- 1Baby Health Behavior Lab, Division of Health Services and Outcomes Research, Children’s Mercy Hospital, Kansas City, MO, United States
- 2Department of Psychology, University of Kansas, Lawrence, KS, United States
- 3Cofrin Logan Center for Addiction Research and Treatment, University of Kansas, Lawrence, KS, United States
- 4Biostatistics and Epidemiology Core, Division of Health Services and Outcomes Research, Children’s Mercy Hospital, Kansas City, MO, United States
- 5Department of Pediatrics, University of Missouri-Kansas City, Kansas City, MO, United States
- 6Division of Behavioral Medicine, Department of Pediatrics, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY, United States
- 7FeedMore WNY, Buffalo, NY, United States
- 8Center for Children’s Healthy Lifestyles and Nutrition, University of Kansas Medical Center, Kansas City, KS, United States
Background: Research has shown that early exposure to added sugars from table food is related to increased intake of added sugars in later childhood. The earliest window of exposure to added sugars may be in infancy via infant formula. However, beyond the well-established factors of maternal lifestyle and modeling, there is a lack of research examining how exposure to added sugars from infant formula influences infant/toddler added sugar intakes from table foods and sugar sweetened beverages (SSB).
Objective: While accounting factors previously associated with infant/toddler added sugar intakes and maternal SSB consumption (proximal measure of maternal modeling), this study aims to examine if there is an association between added sugars in infant formula and added sugar intakes from table foods and SSB during the complementary feeding period.
Methods: This is a secondary, cross-sectional analysis using three-day caregiver-reported 24-h dietary recalls in a cohort of infant/toddlers (n = 95), ages 9- < 16 mos., enrolled in a music intervention trial. Hierarchical stepwise regression was used to estimate the association between exposure to added sugars from infant formula and (1) intake of added sugars from table food and (2) SSB consumption. Infant/toddler SSB consumption was transformed to account for distributional properties. We performed incremental F-tests to determine whether the addition of each step improved model fit (R2).
Results: Early exposure to added sugars via infant formula was associated with infant/toddler SSB (ΔR2 = 0.044, Finc (1, 87) =6.009, p = 0.016) beyond sociodemographic and maternal SSB consumption, but not with infant/toddler added sugar intakes from table foods (ΔR2 = 0.02, Finc (1, 87) =3.308, p = 0.072).
Conclusion: While past studies have identified circumstantial (i.e., sociodemographic), or indirect (i.e., maternal lifestyle and modeling), mechanisms contributing to higher infant/toddler added sugar intakes, this study identifies exposure to added sugars from infant formula as a possible direct mechanism explaining why some infants/toddlers consume more added sugars.
1. Introduction
Despite recent preventative efforts, childhood obesity remains a prevalent health concern for children in the United States. Among the dietary factors related to childhood obesity risk, added sugars have emerged as a leading factor that contributes to the development of childhood obesity (1, 2). As a result, the Dietary Guidelines for Americans (3) and the American Heart Association (4) recommend that children under the age of 2 years avoid added sugars. Alongside obesity (1, 2), the intake of added sugars during infancy and toddlerhood has been associated with early rapid weight gain (5), dental caries (6), asthma (7), cardiovascular disease (4), elevated blood pressure (8), and elevated triglycerides (8).
One well-established factor associated with added sugar intakes is maternal lifestyle and behavioral modeling in relation to dietary intake. Several studies have demonstrated the association of maternal diet on children’s dietary preference. For instance, Scaglioni et al. reported that parental food habits are suggested to influence child food choices (9). Vepsäläinen et al. (10) found that a child’s diet most closely resembles the diet of whomever provides the food to the child, and that is typically the mother (11). Ha et al. (11) and Brekke et al. (12) specifically investigated child added sugar intakes in relation to maternal dietary habits, and they found that low fruit intake and the consumption of sweets during pregnancy was associated with child added sugar intakes. Furthermore, the study of Australian mother-infant dyads, conducted by Ha et al. reported that infants with mothers who consume sugar sweetened beverages (SSB) are 1.8 times more likely to consume added sugars in comparison to children whose mothers did not consume SSB (11). Our team’s recent publication further concurred the findings of Ha et al. supporting that maternal SSB intake is significantly associated with infant/toddler added sugar intakes (13).
Despite a substantial amount of literature relating maternal lifestyle and dietary modeling to infant/toddler added sugar intakes, this factor does not explain the direct mechanism leading to the high added sugar intakes. One possible understudied mechanism affecting infant/toddler added sugar intakes may be early exposure to added sugars via early feeding practices (i.e., infant formula feeding, breastfeeding, or mixture of the two) (14). Research has shown that early exposure to added sugars from table food is related to increased intake of added sugars in later childhood (15); however, this may not be the earliest exposure window to added sugars for most infants. The first nutrient source infants are exposed to is milk, either in the form of breastmilk or infant formula. Although the nutrient profile of infant formula is advertised to be similar to breastmilk, our recent research identified that there are substantial differences between the two sources (14, 16). Our study revealed that most infant formulas produced in the US contain added sugars up to 7.7 g/100 kcal serving (14, 16). As such, when formula is consumed exclusively, infants may yield a daily consumption of added sugars equivalent to two soft drinks (14, 16). Thus, exposure to added sugars through infant formula may be extensive in the first year of life, and particularly during the first 6 months.
