- 1Department of Information, Zhongshan Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
- 2Department of Hematology, Zhongshan Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China, China
- 3Department of Epidemiology and Biostatistics, School of Public Health, Wuhan University, Wuhan, Hubei, China
- 4Xiamen Cardiovascular Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
Background: Modifiable risk factors are major drivers of cardiovascular disease (CVD). We aimed to determine the epidemiological trend and age-period-cohort effects on CVD burden attributable to dietary risks and high body mass index (BMI) across China and Pakistan from 1990 to 2019.
Methods: Data on the all-ages and age-specific CVD burden, age-standardized CVD mortality and disability-adjusted life years (DALYs) rates were obtained from the Global Burden of Disease Study 2019. Joinpoint regression analysis was conducted to find temporal trends and age-period-cohort (APC) modeling was used to estimate age, period, and cohort effects on CVD burden.
Results: Between 1990 and 2019, the all-ages CVD burden attributable to dietary risks and high BMI increased by ~2-3-fold in China and by 3-5-fold in Pakistan. The diet-related CVD age-standardized mortality rate (ASMR) and age-standardized disability-adjusted life years (DALYs) rate significantly decreased in China but increased in Pakistan. Both countries showed a marked increasing trend of CVD ASMR and the age-standardized DALYs rate attributable to high BMI. Taiwan in China showed a remarkable reduction in CVD burden. However, in Pakistan, all regions observed a significantly increasing trend of CVD burden attributable to modifiable risk factors. A higher risk ratio of premature CVD mortality (<70 years) was observed among Chinese attributable to high BMI and among Pakistani attributable to dietary risks. In China, early birth cohorts showed a higher risk ratio and recent birth cohorts experienced a lower risk ratio of CVD burden compared with Pakistan.
Conclusion: In conclusion, dietary risks and high BMI caused a huge CVD burden across China and Pakistan.
Introduction
Cardiovascular disease (CVD) caused 18.6 million deaths worldwide and is considered the leading cause of premature mortality in 2019. Cardiovascular diseases (CVDs), particularly ischemic heart disease (IHD) and stroke accounted for 9.1 million and 6.5 million deaths in the year 2019, respectively (1). By 2030, CVD-related deaths would be more than 23 million across the globe (2). World Health Organization (WHO) estimated that more than three-quarters of CVDs deaths occurred in low- and middle-income countries (LMICs) which is considered a growing epidemic problem (3). Among LMICs, China and Pakistan are home to 1.45 billion and 0.23 billion people and ranked first and fifth with the largest population in 2022 in the world, respectively (4). Both China and Pakistan experiencing an increasing trend of CVD burden (5). The number of CVD deaths increased in China (2.42 million to 4.58 million) and Pakistan (0.17 million to 0.34 million) from 1990 to 2019 (1).
The huge increasing CVD burden in China and Pakistan could be attributed to several modifiable risk factors (1). The United Nations set a target to reduce premature CVD mortality by 25% at the end of 2025 attributable to behavioral and biological risk factors (6). Behavioral and metabolic risk factors such as dietary risks and high body mass index (BMI) are major drivers of CVD. In the GBD study 2019, dietary risks are either an over-consumed diet (sodium, trans-fatty acids, sugar-sweetened beverages, red meat, and processed meat) or an under-consumed diet (whole grains, legumes, vegetables, fruits, nuts and seeds, milk, fiber, calcium, omega-3 fatty acids from seafood, and polyunsaturated fatty acids) (1, 7). High BMI (≥25 kg/m2) is considered an epidemic worldwide. High BMI exacerbates CVD risk factors including blood pressure, lipids, blood sugars, and inflammation, and has a linear association with coronary heart diseases. Globally, dietary risks and high BMI caused 6.8 million and 3.2 million deaths and 153 million and 86 million disability-adjusted life years (DALYs) in 2019, respectively (1).
Several epidemiological studies reported a temporal trend of CVD attributable to smoking, low physical activity, air pollution, and dietary risks in the high socio-demographic index (SDI) and low SDI countries from 1990 to 2017 (8–10). However, no or limited studies (1, 5, 7, 11, 12) observed the recent times trends and age-period-cohort effects on CVD burden attributable to the dietary risk and high BMI at the regional and country level across China and Pakistan. In the age-period-cohort analysis, period and cohort effects would assist public health policymakers to determine the success of earlier health-policy interventions and identifying future targets (13). To provide advice and references for health policymakers, an accurate and comparable analysis of long-term CVD trends at the regional and country level is required. Therefore, we aimed to determine the epidemiological trend and age-period-cohort effect on CVD burden attributable to dietary risks and high BMI across China and Pakistan from 1990 to 2019.
Materials and methods
Data source
In this study, the data were extracted by sex (male, female, and both sex combined) from the global burden of diseases (GBD) free online database (GBD 2019)1 (14) (accessed on July 7, 2022) from 1990 to 2019. In addition, all-ages deaths, the age-standardized mortality rate (ASMR), and age-specific data (i.e., from 25–29 years to 85–89 years) on CVD mortality and disability-adjusted life years (DALYs) attributable to dietary risks and high BMI were extracted. GBD is an international cooperative project that estimates the disease burden at regional, national, and global levels. GDB estimates the burden of disease indices including, prevalence, incidence, mortality rate, years of life lost (YLL), years lived with disability (YLD), and DALYs for several diseases and injuries. Moreover, the GBD data are provided by different organizations like World Bank Open Data, WHO, and Global Health Observatory for different political and social research. The GBD data is managed by the Institute for Health Metrics and Evaluation (IHME), University of Washington. Therefore, a waiver of informed consent was reviewed and approved by the University of Washington Institutional Review Board (15, 16).
Variables understudy
In the present study, the considered modifiable risk factors were dietary risks and high BMI (≥25 kg/m2). The dietary risk factor was a composite of an over-consumed diet (sodium, trans-fatty acids, sugar-sweetened beverages, red meat, and processed meat) and an under-consumed diet (whole grains, legumes, vegetables, fruits, nuts and seeds, milk, fiber, calcium, omega-3 fatty acids from seafood, and polyunsaturated fatty acids) (1). The outcome variables were ASMR, all-ages death numbers, and DALYs of CVD, ischemic heart disease (IHD), and ischemic stroke (IS) for China and Pakistan at the regional and country level from 1990 to 2019. Regions in Pakistan were Islamabad, Punjab, Sindh, Khyber Pakhtunkhwa (KPK), Balochistan, Azad Jammu & Kashmir (AJ& K), Gilgit-Baltistan (GB), and Taiwan in China. DALYs are defined as the sum of years lived with disability (YLDs) and years of life lost (YLLs) (16).
Statistical analysis
Joinpoint regression for trend analysis (1990–2019)
To assess the temporal trends of CVD, IHD, and IS burden, we estimated the average annual percentage change (AAPC) for CVD, IHD, and IS mortality and DALYs with joinpoint regression analysis. AAPC represents the trend of CVD, IHD, and IS burden in the whole period from 1990 to 2019. Additionally, AAPC is a weighted average of the yearly percentage change determined by the joinpoint model, with weights corresponding to the duration of the annual percentage change (APC) interval. The APC shows the CVD, IHD, and IS burden trend in each segment determined by using joinpoint regression software. From 1990 to 2019, we produced AAPCs and their 95% confidence intervals (CIs) for each trend segment identified by the model. Furthermore, we estimated AAPCs of CVD, IHD, and IS deaths for both sexes combined, males, and females. AAPC is considered significant when it is different from 0 at the alpha of 0.05. This analysis was conducted using the joinpoint regression program version 4.9.1.0 (April 2022) from the Surveillance Research Program of the U.S. National Cancer Institute (NCI).
Age-period-cohort analysis
The aim of the age-period-cohort (APC) analysis is to estimate the effects of age, period, and cohort on CVD burden attributable to modifiable risk factors. The age effect represents the association of CVD burden with different age groups. Period effect represents influencing factors, such as a series of historical events and environmental factors, and it reflects variation in the CVD burden over time that influences all age groups simultaneously. The cohort effect shows variations of CVD burden across birth cohorts born in the same year and changes in different lifestyles (17). The common problem associated with the APC analysis is collinearity (i.e., birth cohort = period - age). The APC model is affected by the linearity between two variables, so it is impossible to determine the three independent linear APC variables of age, period, and cohort. We used the APC model with the intrinsic estimator (IE), which is a new method to estimate the coefficients and solve the collinearity problem by generating a distinctive set of trend estimates independent of any arbitrary assignment of identifying limitations on age, period, or cohort coefficients that may not be verified in the data itself (18). Estimated coefficients for the age, period, and cohort effects were produced by the APC analysis using the IE method. The exponential value [exp(coef.) = ecoef.] was created from these coefficients, which denotes the risk ratio (RR) of a particular age, period, or birth cohort relative to the reference group.
In the APC model using the IE method, the age-specific CVD rates were appropriately categorized into 13 age groups (from 25–29 years to 85–89 years). It has 6 periods with 5-year intervals (from 1990–1994 to 2015–2019) and 18 birth cohorts (period-age) (from1905-1909 to 1990–1994). The general form of the APC model is written as Y = log (M) = μ + αage1+ βperiod1 + γcohort1 + ε; where, M is defined as the incidence rate in the age groups, α, β, and γ indicates the functions of age, period, and cohort effect, μ, and ε are the intercept item and the random error. The APC model was used to decompose the three trends and estimate efficient results (19). Moreover, the Akaike information criterion (AIC), and Bayesian information criterion (BIC) were used to estimate and analyze the degree of fitting of the model. The APC analysis was done using Stata 15.0 software (College Station, TX, USA).
