- 1Department of Rehabilitation and Sport Medicine, Hannover Medical School, Hannover, Germany
- 2Department of Dermatology, Johannes Wesling Medical Centre, Minden, Germany
- 3Institute of Cell Biochemistry, Hannover Medical School, Hannover, Germany
- 4Institute of Medical Microbiology and Hospital Epidemiology, Hannover Medical School, Hannover, Germany
- 5German Center for Infection Research (DZIF), Partner-Site Hannover-Braunschweig, Hannover, Germany
- 6Institute for Laboratory Animal Science, Hannover Medical School, Hannover, Germany
- 7Hannover Rehabilitation Services and Science Consulting, Hannover, Germany
Fasting has been practiced with different time span in different areas of the world and for various reasons. One of the types of fasting regimens is Ramadan intermittent fasting (RIF), which is described as intermittent dry fasting and known as the most commonly practiced form of religious fasting. Different studies have shown its effects on body composition parameters and mental health, fatigue and quality of life (QoL). Elucidating the relationship of RIF on biological parameters would also be of importance to show its mechanism. Therefore, we evaluated several biological mediators related to mental health, such as ß-nerve growth factor (ß-NGF), brain-derived neurotrophic factor (BDNF), glial cell line-derived neurotrophic factor (GDNF), and insulin-like growth factor-1 (IGF-1), interleukin-8 (IL-8), tumor necrosis factor-α (TNF-α), and matrix-metalloproteinase-9 (MMP-9). This study consisted of fasting (FG; n = 25) and non-fasting group (NFG; n = 25). Four different time points were assessed for FG: one week before (T1), mid (T2), last days (T3), and one week after (T4) RIF. T1 and T3 were the assessment time points for NFG. Biological mediators were determined from serum samples by using Human Magnetic Luminex and enzyme-linked immunosorbent assay. Furthermore, we then performed correlation analyses between biological mediators and our previously published clinical parameters including body composition and mental health parameters at all time points. Significant alterations were shown in FG for ß-NGF (T2vsT3, p < 0.05; T2vsT4, p < 0.05), GDNF (T1vsT4, p < 0.05; T2vsT4, p < 0.05), IL-8 (T2vsT3, p < 0.05; T3vsT4, p < 0.05), TNF-α (T1vsT3, p < 0.05; T1vsT4, p < 0.001; T2vsT4, p < 0.001), and MMP-9 (T1vsT4, p < 0.01). There were no statistically significant differences between FG and NFG in all biological mediators at T1 and T3. Correlation analysis showed that MMP-9 levels had negative correlation with body mass index (BMI) at T3. At T3 BDNF levels had negative correlation with Epworth Sleepiness Scale (ESS) as one of measured QoL parameters. ß-NGF, GDNF, TNF-α, and MMP-9 had positive correlation with some of body composition and mental health parameters. Findings demonstrate that RIF altered different biological mediators could give benefit to health. Its benefit is mediated by the alteration of biological mediators.
Introduction
Intermittent fasting (IF) has become a lifestyle of eating during specific period of time and fasting for the rest of the day. IF has shown many of the health benefits. It is not only reducing free-radical production and weight loss, but also the adaptive cellular responses between and within organs that restores glucose metabolism, increases stress resistance and suppresses inflammation (1). Previous studies showed the positive effect of IF in animal models on chronic disorders such as obesity, diabetes, cardiovascular disease, cancer and neurological disorders (2, 3). Ramadan intermittent fasting (RIF) is one type of IF that performed by about 1.5 billions of Muslims worldwide annually from dawn to sunset for one month. The time periods of RIF vary from 9 to 22 h per day due to geographical differences and seasonal variation (4). Food, water, smoking and sexual activities are forbidden during the fasting daytime hours of Ramadan month. Our previous studies demonstrated that not only RIF can improve anthropometric parameters, but also can improve mental health, fatigue and quality of life (QoL) (5). However, the physiological mechanism behind these beneficial effects need to be elucidated.
Depression is related to irregularities in hypothalamic–pituitary–adrenal (HPA) axis, altered insulin resistance, plasma glucose, pro-inflammatory cytokines, leptin resistance, and disturbance of neurotransmitters, neuropeptides and neurotrophic factors (6, 7). Interestingly, several studies demonstrated that IF has positive effects on the neuroendocrine system and on depression. IF might induce an antidepressant effect on depression, providing potential new treatment options. It included neurotrophic effects and orexin signaling activation that can release endorphin and ketone via the increased of cAMP response element-binding (CREB) phosphorylation (8). Hence, it is of interest to study the effect of IF on biological mediators related to depression, particularly on neurotrophic factors.
Nerve growth factor (NGF) was the first member described among the neurotrophic factors (9). NGF has been known to involve in the regulation of neurotransmitters and neuropeptides synthesis of nerve cells. It is important for growth, maintenance, proliferation and survival of nerve cells (10). Various clinical studies in human and animals showed an association of low NGF levels with depression compared with healthy controls (11). Brain-derived neurotrophic factor (BDNF), another member of neurotrophic factors, was described as being involved in synaptic plasticity (12), depression (8), and increasing survival of dopaminergic neurons of the developing substantia nigra (13). BDNF has been also studied in different neurological-related diseases, such as major depressive disorders, fibromyalgia syndromes and chronic low back pain (14). Glial cell-derived neurotrophic factor (GDNF) is a small protein and member of neurotrophic factors that are responsible for the development, maintenance and survival of different neurons (15). In mice model, induced GDNF-expression showed protective effects to obesity. In addition, several studies showed that GDNF is known to the mechanism underlying depressive disorders (16).
Other biological mediators related to depression and body composition parameters such as insulin growth factor-1 (IGF-1), tumor necrosis factor alpha (TNF-α), interleukin-8 (IL-8), and matrix metalloproteinase-9 (MMP-9) were also determined (17–19). One of the biological mechanisms for depression is related to inflammation. People with major depressive disorder (MDD) and obesity have been shown to have higher inflammatory markers as compared to healthy control (20–22). IGF-1 has been shown to have anti-inflammatory action by inhibiting the expression of proinflammatory cytokines including IFN-γ, IL-1β and TNF-α and enhancing the production of anti-inflammatory cytokines including IL-4 and IL-10 (23). The abnormalities of IGF-1 in MDD patients have been suggested as a marker and predictive role of the neurotrophin for depression and treatment effectiveness (24). Meanwhile, individuals who had increased level of both pro-inflammatory cytokine tumor necrosis factor-alpha (TNF-α) and interleukin 8 (IL-8) have been reported to develop psychiatric disorders such as major depression, bipolar disorder, schizophrenia and sleep disorder (25, 26). Other study showed that depression condition in young patient, levels of serum MMP-9 were increased which might be used as biomarker for bipolar disorder (27). Another study also showed that patients in acute phase of ischemic stroke condition, serum MMP-9 levels were elevated (28). In addition, animal were treated with MMP-9 inhibitor showed improve specific neurobehavioral deficits associated with Alzheimer’s disease (29).
As mentioned before, neurotrophic factors play a role not only related to depressive disorders, but also to body composition parameters. Therefore, this study was an explorative study that aimed at elucidating the changes in neurotrophic factors upon the observation of RIF. Additionally, we aimed to measure the inflammatory cytokine TNF-α, the chemokine IL-8 and MMP-9. Furthermore, in our previous study showed that RIF improved body composition and mental health parameters, fatigue and QoL (5). For the body composition parameters, we measured body weight (BW), body mass index (BMI), skeletal muscle mass (SMM), body fat mass (BFM), fat free mass (FFM), body fat percentage (BFP), body water mass (BWM) and wait and hip ratio (WHR). For mental health parameters, we determined the effects on fatigue [Fatigue Severity Scale (FSS) and visual analogue scale (VAS)], depression (The Hospital Anxiety and Depression Score (HADS) and Beck’s Depression Inventory (BDI)-II) and QoL [Epworth Sleepiness Scale (ESS)] (5). In this study, we aimed to analyze the correlation between measured biological mediators with our previously published clinical parameters including body composition and mental health parameters at all time points.
