
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 26 July 2023
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1235271
This article is part of the Research Topic Dietary Patterns Affecting Cardiovascular Health View all 23 articles
 Yue Zhang1*†
Yue Zhang1*† Zheng Luo2†
Zheng Luo2† Juan Yi3†
Juan Yi3† Junjie Zhu4
Junjie Zhu4 Yun Qiu5
Yun Qiu5 Xiaoyun Xu2
Xiaoyun Xu2 Wanying Xie6
Wanying Xie6 Jinyi Wu7
Jinyi Wu7 Huihui Lv8
Huihui Lv8 Changhua Mou9
Changhua Mou9 Wei Zhang2*
Wei Zhang2* Xiaopan Li10*
Xiaopan Li10*Objectives: This study aimed to compare the burden and trends of stroke attributed to dietary risk factors in the Belt and Road (“B&R”) countries from 1990 to 2019.
Methods: The 2019 Global Burden of Disease (GBD) Study was used to gather information on the burden of stroke attributable to dietary risk factors. Numbers and age-standardized rates (ASRs) of deaths, disability-adjusted life years (DALYs) were determined in 1990 and 2019 among the “B&R” countries. The average annual percent change (AAPC) was used to analyze the temporal trends of diet-induced stroke DALYs from 1990 to 2019 and in the final decade (2010–2019) by Joinpoint regression analysis.
Results: In 2019, the absolute number of stroke deaths and DALYs attributable to dietary risk factors were 671,872 cases (95% UI 436,354–937,093) and 1.67 million cases (95% UI 1.15–2.24) in China. We found geographical differences in mortality and DALYs of diet-attributable stroke among member countries, with Bulgaria, Hungary and Serbia being the three highest countries in 1990, Bulgaria, North Macedonia and Montenegro in Central Asia in 2019. The ASRs of diet-induced stroke mortality and DALYs were generally declining in most member states from 1990 to 2019, however, the corresponding metrics in Mongolia remained high. The fastest decline in ASR of mortality and DALYs for diet-induced stroke was seen in Estonia, Eastern Europe, with AAPC values of −7.09% (95%CI: −7.72, −6.46%) and − 6.62% (95%CI: −7.20, −6.03%), respectively. We noted a substantial downward trend in ASR of mortality and DALYs from diet-induced stroke changes in the final decade (2010–2019) for most member states. The ASR of DALYs for diet-induced stroke decreased greater in females than in males. For those aged 50–74, the DALYs for stroke due to dietary risk factors in all other member countries of the “B&R” showed a decreasing trend, except for the Philippines, which rose (AAPC = 2.13, 95%CI: 1.40–2.87%) and Turkmenistan, which remained stable (AAPC = 0.05, 95%CI: −0.43–0.33%).
Conclusion: The burden of diet-induced stroke varies substantially across “B&R” countries and threaten public health, relevant evidence-based policies and interventions should be adopted to address the future burden of stroke in “B&R” countries through extensive collaboration.
Stroke is a global public health problem that imposes a heavy disease and financial burden on individuals and society. According to the 2019 Global Burden of Disease, Injury and Risk Factor Study (GBD 2019), stroke was the second-leading cause of death (11.6% of total deaths) and third-leading cause of disability (5.7% of total disability-adjusted life years [DALYs]) worldwide (1). Stroke incidence has maintained stable and mortality have declined over the last 20 year-period, however, DALYs due to stroke and stroke-related survivors have all increased, making stroke prevention a global health priority (2). American Heart Association (AHA) predicts that stroke incidence could reach 4% by 2030 among American adults, resulting in an increase in stroke-related medical costs to $183 billion (3). Additionally, GBD shows that more than 75% of stroke deaths and 80% of DALYs occur in low- and middle-income countries (1).
As we all know, health issues are no longer the responsibility of individual countries with the rapid pace of globalization. In 2013, Chinese government initiates the Belt and Road Initiative (BRI) to accelerate infrastructure, trade development and business partnerships among 66 countries in Asia, Europe, South America and Africa (4, 5). Although the BRI focuses on economic development and infrastructure investment, its impact on global health is emerging (6). In 2017, Chinese government launched the “Health Silk Road” (HSR) initiative to strengthen global health cooperation. Under the framework of HSR, a variety of regional and trans-regional plans have been implemented, including the training of health professionals, the establishment of disease control centers, and the creation of knowledge sharing networks. Through the HSR, China could use BRI transportation networks to provide health care and medical assistance to member countries. Against the backdrop of COVID-19, the BRI provides an important platform for member counties to discuss clinical treatment guidelines and epidemic control strategies (7, 8). Currently, member countries face the threat of stroke to varying degrees, and the distribution of risk factors is constantly changing, so analyzing the differences between member states is essential to allocate resources for prevention strategies (1, 9).
Recent epidemiological evidence has found that the large burden of stroke can be attributed to several modifiable factors, such as obesity, hypertension, diabetes, a sedentary lifestyle, or unhealthy diet (10). Diet is an important risk factor for stroke, a growing number of prospective observational studies have been performed to explore the impact of dietary factors on stroke risk (11). English et al. (12) found that poor diet and nutritional intake were strongly associated with the risk of first stroke, and a Mediterranean-style diet was reported to reduce the risk of first stroke. Baden et al. (13) explored the relationship between plant-based diet quality and total stroke risk and found that people who adhered to a healthy plant-based diet had a lower risk of total stroke.
The GBD 2019 framework, through extensive collection of data sources and statistical modeling, allows for comparable assessment of stroke burden in terms of mortality and DALYs. At present, none of the existing studies on stroke mortality and DALYs attributable to modifiable dietary risk factors had explored differences and the changing trend of DALYs stratified by gender, age and diet-specific risk factors among 66 countries from the BRI. Therefore, this study was conducted to compare the burden and trends of diet-induced stroke from 1990 to 2019 in the “B&R” countries, and to provide the basis for generating prevention and control strategies of stroke for building a healthy “B&R.”
In this study, data on annual diet-induced stroke deaths, DALYs, and respective age-standardized rates (ASR) by gender, age and specific diet risk factor in the “B&R” countries from 1990 to 2019 were extracted from the GBD 2019 database.1 The GBD 2019, which is an international collaborative surveillance system, estimated 369 diseases and injuries, 87 risk factors and combinations of risk factors across 204 countries and territories from 1990 to 2019. It contains a total of 86,249 data input sources from censuses, household surveys, civil registration, vital statistics and other sources. The GBD 2019 Stroke Collaborators has presented methods for processing, standardizing, and modeling stroke mortality and DALYs (1). GBD estimates the burden of disease indices including incidence, prevalence, mortality, years lived with disability (YLD), years of life lost (YLL) and DALYs at regional, national and global levels. Detailed methodology has been published elsewhere (14, 15). The detailed information on the statistical codes for diet-related burden in the GBD study has been previously announced on the following website: http://ghdx.healthdata.org/gbd-2019/code/nonfatal-12. DALYs is a composite indicator to assess the disease burden of disability and premature death, which is obtained by summing YLL and YLD.
