
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Nutr. , 10 August 2023
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1211535
This article is part of the Research Topic Food as Medicine View all 24 articles
Introduction: The association of plant-based dietary patterns with health outcomes has traditionally been assessed without considering nutritional value. The plant-based dietary index (PDI), first published in 2016, overcomes this limitation with both a healthful PDI (hPDI) and an unhealthful PDI (uPDI), based on the quality of plant foods consumed plus the frequency of animal foods. We sought to summarize the breadth of research using the hPDI and uPDI to gain insight into how the quality of plant-based dietary patterns might be associated with health outcomes.
Methods: Scoping review of studies that used the PDI, hPDI, or uPDI to report associations with health outcomes. Multiple databases were searched from 2010 through April 2023 with 2 authors independently assessing eligibility and extracting data. In addition to assessing the association of the indices to health outcomes, we determined the frequency of concordant or discordant findings for hPDI versus PDI and for hPDI versus uPDI.
Results: We included 95 articles (54% longitudinal, 37% cross-sectional, and 9% case–control) with a median sample size of 3,646. Higher hPDI levels were associated with favorable health outcomes in 36% of comparisons (most often for obesity, mortality, diabetes, cardiovascular disease, and psychiatric disorders), compared to 25% for the PDI and only 2% for the uPDI. Conversely, higher levels of the uPDI were associated with unfavorable health outcomes in 33% of comparisons, in contrast to under 1% for the hPDI and 2% for the PDI. When the hPDI association to an outcome was discordant with the uPDI or PDI, the significance and directionality always favored the hPDI over the uPDI, and nearly always favored the hPDI over the PDI.
Discussion: Dietary indices that account for the quality of plant foods can show health benefits that might be missed by a generic plant-based index. A greater focus on the quality of plant foods could improve nutrition guidelines, raise awareness about the benefits of adding unrefined plant foods to the diet, and empower consumers to make incremental additions of such foods to displace unhealthy foods. We anticipate increasing use of indices that address food quality in future research.
Researchers often use food frequency questionnaires to assess how dietary patterns are associated with disease prevalence, incidence, and mortality. Resulting publications have traditionally used this information to create a simple dichotomy into diets with plant versus animal foods (e.g., vegetarian vs. omnivore), without considering the nutritional value of the plant foods consumed. This could potentially reduce, or obscure, any association of whole, fiber-rich healthy plant-foods with reduced disease incidence and mortality, compared to vegetarian diets with less healthy plant-foods, such as refined grains, processed foods, and sugar-sweetened snacks and beverages.
An example of the imprecision resulting from not addressing the overall quality of plant-based diets is the association of higher carbohydrate intake with increased mortality in a global health study (1). The investigators did not distinguish between whole-grain versus refined carbohydrates, making the results about carbohydrates overall difficult to interpret or generalize. Conversely, when carbohydrate quality is explicitly considered, a dose–response relationship is observed for whole-grain carbohydrates high in fiber and a reduced risk of mortality, type 2 diabetes, cardiovascular diseases, and colorectal and breast cancer (2). Similarly, consuming unrefined plant foods (e.g., nuts, fruits, vegetables and whole grains) can reduce the risk of stroke, heart failure, and coronary heart disease, whereas the opposite is seen for refined plant foods (e.g., refined grains and sugar-sweetened beverages) (3).
One solution to the impact of plant-based diet quality on health outcomes has been to calculate an overall plant-based dietary index (PDI) based on a food frequency questionnaire and to then stratify the PDI as a healthful PDI or an unhealthful PDI (Table 1) based on the type of plant foods consumed and the amount of animal foods (4). Plant foods considered healthy include nuts, fruits, legumes, vegetables and whole grains, whereas those considered less healthy include sweets, potatoes, refined grains, fruit juices, and sugar-sweetened beverages. Using this general approach to assessing diet quality, pooled analyses of cohort studies have shown the benefits of a healthful PDI for cardiovascular disease (5, 6), type 2 diabetes (4, 7), and weight reduction (8, 9). Others have used the term provegetarian dietary pattern (PVD), instead of PDI, for a similar classification into healthful versus unhealthful. Showing, for example, how the healthful PVD may reduce breast cancer risk (10).
The advantage of considering plant-based diet quality when assessing health outcomes warrants a scoping review to map the available research evidence and to identify knowledge gaps (11). Although less common than systematic reviews, scoping reviews are increasing in popularity with established methodology and reporting standards (12–14). In contrast to systematic reviews, which synthesize quantitative evidence on the efficacy of an intervention for a specific condition, a scoping review offers primarily qualitative insight into a field of study through a broad, birds-eye view of a topic or subject area (13). Given the relatively recent distinction in the nutrition literature of healthy versus less healthy plant-based diets, we considered a scoping review ideal for exploring how this concept has influenced subsequent publications on the association of plant-based diets with health outcomes. Therefore, the goal of this scoping review is to highlight the importance of assessing plant-based diet quality so others can incorporate plant food quality into reviews, guidelines, and policies that associate diet with health outcomes.
Our scoping review protocol was based on standards developed by JBI, the Joanna Briggs Institute, specifically for conducting a scoping review (13). The manuscript was structured in adherence to the Preferred Reporting Standards for Systematic Reviews and Meta-Analysis (PRISMA) extension for scoping reviews (14). The premise for this review is defined using the PICO criteria below for population, intervention, comparisons, and outcomes:
• Population: adults and children enrolled in studies comparing plant-based diet quality to health outcomes
• Intervention: dietary assessment using a food frequency questionnaire with categorization into an overall PDI or PVD, a healthful PDI or a healthful PVD (hPDI or hPVD), and an unhealthful PDI or an unhealthful PVD (uPDI or uPVD)
• Comparisons: when more than one index is reported, association with outcomes for the overall index versus the healthful index and for the healthful index versus the unhealthful index
• Outcomes: disease incidence, prevalence, or mortality as reported by the investigators, with hazard ratios for the highest dietary index level versus the lowest level (e.g., by quartiles, quintiles, deciles).
To be included in this review, the source article had to report original research assessing the association of a plant-based diet with a clinically relevant health outcome. The study design could be observational (e.g., cohort, case–control, or cross-sectional), experimental (e.g., clinical trial, randomized controlled trial), or population-based (e.g., national survey data) but must have included a healthful plant-based dietary index (hPDI or hPVD), an unhealthful index (uPDI or uPVD), or both. We excluded reviews, systematic reviews, meta-analyses, commentaries, case series, and correspondence (e.g., consensus reports).
Peer-reviewed articles meeting the above criteria, and addressing the PICO question above, were included if published between the period of January 2010 through April 2023, without language restrictions. Searches were performed with the assistance of an experienced information specialist in databases that included MEDLINE/PubMed, CINAHL, EMBASE, and Web of Science. The initial search strategy, drafted by an information specialist and refined through team discussion, was implemented in MEDLINE/Med, CINAHL, and EMBASE and used the terms “((healthy AND unhealthy) OR (healthful AND unhealthful)) AND (vegetarian OR vegan OR plant-based OR provegetarian OR pro-vegetarian OR plant-predominant).” Upon reviewing the initial search results we noted that some of the relevant articles cited publications that might also be relevant to our review, but instead of” unhealthy or unhealthful” used the terms “less healthy or less healthful.” We therefore updated the search with the expanded terms: ““((healthy AND unhealthy) OR (healthful AND unhealthful) OR (healthy AND “less healthy”) OR (healthful AND “less healthful”) OR (healthy AND overall) OR (healthful AND overall)) AND (vegetarian OR vegan OR plant-based OR provegetarian OR pro-vegetarian OR plant-predominant).”
To increase consistency, dual reviewers (HJM, MAW) screened articles for relevance, with disagreements on study selection and data extraction resolved by consensus and discussion, if needed. To reduce the possibility that articles were missed in the MEDLINE/Med, CINAHL, and EMBASE searches, a final search was performed in Web of Science for publications citing any of three key articles considered representative of source articles for the review (see Results for specific articles used).
A data-charting form for Excel was developed to extract all information from each source article, including information on authorship, article characteristics (publication year, country of origin, study aims or purpose), study sample (origin, size, demographics), sampling method (convenience, random, population cohort), sampling time frame (recruitment years), methodology (study design, food frequency questionnaire details), dietary classification (e.g., healthful unhealthful), follow-up information, outcomes assessed (including comparisons, such as by extreme quartiles, quintiles, or deciles), results (usually adjusted hazard ratios), and conclusions. We did not perform a risk of bias assessment for the included source articles because this is unnecessary in a scoping review (11) and is not part of the recommended reporting standards (14).
We performed a descriptive and qualitative analysis, seeking to map the existing evidence and to highlight how considerations of plant-diet quality might impact associations with clinically important outcomes. We did not include quantitative data. Such as effect size, nor did we perform any data pooling using meta-analytic techniques, but we do include quantitative results for individual studies in the online Supplementary Appendix. Findings are reported using the PDI, which was used in 95% of studies, recognizing that this also includes a few studies that used the PVD. As consistent with scoping review methodology, we did formally test hypotheses using measures of statistical significance (12–14).
The primary outcome data from each source article was the association of the PDI, hPDI, and uPDI to each of the reported outcomes, as reflected by comparing the highest level (quartile, quintile, or decile) of each index to the lowest level. An association was termed “favorable” if both statistically significant and a higher index level correlated with a better health outcome (e.g., less disease, lower mortality, better cardiometabolic marker). Conversely, an association was termed “unfavorable” if both statistically significant and a higher index level correlated with a worse health outcome (e.g., more disease, higher mortality, adverse cardiometabolic marker). We did not judge any statistically non-significant associations as favorable versus unfavorable, nor did we seek to make direct statistical comparisons between different indices.
