- 1Department of Biochemistry, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 2Department of Midwifery, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 3Department of Physiology, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 4Department of Biochemistry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Undernutrition is the term used to describe when a person consumes insufficient amounts of nutrients and energy to meet their needs for maintaining health. Despite substantial progress, undernutrition remains a serious public health concern in many low and middle-income nations, including Ethiopia. Women and children are, in reality, the most nutritionally vulnerable individuals, particularly in times of crisis. In Ethiopia, 27 percent of lactating women are thin or malnourished, and 38% of children are stunted. Although the issue of undernutrition may worsen in times of emergency, like war, there are limited studies available in Ethiopia that show the nutritional status of lactating mothers in humanitarian settings.
Objectives: The main aim of this study was to determine the prevalence and investigate the factors associated with undernutrition among internally displaced lactating mothers in Sekota camps, in northern Ethiopia.
Methods: A cross-sectional study through a simple random sampling technique was conducted among 420 randomly selected lactating mothers in Sekota Internally Displaced Persons (IDP) camps. Data were collected using a structured questionnaire and anthropometric measurements. Logistic regression analysis was employed to identify independent factors associated with maternal undernutrition.
Results: Using a cut-off mid-upper arm circumference <23 cm, the prevalence of undernutrition among internally displaced lactating mothers was 54.8%. Large family size [adjusted odds ratio (AOR) = 4.35; 95% CI: 1.32, 10.22], short birth interval (AOR = 4.85; 95% CI: 1.24, 10.00), low maternal daily meal frequency (AOR = 2.54; 95% CI: 1.12, 5.75), and low dietary diversity score (AOR = 1.79; 95% CI: 1.03, 3.10) were all significantly associated with undernutrition.
Conclusion: The prevalence of undernutrition among internally displaced lactating mothers is relatively high. Governments and other concerned organizations involved in providing care and support to Sekota IDP camps should increase their efforts to improve the nutritional status of lactating mothers
Background
Ethiopia is Africa’s oldest independent country and it is the second largest in terms of the population (1). Ethiopia in the northern area has experienced internal conflict during the last 2 years between the government of Ethiopia and forces in its northern Tigray region (2). The conflict has had severe impacts on the civilian population. Many families have been forced to flee their homes (internally displaced) because of the armed conflict. Internally Displaced Persons (IDP) are people who have been forced to leave their homes due to war or other circumstances but do not meet the legal standards of refugees (3). Conflicts have a negative influence on food security by causing huge displacements, severe economic downturns, increased inflation and unemployment, and eroding funds for social protection and healthcare (4). Armed conflict is a significant contributor to the rising burden of malnutrition, resulting from decreased food availability, social disruption, higher food prices, and, eventually, starvation and/or disease. Internally displaced women and children are, in reality, the most vulnerable and conflict-affected individuals in the world (5). Generally, malnutrition among vulnerable and marginalized groups (including lactating women) because of armed conflict is a multifaceted problem that requires a multidisciplinary remedy (6).
Undernutrition is the term used to describe when a person consumes insufficient amounts of nutrients and energy to meet their needs for maintaining health (7). Despite substantial progress, malnutrition remains a serious public health concern in many low and middle-income nations, including Ethiopia, particularly in times of crisis (8). Due to their greater nutritional needs and the harmful consequences of inadequate nutrition on the health of both mothers and their children, lactating women and their children are among the most susceptible categories of the population during emergencies such as war (9). Undernutrition is a serious issue among lactating mothers in developing nations, particularly in Sub-Saharan Africa (10). In Ethiopia, both maternal and child malnutrition are common problems. Generally, 27 percent of Ethiopian women are thin or malnourished, and 38% of children are stunted (11). The prevalence of malnutrition among lactating women in Ethiopia varies by area, as does the anthropometric measurement technique. Some studies utilize mid-upper arm circumference (MUAC), whereas others employ body mass index (BMI). A community-based survey in Ethiopia’s Afar region revealed that 33.3% of mothers were malnourished based on MUAC (12). Using BMI, 21.2 and 17.4% of lactating mothers in the Angecha and Arba Minch districts of southern Ethiopia, respectively, were undernourished (13, 14). Malnutrition among lactating women was reported to be 21.8% in the Dega Damot district (15) and 21% in Dessie town (16) in northern Ethiopia. Another study in the Bale Zone of Oromia regional state found that 24% of lactating mothers living in humanitarian settings were malnourished (17). Although both BMI and MUAC can be used to determine undernutrition in adults, MUAC has long been used as a community-based assessment of undernutrition because it is easier to implement than BMI. Prior research also suggests that MUAC can be an effective indicator of female adult malnutrition, comparable to or even better than BMI (18, 19). Most published research uses the terms malnutrition and undernutrition interchangeably, while malnutrition is a broader term that includes both over-nutrition and undernutrition (20). However, undernutrition is the focus of this study. Although there have been a few studies to assess the nutritional status of lactating mothers in various regions of Ethiopia, screening, and management of malnutrition in humanitarian settings is limited, and there is no published evidence reporting maternal nutritional status in most conflict-affected areas in Ethiopia, particularly to the study setting. Furthermore, it is critical to identify the issue of undernutrition and its risk factors among people living in humanitarian settings, as this could help the government and other humanitarian organizations in designing their interventions. Hence, the objective of this study was to determine the prevalence and investigate the risk factors of undernutrition among internally displaced lactating mothers in Sekota camps, in northern Ethiopia.
