
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 13 February 2023
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1086507
This article is part of the Research TopicDiet Behavior and Heart HealthView all 21 articles
 Jie Hou1,2*†
Jie Hou1,2*† Lifang Zhu1†
Lifang Zhu1† Shuran Jin1
Shuran Jin1 Jinshu Li3
Jinshu Li3 Zhifeng Xing4
Zhifeng Xing4 Yanling Wang5
Yanling Wang5 Xiaoyan Wan6
Xiaoyan Wan6 Xianni Guo7
Xianni Guo7 Anwei Wang8
Anwei Wang8 Xiuhong Wang9
Xiuhong Wang9 Jinming Liu10
Jinming Liu10 Jing Ma11
Jing Ma11 Shuang Zhou12
Shuang Zhou12 Xiangdong Zhang13
Xiangdong Zhang13 Heming Zheng14
Heming Zheng14 Jianhui Wang15
Jianhui Wang15 Hongqi Feng1,2
Hongqi Feng1,2 Shuqiu Sun1,2
Shuqiu Sun1,2 Tong Wang1,2*
Tong Wang1,2*Background: Hypertension is a major public health concern that strongly influences the quality of life of people worldwide. Keshan disease (KD) is an endemic cardiomyopathy related to low selenium, threatening residents in rural areas of 16 provinces in China. Furthermore, the prevalence of hypertension in the KD-endemic areas has been increasing annually. However, hypertension research associated with KD has only focused on endemic regions, and no studies have compared hypertension prevalence between endemic and non-endemic areas. Therefore, this study investigated the prevalence of hypertension to provide a basis for preventing and controlling hypertension in the KD-endemic areas, even in rural areas.
Methods: We extracted blood pressure information from cardiomyopathy investigation data from a cross-sectional study of the KD-endemic and non-endemic areas. The hypertension prevalence between the two groups was compared using the Chi-square test or Fisher s exact test. Additionally, Pearson’s correlation coefficient was employed to evaluate the relationship between the per capita gross domestic product (GDP) and hypertension prevalence.
Results: There was a statistically significant increase of hypertension prevalence in the KD-endemic areas (22.79%, 95% confidence interval [CI]: 22.30–23.27%) over the non-endemic areas (21.55%, 95% CI: 21.09–22.02%). In the KD-endemic areas, more men had hypertension than women (23.90% vs. 21.65%, P < 0.001). Furthermore, the hypertension prevalence was higher in the north than in the south in the KD-endemic areas (27.52% vs. 18.76%, P < 0.001), non-endemic areas (24.86% vs. 18.66%, P < 0.001), and overall (26.17% vs. 18.68%, P < 0.001). Finally, the prevalence of hypertension positively correlated with per capita GDP at province level.
Conclusions: The increasing hypertension prevalence is a public health problem in the KD-endemic areas. Healthy diets, such as high consumption of vegetables and seafoods, and foods that are rich in selenium, might help prevent and control hypertension in the KD-endemic areas and other rural areas in China.
More than 200 million adults have hypertension in China, accounting for over one-fifth of China’s adult population (1). Moreover, hypertension is a major public health concern worldwide and is a risk factor for abundant diseases, such as cardiovascular (2, 3) and kidney diseases (4). More than half of the global adult population have not been diagnosed with or treated for hypertension. Consequently, only approximately 20% of adult patients have experienced hypertension control through medical care (4). Moreover, residents of rural areas may be at higher risk than those in urban areas in low-and middle-income countries.
Keshan disease (KD) is an endemic cardiomyopathy characterized by degeneration, necrosis, and fibrosis of cardiomyocytes, and heart dilatation, threatening the residents of rural areas in 16 provinces of China (5). In addition, hair and serum samples from individuals from these populations and soil and grain samples from the KD-endemic areas indicated low selenium levels (6, 7). Moreover, Mihailović et al. (8) found that patients with arterial hypertension had significantly lower whole-blood and plasma selenium concentrations.
A 10-year follow-up study verified that hypertension is a risk factor for latent KD worsening into chronic KD (9). Recently, with economic development and changes in diet, the prevalence of hypertension in the KD-endemic areas has increased annually (10), exceeding the national average (11). Previous hypertension research associated with KD has focused on the endemic areas, whilst no studies have investigated hypertension disparities between the KD-endemic and non-endemic areas. Therefore, this study used the blood pressure data from a cardiomyopathy investigation of residents of the KD-endemic and non-endemic areas in 2011 to understand the prevalence of hypertension and provide a base for preventing and controlling hypertension in the KD-endemic areas, even in the rural areas in China.
We extracted data from a cross-sectional study comprising KD surveillance in KD-endemic counties and dilated cardiomyopathy surveyed in non-endemic counties in 13 provinces. The provinces included Heilongjiang, Nei Mongol, Jilin, Gansu, Shaanxi, Liaoning, Shanxi, Shandong, Henan, Hebei, Yunnan, Sichuan, and Chongqing. There are more endemic counties and higher KD prevalence in the 13 provinces among 16 provinces affected by KD in China. KD surveillance has been gradually conducted in those provinces since 1990. The other three provinces, Hubei, Guizhou and Tibet, were excluded due to only one KD county and few KD cases occurred. The KD-endemic areas were determined using the Delimitation and Classification of Keshan Disease Areas (GB17020-2010) (12). In this study, we used multistage cluster sampling. For each county, we performed the case search (6) to identify two townships with the most patients with KD or dilated cardiomyopathy. Then, we selected the village with the most patients in either of the two townships for the investigation. The included villages had populations greater than or equal to 500 people. The endemic and non-endemic counties were individually matched based on the geographical location and residents’ lifestyles. Finally, hypertension data were collected from the 49 KD-endemic and 49 non-endemic counties.
All village residents underwent medical examinations, including blood pressure and electrocardiograms. After, patients with suspected KD or dilated cardiomyopathy were examined using echocardiography and chest radiography. We required a response rate of 80% or higher or at least 400 surveyed individuals. If the quantity did not meet these requirements, it would be supplemented by the neighboring village. All included participants had lived in the surveyed village for more than 6 consecutive months or had left for no more than 3 months in the past year. We examined 43,240 and 104,166 people in the KD-endemic and non-endemic areas, respectively. Then, we extracted blood pressure data for 58,994 participants aged 20 years or older for the analysis.
After sitting in a relaxed position comfortably and quietly for more than 5 min, blood pressure was measured using a mercury sphygmomanometer. The participants were informed that smoking, drinking, and other activities resulting in blood pressure instability were forbidden for at least 30 min before the measurement. During the measurement, the elbow and forearm were bent flush with the heart, and the cuff was placed on the right bare upper arm one inch above the bend of the elbow with appropriate tightness. The disk of the stethoscope was placed face down under the cuff, just to the inner side of the upper arm, where the brachial artery pulse could be felt. The cuff was rapidly inflated until the pulse voice disappeared and continued to be pressurized until it was slowly deflated after the gauge reading had risen by 20–30 mmHg. The first loud beat heard was the systolic blood pressure (SBP), and the last beat before it disappeared was the diastolic blood pressure (DBP).
Demographic data including age and sex and the per capita gross domestic product (GDP) were collected for each province in 2011 from the 2012 China Statistical Yearbook (13).
