- 1Nutrition and Food Security Research Center, Department of Community Nutrition, School of Nutrition and Food Science, Isfahan University of Medical Sciences, Isfahan, Iran
- 2Student Research Committee, Isfahan University of Medical Sciences, Isfahan, Iran
- 3Department of Medicine, University of Alberta, Edmonton, AB, Canada
- 4Obesity and Eating Habits Research Center, Endocrinology and Metabolism Molecular-Cellular Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
- 5Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
- 6Integrative Functional Gastroenterology Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Background: Data linking joint healthy lifestyle factors to general and abdominal obesity are scarce, in particular in the Middle East. The aim of this study was to examine the association of combined healthy lifestyle factors with general and abdominal obesity in a large population of Iranian adults.
Methods: This cross-sectional study was done on 3,172 Iranian adults aged ≥18 years. We constructed healthy lifestyle score using information on dietary intakes, physical activity, smoking status, and psychological distress. To evaluate components of healthy lifestyle, we applied a validated 106-item semi-quantitative Food Frequency Questionnaire (FFQ), General Practice Physical Activity Questionnaire (GPPAQ), General Health Questionnaire (GHQ), and other pre-tested questionnaires. General obesity was defined as having a body mass index (BMI) ≥30 kg/m2 and abdominal obesity as a waist circumference (WC) of ≥102 cm in men and ≥88 cm in women.
Results: Mean age of participants was 36.54 ± 7.97 years. General and abdominal obesity were prevalent among 8.7% and 21.5% of study participants, respectively. Linear analysis showed a significant positive relationship between healthy lifestyle score and BMI among men (β: 0.30, 95% CI: 0.05, 0.54). However, no significant association was found between healthy lifestyle and abdominal obesity in men. Among women, one score increase in healthy lifestyle score was associated with a reduction of 0.65 cm in WC. In terms of individual components of healthy lifestyle, we found that low-distressed women had lower odds of abdominal obesity compared with high-distressed women.
Conclusion: We found a significant inverse association between healthy lifestyle and WC among women. However, healthy lifestyle was positively associated with BMI among men.
Introduction
Obesity has been an epidemic public health issue during the past decades which is associated with a greater risk of diabetes, hypertension, osteoarthritis, coronary heart disease (CHD), and some cancers (1–5). By 2030, it is projected that 20% of the worldwide population will be affected by obesity and 38% by overweight (6). In Iran, about half of the adult population are overweight or obese (7). In addition to general obesity, the prevalence of abdominal obesity has been estimated to be high (8). Compared with general obesity, abdominal obesity has been linked with a greater risk of mortality (9). Therefore, the assessment of determinants of general and abdominal obesity is of great importance.
Several modifiable risk factors including poor diet, sedentary lifestyle, smoking, and psychological distress have been assessed in relation to obesity (7, 8, 10–15); however, findings in this regard are conflicting. Healthy lifestyle was linked with a reduced risk of mortality (16). In a meta-analysis, a combination of at least four healthy lifestyle factors (obesity, alcohol consumption, smoking, diet, and physical activity) was associated with a 66% lower risk of all-cause mortality (16). Despite the assessment of individual lifestyle components, including diet, physical activity, or stress in relation to obesity, few studies have examined the association of combined lifestyle factors with general or abdominal obesity. Given the combined effect of these environmental factors on weight gain, it seems that the assessment of combined lifestyle factors can provide additional information on the incidence of this condition. On the other hand, it is not clear that the interaction between the mentioned lifestyle factors presented similar findings compared with individual factors in relation to obesity. In a cross-sectional study in Spain, a combination of four healthy lifestyle behaviors (including adherence to the Mediterranean diet, moderate alcohol consumption, expending ≥200 kcal/day in leisure-time physical activity, and being a non-smoker) was inversely associated with general and abdominal obesity (17). In a prospective cohort study, adherence to a healthy lifestyle [characterized by a healthy body mass index (BMI), high-quality diet, regular exercise, no smoking, and light to moderate alcohol intake] in mothers was associated with a substantially reduced risk of obesity in the children (18).
It must be kept in mind that all published studies so far were restricted to Western societies and few data are available from Asian countries, in particular from the understudied region of the Middle East. Assessing this association is particularly relevant for the Middle Eastern population, due to the high prevalence of a Middle Eastern pattern of obesity, which is characterized by abdominal fat accumulation and enlarged waist circumference (WC), particularly among women (19). In addition, lifestyle factors in the Middle East are different from other parts of the world. Because of cultural expectations, women in the Middle East have lower physical activity levels than men (20). In addition, smoking is more prevalent among men than women in this region (21). Furthermore, earlier studies on the association between healthy lifestyle and obesity have not considered stress as a major component of lifestyle. Therefore, the current study aimed to assess the link between the whole lifestyle factors and general and abdominal obesity among a large population of Iranian adults.
Materials and methods
Participants
This cross-sectional study was done on a large population of adults in Isfahan, Iran. Data of all participants were obtained from the SEPAHAN (Studying the Epidemiology of Psycho-Alimentary Health and Nutrition) project. Details on the study design, participants, and method of data collection were published previously (22). Briefly, this project was carried out in two separate phases. In the first phase, data on demographic variables and dietary intakes of participants, and in the second phase, data on mental health were collected. After merging the data from both phases of this project, 4,763 participants had complete data. In this study, we excluded participants with missing data on dietary intakes, demographic, anthropometric, and psychological data. We also excluded participants with an implausible energy intake (outside the range of 800–4,200 kcal/day). Moreover, pregnant and lactating women were not included in our study. Finally, 3,172 participants (1,398 men and 1,774 women) were included in the current analysis. Before starting the study, a written informed consent form was provided to all participants, and they were asked to sign it. The Bioethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran, approved the SEPAHAN project (22).
Assessment of dietary intakes
In the current study, information on participants’ dietary intakes was evaluated using a validated Willett-format Dish-based 106-item Semi-quantitative Food Frequency Questionnaire (DS-FFQ) (23). This questionnaire was specifically designed and validated for Iranian adults. Information on design, foods included, and the validity of this questionnaire was published elsewhere (23). We asked participants to report their dietary intakes based on nine multiple choice frequency response categories varying from “never or less than once a month” to “12 or more times per day.” The frequency response categories for the food list varied from six to nine choices. For foods with low consumption, we eliminated the high-frequency categories, while for foods with high consumption, we increased the number of multiple-choice categories. To convert the amount of each portion size to grams, we used the booklet of “household measures.” Daily intakes of foods and dishes were calculated according to the consumption frequency of each food item. Also, based on the nutrient contents of all foods and dishes, the daily nutrient intakes for each participant were computed. To obtain the nutrient contents of foods and dishes, we used the US Department of Agriculture’s (USDA) national nutrient databank (24).
To evaluate the validity and reliability of DS-FFQ, a subgroup of 200 participants of the SEPAHAN project was randomly selected (23, 25). All participants completed the DS-FFQ at baseline and 6 months later. During this 6 month, participants provided three dietary records. The findings showed that the DS-FFQ could provide valid and reliable measures of long-term dietary intakes in the Iranian population.
Assessment of physical activity
By using the General Practice Physical Activity Questionnaire (GPPAQ), the physical activity of participants was evaluated (26). GPPAQ is a validated short instrument for the measurement of physical activity that was designed by the London School of Hygiene and Tropical Medicine (27). All participants were asked to report their activities based on this questionnaire. In this study, current physical activity has been used for the objective assessment of overall physical activity levels. The validity of GPPAQ for the assessment of habitual physical activity levels has earlier been shown (27).
