
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 08 January 2024
Sec. Clinical Nutrition
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1227840
This article is part of the Research Topic Anthropometric Assessment View all 13 articles
Background: Malnutrition is a common geriatric syndrome affecting approximately half of the older population with a more pronounced occurrence rate in those hospitalized. It affects the physiology, and results in poor humanistic and clinical outcomes. In Africa, particularly in Ethiopia, albeit multiple studies are available on malnutrition in non-hospitalized older population, similar studies in inpatient settings are scarce. Therefore, this study was conducted with the intention to quantify the prevalence of malnutrition in older patients on inpatient admission and determine its associated factors.
Methods: A total of 157 older inpatients aged 60 years and above were included in the present study. The data collection format was developed after an in-depth review of relevant literatures. The full Mini-Nutritional Assessment (MNA) tool was employed to assess the nutritional status on admission. Data completeness was checked thoroughly. Descriptive statistics and logistic regression analysis were conducted using STATA 15.0. The area under the receiver operating characteristic curve (ROC), Hosmer–Lemeshow test, and classification table were computed to evaluate the final model goodness-of-fit.
Results: Of the total study subjects, 81% were malnourished (MNA score <17) and 17% were at risk for malnutrition (MNA score of 17.5–23.5). However, upon review of the patients’ medical charts, malnutrition diagnosis was recorded in only two patients. Rural residence (AOR = 2.823, 95%CI: 1.088, 7.324), self-reported financial dependence for expenses (AOR = 4.733, 95%CI: 1.011, 22.162), and partial dependence in functional autonomy on admission (AOR = 3.689, 95%CI: 1.190, 11.433) significantly increased the risk of malnutrition. The area under the ROC curve (0.754) and the Hosmer–Lemeshow test (p = 0.7564) indicated that the final model reasonably fits the data. The model`s sensitivity is 96.85%.
Conclusion: In the present study, an alarmingly high prevalence of malnutrition was identified older inpatients. The problem went undiagnosed in a similar percentage of patients. Several available literatures indicate the presence of an association between nutritional status and patient outcomes, thus strict nutritional screening at inpatient admission and intervention are recommended with special emphasis for those from rural areas, with financial dependence, and with functional impairment on admission.
The global population dynamics show that the proportion of the older population is growing over time (1). Older populations are defined as those aged 65 years and above in developed countries, whereas for developing countries, such as Ethiopia, international organizations define older as a person aged 60 years and above (2). The proportion of individuals in this age group is projected to grow by two-fold, from 1 billion in 2020 to 2.1 billion in 2050. The projection also shows that in 2050, approximately 80% of older people will be residing in low- and middle-income countries (3). Ethiopia is also experiencing a demographic transition consistent with the global trend (4). This is presumed to affect almost all aspects of the global society, including the healthcare system (5).
Older people are usually fragile and vulnerable to malnutrition (6), which denotes failure to meet one's energy or protein requirements of high biological value (7). It is estimated that approximately half of the elderly population is affected by malnutrition (8), with a higher rate in hospitalized patients (9, 10). In this age group, low education, older age, anorexia of aging, multimorbidity, cognitive decline, polypharmacy, age-related functional decline, frailty, hospitalization, financial constraints, and empty nest syndrome are among the contributing factors to malnutrition (9, 11, 12). Furthermore, previously available studies mentioned factors such as sex (13, 14), age (13–15), rural residency (11), no formal education (11, 13, 14), low economic status (14, 15), functional impairment (11, 16, 17), smoking (18), having depression (11, 13–15), hospitalization history, alcohol consumption (14), and occupations (15) as malnutrition associated factors.
The occurrence of malnutrition results in deranged physiology and poor clinical outcomes. It affects the quality of life, increases the incidence of infection, causes sarcopenia, results in poor hospital outcomes, and increases the risk of life-threatening complications and mortality (9, 13, 15, 19, 20). As a result, malnutrition screen-and-treat policies are recommended in the hospital setting (21). However, malnutrition and nutritional aspects of some common clinical conditions of older age are often neglected in clinical practice (22). There are various nutritional assessment tools for screening malnutrition among hospitalized patients, but none of them are considered gold standard (23). The Mini-Nutritional Assessment (MNA) tool, a valid nutrition screening and assessment tool for elderly patients (24), has been employed in several nutritional assessment studies (25–27).
The prevalence of malnutrition among hospitalized older patients prominently varies across the available studies. In Europe, malnutrition has been reported in up to 80% of geriatric hospital patients (9), and at risk of malnutrition in nearly half of the elderly population (28). Studies from Australia recorded malnutrition and at risk for malnutrition in up to 88% of hospitalized elderly patients, respectively (25, 29). In one study from Brazil, moderate and severe malnutrition was recorded in more than half (55%) of the elderly patients (28), while in Asia, malnutrition prevalence was as high as 45% (26, 30–35) and at risk for malnutrition up to 67.1% (26, 30, 33–35) were reported.
In Africa, malnutrition among older people is a major challenge to the health care system and requires special pressing consideration. Almost all the available studies on the nutritional status of elderly people in the continent are from community settings (36–39). A review of observational studies from the community and pocket studies from the hospital settings in Africa revealed malnutrition prevalence of up to 56% in the hospitalized older population using the MNA tool (38). In other review studies involving mostly community-based and a few facility-based outpatient studies from Africa, malnutrition prevalence of 17% ranging from 1.8 to 39.47% was reported in the elderly population. The studies incorporated in the review assessed nutritional status using either body mass index (BMI) or MNA (36). In addition, a scoping review of community- and few facility-based, outpatient studies from sub-Saharan Africa indicated malnutrition prevalence between 6 and 54% in older people. The investigators of the studies included in the review employed BMI, the MNA tool, and Mid-Upper Arm Circumference (MUAC), alone or in combination, to assess nutritional status (37). On the other hand, a multi-country, multi-center prospective cohort study was conducted in selected hospitals from South Africa, Ghana, and Kenya. In the study, using Nutritional Risk Screening-2002®, 75.1% of patients screened at admission to the hospitals were at risk of malnutrition (40).