Materials and methods
Local Ethic Committee of Hannover Medical School approved this study (Ethics No. 6899) in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. This study registered at German Registry of Clinical Trial (DRKS-ID: DRKS00008181). Written informed consent was obtained from all subjects and/or their legal guardian(s).
Participants
This study was a sub analysis from previous report (5). Healthy male participants which mostly students of Hannover Medical School were recruited. We divided them into two groups fasting group (FG) and non-fasting group (NFG). The health status of participants were assessed by experienced doctors at Department of Rehabilitation and Sport Medicine, Hannover Medical School. Study inclusion for FG required a minimum age of 18 years old, intended to fast the whole month of Ramadan, have fasted during Ramadan at least once before, understood German or English language. Study inclusion for NFG required a minimum age of 18 years old and did not fast during the study period.
Study design
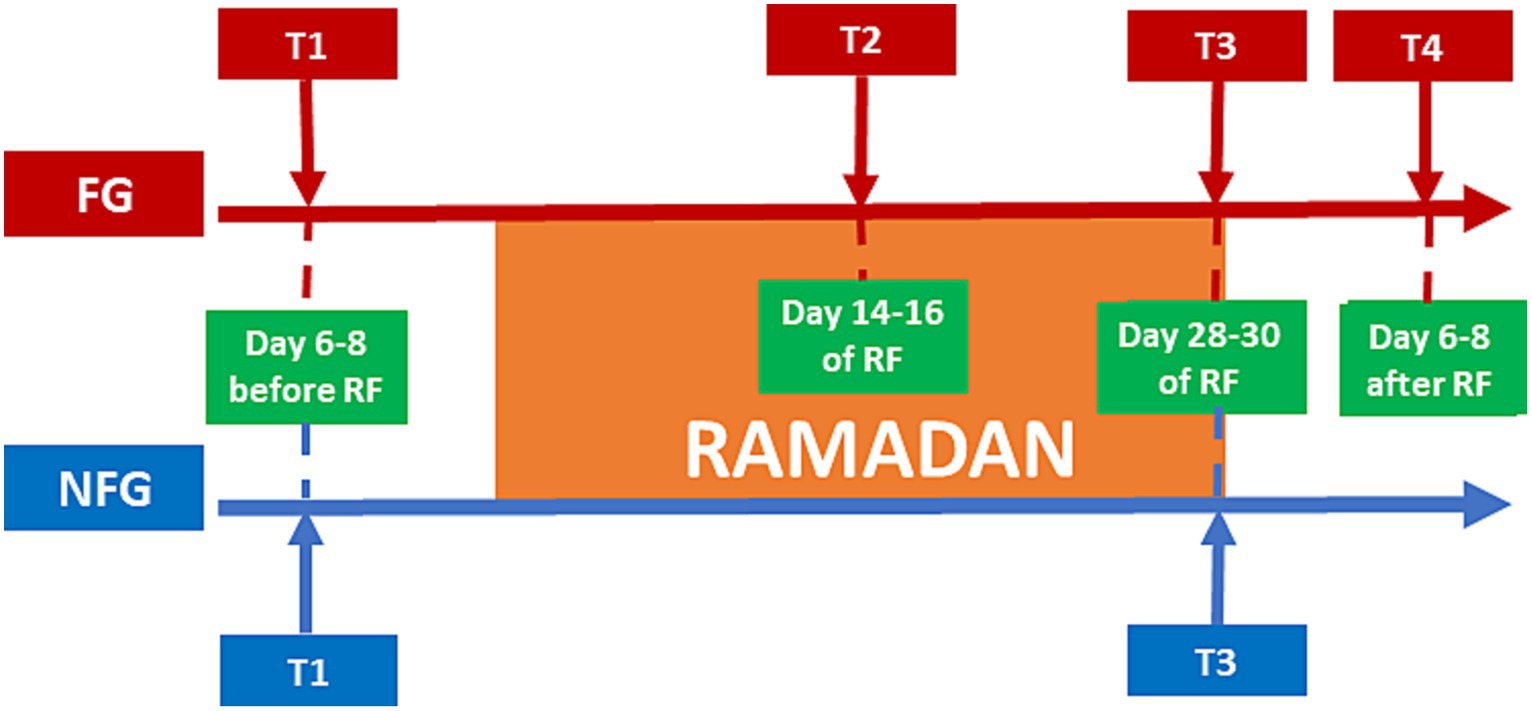
In this current study, the fasting period was about 18–19 h per day. In the FG, subjects were assessed at four time points (Figure 1): one week before the beginning of Ramadan/baseline (T1); middle of Ramadan (T2: day 14th or 15th or 16th); the last days of Ramadan (T3: day 28th or 29th or 30th); and one week after the Ramadan fasting finished (T4: day 6th, 7th, 8th from the end of Ramadan).
In the NFG, subjects were assessed only at 2 time points: before Ramadan (T1) and during the last days of Ramadan (T3).
Serum preparation
Serum was prepared by collecting blood samples from peripheral venous by using Monovette serum tube (Monovette®, Sarstedt, Germany). It was done in the morning time between 08:00 and 10:00 for all time points. Centrifugation was performed after allowing blood clotting at 1500 g for 15 min (Universal 320R, Hettich, Tuttlingen, Germany). These serum samples were stored at −80°C until determination.
ß-NGF, BDNF, GDNF, TNF-α, IL8 and MMP-9 serum level were determined using customized Human Magnetic Luminex Assay (R&D Systems) according to the manufacturer’s instructions. IGF-1 serum levels were determined using Quantikine ELISA Human IGF-1 Immunoassay (R&D Systems Inc.) according to the manufacturer’s instructions.
Body composition and mental health parameters
As discussed above, body composition and mental health parameters have been published in our previous publication (5). We determined the body composition parameters including body weight (BW), body mass index (BMI), skeletal muscle mass (SMM), body fat mass (BFM), fat free mass (FFM), body fat percentage (BFP), body water mass (BWM) and wait and hip ratio (WHR) by using InBody 230 (Model MW160, InBody Co., Ltd., Seoul, Korea). Mental health parameters, fatigue and QoL were assessed by using self-administered questionnaires. The Hospital Depression and Anxiety Score (HADS) and Beck’s Depression Inventory (BDI)-II were used to assess the intensity of anxiety and depression or only depression, respectively. Fatigue was measured by the visual analogue scale (VAS) and fatigue severity scale (FSS). Day sleepiness as QoL parameter was measured by using the Epworth Sleepiness Scale (ESS). In this study, we only showed mental health parameters that have correlation with measured biological mediators (ESS, HADSA, HADSD, BDI-II).
Statistics analysis
The aim of this study is to assess the level of ß-NGF, BDNF, GDNF, IGF-1, IL-8, TNF-α, and MMP-9 before (T1), during (T2 and T3) and after (T4) RIF. Kruskal-Wallis or two-way Friedman ranked test were used to analyze the data, after we tested the data distribution using the Kolmogorov–Smirnov test. We performed the post hoc tests, and Bonferroni correction were used to adjust the significances. We used Spearman’s correlation tests to determine correlation between clinical parameters and biological mediators. Missing data were replaced by using a mean. Statistical analysis was performed by using SPSS version 22 (IBM, New York, United States).