Recently, our team proposed an application of the exposure-learning paradigm in order to explain how early exposure to added sugars via infant formula may lead to a greater preference for sweet tastes and therefore the consumption of more added sugars (14). Furthermore, the sugars (e.g., glucose and corn syrup) commonly found in infant formula are known to provoke a sense of pleasure. These sugars stimulate the brain’s reward system into releasing a greater amount of dopamine, reenforcing the consumption of added sugars (14). Research has shown that consumption of toddler formula, which typically contains high amounts of added sugars [10.5 g/8 fl. oz. serving calculated using Nutrition Data System for Research (NDSR)], is correlated to increased added sugar intakes later in childhood (17, 18). However, there are no studies to our knowledge that have examined the consumption of infant formula at the earliest possible window, which is during infancy. In this study, we examined whether exposure to added sugar in infant formula explains the variance in US infant/toddler consuming formula manufactured in the US (1) added sugar intakes from table foods (i.e., all other dietary sources outside of infant formula) and (2) SSB consumption at 9- < 16 mos., beyond the well-established factors such as sociodemographic and maternal lifestyles and dietary modeling. We hypothesize that exposure to added sugars via infant formula during infancy is associated with infant/toddler added sugar intakes from table foods and SSB consumption at 9- < 16 mos. We hypothesize these results will remain present despite accounting for sociodemographic and maternal modeling behavior. In our analysis, maternal SSB consumption will serve as the proxy measure of maternal lifestyles and behavioral modeling per our previous work, Griebel-Thompson et al. (13) and the work of Ha et al. (11).
2. Materials and methods
2.1. Participants
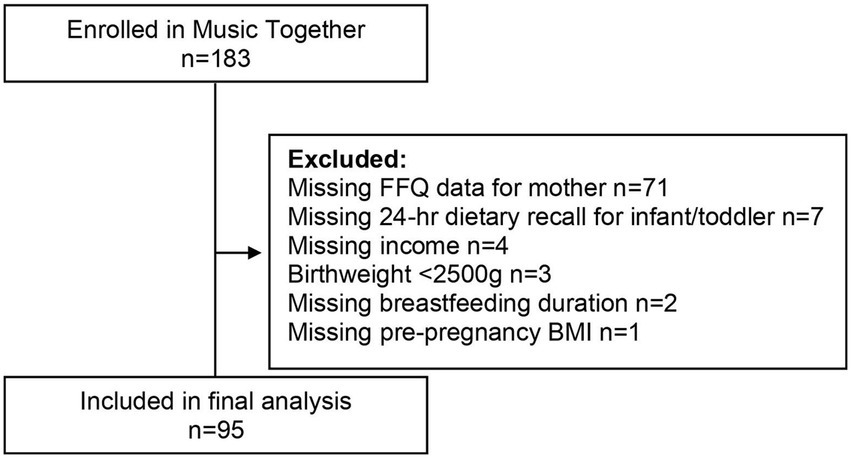
This cross-sectional analysis included baseline data from 95 mother-infant/toddler dyads, age 9- < 16 mos., (Figure 1) participating in a longitudinal randomized controlled trial (ClinicalTrials.gov Identifier: NCT02936284) (5). Trained study personnel obtained informed consent from parents of eligible participants. Participants were able to withdraw at any point of this study. Exclusion criteria included: infants born preterm (<37 weeks gestation), low-birth weight infants (<2,500 g), infants/toddlers with known medical problems, infants/toddlers consuming special diets, infants/toddlers with developmental delays or disabilities, maternal smoking, alcohol abuse, or controlled substance use during pregnancy, mother <18 years of age, high risk pregnancy (Gestational Diabetes Mellitus, pre-eclampsia, etc.), or multiple gestation (5). In accordance with the Institute of Medicine’s Food and Nutrition Board (19), two participants who consumed calories estimated to be ±2 SD from their estimated energy requirement were not included in the present analysis. The University at Buffalo Institutional Review Board (IRB) approved this study (protocol code STUDY00000472 and 5/24/2016).
2.2. Demographic and pregnancy history and feeding practices questionnaire
Researchers applied the shortened form of the feeding questionnaire from the Infant Feeding Practices Study II (20) in order to collect information for this study. The short form of the Infant Feeding Practices Study II uses 13 questions which assess areas of feeding practices including, but not limited to, the initiation and duration of breastfeeding, timing of solid food introduction, age of infant/toddler at cessation of breastfeeding, and maternal pregnancy history. The questionnaire was administered online using SurveyMonkey (https://www.surveymonkey.com, accessed on 24 May 2016).
2.3. Dietary intake
2.3.1. Maternal dietary intake
The application of the Block 2014 Food and Activity Questionnaire, developed by NutritionQuest (Berkley, CA, USA) (21), gathered information on maternal dietary intake. The Block 2014 is a full-length food frequency questionnaire (FFQ) comprised of 127 food and beverage items. It utilizes questions that specifically measure fat, carbohydrate, sugar, and whole grain intakes (21). The 2007–2008 and 2009–2010 NHANES cycles were used to design the Block 2014, while the USDA’s Food and Nutrient Database for Dietary Studies (FNDDS 5.0), Food Pyramid Equivalents Database (FPED), and Nutrient Database for Standard Reference (SR27) were used to create the nutrient and food group analysis database (21). This FFQ assesses SSB intake of sugary beverages including fruit juice, soda, and energy drinks (21). Respondents are provided with options to select from for frequency of intake including: (1) every day, (2) 5–6 times per week, (3) 3–4 times per week, (4) 2 times per week, (5) once per week, (6) 2–3 times per month, (7) once per month, (8) a few times per year, and (9) never.
