- 1Asia-Pacific Association of Agricultural Research Institutions (APAARI), Bangkok, Thailand
- 2International Crops Research Institute for the Semi-Arid Tropics (ICRISAT), Patancheru, India
- 3Asian Institute of Technology (AIT), Khlong Luang, Thailand
- 4Institute of Food, Nutrition, and Health, University of Reading, Reading, United Kingdom
- 5International Rice Research Institute (IRRI), Los Baños, Philippines
- 6One Acre Fund, Kigali, Rwanda
- 7National Institute of Nutrition (NIN), Hyderabad, India
- 8Avinashilingam Institute for Home Science and Higher Education for Women, Coimbatore, Tamil Nadu, India
- 9National Technical Board of Nutrition, Government of India (GoI), Mumbai, India
Millets are recognized for their health and nutritional values, and the United Nations declared 2023 the International Year of Millets. Among the several health and nutritional benefits of millets, their impact on hemoglobin concentration is important since anemia is a major public health issue in many countries. To investigate the effect of millet (including sorghum) consumption on hemoglobin concentration in the blood, a systematic review and meta-analysis were conducted. Thirteen published studies featuring randomized control trials involving 590 individuals in the intervention group and 549 control individuals were eligible for the meta-analysis. The difference-in-differences analysis revealed highly significant (p < 0.01) positive effects of millet consumption on hemoglobin concentration, with an effect size of +0.68 standardized mean difference units. The change in hemoglobin concentration observed in the intervention group was +13.6%, which is statistically significant (p < 0.0005), compared to that in the control group, which was +4.8% and not statistically significant (p = 0.1362). In four studies, the consumption of millets in the intervention group demonstrated a change from mild anemia to normal status among children, whereas there was no change in the control group. The findings provide evidence that the consumption of millets can improve blood hemoglobin concentration, likely resulting from increased iron intake. Further research is needed involving the assessment of iron content and bioavailability to better understand the effect variation among millet types and the mechanisms involved.
1 Introduction
Iron deficiency anemia (IDA) is a global public health issue that affects children and young women in particular. According to the World Health Organization (WHO) estimates for 2019, global anemia prevalence in women of reproductive age and children was 29.9 and 39.8%, respectively, accounting for half a billion women and 269 million children (1). A deficit in dietary iron intake remains a significant challenge, exacerbated by the growing global consumption of refined and highly processed foods, leading to micronutrient deficiency in vulnerable populations. Staple cereals continue to dominate food consumption in developing countries; these mainly include refined wheat, rice, and maize, while other nutrient-rich crops such as millets and sorghum are underutilized (2–4) Supplementation with iron, widespread fortification of foods with iron, and dietary diversity are evidence-based approaches to combating anemia. Interventions aimed at enhancing dietary diversity also facilitate the intake of a wide range of micronutrients, rather than focusing on just one. Studies in different parts of the world have shown that enhancing dietary diversity has resulted in improved hemoglobin levels (5, 6). In this context, millets play an important role in promoting dietary diversity, which in turn ensures the consumption of a wide spectrum of essential vitamins, minerals, and other nutrients. Regions in which millets historically constituted a significant part of the diet have seen their prominence in the dietary landscape gradually diminish over time (7). Whole grain millets have advantages over refined cereals, as they have higher levels of nutrients such as iron, zinc, and protein, to name a few (2). The effect of consuming millets that are rich in iron on blood hemoglobin concentration and anemia has been studied by many researchers. However, this is the first time that evidence on the impact of consuming millet on hemoglobin levels compared to the consumption of other common staples has been collated.
A previous systematic review and meta-analysis showed that millets reduce fasting blood glucose levels (8) and hyperlipidemia (9) and improve growth in children (10). In terms of their effects on anemia, Anitha et al. (11) conducted a systematic review of the potential of millets in raising blood hemoglobin levels, showing that the levels increased from the baseline to the endline. However, the study did not account for changes in the control group. The current systematic review and meta-analysis extends the study conducted by Anitha et al. (11) by accounting for the control group.
The review question, therefore, is, “Does the consumption of millets have positive effects on blood hemoglobin concentration in the controlled assessment design as well, where the control group consumes common staples?