Results
Baseline characteristics of FG and NFG
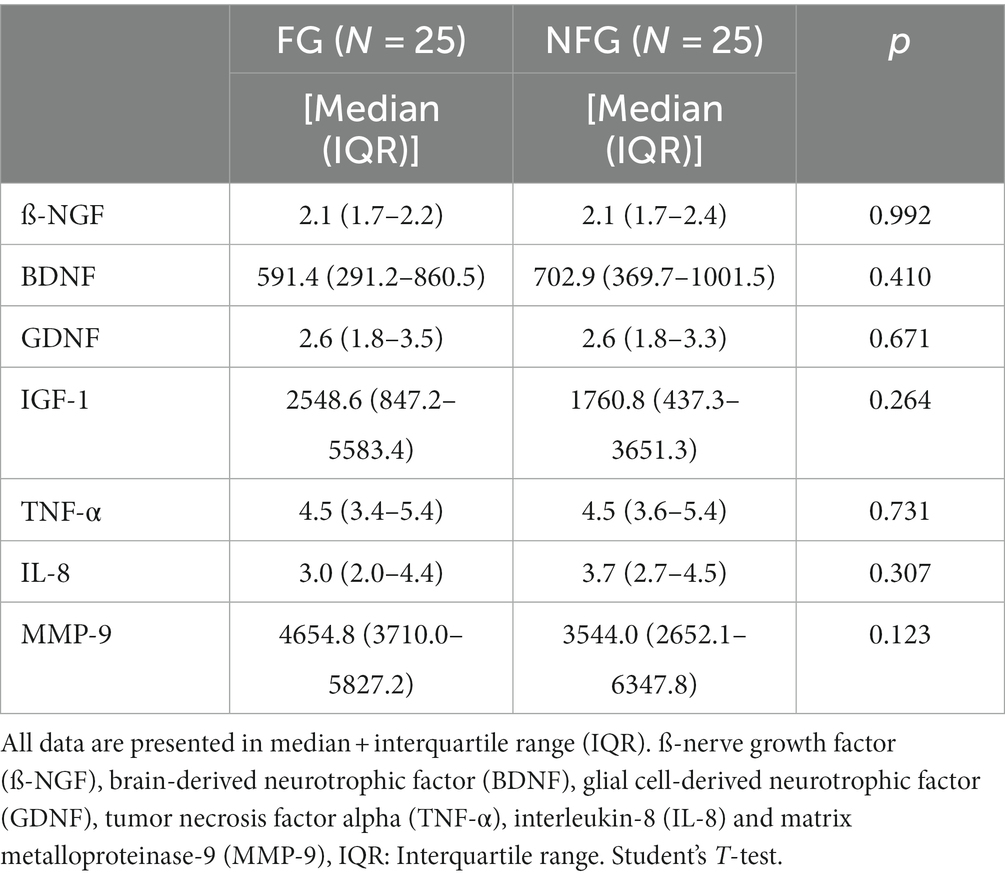
Table 1 shows the baseline data of FG and NFG regarding anthropometric measurements and mental health parameters of both groups that were measured from our previous publication (5). This data demonstrated that there were no statistically significant differences at baseline between FG and NFG. Table 2 shows the baseline data of FG and NFG regarding biological mediators measured in this study. There were no statistically significant differences at baseline between FG and NFG.
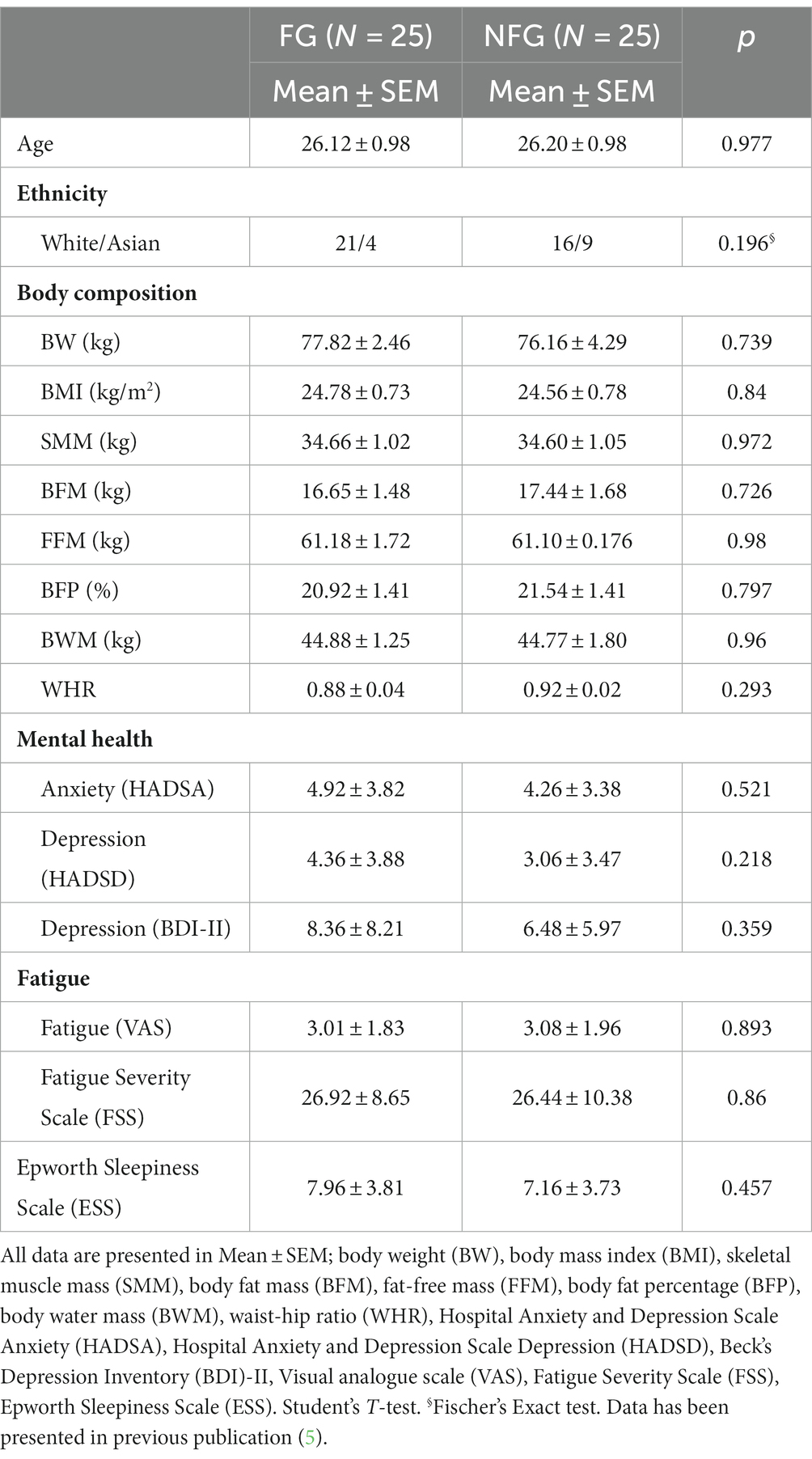
Table 1. Baseline data of fasting and non-fasting group (Body composition and mental health parameters).
Effect of RIF on neurotrophic factors
In this study, both ß-NGF and GDNF showed significant changes during RIF in FG only (Figures 2A,C). ß-NGF levels showed significant increased from the middle of Ramadan (T2) to the last days of Ramadan (T3) and one week after the RIF finished (T4). Whereas GDNF levels showed significant decreased from one week before the beginning of Ramadan/baseline (T1) to T4, but also significant decreased from T2 to T4. Furthermore, BDNF and IGF-1 levels showed no significant changes in FG during the study period (Figures 2B,D). In addition, we observed no statistically significant differences between FG and NFG in ß-NGF, BDNF, GDNF and IGF-1 levels from 1 week before RIF (T1) to the last week of RIF (T3) (Figures 3A–D).