2.3.2. Infant or toddler dietary intake
Infant/toddler dietary intake, including intake of added sugars from infant formula (i.e., sugars added above the level of naturally occurring lactose in the milk-base used in infant formula manufacturing and other added sugars, such as corn syrup solids or glucose), was assessed by three caregiver-reported 24-h dietary recalls. As conducted in the Feeding Infants and Toddlers Study (FITS), trained study personnel collected 24-h dietary recalls from parents/caregivers by phone on random occasions (two weekday, one weekend day) within 10 days of anthropometric measurement (22). We provided parents with handouts in order to ensure accurate reporting. These handouts contained tips on how to report serving sizes, along with answers to frequently asked questions (5). Furthermore, study personnel, trained by a registered dietitian (MS/RD), collected information from parents regarding infant/toddler feeding. If parents reported that the infant/toddler did not have a normal eating day within the past 24-h period, then the recall was administered on a different day (5, 22). These 24-h dietary recalls were derive from the USDA Automated Multiple-Pass Method (23). All study personnel used a script to administer 24-dietary recalls in order to ensure adherence to protocol. We did not include the intake of medicine or supplements in this analysis. Kong et al. described this methodology previously (5).
Information regarding breastfeeding was obtained based on parents’ records of both the duration at the breast and the intake of human milk (5, 22). Reports on nutritional intake from human milk follow the methodology described by the FITS study (22). Briefly, for exclusively breastfed infants ages 7–12 mos, 600 mL of human milk was reported (5, 22). For those consuming both human milk and infant formula, the amount of formula reported was subtracted from 600 mL, and the remainder was reported as human milk (5, 22). For toddlers ≥12 mos., 1 fl. oz. of human milk was reported for every 5 min at the breast (5, 22). We also collected detailed information on the brand of formula consumed including preparation methods and amounts consumed. Finally, SSB are any sugary beverages excluding milk and infant formula/human milk.
Infant dietary intake data, including infant formula brand and types, were collected and analyzed using NDSR software version 2019, which was developed by the Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN (24–26). Study personnel selected generic food in substitute of specific food that could not be found in the database. A total of 15 foods without a comparable generic food were not in the database. The NCC was contacted, and the foods were added to the database.
2.4. Statistical analysis