The composition of “B&R” countries is mainly based on the GBD classification of global regions and international political and economic organizations (16). BRI include 66 member countries, divided as follows: (1) East Asia: China, (2) Central Asia: Armenia, Azerbaijan, Georgia, Kazakhstan, Turkmenistan, Uzbekistan, Kyrgyzstan, Mongolia, Tajikistan, (3) South Asia: India, Nepal, Bangladesh, Bhutan, Pakistan, (4) Southeast Asia: Philippines, Sri Lanka, Thailand, Indonesia, Vietnam, Cambodia, Laos, Malaysia, Maldives, Burma, (5) High-income Asia pacific: Brunei, Singapore, (6) North Africa and Middle East: Jordan, Kuwait, Lebanon, Oman, Afghanistan, Yemen, Bahrain, Iran, Iraq, United Arab Emirates, Qatar, Saudi Arabia, Syria, Egypt, Palestine, Turkey, (7) Central Europe: North Macedonia, Poland, Romania, Croatia, Czechia, Bosnia and Herzegovina, Montenegro, Albania, Bulgaria, Hungary, Slovakia, Slovenia, Serbia, (8) Eastern Europe: Republic of Moldova, Russia, Ukraine, Estonia, Lithuania, Belarus, Latvia, and (9) Western Europe: Cyprus, Greece, Israel. To ensure replicability and transparency of results, our study follows the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) (Supplementary Appendix A) (17).
The absolute numbers and ASR of mortality and DALYs for stroke attributed to dietary risks were calculated in “B&R” countries. For estimated metrics, the 95% uncertainty interval (UI) were reported, and 95% UI was calculated by drawing 1,000 times from each number of posterior distributions, using the 2.5th and 97.5th ordering of the uncertainty distribution (1). ASR, as a weighted mean of the age-specific rates, were estimated using a global age structure from 2019, which allow comparisons across time, countries and subregions. We focused on three specific age groups: 20 to 54 years, 50 to 74 years and ≥ 75 years and 6 dietary risk factors (high in sodium, high in red meat, low in fruits, low in vegetables, low in fiber and low in whole grains). The temporal trends of disease burden were assessed using average annual percent change (AAPC) by using the Joinpoint regression software from 1990 to 2019, 95% confidence intervals (CIs) for trend segment identified. The annual ASR of diet-induced stroke mortality and DALYs was designated as a dependent variable, and the year was assigned as an independent variable. The Heteroscedastic Errors Option was set to constant variance, the maximum number of joinpoints was set at 5, and the Log-linear model (ln y = xb) was chosen. For segmented line regression, the Bayesian information criterion (BIC) was used to calculate the optimal number of change points. The software uses a Z-test to check whether the slope for each trend segment is significantly different from prior segment (18).
In addition, we evaluated AAPCs of age-standardized DALYs for stroke, stratified by sex, age and specific dietary factors. Meanwhile, we compared the changes in AAPC of stroke burden attributed to dietary risk factors in the last decade and throughout the study period (1990–2019 and 2010–2019). If both the AAPC estimate and the lower limit of 95% UI were positive, ASR of mortality and DALYs showed an upward trend. Conversely, if both the AAPC estimate and the upper limit of the 95% UI were negative, then ASR of mortality and DALYs exhibited a decreasing trend (setting 3% as the cut-off point and ≥ 3% as a larger decrease). Other than that, ASR was considered to be stable (19). All analysis was conducted using the Joinpoint Regression Program (Version 4.9.0.0, The National Cancer Institute, MD, United States) (20). The map visualization of the “B&R” member states was performed using “ggmap” package in R software (version 4.3.0, R core team). The “ggmap” package is an extension package, which obtains shapefiles from Google Maps.2 p < 0.05 was considered statistically significant.
Absolute number of mortality and DALYs in 1990 and 2019 caused by stroke attributed to modifiable dietary risk factors in the “B&R” member countries are shown in Table 1. In 2019, the number of stroke deaths and DALYs attributable to dietary risks were 671,872 cases (95% UI 436,354–937,093) and 1.67 million cases (95% UI 1.15–2.24) in China. We found geographical differences in mortality and DALYs of diet-attributable stroke among member countries, with Bulgaria, Hungary, and Serbia being the three highest countries in 1990, Bulgaria, North Macedonia, and Montenegro in Central Asia in 2019. The country with the lowest number of mortality and DALYs is the Qatar in North Africa and Middle East (27 cases, 95% UI, 16–42 and 1716 cases, 95% UI, 1112–2,454) in 2019. From 1990 to 2019, the countries with the largest decreases in the number of diet-induced stroke deaths and DALYs were Czechia and Hungary, and the countries with the largest increases were Albania and Mongolia.

Table 1. The absolute number of mortality and DALYs for stroke attributed to dietary risk factors in the “B&R” countries in 1990 and 2019.
Figure 1 illustrated the ASR of diet-induced stroke mortality and DALYs in 1990 and 2019 in member countries of the “B&R” initiative. In 1990, the regions with higher age-standardized mortality and DALYs from diet-related stroke were concentrated in Central Europe, East Asia and Southeast Asia. In 1990, the country with the lowest age-standardized mortality and DALYs of diet-induced stroke was Lebanon (6.76 per 100,000 population and 149.86 per 100,000 population, respectively), the highest in Burma (103.90 per 100,000 population and 2617.69 per 100,000 population, respectively). In 2019, Israel enjoyed the lowest age-standardized mortality and DALYs of diet-induced stroke (13.42 per 100,000 population and 85.08 per 100,000 population, respectively), the highest in Mongolia (90.27 per 100,000 population and 2127.00 per 100,000 population, respectively). The age-standardized mortality and DALYs of stroke attributable to dietary risk factors were generally declining in most member states from 1990 to 2019. However, the mortality and DALYs of diet-induced stroke in Mongolia has remained high. See Supplementary Table S1 for more details.
