- 1North Gondar Zone Health Office, Debark, Ethiopia
- 2Department of Nutrition and Dietetics, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 3Department of Epidemiology and Biostatistics, School of Public Health, Asrat Woldeyes Health Science Campus, Debre Berhan University, Debre Berhan, Ethiopia
- 4Department of Public Health, College of Medicine and Health Science, Injibara University, Injibara, Ethiopia
Introduction: The double burden of malnutrition refers to the simultaneous presence of under nutrition and overweight, obesity, or diet-related non-communicable diseases which might occur at the population, household, and individual level. The simultaneous presence of overweight/obese mothers with undernourished children in the same household, as well as overweight children with underweight mothers, holds particular significance. This phenomenon primarily impacts low-income and middle-income countries. The prevalence of double-burden malnutrition at the household level has increased significantly in sub-Saharan African countries. However, there is limited knowledge regarding the extent and factors associated with the double burden of malnutrition among mother–child pairs in Ethiopia. Consequently, the objective of this study was to assess the prevalence and determinants of the double burden of malnutrition among mother–child pairs at the household level in Bahir Dar City, Ethiopia.
Method: In the year 2021, a community-based cross-sectional study design was employed among 702 mother–child pairs in Bahir Dar City from February 28 to March 23. A multistage sampling technique was used to identify study participants who were interviewed using an interviewer-administered questionnaire. The nutritional status of children was evaluated using WHO Anthro Software. To determine the strength of the association, multivariable logistic regression analysis was performed, and adjusted odds ratios with their respective 95% confidence intervals were computed.
Results: The prevalence of the double burden of malnutrition among mother–child pairs was 14.5% (95% CI: 12.8, 15.7%}. Participants who were in the richest wealth index were 2.72 {AOR = 2.72, 95% CI 2.01, 5.63} times more odds of double burden of malnutrition than the poorest. The odds of the double burden of malnutrition among children who had high dietary diversity decreased by 63% {AOR = 0.37, 95% CI 0.22, 0.61} than low dietary diversity. Food secure households were 1.96 {AOR = 1.96, 95% CI 1.13, 3.39} times more likely to have the double burden of malnutrition than food insecure households. The odds of the double burden of malnutrition among mothers who completed college and above decreased by 74% {AOR = 0.26 95% CI 0.121, 0.549} than those unable to read and write.
Conclusions and recommendation: The magnitude of the double burden of malnutrition was lower than the Ethiopian Demographic and Health Survey. Wealth index, dietary diversity, food security, and educational status were significantly associated with the double burden of malnutrition. Therefore, it is recommended to implement public health interventions that target the identified associated factors in order to reduce the burden of double malnutrition.
Introduction
The term malnutrition encompasses two primary categories of conditions. The first category is “under nutrition,” which refers to deficiencies in energy and essential micronutrients, leading to conditions such as stunting, wasting, and underweight. The second category is “over nutrition,” which includes conditions such as overweight, obesity, and diet-related non-communicable diseases (NCDs) (1). Nowadays many countries are facing a double burden of malnutrition (DBM), a coexistence of under nutrition and overweight, obesity, or diet-related non-communicable diseases, affecting most low-income and middle-income countries (LMICs) (2, 3). The simultaneous presence of overweight/obese mothers with undernourished children, as well as underweight mothers with overweight children, within the same household, is a significant and noteworthy phenomenon. This phenomenon highlights the complex and multifaceted nature of malnutrition, where different forms of malnutrition can coexist within a single-family unit. Understanding and addressing this double burden of malnutrition is crucial for developing effective interventions and policies to improve the health and well-being of both mothers and children (4).
The global burden of the double burden of malnutrition (DBM) was 16% which is highly prevalent in Sub-Saharan countries (5). The DBM in households ranged from 1.71 to 17.12% in African countries (6), and 23% from further analysis of 2016 Ethiopian Demographic and Health Survey data (EDHS) (7). The double burden of malnutrition at the household level among mother–child pairs was revealed high in different studies such as 30.6% in Indonesia (8), 15.7% in Palestine (9), 6% in India (10), 24.4% in North Africa (11), and 9% in Addis Ababa and the rural district of Kersa, Ethiopia (12).
Maternal and child under nutrition is responsible for over 10% of the global disease burden, while being overweight/obese leads to at least 2.6 million deaths annually (13). The estimated effects of stunting, severe wasting, and intrauterine growth restriction together were responsible for 2.2 million deaths and 21% of disability-adjusted life-years (DALYs) for children younger than 5 years (14). Nutrition-related factors contribute to approximately 45% of deaths in children aged less than 5 years mainly due to under nutrition (15). Maternal obesity leads to gestational diabetes, pre-eclampsia, hemorrhage, and a higher risk of neonatal and infant death (16–19). In addition, 44% of the diabetes burden, 23% of the ischemic heart disease burden, and between 7 and 41% of certain cancer burdens are attributable to overweight and obesity (20).
The emergence of the double burden of malnutrition can be attributed to a series of global changes known as nutritional transition, demographic transition, and epidemiological transition. These transitions encompass shifts in dietary patterns, population dynamics, and disease profiles that have occurred worldwide. These changes have contributed to the coexistence of under nutrition and over nutrition within populations, leading to the complex issue of the double burden of malnutrition (21–24). These life-course trajectories such as rapidly changing diets, norms of eating, and physical activity patterns, and ecological factors such as pathogen burden and extrinsic mortality risk lead to DBM (25).
The World Health Organization (WHO) proposed a roadmap to tackle the DBM through so-called “double-duty actions” (26). The Global Nutrition Report has committed to eradicating all forms of malnutrition by 2030. Maternal–infant and young child nutrition (MIYCN) initiatives align with the Global Action Plan on Non-Communicable Diseases (NCDs), which includes targets to reduce obesity and other risk factors associated with non-communicable diseases (NCDs). These efforts work in tandem to address the multifaceted challenges of malnutrition and promote the health and well-being of mothers, infants, and young children worldwide (13, 27). The Ethiopian government’s obligation to end child under nutrition by 2030 has stepped forward with the recently developed National Food and Nutrition Policy (28). However, malnutrition is one of the major public health concerns worldwide with a significant increase in Sub-Saharan countries including Ethiopia (29–38). The current study was conducted in the year 2021, and holds significance as it aims to assess the double burden of malnutrition and its associated factors among mother–child pairs in Bahir Dar City, located in Northwest Ethiopia. The study provides valuable evidence and insights into new findings, which can be utilized by relevant stakeholders and organizations to develop targeted prevention strategies for addressing the double burden of malnutrition at the household level.
Methods and materials
Study setting
The study was conducted in Bahir Dar City. It is the capital city of the Amhara region and 565 KM away from Addis Ababa, the capital city of Ethiopia. Based on the Bahir Dar City health administration report the total population of Bahir Dar City was estimated to be 389,137, from this 198,459.87 are females and 91,758.5 are women under the reproductive age group. The number of under-five children was estimated to be 52,689.14 and of these 50,120.8 were 6–59 months old (39).
Study design, study period, population, and eligibility criteria
From February 28 to March 23, 2021, a community-based cross-sectional study was conducted to assess both the outcome status and exposure status simultaneously. The source population consisted of all mothers with children aged between 6 and 59 months. The study population was defined as mothers with children aged between 6 and 59 months residing in randomly selected sub-cities and Kebeles of Bahir Dar City. The inclusion criteria for the study were mothers with children aged between 6 and 59 months who had been living in Bahir Dar City for more than 6 months. However, pregnant mothers were excluded from the study.
Sample size determination and sampling techniques
The sample size was determined using the following single population proportion formula, , where margin error = 4%, The proportion (P) of the coexistence of overweight/obese mothers with stunted children = 23% (7), 1−p = 1–0.23 = 0.77, .
