- 1Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, United Kingdom
- 2Department of Data Services, Lean Business Services, Riyadh, Saudi Arabia
- 3Faculty of Medicine, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
- 4Clinical Research Development of Shahid Mohammadi Hospital, Hormozgan University of Medical Sciences, Bandar Abbas, Iran
- 5Pharmaceutical Care Department, Hail General Hospital, Hail Health Cluster, Ministry of Health, Hail, Saudi Arabia
- 6Dammam Medical Complex, Medical and Clinical Affairs, Dammam, Saudi Arabia
- 7Dementia Research Institute at Imperial College London, London, United Kingdom
- 8National Institute for Health Research Imperial College Biomedical Research Centre, Imperial College London, London, United Kingdom
- 9Department of Hygiene and Epidemiology, University of Ioannina School of Medicine, Ioannina, Greece
- 10MRC-PHE Centre for Environment and Health, School of Public Health, Imperial College London, London, United Kingdom
Background: Although the effect of Ramadan intermittent fasting (RIF) on anthropometry and body composition has been questioned, none of the previous studies tried to explain the reported changes in these parameters. Also, systematic reviews that investigated the topic were limited to healthy individuals or a specific disease group.
Methods: The London Ramadan Study (LORANS) is an observational study on health effects of RIF. We measured weight, waist circumference (WC), hip circumference (HC), body mass index (BMI), waist-to-hip ratio (WHR), basal metabolic rate (BMR), fat percentage (FP), free-fat mass (FFM), extremities predicted muscle mass, total body water (TBW), trunk FM, trunk FFM and trunk predicted muscle mass before and immediately after Ramadan. Using mixed-effects regression models, we investigated the effect of RIF with adjustment for potential confounders. We also conducted a meta-analysis of the results of LORANS with other studies that investigated the effect of RIF on anthropometry and body composition. The review protocol is registered with PROSPERO registry (CRD42020186532).
Results: We recruited 146 participants (Mean ± SD age = 43.3 ± 15 years). Immediately after Ramadan, compared with before Ramadan, the mean difference was−1.6 kg (P<0.01) in weight,−1.95cm (P<0.01) in WC,−2.86cm (P <0.01) in HC, −0.60 kg/m2 (P < 0.01) in BMI and −1.24 kg (P < 0.01) in FM. In the systematic review and meta-analysis, after screening 2,150 titles and abstracts, 66 studies comprising 7,611 participants were included. In the general population, RIF was followed by a reduction of 1.12 Kg in body weight (−1.89– −0.36, I2 = 0), 0.74 kg/m2 reduction in BMI (−0.96– −0.53, I2 = 0), 1.54cm reduction in WC (−2.37– −0.71, I2 = 0) and 1.76cm reduction in HC (−2.69– −0.83, I2 = 0). The effect of fasting on anthropometric and body composition parameters starts to manifest in the second week of Ramadan and starts to diminish 3 weeks after Ramadan.
Conclusion: RIF is associated with a reduction in body weight, BMI, WC, HC, FM, FP and TBW. Most of these reductions are partially attributed to reduced FM and TBW. The reductions in these parameters appear to reverse after Ramadan.
Introduction
In the last few decades, more fasting regimens, usually referred to as intermittent fasting, have emerged as a non-pharmaceutical approach in integrative medicine and a method to reduce and control weight to improve health (1, 2). There are different types of intermittent fasting, but the most common ones are alternate-day fasting, time-restricted feeding, twice-a-week method and 24 h fasting (2). Ramadan intermittent fasting (RIF) is a model of time-restricted feeding. Every year, hundreds of millions of Muslims observe RIF. During Ramadan, Muslims fast from dawn to sunset and adopt a different lifestyle that could affect their health. Inevitably, this dramatic change in their dietary habits and lifestyle will be reflected in their anthropometric measurements and body composition, which are tightly connected to their health status. For instance, body weight and shape influence metabolism and insulin sensitivity (3, 4). Most studies that have investigated the effect of RIF on anthropometric and body composition parameters concluded that RIF is associated with lower weight, body mass index (BMI), fat mass (FM), fat percentage (FP), waist circumference (WC) and hip circumference (HC) (5–9). However, a few studies showed no changes or even an increase in these parameters (10–17). Moreover, none of the studies showing reductions in these parameters considered potential confounders that may have affected their findings or explained the observed changes (13, 14, 18–20) and none targeted the general population.
Furthermore, to date, seven meta-analyses have been done on the effect of RamadanRIF on body weight (21–24), BMI (24, 25), WC (26), FP (27), FM (24, 27), and fat-free mass (FFM) (24, 27). Still, none has done a meta-analysis on the effect on HC, muscle mass, total body water (TBW), and waist-to-hip ratio (WHR). The studies on BMI and FFM reported heterogeneous results. Also, except for one review which focused on type 2 diabetes patients (25), all others were limited to healthy individuals; therefore, the findings of these studies are not generalisable to the Muslim population (healthy and unhealthy). Using time of follow-up visits as a subgrouping variable, two reviews (23, 27) conducted a meta-analysis on the effect estimates at two time-points of follow-up (last week of Ramadan–a week after Ramadan; more than 2 weeks after Ramadan), but the other reviews observed the effect at only one time-point of follow-up. Conducting analyses at various time points of follow-up is required to know when the effects start to take place during Ramadan and whether they persist or fade away after Ramadan.
Therefore, to bridge these knowledge gaps, we conducted the London Ramadan Study (LORANS), which is a community-based study targeting the general population, in which we collected data on anthropometry and body composition of individuals as well as potential confounders to apply appropriate adjustments and explain the changes in the investigated parameters. And we conducted a systematic review and meta-analysis (including subgroup analysis based on time-points of follow-up) to investigate the effect of RIF on BMI, weight, FM, muscle mass, TBW, WC, HC, and WHR.
Methods
LORANS
LORANS is an observational study among the general population of Muslims in London during Ramadan 2019 (25 April−16 June 2019). We contacted six large mosques in London and provided them with information about the study. Out of the six, five mosques (Beitulfutuh Mosque, Finsbury Park Mosque, West London Mosque, Almanaar Mosque, and Madina Mosque) agreed to support the study and dedicate a room for recruitment and data collection. Before data collection, from 19 to 24 April, we launched a temporary website (https://fastingresearch.co.uk/) that provided information about the study and its aims and had a booking link enabling interested individuals to book their visits in one of the data collection settings. Further, we visited the five mosques to invite individuals who attended prayer sessions to take part in LORANS and distributed flyers about the study. And we asked mosque leaders to arrange for an announcement about our study right after a Friday midday prayer a couple of weeks before our data collection period.
We set up clinics in the five mosques where participants were recruited and data were collected. Within 10 days before Ramadan, we collected data on 146 participants from the five mosques. Eighty-five participants came for a second measurements visit which was 8–12 days after Ramadan. A comparison between participants who completed the study and those who only attended the first visit showed that the two groups were largely similar except for age and smoking status (Supplementary material 1).
We included all individuals 18 years old and over who were planning to fast for at least 20 days of Ramadan. Pregnant women and those who were not going to be available after Ramadan were excluded.
The measurements were collected from participants before Ramadan (from 26 to 30 April from 1 to 7 pm) and after Ramadan (from 10 to 14 June from 1 to 7 pm). We followed the Airwave study protocol (28) in data collection. We measured height, weight, WC and HC using a stadiometer (Leicester Height Measure), a weighing scale (Marsden digital weighing scale) and a body tape measure. Measurements were reported to the nearest 0.1 kg and 0.01. Each anthropometric measurement was repeated twice, and the average of the two measurements was recorded. Weight was measured without heavy clothes/items and shoes. WC was measured by wrapping the tape measure at the top of the hip bones or the narrowest area to the umbilicus if it was difficult to locate the hip bones. The HC was measured by wrapping the tape measure around the broadest area of the hips. Participants' body composition was measured using a bioelectrical impedance analyser (BIA) (model: Tanita BC-418) with substracting 2 kg from weight measured by the BIA to correct for clothes. For accuracy and safety, before using the BIA, we asked participants whether they have metal implants or pacemakers. Participants' body composition was measured using a multi-frequency segmental bioelectrical impedance analyser (BIA) (model: Tanita BC-418). This BIA model is built to last for around 300,000 measurements without the need of calibration and has eight tactile electrodes for hands and feet. The BIA estimates basal metabolic rate (BMR), FP, FM, FFM, and TBW. The BIA also estimates FP, FM, FFM and predicted muscle mass (PMM) in the trunk and each limb using prediction equations that involve height, weight, age and sex of the participant to calculate body composition parameters (29). It uses inbuilt equations derived from previously conducted regression analyses with Dual Energy X-ray Absorptiometry (DEXA). BIA has been validated in studies using DEXA and magnetic resonance imaging (30, 31). Participants were asked to take off heavy clothes and shoes before taking their measurements or using the BIA. Also, we wiped tactile electrodes with disinfectant Wipes after each use. We calculated BMI by dividing weight (kg) by height in meters squared. We took the average of the four extremities' predicted muscle masses to estimate extremities PMM.
