
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 03 July 2023
Sec. Nutrition and Sustainable Diets
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1122911
This article is part of the Research TopicNutrition and Sustainable Development Goal 17: Partnerships for the GoalsView all 7 articles
Background: Foodservice in hospitals contributes to the environmental footprint of healthcare delivery. There is little known about the role of policy in supporting environmentally sustainable foodservices. The aim of the study was to explore policy in exemplar environmentally sustainable hospital foodservices from the perspective of hospital staff, toward what makes a policy effective, the limitations of policy, and the influential levels and types of policy.
Methods: A generic qualitative inquiry approach was utilized. Staff involved in foodservices were interviewed about the role of policy during 2020–2021 from 14 hospitals across nine countries. Data were analyzed using framework and thematic analysis.
Results: Policies spanned across high level policies at the level of the healthcare organization, local hospital procedures and protocols, as well as public policy from local, state/provincial and national government. Internal organizational policy was used to embed practices within the organization in the long term and help to build a shared vision and goal where public policy had lacked guidance. The creation, content and methods of communication and creating accountability made internal organizational policy successful. Public policy was most effective when it was mandatory, had clearly defined targets and funding to assist implementation. These exemplar hospitals also demonstrated attributes of policy entrepreneurs by engaging with policy makers to share their stories and lobby government for policy change.
Discussion: Policy from within the healthcare organization is an important mechanism for enabling hospitals to deliver and maintain environmentally sustainable foodservice. Public policy must be designed considering the unique implementation challenges hospitals face to ensure they are successful.
Climate change is an ongoing threat to human health and wellbeing (1). The healthcare sector has a role to play beyond reacting to the impacts of climate change, by adopting proactive measures that build an environmentally sustainable health system from within to ensure ongoing and sustainable health and wellbeing for all. One of the principles critical for achieving an environmentally sustainable health system is to reduce emissions from the delivery of health services (2). Foodservices is an aspect of healthcare delivery that can have vast environmental impacts across the supply chain; from how food is farmed and produced through to how waste is managed (3). The provision of food in hospitals in a safe, nutritious, cost effective, efficient way has, to date, taken priority of over climate change mitigation strategies. There is a need to merge these aspects with a consideration for minimizing environmental impacts as well. The EAT Lancet report outlines the danger of unsustainable food to human and planetary health and calls for a Great Food Transformation, to achieve nutritional requirements within planetary health boundaries (4). There is an array for evidence calling for new policy and system wide change for food system reformation (5).
Action taken by the National Health Service in England to establish a Sustainable Development Unit has provided important learning and insights for driving sustainable healthcare change. One of the influencing variables is the role of governance and regulation. Effective regulatory systems can drive implementation and normalize uptake of sustainable practices more widely, by providing guidance and confidence to those leading change (6). Better understanding and application of governance and regulations reduces their likelihood of limiting innovation in sustainable healthcare. Policy has been described as a formal decision or plan of action adopted by an actor to achieve a particular goal (7). Public policy is the formal decision or plan of action that has been taken by government (7). Policies can facilitate effective integration of climate planning into food production, environment and human health policy (8). For example a law that bans organic waste from entering landfill exists in a number of states and cities in the United States (9). In another example, the Farm to Institution New York State policy aims for government run institutions to spend at least 25% of their food dollars on food grown in New York (10).
Individuals working within hospital foodservice can be effective in driving change (11). However, complex system wide sustainability challenges cannot solely rely on individuals to drive widespread change, rather effective policy and systems are needed. Staff working in hospitals and in foodservices are responsible for adhering to and operationalizing policy. As an example of food policy that has driven practice in this setting, in Australia there is federal legislation requiring food safety programs in foodservice for vulnerable persons in hospitals (12). Foodservice staff are required to design, implement, adhere to and monitor their compliance to meet standards and minimize the incidence of foodborne illness. However, it is common for professionals to feel “policy alienation,” a disconnect from the policies they are responsible for following and implementing (13). It has been established that food is an important part to achieve a zero emissions healthcare sector (14). However, translation of policy ambition into meaningful policy is complex (15). Individuals working in foodservice in hospitals experience firsthand the benefits and challenges of policy to support or inhibit environmentally sustainable foodservice. For this reason, it is important to understand their perspectives toward policies, what is effective and what is not, in order to drive truly effective policy formulation and implementation. Exemplar healthcare facilities who have successfully implemented sustainability initiatives within their organizations provide a unique perspective of the role of policy in driving change. This is an area that has not previously been documented in the literature and is important to be able to support effective policy creation. Therefore, the aim of this study was to explore policy in environmentally sustainable hospital foodservice from the perspective of hospital staff who work in exemplar hospital foodservices. Specifically, the aim was to understand their perspectives about the influential levels and types of policy, the characteristics of effective policy, and the limitations of policy. It is expected that understanding these perspectives will guide advocacy efforts for policy change and considerations to strengthen existing and establish new meaningful policy.
