
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 02 May 2023
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1151498
This article is part of the Research TopicFood Literacy and Healthy Diets in Childhood and AdolescenceView all 12 articles
 Maha Hoteit1,2*†
Maha Hoteit1,2*† Rania Mansour3*
Rania Mansour3* Hala Mohsen2†
Hala Mohsen2† Khlood Bookari4,5
Khlood Bookari4,5 Fadwa Hammouh6
Fadwa Hammouh6 Sabika Allehdan7
Sabika Allehdan7 Dalal AlKazemi8
Dalal AlKazemi8 Haleama Al Sabbah9
Haleama Al Sabbah9 Hasnae Benkirane10
Hasnae Benkirane10 Iman Kamel11
Iman Kamel11 Radwan Qasrawi12,13
Radwan Qasrawi12,13 Reema Tayyem14 and the regional food literacy group
Reema Tayyem14 and the regional food literacy groupBackground: Food literacy is capturing the attention worldwide and gaining traction in the Arab countries. Strengthening food and nutrition literacy among Arab teenagers are important promising empowering tools which can protect them from malnutrition. This study aims to assess the nutrition literacy status of adolescents with the food literacy of their parents in 10 Arab countries.
Methods: This cross-sectional study involving a convenient sample of 5,401 adolescent-parent dyads (adolescents: mean age ± SD: 15.9 ± 3.0, females: 46.8%; parents: mean age ± SD: 45.0 ± 9.1, mothers: 67.8%) was launched between 29 April and 6 June 2022 in 10 Arab nations. The Adolescent Nutrition Literacy Scale (ANLS) and the Short Food Literacy Questionnaire (SFLQ) were used to meet the study aims.
Results: More than one-quarter (28%) of adolescents had poor nutrition literacy, with 60% of their parents being food illiterate. The top three countries with nutritionally” less literate” adolescents were Qatar (44%), Lebanon (37.4%), and Saudi Arabia (34.9%). Adolescents’ age, gender, education level, primary caregivers, employment status, and the inclusion of nutrition education in the schools’ curriculum predicted the nutrition literacy levels of Arab adolescents. Besides, parental weight status, health status, parent’s food literacy level, and the number of children per household were significant determinants too. Adolescents studying at a university and having parents with adequate food literacy had the highest odds of being nutritionally literate (OR = 4.5, CI = 1.8–11.5, p = 0.001, OR = 1.8, CI = 1.6–2.1, p < 0.001, respectively).
Conclusion: Nutrition literacy inadequacy among Arab adolescents is a prioritized challenge to be tackled.
Malnutrition still rears its ugly head in many Arab countries, proposing that it is tremendously difficult for the region to meet the 2030 Agenda for Sustainable Development to reach “zero hunger” and eradicate all forms of malnutrition (1). High levels of food insecurity, malnutrition, and obesity is found in the Arab region, with 116 million people being food insecure, 43 million undernourished, and 115 million obese (2). Nonetheless, major inconsistencies among sub-regions do exist. Obesity is more prevalent in Gulf Cooperation Council (GCC); however, undernourishment is more of an issue in the least developed countries (LDCs) and Countries in Conflict (CICs) (3). Recent investigations show that the number of malnourished people in the Arab world increased from 4.8 million to 69 million between 2019 and 2020, accounting for nearly 16% of the population (4). In addition, the Eastern Mediterranean Region (EMR) is charaterized by its diversity into two main groups based on their Gross National Income (GNI): the oil producing high income countries and the low and medium income countries. Both countries are among the world’s most vulneable to the dire impacts of climate change. The EMR suffers from extreme fluctuations in tempratures and precipitation as well as natural water and agricultural land scracity (5). It is predicted that these patterns will worsen in the coming years, with climate change, with intense pressure on agriculture thus compounding the effect of climate change with addditional significant challenges to livelihoods and food security (5). A functional food systems literacy is therefore required to aid people in communicating and collaborating on food system problems, including food insecurity, within dynamic learning approach addressed mainly to resolve the threats induced by the “nutrition transition” phenomena in the EMR. For instance, due to the “nutrition transition,” adolescent obesity has reached a critical level in the Arab countries (6). Ensuring resilient food systems in the Arab world is challenging amidst the overwhelmed population growth, dwindling natural resources, and import dependency (7). Further, the COVID-19 crisis revealed how unprepared the region was to respond appropriately to the pandemic with food supply chains varying in complexity and vulnerable to disruption amongst sub-regions (8). Given these constraints, a multisector approach considering each policy’s situation in the larger food environment and supply chain is required. Arab countries must invest in sectors having long-lasting effects, particularly education. In other words, equipping Arab people with sufficient nutrition knowledge could help meet a range of sustainable nutrition goals. Nutrition education works best in unique intervention points in the life cycle, particularly throughout adolescence (9). Adolescence, a period of life ranging from 10-to 19 years old (10), is an ideal time to plan, apply, and monitor nutrition interventions. Inadequate nutrition in adolescence can potentially retard growth and sexual maturation and displaces adolescents at high risk of developing chronic diseases (11). Referring to the Nutbeams’ model in “health literacy,” (12) two emerging concepts, “food literacy” and the “nutrition literacy,” have grabbed the researchers’ attention since 1990, who provided plenty of definitions for these two terms. Food literacy is beyond nutrition knowledge; it includes skills, and behaviors, from knowing where food comes from to the ability to select and prepare these foods appropriately (13). On the other hand, nutrition literacy is the ability of individuals to obtain, process, and understand the basic nutrition information they need to make appropriate nutrition decisions (14). The latter has been linked to improved diet quality, nutrient adequacy, food label reading, and food security (15–17). Upon this, Arab school is an ideal destination for creating synergies to contribute to sustainable development by offering a unique chance for the formal education system to improve students’ nutrition literacy (18). All school-based activities advocating healthy eating, not only those held in the classroom, are part of an extended nutrition education curriculum known as a “macro-curriculum” (19). To date, the number of studies on adolescent nutrition literacy in the Arab world is limited. Therefore, we conducted this study to be the first to evaluate the nutrition literacy status of adolescents with the food literacy of their parents in ten Arab countries. The hypothesis anticipated in this study is that Arab adolescents express low levels of nutrition literacy, stressing the need to reach a regional consensus to integrate nutrition education into Arab schools’ curricula.