All participants submitted an online questionnaire about their lifestyle and socioeconomic status. Also, 55 participants filled out a 3-day food diary before and during Ramadan. The 3 days consisted of 2 weekdays and 1 weekend day to capture changes in diet during weekends. The food diary included instuctions about how to fill it out and examples for the participants. Nutritics (nutrition software) was used for food diary analysis (32).
The ethics committee at Imperial College London approved the study (reference: 19IC5138, dated 17/4/2019), and all participants gave informed consent before taking part.
Systematic review
We conducted a systematic review following the PRISMA guidelines (Supplementary material 2) and registered the review protocol under the PROSPERO registry of CRD42020186532.
Eligibility criteria
We sought published and unpublished studies that examined the effect of RIF on anthropometric measurements and/or body composition. We considered studies that measured any anthropometric or a body composition measure before and during/after Ramadan. We only included studies that reported measurements as means and SDs to obtain the pooled effect. We excluded reviews, studies that involved any other intervention besides RIF, studies on pregnant women and studies of athletes.
Information sources, search and study selection
We searched three databases: PubMed, Embase and Scopus from inception until 6 May 2022, seeking all relevant published studies without language restrictions. We used this search approach “Ramadan” or “Ramadan fasting” or “Ramadan intermittent fasting” and (“anthropometr*” or “weight” or “BMI” or “fat” or “body composition” or “waist circumference” or “obes*” or “body mass index” or “hip circumference”).
Each of the following procedures was carried out twice and in parallel by two independent reviewers (divided among RA, NW, KB, ME, ZB, ZA, and AA). We screened all titles and abstracts of all potential studies; then we assessed the full-texts of studies that were deemed eligible. We resolved disagreements by consensus.
Data collection process
RA, NW, ME and ZB extracted all relevant data from enrolled studies in a spreadsheet. Extracted data included: author, year, study country, journal, sample size, population type, tools used for measurements, means and SDs of anthropometric and body composition measurements including weight, height, BMI, WC, HC, basal metabolic rate (BMR), FM, muscle mass, FFM, TBW and WHR in all time-points; information on adjustments (if any).
Risk of bias
We modified the Newcastle-Ottawa Quality Assessment Scale of cohort studies (33) to make a version that could be applied in this review. The scale (Supplementary material 3) is based on selection, comparability and outcome. Based on the quality score, we classified studies as either low quality (0–4), satisfactory (5, 6), good (7, 8) or very good (9). RA, NW, ME and ZB assessed the quality of all selected studies independently in parallel and resolved disagreements by consensus. Supplementary material 4 shows the quality scores of selected studies.
Estimating fasting time length
We adopted the same method developed by Faris et al. (26), which basically relies on “timeanddate” (https://www.timeanddate.com/sun/@8469718) to estimate the day length (from sunrise and sunset). Since Muslims start fasting around 80 min before sunrise (Al-Fajr prayer call), 80 min should be added to the day length to estimate the fasting time.
Statistical analysis
LORANS
Using multiple imputations with (“mice”) package in R (Windows 3.6.1), we imputed the second measurements of weight, WC, HC, BMR, FM, FP, FFM, TBW, extremities PMM, trunk FM, trunk FFM and trunk PMM for the 61 participants who didn't attend the second visit. Afterwards, we calculated BMI and WHR based on the imputed values.
We used R (“lme4” package) to apply linear mixed-effects model regression to estimate the impact of RIF on anthropometric measurements and body composition. The linear mixed-effects model allowed us to correct for potential confounders, including both fixed and random factors. The dependent variables were the anthropometric and body composition parameters. The independent variables were age, sex, number of fasting days during Ramadan, day of the second measurement, and location (mosque). Also, we adjusted for energy intake, extremities PMM, fat mass and TBW to explore to what extent these parameters contribute to the changes in the other dependent variables. We ran the analysis using five models. In the first model, we adjusted for age, sex, number of fasting days, second visit day and location. Other models were further adjusted for energy intake (model 2); extremities PMM (model 3); FM (model 4); and TBW (model 5). These adjustments were applied to investigate the effects of potential confounders (which were measured before and after Ramadan) and to explain the observed changes in anthropometric measurements and body composition. Moreover, we grouped the participants based on their baseline BMI (normal weight = 18.5– <25; overweight = 25.0– <30; obesity = ≥30 kg/m2) and retested the changes of anthropometric and body composition indices (using the first model discussed above). When the correlation coefficient was >0.6 between the outcome and potential confounders, we did not apply the model to avoid collinearity. We considered the result to be statistically significant if the p < 0.05.
Meta-analysis
We used R (Windows 3.6.1, “meta” package) to run an inverse variance weighted fixed-effects model to estimate the pooled effect (difference in means after/before Ramadan from included studies) of RIF on anthropometric and body composition measures. Also, we estimated the consistency of included studies by a test of heterogeneity (I2). We grouped studies based on the timing of their follow-up visits. To collate studies with similar follow-up, we grouped studies into four time-points of follow-up: middle of Ramadan (2nd/3rd week of Ramadan), end of Ramadan (4th week of Ramadan), immediately after Ramadan (within 2 weeks after Ramadan) and long after Ramadan (three to 6 weeks after Ramadan). Meta-analysis was separately done for each measured parameter which were BMI, weight, FP, FM, WC, HC, WHR, TBW and muscle mass. If a study measured a parameter at two different time points (e.g., 4th week of Ramadan and long after Ramadan), we included it in both meta-analyses. This approach led to having 25 meta-analyses with three studies being the smallest number of studies in a meta-analysis. The pooled effect with a p < 0.05 was deemed statistically significant.
The potential presence of the small-study effect was assessed qualitatively (visualizing funnel plots) and quantitively (using Egger's regression tests) (34). If Egger's test had a p < 0.1, we applied the trim and fill method to address the asymmetry. Then, we re-estimated the effect under this correction and compared it to the original effect.