2 Materials and methods
2.1 Study period and protocol
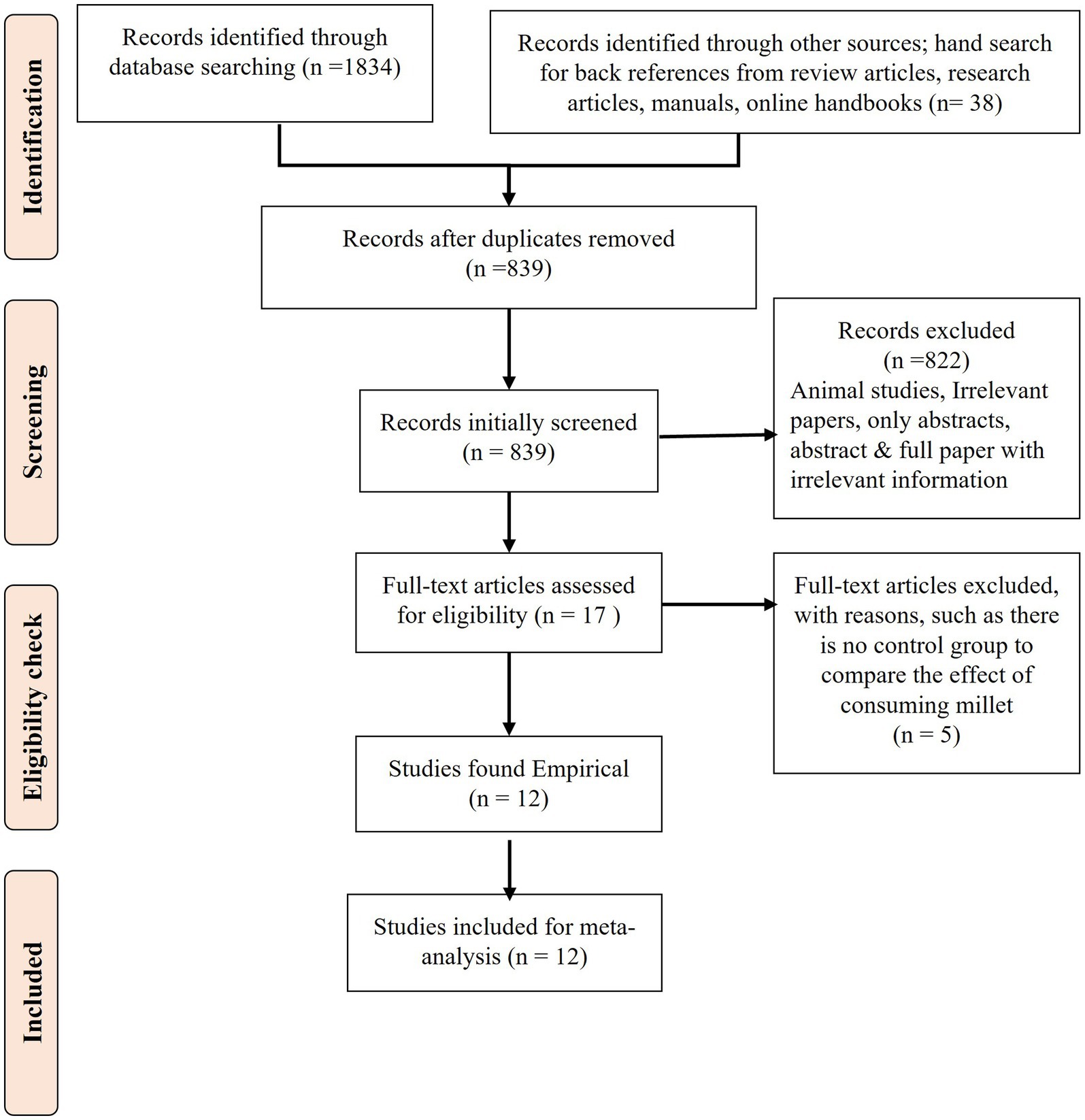
The systematic review and meta-analysis were conducted from October 2017 to September 2022. The PRISMA checklist (12, 13) was used to write the protocol, which was registered with the unique identification number “reviewregistry1114” in the online platform “research registry.” Figure 1 describes the process of the systematic review.
2.2 Search
Studies published in English until September 2022 were obtained through major search engines, namely, Google Scholar, Scopus, Web of Science, PubMed, and CAB abstracts.
2.3 Search strategy
The search was conducted using predetermined terminology such as “hemoglobin level AND millets,” “Anemia AND millets,” “millet consumption AND hemoglobin level,” and “millet consumption and anemia.” The search was repeated by replacing millet with the specific type of millet.
2.4 Inclusion criteria
The review included randomized controlled trials conducted on the effect of the consumption of millets on blood hemoglobin level, where the control group consumed a regular diet, and studies conducted on any age group (children, adolescents, and adults) or gender of any geographical region. Only human studies were considered as were peer-reviewed journal articles and completed MSc or PhD theses that were available online.
2.5 Exclusion criteria
Review articles, animal studies, publications with incomplete data on hemoglobin levels, and papers using only an intervention group were excluded.
2.6 Data items
From each eligible study, information on the authors, year of publication, age group and gender of the study participants, country details, sample size in both intervention and control groups, and study methodology were recorded in an Excel sheet (14, 15) along with the mean and standard deviation difference in hemoglobin levels in g/dl.