Results
CVD burden attributable to dietary risks
For both sexes, the all-ages CVD deaths due to dietary risks significantly increased in China (0.9 million to 1.7 million) and in Pakistan (0.06 million to 0.15 million) by 89 and 150%, respectively during the study period. The CVD ASMR and the age-standardized DALYs rate in China significantly decreased by −1.2% (95%CI: −1.5, −0.9) and by −1.4% (95%CI: −1.7, −1.2) per year. However, in Pakistan, the ASMR of CVD and the age-standardized DALYs rate significantly increased by 0.7% (95%CI: 0.6, 0.7) and by 0.7% (95%CI: 0.6, 0.8) per year. At the regional level in China, Taiwan showed a remarkable reduction in CVD ASMR by −3.2% (95%CI: −3.5, −2.9) and age-standardized DALYs rate by −2.9% (95%CI, −3.1, −2.7). However, in Pakistan, all regions observed significantly increasing trends of CVD ASMR and age-standardized DALYs rate with the highest in KPK. Overall, male showed less improvement in CVD, IHD, and IS ASMR and age-standardized DALYs rate attributable to dietary risks than the female population across China and Pakistan (Tables 1–3; Supplementary Tables S1–S6; Figure 1; Supplementary Figure S1).
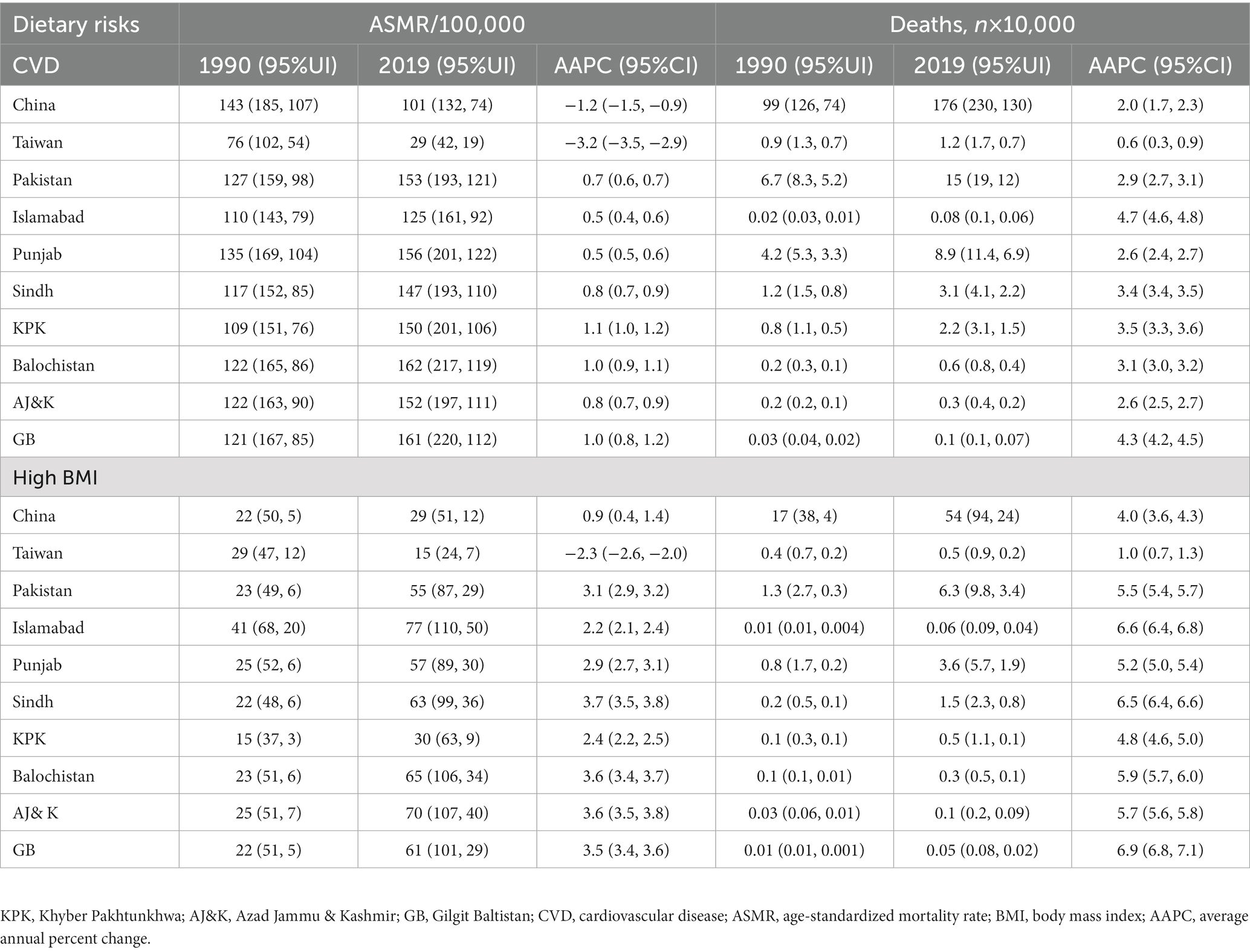
Table 1. The temporal trend in the burden of CVD mortality attributable to the dietary risk and high BMI for both sexes across China and Pakistan from 1990 to 2019.
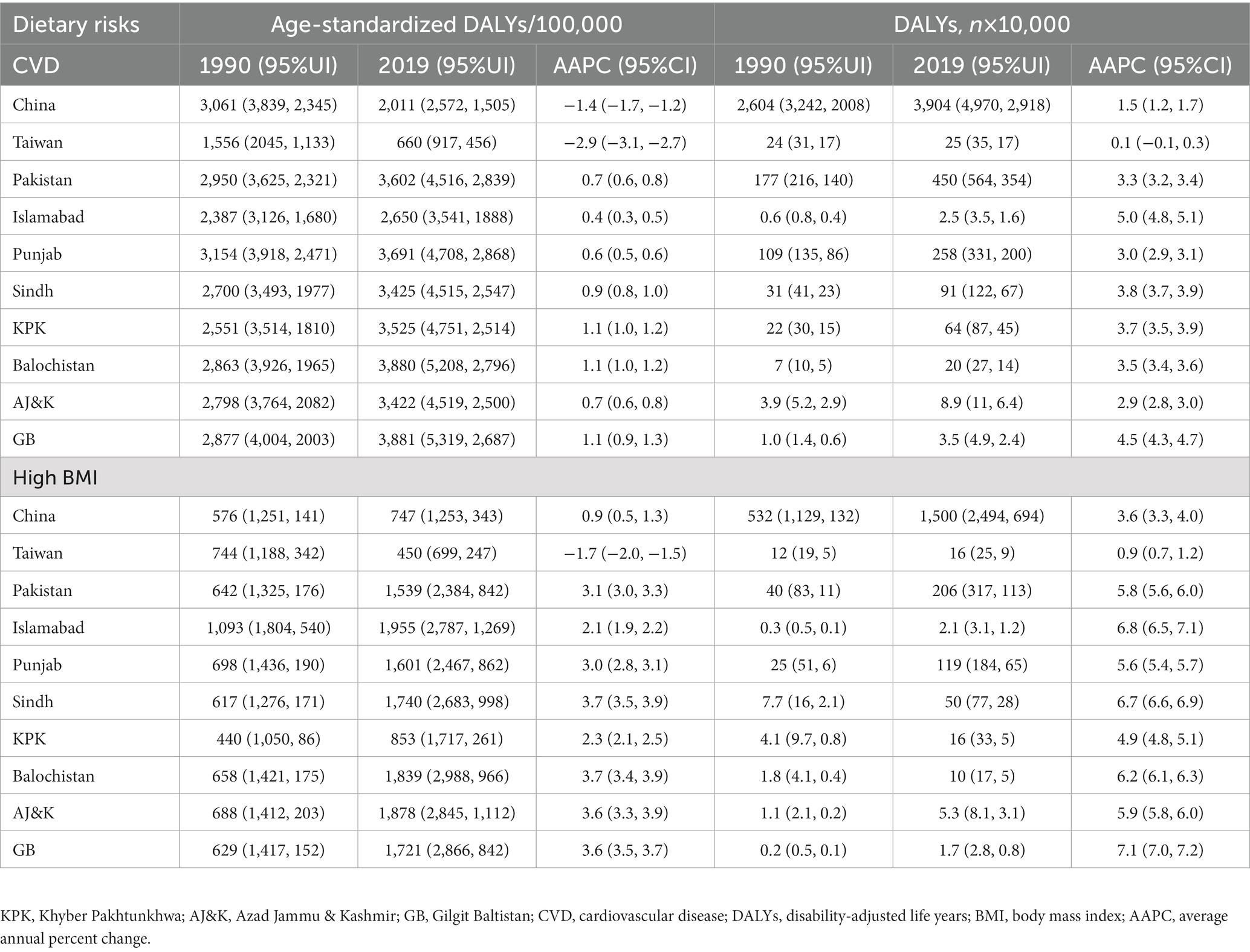
Table 2. The temporal trend in the burden of CVD DALYs attributable to the dietary risk and high BMI for both sexes across China and Pakistan from 1990 to 2019.