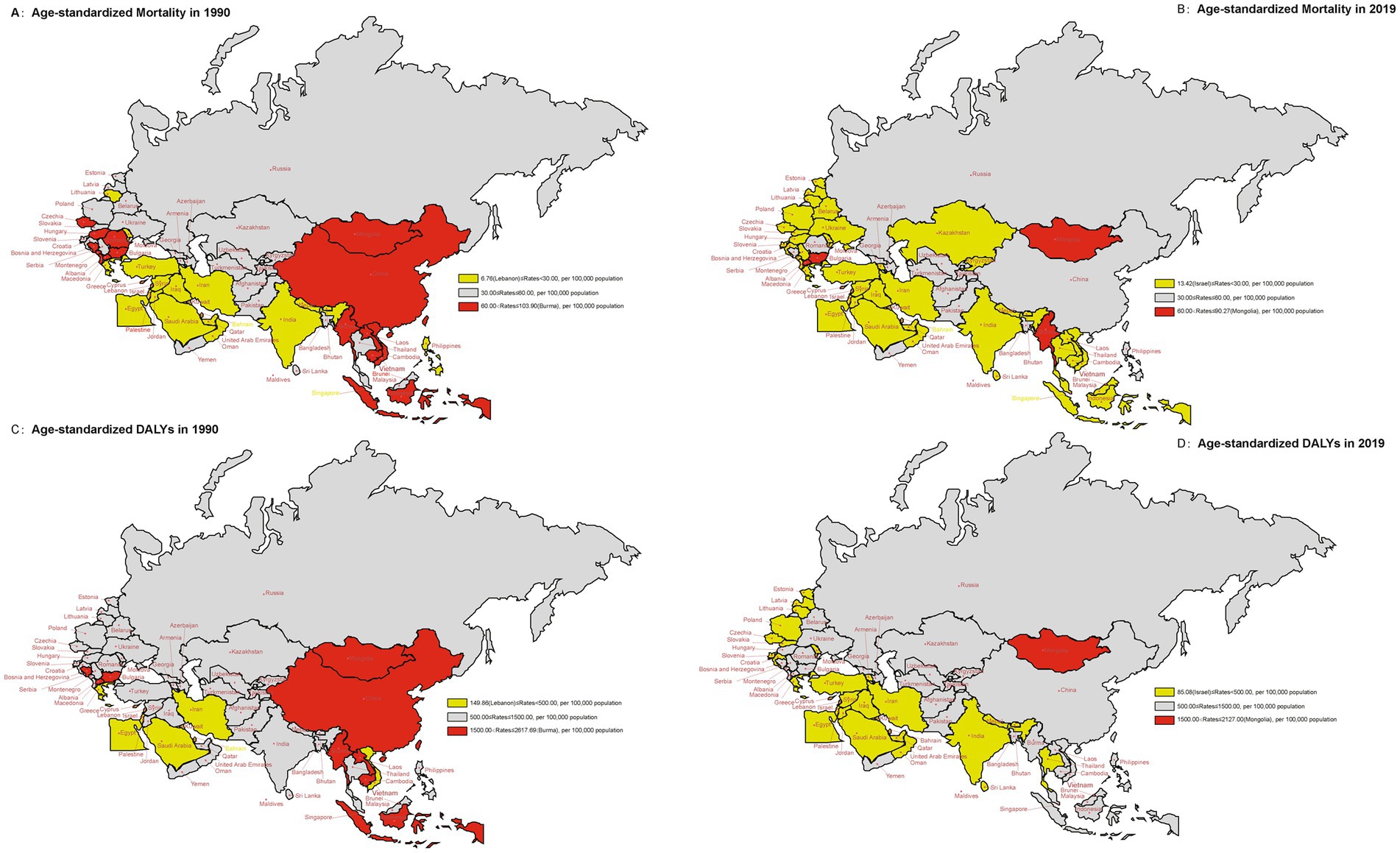
Figure 1. The age-standardized rates of mortality and DALYs due to stroke attributed to dietary risk factors for the “B&R” countries in 1990 and 2019. (A) Age-standardized mortality rate in 1990. (B) Age-standardized mortality rate in 2019. (C) Age-standardized DALYs rate in 1990. (D) Age-standardized DALYs rate in 2019.
The temporal trend of ASR of mortality and DALYs due to diet-induced stroke for 1990–2019 and 2010–2019 in “B&R” countries was displayed in Figure 2. From 1990 to 2019, the fastest decline in ASR of mortality and DALYs for diet-induced stroke was seen in Estonia, Eastern Europe, with AAPC values of −7.09% (95%CI, −7.72, −6.46%) and − 6.62% (95%CI, −7.20, −6.03%), respectively. However, the AAPC of age-standardized metrics showed an increasing trend in Philippines in Southeast Asia (mortality: AAPC = 1.60%; DALYs: AAPC = 2.03%; p < 0.001, respectively). We found no statistically significant differences in AAPC for ASR of diet-induced stroke mortality and DALYs in Kuwait, Mongolia and Turkmenistan in Central Asia and North Africa and Middle East for 1990–2019. In addition, we noted a substantial downward trend in ASR of mortality and DALYs from diet-induced stroke changes in the last decade (2010–2019) for most member states. The ASR of mortality and DALYs due to diet-related stroke in Mongolia remained stable over the full 30 years, yet showed a decreasing trend in the last decade. Trends in age-standardized mortality rates and DALYs for diet-induced stroke in 2010–2019 were not statistically significantly different in Ukraine in Eastern Europe, and Yemen in North Africa and Middle East. See Supplementary Table S2 for more details.
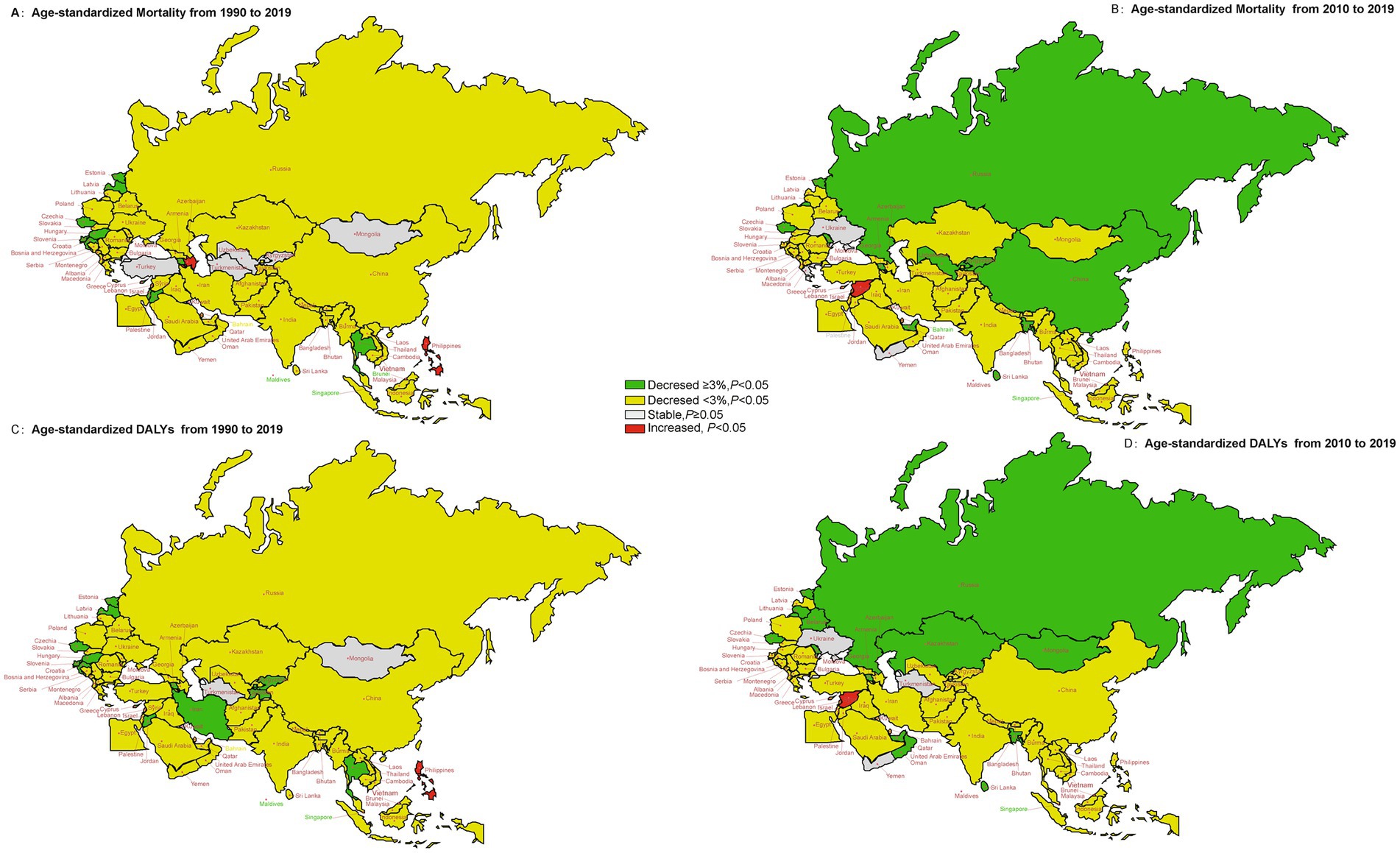
Figure 2. The temporal trend in the age-standardized mortality and DALYs rate of stroke attributed to dietary risk factors for 1990–2019 and 2010–2019 in the “B&R” countries. (A) The AAPC of age-standardized mortality from 1990 to 2019. (B) The AAPC of age-standardized mortality from 2010 to 2019. (C) The AAPC of age-standardized DALYs from 1990 to 2019. (D) The AAPC of age-standardized DALYs from 2010 to 2019.