In previously available studies involving older patients, female sex, a low education level (41), older age (42, 43), unmarried (43, 44), polypharmacy, dysphagia, depression, low functional capacity, eating-related problems, lowered cognitive function (45), diabetes (26), alcohol abuse, and socio-economic status were described as independent risk factors of malnutrition (46–48).
In Ethiopia, a review of community-based studies that assessed undernutrition in the elderly population using BMI recorded a 20.53% pooled prevalence of undernutrition among the older population (39). Hitherto, studies on the prevalence of malnutrition among elderly inpatients in Africa, particularly in Ethiopia, are limited. Therefore, this study was conducted with the primary intention of determining the prevalence of malnutrition in older patients on admission to medical wards and determining its associated factors.
This cross-sectional study was conducted in the period from 6 September 2021 to 26 December 2022 in the medical wards of Jimma Medical Center (JMC), which is a Jimma University-affiliated institution in Jimma town, 352 km south-west of Addis Ababa. It is the only teaching and referral medical center in the southwestern part of the country with a bed capacity of 800, and provides services for a catchment population of about 15 million people. The center has over 1,000 health professionals, and 16 service departments, including emergency, ambulatory, internal medicine, pediatrics, adult and pediatric oncology, surgery, dentistry, physiotherapy, radiology, gynecology and obstetrics, sexual and reproductive health, and pharmacy (49, 50). In the present study, 157 consented older adult patients aged 60 years and above who were admitted to the medical wards (general unit, cardiac unit, stroke unit, and pulmonary unit) of JMC over the study period were considered. Participants with aphasia problems (n = 2) and re-admissions (n = 12) were excluded from the study.
Single population proportion formula was employed for calculating the sample size assuming a confidence level of 95%, a margin of error of 0.05, and a critical value (Z) of 1.96. For the purpose of this study, the prevalence of malnutrition in older people (P = 21.2%) was taken from a previous study in Ethiopia (14). In the year 2019–2020, approximately 398 older adult patients aged 60 years and above were admitted to the medical wards of JMC and this number was considered as a source population. The final minimum sample size was n = 157 after correction. Thus, 157 eligible older adult patients were consecutively assessed over the study period.
The data collection tool comprised both, standard tools and tools designed after an in-depth review and extraction from relevant literatures. It was designed to capture relevant socio-demographic, behavioral, functional, clinical, nutritional, and related information of the participants. The tool was translated to two locally predominant languages (Afan Oromo and Amharic) and back translated into English to check the consistency. Two data collectors (Bachelor's degree nurses) were trained on the data collection tool and procedure. Prior to the actual data collection period, a pre-test was conducted. The data collection procedure throughout the study period was carried out under close supervision of the investigators. Patient charts, laboratory results, patient/caregiver interviews, and practitioners in charge were the sources of data for the present study. All data were collected from eligible patients within 48 h of admission to the ward. Each patient’s diagnosis was reviewed from their medical chart to check on how many of these patients were diagnosed with malnutrition over their hospital stay.
The independent variables were socio-demographic and related variables [age, sex, residence, marital status, educational level, patient’s current working status, occupation, and self-reported financial dependence (not able to cover their personal expense)]; behavioral, functional, and related information [alcohol drinking, cigarette smoking, and khat chewing history; recent traditional medicine use history, cohabitation, and activities of daily living (ADL)]; clinical and related information (presence of past medical history, hospitalization in the previous 1-year, psychological condition on admission). Katz Index of independence was employed to assess ADL, which indicates the functional health status of older patients on admission (51). The tool assesses performance in six daily living functions (eating, dressing, bathing, transferring, continence, and toileting), each of which is assigned a score of 1 or 0. Accordingly, patients are categorized as independent (full function), partially dependent (moderate impairment), or dependent (severe functional impairment) if they scored 6, 3–5, and 2 or less points, respectively. The shortened self-report form of the Geriatric Depression Scale (GDS) which comprised 15 items, was used to objectively assess the psychological condition of older patients on admission (52). Each question in GDS has two alternative responses, either yes or no, and the patients are categorized as having no psychological problem (0–4), mild depression/dementia (5–9), or severe depression/dementia (10–15). The outcome of this study is the nutritional status of older patients on admission to medical wards based on the full MNA tool score.