Materials and methods
Study design, setting, and period
A cross-sectional study design was employed in IDP camps found in Sekota town. Sekota is the capital city of the Waghimra zone, Amhara region in northern Ethiopia. It is 436 and 876 kilometers away from Bahir Dar (the capital city of the Amhara region) and Addis Ababa (the capital city of Ethiopia), respectively. Sekota town is bounded by Gazbibla on the south, Zikuala on the west, Abergele on the north, and the east by the Tigray region. There are currently three temporary IDP camps in the town. These are Weleh, Mindikri, and Tirki. The town currently encompasses more than 65, 000 IDPs in all camps. Of these IDPs, around 3,000 residents are known to be lactating mothers, 4,200 are pregnant and 16,000 children less than 5 years of age collectively live in Sekota camps. The study was conducted from June 3 to July 10, 2022.
Sample size determination
The minimum sample size required for the study was determined by using Epi info version 7.2 StatCalc software with the following assumptions. 95% CI, 5% margin of error, the number of lactating mothers found in Sekota IDP camps, which was 3,000, a 24% prevalence of undernutrition among lactating women in humanitarian settings from a previous study conducted in Ethiopia (17), and a design effect of 1.5. The calculated sample size was 384. Taking 10% of the possible non-response rate into account, the final sample size for the study is 422.
Sampling procedures
As a first step, a camp registration list of lactating mothers was identified using information from a rural health center. The total sample was then proportionately allocated to each camp. Then, using a computer-generated method at the household level, simple random sampling techniques were used to select study participants (Figure 1). When an eligible participant was not identified at their assigned campsite, the interviewers returned to the site at a later time during the data-collecting period.

Figure 1. Schematic presentation of the sampling procedure for the study conducted among lactating mothers in Sekota camps, Ethiopia, 2022.
Eligibility criteria
The source population was all internally displaced lactating mothers living in all Sekota camps. The study population was randomly selected from internally displaced lactating mothers during the specified study period. Lactating mothers who visited the IDP camp during the study period were excluded from the study.
Data collection tools and procedure
Data were collected using an interviewer-administered structured questionnaire and anthropometric measurement. The questionnaire has three sections including sociodemographic variables, maternal reproductive and healthcare-related questions, and dietary diversity-related questions. The individual dietary diversity of lactating mothers was evaluated using the qualitative recall of the mothers’ food consumption over the previous 24-h period. The tool includes 10 food groups (starchy staples, legumes and nuts, dairy, organ meat, any egg, meat poultry and fish, dark green leafy vegetables, other vitamin-A rich fruits and vegetables, other vegetables, and other fruits). It was then determined using a simple count and sum of the number of food groups consumed by each respondent during the prior 24-h recall period.
The MUAC of each lactating mother was measured using non-elastic, non-stretchable adult-size MUAC tapes at the midpoint between the points of the shoulder and elbow of the left upper arm. Since the development of the triceps and biceps muscles may be asymmetrical physiologically, with more muscularity in the dominant (right) arm than the non-dominant (left), the left upper arm has come to be used for MUAC measurement (21). The arm was then flexed 90 degrees from the elbow, and the tape was wrapped around the midpoint, not too tight or too loose. Two measurements were taken and the average was recorded as the final MUAC. The measurements were taken to the nearest 0.1 cm. Three BSc nurses as data collectors and two master-holder public health professionals as supervisors were recruited to collect the data.
Study variables
Dependent variable: Undernutrition.
Independent variables: Sociodemographic variables (age, marital status, educational status, occupation, residence, and family member size), maternal reproductive and healthcare-related variables (age at first pregnancy, ANC follow-up, gravidity, birth interval, place of birth, frequency of breastfeeding, maternal illness, maternal meal frequency, and sources of food), and minimum dietary diversity score.
Operational definitions
Undernutrition: MUAC of less than 23 cm (22).
Illness in the past 2 months: If a lactating, mother encountered any type of illness after entering the camps in the previous 2 months.
Minimum dietary diversity for women (MDD-W): Is defined using the ten food group categories according to the recommendation of the Food and Agriculture Organization (FAO) and the United States Agency of International Development (USAID) (23). The mother was asked what type of food she ate in the 24 h preceding the survey, independent of portion quantity. The Minimum Dietary Diversity Score (MDDS) is classified as
Low: If the mother consumed <5, food groups out of the 10 food groups.
Adequate: If the mother consumed ≥5, food groups out of the ten food groups.
Data processing and analysis
Data were checked for completeness, entered into EPI data (version 3.1), and exported to Statistical Package for Social Science (SPSS) (version 20) for statistical analysis. Descriptive statistics (mean and standard deviation for continuous variables; and frequencies and percentages for categorical variables) were computed. All variables were checked for normality and fulfillment of assumptions using histograms, boxplots, and scatter plots before analysis. In this study, the outcome variable was nutritional status coded 0 as undernutrition and 1 as normal (well nutrition). Binary logistic regression was used to identify the crude relationship of factors associated with undernutrition in lactating mothers, then variables significant at P < 0.25 were entered into the final multivariate model to identify significant factors independently predicting undernutrition among lactating mothers. Both crude odds ratio (COR) and adjusted odds ratios (AOR) together with their corresponding 95% confidence intervals were computed to assess the strength of association between the outcome and independent variables. In the multivariate analysis, variables with a p-value of less than 0.05 were considered significant. In the final model, the Hosmer–Lemeshow test was used to determine model fitness, and a value greater than 0.05 was considered a good fit.