We further assessed secondary outcomes on the concordance, or discordance, of the associations for the 3 indices (PDI, hPDI, uPDI) by comparing the statistical significance and directionality of the relationship to outcome in a specific study. This was used to classify comparisons between hPDI versus PDI and between hPDI versus uPDI as “favors hPDI,” “both same,” or “favors” comparator (PDI or uPDI):
• Favors hPDI: when comparing the hPDI to the PDI (or uPDI) the comparison “favors hPDI” if the hPDI had a significantly favorable HR and the PDI (or uPDI) had a non-significant HR, or if the hPDI had a non-significant HR but the PDI (or uPDI) had significantly unfavorable HR. In both cases the HRs were discordant and the hPDI did “better” than the comparator, leading a result that “favors hPDI.”
• Both same: when comparing the hPDI to the PDI the comparisons was deemed “both same” if the HRs for each index were concordant: both significantly favorable, both non-significant, or both significantly non-favorable. The same criteria applied to comparing the hPDI to the uPDI.
• Favors PDI: when comparing the hPDI to the PDI the comparison “favors PDI” if the PDI had a significantly favorable HR and the hPDI was non-significant, or if the PDI had a non-significant HR but the hPDI had significantly unfavorable HR. In both cases the HRs were discordant and the PDI did “better” than the PDI, leading a result that “favors PDI.”
• Favors uPDI: when comparing the hPDI to the uPDI the comparison “favors uPDI” if the uPDI had a significantly favorable HR and the hPDI was non-significant, or if the uPDI had a non-significant HR but the hPDI had significantly unfavorable HR. In both cases the HRs were discordant and the uPDI did “better” than the uPDI, leading a result that “favors uPDI.”
The above comparisons are reported for studies contributing to specific outcome (e.g., all-cause mortality, hypertension, metabolic syndrome) and were also combined for all comparisons and outcomes to give a global perspective of how stratifying a plant-based diet based on food quality might impact associations.
The literature search (Figure 1) identified 95 source articles (10, 15–108), for which full details of data extraction can be found in the online Supplementary Appendix. The Web of Science search was based on citations of three articles (23, 46, 87), published between 2017 and 2019, identified in the prior searches and considered representative of those sought for the review. Articles were published between 2017 and 2023 with a median sample size of 3,646, ranging from 22 to 592,571, and with upper and lower quartiles of 456 and 14,568, respectively. The countries of origin for the source articles were United States (n = 30 publications), Iran (n = 20), Korea (n = 9), China (n = 8), Spain (n = 8), United States/United Kingdom (n = 3), Australia (n = 3), Germany (n = 3), Singapore (n = 3), Saudi Arabia (n = 2), Greece (n = 2), France (n = 2), Japan (n = 1), and Belgium (n = 1).
All studies were observational, with a longitudinal (cohort) design for 54%, cross-sectional for 37%, case–control format for 9%. The PDI was used in 95% of studies, with only 5 studies reporting PVG as the primary outcome (10, 21, 38, 78, 79). The index combinations were PDI/hPDI/uPDI in 69 studies, PDI/hPDI in 9, hPDI/uPDI in 7, PVG/hPVG/uPVG in 5, PDI/hPDI/uPDI/PVG in 3, and hPDI only in 2. The primary outcomes were obesity in 21 studies, cardiometabolic risk factors in 20, mortality in 10, diabetes in 9, psychiatric disorders in 9, men’s health in 8, cardiovascular disease in 7, breast cancer in 5, inflammation in 5, chronic kidney disease in 3, sleep quality in 3, quality of life in 2, bone biomarkers in 2, and 1 each for asthma, glioma, fecundability, COVID-19, micronutrients, and infant growth.
The hPDI demonstrated the most frequent association with favorable health outcomes (Table 2), with 36.2% having significantly more favorable results (p < 0.05, as reported by the investigators) when comparing the highest hPDI level to the lowest. Conversely, higher uPDI levels were associated with unfavorable health outcomes for 32.5% of comparisons. The hPDI was almost never (0.4%) associated with unfavorable outcomes and the uPDI was rarely associated (2.0%) with favorable outcomes. Although 24.6% of higher PDI levels were associated with favorable health outcomes, the hPDI was about 50% more likely to demonstrate this type of relationship (36.2% vs. 24.6%).
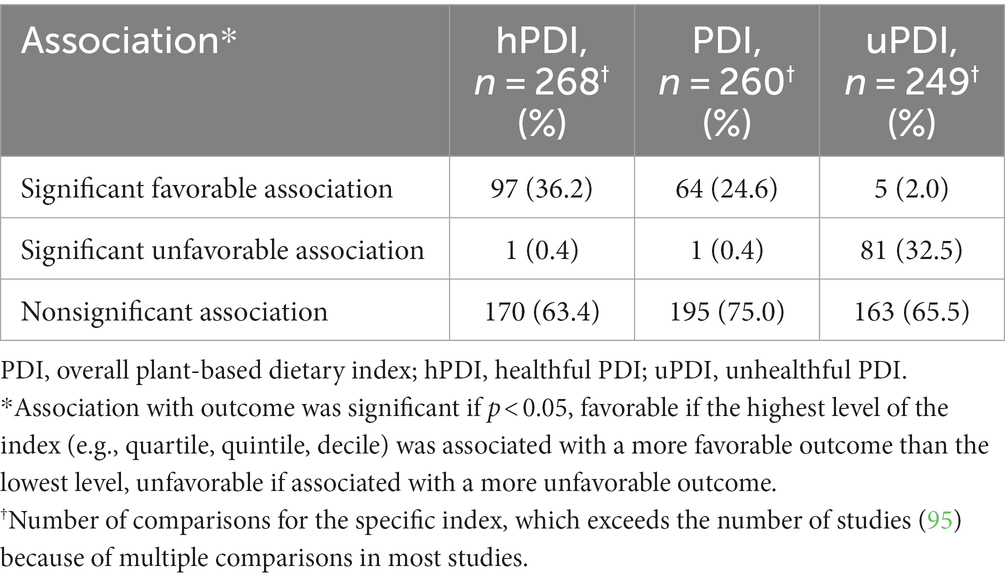
Table 2. Association of plant-based indices with health outcomes, showing the frequency of association type (favorable, unfavorable, or nonsignificant) for each index (hPDI, PDI, or uPDI).
When discordant associations (Table 3) were observed for the hPDI versus a comparator (PDI or uPDI), the results most often favored the hPDI (23.0%) over the PDI and always favored the hPDI (52.3%) over the uPDI. Concordant associations were most often observed for the hPDI versus PDI (70.4%) with a minority of hPDI versus uPDI associations showing concordance (47.7%). For all comparisons combined, 59.6% had concordant results, 36.9% were discordant favoring the hPDI, and only 3.5% were discordant favoring the comparator (PDI or uPDI).
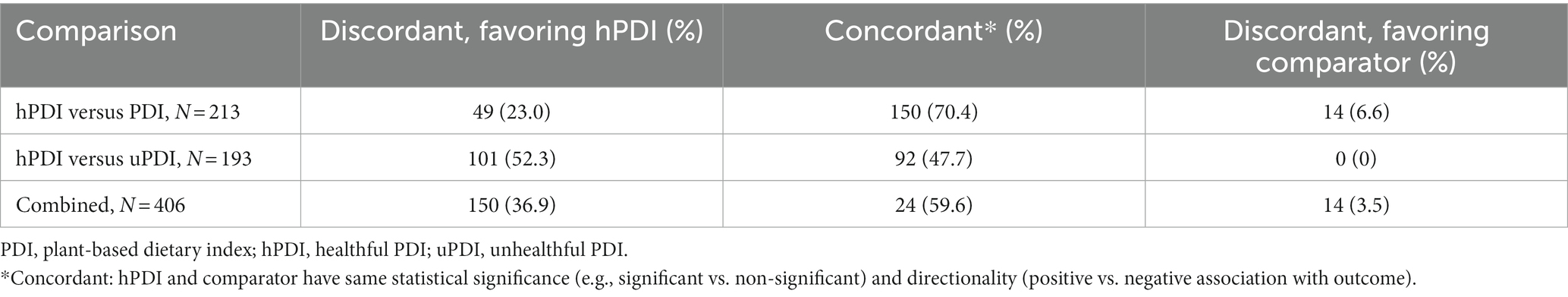
Table 3. Concordant versus discordant comparisons, showing the frequency of comparison outcome (discordant favoring hPDI, concordant, or discordant favoring comparator) for hPDI versus comparators (PDI or uPDI).
For the outcomes in Table 4 with at least 10 comparisons of the highest versus lowest index levels, the most frequent significantly favorable associations with the hPDI were found for psychiatric disorders (94% of comparisons), diabetes (64%), cardiovascular disease (45%), mortality (43%), and obesity (42%). The most frequent significantly unfavorable associations with the uPDI were found for psychiatric disorders (50%), mortality (39%), obesity (36%), and cardiometabolic risk factors (31%). The hPDI level was more frequently associated with favorable outcomes than the uPDI was associated with unfavorable outcomes for psychiatric disorders (94% vs. 50%), diabetes (64% vs. 9%), and cardiovascular disease (45% vs. 9%).
Tables 5–13 show the frequency of concordant versus discordant plant-based index comparisons by specific outcome studied. In Table 5, mortality, comparisons of the hPDI versus PDI are largely concordant, but some of the outcomes for hPDI versus uPDI are often discordant, as seen for all-cause mortality and cardiovascular disease mortality. A similar pattern is seen in Table 7 for psychiatric disorders (anxiety, cognitive impairment, and depression) and in Table 11 for obesity (fatty liver disease, visceral adiposity, central obesity, general obesity, and overweight or obese). Specific outcomes in other tables also show discordance that favors the hPDI over the uPDI, including Table 6 (hypertension, metabolic syndrome, and HDL cholesterol), Table 8 (breast cancer and colorectal cancer), Table 9 (serum insulin and type 2 diabetes), and Table 13 (sleep quality index).