Participant demographic information is reported in either mean and standard deviation or sample size and percentage. Infant/toddler SSB consumption was log transformed to account for distributional properties. Hierarchal stepwise regression estimated whether added sugar intakes from formula (kcal) at 9- < 16 mos. Was associated with infant/toddler added sugar intakes from table foods (kcal) or SSB at 9- < 16 mos., beyond established predictors related to material dietary modeling. In model 1, we controlled for demographic characteristics reported to be associated with infant/toddler added sugar intakes. These include infant/toddler sex, infant/toddler age (mos.), birthweight (kg), parity, maternal body mass index (BMI) (kg/m2), maternal education (y), family income, first introduction of solid foods (mos.), and breastfeeding duration (mos.). In model 2, we controlled for our previously published (13) proxy of maternal modeling, maternal SSB consumption. In model 3, we included added sugars from infant formula (kcal). Incremental F-tests determined whether there was any occurrence of statistically significant change by comparing improvements in the model fit (R2). We also report the effect size of the F statistic which is a measure of the strength of relationship between two variables. The variance inflation factor (VIF) was calculated in all models, and multicollinearity was not observed. Statistical analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, NC, United States, 2020) (27).
3. Results
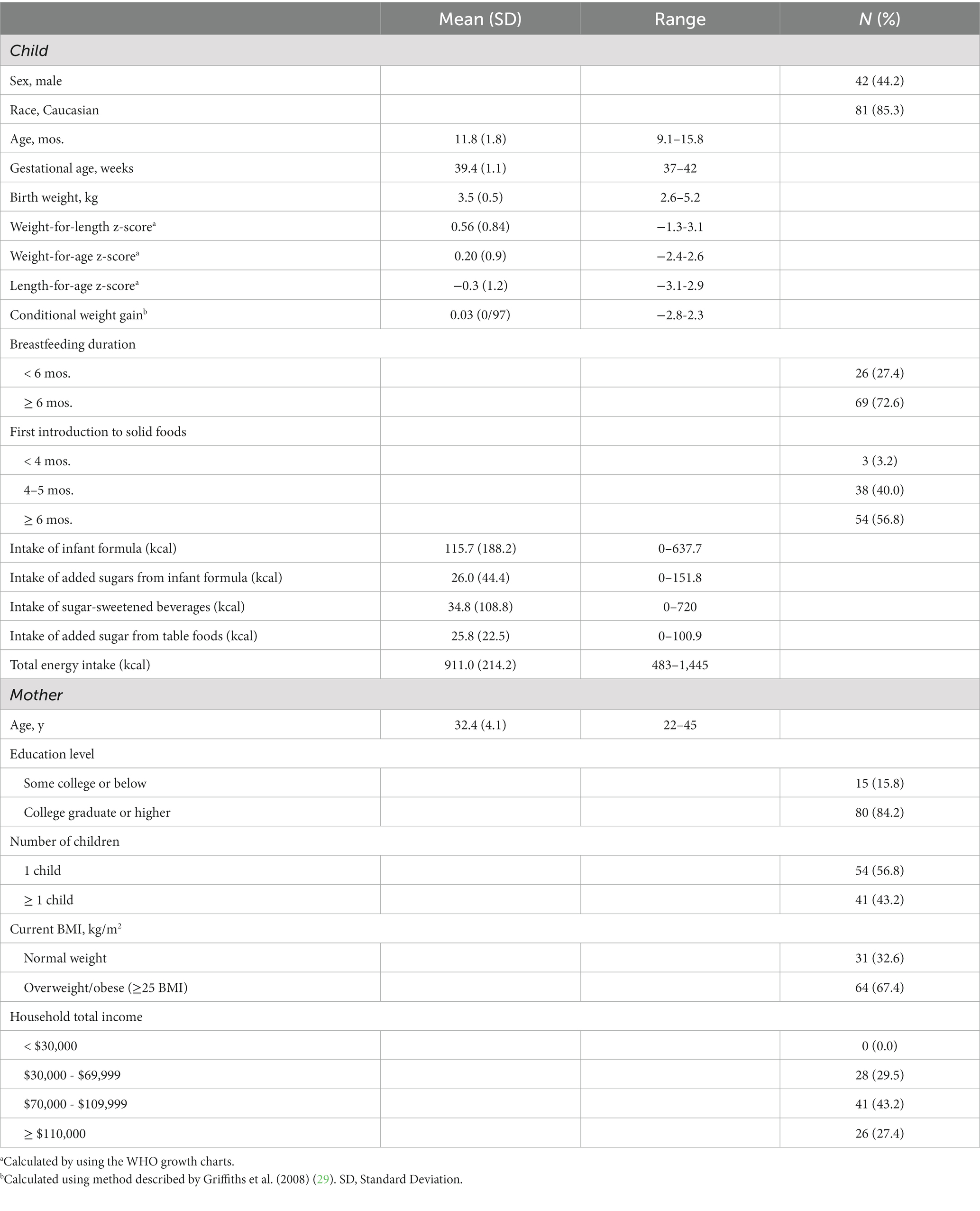
Table 1 presents demographic information of mothers and infants/toddlers. Table 2 shows the results of the hierarchical stepwise regression models depicting the association between exposure to added sugars via infant formula and the outcome of infant/toddler added sugar intakes from table foods. In step 1, 43.9% of variance was accounted for by demographic characteristics that were reported in prior literature to be associated with infant/toddler added sugar intakes. By adding maternal SSB intakes (a proxy maternal modeling) in step 2, the total variance increased to 45.4%. However maternal SSB intakes were not significantly associated with infant/toddler added sugar intakes from table foods (ΔR2 = 0.015, Finc (1, 88) = 2.418, p = 0.124). Model 3 accounts for exposure to added sugars via infant formula. The total variance increased to 47.4%, and early exposure of added sugars via infant formula was not significantly associated with infant/toddler added sugar intakes from table foods (ΔR2 = 0.02, Finc (1, 87) =3.308, p = 0.072).
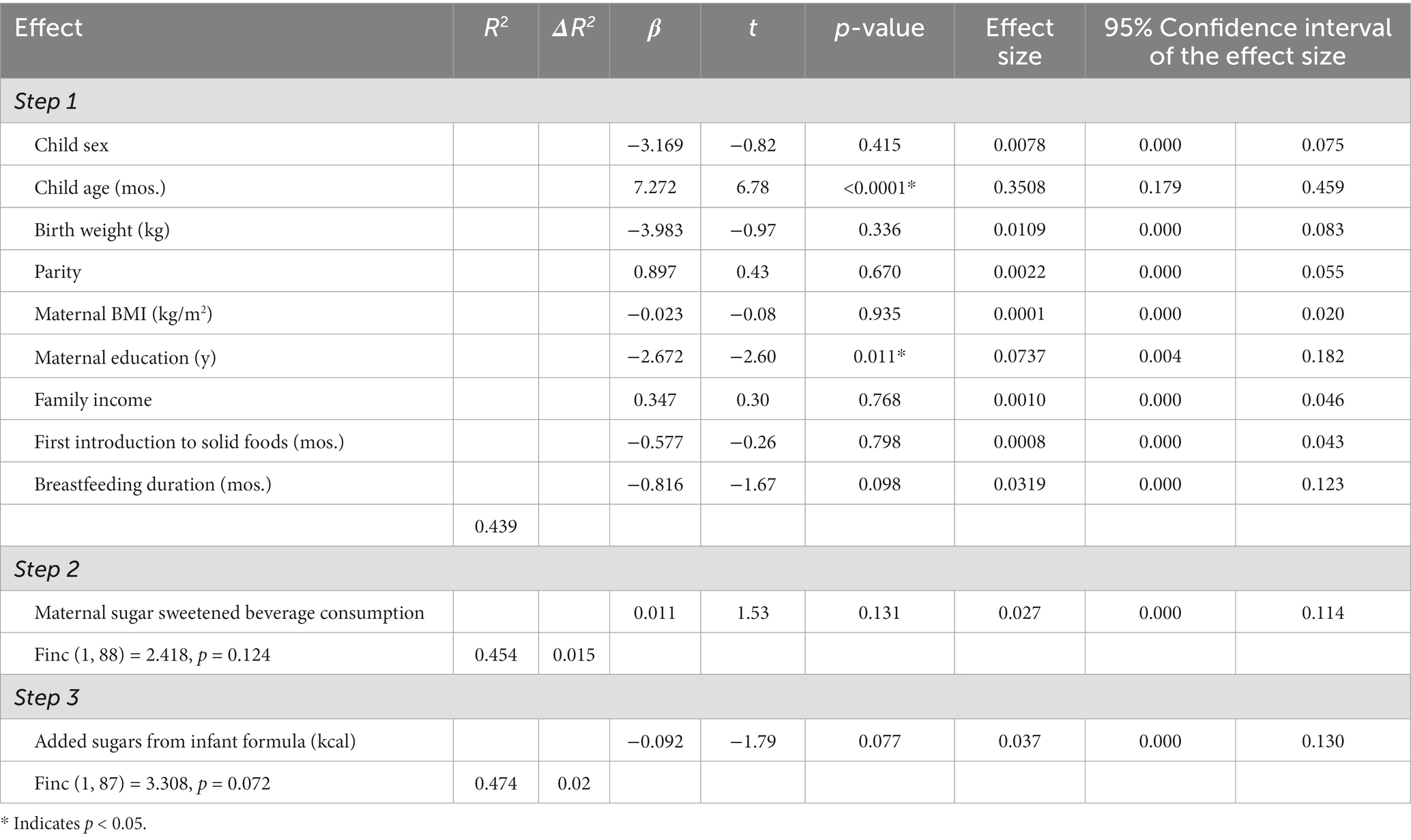
Table 2. Hierarchical regression models of added sugar intakes from formula [R2, change statistics (ΔR2), and regression coefficients (β)] predicting infant added sugar from table food intake (n = 95).
