
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 05 October 2022
Sec. Nutritional Epidemiology
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.973241
This article is part of the Research TopicNutrition and Oral Health: Public Health RelevanceView all 18 articles
Adolescents are a population group that is vulnerable to nutritional problems other than toddlers, especially young women. Special attention to the dietary issues of adolescent girls needs to be obtained along with the increase in the adolescent population in Indonesia because this affects the growth and development of the body and will impact adult nutrition problems. The purpose of the study was to analyze the relationship between diet assessment and oral health status of adolescent girls, the relationship between oral hygiene behavior and oral health status of adolescent girls, and the simultaneous relationship between dietary assessment and oral hygiene behavior with the oral health status of adolescent girls. Analytical research using the survey method was conducted on 96 young women in two junior high schools in Bandung. Assessment of diet seen from eating behavior and anthropometric examination. Eating behavior using the Adolescent Food Habit Checklist Index questionnaire and anthropometric investigations were carried out by looking at body height, body weight, and Mid Upper Arm Circumference using the standards from the Indonesian Minister of Health Regulation 2020. Oral hygiene behavior using the Oral Hygiene Behavior Index questionnaire. Oral health status using the Dental Health Status Assessment. The results were statistically analyzed with Spearman’s Rank Correlation, and Multiple Linear Regression tests showed no significant relationship between dietary assessment and oral health status (eating behavior with a p-value = 0.429 and anthropometric examination with a p-value = 0.262). A significant association between oral hygiene behavior and oral health status, with a p-value of 0.003, while there is no simultaneous relationship between diet assessment and oral hygiene behavior with oral health status, with multiple r2 = 13.2%.
In Indonesia, the prevalence of small infants from the small mother group (body height =150 cm) is currently 34.8% (1). The study of Demographic Health Surveys in 54 countries found that for every 1 cm less in mother’s height, the risk of underweight and stunting in children under five increased. In an analysis of 52 of 54 countries (96%), the association between maternal height and stunting was statistically significant (2). However, the association between maternal and infant length may reflect both genetic background and the environmental determinants and developmental experiences mothers experience during childhood, maturation, and subsequent offspring growth. For example, women with short stature have a higher risk of having babies with lower birth weight (LBW), and teenage pregnancy may also increase the risk of LBW events. In addition, stunting seems to be interpreted as malnutrition themselves, but especially in Indonesia, it was shown that stunting is more influenced by education and social structure than nutrition (3–6). There is a new concept of the modern view of growth regulation that involves social-economic-political-emotional (SEPE), which was explained by Bogin (7). This modern view will be explained why stunting prevention needs to involved not only health parameters.
Prevention of stunting has become a national priority so that the younger generation in Indonesia can grow and develop in the best possible way. The government has issued the National Strategy to Accelerate Stunting Prevention guide for central and local governments to implement stunting prevention efforts. The National Stunting Strategy includes specific and sensitive nutritional interventions to improve nutrition. Specific nutrition interventions aim to address nutrition-related issues directly through the health sector. At the same time, sensitive nutritional interventions aim to address non-health issues contributing to stunting, such as providing clean water, food security, and health insurance (8).
A group at high risk for nutritional problems is adolescents (9). With the increasing adolescent population in Indonesia, adolescent nutrition must be given special attention as it affects physical growth and development and will impact adult nutrition. Nutritional problems in adolescents, whether under- or over-nutrition, can adversely affect public health. Adolescent malnutrition will have a negative impact on public health, such as reduced physical fitness, reduced productivity, and even the fertility of adolescents themselves, especially young women (10).
One of the methods used to assess a person’s nutritional status is dietary assessment. Direct assessment of diet is by looking at eating behavior and anthropometry. Adolescent eating behavior has received increasing attention in recent years amid claims that many adolescents have a poor diet, including high levels of fatty foods and low intakes of fruit and vegetables. Variations in adolescent dietary intake are likely to reflect available diets, values and circumstances of parents, school and peers, and their motivation. If adolescents’ eating habits/behavior are poor, it will affect the clinical condition that indicates a nutritional deficiency, thus affecting their anthropometry (11).
Oral health plays a fundamental role in overall health and wellbeing. Oral health has a significant impact, significantly on the quality of life (12). Many factors affect a person’s oral health: socioeconomic status, education, living and school environment, and individual behavior. Eating behavior and oral health have a synergistic and dynamic relationship (13). Diet, nutritional composition, and poor oral and dental conditions will interact and have a role in the formation play a role in caries’ formation motion of sweet foods contained in individual snack patterns are the main factors of a cariogenic diet. Oral health is closely related to oral hygiene because oral hygiene is a primary factor in creating oral health. Oral hygiene can determine a person’s level of oral health. Young women need to consider maintaining nutritional status and oral hygiene, starting from pre-wedding preparations, especially brides-to-be, to preconception, gestation, and postpartum, which may directly impact the fetus later on; what does it contain (14). Therefore, this study aimed to analyze the association between nutritional assessment, oral hygiene behaviors, and oral health status in adolescent girls. It is hypothesized that there is a simultaneous relationship between the evaluation of diet and oral hygiene behavior with the oral health status of adolescent girls.
