- 1Department of Pediatric Gastroenterology and Metabolic Diseases, Poznan University of Medical Sciences, Poznan, Poland
- 2Department of Clinical Psychology, Poznan University of Medical Sciences, Poznan, Poland
- 3Department of Physiology, Poznan University of Medical Sciences, Poznan, Poland
- 4Department of Pediatric Diabetes, Auxology and Obesity, Poznan University of Medical Sciences, Poznan, Poland
- 5Department of Pediatric Radiology, Poznan University of Medical Sciences, Poznan, Poland
- 6Department of Pharmacognosy and Biomaterials, Poznan University of Medical Sciences, Poznan, Poland
- 7Department of Treatment of Obesity, Metabolic Disorders and Clinical Dietetics, Poznan University of Medical Sciences, Poznan, Poland
Introduction: Previous studies investigating the effectiveness of conjugated linoleic acid (CLA) supplementation in body weight reduction provided unequivocal results. We hypothesized that psychological factors such as self-efficacy, locus of control or dispositional optimism can affect the success of the intervention. Therefore, this study aimed to determine the psychological factors that modulate the effectiveness of CLA supplementation in overweight or obese women and affect the ability to successfully complete the study.
Methods: In total, 74 subjects were recruited into this three-month randomized trial and divided into intervention and control groups receiving, respectively, capsules containing 3 g 80% CLA per day and capsules containing 3 g of sunflower oil. The following psychological tests were performed before the intervention: Multidimensional Health Locus of Control scale, Acceptance of Illness Scale, Satisfaction with Life Scale (SWLS), General Self Efficacy Scale (GSES), Health Behavior Inventory scale and Life Orientation Test (LOT-R).
Results: A total of 60 women completed the study and the subjects who dropped out obtained higher scores in the GSES (p = 0.0490) and the LOT-R (p = 0.0087) tests than subjects who completed the trial. Besides, multivariate linear regression demonstrated that the SWLS test (p = 0.0345) results were independent predictors of body weight changes.
Conclusion: In conclusion, psychological factors like self-efficacy and optimism may be associated with a higher risk of withdrawal from the study, while satisfaction with life may have an impact on the effectiveness of body weight reduction.
Clinical trial registration: [https://drks.de/search/en], identifier [DRKS00010462].
1 Introduction
Obesity is considered a serious threat to public health worldwide, the prevalence of which has dramatically increased among both men and women in all age groups. Since 1980, the excessive body weight rate has doubled, with around a third of the global population being overweight or obese (1). Moreover, it is expected that 1.9 billion people worldwide will be living with obesity by 2035 (2). Several weight management strategies have been suggested, including diet restriction, physical activity, behavioral strategies, pharmacology and bariatric surgery (3). Weight loss is associated with numerous health and psychological benefits, including decreased risk of type 2 diabetes mellitus, cardiovascular diseases, chronic kidney disease, sleep apnea or asthma (4). Despite these benefits, body weight reduction is often difficult to achieve. A meta-analysis encompassing 29 long-term weight loss studies revealed that over half of the lost weight was regained within 2 years, and by the end of 5 years, more than 80% of the lost weight was recovered (5). Therefore, the identification of psychological factors that may determine the success of different strategies for body weight reduction is particularly important. The American Dietetic Association recommends that psychological factors should be assessed together with dietary intake to optimize subjects’ response to body weight loss interventions and to maintain body weight reduction (6). However, to date, the search for psychological factors (e.g., self-efficacy, locus of control, dispositional optimism) that determine the effectiveness of different strategies in body weight reduction has yielded inconsistent findings (7–13).
One of the dietary supplements with potential body weight reduction properties is conjugated linoleic acid (CLA). CLA is a comprehensive term used to describe isomers of octadecadienoic (linoleic) acid that contain conjugated double bonds (14). Ruminants possess an enzyme capable of converting fatty acids into CLA. Thus, food from ruminant sources (meat and dairy products) is a natural source of CLA (15). CLA can also be synthesized using oils abundant in linoleic acid, including safflower and sunflower oils (16). It has been shown that CLAs have various beneficial effects on atherosclerosis, cancer (17), diabetes (18), and inflammatory process (19). However, the anti-obesity effect of CLA is controversial. Onakpoya et al. (20) in the meta-analysis showed that long-term CLA supplementation decreased body weight, body mass index (BMI) and fat mass when compared to placebo. However, the effect was small and did not seem clinically relevant. Contrary, Liang et al. (21) in a recent meta-analysis demonstrated that CLA supplementation during exercise programs was not effective for body-weight control compared to exercise alone but significantly reduced fat mass.
Taking into account the inconsistency in the obtained results we hypothesized that psychological factors might affect the success of the CLA supplementation. Therefore, this study aimed to determine the psychological factors that modulate the effectiveness of CLA supplementation in body weight reduction in overweight or obese women and affect the ability to successfully complete the study.
2 Materials and methods
2.1 Study design
The study was a parallel randomized controlled trial and was performed between July 2014 and May 2015. The Poznan University of Medical Sciences Ethics Committee approved the study protocol (ref. 606/12, 453/13, 358/14, and 398/15) and the research was performed according to the Declaration of Helsinki (22). All study participants were informed that participation was voluntary and that they can withdraw from the study at any time without giving a reason. Informed consent was obtained from all individual participants included in the study. This paper was written according to the consolidated standards of reporting trials (CONSORT, see Supplementary Table S1) (23) and the study project was retrospectively registered in the German Clinical Trials Register database (ID: DRKS00010462, date of registration: 04.05.2016) (24).
2.2 Inclusion and exclusion criteria
The inclusion and exclusion criteria were as described previously (25–30). Briefly, women older than 18 years old with a BMI ≥ 25 kg/m2 and stable body weight (± 3 kg during the last 3 months) were recruited. Subjects with a history of chronic diseases, including celiac disease, type 2 diabetes mellitus, and hepatic and pancreatic diseases, were excluded. Pregnant and breastfeeding women and subjects who previously received CLA supplementation or taking dietary supplements which interfered with fat digestion or absorption were also excluded. Study screening was performed at the Department of Internal Medicine, Metabolic Disorders and Hypertension, Poznan University of Medical Sciences, Poland.
2.3 Interventions protocol
During the 12-week intervention period, the CLA group received six capsules per day containing 3 g 80% CLA (0.5 g per capsule), a 50:50 mixture of cis-9, trans-11 and trans-10, and cis-12 isomers. The placebo group received six identical capsules per day, each containing sunflower oil. The capsules were manufactured and packaged in blisters by the Olimp Laboratories company (Pustynia, Poland). Compliance was monitored by phone calls, with the women consuming at least 75% of the capsules included in the analysis. Participants were instructed not to change their dietary habits and physical activity during the intervention.
2.4 Outcomes
The main outcomes of the study included an assessment of psychological behaviors that could determine the effectiveness of the study intervention. However, this manuscript is part of a larger project which aimed to evaluate the effect of CLA supplementation on starch and lipid digestion using a breath test (29) and the secondary purpose of the project was to assess the effect of CLA supplementation on anthropometric parameters (25), body composition and liver markers (26), atherosclerosis parameters (28), densitometric variables (30), glucose and insulin homeostasis, lipid metabolism and adipokine levels, as reported previously. All outcomes were assessed at the Department of Pediatric Gastroenterology and Metabolic Diseases, Poznan University of Medical Sciences, Poland.
2.5 Anthropometric parameters
Anthropometric parameters were measured in the morning with the participants wearing light clothing and without shoes. Body weight and height were measured using the Radwag scale with a stadiometer (Radwag, Random, Poland). BMI was calculated and overweight was defined as BMI ≥ 25 kg/m2 and obesity as BMI ≥ 30 kg/m2 (1). Subjects who decreased body weight after the intervention period were compared to subjects who increased body weight after the intervention separately in the CLA and control groups.
2.6 Psychological tests
The following tests were used: Multidimensional Health Locus of Control scale (MHLC), Acceptance of Illness Scale (AIS), Satisfaction with Life Scale (SWLS), General Self Efficacy Scale (GSES), Health Behavior Inventory scale (IZZ), and Life Orientation Test (LOT-R).
The MHLC includes 18 statements, each assessed on a six-level scale related to beliefs on expectations in three dimensions of the health locus of control: internality (I)—the internal locus of health control, the influence of others (O)—the external locus of health control and random (R)—chance or random locus of health control. Each index ranges from 0 to 30 points, with higher scores indicating a stronger belief in the influence of a particular factor on health. The MHLC scale has two versions: A and B. In this study, we used version A. The reliability of this Polish version of the MHLC scale determined by the Cronbach α was 0.77 (I), 0.67 (O), and 0.76 (R).
The AIS scale comprises eight statements addressing various aspects such as the constraints brought about by the illness, diminished independence resulting from it, the feeling of being dependent on others, and reduced self-esteem. Participants were asked to express their agreement or disagreement with these statements using a five-point scale, where 1—signifies strongly agree; 2—agree; 3—undecided; 4— disagree; 5—strongly disagree. The total score falls within the range of 8–40, with a higher score indicating a greater degree of acceptance of illness. The Polish version of the AIS scale has good psychometric properties, with reliability measured by the Cronbach’s α = 0.85.
