
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 14 February 2023
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1095523
This article is part of the Research Topic Nutrition and Sustainable Development Goal 2: Zero Hunger View all 24 articles
 Mohammedjemal Alyi1
Mohammedjemal Alyi1 Kedir Teji Roba2
Kedir Teji Roba2 Indeshaw Ketema2*
Indeshaw Ketema2* Sisay Habte2
Sisay Habte2 Abel Tibebu Goshu2
Abel Tibebu Goshu2 Ame Mehadi2
Ame Mehadi2 Yohannes Baye2
Yohannes Baye2 Behailu Hawulte Ayele3
Behailu Hawulte Ayele3Background: Acute malnutrition is a major global health problem primarily affecting under-five children. In sub-Saharan Africa, children treated for severe acute malnutrition (SAM) at an inpatient have high case fatality rate and is associated with relapse of acute malnutrition after discharge from inpatient treatment programs. However, there is limited data on the rate of relapse of acute malnutrition in children after discharge from stabilization centers in Ethiopia. Hence, this study aimed to assess the magnitude and predictors of relapse of acute malnutrition among children aged 6–59 months discharged from stabilization centers in Habro Woreda, Eastern Ethiopia.
Methods: A cross-sectional study was conducted among under-five children to determine the rate and predictors of relapse of acute malnutrition. A simple random sampling method was used to select participants. All randomly selected children aged 6–59 months discharged from stabilization centers between June 2019 and May 2020 were included. Data were collected using pretested semi-structured questionnaires and standard anthropometric measurements. The anthropometric measurements were used to determine relapse of acute malnutrition. Binary logistic regression analysis was used to identify factors associated with relapse of acute malnutrition. An odds ratio with 95% CI was used to estimate the strength of the association and a p-value less than 0.05 was considered statistically significant.
Results: A total of 213 children with mothers/caregivers were included in the study. The mean age in months of children was 33.9 ± 11.4. More than half (50.7%) of the children were male. The mean duration of children after discharge was 10.9 (± 3.0 SD) months. The magnitude of relapse of acute malnutrition after discharge from stabilization centers was 36.2% (95% CI: 29.6,42.6). Several determinant factors were identified for relapse of acute malnutrition. Mid-upper arm circumference less than 110 mm at admission (AOR = 2.80; 95% CI: 1.05,7.92), absence of latrine (AOR = 2.50, 95% CI: 1.09,5.65), absence of follow-up visits after discharge (AOR = 2.81, 95% CI: 1.15,7.22), not received vitamin A supplementation in the past 6 months (AOR = 3.40, 95% CI: 1.40,8.09), household food insecurity (AOR = 4.51, 95% CI: 1.40,15.06), poor dietary diversity (AOR = 3.10, 95% CI: 1.31,7.33), and poor wealth index (AOR = 3.90, 95% CI: 1.23,12.43) were significant predictors of relapse of acute malnutrition.
Conclusion: The study revealed very high magnitude of relapse of acute malnutrition after discharge from nutrition stabilization centers. One in three children developed relapse after discharge in Habro Woreda. Programmers working on nutrition should design interventions that focus on improving household food insecurity through strengthened public Safety Net programs and emphasis should be given to nutrition counseling and education, as well as to continuous follow-up and periodic monitoring, especially during the first 6 months of discharge, to reduce relapse of acute malnutrition.
Malnutrition is a major public health challenge faced by many developing countries (1, 2). It occurs when food intake is not balanced with the body’s dietary needs, particularly in vulnerable groups such as under-five children, pregnant and lactating mothers, and people with chronic illness (3, 4). It is a general term representing both undernutrition and overnutrition (5). Undernutrition contributes significantly to the global disease burden and is responsible for 35% of deaths in children (1).
Acute malnutrition is a life-threatening condition generally resulting from the recent rapid loss of weight or a failure to gain weight due to illness, reduced food intake, and inappropriate childcare practices or combinations of these factors (6). It is determined by the nutritional index of weight-for-height (WFH) and/or mid-upper arm circumference (MUAC) and categorized into moderate acute malnutrition (MAM) and severe acute malnutrition (SAM) (7). SAM is one of the top nutrition-related causes of death in children worldwide (8). Globally, over 49 million under-five children were wasted, and nearly 17 million were severely wasted, with the largest number being found in South Asia (68%) and Africa (28%) (9, 10).
In Ethiopia, SAM is a serious public health problem that poses a significant obstacle to achieving better child health outcomes (11). Despite a substantial decline in the proportion of wasting (7%), stunting (37%), and underweight (21%) in the last two decades, undernutrition in children is still a common problem in Ethiopia (12–14). A previous study conducted in Haramaya district, Ethiopia indicated that about 14, 36, and 23% of children were wasted, stunted and underweighted, respectively (15).
According to the community-based management of acute malnutrition (CMAM) guidelines, children with failed appetite, and/or with a major medical complication and infants under 6 months with bilateral pitting edema or visible wasting should be initially admitted to inpatient treatment programs. Whereas those children with a good appetite, no major medical complications or edema, and no marasmic-kwashiorkor should be linked to outpatient treatment programs (OTP) (16). The protocol for the management of acute malnutrition also recommends that children should be periodically monitored after discharge from the treatment programs (1, 2).
The literature shows that high mortality rate of SAM in children after being discharged from inpatient treatment programs (17–20). Several factors are identified for the relapse, including living in settings of pervasive poverty, low women literacy, food insecurity, inadequate water and sanitation, incomplete vaccination and poor follow-up after discharge (21–23).
In sub-Saharan Africa, children treated as an inpatient with SAM have 10 to 40% case fatality (24). A previous study in Ethiopia showed that 29% of children treated in a Stabilizing center died from SAM (25). Evidence indicates that SAM children discharged as recovered may relapse following exit from CMAM programs (26). For instance, a previous study conducted in Ethiopia showed that 34% of children relapse after being discharged from a CMAM program (27).
Despite the high burden of acute malnutrition in Ethiopia, there is limited data on the rate of relapse of acute malnutrition among children discharged from healthcare facilities after being managed for nutritional problems. Therefore, this study aimed to determine the prevalence of relapse of acute malnutrition and associated factors among 6–59 months old children after discharge from stabilization centers in Habro Woreda, Eastern Ethiopia.
The study was conducted in Habro Woreda from December 15, 2020 to January 15, 2021. Habro Woreda is one of the 15 woredas in the West Hararghe zone of Oromia Regional State, Eastern Ethiopia. Its administrative office is found in Gelemso town, which is located 400 km from Addis Ababa, the capital city of Ethiopia, to the east. The Woreda has 37 kebeles and an estimated total population of 269,279, with an estimated 44,242 under-five children and 55,100 households. There are 7 health centers and 1 general hospital providing nutrition stabilization services in the woreda.
A cross-sectional study was employed to determine the rate of relapse of acute malnutrition and associated factors among children aged 6–59 months previously treated for SAM and discharged as recovered between June 2019 and May 2020 in Habro Woreda. The source population were children aged 6–59 months discharged recovered from SC in Habro Woreda and the study population were those 6–59 months old children following discharge as recovered in the randomly selected kebeles of Habro Woreda. All randomly selected children aged 6–59 months who were discharged recovered 6 months prior to the data collection period with mothers/caregivers who gave consent were included. Children who had incomplete address information on the SC registration logbooks and children with physical deformities during anthropometric measurements were excluded.
The sample size for the first objective was determined using a single population proportion formula with the assumptions of a 15.4% prevalence of relapse of acute malnutrition from a previous study (23), 95% CI, 5% margin of error and 10% non-response rate, yielding the sample size of 220. The sample size for the second objective was calculated using Epi–info version 7.0 by considering various factors associated with relapse of acute malnutrition including the educational status of women (28), follow-up visits after discharge (29), vitamin A supplementation within the last 6 months (27) and pre-lacteal feeding (27) with the assumptions of 95% confidence level, power of 80% and 10% non-response rate, yielding the sample size of 130, 143, 224, and 156, respectively. Finally, the final sample size required for this study was determined by taking the largest sample size observed in the second objective which was 224.