This study was approved by the Human Research Ethics Committee (Project ID: 24912).
A generic qualitative inquiry approach underpinned by pragmatism was used (16). Research guided by pragmatism seeks a deeper understanding of an issue by drawing on experiences of individuals to guide practical and actionable answers (16). The data used in this study were drawn from a multiple case study exploring institutional drivers of environmentally sustainable hospital foodservices, which concluded there is a need for supportive systems and policies to facilitate widespread change (11).
The focus of the current inquiry was to explore staff experiences and perspectives of policy in driving change. In this analysis, “policy” refers to a formal decision/commitment or plan of action adopted by government or the healthcare organization to achieve sustainable foodservices. This could be “public policy,” those created by government at the national, state/provincial or local level. It could also be “internal organizational policy” such as a strategy, protocol, guideline, procedure or any other relevant document created internally by the hospital. They may relate to any stage of the food supply chain including food procurement, processing, service, disposal of food and related wastes. Contracts between the hospital and external stakeholders, such as group purchasing organizations and central production kitchens were within the scope of “policy” as they typically reference relevant policy and its implementation.
Hospitals were recruited purposively. The inclusion criteria for selection required participating hospitals to have clearly demonstrated environmentally sustainable foodservices across any stage of the food supply chain and provided diversity in terms of hospital type and geographical location. They were identified through various mediums such as featured in webinars run by sustainability networks, e.g., Healthcare Without Harm, in literature or reports, listed for receiving relevant awards, such as those by the Soil Association and Practice Greenhealth, and recommended by colleagues active in the field of healthcare foodservice sustainability. The environmentally sustainable foodservice practices were initially identified in these publicly available documents and resources during recruitment, with verification by participants. An online advertisement was also distributed by Healthcare Without Harm and Global Green and Healthy Hospitals to recruit eligible hospitals. Participants were also asked to refer other hospitals they knew of that met the inclusion criteria to allow for snowballing sampling.
Hospital contacts were invited to participate by nominating a staff member with extensive knowledge of the environmentally sustainable foodservice practice/s of the hospital. A senior staff member provided written organizational permission for the staff member to participate in the interview on behalf of the organization. Participants then consented verbally at the beginning of the interview. After the completion of each interview, it was then decided which hospitals to target for further recruitment, in line with the original inclusion criteria. Recruitment continued until the sample of hospitals was deemed as having sufficient “information power.” This was established upon discussion as a research team throughout data collection on whether the study aims could be fulfilled and captured hospitals with a range of practices and from a diversity of contexts and locations (17).
Demographic data were collected verbally and included the following participant information: position title, years in position, employment type and gender. Hospital information was also collected including: size, type of foodservice model and food production and whether it was a public or private facility. Participants were also asked to explain the hospital’s sustainable foodservice practices at the beginning of the interview to verify information previously identified during recruitment (e.g., reports, literature, webinars etc.).
All interviews were conducted between October 2020 and January 2021, using the platform Zoom videoconferencing. The interviewer was an Accredited Practising Dietitian and researcher in environmentally sustainable foodservices. Data were collected via semi structured individual or small group interviews for cases with more than one suitable participant. Interviews were transcribed using Otter.ai., a speech to text transcription application. All transcripts were reviewed for accuracy by the interviewer.
Interview questions were based around the drivers of the hospitals’ success in achieving sustainable foodservices. A specific series of questions were asked about the role of policy, policy content, creation and implementation. Participants were also asked about challenges they experienced associated with policy and implementation of sustainable foodservice practices. The full interview protocol has been previously published (11) and a summary of the subsection of questions related to policy is presented in Figure 1. Where policy was reported by participants as a challenge, they were asked their perceived reasons. Following the interviews, there was email correspondence with a subgroup of hospitals to obtain policy documents and further information on the policies relevant to their interviews, such as level of governance or to clarify how policies related to each other. Where necessary, policy documents were translated to English language using Google Translate.