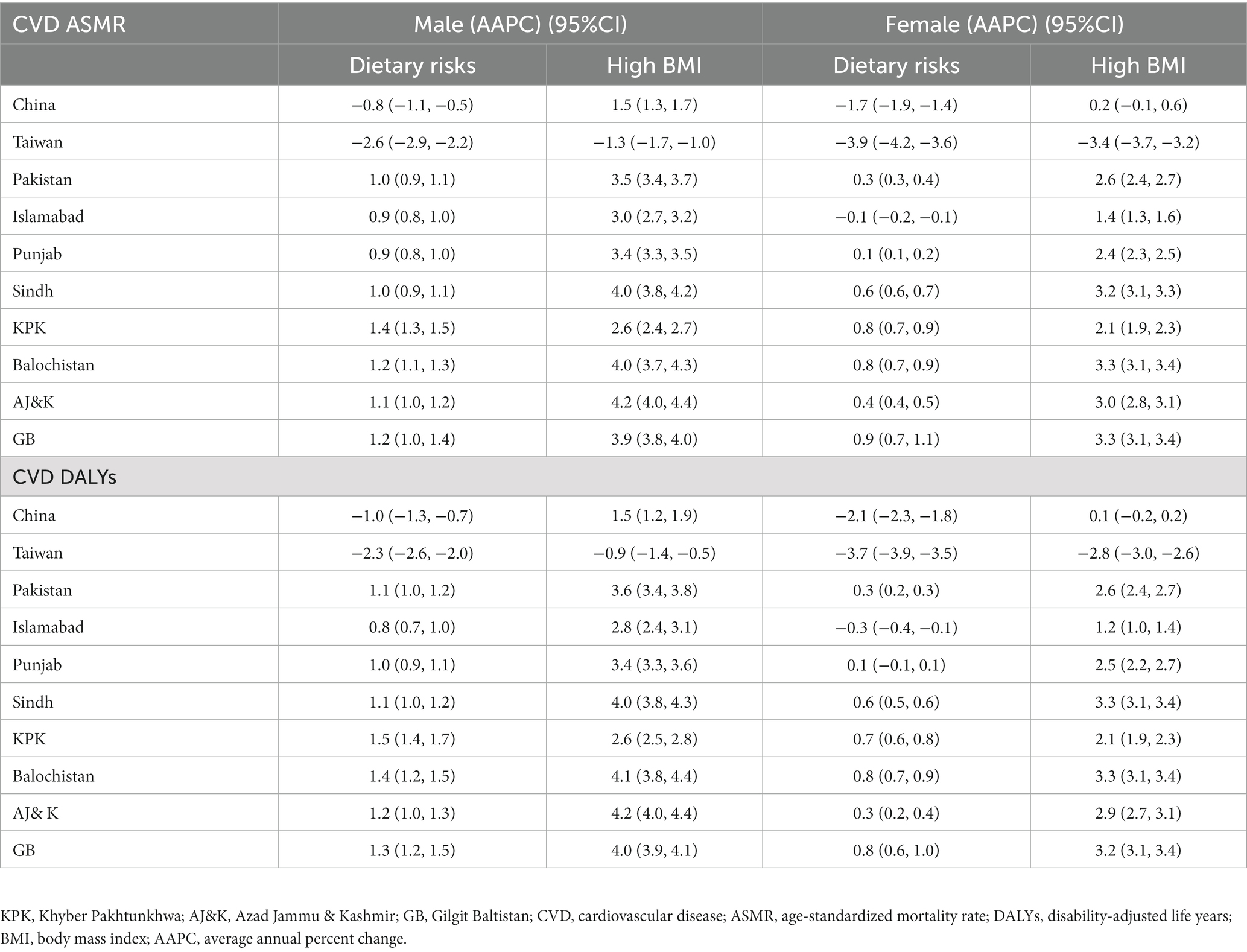
Table 3. The temporal trend in the burden of CVD AMSR and DALYs attributable to the dietary risk and high BMI in males and females across China and Pakistan from 1990 to 2019.
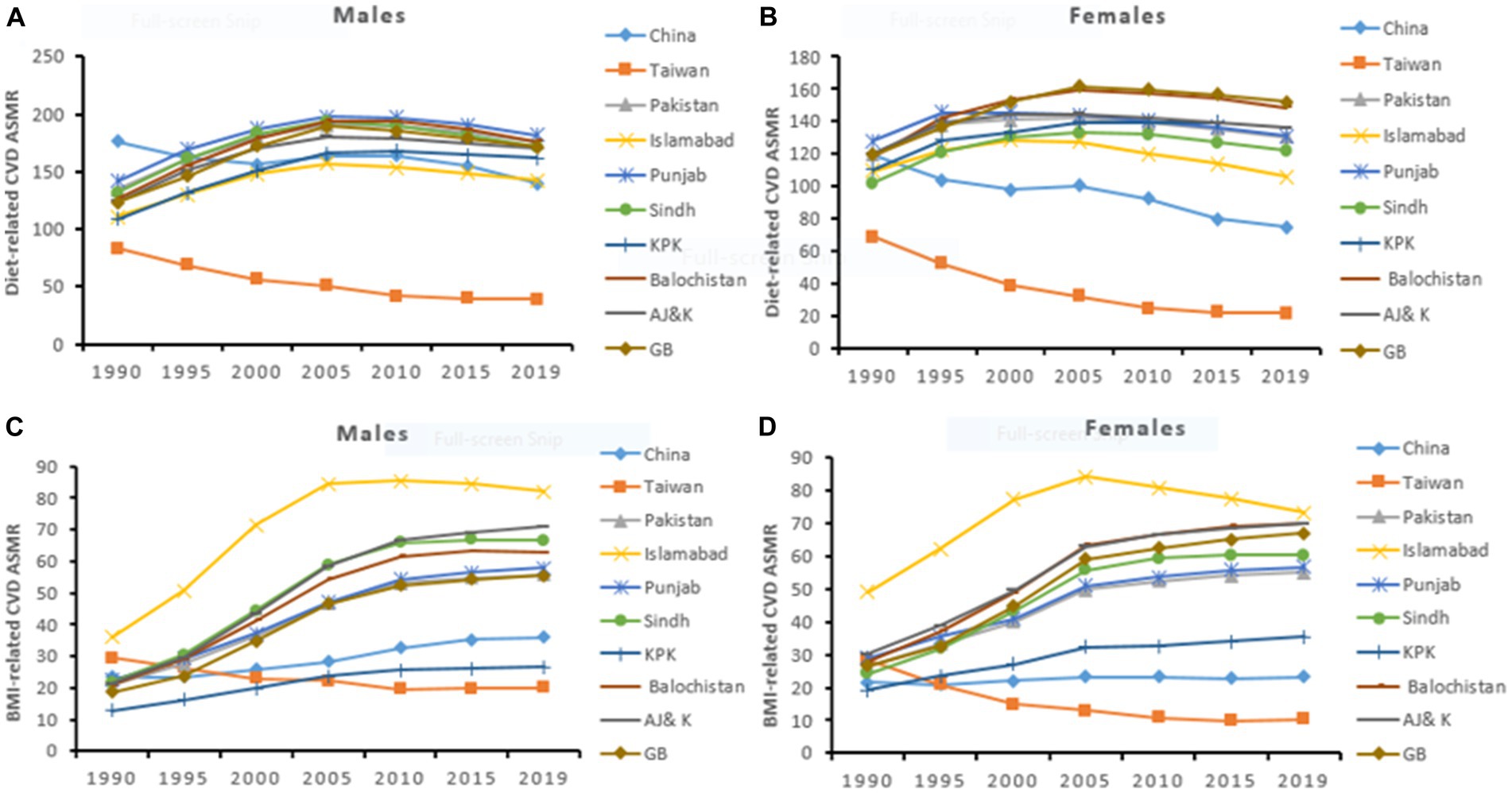
Figure 1. Temporal trend of CVD ASMR (per 100,000) attributable to dietary risks (A,B) and high BMI (C,D) in males and females across China and Pakistan.
CVD burden attributable to high BMI
For both sexes, the all ages-CVD deaths attributable to high BMI remarkably increased in China by 4.0% (95%CI: 3.6, 4.3) and in Pakistan by 5.5% (95%CI: 5.4, 5.7) per year. Similarly, the ASMR of CVD and the age-standardized DALYs rate significantly increased in both China and Pakistan. At the regional level in China, Taiwan experienced a pronounced reduction in CVD ASMR by −2.3% (95%CI: −2.6, −2.0) and age-standardized DALYs rate by −1.7 (95%CI: −2.0, −1.5) per year. On the other hand, in Pakistan, all regions showed a significantly increasing trend of CVD ASMR and age-standardized DALYs rates notably in Sindh, Balochistan, and AJ&K. Moreover, Islamabad experienced higher CVD ASMR and DALYs rates during the study period. The male population showed the fastest increasing trend of CVD, IHD, and IS ASMR and age-standardized DALYs rate than the female population in both countries (Tables 1–3; Supplementary Tables S1–S6; Figure 1; Supplementary Figure S1).