Out of 37 kebeles found in Habro Woreda, 20 kebeles were selected randomly (by lottery method). All malnutrition cases previously admitted for SAM treatment and discharged from seven health centers (Balbeletti, Firi Jiru, Dereku, Gelemso, Wayne Gudo, Ceffe, and Wachu) and Gelemso General Hospital in the selected kebeles of Habro Woreda were traced from SAM records/registration logbooks. The total records of SAM children discharged from SC in selected kebeles with complete information were 297. The total cases of all records of SAM children were allocated to each selected kebele based on their addresses from registration logbooks. The households of each study participant were accessed with health extension workers (HEW) working in each kebele using lists of addresses from registration logbooks. The sampling frame was prepared using children’s serial numbers obtained from registration logbooks. Finally, after proportionally allocating the sample size to each selected kebele based on the number of malnutrition cases, the study participants were selected using a simple random sampling technique.
A pretested validated semi-structured questionnaire adapted from relevant literature (27, 30, 31) and tailored to the study variables was used to collect data. The questionnaire was initially developed in English and translated to the local languages (Afan Oromo and Amharic) and then re-translated into English by language experts to check for consistency. The questionnaire has six (6) parts: Socioeconomic and demographic characteristics (age, sex, place of residence, family size, mother’s occupation, educational status of parents, and family wealth index), anthropometric measurements, previous clinical characteristics, child feeding characteristics, household food security status and housing conditions. Data were collected by trained data collectors and supervisors through face-to-face interviews with mothers/caretakers and anthropometric measurements. Information on clinical data during the treatment period was collected retrospectively from SAM records. To identify the history of morbidity, mothers were asked for any occurrence of illness during the past 2 weeks. Children’s vaccination status was checked by observing their immunization card and if not available, mothers were asked to recall the child’s vaccination. BCG vaccination was also checked if any scar existed on a child’s arm.
Was considered in a child whose MUAC is <125 mm and/or WFH < −2SD and/or the presence of bilateral pitting edema after discharge from inpatient treatment programs. Children whose WFH is < −2SD and/or MUAC 115 to <125 mm were categorized as MAM, whereas children whose WFH < −3SD and/or MUAC < 115 mm were considered SAM (32).
Height and weight were measured following standard techniques by using calibrated instruments, and recorded to the nearest 0.1 cm and 0.1 kg, respectively. The height for children less than 2 years was measured by gently placing a child on his/her back in the middle of the board, facing straight up with shoulder blades, buttocks, and heels touching the surface of the height board and knees fully straight, arms stretched on the child’s sides and feet at right angles. Whereas for children 2 years or older, was measured while a child is standing upright in the middle of the height board with arms at the sides, knees straight and the child’s head, shoulders, buttocks and heels touching the board, and feet close together (16, 33–35). MUAC was measured following recommended steps using a color-coded tape. Presence of edema was assessed, recorded and categorized using recommended procedures. Children whose WFH is below minus two standard deviations (−2SD) and/or MUAC < 125 mm, with/without pitting edema were considered acute malnutrition (7, 32, 36).
Was determined by summing different food groups consumed using a 24-h recall period. A total of eight food groups were used to guide the scoring as per food items consumed. The participants received “1” point if they consumed a minimum of one food item within each subgroup, and “0” point if they did not. Finally, the DDS was computed and categorized as high for a score ≥6, medium for a score of 4–5, and low for a score of ≤3 (37).
Was determined using nine standard Household Food Insecurity Access Scale (HFIAS) questions: an occurrence question followed by the frequency of occurrence of the events. Prior to assigning the food insecurity access, each frequency of occurrence responses was coded as “0” for all cases where the answer to the corresponding occurrence question was “no” and then the four food security categories were created sequentially as recommended by Food and Nutrition Technical Assistance (FANTA) (38). Finally, the HFIAS category one (1) was considered as food secure and the remaining as food insecure.
Was computed using Principal Component Analysis (PCA) as a composite indicator of household living standards. Finally, the wealth tercile was performed and categorized as higher, medium, and lower (39, 40).
A pretested validated semi-structured data collection tool was adopted after a review of related literature to ensure data quality. Two days training were given to data collectors and supervisors on the objectives of the study, the contents of data collection tools, anthropometric measurements, and how to collect and record data appropriately. A pretest was conducted on 5% of the sample size before the actual data collection period to check for the reliability and validity of data collection tools. The collected data were carefully checked for completeness, accuracy and consistency by supervisors and the principal investigator on daily basis. Double data entry was done by two individuals to minimize errors.
The collected data were categorized, coded and entered into Epi-Data version 3.1 and analyzed using STATA software version 14.2. Texts, tables, and figures were used to display descriptive and summary statistics. Binary logistic regression analysis was conducted to identify factors associated with relapse of acute malnutrition. Initially, bivariate logistic regression analysis was conducted to determine the candidate variables for the multivariate logistic regression analysis. The Logistic regression model fitness was checked using Hosmer-Lemeshow and indicates fitted for the model. Multicollinearity was checked (VIF < 10) indicating non-existence of multicollinearity among variables. Variables with a p-value < 0.20 were fitted into a multivariate logistic regression analysis to identify factors significantly associated with relapse of acute malnutrition. Both crude and adjusted odds ratio along with 95% CI was estimated to measure the strength of the association. Finally, a p-value < 0.05 at 95% confidence interval (CI) was considered statistically significant.
A total of 213 children aged 6–59 months with mothers/caregivers were included in the study, giving a response rate of 95.1%. The majority (34.3%) of children were aged 36–47 months with a mean age of 33.9 ± 11.4 months. More than half (50.7%) of the children were male and the majority (83.1%) were rural residents. Regarding mother related variables, more than a quarter (30.9%) were in the age group of 30–34 years with a mean age of 31.3 ± 5.3 years. Nearly three-fourths (74.6%) of mothers were homemakers and the majority (86.8%) had never attended formal education. In this study, 28.6 and 10.8% of the households were mildly and severely food insecure, respectively. The mean dietary diversity score of participants was 4.1 (± 1.3 SD). In the current study, 46% of children ate less than four food groups in the preceding 24-h (Table 1). The most commonly consumed food groups were cereals (98%), fruits and vegetables (74%), legumes (62.4%), and dark green leafy vegetables (55.9%) (Figure 1).
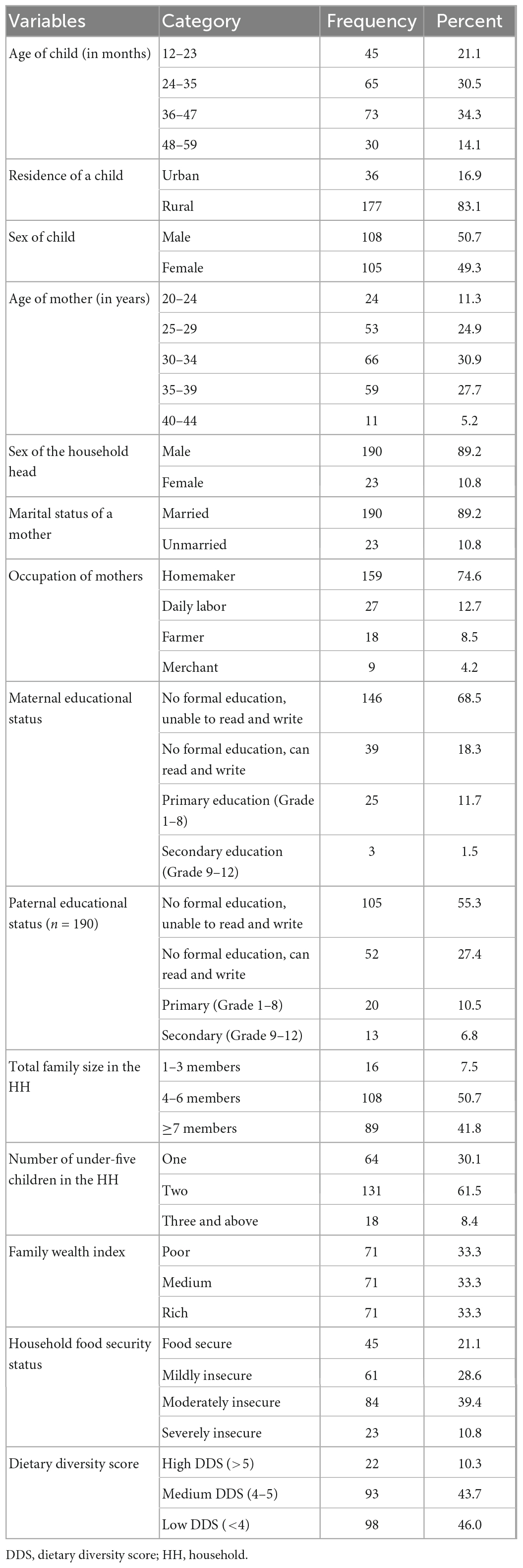
Table 1. Socioeconomic and demographic characteristics of the study participants in Habro Woreda, Eastern Ethiopia, 2021 (N = 213).