Data quality management
To assure data quality, all data collectors and supervisors received training and proper orientation before the actual commencement of data collection. To maintain consistency, the English version of the questionnaire was translated into the local language (Amharic) and then back into English. Two weeks before the actual data collection, the questionnaire was pre-tested on 5% of the study population at other sites with a similar population (Ebinat IDP site), and a few modifications were made. Furthermore, the accuracy, clarity, and completeness of data were reviewed on daily basis by the supervisors and principal investigators.
Results
Sociodemographic characteristics of respondents
A total of 420 lactating mothers participated in this study with a response rate of 99.5%. The mean (± SD) age of study participants was 26.5 (±5) years ranging from 17 to 45 years. Nearly half (51.4%) of the respondents were found in the age group of 25–34. The majority of the study participants (85.7%) were married, 38.6% of them had no formal education, and 52.8% were residing in urban areas. One hundred fifty-nine study participants had at least two under-five children in their households (Table 1).
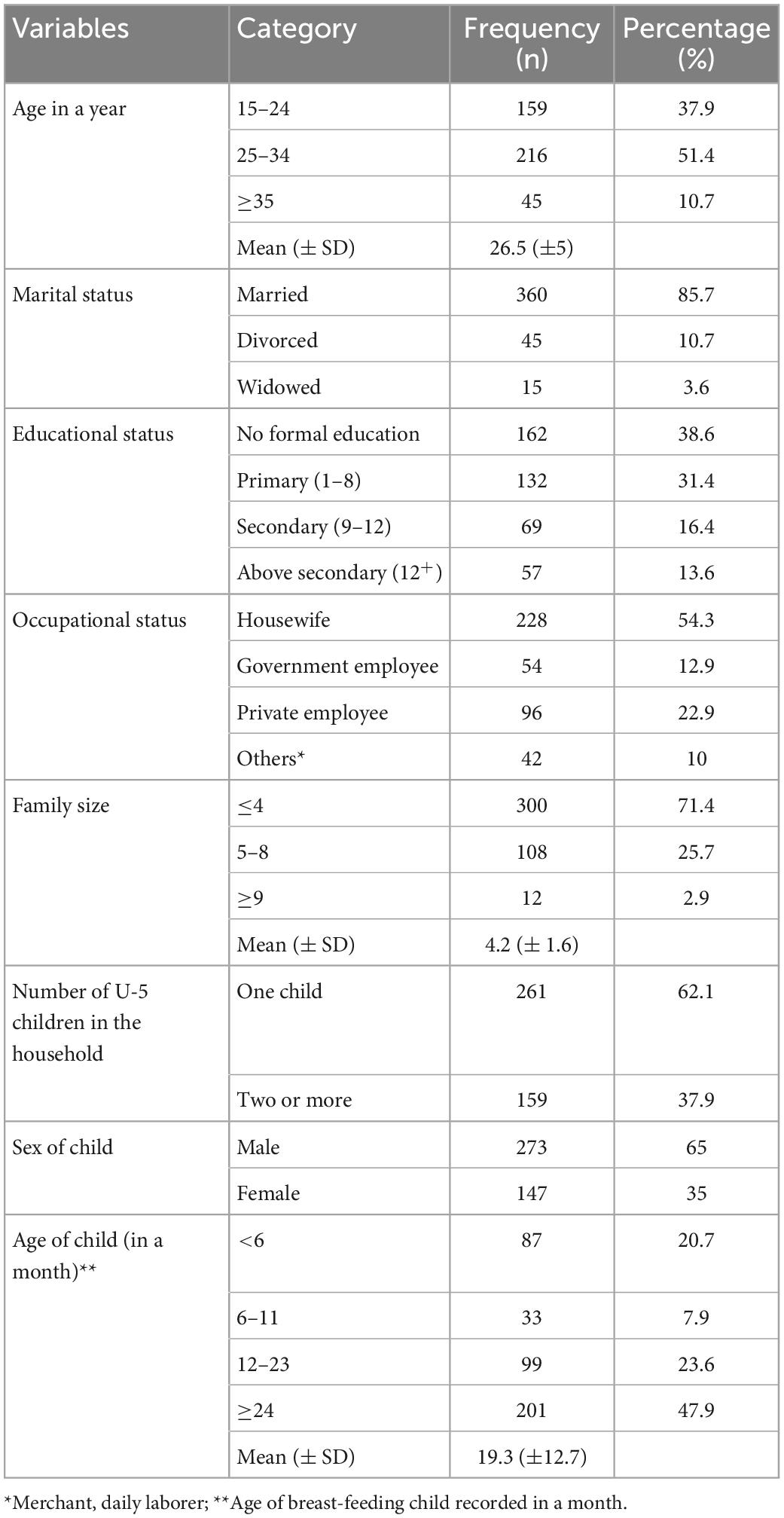
Table 1. Sociodemographic characteristics of lactating mothers in Sekota Internally Displaced Persons (IDP) camps, northern Ethiopia, 2022.