Figure 3 illustrated the AAPC values of age-standardized DALYs rate in each member country of the “B&R” in males and females. Most of countries in the “B&R” countries showed a downward trend in AAPC, Estonia had the highest decline in AAPCs of age-standardized DALYs from 1990 to 2019 (male: AAPC = −6.55, 95%CI: −7.15 to −5.95%; female: AAPC = −6.70, 95%CI: −7.27 to −6.13%). However, an upward trend for both sexes in Philippine was observed (mortality: AAPC = 2.31, 95%CI: 1.64–2.99%; DALYs: AAPC = 1.65, 95%CI: 1.00–2.30%; p < 0.001, respectively). The ASR of DALYs for diet-induced stroke decreased more in females than in males. For males, the AAPCs in Mongolia, Tajikistan, Pakistan and Lebanon were stable between 1990 and 2019, while the change trend of DALYs was stable for female in Azerbaijan and Egypt (p ≥ 0.05) (Supplementary Table S3).
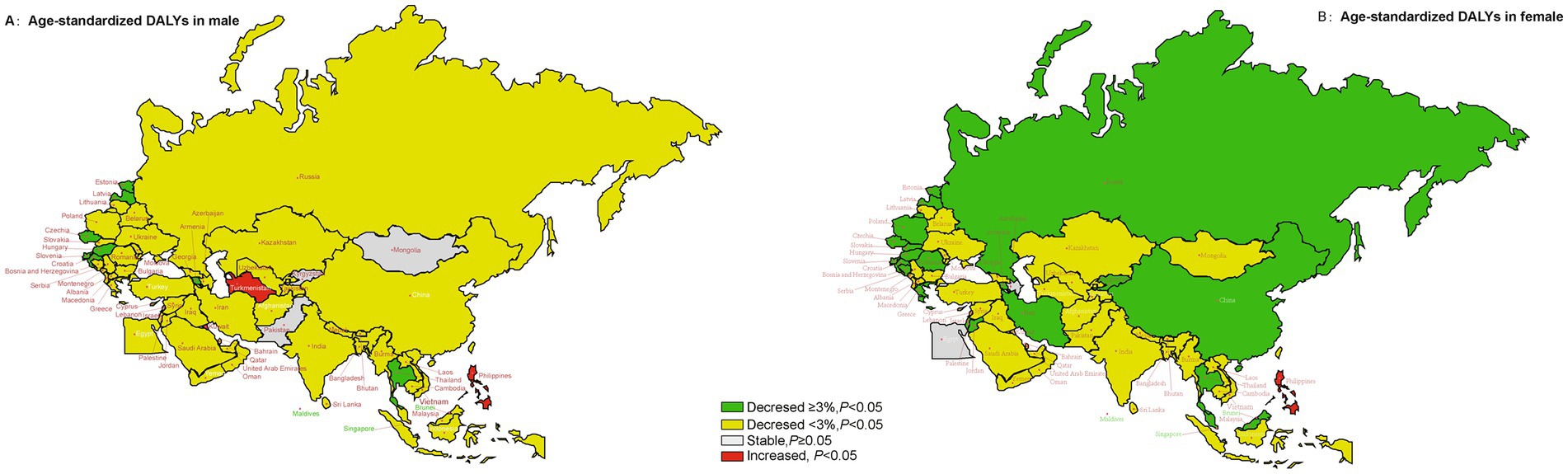
Figure 3. The temporal trend in the age-standardized DALYs rate of stroke attributed to dietary risk factors, stratified by gender for 1990–2019 in the “B&R” countries. (A) The AAPC of age-standardized DALYs rate in male. (B) The AAPC of age-standardized DALYs rate in female.
Figure 4 showed the long-term trends of DALYs rate due to diet-related stroke, stratified by age for 1990–2019 for the “B&R” countries. The DALYs rate for stroke attributable to dietary risk factors showed a decreasing trend in all age groups among the member countries in Europe from 1990 to 2019. For people aged 20–54 years, DALYs showed an increasing trend in Mongolia and Turkmenistan in Central Asia, Philippines and Vietnam in Southeast Asia, Saudi Arabia in North Africa and Middle East. Overall, for those aged 50–74, the DALYs for stroke due to dietary risk factors in all other “B&R” member countries showed a decreasing trend, except for the Philippines, which rose (AAPC = 2.13, 95%CI: 1.40–2.87%) and Turkmenistan, which remained stable (AAPC = 0.05, 95%CI: −0.43–0.33%). For adults aged 75 years or older, the AAPC value of DALYs caused by diet-related stroke showed an increasing trend in Azerbaijan, Tajikistan, Indonesia, Kuwait, and Turkey, however, the AAPC values varied steadily in Mongolia, Uzbekistan, Bangladesh, Pakistan, Philippines, Oman and Montenegro, with no statistical significance. See Supplementary Table S4 for more details.