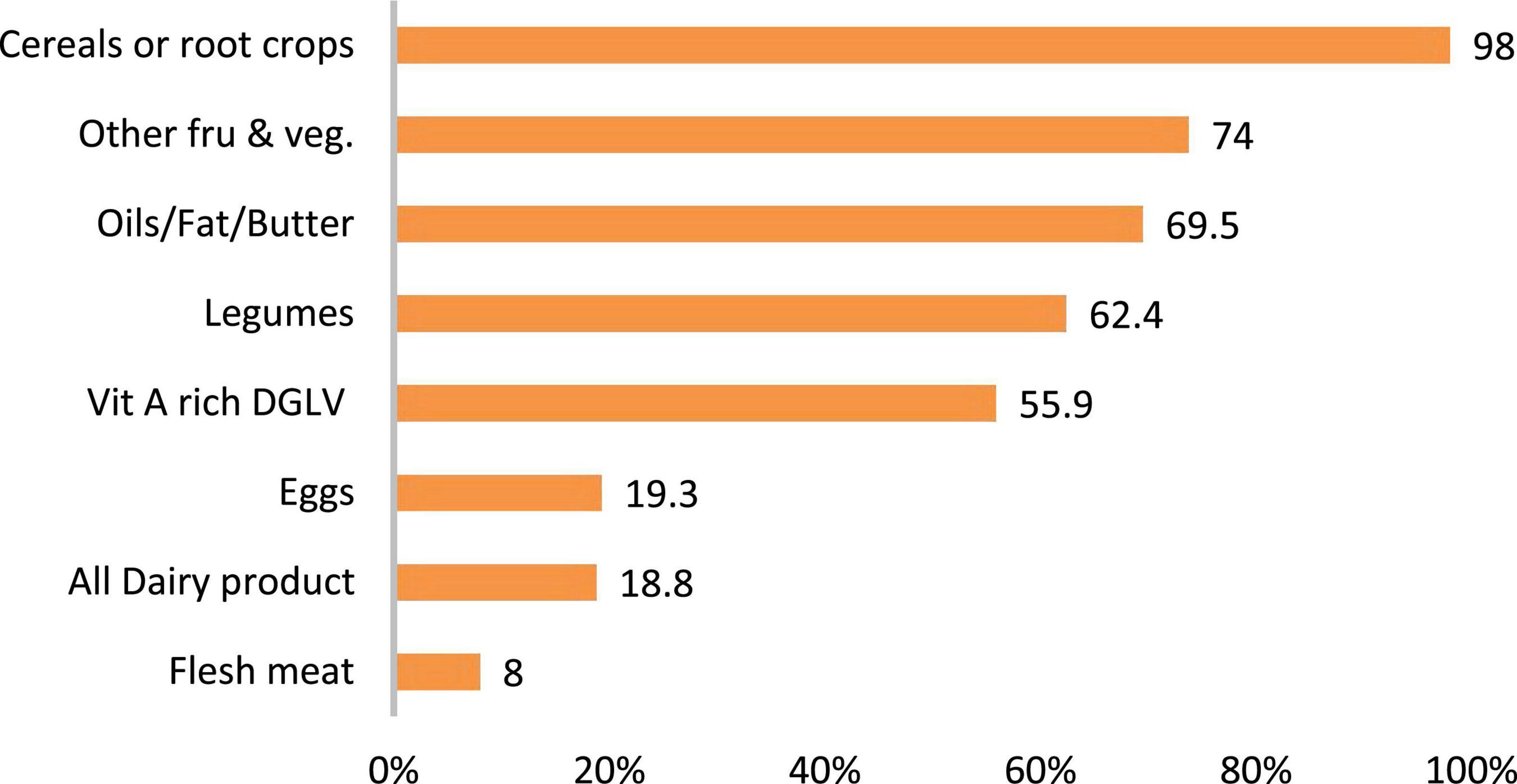
Figure 1. Percentage of food groups consumed by the children in the past 24-h in Habro Woreda, Eastern Ethiopia, 2021 (n = 213). DGLV, dark green leafy vegetables.
The mean duration of study participants after discharge was 10.9 ± 3.0 months. Among the study participants, more than a quarter (27.7%), 47.9 and 11.3% of children had MUAC < 110 mm, severe marasmic and bilateral pitting edema at admission, respectively. The length of stay in the facility was ranging from 3–22 days with an average of 8.4 ± 3.3 days. In this study, nearly half (48.4%) of the children were discharged in the first week of admission. Of discharged children, the majority (88.3%) were transferred to the OTP and only 42.3% of the children were visited by healthcare workers after discharge. Regarding the immunization status, 74.7% of children were fully vaccinated, and 67.1% received vitamin A supplementation in the preceding 6 months (Table 2).
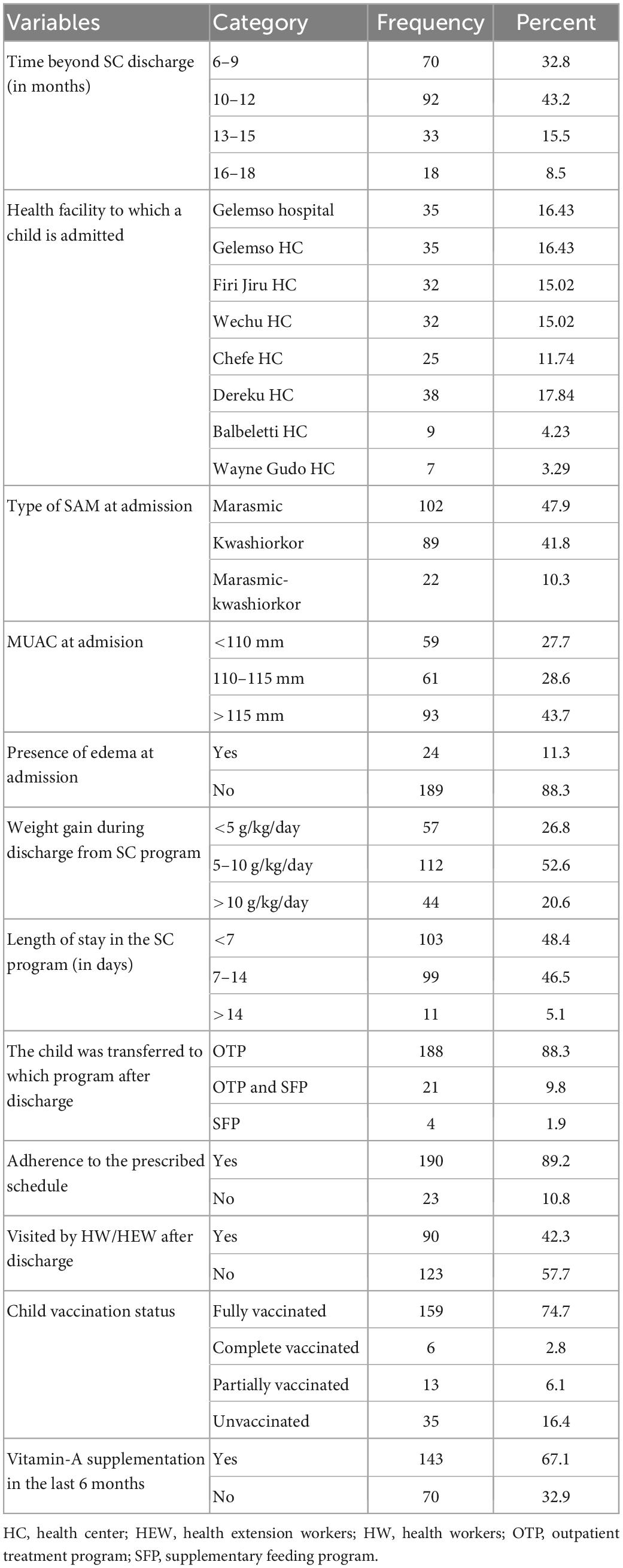
Table 2. Clinical characteristics of children discharged from SAM stabilization centers in Habro Woreda, Eastern Ethiopia, 2021 (N = 213).