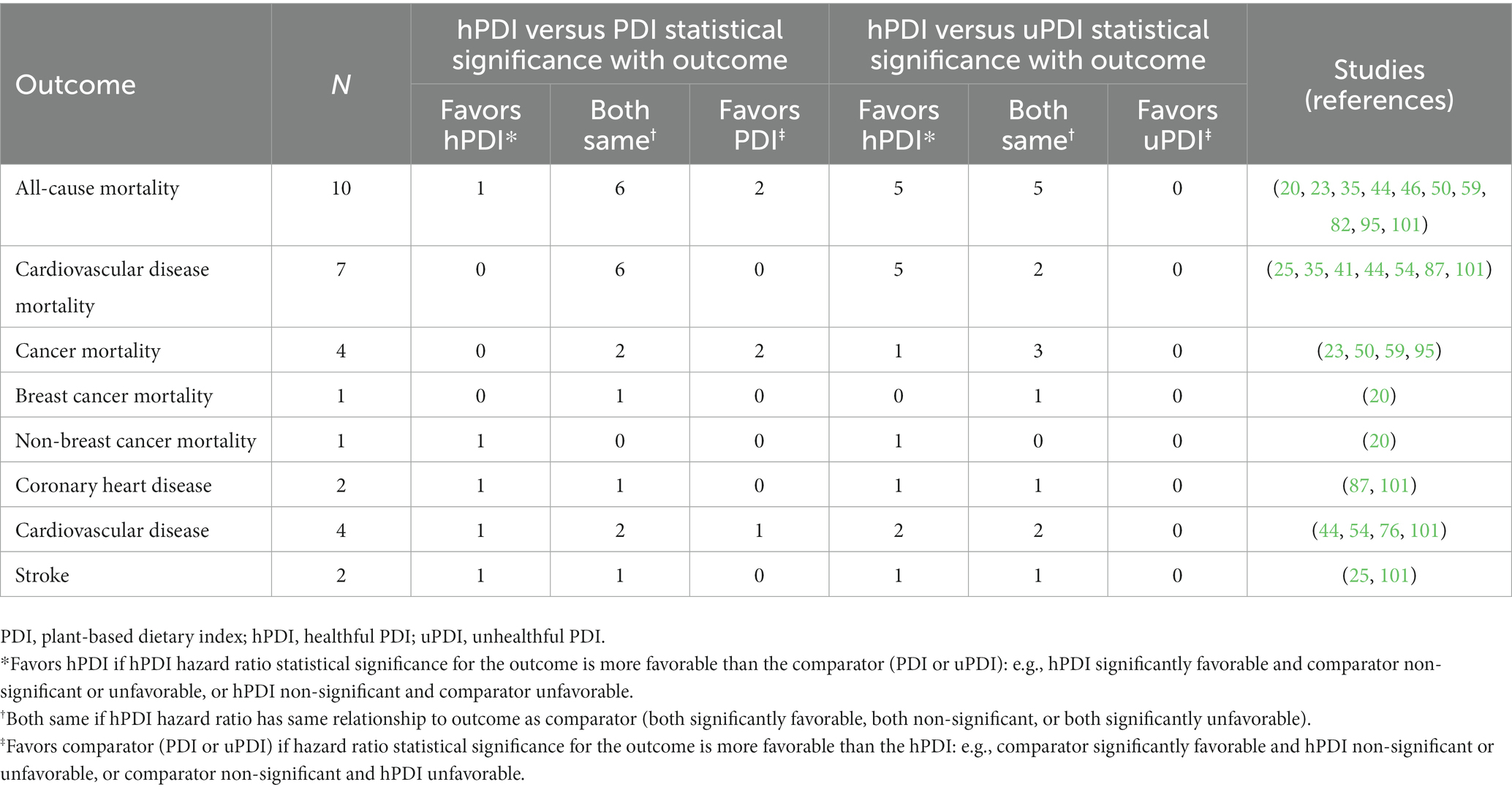
Table 5. Mortality and cardiovascular diseases, concordant versus discordant plant-based index comparisons.
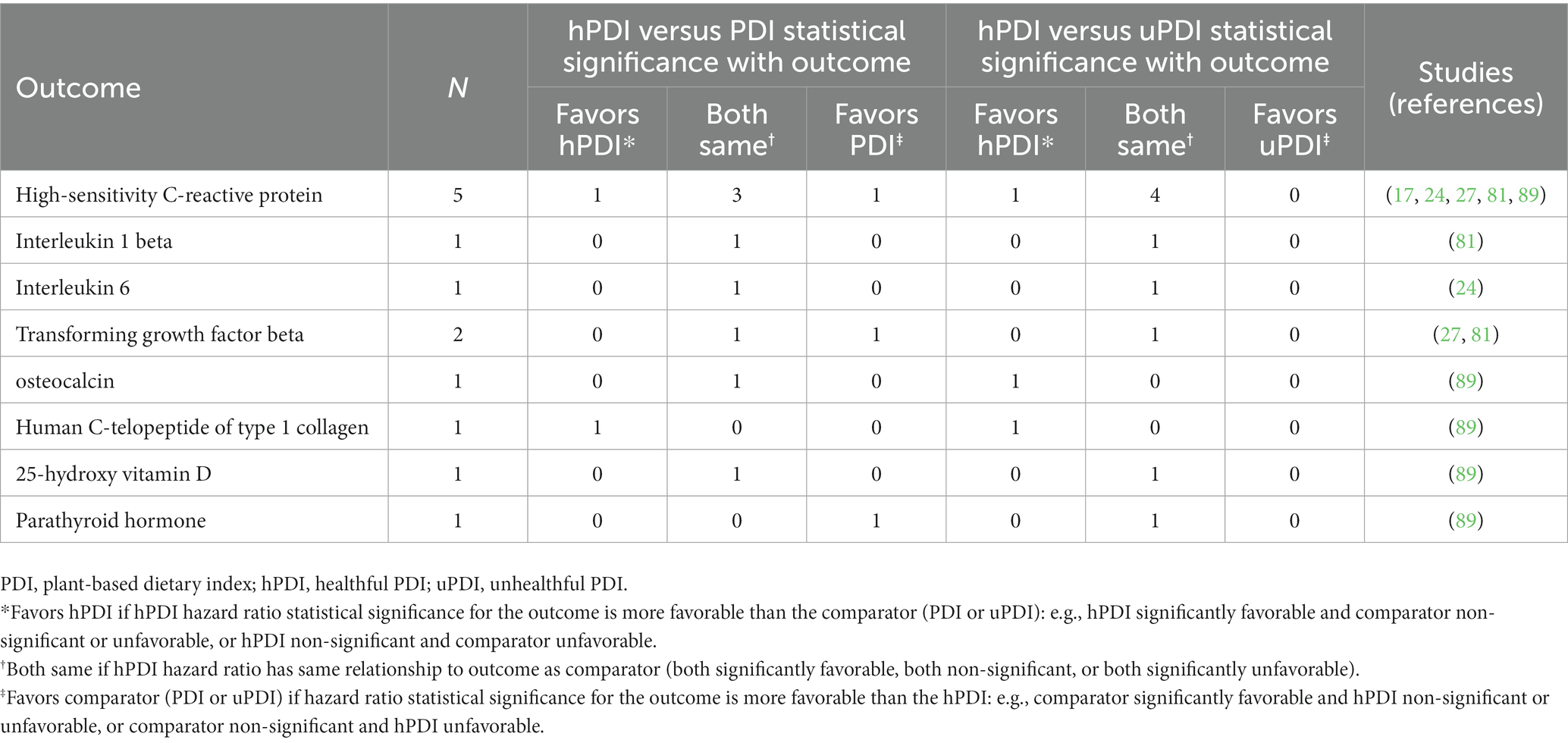
Table 10. Inflammation and inflammatory markers, concordant versus discordant plant-based index comparisons.
The aim of our scoping review was to highlight the importance of assessing plant-based diet quality, beyond using “plant-based” as an umbrella term (e.g., vegan, vegetarian), when assessing the association of diet type with health outcomes. We found a robust, and rapidly growing, body of literature that investigates how the quality and nutritional value of a plant-based diet is positively associated with health outcomes. The 95 studies we identified, most published in 2021 or later, represent diverse population cohorts from investigators in the United States, Western Europe, Middle East, Asia, and Australia. The diverse outcomes (Table 4) are most often related to the broad topics of obesity, cardiometabolic risk factors, overall- and disease-specific mortality, diabetes, cardiovascular disease, psychiatric disorders, men’s health, and cardiovascular disease.
For 33 to 36% of comparisons (Table 2), the highest levels of the hPDI and uPDI are associated with favorable and unfavorable health outcomes, respectively, whereas the highest PDI levels have favorable associations in only 25% of comparisons. Moreover, when the index associations are discordant (Table 3), the hPDI is more favorably associated with outcomes than the uPDI in 52% of comparisons and the hPDI is more favorably associated with outcomes than the PDI in 23% of comparisons. In aggregate, these findings show that stratifying the PDI into healthful versus unhealthful indices is superior to the PDI alone in assessing how plant-based diets are associated with health outcomes.
Our findings also identify some gaps in the existing knowledge base. For example, we did not identify any studies from investigators in Africa, South America, Central America, Scandinavia, or Eastern Europe, which raises concerns about generalizability, potentially to resource-challenged countries and regions. There is also limited information on how plant-based diet quality is associated with many clinical outcomes, based on conditions not listed in Table 4 and on those with only a few source articles (e.g., COVID-19, quality of life, sleep quality, fecundability, infant growth, glioma, bone biomarkers, and some cancers). Even when there are many source articles in an outcome category, more comparable outcomes may only be covered in 1 or 2 studies (Tables 5–13) and the measures used are heterogeneous.
The gaps and heterogeneity noted help to explain why relatively few meta-analyses have been performed using not just PDI, but also hPDI and uPDI. In all published reviews, however, where this distinction has been made, 4–6,9 the investigators find significant quantitative benefits related to diet quality, consistent with our qualitative and descriptive findings. This work builds upon a precursor concept of assessing mortality with a provegetarian food pattern, emphasizing plant-derived foods of any quality, in contrast to broad dietary classifications as vegan, vegetarian, or omnivore. Satija et al. (4) in 2016 ushered in the current focus on healthful versus unhealthful plant-based indices, when they showed substantially lower risk of developing type 2 diabetes with a diet rich in high-quality plant foods (Table 1), and a lower intake of animal foods and less healthy plant foods.