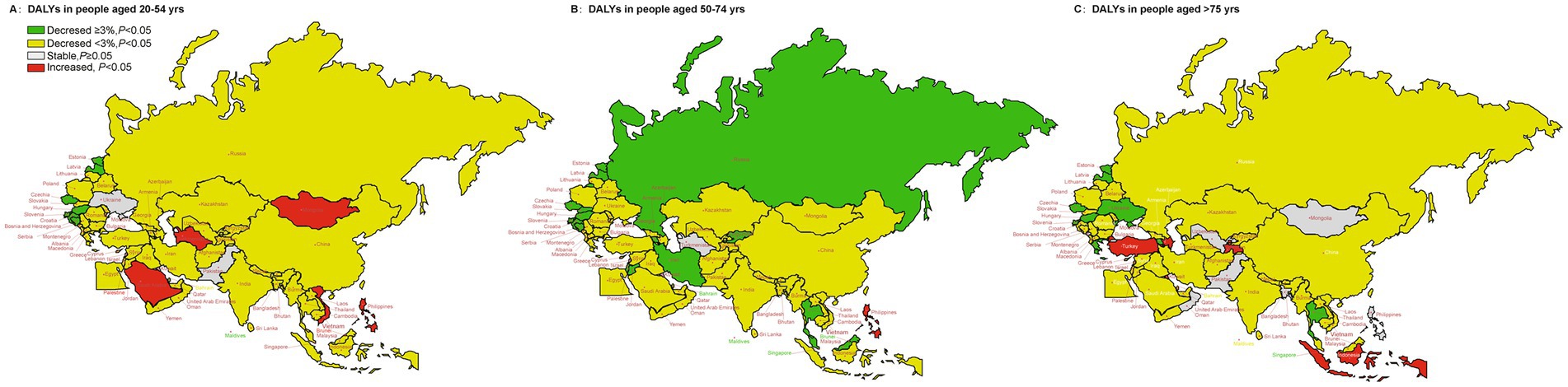
Figure 4. The temporal trend in the DALYs rate of stroke attributed to dietary risk factors, stratified by age for 1990–2019 in the “B&R” countries. (A) The AAPC of DALYs rate in people aged 20–54 years. (B) The AAPC of DALYs rate in people aged 50–74 years. (C) The AAPC of DALYs rate in people aged ≥75 years.
The AAPC of age-standardized rates for DALYs due to stroke, attributable to specific dietary risk factors for 1990–2019 in the “B&R” member countries was displayed in Figure 5. The ASR of stroke attributable to modifiable dietary risk factors in Philippines significantly increased. Regions with high red meat consumption showed an increasing trend in the ASR of stroke DALYs, such as Azerbaijan, Uzbekistan and Turkmenistan in Central Asia, Indonesia, Laos, Burma, Philippines, Vietnam in Southeast Asia, Egypt in North Africa and Middle East, Albania and Bosnia and Herzegovina in Central Europe. From 1990 to 2019, regions with low fruit and vegetable intake showed a decreasing trend in the ASR of stroke DALYs in “B&R” member countries, except for Philippines and United Arab Emirates. Age-standardized DALYs of stroke showed an increasing trend in regions with low intake of whole grains, such as Mongolia, Azerbaijan, Tajikistan and Turkmenistan in Central Asia, Indonesia, Vietnam and Philippines in Southeast Asia, and Egypt in North Africa and Middle East. See Supplementary Table S5 for more details.
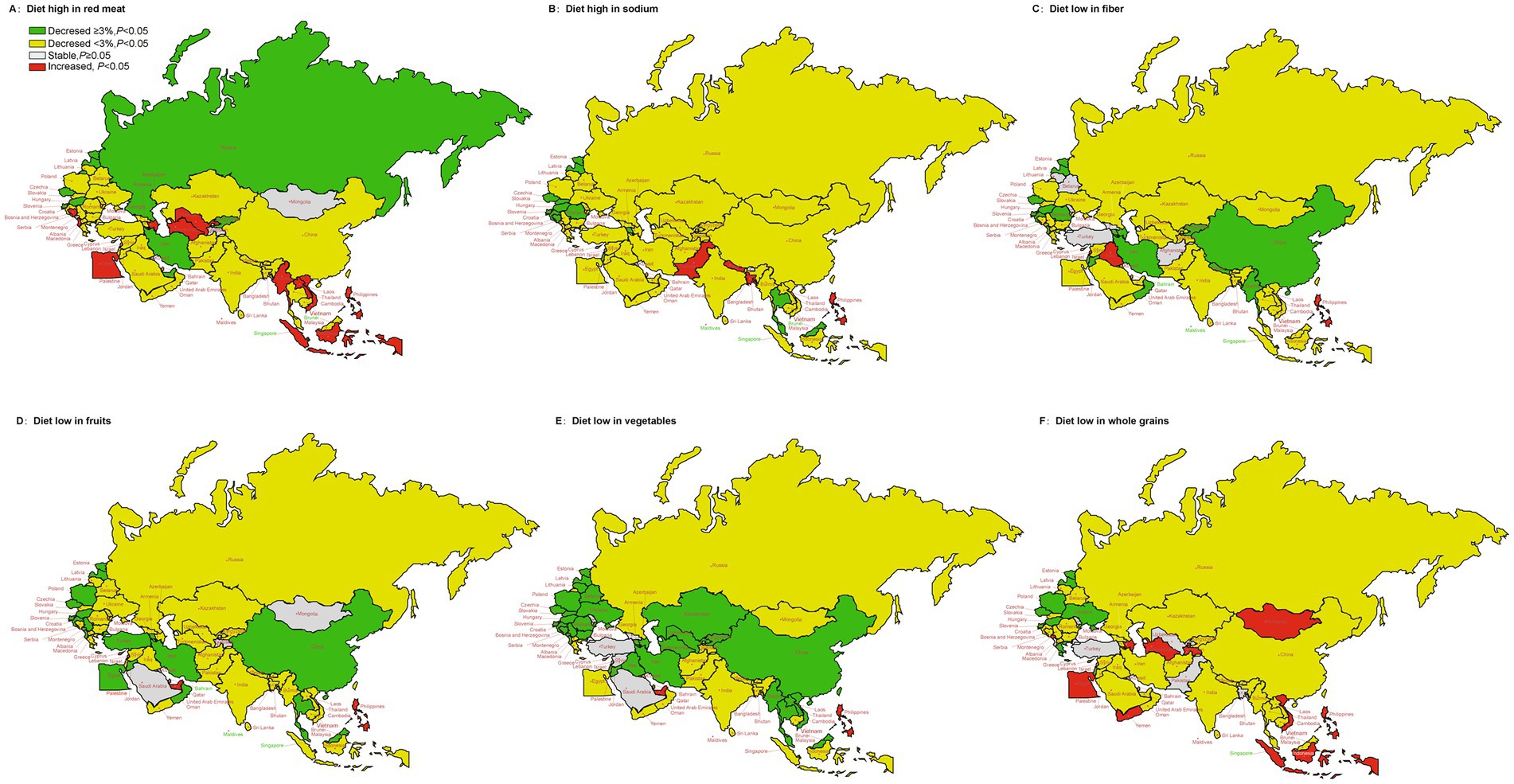
Figure 5. The temporal trend in the DALYs rate of stroke attributed to specific dietary risk factors for 1990–2019 in the “B&R” countries. (A) Diet high in red meat. (B) Diet high in sodium. (C) Diet low in fiber. (D) Diet low in fruits. (E) Diet low in vegetables. (F) Diet low in whole grains.