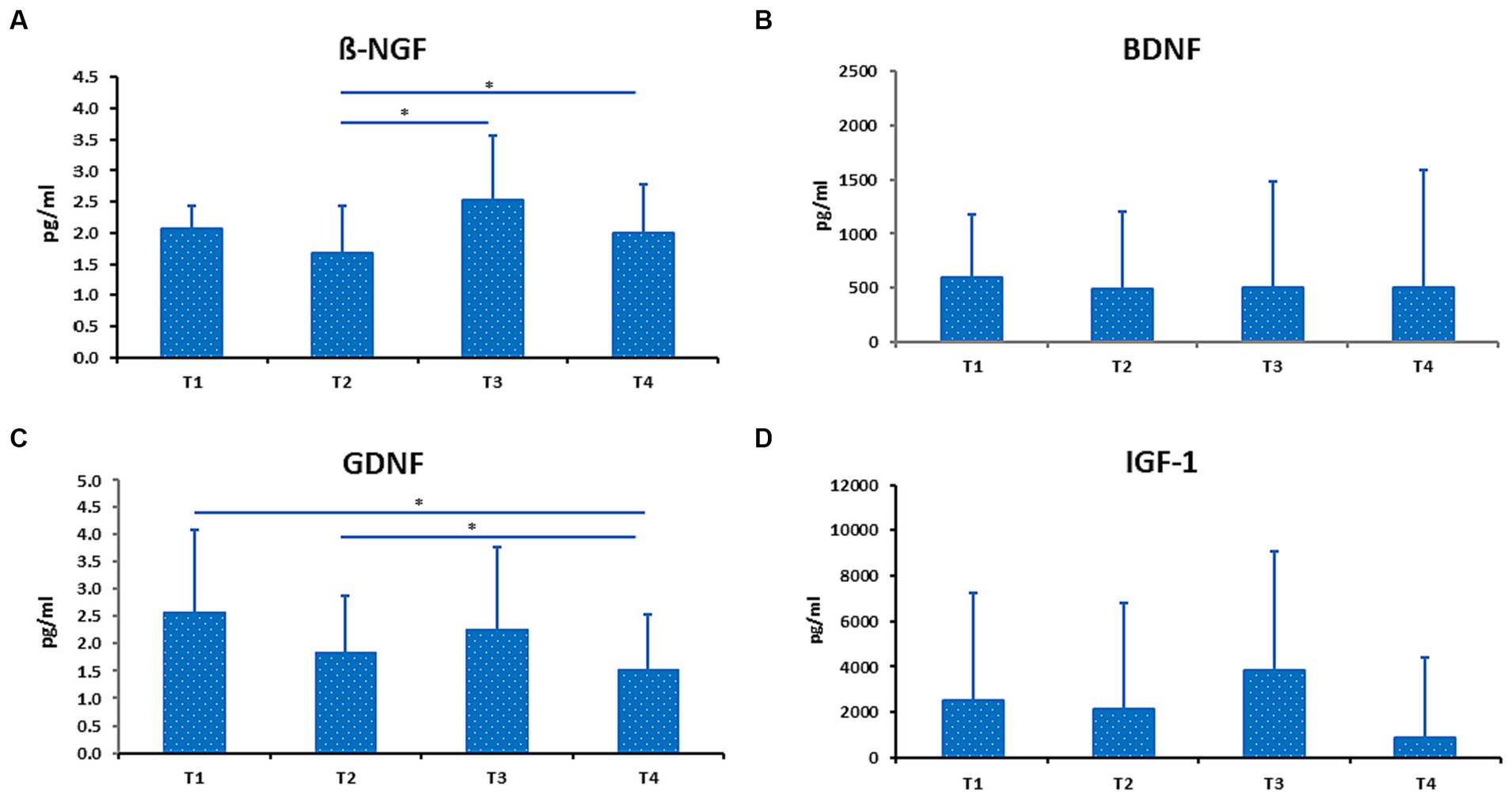
Figure 2. Level of ß-NGF (A), BDNF (B), GDNF (C), and IGF-1 (D) in fasting group (FG). Data presented as median + interquartile range (IQR). * p < 0.05.
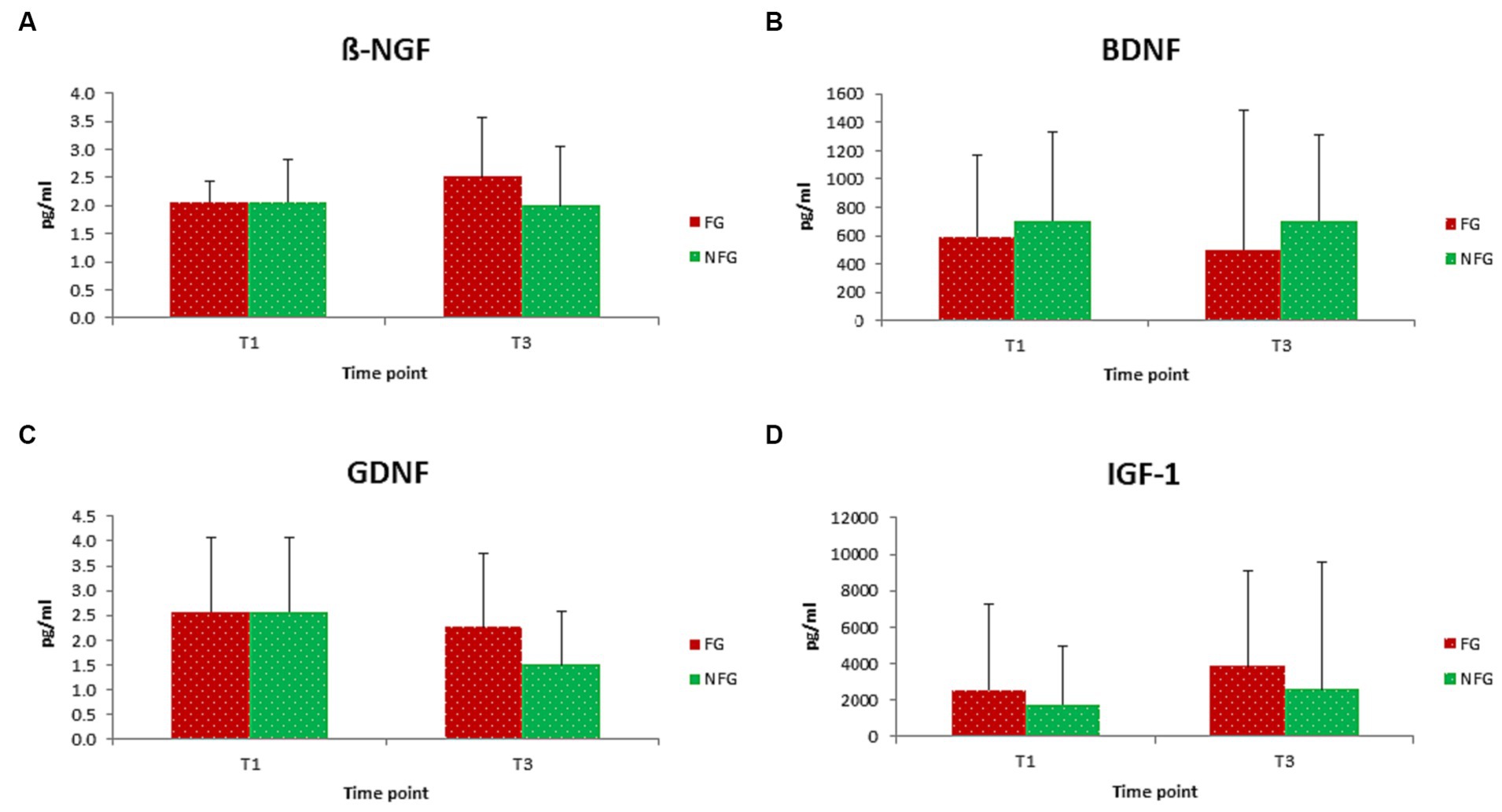
Figure 3. Level of ß-NGF (A), BDNF (B), GDNF (C), and IGF-1 (D) in fasting (FG) and non-fasting group (NFG) at T1 and T3. Data presented as median + interquartile range (IQR).