All participants signed an informed statement to give permission and indicate that they had no direct interest in the study’s results. This study conformed to the Declaration of Helsinki and has been authorized by the Medical Ethics Committee of Harbin Medical University.
The statistical analyses were executed with R Studio version 1.4.1717.1 Hypertension was defined as either a SBP of 140 mmHg or greater or a DBP of 90 mmHg or greater or the presence of both based on the 2019 Annual Report on Cardiovascular Health and Diseases in China (14). Hypertension was classified into three categories: Grade 1 (140–159/90–99 mmHg), Grade 2 (160–179/100–109 mmHg), and Grade 3 (≥180/110 mmHg) (15). We excluded SBP, DBP, or pulse pressure data outside a 99.73% confidence interval (CI). We also screened for duplicated records and, if identified, randomly retained one of the duplicates. Repeat data were defined as consistent information, including province, county, township, age, sex, SBP, DBP, pinyin of name, and telephone number.
The distributions of the participant characteristics were described using the population pyramid. Bar charts were used to depict the prevalence of hypertension in the KD-endemic and non-endemic areas by age categories. Forest plots were employed to describe the hypertension prevalence rate at the province level, while error bars with 95% CIs were used to demonstrate hypertension differences between the sexes. The prevalence was standardized by age and sex based on the 2012 China Statistical Yearbook (13). The prevalence between the two groups was compared using the Chi-square test or Fisher’s exact test, and the relationship between the per capita GDP and hypertension prevalence at province level was analyzed using Pearson’s correlation coefficient. The statistical significance was delimited at P < 0.05.
We recruited 58,994 participants, including 28,738 participants from the KD-endemic areas and 30,256 from the non-endemic areas. Figure 1 presents the age and sex distributions of the respondents. The prevalence of hypertension was higher in the KD-endemic areas (22.79%, 95% CI: 22.30–23.27%) than in the non-endemic areas (21.55%, 95% CI: 21.09–22.02%, P < 0.001, Table 1).
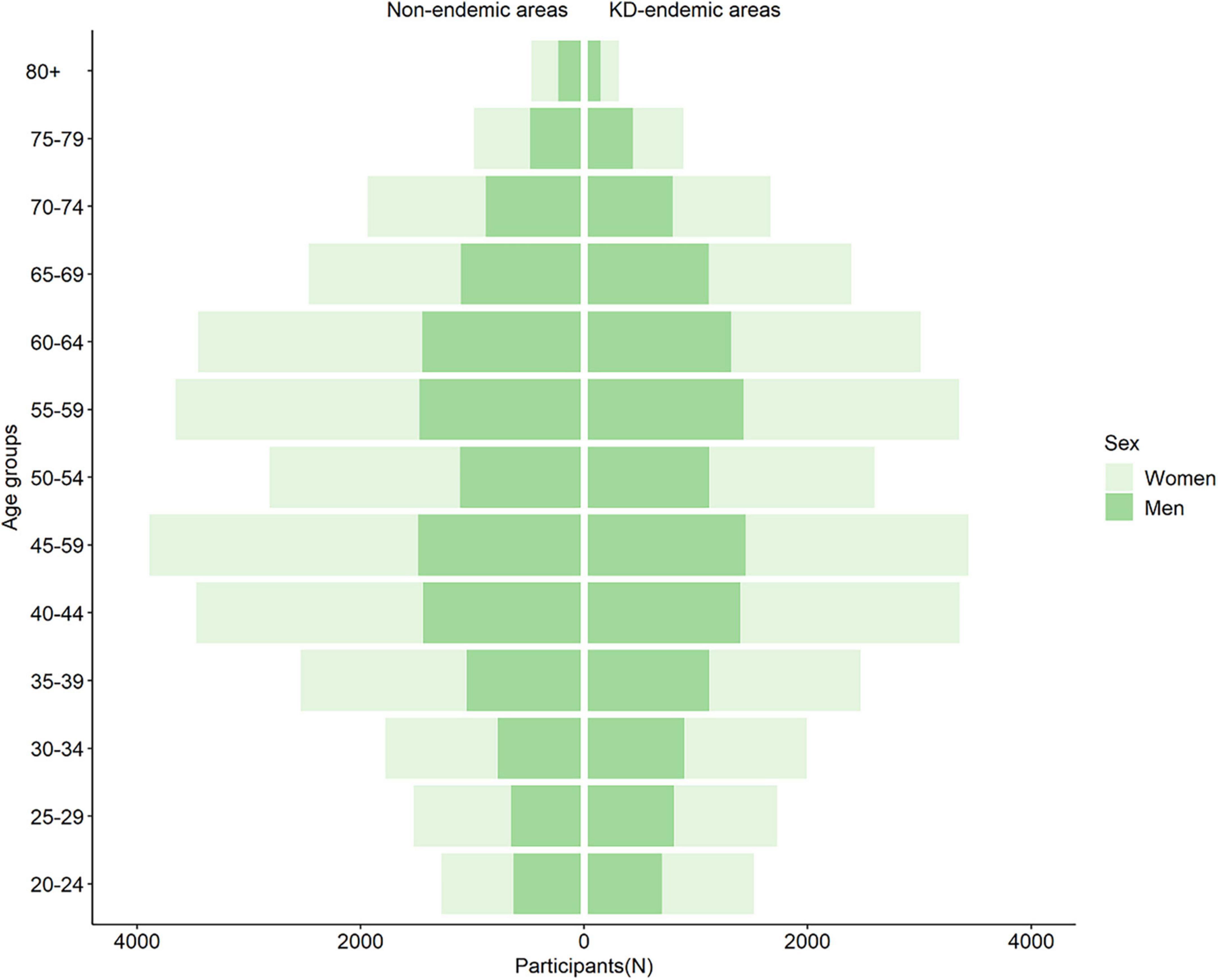
Figure 1. Population pyramid of participants in KD-endemic and non-endemic areas. KD, Keshan disease; N, number.
Hypertension prevalence increased with age; the highest prevalence was in the 75–79 and 80+ year age groups in the endemic and non-endemic areas, respectively. Furthermore, in four age groups (50–54, 55–59, 60–64, and 70–74 years), the prevalence of hypertension was lower in the non-endemic areas than in the KD-endemic areas (P < 0.05, Figure 2 and Supplementary Table 1).