The SWLS was developed to assess life satisfaction and consists of five items rated on a seven-point Likert scale, where 1 means strongly disagree and 7 means strongly agree. The total score for the scale ranges from 5 to 35, with a lower score indicating a lower level of satisfaction with life, while a high score indicates a higher level of satisfaction with life. The reliability coefficient for the scale is good (the Cronbach’s α = 0.88).
The GSES scale is a 10-item self-report scale that measures general self-efficacy. Respondents rate each item on a scale from 1 (not at all true) to 4 (completely true). The total score on the GSES scale can vary between 10 and 40, where higher scores reflect greater levels of self-efficacy. The Cronbach’s α coefficient for the scale is 0.81.
The IZZ scale contains 24 statements describing various health-related behaviors, each assesses on a five-point scale, from “hardly ever,” to “nearly always.” The overall score was computed as the sum of all these statements, resulting in a score range from 24 to 120 points. Moreover, the intensity of four categories of health behaviors was evaluated: eating habits, prophylactic behaviors, a positive mental attitude and health practices. The higher the score, the greater the declared health behavior intensity. The reliability for the total IZZ scale based on the Cronbach’s α coefficient is 0.85.
The LOT-R scale contains 10 statements, with six of a diagnostic value for dispositional optimism and four that were not taken into account in the calculation of the results. A five-point scale was used to evaluate each statement, where 0 points mean that the statement definitely does not apply to me, while 4 points mean that the information definitely applies to me. The overall score is the sum of each statement, including three positive and three negative, so the number of points for the negative statements is inverted before being summed. The overall score ranged from 0 to 24 points with a higher score meaning a higher level of optimism. The Cronbach’s α for the Polish version is 0.76 (31).
2.7 Randomization and blinding
Blocking randomization was performed and a randomization list was generated. The allocation sequence remained undisclosed until participants were registered and subsequently allocated to their respective interventions. During the intervention, both study participants and researchers were not aware of the allocation. After the statistical analysis of the obtained results was completed, the study was unblinded and participants were informed about their study group assignment.
2.8 Minimum sample size
The Statistica 12 PL software (TIBCO Software Inc., Palo Alto, United States) was used to calculate the minimum sample size indicating that 74 subjects should be recruited to the study to obtain 80% power (α = 0.05, β = 0.2). Based on the results of our previous studies, we hypothesized that the mean differences in primary outcomes (starch and lipid digestion assessed by a breath test) would explain approximately 75% of the variances that we previously observed (32, 33). In addition, in the calculation, we assumed that a maximum of 20% of participants resigned from the study during the intervention.
2.9 Statistical analysis
The Statistica 13 PL software (TIBCO Software Inc., Palo Alto, United States) was used for statistical analysis and p < 0.05 was considered statistically significant. Mean, standard deviation (SD), 95% confidence interval (95% CI), median and interquartile range (IQR; Q1–Q3) were calculated. The Shapiro–Wilk was used to assess the normality of the distribution of variables. The Mann–Whitney U-test was used to examine differences between the study groups (CLA group vs. control group), individuals who completed and those who did not complete the study and subjects who decreased and increased body weight after the intervention period. Univariate and multivariate linear regression analysis was performed to assess the relationship between changes in body weight and psychological test results.
3 Results
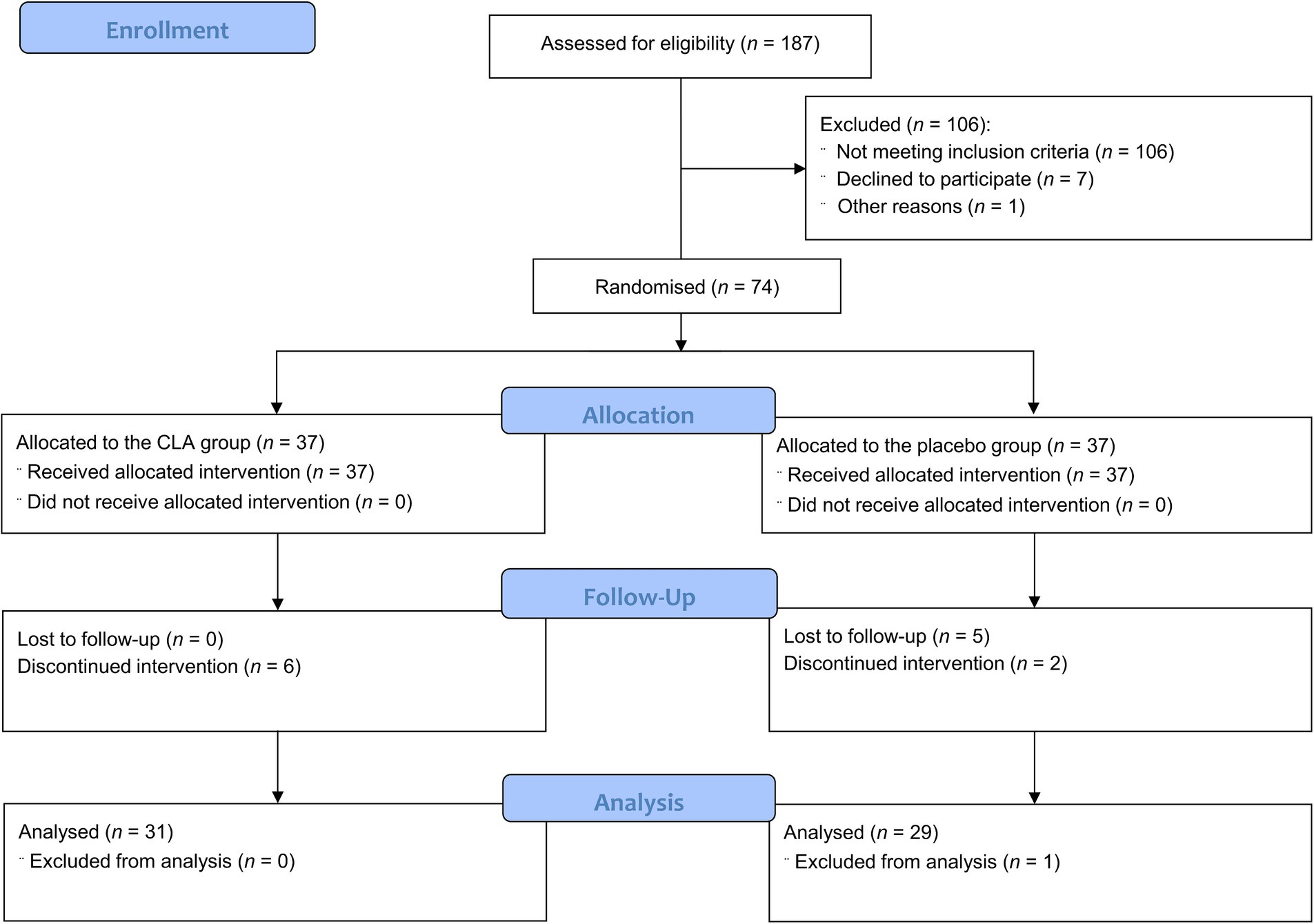
3.1 Participants’ flow
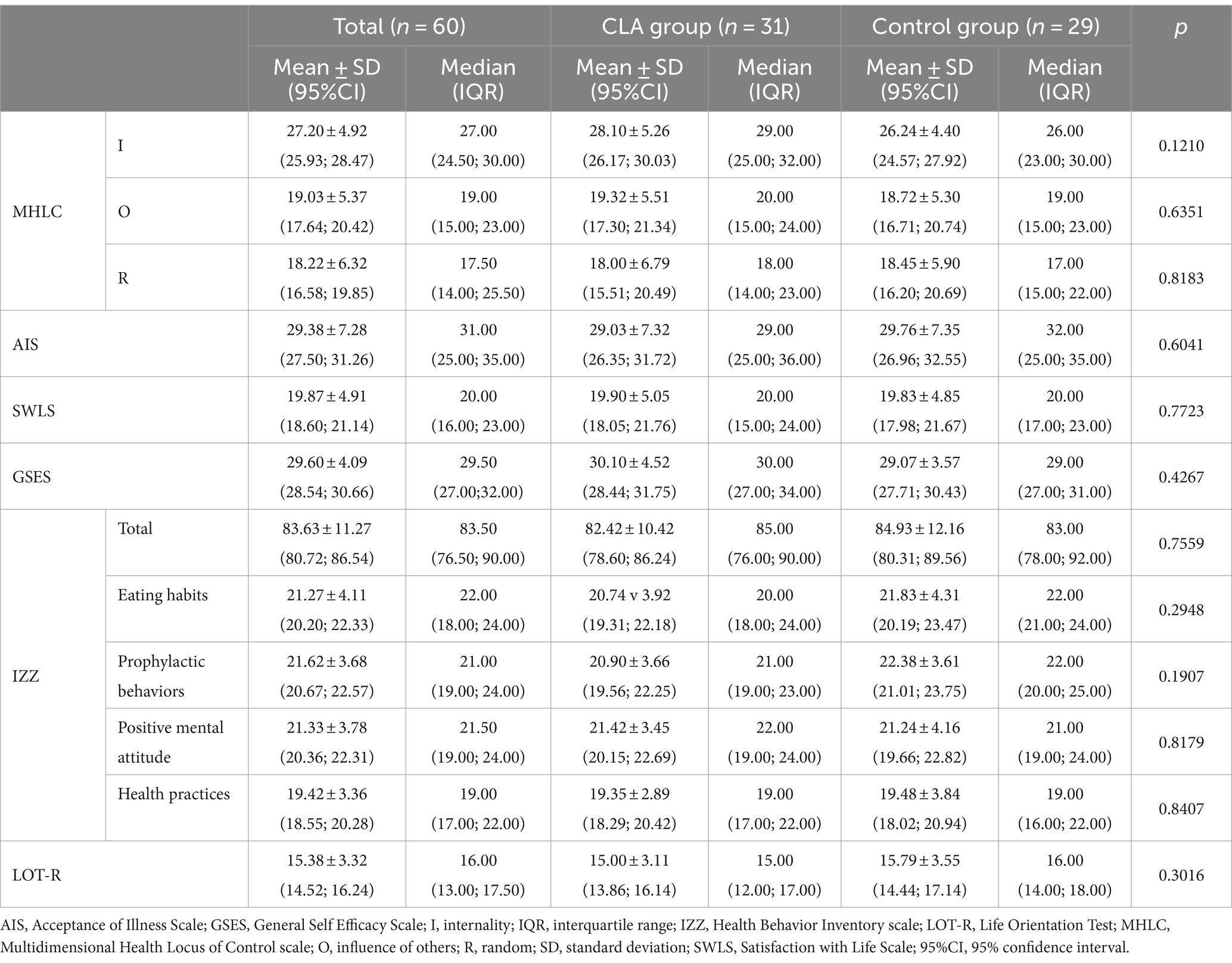
The study workflow is presented in Figure 1. In total, 187 subjects were assessed to meet inclusion and exclusion criteria in the Department of Internal Medicine, Metabolic Disorders and Hypertension, Poznan University of Medical Sciences, Poland. Among them, 81 women were selected for the study. Seven participants refused to participate, so 74 individuals were randomly divided into two groups: the CLA group (n = 37) and the placebo group (n = 37). Moreover, one woman refused to complete the psychological tests and was excluded from the analysis. Sixty participants completed the intervention and were included in the final analysis, with no serious adverse effects reported. Two participants reported nausea and one woman had a rash. The baseline characteristics of the study population were presented previously (25, 26, 29). There were no differences between the CLA and control groups in the results of psychological tests for subjects who were included in the study (Table 1). Similarly, when we compared subjects who completed the study, we noted no significant differences between groups (Table 2).