Effect of RIF on IL-8, TNF-a, and MMP-9
In this study, we measured TNF-α and IL-8 levels during IF in healthy male participants in order to determine the effect of RIF on cytokines and chemokines levels. TNF-α levels were significantly decreased from T1 to T3 and T4. TNF-α levels were also decreased from T2 to T4 (Figure 4A). We also observed decreased levels of IL-8 from T3 to T4, although IL-8 levels were increased from T2 to T3 (Figure 4B).
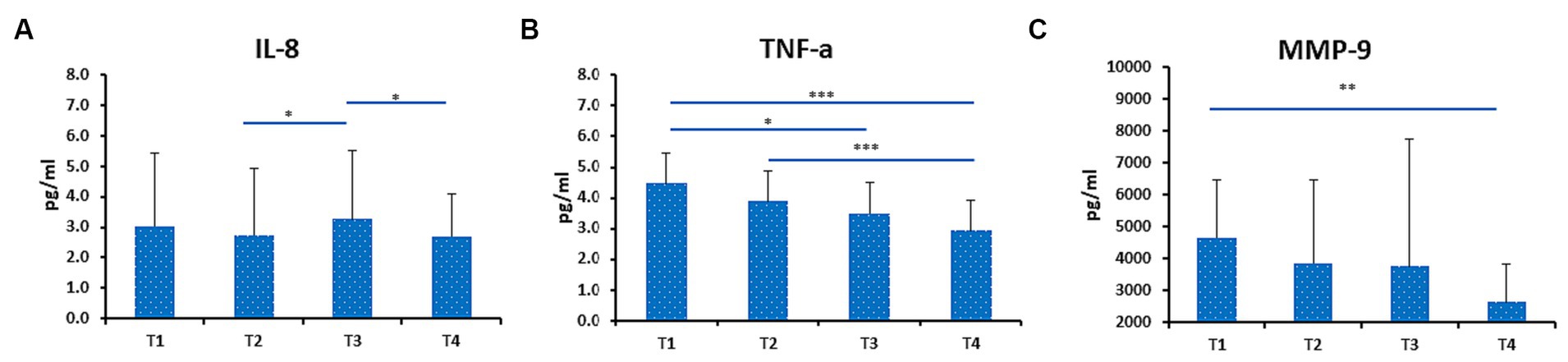
Figure 4. Level of IL-8 (A), TNF-a (B) and MMP-9 (C) in fasting group (FG). Data presented as median + interquartile range (IQR). Data presented as median + interquartile range (IQR). * p < 0.05; ** p < 0.01; ***p < 0.001.
Furthermore, we measured MMP-9 levels that play an important role in obesity-mediated adipose tissue remodeling. Interestingly, we found that MMP-9 was significant decreased from T1 to T4 in FG (Figure 4C). In addition, we compared the levels of IL-8, TNF-α, and MMP-9 levels of both FG and NFG. No statistically significant differences in IL-8, TNF-α, and MMP-9 were observed at T1 and T3 between FG and NFG (Figures 5A–C). Surprisingly, the TNF-α levels were significantly decreased at T1 and T3 of NFG (Figure 5B).
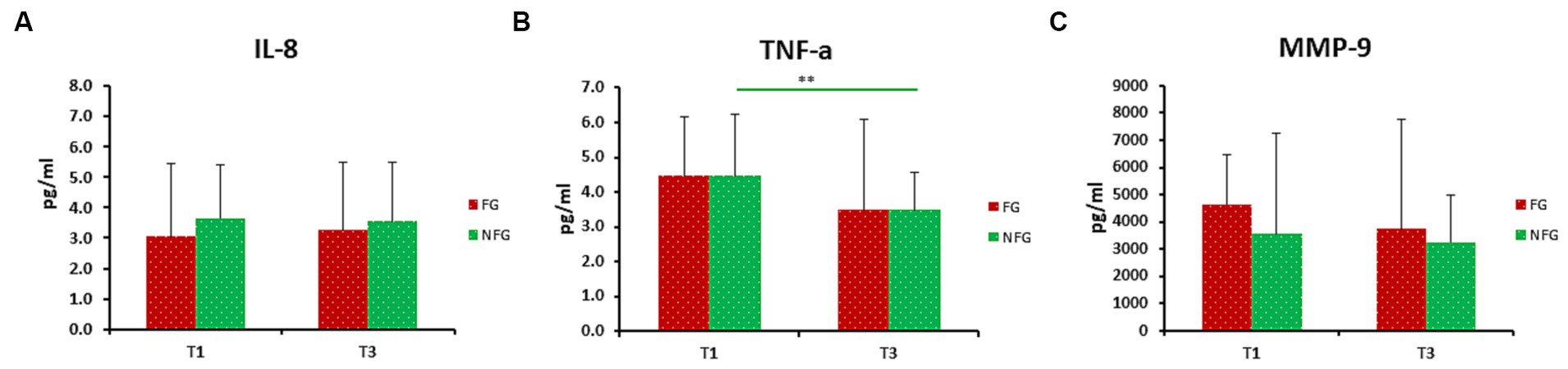
Figure 5. Level of IL-8 (A), TNF-α (B), and MMP-9 (C) in fasting (FG) and non-fasting group (NFG) at T1 and T3. Data presented as median + interquartile range (IQR). ** p < 0.01.
Correlations between biological mediators and clinical parameters during RIF
It is of interest to analyze the correlation between clinical parameters and biological mediators (Table 3). In the last days of Ramadan (T3), MMP-9 levels showed a negative correlation with body mass index (BMI). BDNF levels showed negative correlation with Epworth Sleepiness Scale (ESS). Interestingly, TNF-α levels showed positive correlation with Hospital Anxiety and Depression Scale-Anxiety (HADSA) and Hospital Anxiety and Depression Scale–Depression (HADSD). Meanwhile, GDNF and MMP-9 levels showed positive correlation with HADSD.
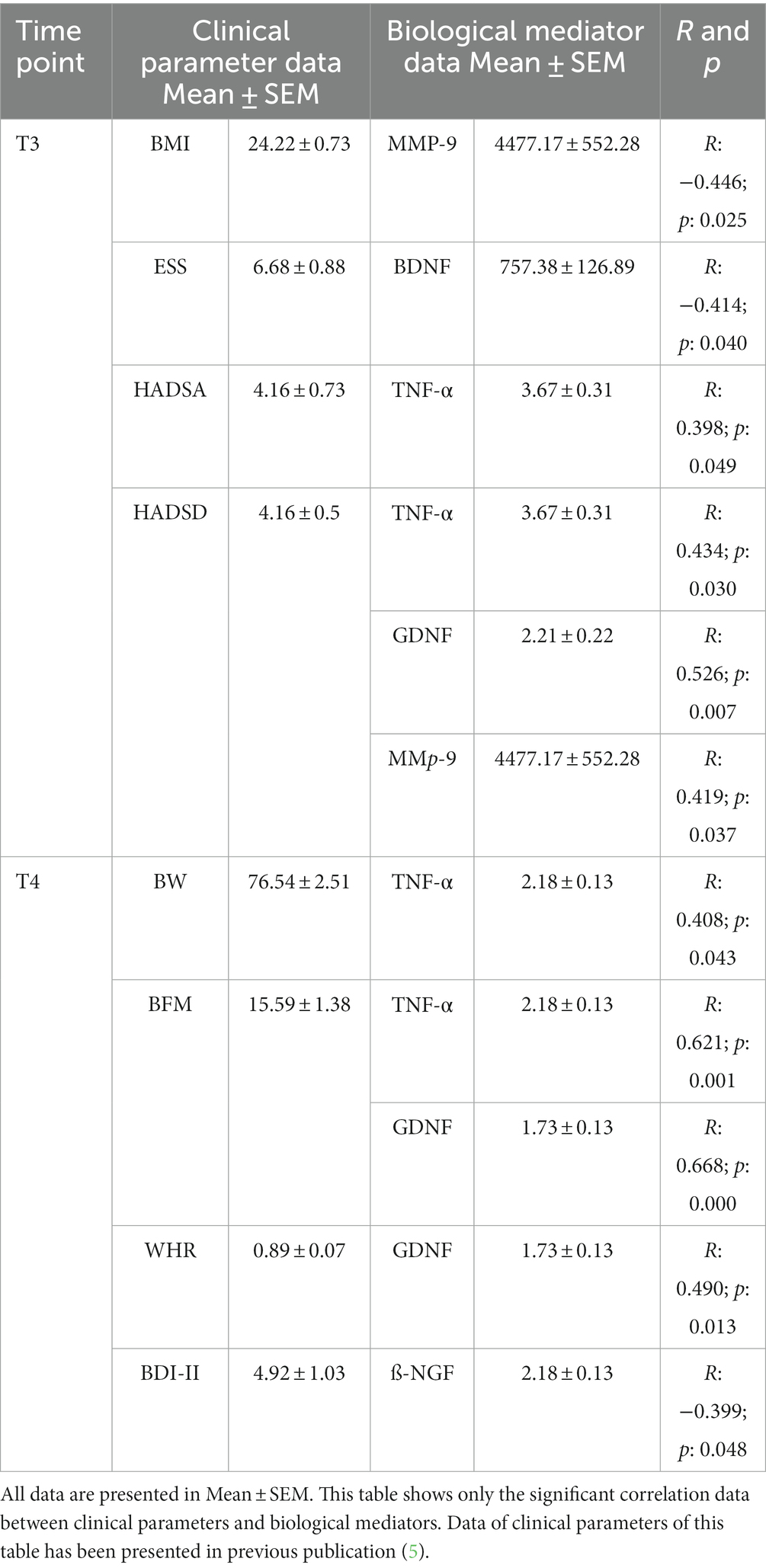
Table 3. Correlation between clinical parameters and biological mediators during RIF in fasting group (N = 25).