A cross-sectional study using the snowball sampling method was conducted in Lebanon and nine other Arab nations: Bahrain, Egypt, Jordan, Kuwait, Morocco, Palestine, Qatar, Saudi Arabia, and United Arab Emirates (UAE). A self-administered questionnaire (82 items)1 was disseminated to be completed by eligible adolescent-parents’ dyads and kept open between 29 April and 6 June 2022. Calls for participation were performed via social network platforms and the research teams’ networks. In each country, a convenient sample of parent’s-adolescents dyads were collected. Research assistants were sending the links for eligible participants, based on the following eligibility criteria: (i) the adolescent is between 10 and 19 years old; (ii) either parent/caregiver (age more than 18 to 85 years old); (iii) having nationality of the mentioned ten countries; and consenting to participate. Besides, we aimed to reach only one adolescent per household. Overall, 5,401 adolescent-parents’ dyads completed the survey and their data were considered for analysis.
The explanatory variables were as the follows: (i) demographic and socio-economic status of adolescents (age, gender, country of nationality, education level, working status, primary caregiver, parental education level, self-reported body weight and height), and whether nutrition education is a part of school’s curriculum; (ii) demographic and socio-economic status of parents (age, gender, country of nationality, marital status, education level, spouse’s education level, job type, number of co-residents per household excluding newborns, number of rooms excluding the kitchen and bathrooms, number of children, self-reported body weight and height, and health status). The body mass index (BMI) was calculated and evaluated per WHO recommendations (20).
The Adolescent Nutrition Literacy Scale (ANLS), developed by Bari (21), was used to assess adolescents’ nutrition literacy. It compromised of 22 items under three sub-sections: Functional Nutrition Literacy (FNL) (7 items); Interactive Nutrition Literacy (INL) (6 items); Critical Nutrition Literacy (CNL) (9 items). Each item has a score range of 1–5. The scoring criteria is as the follows:
Total Nutrition Literacy (TNL): the sum of FNL, INL, and CNL (minimum-maximum score: 22–110; ≥ 66 is an average score).
FNL (questions 1–7): minimum-maximum score: 7–35 (≥ 21 is an average score).
INL (questions 8–13): minimum-maximum score: 6–30 (≥ 18 is an average score).
CNL (questions 14–22): minimum-maximum score: 9–45 (≥ 27 is an average score).
Parental food literacy was evaluated using the Short Food Literacy Questionnaire (SFLQ), developed by Gréa Krause et al. (22). It consists of 12 items (score range: 7 to 52; average score ≥ 36), representing the functional (6 items), interactive (2 items), and critical (4 items) food literacy dimensions.
The study was performed based on the ethical standards laid down in the Helsinki Declaration. We obtained written approval from the Ethics Committee of Al Zahraa University Medical Center (ZhU#17, 2022), Beirut, Lebanon, and the universities from all participating countries. A consent form was added to the survey, informing participants about their, rights and confidentiality. The participation was entirely voluntary with no obligation to do so.
We performed the statistical analysis using the Statistical Package of Social Sciences Software (SPSS) (Version 25.0. IBM Corp: Armonk, NY, USA). A “weighting” variable was created to adjust the representation of the sampled population. Respondents’ characteristics were presented as frequencies (percentages) for categorical variables, while means ± standard deviation (SD) for continuous variables. The adolescence stages were classified as follows: early adolescence (10–13 years old), middle adolescence (14–16 years old), and late adolescence (17–19 years old). The normality of data was checked using the Shapiro–Wilk test. Due to the non-normal distribution, Kruskal-Wallis test was used to determine score differences according to country. Chi-squared test (χ2) was used to determine associations between study variables. In addition, the binary backward stepwise regression was used to examine the predictors of adolescents’ nutrition literacy. A value of p of 5% was considered significant.
A total of 5,401 adolescent-parent dyads participated in this study. Table 1 shows the general characteristics of participants. Regarding the nationality, 11% were from Lebanon, 9.4% from Bahrain, 12.2% from Egypt, 10.4% from Jordan, 8.9% from Kuwait, 10.9% from Morocco, 9.6% from Palestine, 10.2% from Qatar, 9.1% from Saudi Arabia, and 8.3% from UAE.
Among adolescents, 53.2% were males. The mean age ± SD of the adolescents was 15.9 ± 3.0. Moreover, 51% were in the late adolescence stage, whereas the remaining were either in the early (25%) or the middle (24%) adolescence stage, p < 0.001. Around 65% were of normal weight, 27% were overweight, 5% were underweight, and 3% were obese. In addition, 68.5 and 31% were school and university students, respectively. Also, 86% of the adolescents reported both parents as primary caregivers. Around 11.5% were currently working. About 76% were not receiving nutrition education as a part of their schools’ curriculum (Table 1). The highest proportion of adolescents who reported not receiving nutrition education was from Morocco (98%), followed by Lebanon (85%) andKuwait (85%), (Figure 1). Furthermore, 81% of adolescents attending public schools reported not receiving nutrition education, in contrast to 67% of those who were private school students, p < 0.001 (Figure 1).
