- 1MRC Lifecourse Epidemiology Centre, University of Southampton, Southampton, United Kingdom
- 2NIHR Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom
- 3Living Well Partnership, Southampton, United Kingdom
- 4Medicine for Older People, University Hospital Southampton, Southampton, United Kingdom
Introduction: Adequate nutrition is important for health in later life. Older adults are especially vulnerable to adverse outcomes following infection by COVID-19 and have commonly spent a disproportionate time within their own homes to reduce risk of infection. There are concerns that advice to shield may have led to malnutrition as older adults may modify daily routines including usual shopping habits. The aims of this study were to report self-reported pandemic-related changes in diet and examine lifestyle and medical correlates of these changes in older UK community-dwelling adults.
Methods: We recruited 491 participants from the city of Southampton, UK. Participants completed a postal questionnaire in summer/autumn 2021, over a year after the first UK national lockdown was announced. The questionnaire ascertained demographic and lifestyle factors, in addition to number of comorbidities, nutrition risk scores, and presence of frailty. Associations between these participant characteristics in relation to self-reported changes in diet quality (lower, similar or higher when compared to before the first lockdown) were examined using ordinal logistic regression.
Results: Median (lower quartile, upper quartile) age was 79.8 (77.0, 83.7) years. Overall, 11 (4.9%) men and 25 (9.4%) women had poorer diet quality compared to before the first UK lockdown. The following participant characteristics were associated with increased risk of being in a worse category for change in diet quality after adjustment for sex: lower educational attainment (p = 0.009); higher BMI (p < 0.001); higher DETERMINE (a malnutrition assessment) score (p = 0.004); higher SARC-F score (p = 0.013); and self-reported exhaustion in the previous week on at least 3 days (p = 0.002).
Conclusions: Individuals at higher nutritional risk were identified as reporting increased risk of deterioration in diet quality during the pandemic. Further investigation of the factors leading to these changes, and an understanding of whether they are reversible will be important, especially for future pandemic management.
1. Introduction
Frailty is a common condition in late adulthood and is associated with very significant mortality and morbidity (1). Frailty is defined as an increased vulnerability to stressors across multiple bodily systems and sarcopenia is considered to be one of the key pathologies underpinning the frailty syndrome (1). Adequate nutrition is known to be associated with better musculoskeletal health in later life (1, 2). More specifically, sufficient intake of calcium, protein and other vitamins and minerals have been linked to better muscle health (3). Several epidemiological studies have explored the association of dietary habits or healthier diets with muscle health, and the association of individual foods and nutrients with fracture, falls and frailty (4–7).
The emergence of the coronavirus disease (COVID-19), declared a pandemic by the World Health Organization in March 2020, and subsequent restrictive measures introduced in many countries to reduce the transmission of the disease, may have negatively impacted daily routines and lifestyle. This is especially likely among older adults, who are at greatest risk of complications from infection by the COVID-19 virus (8, 9). Potential factors associated with changes in diet quality remain controversial.
We hypothesized that the COVID-19 pandemic may have a differential impact on diet of older adults in the UK dependent on other sociodemographic and medical factors. We therefore aimed to report pandemic-related changes in diet and examine correlates of changes in diet quality in a newly established community-dwelling older adult cohort in the UK, to consider who might be at greatest risk of malnutrition.
2. Methods
2.1. Southampton longitudinal study of ageing (SaLSA)
In July 2021, we identified all patients who were registered at a large General Practice within Southampton, UK over the age of 75 (10). Eligibility to participate in the study was decided by their primary care physician. All participants were >75 years of age at the time of recruitment. We did not approach patients who their primary care physician reported as having any of the following problems; safeguarding issues, patients with mental health and capacity issues, patients with dementia or who were unable to provide consent, patients with learning disabilities, patients who were end of life, patients who were permanently bed bound, and patients in residential or nursing homes. Of 2,523 registered patients over the age of 75 years at the practice, 1993 (79%) were eligible to participate in the study based on the criteria above and 516 complete questionnaires were received. This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Research Ethics Committee (REC) Health Regulator Authority (HRA) (REC reference 21/SC/0036, 17 March 2021).
2.2. Ascertainment of participant characteristics
All participant information was self-reported using postal questionnaires. Sociodemographic factors included: age; sex; ethnicity; educational qualifications achieved; living arrangements; and current marital status. Participants were asked to indicate if they had any of the following qualifications: O Levels/GCSEs; A Levels; vocational training certificates; university degree(s) or Higher National Diploma; or higher professional qualifications. Participants were asked to select one of the following options for their living arrangement: their own property; rented accommodation; residential home; nursing home; or “other.” Self-reported height and weight were used to derive BMI (kg/m2). Information on health behaviors such as smoking, alcohol consumption, and information on malnutrition risk using the DETERMINE tool (11) were also ascertained. In brief, DETERMINE is a tool designed by the American Academy of Family Physicians, the National Council on the Aging and others as part of the Nutrition Screening Initiative which can be used by professionals working with older people to assess their risk for poor nutritional status or malnutrition. Change in the following aspects of lifestyle compared to before the first UK lockdown (23/03/2020) were reported: smoking, alcohol consumption, diet quality (reported as “healthiness of diet”), amount of food consumed, physical activity, sleep, and social contact. The questions used were taken from the Wellcome COVID questionnaire, which was designed to enable researchers to collect COVID related data using the same validated questions used or adopted by other cohorts (accessed at https://www.bristol.ac.uk/alspac/researchers/wellcome-covid-19/) (12). For example, to ascertain change in diet quality, participants were asked to select one of the following options to describe the current healthiness of their diet compared to before the first UK lockdown: “less healthy than before”; “about the same healthiness as before”; or “more healthy than before.”