Assessment of psychological distress
Psychological distress was evaluated using the Iranian validated version of General Health Questionnaire (GHQ) (28). This questionnaire contains 12 items. Each item provides a 4-point rating scale (less than usual, no more than usual, rather more than usual, or much more than usual). By using the bimodal scoring method, we computed the total score of psychological distress for each participant (0-0-1-1). According to this method, total scores of GHQ range from 0 to 12; higher scores indicate a higher degree of psychological distress (29).
Assessment of smoking
In the current study, a pre-tested questionnaire was used to evaluate the smoking status of participants. Participants were asked “How many cigarettes do you smoke every day?” They were able to choose one of the following options: “never smoked,” “I am an ex-smoker,” “1–5 cigarettes per day,” “5–20 cigarettes per day,” and “more than 20 cigarettes per day.” Participants were categorized into non-smokers, former smokers, or current smokers. In the present study, participants who reported smoking ≥1 cigarette per day were considered as current smokers.
Construction of healthy lifestyle score
Diet, physical activity, smoking, and stress were considered to construct healthy lifestyle score. Healthy diet was defined based on Alternative Healthy Eating Index-2010 (AHEI-2010). To calculate AHEI-2010, we used a method designed by Kennedy et al. (30) and Sadeghi et al. (31). This method considered 11 components including fruit, vegetables, whole grains, nuts, and legumes, long-chain n-3 fats [docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA)], polyunsaturated fatty acid (PUFA), wine consumption, sugar-sweetened drinks and fruit juice, red and processed meats, trans-fat, and sodium intake. In the current study, due to a lack of information on wine consumption, 10 components were considered to compute AHEI. First, all study participants were classified into deciles according to the consumption of each component of AHEI-2010. Then participants in the highest decile of whole grains, vegetables, fruits, nuts, and legumes, long-chain n-3 fats (DHA and EPA), and PUFA received the score of 10, and those in the lowest decile were given the score of 1. Participants in other deciles of these food groups received the corresponding scores. In contrast, participants in the highest deciles of sugar-sweetened drinks and fruit juice, red and processed meats, trans-fat, and sodium received the score of 1, and those in the lowest deciles of these components were given the score of 10. Those in other deciles received the corresponding scores. By summing up the scores for these 10 components, we calculated the total HEI score for each participant. The total HEI score varied from 10 to 100. Participants in the highest 40% of AHEI (upper two-fifths) were considered as having a healthy diet.
With regards to physical activity, we classified participants into physically active (≥1 hour/week of moderate physical activity) and physically inactive (<1 hour/week of moderate physical activity). In terms of psychological distress, participants with a score of ≥4 were considered as having psychological distress. Regarding smoking, current smoking was considered as unhealthy behavior, and former smoking and non-smoking were considered as healthy.
Finally, we calculated the total healthy lifestyle score by summing up the scores that each participant received for components of lifestyle. Subjects in the low-risk categories of the above-mentioned components (non/ex-smokers, those in the highest 40% of AHEI score, those with GHQ score of <4, and participants with ≥1 h/week of moderate physical activity) received the score of 1, otherwise, they received the score of 0. Therefore, a composite global healthy lifestyle score ranged from 0 to 4 (Figure 1). In the current study, the number of participants with a score of zero was very low. Therefore, we included participants with a score of 0 or 1 in one category as the score of 0/1 (the lowest category).

Figure 1. The healthy lifestyle score construction. AHEI, alternative healthy eating index; PA, physical activity; Q, quintile; h/wk, hour/week.
Assessment of outcomes
Using a self-reported questionnaire, we gathered participants’ anthropometric information including height, weight, and WC. We computed BMI as weight in kilograms divided by the height in meters squared.
The validity of self-reported weight, height, and WC was evaluated in a pilot study on 200 participants from the same population. In the validation study, self-reported values of anthropometric indices were compared with actual measured values. The findings of this pilot study showed that the self-reported values of anthropometric indices provide a reasonable measure for these indices.
We defined obesity as having a BMI ≥30 kg/m2 and overweight as having a BMI ≥25 kg/m2. In the current study, we defined abdominal obesity based on WC according to the criteria proposed by the National Cholesterol Education Program (NCEP) (7, 32). Men with a WC of ≥102 cm and women with a WC of ≥88 cm, were considered as abdominally obese. We also defined abdominal overweight according to the criteria proposed by Lean et al. (33) as WC ≥94 cm for men and WC ≥80 cm for women.
Assessment of other variables
To gather data on age, gender (male/female), marital status (single/married), family size (≤4/>4 members), breakfast skipping (yes/no) and house possession (owner/non-owner), diabetes (yes/no), use of anti-psychotic drugs (yes/no), and dietary supplements (yes/no), we used a self-administered questionnaire. Participants who were consuming breakfast <4 times/week were considered as breakfast skippers.
Statistical analysis
We categorized participants according to the scores of healthy lifestyle (0/1 to 4). We included participants with a score of 0 or 1 in one category as the score of 0/1 (the lowest category). To assess differences across categories of healthy lifestyle scores, one-way analysis of variance (ANOVA) for continuous variables was used. In addition, Chi-square test was used to compare the distribution of individuals in terms of categorical variables across categories of healthy lifestyle score. To examine the association between healthy lifestyle score and general and abdominal obesity, we used binary logistic regression controlling for several covariates. Age, marital status (single/married), family size (≤4/>4 members), breakfast skipping (yes/no), house possession (owner/non-owner), history of diabetes (yes/no), use of anti-psychotic medications (yes/no), and dietary supplements (yes/no) were adjusted in the first model. For abdominal obesity, we also controlled for BMI in model 2 in addition to the variables included in model 1. In the highest versus lowest comparison, we considered participants in the lowest category of healthy lifestyle score as the reference group. To determine the trend of odds ratios (ORs) across increasing categories of healthy lifestyle score, we considered these categories as an ordinal variable. We also examined the dose-response association between each score increase in healthy lifestyle and general/abdominal obesity using binary logistic regression. The association between individual components of healthy lifestyle score and general and abdominal obesity was also examined in multivariable-adjusted models controlling for the above-mentioned covariates. We also compared the continuous indices of BMI and WC across the categories of healthy lifestyle scores using one-way analysis of covariance (ANCOVA). Moreover, to assess the linear association between healthy lifestyle scores and the mentioned indices, linear regression in an adjusted model was used. In the current study, we performed all statistical analyses in Statistical Package for Social Sciences (SPSS) software, version 18. p-Values of less than 0.05 were considered statistically significant.