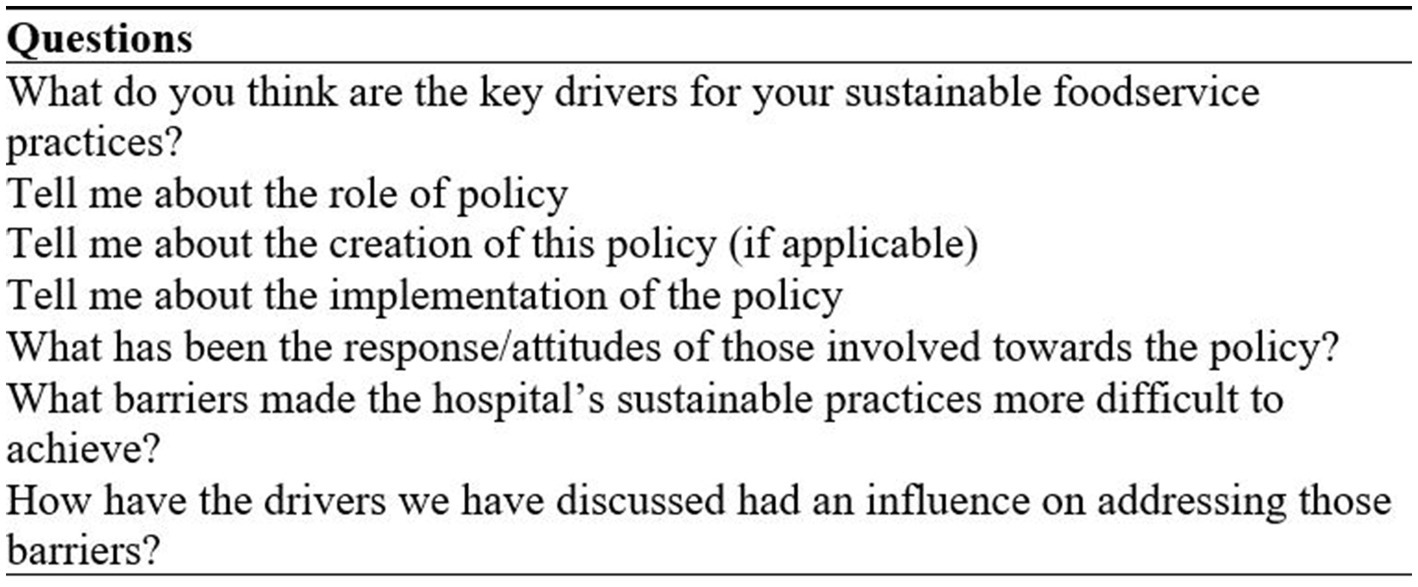
Figure 1. Semi-structured interview questions related to policy [subsection of complete interview protocol previously published (11)].
Framework analysis was used initially to create a framework for analysis (18). Firstly, interview transcripts were reviewed to enable the research team to become familiar with participant responses, and a four category framework was developed based on this interview data. Interview transcripts were then coded deductively against these categories as follows: policy levels/types, characteristics of effective policy, limitations of policy, and hospitals acting as policy entrepreneurs. Within these four categories, data were then analyzed using the process of thematic analysis to elicit further meaning from the data (19). This thematic analysis enabled further subthemes to be identified from within the four categories, without a pre-defined framework. Codes were discussed with other researchers and sub-themes were developed.
A total of 14 hospitals were recruited from nine countries (Australia, Singapore, Taiwan, Canada, Denmark, the United States, Austria, the United Kingdom, Netherlands). Further participant demographic details are outlined in Table 1. There were 21 participants interviewed from these hospitals, with more than one participant from some hospitals where two people were identified to be key informants and/or to support adequate communication where participants spoke English as a second language. Their roles included foodservice, dietetics, executive, health promotion and sustainability. Further participant demographic details are outlined in Table 1.
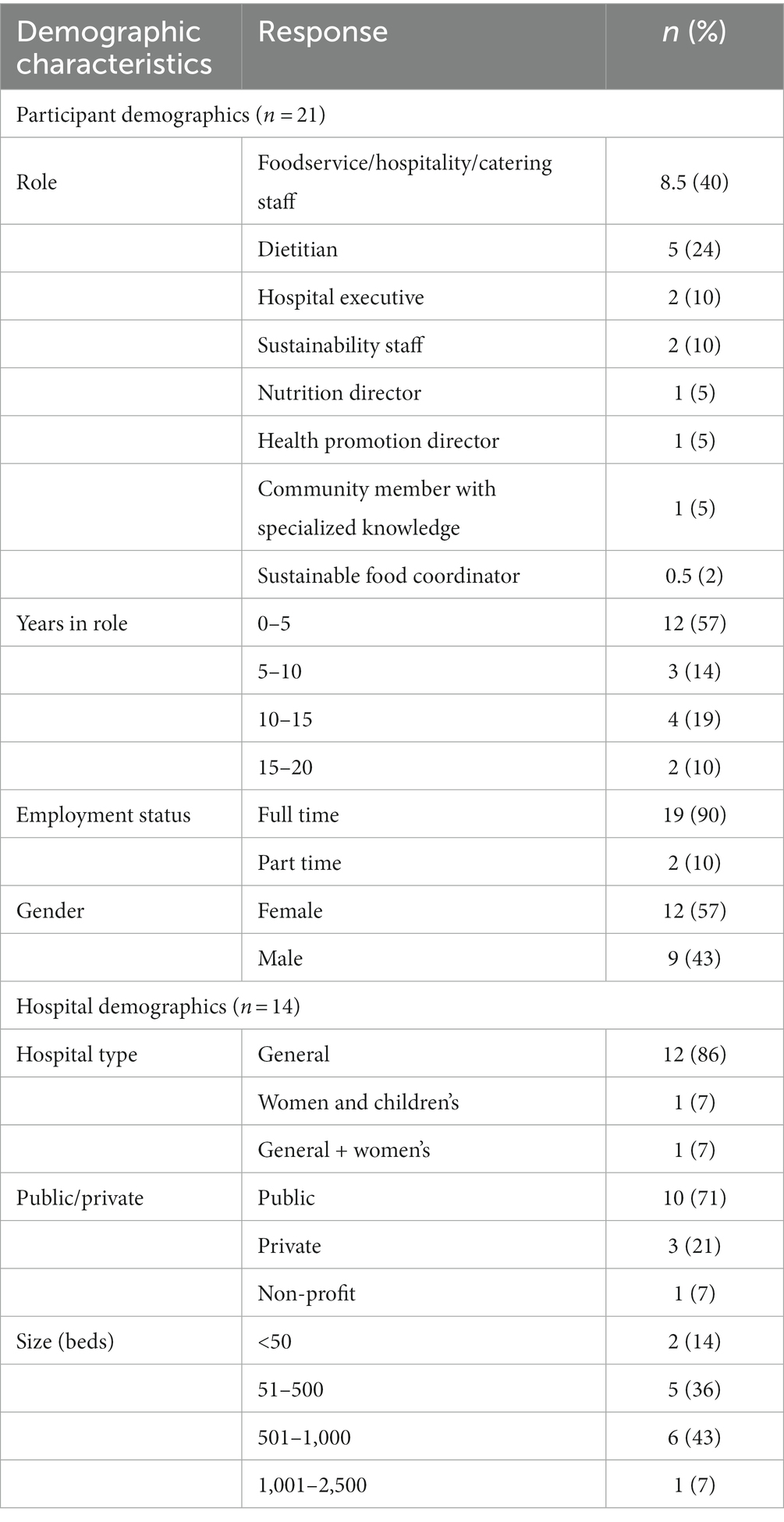
Table 1. Participant and hospital demographics (11).
Examples of sustainable foodservice initiatives implemented within the exemplar facilities were plant based menus, onsite gardens, purchasing of local/seasonal/organic or traditional Indigenous foods, room service model, composting organic food waste, redistributing leftover unserved food to charities and reserving unopened packaged food items.
Responses from interviews revealed the many different policy documents that were influential in sustainable foodservices at these exemplar sites. These consisted of a range of public policies and internal organizational policies. Internal organizational policy included high level guiding documents applicable to the whole healthcare organization such as sustainability commitments, strategic plans and pledges. This then translated into strategies, work plans and specific protocols and instruction documents, for example on how the organization managed food waste, or sustainability criteria for purchasing food.