A benefit of defining a dietary pattern based on the frequency of healthy plant-foods consumed is the ability to study large populations using continuous indices (PDI, hPDI, uPDI), based on dietary assessment data to evaluate the relative quality of individuals’ dietary intakes (9). Moreover, these indices often identify benefits of healthy plant foods that might be missed when using a single overall measure of plant foods in the diet (Tables 2–4). Plant-based diet indices overcome limitations of discrete dietary categories because they align with the continuum of plant-forward, flexitarian, diets that exist in real-world settings. Further, the goal of increasing healthy plant foods in a diet, as opposed to restricting animal foods, is not only appealing but aligns with research showing that mortality may be driven more by the paucity of healthy plant foods (e.g., whole grains, fruits, nuts/seeds, legumes) than by the excess of meat (red and processed) and unhealthy plant foods (e.g., sugar-sweetened beverages) (109).
Differentiating between healthy versus less healthy aspects of plant-based diets has significant implications for researchers, policy makers (e.g., clinical practice guideline developers), and for consumers and the public (Table 14). Beyond focusing on overall diet quality, the healthfulness of individual foods has also received increased attention with nutrient profiling systems such as the Food Compass, which assigns a score from 1 (least healthful) to 100 (most healthful) based on 54 attributes across 9 domains: nutrient ratios, vitamins, minerals, food ingredients, additives, processing, specific lipids, fiber and protein, and phytochemicals (110). The healthy plant foods in Table 1 receive high scores on the Food Compass (110), which is associated with optimal cardiometabolic health and lower all-cause mortality (111). In contrast, the less healthy plant-based foods and the animal foods in Table 1 receive much lower scores.
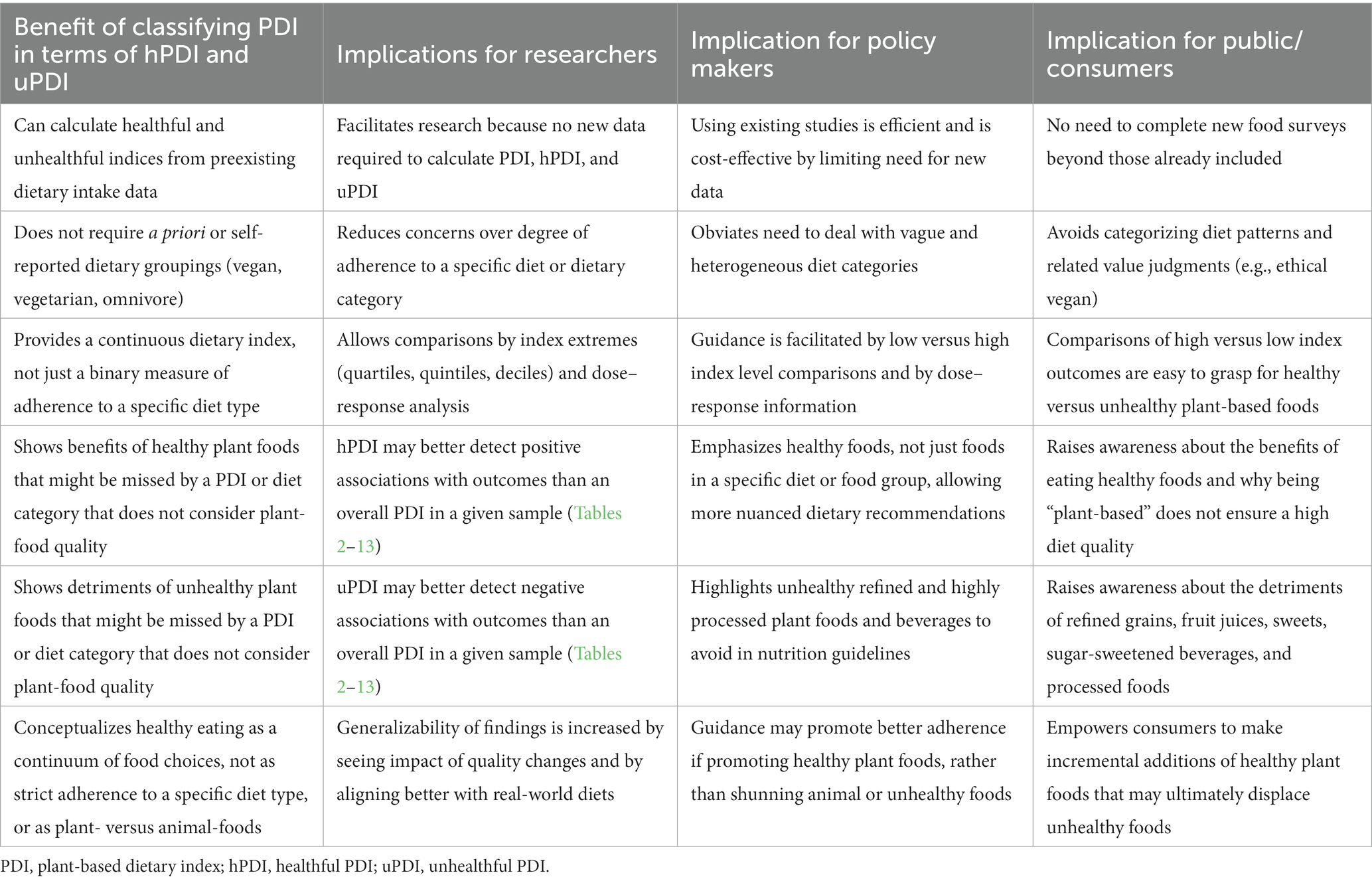
Table 14. Benefits of using the healthful and unhealthful plant-based dietary index in nutrition research.
The inclusion of potatoes as a less healthy food in Table 1 is based on Satija and colleagues (4), who pioneered the concept of hPDI versus uPDI. We did not, however, assess the specific food components of the dietary indices in our included studies, so we do not know how specific investigators categorized potatoes. The association of potato consumption with health outcomes is controversial, with some pooled analyses of prospective studies finding a higher risk of hypertension or type 2 diabetes (112–114), but others showing no association with obesity, mortality, type 2 diabetes, or cardiovascular disease (115, 116). One study found a higher risk of type 2 diabetes with French fries, which was reduced by replacing potatoes with whole grains (112).
The animal foods in Table 1 do not distinguish by their potential health impact (healthy vs. less healthy) even though their inclusion in the diet adversely affects the plant-based dietary indices. Systematic reviews, however, have often shown adverse associations of omnivore diets with many of the health outcomes in our source articles, including obesity (117), type 2 diabetes (118), breast cancer (119), all-cause mortality (120), coronary artery disease (5, 121), inflammatory biomarkers (122), and cardiometabolic risk factors (123, 124). Similarly, the Global Burden of Disease Study found positive associations of high dietary trans fats, red meat, processed meat, and sugar-sweetened beverages with mortality from non-communicable diseases, but larger associations were found when the diet was low in healthy plant foods (whole grains, fruits, nuts, seeds, legumes, or vegetables) (109). Consuming fish and seafood have less consistent health associations compared with meat or plant foods (119, 120, 124), which is also the case for eggs and dairy products (125–127).
Strengths of our research include using a priori protocols for conducting and reporting the scoping review (13, 14), which is the first to systematically assess the contributions of hPDI and uPDI as correlates of health status. As recommended as a best practice when conducting a scoping review (14), we used dual, independent investigators to assess study eligibility and extract data, thereby reducing bias and improving accuracy. We contribute to understanding of how the quality of a plant-based diet can impact associations with health outcomes overall (Tables 2, 3), focusing on the novel concept of concordance versus discordance (Tables 3, 5–13), which has not been previously reported. We identified gaps in the existing knowledge base and provided perspective on the implications of our review findings for investigators, policy makers, and consumers (Table 14).
Limitations of our research, as for any systematic review, relate primarily to the breadth of available source articles. We used rigorous techniques, with dual investigators, to identify source articles in PubMed/MEDLINE, CINAHL, and EMBASE, but recognize that the subsequent Web of Science citation search was done post-hoc, which may have introduced bias, but is similar to checking source article bibliographies for additional relevant articles in a traditional systematic review. A scoping review does not include assessing study quality or pooling data with meta-analytic techniques (13), so we do not know the overall risk of bias or the level of heterogeneity in study protocols, outcome assessment, or results reporting. Our goal, however, was to help inform decisions and raise awareness about the importance of plant-based diet quality when interpreting evidence, in contrast to a systematic review for which risk of bias assessment is an inherent aspect of evidence synthesis.
Although all studies used the hPDI, uPDI, or both (or in a few cases the hPVD, uPVD, or both), there were some differences in how the indices were defined and calculated, even if based on the broad principles in Table 1. The general concept, however, of distinguishing healthy versus less healthy plant-based foods, is incorporated in most current scoring methods for assessing plant-based diet quality (128). Further, the extreme comparisons of index levels were based on varying thresholds, which included quartiles, quintiles, and deciles. We did not provide quantitative estimates of effect size (individual studies or pooled analyses), although this is more a limitation of scoping reviews, in general, than our specific research. Last, we do not know the generalizability of our findings to specific populations (e.g., pregnant or lactating women), but the included articles were often based on large population cohorts (see online Supplementary Appendix) that would support relevance to diverse subject groups.
Another limitation relates to assessing concordance (Table 3) using statistical significance as the primary determinant, and directionality of the association (positive vs. negative) as a secondary determinant for statistically significant associations. This could explain the relatively high levels of concordance between the hPDI and PDI (70.4%), and, to a lesser extent, between the hPDI and uPDI (47.7%), because the magnitude of effect size is not part of this determination. Although we purposefully did not report effect sizes, we did observe that they nearly always favored the hPDI in magnitude, even if not statistically significant (see individual study outcome data in the online Supplementary Appendix).
