- 1Department of Community Nutrition, Vice-Chancellery for Health, Shiraz University of Medical Sciences, Shiraz, Iran
- 2Department of Nutrition, School of Public Health, Zanjan University of Medical Sciences, Zanjan, Iran
- 3Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran
Background: The coronavirus disease 2019 (COVID-19) pandemic clearly affected the lifestyle and dietary habits of millions of people worldwide. The purpose of this study was to evaluate the association of major dietary patterns with socioeconomic status, obesity, and contracting COVID-19.
Methods: We conducted a cross-sectional study using an online survey for data collection with a total of 1,187 participants (over the age of 18 years) who reported their sociodemographic details, anthropometric index (weight and height), and dietary intake. Multivariable logistic regression models were applied to assess the association between major dietary patterns and study outcomes.
Results: A total of 1,106 adults were included in the current analysis. We identified three major dietary patterns (plant-based, meat, and Western dietary patterns). The mean age of participants was significantly higher in the upper tertile of plant-based dietary patterns (DPs) compared to the first tertile, while it was lower in the top tertile of meat and Western DPs. The percentage of participants who lived in urban areas was significantly higher in the third tertile of meat DP than in the first tertile (p < 0.001). Moderate adherence to Western DP was significantly associated with increased odds of obesity (OR: 1.79; 95% CI: 1.17, 2.74). In addition, high adherence to Western DP was significantly related to increased odds of obesity after controlling for confounders. Subjects in the second tertile of the Western DP had higher odds (95% Cl: 1.04, 1.92) for COVID-19 infection than the first tertile.
Conclusion: This study showed that moderate and high adherence to a Western dietary pattern was associated with a higher risk of obesity and COVID-19 infection during the pandemic. Future studies are needed to confirm these findings.
1 Introduction
Coronavirus disease-2019 (COVID-19), caused by a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has become a global public health crisis of this century (1). The pandemic situation and the measures needed to control the spread of the disease have resulted in lockdowns and many restrictions on daily living, with probable consequences on lifestyle, particularly affecting physical activity, sleep quality, eating habits, and mental health (2–4). Available evidence has shown several unhealthy lifestyles during the COVID-19 pandemic, including increased sedentary behavior and less time spent on physical exercise (5).
Moreover, negative emotions (e.g., stress and boredom), sleep disorders, and sedentary behaviors caused by home confinement could promote overconsumption, change dietary patterns, and reduce diet quality (6). These changes result in higher consumption of “comfort foods” and energy imbalance. These foods, mainly rich in simple carbohydrates, unhealthy fat, and sugar, are associated with an increased risk for more severe complications of COVID-19 (7, 8), thereby increasing the risk of developing non-communicable diseases (NCDs), such as obesity, diabetes, and cardiovascular disease (9).
On the other hand, obese subjects are one of the groups with a higher risk for COVID-19 complications (10). Kompaniyets et al. (11) reported that obesity is associated with a 3.07 times higher risk of hospitalization and a 1.42 times higher risk of severe illness when hospitalized. Obesity-induced adipose tissue expansion contributes to increased circulating levels of proinflammatory cytokines (12). This low-grade inflammation state could further exacerbate the inflammation in patients with COVID-19 (13).
Xu et al. observed that prudent dietary patterns, which are characterized by high intake of fresh fruits and vegetables, and low intake of soft drinks and fried food were negatively associated with weight gain among the Chinese population during the COVID-19 pandemic (13). In addition, a healthy dietary pattern, which is based on healthy fats, plant food (fruits, vegetables, cereals, and legumes), and low-fat protein foods, could support the immune system in fighting infections such as COVID-19 (14, 15). A recent meta-analysis showed that the effectiveness of a plant-based diet against COVID-19 infection was 50% (16). Moreover, an observational study indicated that unhealthy or traditional dietary patterns were associated with a higher risk of severe COVID-19 (17).
Dietary patterns are mainly shaped by income and food prices. A decrease in the financial capacity to purchase food due to job instability during the pandemic would lead to adjusting the items of food baskets with more affordable resources (18).
Therefore, the current study is conducted to determine the association of major dietary patterns with socioeconomic status, obesity, and contracting COVID-19 among Iranian adults.
2 Methods and materials
2.1 Study design and population
The present cross-sectional web-based survey was performed among Iranian adults during the COVID-19 pandemic.
The required sample size was calculated using Gpower software (α = 0.05, β = 0.2) according to a previous study. Therefore, the estimated sample size for the study is 515 volunteers. A combination of convenience and snowball sampling was used to employ participants.
Participants aged 18 years or above and living in Iran were considered as inclusion criteria. Participants excluded from the study were those (1) who were pregnant or lactating, (2) who were on specific diets, and (3) who did not fill out the questionnaire appropriately or reported invalid data.
2.2 Study variables and tools
An online questionnaire with an invitation letter was posted through different social media portals (including Instagram and WhatsApp). To prevent duplicate responses, we used an online form that allows only one response per user. We also asked the participants to share the study link to increase the number of persons who receive the invitation link. The purpose of the survey was provided on the cover page of the online questionnaire to inform the participants.
An online questionnaire was prepared in which participants self-reported sections regarding categories of sociodemographic characteristics, food consumption, and anthropometric index (weight and height) during the COVID-19 pandemic.
Dietary intake was assessed using a modified food frequency questionnaire (FFQ). The validity and reliability of the FFQ were evaluated previously (18). The correlation coefficient for reliability was 0.77. Since this survey was conducted during the COVID-19 pandemic, we summarized the questionnaire to prevent the adverse effects of the length of the questionnaire on the response rate. Each item included a typical portion size. Participants reported each food consumption based on servings per week.
