
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 16 March 2023
Sec. Clinical Nutrition
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1040893
This article is part of the Research Topic Body Composition Changes and Nutrition Therapy in Surgical Oncology Patients View all 14 articles
Introduction: The clinical utility of glutamine in patients undergoing colorectal cancer (CRC) surgery remains unclear. Therefore, we aimed to investigate the impact of postoperative treatment with glutamine on postoperative outcomes in patients undergoing CRC surgery.
Methods: We included patients with CRC undergoing elective surgery between January 2014 and January 2021. Patients were divided into the glutamine and control groups. We retrospectively analyzed postoperative infections complications within 30 days and other outcomes using propensity score matching and performed between-group comparisons.
Results: We included 1,004 patients who underwent CRC surgeries; among them, 660 received parenteral glutamine supplementation. After matching, there were 342 patients in each group. The overall incidence of postoperative complications was 14.9 and 36.8% in the glutamine and control groups, respectively, indicating that glutamine significantly reduced the incidence of postoperative complications [p < 0.001; risk ratio (RR) 0.41 [95% CI 0.30–0.54]]. Compared with the control group, the glutamine group had a significantly lower postoperative infection complications rate (10.5 vs. 28.9%; p < 0.001; RR 0.36 [95% CI 0.26–0.52]). Although there was no significant between-group difference in the time to first fluid diet (p = 0.052), the time to first defecation (p < 0.001), first exhaust (p < 0.001), and first solid diet (p < 0.001), as well as hospital stay (p < 0.001) were significantly shorter in the glutamine group than in the control group. Furthermore, glutamine supplementation significantly reduced the incidence of postoperative intestinal obstruction (p = 0.046). Moreover, glutamine supplementation alleviated the decrease in albumin (p < 0.001), total protein (p < 0.001), and prealbumin levels (p < 0.001).
Conclusions: Taken together, postoperative parenteral glutamine supplementation can effectively reduce the incidence of postoperative complications, promote the recovery of intestinal function, and improve albumin levels in patients undergoing CRC surgery.
Worldwide, colorectal cancer (CRC) is the third most common cancer and among the most common mortality causes due to gastrointestinal cancer. In 2021, there were more than 1,800,000 new cases of CRC worldwide (1). Changes in diet and lifestyle have contributed to the incidence of CRC (2). Surgery has become the main treatment for CRC (3). Although there has been a gradual reduction in postoperative complications with the progress of perioperative nursing and technology, the incidence of complications after CRC surgery remains as high as 35% (4). Mechanical bowel preparation before CRC surgery can disrupt intestinal barrier function; further, potential intraoperative bacterial contamination may increase the risk of postoperative infectious complications (5, 6). Postoperative complications prolong hospital stay, increase hospitalization costs, and negatively affect the long-term prognosis of patients (7, 8). A recent meta-analysis reported that postoperative complications increased the risk of recurrence and decreased overall survival among patients with non-metastatic CRC (9). Therefore, reducing postoperative complications is crucial for improving the prognosis of patients.
Recent studies have demonstrated that immunonutritional therapy can reduce postoperative complications by regulating immune function in patients with CRC (8). Glutamine, which is crucially involved in immunonutrition, can regulate inflammatory response and immune balance, maintain the intestinal mucosal barrier, reduce intestinal damage, and reduce intestinal microbiota translocation (5, 8, 10). Accordingly, glutamine may provide a potential strategy for preventing postoperative complications. Additionally, a few studies have demonstrated that glutamine supplementation can reduce the length of hospital stay (5, 11).
However, there remains insufficient evidence for supporting the routine perioperative use of glutamine in patients with CRC. A recent meta-analysis recommended large-scale studies to evaluate the effect of perioperative glutamine supplementation in patients undergoing CRC surgery (8). Accordingly, we used propensity score matching (PSM) to investigate the effect of postoperative glutamine supplementation on postoperative complications and recovery in patients undergoing CRC surgery.
This retrospective cohort study was conducted between January 2014 and January 2021. This study was ethically approved by the Institutional Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. All the patients provided informed consent.
We included patients who underwent elective surgery for primary CRC with and without glutamine supplementation (20% alanyl-glutamine 50–100 mL daily) for ≥5 days from the day of surgery. We excluded cases without primary anastomosis; cases with multiple primary cancers, a history of treatment for other abdominal or pelvic malignancy, or multi-visceral resections; patients with hepatic or renal failures; and emergency cases.