Maternal reproductive and healthcare-related characteristics
Less than half (48.6%) of lactating mothers attended antenatal care (ANC) follow-ups in their last pregnancy. The majority of the study participants (63.6%) had their first pregnancy while still in their teenage. One hundred eighty (42.9%) study participants had a birth interval of fewer than 36 months. More than half of the participants (52.9%) gave birth to their current child at home. The majority (84.3%) of study participants obtained their food from various groups that provide food assistance (Table 2).
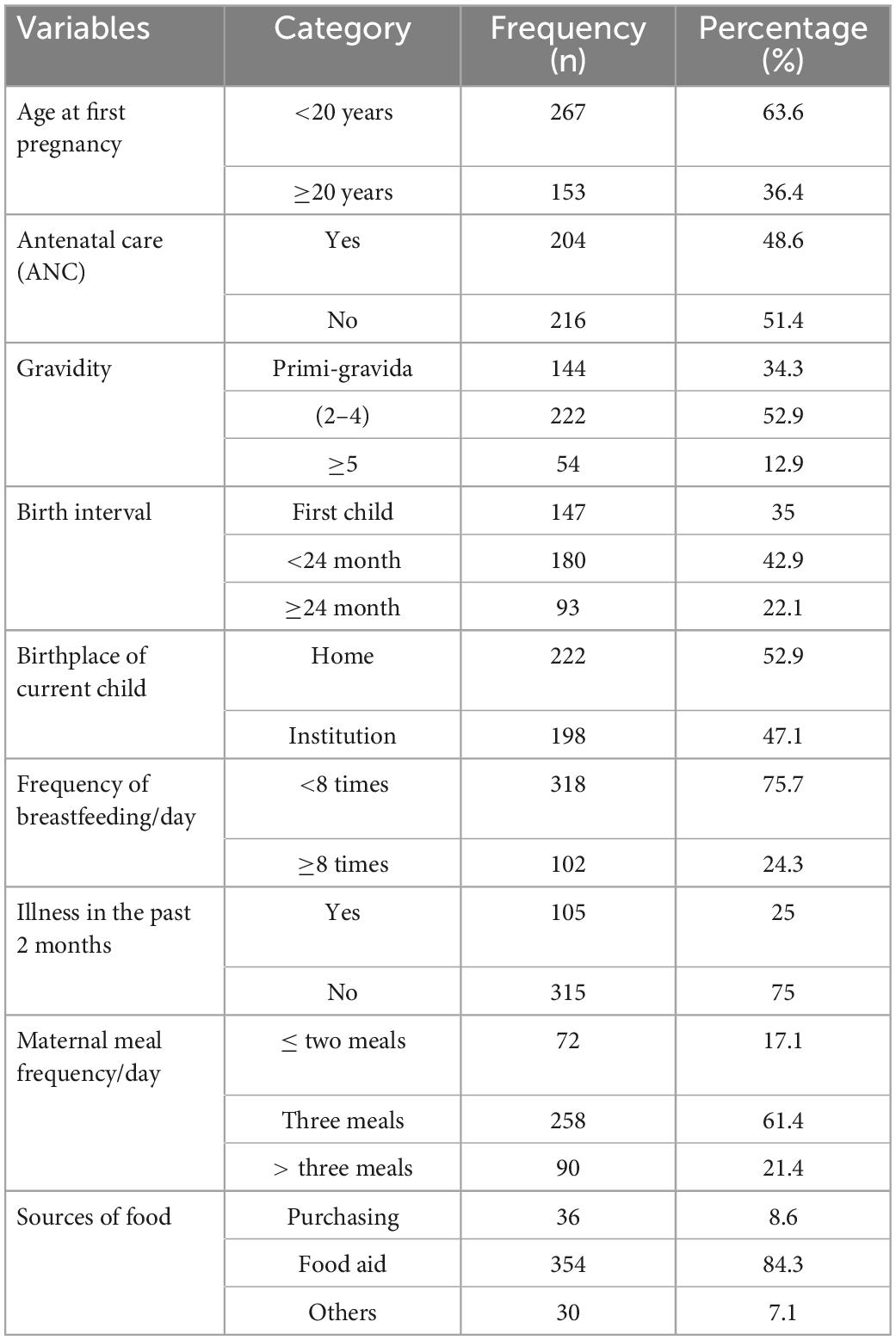
Table 2. Maternal reproductive and healthcare-related characteristics among lactating mothers in Sekota Internally Displaced Persons (IDP) camps, northern Ethiopia, 2022.
Dietary diversity characteristics of respondents
Regarding the food groups consumed by lactating mothers in the previous 24 h, all women consumed starchy staples. Whereas 80.5 and 76.9% of respondents consumed legumes and nuts, and other vegetables, respectively 24 h preceding the survey. More than one-third (42.4%) of lactating mothers’ minimal dietary diversity score was low or inadequate (Table 3).