The nutritional assessment on admission was carried out using the full MNA tool. The MNA tool (24, 53) is recommended as a screening tool for malnutrition in older inpatients. The tool has been evaluated in the older population in Ethiopia (54). It is widely employed in studies and has good reliability and validity. It has 18 questions that can be categorized into four parts: anthropometric, overall assessment, diet assessment, and subjective assessment. The summative score is 30 points: 24–30 points indicate good nutrition; 17.0–23.5 points indicate risk of malnutrition; and less than 17.0 points indicate malnutrition. MNA has 96% sensitivity and 98% specificity (55). In assessing nutritional status on admission, body mass index (BMI) was calculated using the standard formula: BMI = weight in kg/(height in m)2. The weight of the study participants was measured using beam balance. For taking the weight of the participant, each of them was requested to take off their shoes and heavy clothes, including jackets, jerseys, and belts; the balance was calibrated; and the figure was approximated to the nearest 0.01 kg. For measuring height, a seca vertical height scale was used. Patients were asked to take off their shoes and stand upright in the middle of the board. Thereafter, height was measured to the nearest 0.01 cm by making the participant’s back of the head, the shoulder blades, the buttocks, and the heels to touch the measuring board. Upon encountering patients who cannot erect upright because of their illness, their height was estimated from demi-span (56). In line with a standard recommendation, the length from the sternal notch to the finger roots (demi-span) was measured by a flexible validated plastic tape with the patient sitting upright or recumbent depending on the patient’s abilities. Then, height was estimated as follows: for female individuals: Height in cm = (1.35 × demi-span in cm) + 60.1; for male individuals: Height in cm = (1.40 × demi-span in cm) + 57.8.
Data were checked for completeness and accuracy during the data collection period, entry, and before the analysis. Epi data version 4.2.0.0 and STATA V.15.0 were employed for data entry and analysis, respectively. Categorical variables were described in frequency and percentage. Upon performing the Shapiro-Wilk test, the distribution of continuous variables was non-normal, thus presented in the median and interquartile range (IQR). For the binary logistic regression model, nutritional status was dichotomized into 0 = no malnutrition (normal and at risk of malnutrition) and 1 = malnutrition. Candidate variables for regression analysis were selected based on the existing literatures, and all variables with a p < 0.25 in simple logistic regression were incorporated into multiple logistic regression analysis. Collinearity was checked using the variance inflation factor (VIF); all factors included in the multiple logistic regression analysis had a VIF of <10 (maximum 1.48). The interaction was evaluated using statistical models by including product terms for two independent variables presumed to have interactions in the model. The goodness-of-fit of the final model was evaluated by computing the area under the receiver operating characteristic curve (ROC), Hosmer–Lemeshow test, and classification table. In all the analyses, a two-tailed p < 0.05 was used to declare statistical significance.
The median age of the participants was 65 years, and most of them were men (82.2%). Of the total study subjects, farmers accounted for 24.2%, and self-reported financial independence for healthcare expenditure was captured in over three-fourths (78.3%). The socio-demographic and behavioral information of the study subjects are shown in Table 1.
On assessing the activities of daily living using the Katz score, 78% of the participants had impairment in their functional autonomy at admission. Past medical history was captured in 65.6% of the participants, and each of these patients had three known diseases on average. A little above one-third (33.8%) of the participants had a previous hospitalization history. The functional, clinical, and related information of the study subjects is presented in Table 2.
On the MNA tool-based nutritional status assessment at admission, 81% of the study participants had a score less than 17 and were categorized as malnourished. However, upon a thorough review of patients` medical charts over the hospital stay, malnutrition diagnosis was recorded in only two. The prevalence of elderly inpatients’ nutritional category is depicted in Figure 1.
The full MNA tool questions with data captured from the study subjects are presented in Table 3.
Six variables achieved a p < 0.25 in the simple logistic regression analysis; only residence (p = 0.017) and financial dependence (p = 0.041) were significantly associated with nutritional status. Subsequently, multiple logistic regression analysis was performed by incorporating the main variables achieving a p < 0.25 and some pertinent interaction terms (financial dependence#residence, financial dependence#sex, and functional autonomy#sex). However, none of the interaction terms were statistically significant, thus removed from the model and the analysis was rerun without the interaction terms. In the final model, significantly higher odds of malnutrition were observed in older patients from rural areas (AOR = 2.823, 95%CI: 1.088, 7.324, 0.033), with financial dependence (AOR = 4.733, 95%CI: 1.011, 22.162, 0.048), and with partial dependence in functional autonomy on inpatient admission (AOR = 3.689, 95%CI: 1.190, 11.433, 0.024). The model achieved an area under the ROC curve of 0.754 and an insignificant Hosmer–Lemeshow test p-value (0.756) indicating a good fit. On classification table analysis, the model correctly classified 82.20% of the participants achieving a sensitivity of 96.85%. The regression analysis is shown in Table 4.