Since our sampling technique is multistage sampling, a design effect of 1.5 was considered: The sample size becomes: 425*1.5 = 638.
Finally, after we adjust for a non-response rate of 10% the final sample size becomes 637 + 637(0.1) =638 + 63.8 = 701.8 ~ 702.
This study employed a two-stage random sampling technique. Initially, three sub-cities were randomly selected from the six sub-cities in Bahir Dar City. Subsequently, six Kebeles (two from each selected sub-city) were chosen at random using the lottery method. The households within each selected Kebele were sampled using a systematic random sampling approach. After randomly selecting the first household from two households, a sampling interval of two was applied to select subsequent households. If mothers had multiple children, one child was randomly chosen for the assessment of the DBM.
Data collection tools and procedures
Prior to the actual data collection, a pre-test was conducted among 5% (n = 35) of the sample size from Kebeles that were not selected. The data were gathered using interviewer-administered questionnaires, which were adapted from various literature sources. These questionnaires were derived from reports such as EDHS (40), FANTA, and FAO (41), and previous research studies that had conducted similar investigations (15, 29, 42–47), with slight modifications made as necessary. The data collection process was carried out by eight experienced BSc nurses, who were supervised by two Public Health professionals.
Anthropometric measurements were employed to collect data from both mothers and children. For children under 2 years of age, their length was measured while in a recumbent position. The mothers’ body mass index (BMI) was calculated based on their height and weight. Sliding boards were used for length measurement, while digital weight scales were utilized for weight measurement. For children aged 2–5 years and mothers, their height was measured in a standing position with the Frankfurt plane, ensuring that the knees, heels, buttocks, and shoulder blades touched the vertical surface of the stadiometer. The weight of children under 2 years old was measured using a weighing sling (spring balance) after removing their shoes and heavy clothing. A digital weight scale was employed for children aged 2–5 years and mothers to measure their weight.
Asking the mother if the child had eaten anything from any of the normal seven food groups the day before, without imposing any minimum consumption requirements, was how dietary variety was determined. The seven food classes were cereals, roots, and tubers; legumes and nuts; dairy products except breast milk; flesh foods (meat, fish, fowl, or organ meats); eggs; vitamin A-rich fruits and vegetables; and other fruits and vegetables. A scale of 0–7 was used to calculate the dietary diversity score (DDS). Children were deemed to be adequate if they were fed at least four of the seven food groups throughout the reference period (48).
Minimum Dietary Diversity for a Woman (MDD-W), a dichotomous indicator/tool created by the FAO, was used in this study to quantify the dietary diversity of mothers. Ten food groups in total were taken into consideration: all starchy staples; pulses (beans, peas, and lentils); nuts and seeds; dairy products; flesh foods (including organ meat); eggs; vitamin A-rich dark green and leafy vegetables; other vitamin A-rich vegetables and fruits; and other vegetables and fruits. Every woman was classified as having adequate (>5 food groups) or not adequate (≤5 food groups) based on the Minimum Dietary Diversity Score (MDDS) that was computed for her during the previous 24 h (41).
Data quality control
The data collection instrument was initially developed in English and subsequently translated into Amharic. To ensure accuracy, the translated version was then translated back into English. The data collectors and supervisors underwent a two-day training program prior to the commencement of data collection. Any necessary adjustments were made based on the training feedback. The face validity of the tool was assessed by five nutrition experts to ensure its appropriateness and relevance. To minimize missing data, supervisors reviewed each questionnaire on a daily basis, verifying and cross-checking all recorded information against the data collectors’ entries.
Data processing and analysis
The collected data underwent a series of steps to ensure quality and prepare it for analysis. These steps included checking for completeness, compiling the data, coding it, and subsequently entering it into EpiData 3.1. The data was then exported to SPSS version 25.0 software for further analysis. For assessing the nutritional status of children, height-for-age, weight-for-age, and weight-for-height Z-scores were calculated using WHO Anthro version 3.2.2 software.
On the other hand, the mother’s nutritional status was evaluated by calculating the body mass index (BMI) (49). In the logistic regression model, the outcome variable was the double burden of malnutrition (DBM), a dichotomous variable labeled “1” for having DBM and “0” for not having DBM or normal status. Thus, those who had a DBM either due to the mother being overweight/obese (>BMI 25–29.9 kg/m2 overweight and ≥ 30 BMI obese) and the child being undernourished with stunting/wasting/underweight (<-2SD Z-scores) or due to the child being obese/overweight (> + 2SD Z-scores) in comparison with the underweight mothers (<BMI 18.5 kg/m2).
In the analysis, variables that demonstrated a value of p of ≤0.25 in the bivariable logistic regression were selected for inclusion in a multivariable binary logistic regression model. This step was undertaken to account for the potential impact of confounding variables. These variables were included in the multivariable model, enabling us to assess the individual effects of each variable while controlling for the effects of other variables. Variables with a value of p of <0.05 after the multivariable analysis were considered to have a significant association with the outcome variable. The degree of association between variables was measured using adjusted odds ratios, accompanied by their corresponding 95% confidence intervals. The fitness of the model was assessed using the Hosmer-Lemeshow goodness-of-fit test, which yielded a value of p of 0.59, indicating that the model fits the data well as the value of p is greater than 0.05. Additionally, a likelihood ratio test was conducted to compare the null model with the full model. The full model was selected due to its higher likelihood ratio.
To ensure the independence of observations, the intraclass correlation coefficient was calculated. The coefficient was found to be below 10%, indicating that the observations were independent. To evaluate the assumption of multicollinearity, the standard errors of the variables were examined. No issues of multicollinearity were detected as the standard errors were below two for all variables.
Operational definitions
DBM
In this study, participants were categorized as experiencing a double burden of malnutrition if either the mother was overweight/obese and the child was undernourished (with stunting, wasting, or underweight), or if the mother was underweight and the child was overweight (1).
Under nutrition
Mothers body mass index (BMI) ≤ 18.5 kg/m2 (49).
Overweight
Mothers BMI from 25–29.9 kg/m2 (49).
Obesity
Mothers BMI ≥30 kg/m2 (49).
Stunting
Height for age value less than minus two (−2 SD) standard deviations of WHO child growth standard (50).
Wasting
Weight-for-height value less than minus two (−2 SD) standard deviations of WHO child growth standard (50).
Underweight
Weight-for-age value less than minus two (−2 SD) standard deviations of WHO child growth standard (50).
Overweight
Weight-for-height more than plus two (+2 SD) standard deviation of the WHO child growth standards (50).
Food insecurity
Food secure score (0–1), mildly food insecure (2–8), moderately food insecure (9–15), and severely food insecure (16–27) (51).
Maternal dietary diversity
Mothers who consumed ≤5 out of 10 food groups were considered to have low/inadequate dietary diversity, while the mothers who consumed ≥6 out of 10 food groups were considered to have a high dietary diversity score (52).
Child dietary diversity
A child who consumes less than four out of seven food groups was categorized as having low (inadequate) dietary diversity, while those who consume four or more were considered to have high (adequate) dietary diversity (53).
Sedentary behavior
Mother site more than >9 h/day (54).
Results
Socio-demographic and socioeconomic characteristics of the respondents
From a total of 702 mother–child pairs, 661 have participated in the study with a 94.2% response rate. The number of female children was 386 (58.4%). The number of children whose age was >2 years was 385(58.2%). About 373 (56.4%) of the mothers were in the age group of 25–34 years while 196 (29.7%) were age ≥ 35 years. Around 254 (38.4%) of the mothers were housewives, 146 (22.1%) were private employees, and 60 (9.1%) were daily laborers. More than half of the households had ≤5 family members. Concerning the wealth index 264(39.9%) of participants were the poorest, while 101(15.3%) were the richest (Table 1).