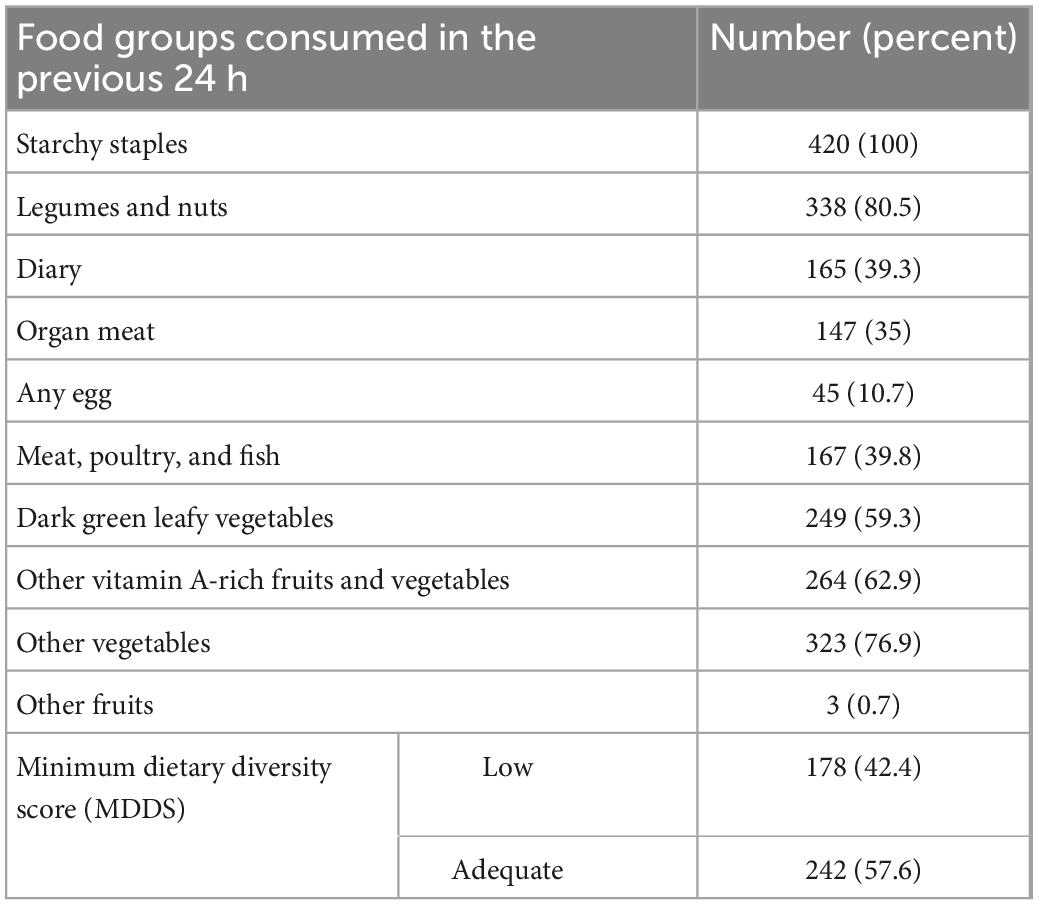
Table 3. Dietary diversity frequency among lactating mothers in Sekota Internally Displaced Persons (IDP) camps, northern Ethiopia, 2022.
Nutritional status of lactating mothers
The nutritional status of lactating mothers was assessed using MUAC. Accordingly, 54.8% (95% CI: 49.9, 59.6) of lactating women were undernourished (Table 4).
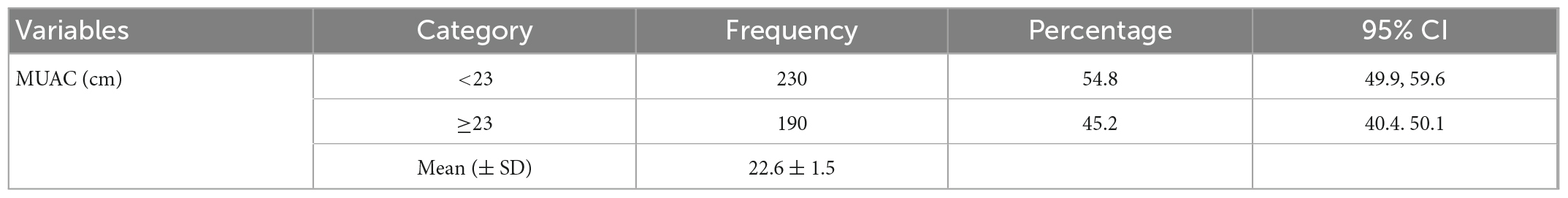
Table 4. Nutritional status among lactating mothers in Sekota Internally Displaced Persons (IDP) camps, northern Ethiopia, 2022.
Factors associated with undernutrition among lactating mothers
The Hosmer–Lemeshow test was used to determine binary regression model fitness. The model fits with a P-value of 0.863 (Table 5). Then, to identify factors associated with undernutrition among lactating mothers in the study population, bivariate and multivariable logistic regression analyses were performed. MUAC was used to determine whether lactating women were undernourished (MUAC < 23 cm) or not (MUAC ≥ 23 cm). On binary logistic regression analysis, maternal age, family size, gravidity, birth interval, the birthplace of the current child, maternal illness in the past 2 months, maternal daily meal frequency, source of food, and minimum dietary diversity score were significantly associated with undernutrition at a p-value of < 0.25. However, in the final multivariate logistic regression model, age, family size, birth interval, daily maternal meal frequency, and dietary diversity score were significantly associated with undernutrition at a p-value of 0.05 (Table 6). Based on the principle of the logistic regression model, we used techniques like the normative category, the smallest value, and the category whose mean is in the middle to choose the reference category (24).