Table 3 displays the results of the hierarchical stepwise regression models regarding the association between exposure to added sugars via infant formula and infant/toddler SSB consumption as the outcome. Step 1, which controlled for demographic variables associated with infant/toddler added sugars intake, accounted for 31.3% of variance. The addition of maternal SSB consumption in step 2 increased the amount of variance accounted for to 31.9% (ΔR2 = 0.006, Finc (1, 88) = 0.775, p = 0.381). Maternal SSB consumption was, however, not significantly associated with infant SSB intake. Finally, the addition of exposure to added sugars via infant formula in step 3 accounted for 36.3% of the variance, and the exposure to added sugar via infant formula was significantly associated with infant/toddler SSB consumption (ΔR2 = 0.044, Finc (1, 87) =6.009, p = 0.016*).
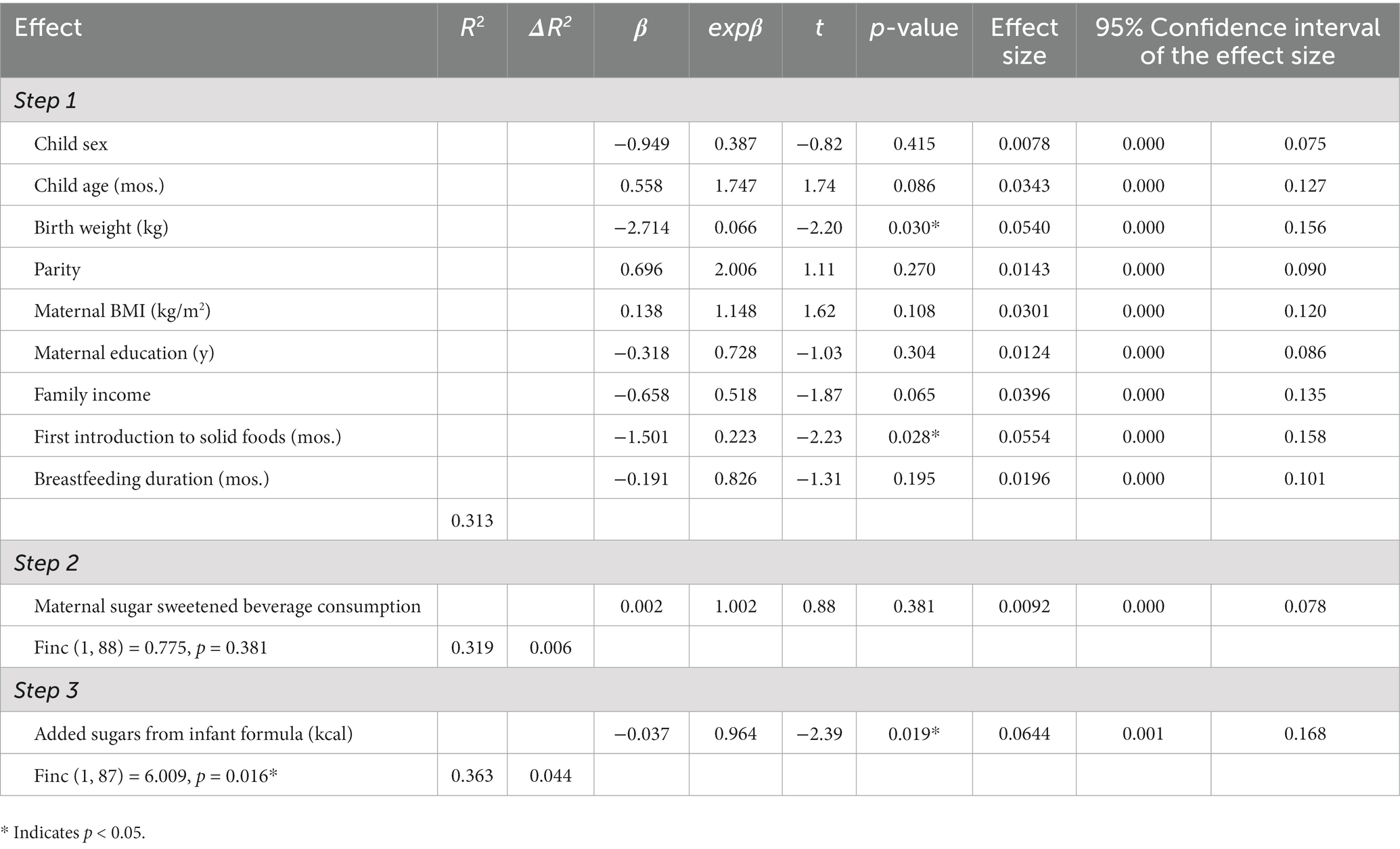
Table 3. Hierarchical regression models of added sugar intakes from formula [R2, change statistics (ΔR2), and regression coefficients (β)] predicting infant sugar sweetened beverage intake (n = 95).