Almost all (99.5%) mothers had ever breastfed their children, and 17.8% were still breastfeeding during the survey. Among currently breastfeeding mothers, 86.8% breastfed their children eight and more times in 24-h. About 77% of children were exclusively breastfed for 6 months, with an average duration of 5.8 (± 1.2 SD) months. More than three-quarters (79.8%) began complementary feeding between 6 and 9 months and 49.8% fed their children less than four times per day (Figure 2). In the present study, 65.3% of the households had latrines and 56.8% got drinking water from piped sources. Less than one-third (30.5%) of the households were getting their food from agricultural production, and there was no food supply for half (49.8%) at the time of the survey (Table 3).
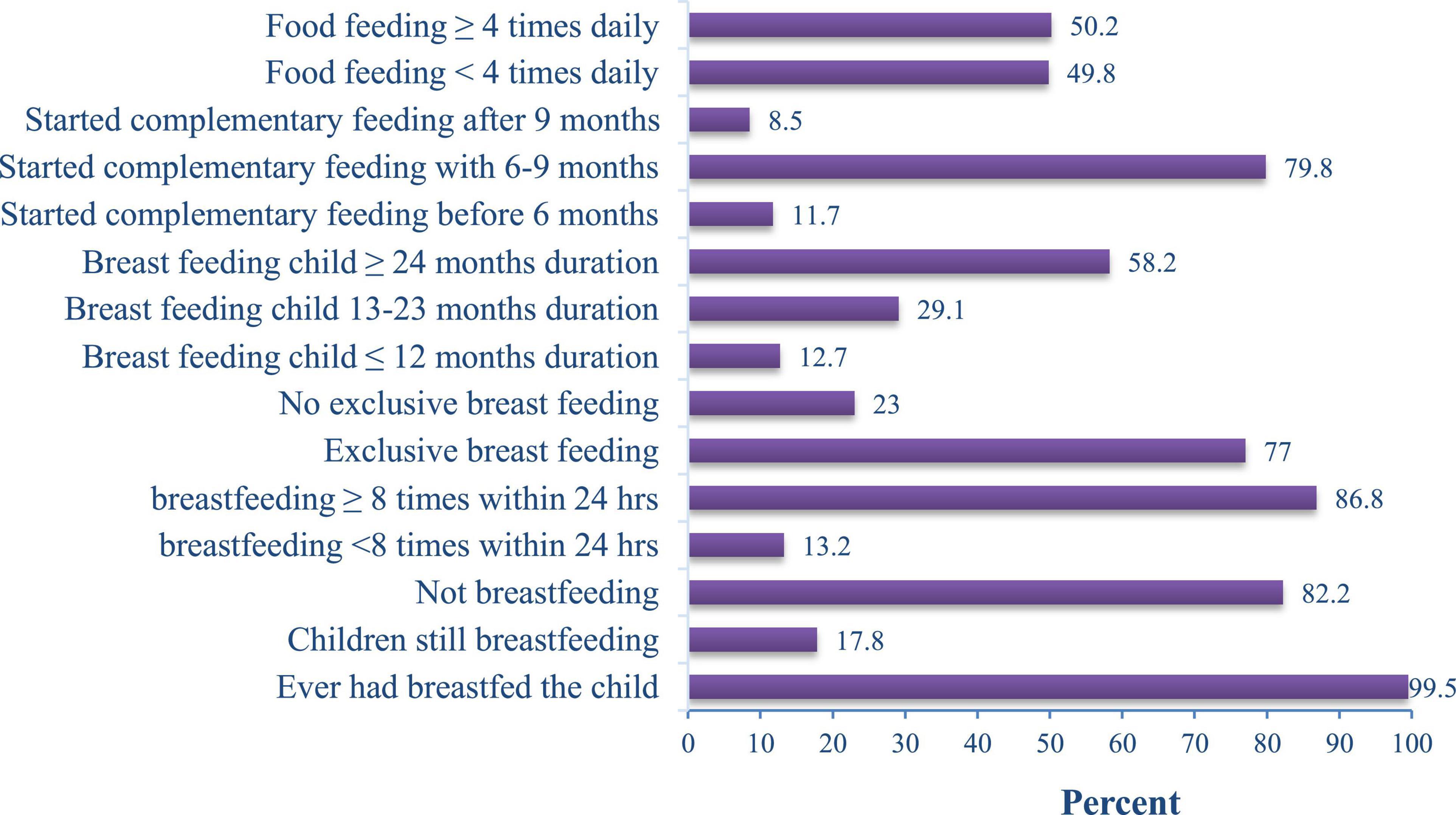
Figure 2. Child feeding practice of mothers/caregivers in Habro Woreda, Eastern Ethiopia, 2021 (n = 213).
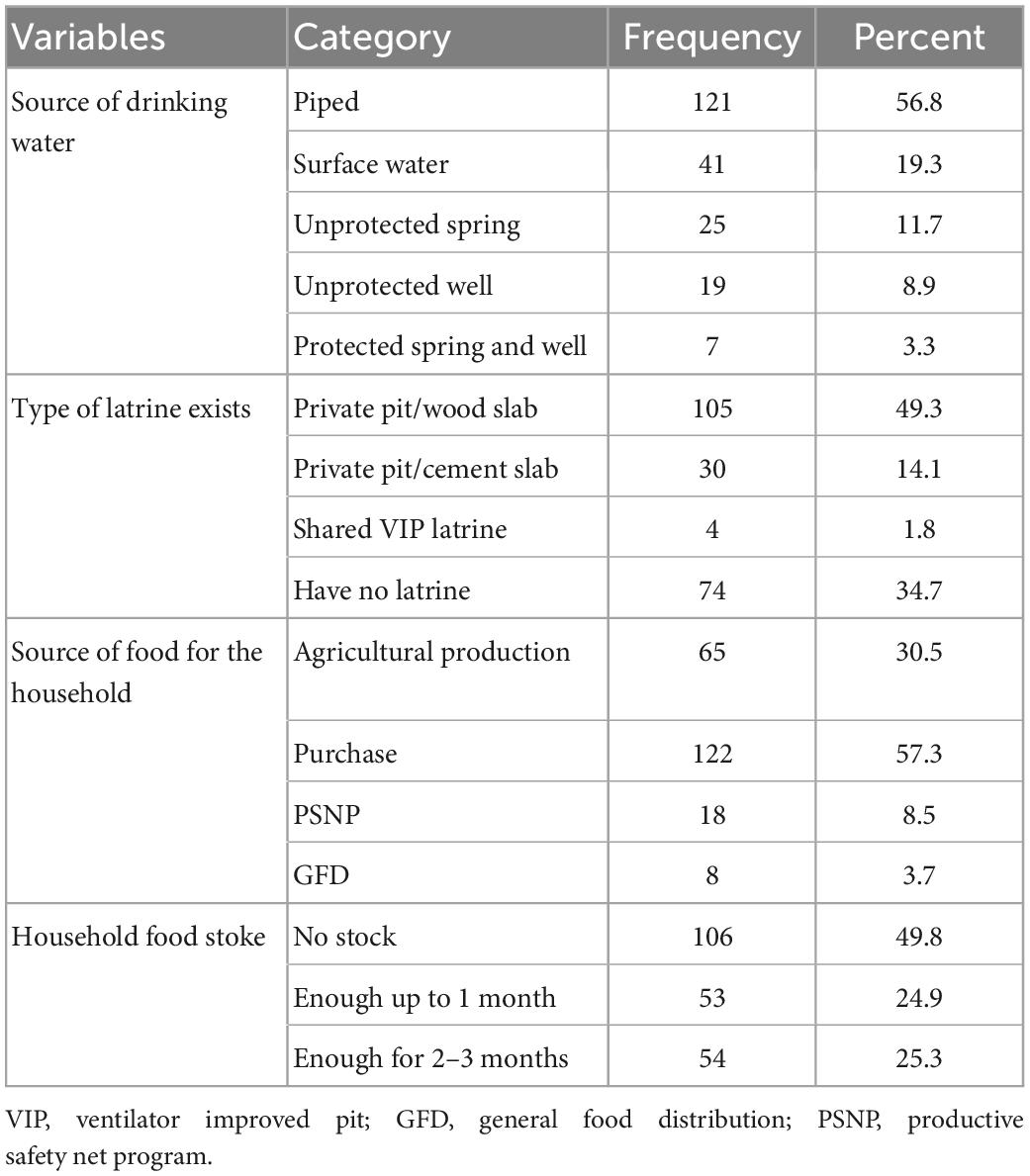
Table 3. Housing conditions of house-holds of children discharged from SAM stabilization centers in Habro Woreda, Eastern Ethiopia, 2021 (N = 213).