We observed positive correlations of TNF-α to body weight (BW) and body fat mass (BFM) at one week after the RIF finished (T4). GDNF levels had positive correlation with BFM and waist-hip-Ratio (WHR). Interestingly, Beck’s depression inventory (BDI)-II, as depression parameter, showed negative correlation with ß-NGF levels.
Discussion
The most understanding by common people, the effect of IF is related to the alteration of anthropometric parameters, which include BMI, body weight, and fat loss (5, 30–32). Interestingly, our previous studies, RIF has a positive influence to mental health, fatigue and QoL (5, 30). This effect might be mediated by different biological mediators, particularly cortisol and BDNF (33). Another study also observed that RIF improved body composition and did not exacerbate depression in MDD patients (34). In this current study, we wanted to elucidate the effects of RIF at different time points on neurotrophic factors such as ß-NGF, GDNF, BDNF and IGF-1. Additionally, we also measured other biological mediators such as TNF-α, IL-8 and MMP-9.
In our current study, ß-NGF showed significant increase from the middle of Ramadan (T2) to the last days of Ramadan (T3) and one week after the RIF finished (T4). A comparable study measuring NGF during RIF in woman only participants also showed significant increase of NGF during mid and end of RIF (35). It is known that NGF has an important role in the regulation of neurotransmitters and neuropeptides synthesis of nerve cells (10), but there is no previous evidence on the effect of fasting on NGF levels and it effects to improve brain health through the induction of the NGF levels. Interestingly, Beck’s depression inventory (BDI)-II showed negative correlation with ß-NGF levels. A meta-analysis and systematic review observed that NGF levels were significantly lower in MDD than in healthy control (36).
Furthermore, we observed significantly decreased levels of GDNF from one week before the beginning of Ramadan/baseline (T1) to T4, and significantly decreased levels from T2 to T4. Interestingly, GDNF levels has a positive correlation with HADSD at T3 and BFM and WHR at T4. GDNF levels were shown to be significantly decreased in depression (37) involved in the dopamine system and has been linked to a potential treatment in drug abuse (38). Concerning special psychiatric conditions and its correlation to metabolic levels, a study by Skibinska et al. (39) showed that in psychiatric disorders, such as depression, GDNF and metabolic features such as cholesterol, showed significant correlation between GDNF and cholesterol GDNF. Transgenic mice showed higher brown fat mass, energy expenditure and even increased expression in skeletal muscle. Nevertheless, GDNF does not appear as a predictor for treatment remission in other psychiatric disorders, such as general anxiety disorder (40). However, the findings towards GDNF and its (patho) physiological role remain controversial and further studies need to elucidate the role of GDNF. Best to our knowledge, this study is the first study to analyze the effect of fasting on GDNF.
RIF associated with the decrease of BDNF levels in schizophrenia patients (41). Furthermore, an increased BDNF level was linked to type II diabetes mellitus (T2DM) and obesity (42). A study using rats suggested that IF could potentially protect from T2DM by increasing the levels of BDNF and neurotrophin (NT)3 (43). Interestingly, contradictory results were obtained regarding BDNF levels during RIF in healthy participants. Some studies showed a significant increase of BDNF levels during RIF (35). Whereas another study showed a decrease of BDNF levels during RIF (44). These conflicting reports regarding how IF influence BDNF levels might be because of the different time periods of RIF due to geographical differences and seasonal variations. Different time point of collecting the samples also might resulting the differences. Meanwhile, our previous study showed significantly decreased (33), it could be that the latter study include both male and female participants.
Concerning to insignificant changes of IGF-1-levels during RIF, our results were in line with another study conducted on well trained men during RIF (45), although we cannot compare directly with subjects of this study. In contrast to these findings another study showed significant reduction of IGF-1 levels during RIF by adaptation mechanisms. As shown in mice model, it was hypothesized that short time starvation leads to survival mode and reduction of the growth hormone IGF-1 (46). Reduced IGF-1 levels were linked to extended life span in mice (47).
Limitation
This study only evaluated the effect of RIF on healthy young males. Therefore, the results could be different in different sex, range of ages (younger/older) and health conditions. We did not include female participants, because they might not fast for the whole of Ramadan due to menstruation. During menstruation periods, females are not obligated to do fasting. It could alter the results. However, we included female participants in other fasting study, although we did not measure similar markers (33). Many biological parameters are quite sensitive to dietary consumption (48–51). Controlling food intake in all participants could lead to better understanding physiological mechanism. However, it could not be done as participants had different cultures, habits and preferences. Otherwise, recording food intake during the study should be done in the future. Assessment of NFG were performed only at T1 and T3, as we hypothesized that NFG would not show any changes during T2 and T4. Main focus of this study, among others, is the difference of FG between before fasting (T1) and the last days of the fasting period (T3). However, we agree that it should be done at all time points for future study.
In summary, RIF as a model of IF could give benefit to health in particular related to mental health and anthropometric parameters. Its benefit is mediated by the alteration of biological parameters, especially neurotrophic factors and cytokines.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethic Committee of Hannover Medical School (ethics no. 6899; registration code of trial: DRKS00008181). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SG: Data curation, Investigation, Project administration, Writing – original draft, Writing – review & editing. AS: Data curation, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. MB: Data curation, Investigation, Methodology, Software, Writing – review & editing. IH: Data curation, Investigation, Project administration, Writing – review & editing. GG: Funding acquisition, Resources, Writing – review & editing. CG: Funding acquisition, Resources, Writing – review & editing. BN: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Department of Rehabilitation Medicine, Hannover Medical School, 30625 Hannover, Germany; Institute of Medical Microbiology and Hospital Epidemiology, Hannover Medical School and German Center for Infection Research (DZIF), 30625 Hannover, Germany; and Institute of Cell Biochemistry, Hannover Medical School, 30625 Hannover, Germany. It was without external funding.