4. Discussion
The intake of added sugars is emerging as a major contributing factor in the development of childhood obesity (1, 2, 13). The earliest possible exposure window to added sugars is via infant formula, but little research has investigated how consumption of infant formula may explain variance in infant added sugar intakes from table foods and SSB within the complementary feeding period. Informed by our recently presented paradigm for the etiology of obesity in early childhood (14), this study examined whether consumption of added sugars in infant formula may be a direct mechanism explaining high intake of added sugar from both table foods and SSB among infants/toddlers during the complementary feeding period. Notably, we examined whether the consumption of added sugars from infant formula explained variance in added sugar intake beyond the factors of sociodemographic and maternal lifestyle and dietary modeling.
Our findings suggest that exposure to added sugars from infant formula is associated with added sugar intakes from SSB of infants/toddlers 9- < 16 mos. of age. While studies investigating this association during infancy are limited, those that have examined it do concur with our findings. Redruello-Requejo et al. (17) studied a cohort of Spanish children and found that those who consumed adapted milks (i.e., toddler formula and enriched milks) in toddlerhood experienced an increase of added sugar intakes with age compared to their counterparts who did not consume adapted milks. Those who did not consume adapted milks experienced more stable levels of added sugar intakes with age. Kostecka et al. (18) studied children ages 13–24 mos. and found that children who drank toddler formula consumed more beverages with sugar including fruit juice, nectars, and sweetened hot beverages (18). While these studies support the premise of our paradigm, that exposure to added sugars from formula may result in an increased consumption of added sugars found in other sources, these studies do not focus on the earliest exposure window (i.e., infant formula during the first year of life). Furthermore, these studies did not consider other potential contributors in their analyses.
Interestingly, the association between early exposure to added sugars through infant formula and intake of added sugars from table foods was not significant in our cohort. While more studies in this area are needed to confirm our result, there are plausible explanations for this finding. First, our sample included infants/toddlers 9- < 16 mos of age who might be consuming little solid food outside of human milk or infant formula. Thus, added sugar intakes from tables foods might be insufficient to estimate its relationship with early exposure to added sugars from infant formula. In the future, a longitudinal study starting at birth may be warranted to pursue this line of work. Next, the fact that our population was rather homogeneous and consisted of highly educated, non-Hispanic/Latino White participants of high-income families may impact this finding. It is well-known that social and demographic factors influence not only the choice to feed infants human milk or infant formula, but also intake of added sugars (28, 30). Finally, it is possible that early exposure to added sugars through infant formula may have a greater influence on SSB intake compared to table food because infant formula is like a beverage, and the exposure learning may be specific to beverages in our present analyses.
In the present study, we recognize that infant/toddler added sugar intakes during the complementary feeding period is complex and multifactorial. Therefore, in our analyses, we first controlled for known or well-established factors such as sociodemographic variables (1, 28), age of introduction of solid foods (31), and lastly maternal SSB consumption (a proxy measure of maternal modeling) in a stepwise manner. To date, the existing literature has only identified circumstantial (i.e., sociodemographic factors) or indirect factors, such as maternal lifestyles and behavioral modeling, as contributors to infant added sugar intakes. Thus, our work may be significant in understanding potential drivers of unhealthful dietary habits. We posit that the consumption of added sugars in infant formula is a direct mechanism, as well as a form of early exposure to artificially reinforcing nutrient sources among children, as described in our recent publication (14). The early exposure to added sugars in infant formula teaches infants that food should be sweet, and this strengthens the inherent preference for sweet foods (e.g., foods high in added sugars) (32–34). This yields to the high intake of added sugars, suggesting it to be a direct mechanism. Furthermore, exposure learning is most influential when there has been no occurrence of prior exposure. This means that infancy may possibly be the most pivotal time for the development of food preference and eating behaviors, making infant formula the most pivotal food source (35, 36).
From a larger, societal perspective, the current food environment makes avoiding added sugars extremely difficult. Popkin et al. found 68% of barcoded foods available in US grocery stores contain added sugars (37). Nearly all the participants in this study consumed added sugars. This demonstrates how difficult it is to follow the recommendation by the Dietary Guidelines for Americans and the American Heart Association that children <2 years avoid added sugars (3, 4). Furthermore, marketing practices in the food industry are problematic. Marketing of infant formula to expecting, new mothers is predatory because not only does it undermine a woman’s right to choose how to feed and care for her infant, but it also undermines public health efforts to promote breastfeeding (38). Similarly, marketing of foods towards children is unethical because children are especially vulnerable to persuasive marketing tactics (39). This is a known contributor to childhood obesity (40). Future research and policy should address both individual and societal level factors in order to reduce the added sugar intakes of children.
A major strength of this study is the use of dietary recall methodology, consisting of three 24-h dietary recalls, which assessed infant intake. Additionally, to ensure accurate reporting, we used the USDA Automated Multiple-Pass Method to collect the 24-h dietary recalls and a registered dietitian (MS/RD) trained all study personnel on this protocol. Application of the hierarchical stepwise regression to statistical analysis strengthened this study. This theory driven technique allowed us to estimate how each step contributed to the overall model. A limitation, however, of this study is likely overestimation from maternal reports on infant/toddler dietary intake (41). It is also a limitation that parenting style (i.e., awareness and perception of the diet-health relationship) and the fact parents provide the food consumed by infants/toddlers 9- < 16 months of age were not accounted for. Lastly, this cohort is predominately white, highly educated, and includes mostly medium and high-income families making results less generalizable, especially to lower income families. Furthermore, the cohort social and demographic homogeneity may explain why previously described variables related to infant/toddler added sugars intake were not significant.
5. Conclusion
The current study suggests that early exposure to added sugars via infant formula may play a critical role in added sugar intakes during the complementary feeding period, even with the consideration of established sociodemographic and maternal dietary modeling variables.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The University at Buffalo Institutional Review Board (IRB). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Informed consent was also obtained from participants’ legal guardians/next of kin for their own participation in the study.