2.7 GRADE assessment
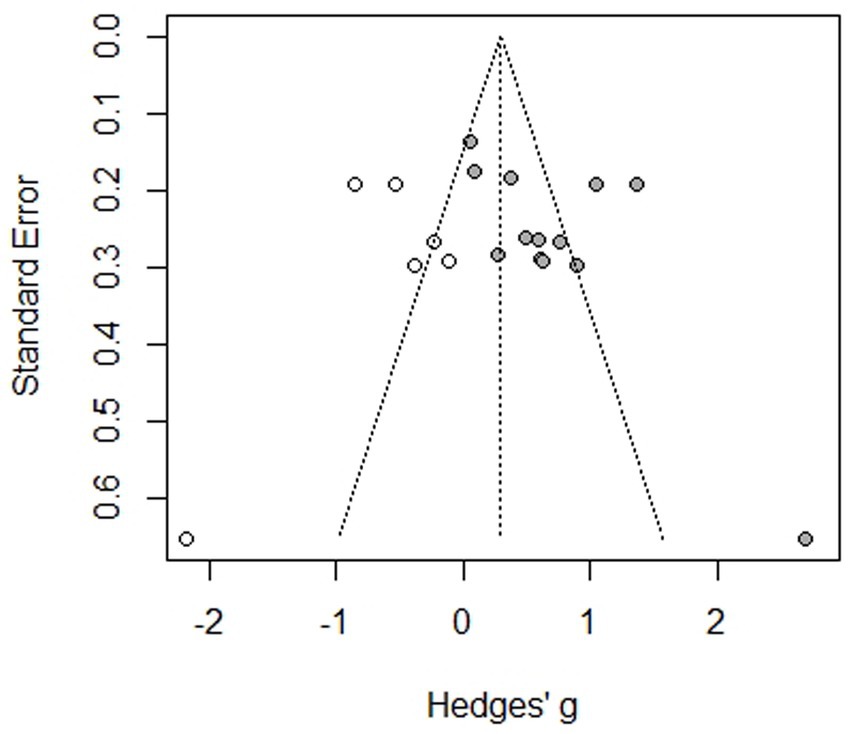
A GRADE assessment was conducted to evaluate the quality of the published articles included in the meta-analysis, based on criteria described by Cochrane (16). Two co-authors of this systematic review independently conducted the GRADE assessment and had no disagreement, obviating the need for another co-author’s input. Quality was assessed based on the ranking of eight criteria, namely, risk of bias, inconsistency, indirectness, imprecision, publication bias, large magnitude of effects, dose–response, and effects of all plausible confounding factors. Ratings were given to downgrade the first five criteria and/or upgrade the sixth to eighth criteria according to the assessment for each criterion. Publication bias was assessed using a funnel plot (17).
2.8 Data analysis
A total of 12 published articles with 13 studies were found eligible for inclusion in the meta-analysis. The mean change and standard deviation of hemoglobin levels were observed in the intervention and control groups consuming a normal diet (i.e., refined rice and/or wheat). The effects of the treatment were evaluated based on the difference-in-differences (DID) method to address the bias arising from changes in the control group and any initial difference between the two groups. The statistical significance of the DID was examined by the Wilcoxon matched-pairs signed rank (WSR) test. Furthermore, the treatment effect was formally