Age-period-cohort effect on CVD burden attributable to dietary risks and high BMI
The risk ratio of CVD mortality and DALYs due to dietary risks and high BMI markedly increased with age. China had the highest risk of CVD mortality across all age groups, particularly at older ages than Pakistan. The risk ratio of premature CVD mortality (<70 years) attributable to dietary risks was higher among Pakistanis. However, the Chinese population showed a higher risk ratio of premature CVD mortality attributable to high BMI. Period effects were generally higher for CVD mortality and DALYs attributable to high BMI with the most remarkable in Pakistan. Compared to the reference cohorts, the risk ratio of cohort effect on CVD burden attributable to dietary risks and high BMI showed a similar downward trend among the Chinese and Pakistani populations. Early birth cohorts in China had a higher risk ratio of CVD mortality and DALYs than in Pakistan. However, recent birth cohorts in China showed relatively a lower risk ratio of CVD burden attributable to modifiable risk factors (Tables 4, 5; Figures 2, 3; Supplementary Figures S2, S3).
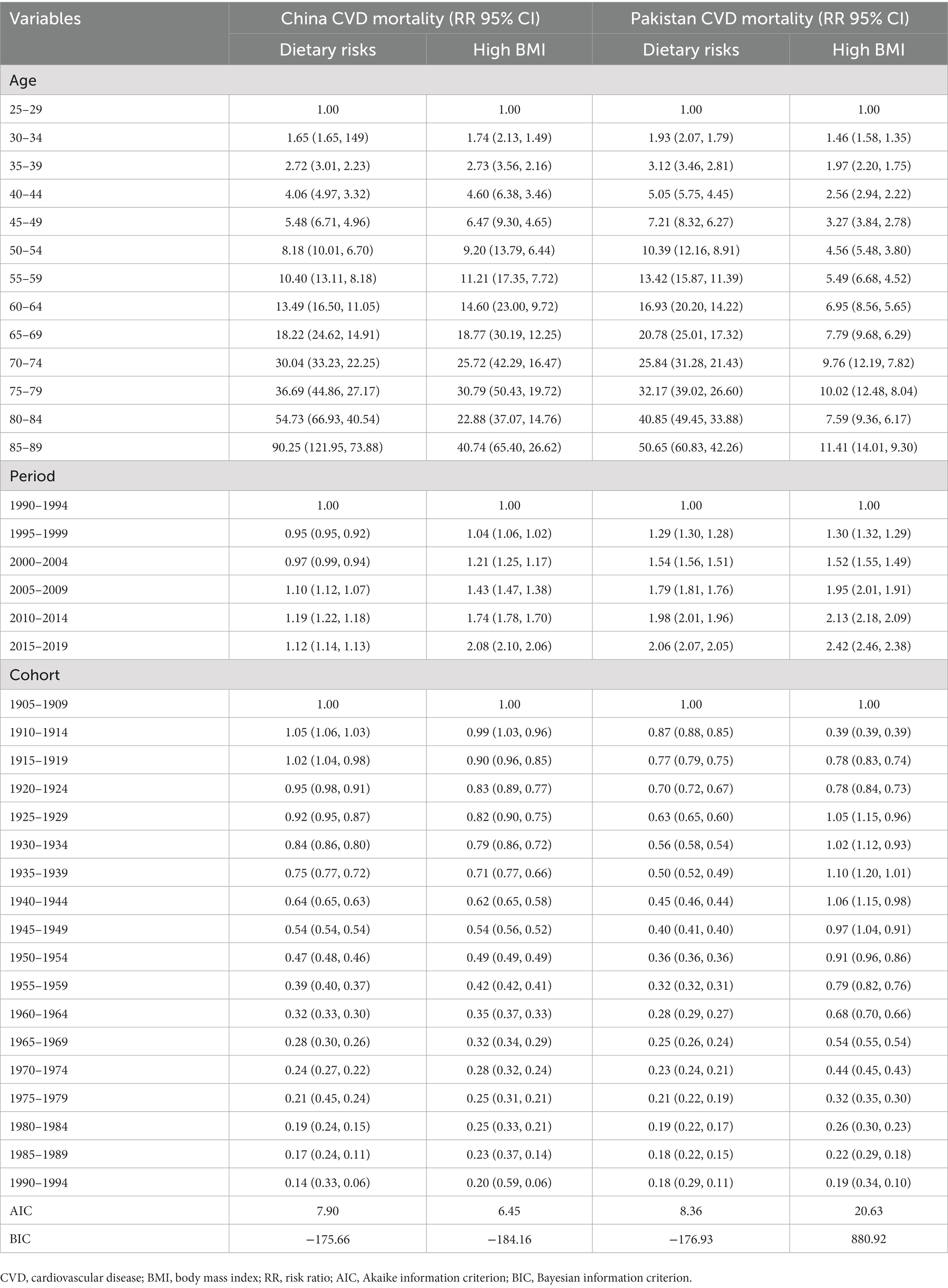
Table 4. Age-Period-Cohort effects on CVD mortality attributable to dietary risks and high BMI across China and Pakistan.
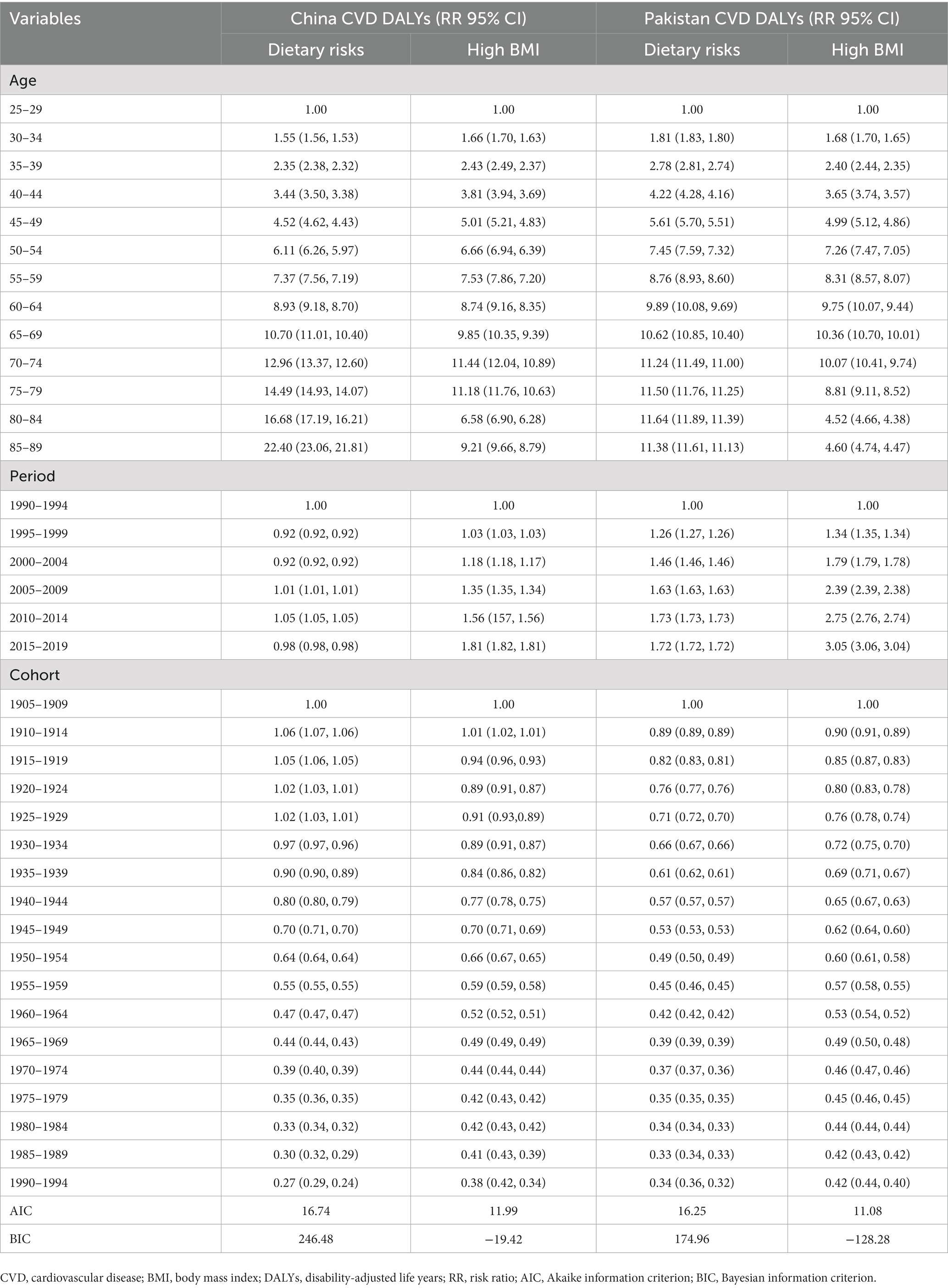
Table 5. Age-Period-Cohort effects on CVD DALYs attributable to dietary risks and high BMI across China and Pakistan.
