
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr. , 06 May 2024
Sec. Nutritional Epidemiology
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1347851
This article is part of the Research Topic Nutrition and Sustainable Development Goal 2: Zero Hunger View all 24 articles
Background: Maternal undernutrition is a major public health concern due to its association with mortality and overall disease burden for mothers and their children. Maternal nutrition determines pregnancy outcomes since reduced intake of nutrients influences gestational age length, placental function, and fetal growth during pregnancy. The complexity of the intergenerational aspects of maternal nutrition may also confound the design of interventions. Therefore, this research aimed to assess the prevalence of undernutrition and associated factors among pregnant women in Ethiopia.
Methods: We identified the literature from PubMed, EMBASE, Scopus, and CINAHL databases. Data were entered into Microsoft Excel and then exported to Stata version 17 statistical software for analysis. The I2 and Q-statistic values detect the level of heterogeneity, and meta regression was performed to investigate between-study heterogeneity using more than one moderator. JBI quality assessment tools were used to include relevant articles. Evidence of publication bias was indicated using the funnel plot and Egger's linear regression test. The effect size was expressed in the form of point estimates and an odds ratio of 95% CI in the fixed-effect model.
Result: In total, 19 studies fulfill the inclusion criteria. The pooled prevalence of undernutrition among pregnant women was 32% (95% CI 31.3–33.2 I2 = 97.5%, P < 0.0). Illiteracy (AOR = 3.6 95% CI; 2.3–5.6), rural residence (AOR = 2.6 95% CI; 1.2–3.5), a lack of prenatal dietary advice (AOR = 2.6 95% CI; 1.8–3.7), household food insecurity (AOR = 2.5 95% CI; 1.9–3.2), and low dietary diversity score (AOR = 3.7 95% CI; 2.2–5.9) appear to be significantly associated with undernutrition among pregnant women.
Conclusion: The review showed that the prevalence of undernutrition is still high among pregnant women. Illiteracy, rural residence, a lack of prenatal dietary advice, household food insecurity, and low dietary diversity score were significantly associated with undernutrition during pregnancy. Interventions should focus on educating the public and helping families access food or supplements they need through local markets, health systems, and community-based support, as undernutrition is caused by numerous interconnected causes.
Systematic review registration: https://www.crd.york.ac.uk/prospero/#myprospero, identifier: CRD42023417028.
According to the World Health Organization (WHO), undernutrition is one of the top 10 ranked risk factors for the burden of disease worldwide (1). It results from either inadequate dietary intake in terms of quantity or quality, inadequate nutrient utilization brought on by infections or other disorders, or from either of the two (2). During the first 1,000 days of a child's life (from conception to 6 months of a baby's life), the mother is the only source of nutrition for the infant via the placenta and then through exclusive breastfeeding during the first 6 months of life (3).
Too many women, particularly young people and those who are nutritionally vulnerable, do not receive the nutrition they require for maintaining their health and providing their unborn children the greatest possible chance to live, grow, and develop (4).
Due to the physiological demands of pregnancy and lactation, pregnant women are frequently nutritionally susceptible (5). Inadequate dietary intakes before, during, and after pregnancy have the potential to harm mothers and their offspring. Comprehensive improvements in women's nutritional and physical wellbeing before and during pregnancy will support healthy fetal development, better labor and delivery outcomes, greater prenatal survival, and perhaps even longer-term health for both the mother and child. However, the quality of diet for pregnant women in many resource-poor settings is very low, and there are discrepancies between intakes and requirements for a variety of micronutrients (6, 7).
Approximately half of the deaths in children under 5 years in low- and middle-income countries are directly or indirectly caused by mothers who are undernourished (8). Based on a pooled estimate carried out in 137 developing nations, maternal undernutrition was responsible for 14.4% of stunting among 44.1 million children of < 2 years of age (9). On the other hand, mothers with better nutritional status take better care of themselves and provide their children with better care (10). Because an undernourished mother is more likely to give birth to an undernourished child, the cycle of undernutrition is perpetuated through generations (11–13).
Undernutrition during pregnancy can lead to preterm birth, intrauterine growth restriction, and reproductive loss through stillbirths. Recent research suggests that healthy eating throughout pregnancy and breastfeeding may also lower the child's risk of developing chronic diseases later in life (14–16). A vulnerability to undernutrition in utero is associated with stunted growth and development in children, short stature in adults, lower intellectual attainment, and lower economic production (17, 18).
Maternal undernutrition is commonly cited as a cause of retarded fetal growth, malformations associated with the central nervous system such as spinal bifida and hydrocephalus and prematurity (19, 20). Serious issues of maternal undernutrition are evident in most countries in Sub-Saharan Africa and south-central and southeastern Asia (7, 21). Previous studies have established that undernourished pregnant women suffer from a combination of chronic energy deficiency that leads their children to have a low birth weight (LBW) and also causes preterm birth and unsuccessful birth outcomes (22–24). Regardless of significant gains and signs of progress in the last decade, maternal undernutrition still remains a major public health problem in Ethiopia. Because the causes of malnutrition are complex, they should be addressed in a systematic way to find the right solutions for the problem. In general, malnutrition is not the result of a single consequence of a single factor but is caused by a mixture of different factors, and the extent of the contribution of each factor may vary. Therefore, this systematic review and meta-analysis aimed to assess the magnitude of undernutrition and associated factors among pregnant women in Ethiopia.
This systematic review and meta-analysis were reported using the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) (25) (Supplementary File 1). The protocol for this review was registered on the (PROSPERO) International Prospective Register of Systematic Reviews (registration number 2023: CRD42023417028).
We identified literature from PubMed, Medline, EMBASE, Scopus, and CINAHL databases (Supplementary File 2). A supplementary search was conducted to find gray literature from the Google search engine and Google Scholar. In addition, we contacted three authors to request for additional information missing from their papers. The study includes articles published from January 2016 to March 2023 in Ethiopia and published in English. We employed the Medical Subject Headings (MeSH) terms and combined keywords to identify studies in these databases.
The study includes case-control, cross-sectional, and cohort studies, irrespective of sample size, published from January 2016 to March 2023 and published only in English. The review included articles defining undernutrition during pregnancy according to the researchers' categories and studies. We excluded the studies if they were not related to the title, were duplicates, were not carried out in Ethiopia, were anonymous reports, and were not published in English. The primary outcome of interest in this study is the prevalence of undernutrition among pregnant women.
We identified an initial set of studies by using the search terms, and then the retrieved studies were exported to the reference manager software, EndNote version 7. Duplicated studies were removed using the EndNote and also removed manually. Two independent reviewers (SB) and (MH) screened the title and abstract for relevance. During this preliminary assessment, primary studies that were found to be irrelevant were excluded. Differences between the two reviewers were resolved by consensus, or if necessary, the third reviewer (MA) was consulted for a disagreement based on the relevance of the stated objectives and inclusion criteria. Finally, studies with relevant information and those that fulfill inclusion criteria were selected for full-text review, and excluded studies were reasoned out via a flow chart.