Self-reported data on weight and height were used to calculate BMI by dividing weight (kg) by high squared (m2) and interpreted according to the criteria of the World Health Organization. Following this, the participants were classified into groups: (i) underweight (BMI < 18.5), (ii) normal weight (BMI between 18.5 and 24.9), (iii) overweight (BMI between 25 and 29.9), and (iv) obese (BMI ≥ 30).
Data on age, gender, education level, place of living, marital status, and smoking during the pandemic were collected. Socioeconomic status (SES) was evaluated based on scoring variables related to their household asset and wealth (homeownership, personal vehicle, washing machine, LCD/LED TV, dishwasher, laptop/computer, refrigerator, and microwave), education, and income. The SES score was computed for each respondent, and participants were then classified into three categories (low, medium, and high) using tertiles of the distribution of the SES scores as cutoff points.
In addition, respondents reported their health status, such as chronic diseases (diseases with proven diagnosis) and whether they were previously infected with COVID-19. According to the UK NHS report, if participants had any of 10 medical conditions (e.g., diabetes, weakened immune system, chronic kidney disease, etc.), they were considered to be “high risk” for COVID-19.
The present online survey was reported based on the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines (19).
2.3 Ethics statement
The study protocol was approved by the ethics committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1401.34).
2.4 Statistical analysis
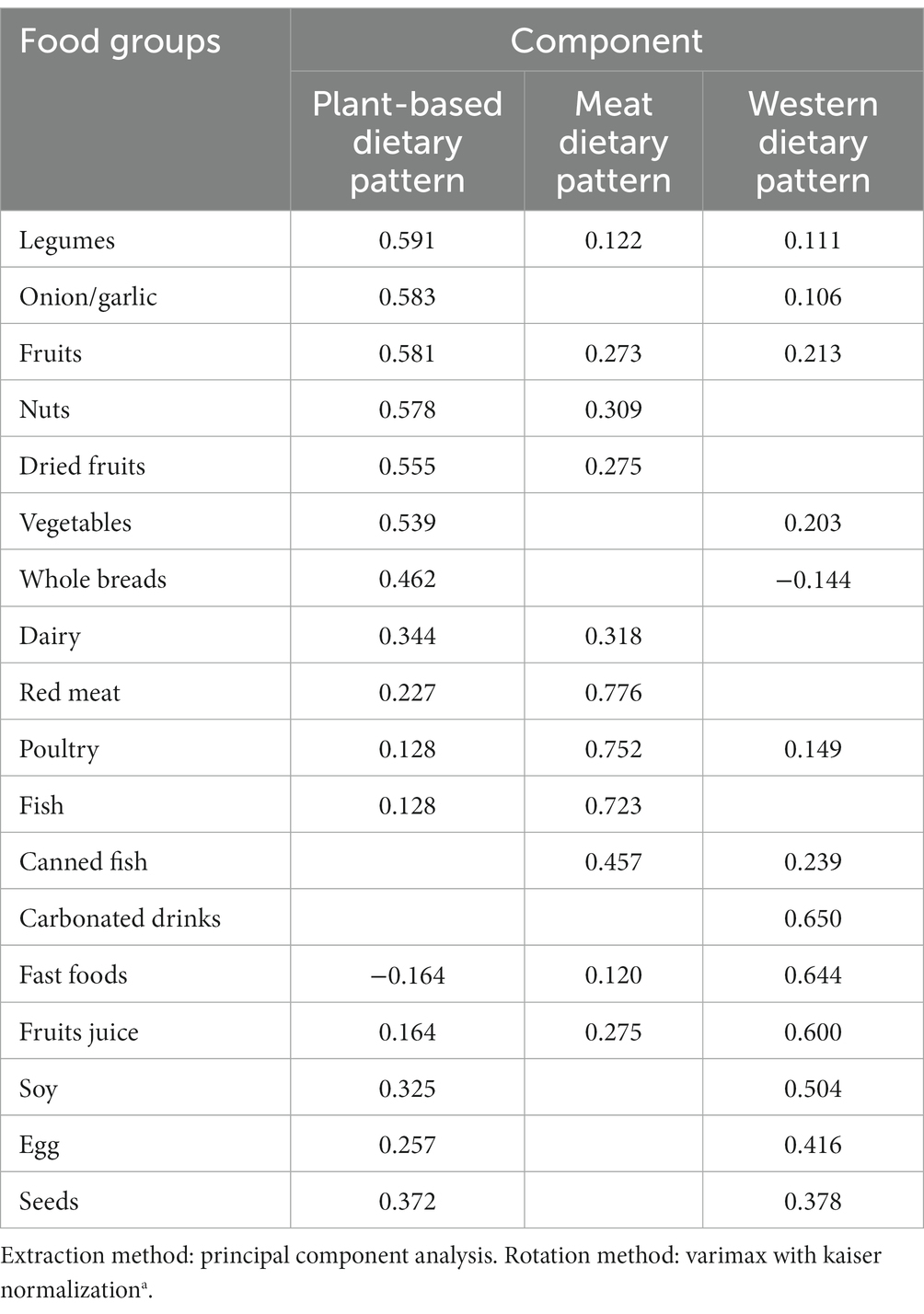
The principal component analysis method was applied to identify dietary patterns. Dietary patterns were identified based on 18 food groups, eigenvalue (>1), factor interpretability, and the explained variance (>5%). Factors were rotated with varimax to achieve uncorrelated factors and improve the interpretability. Each food group received a factor loading associated with each dietary pattern. Factor loadings show the correlation coefficient between the food group and the dietary pattern. In the present study, food groups with factor loadings of more than 0.2 were considered to be important contributors to the pattern. After that, the factor score for each dietary pattern was computed by summing up intakes of food groups weighted by their factor loadings. Respondents received a factor score for each identified dietary pattern and were categorized into tertiles (three groups with equal sample size) of dietary patterns’ scores. Participants in the lowest tertile (T1) had the lowest adherence to the identified dietary pattern, and those in the highest tertile (T3) had the highest adherence to that dietary pattern.