In the current study, 48.8% of children had been sick in the previous two weeks. The mean duration of the child illness was 8.8 (SD ± 8.4) days. Among the sick children, 47.1 and 50% had diarrhea and cough, respectively. Nearly three-fourths (73.1%) of mothers with sick babies sought advice, and 71% of them got advice from healthcare providers (Figure 3).
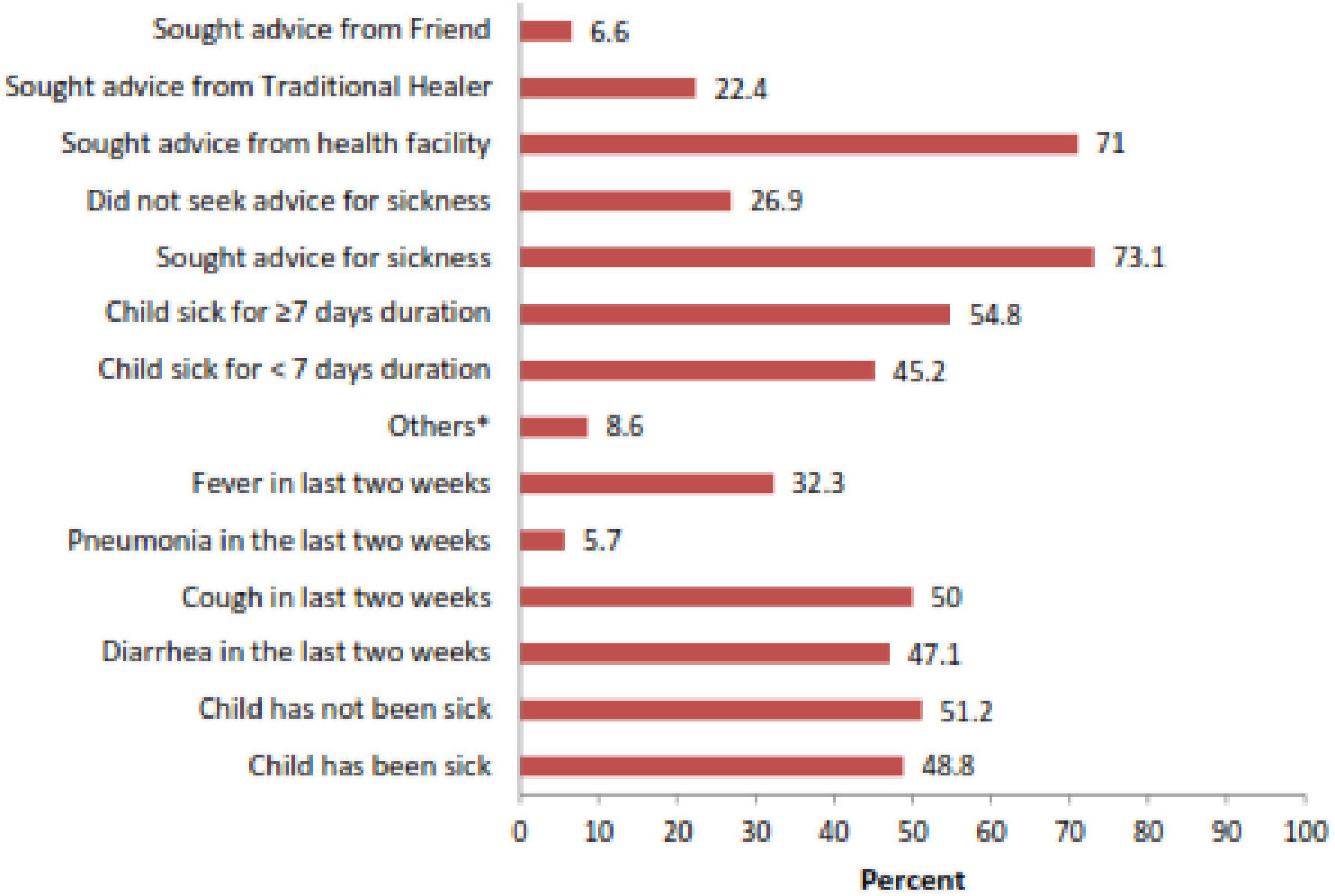
Figure 3. Morbidity status and Health-seeking behavior of the study participants in Habro Woreda, Eastern Ethiopia, 2021 (n = 213). *Others: burns, vomiting, ear infection, and scabies.
The overall magnitude of relapse of acute malnutrition among children following discharge from SC was found to be 36.2% [95% CI: 29.6,42.6]. Among acutely malnourished children, 13.6% were severely malnourished and 4.2% had bilateral pitting edema. In the current study, 53.1 and 48.4% of the children were stunted and underweighted, respectively (Figure 4).
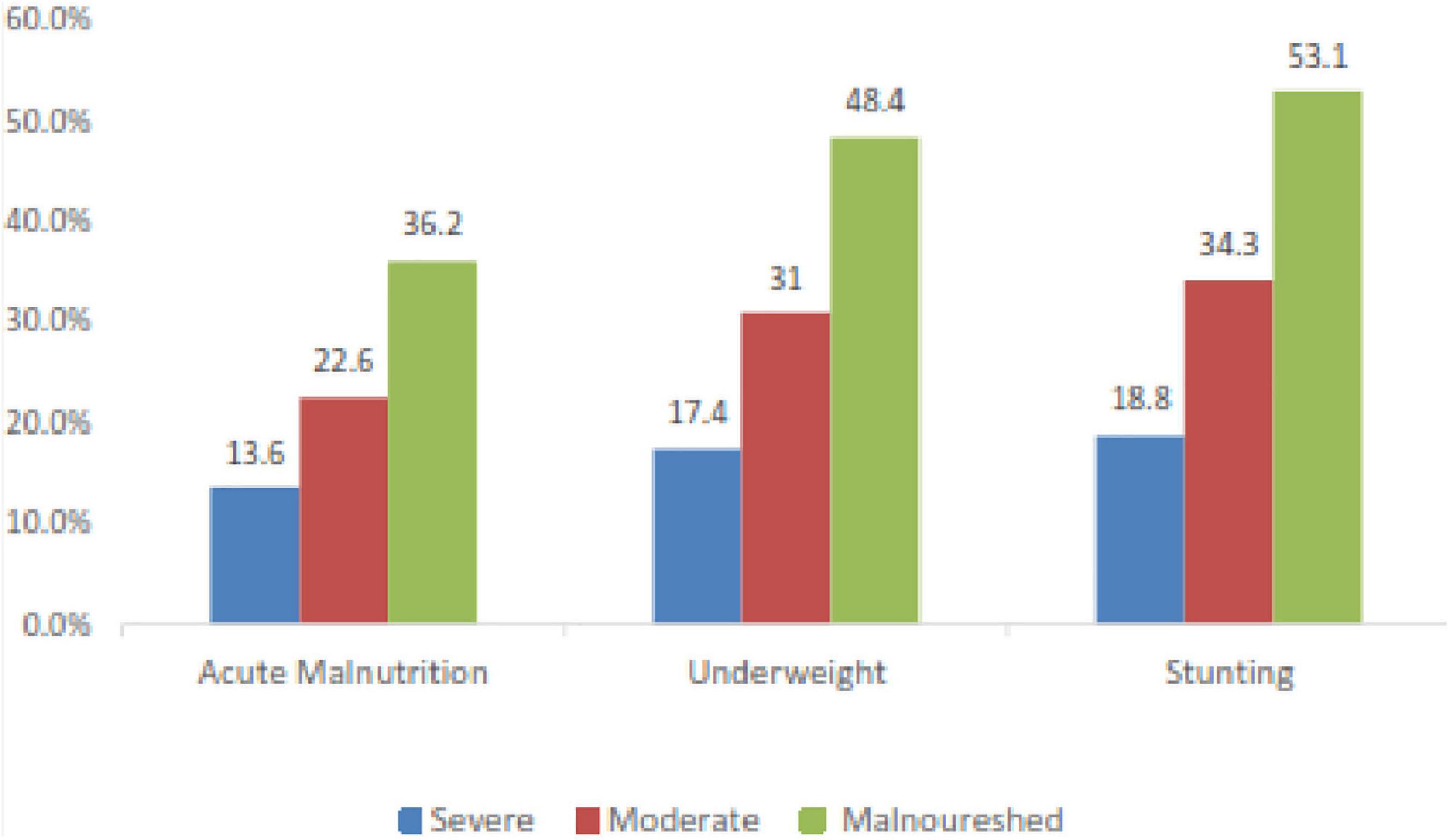
Figure 4. Nutritional status of children discharged from SAM stabilization centers in Habro Woreda, Eastern Ethiopia, 2021 (n = 213).
