17. Yamashima, T, Zhao, L, Wang, XD, Tsukada, T, and Tonchev, AB. Neuroprotective effects of pyridoxal phosphate and pyridoxal against ischemia in monkeys. Nutr Neurosci. (2001) 4:389–97. doi: 10.1080/1028415X.2001.11747375
18. Wang, XD, Kashii, S, Zhao, L, Tonchev, AB, Katsuki, H, Akaike, A, et al. Vitamin B6 protects primate retinal neurons from ischemic injury. Brain Res. (2002) 940:36–43. doi: 10.1016/S0006-8993(02)02587-8
19. Mallone, F, Lucchino, L, Franzone, F, Marenco, M, Carlesimo, SC, and Moramarco, A. High-dose vitamin B supplementation for persistent visual deficit in multiple sclerosis: a pilot study. Drug Discov Ther. (2020) 14:122–8. doi: 10.5582/ddt.2020.03031
20. Ruamviboonsuk, V, and Grzybowski, A. The roles of vitamins in diabetic retinopathy: a narrative review. J Clin Med. (2022) 11:6490. doi: 10.3390/jcm11216490
21. Cui, X, Jauregui, R, Park, KS, and Tsang, SH. Multimodal characterization of a novel mutation causing vitamin B6-responsive gyrate atrophy. Ophthalmic Genet. (2018) 39:512–6. doi: 10.1080/13816810.2018.1474370
22. Li, S, Li, D, Shao, M, Cao, W, and Sun, X. Lack of association between serum vitamin B₆, vitamin B(12), and vitamin D levels with different types of Glaucoma: a systematic review and Meta-analysis. Nutrients. (2017) 9:636. doi: 10.3390/nu9060636
23. Xu, F, Zhao, X, Zeng, SM, Li, L, Zhong, HB, and Li, M. Homocysteine, B vitamins, methylenetetrahydrofolate reductase gene, and risk of primary open-angle glaucoma: a meta-analysis. Ophthalmology. (2012) 119:2493–9. doi: 10.1016/j.ophtha.2012.06.025
24. Li, W, Pan, J, Wei, M, Lv, Z, Chen, S, Qin, Y, et al. Nonocular influencing factors for primary Glaucoma: an umbrella review of Meta-analysis. Ophthalmic Res. (2021) 64:938–50. doi: 10.1159/000519247
25. Rolle, T, Dallorto, L, Rossatto, S, Curto, D, and Nuzzi, R. Assessing the performance of daily intake of a Homotaurine, carnosine, Forskolin, vitamin B2, vitamin B6, and magnesium based food supplement for the maintenance of visual function in patients with primary open angle Glaucoma. J Ophthalmol. (2020) 2020:1–9. doi: 10.1155/2020/7879436
26. Lee, SY, Tseng, VL, Kitayama, K, Avallone, TJ, Yu, F, Pan, D, et al. Associations between niacin intake and Glaucoma in the National Health and nutrition examination survey. J Glaucoma. (2023) 32:443–50. doi: 10.1097/IJG.0000000000002216
27. Kang, JH, Loomis, SJ, Wiggs, JL, Willett, WC, and Pasquale, LR. A prospective study of folate, vitamin B₆, and vitamin B₁₂ intake in relation to exfoliation glaucoma or suspected exfoliation glaucoma. JAMA Ophthalmol. (2014) 132:549–59. doi: 10.1001/jamaophthalmol.2014.100
28. Centers for Disease Control and Prevention About the National Health and Nutrition Examination Survey. (2021). Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm (Accessed November 28, 2023).
29. National Center for Health Statistics. National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/nchs/nhanes.htm (Accessed November 28, 2023).
30. Dong, Y, and Peng, CY. Principled missing data methods for researchers. Springerplus. (2013) 2:222. doi: 10.1186/2193-1801-2-222
31. Methods and Application of Food Composition Laboratory. USDA Agricultural Research Service. Nutrient Data Laboratory. Available from: http://www.ars.usda.gov/nutrientdata (Accessed November 28, 2023).
32. National Center for Health Statistics. National Health and Nutrition Examination Survey (2007–2008). Data documentation, codebook, and frequencies: Dietary Interview - Total Nutrient Intakes, First Day (DR1TOT_E). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/DR1TOT_E.htm (Accessed November 28, 2023).