Comorbidities were ascertained by asking participants whether they were ever diagnosed by a doctor with any of the following conditions: heart attack or angina; stroke or transient ischaemic attack; hypertension; diabetes; asthma, bronchitis, emphysema, or chronic obstructive pulmonary disease (COPD); depression; osteoporosis; anxiety; memory problems or dementia; Parkinson's disease; osteoarthritis or degenerative joint disease; rheumatoid/inflammatory arthritis; cancer; or high cholesterol. The resulting number of comorbidities reported was used as a marker of morbidity. The Strength, Ambulation, Rising from a chair, Stair climbing and history of Falling (SARC-F) screening tool for sarcopenia (13) and the following Fried frailty questions were also included (14): “In the last year, have you lost more than 10 pounds unintentionally?” and “How often in the last week did the following apply?” “I felt that everything I did was an effort” or “I could not get going”.
2.3. Statistical methods
Summary statistics were used to describe baseline participant characteristics and changes in the following aspects of lifestyle compared to before the first UK lockdown: smoking, alcohol consumption, diet quality, amount of food consumed, physical activity, sleep and social contact. Sex-adjusted ordinal logistic regression was used to examine risk of being in a worse category for change in diet quality (compared to before the first UK lockdown) according to various participant characteristics; sex-interaction effects were not statistically significant. The outcome, change in diet quality, was coded as follows: 1: higher than before; 2: about the same as before; 3: lower than before. Therefore, examples of a worse category for change