Public policy documents spanned across national, state/provincial and city levels, standards and strategies. For example, the Denmark Organic Action Plan aimed to increase organic food in public institutions, with the national goal of 60% organic food in public kitchens, set by the Minister for Food, Agriculture, and Fisheries (20). The Ontario Local Food Act was designed to foster resilient local food economies, increase awareness of local food and encourage new markets for local food, by engaging public sector organizations (21).
There were also cases described where policies were associated with grant schemes and programs to support environmentally sustainable foodservice practices. For example, a strategy for public institutions in Quebec to reach a target for local food purchasing had an associated funding program available for projects proposed by institutions to promote and enhance local food in their institution (22).
Participants described several elements of policies which they saw as beneficial in assisting implementation. Firstly, the creation of internal organizational policies and statements were highly valued by participants. They saw it as a way of embedding practices within the organization in the long term and a way to create a shared vision where there was no/little external guidance.
“We wanted to develop some type of commitment, you know, and kind of create as I call it our legacy, you know, so in five to 10 years perhaps when we're not here, that there was something that we had left behind in terms of, you know, reasons why we did the things we did, and kind of what the outcomes were so it was kind of we measured a lot of the things on a scorecard we did, and like there had to be some positive metrics and things that we were able to prove by doing this kind of project.” (P7)
Specific characteristics of how these internal policies were created, their content and how they were communicated are outlined in Table 2.
In terms of public policy, participants shared several aspects that made them more effective and useful such as having clear targets, and funding support available. These are described in Table 2.
There were aspects of policies reported by participants that limited their ability to implement sustainable foodservices. There was an interplay between internal organizational and public policy whereby hospitals were often bridging gaps in public policy through development of their organizational policy.