We used an Excel spreadsheet for data extraction. Two reviewers (DA and DT) extracted the data using a data extraction format that includes authors, year of publication, study area, study design, and sample size. We extracted data on the percentage and factors affecting undernutrition among pregnant women with adjusted odd ratios. The extracted data were then edited and saved in a comma-delimited file for analysis.
The study has two main outcomes: the prevalence of undernutrition among pregnant women and the factors associated with maternal undernutrition during pregnancy. The odds ratio was calculated for the common risk factors of the reported studies.
The authors rigorously assessed the quality of all the selected studies for inclusion in the review. The JBI quality assessment tool was used to assess the quality of each individual study (26) (Supplementary File 3). For each study design, we included a study that scored above the mean value of the checking points.
The data extracted and saved in the comma-delimited file format in an Excel spreadsheet were imported to Stata version 17.0 (Stata Corporation, College Station, TX, USA) statistical software for analysis. We used forest plots to graphically report the results. We checked the presence of heterogeneity among studies using the chi-squared test where a p < 0.05 denoted statistical significance. The I-squared (I2) statistic was used to quantify the level of heterogeneity among the studies. We assumed substantial heterogeneity among studies when the value of I2 was ≥50%. We used the fixed-effects model to conduct meta-analyses where the studies did not have substantial heterogeneity (i.e., I2 statistic < 50%). If the I2 statistic is ≥50% (as suggested by Higgins et al.), indicating high heterogeneity (27), a random effect model was used. We pooled the percentages of undernutrition during pregnancy. We carried out subgroup analyses according to different categories of publication years and regions, and meta regression was performed to investigate between-study heterogeneity by using more than one moderator by the random effect model (Sidik–Jonkman method) instead of the default restricted maximum-likelihood (REML) method. Sensitivity analyses were conducted using a leave-one-out meta-analysis to explore the influence of a single study on the overall effect size estimate on maternal undernutrition during pregnancy. Publication bias was assessed by an inspection of the funnel plot and formal testing for asymmetry of the funnel plot using Egger's linear regression test.
The database search yielded 430 studies; similarly, the gray literature yielded eight articles. In total, the search retrieved 438 articles. A total of 343 studies were not related to our title and not carried out in Ethiopia, 34 articles were found to be duplicates, and six articles were excluded since they were not related to our titles and were confirmed irrelevant to this review. Finally, 55 potential full-text articles were screened. From full-text articles, 36 were excluded for the following reasons: 29 articles had wrong outcomes and seven studies did not discuss factors affecting maternal undernutrition. Finally, 19 studies were included in this review (Figure 1).
Regarding the study area, seven of the studies were conducted in the Oromia region (23, 28–33), six studies in the South Nation Nationalities and People region (SNNPR) (34–39) two studies each in the regions of Amhara (22, 40) and Tigray (41, 42), and one in the Afar (43) and Gambella regions (44) (Table 1). The most commonly associated factors included in this review were illiteracy, rural residence, pregnant women who were married before the age of 18, no antenatal care follow-up, substance use during pregnancy, a lack of prenatal dietary advice, not participating in women's Health Development Army meetings, intestinal parasite infection, skipping meals, household food insecurity, and low dietary diversity.
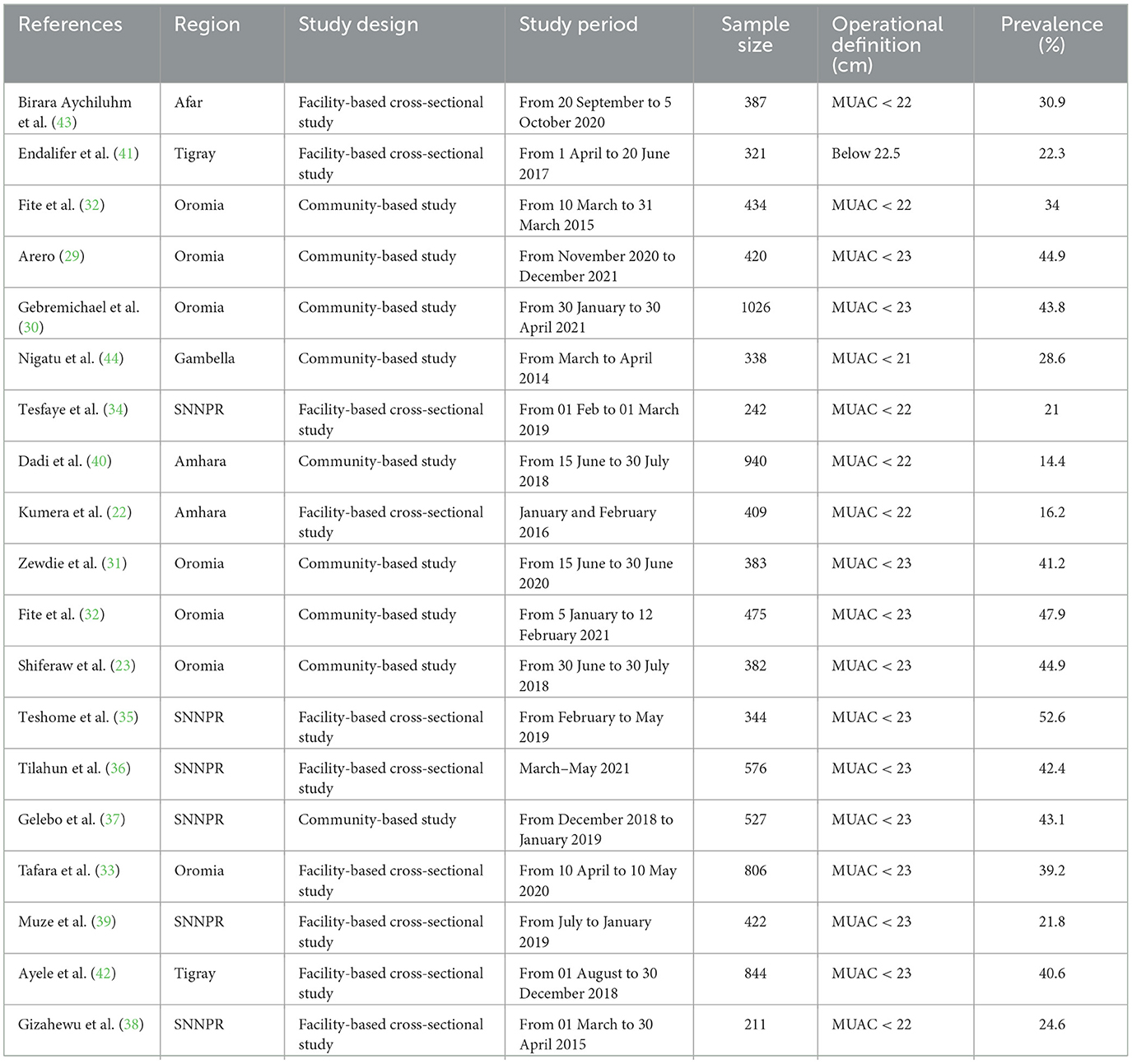
Table 1. The characteristics of studies included show undernutrition among pregnant women in Ethiopia.