Analytical observational school-based studies with a cross-sectional design were used, and survey data were collected through questionnaires and anthropometric surveys. Two schools were selected due to being located at a stunting locus [based on the Decree of the Mayor of Bandung regarding stunting loci in Bandung City (15)]. Participants were recruited by simple random sampling. The subjects of this study were middle school girls who met the following criteria: (i) were in the age range of 10–15 years, (ii) had no chronic systemic disease, and (iii) were willing to participate in the study (proofed by parental signed informed consent).
In this study, correlation analysis was used. The formula used to determine the sample size was the formula used to determine the sample size using correlation analysis, (i) type I error (Zα) = set at 5% with a one-way hypothesis, so Zα = 1.96; (ii) type II error (Zβ) = set at 10% with a one-way hypothesis, then Zβ = 0.84; and (iii) research correlation coefficient (r) = 0.3. Based on the calculation of the sample size formula above, a minimum of 84 people is required (16).
Dietary assessments will be assessed using adolescent girls’ dietary habits and anthropometric surveys. Eating behavior is a student’s repetitive pattern of eating habits, which can be evaluated using a questionnaire. At the same time, anthropometry is assessed by examining the student’s height, including height, weight, and mean upper arm circumference (MUAC). The dietary assessment tool consisted of the Adolescent Eating Habits Checklist (AFHC) questionnaire (7), adapted into Indonesian for this study and tested on 64 adolescents, which is not included in this study. The reliability of the tested questionnaire leads to a Cronbach’s alpha = 0.86.
The AFHC questionnaire contains 23 “correct” or “incorrect” or “not applicable to me” questions. Responses indicating healthy behaviors are scored as 1. Final scores were adjusted for “not applicable” and missing responses using the following formula: AFHC score = number of “healthy” responses × (18/number of items answered). The measurement scale uses the Guttman scale, and the last level multiplied by 100 becomes the interval scale. The examples of the questions for instance, if I am having lunch away from home, I often choose a low-fat option (11).
Anthropometric examination by calculating the formula body-mass-index (BMI) per age and MUAC. BMI category (kg/m2): thin underweight, weight level < 17.00; Mild weight loss 17.00–18.49; Normal 18.50–24.99; Overweight/ Mildly overweight 25.00–26.99; Excess weight level > 27.00, then the BMI results are entered in the Z-Score formula, while the MUAC threshold used is 23.5 cm. Anthropometric examination measuring scale using a ratio scale. The procedure measuring MUAC was to determine the mid-point between the elbow and the shoulder (acromion and olecranon). Placing the colored tape measure around the left arm (the arm should be relaxed and hang down the side of the body). Measure the MUAC while ensuring that the tape neither pinches the arm nor is left loose. Read the measurement from the window of the tape or from the tape. Record the MUAC to the nearest 0.1 cm or 1 mm. If a measurement in the green zone means the child is properly nourished; a measurement in the yellow zone means that the child is at risk of malnutrition; a measurement in the red zone means that the child is acutely malnourished (17).
Oral hygiene behaviors were participants’ verbal care behaviors assessed using a questionnaire. The Oral Hygiene Behavior Questionnaire was developed based on the theory of planned behavior (18) and tested on 50 adolescents that are not included in the main study (Cronbach’s alpha = 0.842). The questionnaire contains 17 items assessing attitudes, subjective norms, and perceived behavioral control. The response score is 0–5. Total scores range from 0 to 85, with higher scores indicating positive oral hygiene behaviors. The measurement scale adopts the Likert scale, and the final result is multiplied by 100 to become the interval scale.
Oral health status is an oral health condition felt by the participant assessed from the questionnaire. Because it was still a pandemic, oral health status was measured using a self-reported dental health status assessment questionnaire (19) trans-adapted into Indonesian (Cronbach’s alpha = 0.758). The original questionnaire contained 10 statement items to assess caries risk, but only seven items remained after undergoing trans-adaptation and pre-test. Responses were scored from 0 to 1. The total score ranged from 0 to 7, with higher scores indicating individuals with better health status. The measurement scale uses a Likert scale. The final score times 100 becomes an interval scale.
Data collection took place in April 2022. Prior to the day of data collection, informed consent was given to the parents of the students who explained the course of the research. In addition, parents are asked to fill in the child’s health data, whether the child has a particular disease or disability. It is necessary to determine the confounding factors in this study. Adolescents with a history of chronic systemic disease were excluded from participation. Aside from the child’s health history, the parents also asked questions regarding social-economic status.
Participants previously received instructions on how to complete the questionnaire. After participants understood, they simultaneously met all questionnaires (AFHC, Oral Hygiene Behavior Questionnaire, Oral Health Status Questionnaire) in two separate rooms. A research assistant accompanied each. After completing the questionnaires, the researchers (principal investigators) administered anthropometric measurements to the participants, whom research assistants assisted. Anthropometric measurements include weighing with a digital scale to measure body weight. All participant were weight with their school uniform clothes on and barefooted. Body height was measured using microtoise stature meter with an accuracy of 0.1 cm (20).