However, internal organizational documents were limited in cases where there were no mechanisms for accountability such as key performance indicators. In cases where there were policies and guiding documents, they may not have specifically addressed food. Contracts between the hospital and suppliers or group purchasing organizations often restricted the purchasing of local and Indigenous foods. There was perceived to be a clash in values between those who set up contracts and the users of contracts. For example, valuing price over sustainably produced foods.
Public policy was often targeted at all public institutions in the region, not solely hospitals, and for that reason they were not fit for purpose for the healthcare setting. There were few policies that were mandated but there was a lack of monitoring by government to hold hospitals accountable. For some hospitals, public policy conflicted with existing requirements. For example, a local food act was difficult to follow as trade law required hospitals to not favor local suppliers and purchase from existing contracts only.
“The policy was there. So we are inspired by it. But in the day to day, it was not easy to follow it because the law was not with us.” (P6)
Some policies were perceived as too vague to be able to follow and did not have specific targets or guidelines or the support and resources to be able to make changes.
“There are still no defined targets or anything in terms of you know thou shall procure you know 10% Ontario product for example and there's no reporting it's kind of a voluntary piece.” (P7)
While participants were not specifically asked about their influence on policy, several exemplar sites willingly shared this. These participants could be described as policy entrepreneurs “energetic actors who engage in collaborative efforts to promote policy innovations” (23).
Within the organization, these individuals communicated the link between health and the environment with collaborative working groups of staff. They collaborated with several departments to create a shared vision for sustainable practices to be embedded into the organization’s processes in the long term, such as producing instruction documents and position statements to achieve this.
Externally, these individuals engaged with policy makers to share their success stories. They were part of or led working groups with other hospitals and public institutions to raise awareness of sustainability issues within hospital foodservices and lobby government for policy change.
“We were trying to educate them in terms of what health care facilities in Ontario had been doing to promote local and so forth in hopes that they would look at our stories and say here's what we've done. And we need you to kind of move this forward so that it does become mandatory for other health care facilities to do that so what we really wanted them to do was a local food act, so it was there, but it wasn't law. And that's what the collaborative group was working on and we had a couple of government officials and the greenbelt fund and so forth that had worked with us on working with the government. We did letters, we shared case studies and all kinds of stuff. And they did end up enacting the local food act which is great.” (P7)
This research sought to explore policy and the role it played in the experience of international hospitals exemplifying environmentally sustainable foodservices. The findings demonstrate different levels and types of policy, each presenting strengths and limitations in supporting hospitals’ success. The results provide clear insights into how policy can be utilized to serve as an effective driver for sustainable foodservices. The findings suggest that, in the case of these hospitals, public policy does not always support implementation, however, it is effective in prompting hospitals to create their organizational policies. Organizational policies in turn are effective in supporting internal foodservice practice change, through the actions of creating and communicating them and their content. A particularly novel finding of the study was the way in which individuals in these institutions can act as policy entrepreneurs to advocate for policy change.
Unfortunately, inaction can be more significant than action, particularly when older policies have not been updated to reflect current sustainability imperatives and international guidance, or where policies have not been developed to support sustainability initiatives. Despite a previous study about the perspectives of stakeholders working across the hospital food supply chain which suggested that government policy is needed to create change, the present study suggests that the existence of government policy is not always enough to support implementation (24). Instead, policy must be carefully designed to consider implementation.
Policy implementation is described as the actions of individuals or groups directed at the achievement of objectives outlined in policy (25). The policy-implementation gap, whereby policy results in non-achievement, is being increasingly understood to be complex and multifaceted (26). Policy support programs are a new and emerging strategy that has been posed as a way to achieve policy success (26). This requires policy design preparation to understand the problem, policy tracking such as developing targets and progress reports, implementation support such as assistance from experts, and policy implementation review. The present study identified several examples of governments where strategies and funding programs were aligned, contributing to hospitals’ success. These findings suggest that greater support is needed for implementation if public policy is to move beyond solely putting an issue on the agenda. Howlett describes the need for consideration of implementation to be at the heart of policy making, and insights from implementation studies informing the policy process (27). To do this, there is a need for greater understanding of the system resources required for policy implementation. This must come from leaders within the system as well as external expertise and from government, which are specific to sustainable food strategies. For example, tailored programs and resources for local food purchasing that address the challenges hospitals face.
Another important aspect of hospitals’ ability to implement change is having accountability mechanisms in place. These mechanisms were identified in this study as a helpful function of organizational policy to support sustainable foodservices. Given the value of organizational policies, results suggest that all hospitals should have a framework from high level organizational strategic plans to local level work plans. This requirement could be embedded into healthcare accreditation and guidelines which would increase likelihood of compliance. An example of national leadership to achieve sustainable healthcare is the work of the Greener NHS National Programme responsible for all aspects of the NHS’s work on sustainability (28).