The Joanna Briggs Institute (JBI) quality appraisal checklist was used for each study design. The disagreement between two reviewers (SB and MH) was resolved by consulting a third reviewer (MA). Cohen's Kappa statistics was used to calculate the degree of agreement between the two reviewers (SB and MH). The inter-rater agreement between the authors for study inclusion, data extraction, and methodological quality was assessed using Cohen's kappa coefficient (values ≤ 0 indicates no agreement, 0.01–0.2 indicates none to slight, 0.21–0.4 indicates fair, 0.41– 0.6 indicates moderate, 0.61–0.8 indicates substantial, and 0.81–1 indicates almost perfect agreement). Kappa coefficient of >0.63 was accepted (45).
The overall pooled prevalence of undernutrition among pregnant women is presented with a forest plot (Figure 2). Therefore, the estimated prevalence of undernutrition among pregnant women in Ethiopia was 32% (95% CI: 31.3–33.2 I2 = 97.5%, P < 0.0).
The presence of a small study effect was checked by using funnel plots and Egger's test from the log-odds ratio of the proportion for a better property of meta-analysis. The SE is dependent on the value of log odds and the underlying proportion. Hence, the funnel plot showed a symmetric distribution, and Egger's test value was 0.92; both results revealed that there was no publication bias (Figure 3).
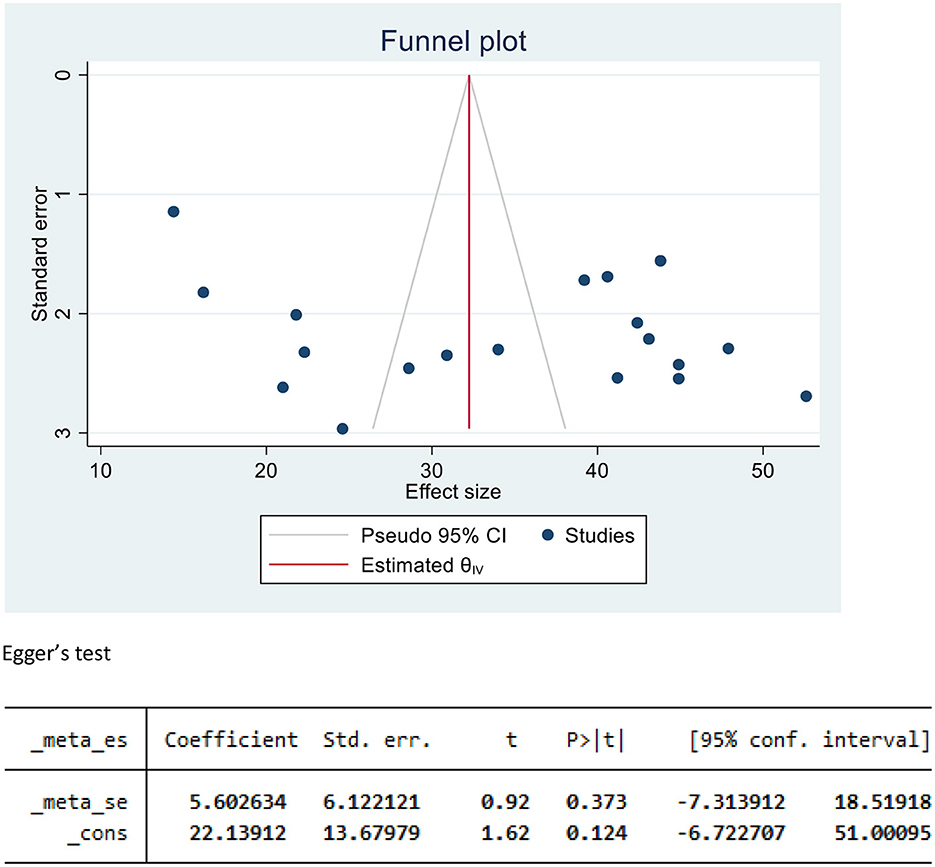
Figure 3. Funnel plot and Egger's test to assess publication bias for undernutrition among pregnant women in Ethiopia, 2023.
Subgroup analysis was employed with the evidence of heterogeneity using I-squared (I2) tests. In this study, the I2 statistic was 97.5%, P < 0.0, which showed evidence of marked heterogeneity. Therefore, subgroup analysis was carried out by using region and publication year as moderators (Figures 4, 5).
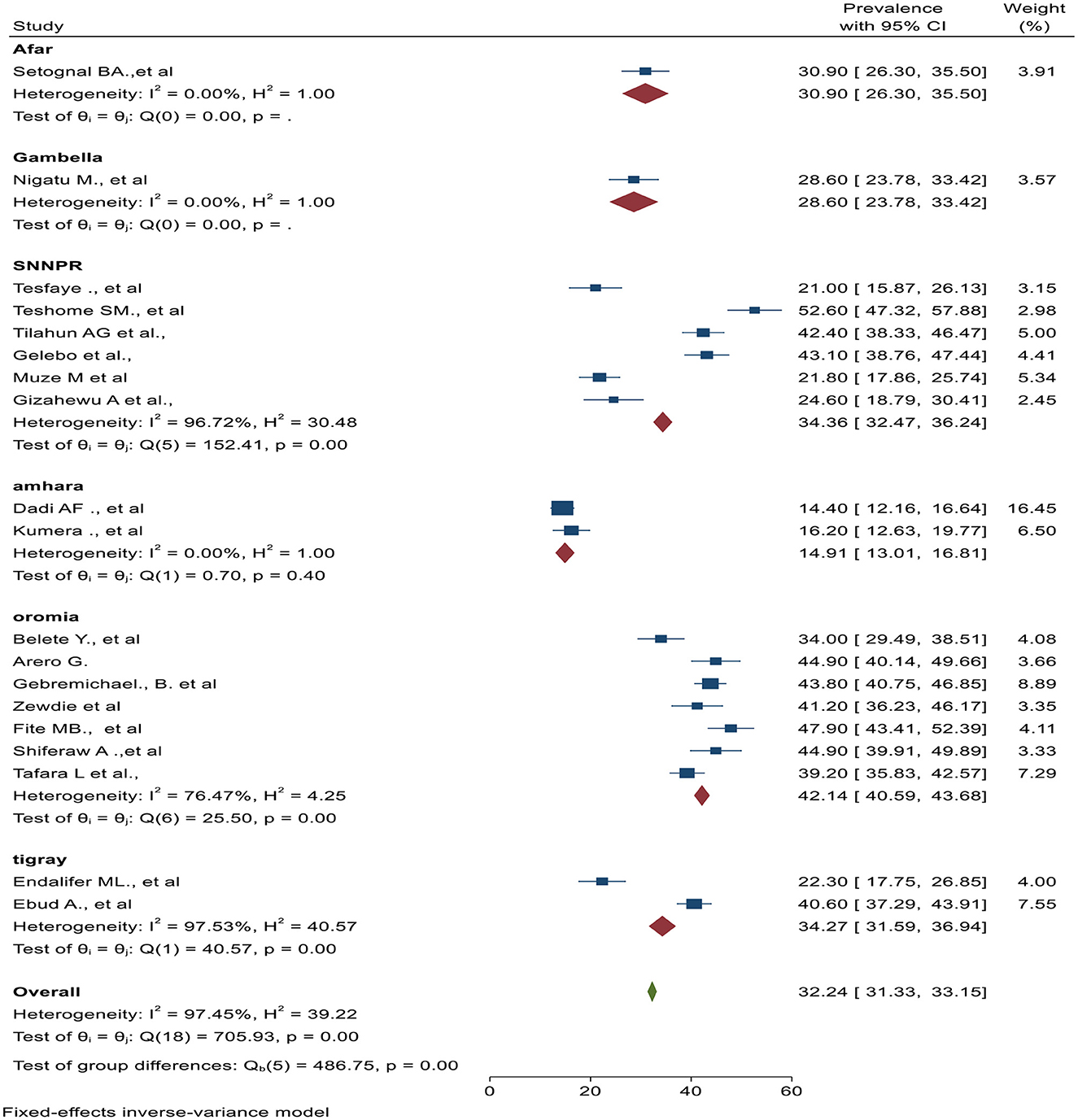
Figure 4. Subgroup analysis by region of studies and pooled effect of undernutrition among pregnant women in Ethiopia, 2023.