estimated by the panel DID regression analysis. Standard errors (SEs) were clustered at the individual level to obtain the SE robust to heteroscedasticity. The Hausman specification test was used to choose between the fixed effect and random effect models for the panel regression. The meta-analysis was conducted using R Studio version 4.2.1 (18) to obtain forest plots to determine intervention effects and funnel plots to determine publication bias. The mean change in hemoglobin level (g/dl) before and after the intervention was shown for each group, along with the standard deviation and sample size, to determine the standardized mean difference (SMD) (19–21). The results of the fixed and random effect models were obtained to describe the effect size (22, 23). In addition, the participants were subgrouped into children, adolescents, and adults to determine the intervention effects by age.
Expected outcome: Impact of millet consumption on hemoglobin levels compared to other staple consumption in any geographical location.
3 Results
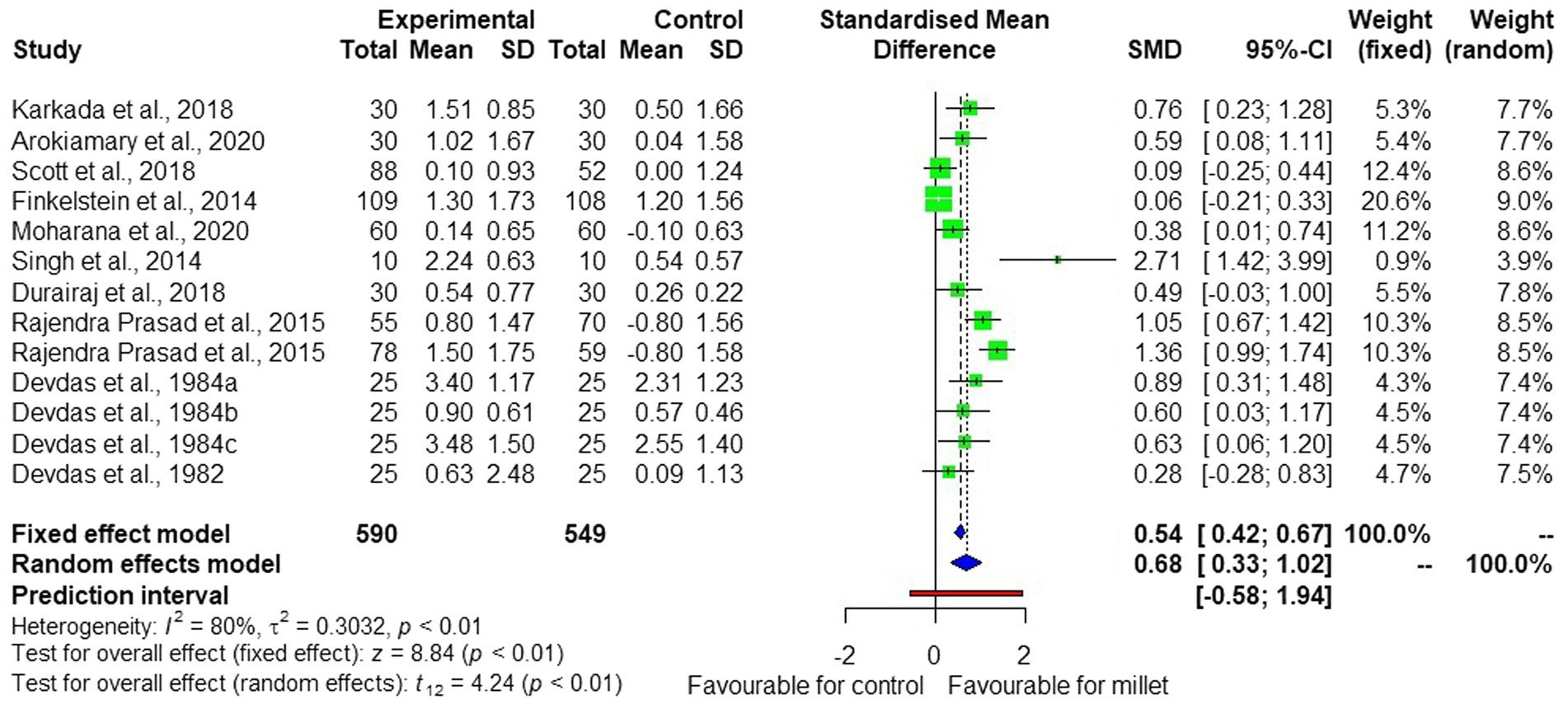
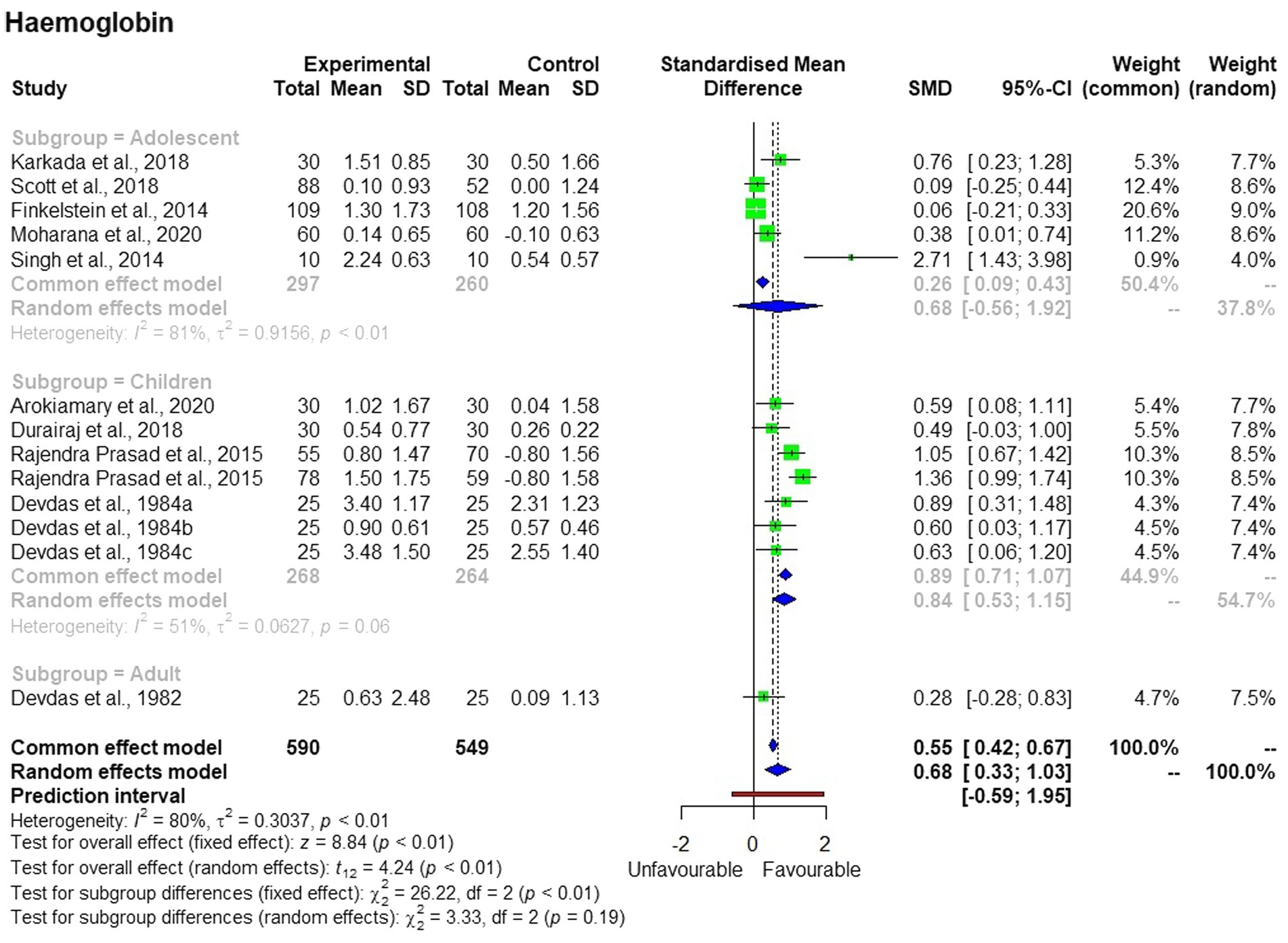
The meta-analysis of the 13 studies from 12 publications (23–35) (Figure 2) shows high heterogeneity (I2 = 80%). The random effect model used to interpret the results showed significant (p < 0.01) effects of millet consumption on blood hemoglobin concentration, with an average standard mean difference (SMD) of +0.68 and a confidence interval of [+0.33; +1.02].