Results
LORANS
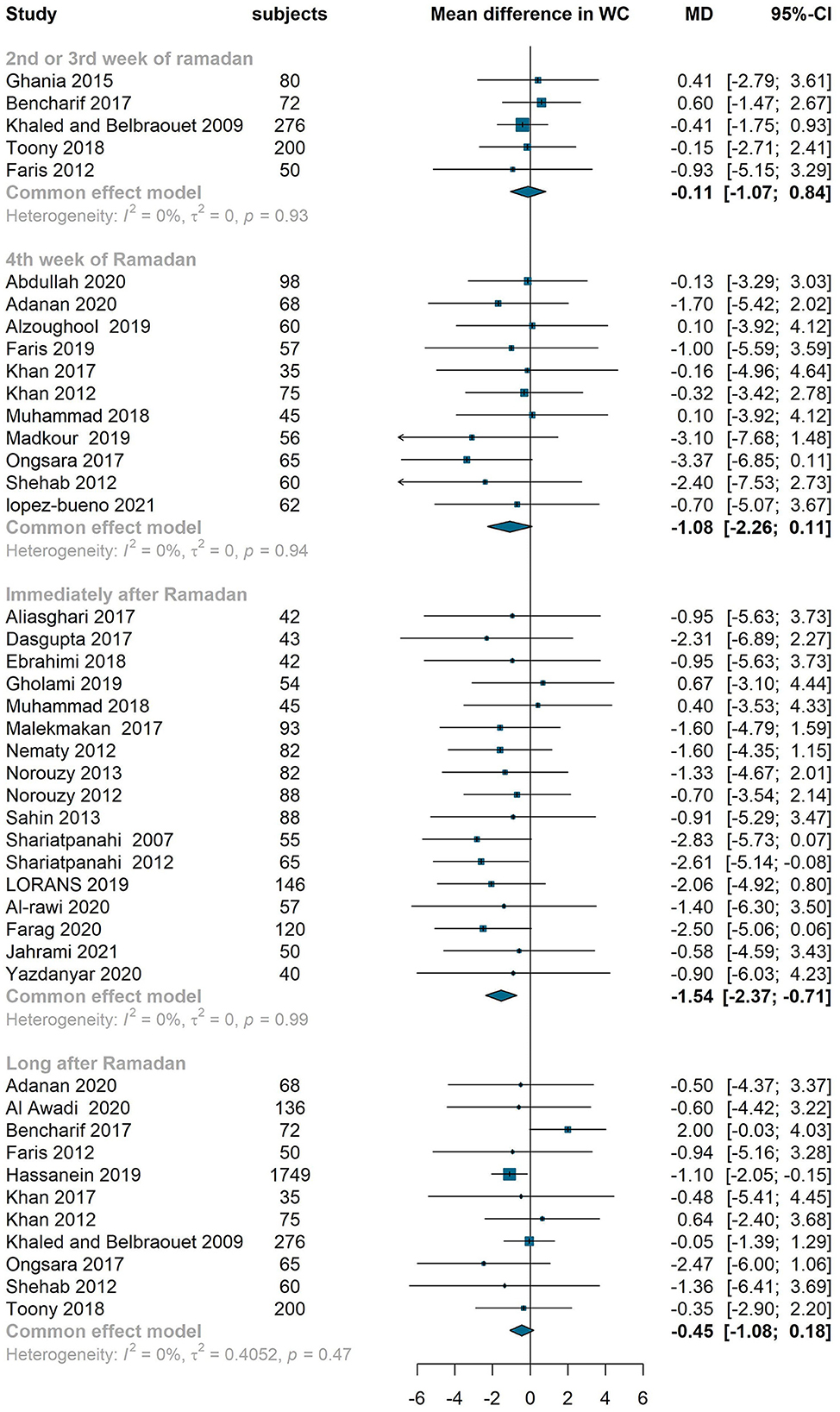
Supplementary material 5 shows the participants' baseline characteristics. Out of the 146 participants, 75 (51.4%) participants were male and mean ± SD age was 43.3 ± 15 years. During Ramadan, total energy intake was 1,507 kcal compared to 1,503 kcal before Ramadan (P = 0.940). Similarly, no significant changes were reported in intakes of carbohydrates (16.9 g, 0.3–34, P = 0.214), protein (−7.4, −16.1–1.3, P = 0.110) or fat (−3.8 g, −10.4–3, P = 0.274) during Ramadan. After Ramadan, there was a significant reduction of 1.6 kg (P < 0.01) in body weight, 1.95 cm (P < 0.01) in WC, 2.86 cm (P < 0.01) in HC, 0.60 kg/m2 (P < 0.01) in BMI, 1.05% (P < 0.01) in FP, 1.24 kg (P < 0.01) in FM and 1.45 liter (P < 0.01) in TBW (Figure 1). We also observed non-significant decreases in FFM (−0.21 kg), trunk FP (−0.85 kg) and trunk FM (−0.53 kg). The change in extremities' PMM was non-significant and negligible. BMR decreased by −12.8 Kcal (P < 0.05) after Ramadan. Further, adjustment for energy intake only diminished the decrease in WC (from −1.95 to −1.49 cm), and trunk FP (from −0.85 to −0.73). None of the observed differences was influenced by adjusting for extremities PMM in the third model. Almost all mean differences were influenced by the fourth and fifth models. After adjustment for FM, the reductions in weight and trunk FFM became non-significant. Also, the reduction in WC became non-significant when adjusted for TBW in the fifth model (Supplementary material 6).
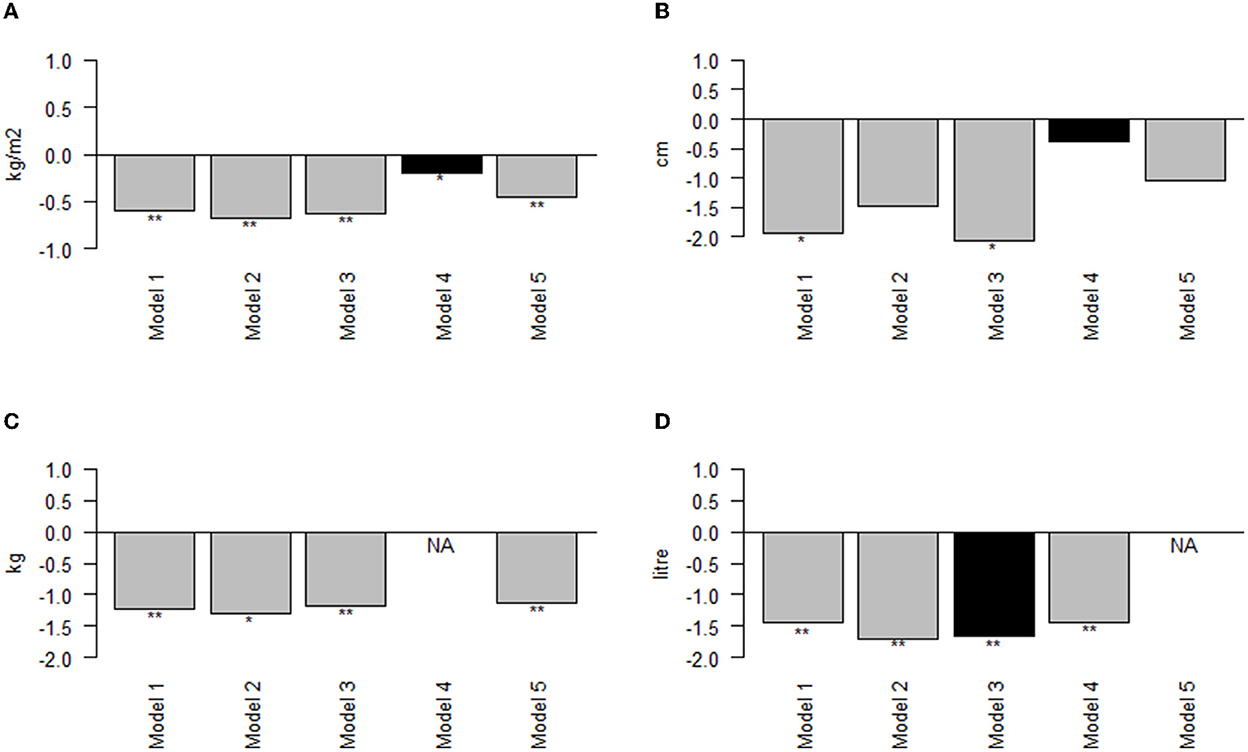
Figure 1. Effect of adjustments on mean difference in BMI, waist circumference, fat mass and total body water from LORANS. (A) Mean difference in BMI; (B) Mean difference in waist circumference; (C) Mean difference in fat mass; (D) Mean difference in total body water; *: P < 0.05; **: P < 0.001; NA, the model adjusts for the outcome; Black bar, the outcome is highly correlated (r > 0.6) with the variable adjusted for.
When we divided participants into groups based on baseline BMI, we noticed that the weight and BMI reductions were non-significant in individuals with obesity. And HC and TBW reductions were non-significant in individuals with normal weight (Supplementary material 7).
Systematic review
After screening 2,150 titles /abstracts and reading 432 full texts, we identified 139 studies (Figure 2). Of these, 73 studies had low-quality scores (quality score average = 3.85 out of 9) and were not included in the review. As a result, we included 66 studies (including LORANS) with a total of 7,496 participants in the meta-analysis. Of these, 55 studies were classified as satisfactory quality with moderate risk of bias and 10 studies as good quality with low risk of bias (Supplementary material 4).