Standardized laparoscopic colorectal cancer and robotic surgery were adopted in our hospital, all of which were performed by four surgeons with an experience of more than 100 laparoscopic colorectal cancer operations. We collected information regarding baseline characteristics, intraoperative details, and postoperative recovery from the electronic medical record system. Tumor staging was determined based on American Joint Committee on Cancer, 8th edition (12). Serum prealbumin, total protein, and albumin levels on the day before surgery and 5 days after surgery were collected.
The primary endpoints were postoperative infection complications within 30 postoperative days, including anastomotic leakage, intra-abdominal infection (excluding anastomotic leakage), wound infection, pneumonia, and urinary infection. The secondary endpoints included serum total protein and albumin levels; time to first exhaust, defecation, fluid diet, and solid diet; rate of postoperative complications, rate of reoperation within 30 postoperative days, postoperative length of hospital stay, and mortality.
The sample size was calculated based on the primary endpoint. A previous study (5) reports that the incidence of infectious complications is 42%; accordingly, assuming an incidence rate of 11% in the glutamine group, ≥31 patients were expected to be required in each group to achieve 80% power with a two-tailed p value <0.05. Eligible participants were divided into the glutamine and control groups based on whether they received intravenous glutamine supplementation. Between-group comparisons of categorical and continuous variables were performed using the chi-square test and Mann–Whitney U test (Kolmogorov–Smirnov tests showed that the data in this study were non-normally distributed), respectively. Dichotomous variables were described using percentages, while continuous variables by median (interquartile range: 25–75 percentile). To reduce potential confounders resulting from between-group differences in baseline characteristics, we performed PSM analysis using patient demographics (male, age, BMI, tumor stage, and neoadjuvant therapy), comorbidities (chronic obstructive pulmonary disease, liver disorder, hypertension, diabetes mellitus, coronary artery disease, and American Society of Anesthesiologists Physical Status classification), malnutrition (preoperative prealbumin, preoperative total protein, and albumin), and surgical data (surgical approach, diverting stoma, duration of surgery, intraoperative blood loss, intraoperative transfusion, and conversion). Using the nearest neighbor matching algorithm, the matching ratio was 1:1. Calipers were set to 0.2 times the standard deviation of the logarithm of the estimated propensity score. All statistical analyses were performed using IBM SPSS version 26. Statistical significance was set at a two-sided p value <0.05.
We included 1,004 consecutive patients undergoing elective surgery for CRC (38.6%, female; median age, 62 years). There were 660 and 344 patients in the glutamine and control groups, respectively. Before matching, there were a significant between-group difference in neoadjuvant therapy, duration of surgery, intraoperative blood loss, and intraoperative transfusion, but not in patient demographics (male, age, BMI, and tumor stage), comorbidities (chronic obstructive pulmonary disease, liver disorder, hypertension, diabetes mellitus, coronary artery disease, and American Society of Anesthesiologists physical status classification), malnutrition (preoperative prealbumin, preoperative total protein, and preoperative albumin), and surgical data (surgical approach, diverting stoma, and conversion; Table 1). After PSM, there were no significant differences in all covariates between the glutamine (n = 342) and control (n = 342) groups (Table 1).
Before matching, the rate of postoperative complications was significantly lower in the glutamine group than in the control group [15.9 vs. 36.6%, respectively; p < 0.001; risk ratio (RR) 0.43 [95% CI 0.35–0.54]; Table 2]. After PSM, the overall incidence of postoperative complications in the glutamine and control groups was 14.9 and 36.8%, respectively (p < 0.001; RR 0.41 [95% CI 0.30–0.54]). The glutamine group had a significantly lower rate of postoperative infections than the control group (10.5 vs. 28.9%, respectively; p < 0.001; RR 0.36 [95% CI 0.26–0.52]). There was no significant between-group difference in the rate of wound infection (p = 0.105), urinary infection (p = 0.101), and bleeding at anastomotic site (p = 0.412); however, the glutamine group had a significantly lower rate of anastomotic leakage (p = 0.043), pulmonary tract infection (p = 0.007), and intraabdominal infection (p < 0.001) than the control group (Table 2).
Regarding postoperative intestinal function recovery, although there was no significant between-group difference in the time to first fluid diet (p = 0.052), the glutamine group showed a significantly shorter time to first exhaust (p < 0.001), first defecation (p < 0.001), and first solid diet (p < 0.001) than the control group. Additionally, glutamine supplementation significantly reduced the incidence of postoperative intestinal obstruction (p = 0.046). The median length of hospital stay was 8 and 9 days in the glutamine and control groups, respectively (p < 0.001). Moreover, the median hospitalization cost in the glutamine group (75871.5RMB) was comparable to that in the control group (84059.7RMB; p = 0.950). There was two death in the glutamine group and two deaths in the control group (Table 2).