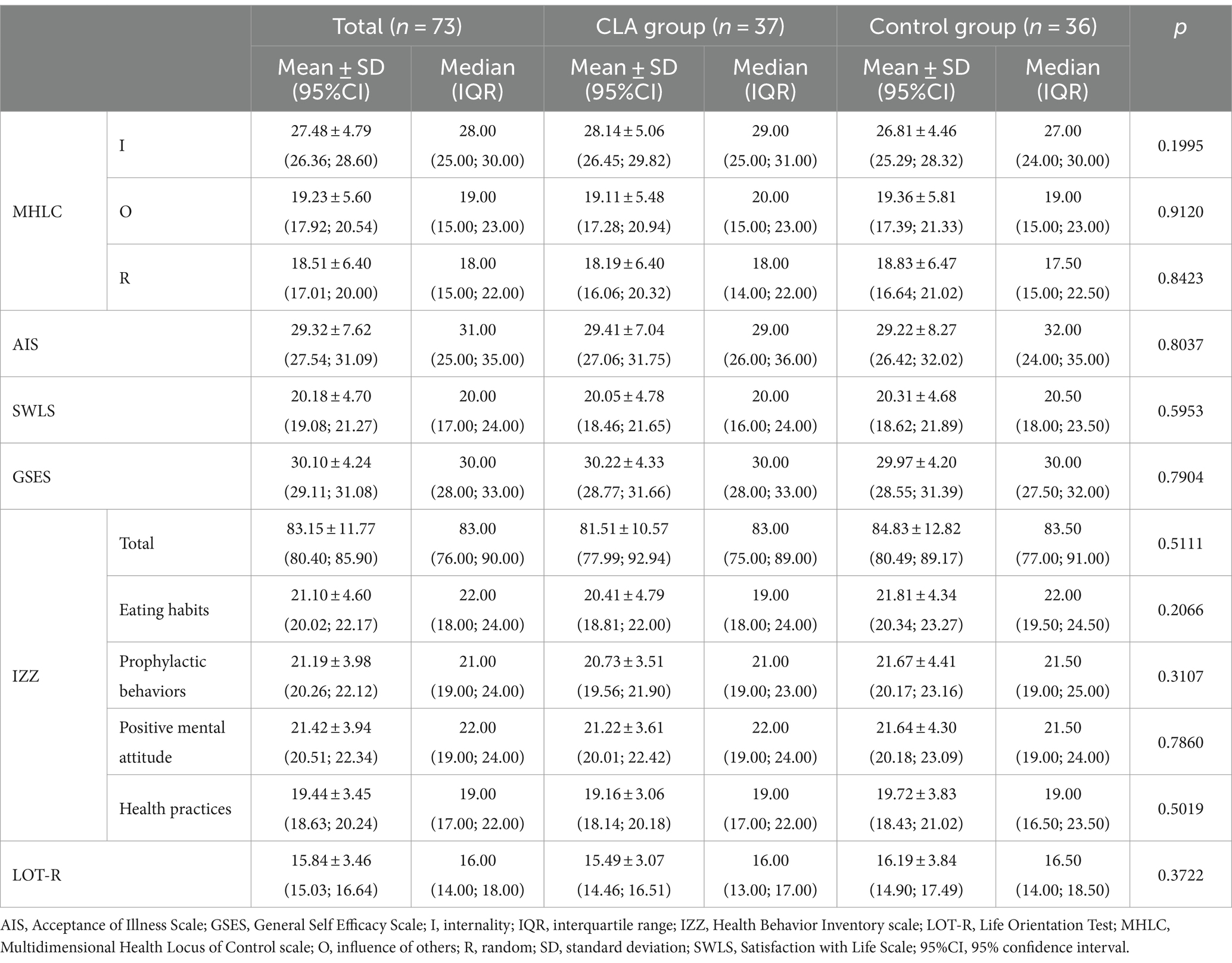
Table 1. Comparison of the results of psychological tests between subjects who were included to the study.
3.2 Comparison of the results of psychological tests between subjects who completed and not complete the study
The analysis revealed that women who dropped out from the project obtained higher scores in the GSES (p = 0.0490) and the LOT-R (p = 0.0087) scores than those who completed the study, indicating that those who did not complete the study had a greater sense of self-efficacy and were characterized by a higher level of optimism (Table 3).
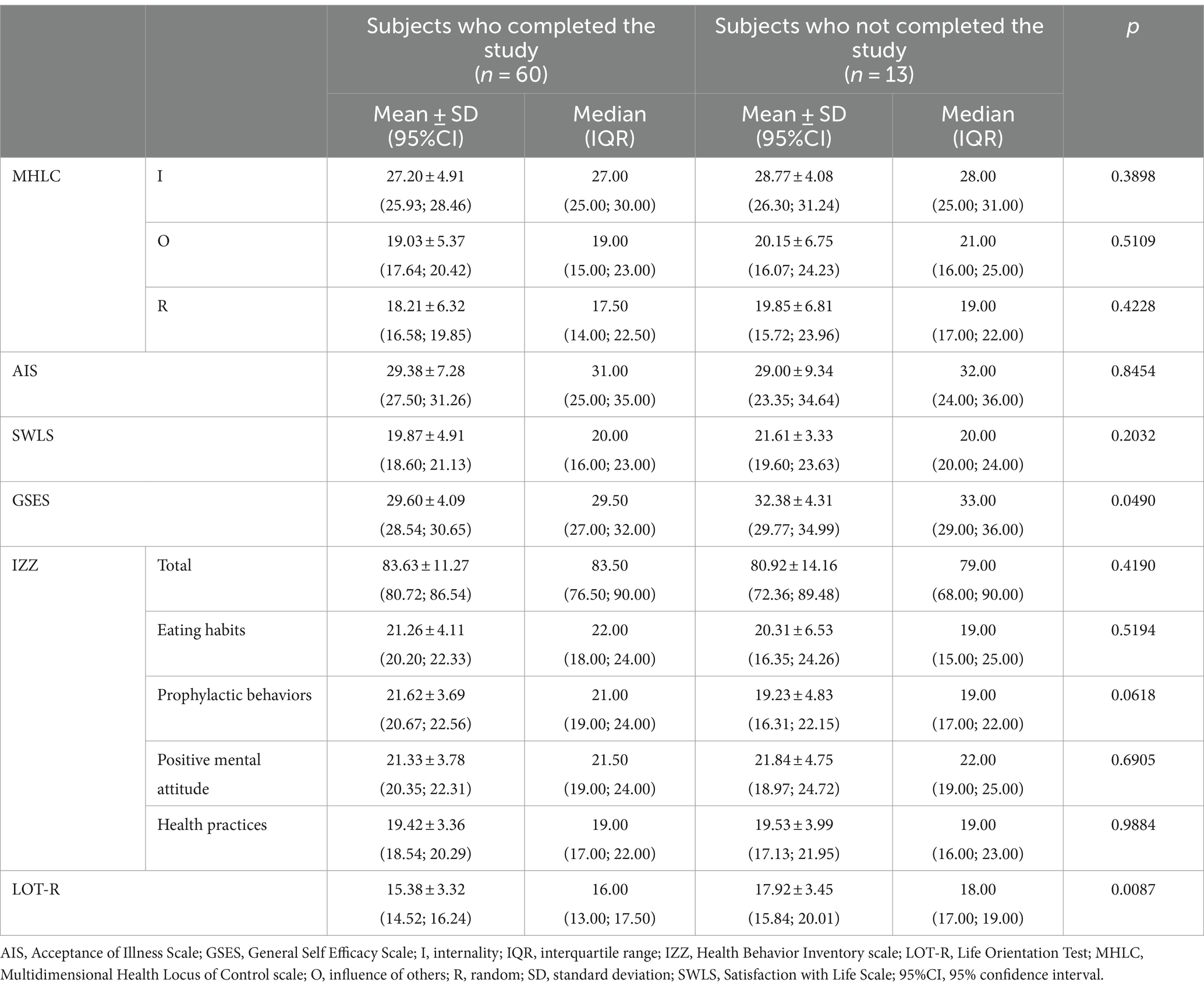
Table 3. Comparison of the results of psychological tests between subjects who completed and not completed the study.