Study characteristics
The included studies were from 20 countries and most commonly (15 studies, 22.7%) were conducted in Iran (Table 1). The majority of the studies targeted healthy individuals (21 studies). Others included type 2 diabetes patients (21 studies), overweight/obese individuals (four studies), chronic kidney disease (CKD) patients (five studies), and individuals with metabolic syndrome (three studies). LORANS was the only community-based study, targeting the general population. Weight was the most commonly investigated anthropometric index (54 studies) followed by BMI (50 studies), WC (33 studies), FP (13 studies), HC (13 studies), WHR (12 studies), FM (11 studies), MM (7 studies) and TBW (7 studies) (Supplementary material 8).
Effect on BMI and weight
We observed a similar pattern (a drop at the end of Ramada/immediately after Ramadan and a rise long after Ramadan) in BMI and weight. Compared to baseline values, BMI reduced at middle of Ramadan by 0.44 kg/m2 (95 % confidence interval −0.87 to 0, I2 = 9%), end of Ramadan by 0.36 kg/m2 (−0.71 to −0.02, I2=0%) and immediately after Ramadan by 0.74 kg/m2 (−0.96 to −0.53, I2=0%). However, the mean difference of BMI between baseline and long after Ramadan was not significant (−0.14 kg/m2, −0.43 to 0.14, I2=0%) (Figure 3). The similar pattern was observed in weight which decreased significantly at middle, end and immediately after Ramadan (−1.55 kg, −2.65– −0.44, I2 = 0%; −1.22 kg, −2.29– −0.15, I2 = 0%; −1.12 kg, −1.89– −0.36, I2 = 0%, respectively) but the reduction was not significant long after Ramadan (−0.32 kg, −1.95–0.31, I2 = 0%) (Figure 4).
Effect on fat, muscle and body water
At the end of Ramadan and immediately after Ramadan, there was a drop in both FP (−0.66 kg, −1.57–0.25, I2 = 0%; −0.46 kg, −1.45–0.53, I2 = 0%) and FM (−0.64 kg, −1.54–0.26, I2 = 0%; −0.49 kg, −1.62–0.65, I2 = 0%). Long after Ramadan, FP (1.15 kg, 0.14–2.16, I2 = 32%) and FM (0.95 kg, −0.15–2.06, I2 = 0%) were higher than the baseline values (Supplementary materials 9, 10). Muscle mass reduced by the end of Ramadan by −0.25 kg (−2.10–1.60, I2 = 0%) (Supplementary material 11). TBW was also reduced at the end of Ramadan by −0.25 kg (−1.16–0.67, I2 = 0%) and immediately after Ramadan by −1.09 kg (−2.29–0.11, I2 = 0%) (Supplementary material 12).
Effect on WC, HC and WHR
WC, HC and WHR are also affected by RIF. The meta-analysis showed reductions compared to baseline in WC in the middle of Ramadan (−0.11 cm, −1.07–0.84, I2 = 0%), at the end of Ramadan (−1.08 cm, −2.26–0.11, I2 = 0%), immediately after Ramadan (−1.54 cm, −2.37– −0.71, I2 = 0%) but no significant difference long after Ramadan (−0.45 cm, −1.08–0.18, I2 = 0%) (Figure 5). HC did not change by the end of Ramadan (−0.07 cm, −1.82–1.69, I2 = 0%), decreased significantly immediately after Ramadan (−1.76 cm, −2.69– −0.83, I2 = 10%) and did not show a significant difference long after Ramadan (0.26 cm, −1.89–2.41, I2 = 0%) (Supplementary material 13). There was a negligible change in the waist to hip ratio at the middle, end and long after Ramadan (Supplementary material 14).
Small-study effects bias
To assess for asymmetry, we constructed funnel plots and ran Egger's test on all subgroups and considered a significant p-value as evidence for asymmetry (Supplementary material 15). The trim and fill method was applied to correct for the potential asymmetry. However, after applying this method, no changes were observed in the effects.
Discussion
LORANS found that RIF is associated with a significant reduction in body weight, WC, HC, BMI, FP, FM, TBW, trunk FFM and trunk PMM immediately after Ramadan. Most of these changes were independent of physical activity, energy intake and extremities PMM but partially dependent on TBW and FM. The meta-analysis has 66 studies (including LORANS) and 7,496 participants indicated a significant reduction in weight, BMI, WC and HC starting within the second and third weeks of Ramadan, continuing in the fourth week of Ramadan, peaking immediately after Ramadan and declining to reach the pre-Ramadan levels 3 weeks or more after Ramadan.
Conducting LORANS enabled us to investigate the effect of adjustments on the changes in anthropometric and body composition indices of interest. The main adjustments that made a change in anthropometric changes after Ramadan were FM and TBW which decreased significantly after Ramadan and are more likely to be mediators rather than confounders. In other words, the observed changes in anthropometric and body composition measures are due to losing fat or dehydration. The latter should not be confused with daily dehydration which happens due to abstinence from water drinking during Ramadan since the measurements were done a few days after Ramadan when participants were supposed to be well-hydrated. Although some studies reported that RIF is associated with lower energy intake and physical activity (85, 86), the two factors didn't change significantly after Ramadan and didn't change the observed effects of RIF on anthropometric and body composition indices in LORANS. Fernando et al. (27) argued that decreased weight and fat might be due to increased energy expenditure, but another study showed that there is no association between RIF and energy expenditure (86).
Several animal and human studies on intermittent fasting reported reduced body fat and maintained muscle and attributed the observed effects to the metabolic switch (87–89). In this state, the body uses ketones and fatty acids for energy and the metabolism becomes more efficient (90). Although we reported similar effects, we are still uncertain about the mechanism behind the effects of RIF on anthropometric measurements and body composition due to the differences between RIF and the other types of intermittent fasting.
In 2022, Erdem et al. conducted a recent study (91) that assigned 360 individuals into five groups, including time-restricted fasting (TRF) with 6 h eating window (TRF-6 h), TRF with 8 h eating window (TRF-8 h) and alternate-day fasting (ADF). There was no restriction on calorie intake in the two TRF models, but it was restricted to <500 kcal 2 days per week in ADF. They measured anthropometric measurements on three-time points (after 1, 6 and 12 weeks). Similarly to Ramadan effects in our study, the authors reported that the three fasting models significantly reduced weight, BMI, and WC but not HC. Interestingly, although energy intake in the two TFR groups was almost identical, the reductions in all indices were greater in group TRF-6 h than in group TRF-8 h. The eating window in the two TRF models is close to that in LORANS (~7 h). However, the eating window was at night in LORANS, but in Erdem et al. study was during daylight hours. Also, unlike RIF, no-calorie drinks were allowed in Erdem et al. study. RIF has no calorie restriction like ADF. In addition, the duration of exposure in LORANS (4 weeks) is not the same as in Erdem et al. (1 week, 6 weeks and 8 weeks). These differences make the direct comparison between RIF and the other three models of intermittent fasting (TRF-6 h, TRF-8 h and ADF) imprecise. However, the anthropometric measurements' reductions in LORANS were half or less than that reduced in the other three models after 6 weeks. Furthermore, a systematic review and meta-analysis (24) compared the effect of RIF on anthropometric and body composition indices to that of non-RIF (all other types of intermittent fasting) combined. This review reported that both reduced the indices, but the non-RIF had a greater effect.
Although this review is the only one that investigated effects on the general population and didn't focus on a particular group of participants, most of our findings are consistent with other reviews. The significant reduction observed in weight during the fourth week and immediately after Ramadan is compatible with four of the previous systematic reviews (21–24, 27). Likewise, the decrease in WC was similar to the decrease reported by Faris et al. (26). For BMI, however, a meta-analysis by Aydin et al. (25) reported no significant decrease in BMI, whereas we observed a significant decrease immediately after Ramadan. This difference is due to the fact that the pooled estimate from Aydin et al. included a wide range of measurement times from the last week of Ramadan up to 6 weeks after Ramadan. We also reported that the differences were not significant long after Ramadan. It is possible that the overall effect estimates are diluted in Aydin et al. and did not reach the significance level. Another review (27) that reported a meta-analysis of data from studies on healthy and overweight/obese individuals showed a significant decrease in FM and FP during the fourth week and immediately after Ramadan followed by a return to baseline levels long after Ramadan. In that meta-analysis, the authors included more studies on overweight/obese individuals than studies on individuals with a healthy weight. This suggests that, compared to normal weight people, overweight/obese individuals lose more FM and FP during Ramadan. However, this was not the case in LORANS.