The median postoperative total protein levels were 61 and 59 g/L in the glutamine and control groups, respectively (p < 0.001). Glutamine alleviated the decrease in perioperative albumin (p < 0.001) and prealbumin (p < 0.001) levels (Table 2). Details of Clavien-Dindo classification of postoperative complications are in Table 3.
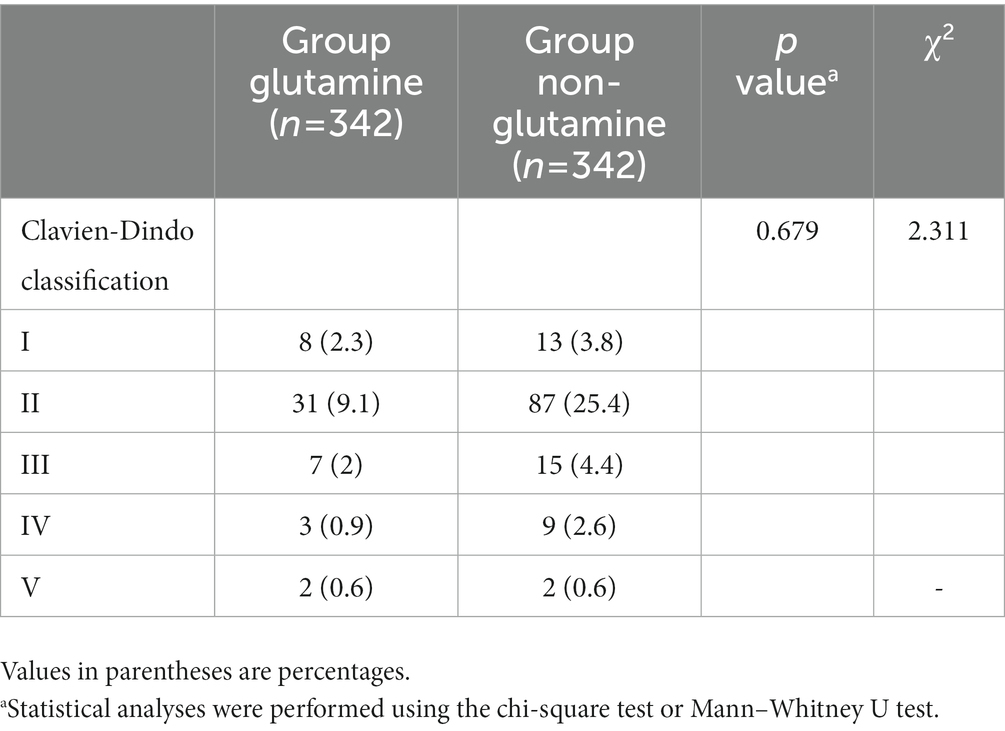
Table 3. Clavien-Dindo classification of postoperative complication after propensity score matching.
To our knowledge, this is the first large-scale study to explore the effects of glutamine on postoperative complications and recovery after CRC surgery. We found that glutamine supplementation could effectively reduce the incidence of postoperative complications; shorten the time to first exhaust, first defecation, and first solid diet; reduce the length of hospital stay; and improve serum prealbumin, total protein, and albumin levels. Postoperative complications negatively affect the short-term and long-term prognosis of patients with CRC. Colorectal surgery research has recently focused on the prevention of postoperative complications. Our findings provide current evidence regarding the prevention of postoperative complications and improvement of postoperative recovery in CRC surgery through glutamine supplementation.