Conflict of interest
BN and CG are employed by Hannover Rehabilitation Services and Science Consulting.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. de Cabo, R , and Mattson, MP . Effects of intermittent fasting on health, aging, and disease. N Engl J Med. (2019) 381:2541–51. doi: 10.1056/NEJMra1905136
2. Mattison, JA , Colman, RJ , Beasley, TM , Allison, DB , Kemnitz, JW , Roth, GS, et al. Caloric restriction improves health and survival of rhesus monkeys. Nat Commun. (2017) 8:14063. doi: 10.1038/ncomms14063
3. Di Francesco, A , Di Germanio, C , Bernier, M , and de Cabo, R . A time to fast. Science. (2018) 362:770–5. doi: 10.1126/science.aau2095
4. Bello, AK , Kurzawa, J , Osman, MA , Olah, ME , Lloyd, A , Wiebe, N, et al. Impact of Ramadan fasting on kidney function and related outcomes in patients with chronic kidney disease: a systematic review protocol. BMJ Open. (2019) 9:e022710. doi: 10.1136/bmjopen-2018-022710
5. Nugraha, B , Ghashang, SK , Hamdan, I , and Gutenbrunner, C . Effect of Ramadan fasting on fatigue, mood, sleepiness, and health-related quality of life of healthy young men in summer time in Germany: a prospective controlled study. Appetite. (2017) 111:38–45. doi: 10.1016/j.appet.2016.12.030
6. Nestler, EJ , Barrot, M , DiLeone, RJ , Eisch, AJ , Gold, SJ , and Monteggia, LM . Neurobiology of depression. Neuron. (2002) 34:13–25. doi: 10.1016/S0896-6273(02)00653-0
7. Fu, X , Wang, Y , Zhao, F , Cui, R , Xie, W , Liu, Q, et al. Shared biological mechanisms of depression and obesity: focus on adipokines and lipokines. Aging (Albany NY). (2023) 15:5917–50. doi: 10.18632/aging.204847
8. Zhang, Y , Liu, C , Zhao, Y , Zhang, X , Li, B , and Cui, R . The effects of calorie restriction in depression and potential mechanisms. Curr Neuropharmacol. (2015) 13:536–42. doi: 10.2174/1570159X13666150326003852
9. Lewin, GR , and Barde, Y-A . Physiology of the Neurotrophins. Annu Rev Neurosci. (1996) 19:289–317. doi: 10.1146/annurev.ne.19.030196.001445
10. Levi-Montalcini, R , Toso, RD , della Valle, F , Skaper, SD , and Leon, A . Update of the NGF saga. J Neurol Sci. (1995) 130:119–27. doi: 10.1016/0022-510X(95)00007-O
11. Mondal, AC , and Fatima, M . Direct and indirect evidences of BDNF and NGF as key modulators in depression: role of antidepressants treatment. Int J Neurosci. (2019) 129:283–96. doi: 10.1080/00207454.2018.1527328
12. Yang, T , Nie, Z , Shu, H , Kuang, Y , Chen, X , Cheng, J, et al. The role of BDNF on neural plasticity in depression. Front Cell Neurosci. (2020) 14:82. doi: 10.3389/fncel.2020.00082
13. Hyman, C , Hofer, M , Barde, Y-A , Juhasz, M , Yancopoulos, GD , Squinto, SP, et al. BDNF is a neurotrophic factor for dopaminergic neurons of the substantia nigra. Nature. (1991) 350:230–2. doi: 10.1038/350230a0
14. Dimmek, DJ , Korallus, C , Buyny, S , Christoph, G , Lichtinghagen, R , Jacobs, R, et al. Brain-derived neurotrophic factor and immune cells in osteoarthritis, chronic low Back pain, and chronic widespread pain patients: association with anxiety and depression. Medicina (Kaunas). (2021) 57:327. doi: 10.3390/medicina57040327
15. Saarma, M , and Sariola, H . Other neurotrophic factors: glial cell line-derived neurotrophic factor (GDNF). Microsc Res Tech. (1999) 45:292–302. doi: 10.1002/(SICI)1097-0029(19990515/01)45:4/5<292::AID-JEMT13>3.0.CO;2-8
16. Tsybko, AS , Ilchibaeva, TV , and Popova, NK . Role of glial cell line-derived neurotrophic factor in the pathogenesis and treatment of mood disorders. Rev Neurosci. (2017) 28:219–33. doi: 10.1515/revneuro-2016-0063
17. Faris, MA , Kacimi, S , Al-Kurd, RA , Fararjeh, MA , Bustanji, YK , Mohammad, MK, et al. Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutr Res. (2012) 32:947–55. doi: 10.1016/j.nutres.2012.06.021
18. Faris, MA-IE , Jahrami, HA , Obaideen, AA , and Madkour, MI . Impact of diurnal intermittent fasting during Ramadan on inflammatory and oxidative stress markers in healthy people: systematic review and meta-analysis. Journal of Nutrition & Intermediary. Metabolism. (2019) 15:18–26. doi: 10.1016/j.jnim.2018.11.005
19. MAE, F , Madkour, MI , Obaideen, AK , Dalah, EZ , Hasan, HA , Radwan, H, et al. Effect of Ramadan diurnal fasting on visceral adiposity and serum adipokines in overweight and obese individuals. Diabetes Res Clin Pract. (2019) 153:166–75. doi: 10.1016/j.diabres.2019.05.023
20. Chae, WR , Nübel, J , Baumert, J , Gold, SM , and Otte, C . Association of depression and obesity with C-reactive protein in Germany: a large nationally representative study. Brain Behav Immun. (2022) 103:223–31. doi: 10.1016/j.bbi.2022.04.024
21. Zeng, Y , Sun, B , Zhang, F , Hu, Z , Li, W , Lan, X, et al. The core inflammatory factors in patients with major depressive disorder: a network analysis. Front Psych. (2023) 14:1216583. doi: 10.3389/fpsyt.2023.1216583
22. Milano, W , Ambrosio, P , Carizzone, F , De Biasio, V , Di Munzio, W , Foia, MG, et al. Depression and obesity: analysis of common biomarkers. Diseases. (2020) 8:23. doi: 10.3390/diseases8020023
23. Szczęsny, E , Slusarczyk, J , Głombik, K , Budziszewska, B , Kubera, M , Lasoń, W, et al. Possible contribution of IGF-1 to depressive disorder. Pharmacol Rep. (2013) 65:1622–31. doi: 10.1016/s1734-1140(13)71523-8
24. Levada, OA , and Troyan, AS . Insulin-like growth factor-1: a possible marker for emotional and cognitive disturbances, and treatment effectiveness in major depressive disorder. Ann General Psychiatry. (2017) 16:38. doi: 10.1186/s12991-017-0161-3
25. Tsai, S-J . Role of interleukin 8 in depression and other psychiatric disorders. Prog Neuro-Psychopharmacol Biol Psychiatry. (2021) 106:110173. doi: 10.1016/j.pnpbp.2020.110173
26. Berthold-Losleben, M , and Himmerich, H . The TNF-α system: functional aspects in depression, narcolepsy and psychopharmacology. Curr Neuropharmacol. (2008) 6:193–202. doi: 10.2174/157015908785777238
27. Rybakowski, JK , Remlinger-Molenda, A , Czech-Kucharska, A , Wojcicka, M , Michalak, M , and Losy, J . Increased serum matrix metalloproteinase-9 (MMP-9) levels in young patients during bipolar depression. J Affect Disord. (2013) 146:286–9. doi: 10.1016/j.jad.2012.07.019
28. Che, B , Zhong, C , Ge, J , Li, R , Zhu, Z , Bu, X, et al. Serum matrix Metalloproteinase-9 is associated with depression after acute ischemic stroke. Circ J. (2019) advpub) 83:2303–11. doi: 10.1253/circj.CJ-19-0376
29. Ringland, C , Schweig, JE , Eisenbaum, M , Paris, D , Ait-Ghezala, G , Mullan, M, et al. MMP9 modulation improves specific neurobehavioral deficits in a mouse model of Alzheimer’s disease. BMC Neurosci. (2021) 22:39. doi: 10.1186/s12868-021-00643-2