The normality of the data distribution was evaluated by the one-sample Kolmogorov–Smirnov test. The quantitative variables were expressed as mean ± SD and qualitative variables as frequency (percentage). To compare the quantitative variables across tertiles of dietary patterns, a one-way analysis of variance (ANOVA) was used, while for categorical variables, the chi-square test was applied. To determine the association of dietary patterns with weight status and contracting COVID-19, multivariable logistic regression was applied. The odds ratios (ORs) and their 95% confidence intervals (95% CIs) were calculated in crude and adjusted models. In Model I, adjustment was made for the main confounders (age and gender). In Model II, additional adjustments were conducted for smoking status, marital status, and SES. The first tertile of dietary patterns was considered the reference category in all analyses.
3 Results
In total, 1,187 subjects were participated in the current study. Removal of participants who were not eligible (e.g., under 18 years) and participants who did not complete the survey resulted in a final sample size of N = 1,106.
Three major dietary patterns were identified using principal components analysis, and they were labeled as “Plant-based dietary pattern (DP),” “Meat DP,” and “Western DP.” These three dietary patterns explained 39.34% of the total variation in dietary intakes in this population. The “Plant-based DP” was characterized by high consumption of legumes, onions/garlic, fruits, nuts, dried fruits, vegetables, whole breads, and dairy. The “Meat DP” was mainly loaded with red meat, poultry, fish, and canned fish. The “Western DP” was associated with higher intakes of fast foods, carbonated drinks, fruit juice, soy, egg, and seeds. All food groups and their loading factors for each dietary pattern are presented in Table 1.
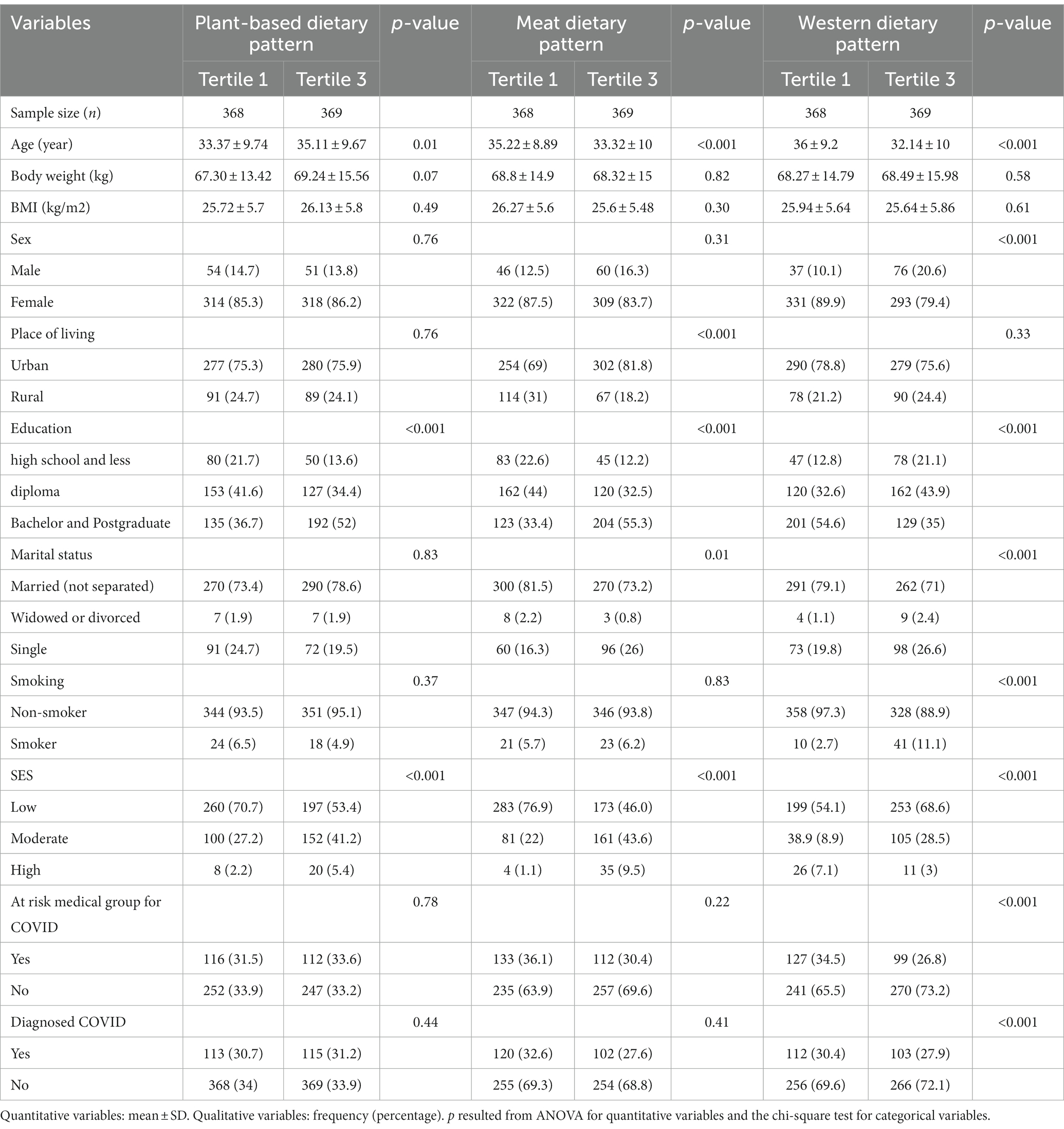
The mean age and BMI of respondents were 34.5 ± 9.4 years and 26 ± 6.57 kg/m2, respectively; 85.2% of included subjects were female. The sociodemographic characteristics of participants across tertiles of the dietary patterns are presented in Table 2. The mean age of subjects was significantly higher in the upper tertile of plant-based DP compared to the first tertile (p = 0.01), while it was lower in the top tertile of meat DP and Western DP (p < 0.001). The percentage of women in the first tertile of Western DP was more than that in the third tertile. The frequency of participants who lived in urban areas was significantly higher in the third tertile of meat DP than in the first tertile (p < 0.001). Most subjects had bachelor’s and postgraduate degrees in the top tertile of plant-based DP and meat DP (p < 0.001), while a high frequency of the participants had bachelor’s and postgraduate degrees in the first tertile of Western DP (p < 0.001). The percentage of married subjects in the highest tertile of meat DP (p = 0.01) and Western DP (p < 0.001) were significantly lower than the first one. The proportion of respondents who had low SES in the first tertile of the plant-based DP and meat DP were notably higher compared to the top tertile (p < 0.001(, while it was higher in the third tertile of Western DP (p < 0.001). Furthermore, the percentage of participants who had a high risk for COVID-19 and had been diagnosed with COVID-19 was significantly lower in the last tertile of Western DP (p < 0.001). Body weight and BMI were not significantly different among the tertiles of the various types of dietary patterns.