in diet quality would be “lower than before” as opposed to “about the same” or “about the same” as opposed to “higher than before.” Participant characteristics considered as exposures included: sociodemographic factors, BMI, current health behaviors, number of comorbidities, SARC-F score, and Fried frailty components (unintentional weight loss and self-reported exhaustion). Cross-tabulations of pandemic-related changes in diet quality and physical activity were examined using chi-squared tests and Fisher's exact tests, as appropriate.
All analyses were conducted using Stata (StataCorp, College Station, TX, USA), release 17.0; p < 0.05 was regarded as statistically significant. The analysis sample comprised the 491 participants who had data on self-reported change in diet quality since before the first UK lockdown.
3. Results
3.1. Descriptive statistics
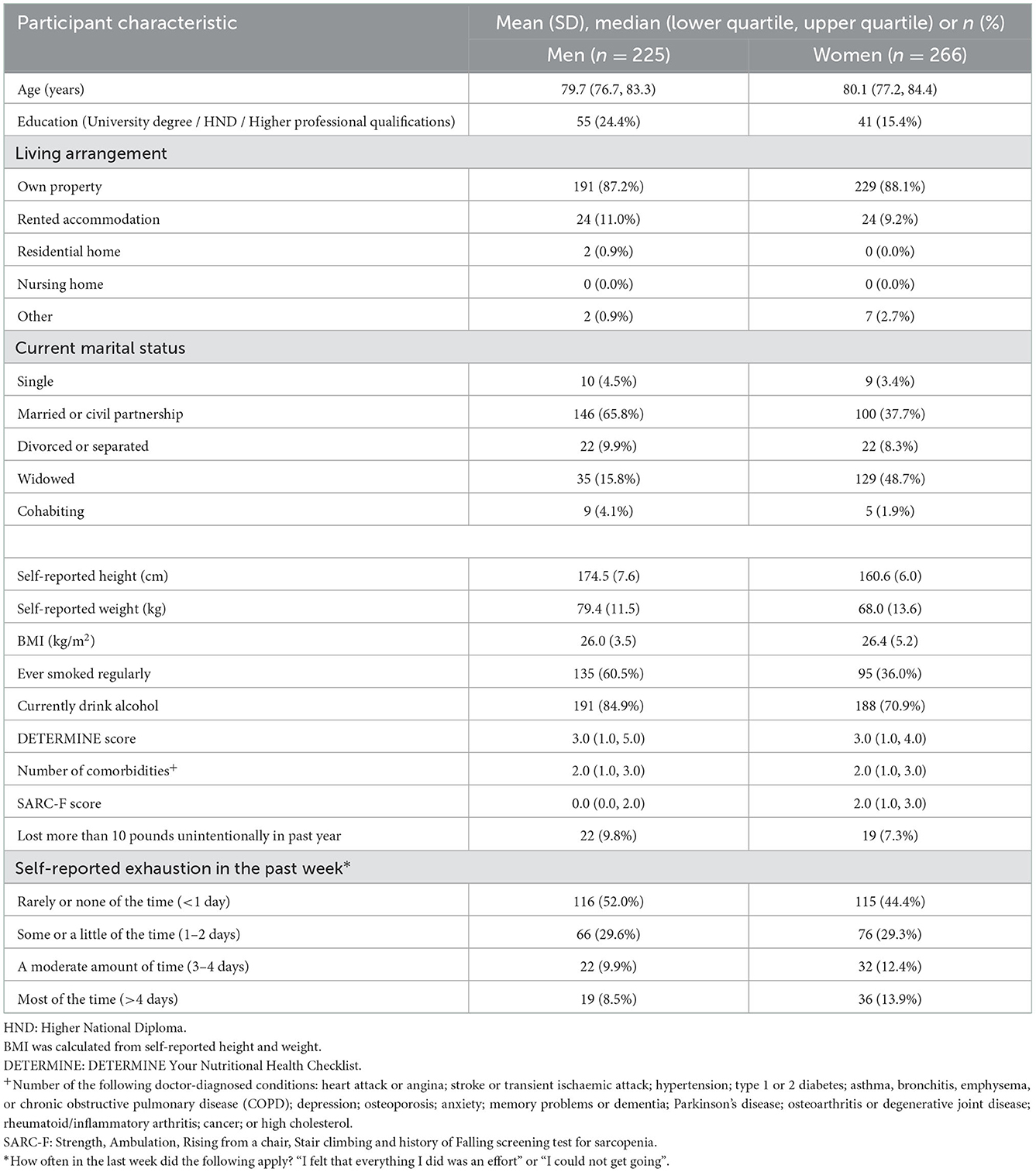
The participant characteristics of the analysis sample at baseline are presented in Table 1. Median (lower quartile, upper quartile) age was 79.8 (77.0, 83.7) years; 482 (99.0%) were of white ethnicity; 420 (87.7%) lived in their own property; and 260 (53.4%) were in a current relationship (married/civil partnership/cohabiting).
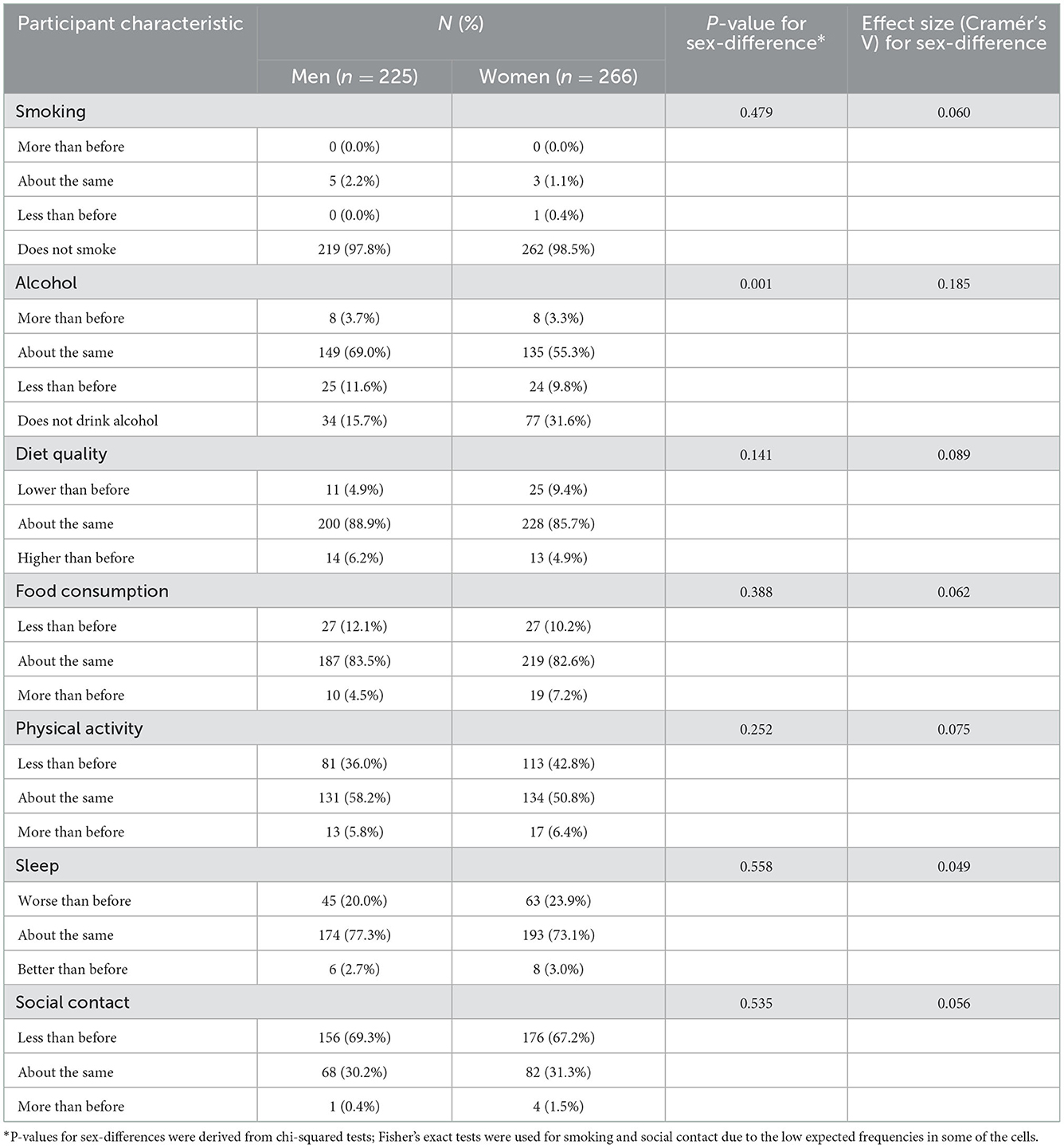
Changes in lifestyle compared to before the first UK lockdown are presented in Table 2. A greater proportion of participants consumed less alcohol than before (11.6% men, 9.8% women) compared to those that consumed more than before (3.7% men, 3.3% women); over 99% of men and women did not smoke or reported no change in their smoking behavior. Most participants reported no change in diet quality (88.9% men, 85.7% women) with smaller numbers reporting declines in diet