Table 6. Factors associated with undernutrition among lactating mothers in Sekota Internally Displaced Persons (IDP) camps, northern Ethiopia, 2022.
Discussion
The prevalence of undernutrition among lactating mothers was found to be 54.8% in this study. In comparison to the findings of this study, most Ethiopian studies reported a lower prevalence of undernutrition among lactating women, such as in the Afar region 33.3% (12), Angecha district 21.2% (13), Arba Minch districts 17.4% (14), Dega Damot district 21.8% (15), Dessie town 21% (16), Moyale district 17.7% (25), and Shebedino district, Sidama region 25.9% (26). The possible reason might be due to the different sociodemographic and economic natures of the study population. It could also be because our study participants are displaced individuals as a result of the civil war, which has had a significant impact on their agricultural productivity and economy in comparison to other regions of the country that have been stable without civil conflicts (27). The finding is even greater than that of a study conducted in the Bale zone of Oromia regional state, which revealed 24% undernutrition among lactating women in a humanitarian setting (17). The higher prevalence in the current study could be attributed to insufficient humanitarian support by the national government or international humanitarian groups in the selected IDP camps.
Predictors of undernutrition among lactating mothers are maternal age, family size, birth interval, maternal meal frequency, and MDDS (Table 6). In this study, young age (<35 years old) has a significantly low risk of undernutrition than those older ages. This could be due to biological changes caused by aging, such as changes in body composition and energy calories contributing to an increased risk of undernutrition (28). Lactating mothers with a family size of ≥9 are 4.35 times more likely to be malnourished than those with smaller family sizes. The finding is similar to the studies conducted in Nekemte (Oromia region) and Wenberma district (Amhara region), Ethiopia (29, 30). The possible reason could be due to the household food insecurity issue in women with large family sizes resulting in undernutrition (31). In this study, lactating mothers with short birth intervals (<24 months) were 4.85 times more likely to be undernourished than their counterparts. This is consistent with the studies conducted in the Afar region (12) and Arba Minch district (14). It might be due to the recurrent loss of macronutrients and micronutrients from the woman’s body during pregnancy, delivery, and breastfeeding as a result of short birth spacing and repeated childbearing. Additionally, a short birth interval does not provide the mother with enough time to recover from the nutritional burden (32). Short birth intervals have also been associated with adverse outcomes in a woman’s nutritional status, such as nutritional depletion, folate depletion, and micronutrient insufficiency (33). Lactating mothers with a low daily meal frequency (≤2 meals) were 2.54 times more likely to be malnourished than those who consumed more frequent feeding. MDDS was also statistically associated with undernutrition among lactating mothers. Lactating mothers with inadequate MDDS were approximately twice more malnourished as those with adequate MDDS. The finding is consistent with the study done in the Afar region (12), Dessie town (16), and Angecha district (13). Taking at least two extra meals per day during lactation is recommended by the essential nutrition action (ENA) for all lactating women (34). Poor dietary intake is clearly one of the immediate causes of malnutrition, even in lactating women. It was also demonstrated that inadequate minimal dietary diversity among lactating mothers is a potential cause of maternal undernutrition since consumption of a variety of food types gives various vital nutrients for optimum growth (35). As a result, dietary sufficiency and a varied diet are crucial for lactating mothers throughout the postpartum period (36). Furthermore, dietary deficiency combined with a lack of diversity may jeopardize maternal health, worsening malnutrition in lactating mothers (37).
Our study, however, has the following limitations. First, we did not include the wealth index, household food security, and the presence of comorbidities (health status) of participants as independent factors, which might have caused a confounding effect. Second, dietary diversity and meal frequency were examined using a 24-h recall, which may not represent the study participants’ regular intake.
Conclusion
The prevalence of undernutrition among internally displaced lactating mothers in Sekota IDP camps was found to be very high. Older Age, large family size, short birth interval, maternal meal frequency, and low dietary diversity score are the factors associated with undernutrition. Governments and other concerned organizations involved in providing care and support to Sekota IDP camps should increase their efforts to improve the nutritional status of lactating mothers.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by from the Debre Tabor University College of Health Sciences Research Ethics Review Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
MM and MTA conceived and designed the study. MW and EC were actively involved in the guidance of the conception of research and critical review of the manuscript. YB, TA, and MA were involved in the proposal development and data collection. MM was actively working on data analysis, and writing the research report, and was a major contributor to drafting the manuscript. All authors have read, provide critical feedback, and approved the final manuscript.