3.1 Association of dietary patterns with BMI and contracting COVID-19
Multivariable-adjusted ORs (95% CI) for the association of dietary patterns with BMI and contracting COVID-19 are shown in Table 3. In the crude and adjusted models, no significant association was found between plant-based DP with underweight, obesity, and contracting COVID-19. In the case of the association of plant-based DP with overweight, the moderate adherence (second tertile) to plant-based DP was significantly related to increased odds of overweight (OR: 1.41; 95% CI: 1.02, 1.96); however, the relationship disappeared after adjusting for potential confounders. In the crude model, participants in the highest tertile of the Western DP had 2.62-fold higher odds (95% Cl: 1.32, 5.2) for underweight than the first one. However, this association disappeared after considering potential confounding variables.
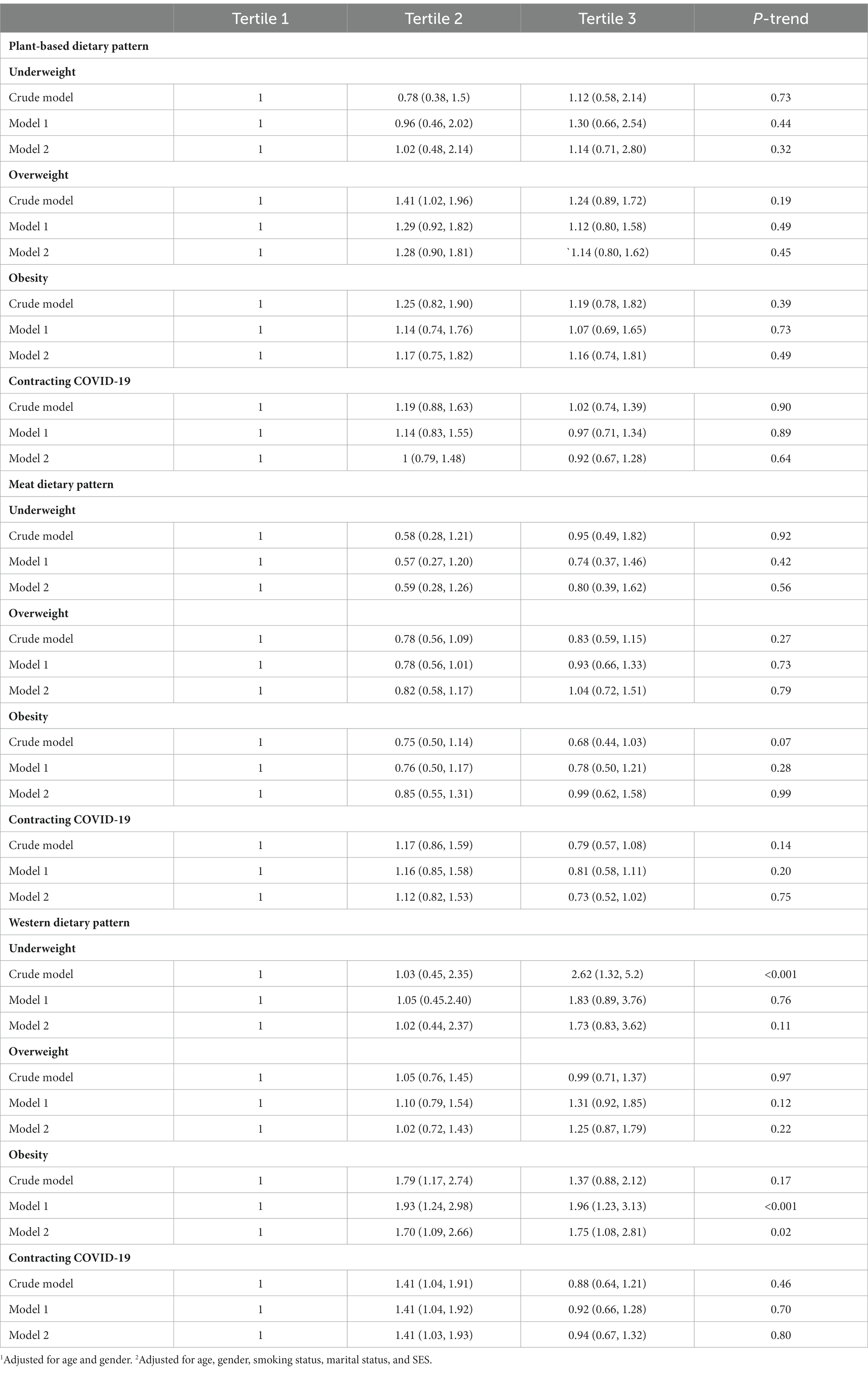
Table 3. Multivariate adjusted odds ratio (OR) and 95% confidence interval (CI) for the association of dietary patterns with BMI and contracting COVID-19.