quality (4.9% men, 9.4% women) and increases in diet quality (6.2% men, 4.9% women); a similar pattern was observed for amount of food consumed. Considerably more participants reported declines in physical activity, sleep quality and social contact in comparison to the number who reported increases. For example, 36.0% of men and 42.8% of women reported declines in physical activity whereas only 5.8% of men and 6.4% of women reported increases. Statistically significant sex-differences in these lifestyle changes were only observed for alcohol consumption (p = 0.001).
3.2. Predictors of change in diet quality compared to before the first UK lockdown
Cross-sectional associations between participant characteristics and risk of being in a worse category for change in diet quality (compared to before the first UK lockdown) are presented in Table 3. The following participant characteristics were associated with increased risk of being in a worse category for change in diet quality after adjustment for sex: lower educational attainment (p = 0.009); higher BMI (p < 0.001); higher nutrition risk score (p = 0.004); higher SARC-F score (p = 0.013); and self-reported exhaustion in the previous week on at least 3 days (p = 0.002). For example, after adjustment for sex, the odds ratio (95% CI) for being in a worse category for change in diet quality was 1.13 (1.06, 1.19) per unit increase in BMI and 2.76 (1.47, 5.18) for those who reported exhaustion in the previous week on at least 3 days compared to those who did not.
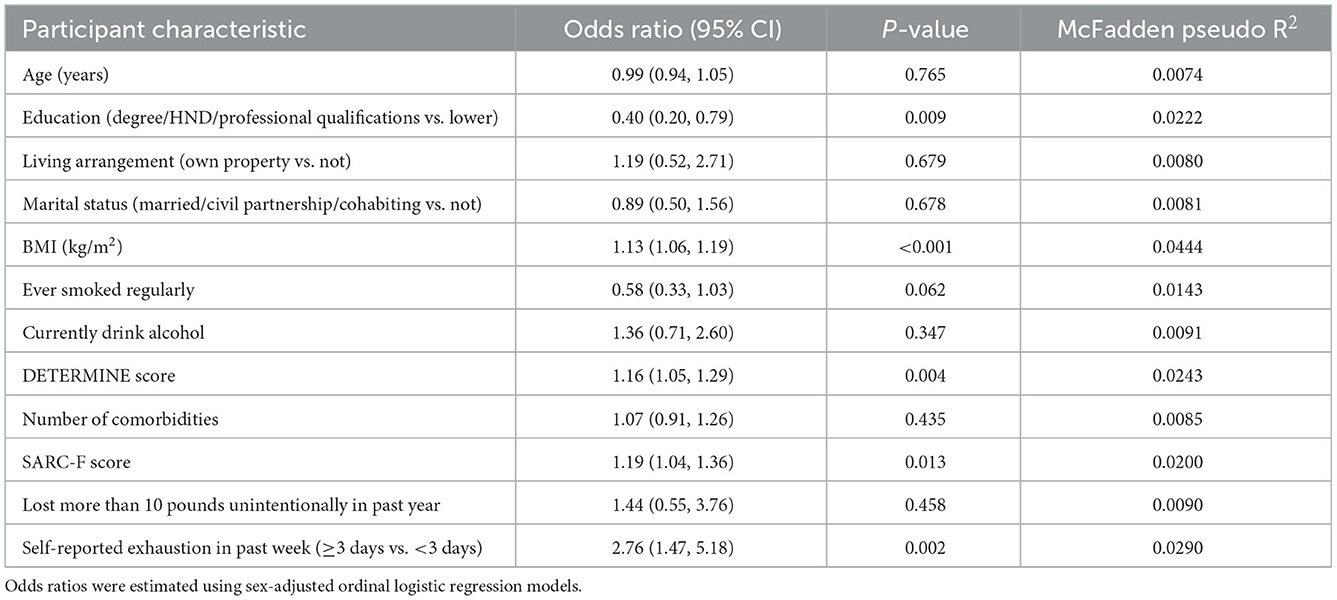
Table 3. Sex-adjusted odds ratios for being in a worse category for change in diet quality compared to before the first UK lockdown according to participant characteristics.