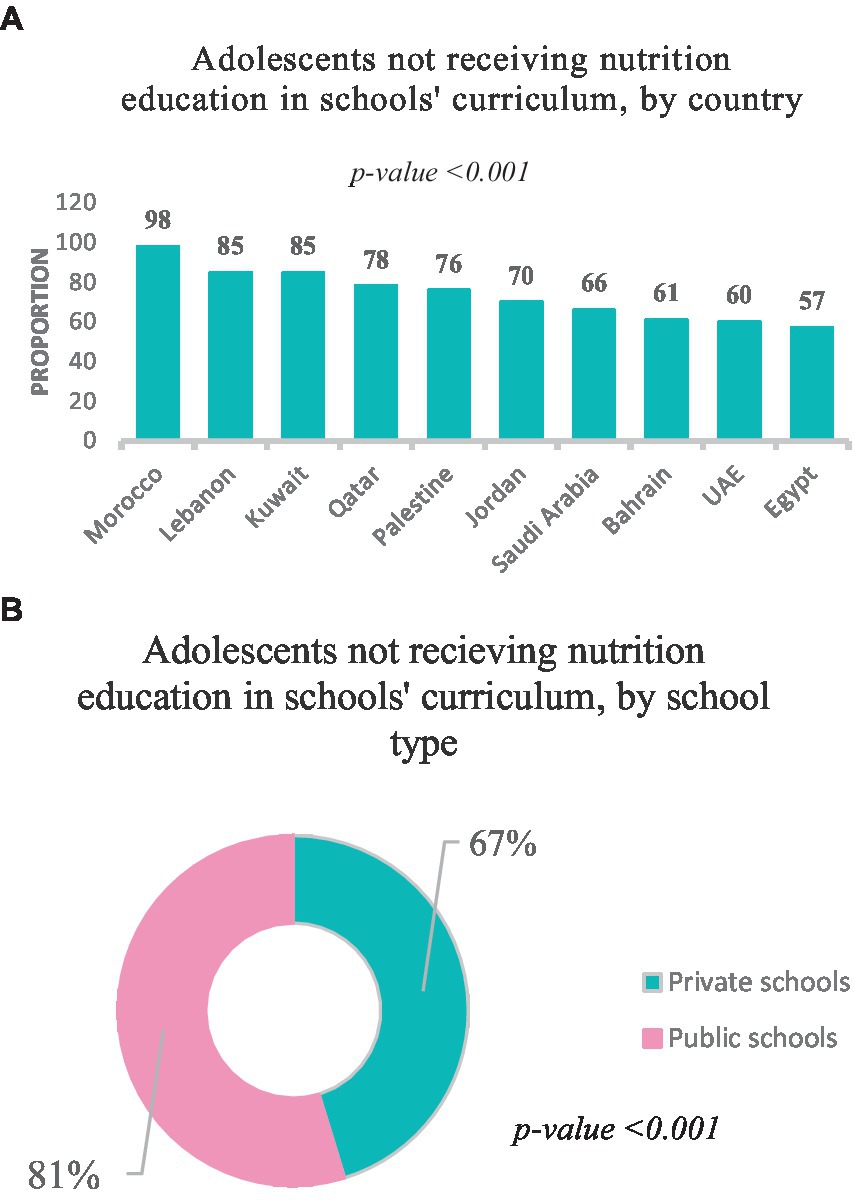
Figure 1. (A) Adolescents not receiving nutrition education in schools’ curriculum, by country (n = 3,699 school attendees). (B) Adolescents not receiving nutrition education in schools’ curriculum, by school type (n = 3,699 school attendees).
As for the parent participants, 67.8% were mothers with a mean age ± SD of 43.0 ± 8.0. More than third of parents were overweight (fathers: 38.5%; mothers: 38.2%, p < 0.001). where39% of parents had no job, and half of themhad health problems (Table 1).
In the overall adolescent population, the mean TNL score was 70.6 ± 9.5, with poor nutrition literacy was found in 28% of adolescents. The FNL, INL, and CNL scores were as follows: 22.7 ± 7, 18.5 ± 5.8, and 29.5 ± 4.6, respectively. Hence, 4 out of 10 adolescents (36%) were with poor FNL and INL, and 21% were with poor CNL (Table 2).
As per country, Qatar and Lebanon showed the highest proportions of adolescents with poor TNL (44 and 37.4%, respectively), followed by Saudi Arabia (35%), Bahrain (29.4%), Kuwait (28%), Palestine (25%), Morocco (24%), Jordan (23%), UAE (18.2%), and Egypt (18.1%), p < 0.001 (Figure 2). Half the Egyptian adolescents (49.6%) were with poor FNL, followed by Qatari (41.7%) and Lebanese (39.4%) adolescents, p < 0.001 (Table 3). Adolescents participants with poor INL were mostly from Qatar (51%), followed by Lebanon (46%) and Bahrain (44.2%), p < 0.001 (Table 3). Similarly, around 3 out of 10 Saudi adolescents (29.4%) showed poor CNL, followed by Bahrain (24.2%) and Qatar (23.8%) p < 0.001 (Table 3). Regarding parents’ food literacy, an overall mean score of 32.8 ± 8.5 was reported, with 60% of parents were found with poor food literacy. Parents from Morocco (77%), Lebanon (71%), and Saudi Arabia (64%) were mostly food illiterate, followed by Qatar (59%), Jordan (58.7%), Palestine (55.3%), Kuwait (54.6%), UAE (52%), Bahrain (45.2%), and Egypt (42.7%), p < 0.001 (Table 3).