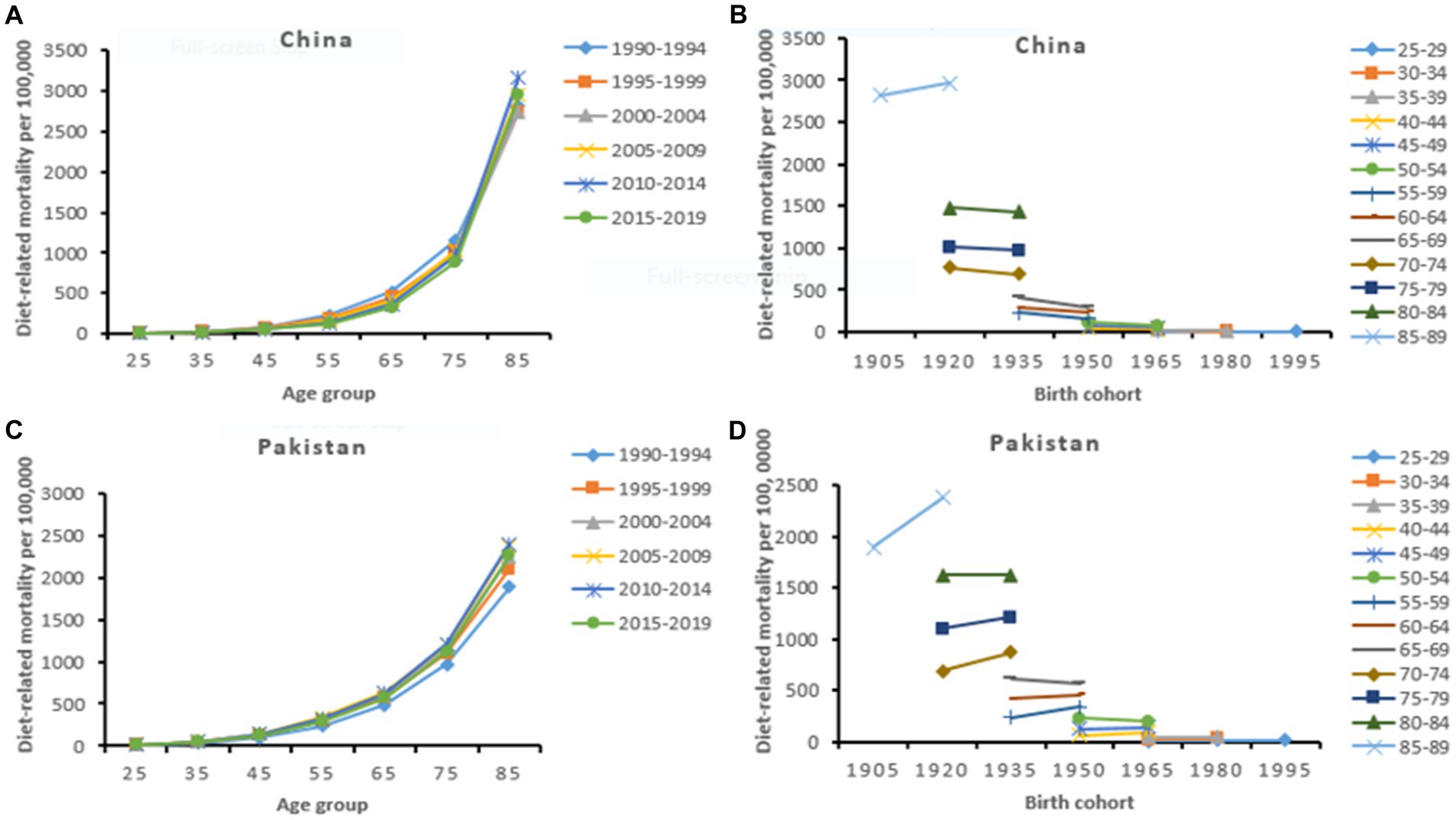
Figure 2. Diet-related age-specific CVD mortality rate by period (A,C) and cohort-specific CVD mortality rate by age group (B,D) across China and Pakistan from 1990 to 2019.
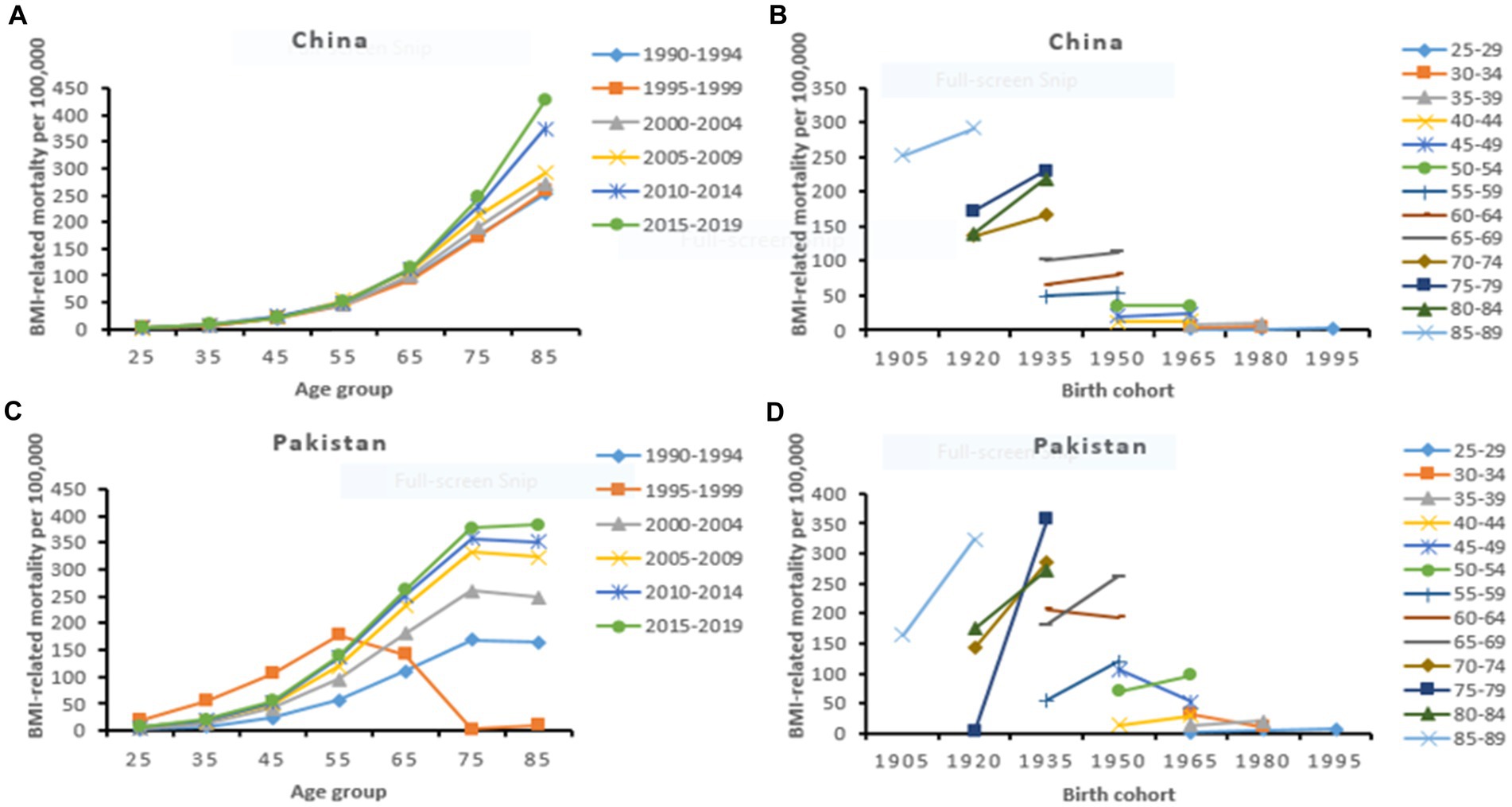
Figure 3. High BMI-related age-specific CVD mortality rate by period (A,C) and cohort-specific CVD mortality rate by age group (B,D) across China and Pakistan from 1990 to 2019.
Discussion
The present GBD study 2019 provides the epidemiological trend (1990–2019) and age-period-cohort effect on CVD mortality and DALYs attributable to dietary risks and high BMI at the regional and country level across China and Pakistan. We observed that the all-ages CVD deaths and DALYs due to dietary risks and high BMI significantly increased in China and Pakistan during the study period. The diet-related CVD ASMR and the age-standardized DALYs rate significantly decreased in China. However, the ASMR of CVD and the age-standardized DALYs rate attributable to dietary risks significantly increased in Pakistan. Both countries showed a marked increasing trend of CVD ASMR and the age-standardized DALYs rate attributable to high BMI. At the regional level in China, Taiwan showed a remarkable reduction in CVD ASMR and age-standardized DALYs rate attributable to dietary risks and high BMI. However, in Pakistan, all regions observed significantly increasing trends of CVD ASMR and age-standardized DALYs rate attributable to aforementioned modifiable risk factors.
Age-period-cohort analysis revealed that the risk ratio of premature CVD mortality (<70 years) attributable to dietary risks was higher among Pakistanis. On the other hand, the Chinese population showed a higher risk ratio of premature CVD mortality attributable to high BMI. The risk ratio of period effect on CVD burden attributable to modifiable risk factors significantly increased across both countries. In China, early birth cohorts showed a higher risk and recent birth cohorts experienced a lower risk of CVD burden compared with Pakistan.
Temporal trend in CVD burden attributable to dietary risks
CVDs are the primary consequences of dietary risks and one-third of global CVD deaths are attributed to dietary risks (1). Our study found that the all-ages CVD deaths and DALYs due to dietary risks nearly doubled in China and tripled in Pakistan. The upward trend in all-ages CVD burden could be explained by population growth and aging across China and Pakistan (1). Aging has a profound impact on heart health and the arterial system and has been linked with a higher risk of CVD (20). Globally, adults aged ≥65 years increased by 3-fold over the last four decades. The older population in China and Pakistan is increasing and is projected to double by 2050 (4). It suggests that both countries are needed to significantly invest in the primary and secondary prevention of CVD among the older population.