The bioelectrical impedance analyser depends on tissues electrical conductivity which varies based on their water content (92). It requires information for each participant (i.e., sex and age) to use an appropriate equation to predict body composition parameters (93). However, BIA uses constant values for density and hydration of FFM and assumes that they are similar in all individuals when estimating FFM (94), then it predicts FM based on the estimated FFM (92). Also, calculated parameters by BIA are not identical to some other reference methods that have higher precision such as DEXA (93). Although BIA may underestimate or overestimate FP (30), it's precision is high enough to be used in epidemiological studies (95). Using DEXA in LORANS would be impractical, and BIA appeared to be the best method to be used due to the study nature, being operator-independent and its high precision (30, 95–98).
This study has several strengths. LORANS is a community-based study while all previous studies didn't target the general population. Also, this is the only systematic review and meta-analysis conducted to observe the effect of RIF on anthropometric measurements and body composition in the general population rather than in specific groups such as healthy individuals (21–23, 26, 27) or T2D patients (25). For the first time, we conducted a meta-analysis on the effect of RIF at four different time points of follow-up which allowed us to make conclusions on the reversibility of the changes in anthropometry and body composition after Ramadan. Moreover, LORANS allowed us to investigate the anthropometric and body composition changes independent of changes in energy intake as well as physiological changes such as TBW and FM. A number of limitations should also be acknowledged. First, the second visit in LORANS was 8–12 days after Ramadan, meaning that the lifestyle changes during these days interfered with the effect of RIF. Another limitation in LORANS is the 41.7% drop-out in the baseline sample. Also, in the meta-analysis, we did not find many studies that have studied indices such as MM, so it was not possible to conduct separate meta-analyses at different time points. Moreover, not all indices were measured at all time points. Thus, the meta-analysis for various time points included different studies which reduced the comparability of the time points. Finally, we observed an indication of small-studies bias in six of the subgroups. However, applying the trim and fill method on these subgroups showed that the effect of bias is minimal.
In the general population, RIF is associated with reductions in weight, BMI, WC and HC. These reductions tend to start at the second/third week of Ramadan, become significant in the fourth week, reach their maximum immediately after Ramadan, and fade away 3–6 weeks after Ramadan. Reductions in TBW and FM might drive the changes in anthropometric and body composition changes during and after Ramadan.
Author contributions
RA-J, AD, and KT conceptualized the paper and interpreted data analysis. RA-J and AD collected data. RA-J, NW, KB, ME, ZB, ZA, and AA screened abstracts and full-texts. RA-J, NW, ME, and ZB extracted data and assessed the quality of reviewed studies. AD, KT, and PE critically reviewed the manuscript and provided feedback. RA-J is the guarantor, wrote the manuscript, and attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors contributed to the article and approved the submitted version.
Funding
This project was partially funded by the Saudi Arabia Cultural Bureau in London. The funder had no role in either the study design, data collection, data analysis, data interpretation or the decision to publishing the study. RA-J was a PhD student sponsored by the funder, and all other researchers are independent of the funder.
Acknowledgments
PE was Director of the MRC Centre for Environment and Health and acknowledges support from the Medical Research Council (MR/L01341X/1, MR/S019669/1). PE also acknowledges support from the National Institute for Health Research NIHR Imperial Biomedical Research Centre, Imperial College London; and the British Heart Foundation Imperial College Centre for Research Excellence. PE was a UK DRI Professor at the UK Dementia Research Institute, Imperial College London, which receives funding from the Medical Research Council, Alzheimer's Society and Alzheimer's Research UK.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1082217/full#supplementary-material
Supplementary material 1. Characteristics of individuals who did not attend the second visit after Ramadan compared to LORANS participants.
Supplementary material 2. PRISMA checklist.
Supplementary material 3. Newcastle-Ottawa quality assessment scale (Adapted).
Supplementary material 4. Quality assessment of potential.
Supplementary material 5. Characteristics of LORANS' participants (n = 146).
Supplementary material 6. Effect of adjustments on mean difference in anthropometric and body composition parameters from LORANS.
Supplementary material 7. Effect of RIF on anthropometric and body composition parameters on LORANS participants grouped by baseline BMI classes.
Supplementary material 8. The included studies in the meta-analysis with measured parameters and time-point of measurement.
Supplementary material 9. Fixed effect meta-analysis of RIF effect on fat percentage.
Supplementary material 10. Fixed effect meta-analysis of RIF effect on fat mass.
Supplementary material 11. Fixed effect meta-analysis of RIF effect on muscle mass during the fourth week of Ramadan.
Supplementary material 12. Fixed effect meta-analysis of RIF effect on total body water.
Supplementary material 13. Fixed effect meta-analysis of RIF effect on hip circumference.
Supplementary material 14. Fixed effect meta-analysis of RIF effect on the waist to hip ratio.
Supplementary material 15. Risk of bias tests.
References
1. Michalsen A, Hoffmann B, Moebus S, Bäcker M, Langhorst J, Dobos GJ. Incorporation of fasting therapy in an integrative medicine ward: evaluation of outcome, safety, and effects on lifestyle adherence in a large prospective cohort study. J Altern Complement Med. (2005) 11:601–7. doi: 10.1089/acm.2005.11.601
2. Cleveland Clinic,. Intermittent Fasting: 4 Different Types Explained (2019). Available online at: https://health.clevelandclinic.org/intermittent-fasting-4-differenttypes-explained/ (accessed December 22, 2020).
3. Duren DL, Sherwood RJ, Czerwinski SA, Lee M, Choh AC, Siervogel RM, et al. Body composition methods: comparisons and interpretation. J Diabetes Sci Technol. (2008) 2:1139–46. doi: 10.1177/193229680800200623
4. Osborne G, Wu F, Yang L, Kelly D, Hu J, Li H, et al. The association between gut microbiome and anthropometric measurements in Bangladesh. Gut Microbes. (2020) 11:63–76. doi: 10.1080/19490976.2019.1614394
5. Akkoca M, Metin Z, Topaloglu O, Tokgöz S, Cihan G, San I. An evaluation of the effects of Ramadan fasting and sahur meal on anthropometric, metabolic and endocrine parameters. Clin Nutr. (2018) 37:S270. doi: 10.1016/j.clnu.2018.06.1950
6. Iqbal M, Jamea AA, Alonso-Alonso M, Al-Regaiey KA, Bashir S. Cortical thickness, neurocognitive, and body composition effects of fasting during Ramadan. J Res Med Sci. (2019) 24:50. doi: 10.4103/jrms.JRMS_783_18
7. Adanan NIH, Md Ali MS, Lim JH, Zakaria NF, Lim CTS, Yahya R, et al. Investigating physical and nutritional changes during prolonged intermittent fasting in hemodialysis patients: a prospective cohort study. J Ren Nutr. (2020) 30:e15–26. doi: 10.1053/j.jrn.2019.06.003
8. Ebrahimi S, Gargari BP, Izadi A, Imani B, Asjodi F. The effects of Ramadan fasting on serum concentrations of vaspin and omentin-1 in patients with nonalcoholic fatty liver disease. Eur J Integr Med. (2018) 19:110–4. doi: 10.1016/j.eujim.2018.03.002
9. Faris MAE, Madkour MI, Obaideen AK, Dalah EZ, Hasan HA, Radwan H, et al. Effect of Ramadan diurnal fasting on visceral adiposity and serum adipokines in overweight and obese individuals. Diabetes Res Clin Pract. (2019) 153:166–75. doi: 10.1016/j.diabres.2019.05.023
10. Adnan WAHWM, Zaharan NL, Wong MH, Lim SK. The effects of intermittent fasting during the month of Ramadan in chronic haemodialysis patients in a tropical climate country. PLoS ONE. (2014) 9:e114262. doi: 10.1371/journal.pone.0114262
11. Alzoughool F, Hourani HM, Atoum M, Abdelgader R, Alanagreh L. Irisin, leptin and adiponectin levels are reduced significantly during fasting. Med J Nutrition Metab. (2019) 12:389–96. doi: 10.3233/MNM-190322
12. Devendra D, Gohel B, Bravis V, Hui E, Salih S, Mehar S, et al. Vildagliptin therapy and hypoglycaemia in Muslim type 2 diabetes patients during Ramadan. Int J Clin Pract. (2009) 63:1446–50. doi: 10.1111/j.1742-1241.2009.02171.x
13. Gholami S, Hazar N, Shafiei S, Hemmati M, Rahmanian M. Biochemical and anthropometric changes during Ramadan among type 2 diabetes mellitus patients. Int J Diabetes Dev Ctries. (2019) 39:160–5. doi: 10.1007/s13410-018-0656-8
14. Karatoprak C, Yolbas S, Cakirca M, Cinar A, Zorlu M, Kiskac M, et al. The effects of long term fasting in Ramadan on glucose regulation in type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci. (2013) 17:2512–6.