Radical resection is the standard treatment for CRC (13). Immunonutrition therapy can effectively reduce the incidence and severity of postoperative complications in patients undergoing radical surgery for CRC (8). Glutamine is the preferred fuel for intestinal mucosal cells and immune cells; accordingly, it is crucially involved in regulating the body’s immune function and maintaining the integrity of the intestinal mucosal barrier (8, 14). Surgical trauma reduces plasma and intracellular glutamine pool levels, which impairs the normal immune function of T cells, the bactericidal function of neutrophils, the phagocytic activity of macrophages, and interleukin-1 production (15–17). The depletion of stored glutamine may cause postoperative complications, including infectious complications, abnormal immune function, increased intestinal permeability, poor wound healing, and even multiple organ failure (5). Low serum glutamine levels are associated with shortened survival of patients with CRC (18). Therefore, glutamine supplementation may be crucial for preventing postoperative complications. In our study, glutamine supplementation effectively reduced the incidence of postoperative complications. Several studies have demonstrated that glutamine supplementation can reduce postoperative complications. O’Riordain et al. (17) found that glutamine supplementation enhanced postoperative T lymphocyte immune function in patients undergoing colorectal surgery. In a study conducted by Cui et al. (11), patients with colon cancer received 0.5 g/kg glutamine 24 h before and 1 h after surgery and found that glutamine supplementation reduced the incidence of postoperative complications. Similarly, Oguz et al. reported that intravenous glutamine supplementation reduced postoperative complications (5). Additionally, the incidence of anastomotic leakage is as high as 3–20% and is related to increased postoperative morbidity, mortality, permanent stoma rate, and recurrence rate (13, 19–21). Accordingly, we focused on the important complication of an anastomotic leak. We found that glutamine supplementation effectively reduced the incidence of anastomotic leaks. Consistent with this finding, Yang et al. reported a significantly lower incidence of anastomotic leak in the glutamine group than in the control group (RR = 0.23, 95% CI: 0.09–0.61) (8). This could be attributed to several factors. On the one hand, glutamine can increase collagen synthesis, and thus accelerate intestinal mucosal healing and regeneration (13, 22). On the other hand, inflammation severity is among the important factors affecting the healing of intestinal anastomosis. Accordingly, glutamine can reduce inflammatory injury and oxidative stress as well as protect the healing of anastomosis (13).
In addition to reducing postoperative complications, glutamine may also promote postoperative recovery of gastrointestinal function. Glutamine can prevent intestinal mucosal atrophy and protect the intestinal mucosal barrier (17). Glutamine supplementation has been shown to prevent chemotherapy-induced diarrhea (23). Using animal experiments with dogs, Ohno et al. reported that glutamine improved intestinal obstruction after abdominal surgery (24). Additionally, Ohno et al. (25) reported that glutamine supplementation improved the decrease in plasma glutamine levels and gastrointestinal motility after gastrectomy. Our findings demonstrated that glutamine supplementation promoted intestinal function recovery, including shortening the time to first exhaust, first defecation, and first solid diet as well as reducing the incidence of postoperative ileus. Additionally, we found that glutamine reduced postoperative hospital stay, which is consistent with previous reports (5, 11, 26) and could be attributed to decreased complications and improved recovery of intestinal function. This in turn could have contributed to reduced hospitalization costs. Thus we observed that additional glutamine supplementation did not increase total hospitalization costs.
Hypoproteinemia is related to increased postoperative morbidity and prolonged hospital stay (27, 28). Major gastrointestinal surgery is often accompanied by a high inflammatory response, which impairs liver protein metabolism. Glutamine can increase hepatocyte synthesis and improve hepatic metabolism (29). Wu et al. reported that glutamine supplementation increased serum albumin levels in patients with gastric cancer undergoing radical surgery (29), which is consistent with our findings. However, while the differences in these indicators (total protein levels, albumin levels, and prealbumin levels) were statistically significant, whether these differences are of significant clinical value remains to be determined.
Our study has two strengths. On the one hand, it is the study with the largest sample size to examine the effects of glutamine on patients undergoing colorectal cancer surgery. On the other hand, we used PSM to balance potential confounding factors between the groups.
This study has several limitations. First, this was a single-center retrospective study and there may be potential confounding factors. Second, we retrospectively collected information regarding the time to first exhaust, defecation, fluid diet, and first solid diet from the electronic medical records, which could lead to potential bias. Prospective studies are warranted to confirm the benefits of glutamine supplementation on the recovery of bowel function after surgery for CRC. Then, we did not measure plasma glutamine levels before and after the intervention. Future studies should consider plasma glutamine levels. Finally, as the current guidelines do not clarify whether or not to supplement glutamine in patients undergoing colorectal cancer surgery, in this study, this decision was not based on clear criteria. This could have led to some selection bias. Given these limitations, prospective randomized controlled studies are needed to validate the benefit of glutamine supplements in patients undergoing colorectal cancer surgery.
In conclusion, we found that postoperative intravenous glutamine supplementation could effectively reduce the incidence of postoperative complications, promote the recovery of intestinal function, and improve albumin levels in patients undergoing CRC surgery.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. The patients/participants provided their written informed consent to participate in this study.