Our findings show that ASMR of CVD and the age-standardized DALYs rate attributable to dietary risks significantly decreased in China as well as at the regional level in Taiwan. The reduction in CVD burden attributable to dietary risks could be explained by improvements in diet quality and changes in diet patterns among the Chinese population. The diet quality as measured by China Dietary Guidelines Index 2018 (CDGI-2018) improved from 41.7 to 52.4 during 1991–2015 among Chinese adults aged 18 years or older. Energy intake from high-quality protein and high-quality fats significantly increased whereas consumption of low-quality carbohydrates significantly decreased (21). A lower risk of CVD mortality was observed among Chinese adults having higher diet index scores and optimal consumption of vegetables, fruits, and lower consumption of red meat (22).
Moreover, the increasing trend in urbanization, higher education level, and socioeconomic status have improved diet quality among the Chinese population and resulted in lower CVD deaths (23, 24). The most recently launched public health and nutrition-related policy “Healthy China Action Plan (2019–2030)” including the popularization of health knowledge and promotion of a balanced diet could further improve diet quality and reduce diet-related CVD mortality and morbidity (25). The diet quality and dietary habits in Taiwan significantly improved such as higher consumption of vegetables, fruits, whole grains, fish, soy products, nuts, and seeds (26, 27). These positive changes in dietary habits could explain the remarkable reduction in the CVD burden at the regional level in Taiwan.
We observed significantly increasing trends of CVD ASMR and age-standardized DALYs rate attributable to dietary risks in Pakistan and across all regions with the highest in KPK. Pakistan is a country with a low socioeconomic status (SES). Poverty and low SES affect diet quality and are associated with adverse health outcomes (28). Moreover, Pakistan is an agricultural country with a large population that lives in rural areas with a lower per capita income (31%) than in urban areas. One-fifth of the population is malnourished and one-third of the population has no access to adequate nutrition (28). All these interrelated factors could explain a marked increase in CVD burden attributable to dietary risks. A previous study also reported that the Pakistani traditional diet was associated with high cardiovascular risk factors (29). The majority of Pakistani people eat deep-frying foods and foods high in saturated fats which ultimately increased the risk of CVD (30).
Pakistan is also initiated public health and nutrition-related policy to promote health knowledge and awareness about healthy food choices as adopted by China (25). Over the last few years, several nutritional programs have been launched by the government and non-government organizations to raise nutritional awareness among the Pakistani population. The government of Pakistan has initiated health and nutrition programs at the school level to provide relevant nutritional information to students (31, 32). At the community level, Nutrition International (NI) works with the Pakistani government to combat micronutrient malnutrition such as deficiency of iron, zinc, folic acid, and vitamin A (32). In the coming years, these nutritional intervention and awareness programs will gradually decrease the CVD burden attributable to dietary risks among the Pakistani population.
Temporal trend in CVD burden attributable to high BMI
Obesity or high BMI is a growing public health epidemic problem and its prevalence increased by 3-fold over the last four and half decades across the globe. High intake of energy-dense foods, lower energy expenditure, and low physical activity lead to obesity (1, 33). High BMI exacerbates cardiovascular risk factors and increased the risk of CVD including hypertension, heart failure, and coronary heart disease (34). We observed that the all-ages CVD deaths and DALYs attributable to high BMI increased by 3-fold in China and by 5-fold in Pakistan. Moreover, the all-ages IHD, IS deaths and DALYs increased by 5-fold in China and by ~6-fold across Pakistan. The ASMR and age-standardized DALYs rate across all CVD categories significantly increased in China and Pakistan. All regions in Pakistan observed significantly increasing trends of CVD ASMR and age-standardized DALYs rate attributable to high BMI notably in Sindh, Balochistan, and AJ& K. However, Taiwan in China showed a marked reduction in CVD ASMR and age-standardized DALYs rate due to high BMI.
High BMI or obesity is a serious public health problem in China. More than half of the adult population and one-fifth of children and adolescents are overweight or obese and the rates are continuously rising in China (35). The continuously increasing burden of obesity could be driven by rapid economic growth. It has reduced poverty and impacted dietary habits, moving away from a traditional and balanced diet and adhering to ultra-processed junk food product. Physical activity substantially decreased with an increasingly sedentary lifestyle in China (36, 37). Such changes in diet patterns and lifestyle and other risk factors including genetic susceptibility, and psychosocial factors are implicated in the increasing trend of obesity in China and associated with a higher risk of CVD (36, 37). In the general Chinese population, obesity was associated with higher odds of CVDs (38).
Over the last two decades, several prevention and interventional programs have been implemented in China, however, obesity and chronic diseases such as CVD have not been effectively prevented and reduced yet (39). Recently in 2020, the National Health Commission of the People’s Republic of China (China NHC) formulated a series of policies, guidelines, and recommendations, which aims to effectively control, prevent, and reduce obesity among Children and adolescents. Moreover, in 2021, the China NHC’s Bureau of Disease Control and Prevention released a set of guidelines for obesity prevention and control among Chinese adults (40). In 2022, “The Expert Consensus on Obesity Prevention and Treatment” was issued which consisted of prevention and control strategies, and future recommendations (39). It reflects that China has made a great effort for obesity prevention which will ultimately decrease obesity-related CVD burden in the recent future. However, if these obesity-related policies and interventions have not effectively implemented, it is projected that about 65.3% of adults and 31.8% of children and adolescents could become overweight and obese by 2030 in China (35, 40).
Our findings show that the CVD ASMR and age-standardized DALYs rate attributable to high BMI markedly increased in Pakistan and across all regions. Pakistan with 50% of obesity is the tenth most obese nation in the world due to intake of a high-fat diet and sedentary lifestyle (41, 42). Among the Pakistani population, diet mostly consisted of saturated fats and trans fatty acids. The trend of eating fast food, processed foods, and junk food increased among the young population. Moreover, rapid urbanization and modernization have shifted the intake of a traditional low-fat diet to a high-fat diet (43). According to a systematic review and meta-analysis, Pakistani adolescents had a low level of physical activity and less than one-fifth has achieved recommended levels (44). The higher consumption of high-fat and saturated-fat diets, and low physical activity could be the contributing factors to increasing obesity which resulted in high CVD mortality and morbidity among the Pakistani population (45, 46).
Pakistan urgently needs to develop and formulate a prevention and control strategy for obesity at the national level by implementing the World Health Organization (WHO) policies and recommendations for preventing obesity and diabetes in the Eastern Mediterranean Region (47). The government and non-government organizations should initiate and promote public awareness programs about the impact of a healthy diet and physical activity on individual and national health. School and college-based awareness and intervention pogroms should be initiated across the country for promoting healthy dietary habits and physical activity among the younger population. Adopting healthy dietary habits and sufficient physical activity could reduce the high BMI-related CVD burden in Pakistan (48).
Overall, male showed less improvement and high burden in CVD, IHD, and IS ASMR and age-standardized DALYs rate attributable to dietary risks and high BMI than the female population across China and Pakistan. Generally, men showed poor dietary habits and lower Healthy Eating Index (HEI) scores (49), a higher prevalence of obesity (50), and experienced earlier (10–15 years) coronary heart disease than women. Moreover, women had a lower incidence of CVD than men due to estrogen’s protective effect on the cardiovascular system (51, 52). Our findings are coinciding with several previous studies (7, 11, 53).
Age-period-cohort effect on CVD burden attributable to dietary risks and high BMI
We found that the risk ratio of CVD mortality and DALYS showed a linear association with age. Age is an independent risk factor of CVD and the proportion of CVD incidence increased with aging among both men and women (54, 55). The age effect on CVD burden attributable to modifiable risk factors was remarkable in China. Moreover, the risk ratio of premature CVD mortality (<70 years) attributable to high BMI was higher among the Chinese population. Between 1993 and 2015, the prevalence of overweight (26.6 to 41.3%), obesity (4.2 to 15.7%), and abdominal obesity (20.2 to 46.9%) increased among Chinese adults aged 18–80 years. The absolute increase in BMI was positively correlated with age and older people showed a marked increasing trend in obesity (56) and a higher risk of CVD mortality and morbidity (20). On the other hand, the Pakistani population showed a higher risk ratio of premature CVD mortality attributable to dietary risk. Several factors such as malnutrition (28) poverty and low diet quality (29) poor dietary habits (30) and a poor healthcare system (57) may contribute to the increased risk of diet-related premature CVD mortality in Pakistan.
In our findings, the risk ratio of period effect on CVD burden attributable to modifiable risk factors significantly increased across both countries. The period effect was generally higher for CVD mortality and DALYs attributable to high BMI notably in Pakistan. Pakistan is facing twin problems of poor nutrition and over-nutrition and around 5.4 million school-aged children will be obese by 2030 (42). The increasing risk of BMI-related CVD burden in Pakistan could be attributed to the high trend of fast food, urbanization, moderation, and low physical activity. The fast food industry is the 2nd largest in Pakistan with 180 million consumers (58). The trend of fast food consumption is tremendously increasing among the young population (43). Due to rapid urbanization and modernization people have adopted a westernized high-fat diet over a traditional low-fat diet (43). Moreover, Pakistani adolescents had a low level of physical activity, and less than one-fifth achieved recommended levels (44).