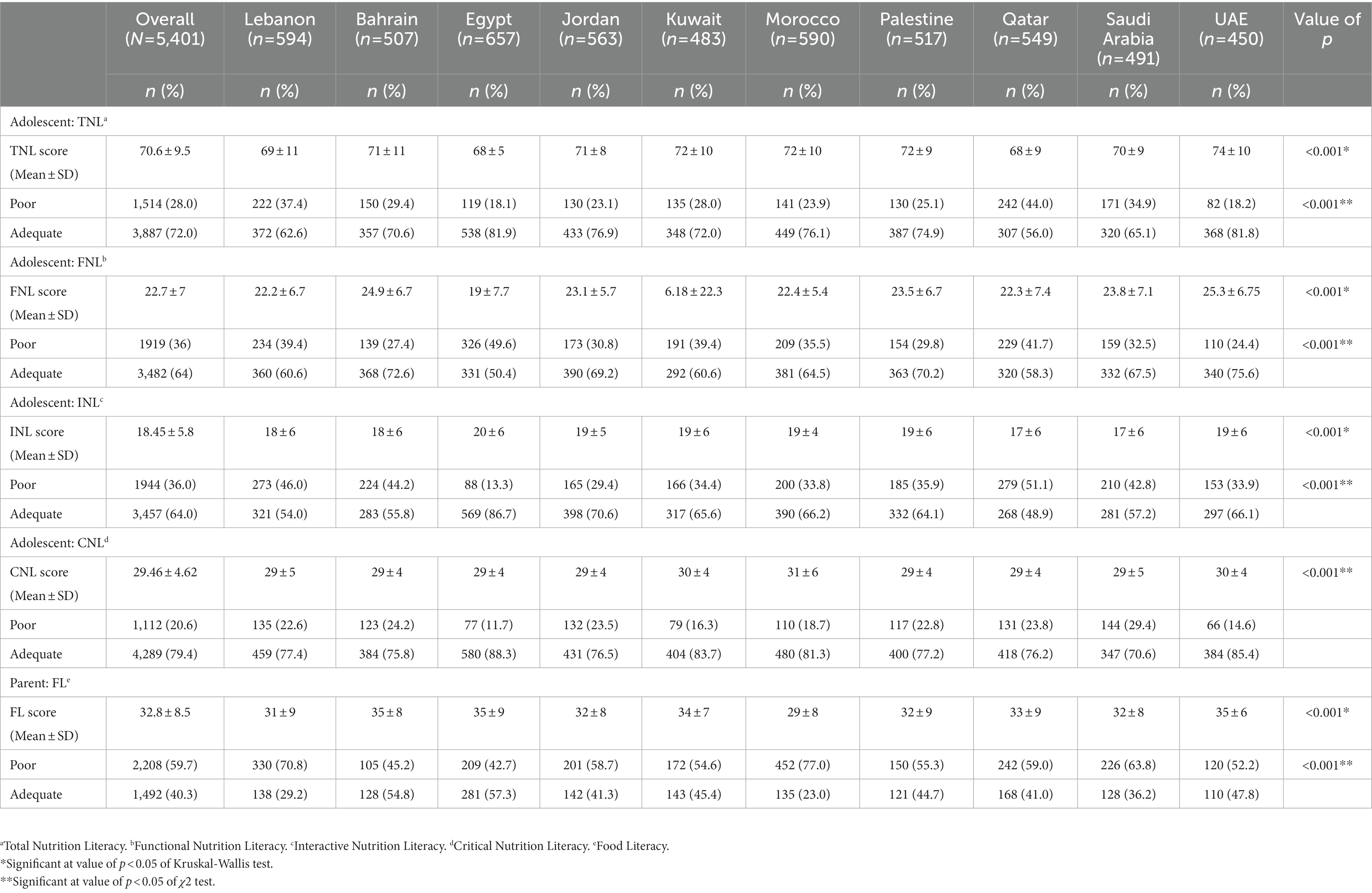
Table 3. The level of adolescents’ nutrition literacy and the food literacy of their parents, overall and by country.
Supplementary Table S1 shows the determinants of adolescents’ nutrition literacy. Most older adolescents (77.6%) had adequate TNL, compared to 63.6 and 68.2% of those in the young and middle stages respectively, p < 0.001. Similarly, FNL, INL, and CNL, were adequate among older adolescents compared to young and middle stage adolescents (72.5, 66.5, and 80%, respectively, all value of ps <0.001). In terms of adolescents’ gender, poor nutrition literacy was found significantly more among males compared to females; TNL (32.2% vs. 23.5%, p < 0.001), FNL (40.3% vs., 30.3%, p < 0.001), and INL (37.8% vs. 34%, p = 0.003), respectively. Poor nutrition literacy was also found more among obese adolescents; TNL (35.4%), FNL (43%), and INL (41.3%), although these findings were not significant (p = 0.17, p = 0.09, and p = 0.06, respectively). Parents who were underweight and with obesity had more adolescents with poor TNL (38 and 31.6%, respectively), compared to normal-weight and overweight parents (26.7 and 26.5%, respectively) p < 0.001. Further, it was noted that nearly half the obese parents (41.2%) had adolescent with poor FNL, p < 0.001. On the other hand, adequate level of nutrition literacy scores was found more among adolescents studying at university, with TNL (81%, p < 0.001), FNL (75%, p < 0.001), INL (68.7%, p < 0.001), and CNL (81%, p = 0.002), compared to those at school level (67.8, 59.5, 62, and 78.8%, respectively), and those not attending a school or university (50, 66.7%. 47.4, and 52.6%, respectively) (Supplementary Table S1).