15. Sulu B, Öztürk B, Güven A, Kilic K. The effect of long-term controlled fasting (the Ramadan model) on body mass index, blood biochemistry and oxidative stress factors. Turkiye Klinikleri Tip Bilimleri Dergisi. (2010) 30:855–63. doi: 10.5336/medsci.2008-9981
16. Nachvak SM, Pasdar Y, Pirsaheb S, Darbandi M, Niazi P, Mostafai R, et al. Effects of Ramadan on food intake, glucose homeostasis, lipid profiles and body composition composition. Eur J Clin Nutr. (2018) 73:594–600. doi: 10.1038/s41430-018-0189-8
17. Ongsara S, Boonpol S, Prompalad N, Jeenduang N. The effect of Ramadan fasting on biochemical parameters in healthy thai subjects. J Clin Diagn Res. (2017) 11:Bc14–bc8. doi: 10.7860/JCDR/2017/27294.10634
18. Bouida W, Baccouche H, Sassi M, Dridi Z, Chakroun T, Hellara I, et al. Effects of Ramadan fasting on platelet reactivity in diabetic patients treated with clopidogrel. Thromb J. (2017) 15:15. doi: 10.1186/s12959-017-0138-0
19. Dasgupta A, Garg S, Pal B, Maharana SP, Bandhopadhayay L, Mallick N Jr. Is ramadan fasting cardio-protective? a study in a village of West Bengal. Ind J Commun Health. (2017) 29:203–8. doi: 10.47203/IJCH.2017.v29i02.015
20. Faris MAIE, Kacimi S, Al-Kurd RA, Fararjeh MA, Bustanji YK, Mohammad MK, et al. Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutr Res. (2012) 32:947–55. doi: 10.1016/j.nutres.2012.06.021
21. Jahrami HA, Alsibai J, Clark CCT, Faris MAE. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur J Nutr. (2020) 59:2291–316. doi: 10.1007/s00394-020-02216-1
22. Kul S, Savaş E, Öztürk ZA, Karadag G. Does Ramadan fasting alter body weight and blood lipids and fasting blood glucose in a healthy population? A meta-analysis. J Relig Health. (2014) 53:929–42. doi: 10.1007/s10943-013-9687-0
23. Sadeghirad B, Motaghipisheh S, Kolahdooz F, Zahedi MJ, Haghdoost AA. Islamic fasting and weight loss: a systematic review and meta-analysis. Public Health Nutr. (2014) 17:396–406. doi: 10.1017/S1368980012005046
24. Correia JM, Santos I, Pezarat-Correia P, Silva AM, Mendonca GV. Effects of Ramadan and non-Ramadan intermittent fasting on body composition: a systematic review and meta-analysis. Front Nutr. (2020) 7:625240. doi: 10.3389/fnut.2020.625240
25. Aydin N, Kul S, Karadag G, Tabur S, Araz M. Effect of Ramadan fasting on glycaemic parameters and body mass index in type II diabetic patients: a meta-analysis. Indian J Med Res. (2019) 150:546–56. doi: 10.4103/ijmr.IJMR_1380_17
26. Faris MAE, Jahrami HA, Alsibai J, Obaideen AA. Impact of Ramadan diurnal intermittent fasting on metabolic syndrome components in healthy, non-athletic muslim people aged over 15 years: a systematic review and meta-analysis. Br J Nutr. (2019) 123:1—22. doi: 10.1017/S000711451900254X
27. Fernando HA, Zibellini J, Harris RA, Seimon RV, Sainsbury A. Effect of Ramadan fasting on weight and body composition in healthy non-athlete adults: a systematic review and meta-analysis. Nutrients. (2019) 11:478. doi: 10.3390/nu11020478
28. Elliott P, Vergnaud A-C, Singh D, Neasham D, Spear J, Heard A. The airwave health monitoring study of police officers and staff in great britain: rationale, design and methods. Environ Res. (2014) 134:280–5. doi: 10.1016/j.envres.2014.07.025
29. Nichols J, Going S, Loftin M, Stewart D, Nowicki E, Pickrel J. Comparison of two bioelectrical impedance analysis instruments for determining body composition in adolescent girls. Int J Body Compos Res. (2006) 4:153–60.
30. Sun G, French CR, Martin GR, Younghusband B, Green RC, Xie YG, et al. Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am J Clin Nutr. (2005) 81:74–8. doi: 10.1093/ajcn/81.1.74
31. Wang JG, Zhang Y, Chen HE Li Y, Cheng XG, Xu L, et al. Comparison of two bioelectrical impedance analysis devices with dual energy X-ray absorptiometry and magnetic resonance imaging in the estimation of body composition. J Strength Cond Res. (2013) 27:236–43. doi: 10.1519/JSC.0b013e31824f2040
33. Wells G, Shea, B, O'Connell, D, Peterson, J, Welch, V, Losos, M, . The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analyses. The Ottawa Hospital Research Institute (2019). Available online at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed May 5, 2020).
34. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629. doi: 10.1136/bmj.315.7109.629
35. Ahmadinejad Z, Ziaee V, Rezaee M, Yarmohammadi L, Shaikh H, Bozorgi F, et al. The effect of ramadan fasting on thyroid hormone profile: a cohort study. Pakistan J Biol Sci. (2006) 9:1999–2002. doi: 10.3923/pjbs.2006.1999.2002
36. Al Awadi FF, Echtay A, Al Arouj M, Sabir Ali S, Shehadeh N, Al Shaikh A, et al. Patterns of diabetes care among people with type 1 diabetes during Ramadan: an international prospective study (DAR-MENA T1DM). Adv Ther. (2020) 37:1550–63. doi: 10.1007/s12325-020-01267-4
37. Aliasghari F, Izadi A, Gargari BP, Ebrahimi S. The effects of Ramadan fasting on body composition, blood pressure, glucose metabolism, and markers of inflammation in NAFLD patients: an observational trial. J Am Coll Nutr. (2017) 36:640–5. doi: 10.1080/07315724.2017.1339644
38. Akanji AO, Mojiminiyi OA, Abdella N. Beneficial changes in serum apo A-1 and its ratio to apo B and HDL in stable hyperlipidaemic subjects after Ramadan fasting in Kuwait. Eur J Clin Nutr. (2000) 54:508–13. doi: 10.1038/sj.ejcn.1601047
39. Bahmani A. Islamic fasting and its effect on pre-diabetic population. Sci J Kurdistan Univ Med Sci. (2013) 18:40–6.
40. Bashier A, Khalifa AA, Abdelgadir EI, Al Saeed MA, Al Qaysi AA, Bayati MBA, et al. Safety of sodium-glucose cotransporter 2 inhibitors (SGLT2-I) during the month of Ramadan in muslim patients with type 2 diabetes. Oman Med J. (2018) 33:104–10. doi: 10.5001/omj.2018.21
41. Bernieh B, Al Hakim MR, Boobes Y, Abu Zidan FM. Fasting Ramadan in chronic kidney disease patients: clinical and biochemical effects. Saudi J Kidney Dis Transpl. (2010) 21:898–902.
42. Bencharif M, Chaima B, Amal F, Youcef B. Effect of pre-Ramadan education on dietary intake and anthropometry-comparison between two groups of diabetic patients. Romanian J Diabet Nutr Metab Dis. (2017) 24:295–307. doi: 10.1515/rjdnmd-2017-0035
43. Elfert AA, AbouSaif SA, Abdel Kader NA, AbdelAal E, Elfert AY, Moez A, et al. A multicenter pilot study of the effects of Ramadan fasting on patients with liver cirrhosis. Tanta Med Sci J. (2011).