Moreover, moderate adherence to Western DP was significantly associated with increased odds of obesity (OR: 1.79; 95% CI: 1.17, 2.74). This relation remained significant even after adjusting for confounders. In addition, high adherence to Western DP was significantly related to increased odds of obesity after controlling for confounders (model 1: OR: 1.96; 95% CI: 1.23, 3.13; model 2: OR: 1.75; 95% CI: 1.08, 2.81). Regarding contracting COVID-19, participants in the second tertile of the Western DP had 1.41-fold higher odds (95% Cl: 1.04, 1.92) for COVID-19 infection. This association remains significant after adjusting for confounding variables. However, neither crude nor adjusted models found any significant association among meat DP, BMI status, and contracting COVID-19.
4 Discussion
Our study aimed to investigate the association of major dietary patterns with socioeconomic status (SES), obesity, and contracting COVID-19 among Iranian adults. The findings from this cross-sectional survey provided valuable insights into the relationship between dietary patterns and these health outcomes. We found that participants with moderate and high adherence to Western DP had higher odds of obesity. In addition, we found that participants with moderate adherence to Western DP had higher odds of contracting COVID-19. However, we could not find any significant correlation between meat DP and plant-based DP with contracting COVID-19.
When examining the association between dietary patterns and BMI, we found that adherence to the Western DP was significantly associated with an increased likelihood of obesity. The Western DP is a widely followed eating pattern characterized by high salt, trans fats, saturated fats, and simple carbohydrates. However, it lacks complex carbohydrates and fibers. Moreover, it is considered a calorie-dense diet deficient in essential nutrients such as vitamins and minerals (20). These findings are consistent with previous studies that have shown the detrimental effects of Western DP on weight status. It has been reported in a population-based study that following the Western DP closely correlated with higher risks of obesity and weight gain (21). A cohort of healthy reproductive-age women study showed that adherence to the Western DP is associated with higher odds of obesity (OR: 2.68) (22). The findings of the cross-sectional study showed that modern dietary pattern (higher intake of soft drinks, fried foods, pickles, and lower intake of fresh vegetables) was positively associated with weight gain in men and women during the COVID-19 pandemic (23). In addition, our results align with a previous meta-analysis, indicating a 65% heightened risk of obesity linked to the Western DP (24). In terms of the mechanism, the Western DP led to hyperinsulinemia, which causes increased fat storage, appetite, hyperphagia, and carbohydrate craving (25).
Obesity is one of the main risk factors for increasing the risk of contracting COVID-19. Singh et al. (26) in a systematic review and meta-analysis study, showed that obesity was associated with an increased risk of severe disease and mortality rate among patients with COVID-19. In terms of odds of contracting COVID-19, we found that participants with moderate adherence to Western DP had significantly higher odds of COVID-19. In line with our findings, it has been reported in previous studies that moderate or higher adherence to Western DP led to a significant increase in the risk of infectious diseases such as COVID-19. Ebrahimzadeh et al. (17) in a cross-sectional study, showed that participants who followed unhealthy dietary patterns such as Western DP had a higher risk for COVID-19 and its related symptoms such as cough, fever, chilling, weakness, myalgia, nausea and vomiting, and sore throat.
Various mechanisms have been proposed that consumption of the Western diet increases the risk of chronic diseases such as fatty liver (27), cardiovascular diseases (28), metabolic syndrome (29), and infectious diseases. Long-term adherence to the Western dietary pattern increases the level of inflammatory factors (30), oxidative stress (31), and lipid peroxidation (32), all of which can be involved in the development of chronic diseases. In this study, unlike most of the previous studies, we considered the meat group as a separate dietary pattern, while in some studies, the high consumption of meats, especially red meat, is considered part of the Western dietary pattern.
Interestingly, the plant-based DP did not show a significant association with underweight, obese, or overweight and contracting COVID-19 in the adjusted models. In contrast to our findings, according to Kim et al.’s (33) population-based case–control study conducted in six countries, there was a significant 73% reduction in the likelihood of experiencing moderate-to-severe COVID-19 severity with a strong adherence to a plant-based DP. In addition, it has been reported in another study that higher adherence to plant-based DP caused a significant improvement against SARS-CoV-2 infection (16). Moreover, some studies indicated that higher adherence to the Mediterranean DP is negatively associated with COVID-19 infection-related deaths (34, 35).
Part of the contrast observed in our study with other studies could be due to the difference in the type of food selected in the plant-based DP and infection rates. Fruits and vegetables provide a wealth of vitamins, folate, fiber, and various phytochemicals such as carotenoids and flavonoids. In addition, whole grains are a rich source of group B vitamins, which have the ability to strengthen the endogenous antioxidant system (36–38). These compounds possess immune-protective properties due to their anti-inflammatory, antibacterial, and antiviral effects (39–41). It has been reported in a previous study that consuming a minimum of 0.67 daily servings of vegetables (excluding potatoes, whether cooked or raw) has been linked to a reduced risk of contracting COVID-19 (42). According to recent ecological studies on COVID-19, countries that have a significant intake of food rich in antioxidants or foods with anti-angiotensin-converting enzyme (ACE) activity, like raw or fermented cabbage, show a lower rate of COVID-19-related fatalities when compared to other countries (43, 44).