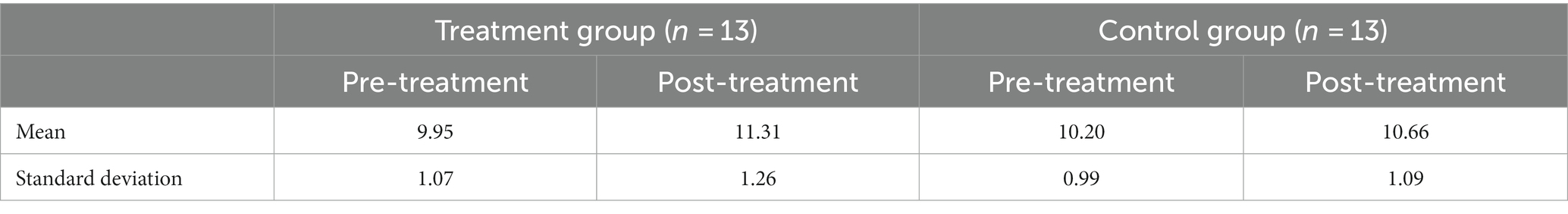
Descriptive statistics (Table 1) show that the mean hemoglobin concentration in the intervention group was 9.95 ± 1.07 g/dL before consuming non-refined millet-based food, which increased to 11.31 ± 1.09 g/dL after the intervention. In the control group, it was 10.20 ± 0.99 before the intervention and 10.66 ± 1.09 after the intervention.
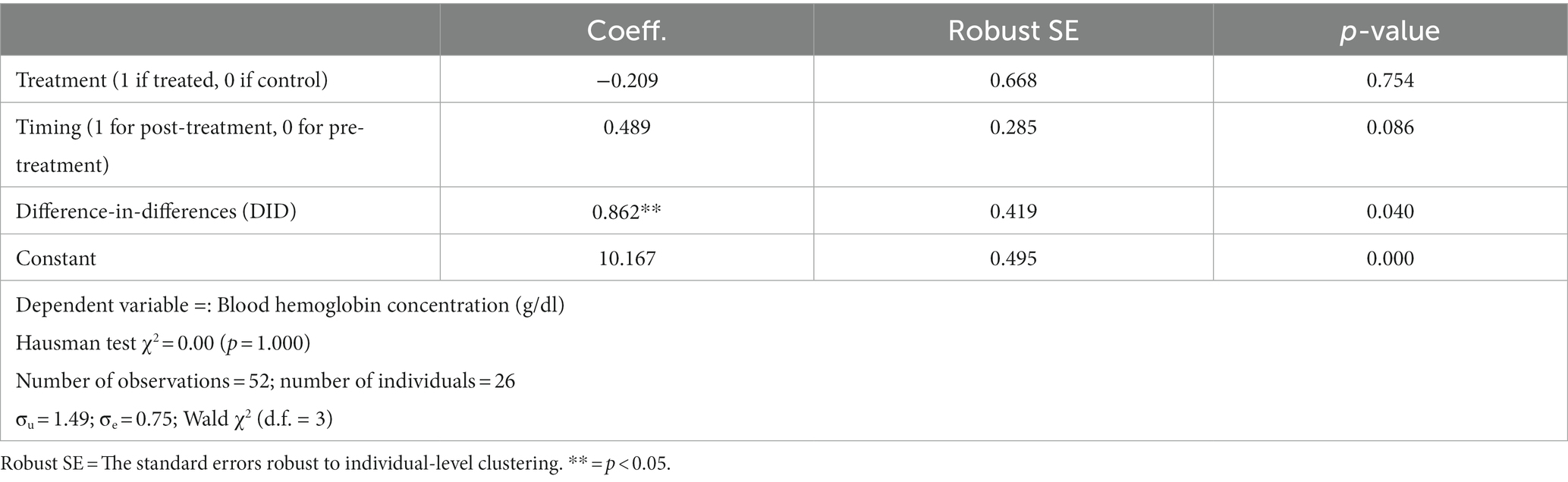
The WSR test shows that the percentage change in the hemoglobin concentration in the treatment group was +13.6% (p = 0.000), whereas the change in the control group was not statistically significant (p = 0.136) (Table 2). The DID result suggests that the average treatment effect of millet-based diets on blood hemoglobin concentration was +8.8%.