Our findings, based on 95 included studies, demonstrate that distinguishing healthy versus less healthy plant foods in dietary indices can better detect significant associations with health outcomes than a single, overall plant-based dietary index. A high level of healthy plant food consumption was most often associated with favorable outcomes for obesity, mortality, diabetes, cardiovascular disease, and psychiatric disorders, whereas a high level of less healthy plant food consumption was most often associated with unfavorable outcomes for obesity, mortality, psychiatric disorders, and cardiometabolic risk factors. When there were discordant associations for the hPDI compared to the uPDI or PDI, the findings always favored the hPDI over the uPDI, and nearly always favored the hPDI over the PDI.
These results, combined with the implications of healthy plant food consumption for researchers, policy makers, and consumers (Table 14), suggest that the current global trend of rapid growth in related research and publications is likely to continue. Future research should incorporate measures of diet quality when assessing the association of plant-based diets with health outcomes. With increasing reporting and standardization of plant-based indices that adjust for diet quality, we anticipate a blossoming number of systematic reviews and meta-analyses that will assist guideline developers and policy makers in making informed, evidence-based recommendations.
RR conception and design of the work, data analysis and interpretation, drafting of the work, approval for publication of the content, accountability for all aspects of the work. HJ and MW design of the work, data acquisition, critical revision of content, approval for publication of the content, accountability for all aspects of the work. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor AB declared a shared committee American College of Lifestyle Medicine with the authors RR at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1211535/full#supplementary-material
1. Dehghan, M, Mente, A, Zhang, X, Swaminathan, S, Li, W, Mohan, V, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. (2017) 390:2050–62. doi: 10.1016/S0140-6736(17)32252-3
2. Reynolds, A, Mann, J, Cummings, J, Winter, N, Mete, E, and Te Morenga, L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. (2019) 393:434–45. doi: 10.1016/S0140-6736(18)31809-9
3. Bechthold, A, Boeing, H, Schwedhelm, C, Hoffmann, G, Knüppel, S, Iqbal, K, et al. Food groups and risk of coronary heart disease, stroke and heart failure: a systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr. (2019) 59:1071–90. doi: 10.1080/10408398.2017.1392288
4. Satija, A, Bhupathiraju, SN, Rimm, EB, Spiegelman, D, Chiuve, SE, Borgi, L, et al. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med. (2016) 13:e1002039. doi: 10.1371/journal.pmed.1002039
5. Quek, J, Lim, G, Lim, WH, Ng, CH, So, WZ, Toh, J, et al. The association of plant-based diet with cardiovascular disease and mortality: a meta-analysis and systematic review of prospective cohort studies. Front Cardiovasc Med. (2021) 8:756810. doi: 10.3389/fcvm.2021.756810
6. Gan, ZH, Cheong, HC, Tu, YK, and Kuo, PH. Association between plant-based dietary patterns and risk of cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. Nutrients. (2021) 13:3952. doi: 10.3390/nu13113952
7. Chen, Z, Drouin-Chartier, JP, Li, Y, Baden, MY, Manson, JE, Willett, WC, et al. Changes in plant-based diet indices and subsequent risk to type 2 diabetes in women and men: three U.S. prospective cohorts. Diabetes Care. (2021) 44:663–71. doi: 10.2337/dc20-1636
8. Satija, A, Malik, V, Rimm, EB, Sacks, F, Willett, W, and Hu, FB. Changes in intake of plant-based diets and weight change: results from 3 prospective cohort studies. Am J Clin Nutr. (2019) 110:574–82. doi: 10.1093/ajcn/nqz049
9. Jarvis, SE, Nguyen, M, and Malik, VS. Association between adherence to plant-based dietary patterns and obesity risk: a systematic review of prospective cohort studies. Appl Physiol Nutr Metab. (2022) 47:1115–33. doi: 10.1139/apnm-2022-0059
10. Romanos-Nanclares, A, Toledo, E, Sánchez-Bayona, R, Sánchez-Quesada, C, Martínez-González, MÁ, and Gea, A. Healthful and unhealthful provegetarian food patterns and the incidence of breast cancer: results form a Mediterranean cohort. Nutrition. (2020) 79-80:110884–15. doi: 10.1016/j.nut.2020.110884
11. Munn, Z, Peters, MDJ, Stern, C, Tufanaru, C, McArthur, A, and Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMJ Med Res Methodol. (2018) 18:143. doi: 10.1186/s12874-018-0611-x
12. Lockwood, C, dos Santos, KB, and Pap, R. Practical guidance for knowledge synthesis: scoping review methods. Asian Nursing Res. (2019) 13:287–94. doi: 10.1016/j.anr.2019.11.002
13. Peters, MDJ, Godfrey, C, McInerney, P, Munn, Z, Tricco, AC, and Khalil, H. Chapter 11: scoping reviews (2020 version) In: E Aromataris and Z Munn, editors. JBI Manual for Evidence Synthesis. Adelaide, Australia: JBI (2020)
14. Tricco, AC, Lillie, E, Zarin, W, O'Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Int Med. (2018) 169:467–73. doi: 10.7326/M18-0850
15. Ait-Hadad, W, Bédard, A, Delvert, R, Orsi, L, Chanoine, S, Dumas, O, et al. Plant-based diets and the incidence of asthma symptoms among elderly women, and the mediating role of body mass index. Nutrients. (2022) 15:52. doi: 10.3390/nu15010052
16. Aljuraiban, G, Chan, Q, Gibson, R, Stamler, J, Daviglus, ML, Dyer, AR, et al. INTERMAP research group. Association between plant-based diets and blood pressure in the INTERMAP study. BMJ Nutr Prev Health. (2020) 3:133–42. doi: 10.1136/bmjnph-2020-000077
17. Aljuraiban, GS, Gibson, R, Al-Freeh, L, Al-Musharaf, S, Shivappa, N, Hébert, JR, et al. Associations among plant-based dietary indexes, the dietary inflammatory index, and inflammatory potential in female college students in Saudi Arabia: a cross-sectional study. J Acad Nutr Diet. (2021) 1:S2212–672. doi: 10.1016/j.jand.2021.08.111
18. Aljuraiban, GS. Plant-based dietary indices and stress in female college students: a cross-sectional study. Br J Nutr. (2022) 127:123–32. doi: 10.1017/S0007114521001689
19. Amini, MR, Shahinfar, H, Djafari, F, Sheikhhossein, F, Naghshi, S, Djafarian, K, et al. The association between plant-based diet indices and metabolic syndrome in Iranian older adults. Nutr Health. (2021) 27:435–44. doi: 10.1177/0260106021992672
20. Anyene, IC, Ergas, IJ, Kwan, ML, Roh, JM, Ambrosone, CB, Kushi, LH, et al. Plant-based dietary patterns and breast cancer recurrence and survival in the pathways study. Nutrients. (2021) 13:3374. doi: 10.3390/nu13103374
21. Asfura-Carrasco, D, Santiago, S, Zazpe, I, Gómez-Donoso, C, Bes-Rastrollo, M, and Martínez-González, MÁ. Healthful and unhealthful provegetarian food patterns and micronutrient intake adequacy in the SUN cohort. Public Health Nutr. (2022) 26:1–12. doi: 10.1017/S136898002200204X
22. Baden, MY, Kino, S, Liu, X, Li, Y, Kim, Y, Kubzansky, LD, et al. Changes in plant-based diet quality and health-related quality of life in women. Br J Nutr. (2020) 124:960–70. doi: 10.1017/S0007114520002032
23. Baden, MY, Liu, G, Satija, A, Sun, Q, Fung, TT, Rimm, EB, et al. Changes in plant-based diet quality and total and cause-specific mortality. Circulation. (2019) 140:979–91. doi: 10.1161/CIRCULATIONAHA.119.041014
24. Baden, MY, Satija, A, Hu, FB, and Huang, T. Change in pant-based diet quality is associated with changes in plasma adiposity-associated biomarker concentrations in women. J Nutr. (2019) 149:676–86. doi: 10.1093/jn/nxy301
25. Baden, MY, Shan, Z, Wang, F, Li, Y, Manson, JE, Rimm, EB, et al. Quality of plant-based diet and risk of total, ischemic, and hemorrhagic stroke. Neurology. (2021) 96:e1940–53. doi: 10.1212/WNL.0000000000011713
26. Bhupathiraju, SN, Sawicki, CM, Goon, S, Gujral, UP, Hu, FB, Kandula, NR, et al. A healthy plant-based diet is favorably associated with cardiometabolic risk factors among participants of south Asian ancestry. Am J Clin Nutr. (2022) 116:1078–90. doi: 10.1093/ajcn/nqac174
27. Bolori, P, Setaysh, L, Rasaei, N, Jarrahi, F, Yekaninejad, MS, and Mirzaei, K. Adherence to a healthy plant diet may reduce inflammatory factors in obese and overweight women-a cross-sectional study. Diabetes Metab Syndr. (2019) 13:2795–802. doi: 10.1016/j.dsx.2019.07.01