3.3 Comparison of subjects who decreased and increased body weight after the intervention period
There were no differences in the psychological test results in the total population between subjects who decreased and increased body weight after the intervention period (Table 4). Similarly, there were no differences in the results of the psychological questionnaires between participants who decreased and increased body weight, both in the CLA and control groups (Table 5).
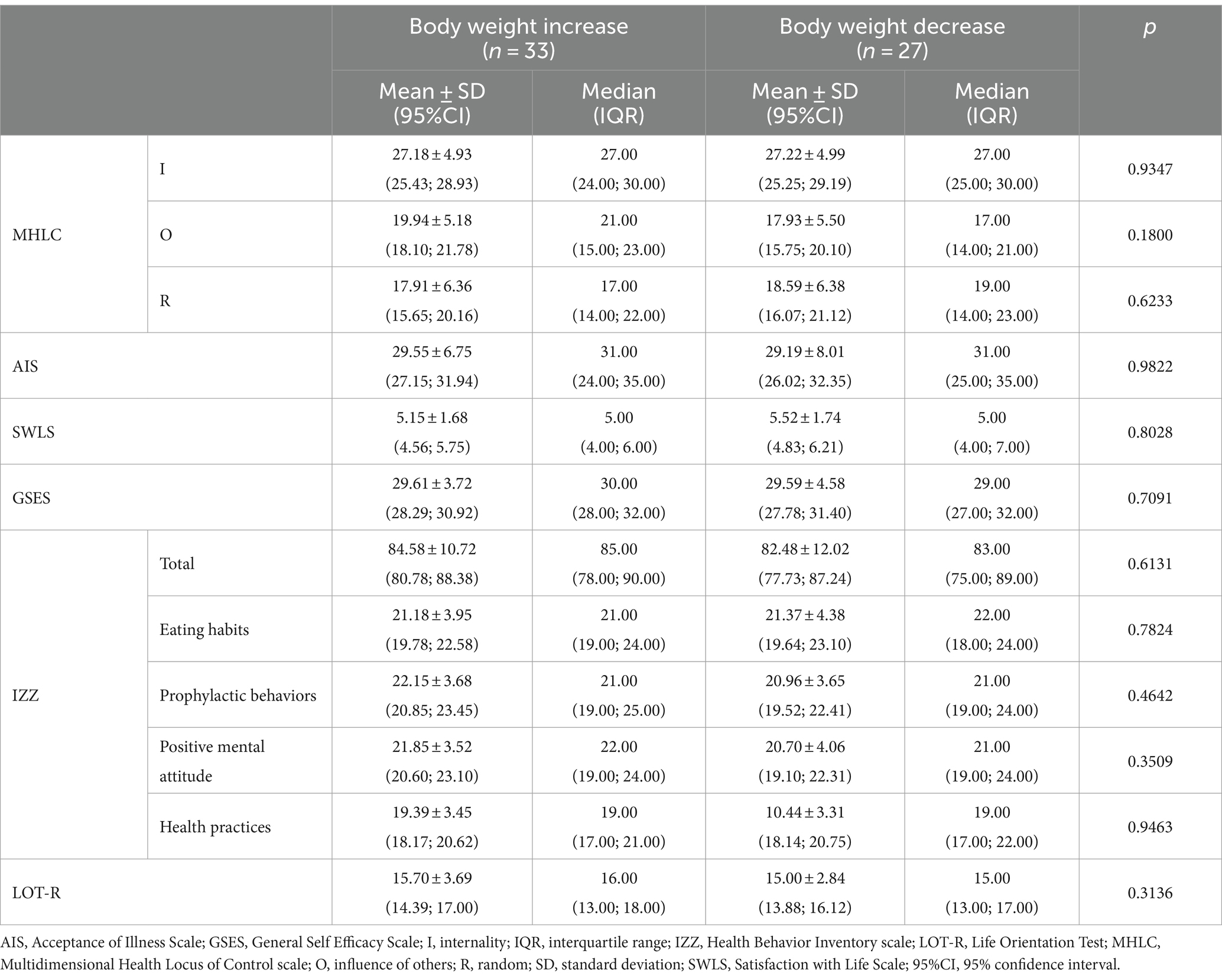
Table 4. Comparison of the results of psychological tests between subjects who decreased and increased body weight.
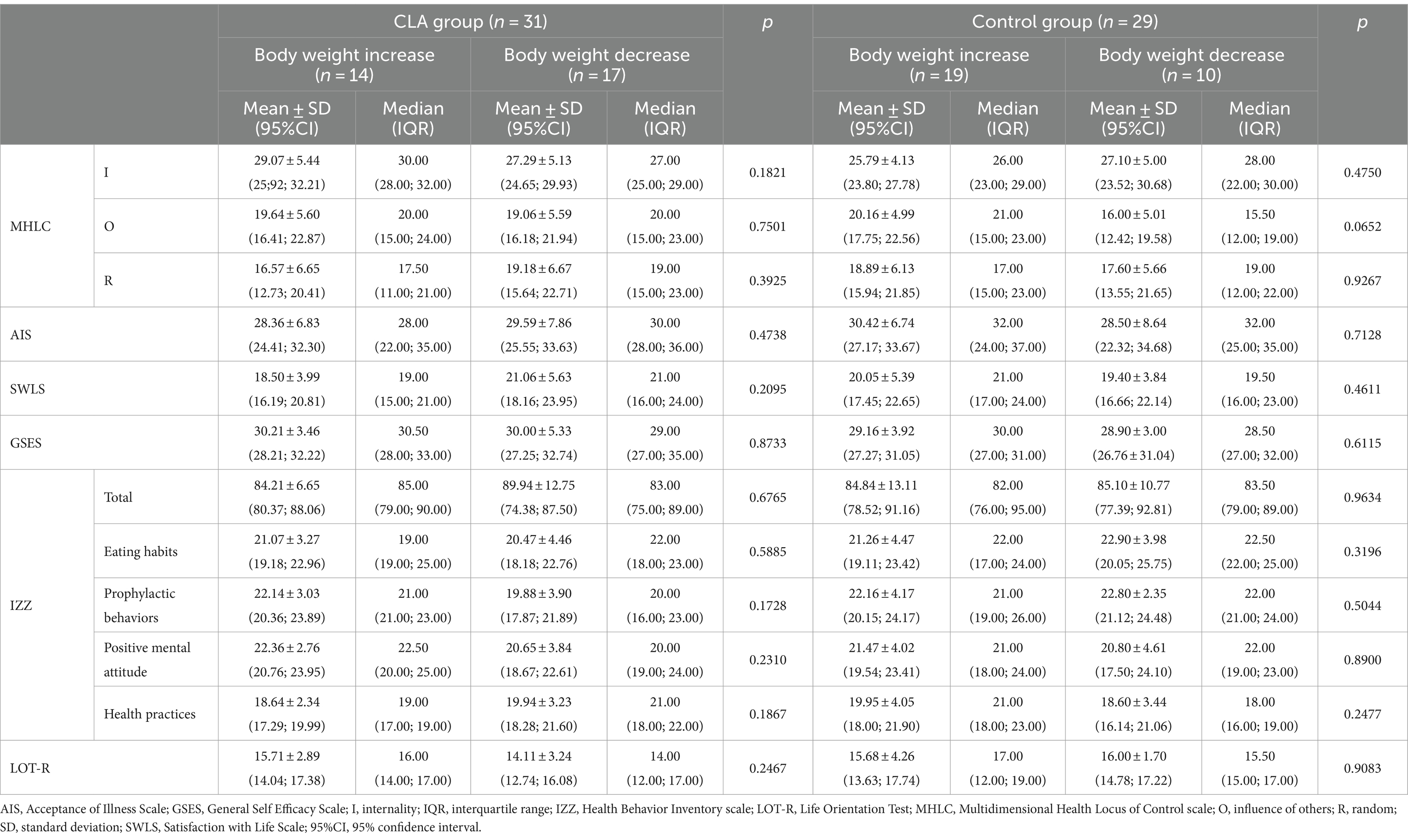
Table 5. Comparison of the results of psychological tests between subjects in the intervention and control groups who decreased and increased body weight.