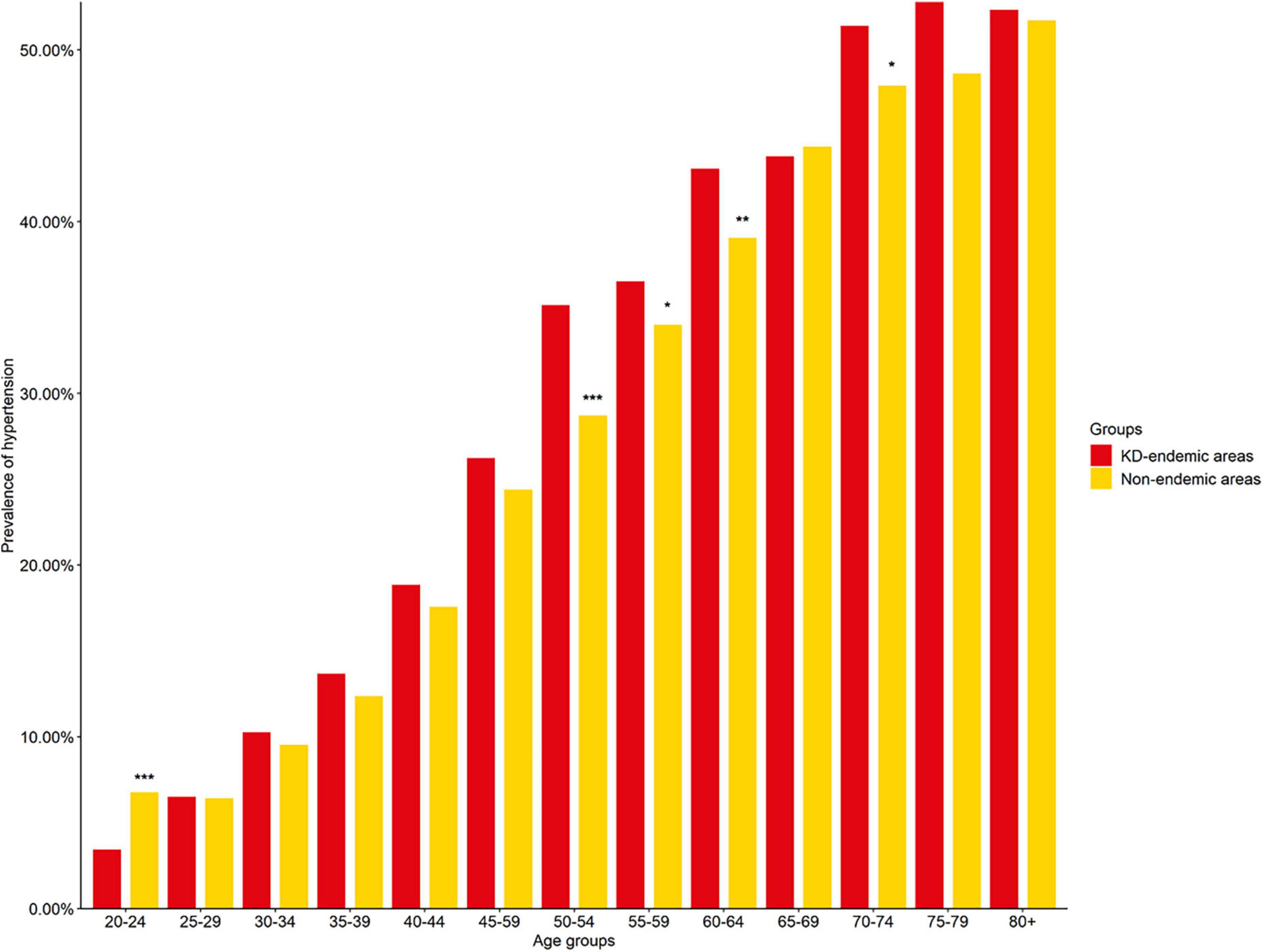
Figure 2. Hypertension prevalence in KD-endemic and non-endemic areas by age groups. The prevalence was standardized by age and sex based on the 2012 China Statistical Yearbook. KD. Keshan disease; *P < 0.05 compared with KD-endemic areas; **P < 0.01 compared with KD-endemic areas; ***P < 0.001 compared with KD-endemic areas.
The prevalence of hypertension among men in the KD-endemic areas exceeded that among men in the non-endemic areas and women in the KD-endemic areas (P < 0.001, Figure 3). The prevalence of Grade 1 and 2 hypertension was higher in the KD-endemic areas than in the non-endemic areas, whereas the prevalence of Grade 3 hypertension was the opposite (P < 0.001, Table 2).
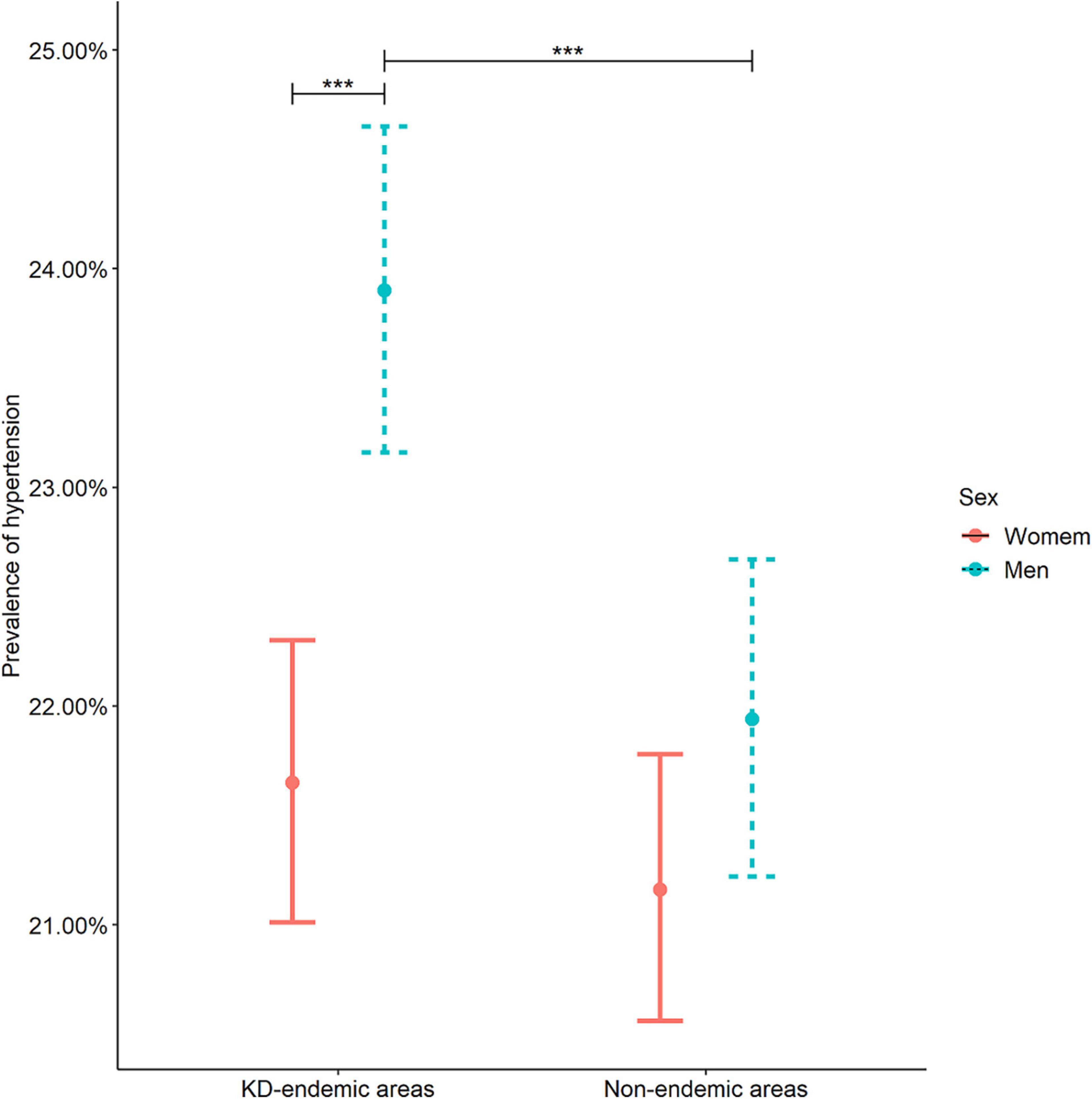
Figure 3. Hypertension prevalence in KD-endemic and non-endemic areas by sex. Error bars with 95% CIs were used to demonstrate hypertension differences between the sexes. The prevalence was standardized by age and sex based on the 2012 China Statistical Yearbook. KD, Keshan disease; ***P < 0.001 compared with women in the KD-endemic areas or men in the non-endemic areas.