Mothers with university degree had predominately adolescent with adequate INL (67%, p < 0.001) and CNL (81.6%, p < 0.001). Similarly, adolescents of fathers having university degree showed adequate TNL (72.2%, p = 0.012), FNL (63.5%, p = 0.008), INL (67%, p < 0.001), and CNL (80.4%, p < 0.001). In addition, adolescents having both parents as primary caregivers expressed adequate TNL (68.6%, p < 0.001), INL (58.8%, p = 0.03), and CNL (61.3%, p < 0.001). Moreover, working adolescents had predominately adequate TNL (79.8% vs. 70.8%, p < 0.001) and FNL (68.4% vs. 61.6%, p = 0.03), compared to non-workers. However, the school type was not a significant correlate except in the FNL, with adolescents in private schools scoring better in FNL compared to those in public schools (66% vs. 64.3%, p < 0.001). Adolescents receiving nutrition education showed significantly better TNL and INL in contrast to others who did not report so (73.6% vs. 65.9%, p < 0.001) and (68.5% vs. 59.8%, p < 0.001), respectively. Most married parents had adolescent with adequate TNL (68.6%, p < 0.001), INL (61.5%, p < 0.001), and CNL (79.4%, p < 0.001). Moreover, parents having 2–3 children had a higher proportion of adolescent with adequate TNL (69.4%, p = 0.015), INL (65%, p < 0.001), and CNL (82%, p < 0.001). Around 36% of parents with reported disease (vs. 18% healthy) had adolescent with poor TNL, p = 0.017. As well, a higher proportion of food illiterate parents (vs. food literate) had adolescent who were nutritionally illiterate too, in TNL (36.6% vs. 25.8%, p < 0.001) INL (45.2% vs. 27.5%, p < 0.001) and CNL (25.3% vs. 15%, p < 0.001) dimensions (Supplementary Table S1).
Table 4 shows the significant predictors of adolescents’ nutrition literacy. Older adolescents (vs. younger adolescents) were 1.6 times (OR = 1.6, CI = 1.4–1.9, p < 0.001) more likely to be nutritionally literate. Female adolescents had a 30% more probability of having adequate nutrition literacy (vs. males OR = 0.7, CI = 0.6–0.8, p < 0.001). Besides, adolescents who were university students (OR = 4.5, CI = 1.8–11.5, p = 0.001) were 4.5 times more likely to be nutritionally literate. Adolescents with parents who were either overweight or obese were 1.5 times more likely to be with adequate nutrition literacy (OR = 1.5, CI = 1.0–2.2, p = 0.04). Further, adolescents with both parents as primary caregivers (vs. either parent and others, OR = 0.7, C I = 0.6–0.8, p < 0.001, and OR = 0.7, CI = 0.5–1, p = 0.03, respectively) were 30, and 60% (vs. living alone, OR = 0.4, CI = 0.1, 1.1, p = 0.001) more likely to be nutritionally literate. Furthermore, working adolescents were 1.5 times more likely to have adequate nutrition literacy (OR = 1.5, CI = 1.2–1.8, 0.001). Parents with one child (vs. ≥ 3 children) were 30% more likely to be with adequate nutrition literacy (OR = 0.7, CI = 0.5–0.9, p < 0.001). Adolescents receiving nutrition education were 30% more likely to be nutritionally literate (OR = 1.3, CI = 1.1–1.5, p = 0.01). Parents who reported to be healthy were 20% more likely to have adolescent who are nutritionally literate (OR = 1.2, CI = 1.0–1.4, p = 0.01). In addition, food literate parents were 2 times more likely to have nutritionally literate adolescent (OR = 1.8, CI = 1.6–2.1, p < 0.001) (Table 4).
This study assessed the Arab adolescents’ nutrition literacy and the food literacy of their parents. About 28% of adolescents had poor nutrition literacy, with 60% of their parents being food “less literate.” Nutrition illiteracy was most prevalent in Qatar (44%), Lebanon (37.4%), and Saudi Arabia (34.9%). Adolescents’ age, gender, education level, primary caregiving, employment status, and receiving nutrition education in schools predicted their nutrition literacy levels. Besides, parental weight status, health status, parent food literacy level, and the number of children per household were significant determinants.
There is scarcity of studies evaluating nutrition literacy among the Arab population. All in all, only three studies on this topic were conducted and were chiefly in Lebanon and Palestine (16, 23, 24). Our study findings are in concordance with that previously reported in Lebanon which highlight inadequate nutrition literacy status among adolescents (23), but in high contrast to that observed among Palestinian adults (75% were nutritionally illiterate) (24). Apart from the Arab region, our observed mean score ± SD of nutrition literacy (70.6 ± 9.5) is quite close to that reported among a study in China (61.7 ± 14.37) (25) and 3 studies in Turkey (67.6 ± 7.9; 72.3 ± 8.2; 70.31 ± 8.6) (17, 26, 27). In the present study, Qatari adolescents pose an added risk of nutrition illiteracy (44%). A review of studies in Qatar shows that the high gross domestic product has led to the adoption of western lifestyles in the country, promoting childhood overweight and obesity (28). Besides, the highest levels of obesity among Arab countries were observed in Bahrain, Kuwait, Qatar, and UAE (29). Nutrition literacy is a critical influencing factor of obesity, with a higher literacy level associated with appropriate dietary habits and food-related behaviors (30). Lebanon, on the other hand, ranked second in the present study for adolescent nutrition illiteracy. Between 1997 and 2009, significant changes were observed in the diet of the Lebanese population, with high intakes of salty snacks, added fats, and oils (31). This dietary transition, along with the increase in sedentary behaviors, poor nutrition knowledge, and the economic collapse, has put Lebanon at risk of further constraints in terms of malnutrition prevalence (31). In this context, our study shows that 75.6% of adolescents do not receive nutrition education in schools. Further, nutrition education was mostly provided for Egyptian adolescents who were mostly nutritionally literate. Hence, the latter finding reemphasize the relevance of nutrition education in improving students’ nutrition literacy. In this regard, several school-based nutrition education programs have shown effectiveness in promoting nutrition knowledge, healthy dietary habits, and self-efficacy among students (32–35). Therefore, such interventions are indispensable in the Arab region where malnutrition prevalence is of mounting concern. In addition to classroom approaches, farm-to-school programs, school gardens, and cooking programs might be also prioritized (19). In this study, adolescents of older age reported better nutrition literacy levels than