In the multivariate logistic regression analysis, MUAC at admission, latrine availability, follow-up visits after discharge, vitamin A supplementation in the past 6 months, household food security status, dietary diversity, and wealth index were significantly associated with relapse of acute malnutrition. In the current study, the odds of relapse of acute malnutrition among children admitted with MUAC < 110 mm was [AOR = 2.80; 95% CI: 1.05, 7.92] and children from households with no latrines were 2.5 times [AOR = 2.50; 95% CI: 1.08,5.65] more acutely malnourished than their counterparts. Children who were not visited by healthcare workers after discharge and not supplemented with vitamin A in the past 6 months were 2.81 times [AOR = 2.81; 95% CI: 1.15,7.22] and 3.4 times [AOR = 3.40; 95% CI: 1.40,8.09] more acutely malnourished than their counterparts, respectively. Similarly, children whose dietary diversity was less than four food groups were 3.1 times [AOR = 3.10; 95% CI: 1.31,7.33] more acutely malnourished than children who had greater than or equal to four food groups. In addition, children from food-insecure households were 4.51 times [AOR = 4.51; 95% CI: 1.40,15.06] more acutely malnourished than their counterparts. Moreover, the odds of relapse of acute malnutrition among the poorest wealth quintile was [AOR = 3.90; 95% CI: 1.23, 12.43] (Table 4).
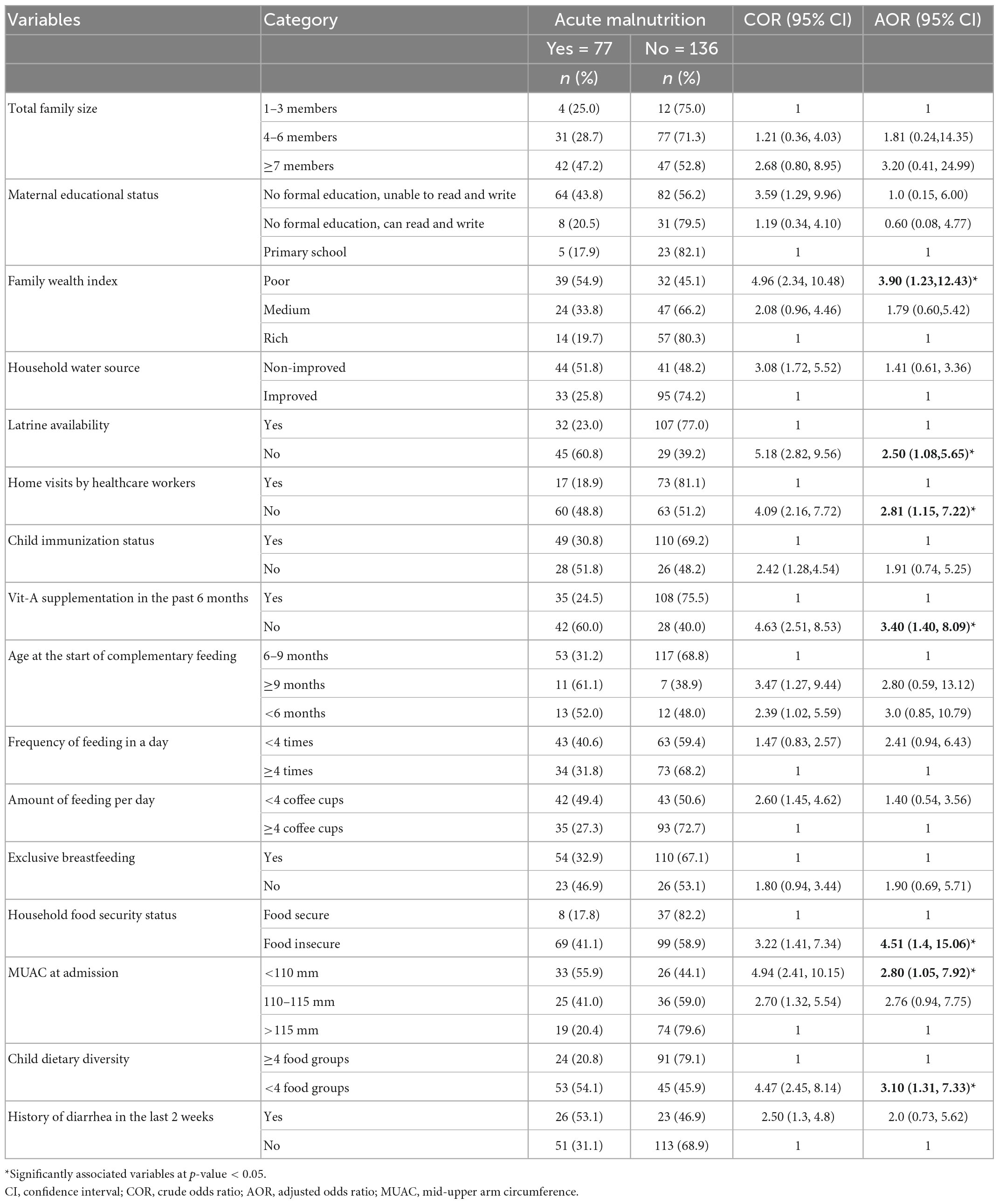
Table 4. Factors associated with relapse of acute malnutrition among children discharged from stabilization centers in Habro Woreda, Eastern Ethiopia, 2021 (N = 213).
In the current study, children were assessed after an average of 10.9 months of discharge. Variables such as MUAC at admission, follow-up visits after discharge, dietary diversity, household food security status, vitamin A supplementation in the past 6 months, latrine availability and wealth index were identified as being associated with relapse of acute malnutrition.
One in three children was acutely malnourished after discharge from inpatient treatment programs in this study. This finding is consistent with studies conducted in the South Gondar zone, Ethiopia (27), and the Democratic Republic of Congo (41). However, is lower than the finding of study from Kenya (42). The discrepancy could be due to the small sample size in the current study, the difference in study design and length of time after discharge. In disparity, is higher than the findings from Burkina Faso (23), Nigeria (43), and Bangladesh (29). The reason for discrepancy could be due to the difference in sample size, nutrition intervention after discharge and socioeconomic characteristics. This suggests the requirement for appropriate nutrition education, counseling and follow-up of care after discharge to reduce the burden of relapse.
Children with MUAC < 110 mm at admission were more likely to relapse acute malnutrition than their counterparts. This finding is consistent with studies conducted in Burkina Faso (23), Nigeria (44), and Nepal (45). The possible reason for this consistency could be, children admitted for SAM treatment and discharged as recovered might have chances to develop a new episode of acute malnutrition. Continued nutritional support, potentially in the form of a supplementary feeding program, may contribute to lower acute malnutrition rates (46).
In the current study, the absence of latrine was associated with relapse of acute malnutrition. Children from households with no latrine were more acutely malnourished than their counterparts. This finding is supported by the study conducted in the Afar region, Ethiopia (4). This could be, due to the fact that good sanitation could prevent contamination of the environment by excreta and the transmission of pathogens from the feces of an infected person to a new host (47). In contrast, poor environmental sanitation is an important cause of infectious diseases, especially diarrhea and intestinal parasite; which contributes to malnutrition (48).
According to the WHO recommended schedules, children discharged from inpatient programs should be followed by healthcare workers at 1, 3 and 6 months, and then twice yearly until the child is at least three years old (1). However, such a follow-up was not routinely done in the current study. Children who were not visited by healthcare workers after discharge were more acutely malnourished than their counterparts. This finding is supported by the study conducted in the South Gondar zone, Ethiopia (27). The result indicates that follow-up visits after discharges are very crucial for the successful management of acute malnutrition, since some cases relapsed or developed comorbidities during this period. This might be due to lack of organized or insufficient capacity of health system to follow-up after discharges. Even though there are health extension workers in this setting, there might be lack of coordination and communication gap between health extension workers and health facilities providing inpatient treatment of SAM.
In the current study, children who did not receive vitamin-A supplementation in the past 6 months were more acutely malnourished than their counterparts. This finding is similar to the study conducted in the South Gondar zone, Ethiopia (27). This could be, due to the protective role of vitamin A in promoting and regulating activities in both the inborn and adaptive immune system, thus enhancing immune function, is a rationale for supplementing every 6 months (49, 50).