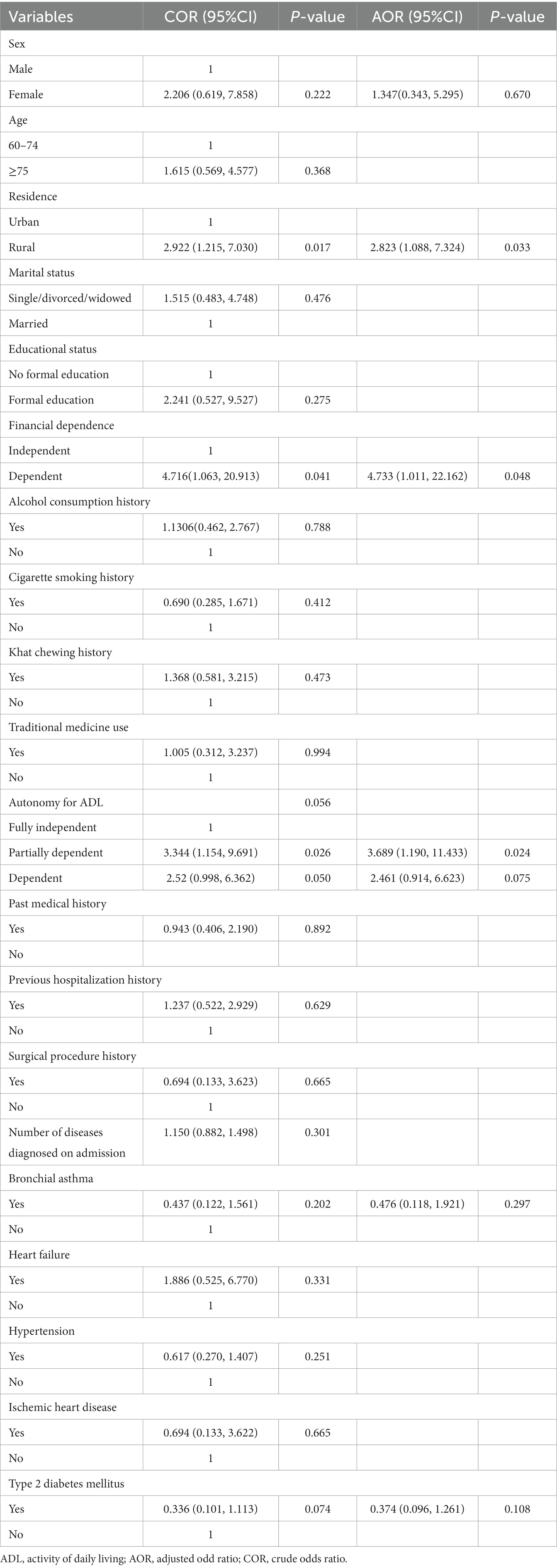
Table 4. Logistic regression analysis to identify factors associated with the nutritional status of elderly patients on hospital admission.
This single-center prospective cross-sectional study is a pioneer in quantifying the prevalence of malnutrition and determining associated factors in older patients on admission to medical wards in Ethiopia. Patients were assessed for nutritional status within 48 h of admission to medical wards using the full MNA tool. Accordingly, almost all admitted elderly patients (98%) were either malnourished (81%) or at risk of malnutrition (17%). However, clinicians recorded malnutrition diagnosis in only two patients’ medical charts, which indicates that malnutrition diagnosis is neglected in almost all patients.
In the previous studies from Ethiopia, the pooled prevalence of undernutrition among the older population was 20.53% (39); however, the included studies were entirely community based. In Egypt, a similar study involving 194 older patients admitted with cancer reported malnutrition in 33% of the participants (57). In the study from Egypt (57), the study participants were a cohort of patients with cancer, which along with other dissimilarities in the study participants’ characteristics might have contributed to a lower prevalence of malnutrition as compared to our result. In Europe, malnutrition has been reported in as high as 80% of older patients (9), which is consistent with our findings. Other similar studies from Europe (27, 28), Australia (25, 29), Brazil (28), and Asia (26, 30–35) reported malnutrition far lower than our findings. This could be attributed to potential differences in the study participants’ characteristics. The observed, alarmingly high prevalence of malnourished patients in our study requires immediate intervention. In fact, the elderly often become dependent on others for their food and nutrition (58), in the context of poor social support status seen in Ethiopia (59), huge vulnerability to malnutrition is expected. The policy direction for old age and food insecurity seen in Ethiopia due to underlying multifactorial causes might also contribute to the observed malnutrition prevalence in older inpatients (60). Evidence also shows that medical comorbidity, physical impairments (9, 10), and hospitalization (9, 11) affect nutritional status in elderly people. In the present study, a higher proportion of elderly patients had a past medical history (65.6%) and physical impairment (59.2%). However, in this study, the presence of past medical history was not significantly associated with malnutrition.
In this study, significantly higher odds of malnutrition were observed in older patients who were from rural areas. This finding is in line with other study findings from Ethiopia (18, 61). The possible difference in socio-economic status and dietary habits may have increased rural residents' risk for malnutrition. Also, several studies involving elderly people reported the existence of a significant association between functional autonomy and malnutrition (62, 63). A similar finding has also been observed in our study where the risk of malnutrition is high among patients who do have partial impairment in performing activities of daily living on admission in contrast to those who do not. Older patients with partial dependence on functional autonomy on admission had over 3.6-fold increased risk for malnutrition as compared to those who are fully independent. This is due to the fact that these patients lack functional autonomy to care after oneself and to prepare and eat foods requiring the attention of others (64). This fact is corroborated by our study finding in which most of the participants (86.6%) believed their food intake was decreased either moderately or severely.
Food and nutrition insecurity due to lower economic status also increases the risk for malnutrition (48), which is also observed in our study where older patients who were financially dependent for their expenses had a 4.73-fold increased risk for malnutrition as compared to their counterparts. This finding is consistent with other similar studies (15, 48). On the other hand, previously existing studies described female sex, low education level (41), older age (42, 43), unmarried (43, 44), polypharmacy, dysphagia, neuropsychological problem (45), alcohol abuse, and tobacco use as independent risk factors of malnutrition. The relatively longer life expectancies than men and the higher likelihood to encounter adverse economic and social circumstances in old age are assumed to increase the risk of malnutrition in women. As people get older, age-related alterations, such as physical frailty, loss of taste and poor appetite, the feeling of worthlessness, and a sense of neglect, can impact eating habits with adverse consequences on nutritional status (65). Beyond their impact on nutritional status, educational level, marital status, and sex, they were also found to affect discharge outcomes (66). In the present study, as seen in Table 4, the crude odds ratio shows an increased risk of malnutrition in the female sex, in patients with no formal education, older age, marital status of single, and alcohol abuse, however, none of them achieved a statistically significant association with malnutrition. This could be due to the small sample size employed in our study. Regarding polypharmacy (prescription drugs taken by the patients) and neuropsychological problems, these variables are already components of the full MNA tool used for outcome measurement (see Table 3), thus rationally excluded from considering them as independent variables in the logistic regression analysis in the present study.