We observed that compared to the reference cohort, the risk ratio of cohort effect on CVD burden attributable to dietary risks and high BMI showed a similar monotonic downward pattern among the Chinese and Pakistani populations. Early birth cohorts in China had a higher risk ratio of CVD mortality and DALYs. However, recent birth cohorts in China showed relatively a lower risk ratio of CVD mortality and DALYs than in Pakistan. Advancement in techniques for diagnosis, management, treatment, improvement in healthcare facilities, early-life nutrition, education level, and socioeconomic status may play a critical role in the lower risk ratio of CVD burden in the recent birth cohorts in China (17, 59, 60). In accordance with our findings, several studies observed that early birth cohorts showed higher risk and recent birth cohorts experienced a lower risk of CVD burden in China (17, 59, 61, 62).
Our study has several limitations. First, our findings are obtained from GBD data and all GBD limitations are apply to our results as mentioned previously (63). Second, we observed epidemiological trends of CVD mortality and morbidity attributable to overall dietary risks and could not find for the individual dietary risk factor. Third, the age-period-cohort effect on CVD burden attributable to dietary risks and high BMI was not conducted for different genders and at the regional level across China and Pakistan.
Conclusion
Our findings indicate that the all-ages CVD deaths and DALYs due to dietary risks and high BMI significantly increased across China and Pakistan from 1990 to 2019. The diet-related CVD ASMR and the age-standardized DALYs rate significantly decreased in China. However, the ASMR of CVD and the age-standardized DALYs rate attributable to dietary risks significantly increased in Pakistan. Both countries showed a marked increasing trend of CVD ASMR and the age-standardized DALYs rate attributable to high BMI. Age-period-cohort analysis showed a higher risk ratio of premature CVD mortality (<70 years) among Chinese attributable to high BMI and Pakistani attributable to dietary risks. In China, early birth cohorts showed higher risk and recent birth cohorts experienced a lower risk of CVD burden compared with Pakistan. Besides government-level initiatives, proper nursing care could play a significant role in preventing and controlling premature CVD mortality across China and Pakistan (64). These findings can provide evidence-based references for health-policy makers to priorities strategies for the premature CVD burden attributable to dietary risk and high BMI across China and Pakistan.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
Ethical approval was not provided for this study on human participants because ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The requirement for informed consent was waived. The ethics committee waived the requirement of written informed consent for participation.
Author contributions
XY, WY, and Nawsherwan: study design and critical revision of manuscript and writing— review and editing. XY, SM, and Nawsherwan: data collection and analysis and drafting the manuscript. Nawsherwan and SM: data collection. Nawsherwan and SM: data analysis. WY and Nawsherwan: writing—original draft preparation. Nawsherwan: visualization. XY and WY: supervision. WY: project administration. All authors have read and agreed to the published version of the manuscript.
Acknowledgments
We would like to thank all authors for their substantial, direct, and intellectual contribution to this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1158769/full#supplementary-material
Footnotes
References
1. Roth Gregory, A, Mensah George, A, Johnson Catherine, O, Addolorato, G, Ammirati, E, Baddour Larry, M, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
2. Lozano, R, Naghavi, M, Foreman, K, Lim, S, Shibuya, K, Aboyans, V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. (2012) 380:2095–128. doi: 10.1016/S0140-6736(12)61728-0
3. Roth Gregory, A, Johnson, C, Abajobir, A, Abd-Allah, F, Abera Semaw, F, Abyu, G, et al. Global, regional, and National Burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
4. Economic UNDo, Social Affairs PD. World population prospects 2022: Summary of results. UN DESA/POP/2022/TR/NO. 3. (2022).
5. Zhao, D. Epidemiological features of cardiovascular disease in Asia. JACC. (2021) 1:1–13. doi: 10.1016/j.jacasi.2021.04.007
6. Chestnov, O. World Health Organization global action plan for the prevention and control of noncommunicable diseases. Geneva: Switzerland (2013).
7. Nawsherwan, BW, Le, Z, Mubarik, S, Fu, G, and Wang, Y. Prediction of cardiovascular diseases mortality- and disability-adjusted life-years attributed to modifiable dietary risk factors from 1990 to 2030 among East Asian countries and the world. Front Nutr. (2022) 9:898978. doi: 10.3389/fnut.2022.898978
8. Wang, F, Yu, Y, Mubarik, S, Zhang, Y, Liu, X, Cheng, Y, et al. Global burden of ischemic heart disease and attributable risk factors, 1990-2017: A secondary analysis based on the global burden of disease study 2017. Clin Epidemiol. (2021) 13:859–70. doi: 10.2147/clep.S317787.
9. Amini, M, Zayeri, F, and Salehi, M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. (2021) 21:401. doi: 10.1186/s12889-021-10429-0
10. Wu, X, Zhu, B, Xu, S, Bi, Y, Liu, Y, and Shi, J. A cross country comparison for the burden of cardiovascular disease attributable to tobacco exposure in China, Japan, USA and world. BMC Public Health. (2020) 20:888. doi: 10.1186/s12889-020-09031-7
11. Dong, C, Bu, X, Liu, J, Wei, L, Ma, A, and Wang, T. Cardiovascular disease burden attributable to dietary risk factors from 1990 to 2019: A systematic analysis of the global burden of disease study. Nutr Metab Cardiovasc Dis. (2022) 32:897–907. doi: 10.1016/j.numecd.2021.11.012
12. Rehman, S, Rehman, E, Ikram, M, and Jianglin, Z. Cardiovascular disease (CVD): assessment, prediction and policy implications. BMC Public Health. (2021) 21:1299. doi: 10.1186/s12889-021-11334-2
13. Rosenberg, PS, and Anderson, WF. Proportional hazards models and age–period–cohort analysis of cancer rates. Stat Med. (2010) 29:1228–38. doi: 10.1002/sim.3865
14. Vos, T, Lim, SS, Abbafati, C, Abbas, KM, Abbasi, M, Abbasifard, M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
15. Roth, GA, Abate, D, Abate, KH, Abay, SM, Abbafati, C, Abbasi, N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
16. Kyu, HH, Abate, D, Abate, KH, Abay, SM, Abbafati, C, Abbasi, N, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1859–922. doi: 10.1016/S0140-6736(18)32335-3
17. Wang, Z, Hu, S, Sang, S, Luo, L, and Yu, C. Age–period–cohort analysis of stroke mortality in China: data from the global burden of disease study 2013. Stroke. (2017) 48:271–5. doi: 10.1161/STROKEAHA.116.015031
18. Yang, Y, Fu, WJ, and Land, KC. A methodological comparison of age-period-cohort models: the intrinsic estimator and conventional generalized linear models. Sociol Methodol. (2004) 34:75–110. doi: 10.1111/j.0081-1750.2004.00148.x
19. Keyes, KM, and Miech, R. Age, period, and cohort effects in heavy episodic drinking in the US from 1985 to 2009. Drug Alcohol Depend. (2013) 132:140–8. doi: 10.1016/j.drugalcdep.2013.01.019
20. North, BJ, and Sinclair, DA. The intersection between aging and cardiovascular disease. Circ Res. (2012) 110:1097–108. doi: 10.1161/circresaha.111.246876.
21. Huang, L, Wang, L, Jiang, H, Wang, H, Wang, Z, and Zhang, B. Trends in dietary carbohydrates, protein and fat intake and diet quality among Chinese adults, 1991–2015: results from the China Health and Nutrition Survey. Public Health Nutr. (2022) 26:834–43. doi: 10.1017/S1368980022002099
22. Neelakantan, N, Koh, W-P, Yuan, J-M, and van Dam, RM. Diet-quality indexes are associated with a lower risk of cardiovascular, respiratory, and all-cause mortality among Chinese adults. J Nutr. (2018) 148:1323–32. doi: 10.1093/jn/nxy094 %J The Journal of Nutrition
23. He, Y, Fang, Y, Bromage, S, Fung, TT, Bhupathiraju, SN, Batis, C, et al. Application of the global diet quality score in Chinese adults to evaluate the double burden of nutrient inadequacy and metabolic syndrome. J Nutr. (2021) 151:93S–100S. doi: 10.1093/jn/nxab162
24. Huang, Y, Wang, H, and Tian, X. Changing diet quality in China during 2004–2011. Int J Environ Res Public Health. (2017) 14:13. doi: 10.3390/ijerph14010013
25. Gao, C, Xu, J, Liu, Y, and Yang, Y. Nutrition policy and healthy China 2030 building. Eur J Clin Nutr. (2021) 75:238–46. doi: 10.1038/s41430-020-00765-6
26. Pan, W-H, Wu, H-J, Yeh, C-J, Chuang, S-Y, Chang, H-Y, Yeh, N-H, et al. Diet and health trends in Taiwan: comparison of two nutrition and health surveys from 1993-1996 and 2005-2008. Asia Pac J Clin Nutr. (2011) 20:238–50.
27. Pan, W-H, Wu, S-Y, Yeh, N-H, and Hung, S-Y. Healthy Taiwanese eating approach (TEA) toward Total wellbeing and healthy longevity. Nutrients. (2022) 14:2774. doi: 10.3390/nu14132774
28. Shabnam, N, Ashraf, MA, Laar, RA, and Ashraf, R. Increased household income improves nutrient consumption in Pakistan: a cross-sectional study. Front Nutr. (2021) 8:672754. doi: 10.3389/fnut.2021.672754.
29. Safdar, NF, Bertone-Johnson, E, Cordeiro, L, Jafar, TH, and Cohen, NL. Do dietary patterns explain high prevalence of cardiovascular risk factors among Pakistani urban adults? A cross-sectional study. BMC Nutr. (2016) 2:58. doi: 10.1186/s40795-016-0097-z
30. Hanif, MK, Fan, Y, Wang, L, Jiang, H, Li, Z, Ma, M, et al. Dietary habits of patients with coronary artery disease: a case-control study from Pakistan. Int J Environ Res Public Health. (2022) 19:8635. doi: 10.3390/ijerph19148635.