The collected data were processed descriptively and analytically. For descriptive data, statistical measures of counts and percentages for categorical and numerical data, by plotting mean, standard deviation, median, and range. When the data are not normally distributed, analyze the data using statistical tests with Pearson’s correlation analysis or Spearman’s rank correlation. Normality tests used Kolmogorov-Smirnov data, while multiple linear regression analysis was used to analyze simultaneous associations between dietary ratings, oral hygiene behaviors, and oral health status. Use a p-value < 0.05 to determine the significance of test results.
This study has been ethically reviewed by the Research Ethics Committee of Padjadjaran University No: 463/UN6.KEP/EC/2022.
Ninety-six students completed questionnaires and anthropometric measurements. Table 1 shows the characteristics of the participants. As seen from the characteristics table, the average age of adolescent girls in both schools is 13.8 years old, with a range of 12–15 years. Family socioeconomic status was predominantly middle class (47.9%); most educational qualifications were classified as low 43.8% (secondary school and below), and anthropometric findings were described as normal (85.4%) based on BMI/age and based on MUAC was normal (52.1%).
A description of the variables studied; the oral hygiene behavior score, the eating behavior score, and the oral health status score are presented in Table 2. As seen from the table, the data for the three variables based on the normality test yielded a p-value < 0.05; the data are not normally distributed, leading to non-parametric statistics being used for further analysis.
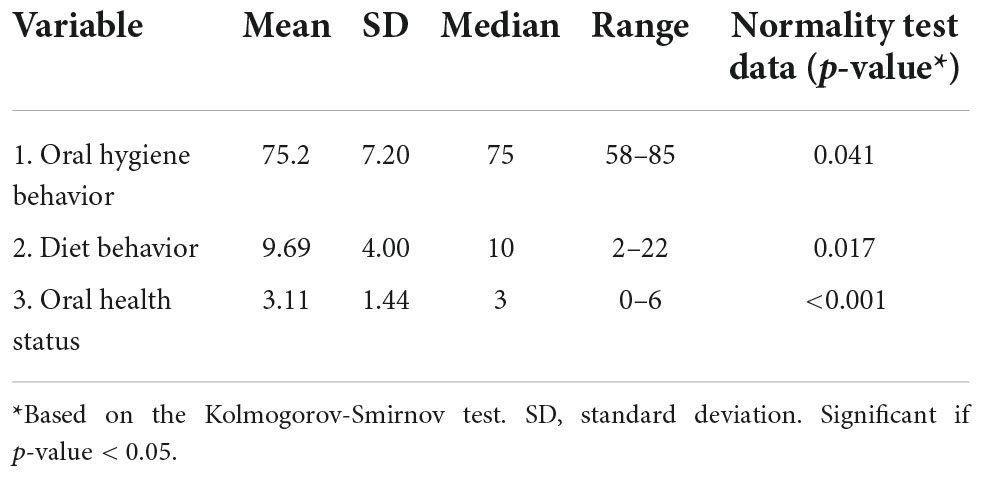
Table 2. Statistical description of nutritional (diet) behavior and oral hygiene behavior scores by adolescent oral health status.
The statistical analysis by Spearman rank correlation in Table 3 shows that the correlation between oral health status score and oral hygiene behavior score was r = 0.300; p = 0.003, which means that the higher the oral hygiene behavior score, consequently increase the oral health condition score. While the relationship between eating behavior and oral health status in adolescent girls showed a non-significant correlation (r = 0.082; p = 0.429).
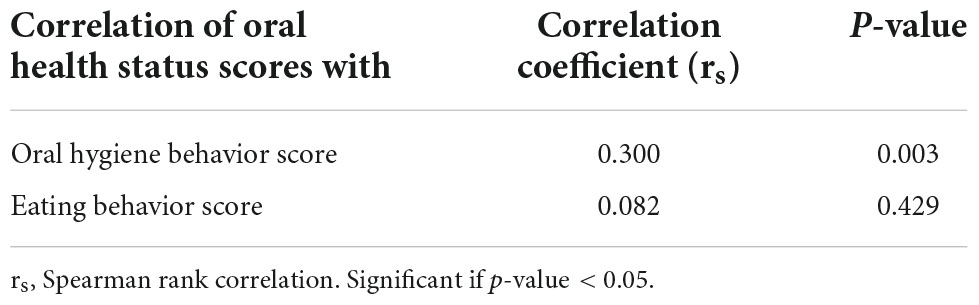
Table 3. Correlation of nutritional assessments (eating behaviors) and oral hygiene behaviors with oral health status in adolescents.