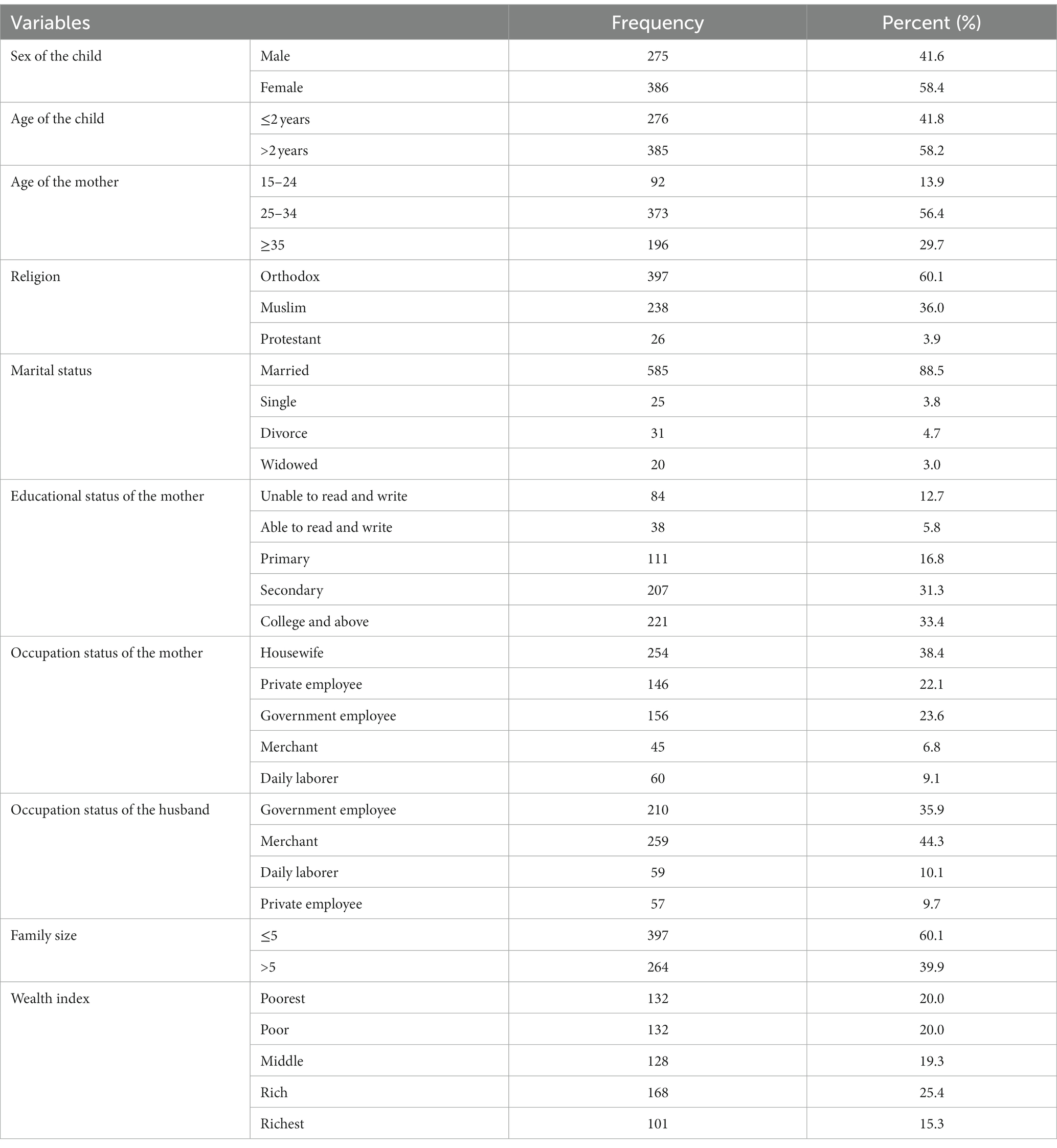
Table 1. Socio-demographic and socio-economic characteristics of mother–child pairs in Bahir Dar City, Northwest Ethiopia (N = 661).
Maternal and child characteristics
Nearly 205 (31.0%) of the children had low dietary diversity. Dietary diversity of the mothers was inadequate for 292 (44.2%). Most of the participants 578 (87.4%) sit for ≤540 min per day (Table 2).
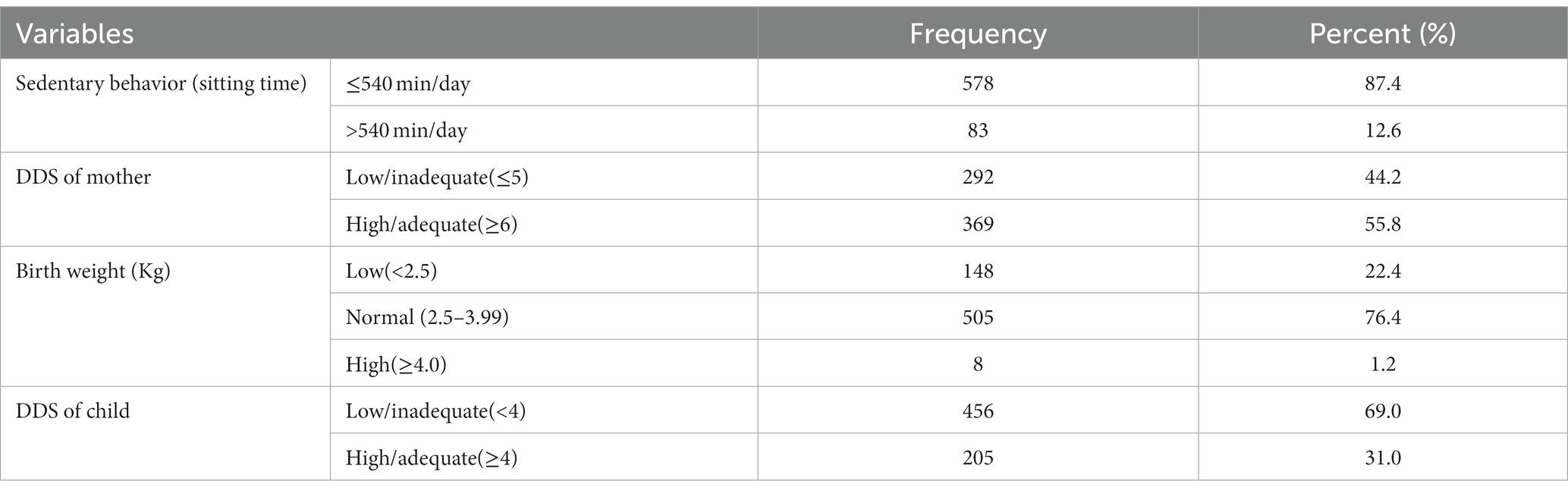
Table 2. Maternal and child characteristics of the double burden of malnutrition among mother–child pairs in Bahir Dar City, Northwest Ethiopia (N = 661).
Food security status
A total of 379 (57.25%) participants of the households had food security, while, 30(4.5%) were sever food insecure (Figure 1).