younger ones. Variations in nutrition literacy levels among adolescence age could be due to increased exposure to and interest in health-related information with advancing age (36). Furtherly, female adolescents were more nutritionally literate than males. This is consistent with data from Turkey (17, 27) and Iran (15, 37). One possible explanation for gender disparities is that females focus on the nutritional value of food and prioritize healthy eating more than men (38). Women have better nutrition knowledge, and recognize nutrition as a critical contributor to their conception of health (39). Furthermore, higher education levels determined better adolescents’ nutrition literacy in our study, which is consistent with data from China (25) and Italy (40). Individuals with the highest education level have a better ability to understand, process, and apply nutrition information. Our findings also showed that working adolescents had better nutrition literacy than their counterparts. We believe that adolescent workers are most likely employed in surroundings that promote health and nutrition. In addition, adolescents having both parents as primary caregivers had the most adequate nutrition literacy, which goes hand in hand with findings from China (25). Above all, obese and overweight parents had more nutritionally illiterate adolescent than their counterparts. Obesity among parents might drive their children to attain more nutrition information to help them change their dietary habits and lose or maintain body weight. Diseased parents in the current study had mostly nutritionally illiterate adolescent. These findings suggest that the occurrence of nutrition-related diseases among parents, which usually correlates with unhealthy diets and lack nutrition knowledge, may negatively affect their children’s nutrition literacy. Moreover, food literate parents had mostly nutritionally literate adolescent. This finding is supported by those reported in Greece (41) and the United States (42), where parental nutrition literacy was positively correlated with healthy parental feeding practices (PFP), and child Healthy Eating Index (HEI). Food literate parents are more likely to engage their children in nutrition communication and expose them to reliable information sources about nutrition from professionals (43). Our data may be useful reference for policymakers and curriculum developers to assess education and develop practical learning and teaching strategies to improve student’s food and nutrition literacy as indicated in a recent systematic review (44).
The current study had some limitations that should be acknowledged. First, due to the unavailability of valid questionnaires regarding nutrition and food literacy in the region, the questionnaires in this study were derived from many credible, valid sources and translated to Arabic then back translated to English by experts. Second, due to its cross-sectional design, causal inferences cannot be drawn. Third, the self-administered questionnaire causes inevitable information bias. Fourth, convenience sampling could lead to skewed sample characteristics. Fifth, we collected no information on adolescents’ food habits which most probably correlate with nutrition literacy. Nonetheless, this study is the first of the region’s kind, with a large sample of Arab adolescents and their parents addressing the nutrition and food literacy topics.
This study shows that nutrition literacy inadequacy among Arab adolescents is a prioritized challenge to be addressed. The “macro-curriculum” concept in schools includes intervention packages to implement, leading to the best possible nutrition outcomes. The target group for interventions includes school-age children, teachers at both public and private institutions, as well as the ministries of education and health in each Arab nation. Classroom activities, such as counting with pictures of fruits and vegetables, learning about cultural food traditions, and measuring ingredients for a recipe, could be included in school interventions. Additionally, schools can send daily messages with nutrition content, such as morning announcements, to other family members. Staff meetings, parent-teacher interviews, and home cooking activities are also things to be considered.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Al Zahraa University Medical Center (ZhU#17, 2022), Beirut, Lebanon, and the universities from all participating countries. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Bahrain: Tariq Abdulkarim Alalwan; Palestine: Malak Amro; Qatar: Aljazi AlQahtani; United Arab Emirates: Leila Cheikh Ismail.
MH: conceptualization, validation, and project administration. HM, KB, FH, SA, DA, HA, HB, IK, RQ, and RT: methodology. RQ: software. HM: formal analysis. MH and HM: data curation and writing—original draft preparation. All authors: writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Open access funding provided by the Qatar National Library.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1151498/full#supplementary-material
1. United Nations International Children’s Emergency Fund (UNICEF). Hunger and malnutrition in the Arab region stand in the way of achieving zero hunger by 2030. (2021). Available at: https://www.unicef.org/mena/press-releases/hunger-and-malnutrition-arab-region-stand-way-achieving-zero-hunger-2030-un-report (Accessed on 2 June, 2022).
2. Food and Agricultural Organization (FAO), International Fund for Agricultural development (IFAD), United Nations International Children’s Emergency Fund (UNICEF), World Food Program (WFP), World Health Organization (WHO), & Economic, Social Commission for Western Asia (ESCWA). Near east and North Africa regional overview of food security and nutrition 2020: Enhancing resilience of food Systems in the Arab States. (2021). Available at:. https://reliefweb.int/report/world/near-east-and-north-africa-regional-overview-food-security-and-nutrition-2020-enhancing (Accessed on 17 June, 2022).
3. Economic and Social Commission for Western Asia (ESCWA) and Food and Agricultural Organization (FAO). (2021). Arab food security: Vulnerabilities and pathways - Lebanon. Available at: https://reliefweb.int/report/lebanon/arab-food-security-vulnerabilities-and-pathways (Accessed on 2 June, 2022).
4. Agence France-Presse (AFP). A third of people in 420m-strong Arab world do not have enough to eat Arab News (2021). Available at: https://www.arabnews.com/node/1988326/middle-east (Accessed June 17, 2022).