3.4 Linear regression analysis
Univariate linear regression analysis was subsequently performed to assess the relationship between age, group and results of psychological tests with body weight changes after the intervention. Table 6 shows that the SWLS results (p = 0.0290) were significantly associated with body weight changes. The variables from univariate analysis with p < 0.1 (MHLC O and SWLS), as well as age and group, were subsequently entered into multivariate linear regression (Table 7) demonstrating that the SWLS results (p = 0.0345) were independent negative predictors of body weight changes. Higher levels of life satisfaction were associated with more significant weight loss after the intervention.
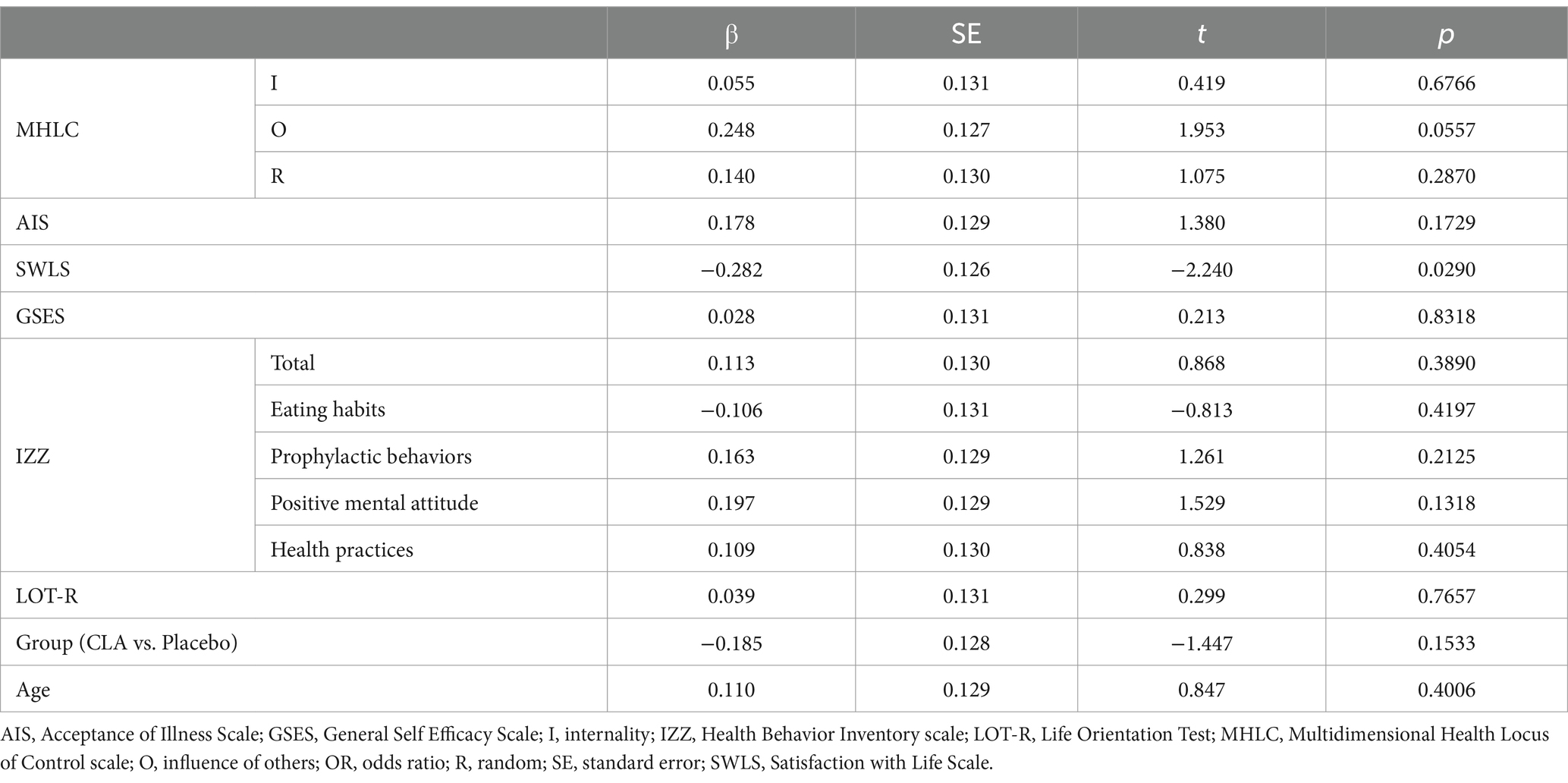
Table 6. Univariate linear regression analysis for the various different variables associated with body weight changes.
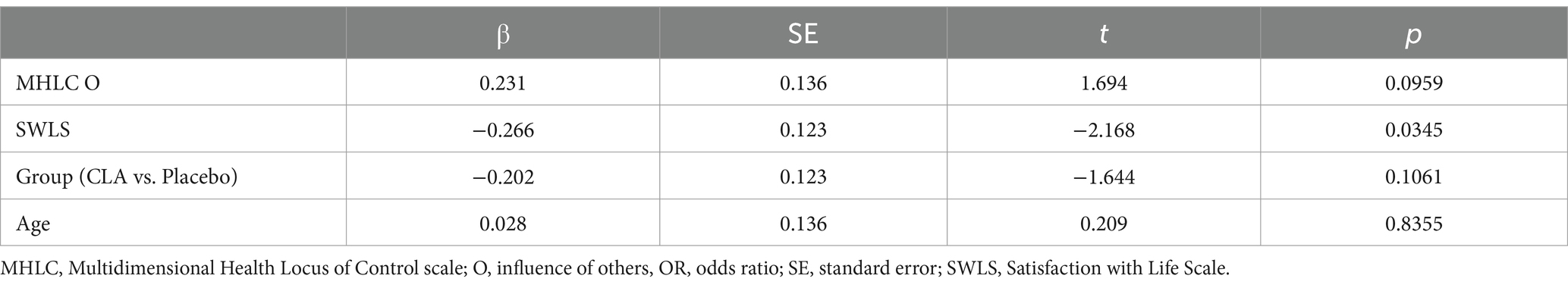
Table 7. Multivariate linear regression analysis for the various different variables associated with body weight changes.
4 Discussion
Here, we found that psychological factors like high self-efficacy and optimism levels may determine the risk of discontinuation of the intervention, while satisfaction with life may impact the effectiveness of the intervention in body weight reduction.
To obtain body weight reduction, 74 women included in this three-month randomized trial were divided into two groups receiving, respectively, capsules containing CLA or sunflower oil. However, as we reported previously (25, 26), a 12-week intervention with CLA supplementation was ineffective in reducing anthropometric indicators including body weight, BMI and waist circumference, as we observed no differences between the intervention and placebo groups. However, significant differences between groups were found in hip circumference (25) and body composition parameters (total body fat, android adipose tissue, gynoid adipose tissue, visceral adipose tissue and lean body mass to height) (26). These results were in contrast to the previous meta-analysis which reported that CLA supplementation significantly reduced body weight and BMI in participants with metabolic syndrome (34). Another meta-analysis conducted by Onakpoya et al. (20) assessed long-term (> 6 months) effects of CLA and also noticed a significant reduction in body weight and fat mass in excessive body weight subjects. However, the authors of this meta-analysis emphasized that these effects are small, therefore, the clinical relevance is uncertain. The next meta-analysis noted that supplementation with CLA, slightly but not clinically relevant, reduced body weight and fat mass, as well as increased lean body mass in overweight and obese subjects (35). Also, a recent meta-analysis demonstrated an improvement in anthropometric parameters and body composition after CLA supplementation in adults (36). However, Liang et al. (21), in their meta-analysis, demonstrated that CLA supplementation during exercise programs did not improve body weight but significantly reduced fat mass. Taking into account the inconsistency in the obtained results we hypothesized that psychological factors might affect the success of the CLA intervention and ability to complete the study.
Self-efficacy refers to the level of confidence a subject possesses in their ability to successfully engage in behaviors that enable them to accomplish specific tasks (37). This confidence can be specific to a particular domain or include a general belief about the likelihood of success in various activities (38). It was suggested that subjects with a higher level of self-efficacy are more likely to be successful during a behavioral change intervention (37). Moreover, a higher level of self-efficacy is more likely to adopt and engage in various health behaviors (39, 40). However, studies assessing self-efficacy’s role in body weight reduction provide unequivocal results (41–44). Some studies reported no association between baseline self-efficacy and weight change (41), while others found that higher baseline self-efficacy was associated with more significant weight loss (43, 44) Conversely, some researchers suggested that higher self-efficacy at baseline was associated with lower weight loss (12, 42). Self-efficacy was also related to the ability to weight loss maintenance. Mishali et al. (45) found that subjects who managed to maintain their weight reduction 2–5 years after the bariatric surgery had higher general self-efficacy than those who did not. In addition, recently, self-efficacy was found to be a strong factor of health behavior change in overweight and obese subjects (46). Our study, however, did not show an association between self-efficacy and the ability to reduce body weight after CLA supplementation in overweight and obese women. Nevertheless, self-efficacy may determine success in completing the intervention, as we observed that subjects who did not complete the study had a greater level of self-efficacy. Our findings are in contrast to previous results. Björkman et al. (13) reported that subjects with early attrition scored lower on self-efficacy compared to those patients who completed the 12-month treatment. However, this study assessed self-efficacy using other methods than in our project. Our findings can be explained by the fact that high baseline self-efficacy in the context of weight loss efforts might suggest either overconfidence or a limited understanding of the challenges associated with weight management (47).