Table 4 presents the comparative analysis of oral health status scores of various characteristics of adolescent girls. From the table, it shows that there is a difference in oral health status scores; the socioeconomic status of the family (p = 0.033), the most significant oral health status score, in the middle socioeconomic status with a median = 4, while the lower and upper socioeconomic status with a median = 3. For parental education, there seems to be a tendency that the higher the parental education, the higher the oral health status, although statistically not significant (p = 0.088/p > 0.05). Comparison of oral health status scores based on dietary assessment from anthropometric examinations (BMI/Age and MUAC) obtained a p-value = 0.262, which showed no significant difference or in other words anthropometric examination is not significantly related to the oral health status of adolescent girls.
Furthermore, to analyze the relationship between dietary assessment and oral hygiene behavior from various variables (because the data is not homogeneous) with oral health status scores using multiple linear regression analysis. The variables involved in this analysis have a p-value < 0.25 from the results of the bivariable study; parents’ education, socioeconomic, eating behavior scores, and oral hygiene scores. The results of multiple linear regression analysis are presented in Table 5.
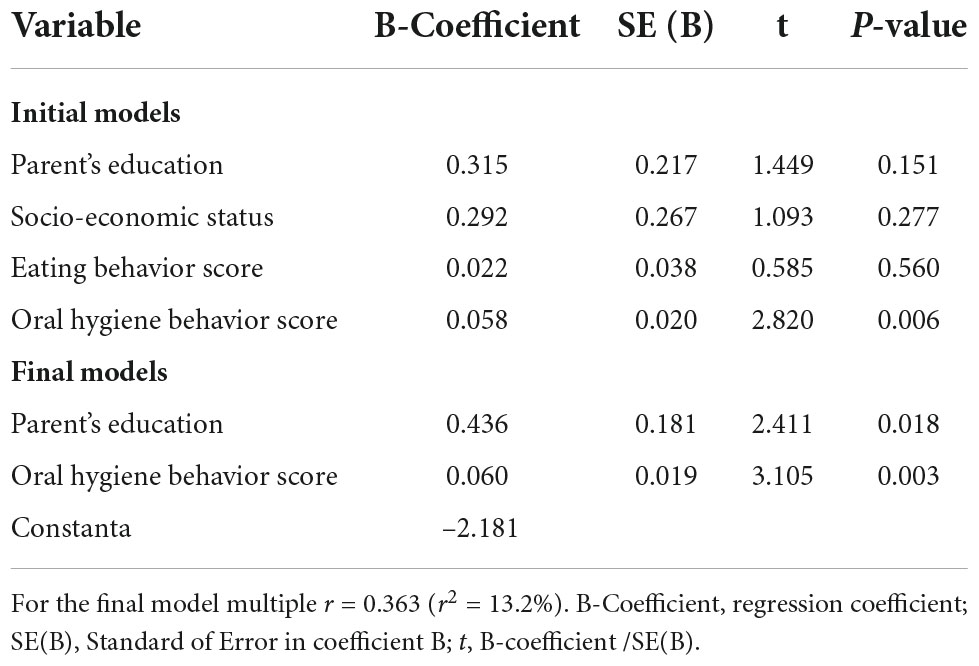
Table 5. Relationship of oral health status scores with various variables based on multiple linear regression.
Table 5 presents the analysis of the relationship between oral health status scores based on multiple linear regression of various variables. The first step is to estimate the model or any variables studied because the variables studied are dietary assessments (eating behavior and anthropometric examination) with oral health status with data that varies on research subjects or is not homogeneous, so that confounding variables such as status socioeconomic and education are also included in the initial model in this multiple linear regression analysis. The second step is to carry out classical assumptions, namely to obtain a model estimated to be feasible or not in interpreting the influence of the independent variable on the dependent variable. The variables involved in the final model have a p-value < 0.25. From the four initial models that have been analyzed, the final model that relates to oral health status scores is parental education and oral hygiene behavior scores with a positive B coefficient, meaning that the more parents’ education and oral hygiene scores increase the oral health status score. The magnitude of the coefficient of determination (r2 multiple) = 13.2%; it means that 13.2% of the variation of the oral health status score is influenced by parental education and oral hygiene behavior scores, and the remaining 86.8% is influenced by other factors not studied. This analysis concludes that the hypothesis is rejected, which states that there is a simultaneous correlation between the evaluation of diet and oral hygiene behavior with the oral health status of adolescent girls.
The characteristics of the research subjects obtained based on the inclusion and exclusion criteria were 96 people with an average age of 13.8 years with a range of 12–15 years. According to WHO (21), the age of 10–15 is the early adolescent stage. At this stage, it can be used as a basis for nutritional counseling and planning for youth education programs (21). Some things need to be considered in young women, which is maintaining nutritional status and oral hygiene, starting with preparing themselves from pre-wedding, especially the bride-to-be, until the pre-pregnancy, pregnancy, and postnatal period (22). Based on the 2018 Indonesian Research Data report, 57.6% of Indonesians experience dental and oral health problems in the form of dental caries and periodontal disease. A significant increase in dental and oral issues occurs in adolescents aged 12–18 (23). In addition, the Ministry of Health also released the Effective Medical Demand (EMD) value in adolescent girls, which was higher (9.1) than in teenage boys (7.1) (24). Therefore, adolescent girls are more prone to dental and oral problems than boys.