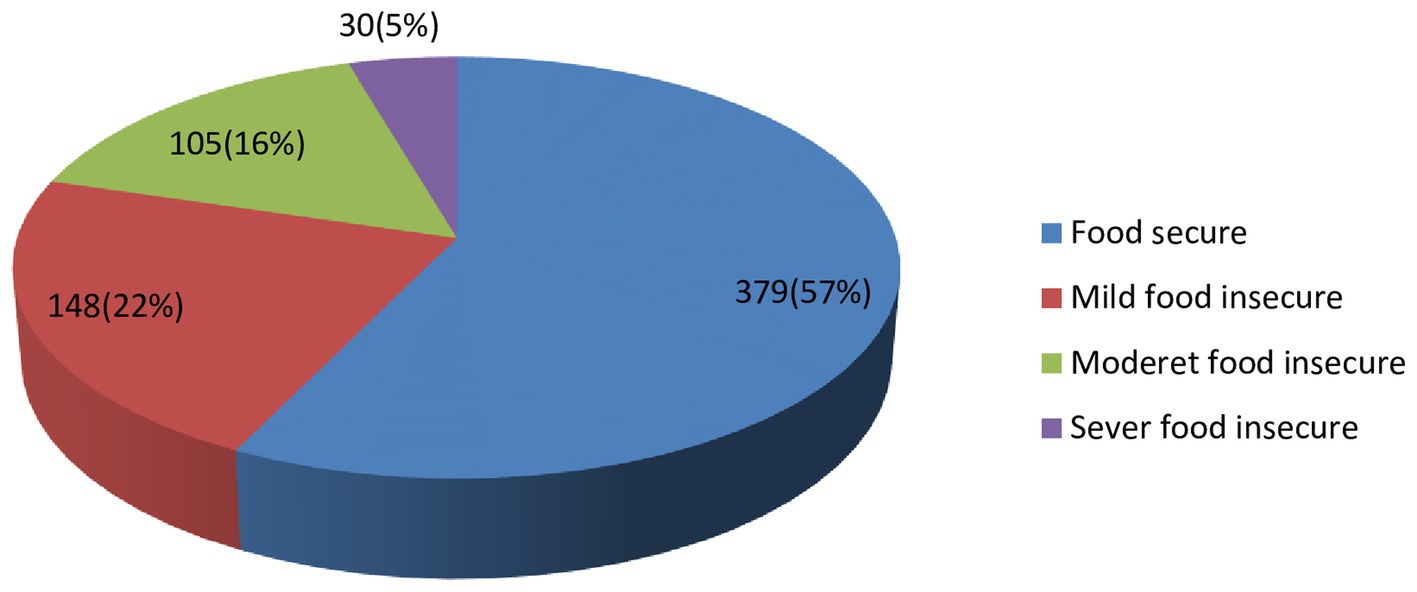
Figure 1. Household food security characteristics of the DBM among mother-child (instead mother to child) pairs in Bahir Dar City, Northwest Ethiopi (N = 661).
Prevalence of double burden of malnutrition
The overall double burden of malnutrition was 14.5 95% CI (12.8 15.7%). Among this, 11.3% (95% CI: 10.51, 12.09%) of mothers were overweight/obese and the child was undernourished (with stunting, wasting, or underweight), and 3.2% were underweight mothers and obese/overweight child (Table 3).
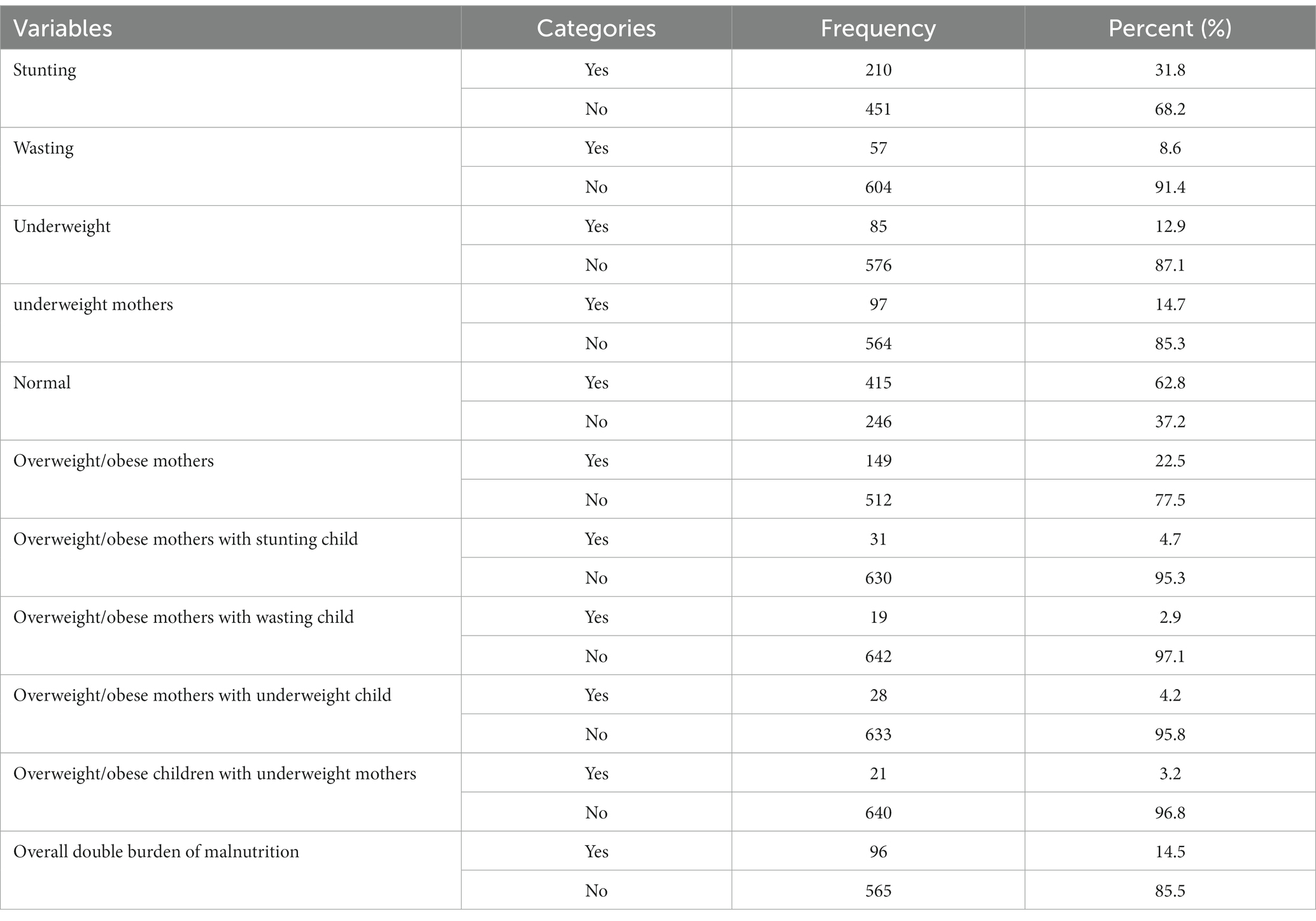
Table 3. Nutritional statuses of mothers and children and the prevalence of the double burden of malnutrition among mother–child pair in Bahir Dar City, Northwest Ethiopia (N = 661).
Factors associated with the double burden of malnutrition among mother–child pair
In the bivariable binary logistic regression analysis, several variables showed a significant association (with a value of p ≤0.25) with the double burden of malnutrition. These variables included household food security, wealth index, child’s dietary diversity score (DDS), mother’s age, and mother’s educational status. However, In the multivariable binary logistic regression analysis, subsequent to adjusting for confounding factors, notable associations were observed between the double burden of malnutrition and household food security, wealth index, children’s dietary diversity status, and mother’s educational status. These variables retained their significance even after controlling for potential confounders. The confounding factors taken into account for the multivariable analysis included variables such as household food security, wealth index, mother’s dietary diversity score (DDS), child’s dietary diversity score (DDS), mother’s age, and mother’s educational status. The analysis involved controlling for the effects of these variables on one another to accurately interpret their individual effects. Participants from food-secured households had 1.96 times higher odds of experiencing the double burden of malnutrition compared to households that were food insecure (AOR = 1.96, 95% CI 1.13, 3.39). Similarly, participants from the richest households had 2.72 times higher odds of experiencing the double burden of malnutrition compared to those from the poorest wealth index (AOR = 2.72, 95% CI 2.01, 5.63). The odds of experiencing the double burden of malnutrition among children with high dietary diversity decreased by 63% compared to those with low dietary diversity (AOR = 0.37, 95% CI 0.22, 0.61). Furthermore, the odds of the double burden of malnutrition among mothers who completed college and above decreased by 74% compared to those who were unable to read and write (AOR = 0.26, 95% CI 0.121, 0.549) (Table 4).