Children whose dietary diversity was below four food groups were more acutely malnourished compared to children with greater than or equal to four diversified foods. This finding is consistent with studies conducted in Pakistan and Bangladesh (19, 51). The reason for this consistency could be that a household’s capability to acquire necessary foods and general availability of food is a precondition to achieving the diversification of children’s diets (52). Overall, children’s food in this study seemed monotonous, primarily cereal-based. Additionally, since children are in a period of rapid growth and development, failure to supply adequate and diversified food for daily bodily demands would result in growth faltering. In the current study, relapse of acute malnutrition after discharge was related to household (HH) food insecurity status. The odds of relapse among children in food insecure HHs was higher than in food secure HHs. This finding is in line with studies conducted in the Jimma zone, Ethiopia (14), South Gondar zone, Ethiopia (27), and Nigeria (53). Food insecurity can be linked to insufficient intake of diversified foods and studies have reported consumption of less diversified food as being associated with acute malnutrition (14). In addition, children who have a practice of feeding less diversified diet are easily exposed to infection due to poor immunity.
The low socioeconomic status of the HH increased the likelihood of being more acutely malnourished. In the present study, children from HHs with poor wealth index were more acutely malnourished than children from HHs with high wealth index. This finding agreed with studies conducted in Haramaya district, Ethiopia (15), Hawassa, Ethiopia (28), and India (54). This could be justified by, the low-income levels of the HHs limiting the type and the amounts of food available for consumption which in turn may lead to feed children less diversified diets.
Despite these important merits, the study had some limitations. Primarily, due to the nature of the cross-sectional study design, it was difficult to establish the cause-effect relationship between the study variables. Secondly, the small sample size used in the study may not represent a larger population. In addition, recall bias was one of the limitations of the study since some questions were asked about the events that occured 24-h back. This was minimized by probing the respondents about the events.
The magnitude of relapse of acute malnutrition following discharge from inpatient treatment programs was very high. One in three children was acutely malnourished after discharge in Habro Woreda, Eastern Ethiopia, alarming for the requirements of appropriate nutrition education, counseling and follow-up of care. MUAC at admission, follow-up visits after discharge, dietary diversity, household food security status, vitamin A supplementation in the past 6 months, latrine availability, and wealth index were predictors of relapse of acute malnutrition. Therefore, programmers and stakeholders working on nutrition should design interventions that focus on improving household food insecurity through public Safety Net programs should be strengthened, and nutrition counseling and education, are crucial to protect children against post-discharge relapse of acute malnutrition. Moreover, healthcare workers should give due emphasis to organized continuous follow-up and periodic monitoring for early detection of those at risk of relapse, especially during the first 6 months of discharge, to reduce and control the risk of relapse of acute malnutrition. The relapse rate should be a performance indicator of stabilization centers. Furthermore, a study that focuses on operational and behavioral change is recommended to fill the gap in the study area.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The study was conducted following the principles of the Helsinki Declaration. The studies involving human participants were reviewed and approved by Haramaya University, College of Health and Medical Sciences Institutional Health Research Ethics Review Committee (IHRERC). Written informed consent to participate in this study was provided by the participants or their legal guardian/caretakers of the children.
MA, BHA, and KTR conceived, designed the study, acquired the data, analyzed, and interpreted the findings. IK, SH, ATG, YB, and AM revised and provided the critical intellectual feedback. AM and IK drafted the manuscript. All authors have read and approved the final manuscript for submission.
This study was financially supported by the Haramaya University. The funder had no role in the study selection, data collection, analysis, conclusion, and interpretation of the study.
Firstly, we would like to forward our kindest regards to the study participants. Secondly, we would like to express our gratitude to Haramaya University, College of Health and Medical Sciences for providing minimal financial support. We also extend our thanks to data collectors and supervisors; they are the backbone to finalize the reports.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; HAZ, height for age Z-score; MUAC, mid-upper arm circumference; OTP, outpatient treatment program; WHZ, weight for height Z-score; HW/HEW, healthcare workers/health extension workers.
1. World Health Organization [WHO]. Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children. Geneva: World Health Organization (2013).
2. Welfare NRHMaf. Guidelines for Management of Severe Acute Malnutrition (SAM) Children at Nutrition Rehabilitation Center. Tamil Nadu: National Rural Health Mission (2012). p. 1–68.
3. Picot, J, Hartwell D, Harris P, Mendes D, Clegg A, Takeda A. The effectiveness of interventions to treat severe acute malnutrition in young children: A systematic review. Health Technol Assess. (2012) 16:1–316. doi: 10.3310/hta16190
4. Gizaw Z, Woldu W, Bitew B. Acute malnutrition among children aged 6–59 months of the nomadic population in Hadaleala district, Afar region, northeast Ethiopia. Italian J Pediatr. (2018) 44:21. doi: 10.1186/s13052-018-0457-1
5. European Commission. DG ECHO Thematic Policy Document No. 4 Nutrition: Addressing Nutrition in Emergencies. Brussels: European Commission (2013).
6. WFP. Nutrition at the World Food Programme: Programming for Nutrition-Specific Interventions. Italy: WFP Rome (2012).
7. Golden M, Grellety Y. Guidelines for the Management of the Severely Malnourished. New York, NY: ACF International (2006).
8. Olofin I, McDonald C, Ezzati M, Flaxman S, Black R, Fawzi W. Associations of suboptimal growth with all-cause and cause-specific mortality in children under five years: A pooled analysis of ten prospective studies. PLoS One. (2013) 8:e64636. doi: 10.1371/journal.pone.0064636
9. UNICEF/WHO/WBG. Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition. Geneva: WHO (2021).
10. Black R, Allen L, Bhutta Z, Caulfield L, de Onis M, Ezzati M, et al. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet. (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
11. Alemu M, Nicola J, Bekele T. Tackling Child Malnutrition in Ethiopia: Young Lives Project Working Paper No 19. London: Save the Children UK (2005).
12. Central Statistical Agency. Ethiopia Mini Demographic and Health Survey 2014. Addis Ababa: Central Statistical Agency (2014).
13. Ethiopian Public Health Institute [EPHI] (Ethiopia), ICF. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. Rockville, Maryland, USA. Rockville, MD: EPHI and ICF (2019).
14. Miskir A, Godana W, Girma M. Determinants of acute malnutrition among under-five children in Karat Town Public Health Facilities, Southern Ethiopia: A case-control study. Qual Primary Care. (2017) 25:242–52.
15. Redi F, Egata G, Kedir A. Prevalence of malnutrition among children aged 6-59 in Haramaya district, Oromia, Ethiopia. J Biometr Biostatistics. (2017) 8:1–4. doi: 10.4172/2155-6180.1000357
16. Federal Ministry of Health. Protocol for the Management of Severe Acute Malnutrition. Addis Ababa: Federal Ministry of Health (2007).
17. Berkley JA, Ngari M, Thitiri J, Mwalekwa L, Timbwa M, Hamid F, et al. Daily co-trimoxazole prophylaxis to prevent mortality in children with complicated severe acute malnutrition: A multicentre, double-blind, randomised placebo-controlled trial. Lancet Glob Health. (2016) 4:e464–73. doi: 10.1016/S2214-109X(16)30096-1
18. Chisti M, Salam M, Ashraf H, Faruque A, Bardhan P, Shahid A, et al. Prevalence, clinical predictors, and outcome of hypocalcaemia in severely-malnourished under-five children admitted to an urban hospital in Bangladesh: A case-control study. J Health Popul Nutr. (2014) 32:270.
19. Dale N, Salim L, Lenters L, Sadruddin S, Myatt M, Zlotkin S. Recovery and relapse from severe acute malnutrition after treatment: A prospective, observational cohort trial in Pakistan. Public Health Nutr. (2018) 21:2193–9. doi: 10.1017/S1368980018000745
20. Kerac M, Seal A. Preventing acute malnutrition in young children: Improving the evidence for current and future practice. PLoS Med. (2014) 11:e1001715. doi: 10.1371/journal.pmed.1001715
21. Chang C, Trehan I, Wang R, Thakwalakwa C, Maleta K, Deitchler M, et al. Children successfully treated for moderate acute malnutrition remain at risk for malnutrition and death in the subsequent year after recovery. J Nutr. (2013) 143:215–20. doi: 10.3945/jn.112.168047
22. Nyirenda G, Belachew T. Concern Worldwide Final Evaluation of National CMAM Programme Ethiopia. Ethiopia: Valid International & Jimma University (2010).