The annual average temperature of the capital cities in the provinces included in this investigation was 11.7°C. Therefore, provinces with an annual average temperature above 11.7°C were classified as being in the south and included Shandong, Shaanxi, Henan, Hebei, Yunnan, Sichuan, and Chongqing. Conversely, provinces with an annual average temperature below 11.7°C were classified as being in the north and included Heilongjiang, Jilin, Liaoning, Nei Mongol, Shanxi, and Gansu.
In the north, the prevalence of hypertension was significantly higher in the KD-endemic areas than in the non-endemic areas (P < 0.001). Moreover, the prevalence of hypertension was significantly higher in the north than in the south, regardless of the endemic classification (P < 0.001, Table 3).
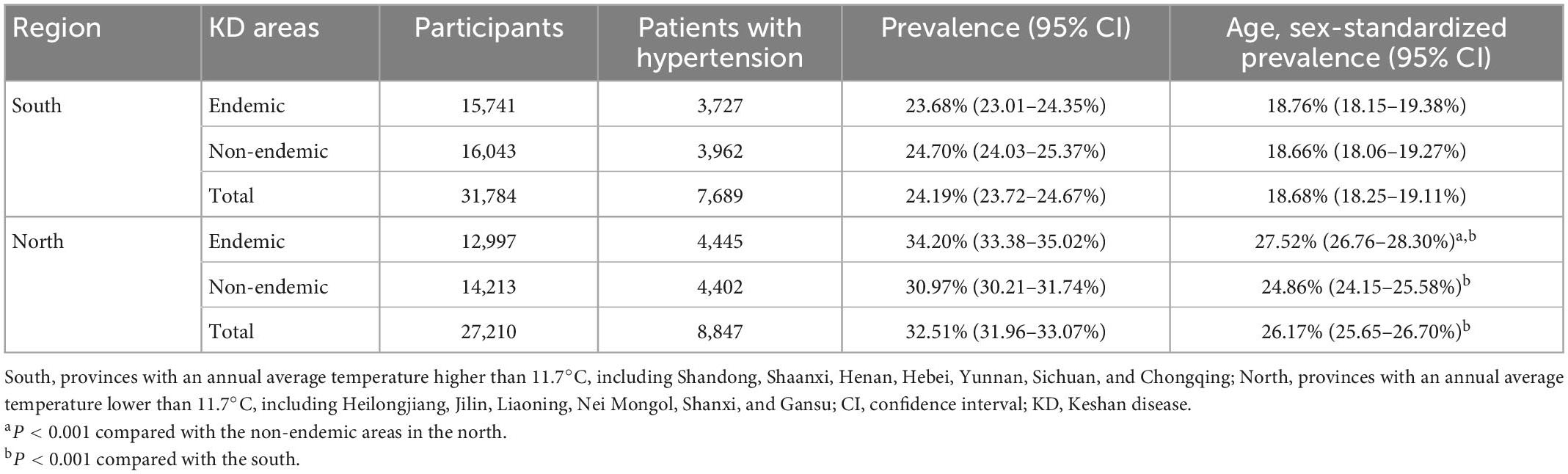
Table 3. Prevalence of hypertension in KD-endemic and non-endemic areas in the southern and northern regions of China.
In the Shanxi, Henan, Heilongjiang, and Chongqing provinces, the prevalence of hypertension was significantly lower in the non-endemic areas than in the endemic areas (P < 0.001, Figure 4 and Supplementary Table 2). However, the opposite was observed in the Sichuan (P < 0.001), Shandong (P < 0.001), and Shaanxi (P < 0.05) provinces.
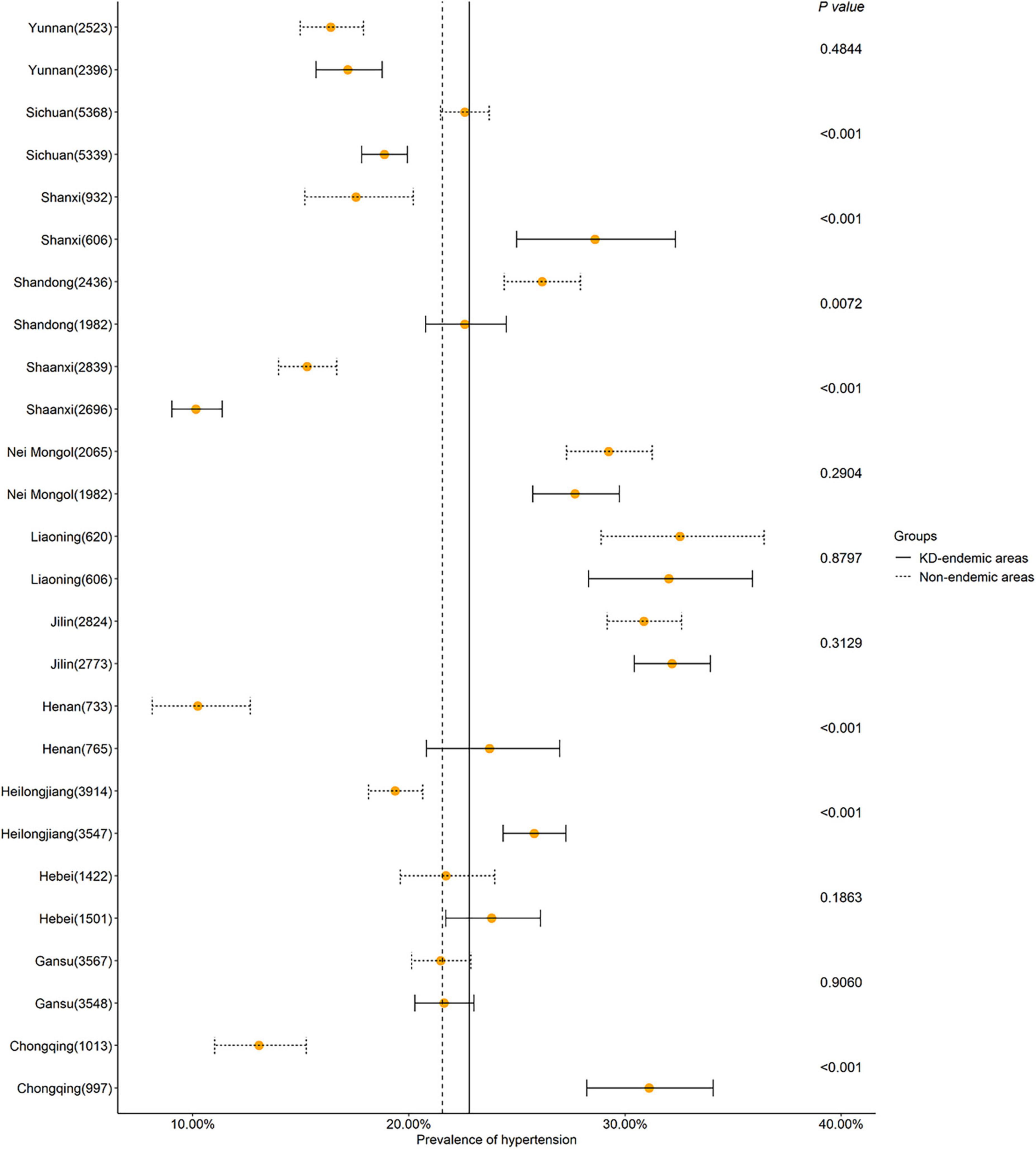
Figure 4. Hypertension prevalence in KD-endemic and non-endemic areas by province. Forest plots were employed to describe the hypertension prevalence rate at the province level. The prevalence was standardized by age and sex based on the 2012 China Statistical Yearbook. KD, Keshan disease; The number in the bracket represents the total number of participants in each province. The upright solid line indicates the hypertension prevalence in the KD-endemic areas in total. The upright dotted line indicates the hypertension prevalence in the non-endemic areas in total.