3.3. Association between change in diet quality and change in physical activity
Changes in diet quality and physical activity compared to before the first UK lockdown were correlated among men (p = 0.002) and women (p = 0.007). For example, among men who did not report declines in physical activity, only 1.4% reported declines in diet quality, compared to 11.1% among those who did report declines in physical activity; corresponding figures among women were 5.3% and 15.0%, respectively (Table 4).
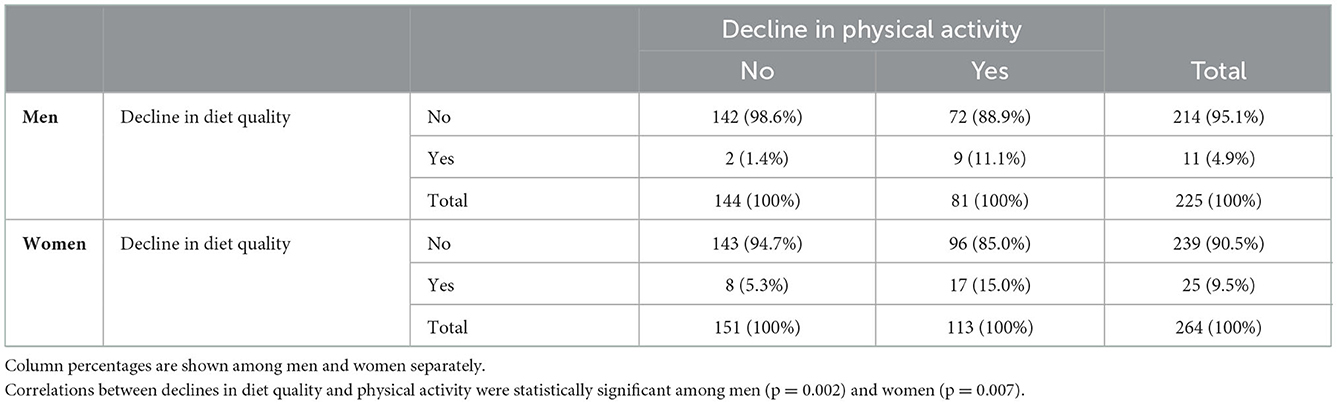
Table 4. Cross tabulations of declines in diet quality and physical activity since before the first UK lockdown among men and women.
4. Discussion
This study has described changes in lifestyle factors and examined correlates of change in diet quality compared to before the first UK national lockdown in March 2020. Although self-reported changes in alcohol consumption and smoking were minimal, considerably more participants reported declines in physical activity, sleep quality and social contact in comparison to those who reported increases. Most participants reported no change in diet quality with small proportions reporting declines or increases in diet quality. However, the following were associated with increased risk of being in a worse category for change in diet quality after adjustment for sex: lower educational attainment; higher BMI; higher DETERMINE score; higher SARC-F score; and self-reported exhaustion. This suggests that there is a small subset of older community-dwelling adults whose diet deteriorated over the first year of the COVID-19 pandemic. Worryingly, this included individuals with a higher DETERMINE score, a score used by health professionals to identify older adults at risk of malnutrition and/or higher SARC-F score, where a cut-off of 4 or higher is suggestive of sarcopenia and poor outcomes.
Our results are in accord with previous work where in a study of Dutch adults, younger generations were more likely, when compared to older generations, to be influenced by COVID-19 lockdowns and to change their eating behaviors (15). This observation was also supported by a recent systematic review looking into the impact of the COVID-19 pandemic on diet where 6 out of 10 studies examined observed no significant changes in dietary habits of older adults (16). However, the included studies were heterogenous in findings, and did not consider correlates of dietary decline or associated health outcomes. For example, in 2 studies, no more than 50% of participants were found not to have altered their dietary habits (17, 18).
In other work, older participants tended to be less likely to report changes in food behaviors, overall diet healthfulness, and food security compared to younger participants in the International Food Policy Study conducted across 5 countries (19). Other researchers have reported that age was negatively associated with healthy dietary change (20, 21) and increased intake of junk food (22). Constant et al. found that individuals aged 40–60 and 60+ years were around 20% less likely to have made a “positive” lifestyle change in eating habits during the lockdown period in France (23). Similar findings were reported in a recent study by Bevilacqua et al. of participants from two UK cohorts of community-dwelling older adults: during the first months of the pandemic, individuals from the younger cohort (median age 65 years) reported more negative changes to their diets when compared to those from the older cohort (median age 84 years) (24). In addition, Bevilacqua et al. reported that younger women were more likely to have increased their food intake and reduced the quality of their diet compared to men (24), a tendency that we also notice in our sample population, with more women than men reporting both a decrease in diet quality (9.4% vs. 4.9%) and an increase in food intake (7.2% vs. 4.5%); however, in our study this difference was not statistically significant. Quarantine due to the COVID-19 pandemic had a negative impact on physical and mental health as well as on lifestyle in older adults from five Central American countries; a greater effect was reported on having a balanced diet, frequency of falls, and functional ability amongst others (25). Luo et al. also report that older individuals were more likely to change dietary habits during the pandemic (26).