28. Carto, C, Pagalavan, M, Nackeeran, S, Blachman-Braun, R, Kresch, E, Kuchakulla, M, et al. Consumption of a healthy plant-based diet is associated with a decreased risk of erectile dysfunction: a cross-sectional study of the National Health and nutrition examination survey. Urology. (2022) 161:76–82. doi: 10.1016/j.urology.2021.12.021
29. Chen, G, Su, M, Chu, X, Wei, Y, Chen, S, Zhou, Y, et al. Plant-based diets and body composition in Chinese omnivorous children aged 6-9 years old: a cross-sectional study. Front Nutr. (2022) 9:918944. doi: 10.3389/fnut.2022.918944
30. Chen, GC, Koh, WP, Neelakantan, N, Yuan, JM, Qin, LQ, and Van, DRM. Diet quality indices and risk of type 2 diabetes mellitus: the Singapore Chinese health study. Am J Epidemiol. (2018) 187:2651–61. doi: 10.1093/aje/kwy183
31. Chen, Z, Qian, F, Liu, G, Li, M, Voortman, T, Tobias, DK, et al. Prepregnancy plant-based diets and the risk of gestational diabetes mellitus: a prospective cohort study of 14,926 women. Am J Clin Nutr. (2021) 114:1997–2005. doi: 10.1093/ajcn/nqab275
32. Daneshzad, E, Keshavarz, SA, Qorbani, M, Larijani, B, Bellissimo, N, and Azadbakht, L. Association of dietary acid load and plant-based diet index with sleep, stress, anxiety and depression in diabetic women. Br J Nutr. (2020) 123:901–12. doi: 10.1017/S0007114519003179
33. Daneshzad, E, Moradi, M, Maracy, MR, Brett, NR, Bellissimo, N, and Azadbakht, L. The association of maternal plant-based diets and the growth of breastfed infants. Health Promot Perspect. (2020) 10:152–61. doi: 10.34172/hpp.2020.25
34. Daneshzad, E, Jahangir, F, Heshmati, J, Larijani, B, Surkan, PJ, and Azadbakht, L. Associations between plant-based dietary indices and dietary acid load with cardiovascular risk factors among diabetic patients. Int J Diabetes Dev Countries. (2021) 41:71–83. doi: 10.1007/s13410-020-00862-z
35. Delgado-Velandia, M, Maroto-Rodríguez, J, Ortolá, R, García-Esquinas, E, Rodríguez-Artalejo, F, and Sotos-Prieto, M. Plant-based diets and all-cause and cardiovascular mortality in a nationwide cohort in Spain: the ENRICA study. Mayo Clin Proc. (2022) 97:2005–15. doi: 10.1016/j.mayocp.2022.06.008
36. Flores, AC, Heron, C, Kim, JI, Martin, B, Al-Shaar, L, Tucker, KL, et al. Prospective study of plant-based dietary patterns and diabetes in Puerto Rican adults. J Nutr. (2021) 151:3795–800. doi: 10.1093/jn/nxab301
37. Ghadiri, M, Cheshmazar, E, Shateri, Z, Gerami, S, Nouri, M, and Gargari, BP. Healthy plant-based diet index as a determinant of bone mineral density in osteoporotic postmenopausal women: a case-control study. Front Nutr. (2023) 9:1083685. doi: 10.3389/fnut.2022.1083685
38. Gómez-Donoso, C, Martínez-González, MÁ, Martínez, JA, Gea, A, Sanz-Serrano, J, Perez-Cueto, FJA, et al. A provegetarian food pattern emphasizing preference for healthy plant-derived foods reduces the risk of overweight/obesity in the SUN cohort. Nutrients. (2019) 11:1553. doi: 10.3390/nu11071553
39. Gómez-Martínez, C, Babio, N, Júlvez, J, Nishi, SK, Fernández-Aranda, F, Martínez-González, MÁ, et al. Impulsivity is longitudinally associated with healthy and unhealthy dietary patterns in individuals with overweight or obesity and metabolic syndrome within the framework of the PREDIMED-plus trial. Int J Behav Nutr Phys Act. (2022) 19:101. doi: 10.1186/s12966-022-01335-8
40. Hamaya, R, Ivey, KL, Lee, DH, Wang, M, Li, J, Franke, A, et al. Association of diet with circulating trimethylamine-N-oxide concentration. Am J Clin Nutr. (2020) 112:1448–55. doi: 10.1093/ajcn/nqaa225
41. Heianza, Y, Zhou, T, Sun, D, Hu, FB, Manson, JE, and Qi, L. Genetic susceptibility, plant-based dietary patterns, and risk of cardiovascular disease. Am J Clin Nutr. (2020) 112:220–8. doi: 10.1093/ajcn/nqaa107
42. Jung, S, and Park, S. Positive association of unhealthy plant-based diets with the incidence of abdominal obesity in Korea: a comparison of baseline, most recent, and cumulative average diets. Epidemiol Health. (2022) 44:e2022063. doi: 10.4178/epih.e2022063
43. Kawasaki, Y, Akamatsu, R, Fujiwara, Y, Omori, M, Sugawara, M, Yamazaki, Y, et al. Later chronotype is associated with unhealthful plant-based diet quality in young Japanese women. Appetite. (2021) 166:105468. doi: 10.1016/j.appet.2021.105468
44. Kim, H, Caulfield, LE, Garcia-Larsen, V, Steffen, LM, Coresh, J, and Rebholz, CM. Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. J Am Heart Assoc. (2019) 8:e012865. doi: 10.1161/JAHA.119.012865
45. Kim, H, Caulfield, LE, Garcia-Larsen, V, Steffen, LM, Grams, ME, Coresh, J, et al. Plant-based diets and incident chronic kidney disease and kidney function. Clin J Am Soc Nephrol. (2019) 14:682–91. doi: 10.2215/CJN.12391018
46. Kim, H, Caulfield, LE, and Rebholz, CM. Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J Nutr. (2018) 148:624–31. doi: 10.1093/jn/nxy019
47. Kim, H, Lee, K, Rebholz, CM, and Kim, J. Association between unhealthy plant-based diets and the metabolic syndrome in adult men and women: a population-based study in South Korea. Br J Nutr. (2021) 125:577–90. doi: 10.1017/S0007114520002895
48. Kim, H, Lee, K, Rebholz, CM, and Kim, J. Plant-based diets and incident metabolic syndrome: results from a south Korean prospective cohort study. PLoS Med. (2020) 17:e1003371. doi: 10.1371/journal.pmed.1003371
49. Kim, H, Rebholz, CM, Garcia-Larsen, V, Steffen, LM, Coresh, J, and Caulfield, LE. Operational differences in plant-based diet indices affect the ability to detect associations with incident hypertension in middle-aged US adults. J Nutr. (2020) 150:842–50. doi: 10.1093/jn/nxz275
50. Kim, J, Kim, H, and Giovannucci, EL. Plant-based diet quality and the risk of total and disease-specific mortality: a population-based prospective study. Clin Nutr. (2021) 40:5718–25. doi: 10.1016/j.clnu.2021.10.013
51. Kim, J, Kim, H, and Giovannucci, EL. Quality of plant-based diets and risk of hypertension: a Korean genome and examination study. Eur J Nutr. (2021) 60:3841–51. doi: 10.1007/s00394-021-02559-3
52. Kim, J, Boushey, CJ, Wilkens, LR, Haiman, CA, Le Marchand, L, and Park, SY. Plant-based dietary patterns defined by a priori indices and colorectal cancer risk by sex and race/ethnicity: the multiethnic cohort study. BMC Med. (2022) 20:430. doi: 10.1186/s12916-022-02623-7
53. Kim, J, and Giovannucci, E. Healthful plant-based diet and incidence of type 2 diabetes in Asian population. Nutrients. (2022) 14:3078. doi: 10.3390/nu14153078
54. Kouvari, M, Tsiampalis, T, Chrysohoou, C, Georgousopoulou, E, Skoumas, J, Mantzoros, CS, et al. Quality of plant-based diets in relation to 10-year cardiovascular disease risk: the ATTICA cohort study. Eur J Nutr. (2022) 61:2639–49. doi: 10.1007/s00394-022-02831-0
55. Kouvari, M, Tsiampalis, T, Kosti, RI, Naumovski, N, Chrysohoou, C, Skoumas, J, et al. Quality of plant-based diets is associated with liver steatosis, which predicts type 2 diabetes incidence ten years later: results from the ATTICA prospective epidemiological study. Clin Nutr. (2022) 41:2094–102. doi: 10.1016/j.clnu.2022.07.026
56. Kuchakulla, M, Nackeeran, S, Blachman-Braun, R, and Ramasamy, R. The association between plant-based content in diet and testosterone levels in US adults. World J Urol. (2021) 39:1307–11. doi: 10.1007/s00345-020-03276-y
57. Laouali, N, Shah, S, MacDonald, CJ, Mahamat-Saleh, Y, El Fatouhi, D, Mancini, F, et al. BMI in the associations of plant-based diets with type 2 diabetes and hypertension risks in women: the E3N prospective cohort study. J Nutr. (2021) 151:2731–40. doi: 10.1093/jn/nxab158
58. Lee, K, Kim, H, Rebholz, CM, and Kim, J. Association between different types of plant-based diets and risk of dyslipidemia: a prospective cohort study. Nutrients. (2021) 13:220. doi: 10.3390/nu13010220
59. Li, H, Zeng, X, Wang, Y, Zhang, Z, Zhang, Z, Zhu, Y, et al. A prospective study of healthful and unhealthful plant-based diet and risk of overall and cause-specific mortality. Eur J Nutr. (2022) 61:387–98. doi: 10.1007/s00394-021-02660-7
60. Li, X, Peng, Z, Li, M, Zeng, X, Li, H, Zhu, Y, et al. A healthful plant-based diet is associated with lower odds of nonalcoholic fatty liver disease. Nutrients. (2022) 14:4099. doi: 10.3390/nu14194099
61. Liang, F, Fu, J, Turner-McGrievy, G, Wang, Y, Qiu, N, Ding, K, et al. Association of body mass index and plant-based diet with cognitive impairment among older Chinese adults: a prospective, nationwide cohort study. Nutrients. (2022) 14:3132. doi: 10.3390/nu14153132