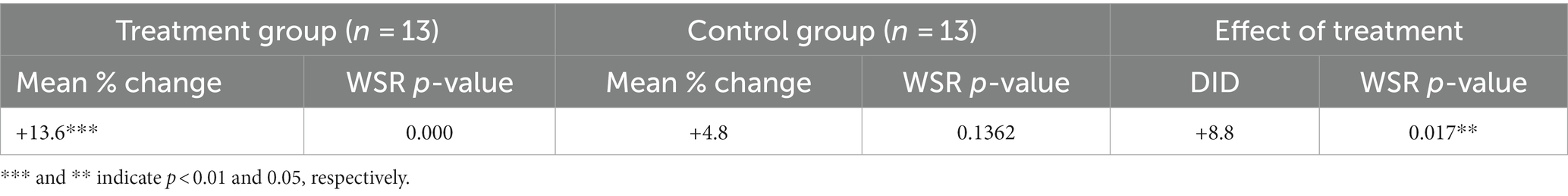
Table 2. Changes and difference-in-differences (DID) in blood hemoglobin concentration using the Wilcoxon matched-pairs signed rank (WSR) test.
Table 3 provides a formal estimation of the treatment effects on blood hemoglobin concentration. The Hausman test was not significant, suggesting the use of the random effect model. The DID estimator indicates that the effect of millet-based diets on hemoglobin concentration was +0.862 g/dL on average.
Interestingly, the subgroup analysis showed that the treatment effects were significant only in the children’s group but not in the adolescent and adult groups (Figure 3). The changes in hemoglobin concentration differed among the three subgroups.
4 Discussion
The studies included 297 adolescents, 268 children, and 25 adults in the intervention groups who consumed millet-based food. The control groups had a total of 260 adolescents, 264 children, and 25 adults. Four studies used pearl millet, two used finger millet, one used mixed millet, and one used sorghum (Supplementary Table S1). The millets, specifically finger millet, pearl millet, and sorghum, are generally not refined in India; therefore, the current study assumes that these are whole grain or whole grain flour. However, rice is consumed in refined form in India. One study was conducted for 25 days and another for 45 days, while the rest of the studies were conducted from 100 days to 4.5 years. The mean hemoglobin concentration in the intervention group before the intervention was 9.95 ± 1.07 g/dL, which increased to 11.3 ± 1.09 g/dL, indicating that, overall, individuals with mild anemia saw an improvement to normal levels. In particular, four studies conducted on children reported an increase in hemoglobin levels, demonstrating a shift from mild anemia to a normal status. In the control group, the mean hemoglobin concentration was 10.2 ± 0.99 g/dL before the treatment, which increased to 10.6 ± 1.09 g/dL after the consumption of their regular staple. This also shows that the anemia status in the control group did not change.
The difference between children and adults in the subgroup analysis could be due to the limited number of studies, especially on adults. The low heterogeneity in the children’s group could have arisen from three studies that used the same type of millet, the small sample size, the same geographical location, and the same population.
The interventions in all the studies reviewed in this study were through controlled trials. However, the studies did not provide information on whether they were randomized in terms of selection and assigning samples. Furthermore, the blinding of the intervention was generally not conducted, which is understandable due to the obvious distinction between millet-based meals and common staple foods in terms of texture and appearance. One study noted the attrition of the participants, which was not justified by the study. The heterogeneity of the studies was high (80%), which may be due to the difference in the age group of participants. Only one study was conducted on adults.
The funnel plot (Figure 4) shows that there is less publication bias, which is evident from the studies that are not scattered in the middle or at the base of the triangle, with the exception of one study. The small sample size in the studies would have made a difference, and therefore, the quality of the obtained evidence was rated as moderate. Although the evidence generated is valuable, it is important to conduct similar studies across various geographical regions with various age groups to strengthen the evidence.
5 Conclusion
This study conducted a meta-analysis of 13 studies involving 1,139 participants in the intervention and control groups. Results show that the consumption of millet-based food had a significant positive effect on blood hemoglobin levels. Yet, it is worth noting that these effects were significant only among the children’s group. More robust findings would have been possible if the studies had confirmed the intake of iron in the intervention and control groups.
The limitations of this study include the limited number of studies reviewed in each age group, the limited types of millets tested, and the lack of geographical diversity. Similar studies across diverse geographical regions and sociocultural groups should be conducted to corroborate the evidence of the beneficial effects of millet consumption in addressing anemia.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SA: Conceptualization, Data curation, Formal analysis, Validation, Writing – original draft. TT: Formal analysis, Methodology, Writing – review & editing. DG: Writing – review & editing. JK-P: Conceptualization, Funding acquisition, Supervision, Writing – review & editing. RoB: Data curation, Formal analysis, Validation, Writing – review & editing. NS: Methodology, Writing – review & editing. SU: Writing – review & editing. MV: Methodology, Writing – review & editing. AR: Writing – review & editing. DP: Writing – review & editing. TL: Writing – review & editing. KS: Writing – review & editing. RaB: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Odisha Millet Mission as part of the International Year of Millet 2023.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1305394/full#supplementary-material
References
1. WHO Global anaemia estimates eds (2021). Available at: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children (Accessed August 17, 2023).