Results
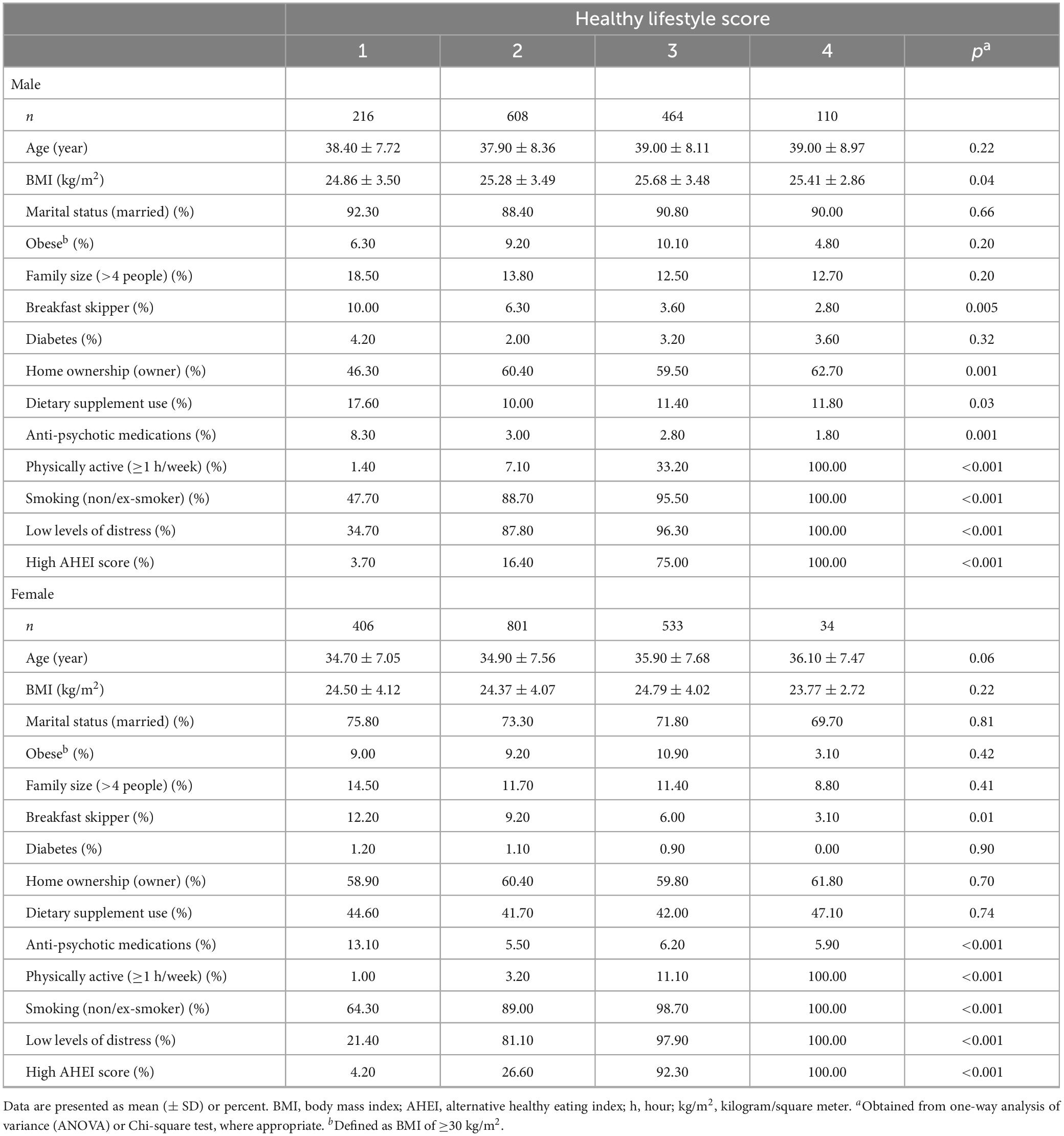
In total, 3,172 individuals, with a mean age of 36.54 ± 7.97 years, were included in the current analysis. General and abdominal obesity were prevalent among 8.7% and 21.5% of study participants, respectively. General characteristics of men and women across categories of healthy lifestyle score are presented in Table 1. Compared with men in the lowest category of healthy lifestyle score, those in the highest category had higher BMI and greater adherence to AHEI and were less likely to be breakfast skippers, psychologically distressed, use dietary supplements and anti-psychotic medications, and were more likely to be house owner, physically active, and non/ex-smokers. Among women, those in the highest category of healthy lifestyle score had higher AHEI score and were less likely to be breakfast skippers, psychologically distressed, use anti-psychotic medications, and were more likely to be physically active and non/ex-smoker than women in the lowest category. No other significant differences were seen across categories of healthy lifestyle score in either gender.
Dietary intakes of men and women across different levels of healthy lifestyle score are shown in Table 2. Compared with men in the lowest category of healthy lifestyle, those in the highest category had higher intakes of fruits, vegetables, fish, legumes plus nuts, whole grains, proteins, dietary fiber, vitamin B6, omega-3 fatty acids, and lower intakes of refined grains and caffeine. Among women, greater adherence to healthy lifestyle was associated with higher intakes of fruits, vegetables, fish, legumes plus nuts, whole grains, proteins, carbohydrates, dietary fiber, vitamin B6, omega-3 fatty acids, and lower intakes of refined grains, fats, red meat, and caffeine. No other significant difference was found.
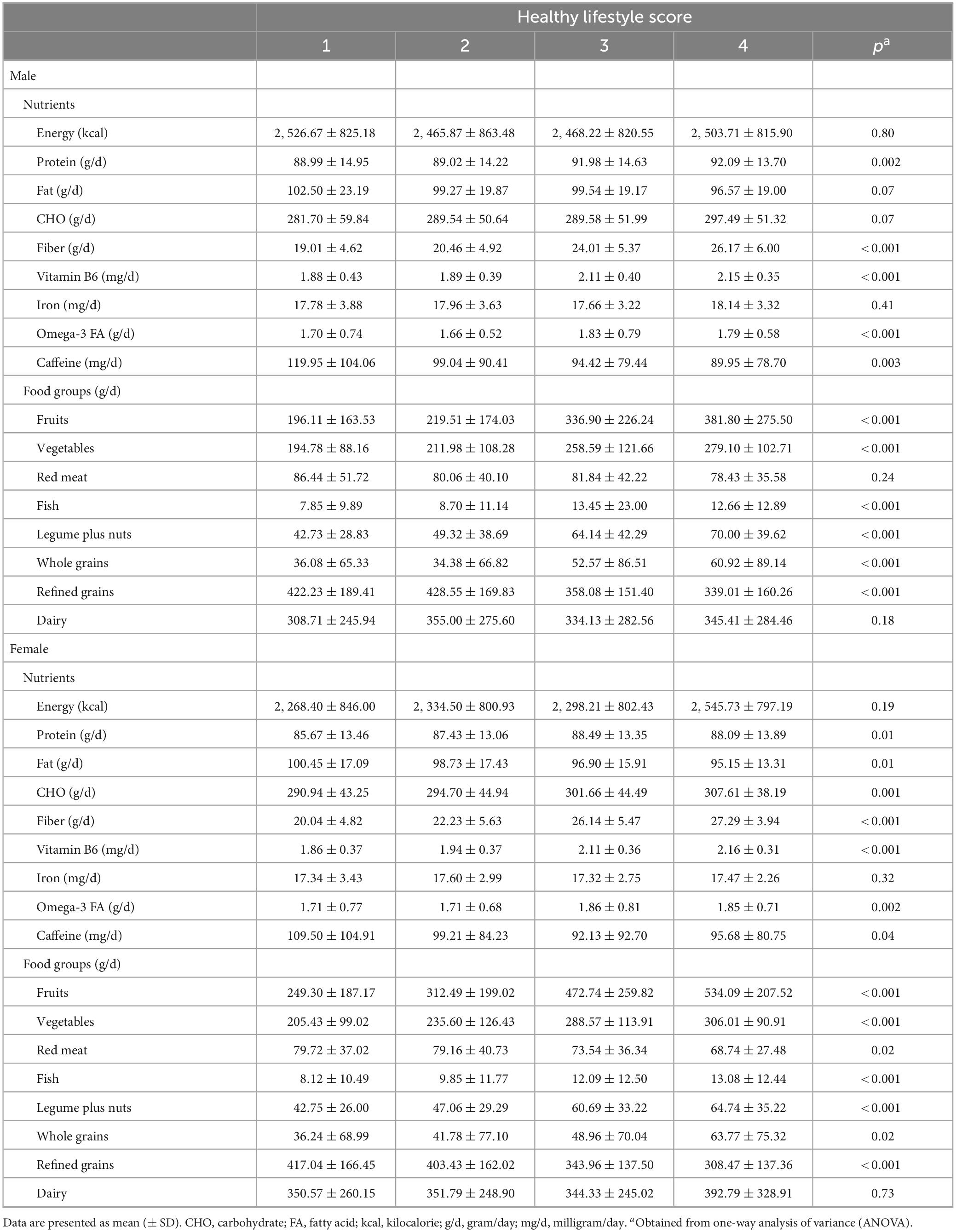
Table 2. Dietary intakes of selected nutrients and food groups of men and women across different levels of healthy lifestyle score.