We could not find any significant correlation among meat DP, BMI status, and contracting COVID-19. However, Chen et al. (45) reported that students with a higher BMI consumed more meat products than others during the COVID-19 pandemic. Another study indicated that lower consumption of legumes, vegetables, and fruits and a higher intake of meat, sweets, salty snacks, and fast food are associated with obesity during the COVID-19 lockdown in Poland (46). In a population base study among the participants in the UK, it has been reported that participants in the 4th quartile of processed meat intake had higher odds for COVID-19, but in line with our findings, they did not find any significant correlation between total meat intake and COVID-19 (42). Sausages, bacon, and ham are the primary sources of processed meat consumption in many countries, and they frequently contain salt enriched with nitrates/nitrites (47). This type of meat also contains many preservatives and additives, many of which are harmful to health. Processed meats tend to have higher concentrations of both total and saturated fat (48, 49). Consumption of processed meats, commonly associated with a Western DP, might have a negative impact on immunity (50). Therefore, other dietary habits connected to processed meat intake may be responsible for the observed link with susceptibility to COVID-19.
This finding suggests that although plant-based DP is generally considered a healthy dietary pattern, moderate adherence to it may not have a significant impact on weight status among Iranian adults. Further research is needed to explore the potential factors influencing this result.
As a novelty, this study is the first one to evaluate the association of major dietary patterns with the risk of COVID-19 contracting. Our study has other strong points, including a large and diverse population sample. This evidence can be used to develop preventive measures against COVID-19 contracting and weight gain during the COVID-19 pandemic.
In interpreting the results of our study, it is important to acknowledge some limitations. First, the cross-sectional nature of the study design limits our ability to establish causality between dietary patterns and health outcomes. Second, the self-reported dietary assessment method might introduce recall bias and measurement error. Additionally, the reliance on self-reported weight and height for BMI calculation may introduce inaccuracies in the classification of weight status. Finally, the study sample mainly consisted of female participants, which may limit the generalizability of the findings to the entire Iranian adult population.
In conclusion, our study highlights the associations between major dietary patterns, socioeconomic status, obesity, and contracting COVID-19 among Iranian adults. The Western DP showed unfavorable associations with obesity and increased odds of contracting COVID-19, while the plant-based DP did not show significant associations with weight status or COVID-19 infection in the adjusted models. These findings emphasize the importance of promoting healthy dietary patterns, such as plant-based diets, for preventing obesity and potentially reducing the risk of COVID-19 infection. Future research should focus on longitudinal designs and more diverse populations to further investigate these associations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Studies involving humans were approved by Research Ethics Committee of Shiraz University of Medical sciences (IR. SUMS.REC.1401.344). The current study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was provided by participants.
Author contributions
MM: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft. MR: Writing – original draft. AS: Writing – original draft, Investigation. SS: Data curation, Investigation, Methodology. SM: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The present study was approved and financially supported by a grant from Vice-Chancellor for Research, Shiraz University of Medical Sciences, Shiraz, Iran (Ethics code: IR.SUMS.REC.1401.344; grant number: 23989).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Xu, J, Xu, X, Jiang, L, Dua, K, Hansbro, PM, and Liu, G. SARS-CoV-2 induces transcriptional signatures in human lung epithelial cells that promote lung fibrosis. Respir Res. (2020) 21:1–12. doi: 10.1186/s12931-020-01445-6
2. Maharat, M, Sajjadi, SF, and Moosavian, SP. Changes in dietary habits and weight status during the COVID-19 pandemic and its association with socioeconomic status among Iranians adults. Front Public Health. (2023) 10:1080589. doi: 10.3389/fpubh.2022.1080589
3. Pinto, J, van Zeller, M, Amorim, P, Pimentel, A, Dantas, P, Eusébio, E, et al. Sleep quality in times of Covid-19 pandemic. Sleep Med. (2020) 74:81–5. doi: 10.1016/j.sleep.2020.07.012
4. Kauhanen, L, Wan Mohd Yunus, WMA, Lempinen, L, Peltonen, K, Gyllenberg, D, Mishina, K, et al. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. (2023) 32:995–1013. doi: 10.1007/s00787-022-02060-0
5. Arena, R, Pronk, NP, Laddu, D, Whitsel, LP, Sallis, JF, Lavie, CJ, et al. Mapping one million COVID-19 deaths and unhealthy lifestyle behaviors in the United States: recognizing the syndemic pattern and taking action. Am J Med. (2022) 135:1288–95. doi: 10.1016/j.amjmed.2022.06.006
6. Noll, PRES, Nascimento, MG, Bayer, LHCM, Zangirolami-Raimundo, J, Turri, JAO, Noll, M, et al. Changes in food consumption in postmenopausal women during the COVID-19 pandemic: a longitudinal study. Nutrients. (2023) 15:3494. doi: 10.3390/nu15153494
7. Butler, MJ, and Barrientos, RM. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav Immun. (2020) 87:53–4. doi: 10.1016/j.bbi.2020.04.040
8. Zhang, X, Chen, B, Jia, P, and Han, J. Locked on salt? Excessive consumption of high-sodium foods during COVID-19 presents an underappreciated public health risk: a review. Environ Chem Lett. (2021) 19:3583–95. doi: 10.1007/s10311-021-01257-0
9. Al-Jawaldeh, A, and Abbass, MM. Unhealthy dietary habits and obesity: the major risk factors beyond non-communicable diseases in the eastern mediterranean region. Front Nutr. (2022) 9:817808. doi: 10.3389/fnut.2022.817808
10. Alwarawrah, Y, Kiernan, K, and MacIver, NJ. Changes in nutritional status impact immune cell metabolism and function. Front Immunol. (2018) 9:1055. doi: 10.3389/fimmu.2018.01055
11. Kompaniyets, L, Goodman, AB, Belay, B, Freedman, DS, Sucosky, MS, Lange, SJ, et al. Body mass index and risk for COVID-19–related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death—United States, march–December 2020. Morb Mortal Wkly Rep. (2021) 70:355. doi: 10.15585/mmwr.mm7010e4
12. Hauner, H . Secretory factors from human adipose tissue and their functional role. Proc Nutr Soc. (2005) 64:163–9. doi: 10.1079/PNS2005428
13. Muscogiuri, G, Pugliese, G, Barrea, L, Savastano, S, and Colao, A. Commentary: obesity: the “Achilles heel” for COVID-19? Metabolism. (2020):108. doi: 10.1016/j.metabol.2020.154251
14. Singh, S, and Singh, RK. Nutritional interventions to augment immunity for COVID-19. Nutr Diabetes. (2022) 12:13. doi: 10.1038/s41387-022-00194-3
15. Brown, RB . Low dietary sodium potentially mediates COVID-19 prevention associated with whole-food plant-based diets. Br J Nutr. (2023) 129:1136–41. doi: 10.1017/S0007114522002252
16. Rahmati, M, Fatemi, R, Yon, DK, Lee, SW, Koyanagi, A, Il Shin, J, et al. The effect of adherence to high-quality dietary pattern on COVID-19 outcomes: a systematic review and meta-analysis. J Med Virol. (2023) 95:e28298. doi: 10.1002/jmv.28298
17. Ebrahimzadeh, A, Taghizadeh, M, and Milajerdi, A. Major dietary patterns in relation to disease severity, symptoms, and inflammatory markers in patients recovered from COVID-19. Front Nutr. (2022) 9:929384. doi: 10.3389/fnut.2022.929384
18. Darmon, N, and Drewnowski, A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. (2015) 73:643–60. doi: 10.1093/nutrit/nuv027
19. Eysenbach, G . Improving the quality of web surveys: The checklist for reporting results of internet E-surveys (CHERRIES). Gunther Eysenbach Centre for Global eHealth Innovation: Toronto, Canada (2004). e34 p.
