- 1Department of Biology, Laboratory of Physiopathology, Molecular Genetics & Biotechnology, Faculty of Sciences Ain Chock, Health and Biotechnology Research Centre, Hassan II University of Casablanca, Casablanca, Morocco
- 2Department of Biology, Laboratory of Microbiology, Pharmacology, Toxicology, Biotechnology and Environment Faculty of Sciences Ain Chock, Hassan II University of Casablanca, Casablanca, Morocco
- 3Health Technologies Engineering Department, Research Group in Biomedical Engineering and Pharmaceutical Sciences, ENSAM, Mohammed V University, Agdal, Morocco
- 4Gastroenterology Department, Ibn Sina Hospital, Mohammed V University, Agdal, Morocco
- 5Department of Clinical Nutrition and Dietetics, Faculty of Pharmacy, Applied Science Private University, Amman, Jordan
- 6Department of Clinical Nutrition and Dietetics, College of Health Sciences, Research Institute of Medical and Health Sciences (RIMHS), University of Sharjah, Sharjah, United Arab Emirates
- 7Research Institute of Medical and Health Sciences (RIMHS), University of Sharjah, Sharjah, United Arab Emirates
Background: During Ramadan, many patients with diabetes, renal, cardiovascular, gastrointestinal diseases, headaches, and epilepsy choose to fast even against their doctor's advice. The impact of this intermittent fasting on health and disease could be different in men and women. The aim of this study was to determine the effect of sex as a factor in diseases outcomes of patients who opt to fast during Ramadan.
Main Body: The articles included in this study reported data on six diseases: diabetes, renal, cardiovascular, gastrointestinal diseases, headaches, and epilepsy. A systematic search was performed on PubMed and Scopus for observational and clinical studies mentioning Ramadan, diabetes, renal, cardiovascular, gastrointestinal diseases, headaches, and epilepsy in both men and women. Data was extracted by two independent reviewers using a standardized data-collection form. From 381 original articles, 38 studies were selected, including 25,023 patients of which 44.4% were women. Sex-based differences were reported by 18 studies for several variables such as body mass index, blood glucose, the frequency of hypoglycemia, renal colic, mortality, thrombosis, and gastrointestinal diseases in patients fasting during Ramadan. Most of the differences between men and women were reported both in the baseline period before Ramadan and during Ramadan. Indeed, during the period outside Ramadan, the frequency of renal colic, cardiovascular, gastrointestinal diseases, were higher in men; while body mass index, Thrombosis, and headache were higher in women. In the remaining 21 studies, it was reported that the sex factor was not associated with the effect of Ramadan fasting in the frequency and other outcomes of these diseases.
Conclusion: Currently, small attention is paid to sex as a determinant factor in patients while fasting during Ramadan. There appeared to be differences in the frequency and incidence of diseases in men and women during Ramadan. Closer attention to sex differences regarding the frequency and the progression of the diseases during fasting may help to improve patient care, especially to benefit those patients willing to fast during Ramadan.
Introduction
Sex represents an important factor in biomedical science and may influence biological parameters, state of health, knowledge, attitude, and behavior in healthy and unhealthy participants. Consequently, rigorous science must include males and females (1). Sex and gender analysis promote rigorous and reproducible and responsible science (2). Several countries (e.g., USA, Canada, and the European Union) implemented policies in relation to sex as a biological variable in human research. For example, the US National Institute of Health implemented in 2016 a policy that expects scientists to account for the possible role of sex factors in human studies (3). In addition, Canada implemented a Sex and Gender-Based Analysis policy to ensure that health research in Canada addresses biological (sex) and sociocultural (gender) differences between diverse groups of people. Five years after the implementation of these policies, most of the studies have included women as participants in their research (3). Still, most of these studies (72.0%) did not mention whether sex was included in their analysis, did not report any sex-specific outcomes, and did not explain for not doing so (4).
Considering that editors play an important role in the articulation of an ethical framework that influences the conduct of research, the European Association of Science Editors developed a set of guidelines for reporting Sex and Gender Equity in Research (SAGER). These guidelines require authors to report sex and gender information in the title, abstract, study design, data analyses, results, and interpretation of findings (5).
In a review of national research ethics regulations and guidelines in Middle Eastern Arab countries published in 2012, the authors concluded that there is a need for more research on women in the Middle East (6). In the last decade, several Arab and Muslim countries implemented national policies related to the protection of research participants in biomedical research and required investigators to include women as participants.