Gender-stratified multivariable-adjusted means and standard errors (SE) and β-coefficients for the associations of healthy lifestyle score with BMI and WC in men and women are presented in Table 3. Among men, we found a significant difference in BMI across categories of healthy lifestyle score; however, after controlling for potential confounders, this difference became non-significant. Linear regression analysis showed a significant positive relationship between healthy lifestyle score and BMI among men so that in the fully adjusted model, one score increase in healthy lifestyle score was associated with a 0.3 kg/m2 increase in BMI. For WC among men, no significant association was found with healthy lifestyle scores. Among women, we found no significant association between healthy lifestyle score and BMI either based on the multivariable-adjusted means or based on β-coefficients for the linear association. However, for WC, after adjusting for confounding variables, one score increase in the healthy lifestyle score was associated with a reduction of 0.65 cm in WC.
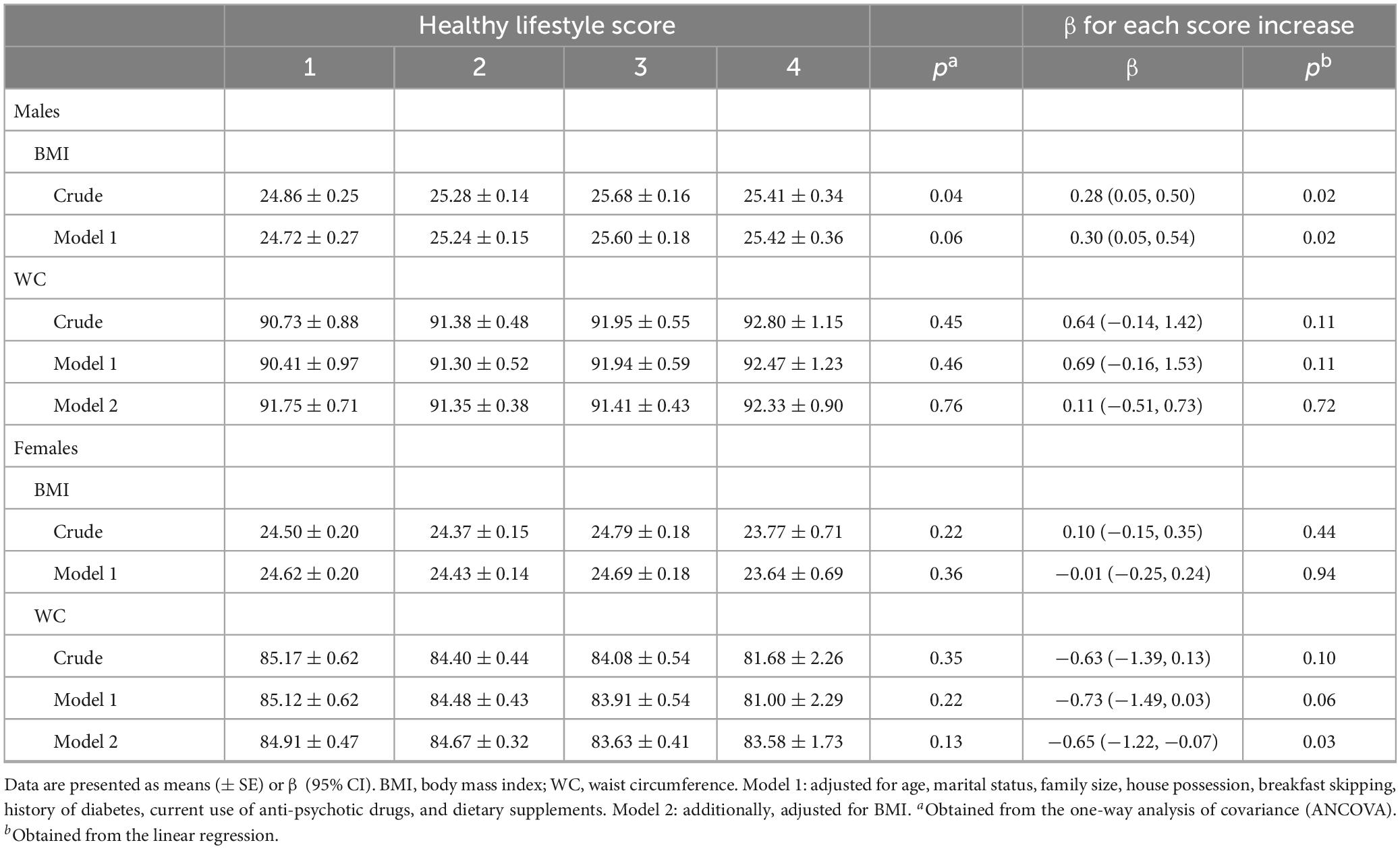
Table 3. Gender-stratified multivariable-adjusted means (± SE) and β-coefficients for the associations of healthy lifestyle score with BMI and WC in men and women.
Multivariable-adjusted OR and 95% confidence intervals (CIs) for the association of healthy lifestyle score with general and abdominal obesity are indicated in Table 4. Among men, after taking potential confounders into account, healthy lifestyle scores were not associated with overweight, obesity, and abdominal obesity (WC ≥102 or WC ≥94 cm). This non-significant association was also seen in the dose-response analysis based on one score increase in healthy lifestyle. Such non-significant associations were also observed among women.