From the results of the present study and the potential complications of undernutrition in elderly patients, the investigators recommend the installation of a system for the prevention, early detection, and management of malnutrition in elderly patients. First, for the prevention of malnutrition and its complications, Ethiopia: Food-Based Dietary Guidelines (67) encourage elderly people to take adequate fluid and diversified diets, such as meat, poultry products, fruits, and vegetables to prevent malnutrition. However, practically, given that the elderly are one of the poorest and most marginalized sections of the population in Ethiopia (68, 69), the authors have reservation on the possibility for successful implementation of governmental and non-governmental stakeholders. Second, the authors of the present study recommend early screening of elderly patients for nutritional status and managing those affected by malnutrition with oral nutritional supplementation, such as plumpy nut, and diet enhancement in the hospital settings according to the national and relevant international guidelines, such as European Society for Clinical Nutrition and Metabolism (70). In doing so, special consideration for older patients with functional impairment on admission might be helpful. Finally, we also recommend a multicenter, large sample size study to increase the power of generalizability of the findings in the present study.
In this study, the collection of relevant data objectively from the older patients using standardized techniques and the exploratory nature of the study for the setting, as well as for Ethiopia, could be mentioned as merits. However, the study has some limitations. The single-center consideration and the small sample size employed may affect the accuracy and generalizability of the findings. Also, the causal association cannot be assessed due to the intrinsic nature of the cross-sectional design. Some pertinent variables, such as a number of family size, the presence of eating-related problems, and biochemical parameters for nutritional assessments were not addressed in the present study. We could not also rule out the possibility of response bias where some respondents may not actually answer some questions truthfully, which may distort study results.
In conclusion, using the full MNA tool, an alarmingly high prevalence of malnutrition and at risk of malnutrition was identified. Nevertheless, the problem went undiagnosed in a similar proportion of the patients. Owing to the existence of multiple evidences on the adverse clinical and humanistic consequences of malnutrition, the authors recommend designing immediate strategies for routine screening at admission and nutritional intervention with special emphasis on older patients from rural areas, with financial constraints, and with functional impairment on admission. Further large sample size study, incorporating pertinent variables missed in the present study and possibly assessing the clinical consequences of malnutrition in older patients in the local context is recommended.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The study involving humans was approved by the Institutional Review Board (IRB) of Jimma University. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
BT, MY, and DB substantially contributed to the data acquisition and results explanation and drafted the manuscript. BT performed the data analysis. TB contributed to the explanation of the results and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
This study was supported by the Research and Innovation Director Office of Jimma University Institute of Health (JUIH2013EFY).
First and foremost, the authors would like to thank the Director Office of Jimma University's Institute for Health Research and Innovation for funding this research. The authors also like to express their gratitude to the study subjects for their thoughtful participation throughout the investigation. The personnel working in internal medicine as well as the data collectors should also be sincerely thanked for their assistance. Finally, the authors are grateful to Assefa Legesse, a senior Biostatistician, for critically reviewing the statistics part.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. United Nations. World population ageing 2019 highlights. New York, NY: (2019). Available at: https://digitallibrary.un.org/record/3846855/files/WorldPopulationAgeing2019-Highlights.pdf
2. UNHCR. Older persons - emergency handbook. (2023) Available at: https://emergency.unhcr.org/entry/43935/older-persons (Accessed January 3, 2023).
3. WHO. Ageing and health. Available at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (Accessed December 2, 2022).
4. Minale, AS. Demographic transition in Ethiopia: evidence of change from 1990 to 2016. Ethiop J Soc Sci. (2020) 6:1–19.
5. WHO. UN decade of healthy ageing. (2020) Available at: https://www.who.int/initiatives/decade-of-healthy-ageing (Accessed January 3, 2023).
6. World Health Organization. Integrated care for older people: guidelines on community-level interventions to manage declines in intrinsic capacity. World Health Organization (2017). Available at: https://apps.who.int/iris/handle/10665/258981 (Accessed September 14, 2023).
7. Cleveland Clinic. Malnutrition: definition, causes, symptoms and treatment. Available at: https://my.clevelandclinic.org/health/diseases/22987-malnutrition (Accessed September 19, 2023).