Fasting is an important ritual in the three major monotheistic religions. Yom Kippour, Carême, and Ramadan are three fasting modalities of abstinence and the opportunity to focus on spirituality. Ramadan fasting (RF) is observed from predawn to sunset for 29–30 consecutive days by two billion Muslims worldwide, mostly living in Asia. The duration of RF varies from 12 to 22 h per day according to the geographical location and solar season. During the month of Ramadan, both men and women refrain from food, water, and sexual activities during daytime. This abstinence does not apply to nighttime.
According to the Holy Quran, travelers, persons with health concerns, elderly children and pregnant, nursing, and menstruating women are exempted from observing RF. Thus, the length of fasting is shorter in premenopausal women (23–25 days) in comparison to men (29–30 days) (7). Since 1952, more than 1,900 articles have been published on the impact of RF on health and disease conditions. Most of these articles (97%) were published in the last three decades (Faris et al., Unpublished data).
Several studies (approximately 250 studies) on healthy participants reviewed recently (8–12) demonstrated that RF induced chronobiological changes (13, 14) and was not associated with adverse metabolic impacts (8, 10–12). Indeed, RF may be accompanied by a moderate improvement of lipid and lipoprotein parameters (15, 16), especially HDL-Cholesterol levels in healthy participants (16), and beneficial effects related to insulin sensitivity, weight and body fat in healthy young men (17). However, RF was associated with a decrease in nocturnal sleep duration (18), daytime alertness, psychomotor performance (13, 19, 20), and rapid eye movement sleep (21) in healthy men. In a healthy population, recent reviews by Faris et al., and Mirmiran et al., also showed that the impact of RF was different in men and women, lipid profile (9, 12, 16), total sleep time (18). Moreover, both HbA1c% and weight decreased only in men with diabetes (22).
The early studies on Ramadan that included men and women were published after 1987 (23) and they included a small number of women. For example, the study done in Malaysia by Husain in 1987 included 12 men and nine women, and the one done by Sajid in 1991 included 46 men and only five women (24).
In patients with type 2, the study of Salti et al., which was conducted in 13 countries including a large sample of patients with diabetes, reported that severe hypoglycemic episodes were significantly more frequent during Ramadan compared with other months in patients with diabetes. Unfortunately, a sex-based analysis was not performed in this study (25). A recent review on diabetes showed that sex was one of the factors that influenced the effect of RF on hypoglycemia events, which were more frequent in women (26). There is currently no reviews addressing the question whether sex has an impact as a biological factor in dtermining the ompacts of RF in patients with diseases such as diabetes, renal, cardiovascular, gastrointestinal diseases, headaches, and epilepsy.
In this study, we conducted a systematic review of all published articles on Ramadan, to determine the effect of sex as a biological factor in disease outcomes of patients who opt to observe RF. The included articles reported data on six diseases: diabetes, renal, cardiovascular, gastrointestinal diseases, headaches, and epilepsy; and reported outcomes such as disease frequencies, physical, clinical, and biochemical parameters.
Methods
A systematic search of the peer-reviewed published literature was conducted through October 2021, according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (27), using existing literature in Medline and SCOPUS Electronic databases, with no time limit. The search terms combined Ramadan (or Ramazan or Ramadhan) fasting with one of these pathologies: diabetes, renal diseases, cardiovascular disease (CVD), gastrointestinal diseases (GITDs), headaches, and epilepsy. Reference lists of the obtained studies were hand searched, and authors were contacted to find relevant articles and reviews and to make sure that all related publications were included in the current review.
Eligibility Criteria
We applied the following inclusion criteria to select the observational and clinical studies: (1) reported data on at least one of these diseases: diabetes, renal, CVD, GITDs, headache; epilepsy; (2) reported data before and during/at the end of Ramadan; (3) compared variables in the same patients' groups; (4) reported descriptive statistics separately for men and women or reporting sex-based statistical comparison; (5) reported on any examination of primary data on disease frequency, complications, physical, biochemical parameters.
We excluded any study meeting at least one of the following exclusion criteria: (1) including only healthy participants; (2) including only one sex; (3) comparing data before and after Ramadan without providing outcomes during the month of Ramadan; (4) comparing only a fasting group to a non-fasting group; (5) including a small population size for men or women (<10 men or <10 women); (6) reporting only data about knowledge, attitude and practice; (7) studies in languages other than English, French, or Arabic.