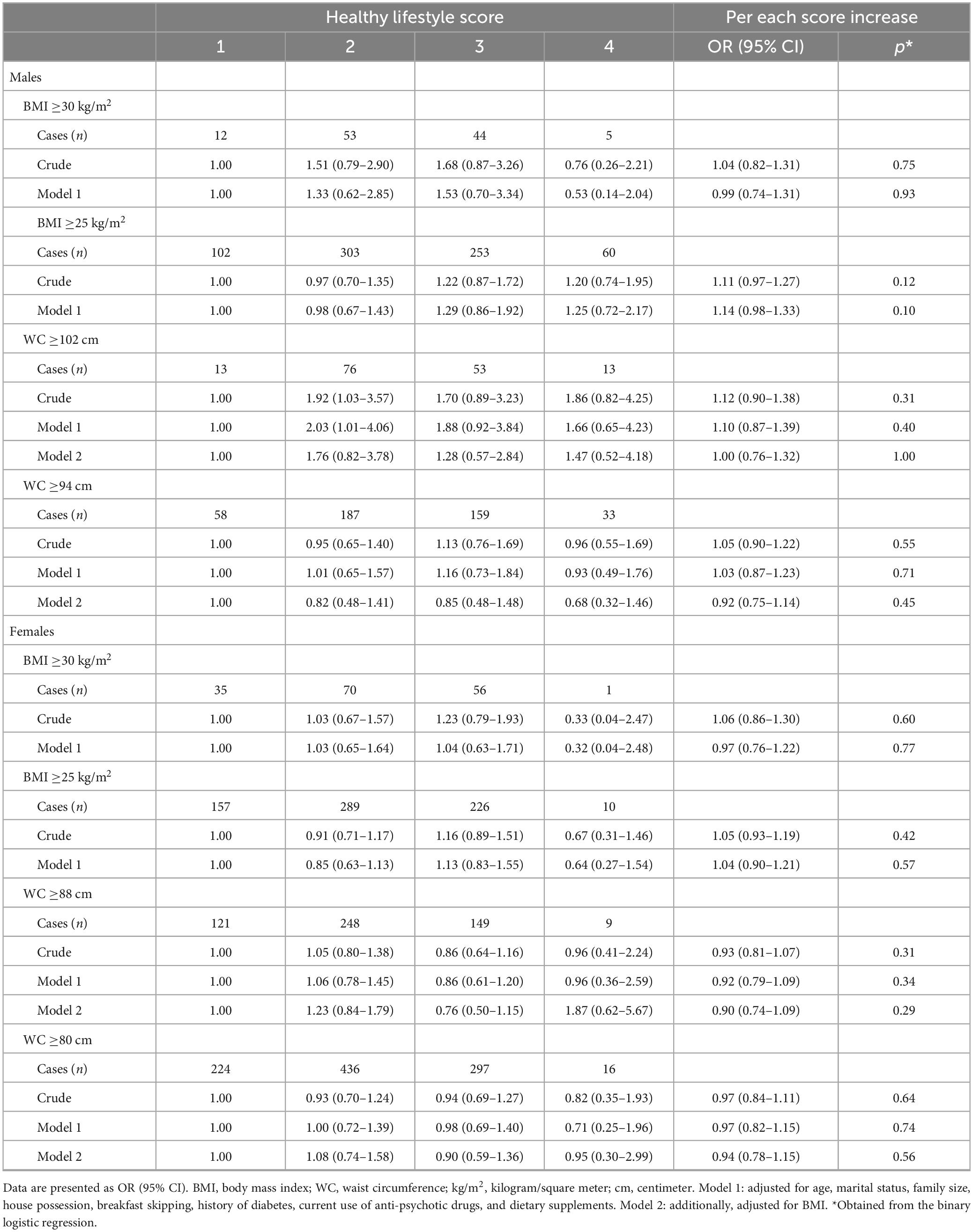
Table 4. Gender-stratified multivariable odds ratios (ORs) and 95% confidence intervals (CIs) for general and abdominal obesity across different levels of healthy lifestyle score.
The associations between individual components of healthy lifestyle and general and abdominal obesity are shown in Table 5. After controlling for potential confounding variables, none of the components of healthy lifestyle was associated with overweight, obesity, and abdominal obesity in men. However, in women, non-smokers had 61% higher odds of abdominal obesity (WC ≥80 cm) compared with smokers (OR: 1.61, 95% CI: 1.03–2.50). In addition, participants who had a low level of psychological distress had 29% lower odds of abdominal obesity compared with those who had a high level of distress (OR: 0.71, 95% CI: 0.51–0.98). For other associations assessed among women, we found no significant association in multivariable-adjusted models.
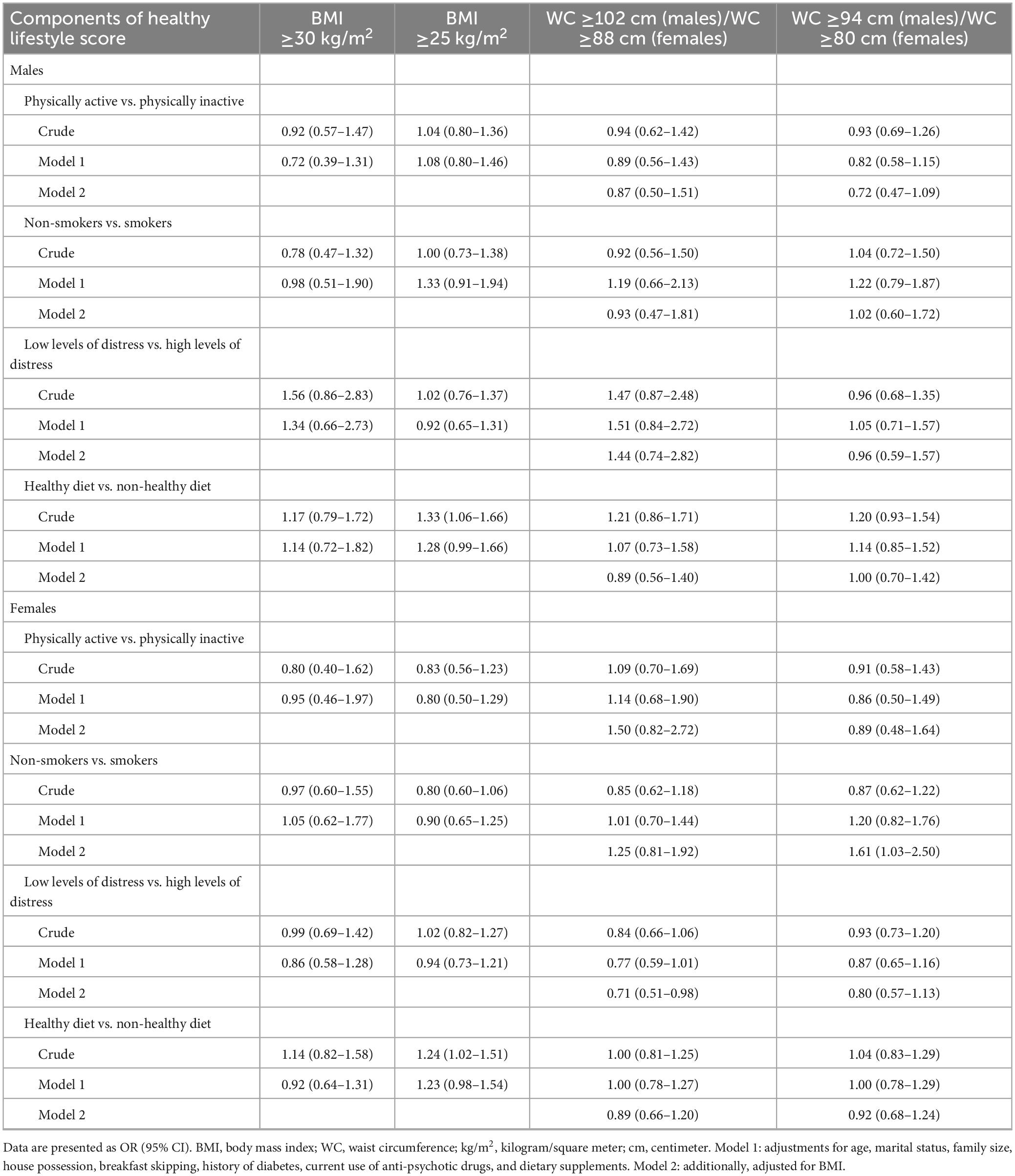
Table 5. Gender-stratified multivariable odds ratios (ORs) and 95% confidence intervals (CIs) for general and abdominal obesity across different levels of individual components of healthy lifestyle score.