Based on latest data from the GBD Study 2019, we explored the impact of dietary risks on stroke deaths and DALYs in the member states of the “B&R” over past three decade (1990–2019) and the final decade (2010–2019). The results showed geographical differences in mortality and DALYs of diet-attributable stroke among member countries, the age-standardized mortality and DALYs were generally declining in most member states. The decreases in ASRs of diet-related stroke burden may be attributed to decreases in the improvement of living standard, increased awareness of self-health, improved screening programs, the diagnosis of patients in the early stages of disease and better access to effective therapy (21–23). Bulgaria, Hungary, and Serbia were the three countries with the highest diet-attributable ASR of stroke mortality and DALYs in 1990, and Bulgaria, North Macedonia, and Montenegro in Central Asia in 2019. Central Asian countries have seen a shift from traditional Asian to westernized diets, in addition to dietary risks, diabetes, hypertension and cigarette consumption remain the main risk factors for cardiovascular diseases in this region (24). Another possible explanation for this observation was that the highest percentage of total stroke burden was attributable to YLL, suggesting differences in the quality of acute stroke care in these countries. Lack of education and inadequate preventive measures on the treatment of stroke are also key factors contributing to the progressive stroke burden in Central Asia (25). We also found that the mortality and DALYs of diet-induced stroke in Mongolia remained high. It was reported that in Mongolia, low intake of vegetables and fruits resulted in morbidity and mortality of cardiovascular disease that greatly exceed those of Western countries (26). A substantial downward trend in ASR of mortality and DALYs from diet-induced stroke in the final decade (2010–2019) for most member states, compared to the past 3 decades. This phenomenon may be explained by the improvement of stroke awareness in the community, economic development, increased numbers of neurologists, government insurance coverage and so on.
Findings from this study found that the fastest decline in ASR of mortality and DALYs for diet-induced stroke was seen in Estonia, Eastern Europe. Estonia has established detailed stroke registration and management system since the 1970s, and the results of the third population-based stroke register in 2005 showed a decrease in stroke incidence and 28 days case fatality rates compared to the previous decade (27, 28). Furthermore, we noted that the AAPC of age-standardized metrics showed an increasing trend in Philippines in Southeast Asia. A study found that stroke mortality in Philippines has remained high over the past decade, which is similar to our findings (29). In low- and middle-income countries, dietary patterns are changing considerably, such as the replacement of staple-based diets with increased fat, meat and salt intakes (30). Numerous epidemiological studies have focused on dietary habits, as one of the modifiable risk factors and their impact on stroke risk, found a strong association between low-quality diet and stroke risk, however adherence to Mediterranean-style diet pattern has been pointed out to decrease the risk of first stroke (12, 31). Rosato et al. (32) confirmed that dietary patterns of the “B&R” Mediterranean countries exerted a protective effect on the risk of stroke. The Philippines is constantly facing the enormous burden of malnutrition, especially among adults suffering from various forms of malnutrition, and there has also been a noticeable change in food consumption (33, 34). The 2018 Expanded National Nutrition Survey in Philippines analyzed the relationship between food intake and diet quality, and found that the breakfast that Filipinos regularly eat was not nutritious enough (35). This partly explains the increasing trend of diet-induced stroke DALYs in Philippines over the 30 years period.
Meanwhile, our study found that the temporal trends of diet-induced stroke DALYs varied considerably by sex, age and specific dietary risk factors. Females displayed lower negative AAPCs than males in most member counties, suggesting a higher downturn in ASR in females. Gender is a key risk factor for cardiovascular diseases, with biological sex (determined by sex chromosomes and gonadal hormones) and gender (social and cultural behaviors) influencing differences in disease susceptibility and pathology between men and women (36). Thus, this discrepancy is likely due to the different distribution of stroke risk factors between genders and other pathophysiological factors, such as the protective impact of estrogen for females (37). The DALYs rate for diet-induced stroke showed a decreasing trend in all age groups among the member countries in Europe. Dokova et al. (38) found that ASR of stroke DALY declined in West, Central, and East Europe regions and in all twenty East and Central European countries but at a different pace, which is consistent with our study. For those aged 50–74, the DALYs for stroke due to dietary risk factors in all other “B&R” member countries showed a decreasing trend, except for the Philippines, which rose and Turkmenistan, which remained stable. As we have discussed above, inadequate stroke units and rehabilitation facilities, lack of education on stroke prevention and treatment, and traditional diet pattern (high nutrient and fibrous) contribute to the high DALYs of stroke in Central Asia.
Evidence suggested that the main dietary risk factors for deaths and DALYs were low in whole grains, high in sodium, low in fruits and vegetables globally and in many countries (39). Wang et al. (40) demonstrated that ASR of stroke mortality attributable to high sodium intake showed a downward trend from 1990 to 2019 in China, which was consistent with our results. In China, the daily sodium intake was the highest worldwide and started to decrease from 15 g in 1988 (41) to 4.7 g in 2016 (42), therefore, ASR for stroke mortality due to high sodium intake showed a downward trend. This suggests that the implementation of salt reduction policies has had a significant influence on the reduction of stroke mortality and DALYs. It has been observed that age-standardized DALYs of stroke showed an upward tendency in regions with low intake of whole grains, such as Mongolia, Azerbaijan, Tajikistan and Turkmenistan in Central Asia, Indonesia, Vietnam and Philippines in Southeast Asia, and Egypt in North Africa and Middle East, which belonged to low- and middle-income countries. A review article reports that in low- and middle-income countries, consumption of animal-derived foods, oils and sugar is increasing, while consumption of whole grains is low (43). Additionally, dietary fiber is found in fruits and vegetables, and it has been shown to reduce the risk of stroke. A balanced diet is one of the essential elements of a healthy lifestyle, according to studies showing that two-fifths of acute ischemic stroke episodes can be prevented (44). Current comparative risk assessments may significantly underestimate the protective effect of fruit and vegetable intake on stroke. In fact, other factors such as economic income, educational level, and dietary environment have an impact on food choice and diet quality (45). In order to improve diet quality, active collaboration in different areas is necessary given the complexity of dietary practices and the diversity of impacts on diet. Besides, the important contribution of potential interactions or synergistic effects between different dietary risk factors to stroke burden should also be considered. By evaluating and comparing the ASR of diet-induced stroke mortality and DALYs in the “B&R” countries, it is found that different countries face different diet-related stroke challenges. Therefore, under the HSR framework, establishing scientific and effective dietary policy applicable to each country, and improving diet quality will remain the key measures of stroke in “B&R” countries.