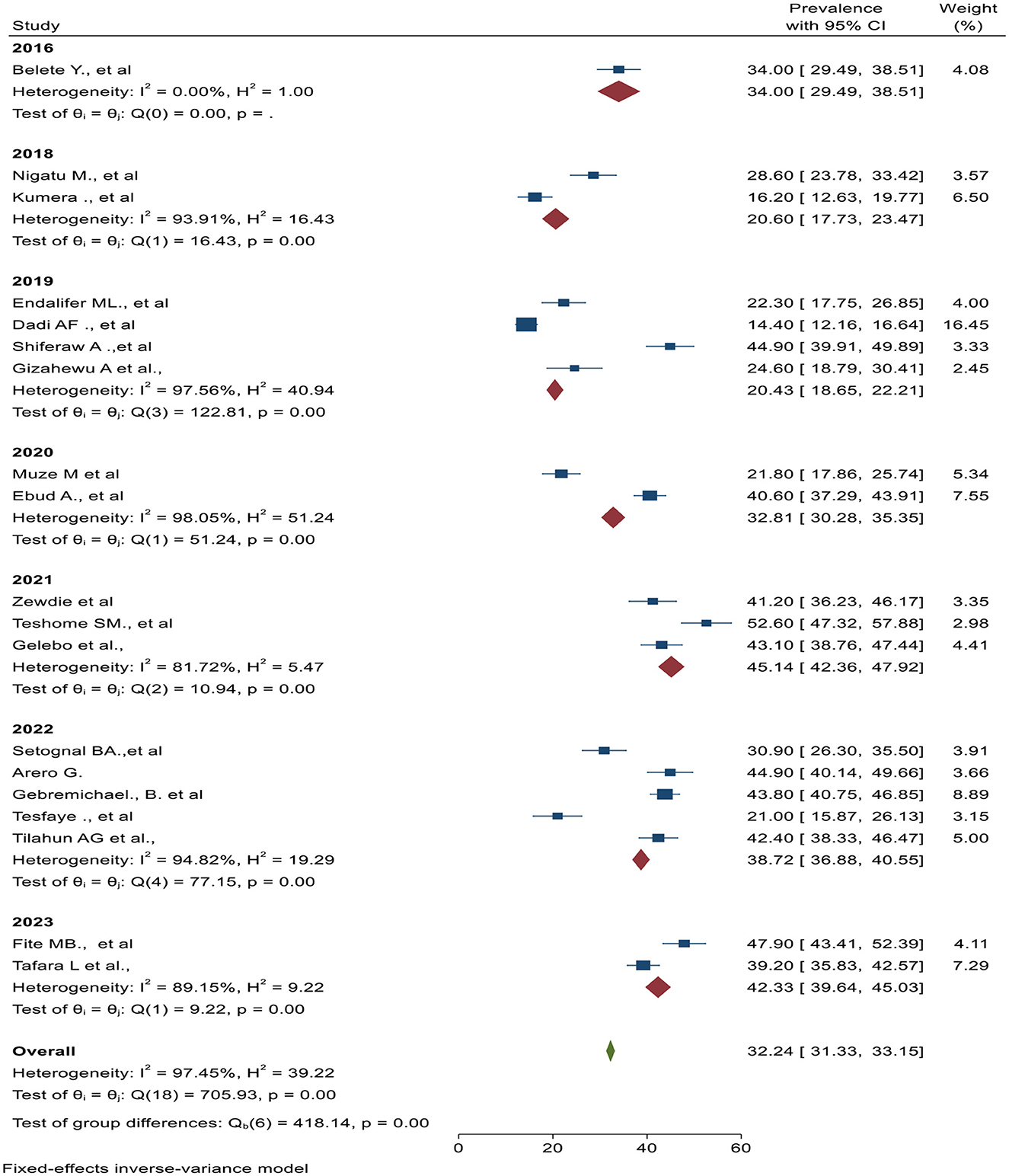
Figure 5. Subgroup analysis by publication year of studies and pooled effect of undernutrition among pregnant women in Ethiopia, 2023.
Using meta-analysis regression, we collected a summary report of the heterogeneity statistics test among 19 primary studies included in this review. We used a different type of random effect model (Sidik–Jonkman method) instead of the default restricted maximum-likelihood (REML) method since REML assumes that the error distribution is normal, whereas the Sidik–Jonkman estimator does not. After the heterogeneity test, using meta regression reported an I2 statistic of 96%, which suggested very high heterogeneity even after including publication year and sample size as the moderators. The adjusted R2 statistic was used to assess the proportion of between-study variance explained by the covariates (publication year and sample size). In this study, approximately 14% of the between-study variance is explained by the covariate (Figure 6).
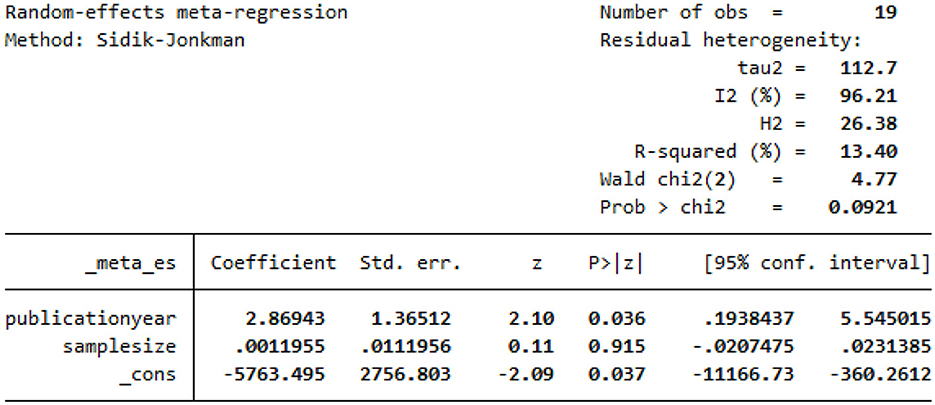
Figure 6. Meta-regression to assess heterogeneity and meta-analysis model using a publication year and sample size as moderators for undernutrition among pregnant women in Ethiopia, 2023.