33. National Health and Nutrition Examination Survey (2007–2008). National Center for Health Statistics. Dietary Interview - Individual Foods, Second Day (DR2IFF_E). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/DR2IFF_E.htm
34. Wang, YE, Tseng, VL, Yu, F, Caprioli, J, and Coleman, AL. Association of Dietary Fatty Acid Intake with Glaucoma in the United States. JAMA Ophthalmol. (2018) 136:141–7. doi: 10.1001/jamaophthalmol.2017.5702
35. Taechameekietichai, T, Chansangpetch, S, Peerawaranun, P, and Lin, SC. Association between daily niacin intake and Glaucoma: National Health and nutrition examination survey. Nutrients. (2021) 13. doi: 10.3390/nu13124263
36. Wu, CM, Wu, AM, Tseng, VL, Yu, F, and Coleman, AL. Frequency of a diagnosis of glaucoma in individuals who consume coffee, tea and/or soft drinks. Br J Ophthalmol. (2018) 102:1127–33. doi: 10.1136/bjophthalmol-2017-310924
37. National Health and Nutrition Examination Survey. (2005–2006). National Center for Health Statistics. Ophthalmology - Retinal Imaging (OPXRET_D). Centers for Disease Control and Prevention. Available from: http://wwwn.cdc.gov/nchs/nhanes/2005-2006/OPXRET_D.htm (Accessed November 28, 2023).
38. National Health and Nutrition Examination Survey. (2005–2006). National Center for Health Statistics. Ophthalmology - Frequency Doubling Technology (OPXFDT_D). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/OPXFDT_D.htm (Accessed November 28, 2023).
39. Liu, Z, Hu, Y, Wang, Y, Xu, B, Zhao, J, and Yu, Z. Relationship between high dose intake of vitamin B12 and glaucoma: evidence from NHANES 2005-2008 among United States adults. Front Nutr. (2023) 10:1130032. doi: 10.3389/fnut.2023.1130032
40. Lee, JY, Choi, JA, Park, SP, and Jee, D. Association between high blood folate levels and Glaucoma in a representative Korean population. Invest Ophthalmol Vis Sci. (2024) 65:6. doi: 10.1167/iovs.65.1.6
41. National Health and Nutrition Examination Survey. (2007–2008). National Center for Health Statistics. Demographic Variables & Sample Weights (DEMO_E). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/DEMO_E.htm (Accessed November 28, 2023).
42. Cortés Álvarez, SI, Flores-Ruelas, Y, Del Toro-Equihua, M, Pérez-Manzo, L, Delgado-Enciso, I, and Sánchez-Ramírez, CA. Serum 25-Hydroxyvitamin D correlates with systolic blood pressure in obese male schoolchildren. Nutr Hosp. (2022) 39:562–8. doi: 10.20960/nh.03911
43. Whelton, PK, Carey, RM, Aronow, WS, Casey, DE Jr, Collins, KJ, Dennison Himmelfarb, C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of High Blood Pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. (2018) 138:e426–83. doi: 10.1161/CIR.0000000000000597
44. National Health and Nutrition Examination Survey. (2005–2006). National Center for Health Statistics. Body Measures (BMX_D). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/BMX_D.htm#BMXWAIST (Accessed November 28, 2023).
45. National Health and Nutrition Examination Survey. (2005–2006). National Center for Health Statistics. Cholesterol - Total (TCHOL_D). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/TCHOL_D.htm#LBDTCSI (Accessed November 28, 2023).
46. National Health and Nutrition Examination Survey. (2005–2006). National Center for Health Statistics. Data Documentation, Codebook, and Frequencies C-Reactive Protein (CRP) (CRP_D). Available at: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/CRP_D.htm#LBXCRP
47. National Health and Nutrition Examination Survey. (2005–2006). National Center for Health Statistics. Smoking - Cigarette Use (SMQ_D). Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/SMQ_D.htm
48. Lindschinger, M, Tatzber, F, Schimetta, W, Schmid, I, Lindschinger, B, Cvirn, G, et al. Bioavailability of natural versus synthetic B vitamins and their effects on metabolic processes. MMW Fortschr Med. (2020) 162:17–27. doi: 10.1007/s15006-020-0230-4
49. Nelson, EW Jr, Lane, H, and Cerda, JJ. Comparative human intestinal bioavailability of vitamin B-6 from a synthetic and a natural source. J Nutr. (1976) 106:1433–7. doi: 10.1093/jn/106.10.1433
50. National Health and Nutrition Examination Survey 2005-2006: National Center for Health Statistics. Smoking - Cigarette Use (SMQ_D) Centers for Disease Control and Prevention. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/SMQ_D.htm#SMQ040 (Accessed November 28, 2023).