Pearson’s correlation coefficient was determined to be r = 0.6672 (P = 0.0127), suggesting that the prevalence of hypertension positively correlated with the per capita GDP by province (Figure 5, Supplementary Table 3 and Supplementary Figure 1).
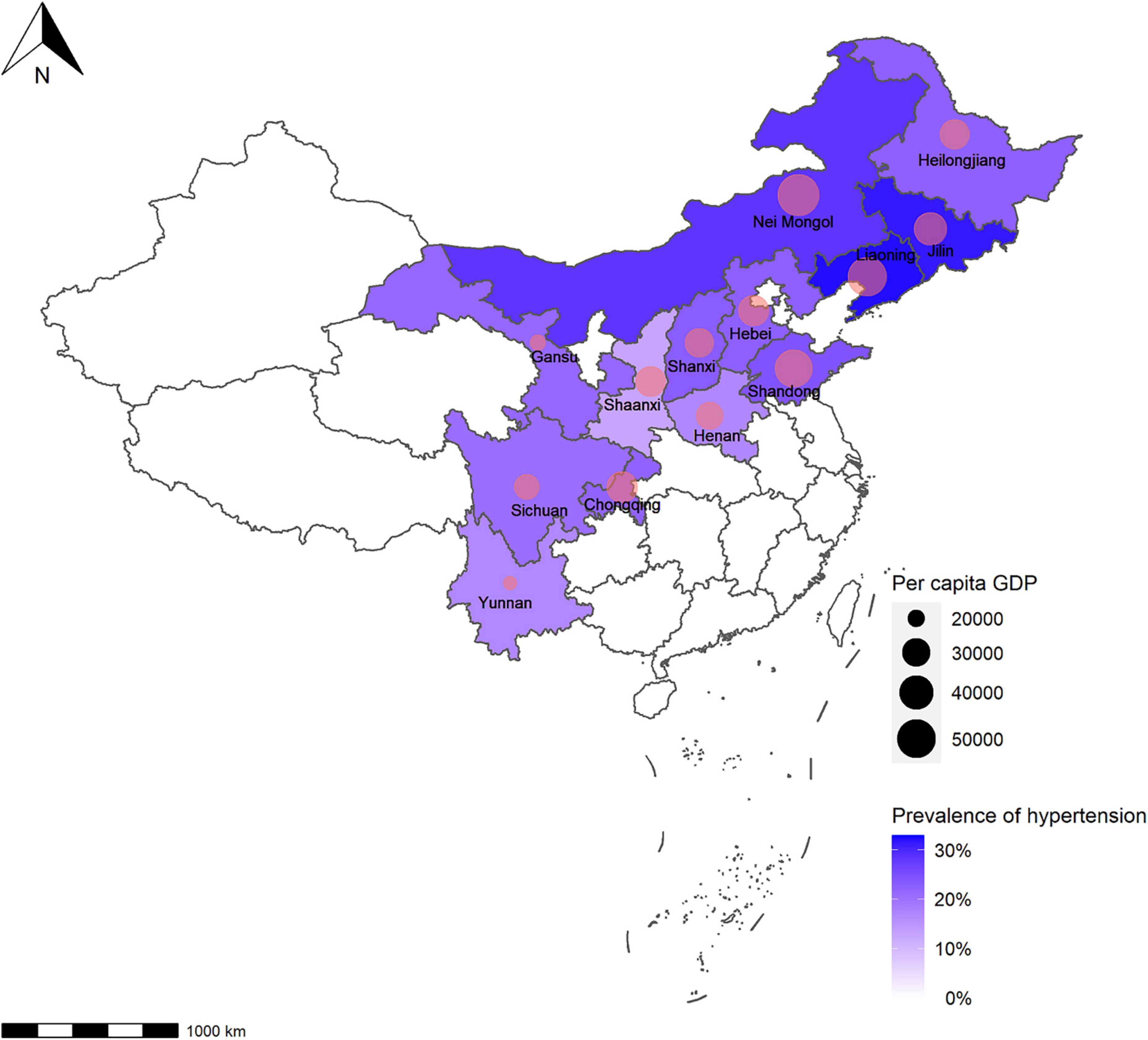
Figure 5. Hypertension prevalence and per capita GDP at province level. The relationship between the per capita GDP and hypertension prevalence at province level was analyzed using Pearson’s correlation coefficient (r = 0.6672, P = 0.0127). The prevalence was standardized by age and sex based on the 2012 China Statistical Yearbook. GDP, gross domestic product.
We conducted a large-scale and representative study, reporting for the first time that the prevalence of hypertension is higher in the KD-endemic areas than in the non-endemic areas. This may be related to the suboptimal selenium intake of residents in the KD-endemic areas. The Western European longitudinal population study demonstrated that a 20 μg/L or higher blood selenium level at baseline reduced the risk of hypertension by 37% in men (16), and adults with low toenail selenium concentrations had an increased risk of hypertension (17). Furthermore, Xie et al. (18) reported a negative correlation between selenium intake and hypertension in participants in northern provinces but a positive correlation in participants in southern provinces in China. Lower urinary selenium concentrations were also associated with higher SBP and DBP values in Asian countries (19), similar to the associations identified between the serum selenium level and SBP and DBP in pregnant women (20). However, some studies have suggested a positive correlation between selenium levels and hypertension (21–23), which may be due to the presence of high levels of selenium in the areas investigated. About half of the Chinese population does not meet the recommended selenium intake defined by the Food and Agriculture Organization and the World Health Organization (24). Therefore, increasing the intake of selenium-rich foods might be beneficial for the residents of low-selenium areas, reducing the prevalence of hypertension.