Leave-one-out meta-analysis was performed to explore the influence of a single study on the overall effect size estimate on maternal undernutrition during pregnancy. The prevalence of undernutrition among pregnant women was high (35.8%) in Dadi AF. et al.'s study and low (31.1%) in Gebremichael B. et al.'s study (Figure 7).
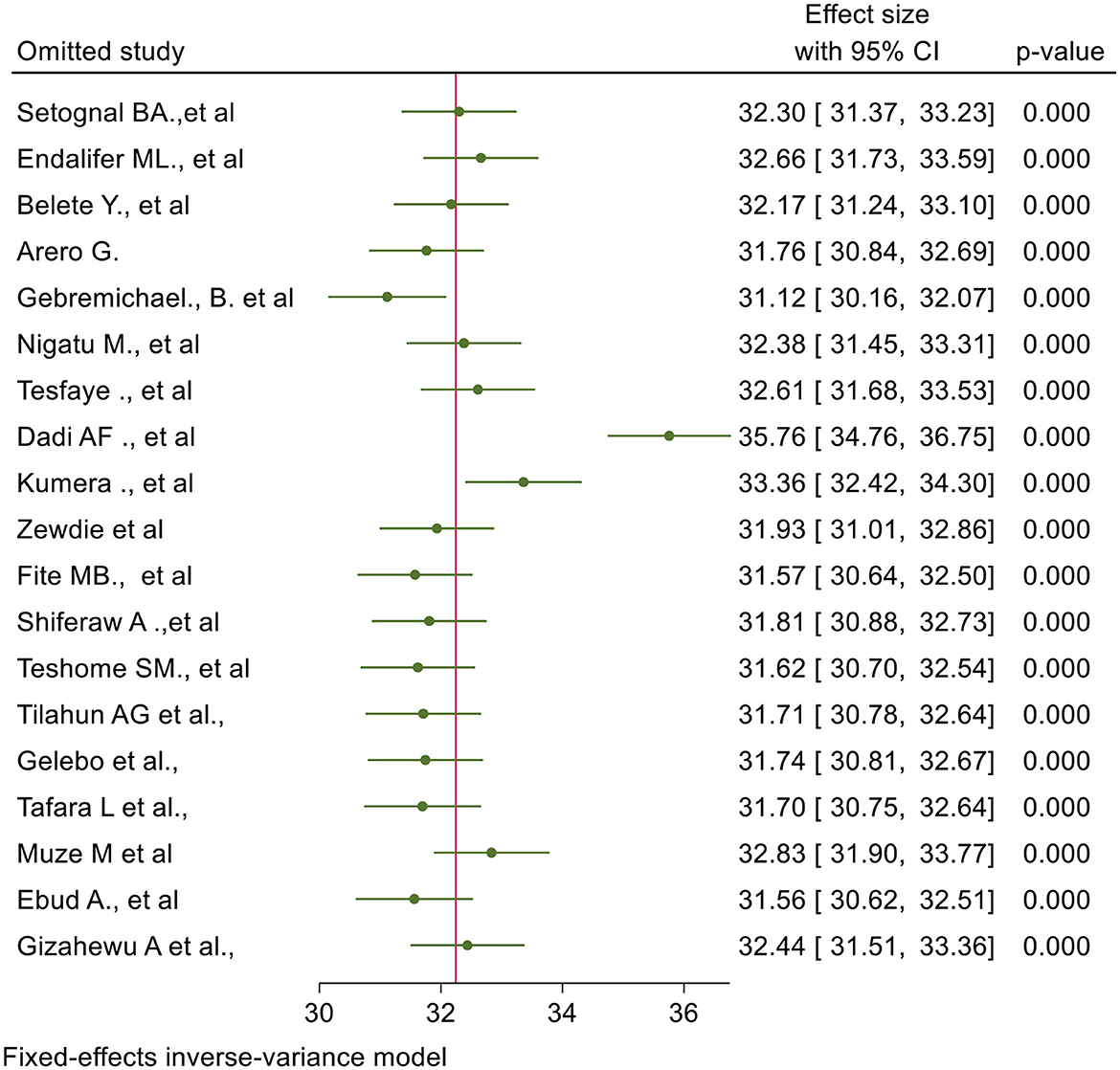
Figure 7. Leave one out meta analysis for studies included in a systematic review and meta-analysis of undernutrition during pregnancy in Ethiopia, 2023.
Factors such as illiteracy, rural residence, pregnant women who were married before the age of 18, no antenatal care follow-up, substance use during pregnancy, a lack of prenatal dietary advice, not participating in women's Health Development Army meetings, intestinal parasite infection, skipping meals, household food insecurity, and low dietary diversity were associated with undernutrition among pregnant women.
Illiterate (AOR = 3.6 95% CI; 2.3–5.6) women were 3.6 times more undernourished than literate women during pregnancy. The odds of undernutrition among rurally residing (AOR = 2.6 95% CI; 1.2–3.5) pregnant women were 2.6 times more likely than their urban counterparts. The pregnant women who have had low prenatal dietary advice (AOR = 2.6 95% CI; 1.8–3.7) were 2.6 times more likely undernourished than women who got the prenatal dietary advice. Women who have had high household food insecurity (AOR = 2.5 95%CI; 1.9–3.2) had 2.5 times higher odds of developing undernutrition during pregnancy. The odds of undernutrition among pregnant women who have had low dietary diversity (AOR = 3.695%CI; 2.2–5.9) were 3.6 times more likely than their counterparts.
Undernutrition is defined as a person's inability to consume enough calories and other nutrients to meet their needs and maintain their health (46). Worldwide, nearly about 462 million pregnant women are malnourished, and Africa is the most heavily overburdened continent (14, 47). Undernutrition during pregnancy occurs due to a dual load caused by increased demands during pregnancy and inadequate intake of food (48). Undernutrition is a key contributor to maternal mortality and morbidity and adverse birth outcomes (49). This review aimed to identify the national burden of undernutrition among pregnant women and the factors associated with it.
The pooled estimate of undernutrition among pregnant women remains high in Ethiopia with a 34% prevalence 32% (95% CI 31.3–33.2). This is quite more prevalent compared with the neighboring country Sudan (12.5%) (50). However, this finding is in line with the World Health Organization (51) report on Africa with prevalence rates of undernutrition being above 15% (51). A review performed on Sub-Saharan Africa indicates that maternal undernutrition during pregnancy is 23.5%; however, heterogeneity of studies in the measurement of undernutrition during pregnancy affected the outcomes of interest (52). The finding provides remarkable evidence that in Ethiopia, undernutrition among pregnant women continues to be a public health problem, and its adverse birth outcomes are still not halted (34).