62. Lim, SX, Loy, SL, Colega, MT, Lai, JS, Godfrey, KM, Lee, YS, et al. Prepregnancy adherence to plant-based diet indices and exploratory dietary patterns in relation to fecundability. Am J Clin Nutr. (2022) 115:559–69. doi: 10.1093/ajcn/nqab344
63. Liu, X, Dhana, K, Barnes, LL, Tangney, CC, Agarwal, P, Aggarwal, N, et al. A healthy plant-based diet was associated with slower cognitive decline in African American older adults: a biracial community-based cohort. Am J Clin Nutr. (2022) 116:875–86. doi: 10.1093/ajcn/nqac204
64. Loeb, S, Fu, BC, Bauer, SR, Pernar, CH, Pernar, CH, Chan, JM, et al. Association of plant-based diet index with prostate cancer risk. Am J Clin Nutr. (2022) 115:662–70. doi: 10.1093/ajcn/nqab365
65. Lotfi, M, Nouri, M, Turki Jalil, A, Rezaianzadeh, A, Babajafari, S, Ghoddusi Johari, M, et al. Plant-based diets could ameliorate the risk factors of cardiovascular diseases in adults with chronic diseases. Food Sci Nutr. (2022) 11:1297–308. doi: 10.1002/fsn3.3164
66. Lu, Y, Kang, J, Li, Z, Wang, X, Liu, K, Zhou, K, et al. The association between plant-based diet and erectile dysfunction in Chinese men. Basic Clin Androl. (2021) 31:11. doi: 10.1186/s12610-021-00129-5
67. Lu, Y, Tian, J, Wang, S, Wang, X, Song, Y, Liu, K, et al. The association between plant-based diet and erectile function in Chinese young healthy men: a population-based study. Andrologia. (2021) 53:e14038. doi: 10.1111/and.14038
68. Maroto-Rodriguez, J, Delgado-Velandia, M, Ortolá, R, Carballo-Casla, A, García-Esquinas, E, Rodríguez-Artalejo, F, et al. Plant-based diets and risk of frailty in community-dwelling older adults: the seniors-ENRICA-1 cohort. Geroscience. (2023) 45:221–32. doi: 10.1007/s11357-022-00614-3
69. Mazidi, M, and Kengne, AP. Higher adherence to plant-based diets are associated with lower likelihood of fatty liver. Clin Nutr. (2019) 38:1672–7. doi: 10.1016/j.clnu.2018.08.010
70. McFarlane, C, Krishnasamy, R, Stanton, T, Savill, E, Snelson, M, Mihala, G, et al. Diet quality and protein-bound uraemic toxins: investigation of novel risk factors and the role of microbiome in chronic kidney disease. J Ren Nutr. (2021) 21:S1051–2276. doi: 10.1053/j.jrn.2021.10.003
71. Merino, J, Joshi, AD, Nguyen, LH, Leeming, ER, Mazidi, M, Drew, DA, et al. Diet quality and risk and severity of COVID-19: a prospective cohort study. Gu. (2021) 70:2096–104. doi: 10.1136/gutjnl-2021-325353
72. Mokhtari, E, Mirzaei, S, Asadi, A, Akhlaghi, M, and Saneei, P. Association between plant-based diets and metabolic health status in adolescents with overweight and obesity. Sci Rep. (2022) 12:13772. doi: 10.1038/s41598-022-17969-4
73. Mousavi, SM, Ebrahimi-Mousavi, S, Hassanzadeh Keshteli, A, Afshar, H, Esmaillzadeh, A, and Adibi, P. The association of plant-based dietary patterns and psychological disorders among Iranian adults. J Affect Disord. (2022) 300:314–21. doi: 10.1016/j.jad.2022.01.028
74. Mousavi, SM, Shayanfar, M, Rigi, S, Mohammad-Shirazi, M, Sharifi, G, and Esmaillzadeh, A. Adherence to plant-based dietary patterns in relation to glioma: a case-control study. Sci Rep. (2021) 11:21819. doi: 10.1038/s41598-021-01212-7
75. Mouzannar, A, Kuchakulla, M, Blachman-Braun, R, Nackeeran, S, Becerra, M, Nahar, B, et al. Impact of plant-based diet on PSA level: data from the National Health and nutrition examination survey. Urology. (2021) 156:205–10. doi: 10.1016/j.urology.2021.05.086
76. Musicus, AA, Wang, DD, Janiszewski, M, Eshel, G, Blondin, SA, Willett, W, et al. Health and environmental impacts of plant-rich dietary patterns: a US prospective cohort study. Lancet Planet Health. (2022) 6:e892–900. doi: 10.1016/S2542-5196(22)00243-1
77. Nouri, M, Abdollahi, N, Leilami, K, and Shirani, M. The relationship between plant-based diet index and semen parameters of men with infertility: a cross-sectional study. Int J Fertil Steril. (2022) 16:310–9. doi: 10.22074/ijfs.2021.538675.1184
78. Oncina-Cánovas, A, Vioque, J, González-Palacios, S, Salas-Salvadó, J, Corella, D, Zomeño, D, et al. Pro-vegetarian food patterns and cardiometabolic risk in the PREDIMED-plus study: a cross-sectional baseline analysis. Eur J Nutr. (2022) 61:357–72. doi: 10.1007/s00394-021-02647-4
79. Oncina-Cánovas, A, González-Palacios, S, Notario-Barandiaran, L, Torres-Collado, L, Signes-Pastor, A, De-Madaria, E, et al. Adherence to pro-vegetarian food patterns and risk of oesophagus, stomach, and pancreas cancers: a multi case-control study (the PANESOES study). Nutrients. (2022) 14:5288. doi: 10.3390/nu14245288
80. Payandeh, N, Shahinfar, H, Amini, MR, Jafari, A, Safabakhsh, M, Imani, H, et al. The lack of association between plant-based dietary pattern and breast cancer: a hospital-based case-control study. Clin Nutr Res. (2021) 10:115–26. doi: 10.7762/cnr.2021.10.2.115
81. Pourreza, S, Khademi, Z, Mirzababaei, A, Yekaninejad, MS, Sadeghniiat-Haghighi, K, Naghshi, S, et al. Association of plant-based diet index with inflammatory markers and sleep quality in overweight and obese female adults: a cross-sectional study. Int J Clin Pract. (2021) 75:e14429. doi: 10.1111/ijcp.14429
82. Ratjen, I, Enderle, J, Burmeister, G, Koch, M, Nöthlings, U, Hampe, J, et al. Post-diagnostic reliance on plant-compared with animal-based foods and all-cause mortality in omnivorous long-term colorectal cancer survivors. Am J Clin Nutr. (2021) 114:441–9. doi: 10.1093/ajcn/nqab061
83. Ratjen, I, Morze, J, Enderle, J, Both, M, Borggrefe, J, Müller, HP, et al. Adherence to a plant-based diet in relation to adipose tissue volumes and liver fat content. Am J Clin Nutr. (2020) 112:354–63. doi: 10.1093/ajcn/nqaa119
84. Rigi, S, Mousavi, SM, Benisi-Kohansal, S, Azadbakht, L, and Esmaillzadeh, A. The association between plant-based dietary patterns and risk of breast cancer: a case-control study. Sci Rep. (2021) 11:3391. doi: 10.1038/s41598-021-82659-6
85. Romanos-Nanclares, A, Willett, WC, Rosner, BA, Collins, LC, Hu, FB, Toledo, E, et al. Healthful and unhealthful plant-based diets and risk of breast cancer in U.S. women: results from the Nurses' health studies. Cancer Epidemiol Biomark Prev. (2021) 30:1921–31. doi: 10.1158/1055-9965.EPI-21-0352
86. Sasanfar, B, Toorang, F, Booyani, Z, Vassalami, F, Mohebbi, E, Azadbakht, L, et al. Adherence to plant-based dietary pattern and risk of breast cancer among Iranian women. Eur J Clin Nutr. (2021) 75:1578–87. doi: 10.1038/s41430-021-00869-7
87. Satija, A, Bhupathiraju, SN, Spiegelman, D, Chiuve, SE, Manson, JE, Willett, W, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. (2017) 70:411–22. doi: 10.1016/j.jacc.2017.05.047
88. Shahavandi, M, Djafari, F, Shahinfar, H, Davarzani, S, Babaei, N, Ebaditabar, M, et al. The association of plant-based dietary patterns with visceral adiposity, lipid accumulation product, and triglyceride-glucose index in Iranian adults. Complement Ther Med. (2020) 53:102531. doi: 10.1016/j.ctim.2020.102531
89. Shahinfar, H, Amini, MR, Payandeh, N, Naghshi, S, Sheikhhossein, F, Djafarian, K, et al. The link between plant-based diet indices with biochemical markers of bone turn over, inflammation, and insulin in Iranian older adults. Food Sci Nutr. (2021) 9:3000–14. doi: 10.1002/fsn3.2258
90. Shin, N, and Kim, J. Association between different types of plant-based diet and dyslipidaemia in Korean adults. Br J Nutr. (2022) 128:542–8. doi: 10.1017/S0007114521003482
91. Shirzadi, Z, Daneshzad, E, Dorosty, A, Surkan, PJ, and Azadbakht, L. Associations of plant-based dietary patterns with cardiovascular risk factors in women. J Cardiovasc Thorac Res. (2022) 14:1–10. doi: 10.34172/jcvtr.2022.01
92. Song, S, Lee, K, Park, S, Shin, N, Kim, H, and Kim, J. Association between unhealthful plant-based diets and possible risk of dyslipidemia. Nutrients. (2021) 13:4334. doi: 10.3390/nu13124334
93. Sotos-Prieto, M, Struijk, EA, Fung, TT, Rodríguez-Artalejo, F, Willett, WC, Hu, FB, et al. Association between the quality of plant-based diets and risk of frailty. J Cachexia Sarcopenia Muscle. (2022) 13:2854–62. doi: 10.1002/jcsm.13077
94. Stanford, J, Charlton, K, Stefoska-Needham, A, Zheng, H, Bird, L, Borst, A, et al. Associations among plant-based diet quality, uremic toxins, and gut microbiota profile in adults undergoing hemodialysis therapy. J Ren Nutr. (2021) 31:177–88. doi: 10.1053/j.jrn.2020.07.008
95. Wang, DD, Li, Y, Nguyen, XT, Ho, YL, Hu, FB, Willett, WC, et al. Degree of adherence to based diet and total and cause-specific mortality: prospective cohort study in the million veteran program. Public Health Nutr. (2022):1–38. doi: 10.1017/S1368980022001653