5. Al-Jawaldeh, A, Nabhani, M, Taktouk, M, and Nasreddine, L. Climate change and nutrition: implications for the eastern Mediterranean region. Int J Environ Res Public Health. (2022) 19:17086. doi: 10.3390/ijerph192417086
6. Musaiger, AO, Al-Mannai, M, Al-Lalla, O, Saghir, S, Halahleh, I, Benhamed, MM, et al. Obesity among adolescents in five Arab countries; relative to gender and age. Nutric. Hospit. (2013) 28:1922–5.doi: 10.3305/nh.2013.28.6.6412
7. Economic and Social Commission for Western Asia (ESCWA). Tracking food security in the Arab region. (2019). Available at: https://www.unescwa.org/publications/tracking-food-security-arab-region (Accessed on 2 June, 2022).
8. Hoteit, M, Mortada, H, Al-Jawaldeh, A, Yazbeck, B, AlKhalaf, M, Bookari, K, et al. Dietary diversity in the eastern Mediterranean region before and during the COVID-19 pandemic: disparities, challenges, and mitigation measures. Front Nutr. (2022) 9:813154. doi: 10.3389/fnut.2022.813154
9. Mangal, A, Raikar, K, Thakur, A, Vaghela, JF, Banerjee, S, and Gupta, V. A study to assess the effectiveness of a nutrition education session using flipchart among school-going adolescent girls. J. Educat. Health Promot. (2020) 9:183. doi: 10.4103/jehp.jehp_258_18
10. World Health Organization. Regional Office for South-East Asia. Adolescent health at a glance in South-East Asia region, 2007: Fact sheet WHO Regional Office for South-East Asia (2007). Available at: https://apps.who.int/iris/handle/10665/204750 (Accessed on 24 January, 2022).
11. World Health Organization. Nutrition in adolescence – Issues and challenges for the health sector: Issues in adolescent health and development. (2005). Available at: https://apps.who.int/iris/bitstream/handle/10665/43342/9241593660_eng.pdf;sequence=1 (Accessed on 15 June, 2022).
12. Nutbeam, D. The evolving concept of health literacy. Soc Sci Med. (2008) 67:2072–8. doi: 10.1016/j.socscimed.2008.09.050
13. Vaitkeviciute, R, Ball, LE, and Harris, N. The relationship between food literacy and dietary intake in adolescents: a systematic review. Public Health Nutr. (2014) 18:649–58. doi: 10.1017/s1368980014000962
14. Silk, KJ, Sherry, J, Winn, B, Keesecker, N, Horodynski, MA, and Sayir, A. Increasing nutrition literacy: testing the effectiveness of print, web site, and game modalities. J Nutr Educ Behav. (2008) 40:3–10. doi: 10.1016/j.jneb.2007.08.012
15. Doustmohammadian, A, Omidvar, N, Keshavarz-Mohammadi, N, Eini-Zinab, H, Amini, M, Abdollahi, M, et al. Low food and nutrition literacy (FNLIT): a barrier to dietary diversity and nutrient adequacy in school age children. BMC Res Notes. (2020) 13:286. doi: 10.1186/s13104-020-05123-0
16. Tell, M. A., Natour, N., Badrasawi, M., and Shawish, E. The relationship between nutrition literacy and nutrition information seeking attitudes and healthy eating patterns in the Palestinian society. (2021). Available at: https://www.researchsquare.com/article/rs-923058/v1
17. Koca, B, and Arkan, G. The relationship between adolescents’ nutrition literacy and food habits, and affecting factors. Public Health Nutr. (2020) 24:1–12. doi: 10.1017/s1368980020001494
18. United Nations Educational, Scientific and Cultural Organization (UNESCO). Health and Education Resource Centre. School health and nutrition (2018). Available at: https://healtheducationresources.unesco.org/taxonomy/term/2602?pg=15 (Accessed on 2 June, 2022).
19. United Nations Standing Committee on Nutrition (UNSCN). Schools as a system to improve nutrition. A new statement for school-based food and nutrition interventions. (2017). Available at: https://www.unscn.org/uploads/web/news/document/School-Paper-EN-WEB-nov2017.pdf (Accessed on 15 May, 2022).
20. World Health Organization (WHO). Body mass index (BMI). (2022). Available at: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (Accessed on 17 June, 2022).
21. Bari, NN Nutrition literacy status of adolescent students in Kampala district, Uganda. Master Thesis, Oslo and Akershus University College of Applied Sciences (Master’s thesis). Oslo and Akershus University College of Applied Sciences, Lillestrøm, Norway. (2012)
22. Gréa Krause, C, Beer-Borst, S, Sommerhalder, K, Hayoz, S, and Abel, T. A short food literacy questionnaire (SFLQ) for adults: findings from a swiss validation study. Appetite. (2018) 120:275–80. doi: 10.1016/j.appet.2017.08.039
23. Taleb, S, and Itani, L. Nutrition literacy among adolescents and its association with eating habits and BMI in Tripoli, Lebanon. Diseases. (2021) 9:25. doi: 10.3390/diseases9020025
24. Natour, N, AL-Tell, M, and Ikhdour, O. Nutrition literacy is associated with income and place of residence but not with diet behavior and food security in the Palestinian society. BMC. (2021) 7:78. doi: 10.1186/s40795-021-00479-3
25. Zeng, M, Zhu, Y, Cai, Z, Xian, J, Li, S, Wang, T, et al. Nutrition literacy of middle school students and its influencing factors: a cross-sectional study in Chongqing, China. Front. Public Health. (2022) 10:807526. doi: 10.3389/fpubh.2022.807526
26. Ayer, Ç, and Ergin, A. Status of nutritional literacy in adolescents in the semi-rural area in Turkey and related factors. Public Health Nutr. (2021) 24:3870–8. doi: 10.1017/s1368980021002366
27. Yilmazel, G, and Bozdogan, S. Nutrition literacy, dietary habits and food label use among Turkish adolescents. Prog Nutr. (2021) 23:e2021007–7. doi: 10.23751/pn.v23i1.8563
28. Mandeya, J, and Kridli, S. Childhood overweight and obesity in Qatar: a literature review. Avicenna. (2014) 2014:2. doi: 10.5339/avi.2014.2
29. Nasreddine, L, Ayoub, JJ, and Al Jawaldeh, A. Review of the nutrition situation in the Eastern Mediterranean region. East Mediterr Health J. (2018) 24:77–91. doi: 10.26719/2018.24.1.77
30. Li, S, Zhu, Y, Zeng, M, Li, Z, Zeng, H, Shi, Z, et al. Association between nutrition literacy and overweight/obesity of adolescents: a cross-sectional study in Chongqing, China. Front Nutr. (2022) 9:893267. doi: 10.3389/fnut.2022.893267
31. Nasreddine, L, Ayoub, JJ, Hachem, F, Tabbara, J, Sibai, AM, Hwalla, N, et al. Differences in dietary intakes among Lebanese adults over a decade: results from two national surveys 1997–2008/2009. Nutrients. (2019) 11:1738. doi: 10.3390/nu11081738
32. National Cancer Institute. Evidence-Based Cancer Control Programs. Teens eating for energy and nutrition at school (teens). (2020). Available at: https://ebccp.cancercontrol.cancer.gov/programDetails.do?programId=246210 (Accessed on 14 June, 2022).