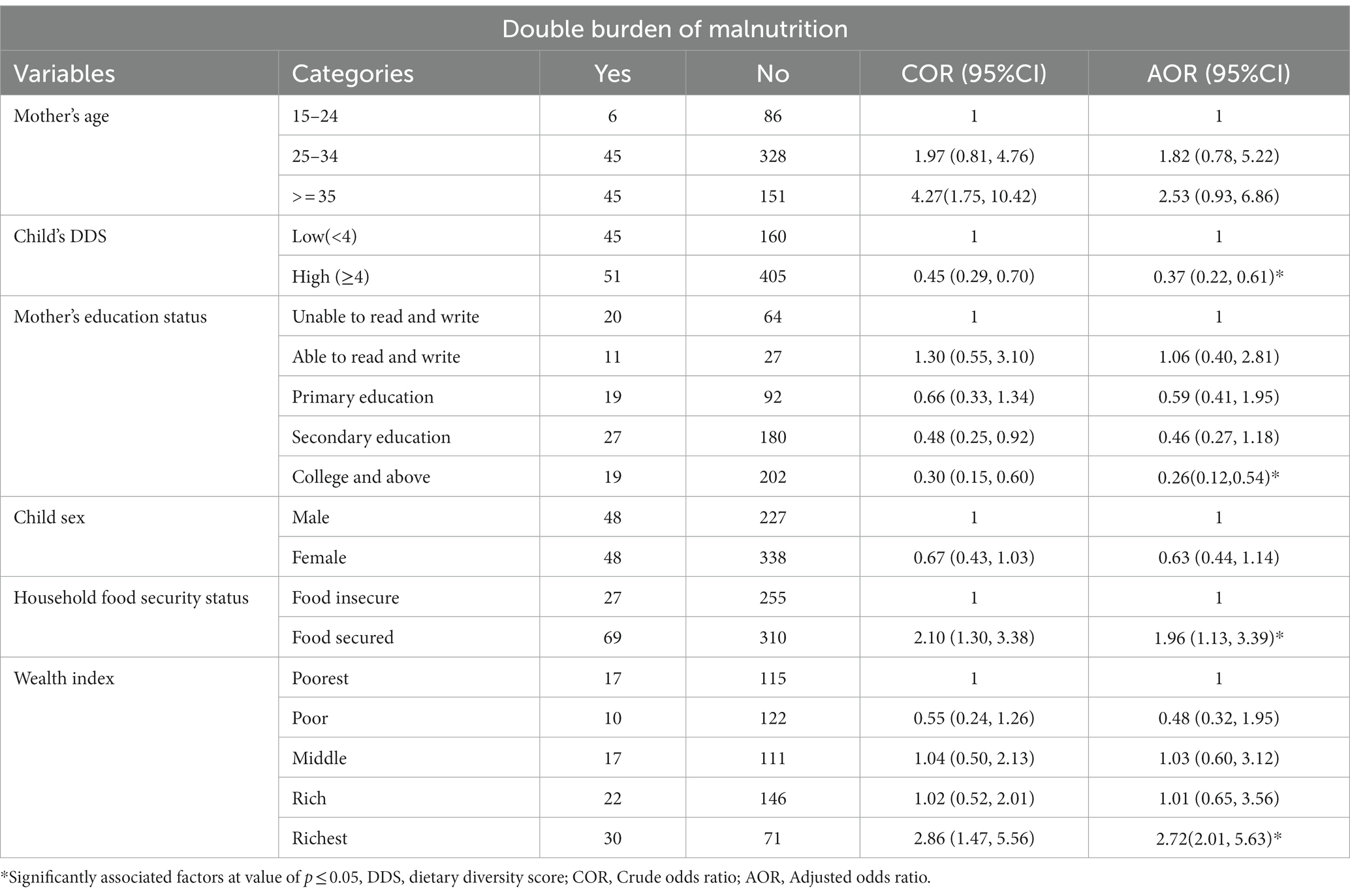
Table 4. Factors associated with the DBM (overweight/obese mothers with underweight/stunted/wasted children) or (underweight mothers with overweight children) in Bahir Dar City, Northwest Ethiopia (N = 661).
Discussion
In this study, the overall prevalence of DBM among mother–child pairs in Bahir Dar City was 14.5% (95% CI (12.8 15.7%), which is close to the study conducted in Palestine (15.7%) (9). However, the results of this study were lower than studies conducted in Ethiopia (23%) (7), West Java, Indonesia (21.2–30.6%) (8) (55), Manipal Karnataka (23%) (56), South Karnataka, India (27.4%) (57), and rural district peninsular Malaysia (29.6%) (58). This variation could potentially be attributed to factors such as socioeconomic status, the geographical location of the study (urban or rural), and the utilization of different cutoff points and criteria for defining malnutrition. These factors may contribute to the observed discrepancies in the findings.
Conversely, the prevalence in the current study was higher than other studies study done in Addis Ababa and the rural district of Kersa (9%) (12), Tanzania(11·3%) (59), rural areas of Western Kenya (3%) (60), Bangladesh (5.5, 6.3%) (61, 62), Nepal (6.6%) (63), Brazil (2.6%) (44), India (7 to 12.3%) (64, 65), Peru (7%) (66), South and Southeast Asia (12%) (67). These differences could be attributed to the economic development of the population and the process of urbanization, which are associated with dietary changes and the prevalence of obesity. Additionally, it is worth noting that this study examines various forms of malnutrition, while the study in Kenya focuses specifically on the double burden of malnutrition in the context of stunted children with overweight mothers. This difference in study design and focus may contribute to variations in the results obtained.
The present study outlined that maternal educational status was negatively associated with the double burden of malnutrition. Mothers with higher educational status (college and above) were 74% less likely to be associated with DBM as compared to illiterate mothers (unable to read and write). This finding is in line with studies conducted in Ethiopia (7), South and Southeast Asia (67), Pakistan (43), and Peninsular Malaysia (68). One possible explanation for this discrepancy is that educated mothers have the ability to read, learn, and comprehend health and nutrition-related information, which can lead to positive changes in feeding behaviors (27). Educated mothers tend to possess greater knowledge and awareness about diets and lifestyle factors, enabling them to make more informed decisions regarding their own and their children’s nutrition.
The wealth index is also another factor associated with DBM. Participants who were in the richest wealth category had higher odds of DBM compared with the poorest categories. The finding was supported by studies conducted in Addis Ababa and the rural district of Kersa (12), Kenya (47), Indonesia (55), Bangladesh (62), Peninsular Malaysia (68), Tanzania (59, 69), South and Southeast Asian (67), Pakistan (43), and India (64). This could be attributed to the fact that households in the highest wealth index category may undergo a dietary transition, leading to increased consumption of energy-dense foods, a lack of physical exercise, and a higher intake of soft drinks and fatty foods, but poor in nutrients (64). These factors contribute to a higher risk of overweight and obesity among individuals in these households.