This review aims to identify illiterate pregnant women who are known to be at risk for undernutrition. Education at higher levels increases knowledge of healthy prenatal and nutritional practices. Illiteracy has a direct correlation to women's ignorance of the importance of eating a balanced diet while being pregnant (53). Although significant nutrition interventions have been made, nutrition remains the primary priority area in Ethiopia (54). Given this, evidence from the region and other comparable settings demonstrates that significant rates of undernutrition persist, even in areas and households where food is abundant. In order to properly plan nutrition interventions for vulnerable population groups including nursing mothers and pregnant women, nutrition knowledge is a crucial component of dietary practices (55, 56). Additionally, women with low levels of education may have little to no influence over financial decisions, consumables food purchases, and food distribution in the home, which may contribute to their poor nutritional health (22).
According to this review, women who lived in rural areas had 2.6 times the likelihood of being undernourished compared to women who lived in urban areas. This result is in line with a systematic review and meta-analysis that highlights the burden of malnutrition among pregnant women in Africa (52). This could be explained by the fact that women in rural areas might not have access to antenatal health care services, information about eating a balanced diet, and other maternal health services (57).
Our analysis found a link between maternal undernutrition and a lack of prenatal dietary advice. Mothers who did not receive prenatal dietary recommendations were 2.6 times more undernourished than mothers who did receive recommendations. These findings highlight the value of nutritional counseling and appropriate feeding practices as interventions. According to a study from Bangladesh, pregnant women who are counseled to alter their eating habits can satisfy the increased nutritional requirements (58). This finding explains the critical necessity for healthcare providers to set up suitable monitoring and feedback mechanisms for antenatal nutrition education and counseling and doing so could increase women's understanding of proper nutrition.
The analysis also found that one of the characteristics that were independently linked to undernutrition during pregnancy was a lack of maintaining household food security. Compared to pregnant women from food-secure homes, those from food-insecure households had a 2.5 times higher risk of being undernourished. When families lack access to food, they frequently fall short of their daily nutritional needs and have inadequate dietary intake, which causes women to be undernourished (59). Our finding of an increased prevalence of maternal undernutrition in food-insecure households may reflect inequitable intra-household food allocation, whereby the nutritional needs of the child or other household members are given priority over those of the mother (60–62).
Women with low dietary diversity scores were 3.6 times more likely to be undernourished than women with dietary diversity scores above the mean values. Scientific literature backs up the strong link between nutrient adequacy and dietary variety (63, 64). This has been explained by the fact that there is no single food that contains all the required nutrients for optimal health (65). In the majority of developing countries, micronutrient inadequacy continues to pose a substantial threat to public health (66). Unfortunately, pregnant women and other women of reproductive age are the most vulnerable due to their higher dietary needs (67). Iron deficiency-related anemia and other micronutrient deficiencies are still widespread in impoverished countries because pregnant women are not getting adequate nutrition (68–70).
The search strategy was limited to studies published in English and observational studies, causing reporting bias. The estimated magnitude of undernutrition during pregnancy in Ethiopia may need precaution in the interpretation of findings because no data were found in some regions.
This review showed that the prevalence of undernutrition is still high among pregnant women. Illiteracy, rural residence, a lack of prenatal dietary advice, household food insecurity, and low dietary diversity were significantly associated with undernutrition during pregnancy. Interventions should focus on educating the public and assisting families in obtaining the food or supplements they require through local markets, healthcare systems, and community-based assistance. It also emphasizes the need for better prenatal counseling on dietary diversity. The study also highlights that there is a nutritional disparity between pregnant women in urban and rural areas and that it is important to focus on the nutritional practices of rural women. Even though anemia and malaria may not be connected directly to nutritional habits, it is almost inevitable that malaria infection will be associated with anemia; thus, the interaction between these interconnected health determinants should be the prime agenda, especially in malaria-affected heavily endemic areas.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
SZ: Conceptualization, Data curation, Investigation, Supervision, Writing—original draft, Writing—review & editing. MB: Formal analysis, Investigation, Methodology, Software, Supervision, Visualization, Writing—review & editing. MA: Data curation, Investigation, Software, Visualization, Writing—review & editing. DTA: Resources, Software, Supervision, Validation, Visualization, Writing—review & editing. DA: Conceptualization, Investigation, Validation, Visualization, Writing—original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1347851/full#supplementary-material
1. WHO Global Health Risks (2009). Available online at: https://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf (accessed December 16, 2021).
2. Grebmer VK, Bernstein J, Patterson F. Global Hunger Index. (2019). Available online: https://www.globalhungerindex.org/pdf/en/2019.pdf (accessed December 16, 2021).
3. Mason JB, Shrimpton R, Saldanha LS, Ramakrishnan U, Victora CG, Girard AW, et al. The first 500 days of life: policies to support maternal nutrition. Glob Health Action. (2014) 7:23623. doi: 10.3402/gha.v7.23623
4. Mihretie Y. The prevalence of under nutrition and associated factors among adolescent pregnant women: a narrative review. J Med Care Rev. (2020) 3:333–42. doi: 10.15520/mcrr.v3i2.87
5. Food and Agriculture Organization of the United Nations [FAO] (2004). Available online at: http://www.fao.org/nutrition/nutrition-education/food-dietary-guidelines/en/ (accessed January 4, 2022).
6. Food and Nutrition Technical Assistance Project (FANTA) Minimum Dietary Diversity for Women (MDD-W). A Guide to Measurement. Available online at: http://www.fantaproject.org/monitoring-and-evaluation/minimum-dietary-diversity308women-indicator-MDD-W (accessed April 4, 2023).
7. Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
8. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
9. Danaei G, Andrews KG, Sudfeld CR, Fink G, McCoy DC, Peet E, et al. Risk factors for childhood stunting in 137 developing countries: a comparative risk assessment analysis at global, regional, and country levels. PLoS Med. (2016) 13:e1002164. doi: 10.1371/journal.pmed.1002164
10. Smith LC, Ramakrishnan U, Ndiaye A, Haddad L, Martorell R. The importance of Women's status for child nutrition in developing countries: international food policy research institute (IFPRI) research report abstract 131. Food Nutr Bull. (2003) 24:287–8. doi: 10.1177/156482650302400309
11. Leary SD, Ness A, Emmett P. Davey 318 Smith, ALSPAC Study Team. Maternal diet in pregnancy and offspring height, sitting height and leg length. J Epidemiol Community Health. (2005) 59:467–72. doi: 10.1136/jech.2004.029884
12. Prentice AM, Ward KA, Goldberg GR, Jarjou LM, Moore SE, Fulford AJ, et al. Critical windows for nutritional interventions against stunting. Am Clini Nutr. (2013) 97:911–8. doi: 10.3945/ajcn.112.052332
13. United Nations (1993). Maternal and Child Nutrition- SCN News, Number 11. Available online at: https://www.unscn.org/layout/modules/resources/files/scnnews11.pdf (accessed December 25, 2022).
14. Zahangir MS, Hasan MM, Richardson A, Tabassum S. Malnutrition and non-communicable diseases among Bangladeshi women: an urban–rural comparison. Nutr Diabet. (2017) 7:e250. doi: 10.1038/nutd.2017.2
15. IYCNP (2012). Guidance for Formative Research on Maternal Nutrition. Available online at: http://www.iycn.org/resource/guidance-for-formative-research-on-maternal-nutrition/ (accessed January 12, 2020).