The results of the correlation analysis of eating behavior scores in this study showed a non-significant relationship; This means that good eating behavior does not necessarily indicate good health status. Assessment of diet (eating behavior) is related to a person’s nutritional status. The better a person’s nutritional status, the better the dental health status. This is in line with Budisuari’s study which states that a person’s eating habits or patterns can affect the occurrence of caries, especially if a person tends to consume sugar which is the leading cause of caries. The level of sugar consumption has increased overall in developing countries, and the increase in the prevalence of dental caries in developing countries has been ascribed to the rise in sugar consumption (25). Adolescents begin to decide what to eat without relying on their parents anymore. They also tend to be craving between meals and are very interested in consuming sugary snacks, such as chocolate, candy, and carbonated drinks, which triggers an increase in caries (26). The existence of sweet foods, snacks, and carbonated beverages inside and outside the school complex has reached students to buy and consume them, the interest of teenagers also supports this at this age who are more interested in the taste and appearance of food than its nutritional value (27), but in this study, the eating behavior of adolescent girls was not significantly associated with oral health status. This is understandable because eating behavior is not the only one of the factors that can affect oral health status. Oral health status is influenced by the interaction of four factors: behavior, environment, health services, and genetics. In developing countries such as Indonesia, behavior is indeed the most dominant factor in influencing the status of dental and oral health (28).
In this study, anthropometric examination was not significantly associated with oral health status in adolescent girls. The correlation of anthropometric examination and oral health can be explained as follows; the anthropometric examination is related to a person’s nutritional status, and this is in line with the study by Busman and Atigah which states that nutritional status is a sign of the body’s appearance caused by a balance between nutrient intake and health expenditure as seen through the variables of height, weight, and growth. Lack of nutrition is caused by various factors, including infectious diseases and food intake (29). Another study from Ratnasari and Junaidi (30), the effect of dental caries can cause disturbances in the digestive process and eating difficulties that generate growth and development disorders, and vice versa, meaning that the better a person’s nutritional status, the better the dental health status. Nutrition is essential in developing and defending oral health, especially teeth and gingiva. Healthy or unhealthy conditions of teeth and gingiva can affect food intake. In adolescents with dental caries, there is often a disturbance in the information about food substances which is a factor causing lack of nutrition, and it can cause a decrease in the body’s biological function or malnutrition (29). The oral health is part of the health of the body that affects each other. In this study, anthropometric assessments of adolescent girls were not significantly associated with oral health status. This is consistent with Nurlaila and Herwati a survey conducted in Karangantu District, Banten Province, that found no significant association between nutritional status and dental caries in school children aged 9–14. This situation is more because cariogenic food can have a direct impact as the cause of dental caries if it is supported by a state of low tooth resistance, a form of saliva that is less than normal and dense (31).
Adolescents are not only physically mature but also cognitively and emotionally. They seek identity, strive to be independent and acceptable, and pay a great interest to their self-appearance. These changes significantly impact eating behavior and skipping between meals, snacking, and café’s dine in. These habits are further influenced by families, groups, and the media. In addition, the influence of the physical environment, such as air that has experienced air pollution and extreme temperatures, as well as physical activity, although generally considered positive, can give stress to the body, affecting a person’s nutritional needs. In addition, the influence of the non-physical environment, such as the family and community environment, socio-cultural factors, and socioeconomic factors, also affect the nutritional status of adolescents (26).
The results of the correlation analysis of oral health status scores with oral hygiene behavior scores showed that there was a significant relationship (rs = 0.300; p = 0.003). This means that the higher the oral hygiene score, the higher the oral health status score. Good oral hygiene behavior will affect oral health status. Study by Budisuari stated that tooth brushing behavior affects the occurrence of caries. This is related to the process of caries itself, where if sucrose stays in the mouth for a long time and is not cleaned immediately, it will lead to the possibility of caries. This follows Gustafson’s opinion, stating that sugar consumption increases caries attack activity. The most significant risk is if sugar is eaten in a form that is easily attached and not cleaned immediately (32). Another study that supports this opinion conducted by Stephen, stated that after consuming carbohydrates, the pH of the mouth will drop in 5–10 min to 5.5, which is acidic, but will return to normal within 30–45 min, with the addition of sucrose in the form of drinks, bread, chocolate, caramel and candy between meals can cause an increase in caries activity. Still, if consumed at mealtimes, the formation rate will be reduced, or in other word, no caries will form (33). Two approaches can be taken to improve one’s oral hygiene. First, the individual approach through accelerating the increase in the ability to help oneself behave in a healthy life. For individuals who suffer from systemic disorders and periodontal disease, the behavior of maintaining oral hygiene should be intensified. The individual approach includes age, knowledge, children’s dependents, type of work, expenses, sources of costs, distance to the dentist, smoking habits, attitudes, and actions. Meanwhile, another study stated that individual factors include oral hygiene, frequency of brushing teeth, and eating acidic foods (PH < 7) (34).