Discussion
In the current study, we found a significant positive association between healthy lifestyle and BMI among men. Also, we found a significant inverse association between healthy lifestyle and WC among women. However, when we did analyses on binary variables including general and abdominal obesity, these associations became non-significant. In terms of individual components of healthy lifestyle, we found that non-smokers had higher odds of abdominal obesity than smokers in women. Furthermore, low-distressed women had lower odds of abdominal obesity compared with high-distressed women. To the best of our knowledge, this study is the first to examine the association between healthy lifestyle and general and abdominal obesity in a Middle Eastern population.
It is well-known that obesity, especially abdominal obesity, is a main risk factor for several metabolic disorders including cardiovascular diseases (CVDs) and diabetes mellitus (34–36). In the current century, the prevalence of obesity is increasing (8). Moreover, it has become an epidemic in the Middle Eastern population; so that more than two-thirds of Middle Eastern women are affected (8). Several modifiable risk factors including poor diet, sedentary lifestyle, smoking, and psychological distress have long been known to contribute to the obesity epidemic (7, 8, 10–15); however, little attention has been laid on the combined effect of these environmental factors on general and abdominal obesity. In the current study, we found a significant positive association between healthy lifestyle and the odds of general obesity among men. Contrary to our findings, Shook et al. (37) reported that adherence to a multiple national healthy lifestyle was inversely associated with odds of obesity among US children. However, in the study of Shook et al., only physical activity, drinking water, and diet quality were considered as components of healthy lifestyle. In a cross-sectional study in Spain, a combination of four healthy lifestyle behaviors including adherence to the Mediterranean diet, moderate alcohol consumption, expending ≥200 kcal/day in leisure-time physical activity, and non-smoking was associated with a lower prevalence of general and abdominal obesity (17). In addition, some studies revealed a significant inverse association between healthy lifestyle and obesity-related disorders including metabolic syndrome (38), diabetes, and hypertension (39). The controversy between our findings and those obtained from the previous studies might be attributed to the different components of healthy lifestyle among the previous studies. For instance, none of the previous studies considered psychological distress as a component of healthy lifestyle. In addition, different cut-off points used to determine each component of healthy lifestyle might be other reason for the controversy. Also, adjustments for different confounders might be another reason for this controversy. Moreover, it should be noted that there is a specific pattern of general obesity in the Middle Eastern population which is a bit different from others (19). Another reason for the unreasonable association between healthy lifestyle and general obesity in the current study might be due to the cross-sectional design of our study. On the other hand, obese participants usually tend to adhere to a healthy lifestyle in order to weight loss. Therefore, our findings on the link between healthy lifestyle and general obesity should be considered with caution, and further studies are needed to reveal facts in this regard.
In this study, a significant inverse association was found between healthy lifestyle and abdominal obesity among women. In line with our findings, the SUN cohort study showed that participants in the highest category of healthy lifestyle score (7–9 points) had a significantly reduced risk of developing abdominal obesity compared with those in the lowest category (0–3 points) (38). Such an inverse association was reported in a cross-sectional study from Spain (17). Diet, physical activity, and other components of healthy lifestyle score may influence obesity through several different pathways. Adherence to a healthy diet, which is associated with high consumption of whole grain foods and dietary fiber, can explain the favorable association at least to some extent (40). In addition, having a poor diet, cigarette smoking, psychological distress, and a sedentary lifestyle are associated with increased serum levels of inflammatory biomarkers (41–44). Inflammation can stimulate the accumulation of fatty acids in the abdomen (45).
In terms of individual components of healthy lifestyle, we found that non-smokers had higher odds of abdominal obesity than smokers in women. In contrast, Cheng et al. (46) reported that smoking was significantly associated with higher WC. Also, in a cross-sectional study, Clair et al. (47) showed a positive association between cigarettes smoked per day and central fat accumulation. Such a positive relationship between smoking and central obesity was also shown by other researchers (48, 49). The difference between our findings and other studies might be due to the different pattern of abdominal obesity in the Middle East, named Middle Eastern abdominal obesity, which is characterized by abdominal fat accumulation and enlarged WC, particularly among women (19). Also, the use of different methods to assess abdominal fat and different adjustments in analyses are other reasons for the controversy. Moreover, since the design of our study was cross-sectional, outcome may occur before exposure. On the other hand, abdominal obese individuals try to have a healthy lifestyle and therefore, they may tend to quit smoking.
In the present study, a significant positive association was found between psychological distress and abdominal obesity among women. Such association was also reported in previous investigations (50, 51). Psychological distress can increase food eating (52). On the other hand, distressed people tend to eat a high amount of food for decreasing their distress. Also, increased levels of glucocorticoids in distressed subjects increase the accumulation of fat in the abdomen (52).
Our study has several strengths including the large sample size, careful assessment of confounding variables as well as dietary intakes, psychological distress, and physical activity with validated questionnaires. Unlike earlier studies in which a single lifestyle behavior was assessed in relation to obesity, we examined the combined lifestyle score in relation to general and abdominal obesity. However, some limitations should be considered for interpreting our findings. Due to the cross-sectional design of the study, causality cannot be inferred. It is likely that obese people change their lifestyle in an effort to combat their weight status. Future investigations are needed to have a better understanding of the direction of this association. Measurement errors in epidemiologic studies are inevitable, in particular when one intends to assess diet and physical activity. However, such errors would attenuate the true associations. We tried to control for several potential confounding variables associated with the exposures and outcomes; however, residual confounding in our study, as in all epidemiological studies, is unavoidable. In addition, we used a self-report questionnaire to collect information on weight, height, and WC rather than a valid measurement. It has been reported that obese and overweight subjects tend to over-report height and underreport weight compared to normal-weight subjects (53).
Conclusion
In conclusion, we found a significant positive association between healthy lifestyle and BMI among men. Also, we found a significant inverse association between healthy lifestyle and WC among women. In terms of individual components of healthy lifestyle, we found that non-smokers had higher odds of abdominal obesity than smokers in women. In addition, low-distressed women had lower odds of abdominal obesity compared with high-distressed women. Further studies, in particular of prospective nature, are required to confirm our findings.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Bioethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent was gathered from each participant.
Author contributions
OS: Methodology, Formal analysis, Writing – original draft. NE: Formal analysis, Writing – review & editing. AK: Methodology, Conceptualization, Project administration, Writing – review & editing. GA: Methodology, Funding acquisition, Writing – review & editing. AE: Methodology, Supervision, Conceptualization, Formal analysis, Project administration, Writing – review & editing. PA: Methodology, Conceptualization, Project administration, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was financially supported by Isfahan University of Medical Sciences in collaboration with the Students’ Scientific Research Center, Tehran University of Medical Sciences, Tehran, Iran as well. Additionally, this project received support from the National Institute for Medical Research Development, Ministry of Health and Medical Education, Tehran, Iran (grant No. 982674).