30. Nugraha, B , Riat, A , Ghashang, SK , Eljurnazi, L , and Gutenbrunner, C . A prospective clinical trial of prolonged fasting in healthy young males and females-effect on fatigue, sleepiness, mood and body composition. Nutrients. (2020) 12:E2281. doi: 10.3390/nu12082281
31. Das, A , Hasmat, N , Kumar Ghosh, S , and Sahu, S . Effects of Ramadan intermittent fasting and pattern of nutrients intake on BMI and MUAC of a population consisting of Indian Muslims. Biol Rhythm Res. (2021) 52:1260–9. doi: 10.1080/09291016.2019.1700328
32. Jahrami, HA , Alsibai, J , Clark, CCT , and Faris, MA-IE . A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur J Nutr. (2020) 59:2291–316. doi: 10.1007/s00394-020-02216-1
33. Riat, A , Suwandi, A , Ghashang, SK , Buettner, M , Eljurnazi, L , Grassl, GA, et al. Ramadan fasting in Germany (17–18 h/day): effect on cortisol and brain-derived neurotrophic factor in association with mood and body composition parameters. Front Nutr. (2021) 8:697920. doi: 10.3389/fnut.2021.697920
34. Jahrami, H , BaHammam, AS , Haji, EA , Bragazzi, NL , Rakha, I , Alsabbagh, A, et al. Ramadan fasting improves body composition without exacerbating depression in males with diagnosed major depressive disorders. Nutrients. (2021) 13:2718. doi: 10.3390/nu13082718
35. Bastani, A , Rajabi, S , and Kianimarkani, F . The effects of fasting during Ramadan on the concentration of serotonin, dopamine, brain-derived neurotrophic factor and nerve growth factor. Neurol Int. (2017) 9:7043. doi: 10.4081/ni.2017.7043
36. Chen, Y-W , Lin, P-Y , Tu, K-Y , Cheng, Y-S , Wu, C-K , and Tseng, P-T . Significantly lower nerve growth factor levels in patients with major depressive disorder than in healthy subjects: a meta-analysis and systematic review. Neuropsychiatr Dis Treat. (2015) 11:925–33. doi: 10.2147/NDT.S81432
37. Liu, X , Li, P , Ma, X , Zhang, J , Sun, X , Luo, X, et al. Association between plasma levels of BDNF and GDNF and the diagnosis, treatment response in first-episode MDD. J Affect Disord. (2022) 315:190–7. doi: 10.1016/j.jad.2022.07.041
38. Barak, S , Ahmadiantehrani, S , Logrip, ML , and Ron, D . GDNF and alcohol use disorder. Addict Biol. (2019) 24:335–43. doi: 10.1111/adb.12628
39. Skibinska, M , Kapelski, P , Pawlak, J , Rajewska-Rager, A , Dmitrzak-Weglarz, M , Szczepankiewicz, A, et al. Glial cell line-derived neurotrophic factor (GDNF) serum level in women with schizophrenia and depression, correlation with clinical and metabolic parameters. Psychiatry Res. (2017) 256:396–402. doi: 10.1016/j.psychres.2017.07.014
40. Shen, Z , Zhu, J , Yuan, Y , Ren, L , Qian, M , Lin, M, et al. The roles of brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF) in predicting treatment remission in a Chinese Han population with generalized anxiety disorder. Psychiatry Res. (2019) 271:319–24. doi: 10.1016/j.psychres.2018.08.111
41. Fawzi, MH , Fawzi, MM , Said, NS , Fawzi, MM , Fouad, AA , and Abdel-Moety, H . Effect of Ramadan fasting on anthropometric, metabolic, inflammatory and psychopathology status of Egyptian male patients with schizophrenia. Psychiatry Res. (2015) 225:501–8. doi: 10.1016/j.psychres.2014.11.057
42. Rozanska, O , Uruska, A , and Zozulinska-Ziolkiewicz, D . Brain-derived neurotrophic factor and diabetes. Int J Mol Sci. (2020) 21:841. doi: 10.3390/ijms21030841
43. Elesawy, BH , Raafat, BM , Muqbali, AA , Abbas, AM , and Sakr, HF . The impact of intermittent fasting on brain-derived neurotrophic factor, Neurotrophin 3, and rat behavior in a rat model of type 2 diabetes mellitus. Brain Sci. (2021) 11:242. doi: 10.3390/brainsci11020242
44. Abdulsada, MM , Wilhelm, ZR , Opekun, AR , Devaraj, S , Jalal, PK , and Mindikoglu, AL . The effect of four-week intermittent fasting from dawn to sunset on circulating brain-derived neurotrophic factor levels in subjects with metabolic syndrome and healthy subjects. Metabolism Open. (2021) 9:100070. doi: 10.1016/j.metop.2020.100070
45. Saifi, B , Dousti Majd, N , Meshkat, M , and Amali, A . The comparison of serum levels of IGF1 before and after fasting in healthy adults. J Nutr Fast Health. (2023) 11:118–23. doi: 10.22038/jnfh.2023.70510.1429
46. Lee, C , Safdie, FM , Raffaghello, L , Wei, M , Madia, F , Parrella, E, et al. Reduced IGF-I differentially protects normal and cancer cells and improves chemotherapeutic index in mice. Cancer Res. (2010) 70:1564–72. doi: 10.1158/0008-5472.CAN-09-3228
47. Fontana, L , Partridge, L , and Longo, VD . Extending healthy life span—from yeast to humans. Science. (2010) 328:321–6. doi: 10.1126/science.1172539
48. Münger, LH , Garcia-Aloy, M , Vázquez-Fresno, R , Gille, D , Rosana, ARR , Passerini, A, et al. Biomarker of food intake for assessing the consumption of dairy and egg products. Genes Nutr. (2018) 13:26. doi: 10.1186/s12263-018-0615-5
49. Picó, C , Serra, F , Rodríguez, AM , Keijer, J , and Palou, A . Biomarkers of nutrition and health: new tools for new approaches. Nutrients. (2019) 11:1092. doi: 10.3390/nu11051092
50. Abdelrahim, DN , El Herrag, SE , Khaled, MB , Radwan, H , Naja, F , Alkurd, R, et al. Changes in energy and macronutrient intakes during Ramadan fasting: a systematic review, meta-analysis, and meta-regression. Nutr Rev. (2023) 1–32. doi: 10.1093/nutrit/nuad141
Keywords: Ramadan intermittent fasting, neurotrophic factors (NTFs), Interleukin-8 (IL-8), TNF-α – tumor necrosis factor alpha, anthropometric, matrix metalloprotein-9 (MMP-9), mental health parameters and quality of life (QoL) parameters
Citation: Ghashang SK, Suwandi A, Buettner M, Hamdan I, Grassl GA, Gutenbrunner C and Nugraha B (2024) Alterations in anthropometric, inflammatory and mental health parameters during Ramadan intermittent fasting in a group of healthy people: a prospective cohort study. Front. Nutr. 11:1298281. doi: 10.3389/fnut.2024.1298281
Edited by:
MoezAlIslam Ezzat Faris, University of Sharjah, United Arab EmiratesReviewed by:
Mostafa Waly, Sultan Qaboos University, OmanSubhashis Sahu, University of Kalyani, India
Falak Zeb, University of Sharjah, United Arab Emirates
Copyright © 2024 Ghashang, Suwandi, Buettner, Hamdan, Grassl, Gutenbrunner and Nugraha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Boya Nugraha, Ym95YS5udWdyYWhhQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Samaneh Khosandam Ghashang
Samaneh Khosandam Ghashang Abdulhadi Suwandi
Abdulhadi Suwandi Manuela Buettner
Manuela Buettner Imad Hamdan
Imad Hamdan Guntram A. Grassl
Guntram A. Grassl Christoph Gutenbrunner
Christoph Gutenbrunner Boya Nugraha
Boya Nugraha