31. Badruddin, SH, Agha, A, Peermohamed, H, Rafique, G, Khan, KS, and Pappas, G. Tawana project-school nutrition program in Pakistan-its success, bottlenecks and lessons learned. Asia Pac J Clin Nutr. (2008) 17:357–60.
32. Prakash, J, Waisundara, V, and Prakash, V eds. Chapter 2 – food, nutrition, and health issues in Pakistan In: Nutritional and health aspects of food in south Asian countries : India: Academic Press (2020). 259–67.
33. Sahrai, MS, Huybrechts, I, Biessy, C, Rinaldi, S, Ferrari, P, Wasiq, AW, et al. Determinants of obesity and metabolic health in the afghan population: protocol, methodology, and preliminary results. J Epidemiol Global Health. (2022) 12:113–23. doi: 10.1007/s44197-021-00026-0
34. Lavie Carl, J, Laddu, D, Arena, R, Ortega Francisco, B, Alpert Martin, A, and Kushner, RF. Healthy weight and obesity prevention. J Am Coll Cardiol. (2018) 72:1506–31. doi: 10.1016/j.jacc.2018.08.1037
35. Wang, Y, Zhao, L, Gao, L, Pan, A, and Xue, H. Health policy and public health implications of obesity in China. Lancet Diabet Endocrinol. (2021) 9:446–61. doi: 10.1016/S2213-8587(21)00118-2
36. Pan, X-F, Wang, L, and Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabet Endocrinol. (2021) 9:373–92. doi: 10.1016/S2213-8587(21)00045-0
37. Hemmingsson, E. The unparalleled rise of obesity in China: a call to action. Int J Obes. (2021) 45:921–2. doi: 10.1038/s41366-021-00774-w
38. Guo, X, Li, Z, Zhou, Y, Yu, S, Yang, H, Sun, G, et al. The effects of transitions in metabolic health and obesity status on incident cardiovascular disease: insights from a general Chinese population. Eur J Prev Cardiol. (2021) 28:1250–8. doi: 10.1177/2047487320935550
39. Chinese Preventive Medicine Association Behavioral Health Section; Chinese Preventive Medicine Association Sports and Health Section. [Expert Consensus on Obesity Prevention and Treatment in China]. Zhonghua Liu Xing Bing Xue Za Zhi. (2022) 43(5):609–625. Chinese. doi: 10.3760/cma.j.cn112338-20220402-00253.
40. Peng, W, Zhang, J, Zhou, H, Zhang, A, Wang, Y, Tian, X, et al. Obesity intervention efforts in China and the 2022 World Obesity Day. Global Health J. (2022) 6:118–21. doi: 10.1016/j.glohj.2022.07.007
41. Laar, RA, Shi, S, Ashraf, MA, Khan, MN, Bibi, J, and Liu, Y. Impact of physical activity on challenging obesity in Pakistan: a knowledge, attitude, and practice (KAP) study. Int J Environ Res Public Health. (2020) 17:7802. doi: 10.3390/ijerph17217802
42. Tanveer, M, Hohmann, A, Roy, N, Zeba, A, Tanveer, U, and Siener, M. The current prevalence of underweight, overweight, and obesity associated with demographic factors among Pakistan school-aged children and adolescents—an empirical cross-sectional study. Int J Environ Res Public Health. (2022) 19:11619. doi: 10.3390/ijerph191811619
43. Siddiqui, M, Hameed, R, Nadeem, M, Mohammad, T, Simbak, N, Latif, A, et al. Obesity in Pakistan; current and future perceptions. J Curr Trends Biomed Eng Biosci. (2018) 17:001–4. doi: 10.19080/CTBEB.2018.17.555958
44. Imtiaz, A, ulHaq, Z, Afaq, S, Khan, MN, and Gillani, B. Prevalence and patterns of physical activity among school aged adolescents in Pakistan: a systematic review and meta-analysis. Int J Adolesc Youth. (2020) 25:1036–57. doi: 10.1080/02673843.2020.1831559
45. Maki, KC, Dicklin, MR, and Kirkpatrick, CF. Saturated fats and cardiovascular health: current evidence and controversies. J Clin Lipidol. (2021) 15:765–72. doi: 10.1016/j.jacl.2021.09.049.
46. Kubota, Y, Evenson, KR, Maclehose, RF, Roetker, NS, Joshu, CE, and Folsom, AR. Physical activity and lifetime risk of cardiovascular disease and cancer. Med Sci Sports Exerc. (2017) 49:1599–605. doi: 10.1249/mss.0000000000001274.
47. Alwan, A, McColl, K, and Al-Jawaldeh, A, World Health Organization. Proposed policy priorities for preventing obesity and diabetes in the Eastern Mediterranean Region. Geneva: World Health Organization (2017).
48. Sherin, A. Obesity: how to prevent Pakistani people from getting heavier? Khyber Med Univ J. (2014) 5:59–60.
49. Miller, V, Webb, P, Cudhea, F, Shi, P, Zhang, J, Reedy, J, et al. Global dietary quality in 185 countries from 1990 to 2018 show wide differences by nation, age, education, and urbanicity. Nat Food. (2022) 3:694–702. doi: 10.1038/s43016-022-00594-9
50. Mu, L, Liu, J, Zhou, G, Wu, C, Chen, B, Lu, Y, et al. Obesity prevalence and risks among Chinese adults: findings from the China PEACE million persons project, 2014–2018. Circ Cardiovasc Qual Outcomes. (2021) 14:e007292. doi: 10.1161/circoutcomes.120.007292.
51. Mendelsohn, ME, and Karas, RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. (1999) 340:1801–11. doi: 10.1056/NEJM199906103402306
52. Xie, J, Wu, EQ, Zheng, Z-J, Sullivan, PW, Zhan, L, and Labarthe, DR. Patient-reported health status in coronary heart disease in the United States: age, sex, racial, and ethnic differences. Circulation. (2008) 118:491–7. doi: 10.1161/CIRCULATIONAHA.107.752006
53. Bots, SH, Peters, SA, and Woodward, M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. BMJ Glob Health. (2017) 2:e000298. doi: 10.1136/bmjgh-2017-000298
54. Rodgers, JL, Jones, J, Bolleddu, SI, Vanthenapalli, S, Rodgers, LE, Shah, K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. (2019) 6:19. doi: 10.3390/jcdd6020019.
55. Yazdanyar, A, and Newman, AB. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. (2009) 25:563–77. doi: 10.1016/j.cger.2009.07.007
56. Ma, S, Xi, B, Yang, L, Sun, J, Zhao, M, and Bovet, P. Trends in the prevalence of overweight, obesity, and abdominal obesity among Chinese adults between 1993 and 2015. Int J Obes. (2021) 45:427–37. doi: 10.1038/s41366-020-00698-x
57. Kurji, Z, Premani, ZS, and Mithani, Y. Analysis of the health care system of Pakistan: lessons learnt and way forward. J Ayub Med Coll Abbottabad. (2016) 28:601–4.
59. Cui, J, Guo, X, Yuan, X, Wu, H, Yu, G, Li, B, et al. Analysis of rheumatic heart disease mortality in the Chinese population: A JoinPoint and age-period-cohort study. Int J Environ Res Public Health. (2022) 19:9872. doi: 10.3390/ijerph19169872
60. Zhao, D, Liu, J, Wang, M, Zhang, X, and Zhou, M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. (2019) 16:203–12. doi: 10.1038/s41569-018-0119-4
61. Chen, F, Zhang, Y, Chen, S, Si, A, and Hu, W. Cardiovascular disease mortality attributable to low whole-grain intake in CHINA: an age-period-cohort and Joinpoint analysis. Int J Environ Res Public Health. (2022) 19:7096. doi: 10.3390/ijerph19127096
62. Cao, J, Eshak, ES, Liu, K, Gero, K, Liu, Z, and Yu, C. Age-period-cohort analysis of stroke mortality attributable to high sodium intake in China and Japan: GBD data 1990 to 2016. Stroke. (2019) 50:1648–54. doi: 10.1161/STROKEAHA.118.024617
63. Afshin, A, Sur, PJ, Fay, KA, Cornaby, L, Ferrara, G, Salama, JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
Keywords: cardiovascular diseases, mortality, dietary risks, high body mass index, nursing care, China, Pakistan
Citation: Yan W, Yan X, Mubarik S and Nawsherwan (2023) Epidemiological trend and age-period-cohort effects on cardiovascular disease mortality and disability-adjusted life years attributable to dietary risks and high body mass index at the regional and country level across China and Pakistan. Front. Nutr. 10:1158769. doi: 10.3389/fnut.2023.1158769
Edited by:
Iain Brownlee, Northumbria University, United KingdomReviewed by:
Muhammad Fawad, Zhejiang University, ChinaAbbas Khan, Lahore College for Women University, Pakistan
Copyright © 2023 Yan, Yan, Mubarik and Nawsherwan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuzhen Yan, Mzc4NzY3MDE0QHFxLmNvbQ==; Nawsherwan, bmF3c2hlcm1rZDE3N0BnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 Wu Yan1†
Wu Yan1† Xiuzhen Yan
Xiuzhen Yan Nawsherwan
Nawsherwan