Acknowledgments
The authors acknowledge their staff, the fieldworkers, and the SEPAHAN project participants that without them this work would not have been possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lennon H, Sperrin M, Badrick E, Renehan A. The obesity paradox in cancer: a review. Curr Oncol Rep. (2016) 18:56. doi: 10.1007/s11912-016-0539-4
2. Singla R, Murthy M, Singla S, Gupta Y. Friendly Fat Theory - Explaining the Paradox of Diabetes and Obesity. Eur Endocrinol. (2019) 15:25–8. doi: 10.17925/ee.2019.15.1.25
3. Wang T, He C. Pro-Inflammatory Cytokines: The Link between Obesity and Osteoarthritis. Cytokine Growth Factor Rev. (2018) 44:38–50. doi: 10.1016/j.cytogfr.2018.10.002
4. Sadeghi O, Saneei P, Nasiri M, Larijani B, Esmaillzadeh A. Abdominal Obesity and Risk of Hip Fracture: A Systematic Review and Meta-Analysis of Prospective Studies. Adv Nutr. (2017) 8:728–38. doi: 10.3945/an.117.015545
5. Miri A, Nasiri M, Zonoori S, Yarahmad F, Dabbagh-Moghadam A, Askari G, et al. The Association between Obesity and Migraine in a Population of Iranian Adults: A Case-Control Study. Diabetes Metab Syndr. (2018) 12:733–6. doi: 10.1016/j.dsx.2018.04.020
6. May A, Freedman D, Sherry B, Blanck H, Control C. Prevention. Obesity—United States, 1999–2010. MMWR Surveill Summ. (2013) 62:120–8.
7. Sadeghi O, Keshteli A, Doostan F, Esmaillzadeh A, Adibi P. Association between Dairy Consumption, Dietary Calcium Intake and General and Abdominal Obesity among Iranian Adults. Diabetes Metab Syndr. (2018) 12:769–75. doi: 10.1016/j.dsx.2018.04.040
8. Dabbagh-Moghadam A, Mozaffari-Khosravi H, Nasiri M, Miri A, Rahdar M, Sadeghi O. Association of White and Red Meat Consumption with General and Abdominal Obesity: A Cross-Sectional Study among a Population of Iranian Military Families in 2016. Eat Weight Disord. (2017) 22:717–24. doi: 10.1007/s40519-017-0385-x
9. Ekelund U, Ward H, Norat T, Luan J, May A, Weiderpass E, et al. Physical Activity and All-Cause Mortality across Levels of Overall and Abdominal Adiposity in European Men and Women: The European Prospective Investigation into Cancer and Nutrition Study (Epic). Am J Clin Nut.r (2015) 101:613–21. doi: 10.3945/ajcn.114.100065
10. Anjom-Shoae J, Keshteli A, Sadeghi O, Pouraram H, Afshar H, Esmaillzadeh A, et al. Association between Dietary Insulin Index and Load with Obesity in Adults. Eur J Nutr. (2019): [Epub ahead of print]. doi: 10.1007/s00394-019-02012-6
11. Mansouri M, Hasani-Ranjbar S, Yaghubi H, Rahmani J, Tabrizi Y, Keshtkar A, et al. Breakfast Consumption Pattern and Its Association with Overweight and Obesity among University Students: A Population-Based Study. Eat Weight Disord. (2018) doi: 10.1007/s40519-018-0609-8
12. Mansouri M, Miri A, Varmaghani M, Abbasi R, Taha P, Ramezani S, et al. Vitamin D Deficiency in Relation to General and Abdominal Obesity among High Educated Adults. Eat Weight Disord. (2019) 24:83–90. doi: 10.1007/s40519-018-0511-4
13. Sadeghi O, Askari G, Maghsoudi Z, Ghiasvand R, Khorvash F. The Association between Abdominal Obesity and Characteristics of Migraine Attacks in Iranian Adults. Iran J Nurs Midwifery Res. (2016) 21:271–7. doi: 10.4103/1735-9066.180378
14. Isacco L, Miles-Chan J. Gender-Specific Considerations in Physical Activity, Thermogenesis and Fat Oxidation: Implications for Obesity Management. Obes Rev. (2018) 19:73–83. doi: 10.1111/obr.12779
15. Van den Berk-Clark C, Secrest S, Walls J, Hallberg E, Lustman P, Schneider F, et al. Association between Posttraumatic Stress Disorder and Lack of Exercise, Poor Diet, Obesity, and Co-Occuring Smoking: A Systematic Review and Meta-Analysis. Health Psychol. (2018) 37:407–16. doi: 10.1037/hea0000593
16. Loef M, Walach H. The Combined Effects of Healthy Lifestyle Behaviors on All Cause Mortality: A Systematic Review and Meta-Analysis. Prev Med. (2012) 55:163–70. doi: 10.1016/j.ypmed.2012.06.017
17. Bullo M, Garcia-Aloy M, Martinez-Gonzalez M, Corella D, Fernandez-Ballart J, Fiol M, et al. Association between a Healthy Lifestyle and General Obesity and Abdominal Obesity in an Elderly Population at High Cardiovascular Risk. Prev Med. (2011) 53:155–61. doi: 10.1016/j.ypmed.2011.06.008
18. Dhana K, Haines J, Liu G, Zhang C, Wang X, Field A, et al. Association between Maternal Adherence to Healthy Lifestyle Practices and Risk of Obesity in Offspring: Results from Two Prospective Cohort Studies of Mother-Child Pairs in the United States. BMJ. (2018) 362:k2486. doi: 10.1136/bmj.k2486
19. Esmaillzadeh A, Azadbakht L. Major Dietary Patterns in Relation to General Obesity and Central Adiposity among Iranian Women. J Nutr. (2008) 138:358–63. doi: 10.1093/jn/138.2.358
20. Bull F, Dvorak J. Tackling Chronic Disease through Increased Physical Activity in the Arab World and the Middle East: Challenge and Opportunity. Br J Sports Med. (2013) 47:600–2. doi: 10.1136/bjsports-2012-092109
21. Khattab A, Javaid A, Iraqi G, Alzaabi A, Ben Kheder A, Koniski M, et al. Smoking Habits in the Middle East and North Africa: Results of the Breathe Study. Respir Med. (2012) 106:S16–24. doi: 10.1016/s0954-611170011-2
22. Adibi P, Keshteli A, Esmaillzadeh A, Afshar H, Roohafza H, Bagherian-Sararoudi R, et al. The Study on the Epidemiology of Psychological, Alimentary Health and Nutrition (Sepahan): Overview of Methodology. J Res Med Sci. (2012) 17:S292–8.
23. Keshteli A, Esmaillzadeh A, Rajaie S, Askari G, Feinle-Bisset C, Adibi PA. Dish-Based Semi-Quantitative Food Frequency Questionnaire for Assessment of Dietary Intakes in Epidemiologic Studies in Iran: Design and Development. Int J Prev Med. (2014) 5:29–36.
24. Kimura Y, Wada T, Okumiya K, Ishimoto Y, Fukutomi E, Kasahara Y, et al. Eating Alone among Community-Dwelling Japanese Elderly: Association with Depression and Food Diversity. J Nutr Health Aging. (2012) 16:728–31. doi: 10.1007/s12603-012-0067-3
25. Sadeghi O, Hassanzadeh-Keshteli A, Afshar H, Esmaillzadeh A, Adibi P. The Association of Whole and Refined Grains Consumption with Psychological Disorders among Iranian Adults. Eur J Nutr. (2019) 58:211–25. doi: 10.1007/s00394-017-1585-x
26. Health Do. The General Practice Physical Activity Questionnaire (GPPAQ): A Screening Tool to Assess Adult Physical Activity Levels, within Primary Care. Geneva: Health Do (2009).
27. Promoting N. Creating Built or Natural Environments That Encourage and Support Physcial Activity: Scope. London: National Institute for Health and Clinical Excellence (2006).