8. Volkert, D, Beck, AM, Cederholm, T, Cereda, E, Cruz-Jentoft, A, Goisser, S, et al. Management of malnutrition in older patients—current approaches, evidence and open questions. J Clin Med. (2019) 8:974. doi: 10.3390/jcm8070974
9. Corcoran, C, Murphy, C, Culligan, EP, Walton, J, and Sleator, RD. Malnutrition in the elderly. Sci Prog. (2019) 102:171–80. doi: 10.1177/0036850419854290
10. Norman, K, Haß, U, and Pirlich, M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients. (2021) 13. doi: 10.3390/nu13082764
11. Ahmad, MH, Salleh, R, Siew Man, C, Pardi, M, Che Abdul Rahim, N, Shahril, N, et al. Malnutrition among the elderly in Malaysia and its associated factors: findings from the National Health and Morbidity Survey 2018. J Nutr Metab. (2021) 2021:1–8. doi: 10.1155/2021/6639935
12. Volkert, D, Kiesswetter, E, Cederholm, T, Donini, LM, Eglseer, D, Norman, K, et al. Development of a model on determinants of malnutrition in aged persons: a MaNuEL project. Gerontol Geriatr Med. (2019) 5:2333721419858438. doi: 10.1177/2333721419858438
13. Derbie, L, Oumer, A, Ayele, K, and Berhane, A. Determinants of nutritional status among old age population in eastern Ethiopia: a general linear model approach. J Nutr Sci. (2022) 11:e70. doi: 10.1017/jns.2022.62
14. Mezemir, Y, Egata, G, Geset, D, and Lambebo, A. Nutritional status and associated factors among the community-dwelling elderly population in Debre Berhan Town, North Shewa Zone, Ethiopia. Nutr Diet Supp. (2020) 12:289–99. doi: 10.2147/nds.s280589
15. Abate, T, Mengistu, B, Atnafu, A, and Derso, T. Malnutrition and its determinants among older adults people in Addis Ababa, Ethiopia. BMC Geriatr. (2020) 20:1–9. doi: 10.1186/s12877-020-01917-w
16. Leão, LL, Engedal, K, Monteiro-Junior, RS, Tangen, GG, and Krogseth, M. Malnutrition is associated with impaired functional status in older people receiving home care nursing service. Front Nutr. (2021) 8:684438. doi: 10.3389/fnut.2021.684438
17. Nagai, K, Komine, T, Ikuta, M, Gansa, M, Matsuzawa, R, Tamaki, K, et al. Decline of instrumental activities of daily living is a risk factor for nutritional deterioration in older adults: a prospective cohort study. BMC Geriatr. (2023) 23:480. doi: 10.1186/s12877-023-04185-6
18. Ferede, YM, Derso, T, and Sisay, M. Prevalence of malnutrition and associated factors among older adults from urban and rural residences of Metu district, Southwest Ethiopia. BMC Nutr. (2022) 8:52. doi: 10.1186/s40795-022-00532-9
19. Mulugeta, G, Dingeta, T, Mitiku, H, and Weldegebreal, F. Undernutrition and associated factors among elderly people served in Public Servants Social Security Agency in Harar, Eastern Ethiopia. SAGE Open Med. (2022) 10:205031212211086. doi: 10.1177/20503121221108615
20. Yanni, Z, Qiulin, Z, Shanjun, T, Hao, L, and Guohao, W. Interpretation of ESPEN practical guideline: clinical nutrition and hydration in geriatrics. Chin J Digest Surg. (2022) 21:708–25. doi: 10.3760/cma.j.cn115610-20220325-00164
21. Harris, PS, Payne, L, Morrison, L, Green, SM, Ghio, D, Hallett, C, et al. Barriers and facilitators to screening and treating malnutrition in older adults living in the community: a mixed-methods synthesis. BMC Fam Pract. (2019) 20:100. doi: 10.1186/s12875-019-0983-y
22. Vranešić Bender, D, and Krznarić, Ž. Nutritional issues and considerations in the elderly: an update. Croat Med J. (2020) 61:180–3. doi: 10.3325/cmj.2020.61.180
23. Naser, IA, Abushabab, AM, Tair, ASA, and Almasri, IM. Agreement between different nutritional assessments tools used for elderly hospitalized patients. Curr Res Nutr Food Sci J. (2022) 10:532–43. doi: 10.12944/CRNFSJ.10.2.10
24. Guigoz, Y, and Vellas, B. Nutritional assessment in older adults: MNA® 25 years of a screening tool & a reference standard for care and research; what next? J Nutr Health Aging. (2021) 25:528–83. doi: 10.1007/s12603-021-1601-y
25. Lambert, K, Taylor, E, Bowden, S, and Charlton, K. Nutritional status according to the mini nutritional assessment predicts speed and degree of functional improvement and discharge outcomes in rehabilitation patients. J Nutri Geront Geriatr. (2020) 39:16–29. doi: 10.1080/21551197.2019.1689882
26. Li, T, Zhang, Y, Gong, C, Wang, J, Liu, B, Shi, L, et al. Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur J Clin Nutr. (2020) 74:871–5. doi: 10.1038/s41430-020-0642-3
27. Rondanelli, M, Talluri, J, Peroni, G, Donelli, C, Guerriero, F, Ferrini, K, et al. Beyond body mass index. IS the body cell mass index (BCMI) a useful prognostic factor to describe nutritional, inflammation and muscle mass status in hospitalized elderly? Body cell mass index links in elderly. Clin Nutr. (2018) 37:934–9. doi: 10.1016/j.clnu.2017.03.021
28. Slee, A, Birch, D, and Stokoe, D. The relationship between malnutrition risk and clinical outcomes in a cohort of frail older hospital patients. Clin Nutr ESPEN. (2016) 15:57–62. doi: 10.1016/j.clnesp.2016.06.002
29. Marshall, S, Young, A, Bauer, J, and Isenring, E. Nutrition screening in geriatric rehabilitation: criterion (concurrent and predictive) validity of the malnutrition screening tool and the mini nutritional assessment-short form. J Acad Nutr Diet. (2016) 116:795–801. doi: 10.1016/j.jand.2015.06.012
30. Hiraike, T, Momoki, C, and Habu, D. Comparison of the adequacy of geriatric nutritional risk index with that of the mini nutritional assessment-short form and global leadership initiative on malnutrition criteria in assessing nutritional status to predict the 1-year prognosis of hospitalized Japanese older adults: a single-institutional cohort study. BMC Geriatr. (2023) 23:35. doi: 10.1186/s12877-023-03740-5
31. Hu, X, Zhang, L, Wang, H, Hao, Q, Dong, B, and Yang, M. Malnutrition-sarcopenia syndrome predicts mortality in hospitalized older patients. Sci Rep. (2017) 7:1–9. doi: 10.1038/s41598-017-03388-3
32. Liu, GX, Chen, Y, Yang, YX, Yang, K, Liang, J, Wang, S, et al. Pilot study of the Mini Nutritional Assessment on predicting outcomes in older adults with type 2 diabetes. Geriatr Gerontol Int. (2017) 17:2485–92. doi: 10.1111/ggi.13110
33. Miao, JP, Quan, XQ, Zhang, CT, Zhu, H, Ye, M, Shen, LY, et al. Comparison of two malnutrition risk screening tools with nutritional biochemical parameters, BMI and length of stay in Chinese geriatric inpatients: a multicenter, cross-sectional study. BMJ Open. (2019) 9:1–9. doi: 10.1136/bmjopen-2018-022993
34. Thiam, CN, Mathavan, S, Abdullah, A, and Chong, EGM. Malnutrition among patients admitted to the subacute geriatric ward during the COVID-19 pandemic era: a cross-sectional study in a tertiary hospital in Malaysia. Med J Malay. (2022) 77:313–9.