Z-QW, FP, and GT: conceptualization. FP, GT, and Y-HQ: data collection and analyses. GT and FP: writing—original draft preparation. Z-QW, FP, GT, and Y-HQ: writing—review and editing and had primary responsibility for the final content. All authors contributed to the article and approved the submitted version.
This study was funded by Chongqing Key Diseases Research and Application Demonstration Program, No. 2019ZX003.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. El Zoghbi, M, and Cummings, LC. New era of colorectal cancer screening. World J Gastrointest Endoscopy. (2016) 8:252–8. doi: 10.4253/wjge.v8.i5.252
3. Tang, G, and Zhang, L. Update on strategies of probiotics for the prevention and treatment of colorectal cancer. Nutr Cancer. (2022) 74:27–38. doi: 10.1080/01635581.2020.1865420
4. Pallan, A, Dedelaite, M, Mirajkar, N, Newman, PA, Plowright, J, and Ashraf, S. Postoperative complications of colorectal cancer. Clin Radiol. (2021) 76:896–907. doi: 10.1016/j.crad.2021.06.002
5. Oguz, M, Kerem, M, Bedirli, A, Mentes, BB, Sakrak, O, Salman, B, et al. L-alanin-L-glutamine supplementation improves the outcome after colorectal surgery for cancer. Colorect Dis. (2007) 9:515–20. doi: 10.1111/j.1463-1318.2006.01174.x
6. Foitzik, T, Kruschewski, M, Kroesen, AJ, Hotz, HG, Eibl, G, and Buhr, HJ. Does glutamine reduce bacterial translocation? A study in two animal models with impaired gut barrier. Int J Color Dis. (1999) 14:143–9. doi: 10.1007/s003840050200
7. Slankamenac, K, Slankamenac, M, Schlegel, A, Nocito, A, Rickenbacher, A, Clavien, PA, et al. Impact of postoperative complications on readmission and long-term survival in patients following surgery for colorectal cancer. Int J Color Dis. (2017) 32:805–11. doi: 10.1007/s00384-017-2811-y
8. Yang, T, Yan, X, Cao, Y, Bao, T, Li, G, Gu, S, et al. Meta-analysis of glutamine on immune function and post-operative complications of patients with colorectal cancer. Front Nutr. (2021) 8:765809. doi: 10.3389/fnut.2021.765809
9. Mualla, NM, Hussain, MR, Akrmah, M, Malik, P, Bashir, S, and Lin, JJ. The impact of postoperative complications on long-term oncological outcomes following curative resection of colorectal cancer (stage I-III): a systematic review and meta-analysis. Cureus. (2021) 13:e12837. doi: 10.7759/cureus.12837
10. Gianotti, L, Braga, M, Biffi, R, Bozzetti, F, and Mariani, L. Perioperative intravenous glutamine supplemetation in major abdominal surgery for cancer: a randomized multicenter trial. Ann Surg. (2009) 250:684–90. doi: 10.1097/SLA.0b013e3181bcb28d
11. Cui, Y, Hu, L, Liu, YJ, Wu, YM, and Jing, L. Intravenous alanyl-L-glutamine balances glucose-insulin homeostasis and facilitates recovery in patients undergoing colonic resection: a randomised controlled trial. Eur J Anaesthesiol. (2014) 31:212–8. doi: 10.1097/EJA.0b013e328360c6b9
12. Weiser, MR. AJCC 8th edition: colorectal cancer. Ann Surg Oncol. (2018) 25:1454–5. doi: 10.1245/s10434-018-6462-1
13. Habibi, M, Oner, OZ, Oruc, MT, Bulbuller, N, Ozdem, S, Ozdemir, S, et al. Effects of a glutamine enema on anastomotic healing in an animal colon anastomosis model. Ann Coloproctol. (2015) 31:213–21. doi: 10.3393/ac.2015.31.6.213
14. Plauth, M, Raible, A, Vieillard-Baron, D, Bauder-Gross, D, and Hartmann, F. Is glutamine essential for the maintenance of intestinal function? A study in the isolated perfused rat small intestine. Int J Color Dis. (1999) 14:86–94. doi: 10.1007/s003840050191
15. Hong, RW, Rounds, JD, Helton, WS, Robinson, MK, and Wilmore, DW. Glutamine preserves liver glutathione after lethal hepatic injury. Ann Surg. (1992) 215:114–9. doi: 10.1097/00000658-199202000-00004
16. Ogle, CK, Ogle, JD, Mao, JX, Simon, J, Noel, JG, Li, BG, et al. Effect of glutamine on phagocytosis and bacterial killing by normal and pediatric burn patient neutrophils. JPEN J Parenter Enteral Nutr. (1994) 18:128–33. doi: 10.1177/0148607194018002128