28. Schmitz N, Kruse J, Heckrath C, Alberti L, Tress W. Diagnosing Mental Disorders in Primary Care: The General Health Questionnaire (Ghq) and the Symptom Check List (Scl-90-R) as Screening Instruments. Soc Psychiatry Psychiatr Epidemiol. (1999) 34:360–6. doi: 10.1007/s001270050156
29. Montazeri A, Harirchi A, Shariati M, Garmaroudi G, Ebadi M, Fateh A. The 12-Item General Health Questionnaire (Ghq-12): Translation and Validation Study of the Iranian Version. Health Qual Life Outcomes. (2003) 1:66. doi: 10.1186/1477-7525-1-66
30. Kennedy E. Putting the pyramid into action: the healthy eating index and food quality score. Asia Pac J Clin Nutr. (2008) 17:70–4.
31. Sadeghi O, Shayanfar M, Mohammad-Shirazi M, Sharifi G, Esmaillzadeh A. A case-control study on dietary quality indices and glioma. Br J Nutr. (2019) [Epub ahead of print]. doi: 10.1017/s0007114519000953
32. Ncepne Panel. Third Report of the National Cholesterol Education Program (Ncep) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel Iii) Final Report. Circulation. (2002) 106:3143–421.
33. Lean M, Han T, Morrison C. Waist circumference as a measure for indicating need for weight management. BMJ. (1995) 311:158–61. doi: 10.1136/bmj.311.6998.158
34. Carbone S, Canada J, Billingsley H, Siddiqui M, Elagizi A, Lavie C. Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag. (2019) 15:89–100. doi: 10.2147/vhrm.s168946
35. Hasegawa K, Komiyama M, Takahashi Y. Obesity and cardiovascular risk after quitting smoking: the latest evidence. Eur Cardiol. (2019) 14:60–1. doi: 10.15420/ecr.2019.4.2
36. Lee M, Lee M, Oh K. Adipose tissue-derived signatures for obesity and type 2 diabetes: adipokines, batokines and micrornas. J Clin Med. (2019) 8:854. doi: 10.3390/jcm8060854
37. Shook R, Halpin K, Carlson J, Davis A, Dean K, Papa A, et al. Adherence with multiple national healthy lifestyle recommendations in a large pediatric center electronic health record and reduced risk of obesity. Mayo Clin Proc. (2018) 93:1247–55. doi: 10.1016/j.mayocp.2018.04.020
38. Garralda-Del-Villar M, Carlos-Chilleron S, Diaz-Gutierrez J, Ruiz-Canela M, Gea A, Martinez-Gonzalez M, et al. Healthy lifestyle and incidence of metabolic syndrome in the sun cohort. Nutrients. (2018) 11:10065. doi: 10.3390/nu11010065
39. Leiva A, Petermann-Rocha F, Martinez-Sanguinetti M, Troncoso-Pantoja C, Concha Y, Garrido-Mendez A, et al. [Association of a healthy lifestyle index with cardiovascular risk factors in chileans adults]. Rev Med Chil. (2018) 146:1405–14. doi: 10.4067/s0034-98872018001201405
40. Schlesinger S, Neuenschwander M, Schwedhelm C, Hoffmann G, Bechthold A, Boeing H, et al. Food groups and risk of overweight, obesity, and weight gain: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr. (2019) 10:205–18. doi: 10.1093/advances/nmy092
41. Larson K, Bundy A, Alvine T, Roemmich J. Paternal high fat diet and exercise differentially regulate placental development and inflammation in a sex-specific manner in C57bl6/J Mice (P19-003-19). Curr Dev Nutr. (2019) 3(Suppl 1):19–13. doi: 10.1093/cdn/nzz049.P19-003-19
42. Yan H, Cao S, Li Y, Zhang H, Liu J. Reduced meal frequency alleviates high-fat diet-induced lipid accumulation and inflammation in adipose tissue of pigs under the circumstance of fixed feed allowance. Eur J Nutr. (2019) [Epub ahead of print]. doi: 10.1007/s00394-019-01928-3
43. Chang H, Munroe S, Gray K, Porta G, Douaihy A, Marsland A, et al. The role of substance use, smoking, and inflammation in risk for suicidal behavior. J Affect Disord. (2019) 243:33–41. doi: 10.1016/j.jad.2018.09.005
44. Ong A, Williams D. Lifetime discrimination, global sleep quality, and inflammation burden in a multiethnic sample of middle-aged adults. Cultur Divers Ethnic Minor Psychol. (2019) 25:82–90. doi: 10.1037/cdp0000233
45. Izaola O, de Luis D, Sajoux I, Domingo J, Vidal M. [Inflammation and Obesity (Lipoinflammation)]. Nutr Hosp. (2015) 31:2352–8.
46. Cheng E, Burrows R, Correa P, Güichapani C, Blanco E, Gahagan S. Light smoking is associated with metabolic syndrome risk factors in chilean young adults. Acta Diabetol. (2019) 56:473–9. doi: 10.1007/s00592-018-1264-2
47. Clair C, Chiolero A, Faeh D, Cornuz J, Marques-Vidal P, Paccaud F, et al. Dose-dependent positive association between cigarette smoking, abdominal obesity and body fat: cross-sectional data from a population-based survey. BMC Public Health. (2011) 11:23. doi: 10.1186/1471-2458-11-23
48. Barrett-Connor E, Khaw K. Cigarette smoking and increased central adiposity. Ann Intern Med. (1989) 111:783–7. doi: 10.7326/0003-4819-111-10-783
49. Akbartabartoori M, Lean M, Hankey C. Relationships between cigarette smoking, body size and body shape. Int J Obes. (2005) 29:236–43. doi: 10.1038/sj.ijo.0802827
50. Rutters F, Pilz S, Koopman A, Rauh S, Pouwer F, Stehouwer C, et al. Stressful life events and incident metabolic syndrome: the hoorn study. Stress. (2015) 18:507–13. doi: 10.3109/10253890.2015.1064891
51. Brunner E, Chandola T, Marmot M. Prospective effect of job strain on general and central obesity in the whitehall ii study. Am J Epidemiol. (2007) 165:828–37. doi: 10.1093/aje/kwk058
52. Ans A, Anjum I, Satija V, Inayat A, Asghar Z, Akram I, et al. Neurohormonal regulation of appetite and its relationship with stress: a mini literature review. Cureus. (2018) 10:e3032. doi: 10.7759/cureus.3032
Keywords: lifestyle, diet, obesity, body mass index, waist circumference
Citation: Sadeghi O, Eshaghian N, Keshteli AH, Askari G, Esmaillzadeh A and Adibi P (2024) Association of combined healthy lifestyle with general and abdominal obesity. Front. Nutr. 10:1332234. doi: 10.3389/fnut.2023.1332234
Received: 02 November 2023; Accepted: 18 December 2023;
Published: 16 January 2024.
Edited by:
Weimin Ye, Karolinska Institutet (KI), SwedenReviewed by:
Andrea Rigby, Penn State Health Medical Group – Middletown, United StatesSalvatore Vaccaro, IRCCS Local Health Authority of Reggio Emilia, Italy
Copyright © 2024 Sadeghi, Eshaghian, Keshteli, Askari, Esmaillzadeh and Adibi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad Esmaillzadeh, YS1lc21haWxsemFkZWhAdHVtcy5hYy5pcg==
 Omid Sadeghi
Omid Sadeghi Niloofar Eshaghian
Niloofar Eshaghian Ammar Hassanzadeh Keshteli3
Ammar Hassanzadeh Keshteli3 Ahmad Esmaillzadeh
Ahmad Esmaillzadeh Peyman Adibi
Peyman Adibi