Children who had high DDS had lower odds of DBM. This finding was supported by studies done in Tanzania (69), Indonesia (55), and Malaysia (70). DDS refers to the number of food groups consumed in a given time, often in 24 h, and that emerged as a measure of the nutritional adequacy of a given individual (71). This could be because a lower dietary diversity score (DDS) relates to inadequacy of nutrient quality and quantity as well, which significantly exacerbates micronutrient deficiencies, which in turn contribute to chronic malnutrition and stunting. Insufficient consumption of essential nutrients hampers proper growth and development, resulting in long-term effects on the physical and cognitive well-being of individuals.
Notably, this study showed that household food security is often associated with increased odds of double burden of malnutrition (DBM), which is reported to be the opposite of most of the studies conducted worldwide (44, 55, 72). The consumption of high amounts of saturated fat, sugar, and refined foods, coupled with a limited intake of fiber-rich foods and a lack of physical activity, can increase the risk of overweight or obesity in mothers. Conversely, under nutrition in children can arise not only from inadequate food intake but also from poor hygiene and sanitation practices. These factors can make children more susceptible to recurrent infections, which can affect the absorption and utilization of nutrients in their bodies (73).
Conclusion
In this study, the odds of experiencing the double burden of malnutrition among mother–child pairs were found to be lower compared to the findings reported in the EDHS 2016 (Ethiopian Demographic and Health Survey) report. In this study, educational status, wealth index, child dietary diversity score, and household food security status were identified as significant factors associated with the double burden of malnutrition. The study also highlights the importance of educating parents and caregivers about the benefits of food diversity for their children. In the future, researchers plan to conduct a prospective follow-up study on the double burden of malnutrition, considering additional variables such as micronutrient deficiencies and common non-communicable diseases. This will provide a more comprehensive understanding of the factors contributing to the double burden of malnutrition and its long-term implications.
Limitations and strengths of the study
The study examined both dimensions of the double burden of malnutrition, which involve scenarios of undernourished mothers with over nourished children and over nourished mothers with undernourished children. However, there are certain limitations to consider. Firstly, the nutritional status of the mothers was assessed solely based on BMI (Body Mass Index), which may not provide a comprehensive representation of their overall nutritional status. Secondly, since the study was cross-sectional in nature, it did not establish a causal relationship between the variables examined. These limitations should be taken into account when interpreting the findings of the study.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Bahir Dar University, College of Medicine and Health Science. The studies were conducted in accordance with the local legislation and institutional requirements. Oral informed consent was obtained from each rspondents/participating mother.
Author contributions
SM: Writing – original draft, Writing – review & editing. DB: Writing – original draft, Writing – review & editing. YM: Writing – original draft, Writing – review & editing. ZG: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Abbreviations
BMI, Body Mass Index; DBM, Double Burden of Malnutrition; DDS, Dietary Diversity Score; HFS, Household Food Security; NCDs, Non-Communicable Disease.
References
1. Shimpton, R, and Rokx, C. The double burden of malnutrition – a review of global evidence. HNP Discussion Paper. Washington, DC: The International Bank for Reconstruction and Development/The World Bank (2012).
2. Menon, S, and Peñalvo, JL. Actions targeting the double burden of malnutrition: A scoping review. Nutrients. (2020) 12:1–14. doi: 10.3390/nu12010081
3. Seferidi, P, Hone, T, Duran, AC, Bernabe-Ortiz, A, and Millett, C. Global inequalities in the double burden of malnutrition and associations with globalisation: a multilevel analysis of demographic and health surveys from 55 low-income and middle-income countries, 1992–2018. Lancet Glob Health. (2022) 10:e482–90. doi: 10.1016/S2214-109X(21)00594-5
4. Musavi, M, Sadehhal, S, and Nezhad, MA. The direct and indirect effects of macronutrients on energy intake in lactating mothers. Int J Pediatr. (2023) 11:6. doi: 10.22038/IJP.2021.60965.4707
5. Bose, A, Mondal, N, and Sen, J. Household levels of double burden of malnutrition in low–middle-income countries: a review. J. Anthropol Surv India. (2022) 71:125–60. doi: 10.1177/2277436x211043628
6. Santos, R, Jerome, CS, Azandjeme, C, Mizehoun-adissoda, C, and Metonnou, C. Prevalence and predictors of double burden of malnutrition within households in Africa: a systematic review. Food Nutr Sci. (2023) 14:908–27. doi: 10.4236/fns.2023.1410058
7. Eshete, T, Kumera, G, Bazezew, Y, Marie, T, Alemu, S, and Shiferaw, K. The coexistence of maternal overweight or obesity and child stunting in low-income country: further data analysis of the 2016 Ethiopia demographic health survey (EDHS). Sci Afr. (2020) 9:e00524. doi: 10.1016/j.sciaf.2020.e00524
8. Sekiyama, M, Jiang, HW, Gunawan, B, Dewanti, L, Honda, R, Shimizu-Furusawa, H, et al. Double burden of malnutrition in rural west java: household-level analysis for father-child and mother-child pairs and the association with dietary intake. Nutrients. (2015) 7:8376–91. doi: 10.3390/nu7105399
9. El Kishawi, RR, Soo, KL, Abed, YA, and Muda, WAMW. Prevalence and associated factors for dual form of malnutrition in mother-child pairs at the same household in the Gaza strip-Palestine. PLoS One. (2016) 11:1–14. doi: 10.1371/journal.pone.0151494
10. Patel, R, Srivastava, S, Kumar, P, and Chauhan, S. Factors associated with double burden of malnutrition among mother-child pairs in India: A study based on National Family Health Survey 2015–16. Child Youth Serv Rev. (2020) 116:105256. doi: 10.1016/j.childyouth.2020.105256
11. Sassi, S, Abassi, MM, Traissac, P, Ben Gharbia, H, Gartner, A, Delpeuch, F, et al. Intra-household double burden of malnutrition in a north African nutrition transition context: magnitude and associated factors of child anaemia with mother excess adiposity. Public Health Nutr. (2019) 22:44–54. doi: 10.1017/S1368980018002495
12. Bliznashka, L, Blakstad, MM, Berhane, Y, Tadesse, AW, Assefa, N, Danaei, G, et al. Household-level double burden of malnutrition in Ethiopia: a comparison of Addis Ababa and the rural district of Kersa. Public Health Nutr. (2021) 24:6354–68. doi: 10.1017/S1368980021003700
13. International Food Policy Research Institute. (2016). Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030. Washington, D.C.