35. Zhu, Z, Xu, J, Lin, Y, Chai, K, Zhou, Y, Jia, R, et al. Correlation between nutritional status and oral health quality of life, self-efficacy of older inpatients and the influencing factors. BMC Geriatr. (2022) 22:280. doi: 10.1186/s12877-022-02830-0
36. Ewunie, TM, Hareru, HE, Dejene, TM, and Abate, SM. Malnutrition among the aged population in Africa: a systematic review, meta-analysis, and meta-regression of studies over the past 20 years. PLoS One. (2022) 17:e0278904. doi: 10.1371/journal.pone.0278904
37. Obeng, P, Kyereh, HK, Sarfo, JO, Ansah, EW, and Attafuah, PYA. Nutritional status and associated factors of older persons in sub-Saharan Africa: a scoping review. BMC Geriatr. (2022) 22:416. doi: 10.1186/s12877-022-03062-y
38. Seid, AM, and Babbel, NF. Prevalence of malnutrition among old age people in Africa. Front Aging. (2022) 3:1002367. doi: 10.3389/fragi.2022.1002367
39. Yisak, H, Zemene, MA, Arage, G, Demelash, AT, Anley, DT, Ewunetei, A, et al. Undernutrition and associated factors among older adults in Ethiopia: systematic review and meta-analysis. BMJ Open. (2023) 13:e062845. doi: 10.1136/bmjopen-2022-062845
40. Blaauw, R, Achar, E, Dolman, RC, Harbron, J, Moens, M, Munyi, F, et al. The problem of hospital malnutrition in the African continent. Nutrients. (2019) 11:2028. doi: 10.3390/nu11092028
41. Bardon, LA, Corish, CA, Lane, M, Bizzaro, MG, Loayza Villarroel, K, Clarke, M, et al. Ageing rate of older adults affects the factors associated with, and the determinants of malnutrition in the community: a systematic review and narrative synthesis. BMC Geriatr. (2021) 21:676. doi: 10.1186/s12877-021-02583-2
42. Liu, X, Cao, J, Zhu, Z, Zhao, X, Zhou, J, Deng, Q, et al. Nutritional risk and nutritional status in hospitalized older adults living with HIV in Shenzhen, China: a cross-sectional study. BMC Infect Dis. (2021) 21:618. doi: 10.1186/s12879-021-06322-1
43. Streicher, M, Van Zwienen-Pot, J, Bardon, L, Nagel, G, Teh, R, Meisinger, C, et al. Determinants of incident malnutrition in community-dwelling older adults: A MaNuEL multicohort meta-analysis. J Am Geriatr Soc. (2018) 66:2335–43. doi: 10.1111/jgs.15553
44. Besora-Moreno, M, Llauradó, E, Tarro, L, and Solà, R. Social and economic factors and malnutrition or the risk of malnutrition in the elderly: a systematic review and meta-analysis of observational studies. Nutrients. (2020) 12:737. doi: 10.3390/nu12030737
45. Andersen, AL, Nielsen, RL, Houlind, MB, Tavenier, J, Rasmussen, LJH, Jørgensen, LM, et al. Risk of malnutrition upon admission and after discharge in acutely admitted older medical patients: a prospective observational study. Nutrients. (2021) 13:2757. doi: 10.3390/nu13082757
46. Kubrak, C, and Jensen, L. Malnutrition in acute care patients: a narrative review. Int J Nurs Stud. (2007) 44:1036–54. doi: 10.1016/j.ijnurstu.2006.07.015
47. Ross, LJ, Wilson, M, Banks, M, Rezannah, F, and Daglish, M. Prevalence of malnutrition and nutritional risk factors in patients undergoing alcohol and drug treatment. Nutrition. (2012) 28:738–43. doi: 10.1016/j.nut.2011.11.003
48. Silva, FRDM, De Oliveira, MGOA, Souza, ASR, Figueroa, JN, and Santos, CS. Factors associated with malnutrition in hospitalized cancer patients: a croos-sectional study. Nutr J. (2015) 14:123. doi: 10.1186/s12937-015-0113-1
49. Jimma Medical Center – Jimma University. Available at: https://ju.edu.et/jimma-medical-center/ (Accessed September 15, 2023).
50. Jimma University. Combat AMR network. Available at: https://combat-amr.org/jimma-university-specialized-hospital/ (Accessed February 23, 2023).