20. Aljadani, H . Impact of different dietary patterns and micronutrients on the immune system and COVID-19 infection. Curr Res Nutr Food Sci. (2021) 9:127–138. doi: 10.12944/CRNFSJ.9.1.13
21. Chen, Y, Kang, M, Kim, H, Xu, W, and Lee, JE. Associations of dietary patterns with obesity and weight change for adults aged 18–65 years: evidence from the China health and nutrition survey (CHNS). PLoS One. (2023) 18:e0279625. doi: 10.1371/journal.pone.0279625
22. Bedrick, BS, Eskew, AM, Chavarro, JE, and Jungheim, ES. Dietary patterns, physical activity, and socioeconomic associations in a Midwestern cohort of healthy reproductive-age women. Matern Child Health J. (2020) 24:1299–307. doi: 10.1007/s10995-020-02987-3
23. Xu, X, Yan, AF, Wang, Y, and Shi, Z. Dietary patterns and changes in weight status among Chinese men and women during the COVID-19 pandemic. Front Public Health. (2021) 9:709535. doi: 10.3389/fpubh.2021.709535
24. Mu, M, Xu, LF, Hu, D, Wu, J, and Bai, MJ. Dietary patterns and overweight/obesity: a review article. Iran J Public Health. (2017) 46:869–76.
25. Kopp, W . How western diet and lifestyle drive the pandemic of obesity and civilization diseases. Diabetes Metab Syndr Obes. (2019) 12:2221–36. doi: 10.2147/DMSO.S216791
26. Singh, R, Rathore, SS, Khan, H, Karale, S, Chawla, Y, Iqbal, K, et al. Association of Obesity with COVID-19 severity and mortality: an updated systemic review, Meta-analysis, and Meta-regression. Front Endocrinol (Lausanne). (2022) 13:780872. doi: 10.3389/fendo.2022.780872
27. Oddy, WH, Herbison, CE, Jacoby, P, Ambrosini, GL, O'sullivan, TA, Ayonrinde, OT, et al. The Western dietary pattern is prospectively associated with nonalcoholic fatty liver disease in adolescence. Official J Am College Gastroenterol. (2013) 108:778–85. doi: 10.1038/ajg.2013.95
28. Hojhabrimanesh, A, Akhlaghi, M, Rahmani, E, Amanat, S, Atefi, M, Najafi, M, et al. A Western dietary pattern is associated with higher blood pressure in Iranian adolescents. Eur J Nutr. (2017) 56:399–408. doi: 10.1007/s00394-015-1090-z
29. Shang, X, Li, Y, Liu, A, Zhang, Q, Hu, X, Du, S, et al. Dietary pattern and its association with the prevalence of obesity and related cardiometabolic risk factors among Chinese children. PLOS ONE. (2012).