The second approach, the contextual approach, includes the ratio of dentists to the population, the ratio of hospitals to residents, the ratio of dental clinics to residents, and the ratio of health centers to residents. Other contextual factors are the source of drinking water and the acidity of the water. Piped drinking water in all areas and distribution is under the supervision of the local PDAM, as well as water acidity tests by the health center are carried out periodically. In addition, other contextual factors also include the availability of dental nurses, dentists, per capita health budget, and other environmental factors that significantly influence the prevalence of oral dental disease (34). From the results of multiple linear regression analysis, the final model that relates to the oral health status score is the oral hygiene behavior score, with a positive B coefficient, meaning that the higher the oral hygiene score, the higher the oral health status score. From the magnitude of the coefficient of determination (r2 multiple) = 13.2%, it means that 13.2% variation of the score of oral health status is influenced by parental education and oral hygiene behavior scores, and the remaining 86.8% is influenced by other factors not studied. H L Blum stated that the degree of health of a person or society is influenced by four factors, namely: environment, behavior, heredity, and health services. According to Laurence Green, three factors influence a person’s behavior, namely predisposing factors, supporting factors, and reinforcing factors. Health behavior is divided into knowledge, attitude, and action. Knowledge is a very important domain for the formation of one’s actions. Factors that affect a person’s knowledge are education, occupation, age, interests, experience, and ease of getting information (35).
Adolescents’ dental and oral health maintenance is often neglected, while adolescents are also vulnerable to oral health problems during puberty. In addition, many bad habits of teenagers can cause damage to the teeth and mouth. These bad habits include laziness of night time tooth-brushing, the practice of consuming sweet foods, and the pattern of drinking sweet or soda beverage (36). Contextual factors that influence oral health status are environmental factors and followed by behavioral factors. Environmental factors affect the oral health status of about 40%, and behavioral factors affect about 30%, so it can be said that environmental and behavioral factors will affect more than two-thirds of oral health status in the community (34). Personal factors that play a role in improving oral health status include age and gender. In addition, education, occupation, economic status, knowledge, attitudes, and actions also play a role in improving oral health status. Patterns of healthy living behavior of individuals and families, non-smoking behavior followed by the ability to help oneself also affect oral health. Research in the UK states that social factors, on individual factors, are the main determinants of dental and oral health status. Individual factors were obtained from the frequency of tooth brushing, oral hygiene, and eating habits of vinegar/acidic food (PH < 7) (5, 34).
Nutrition and oral health have a two-way relationship; proper nutrition is essential in maintaining oral health. Otherwise, oral health is also crucial for maintaining adequate nutritional intake. Untreated dental caries can cause pain, causing not only eating problems but also speech and sleep problems. Furthermore, these eating disorders can have long-term impacts such as iron deficiency, anemia, and malnutrition (37–39). In a study by Morenike et al. (40) in Nigeria, it was stated that malnutrition could lead to enamel hypoplasia, which creates a niche environment for plaque retention. Furthermore, malnutrition results in hypofunction of the salivary glands, changing saliva composition and reducing its buffering capacity, thereby increasing caries formation. In addition, the study found that nutritional deficiencies were associated with oral hygiene. Previous studies also conducted in Nigeria have identified that oral hygiene is associated with a higher prevalence of caries. In contrast, other studies have highlighted the increased prevalence of caries due to poor oral hygiene (40). Although nutrition and oral hygiene can affect the oral health status of young women, which will have an impact on their quality of life (one of which is malnutrition which later as a mother-to-be can cause the risk of stunting in her child), many other factors that have been described previously, can also affect oral health status in adolescent girls. Therefore, the limitations of this study are the existence of variables or other factors related to oral health, both individually and family dimensions, as well as overall, as well as the use of self-assessment that is not supported by clinical examinations due to the COVID-19 pandemic.
There is a relationship between oral hygiene behavior and adolescent girls’ oral health status. However, the simultaneous relationship between dietary assessment and oral hygiene behavior with the oral health status of adolescent girls was not proven—similarly, the relationship between dietary assessment and oral health status of adolescent girls.
The above indicates the need for further research on other factors that can be related to oral health so that it can complement the research that has been done so that it can become a study in stunting prevention, as well as dental and oral examinations on research subjects.
Oral health and nutrition education with health promotion and nutrition counseling. It is hoped that there will be a collaboration with other professions, including doctors, parents, schools, nutritionists, health educators, and the youth health community who can help regulate adolescent nutrition. In addition, it is recommended to visit a dental polyclinic, a dentist’s private practice or a health center that must be done at least every 6 months.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Research Ethics Committee of Padjadjaran University No: 463/UN6.KEP/EC/2022. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
AS and RI conceptualized the study design. YM and AS collected the data. YM analyzed the data. IM, AS, and YM conceptualized the first draft. RI reviewed the first draft. AS finalized the writing. All authors contributed to the article and approved the submitted version.