14. Black, RE, Allen, LH, Bhutta, ZA, Caulfield, LE, de Onis, M, Ezzati, M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
15. Yue, T, Zhang, Q, Li, G, and Qin, H. Global burden of nutritional deficiencies among children under 5 years of age from 2010 to 2019. Nutrients. (2022) 14:1–17. doi: 10.3390/nu14132685
16. Chu, DT, Minh Nguyet, NT, Dinh, TC, Thai Lien, NV, Nguyen, KH, Nhu Ngoc, VT, et al. An update on physical health and economic consequences of overweight and obesity. Diabetes Metab Syndr. (2018) 12:1095–100. doi: 10.1016/j.dsx.2018.05.004
17. Aballay, LR, Eynard, AR, Díaz Mdel, P, Navarro, A, and Muñoz, SE. Overweight and obesity: A review of their relationship to metabolic syndrome, cardiovascular disease, and cancer in South America. Nutr Rev. (2013) 71:168–79. doi: 10.1111/j.1753-4887.2012.00533.x
18. Indarti, J, Susilo, SA, Hyawicaksono, P, Berguna, JSN, Tyagitha, GA, and Ikhsan, M. Maternal and perinatal outcome of maternal obesity at RSCM in 2014–2019. Obstet Gynecol Int. (2021) 2021:1–6. doi: 10.1155/2021/6039565
19. Poston, L, Caleyachetty, R, Cnattingius, S, Corvalán, C, Uauy, R, Herring, S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. (2016) 4:1025–36. doi: 10.1016/S2213-8587(16)30217-0
20. Ellulu, M, Abed, Y, Rahmat, A, Ranneh, Y, and Ali, F. Epidemiology of obesity in developing countries: challenges and prevention. Glob. Epidemic Obes. (2014) 2:2. doi: 10.7243/2052-5966-2-2
21. Verma, J, and Pant, H. Innovations in agriculture, environment and Health Research for Ecological Restoration (2020). Available at: https://www.researchgate.net/publication/342589030
22. Amuna, P, and Zotor, FB. Epidemiological and nutrition transition in developing countries: impact on human health and development. Proc Nutr Soc. (2008) 67:82–90. doi: 10.1017/S0029665108006058
23. Mbogori, T, Kimmel, K, Zhang, M, Kandiah, J, and Wang, Y. Nutrition transition and double burden of malnutrition in Africa: A case study of four selected countries with different social economic development. AIMS Public Health. (2020) 7:425–39. doi: 10.3934/publichealth.2020035
24. Schmidhuber, J, and Shetty, P. The nutrition transition to 2030. Why developing countries are likely to bear the major burden. Food Econ Acta Agric Scand A. (2005) 2:150–66. doi: 10.1080/16507540500534812
25. Wells, JC, Sawaya, AL, Wibaek, R, Mwangome, M, Poullas, MS, Yajnik, CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. (2020) 395:75–88. doi: 10.1016/S0140-6736(19)32472-9
26. Ruel, M Sr, and Hawkes, C. Double duty actions to tackle all forms of malnutrition (P10-053-19). Curr Dev Nutr. (2019) 3:P10-053-19. doi: 10.1093/cdn/nzz034.p10-053-19
27. Fanzo, J, Hawkes, C, Udomkesmalee, E, Afshin, A, Allemandi, L, Assery, O, et al. 2018 global nutrition report. London, UK: Global Nutrition Report (2019).
28. Truebswasser, U, Genye, T, and Bossuyt, A. Review of the Nutrition Policy Landscape in Ethiopia 2010–2020. International food policy research institute (2020); 1–51. Available at: http://www.nipn.ephi.gov.et/sites/default/files/inline-files/Nutrition_Policy_Landscape_FINAL_Report.pdf
29. Ahmed, KY, Abrha, S, Page, A, Arora, A, Shiferaw, S, Tadese, F, et al. Trends and determinants of underweight and overweight/obesity among urban Ethiopian women from 2000 to 2016. BMC Public Health. (2020) 20:1276–13. doi: 10.1186/s12889-020-09345-6
30. Azanaw, MM, Zewde, EA, Gebremariam, AD, Dagnaw, FT, Asnakew, DT, Chanie, ES, et al. Spatiotemporal distribution and determinants of overweight or obesity among urban women in Ethiopia: a multivariate decomposition analysis. BMC Womens Health. (2022) 22:494–15. doi: 10.1186/s12905-022-02102-4
31. Yeshaw, Y, Kebede, SA, Liyew, AM, Tesema, GA, Agegnehu, CD, Teshale, AB, et al. Determinants of overweight/obesity among reproductive age group women in Ethiopia: multilevel analysis of Ethiopian demographic and health survey. BMJ Open. (2020) 10:1–7. doi: 10.1136/bmjopen-2019-034963
32. Abrha, S, Shiferaw, S, and Ahmed, KY. Overweight and obesity and its socio-demographic correlates among urban Ethiopian women: evidence from the 2011 EDHS. BMC Public Health. (2016) 16:1–7. doi: 10.1186/s12889-016-3315-3
33. Mengesha Kassie, A, Beletew Abate, B, Wudu Kassaw, M, and Gebremeskel, AT. Prevalence of underweight and its associated factors among reproductive age group women in Ethiopia: analysis of the 2016 Ethiopian demographic and health survey data. J Environ Public Health. (2020) 2020:1–10. doi: 10.1155/2020/9718714
34. Menalu, MM, Bayleyegn, AD, Tizazu, MA, and Amare, NS. Assessment of prevalence and factors associated with malnutrition among under-five children in Debre Berhan town. Ethiop Int J Gen Med. (2021) 14:1683–97. doi: 10.2147/IJGM.S307026
35. Abdulahi, A, Shab-Bidar, S, Rezaei, S, and Djafarian, K. Nutritional status of under five children in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. (2017) 27:175–88. doi: 10.4314/ejhs.v27i2.10
36. Tekile, AK, Woya, AA, and Basha, GW. Prevalence of malnutrition and associated factors among under-five children in Ethiopia: evidence from the 2016 Ethiopia demographic and health survey. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4444-4
37. Yisak, H, Gobena, T, and Mesfin, F. Prevalence and risk factors for under nutrition among children under five at Haramaya district Eastern Ethiopia. BMC Pediatr. (2015) 15:1–7. doi: 10.1186/s12887-015-0535-0
38. Kassie, GW, and Workie, DL. Determinants of under-nutrition among children under five years of age in Ethiopia. BMC Public Health. (2020) 20:399–11. doi: 10.1186/s12889-020-08539-2
39. Bahir Dar special zone health office, Total population estimation of Bahir Dar City; Bahir Dar special zone health office. 2020 annual report. Unpublished. (2020)
40. Central Statistical Agency(CSA). Ethiopian demographic and health survey(EDHS), Federal Democratic Republic of Ethiopia. Ethiopia,. ICF International Calverton, Maryland, USA: Addis Ababa (2016).
41. Food and Agriculture Organization (FAO)FHI 360, Minimum dietary diversity for women: a guide for measurement. Rome, Italy: Food and Agriculture Organization of the United Nations (2016). Available at: http://www.fao.org/3/a-i5486e.pdf (Accessed February 8, 2024).
42. Prasetyo, YB, Permatasari, P, and Susanti, HD. The effect of mothers’ nutritional education and knowledge on children’s nutritional status: a systematic review. International journal of child care and education. Policy. (2023) 17:1–16. doi: 10.1186/s40723-023-00114-7
43. Asibul Anik, AI, Mosfequr Rahman, M, Mostafizur Rahman, M, Ismail Tareque, M, Nuruzzaman Khan, M, Mahmudul Alam, M, et al. Double burden of malnutrition at household level: a comparative study among Bangladesh, Nepal, Pakistan, and Myanmar. PLoS One. (2019) 14:1–16. doi: 10.1371/journal.pone.0221274
44. Gubert, MB, Spaniol, AM, Segall-Corrêa, AM, and Pérez-Escamilla, R. Understanding the double burden of malnutrition in food insecure households in Brazil. Matern Child Nutr. (2017) 13:1–9. doi: 10.1111/mcn.12347
45. Government of the Federal Democratic Republic of Ethiopia. National Nutrition Programme Republic of Ethiopia. (2015).
46. Ahmed, T, Hossain, M, and Sanin, KI. Global burden of maternal and child undernutrition and micronutrient deficiencies. Ann Nutr Metab. (2012) 61:8–17. doi: 10.1159/000345165
47. Masibo, PK, Humwa, F, and MacHaria, TN. The double burden of overnutrition and undernutrition in mother-child dyads in Kenya: demographic and health survey data, 2014. J Nutr Sci. (2020) 9:9. doi: 10.1017/jns.2019.39
48. World Health Organization (WHO). United nations Chil- dren’s fund (UNICEF), indicators for assessing infant and young child feeding practices. Geneva, Switzerland: WHO (2008).