Men are more prone to hypertension than women (25–27), which is consistent with our study’s results (Supplementary Figures 2, 3). We found that the prevalence of hypertension was higher in men than in women in the KD-endemic areas. Everett and Zajacova (28) reported that among Americans aged 24–34 years, women were far less likely to be hypertensive because they were more aware of hypertension than men. Women had more advanced hypertension awareness than men in China (1), the United States (29), and Romania (30). Meanwhile, men consumed alcohol in larger amounts and more frequently than women (31). After stratifying by sex, daily drinking increased the risk of hypertension in men but did not affect women in Southwest China (32). A J-shaped relationship between alcohol consumption and hypertension has been identified in women, while alcohol consumption was linearly correlated with the risk of hypertension in men (33, 34). These studies indicate that alcohol consumption could be the reason for a higher hypertension prevalence in men.
We found the hypertension prevalence was higher in the north than in the south, perhaps highlighting the role of temperature. A previous study reported that the prevalence of hypertension and the average SBP and DBP in northern tourists in Hainan, located in one of the most southern regions of China, were significantly higher than those of local residents and northern residents living in Hainan for more than 5 years (35). Moreover, Duranton et al. (36) collected data from 261 hemodialysis patients in different latitudes, discovering that the rising outdoor temperatures and prolonged sunshine hours were associated with decreased blood pressure before dialysis. When the temperature dropped by 1°C, the SBP and DBP for the total population rose by 0.55 and 0.26 mmHg, respectively (37). Moreover, residents in the north of China had 2.32 g more sodium daily than those in the south of China (38). One study reported that individuals with hypertension or normal blood pressure could lower their blood pressure by moderately reducing their salt intake for 4 weeks or more (39). Another study reported a reduction in SBP and DBP by 1.10 mmHg and 0.33 mmHg, respectively, for every 50 mmol of sodium excretion in 24 h (40). Thus, temperature and the amount of salt in the diet may explain the distinct hypertension prevalence in the northern and southern regions.
Income has been identified as a hypertension risk factor (41), and our study supports these findings. We identified a positive correlation between the prevalence of hypertension and per capita GDP by province. In Bengal, adults in richer household wealth quintiles had a significantly higher prevalence and odds of hypertension (42), and women in the highest wealth quantile were more prone to hypertension in Kenya (43). In developing countries, generally, hypertension is positively correlated with economic status, but the opposite is true in many developed countries, such as the United States and Canada (44). It was revealed that higher income, occupation, and the mother’s education level were protective factors for hypertension among African Americans (45). Diet might also play a key role in influencing blood pressure by income. In developed countries, individuals with high socioeconomic status (based on occupation, education, and income) mainly consume foods abundant in fiber and protein and low in fat (46). In China, dietary consumption patterns are changing; the consumption of vegetable oil, animal foods, and sweeteners is increasing, and the consumption of coarse grains and beans is decreasing (47), especially among wealthier individuals (48). Vegetables might help reduce blood pressure (49, 50), and vegans and vegetarians have been shown to have lower SBP and DBP values than omnivores (51). A national cross-sectional study among Chinese adolescents aged 13–17 years found that adolescents whose daily vegetable consumption was three or more servings (one serving is approximately one cup, approximately 200 g) had a lower hazard ratio for high blood pressure than those who consumed less than one serving daily (52). Another study reported that both raw (tomatoes, carrots, and shallots) and cooked (tomatoes, peas, and celery) vegetable intake significantly affected blood pressure (53). Conversely, a Korean study found that vegetable intake did not influence the risk of hypertension (54), which might be owing to the manner of cooking. The Dietary Approaches to Stop Hypertension Diet, comprising whole cereal, vegetables, fruits, and low-fat food, was as effective as some antihypertensive drugs and significantly reduced blood pressure (55). Not only vegetables but also seafoods lessened the risk of hypertension. The inverse relationship was identified between high seafood intake and childhood hypertension in Iranian students aged 7–12 years (56). Seafood is abundant in omega-3 polyunsaturated fatty acids, resulting in a small but significant decrease in blood pressure (57). Moreover, one study found that people in the highest quarter of the Omega-3 Index had an SBP and DBP 4 mmHg and 2 mmHg lower, respectively, than those in the lowest quarter (58). It was noteworthy that obtaining more omega-3 polyunsaturated fatty acids from the diet led to a clinically related decrease in DBP in a randomized controlled trial (59). Since the KD-endemic areas all lie within the agricultural hinterland, increasing the intake of seafood is widely advocated for preventing hypertension in the affected population and may be an important control strategy.
This study has some limitations. First, only those aged 20 or older were included owing to the 2012 China Statistical Yearbook age group classifications; adults aged 18 and 19 years were not included. Second, the survey included many participants from several rural areas of China. Thus, we did not collect information on the participants’ hypertension drug use.
In conclusion, the prevalence of hypertension was higher in the KD-endemic areas than in the non-endemic areas. Therefore, healthy diets, such as high consumption of vegetables and seafoods, and foods that are rich in selenium, might help prevent and control hypertension in the KD-endemic areas. In addition, this study provides a better understanding of hypertension statuses in rural China, which may help with prevention.
The datasets presented in this article are not readily available because the data supporting the results of this study were obtained from the Center for Endemic Disease Control, Chinese Center for Disease Control and Prevention. The data were licensed to be used in the current study, but sharing of data was not allowed; therefore, the data resource is not publicly available. Nonetheless, the data can be available upon rational demand and with the approval of the Center for Endemic Disease Control. Requests to access the datasets should be directed to JH, aG91amllQGVtcy5ocmJtdS5lZHUuY24=.
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of Harbin Medical University. The patients/participants provided their written informed consent to participate in this study.
JH and TW performed the design and concretization of the study. JH, LZ, and SJ performed the data analysis and participated in the writing of manuscript and revision and result interpretation. JH, JSL, ZX, YW, XYW, XG, AW, XHW, JML, JM, SZ, XZ, HZ, JW, HF, and SS contributed to the field investigation and data collection. TW contributed to the project funds. All authors read the final version and approved it.
This work was sponsored by Endemic Disease Prevention Project from Ministry of Health of People’s Republic of China.
We appreciate all the people who participated in this project. We thank all the members of our research team. We are grateful to Editage (www.editage.cn) for English language editing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1086507/full#supplementary-material
KD, keshan disease; GDP, gross domestic product; SBP, systolic blood pressure; DBP, diastolic blood pressure; CI, confidence interval.
1. Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. (2018) 137:2344–56. doi: 10.1161/CIRCULATIONAHA.117.032380
2. Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. (2014) 371:818–27. doi: 10.1056/NEJMoa1311890
3. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces,1990-2017:a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
4. World Health Organization. Hypertension. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed April 10, 2021).
6. Hou J, Zhu L, Chen C, Feng H, Li D, Sun S, et al. Association of selenium levels with the prevention and control of Keshan disease: a cross-sectional study. J Trace Elem Med Biol. (2021) 68:126832. doi: 10.1016/j.jtemb.2021.126832
7. Liu X, Wang Y, Han S, Zhang Y, Zou Y, Su S, et al. A spatial ecological study on serum selenium and Keshan disease in Heilongjiang Province, China. Biol Trace Elem Res. (2021) 199:3253–61. doi: 10.1007/s12011-020-02478-0
8. Mihailović M, Avramović D, Jovanović I, Pesut O, Matić D, Stojanov V. Blood and plasma selenium levels and GSH-Px activities in patients with arterial hypertension and chronic heart disease. J Environ Pathol Toxicol Oncol. (1998) 17:285–9.