51. Shirley Ryan AbilityLab. Katz index of independence in activities of daily living | RehabMeasures database. Available at: https://www.sralab.org/rehabilitation-measures/katz-index-independence-activities-daily-living (Accessed December 3, 2022).
52. Geriatric Depression Scale (GDS): The Long Form And Short Form. (2022). Available at: https://geriatricacademy.com/geriatric-depression-scale/ (Accessed September 15, 2023).
53. Nestle Nutrition Institute. What is the MNA®? | MNA elderly. Available at: https://www.mna-elderly.com/ (Accessed September 15, 2023).
54. Hailemariam, H, Singh, P, and Fekadu, T. Evaluation of mini nutrition assessment (MNA) tool among community dwelling elderly in urban community of Hawassa city, Southern Ethiopia. BMC Nutr. (2016) 2:11. doi: 10.1186/s40795-016-0050-1
55. Nestle Nutrition Institute. Validity in screening tools | MNA. Available at: https://www.mna-elderly.com/validity-in-screening-tools (Accessed September 15, 2023).
56. RxKinetics. Estimating height in bedridden patients. Available at: https://rxkinetics.com/height_estimate.html (Accessed September 15, 2023).
57. Abd Allah, ES, Gad, HMM, and Abdel-Aziz, HR. Nutritional status and its contributing factors among older adults with cancer receiving chemotherapy. Clin Nurs Res. (2020) 29:650–8. doi: 10.1177/1054773820947953
58. Compass. The food they (don’t) eat: elder abuse by neglect? Compass. Available at: https://www.compass.info/featured-topics/health-wellbeing/the-food-they-dont-eat-elder-abuse-by-neglect// (Accessed September 18, 2023).
59. Alambo, FI, and Yimam, HA. Elderly care and social support systems among the Gedeo of southern Ethiopia: Socio-cultural contexts, forms, dynamics and challenges. Afr Stud Q. (2019) 18:15–28.
60. United Nations. Economic Commission for Africa; Food and Agriculture Organization of the United Nations. Africa regional overview of food security and nutrition: addressing the threat from climate variability and extremes for food security and nutrition. (2018). Available at: https://hdl.handle.net/10855/43032 (Accessed May 18, 2023)
61. Abdu, AO, Yimamu, ID, and Kahsay, AA. Predictors of malnutrition among older adults aged above 65 years in eastern Ethiopia: neglected public health concern. BMC Geriatr. (2020) 20:497. doi: 10.1186/s12877-020-01911-2
62. Reza, S, Alam, MR, Chowdhury, AI, Mamun, MAA, Akhter, M, and Habib, MA. Assessing nutritional status and functionality in geriatric population of Bangladesh: the hidden epidemic of geriatric malnutrition. Gerontol Geriatr Med. (2023) 9:23337214231172663. doi: 10.1177/23337214231172663
63. Shankar, A, McMunn, A, Demakakos, P, Hamer, M, and Steptoe, A. Social isolation and loneliness: prospective associations with functional status in older adults. Health Psychol. (2017) 36:179–87. doi: 10.1037/hea0000437
64. Eskin, S, and Tureyen, A. Nutritional status and independence in daily life activities of individuals aged 65 or over during the COVID-19 Pandemic in Turkey. Med Sci. (2021) 10:1253. doi: 10.5455/medscience.2021.04.131
65. Sergi, G, Bano, G, Pizzato, S, Veronese, N, and Manzato, E. Taste loss in the elderly: possible implications for dietary habits. Crit Rev Food Sci Nutr. (2017) 57:3684–9. doi: 10.1080/10408398.2016.1160208
66. Giannico, OV, Ambrosino, I, Patano, F, Germinario, C, Quarto, M, and Moretti, AM. Educational level, marital status and sex as social gender discharge determinants in chronic obstructive pulmonary disease exacerbations: a time-to-event analysis. Monaldi Arch Chest Dis. (2019) 89:171–178. doi: 10.4081/monaldi.2019.1017
67. Federal Government of Ethiopia, Ministry of Health, Ethiopian Public Health Institute Ethiopia’s first food-based dietary guidelines (FBDG) launched. Available at: https://www.moh.gov.et/site/node/327 (Accessed September 18, 2023).
68. Baru, A, Wonde, D, and Jibat, N. Socio - economic situation of the elderly in Jimma Zone, Oromia/Ethiopia. Ethiop J Soc Sci Lang Stud. (2018) 5:3–22.
69. Refugees UNHC for Refworld Vulnerability of older people in Ethiopia: the case of Oromia, Amhara and SNNP regional states. Refworld. Available at: https://www.refworld.org/docid/5301dd884.html (Accessed September 18, 2023).
Keywords: aged, inpatients, nutrition assessment, risk factors, Jimma
Citation: Tesfaye BT, Yizengaw MA, Birhanu TE and Bosho DD (2024) Nutritional status of hospitalized elderly patients in Ethiopia: a cross-sectional study of an important yet neglected problem in clinical practice. Front. Nutr. 10:1227840. doi: 10.3389/fnut.2023.1227840
Received: 23 May 2023; Accepted: 12 December 2023;
Published: 08 January 2024.
Edited by:
Roberta Zupo, University of Bari Aldo Moro, ItalyReviewed by:
Maria Consuelo Velazquez-Alva, Autonomous Metropolitan University Xochimilco Campus, MexicoCopyright © 2024 Tesfaye, Yizengaw, Birhanu and Bosho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Behailu Terefe Tesfaye, dGVyZWZlYmhAZ21haWwuY29t; YmVoYWlsdS50ZXJlZmVAanUuZWR1LmV0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.