44. Feizollahzadeh S, Rasuli J, Kheirouri S, AlizadehM. Augmented plasma adiponectin after prolonged fasting during Ramadan in men. Health Promot Perspect. (2014) 4:77–81. doi: 10.5681/hpp.2014.010
45. Finch GM, Day JE, Razak, Welch DA, Rogers PJ. Appetite changes under free-living conditions during Ramadan fasting. Appetite. (1998) 31:159–70. doi: 10.1006/appe.1998.0164
46. Hassanein M, Al Awadi FF, El Hadidy KES, Ali SS, Echtay A, Djaballah K, et al. The characteristics and pattern of care for the type 2 diabetes mellitus population in the MENA region during Ramadan: an international prospective study (DAR-MENA T2DM). Diabetes Res Clin Pract. (2019) 151:275–84. doi: 10.1016/j.diabres.2019.02.020
47. Hassanein M, Hanif W, Malik W, Kamal A, Geransar P, Lister N, et al. Comparison of the dipeptidyl peptidase-4 inhibitor vildagliptin and the sulphonylurea gliclazide in combination with metformin, in Muslim patients with type 2 diabetes mellitus fasting during Ramadan: results of the VECTOR study. Curr Med Res Opin. (2011) 27:1367–74. doi: 10.1185/03007995.2011.579951
48. Khan N, Rasheed A, Ahmed H, Aslam F, Kanwal F. Effect of Ramadan fasting on glucose level, lipid profile, HbA1c and uric acid among medical students in Karachi, Pakistan. East Mediterr Health J. (2017) 23:274–9. doi: 10.26719/2017.23.4.274
49. Khattak MMAK, Mazlan Mamat N, Azdie Mohd Abu Bakar W, Firdaus Nazri Shaharuddin M. Does religious fasting affect energy and macro-nutrients intakes? Nutr Food Sci. (2013) 43:254–60. doi: 10.1108/00346651311327909
50. Kiyani MM, Memon AR, Amjad MI, Ameer MR, Sadiq M, Mahmood T. Study of human biochemical parameters during and after Ramadan. J Relig Health. (2017) 56:55–62. doi: 10.1007/s10943-015-0084-8
51. Muhammad H, Latifah FN, Susilowati R. The yo-yo effect of Ramadan fasting on overweight/obese individuals in Indonesian: a prospective study. Med J Nutrition Metab. (2018) 11:127–33. doi: 10.3233/MNM-17188
52. Madkour MI, A TE-S, Jahrami HA, Sherif NM, Hassan RE, Awadallah S, et al. Ramadan diurnal intermittent fasting modulates SOD2, TFAM, Nrf2, and sirtuins (SIRT1, SIRT3) gene expressions in subjects with overweight and obesity. Diabet Res Clin Pract. (2019) 155:107801. doi: 10.1016/j.diabres.2019.107801
53. Malekmakan L, Sayadi M, Pakfetrat M, Moosavi B, Mousavinezhad H. The effect of fasting on anthropometric parameters and blood pressure levels: a report from Southern Iran. Int Cardiovasc Res J. (2017) 11:143–7.
54. Khaled BM, Belbraouet S. Effect of Ramadan fasting on anthropometric parameters and food consumption in 276 type 2 diabetic obese women. Int J Diabetes Dev Ctries. (2009) 29:62–8. doi: 10.4103/0973-3930.53122
55. Namaghi MA, Eslami S, Nematy M, Khoshnasab A, Rezvani R, Philippou E, et al. Intermittent fasting during ramadan and its effects in individuals with metabolic syndrome. Br J Nutr. (2019) 54:159–64. doi: 10.1097/NT.0000000000000351
56. Nematy M, Alinezhad-Namaghi M, Rashed MM, Mozhdehifard M, Sajjadi SS, Akhlaghi S, et al. Effects of Ramadan fasting on cardiovascular risk factors: a prospective observational study. Nutr J. (2012) 11:69. doi: 10.1186/1475-2891-11-69
57. Norouzy A, Salehi M, Philippou E, Arabi H, Shiva F, Mehrnoosh S, et al. Effect of fasting in Ramadan on body composition and nutritional intake: a prospective study. J Hum Nutr Diet. (2013) 26(Suppl. 1):97–104. doi: 10.1111/jhn.12042
58. Norouzy A, Mohajeri SM, Shakeri S, Yari F, Sabery M, Philippou E, et al. Effect of Ramadan fasting on glycemic control in patients with Type 2 diabetes. J Endocrinol Invest. (2012) 35:766–71. doi: 10.3275/8015
59. Patel P, Mirakhur A, El-Magd KMA, El-Matty ANA, Al-Ghafri D. Type 2 diabetes and its characteristics during Ramadan in Dhahira Region, Oman. Oman Med J. (2007) 22:16–23.
60. Sahin SB, Ayaz T, Ozyurt N, Ilkkilic K, Kirvar A, Sezgin H. The impact of fasting during Ramadan on the glycemic control of patients with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. (2013) 121:531–4. doi: 10.1055/s-0033-1347247
61. Shariatpanahi ZV, Shariatpanahi MV, Shahbazi S, Hossaini A, Abadi A. Effect of Ramadan fasting on some indices of insulin resistance and components of the metabolic syndrome in healthy male adults. Br J Nutr. (2008) 100:147–51. doi: 10.1017/S000711450787231X
62. Shehab A, Abdulle A, El Issa A, Al Suwaidi J, Nagelkerke N. Favorable changes in lipid profile: the effects of fasting after Ramadan. PLoS ONE. (2012) 7:e47615. doi: 10.1371/journal.pone.0047615
63. Syam AF, Suryani Sobur C, Abdullah M, Makmun D. Ramadan fasting decreases body fat but not protein mass. Int J Endocrinol Metab. (2016) 14:e29687. doi: 10.5812/ijem.29687
64. Ghania T, Boumediene Meghit K, Mustapha D, Sarah S, Ghizlane B. Effect of Ramadan fasting on serum glucose and lipid profile among algerian type 2 diabetes patients. Romanian J Diabet Nutr Metab Dis. (2015) 22:385–92. doi: 10.1515/rjdnmd-2015-0045
65. Toony LFE, Hamad DA, Omar OM. Outcome of focused pre-Ramadan education on metabolic and glycaemic parameters in patients with type 2 diabetes mellitus. Diabetes Metab Syndr. (2018) 12:761–7. doi: 10.1016/j.dsx.2018.04.036
66. Yarahmadi S, Larijani B, Bastanhagh MH, Pajouhi M, Baradar Jalili R, Zahedi F, et al. Metabolic and clinical effects of Ramadan fasting in patients with type II diabetes. J Coll Physicians Surg Pak. (2003) 13:329–32.
67. Shariatpanahi MV, Shariatpanahi ZV, Shahbazi S, Moshtaqi M. Effect of fasting with two meals on BMI and inflammatory markers of metabolic syndrome. Pak J Biol Sci. (2012) 15:255–8. doi: 10.3923/pjbs.2012.255.258
68. Imtiaz S, Salman B, Dhrolia MF, Nasir K, Abbas HN, Ahmad A. Clinical and biochemical parameters of hemodialysis patients before and during islamic month of Ramadan. Iran J Kidney Dis. (2016) 10:75–8.
69. Laajam MA. Ramadan fasting and non-insulin-dependent diabetes: effect on metabolic control. East Afr Med J. (1990) 67:732–6.