96. Wang, F, Baden, MY, Guasch-Ferré, M, Wittenbecher, C, Li, J, Li, Y, et al. Plasma metabolite profiles related to plant-based diets and the risk of type 2 diabetes. Diabetologia. (2022) 65:1119–32. doi: 10.1007/s00125-022-05692-8
97. Wang, F, Ugai, T, Haruki, K, Wan, Y, Akimoto, N, Arima, K, et al. Healthy and unhealthy plant-based diets in relation to the incidence of colorectal cancer overall and by molecular subtypes. Clin Transl Med. (2022) 12:e893. doi: 10.1002/ctm2.893
98. Wang, YB, Shivappa, N, Hébert, JR, Page, AJ, Gill, TK, and Melaku, YA. Association between dietary inflammatory index, dietary patterns, plant-based dietary index and the risk of obesity. Nutrients. (2021) 13:1536. doi: 10.3390/nu13051536
99. Waterplas, J, Versele, V, D'Hondt, E, Lefevre, J, Mertens, E, Charlier, R, et al. A 10-year longitudinal study on the associations between changes in plant-based diet indices, anthropometric parameters and blood lipids in a Flemish adult population. Nutr Diet. (2020) 77:196–203. doi: 10.1111/1747-0080.12578
100. Weber, KS, Ratjen, I, Enderle, J, Seidel, U, Rimbach, G, and Lieb, W. Plasma boron concentrations in the general population: a cross-sectional analysis of cardio-metabolic and dietary correlates. Eur J Nutr. (2022) 61:1363–75. doi: 10.1007/s00394-021-02730-w
101. Weston, LJ, Kim, H, Talegawkar, SA, Tucker, KL, Correa, A, and Rebholz, CM. Plant-based diets and incident cardiovascular disease and all-cause mortality in African Americans: a cohort study. PLoS Med. (2022) 19:e1003863. doi: 10.1371/journal.pmed.1003863
102. Wu, B, Zhou, RL, Ou, QJ, Chen, YM, Fang, YJ, and Zhang, CX. Association of plant-based dietary patterns with the risk of colorectal cancer: a large-scale case-control study. Food Funct. (2022) 13:10790–801. doi: 10.1039/D2FO01745H
103. Wu, J, Song, X, Chen, G-C, Neelakantan, N, van Dam, RM, Feng, L, et al. Dietary pattern in midlife and cognitive impairment in late life: a prospective study in Chinese adults. Am J Clin Nutr. (2019) 110:912–20. doi: 10.1093/ajcn/nqz150
104. Yang, H, Breyer, BN, Rimm, EB, Giovannucci, E, Loeb, S, Kenfield, SA, et al. Plant-based diet index and erectile dysfunction in the health professionals follow-up study. BJU Int. (2022) 130:514–21. doi: 10.1111/bju.15765
105. Zamani, B, Daneshzad, E, Siassi, F, Guilani, B, Bellissimo, N, and Azadbakht, L. Association of plant-based dietary patterns with psychological profile and obesity in Iranian women. Clin Nutr. (2020) 39:1799–808. doi: 10.1016/j.clnu.2019.07.019
106. Zamani, B, Milajerdi, A, Tehrani, H, Bellissimo, N, Brett, NR, and Azadbakht, L. Association of a plant-based dietary pattern in relation to gestational diabetes mellitus. Nutr Diet. (2019) 76:589–96. doi: 10.1111/1747-0080.12512
107. Zhu, A, Yuan, C, Pretty, J, and Ji, JS. Plant-based dietary patterns and cognitive function: a prospective cohort analysis of elderly individuals in China (2008-2018). Brain Behav. (2022) 12:e2670. doi: 10.1002/brb3.2670
108. Zhou, Y-F, Song, X-Y, Wu, J, Chen, GC, Neelakantan, N, van Dam, RM, et al. Association between dietary patterns in midlife and healthy ageing in Chinese adults: the Singapore Chinese health study. J Am Med Dir Assoc. (2021) 22:1279–86. doi: 10.1016/j.jamda.2020.09.045
109. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
110. Mozaffarian, D, El-Abbadi, NH, O’Hearn, M, Erndt-Marino, J, Masters, WA, Jacques, P, et al. Food compass is a nutrient profiling system using expanded characteristics for assessing healthfulness of foods. Nat Food. (2021) 2:809–18. doi: 10.1038/s43016-021-00381-y
111. O’Hearn, M, Erndt-Marino, J, Gerber, S, Lauren, BN, Economos, C, Wong, JB, et al. Validation of food compass with a healthy diet, cardiometabolic health, and mortality among U.S. adults, 1999-2018. Nat Commun. (2022) 13:7066. doi: 10.1038/s41467-022-34195-8
112. Muraki, I, Rimm, EB, Willett, WC, Manson, JE, Hu, FB, and Sun, Q. Potato consumption and risk of type 2 diabetes: results from three prospective cohort studies. Diabetes Care. (2016) 39:376–84. doi: 10.2337/dc15-0547
113. Borgi, L, Rimm, EB, Willett, WC, and Forman, JP. Potato intake and incidence of hypertension: results from three prospective US cohort studies. BMJ. (2016) 353:i2351. doi: 10.1136/bmj.i2351
114. Zhang, Y, You, D, Lu, N, Duan, D, Feng, X, Astell-Burt, T, et al. Potatoes consumption and risk of type 2 diabetes: a meta-analysis. Iran J Public Health. (2018) 47:1627–35.
115. Hashemian, M, Murphy, G, Etemadi, A, Liao, LM, Dawsey, SM, Malekzadeh, R, et al. Potato consumption and the risk of overall and cause specific mortality in the NIH-AARP study. PLoS One. (2019) 14:e0216348. doi: 10.1371/journal.pone.0216348
116. Borch, D, Juul-Hindsgaul, N, Veller, M, Astrup, A, Jaskolowski, J, and Raben, A. Potatoes and risk of obesity, type 2 diabetes, and cardiovascular disease in apparently healthy adults: a systematic review of clinical intervention and observational studies. Am J Clin Nutr. (2016) 104:489–98. doi: 10.3945/ajcn.116.132332
117. Tran, E, Dale, HF, Jensen, C, and Lied, GA. Effects of plant-based diets on weight status: a systematic review. Diabetes Metab Syndr Obes. (2020) 13:3433–48. doi: 10.2147/DMSO.S272802
118. Qian, F, Liu, G, Hu, FB, Bhupathiraju, SN, and Sun, Q. Association between plant-based dietary patterns and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA Intern Med. (2019) 179:1335–44. doi: 10.1001/jamainternmed.2019.2195
119. Wu, J, Zeng, R, Huang, J, Li, X, Zhang, J, Ho, JC, et al. Dietary protein sources and incidence of breast cancer: a dose-response meta-analysis of prospective studies. Nutrients. (2016) 8:730. doi: 10.3390/nu8110730
120. Schwingshackl, L, Schwedhelm, C, Hoffmann, G, Lampousi, AM, Knüppel, S, Iqbal, K, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. (2017) 105:1462–73. doi: 10.3945/ajcn.117.153148
121. Kwok, CS, Saadia, U, Myint, PK, Mamas, MA, and Loke, YK. Vegetarian diet, seventh day Adventists and risk of cardiovascular mortality: a systematic review and meta-analysis. Int J Cardiol. (2014) 176:680–6. doi: 10.1016/j.ijcard.2014.07.080
122. Aleksandrova, K, Koelman, L, and Rodrigues, CE. Dietary patterns and biomarkers of oxidative stress and inflammation: a systematic review of observational and intervention studies. Redox Biol. (2021) 42:101869. doi: 10.1016/j.redox.2021.101869
123. Gibbs, J, Gaskin, E, Ji, C, Miller, MA, and Cappuccio, FP. The effect of plant-based dietary patterns on blood pressure: a systematic review and meta-analysis of controlled intervention trials. J Hypertens. (2021) 39:23–37. doi: 10.1097/HJH.0000000000002604
124. Guasch-Ferré, M, Satija, A, Blondin, SA, Janiszewski, M, Emlen, E, O'Connor, LE, et al. Meta-analysis of randomized controlled trials of red meat consumption in comparison with various comparison diets on cardiovascular risk factors. Circulation. (2019) 139:1828–45. doi: 10.1161/CIRCULATIONAHA.118.035225
125. Lu, W, Chen, H, Niu, Y, Wu, H, Xia, D, and Wu, Y. Dairy products intake and cancer mortality risk: a meta-analysis of 11 population-based cohort studies. Nutr J. (2016) 15:91. doi: 10.1186/s12937-016-0210-9
126. Guo, J, Astrup, A, Lovegrove, JA, Gijsbers, L, Givens, DI, and Soedamah-Muthu, SS. Milk and dairy consumption and risk of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol. (2017) 32:269–87. doi: 10.1007/s10654-017-0243-1
127. Lee, J, Fu, Z, Chung, M, Jang, DJ, and Lee, HJ. Role of milk and dairy intake in cognitive function in older adults: a systematic review and meta-analysis. Nutr J. (2018) 17:82. doi: 10.1186/s12937-018-0387-1
Keywords: vegan, vegetarian, plant-based diet, food frequency questionnaire, plant-based dietary index, diet quality, health outcomes, food as medicine
Citation: Rosenfeld RM, Juszczak HM and Wong MA (2023) Scoping review of the association of plant-based diet quality with health outcomes. Front. Nutr. 10:1211535. doi: 10.3389/fnut.2023.1211535
Received: 28 April 2023; Accepted: 28 July 2023;
Published: 10 August 2023.
Edited by:
Andrea K. Boggild, University of Toronto, CanadaReviewed by:
Katharina Christina Wirnitzer, Pedagogical University Tyrol, AustriaCopyright © 2023 Rosenfeld, Juszczak and Wong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Richard M. Rosenfeld, cmljaHJvc2VuZmVsZEBtc24uY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.