17. O’Riordain, MG, Fearon, KC, Ross, JA, Rogers, P, Falconer, JS, Bartolo, DC, et al. Glutamine-supplemented total parenteral nutrition enhances T-lymphocyte response in surgical patients undergoing colorectal resection. Ann Surg. (1994) 220:212–21. doi: 10.1097/00000658-199408000-00014
18. Ling, HH, Pan, YP, Fan, CW, Tseng, WK, Huang, JS, Wu, TH, et al. Clinical significance of serum glutamine level in patients with colorectal cancer. Nutrients. (2019) 11:898. doi: 10.3390/nu11040898
19. Tang, G, Du, D, Tao, J, and Wei, Z. Effect of Indocyanine green fluorescence angiography on anastomotic leakage in patients undergoing colorectal surgery: a meta-analysis of randomized controlled trials and propensity-score-matched studies. Front Surg. (2022) 9:815753. doi: 10.3389/fsurg.2022.815753
20. Yang, J, Chen, Q, Jindou, L, and Cheng, Y. The influence of anastomotic leakage for rectal cancer oncologic outcome: a systematic review and meta-analysis. J Surg Oncol. (2020) 121:1283–97. doi: 10.1002/jso.25921
21. Ha, GW, Kim, JH, and Lee, MR. Oncologic impact of anastomotic leakage following colorectal cancer surgery: a systematic review and meta-analysis. Ann Surg Oncol. (2017) 24:3289–99. doi: 10.1245/s10434-017-5881-8
22. Gökpinar, I, Gürleyik, E, Pehlivan, M, Ozcan, O, Ozaydin, I, Aslaner, A, et al. [early enteral and glutamine enriched enteral feeding ameliorates healing of colonic anastomosis: experimental study]. Ulusal travma ve acil cerrahi dergisi. Turk J Trauma Emerg Surg. (2006) 12:17–21.
23. Thomsen, M, and Vitetta, L. Adjunctive treatments for the prevention of chemotherapy- and radiotherapy-induced mucositis. Integr Cancer Ther. (2018) 17:1027–47. doi: 10.1177/1534735418794885
24. Ohno, T, Mochiki, E, Ando, H, Fukasawa, T, Toyomasu, Y, Ogata, K, et al. Glutamine decreases the duration of postoperative ileus after abdominal surgery: an experimental study of conscious dogs. Dig Dis Sci. (2009) 54:1208–13. doi: 10.1007/s10620-008-0478-5
25. Mochiki, E, Ohno, T, Yanai, M, Toyomasu, Y, Andoh, H, and Kuwano, H. Effects of glutamine on gastrointestinal motor activity in patients following gastric surgery. World J Surg. (2011) 35:805–10. doi: 10.1007/s00268-011-0962-5
26. Powell-Tuck, J. Total parenteral nutrition with glutamine dipeptide shortened hospital stays and improved immune status and nitrogen economy after major abdominal surgery. Gut. (1999) 44:155. doi: 10.1136/gut.44.2.155
27. Lohsiriwat, V, Chinswangwatanakul, V, Lohsiriwat, S, Akaraviputh, T, Boonnuch, W, Methasade, A, et al. Hypoalbuminemia is a predictor of delayed postoperative bowel function and poor surgical outcomes in right-sided colon cancer patients. Asia Pac J Clin Nutr. (2007) 16:213–7.
28. Haskins, IN, Baginsky, M, Amdur, RL, and Agarwal, S. Preoperative hypoalbuminemia is associated with worse outcomes in colon cancer patients. Clin Nutr. (2017) 36:1333–8. doi: 10.1016/j.clnu.2016.08.023
Keywords: glutamine, colorectal cancer, postoperative complications, intestinal function, albumin, propensity score
Citation: Tang G, Pi F, Qiu Y-H and Wei Z-Q (2023) Postoperative parenteral glutamine supplementation improves the short-term outcomes in patients undergoing colorectal cancer surgery: A propensity score matching study. Front. Nutr. 10:1040893. doi: 10.3389/fnut.2023.1040893
Received: 09 September 2022; Accepted: 06 March 2023;
Published: 16 March 2023.
Edited by:
Shanjun Tan, Fudan University, ChinaReviewed by:
Nazila Farrin, Tabriz University of Medical Sciences, IranCopyright © 2023 Tang, Pi, Qiu and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng-Qiang Wei, MTk4MDkwMDU0N0BxcS5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.