Dispositional optimism refers to psychological factors that involve a general belief or expectation that positive outcomes, rather than negative outcomes, will prevail in one’s future (48). This trait has been associated with various effects on health behaviors, emotional wellbeing, and health outcomes (49). Dispositional optimism may also be linked to a reduced risk of some diseases and mortality rates (50). Several studies also investigated the association between optimism level and body weight, with most reporting a negative association between body weight and optimism level, especially in women (51, 52). Robert et al. (53) showed that individuals with a more optimistic outlook were less prone to being underweight or obese in comparison to those with a less optimistic disposition, whereas Fontaine and Cheskin (54) noted that the overall LOT-R and optimism subscales did not correlate with either attendance or weight reduction. Herein, we did not observe any differences in the LOT-R test results between subjects who decreased and increased body weight after the intervention period. Nevertheless, subjects who dropped out obtained higher scores in the LOT-R tests and were characterized by higher optimism levels. This is one of the first studies which compared the LOT-R test results between subjects who completed and did not complete the trial. Unfortunately, the number of subjects who dropped out of the study was relatively small compared to the group that completed the study, therefore, the apparent difference between subjects could be due to random chance. Indeed, optimistic subjects were previously considered to be more persistent in achieving their goals than less optimistic subjects (55). Moreover, some studies showed that optimism reduces dropout intentions (56) and actual college education dropout among students (57).
Health behaviors encompass all actions related to a subject’s health, which can positively or negatively affect their wellbeing (58). Engaging in pro-health behaviors contributes to the improvement of one’s overall health, whereas engaging in detrimental health behaviors can have adverse consequences on one’s wellbeing (59). Moreover, individuals who are highly motivated to improve their health may be more likely to complete the study, resulting in lower drop-out rates, whereas less motivated or interested individuals may be more inclined to drop out (60, 61). Our study, however, did not confirm this hypothesis as we showed no differences in total scores in the IZZ test and the scores obtained in each domain (eating habits, prophylactic behaviors, positive mental attitude, health practices) between subjects who completed and did not complete the study and between participants who decreased and increased body weight after the intervention period.
Locus of control refers to the belief subjects have in the amount of control they have over their lives (62). Based on the MHLC questionnaire, the locus of control can be divided into three dimensions: internal locus of control, chance or random locus of control and powerful others (external) locus of control (63). The internal locus of control seems to be more advantageous, as subjects who hold the belief that they are accountable for their health tend to exhibit healthier behaviors more frequently (64). In contrast, people with an external locus of control believe that their health is influenced by others, e.g., health professionals (65). Subjects with a random locus of control believe that health outcomes are determined by chance, luck, fate, or randomness and may be less likely to take preventative measures since they feel health outcomes are largely unpredictable or uncontrollable (63). Previous studies showed that subjects with excessive body weight are both more externally (66, 67) and more internally (68) oriented than non-obese subjects. Furthermore, a recent meta-analysis reported that an external locus of control was inversely correlated with healthy lifestyle behavior, including diet and physical activity, but was positively associated with BMI in individuals with type 2 diabetes mellitus (69). Moreover, studies that investigated the relationship between locus control and body weight reduction reported inconsistent findings. An internal locus of control was identified as a predictor of body weight decrease in several (11, 70), albeit not all, studies (13). Adolfsson et al. (11) found that body weight reduction was significantly associated with an internal locus of control among participants in a behavior modification weight loss program. In addition, Gierszewski (70) showed a negative relationship between social support and weight reduction in the case of an internal locus of control for subjects who participate in nutrition and weight reduction program. Contrary, Björkman et al. (13) found no statistically significant associations between body weight decrease after a very low-energy diet intervention and locus of control. However, women who completed the treatment had higher locus of control scores than women who dropped out. These results are partly in line with our results as we found no differences in scores obtained in the MHLC scale between subjects who successfully decreased and increased body weight. However, we also did not note differences in locus of control between participants who completed and did not complete the intervention.
Acceptance of the disease and satisfaction with life are two very important factors affecting the mental state (71). Previously, Katsaiti (72) reported that excessive body weight had a detrimental impact on life satisfaction, whereas Wang et al. (73) showed that greater adiposity was associated with lower quality of life but not life satisfaction in elderly subjects. Moreover, Urbano-Mairena et al. (74) showed that optimal body weight had a positive impact on life satisfaction in children compared to overweight and obese individuals. In addition, Górczewska and Jakubowska-Pietkiewicz (71) found that subjects with malnutrition had the lowest acceptance of the disease, while overweight women presented the lowest satisfaction with life. These factors also offer insights into the subject’s adaptation to the disease and, therefore, may determine the effectiveness of body weight reduction intervention. When subjects accept their health condition, they are more likely to engage in behaviors aimed at managing and improving their health which could include activities leading to body weight reduction (75, 76). Moreover, subjects who are more satisfied with their lives may be more motivated to care of their health, which could involve maintaining a healthy diet and regular physical activity (77). Indeed, we demonstrated that the SWLS test results but not the AIS test were independent predictors of body weight changes.
Our study has some limitations, including the small sample size, short intervention period and lack of information about the adherence levels. Moreover, to get a more homogeneous population, our study was conducted in overweight or obese women. Therefore, our results may not be generalized to other populations. Besides, psychological factors after the intervention were not evaluated to determine how the intervention affected psychological outcomes. Furthermore, we only evaluated general self-efficacy and did not determine situation-specific self-efficacy. Additionally, the number of subjects who dropped out of the study was relatively small compared to the group that completed the study. Therefore, the apparent difference between subjects who completed and did not complete the trial could be due to random chance. The use of sunflower oil as a placebo might also be considered as a study limitation as this oil contains linoleic acid, which can be partly biohydrogenated by the bacteria into CLA (78).
This is the first study that analyzed how psychological factors may determine the effectiveness of CLA supplementation in body weight reduction in overweight and obese women and the psychological factors responsible for the discontinuation of the intervention. Although we used CLA as a supplement in the study, the findings appear to be broadly applicable to other weight-loss research, as the obtained results emphasize the importance of a multidisciplinary approach in clinical studies. The strengths of the study also included strictly defined inclusion and exclusion criteria and a homogeneous population. Moreover, this well-designed randomized controlled trial was performed per CONSORT guidelines (23).
5 Conclusion
In conclusion, psychological factors like self-efficacy and optimism may be associated with a higher risk of withdrawal from the study, while satisfaction with life may have an impact on the effectiveness of body weight reduction. However, further larger studies are needed to confirm these findings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Poznan University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MJ: Data curation, Formal analysis, Writing – original draft. JP: Data curation, Writing – review & editing. AB-P: Investigation, Methodology, Writing – review & editing. EM: Conceptualization, Investigation, Methodology, Writing – review & editing. AL: Methodology, Writing – review & editing. KJ-P: Writing – review & editing. JC-P: Writing – review & editing. PB: Writing – review & editing. JW: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Nutricia Foundation (grant no. 504–06–01103115-000-15-07588).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1342452/full#supplementary-material
References
1. World Health Organization. Obesity and overweight. World Health Organization (2016). Available at: http://www.who.int/mediacentre/factsheets/fs311/en/ (Accessed March 20, 2017).
2. World Obesity Federation. World obesity atlas. (2023). Available at: https://data.worldobesity.org/publications/?cat=19 (Accessed June 10, 2023).