2. Longvah, T, Ananthan, R, Bhaskarachary, K, and Venkaiah, K. Indian food composition table, National Institute of Nutrition; Indian Council of Medical Research: Hyderabad, India. (2017). pp. 1–578.
3. Vaidyanathan, G. Healthy diets for people and the planet. Nature. (2021) 600:22–5. doi: 10.1038/d41586-021-03565-5
4. Willett, W, Rockström, J, Loken, B, Springmann, M, Lang, T, Vermeulen, S, et al. Food in the Anthropocene: the EAT-lancet commission on healthy diets from sustainable food systems. Lancet. (2019) 393:447–92. doi: 10.1016/S0140-6736(18)31788-4
5. Shinde, S, Madzorera, I, and Fawzi, WW. Association of iron supplementation and dietary diversity with nutritional status and learning outcomes among adolescents: results from a longitudinal study in Uttar Pradesh and Bihar, India. J Glob Health. (2021) 11:04037. doi: 10.7189/jogh.11.04037
6. Saaka, M, and Galaa, SZ. How is dietary diversity related to haematological status of preschool children in Ghana? Food. Nutr Res. (2017) 61:1333389. doi: 10.1080/16546628.2017.1333389
7. Kane-Potaka, J, and Kumar, P. “Smart food – food that is good for you, the planet and the farmer,” In State of India's livelihoods report (2019) (New Delhi: Access Development Services), 71–82. Available at: SOIL-Smart-Foods.pdf (smartfood.org).
8. Anitha, S, Tsusaka, TW, Botha, R, Givens, DI, Rajendran, A, Parasannanavar, DJ, et al. Impact of regular consumption of millets on fasting and post prandial blood glucose level: a systematic review and meta-analysis. Front Sustain Food Syst. (2023) 7:1226474. doi: 10.3389/fsufs.2023.1226474
9. Anitha, S, Tsusaka, TW, Botha, R, Kane-Potaka, J, Givens, DI, Rajendran, A, et al. Are millets more effective in managing hyperlipidaemia and obesity than major cereal staples? A systematic review and meta-analysis. Sustainability. (2022) 14:6659. doi: 10.3390/su14116659
10. Anitha, S, Givens, DI, Subramaniam, K, Upadhyay, S, Kane-Potaka, J, Vogtschmidt, YD, et al. Can feeding a millet-based diet improve the growth of children?—a systematic review and meta-analysis. Nutrients. (2022) 14:225. doi: 10.3390/nu14010225
11. Anitha, S, Kane-Potaka, J, Botha, R, Givens, DI, Sulaiman, NLB, Upadhyay, S, et al. Millets can have a major impact on improving iron status, haemoglobin level and in reducing iron deficiency anaemia—a systematic review and meta-analysis. Front Nutr. (2021) 8:725529. doi: 10.3389/fnut.2021.725529
12. Mohar, D, Liberati, A, Tetzlaff, J, and Altman, DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. Open Med. (2009) 3:8. doi: 10.1136/bmj.b2535
13. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 88:105906. doi: 10.1371/journal.pmed.1003583
14. Harrer, M, Cuijpers, P, Furukawa, TA, and Ebert, DD. Doing meta-analysis with R: a hands-on guide. (2019). Available at: https://bookdown.org/MathiasHarrer/Doing_Meta_Analysis_in_R/ (Accessed February 28, 2021).
15. Atkinson, LZ, and Cipriani, A. How to carry out a literature search for a systematic review: a practical guide. BJPsych Adv. (2018) 24:74–82. doi: 10.1192/bja.2017.3
16. Ryan, R, and Hill, S. How to GRADE the quality of the evidence? Cochrane consumers and communication group. Version 3.0. (2016). Available at: http://cccrg.cochrance.org/author-resources (Accessed December 7, 2021).
17. Higgins, JPT, Thomas, J, Chandler, J, Cumpston, M, Li, T, and Page, MJ. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021); Welch, V.A., Ed.; Cochrane: London, UK, (2021). Available at: www.training.cochrane.org/handbook (Accessed April 13, 2021).
18. R Core Team. R: a language and environment for statistical computing ; R Foundation for Statistical Computing: Vienna, Austria, (2022). Available at: https://www.R-project.org/ (Accessed September 4, 2022).
19. Ahn, E, and Kang, H. Introduction to systematic review and meta-analysis. Korean J Anaesthesiol. (2019) 71:103–12. doi: 10.4097/kjae.2018.71.2.103
20. Hak, T, Van Rhee, HJ, and Suurmond, R. How to interpret results of meta-analysis; Erasmus Rotterdam Institute of Management: Rotterdam, the Netherlands, (2016); pp. 1–2. Available at: https://www.erim.eur.nl/research-support/metaessentials/downloads (Accessed April 26, 2021).