Differences in socioeconomic status and food availability, especially during the early phases of the pandemic, may account for some of the differences observed between studies. Energy-dense foods with high sugar and fat may be cheaper and more palatable, with access different in different groups of adults in different countries (27). Lower educational attainment was associated with an increased risk of being in a worse category for change in diet quality in our cohort. Participants with higher adherence to a Mediterranean diet during the COVID-19 pandemic were more likely to have a higher education level in a study in Spain; education level was related to following a Mediterranean diet while advised to stay at home during early pandemic restrictions (28). Higher educational level has been commonly associated with higher socioeconomic status which is often related to better diet quality (27). Finally higher education levels predict an increase in healthier dietary patterns in non-COVID related studies (29).
While dietary change during the pandemic has been studied by other researchers (29, 30), far fewer have considered much older adults. The dietary habits of older people living with frailty may have been more strongly affected by social isolation during the COVID-19 pandemic than those who were not frail as reported in one study. In addition, reduced food shopping times during social isolation was significantly higher among frail individuals while frail older adults consumed less high-quality proteins but more protein rich foods and vegetables which might indicate an attempt to improve dietary habits (30). These observations accord with our work where self-reported exhaustion, one of the elements of the Fried Frailty criteria, was associated with an increased risk of being in a worse category for change in diet quality. It is of course possible that the deterioration reported by some older adults was unrelated to the COVID-19 pandemic. While this is possible, recent qualitative work in another older UK cohort would suggest that although causality cannot be established, the pandemic has impacted the way older adults access shops (31).
This study has some limitations. First, all information was ascertained through self-reported questionnaires. Second, recall bias may have occurred as participants reported changes in lifestyle factors since the UK national lockdown instead of reporting current lifestyle behaviors at two separate time points before and after the lockdown. Third, investigating the impact of having COVID-19 or experiencing COVID-19 related symptoms on changes in lifestyle factors was not possible as only a very small proportion of participants had a confirmed COVID-19 infection. Furthermore, detailed dietary data were not available. In our study, 1,993 patients were invited to participate in the study by postal invitation which led to the return of 516 complete questionnaires (26% response rate). However, a previous study which tested the feasibility of setting up a UK sarcopenia registry only achieved a 12% response rate when potential participants aged 65 and over were approached via mailshots from local primary care practices (32). This suggests that our response rate was not unusually low, given that we were contacting participants from the general population. Fourth, participants completed questionnaires from July 2021 until April 2022; the COVID-19 UK Government guidelines and restrictions changed during this time so the reference point for comparing their lifestyles from before the first UK lockdown would have differed between participants. Fifth, the fairly small sample size used for analysis may have limited the power to detect statistically significant differences in declines in diet quality according to the various participant characteristics considered. Finally, as in all cohort studies, participants who consented to be included are likely to have been healthier than those who refused which may have limited the generalisability of findings. This is supported by the fact that 87.7% of participants lived in their own property and 53.4% were in a current relationship. However, as our analyses were internal, substantial bias should only have been introduced if the associations examined differed markedly between those who participated in the study and those who did not; this seems unlikely. To confirm this, we assessed demographic characteristics of our population against national survey data for England (accessed at https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england); prevalence of current smoking in our analysis sample (men 3%, women 2%) was slightly lower than reported among participants aged 75 years and older from the nationally representative 2019 Health Survey for England (men 6%, women 6%). However, these are fairly similar, given the variability expected from the reasonably small SaLSA sample and also the Health Survey for England which reported a 3% current smoking prevalence among men aged 75 years and older in 2018. However, mean BMI in our analysis sample (men 26.0, women 26.4) was slightly lower than reported among participants aged 75 years and older from the 2019 Health Survey for England (men 27.6, women 27.7), suggesting that our cohort may indeed be slightly healthier than national averages. Finally, although all data collected were obtained through self-administered questionnaires, we used validated tools wherever possible.
5. Conclusion
Older individuals are a particularly vulnerable population for COVID-19 infection and were commonly advised to shield to reduce exposure to the virus, which may have impacted access to usual food choices. We have found that greater nutritional risk was associated with being in a worse category for change in diet quality, highlighting the need to consider this when providing support for shopping and nutritional guidance to older adults in any future pandemics and should be considered when evaluating older adults as we emerge from the current pandemic.
Data availability statement
The datasets presented in this article are not readily available because a steering committee will be set up to manage data access requests. Requests to access the datasets should be directed to ZmFpZHJhLmxhc2tvdUBzb3Rvbi5hYy51aw==.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Ethics Committee (REC) Health Regulator Authority (HRA) (REC reference 21/SC/0036, 17/03/2021). The patients/participants provided their written informed consent to participate in this study.