9. Liu X, Yang G, Wang L, Wei J, Tan W, Zhu Y. Progressive risks of latent Keshan disease: a long term follow-up study. J Sichuan Univ Med Sci. (2016) 47:398–401. doi: 10.13464/j.scuxbyxb.2016.03.020
10. Pang R, Zhang J. Dynamics of incident hypertension in Keshan disease area from 2011 to 2016. Cardiovasc Dis J Integr Tradit West Med. (2017) 5:91+94. doi: 10.16282/j.cnki.cn11-9336/r.2017.02.067
11. Wang Z, Wang T, Zhen R, Chen X, Xu C, Han X, et al. Prevalence, awareness, treatment, and control of hypertension among residents in the severe historical endemic areas of Keshan disease in Heilongjiang Province. Chin. J. Endemiol. (2017) 36:434–9.
12. The Ministry of Health of the People’s Republic of China, The standardization Administration of the People’s Republic of China. Delimitation and Classification of Keshan Disease Areas (GB17020-2010). (2011). Available online at: http://www.nhc.gov.cn/wjw/s9500/201106/51931/files/331adfa14f7e4f6a9a40c7e055fb4ba1.pdf (accessed April 10, 2022).
13. National Bureau of Statistics. 2012 China Statistical Yearbook. (2013). Available online at: http://www.stats.gov.cn/tjsj/ndsj/2012/indexch.htm (Accessed April 10, 2022).
14. National Center for Cardiovascular Diseases, China. Annual Report on Cardiovascular Health and Diseases in China (2019). (2020). Available online at: https://www.nccd.org.cn/Sites/Uploaded/File/2021/5/%E4%B8%AD%E5%9B%BD%E5%BF%83%E8%A1%80%E7%AE%A1%E5%81%A5%E5%BA%B7%E4%B8%8E%E7%96%BE%E7%97%85%E6%8A%A5%E5%91%8A%EF%BC%882019%EF%BC%89%E5%90%88.pdf (accessed April 10, 2022).
15. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. (2018) 36:1953–2041. doi: 10.1097/HJH.0000000000001940
16. Nawrot T, Staessen J, Roels H, Den Hond E, Thijs L, Fagard R, et al. Blood pressure and blood selenium: a cross-sectional and longitudinal population study. Eur Heart J. (2007) 28:628–33. doi: 10.1093/eurheartj/ehl479
17. Liu L, Lin G, Wang H, Zhang B, Du S. Selenium exposure and incident hypertension among Chinese adults (P24-020-19). Curr Dev Nutr. (2019) 3:nzz044.P24-020-19. doi: 10.1093/cdn/nzz044.P24-020-19
18. Xie C, Xian J, Zeng M, Cai Z, Li S, Zhao Y, et al. Regional difference in the association between the trajectory of selenium intake and hypertension: a 20-year cohort study. Nutrients. (2021) 13:1501. doi: 10.3390/nu13051501
19. Mizuno Y, Shimizu-Furusawa H, Konishi S, Inaoka T, Ahmad S, Sekiyama M, et al. Associations between urinary heavy metal concentrations and blood pressure in residents of Asian countries. Environ Health Prev Med. (2021) 26:101. doi: 10.1186/s12199-021-01027-y
20. Eze S, Ododo N, Ugwu E, Enebe J, Onyegbule O, Eze I, et al. Serum selenium levels of pre-eclamptic and normal pregnant women in Nigeria: a comparative study. PLoS One. (2020) 15:e0238263. doi: 10.1371/journal.pone.0238263
21. Vinceti M, Chawla R, Filippini T, Dutt C, Cilloni S, Loomba R, et al. Blood pressure levels and hypertension prevalence in a high selenium environment: results from a cross-sectional study. Nutr Metab Cardiovasc Dis. (2019) 29:398–408. doi: 10.1016/j.numecd.2019.01.004
22. Wu G, Li Z, Ju W, Yang X, Fu X, Gao X. Cross-sectional study: relationship between serum selenium and hypertension in the Shandong Province of China. Biol Trace Elem Res. (2018) 185:295–301. doi: 10.1007/s12011-018-1272-7
23. Bastola M, Locatis C, Maisiak R, Fontelo P. Selenium, copper, zinc and hypertension: an analysis of the National Health and Nutrition Examination Survey (2011-2016). BMC Cardiovasc Disord. (2020) 20:45. doi: 10.1186/s12872-020-01355-x
24. Dinh Q, Cui Z, Huang J, Tran T, Wang D, Yang W, et al. Selenium distribution in the Chinese environment and its relationship with human health: a review. Environ Int. (2018) 112:294–309. doi: 10.1016/j.envint.2017.12.035
25. Defianna S, Santosa A, Probandari A, Dewi F. Gender differences in prevalence and risk factors for hypertension among adult populations: a cross-sectional study in Indonesia. Int J Environ Res Public Health. (2021) 18:6259. doi: 10.3390/ijerph18126259
26. Bachir Cherif A, Bouamra A, Taleb A, Nedjar R, Bouraghda A, Hamida F, et al. Differences in prevalence, treatment and control rates of hypertension between male and female in the area of Blida (Algeria). Ann Cardiol Angeiol (Paris). (2017) 66:123–9. doi: 10.1016/j.ancard.2017.04.009
27. Agho K, Osuagwu U, Ezeh O, Ghimire P, Chitekwe S, Ogbo F. Gender differences in factors associated with prehypertension and hypertension in Nepal: a nationwide survey. PLoS One. (2018) 13:e0203278. doi: 10.1371/journal.pone.0203278
28. Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography Soc Biol. (2015) 61:1–17. doi: 10.1080/19485565.2014.929488
29. Zhang Y, Moran A. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. (2017) 70:736–42. doi: 10.1161/HYPERTENSIONAHA.117.09801
30. Dorobantu M, Gheorghe-Fronea O, Scafa-Udriste A, Onciul S, Pop C, Dorobantu L, et al. Gender disparities in the prevalence, awareness, treatment, and control of high blood pressure. Curr Pharm Des. (2021) 27:3172–9. doi: 10.2174/1381612827666210125154749
31. Erol A, Karpyak V. Sex and gender-related differences in alcohol use and its consequences: contemporary knowledge and future research considerations. Drug Alcohol Depend. (2015) 156:1–13. doi: 10.1016/j.drugalcdep.2015.08.023
32. Wang Y, Yao Y, Chen Y, Zhou J, Wu Y, Fu C, et al. Association between drinking patterns and incident hypertension in Southwest China. Int J Environ Res Public Health. (2022) 19:3801. doi: 10.3390/ijerph19073801
33. Briasoulis A, Agarwal V, Messerli F. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich). (2012) 14:792–8. doi: 10.1111/jch.12008
34. Sesso H, Cook N, Buring J, Manson J, Gaziano J. Alcohol consumption and the risk of hypertension in women and men. Hypertension. (2008) 51:1080–7. doi: 10.1161/HYPERTENSIONAHA.107.104968
35. Lin K, Lin L, He C, Pang M, Chen H. Epidemic characteristics of hypertension in south and north China. Med J Wuhan Univ. (2014) 35:114–7. doi: 10.14188/j.1671-8852.2014.01.015