3. Wharton, S, Lau, DCW, Vallis, M, Sharma, AM, Biertho, L, Campbell-Scherer, D, et al. Obesity in adults: a clinical practice guideline. CMAJ. (2020) 192:E875–91. doi: 10.1503/cmaj.191707
4. Haase, CL, Lopes, S, Olsen, AH, Satylganova, A, Schnecke, V, and McEwan, P. Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Int J Obes. (2021) 45:1249–58. doi: 10.1038/s41366-021-00788-4
5. Anderson, JW, Konz, EC, Frederich, RC, and Wood, CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. (2001) 74:579–84. doi: 10.1093/AJCN/74.5.579
6. Seagle, HM, Strain, GW, Makris, A, and Reeves, RS. Position of the American dietetic association: weight management. J Am Diet Assoc. (2009) 109:330–46. doi: 10.1016/J.JADA.2008.11.041
7. Bąk-Sosnowska, M, Pawlak, A, and Skrzypulec-Plinta, V. Do psychological factors help to reduce body mass in obesity or is it vice versa? Selected psychological aspects and effectiveness of the weight-loss program in the obese patients. Health Psychol Res. (2013) 1:10. doi: 10.4081/HPR.2013.E10
8. Hays, LM, Finch, EA, Saha, C, Marrero, DG, and Ackermann, RT. Effect of self-efficacy on weight loss: a psychosocial analysis of a community-based adaptation of the diabetes prevention program lifestyle intervention. Diabetes Spectr. (2014) 27:270–5. doi: 10.2337/DIASPECT.27.4.270
9. Linde, JA, Rothman, AJ, Baldwin, AS, and Jeffery, RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychol. (2006) 25:282–91. doi: 10.1037/0278-6133.25.3.282
10. Nezami, BT, Lang, W, Jakicic, JM, Davis, KK, Polzien, K, Rickman, AD, et al. The effect of self-efficacy on behavior and weight in a behavioral weight-loss intervention. Health Psychol. (2016) 35:714–22. doi: 10.1037/HEA0000378
11. Adolfsson, B, Andersson, I, Elofsson, S, Rössner, S, and Undén, AL. Locus of control and weight reduction. Patient Educ Couns. (2005) 56:55–61. doi: 10.1016/j.pec.2003.12.005
12. Matsuo, T, Murotake, Y, Kim, MJ, Akiba, T, Shimojo, N, Kim, MK, et al. High general self-efficacy is associated with less weight loss under a supervised dietary modification program. Obes Res Clin Pract. (2010) 4:e135–44. doi: 10.1016/J.ORCP.2009.12.002
13. Björkman, S, Wallengren, O, Laurenius, A, Eliasson, B, and Larsson, I. Locus of control and self-efficacy in relation to 12-month weight change after non-surgical weight loss treatment in adults with severe obesity – a clinical cohort study. Obes Med. (2022) 32:100409. doi: 10.1016/J.OBMED.2022.100409
14. Ibrahim, K, and El-Sayed, E. Dietary conjugated linoleic acid and medium-chain triglycerides for obesity management. J Biosci. (2021) 46:12. doi: 10.1007/s12038-020-00133-3
15. Griinari, JM, Corl, BA, Lacy, SH, Chouinard, PY, Nurmela, KVV, and Bauman, DE. Conjugated linoleic acid is synthesized endogenously in lactating dairy cows by delta(9)-desaturase. J Nutr. (2000) 130:2285–91. doi: 10.1093/JN/130.9.2285
16. Ma, DWL, Wierzbicki, AA, Field, CJ, and Clandinin, MT. Preparation of conjugated linoleic acid from safflower oil. JAOCS. (1999) 76:729–30. doi: 10.1007/s11746-999-0167-3
17. den Hartigh, LJ . Conjugated linoleic acid effects on cancer, obesity, and atherosclerosis: a review of pre-clinical and human trials with current perspectives. Nutrients. (2019) 11:370. doi: 10.3390/NU11020370
18. Castro-Webb, N, Ruiz-Narváez, EA, and Campos, H. Cross-sectional study of conjugated linoleic acid in adipose tissue and risk of diabetes. Am J Clin Nutr. (2012) 96:175–81. doi: 10.3945/AJCN.111.011858
19. Olson, JM, Haas, AW, Lor, J, McKee, HS, and Cook, ME. A comparison of the anti-inflammatory effects of cis-9, trans-11 conjugated linoleic acid to celecoxib in the collagen-induced arthritis model. Lipids. (2017) 52:151–9. doi: 10.1007/S11745-016-4228-8
20. Onakpoya, IJ, Posadzki, PP, Watson, LK, Davies, LA, and Ernst, E. The efficacy of long-term conjugated linoleic acid (CLA) supplementation on body composition in overweight and obese individuals: a systematic review and meta-analysis of randomized clinical trials. Eur J Nutr. (2012) 51:127–34. doi: 10.1007/S00394-011-0253-9
21. Liang, CW, Cheng, HY, Lee, YH, Liou, TH, De, LC, and Huang, SW. Effects of conjugated linoleic acid and exercise on body composition and obesity: a systematic review and meta-analysis. Nutr Rev. (2023) 81:397–415. doi: 10.1093/NUTRIT/NUAC060
22. Sawicka-Gutaj, N, Gruszczyński, D, Guzik, P, Mostowska, A, and Walkowiak, J. Publication ethics of human studies in the light of the declaration of Helsinki – a mini-review. JMS. (2022) 91:e700–13. doi: 10.20883/MEDICAL.E700
23. Moher, D, Hopewell, S, Schulz, KF, Montori, V, Gøtzsche, PC, Devereaux, PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. (2010) 340:c869. doi: 10.1136/bmj.c869
24. Metabolic consequences of conjugated linoleic acid supplementation in overweight and obese subjects. German clinical trials register. Available at: https://drks.de/search/en/trial/DRKS00010462 (Accessed April 22, 2023).
25. Madry, E, Chudzicka-Strugala, I, Grabańska-Martyńska, K, Malikowska, K, Grebowiec, P, Lisowska, A, et al. Twelve weeks CLA supplementation decreases the hip circumference in overweight and obese women. A double-blind, randomized, placebo-controlled trial. Acta Sci Pol Technol Aliment. (2016) 15:107–13. doi: 10.17306/J.AFS.2016.1.11
26. Mądry, E, Malesza, IJ, Subramaniapillai, M, Czochralska-Duszyńska, A, Walkowiak, M, Miśkiewicz-Chotnicka, A, et al. Body fat changes and liver safety in obese and overweight women supplemented with conjugated linoleic acid: a 12-week randomised, double-blind, placebo-controlled trial. Nutrients. (2020) 12:1–9. doi: 10.3390/NU12061811
27. Łochocka, K, Glapa, A, Nowak, JK, Duś-Żuchowska, M, Grabańska, K, Bogdański, P, et al. Clinical outcomes of conjugated linoleic acid supplementation in the overweight and the obese: a study protocol. JMS. (2014) 83:318–21. doi: 10.20883/MEDICAL.E86
28. Dus-Zuchowska, M, Madry, E, Krzyzanowska, P, Bogdanski, P, and Walkowiak, J. Twelve-week-conjugated linoleic acid supplementation has no effects on the selected markers of atherosclerosis in obese and overweight women. Food Nutr Res. (2016) 60:32776. doi: 10.3402/FNR.V60.32776
29. Walkowiak, J, Malikowska, K, Glapa, A, Bogdański, P, Fidler-Witoń, E, Szulińska, M, et al. Conjugated linoleic acid does not affect digestion and absorption of fat and starch-a randomized, double-blinded, placebo-controlled parallel study. J Breath Res. (2017) 12:016010. doi: 10.1088/1752-7163/AA872D
30. Jamka, M, Czochralska-Duszyńska, A, Mądry, E, Lisowska, A, Jończyk-Potoczna, K, Cielecka-Piontek, J, et al. The effect of conjugated linoleic acid supplementation on densitometric parameters in overweight and obese women - a randomised controlled trial. Medicina (Kaunas). (2023) 59:1690. doi: 10.3390/MEDICINA59091690
31. Juczyński, Z . Measurement tools in health promotion and psychology. Warszawa: Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego (2012).
32. Walkowiak, J, Bajerska, J, Kargulewicz, A, Lisowska, A, Siedlerski, G, Szczapa, T, et al. Single dose of green tea extract decreases lipid digestion and absorption from a test meal in humans. Acta Biochim Pol. (2013) 60:481–3. doi: 10.18388/abp.2013_2010
33. Lochocka, K, Bajerska, J, Glapa, A, Fidler-Witon, E, Nowak, JK, Szczapa, T, et al. Green tea extract decreases starch digestion and absorption from a test meal in humans: a randomized, placebo-controlled crossover study. Sci Rep. (2015) 5:12015. doi: 10.1038/SREP12015
34. Kim, B, Lim, HR, Lee, H, Lee, H, Kang, W, and Kim, E. The effects of conjugated linoleic acid (CLA) on metabolic syndrome patients: a systematic review and meta-analysis. J Funct Foods. (2016) 25:588–98. doi: 10.1016/J.JFF.2016.07.010
35. Namazi, N, Irandoost, P, Larijani, B, and Azadbakht, L. The effects of supplementation with conjugated linoleic acid on anthropometric indices and body composition in overweight and obese subjects: a systematic review and meta-analysis. Crit Rev Food Sci Nutr. (2019) 59:2720–33. doi: 10.1080/10408398.2018.1466107
36. Asbaghi, O, Shimi, G, Hosseini Oskouie, F, Naseri, K, Bagheri, R, Ashtary-Larky, D, et al. The effects of conjugated linoleic acid supplementation on anthropometrics and body composition indices in adults: a systematic review and dose-response meta-analysis. Br J Nutr. (2024) 131:406–28. doi: 10.1017/S0007114523001861
37. Bandura, A . Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1977) 84:191–215. doi: 10.1037/0033-295X.84.2.191
38. Elias, SM, Barney, CE, and Bishop, JW. The treatment of self-efficacy among psychology and management scholars. J Appl Soc Psychol. (2013) 43:811–22. doi: 10.1111/JASP.12007