Author contributions
FL produced the first draft of the manuscript. LW conducted the statistical analyses. GB, IB, and HP made substantial additions to the manuscript. ED and CC designed the study and revised the manuscript. All authors made substantial contributions to the manuscript and approved the final version.
Funding
FL and HP are supported by the NIHR Southampton Biomedical Research Centre, Nutrition, and the University of Southampton. These funding bodies had no role in writing of the manuscript or in the decision to submit for publication.
Acknowledgments
The authors would like to thank the administration staff at Living Well Partnership for their assistance in establishing this cohort.
Conflict of interest
ED has received honoraria and speaker fees from Pfizer, Lilly, UCB and Viatris. CC reports personal fees outside the submitted work from Amgen, Danone, Eli Lilly, GSK, Kyowa Kirin, Medtronic, Merck, Nestle, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB. HP has received lecture fees from Abbott, Pfizer, and HC-UK conferences outside of the submitted work.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
This report is independent research and the views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
1. Lochlainn MN, Cox NJ, Wilson T, Hayhoe RPG, Ramsay SE, Granic A, et al. Nutrition and frailty: opportunities for prevention and treatment. Nutrients. (2021) 13:2349. doi: 10.3390/nu13072349
2. Shad BJ, Wallis G, van Loon LJC, Thompson JL. Exercise prescription for the older population: the interactions between physical activity, sedentary time, and adequate nutrition in maintaining musculoskeletal health. Maturitas. (2016) 93:78–82. doi: 10.1016/j.maturitas.2016.05.016
3. Cruz-Jentoft AJ, Landi F, Schneider SM, Zúñiga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. (2014) 43:748. doi: 10.1093/ageing/afu115
4. Atlihan R, Kirk B, Duque G. Non-pharmacological interventions in osteosarcopenia: a systematic review. J Nutr Health Aging. (2021) 25:25–32. doi: 10.1007/s12603-020-1537-7
5. Jennings A, Mulligan AA, Khaw KT, Luben RN, Welch AA. A mediterranean diet is positively associated with bone and muscle health in a non-mediterranean region in 25,450 men and women from EPIC-Norfolk. Nutrients. (2020) 12:1154. doi: 10.3390/nu12041154
6. Granic A, Sayer AA, Robinson SM. Dietary patterns, skeletal muscle health, and sarcopenia in older adults. Nutrients. (2019) 11:745. doi: 10.3390/nu11040745
7. Fabiani R, Naldini G, Chiavarini M. Dietary patterns in relation to low bone mineral density and fracture risk: a systematic review and meta-analysis. Adv Nutr. (2019) 10:219–36. doi: 10.1093/advances/nmy073
8. Lithander FE, Neumann S, Tenison E, Lloyd K, Welsh TJ, Rodrigues JCL, et al. COVID-19 in older people: a rapid clinical review. Age Ageing. (2020) 49:501–15. doi: 10.1093/ageing/afaa093
9. Bricio-Barrios JA, Ríos-Silva M, Huerta M, Cárdenas-María RY, García-Ibáñez AE, Díaz-Mendoza MG, et al. Impact on the nutritional and functional status of older mexican adults in the absence of recreational activities due to COVID-19: a longitudinal study from 2018 to 2021. J Appl Gerontol. (2022) 41:2096–2104. doi: 10.1177/07334648221099278
10. Laskou F, Linfield A, Aggarwal P, Dennison EM, Patel HP. Establishing a resource to assess musculoskeletal health in older adults in the post-COVID-19 era: time to SaLSA? Osteology. (2022) 2:41–51. doi: 10.3390/osteology2010005
11. Posner BM, Jette AM, Smith KW, Miller DR. Nutrition and health risks in the elderly: the nutrition screening initiative. Am J Public Health. (1993) 83:972. doi: 10.2105/AJPH.83.7.972
12. University of Bristol. The Wellcome Covid-19 Questionnaire. (2021). https://www.bristol.ac.uk/alspac/researchers/wellcome-covid-19/ (accessed December 19, 2022).