49. Bhattacharya, A, Pal, B, Mukherjee, S, and Roy, SK. Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC Public Health. (2019) 19:1045–11. doi: 10.1186/s12889-019-7372-2
50. Kothari, MT, Abderrahim, N, Coile, A, and Cheng, Y. Nutritional status of women and children: A (2014) Update on nutritional status by sociodemographic and water, sanitation, and hygiene (WASH) indicators collected in demographic and health surveys, vol. 6. Maryland, USA: ICF International (2014).
51. Swindale, A, and Bilinsky, P. Household food insecurity access scale (HFIAS) for measurement of household food access: indicator guide (v. 3). Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Educational Development (2007).
52. Ansari, G, Jain, S, and Bhatia, N. Association of Maternal Dietary Diversity and Nutritional Status with Child’s dietary diversity and nutritional status (2–5 years) in India. World Nutr. (2020) 11:110–28. doi: 10.26596/wn.2020111110-128
53. Keno, S, Bikila, H, Shibiru, T, and Etafa, W. Dietary diversity and associated factors among children aged 6 to 23 months in Chelia District. Ethiopia BMC Pediatr. (2021) 21:1–10. doi: 10.1186/s12887-021-03040-0
54. Topothai, T, Tangcharoensathien, V, Edney, SM, Suphanchaimat, R, Lekagul, A, Waleewong, O, et al. Patterns and correlates of physical activity and sedentary behavior among Bangkok residents: A cross-sectional study. PLoS One. (2023) 18:e0292222. doi: 10.1371/journal.pone.0292222
55. Mahmudiono, T, Nindya, TS, Andrias, DR, Megatsari, H, Rachmah, Q, and Rosenkranz, RR. Comparison of maternal nutrition literacy, dietary diversity, and food security among households with and without double burden of malnutrition in Surabaya Indonesia. Malays J Nutr. (2018) 24:359–70.
56. Garg, M, and Jindal, S. Dual burden of malnutrition in mother-child pairs of the same household: effect of nutrition transition. J Nutr Res. (2013) 1:1–7. doi: 10.55289/jnutres/v1i1.1
57. Garg, M, Kapur, D, and Kumar, P. Assessment of familial co-existence of dual forms of malnutrition in mother-child pairs and associated risk factors in South Karnataka. Health Popul Perspect Issues. (2018) 41:5–24.
58. Ihab, AN, Rohana, AJ, Wan Manan, WM, Wan Suriati, WN, Zalilah, MS, and Rusli, AM. The coexistence of dual form of malnutrition in a sample of rural Malaysia. Int J Prev Med. (2013) 4:690–9.
59. Faustini, FT, Mniachi, AR, and Msengwa, AS. Coexistence and correlates of forms of malnutrition among mothers and under-five child pairs in Tanzania. J Nutr Sci. (2022) 11:e103–8. doi: 10.1017/jns.2022.103
60. Fongar, A, Gödecke, T, and Qaim, M. Various forms of double burden of malnutrition problems exist in rural Kenya. BMC Public Health. (2019) 19:1543–9. doi: 10.1186/s12889-019-7882-y
61. Rahman, MA, Halder, HR, Siddiquee, T, Farjana, SA, Roshid, HO, Khan, B, et al. Prevalence and determinants of double burden of malnutrition in Bangladesh: evidence from a nationwide cross-sectional survey. Forum Nutr. (2021) 46:11. doi: 10.1186/s41110-021-00140-w
62. Das, S, Fahim, SM, Islam, MS, Biswas, T, Mahfuz, M, and Ahmed, T. Prevalence and sociodemographic determinants of household-level double burden of malnutrition in Bangladesh. Public Health Nutr. (2019) 22:1425–32. doi: 10.1017/S1368980018003580
63. Sunuwar, DR, Singh, DR, and Pradhan, PMS. Prevalence and factors associated with double and triple burden of malnutrition among mothers and children in Nepal: evidence from 2016 Nepal demographic and health survey. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-8356-y
64. Singh, S, Shri, N, and Singh, A. Inequalities in the prevalence of double burden of malnutrition among mother–child dyads in India. Sci Rep. (2023) 13:16923–13. doi: 10.1038/s41598-023-43993-z
65. Paul, P, and Chakrabarty, S. Double burden of malnutrition of mother-child pairs in the same households: a case study from the Bengali slum dwellers in West Bengal, India. J Anthropol. (2021) 17:197–205.
66. Pomati, M, Mendoza-Quispe, D, Anza-Ramirez, C, Hernández-Vásquez, A, Carrillo Larco, RM, Fernandez, G, et al. Trends and patterns of the double burden of malnutrition (DBM) in Peru: a pooled analysis of 129,159 mother–child dyads. Int J Obes. (2021) 45:609–18. doi: 10.1038/s41366-020-00725-x
67. Biswas, T, Townsend, N, Magalhaes, RJS, Hasan, M, and Mamun, A. Patterns and determinants of the double burden of malnutrition at the household level in south and Southeast Asia. Eur J Clin Nutr. (2021) 75:385–91. doi: 10.1038/s41430-020-00726-z
68. Wong, CY, Zalilah, MS, Chua, EY, Norhasmah, S, Chin, YS, and Siti Nur’Asyura, A. Double-burden of malnutrition among the indigenous peoples (orang Asli) of peninsular Malaysia global health. BMC Public Health. (2015) 15:1–9. doi: 10.1186/s12889-015-2058-x
69. Chen, S, Shimpuku, Y, Honda, T, and Mwakawanga BM, DL. Dietary diversity moderates household economic inequalities in the double burden of malnutrition in Tanzania (2023):1–37. doi: 10.1101/2023.10.10.23296857v1,
70. Saibul, N, Shariff, ZM, Lin, KG, Kandiah, M, Nawalyah, AG, and Hejar, AR. Food variety score is associated with dual burden of malnutrition in “orang Asli” (Malaysian indigenous peoples) households: implications for health promotion. Asia Pac J Clin Nutr. (2009) 18:412–22.
71. Ty, H, and Krawinkel, M. Dietary diversity score: a measure of nutritional adequacy or an Indicator of dietary diversity score: a measure of nutritional adequacy or an Indicator of healthy diet? J Nutr Health Sci. (2017) 3:3033. doi: 10.15744/2393-9060.3.303
72. Sansón-Rosas, AM, Bernal-Rivas, J, Kubow, S, Suarez-Molina, A, and Melgar-Quiñonez, H. Food insecurity and the double burden of malnutrition in Colombian rural households. Public Health Nutr. (2021) 24:4417–29. doi: 10.1017/S1368980021002895
Keywords: double burden, malnutrition, mother–child pairs, household, Bahir Dar, Ethiopia
Citation: Mekonnen S, Birhanu D, Menber Y, Gebreegziabher ZA and Belay MA (2024) Double burden of malnutrition and associated factors among mother–child pairs at household level in Bahir Dar City, Northwest Ethiopia: community based cross-sectional study design. Front. Nutr. 11:1340382. doi: 10.3389/fnut.2024.1340382
Edited by:
Roberta Zupo, University of Bari Aldo Moro, ItalyReviewed by:
Orazio Valerio Giannico, Local Health Authority of Taranto, ItalyMahbuba Kawser, University of Dhaka, Bangladesh
Copyright © 2024 Mekonnen, Birhanu, Menber, Gebreegziabher and Belay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mahider Awoke Belay, bWFoaWRlcnNlbGFtQGdtYWlsLmNvbQ==
 Solomon Mekonnen1
Solomon Mekonnen1 Dereje Birhanu
Dereje Birhanu Yonatan Menber
Yonatan Menber Zenebe Abebe Gebreegziabher
Zenebe Abebe Gebreegziabher Mahider Awoke Belay
Mahider Awoke Belay