39. Sohler, NL, Jerant, A, and Franks, P. Socio-psychological factors in the expanded health belief model and subsequent colorectal cancer screening. Patient Educ Couns. (2015) 98:901–7. doi: 10.1016/J.PEC.2015.03.023
40. Gwaltney, CJ, Metrik, J, Kahler, CW, and Shiffman, S. Self-efficacy and smoking cessation: a meta-analysis. Psychol Addict Behav. (2009) 23:56–66. doi: 10.1037/A0013529
41. Fontaine, KR, and Cheskin, LJ. Self-efficacy, attendance, and weight loss in obesity treatment. Addict Behav. (1997) 22:567–70. doi: 10.1016/S0306-4603(96)00068-8
42. Martin, PD, Dutton, GR, and Brantley, PJ. Self-efficacy as a predictor of weight change in African-American women. Obes Res. (2004) 12:646–51. doi: 10.1038/OBY.2004.74
43. Wamsteker, EW, Geenen, R, Iestra, J, Larsen, JK, Zelissen, PMJ, and Van Staveren, WA. Obesity-related beliefs predict weight loss after an 8-week low-calorie diet. J Am Diet Assoc. (2005) 105:441–4. doi: 10.1016/j.jada.2004.12.031
44. Linde, JA, Jeffery, RW, Levy, RL, Sherwood, NE, Utter, J, Pronk, NP, et al. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. Int J Obes Relat Metab Disord. (2004) 28:418–25. doi: 10.1038/SJ.IJO.0802570
45. Mishali, M, and Kisner, M. Psycho-behavioral factors related to weight regain after bariatric surgery. Obes Surg. (2022) 32:3041–6. doi: 10.1007/S11695-022-06195-6
46. Timkova, V, Minarikova, D, Fabryova, L, Buckova, J, Minarik, P, Katreniakova, Z, et al. Facilitators and barriers to behavior change in overweight and obesity management using the COM-B model. Front Psychol. (2024) 15:1280071. doi: 10.3389/FPSYG.2024.1280071
47. Sutin, AR, and Terracciano, A. Perceived weight discrimination and obesity. PLoS One. (2013) 8:e70048. doi: 10.1371/JOURNAL.PONE.0070048
48. Scheier, MF, and Carver, CS. On the power of positive thinking: the benefits of being optimistic. Curr Dir Psychol Sci. (1993) 2:26–30. doi: 10.1111/1467-8721.ep10770572
49. Carver, CS, Scheier, MF, and Segerstrom, SC. Optimism. Clin Psych Rev. (2010) 30:879–89. doi: 10.1016/J.CPR.2010.01.006
50. Tindle, HA, Chang, YF, Kuller, LH, Manson, JE, Robinson, JG, Rosal, MC, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the women’s health initiative. Circulation. (2009) 120:656–62. doi: 10.1161/CIRCULATIONAHA.108.827642
51. Serlachius, A, Pulkki-Råback, L, Juonala, M, Sabin, M, Lehtimäki, T, Raitakari, O, et al. Does high optimism protect against the inter-generational transmission of high BMI? The cardiovascular risk in young Finns study. J Psychosom Res. (2017) 100:61–4. doi: 10.1016/J.JPSYCHORES.2017.07.006
52. Kelloniemi, H, Ek, E, and Laitinen, J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. (2005) 45:169–76. doi: 10.1016/J.APPET.2005.05.001
53. Robert, M, Buscail, C, Allès, B, Shankland, R, Tavolacci, MP, Déchelotte, P, et al. Dispositional optimism is associated with weight status, eating behavior, and eating disorders in a general population-based study. Int J Eat Disord. (2020) 53:1696–708. doi: 10.1002/EAT.23347
54. Fontaine, FR, and Cheskin, LJ. Optimism and obesity treatment outcomes. J Clin Psychol. (1999) 55:141–3. doi: 10.1002/(SICI)1097-4679(199901)55:1<141::AID-JCLP15>3.0.CO;2-G
55. Nes Solberg, L, Segerstrom, SC, and Sephton, SE. Engagement and arousal: optimism’s effects during a brief stressor. Personal Soc Psychol Bull. (2005) 31:111–20. doi: 10.1177/0146167204271319
56. Chemers, MM, Hu, LT, and Garcia, BF. Academic self-efficacy and first-year college student performance and adjustment. J Educ Psychol. (2001) 93:55–64. doi: 10.1037/0022-0663.93.1.55
57. Solberg Nes, L, Evans, DR, and Segerstrom, SC. Optimism and college retention: mediation by motivation, performance, and adjustment. J Appl Soc Psychol. (2009) 39:1887–912. doi: 10.1111/J.1559-1816.2009.00508.X
58. Gniazdowski, A . Health behaviors: Theoretical issues, an attempt to characterize the health behaviors of polish society. Łódź: Instytut Medycyny Pracy im prof. dr med. Jerzego Nofera (1990).
60. Carter, KF, and Kulbok, PA. Motivation for health behaviours: a systematic review of the nursing literature. J Adv Nurs. (2002) 40:316–30. doi: 10.1046/J.1365-2648.2002.02373.X
61. Coa, K, and Patrick, H. Baseline motivation type as a predictor of dropout in a healthy eating text messaging program. JMIR Mhealth Uhealth. (2016) 4:e5992. doi: 10.2196/MHEALTH.5992
62. Rotter, JB . Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr Gen Appl. (1966) 80:1–28. doi: 10.1037/H0092976
63. Wallston, KA, Wallston, BS, and DeVellis, R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Behav. (1978) 6:160–70. doi: 10.1177/109019817800600107
64. Cobb-Clark, DA, Kassenboehmer, SC, and Schurer, S. Healthy habits: the connection between diet, exercise, and locus of control. J Econ Behav Organ. (2014) 98:1–28. doi: 10.1016/J.JEBO.2013.10.011
65. Sanders, GS, and Suls, JM. Who is responsible for your health? The construct of health locus of control In: G Sanders and J Suls, editors. Social psychology of health and illness. New York: Psychology Press (1892). 65.
66. Tobias, L, and MacDonald, M. Internal locus of control and weight loss: an insufficient condition. J Consult Clin Psychol. (1977) 45:627–53. doi: 10.1037//0022-006X.45.4.647
67. Gruszka, W, Owczarek, AJ, Glinianowicz, M, Bąk-Sosnowska, M, Chudek, J, and Olszanecka-Glinianowicz, M. Can nutritional status in adults be influenced by health locus of control? Int J Environ Res Public Health. (2022) 19:15513. doi: 10.3390/IJERPH192315513
68. Mills, JK, and Cullen, TJ. Locus of control orientation among obese adults in outpatient treatment for obesity. J Psychol. (1994) 128:333–7. doi: 10.1080/00223980.1994.9712737
69. Geerling, R, Kothe, EJ, Anglim, J, Emerson, C, Holmes-Truscott, E, and Speight, J. Personality and weight management in adults with type 2 diabetes: a systematic review. Front Clin Diabetes Healthc. (2022) 3:1044005. doi: 10.3389/FCDHC.2022.1044005
70. Gierszewski, S . The relationship of weight loss, locus of control, and social support. Nurs Res. (1983) 32:43–7. doi: 10.1097/00006199-198301000-00009
71. Górczewska, B, and Jakubowska-Pietkiewicz, E. Is acceptance of disease and life satisfaction of women with postmenopausal osteoporosis dependent on BMI? Psychiatr Pol. (2022) 56:623–34. doi: 10.12740/PP/ONLINEFIRST/130158
72. Katsaiti, MS . Obesity and happiness. Appl Econ. (2011) 44:4101–14. doi: 10.1080/00036846.2011.587779
73. Wang, L, Crawford, JD, Reppermund, S, Trollor, J, Campbell, L, Baune, BT, et al. Body mass index and waist circumference predict health-related quality of life, but not satisfaction with life, in the elderly. Qual Life Res. (2018) 27:2653–65. doi: 10.1007/S11136-018-1904-6
74. Urbano-Mairena, J, Mendoza-Muñoz, M, Carlos-Vivas, J, Pastor-Cisneros, R, Castillo-Paredes, A, Rodal, M, et al. Role of satisfaction with life, sex and body mass index in physical literacy of Spanish children. Children. (2024) 11:181. doi: 10.3390/CHILDREN11020181
75. Starczewska, M, Kujawska, R, Stanisławska, M, Rybicka, A, and Grochans, E. The analysis of health behaviours and illness acceptance in patients with diabetes. Fam Med Prim Care Rev. (2018) 20:352–5. doi: 10.5114/FMPCR.2018.79347
76. Seń, M, Grabowska, B, and Wójcik, J. Health behaviours and degree of acceptance of disease and eating habits among patients with hypothyroidism and Hashimoto’s autoimmune thyroiditis. Med Og Nauk Zdr. (2020) 26:384–9. doi: 10.26444/monz/126691
77. Grant, N, Wardle, J, and Steptoe, A. The relationship between life satisfaction and health behavior: a cross-cultural analysis of young adults. Int J Behav Med. (2009) 16:259–68. doi: 10.1007/S12529-009-9032-X
Keywords: healthy behaviors, psychological factors, wellbeing, self-esteem, self-efficacy
Citation: Jamka M, Popek J, Bukowska-Posadzy A, Mądry E, Lisowska A, Jończyk-Potoczna K, Cielecka-Piontek J, Bogdański P and Walkowiak J (2024) Psychological determinants of the effectiveness of conjugated linoleic acid supplementation in overweight and obese women—a randomized controlled trial. Front. Nutr. 11:1342452. doi: 10.3389/fnut.2024.1342452
Edited by:
Andrew Scholey, Monash University, AustraliaReviewed by:
Marija Takic, University of Belgrade, SerbiaOmorogieva Ojo, University of Greenwich, United Kingdom
Copyright © 2024 Jamka, Popek, Bukowska-Posadzy, Mądry, Lisowska, Jończyk-Potoczna, Cielecka-Piontek, Bogdański and Walkowiak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jarosław Walkowiak, amFyd2Fsa0B1bXAuZWR1LnBs
 Małgorzata Jamka
Małgorzata Jamka Joanna Popek
Joanna Popek Anna Bukowska-Posadzy2
Anna Bukowska-Posadzy2 Edyta Mądry
Edyta Mądry Aleksandra Lisowska
Aleksandra Lisowska Katarzyna Jończyk-Potoczna
Katarzyna Jończyk-Potoczna Judyta Cielecka-Piontek
Judyta Cielecka-Piontek Paweł Bogdański
Paweł Bogdański Jarosław Walkowiak
Jarosław Walkowiak