33. Indriasari, R, Nadjamuddin, U, Arsyad, DS, and Iswarawanti, DN. School-based nutrition education improves breakfast-related personal influences and behavior of Indonesian adolescents: a cluster randomized controlled study. Nutr Res Pract. (2021) 15:639. doi: 10.4162/nrp.2021.15.5.639
34. Wang, D, Stewart, D, Chang, C, and Shi, Y. Effect of a school-based nutrition education program on adolescents’ nutrition-related knowledge, attitudes and behavior in rural areas of China. Environ Health Prev Med. (2015) 20:271–8. doi: 10.1007/s12199-015-0456-4/
35. Asakura, K, Mori, S, Sasaki, S, and Nishiwaki, Y. A school-based nutrition education program involving children and their guardians in Japan: facilitation of Guardian-child communication and reduction of nutrition knowledge disparity. Nutr J. (2021) 20.
36. Berkman, ND, Sheridan, SL, Donahue, KE, Halpern, DJ, Viera, A, Crotty, K, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess. (2011) 199:1–941.
37. Ashoori, M, Omidvar, N, Eini-Zinab, H, Shakibazadeh, E, Doustmohamadian, A, Abdar-Esfahani, B, et al. Food and nutrition literacy status and its correlates in Iranian senior high-school students. BMC Nutr. (2021) 7:19. doi: 10.1186/s40795-021-00426-2
38. Wardle, J, Haase, AM, and Steptoe, A. Body image and weight control in young adults: international comparisons in university students from 22 countries. Int J Obes. (2005) 30:644–51. doi: 10.1038/sj.ijo.0803050
39. Li, C-P. Gender differences in nutrition knowledge, attitude, and practice among elderly people. Int J Manag Econ Soc Sci. (2017) 6:199–211.
40. Palumbo, R, Adinolfi, P, Annarumma, C, Catinello, G, Tonelli, M, Troiano, E, et al. Unravelling the food literacy puzzle: evidence from Italy. Food Policy. (2019) 83:104–15. doi: 10.1016/j.foodpol.2018.12.004
41. Costarelli, V, Michou, M, Panagiotakos, DB, and Lionis, C. Parental health literacy and nutrition literacy affect child feeding practices: a cross-sectional study. Nutr Health. (2021) 28:59–68. doi: 10.1177/02601060211001489
42. Gibbs, HD, Kennett, AR, Kerling, EH, Yu, Q, Gajewski, B, Ptomey, LT, et al. Assessing the nutrition literacy of parents and its relationship with child diet quality. J Nutr Educ Behav. (2016) 48:505–509.e1. doi: 10.1016/j.jneb.2016.04.006
43. McIntosh, WA, Kubena, KS, Tolle, G, Dean, WR, Jan, JS, and Anding, J. Mothers and meals. The effects of mothers’ meal planning and shopping motivations on children’s participation in family meals. Appetite. (2010) 55:623–8. doi: 10.1016/j.appet.2010.09.016
Keywords: Arab countries, nutrition literacy, food literacy, adolescents, parents
Citation: Hoteit M, Mansour R, Mohsen H, Bookari K, Hammouh F, Allehdan S, AlKazemi D, Al Sabbah H, Benkirane H, Kamel I, Qasrawi R, Tayyem R and the regional food literacy group (2023) Status and correlates of food and nutrition literacy among parents-adolescents’ dyads: findings from 10 Arab countries. Front. Nutr. 10:1151498. doi: 10.3389/fnut.2023.1151498
Received: 26 January 2023; Accepted: 03 April 2023;
Published: 02 May 2023.
Edited by:
Salwa Albar, King Abdulaziz University, Saudi ArabiaReviewed by:
Fatemeh Mohammadi-Nasrabadi, National Nutrition and Food Technology Research Institute, IranCopyright © 2023 Hoteit, Mansour, Mohsen, Bookari, Hammouh, Allehdan, AlKazemi, Al Sabbah, Benkirane, Kamel, Qasrawi, Tayyem and the regional food literacy group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maha Hoteit, bWFoYS5ob3RlaXRAY25ycy5lZHUubGI=; Rania Mansour, cmFuaWEubWFuc291ckBkb2hhaW5zdGl0dXRlLmVkdS5xYQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.