16. Salam RA, Das JK, Ali A, Lassi ZS, Bhutta ZA. Maternal undernutrition and intrauterine growth restriction. Expert Rev Obstet Gynecol. (2013) 8:559–67. doi: 10.1586/17474108.2013.850857
17. Lesage J, Hahn D, Leonhardt M, Blondeau B, Breant B, Dupouy JP. Maternal undernutrition during late gestation-induced intrauterine growth restriction in the rat is associated with impaired placental GLUT3 expression, but does not correlate with endogenous corticosterone levels. J Endocrinol. (2002) 174:37. doi: 10.1677/joe.0.1740037
18. Hanson MA, Bardsley A, De-Regil LM, Moore SE, Oken E, Poston L, et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “think nutrition first”. Int J Gynaecol Obstet. (2015) 131:S213–53. doi: 10.1016/S0020-7292(15)30034-5
19. Lartey A. Maternal and child nutrition in Sub-Saharan Africa: challenges and interventions. Proc Nutr Soc. (2008) 67:105–8. doi: 10.1017/S0029665108006083
20. WHO. Maternal anthropometry for prediction of pregnancy outcomes: Memorandum from a USAID/WHO/PAHO/Mother care meeting. Bull WHO. (1991) 69:523–32.
21. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 2012, 1990–2010: a systematic analysis for the global burden of disease study (2010). Lancet. (2012) 380:2224–60. doi: 10.1016/2FS0140-6736(12)61766-8
22. Kumera G, Gedle D, Alebel A, Feyera F, Eshetie S. Undernutrition and its association with socio-demographic, anemia and intestinal parasitic infection among pregnant women attending antenatal care at the University of Gondar Hospital, Northwest Ethiopia. Matern Health Neonatol Perinatol. (2018) 4:1–0. doi: 10.1186/s40748-018-0087-z
23. Shiferaw A, Husein G. Acute under nutrition and associated factors among pregnant women in Gumay District, Jimma Zone, South West Ethiopia. J Women's Health Care. (2019) 8:2167–0420. doi: 10.35248/2167-0420.19.8.459
24. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet. (2008) 371:417–40. doi: 10.1016/S0140-6736(07)61693-6
25. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:89. doi: 10.1186/s13643-021-01626-4
26. Munn Z, Tufanaru C, Aromataris E. JBI's systematic reviews: data extraction and synthesis. AJN Am J Nurs. (2014) 114:49–54. doi: 10.1097/01.NAJ.0000451683.66447.89
27. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
28. Yimer B, Baraki N, Mekonnen F. Under nutrition and associated factors among adolescent pregnant women in Shashemenne District, West Arsi Zone, Ethiopia: a community based study. J Nutr Food Sci. (2016) 6:1. doi: 10.4172/2155-9600.1000454
29. Arero G. Undernutrition and associated factors among pregnant women in East Borena Zone, Liban District, Oromia Regional State, Ethiopia. Front Nutr. (2021) 9:1008701. doi: 10.3389/fnut.2022.1008701
30. Gebremichael B, Misgana T, Tamiru D, Tariku M, Tesfaye D, Alemu D, et al. Undernutrition and associated factors among rural pregnant women in Eastern Ethiopia. SAGE Open Med. (2022) 10:20503121221104430. doi: 10.1177/20503121221104430
31. Zewdie S, Fage SG, Tura AK, Weldegebreal F. Undernutrition among pregnant women in rural communities in southern Ethiopia. Int J Women's Health. (2021) 8:73–9. doi: 10.2147/IJWH.S285132
32. Fite MB, Tura AK, Yadeta TA, Oljira L, Roba KT. Factors associated with undernutrition among pregnant women in Haramaya district, Eastern Ethiopia: a community-based study. PLoS ONE. (2023) 18:e0282641. doi: 10.1371/journal.pone.0282641
33. Tafara L, Bikila H, Feyisa I, Desalegn M, Kaba Z. The prevalence of under nutrition and associated factors among pregnant women attending antenatal care service in public hospitals of western Ethiopia. PLoS ONE. (2023) 18:e0278180. doi: 10.1371/journal.pone.0278180
34. Tesfaye A, Sisay G, Kabthymer RH, Tesfaye T. Under-nutrition and associated factors among pregnant women in public health care hospitals of Gedeo Zone, southern Ethiopia: a cross-sectional study. Heliyon. (2022) 8:e09511. doi: 10.1016/j.heliyon.2022.e09511
35. Teshome SM, Meskel D, Worsa TK, Datiko A, Malik T. Undernutrition and associated factors among pregnant women in Kacha Birra district, southern Ethiopia. Austin J Nutr Metab. (2021) 8:1098. Available online at: https://api.semanticscholar.org/CorpusID:234905884
36. Tilahun AG, Fufa DA, Taddesse RD. Undernutrition and its associated factors among pregnant women at the public hospitals of Bench-Sheko and Kaffa zone, southwest Ethiopia. Heliyon. (2022) 8:e09380. doi: 10.1016/j.heliyon.2022.e09380
37. Gelebo DG, Gebremichael MA, Asale GA, Berbada DA. Prevalence of undernutrition and its associated factors among pregnant women in Konso district, southern Ethiopia: a community-based cross-sectional study. BMC Nutr. (2021) 7:1–3. doi: 10.1186/s40795-021-00437-z
38. Gizahewu A, Billoro BB, Yousfan MA. Under nutrition and associated factors among pregnant women at ANC Clinic, Nigist Eleni Mohammad Memorial General Hospital, Hossana, Southern Ethiopia. Food Nutr.: Curr. Res. (2019) 2:158–65. Available online at: https://www.scitcentral.com/article/17/715/Under-Nutrition-and-Associated-Factors-among-Pregnant-Women-at-ANC-Clinic,-Nigist-Eleni-Mohammad-Memorial-General-Hospital,-Hossana,-Southern-Ethiopia
39. Muze M, Yesse M, Kedir S, Mustefa A. Prevalence and associated factors of undernutrition among pregnant women visiting ANC clinics in Silte zone, Southern Ethiopia. BMC Pregn Childbirth. (2020) 20:1–8. doi: 10.1186/s12884-020-03404-x
40. Dadi AF, Desyibelew HD. Undernutrition and its associated factors among pregnant mothers in Gondar town, Northwest Ethiopia. PLoS ONE. (2019) 14:e0215305. doi: 10.1371/journal.pone.0215305
41. Endalifer M, Tewabe M, Adar A. Undernutrition and associated factors among pregnant women attending ANC follow up in Alamata general hospital, Northern Region, Ethiopia, (2017). J Nutr Health Food Eng. (2019) 9:70–8. doi: 10.15406/jnhfe.2019.09.00329
42. Ayele E, Gebreayezgi G, Mariye T, Bahrey D, Aregawi G, Kidanemariam G. Prevalence of undernutrition and associated factors among pregnant women in a public general hospital, Tigray, Northern Ethiopia: a cross-sectional study design. J Nutr Metabol. (2020) 2020:2736536. doi: 10.1155/2020/2736536
43. Birara Aychiluhm S, Gualu A, Wuneh, AG. Undernutrition and its associated factors among pregnant women attending antenatal care at public health facilities in pastoral communities of Afar Regional State, northeast Ethiopia. Pastoralism, (2022) 12:1–11. doi: 10.1186/s13570-022-00251-7
44. Nigatu M, Gebrehiwot TT, Gemeda DH. Household food insecurity, low dietary diversity, and early marriage were predictors for Undernutrition among pregnant women residing in Gambella, Ethiopia. Adv Public Health. (2018) 2018:1–0. doi: 10.1155/2018/1350195
45. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33:159–74. doi: 10.2307/2529310
46. World Health Organization. Malnutrition Quantifying the Health Impact at National and Local Levels. Geneva: WHO. (2005).