Acknowledgments
We express our deep sense of gratitude and immense respect to the study participants who were willing to participate in this study. Our grateful acknowledgment also goes to the data collectors and supervisors for their valuable contribution during the data collection process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Genet A. Population growth and land use Land cover change scenario in Ethiopia. Int J Environ Prot Policy. (2020) 8:77–85. doi: 10.11648/j.ijepp.20200804.12
2. Gesesew H, Berhane K, Siraj E, Siraj D, Gebregziabher M, Gebre Y, et al. The impact of war on the health system of the Tigray region in Ethiopia: an assessment. BMJ Glob Heal. (2021) 6:e007328. doi: 10.1136/bmjgh-2021-007328
3. Hickel M. Protection of internally displaced persons affected by armed conflict: concept and challenges. Int Rev Red Cross. (2001) 83:699. doi: 10.1017/s1560775500119261
4. FAO. Monitoring Food Security in Countries With Conflict Situations: A Joint FAO/WFP Update for the United Nations Security Council. New York: Food and Agriculture Organization of the United Nations (2018). p. 1–53.
5. Eran B, Ties B, Nadia A, Ana L, Espoir Bwenge ME. The effects of armed conflict on the health of women and children. Lancet. (2022) 397:522–32. doi: 10.1016/s0140-6736(21)00131-8
6. Corley A. Linking armed conflict to malnutrition during pregnancy, breastfeeding, and childhood. Glob Food Sec. (2021) 29:100531. doi: 10.1016/j.gfs.2021.100531
7. Blössner M, De Onis M, Prüss-üstün A, Campbell-lendrum D, Corvalán C, Woodward A. Malnutrition Quantifying the Health Impact at National and Local Levels. Geneva: WHO (2005).
8. Victora C, Christian P, Vidaletti L, Gatica-Domínguez G, Menon P, Black R. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. Lancet. (2021) 397:1388–99. doi: 10.1016/s0140-6736(21)00394-9
9. Marshall N, Abrams B, Barbour L, Catalano P, Christian P, Friedman J, et al. The importance of nutrition in pregnancy and lactation: lifelong consequences. Am J Obstet Gynecol. (2022) 226:607–32. doi: 10.1016/j.ajog.2021.12.035
10. Wubetie B, Mekonen T. Undernutrition and associated factors among lactating mothers in rural Yilmana Densa District, Northwest Ethiopia: a community-based cross-sectional study. Food Sci Nutr. (2022) 1–11. doi: 10.1002/fsn3.3176
11. Amaha N, Woldeamanuel B. Maternal factors associated with moderate and severe stunting in Ethiopian children: analysis of some environmental factors based on 2016 demographic health survey. Nutr J. (2021) 20:1–9. doi: 10.1186/s12937-021-00677-6
12. Mulaw G, Mare K, Anbesu E. Nearly one-third of lactating mothers are suffering from undernutrition in pastoral community, Afar region, Ethiopia: community-based cross-sectional study. PLoS One. (2021) 16:1–16. doi: 10.1371/journal.pone.0254075
13. Boke M, Yesuf A, Gutema B. Prevalence of undernutrition and associated factors among lactating mothers of angecha District, Kembata Tembaro Zone, Southern Ethiopia. J Nutr Metab. (2021) 2021:6691982. doi: 10.1155/2021/6691982
14. Tikuye H, Gebremedhin S, Mesfin A, Whiting S. Prevalence and factors associated with undernutrition among exclusively breastfeeding women in Arba Minch Zuria District, Southern Ethiopia: a cross-sectional community-based study. Ethiop J Health Sci. (2019) 29:913–22. doi: 10.4314/ejhs.v29i1.13
15. Almaw Derseh H, Zeleke L, Endalifer M, Muhammad E, Derso T. Undernutrition and associated factors among lactating mothers in Dega Damot Woreda, Northwest Ethiopia. J Nutr Metab. (2020) 2020:1–9. doi: 10.1155/2020/4627278
16. Seid A, Cherie H. Dietary diversity, nutritional status and associated factors among lactating mothers visiting government health facilities at Dessie town, Amhara region, Ethiopia. PLoS One. (2022) 17:1–14. doi: 10.1371/journal.pone.0263957
17. Gebre B, Biadgilign S, Taddese Z, Legesse T, Letebo M. Determinants of malnutrition among pregnant and lactating women under humanitarian setting in Ethiopia. BMC Nutr. (2018) 4:1–8. doi: 10.1186/s40795-018-0222-2
18. Das A, Saimala G, Reddy N, Mishra P, Giri R, Kumar A, et al. Mid-upper arm circumference as a substitute of the body mass index for assessment of nutritional status among adult and adolescent females: learning from an impoverished Indian state. Public Health. (2020) 179:68–75. doi: 10.1016/j.puhe.2019.09.010
19. Jeyakumar A, Ghugre P, Gadhave S. Mid-Upper-Arm Circumference (MUAC) as a Simple Measure to Assess the Nutritional Status of Adolescent Girls as Compared With BMI. Infant Child Adolesc Nutr. (2013) 5:22–5. doi: 10.1177/1941406412471848
20. Siddiqui F, Salam R, Lassi Z, Das J. The intertwined relationship between malnutrition and poverty. Front Public Health. (2020) 8:1–5. doi: 10.3389/fpubh.2020.00453