Author contributions
AG-T, EC, TF, RP, and KK conceptualized the work. KM collected the data. AG-T, RP, and EC analyzed the data. AG-T wrote the first draft with contributions from KK. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by National Institute on Child Health and Human Development of the National Institutes of Health Grant ID: R01 HD087082.
Acknowledgments
The authors would like to thank the participants of this study.
Conflict of interest
KM is employed by FeedMore WNY.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Herrick, KA , Fryar, CD , Hamner, HC , Park, S , and Ogden, CL . Added sugars intake among US infants and toddlers. J Acad Nutr Diet. (2020) 120:23–32. doi: 10.1016/j.jand.2019.09.007
2. Magriplis, E , Michas, G , Petridi, E , Chrousos, GP , Roma, E , Benetou, V, et al. Dietary sugar intake and its association with obesity in children and adolescents. Children. (2021) 8:676. doi: 10.3390/children8080676
3. U.S. Department of Agriculture and U.S. Department of Health and Human Services . Dietary guidelines for Americans, 2020–2025. 9th edition. December 2020. Available online: Dietary.Guidelines.gov (Accessed June 03, 2023).
4. Vos, MB , Kaar, JL , Welsh, JA , van Horn, L , Feig, DI , Anderson, CAM, et al. Added sugars and cardiovascular disease risk in children: a scientific statement from the American Heart Association. Circulation. (2017) 135:e1017–34. doi: 10.1161/CIR.0000000000000439
5. Kong, KL , Burgess, B , Morris, KS , Faith, MS , and Paluch, RA . High intake of added sugars is linked to rapid weight gain in infancy, breastfeeding ≥12 months may protect against this: a preliminary investigation. Pediatr Obes. (2021) 16:e12728. doi: 10.1111/ijpo.12728
6. Armfield, JM , Spencer, AJ , Roberts-Thomson, KF , and Plastow, K . Water fluoridation and the association of sugar-sweetened beverage consumption and dental caries in Australian children. Am J Public Health. (2013) 103:494–500. doi: 10.2105/AJPH.2012.300889
7. Park, S , Blanck, HM , Sherry, B , Jones, SE , and Pan, L . Regular-soda intake independent of weight status is associated with asthma among US high school students. J Acad Nutr Diet. (2013) 113:106–11. doi: 10.1016/j.jand.2012.09.020
8. Kell, KP , Cardel, MI , Bohan Brown, MM , and Fernández, JR . Added sugars in the diet are positively associated with diastolic blood pressure and triglycerides in children. Am J Clin Nutr. (2014) 100:46–52. doi: 10.3945/ajcn.113.076505
9. Scaglioni, S , De Cosmi, V , Ciappolino, V , Parazzini, F , Brambilla, P , and Agostoni, C . Factors influencing children’s eating behaviours. Nutrients. (2018) 10:706. doi: 10.3390/nu10060706
10. Vepsäläinen, H , Nevalainen, J , and Fogelholm, M . ike parent, like child? Dietary resemblance in families. Int J Behav Nutr Phys Act. (2018) 15:62. doi: 10.1186/s12966-018-0693-1
11. Ha, D , do, L , Spencer, A , Thomson, W , Golley, R , Rugg-Gunn, A, et al. Factors influencing early feeding of foods and drinks containing free sugars—a birth cohort study. Environ Res Public Health. (2017) 14:1270. doi: 10.3390/ijerph14101270
12. Brekke, HK , van Odijk, J , and Ludvigsson, J . Predictors and dietary consequences of frequent intake of high-sugar, low-nutrient foods in 1-year-old children participating in the ABIS study. Br J Nutr. (2007) 97:176–81. doi: 10.1017/S0007114507244460
13. Griebel-Thompson, AK , Murray, A , Morris, KS , Paluch, RA , Jacobson, L , and Kong, KL . The association between maternal sugar-sweetened beverage consumption and infant/toddler added sugar intakes. Nutrients. (2022) 14:4359. doi: 10.3390/nu14204359
14. Fazzino, TL , and Kong, KL . A new paradigm for investigating the etiology of obesity in early childhood: exposure to added sugars and hyper-palatable foods in infancy and dysregulation of food reinforcement processes. Obes Rev. (2023) 24:e13526. doi: 10.1111/obr.13526
15. Buckley, D , DeBoisblanc, B , Galliano, D , Wharton, F , and Dugas, A . Longitudinal study of sugar intake in infancy † 617. Pediatr Res. (1998) 43:108–8. doi: 10.1203/00006450-199804001-00638
16. Kong, KL , Burgess, B , Morris, KS , Re, T , Hull, HR , Sullivan, DK, et al. Association between added sugars from infant formulas and rapid weight gain in US infants and toddlers. J Nutr. (2021) 151:1572–80. doi: 10.1093/jn/nxab044
17. Redruello-Requejo, M , Samaniego-Vaesken, ML , Partearroyo, T , Rodríguez-Alonso, P , Soto-Méndez, MJ , Hernández-Ruiz, Á, et al. Dietary intake of individual (intrinsic and added) sugars and food sources from Spanish children aged one to <10 years—results from the EsNuPI study. Nutrients. (2022) 14:1667. doi: 10.3390/nu14081667
18. Kostecka, M , Jackowska, I , and Kostecka, J . A comparison of the effects of young-child formulas and cow’s milk on nutrient intakes in polish children aged 13–24 months. Nutrients. (2021) 13:2511. doi: 10.3390/nu13082511
19. Food and Nutrition Board . Dietary reference intakes for energy, carbohydrate, Fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). Washington, DC, USA: National Academy Press (2005).