47. Adebowale SA, Adepoju OT, Okareh TO, Fagbamigbe FA. Social epidemiology of adverse nutritional status outcomes among women in Nigeria: NDHS, (2008). Pak J Nutr. (2011) 10:888–98. doi: 10.3923/pjn.2011.888.898
48. Ghosh S, Spielman K, Kershaw M, Ayele K, Kidane Y, Zillmer K, et al. Nutrition-specific and nutrition-sensitive factors associated with mid-upper arm circumference as a measure of nutritional status in pregnant Ethiopian women: implications for programming in the first 1000 days. PLoS ONE. (2019) 14:e0214358. doi: 10.1371/journal.pone.0214358
49. Edris M, Tekle H, Fitaw Y, Gelaw B, Engedaw D, Alemu T. Maternal Nutrition for the Ethiopian Health Center Team. Ethiopian Public Health Training Initiative (EPHTI), University of Gondar (2005).
50. Hassan B, Rayis DA, Ahmed AB, ALhabardi N, Adam I. Prevalence and associated factors of undernutrition among pregnant Sudanese women. Trans R Soc Trop Med Hyg. (2022). 116:352–8. doi: 10.1093/trstmh/trab128
51. World Health Organization. Nutrition in the WHO African Region. Brazzaville: World Health Organization. (2017). p. 1–85. Available online at: http://apps.who.int/iris (accessed December 23, 2019).
52. Desyibelew HD, Dadi AF. Burden and determinants of malnutrition among pregnant women in Africa: A systematic review and meta-analysis. PLoS ONE. (2019) 14:e0221712. doi: 10.1371/journal.pone.0221712
53. Joseph. Dietary diversity, nutrient intake and nutritional status of pregnant women aged 18–45 years in developing countries. A systematic review. Int J Food Sci Nutr. (2018) 3:217–20. Available online at: https://www.foodsciencejournal.com/assets/archives/2018/vol3issue4/3-4-67-550.pdf
54. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa: CSA and ICF (2016).
55. Perumal N, Cole DC, Ouédraogo HZ, Sindi K, Loechl C, Low J, et al. Health and nutrition knowledge, attitudes and practices of pregnant women attending and not-attending ANC clinics in Western Kenya: a cross-sectional analysis. BMC Pregn Childb. (2013) 2013:1–12. doi: 10.1186/1471-2393-13-146
56. Popa AD, Nită O, Graur Arhire LI, Popescu RM, Botnariu GE, Mihalache L, et al. Nutritional knowledge as a determinant of vitamin and mineral supplementation during pregnancy. BMC Public Health. (2013) 13:1105. doi: 10.1186/1471-2458-13-1105
57. Uthman O, Aremu O. Malnutrition among women in sub-Saharan Africa: rural-urban disparity. Rural Remote Health. (2008) 8:2. doi: 10.22605/RRH931
58. Nguyen PH, Sanghvi T, Kim SS, Tran LM, Afsana K, Mahmud Z, et al. Factors influencing maternal nutrition practices in a large scale maternal, newborn and child health program in Bangladesh. PLoS ONE. (2017) 12:e0179873. doi: 10.1371/journal.pone.0179873
59. Ethiopian Federal Ministry of Health. National Nutrition Strategy, Addis Ababa (2008). Available online at: https://www.iycn.org/files/National-Nutrition-Strategy.pdf (accessed November 30, 2023).
60. FAO, IFAD, UNICEF, WFP, WHO. The State of Food Security and Nutrition in the World, 2019. In: Safeguarding Against Economic Slowdowns and Downturns. Rome: FAO (2019).
61. USAID. Maternal Dietary Diversity and the Implications for Children's Diets in the Context of Food Security. (2012). Available online at: http://www.iycn.org (accessed February 6, 2023).
62. Acharya SR, Bhatta J, Timilsina DP. Factors associated with nutritional status of women of reproductive age group in rural, Nepal. Asian Pacific J Health Sci. (2017) 4:19–24. doi: 10.21276/apjhs.2017.4.4.6
63. Kennedy G, Fanou N, Seghieri C, Brouwer ID. Dietary diversity as a measure of the micronutrient adequacy of women's diets: results from Bamako, Mali site. In: Food and Nutrition Technical Assistance II Project (FANTA-2). Washington, DC (2009).
64. Mirmiran P, Azadbakht L, Azizi F. Dietary diversity within food groups: an indicator of specific nutrient adequacy in Tehranian women. J Am Coll Nutr. (2006) 25:354–61. doi: 10.1080/07315724.2006.10719546
65. Kennedy GL. Evaluation of Dietary Diversity Scores for Assessment of Micronutrient Intake and Food Security in Developing Countries. Wageningen: Wageningen University and Research (2009).
66. Kennedy GL, Pedro MR, Seghieri C, Nantel G, Brouwer I. Dietary diversity score is a useful indicator of micronutrient intake in non-breast-feeding Filipino children. J Nutr. (2007) 137:472–7. doi: 10.1093/jn/137.2.472
67. Lee SE, Talegawkar SA, Merialdi M, Caulfield LE. Dietary intakes of women during pregnancy in low-and middle-income countries. Public Health Nutr. (2013) 16:1340–53. doi: 10.1017/S1368980012004417
68. Rodriguez-Bernal CL, Rebagliato M, Ballester F. Maternal nutrition and fetal growth: the role of iron status and intake during pregnancy. Nutr Diet Suppl. (2012) 6:25–37. doi: 10.2147/NDS.S13093
69. Abebe H, Abebe Y, Loha E, Stoecker BJ. Consumption of vitamin A rich foods and dark adaptation threshold of pregnant women at Damot Sore District, Wolayita, Southern Ethiopia. Ethiop J Health Sci. (2014) 24:219–26. doi: 10.4314/ejhs.v24i3.5
Keywords: undernutrition, women, associated factors, meta-analysis, Ethiopia
Citation: Zewude SB, Beshah MH, Ahunie MA, Arega DT and Addisu D (2024) Undernutrition and associated factors among pregnant women in Ethiopia. A systematic review and meta-analysis. Front. Nutr. 11:1347851. doi: 10.3389/fnut.2024.1347851
Received: 06 December 2023; Accepted: 16 April 2024;
Published: 06 May 2024.
Edited by:
Mauro Serafini, University of Teramo, ItalyReviewed by:
Aaron Christian, University of Ghana, GhanaCopyright © 2024 Zewude, Beshah, Ahunie, Arega and Addisu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shimeles Biru Zewude, bmF0aGFuc2hpbWVsZXNAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.