Environmentally sustainable hospital foodservices intersects healthcare policy and food policy. Sustainability in the healthcare sector is growing momentum as recently 50 countries committed to developing climate resilient and low-carbon healthcare systems at United Nations Climate Change Conference in Glasgow (29). Simultaneously, food policy that promotes sustainable food systems has recognized the role of large public institutions, which includes the healthcare sector. With government mandating food policy that applies to all public institutions, there is a risk that the unique barriers faced by hospitals and their staff are not adequately considered. Results of this study are particularly relevant for future implementation as they indicate the need for collaboration between policy makers to ensure alignment across healthcare, agriculture and food systems, rather than a siloed approach which is frequently seen. This includes bridging the gap between healthcare networks, government and food policy experts. There is a need to create spaces for cross sectoral dialogue and collaboration to coordinate synergistic actions across sectors and levels of governance (30). Climate related considerations can be incorporated into planning and policy in two ways. Vertical integration is across governance levels and jurisdictions while horizontal integration is of policy goals across different sectors (31). This is a common concept used in sustainable development and ensures that policy makers from different professional backgrounds engage in a common task. Considering integration in both directions ensures policy coherence and prevents conflicting and misaligned policies, as identified in this study.
When considering the advancement of policy, a critical concept is that of policy entrepreneurs. These are people or groups willing to invest their own resources in the hope of a future return (32). Although it was not a specific aim of the study, there were several hospitals in this study that shared their work as policy entrepreneurs. This requires a unique skill set. For example, transforming policy ideas into innovation is a difficult task requiring strategies that are reliant on policy entrepreneurs’ attributes and skills (23). Attributes can be nurtured, and include ambition, social acuity, credibly, sociability and tenacity (23). While skills can be learned including strategic thinking, team building, collecting evidence, making arguments, engaging audiences, negotiating and networking (23). With these skills and attributes, policy entrepreneurs use strategies such as problem framing, using networks, working with advocacy coalitions, leading by example and scaling up change processes. As described in previous research, there are several different values that drive a hospital to pursue sustainable practices (11). Regardless of the values driving the hospital, policy entrepreneurs have social acuity and skills in defining and framing the problem such that policy actors can align with a shared agenda. This was specifically identified in previous research focused on the role of policy entrepreneurship in the creation of urban food strategy development in two European cities (33). Although the food narrative was different between the two cities and was reliant on existing issues, policy entrepreneur networks played the vital role of creating the narrative and building a shared vision among actors (33). This process of reframing issues to align different actors with a joint agenda is important for hospitals to become engaged in, in order to bring about wider change beyond their hospitals.
Given the unique skillset required to be an effective policy entrepreneur, training and tertiary education should be provided informed by the policy entrepreneur literature, based on the important attributes, skills and strategies, contextualized to the healthcare policy setting. The impact of providing policy entrepreneurship training to nurses working in maternal and child healthcare clinics has been investigated (34). This training had a significant effect on policy entrepreneurship behavior and regardless of the level of self-efficacy participants had prior, after training they were able to turn their intentions into behavior. In this way, bureaucrats who do not normally have formal influence in policy design, can use their extensive knowledge of their field toward improving the design of policy. Alongside this, upskilling hospital staff to identify and be prepared for “policy windows” is important. This is described as when the problem, policy and the political streams align and present a window of opportunity for action to be taken (32).
A recent review of research and training related to healthy and environmentally sustainable food procurement and foodservice identified the gap in education and training that exists for nutrition professionals (35). By filling pre-existing training gaps, both with content related to healthy and environmentally sustainable food systems as well as policy entrepreneurship, healthcare workers can mobilize to transform the system they work within. However, healthcare institutions must thoughtfully consider how to support staff to pursue policy entrepreneurship activities. For example, this could be targeted at individuals who are interested, motivated and in positions suited to policy entrepreneur activities. It could be embedded into their position description to provide accountability and individuals would work collaboratively with working groups internally and external sustainability member organizations to increase likelihood of success.
This study is the first to explore policy from the perspectives of those with lived experience working in hospitals that have successful sustainable foodservices. High quality qualitative research demonstrates internal coherence, the alignment between philosophy, methodology and methods such that research questions can be answered to their full potential (36). This study, underpinned by pragmatism, guided our research question to focus on the experiences and actions of staff in relation to policy (16). This approach is a strength of the study as it provided rich and useful information on the effectiveness and drawbacks of policy and viewpoints to strengthen pre-existing and future policy. While this study explored perspectives, another area which would aid policy advocacy is investigating policy decision making processes, implementation, and impact (25). It is important to note that interviews were conducted during late 2020 to early 2021, toward the end of the first year of the COVID-19 pandemic which limited recruitment. It is likely that the perspectives shared by participants may have referred to practice both prior to the pandemic and during the pandemic, while the healthcare system was in a state of major change and stress. Additionally, the sustainable food practices reported by hospitals could not be verified through observation at each hospital due to international travel restrictions at the time. Another point to consider is that while this research explored the role of policy, interviews were conducted with people involved in foodservices and not with staff specifically involved in policy development and implementation. Obtaining this greater understanding of the policy development and translation process from the perspective of policy makers is an important area for future research.