21. Blackwell N, Myatt M, Allafort-Duverger T, Balogoun A, Ibrahim A, Briend A. Mothers understand and can do it (MUAC): a comparison of mothers and community health workers determining mid-upper arm circumference in 103 children aged from 6 months to 5 years. Arch Public Health. (2015) 73:26. doi: 10.1186/s13690-015-0074-z
22. Kumar P, Sareen N, Agrawal S, Kathuria N, Yadav S, Sethi V. Screening maternal acute malnutrition using adult mid – upper arm circumference in resource – poor settings. Indian J Community Med. (2018) 43:132–4. doi: 10.4103/ijcm.IJCM_248_17
24. Ranganathan P, Pramesh C, Aggarwal R. Common pitfalls in statistical analysis: measures of agreement. Perspect Clin Res. (2017) 8:187–91. doi: 10.4103/picr.picr_123_17
25. Bekele H, Jima G, Regesu A. Undernutrition and associated factors among lactating women: community-based cross-sectional study in Moyale District, Borena Zone, Southern Ethiopia. Adv Public Health. (2020) 2020:1–10. doi: 10.1155/2020/4367145
26. Hechera Y, Dona A. Prevalence of undernutrition and its associated factors among lactating women in the Shebedino District, Sidama Regional State, Ethiopia. Inq J Heal Care Organ. (2022) 59:1–8. doi: 10.1177/00469580221087883
27. Olusegun F, Dare A, George M, Adebayo O. Effect of Conflict and Food Price Shocks on Calorie Intake and Acute Malnutrition in Nigeria: A Micro-Panel Data Analysis. Coventry: Warwick University (2019). 2229 p. doi: 10.22004/ag.econ.289676
28. Norman K, Hab U, Pirlich M. Malnutrition in older adults—recent advances and remaining challenges. Nutrients. (2021) 13:2764. doi: 10.3390/nu13082764
29. Gemede D, Wirtu D, Kenie D. Nutritional Status and associated factors among lactating mothers in nekemte referral hospital and health centers, ethiopia. Int J Nutr Food Sci. (2015) 4:216–22. doi: 10.11648/j.ijnfs.20150402.23
30. Berihun S, Kassa G, Teshome M. Factors associated with underweight among lactating women in Womberma woreda, Northwest Ethiopia; a cross-sectional study. BMC Nutr. (2017) 3:1–7. doi: 10.1186/s40795-017-0165-z
31. Weigel M, Armijos R, Racines M, Cevallos W. Food insecurity is associated with undernutrition but not overnutrition in ecuadorian women from low-income urban neighborhoods. J Environ Public Health. (2016) 2016:8149459. doi: 10.1155/2016/8149459
32. Rana M, Gautam A, Goli S, Uttamacharya, Reja T, Nanda P, et al. Planning of births and maternal, child health, and nutritional outcomes: recent evidence from India. Public Health. (2019) 169:14–25. doi: 10.1016/j.puhe.2018.11.019
33. Conde-Agudelo A, Rosas-Bermudez A, Castaño F, Norton M. Effects of Birth Spacing on Maternal, Perinatal, Infant, and Child Health: a Systematic Review of Causal Mechanisms. Stud Fam Plann. (2012) 43:93–114. doi: 10.1111/j.1728-4465.2012.00308.x
34. WHO. Essential Nutrition Actions: Improving Maternal, Newborn, Infant and Young Child Health and Nutrition. Geneva: WHO (2013).
35. Fufa D, Laloto T. Assessment of dietary diversity and associated factors among lactating mothers in Debub Bench District. Heliyon. (2021) 7:e07769.
36. Sebeta A, Girma A, Kidane R, Tekalign E, Tamiru D. Nutritional status of postpartum mothers and associated risk factors in Shey-Bench District, Bench-Sheko Zone, Southwest Ethiopia: a community based cross-sectional study. Nutr Metab Insights. (2022) 15:117863882210882. doi: 10.1177/11786388221088243
Keywords: lactating mothers, internally displaced people, Sekota, Ethiopia, undernutrition
Citation: Mengstie MA, Worke MD, Belay Y, Chekol Abebe E, Asmamaw Dejenie T, Abdu Seid M and Azezew MT (2023) Undernutrition and associated factors among internally displaced lactating mothers in Sekota camps, northern Ethiopia: A cross-sectional study. Front. Nutr. 10:1108233. doi: 10.3389/fnut.2023.1108233
Received: 25 November 2022; Accepted: 31 January 2023;
Published: 14 February 2023.
Edited by:
Yuxuan Gu, Nanjing Normal University, ChinaReviewed by:
Kazi Jamil, Kuwait Institute for Scientific Research, KuwaitBekahegn Girma, Dilla University, Ethiopia
Copyright © 2023 Mengstie, Worke, Belay, Chekol Abebe, Asmamaw Dejenie, Abdu Seid and Azezew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Misganaw Asmamaw Mengstie,  bWlzZ2FuYXcxMThAZ21haWwuY29t; orcid.org/000-0002-9711-8640
bWlzZ2FuYXcxMThAZ21haWwuY29t; orcid.org/000-0002-9711-8640
 Misganaw Asmamaw Mengstie
Misganaw Asmamaw Mengstie Mulugeta Dile Worke
Mulugeta Dile Worke Yalemshet Belay3
Yalemshet Belay3 Endeshaw Chekol Abebe
Endeshaw Chekol Abebe Tadesse Asmamaw Dejenie
Tadesse Asmamaw Dejenie Mohammed Abdu Seid
Mohammed Abdu Seid Muluken Teshome Azezew
Muluken Teshome Azezew