20. Fein, SB , Labiner-Wolfe, J , Shealy, KR , Li, R , Chen, J , and Grummer-Strawn, LM . Infant feeding practices study II: study methods. Pediatrics. (2008) 122:S28–35. doi: 10.1542/peds.2008-1315c
21. Block, G . A review of validations of dietary assessment methods. Am J Epidemiol. (1982) 115:492–505. doi: 10.1093/oxfordjournals.aje.a113331
22. Anater, AS , Catellier, DJ , Levine, BA , Krotki, KP , Jacquier, EF , Eldridge, AL, et al. The feeding infants and toddlers study (FITS) 2016: study design and methods. J Nutr. (2018) 148:1516S–24S. doi: 10.1093/jn/nxy035
23. Raper, N , Perloff, B , Ingwersen, L , Steinfeldt, L , and Anand, J . An overview of USDA’s dietary intake data system. J Food Compos Anal. (2004) 17:545–55. doi: 10.1016/j.jfca.2004.02.013
24. Schakel, SF . Maintaining a nutrient database in a changing marketplace: keeping pace with changing food products—a research perspective. J Food Compos Anal. (2001) 14:315–22. doi: 10.1006/jfca.2001.0992
25. Schakel, SF , Sievert, YA , and Buzzard, IM . Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. (1988) 88:1268–71. doi: 10.1016/S0002-8223(21)07997-9
26. Schakel, SF , Buzzard, IM , and Gebhardt, SE . Procedures for estimating nutrient values for food composition databases. J Food Compos Anal. (1997) 10:102–14. doi: 10.1006/jfca.1997.0527
27. SAS Institute Inc . SAS/ACCESS® 9.4 Interface to ADABAS: Reference. Cary, NC: SAS Institute Inc. (2013).
28. Bably, MB , Paul, R , Laditka, SB , and Racine, EF . Factors associated with the initiation of added sugar among low-income young children participating in the special supplemental nutrition program for women, infants, and children in the US. Nutrients. (2021) 13:3888. doi: 10.3390/nu13113888
29. Griffiths, LJ , Smeeth, L , Hawkins, SS , Cole, TJ , and Dezateux, C . Effects of infant feeding practice on weight gain from birth to 3 years. Arch. Dis. Child. (2009) 94:577–582.
30. Standish, KR , and Parker, MG . Social determinants of breastfeeding in the United States. Clin Ther. (2022) 44:186–92. doi: 10.1016/j.clinthera.2021.11.010
31. Bournez, M , Ksiazek, E , Charles, MA , Lioret, S , Brindisi, MC , de Lauzon-Guillain, B, et al. Frequency of use of added sugar, salt, and fat in infant foods up to 10 months in the nationwide ELFE cohort study: associated infant feeding and caregiving practices. Nutrients. (2019) 11:733. doi: 10.3390/nu11040733
32. Mennella, JA , and Bobowski, NK . The sweetness and bitterness of childhood: insights from basic research on taste preferences. Physiol Behav. (2015) 152:502–7. doi: 10.1016/j.physbeh.2015.05.015
33. Beauchamp, GK , and Moran, M . Acceptance of sweet and salty tastes in 2-year-old children. Appetite. (1984) 5:291–305. doi: 10.1016/S0195-6663(84)80002-1
34. Pepino, MY . Factors contributing to individual differences in sucrose preference. Chem Senses. (2005) 30:i319–20. doi: 10.1093/chemse/bjh243
35. Birch, LL , and Doub, AE . Learning to eat: birth to age 2 y. Am J Clin Nutr. (2014) 99:723S–8S. doi: 10.3945/ajcn.113.069047
36. Birch, LL . Development of food preferences. Annu Rev Nutr. (1999) 19:41–62. doi: 10.1146/annurev.nutr.19.1.41
37. Popkin, BM , and Hawkes, C . Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol. (2016) 4:174–86. doi: 10.1016/S2213-8587(15)00419-2
38. World health organization . How the marketing of formula milk influences our decisions on infant feeding In:. Health organization and the United Nations Children’s fund (UNICEF). Geneva: World health organization (2022) License: CC BY-NC-SA 3.0 IGO
39. Smith, R , Kelly, B , Yeatman, H , and Boyland, E . Food marketing influences children’s attitudes, preferences and consumption: a systematic critical review. Nutrients. (2019) 11:875. doi: 10.3390/nu11040875
40. Harris, JL , Pomeranz, JL , Lobstein, T , and Brownell, KD . A crisis in the marketplace: how food marketing contributes to childhood obesity and what can be done. Annu Rev Public Health. (2009) 30:211–25. doi: 10.1146/annurev.publhealth.031308.100304
Keywords: parental modeling, infant formula, added sugar intakes, infant dietary intake, 24-h dietary recall
Citation: Griebel-Thompson AK, Fazzino TL, Cramer E, Paluch RA, Morris KS and Kong KL (2023) Early exposure to added sugars via infant formula may explain high intakes of added sugars during complementary feeding beyond maternal modeling. Front. Nutr. 10:1188852. doi: 10.3389/fnut.2023.1188852
Edited by:
Emmanouella Magriplis, Agricultural University of Athens, GreeceReviewed by:
Kalliopi Karatzi, Agricultural University of Athens, GreeceTania Aburto, National Institute of Public Health (Mexico), Mexico
Copyright © 2023 Griebel-Thompson, Fazzino, Cramer, Paluch, Morris and Kong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai Ling Kong, a2tvbmdAY21oLmVkdQ==
 Adrianne K. Griebel-Thompson
Adrianne K. Griebel-Thompson Tera L. Fazzino
Tera L. Fazzino Emily Cramer4,5
Emily Cramer4,5 Rocco A. Paluch
Rocco A. Paluch Katherine S. Morris
Katherine S. Morris Kai Ling Kong
Kai Ling Kong