23. Somassè Y, Dramaix M, Bahwere P, Donnen P. Relapses from acute malnutrition and related factors in a community-based management programme in Burkina Faso. Matern Child Nutr. (2016) 12:908–17. doi: 10.1111/mcn.12197
24. Tickell K, Denno D. Inpatient management of children with severe acute malnutrition: A review of WHO guidelines. Bull World Health Organ. (2016) 94:642. doi: 10.2471/BLT.15.162867
25. Desta K. Survival status and predictors of mortality among children aged 0–59 months with severe acute malnutrition admitted to stabilization center at Sekota Hospital Waghemra Zone. J Nutr Disord Ther. (2015) 5:160. doi: 10.4172/2161-0509.1000160
26. Stobaugh H, Rogers B, Webb P, Rosenberg I, Thakwalakwa C, Maleta K, et al. Household-level factors associated with relapse following discharge from treatment for moderate acute malnutrition. Br J Nutr. (2018) 119:1039–46. doi: 10.1017/S0007114518000363
27. Abitew D, Worku A, Mulugeta A, Bazzano A. Rural children remain more at risk of acute malnutrition following exit from community-based management of acute malnutrition program in South Gondar Zone, Amhara Region, Ethiopia: A comparative cross-sectional study. PeerJ. (2020) 8:e8419. doi: 10.7717/peerj.8419
28. Tsedeke W, Tefera B, Debebe M. Prevalence of acute malnutrition (wasting) and associated factors among preschool children aged 36–60 months at Hawassa Zuria, South Ethiopia: A community-based cross-sectional study. J Nutr Food Sci. (2016) 6:2.
29. Ashraf H, Alam N, Chisti M, Mahmud S, Hossain M, Ahmed T, et al. A follow-up experience of 6 months after treatment of children with severe acute malnutrition in Dhaka, Bangladesh. J Tropic Pediatr. (2012) 58:253–7. doi: 10.1093/tropej/fmr083
30. Prost A, Nair N, Copas A, Pradhan H, Saville N, Tripathy P, et al. Mortality and recovery following moderate and severe acute malnutrition in children aged 6–18 months in rural Jharkhand and Odisha, eastern India: A cohort study. PLoS Med. (2019) 16:e1002934. doi: 10.1371/journal.pmed.1002934
31. Tadesse E, Worku A, Berhane Y, Ekström E. An integrated community-based outpatient therapeutic feeding programme for severe acute malnutrition in rural Southern Ethiopia: Recovery, fatality, and nutritional status after discharge. Matern Child Nutr. (2018) 14:e12519. doi: 10.1111/mcn.12519
32. World Health Organization [WHO]. WHO Child Growth Standards and The Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children’s Fund. Geneva: World Health Organization (2009).
33. Ministry of Health Republic of South Sudan. Guideline For Inpatient Management Of Severe Acute Malnutrition. Juba: Ministry of Health (2018).
34. Federal Ministry of Health of Ethiopia. Interim Guidelines for Emergency Nutrition Surveys in Ethiopia. Addis Ababa: Federal Ministry of Health of Ethiopia (2008).
35. Federal Ministry of Health [FMoH]. National Guideline for the Management of Acute Malnutrition. Addis Ababa: Federal Ministry of Health (2019).
36. World Food Programme. National Guidelines on the Management of Severe Acute Malnutrition for Children under Five Years. Federal Ministry of Health Ethiopia. Rome: World Food Programme (2016). p. 1–144.
37. Swindale A, Bilinsky P. Household Dietary Diversity Score (HDDS) for Measurement of Household Food Access: Indicator Guide. Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Educational Development (2006).
38. Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide: Version 3. (2007). doi: 10.1037/e576842013-001
39. Central Statistical Agency [CSA] (Ethiopia), ICF International. Ethiopia Demographic and Health Survey 2016: key indicators report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. Addis Ababa: Central Statistical Agency (2016).
40. Wete A, Zerfu T, Anbese A. The magnitude and associated factors of wasting among under five orphans in Dilla town, southern Ethiopia: 2018: A cross-sectional study. BMC Nutr. (2019) 5:33. doi: 10.1186/s40795-019-0295-6
41. Grellety E, Babakazo P, Bangana A, Mwamba G, Lezama I, Zagre N, et al. Effects of unconditional cash transfers on the outcome of treatment for severe acute malnutrition (SAM): A cluster-randomised trial in the Democratic Republic of the Congo. BMC Med. (2017) 15:87. doi: 10.1186/s12916-017-0848-y
42. Ngari M, Mwalekwa L, Timbwa M, Hamid F, Ali R, Iversen P, et al. Changes in susceptibility to life-threatening infections after treatment for complicated severe malnutrition in Kenya. Am J Clin Nutr. (2018) 107:626–34. doi: 10.1093/ajcn/nqy007
43. John C, Diala U, Adah R, Lar L, Envuladu E, Adedeji I, et al. Survival and nutritional status of children with severe acute malnutrition, six months post-discharge from outpatient treatment in Jigawa state, Nigeria. PLoS One. (2018) 13:e0196971. doi: 10.1371/journal.pone.0196971
44. Adegoke O, Arif S, Bahwere P, Harb J, Hug J, Jasper P, et al. Incidence of severe acute malnutrition after treatment: A prospective matched cohort study in Sokoto, Nigeria. Matern Child Nutr. (2021) 17:e13070. doi: 10.1111/mcn.13070
45. Guesdon B, Katwal M, Poudyal A, Bhandari T, Counil E, Nepali S. Anthropometry at discharge and risk of relapse in children treated for severe acute malnutrition: A prospective cohort study in rural Nepal. Nutr J. (2021) 20:32. doi: 10.1186/s12937-021-00684-7
46. Mengesha M, Deyessa N, Tegegne B, Dessie Y. Treatment outcome and factors affecting time to recovery in children with severe acute malnutrition treated at outpatient therapeutic care program. Glob Health Action. (2016) 9:30704. doi: 10.3402/gha.v9.30704
47. Brown J, Cairncross S, Ensink J. Water, sanitation, hygiene and enteric infections in children. Arch Dis Childhood. (2013) 98:629–34. doi: 10.1136/archdischild-2011-301528
48. Bellamy C. The State of the World’s Children 1998: Focus on Nutrition. New York, NY: UNICEF (1998).
49. Huang Z, Liu Y, Qi G, Brand D, Zheng S. Role of vitamin A in the immune system. J Clin Med. (2018) 7:258. doi: 10.3390/jcm7090258
50. World Health Organization [WHO]. Guideline: Vitamin A supplementation in Infants and Children 6-59 Months of Age. Geneva: World Health Organization (2011).
51. Thorne-Lyman A, Valpiani N, Sun K, Semba R, Klotz C, Kraemer K, et al. Household dietary diversity and food expenditures are closely linked in rural Bangladesh, increasing the risk of malnutrition due to the financial crisis. J Nutr. (2010) 140:182S–8S. doi: 10.3945/jn.109.110809
52. Torheim LE, Ouattara F, Diarra MM, Thiam FD, Barikmo I, Hatløy A, et al. Nutrient adequacy and dietary diversity in rural Mali: Association and determinants. Eur J Clin Nutr. (2004) 58:594–604. doi: 10.1038/sj.ejcn.1601853
53. Ajao K, Ojofeitimi E, Adebayo A, Fatusi A, Afolabi O. Influence of family size, household food security status, and child care practices on the nutritional status of under-five children in Ile-Ife, Nigeria. Afr J Reprod Health. (2010) 14: 117–26.
Keywords: relapse, acute malnutrition, stabilization center, children, Habro Woreda, Eastern Ethiopia
Citation: Alyi M, Roba KT, Ketema I, Habte S, Goshu AT, Mehadi A, Baye Y and Ayele BH (2023) Relapse of acute malnutrition and associated factors after discharge from nutrition stabilization centers among children in Eastern Ethiopia. Front. Nutr. 10:1095523. doi: 10.3389/fnut.2023.1095523
Received: 11 November 2022; Accepted: 23 January 2023;
Published: 14 February 2023.
Edited by:
Harsharn Gill, RMIT University, AustraliaReviewed by:
Isaac Agbemafle, University of Health and Allied Sciences, GhanaCopyright © 2023 Alyi, Roba, Ketema, Habte, Goshu, Mehadi, Baye and Ayele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Indeshaw Ketema,  ZW5kYXNoYXcyNEBnbWFpbC5jb20=
ZW5kYXNoYXcyNEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.