Policy is a necessary and important lever of changing foodservice delivery in hospitals to become more environmentally sustainable. However the design of policy must be tailored to consider implementation challenges unique to healthcare to ensure that policy is fit for purpose rather than existing as a hindrance. Policy makers aiming to improve sustainability of food systems in public institutions will see their efforts fail if they do not properly account for the factors that contribute to implementation success. National strategy is needed to coordinate state/provincial and local level government with an aligned agenda for sustainable healthcare. In doing so, planetary health will be recognized as vital in sustaining human health.
The datasets presented in this article are not readily available because the authors did not receive consent for sharing data. Requests to access the datasets should be directed to am9yamEuY29sbGluc0Btb25hc2guZWR1.
The studies involving human participants were reviewed and approved by the Monash University Human Research Ethics Committee (Project ID: 24912). The patients/participants provided their written informed consent to participate in this study.
SC undertook investigation and formal analysis and wrote the original draft. JP verified coding and interpretation. All authors contributed to review and editing and involved in conceptualization and methodology.
SC was supported by the Australian Government Research Training Program (RTP) Scholarship.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Watts, N, Amann, M, Arnell, N, Ayeb-Karlsson, S, Belesova, K, Berry, H, et al. The 2018 report of the lancet countdown on health and climate change: shaping the health of nations for centuries to come. Lancet. (2018) 392:2479–514. doi: 10.1016/S0140-6736(18)32594-7
2. MacNeill, AJ, McGain, F, and Sherman, JD. Planetary health care: a framework for sustainable health systems. Lancet Planet Health. (2021) 5:e66–8. doi: 10.1016/S2542-5196(21)00005-X
3. Carino, S, Porter, J, Malekpour, S, and Collins, J. Environmental sustainability of hospital foodservices across the food supply chain: a systematic review. J Acad Nutr Diet. (2020) 120:825–73. doi: 10.1016/j.jand.2020.01.001
4. Willett, W, Rockström, J, Loken, B, Springmann, M, Lang, T, Vermeulen, S, et al. Food in the anthropocene: the EAT–lancet commission on healthy diets from sustainable food systems. Lancet. (2019) 393:447–92. doi: 10.1016/S0140-6736(18)31788-4
6. Pencheon, D. Developing a sustainable health care system: the United Kingdom experience. Med J Aust. (2018) 208:284–5. doi: 10.5694/mja17.01134
7. Smith, M, and Richards, D. Governance and public policy in the UK. Oxford: Oxford University Press (2001).
8. Soto Golcher, C, and Visseren-Hamakers, IJ. Framing and integration in the global forest, agriculture and climate change nexus. Environ Plan C Polit Space. (2018) 36:1415–36. doi: 10.1177/2399654418788566
9. National Conference of State Legislatures. Fighting food waste. (2020). Available at: https://www.ncsl.org/research/environment-and-natural-resources/fighting-food-waste.aspx (Accessed November 19, 2021).
10. Libman, K, Li, A, and Grace, C. The public plate in New York state: growing health, farms and jobs with local food. New York, NY: New York Academy of Medicine (2017).
11. Carino, S, Malekpour, S, Porter, J, and Collins, J. The drivers of environmentally sustainable hospital foodservices. Front Nutr. (2021) 8:740376. doi: 10.3389/fnut.2021.740376
12. Food Standards Australia New Zealand. Food safety standards (chapter 3). Available at: https://www.foodstandards.gov.au/foodsafety/standards/Pages/Food-Safety-Standards-(Chapter-3).aspx (Accessed November 23, 2021).
13. Tummers, L, Bekkers, V, and Steijn, B. Policy alienation of public professionals: application in a new public management context. Publ Manag Rev. (2009) 11:685–706. doi: 10.1080/14719030902798230
14. Health Care Without Harm. Global road map for health care Decarbonization annex C. Available at: https://healthcareclimateaction.org/sites/default/files/2021-06/Health%20Care%20Without%20Harm%20Road%20Map%20for%20Health%20Care%20Decarbonization%20Annex%20C_final.pdf (Accessed March 9, 2023).