The authors thank Universitas Padjadjaran Academic Leadership Grant for funding this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Irwansyah I, Ismail D, Hakimi M. Kehamilan remaja dan kejadian stunting pada anak usia 6-23 bulan di Lombok Barat. Berita Kedokteran Masyarakat. (2016) 32:209. doi: 10.22146/bkm.8628
2. National Population and Family Planning Board, Statistics Indonesia, Ministry of Health, ICF. Indonesia Demographic and Health Survey 2017. Jakarta: National Population and Family Planning Board (2018).
3. Scheffler C, Hermanussen M, Bogin B, Liana DS, Taolin F, Cempaka PMVP, et al. Stunting is not a synonym of malnutrition. Eur J Clin Nutr. (2020) 74:10. doi: 10.1038/s41430-019-0520-z
4. Beal T, Tumilowicz A, Sutrisna A, Izwardy D, Neufeld LM. A review of child stunting determinants in Indonesia. Maternal Child Nutr. (2018) 14:1–10. doi: 10.1111/mcn.12617
5. Indriyanti R, Nainggolan TR, Sundari AS, Chemiawan E, Gartika M, Setiawan AS. Modelling the maternal oral health knowledge, age group, social-economic status, and oral health-related quality of life in stunting children. Int J Stat Med Res. (2021) 10:200–7. doi: 10.6000/1929-6029.2021.10.19
6. Scheffler C, Hermanussen M, Soegianto SDP, Homalessy AV, Touw SY, Angi SI, et al. Stunting as a synonym of social disadvantage and poor parental education. Int J Environ Res Public Health. (2021) 18:1350. doi: 10.3390/ijerph18031350
7. Bogin B. Social-Economic-Political-Emotional (SEPE) factors regulate human growth. Hum Biol Public Health. (2021) 1:1–20. doi: 10.1186/s40101-022-00287-z
8. Millati NA, Kirana TS, Ramadhani DA, Alvewria M. Cegah Stunting Sebelum Genting. 1st ed. Jakarta: PT Gramedia (2021). p. 320.
9. Lassi Z, Moin A, Bhutta Z. Nutrition in middle childhood and adolescence. In: Bundy DAP, Silva ND, Horton S, editors. Disease Control Priorities, Third Edition (Volume 8): Child and Adolescent Health and Development. Washington, DC: The World Bank (2017). doi: 10.1596/978-1-4648-0423-6_ch11
10. Setyawati VAV, Setyowati M. Karakter gizi remaja putri urban dan rural di provinsi Jawa Tengah. Jurnal Kesehatan Masyarakat. (2015) 1:43–52. doi: 10.15294/kemas.v11i1.3463
11. Johnson F, Wardle J, Griffith J. The adolescent food habits checklist: reliability and validity of a measure of healthy eating behaviour in adolescents. Eur J Clin Nutr. (2002) 56:644–9. doi: 10.1038/sj.ejcn.1601371
12. Lam PPY, Du R, Peng S, McGrath CPJ, Yiu CKY. Oral health status of children and adolescents with autism spectrum disorder: a systematic review of case-control studies and meta-analysis. Autism. (2020) 24:1047–56. doi: 10.1177/1362361319877337
13. Kapoor G, Goswami M, Sharma S, Mehta A, Dhillon JK. Assessment of oral health status of children with leukemia: a cross-sectional study. Special Care Dentistry. (2019) 39:564–71. doi: 10.1111/scd.12419
14. Honne T, Pentapati K, Kumar N, Acharya S. Relationship between obesity/overweight status, sugar consumption and dental caries among adolescents in South India. Int J Dent Hygiene. (2012) 10:240–4.
16. Serdar CC, Cihan M, Yücel D, Serdar MA. Sample size, power and effect size revisited: simplified and practical approaching pre-clinical, clinical and laboratory studies. Biochem Med. (2021) 31:1–27. doi: 10.11613/BM.2021.010502
17. Kshatriya GK, Chakraborty R, Mondal N, Bose K. Validating mid-upper arm circumference (MUAC) cut off points as an indicator of nutritional status among nine tribal populations of India. Anthropol Rev. (2021) 84:301–15. doi: 10.2478/anre-2021-0018
18. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
19. Levin L, Shpigel I, Peretz B. The use of a self-report questionnaire for dental health status assessment: a preliminary study. Br Dent J. (2013) 214:1–4.
20. Nus-Lab,. Instruction Manual Microtoise: Model PL 202. (2022). Available online at: https://e-katalog.lkpp.go.id/jcommon.blob.filedownloader/download?id=ea4070db6759238fc0b0cdfff7e35158da673b24cab3a2990b04303af5d4df77a1475sdb5b58d10336545c597693fc4f1f59403eeb7f296939c4edc3ff7d91df859fdec4cf42599867b260f6cf49a9208fc1bfad59ed4e69e29c3e23c1d877fbe (accessed Aug 13, 2022).
21. WHO. Orientation Progam on Adolescents Health for Health-Care Providers. Department of Child and Adolescent Health and Development (CAH). Geneva: World Health Organization (2021). p. 403.