51. Morris, MS, Picciano, MF, Jacques, PF, and Selhub, J. Plasma pyridoxal 5′-phosphate in the US population: the National Health and nutrition examination survey, 2003-2004. Am J Clin Nutr. (2008) 87:1446–54. doi: 10.1093/ajcn/87.5.1446
52. Gdynia, HJ, Müller, T, Sperfeld, AD, Kühnlein, P, Otto, M, Kassubek, J, et al. Severe sensorimotor neuropathy after intake of highest dosages of vitamin B6. Neuromuscul Disord. (2008) 18:156–8. doi: 10.1016/j.nmd.2007.09.009
53. Perry, TA, Weerasuriya, A, Mouton, PR, Holloway, HW, and Greig, NH. Pyridoxine-induced toxicity in rats: a stereological quantification of the sensory neuropathy. Exp Neurol. (2004) 190:133–44. doi: 10.1016/j.expneurol.2004.07.013
54. Konstas, AGP, and Ringvold, A. Epidemiology of exfoliation syndrome. J Glaucoma. (2018) 27:S4–s11. doi: 10.1097/IJG.0000000000000908
55. Santos, AJM, Khemiri, S, Simões, S, Prista, C, Sousa, I, and Raymundo, A. The importance, prevalence and determination of vitamins B6 and B12 in food matrices: a review. Food Chem. (2023) 426:136606. doi: 10.1016/j.foodchem.2023.136606
56. Stach, K, Stach, W, and Augoff, K. Vitamin B6 in health and disease. Nutrients. (2021) 13. doi: 10.3390/nu13093229
57. Galluzzi, L, Vacchelli, E, Michels, J, Garcia, P, Kepp, O, Senovilla, L, et al. Effects of vitamin B6 metabolism on oncogenesis, tumor progression and therapeutic responses. Oncogene. (2013) 32:4995–5004. doi: 10.1038/onc.2012.623
58. Hellmann, H, and Mooney, S. Vitamin B6: a molecule for human health? Molecules. (2010) 15:442–59. doi: 10.3390/molecules15010442
59. Bilski, P, Li, MY, Ehrenshaft, M, Daub, ME, and Chignell, CF. Vitamin B6 (pyridoxine) and its derivatives are efficient singlet oxygen quenchers and potential fungal antioxidants. Photochem Photobiol. (2000) 71:129–34. doi: 10.1562/0031-8655(2000)071<0129:SIPVBP>2.0.CO;2
60. Koklesova, L, Mazurakova, A, Samec, M, Biringer, K, Samuel, SM, Büsselberg, D, et al. Homocysteine metabolism as the target for predictive medical approach, disease prevention, prognosis, and treatments tailored to the person. EPMA J. (2021) 12:477–505. doi: 10.1007/s13167-021-00263-0
61. Mooney, S, Leuendorf, JE, Hendrickson, C, and Hellmann, H. Vitamin B6: a long known compound of surprising complexity. Molecules. (2009) 14:329–51. doi: 10.3390/molecules14010329
62. Adornetto, A, Rombolà, L, Morrone, LA, Nucci, C, Corasaniti, MT, Bagetta, G, et al. Natural products: evidence for neuroprotection to be exploited in Glaucoma. Nutrients. (2020) 12. doi: 10.3390/nu12103158
63. Calderón-Ospina, CA, and Nava-Mesa, MO. B vitamins in the nervous system: current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. CNS Neurosci Ther. (2020) 26:5–13. doi: 10.1111/cns.13207
Keywords: cross-sectional study, glaucoma, vitamin B6, National Health and Nutrition Examination Survey, nutrition
Citation: Yang Z, Zhang J and Zheng Y (2024) Higher vitamin B6 dietary consumption is associated with a lower risk of glaucoma among United States adults. Front. Nutr. 11:1363539. doi: 10.3389/fnut.2024.1363539
Edited by:
Mauro Serafini, University of Teramo, ItalyReviewed by:
Reza Rastmanesh, American Physical Society, United StatesWeihua Yang, Jinan University, China
Copyright © 2024 Yang, Zhang and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yajuan Zheng, eWp6aGVuZ0BqbHUuZWR1LmNu
 Ziling Yang
Ziling Yang Jinming Zhang
Jinming Zhang Yajuan Zheng
Yajuan Zheng