16. Patton, M. Pragmatism and generic qualitative inquiry In: Felts DC editor. Qualitative research and evaluation methods. 4th ed. Thousand Oaks, CA: Sage (2015) 152–157.
17. Malterud, K, Siersma, VD, and Guassora, AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. (2016) 26:1753–60. doi: 10.1177/1049732315617444
18. Ritchie, J, and Spencer, L. Qualitative data analysis for applied policy research In: A Bryman and R Burgess, editors. Analysing qualitative data. London: Routledge (2002). 173–94.
19. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qualitat Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
20. Organic Action Plan for Denmark. Working together for more organics. Available at: https://www.foedevarestyrelsen.dk/english/SiteCollectionDocuments/Kemi%20og%20foedevarekvalitet/Oekologiplan%20Danmark_English_Print.pdf (Accessed November 23, 2021).
21. Local food act. Available at: https://www.ontario.ca/laws/statute/13l07 (Accessed November 23, 2021).
22. Agriculture, Pêcheries et Alimentation Québec. Programme de développement des marchés bioalimentaires. Available at: https://www.mapaq.gouv.qc.ca/SiteCollectionDocuments/Formulaires/Programme_dev_marches_bioalimentaires.pdf (Accessed November 23, 2021).
23. Mintrom, M. So you want to be a policy entrepreneur? Policy Desi Pract. (2019) 2:307–23. doi: 10.1080/25741292.2019.1675989
24. Carino, S, Collins, J, Malekpour, S, and Porter, J. Environmentally sustainable hospital foodservices: drawing on staff perspectives to guide change. Sustain Prod Consumpt. (2021) 25:152–61. doi: 10.1016/j.spc.2020.08.003
25. Van Meter, DS, and Van Horn, CE. The policy implementation process: a conceptual framework. Admin Soc. (1975) 6:445–88. doi: 10.1177/009539977500600404
26. Hudson, B, Hunter, D, and Peckham, S. Policy failure and the policy-implementation gap: can policy support programs help? Policy Des Pract. (2019) 2:1–14. doi: 10.1080/25741292.2018.1540378
27. Howlett, M. Moving policy implementation theory forward: a multiple streams/critical juncture approach. Publ Pol Admin. (2019) 34:405–30. doi: 10.1177/0952076718775791
28. National Health Service England. Sustainable development unit archive. Available at: https://www.england.nhs.uk/greenernhs/whats-already-happening/sustainable-development-unit-archive/ (Accessed November 23, 2021).
29. World Health Organization. Countries commit to develop climate-smart health care at COP26 UN climate conference. Available at: https://www.who.int/news/item/09-11-2021-countries-commit-to-develop-climate-smart-health-care-at-cop26-un-climate-conference (Accessed November 23, 2021).
30. United Nations Systems Standing Committee on Nutrition. Enhancing coherence between trade policy and nutrition action. Available at: https://openaccess.city.ac.uk/id/eprint/14517 (Accessed November 23, 2021).
31. Adelle, C, and Russel, D. Climate policy integration: a case of déjà vu? Environ Pol Gov. (2013) 23:1–12. doi: 10.1002/eet.1601
32. Kingdon, JW, and Stano, E. Agendas, alternatives, and public policies. Boston, MA: Little, Brown & Co (1984).
33. Giambartolomei, G, Forno, F, and Sage, C. How food policies emerge: the pivotal role of policy entrepreneurs as brokers and bridges of people and ideas. Food Policy. (2021) 103:102038. doi: 10.1016/j.foodpol.2021.102038
34. Frisch-Aviram, N, Beeri, I, and Cohen, N. How policy entrepreneurship training affects policy entrepreneurship behavior among street-level bureaucrats–a randomized field experiment. J Eur Publ Pol. (2021) 28:698–722. doi: 10.1080/13501763.2021.1912146
35. Stephens, LD, Porter, J, and Lawrence, M. Healthy and environmentally sustainable food procurement and foodservice in Australian aged care and healthcare services: a scoping review of current research and training. Sustainability. (2021) 13:11207. doi: 10.3390/su132011207
Keywords: foodservice, environmental sustainability, hospitals, policy, healthcare, qualitative
Citation: Carino S, Collins J, Malekpour S and Porter J (2023) The role of policy in supporting environmentally sustainable foodservice in healthcare: lessons from exemplar hospitals. Front. Nutr. 10:1122911. doi: 10.3389/fnut.2023.1122911
Received: 13 December 2022; Accepted: 12 June 2023;
Published: 03 July 2023.
Edited by:
John Msuya, Sokoine University of Agriculture, TanzaniaReviewed by:
Suresh M, Amrita Vishwa Vidyapeetham University, IndiaCopyright © 2023 Carino, Collins, Malekpour and Porter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jorja Collins, am9yamEuY29sbGluc0Btb25hc2guZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.