Based on the broadest epidemiological dataset available to date, this study analyzes estimates of stroke mortality and DALYs attributable to dietary risk factors from 1990 to 2019, and the corresponding changes in the last decade for the first time. Meanwhile temporal trend in diet-induced stroke DALYs were also explored by sex, age, and specific dietary factors. The main strength is the data collection of “B&R” member countries using the same methods and modeling used in the GBD study. Several limitations exist in this study. Firstly, dietary risks from GBD dataset were not strictly categorized, for example vegetables, fruits and whole grains are all rich in fiber, to some extent they overlap with the fiber group. Also, we did not consider potential interactions or synergistic effects between different dietary risk factors. Secondly, underreporting or misclassification of stroke cases existed in each member country due to different diagnostic criteria, definition and measurement of dietary risk are not the same around the “B&R” countries. Thirdly, given the diversity of whole grain products, it is quite difficult to accurately measure intake, which can lead to measurement errors. Fourthly, while certain confounders (smoking, drinking, BMI) were taken into account in the GBD framework, other variables, such as socioeconomic status and access to healthcare, could still be sources of bias. Finally, our study is based on a secondary analysis of GBD, thus GBD all limitations also apply to our study, which is why age groups were not mutually exclusive in this analysis.
This study compared stroke mortality and DALYs attributable to dietary risk factors from 1990 to 2019, and the corresponding changes in the last decade, and explored the temporal trend of ASR for diet-induced stroke DALYs stratified by gender, age and specific dietary risk factors in “B&R” countries in the past three decades. We found geographical differences in mortality and DALYs for diet-induced stroke among member countries, with a general downward trend in these indicators from 1990 to 2019 in most member countries. A substantial downward trend in ASR of mortality and DALYs from diet-induced stroke changes in the final decade. Notably, the AAPCs of age-standardized stroke mortality and DALYs attributable to dietary risk factors significantly increased in Philippines. The ASR of DALYs for diet-induced stroke decreased more in females than in males. Therefore, prioritization of public health interventions among “B&R” member countries should be evidence-based and data-driven to address the risks and challenges posed by diet-induced stroke through enhanced health collaboration and resource sharing.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
YZ and XL conceived and designed the study. YZ, XL, JW, JZ, and YQ analyzed the data. ZL, JY, WX, HL, CM, XX, and WZ provided advice and consultation. YZ wrote the manuscript. All authors read and approved the submitted manuscript.
This work was supported by the Basic Research Program of Shanxi Province (Free exploration) project (20210302123216 to YZ), the Science and Technology Innovation Project of Higher Education Institutions in Shanxi Province (2021L221 to YZ), the Special Disease Construction Project of Pudong Health and Family Planning Commission of Shanghai (Grant No. PWZzb2022-20 to ZL), Discipline Construction Project of Pudong Health and Family Planning Commission of Shanghai (Grant No. PWYts2021-02 to ZL), and the General Program of Health Bureau of the Shanghai (202150015 to ZL). All authors had full access to all data in the study and had responsibility for the decision to submit for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1235271/full#supplementary-material
1. GBD 2019 Stroke Collaborators . Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
3. Heidenreich, PA , Trogdon, JG , Khavjou, OA , Butler, J , Dracup, K , Ezekowitz, MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. (2011) 123:933–44. doi: 10.1161/CIR.0b013e31820a55f5
4. Liu, W , Hughes, AC , Sachdeva, G , Narain, D , Zhou, T , Wang, Y, et al. The belt and road initiative and the sustainable development goals. One Earth. (2020) 3:263–7. doi: 10.1016/j.oneear.2020.08.020
5. Tang, K , Li, Z , Li, W , and Chen, L . China's silk road and global health. Lancet. (2017) 390:2595–601. doi: 10.1016/S0140-6736(17)32898-2
6. Hu, R , Liu, R , and Hu, N . China's belt and road initiative from a global health perspective. Lancet Glob Health. (2017) 5:e752–3. doi: 10.1016/S2214-109X(17)30250-4
7. Zeng, PW , Bouey, PJ , Dossani, DR , Wang, DH , and Li, PG . The belt and road initiative and disease control amid the COVID-19 pandemic. J Travel Med. (2021) 28:taab034. doi: 10.1093/jtm/taab034
8. Huang, Y . The health silk road: how China adapts the belt and road initiative to the COVID-19 pandemic. Am J Public Health. (2022) 112:567–9. doi: 10.2105/AJPH.2021.306647
9. Ma, Q , Li, R , Wang, L , Yin, P , Wang, Y , Yan, C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the global burden of disease study 2019. Lancet Public Health. (2021) 6:e897–906. doi: 10.1016/S2468-2667(21)00228-0
10. Harshfield, EL , Georgakis, MK , Malik, R , Dichgans, M , and Markus, HS . Modifiable lifestyle factors and risk of stroke: a Mendelian randomization analysis. Stroke. (2021) 52:931–6. doi: 10.1161/STROKEAHA.120.031710
11. Guo, N , Zhu, Y , Tian, D , Zhao, Y , Zhang, C , Mu, C, et al. Role of diet in stroke incidence: an umbrella review of meta-analyses of prospective observational studies. BMC Med. (2022) 20:194. doi: 10.1186/s12916-022-02381-6
12. English, C , MacDonald-Wicks, L , Patterson, A , Attia, J , and Hankey, GJ . The role of diet in secondary stroke prevention. Lancet Neurol. (2021) 20:150–60. doi: 10.1016/S1474-4422(20)30433-6
13. Baden, MY , Shan, Z , Wang, F , Li, Y , Manson, JE , Rimm, EB, et al. Quality of plant-based diet and risk of total, ischemic, and hemorrhagic stroke. Neurology. (2021) 96:e1940–53. doi: 10.1212/WNL.0000000000011713
14. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
15. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
16. Murray, CJ , Ezzati, M , Flaxman, AD , Lim, S , Lozano, R , Michaud, C, et al. GBD 2010: design, definitions, and metrics. Lancet. (2012) 380:2063–6. doi: 10.1016/S0140-6736(12)61899-6
17. Stevens, GA , Alkema, L , Black, RE , Boerma, JT , Collins, GS , Ezzati, M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. PLoS Med. (2016) 13:e1002056. doi: 10.1371/journal.pmed.1002056
18. Chen, H , Zhou, Z , Li, Z , Liang, S , Zhou, J , Zou, G, et al. Time trends in the burden of stroke and subtypes attributable to PM2.5 in China from 1990 to 2019. Front Public Health. (2022) 10:1026870. doi: 10.3389/fpubh.2022.1026870
19. Wang, H , Zhang, H , and Zou, Z . Changing profiles of cardiovascular disease and risk factors in China: a secondary analysis for the global burden of disease study 2019. Chin. Med. J. Publish Ahead of Print. (2023). doi: 10.1097/CM9.0000000000002741 [Epub ahead of print].
20. Joinpoint Regression Program . Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute. Available at: https://surveillance.cancer.gov/help/joinpoint/tech-help/citation.