30. Naja, F, Shivappa, N, Nasreddine, L, Kharroubi, S, Itani, L, Hwalla, N, et al. Role of inflammation in the association between the western dietary pattern and metabolic syndrome among Lebanese adults. Int J Food Sci Nutr. (2017) 68:997–1004. doi: 10.1080/09637486.2017.1312297
31. Mattioli, AV, and Farinetti, A. Comment on “Western dietary pattern antioxidant intakes and oxidative stress: importance during the SARS-CoV-2/COVID-19 pandemic”. Adv Nutr. (2021) 12:1044–5. doi: 10.1093/advances/nmab029
32. Bouchard-Mercier, A, Rudkowska, I, Lemieux, S, Couture, P, and Vohl, M-C. The metabolic signature associated with the Western dietary pattern: a cross-sectional study. Nutr J. (2013) 12:1–9. doi: 10.1186/1475-2891-12-158
33. Kim, H, Rebholz, CM, Hegde, S, LaFiura, C, Raghavan, M, Lloyd, JF, et al. Plant-based diets, pescatarian diets and COVID-19 severity: a population-based case-control study in six countries. BMJ Nutr Prev Health. (2021) 4:257–66. doi: 10.1136/bmjnph-2021-000272
34. Greene, MW, Roberts, AP, and Frugé, AD. Negative association between Mediterranean diet adherence and COVID-19 cases and related deaths in Spain and 23 OECD countries: an ecological study. Front Nutr. (2021) 8:591964. doi: 10.3389/fnut.2021.591964
35. Zargarzadeh, N, Tadbir Vajargah, K, Ebrahimzadeh, A, Mousavi, SM, Khodaveisi, H, Akhgarjand, C, et al. Higher adherence to the Mediterranean dietary pattern is inversely associated with severity of COVID-19 and related symptoms: a cross-sectional study. Front Med (Lausanne). (2022) 9:911273. doi: 10.3389/fmed.2022.911273
36. Wallace, TC, Bailey, RL, Blumberg, JB, Burton-Freeman, B, Chen, CO, Crowe-White, KM, et al. Fruits, vegetables, and health: a comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit Rev Food Sci Nutr. (2020) 60:2174–211. doi: 10.1080/10408398.2019.1632258
37. Liu, RH . Dietary bioactive compounds and their health implications. J Food Sci. (2013) 78:A18–25. doi: 10.1111/1750-3841.12101
38. Arabzadegan, N, Daneshzad, E, Fatahi, S, Moosavian, SP, Surkan, PJ, and Azadbakht, L. Effects of dietary whole grain, fruit, and vegetables on weight and inflammatory biomarkers in overweight and obese women. Eat Weight Disord. (2020) 25:1243–51. doi: 10.1007/s40519-019-00757-x
39. Hosseini, B, Berthon, BS, Saedisomeolia, A, Starkey, MR, Collison, A, Wark, PA, et al. Effects of fruit and vegetable consumption on inflammatory biomarkers and immune cell populations: a systematic literature review and meta-analysis. Am J Clin Nutr. (2018) 108:136–55. doi: 10.1093/ajcn/nqy082
40. Gibson, A, Edgar, JD, Neville, CE, Gilchrist, SE, McKinley, MC, Patterson, CC, et al. Effect of fruit and vegetable consumption on immune function in older people: a randomized controlled trial. Am J Clin Nutr. (2012) 96:1429–36. doi: 10.3945/ajcn.112.039057
41. Izadi, V, Haghighatdoost, F, Moosavian, P, and Azadbakht, L. Effect of low-energy-dense diet rich in multiple functional foods on weight-loss maintenance, inflammation, and cardiovascular risk factors: a randomized controlled trial. J Am Coll Nutr. (2018) 37:399–405. doi: 10.1080/07315724.2017.1412275
42. Vu, T-HT, Rydland, KJ, Achenbach, CJ, Van Horn, L, and Cornelis, MC. Dietary behaviors and incident COVID-19 in the UK biobank. Nutrients. (2021) 13:2114. doi: 10.3390/nu13062114
43. Bousquet, J, Anto, JM, Iaccarino, G, Haahtela, T, and Zuberbier, T. Is diet partly responsible for differences in COVID-19 death rates between and within countries? BMC. (2020).
44. Lange, KW . Food science and COVID-19. Food Sci Human Wellness. (2021) 10:1–5. doi: 10.1016/j.fshw.2020.08.005
45. Chen, HWJ, Marzo, RR, Anton, H, Abdalqader, MA, Rajasekharan, V, Baobaid, MF, et al. Dietary habits, shopping behavior and weight gain during COVID-19 pandemic lockdown among students in a private university in Selangor, Malaysia. J Public Health Res. (2021) 10 jphr. 2021.921. doi: 10.4081/jphr.2021.2921
46. Sidor, A, and Rzymski, P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. (2020) 12:1657. doi: 10.3390/nu12061657
47. Hobbs-Grimmer, D, Givens, D, and Lovegrove, J. Associations between red meat, processed red meat and total red and processed red meat consumption, nutritional adequacy and markers of health and cardio-metabolic diseases in British adults: a cross-sectional analysis using data from UK National Diet and nutrition survey. Eur J Nutr. (2021) 60:2979–97. doi: 10.1007/s00394-021-02486-3
48. Linseisen, J, Rohrmann, S, Norat, T, Gonzalez, CA, Iraeta, MD, Gómez, PM, et al. Dietary intake of different types and characteristics of processed meat which might be associated with cancer risk–results from the 24-hour diet recalls in the European prospective investigation into Cancer and nutrition (EPIC). Public Health Nutr. (2006) 9:449–64. doi: 10.1079/PHN2005861
49. Linseisen, J, Kesse, E, Slimani, N, Bueno-De-Mesquita, H, Ocké, M, Skeie, G, et al. Meat consumption in the European prospective investigation into Cancer and nutrition (EPIC) cohorts: results from 24-hour dietary recalls. Public Health Nutr. (2002) 5:1243–58. doi: 10.1079/PHN2002402
Keywords: dietary pattern, weight, COVID-19, socioeconomic status, adults
Citation: Maharat M, Rahimlou M, Sioofi A, Sajjadi SF and Moosavian SP (2024) Association of major dietary patterns with socioeconomic status, obesity, and contracting COVID-19 among Iranian adults. Front. Nutr. 11:1301634. doi: 10.3389/fnut.2024.1301634
Edited by:
Xiaoyue (Luna) Xu, University of New South Wales, AustraliaReviewed by:
Elma Izze da Silva Magalhães, Federal University of Rio Grande do Sul, BrazilHana W. Jun Chen, Management and Science University, Malaysia
Copyright © 2024 Maharat, Rahimlou, Sioofi, Sajjadi and Moosavian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seyedeh Parisa Moosavian, cF9tb29zYXZpYW5AeWFob28uY29t
 Maryam Maharat1
Maryam Maharat1 Mehran Rahimlou
Mehran Rahimlou Seyedeh Forough Sajjadi
Seyedeh Forough Sajjadi Seyedeh Parisa Moosavian
Seyedeh Parisa Moosavian