22. Safitri A. Kesiapan remaja puteri dalam menghadapi 1000 hari pertama kehidupan ditinjau dari kualitas dan kuantitas konsumsi pangan. Gizi Indonesia. (2018) 41:59. doi: 10.36457/gizindo.v41i2.252
23. Kementerian Kesehatan Republik Indonesia. Laporan Nasional Riskesdas 2018. Jakarta: Badan Penerbit Penelitian dan Pengembangan Kesehatan (2019). p. 1–627.
24. Kementerian Kesehatan Republik Indonesia. Laporan Nasional Riskesdas 2013. Jakarta: Badan Penerbit Penelitian dan Pengembangan Kesehatan (2013). p. 1–304.
25. Budisuari M, Mukjarab M. Hubungan pola makan dan kebiasaan menyikat gigi dengan kesehatan gigi dan mulut (karies) di Indonesia. Bulletin Penelitian Sistem Kesehata. (2010) 1:83–91.
26. Winpenny EM, Penney TL, Corder K, White M, van Sluijs EMF. Changes in consumption of added sugars from age 13 to 30 years: a systematic review and meta-analysis of longitudinal studies. Obesity Rev. (2017) 18:1336–48. doi: 10.1111/obr.12588
27. Fidler Mis N, Braegger C, Bronsky J, Campoy C, Domellöf M, Embleton ND, et al. Sugar in infants, children and adolescents: a position paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. (2017) 65:681–96. doi: 10.1097/MPG.0000000000001733
28. Gopdianto, R, Rattu AJM, Mariati NW. Status kebersihan mulut dan perilaku menyikat gigi anak SD Negeri 1 Malalayang. Egigi. (2014) 3.
29. Busman DE, Atigah SN. Status kesehatan rongga mulut anak dilihat dari kepedulian orang tua tentang kebersihan rongga mulut anak dan status gizi di SD Negeri No. 98/III Desa Baru Lempur, Kerinci. Menara Ilmu. (2018) 12:14–23.
30. Ratnasari J, Gultom E. Andriyani ETingkat keparahan karies dan status gizi pada anak sekolah usia 7 – 8 tahun. J Keprawatan. (2014) 4:77–87.
31. Nurlaila AM, Herwati D. Hubungan status gizi dengan karies gigi pada murid-murid di sekolah dasar kecamatan Karangantu. INA J Dent. (2005) 12:5–9.
32. Budisuari MA, Mam O. Hubungan pola makan dan kebiasaan menyikat gigi dengan kesehatan gigi dan mulut (karies) di Indonesia. Bulletin Penelitian Sistem Kesehatanl. (2010) 13:83–91.
33. Stephen A, Alles M, de Graaf C, Fleith M, Hadjilucas E, Isaacs E, et al. The role and requirements of digestible dietary carbohydrates in infants and toddlers. Eur J Clin Nutr. (2012) 66:765–79. doi: 10.1038/ejcn.2012.27
34. Notoharjo IT. Percepatan Pengendalian Masalah Status Kesehatan Gigi Mulut Melalui Pendekatan Individu dan Kontekstual. Jakarta: Lembaga Penerbit Badan Litbangkes (2020). p. 1–80.
35. Knollmueller RN, Blum HL. Planning for health; development and application of social change theory. Am J Nurs. (1975) 75:1388. doi: 10.2307/3423644
36. Senjaya AA, Yasa KAT. Hubungan Pengetahuan dengan kebersihan gigi dan mulut siswa kelas VII di SPMN 3 Selemadeg Timur Tabanan Tahun 2018. Jurnal Kesehatan Gigi. (2019) 6:19.
37. Gigi-mulut K. Nutrisi dan kesehatan gigi-mulut pada anak. Sari Pediatri. (2015) 17:71–5. doi: 10.14238/sp17.1.2015.71-5
38. Sadida ZJ, Indriyanti R, Setiawan AS. Does growth stunting correlate with oral health in children?: a systematic review. Eur J Dent. (2022) 16:32–40. doi: 10.1055/s-0041-1731887
39. Setiawan AS, Abhista N, Andisetyanto P, Indriyanti R, Suryanti N. Growth stunting implication in children: a review on primary tooth eruption. Eur J Gen Dent. (2022) 11:7–16. doi: 10.1055/s-0042-1742357
Keywords: adolescent school girls, oral health status, oral health behavior, diet assessment, stunting and skinniness
Citation: Mahriani Y, Indriyanti R, Musnamirwan IA and Setiawan AS (2022) A cross-sectional study on dietary assessment, oral hygiene behavior, and oral health status of adolescent girls. Front. Nutr. 9:973241. doi: 10.3389/fnut.2022.973241
Received: 19 June 2022; Accepted: 07 September 2022;
Published: 05 October 2022.
Edited by:
Md Anwarul Azim Majumder, The University of the West Indies at Cave Hill, BarbadosReviewed by:
Fatme Al Anouti, Zayed University, United Arab EmiratesCopyright © 2022 Mahriani, Indriyanti, Musnamirwan and Setiawan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arlette Suzy Setiawan, YXJsZXR0ZS5wdXNwYUB1bnBhZC5hYy5pZA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.