13. Malmstrom TK, Morley JE, SARC-F. A simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. (2013) 14:531–2. doi: 10.1016/j.jamda.2013.05.018
14. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.M146
15. Poelman MP, Gillebaart M, Schlinkert C, Dijkstra SC, Derksen E, Mensink F, et al. Eating behavior and food purchases during the COVID-19 lockdown: a cross-sectional study among adults in the Netherlands. Appetite. (2021) 157:105002. doi: 10.1016/j.appet.2020.105002
16. Larson EA, Bader-Larsen KS, Magkos F. The Effect of COVID-19-related lockdowns on diet and physical activity in older adults: a systematic review. Aging Dis. (2021) 12:1935. doi: 10.14336/AD.2021.0606
17. Cicero AFG, Fogacci F, Giovannini M, Mezzadri M, Grandi E, Borghi C. COVID-19-related quarantine effect on dietary habits in a northern italian rural population: data from the brisighella heart study. Nutrients. (2021) 13:1–10. doi: 10.3390/nu13020309
18. Rolland B, Haesebaert F, Zante E, Benyamina A, Haesebaert J, Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: survey study. JMIR Public Heal Surveill. (2020) 6:e19630. doi: 10.2196/19630
19. Acton RB, Vanderlee L, Cameron AJ, Goodman S, Jáuregui A, Sacks G, et al. Self-reported impacts of the COVID-19 pandemic on diet-related behaviours and food security in five countries: results from the international food policy study 2020. J Nutr. (2022) 152(Suppl. 1):35S−46. doi: 10.1093/jn/nxac025
20. Górnicka M, Drywień ME, Zielinska MA, Hamułka J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among polish adults: a cross-sectional online survey PLifeCOVID-19 study. Nutrients. (2020) 12:2324. doi: 10.3390/nu12082324
21. Lamarche B, Brassard D, Lapointe A, Laramée C, Kearney M, Côté M, et al. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: results from NutriQuébec. Am J Clin Nutr. (2021) 113:984–92. doi: 10.1093/ajcn/nqaa363
22. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Cinelli G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. (2020) 18:1–15. doi: 10.1186/s12967-020-02399-5
23. Constant A, Conserve DF, Gallopel-Morvan K, Raude J. Socio-cognitive factors associated with lifestyle changes in response to the COVID-19 epidemic in the general population: results from a cross-sectional study in France. Front Psychol. (2020) 11:579460. doi: 10.3389/fpsyg.2020.579460
24. Bevilacqua G, D'Angelo S, Linaker C, Paul A, Bloom I, Zhang J, et al. Physical activity and diet in a global pandemic: an investigation of the impact of COVID-19 on factors relevant for musculoskeletal health at two different stages of the lifecourse. Front Endocrinol. (2022) 13:882399. doi: 10.3389/fendo.2022.882399
25. Mendoza-Ruvalcaba NM, Gutiérrez-Herrera R, López C, Hesse H, Soto-Añari M, Ramos-Henderson M, et al. Impact of quarantine due to COVID-19 pandemic on health and lifestyle conditions in older adults from Centro American countries. PLoS ONE. (2022) 17:e0264087. doi: 10.1371/journal.pone.0264087
26. Luo Y, Chen L, Xu F, Gao X, Han D, Na L. Investigation on knowledge, attitudes and practices about food safety and nutrition in the China during the epidemic of corona virus disease 2019. Public Health Nutr. (2021) 24:267–74. doi: 10.1017/S1368980020002797
27. Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. (2015) 73:643–60. doi: 10.1093/nutrit/nuv027
28. Rodríguez-Pérez C, Molina-Montes E, Verardo V, Artacho R, García-Villanova B, Guerra-Hernández EJ, et al. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients. (2020) 12:1–19. doi: 10.3390/nu12061730
29. Thorpe MG, Milte CM, Crawford D, McNaughton SA. Education and lifestyle predict change in dietary patterns and diet quality of adults 55 years and over. Nutr J. (2019) 18:1–13. doi: 10.1186/s12937-019-0495-6
30. Kinoshita K, Satake S, Arai H. Impact of frailty on dietary habits among community-dwelling older persons during the COVID-19 pandemic in Japan. J Frailty Aging. (2022) 11:109. doi: 10.14283/jfa.2021.45
31. Bloom I, Zhang J, Parsons C, Bevilacqua G, Dennison EM, Cooper C, et al. Nutritional risk and its relationship with physical function in community-dwelling older adults. Aging Clin Exp Res. (2022) 34:2031–9. doi: 10.1007/s40520-022-02171-3
Keywords: diet, older adults, COVID-19, sarcopenia, frailty
Citation: Laskou F, Bevilacqua G, Westbury LD, Bloom I, Aggarwal P, Cooper C, Patel HP and Dennison E (2023) A study of diet in older community-dwelling adults in the UK during the COVID-19 pandemic: Findings from the Southampton Longitudinal Study of Ageing (SaLSA). Front. Nutr. 9:988575. doi: 10.3389/fnut.2022.988575
Received: 07 July 2022; Accepted: 28 December 2022;
Published: 13 January 2023.
Edited by:
William Tebar, University of São Paulo, BrazilReviewed by:
HeeSoon Lee, Bowling Green State University, United StatesKornanong Yuenyongchaiwat, Thammasat University, Thailand
Tino Prell, University Hospital in Halle, Germany
Copyright © 2023 Laskou, Bevilacqua, Westbury, Bloom, Aggarwal, Cooper, Patel and Dennison. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elaine Dennison,  ZW1kQG1yYy5zb3Rvbi5hYy51aw==
ZW1kQG1yYy5zb3Rvbi5hYy51aw==
 Faidra Laskou
Faidra Laskou Gregorio Bevilacqua
Gregorio Bevilacqua Leo D. Westbury
Leo D. Westbury Ilse Bloom1
Ilse Bloom1 Harnish P. Patel
Harnish P. Patel Elaine Dennison
Elaine Dennison