21. Kaczorowski, J , Chambers, LW , Dolovich, L , Paterson, JM , Karwalajtys, T , Gierman, T, et al. Improving cardiovascular health at population level: 39 community cluster randomised trial of cardiovascular health awareness program (CHAP). BMJ. (2011) 342:d442. doi: 10.1136/bmj.d442
22. Zhelev, Z , Walker, G , Henschke, N , Fridhandler, J , and Yip, S . Prehospital stroke scales as screening tools for early identification of stroke and transient ischemic attack. Cochrane Database Syst Rev. (2019) 4:Cd011427. doi: 10.1002/14651858.CD011427.pub2
23. Ghincea, CV , Anderson, DA , Ikeno, Y , Roda, GF , Eldeiry, M , Bronsert, MR, et al. Utility of neuromonitoring in hypothermic circulatory arrest cases for early detection of stroke: listening through the noise. J Thorac Cardiovasc Surg. (2021) 162:1035–1045.e5. doi: 10.1016/j.jtcvs.2020.01.090
24. Redon, J , Olsen, MH , Cooper, RS , Zurriaga, O , Martinez-Beneito, MA , Laurent, S, et al. Stroke mortality and trends from 1990 to 2006 in 39 countries from Europe and Central Asia: implications for control of high blood pressure. Eur Heart J. (2011) 32:1424–31. doi: 10.1093/eurheartj/ehr045
25. Collins, D , Laatikainen, T , and Farrington, J . Implementing essential interventions for cardiovascular disease risk management in primary healthcare: lessons from Eastern Europe and Central Asia. BMJ Glob Health. (2020) 5:e002111. doi: 10.1136/bmjgh-2019-002111
26. Aira, T , Wang, W , Riedel, M , and Witte, SS . Reducing risk behaviors linked to noncommunicable diseases in Mongolia: a randomized controlled trial. Am J Public Health. (2013) 103:1666–74. doi: 10.2105/AJPH.2012.301175
27. Vibo, R , Kõrv, J , and Roose, M . The third stroke registry in Tartu, Estonia: decline of stroke incidence and 28-day case-fatality rate since 1991. Stroke. (2005) 36:2544–8. doi: 10.1161/01.STR.0000189633.33623.69
28. Kôrv, J , Roose, M , and Kaasik, AE . Changed incidence and case-fatality rates of first-ever stroke between 1970 and 1993 in Tartu, Estonia. Stroke. (1996) 27:199–203. doi: 10.1161/01.STR.27.2.199
29. Collantes, ME , Navarro, J , Belen, A , and Gan, R . Stroke systems of care in the Philippines: addressing gaps and developing strategies. Front Neurol. (2022) 13:1046351. doi: 10.3389/fneur.2022.1046351
30. de Juras, AR , Hsu, WC , Cheng, YY , Ku, LE , Yu, T , Peng, CJ, et al. Sex differences in dietary patterns of adults and their associations with the double burden of malnutrition: a population-based National Survey in the Philippines. Nutrients. (2022) 14:3495. doi: 10.3390/nu14173495
31. Kontogianni, MD , and Panagiotakos, DB . Dietary patterns and stroke: a systematic review and re-meta-analysis. Maturitas. (2014) 79:41–7. doi: 10.1016/j.maturitas.2014.06.014
32. Rosato, V , Temple, NJ , La Vecchia, C , Castellan, G , Tavani, A , and Guercio, V . Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr. (2019) 58:173–91. doi: 10.1007/s00394-017-1582-0
33. de Juras, AR , Hsu, WC , and Hu, SC . Prevalence and determinants of the co-occurrence of overweight or obesity and micronutrient deficiencies among adults in the Philippines: results from a National Representative Survey. Nutrients. (2021) 13:2339. doi: 10.3390/nu13072339
34. Collantes, MV , Zuñiga, YH , Granada, CN , Uezono, DR , De Castillo, LC , Enriquez, CG, et al. Current state of stroke Care in the Philippines. Front Neurol. (2021) 12:665086. doi: 10.3389/fneur.2021.665086
35. Angeles-Agdeppa, I , Custodio, MRS , and Toledo, MB . Breakfast in the Philippines: food and diet quality as analyzed from the 2018 expanded National Nutrition Survey. Nutr J. (2022) 21:52. doi: 10.1186/s12937-022-00804-x
36. Reue, K , and Wiese, CB . Illuminating the mechanisms underlying sex differences in cardiovascular disease. Circ Res. (2022) 130:1747–62. doi: 10.1161/CIRCRESAHA.122.320259
37. Arnold, AP , Cassis, LA , Eghbali, M , Reue, K , and Sandberg, K . Sex hormones and sex chromosomes cause sex differences in the development of cardiovascular diseases. Arterioscler Thromb Vasc Biol. (2017) 37:746–56. doi: 10.1161/ATVBAHA.116.307301
38. Dokova, KG , and Feigin, VL . Trends in stroke burden in central and Eastern Europe from 1990–2019. Neuroepidemiology. (2022) 56:333–44. doi: 10.1159/000525880
39. GBD 2017 Diet Collaborators . Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
40. Wang, Y , Wang, J , Chen, S , Li, B , Lu, X , and Li, J . Different changing patterns for stroke subtype mortality attributable to high sodium intake in China during 1990 to 2019. Stroke. (2023) 54:1078–87. doi: 10.1161/STROKEAHA.122.040848
41. Cooperative Research Group . Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt cooperative research group. BMJ. (1988) 297:319–28. doi: 10.1136/bmj.297.6644.319
42. Hipgrave, DB , Chang, S , Li, X , and Wu, Y . Salt and sodium intake in China. JAMA. (2016) 315:703–5. doi: 10.1001/jama.2015.15816
43. Popkin, BM . Synthesis and implications: China's nutrition transition in the context of changes across other low- and middle-income countries. Obes Rev. (2014) 15:60–7. doi: 10.1111/obr.12120
44. Lv, J , Yu, C , Guo, Y , Bian, Z , Yang, L , Chen, Y, et al. Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J Am Coll Cardiol. (2017) 69:1116–25. doi: 10.1016/j.jacc.2016.11.076
Keywords: “B&R” countries, stroke, burden of disease, dietary risk factors, disability-adjusted life years, average annual percent change, trend analysis
Citation: Zhang Y, Luo Z, Yi J, Zhu J, Qiu Y, Xu X, Xie W, Wu J, Lv H, Mou C, Zhang W and Li X (2023) Burden and trends of stroke attributable to dietary risk factors from 1990 to 2019 in the Belt and Road Initiative countries: an analysis from the global burden of disease study 2019. Front. Nutr. 10:1235271. doi: 10.3389/fnut.2023.1235271
Received: 06 June 2023; Accepted: 11 July 2023;
Published: 26 July 2023.
Edited by:
Iain Brownlee, Northumbria University, United KingdomReviewed by:
Biju Soman, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), IndiaCopyright © 2023 Zhang, Luo, Yi, Zhu, Qiu, Xu, Xie, Wu, Lv, Mou, Zhang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaopan Li, eGlhb3BhbmxpMDIyNEAxMjYuY29t; Yue Zhang, eXVlemhhbmdAc3htdS5lZHUuY24=; Wei Zhang, d29haWpzZkAxMjYuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.