21. Isreal, H, and Richter, RP. A guide to understanding meta-analysis. J Orthop Sports Phys Ther. (2011) 41:496–504. doi: 10.2519/jospt.2011.3333
22. Bell, A, Fairbrother, M, and Jones, K. Fixed and random effects models: making an informed choice. Qual Quant. (2019) 53:1051–74. doi: 10.1007/s11135-018-0802-x
23. Balduzzi, S, Rücker, G, and Schwarzer, G. How to perform a meta-analysis with R: a practical tutorial? Evid Based Ment Health. (2019) 22:153–60. doi: 10.1136/ebmental-2019-300117
24. Karkada, S, Upadhya, S, Upadhya, S, and Bhat, G. Beneficial effect of ragi (finger millet) on haematological parameters, body mass index, and scholastic performance among anemic adolescent high-school girls (AHSG). Compr Child Adolesc Nurs. (2018) 42:141–50. doi: 10.1080/24694193.2018.1440031
25. Arokiamary, S, Senthilkumar, R, and Kanchana, S. Impact of pearl millet based complementary food on biochemical and cognitive profiles of school children (5-6 year old). European J Nutr Food Saf. (2020) 12:24–34. doi: 10.9734/ejnfs/2020/v12i730245
26. Scott, SP, Murray-Kolb, LE, Wenger, MJ, Udipi, SA, Ghugre, PS, Boy, E, et al. Cognitive performance in Indian school going adolescents is positively affected by consumption of iron-biofortified pearl millet: a 6-month randomized controlled efficacy trial. J Nutr. (2018) 148:1462–71. doi: 10.1093/jn/nxy113
27. Finkelstein, JL, Mehta, S, Udipi, SA, Ghugre, PS, Luna, SV, Wenger, MJ, et al. A randomized trial of iron-biofortified pearl millet in school children in India. J Nutr. (2015) 145:1576–81. doi: 10.3945/jn.114.208009
28. Moharana, A, Khosla, P, Nayak, D, and Tripathy, P. Effect of finger millet [ragi] ladoo consumption on the level of hemoglobin. Eur J Mol Clin Med. (2020) 7:1018–22.
29. Singh, TS, Goyal, M, and Sheth, M. Intervention trials with pearl millet-based iron rich ladoo and iron folic acid (IFA) tablets on hemoglobin status of adolescent females in Bikaner city. Stud Ethno-Med. (2014) 8:77–82. doi: 10.1080/09735070.2014.11886475
30. Durairaj, M, Gurumurthy, G, Nachimuthu, V, Muniappan, K, and Balasubramanian, S. Dehulled small millets: the promising nutri cereals for improving the nutrition of children. Matern Child Nutr. (2019) 15:e12791. doi: 10.1111/mcn.12791
31. Rajendra Prasad, MP, Senhur, B, Kommi, K, Madhari, R, Rao, MV, and Patil, JV. Impact of sorghum supplementation on growth and micronutrient status of school going children in southern India–a randomized trial. Indian J Pediatr. (2015) 83:9–14. doi: 10.1007/s12098-015-1782-7
32. Devdas, RP, Chandrasekhar, U, and Bhooma, N. Nutritional outcomes of a rural diet supplemented with low-cost locally available foods – V impact on pre-schoolers followed over a period of four and a half years. Indian J Nutr Diet. (1984) 21:153–64.
33. Devdas, RP, Chandrasekhar, U, and Bhooma, N. Nutritional outcomes of a rural diet supplemented with low cost locally available foods – VIII impact on preschool children from a tribal community. Indian J Nutr Diet. (1984) 21:315–21.
34. Devdas, RP, Chandrasekhar, U, and Bhooma, N. Nutritional outcomes of a rural diet supplemented with low cost locally available foods – VI impact on school children. Indian J Nutr Diet. (1984) 21:187–93.
Keywords: iron deficiency anemia, millets, hemoglobin, dietary iron, difference-in-differences
Citation: Anitha S, Tsusaka TW, Givens DI, Kane-Potaka J, Botha R, Sulaiman NLB, Upadhyay S, Vetriventhan M, Rajendran A, Parasannanavar DJ, Longvah T, Subramaniam K and Bhandari RK (2024) Does millet consumption contribute to raising blood hemoglobin levels compared to regular refined staples?: a systematic review and meta-analysis. Front. Nutr. 11:1305394. doi: 10.3389/fnut.2024.1305394
Edited by:
Ana Carla Cepeda Lopez, Hospital Zambrano Hellion TecSalud, MexicoReviewed by:
Fahrul Nurkolis, State Islamic University of Sunan Kalijaga (UIN Sunan Kalijaga Yogyakarta), IndonesiaChristèle Icard-Vernière, Institut de Recherche Pour le Développement (IRD), France
Copyright © 2024 Anitha, Tsusaka, Givens, Kane-Potaka, Botha, Sulaiman, Upadhyay, Vetriventhan, Rajendran, Parasannanavar, Longvah, Subramaniam and Bhandari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seetha Anitha, ZHIuYW5pdGhhc2VldGhhQGdtYWlsLmNvbQ==
 Seetha Anitha
Seetha Anitha Takuji W. Tsusaka
Takuji W. Tsusaka D. Ian Givens
D. Ian Givens Joanna Kane-Potaka5
Joanna Kane-Potaka5 Shweta Upadhyay
Shweta Upadhyay Ananthan Rajendran
Ananthan Rajendran Thingnganing Longvah
Thingnganing Longvah Kowsalya Subramaniam
Kowsalya Subramaniam Raj Kumar Bhandari
Raj Kumar Bhandari