70. Pathan M, Patil R. Effect of Ramadan fasting on body weight and lipid profile. Biomed Pharmacol J. (2010) 3. Available online at: http://biomedpharmajournal.org/?p=1278
71. Traoré M, Lemieux S, Galibois I. Metabolic and clinical profiles before, during and after Ramadan in Malians with type 2 diabetes. Nutrition Clinique et Metabolisme. (2014) 28:83–9. doi: 10.1016/j.nupar.2013.12.006
72. Abdullah K, Al-Habori M, Al-Eryani E. Ramadan intermittent fasting affects adipokines and leptin/adiponectin ratio in type 2 diabetes mellitus and their first-degree relatives. Biomed Res Int. (2020) 2020:1281792. doi: 10.1155/2020/1281792
73. Al-Rawi N, Madkour M, Jahrami H, Salahat D, Alhasan F, BaHammam A, et al. Effect of diurnal intermittent fasting during Ramadan on ghrelin, leptin, melatonin, and cortisol levels among overweight and obese subjects: a prospective observational study. PLoS ONE. (2020) 15:e0237922. doi: 10.1371/journal.pone.0237922
74. Das A, Hasmat N, Kumar Ghosh S, Sahu S. Effects of Ramadan intermittent fasting and pattern of nutrients intake on BMI and MUAC of a population consisting of Indian Muslims. Biol Rhythm Res. (2021) 52:1260–9. doi: 10.1080/09291016.2019.1700328
75. Farag HAM, Baqi HR, Qadir SA, El Bilbeisi AH, Hamafarj KK, Taleb M, et al. Effects of Ramadan fasting on anthropometric measures, blood pressure, and lipid profile among hypertensive patients in the Kurdistan region of Iraq. SAGE Open Med. (2020) 8. doi: 10.1177/2050312120965780
76. Gad AI, Abdel-Ghani HA, Barakat AAEA. Effect of Ramadan fasting on hepatic steatosis as quantified by controlled attenuation parameter (CAP): a prospective observational study. Egyptian Liver J. (2022) 12:22. doi: 10.1186/s43066-022-00187-y
77. Harbuwono DS, Sazli BI, Kurniawan F, Darmowidjojo B, Koesnoe S, Tahapary DL. The impact of Ramadan fasting on Fetuin-A level in type 2 diabetes mellitus. Heliyon. (2021) 7:e06773. doi: 10.1016/j.heliyon.2021.e06773
78. Ismail AAE, Megallaa MH, Badrah MH, Farghaly MAA. Study of the metabolic effects of ramadan fasting on patients with type 2 diabetes. Relation to glycemic control, hypoglycemic events and diabetic complications. Clin Diabetol. (2021) 10:161–8. doi: 10.5603/DK.a2020.0004
79. Jahrami H, BaHammam AS, Haji EA, Bragazzi NL, Rakha I, Alsabbagh A, et al. Ramadan fasting improves body composition without exacerbating depression in males with diagnosed major depressive disorders. Nutrients. (2021) 13:2718. doi: 10.3390/nu13082718
80. López-Bueno M, Fernández-Aparicio Á, González-Jiménez E, Montero-Alonso M, Schmidt-RioValle J. Self-care by muslim women during ramadan fasting to protect nutritional and cardiovascular health. Int J Environ Res Public Health. (2021) 18:12393. doi: 10.3390/ijerph182312393
81. Mohamed H, Abbas AM, Huneif MA, Alqahtani SM, Ahmed AM, Babker AMA, et al. Influence of ramadan fasting on hemoglobin a1c, lipid profile, and body mass index among type 2 diabetic patients in najran city, saudi arabia. Open Access Macedonian J Med Sci. (2021) 9:318–25. doi: 10.3889/oamjms.2021.6084
82. Mohammadzadeh A, Roshanravan N, Mesri Alamdari N, Safaiyan A, Mosharkesh E, Hadi A, et al. The interplay between fasting, gut microbiota, and lipid profile. Int J Clin Pract. (2021) 75:e14591. doi: 10.1111/ijcp.14591
83. Urooj A, Pai Kotebagilu N, Shivanna LM, Anandan S, Thantry AN, Siraj SF. Effect of ramadan fasting on body composition, biochemical profile, and antioxidant status in a sample of healthy individuals. Int J Endocrinol Metab. (2020) 18:e107641. doi: 10.5812/ijem.107641
84. Yazdanyar T, Sohrab M, Ramezani A, Aliabadi PK, Bahar A, Shirzad M, et al. The impact of fasting on metabolic and anthropometric parameters in type II diabetic patients: a prospective observational study. J Clin Diagnos Res. (2020) 14:OC18–23. doi: 10.7860/JCDR/2020/44868.14369
85. Poh B, Zawiah H, Ismail M, Henry C. Changes in body weight, dietary intake and activity pattern of adolescents during Ramadan. Malays J Nutr. (1996) 2:1–10.
86. Lessan N, Saadane I, Alkaf B, Hambly C, Buckley AJ, Finer N, et al. The effects of Ramadan fasting on activity and energy expenditure. Am J Clin Nutr. (2018) 107:54–61. doi: 10.1093/ajcn/nqx016
87. Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG, et al. Flipping the metabolic switch: understanding and applying the health benefits of fasting. Obesity. (2018) 26:254–68. doi: 10.1002/oby.22065
88. Moro T, Tinsley G, Bianco A, Marcolin G, Pacelli QF, Battaglia G, et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J Transl Med. (2016) 14:290. doi: 10.1186/s12967-016-1044-0
89. van Norren K, Rusli F, van Dijk M, Lute C, Nagel J, Dijk FJ, et al. Behavioural changes are a major contributing factor in the reduction of sarcopenia in caloric-restricted ageing mice. J Cachexia Sarcopenia Muscle. (2015) 6:253–68. doi: 10.1002/jcsm.12024
90. de Cabo R, Mattson MP. Effects of intermittent fasting on health, aging, and disease. N Engl J Med. (2019) 381:2541–51. doi: 10.1056/NEJMra1905136
91. Erdem NZ, Bayraktaroglu E, Samanci RA, Geçgil-Demir E, Tarakçi NG, Mert-Biberoglu F. The effect of intermittent fasting diets on body weight and composition. Clin Nutr ESPEN. (2022) 51:207–14. doi: 10.1016/j.clnesp.2022.08.030
92. Pichard C, Kyle UG, Gremion G, Gerbase M, Slosman DO. Body composition by x-ray absorptiometry and bioelectrical impedance in female runners. Med Sci Sports Exerc. (1997) 29:1527–34. doi: 10.1097/00005768-199711000-00021
93. Beestone C,. Bioelectrical Impedance Analysis (BIA). (2018). Available online at: https://www.scienceforsport.com/bioelectrical-impedance-analysis-bia/ (accessed December 9, 2020).
94. Statement NIoHTAC. Bioelectrical impedance analysis in body composition measurement. Am J Clin Nutr. (1996) 64:524s–32. doi: 10.1093/ajcn/64.3.524S
95. Sun SS, Chumlea WC, Heymsfield SB, Lukaski HC, Schoeller D, Friedl K, et al. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am J Clin Nutr. (2003) 77:331–40. doi: 10.1093/ajcn/77.2.331
96. Segal KR, Van Loan M, Fitzgerald PI, Hodgdon JA, Van Itallie TB. Lean body mass estimation by bioelectrical impedance analysis: a four-site cross-validation study. Am J Clin Nutr. (1988) 47:7–14. doi: 10.1093/ajcn/47.1.7
97. Lukaski HC. Methods for the assessment of human body composition: traditional and new. Am J Clin Nutr. (1987) 46:537–56. doi: 10.1093/ajcn/46.4.537
Keywords: anthropometry, weight, waist circumference, body mass index, fat, muscle mass, systematic review
Citation: Al-Jafar R, Wahyuni NS, Belhaj K, Ersi MH, Boroghani Z, Alreshidi A, Alkhalaf Z, Elliott P, Tsilidis KK and Dehghan A (2023) The impact of Ramadan intermittent fasting on anthropometric measurements and body composition: Evidence from LORANS study and a meta-analysis. Front. Nutr. 10:1082217. doi: 10.3389/fnut.2023.1082217
Received: 28 October 2022; Accepted: 02 January 2023;
Published: 17 January 2023.
Edited by:
MoezAlIslam Ezzat Faris, University of Sharjah, United Arab EmiratesReviewed by:
Mohd Adzim Khalili Rohin, Sultan Zainal Abidin University, MalaysiaZahra Vahdat Shariatpanahi, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2023 Al-Jafar, Wahyuni, Belhaj, Ersi, Boroghani, Alreshidi, Alkhalaf, Elliott, Tsilidis and Dehghan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rami Al-Jafar,  ci5hbC1qYWZhcjE4QGltcGVyaWFsLmFjLnVr
ci5hbC1qYWZhcjE4QGltcGVyaWFsLmFjLnVr
†ORCID: Rami Al-Jafar orcid.org/0000-0002-9393-7585
 Rami Al-Jafar
Rami Al-Jafar Nisa Sri Wahyuni1
Nisa Sri Wahyuni1 Mohammad Hamed Ersi
Mohammad Hamed Ersi Amer Alreshidi
Amer Alreshidi Konstantinos K. Tsilidis
Konstantinos K. Tsilidis