36. Duranton F, Palma A, Stegmayr B, Wauthier M, Torres A, Argilés À. Blood pressure seasonality in hemodialysis patients from five European cities of different latitudes. Kidney Blood Press Res. (2018) 43:1529–38. doi: 10.1159/000494019
37. Hu J, He G, Luo J, Xu Y, Xu X, Song X, et al. Temperature-adjusted hypertension prevalence and control rate: a series of cross-sectional studies in Guangdong Province, China. J Hypertens. (2021) 39:911–8. doi: 10.1097/HJH.0000000000002738
38. Wang M, Huang Y, Song Y, Chen J, Liu X. Study on environmental and lifestyle factors for the North-South differential of cardiovascular disease in China. Front Public Health. (2021) 9:615152. doi: 10.3389/fpubh.2021.615152
39. He F, MacGregor G. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. (2002) 16:761–70. doi: 10.1038/sj.jhh.1001459
40. Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell N, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. (2020) 368:m315. doi: 10.1136/bmj.m315
41. Sharma J, Mabhida S, Myers B, Apalata T, Nicol E, Benjeddou M, et al. Prevalence of hypertension and its associated risk factors in a rural black population of Mthatha Town, South Africa. Int J Environ Res Public Health. (2021) 18:1215. doi: 10.3390/ijerph18031215
42. Kibria G, Hashan M, Hossain M, Zaman S, Stennett C. Clustering of hypertension, diabetes and overweight/obesity according to socioeconomic status among Bangladeshi adults. J Biosoc Sci. (2021) 53:157–66. doi: 10.1017/S0021932020000085
43. Yaya S, El-Khatib Z, Ahinkorah B, Budu E, Bishwajit G. Prevalence and socioeconomic factors of diabetes and high blood pressure among women in Kenya: a cross-sectional study. J Epidemiol Glob Health. (2021) 11:397–404. doi: 10.1007/s44197-021-00004-6
44. Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. (2015) 33:221–9. doi: 10.1097/HJH.0000000000000428
45. Glover L, Cain-Shields L, Wyatt S, Gebreab S, Diez-Roux A, Sims M. Life course socioeconomic status and hypertension in African American adults: the Jackson Heart Study. Am J Hypertens. (2020) 33:84–91. doi: 10.1093/ajh/hpz133
46. Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr. (2008) 87:1107–17. doi: 10.1093/ajcn/87.5.1107
47. Popkin B. Synthesis and implications: China’s nutrition transition in the context of changes across other low- and middle-income countries. Obes Rev. (2014) 15(Suppl. 1):60–7. doi: 10.1111/obr.12120
48. Popkin B. The nutrition transition: an overview of world patterns of change. Nutr Rev. (2004) 62:S140–3. doi: 10.1111/j.1753-4887.2004.tb00084.x
49. van der Avoort C, Jonvik K, Nyakayiru J, van Loon L, Hopman M, Verdijk LB. A nitrate-rich vegetable intervention elevates plasma nitrate and nitrite concentrations and reduces blood pressure in healthy young adults. J Acad Nutr Diet. (2020) 120:1305–17. doi: 10.1016/j.jand.2020.02.014
50. He Z. A Prospective Cohort Study on Fruit and Vegetable Intake and Incidence and Progression of Hypertension in Chinese. Ph.D. thesis. Beijing: Peking Union Medical College (2021).
51. Pettersen B, Anousheh R, Fan J, Jaceldo-Siegl K, Fraser G. Vegetarian diets and blood pressure among white subjects: results from the Adventist Health Study-2 (AHS-2). Public Health Nutr. (2012) 15:1909–16. doi: 10.1017/S1368980011003454
52. Yang Y, Dong B, Zou Z, Wang S, Dong Y, Wang Z, et al. Association between vegetable consumption and blood pressure, stratified by BMI, among Chinese adolescents aged 13-17 years: a national cross-sectional study. Nutrients. (2018) 10:451. doi: 10.3390/nu10040451
53. Chan Q, Stamler J, Brown I, Daviglus M, Van Horn L, Dyer A, et al. Relation of raw and cooked vegetable consumption to blood pressure: the INTERMAP Study. J Hum Hypertens. (2014) 28:353–9. doi: 10.1038/jhh.2013.115
54. Kim J, Kim J. Association between fruit and vegetable consumption and risk of hypertension in middle-aged and older Korean adults. J Acad Nutr Diet. (2018) 118:1438–49. doi: 10.1016/j.jand.2017.08.122
55. Strilchuk L, Cincione R, Fogacci F, Cicero A. Dietary interventions in blood pressure lowering: current evidence in 2020. Kardiol Pol. (2020) 78:659–66. doi: 10.33963/KP.15468
56. Cabo J, Alonso R, Mata P. Omega-3 fatty acids and blood pressure. Br J Nutr. (2012) 107(Suppl. 2):S195–200. doi: 10.1017/S0007114512001584
57. Izadi A, Khedmat L, Tavakolizadeh R, Mojtahedi S. The intake assessment of diverse dietary patterns on childhood hypertension: alleviating the blood pressure and lipidemic factors with low-sodium seafood rich in omega-3 fatty acids. Lipids Health Dis. (2020) 19:65. doi: 10.1186/s12944-020-01245-3
58. Filipovic M, Aeschbacher S, Reiner M, Stivala S, Gobbato S, Bonetti N, et al. Whole blood omega-3 fatty acid concentrations are inversely associated with blood pressure in young, healthy adults. J Hypertens. (2018) 36:1548–54. doi: 10.1097/HJH.0000000000001728
Keywords: hypertension, Keshan disease, cross-sectional study, blood pressure, selenium, diet
Citation: Hou J, Zhu L, Jin S, Li J, Xing Z, Wang Y, Wan X, Guo X, Wang A, Wang X, Liu J, Ma J, Zhou S, Zhang X, Zheng H, Wang J, Feng H, Sun S and Wang T (2023) Prevalence of hypertension in endemic and non-endemic areas of Keshan disease: A cross-sectional study in rural areas of China. Front. Nutr. 10:1086507. doi: 10.3389/fnut.2023.1086507
Received: 01 November 2022; Accepted: 30 January 2023;
Published: 13 February 2023.
Edited by:
Yong Zhao, Chongqing Medical University, ChinaReviewed by:
Jin Wei, Second Affiliated Hospital of Xi’an Jiaotong University, ChinaCopyright © 2023 Hou, Zhu, Jin, Li, Xing, Wang, Wan, Guo, Wang, Wang, Liu, Ma, Zhou, Zhang, Zheng, Wang, Feng, Sun and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Hou,  aG91amllQGVtcy5ocmJtdS5lZHUuY24=; Tong Wang,
aG91amllQGVtcy5ocmJtdS5lZHUuY24=; Tong Wang,  d2FuZ3RvbmdAZW1zLmhyYm11LmVkdS5jbg==
d2FuZ3RvbmdAZW1zLmhyYm11LmVkdS5jbg==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.