Study Screening and Data Extraction
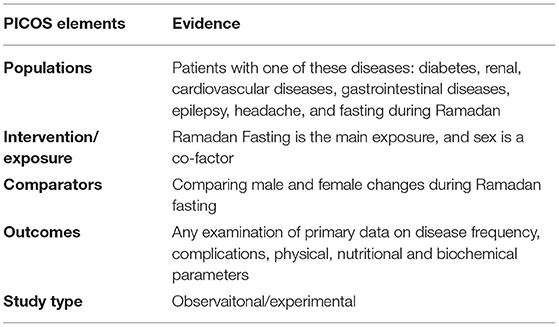
Two authors (RR, DA) removed irrelevant publications such as conference abstracts, reviews, and books, and applied the inclusion and exclusion criteria to the title and abstract. All records that were not excluded based on the title and abstract advanced to the full-text review to confirm eligibility according to the PICOS criteria (Populations, Intervention, Comparisons, Outcomes, and study design), set out in Table 1. Two authors (RR and AN) reviewed the full text of the articles selected from the title and abstract review; reasons for exclusion per article were recorded. The full-text review was done by a first reviewer and then by a second reviewer. The first reviewer made the data extraction, and then the second reviewer verified the results.
Using a standardized data-collection form, the following data were extracted from each included study: the first author's last name, publication year, study location, study design, disease condition, population size, number of women, percentage of women, variables, sex effect in baseline, Ramadan effect and sex effect during Ramadan. Data was extracted by RR and confirmed by all authors.
Outcome Measures
In this study, the main outcome was the comparison between the two sexes of the effect of RF on the outcomes of the disease.
Results
Study Characteristics
In this review, the primary search, after removing the duplicated, identified 715 citations from databases and the bibliography of the full-text articles. After the first screening phase of titles and abstracts, we excluded 334 articles because they did not meet the eligibility criteria especially reporting descriptive statistics related to sex-based differences in patients fasting during Ramadan. A total number of 381 articles appeared to be relevant for the full-text analysis. The second screening phase of the full-text articles resulted in the exclusion of 343 additional articles, and 38 articles remained for data extraction. The search strategy is presented in Figure 1. Of the included studies, 19 were retrospective, 12 were prospective studies, and six were cross-section surveys, and only one study was a randomized clinical trial.
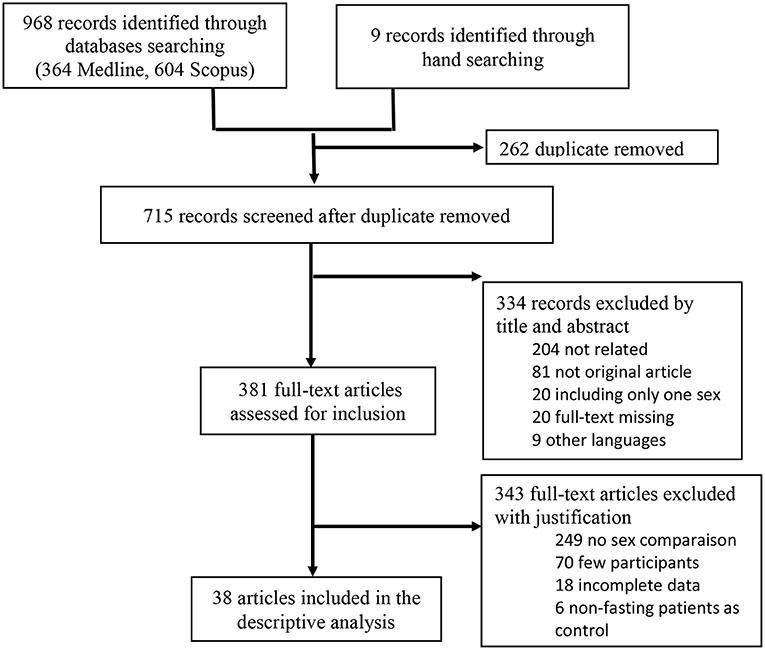
Figure 1. The flow chart with the different phases of the systematic review according to the PRISMA statement.
Publications reporting sex-related statistics during Ramadan represented only 10.0% of the total publications on RF and diseases including men and women (Table 2). This percentage was lower (4%) for the studies on Ramadan and diabetes.
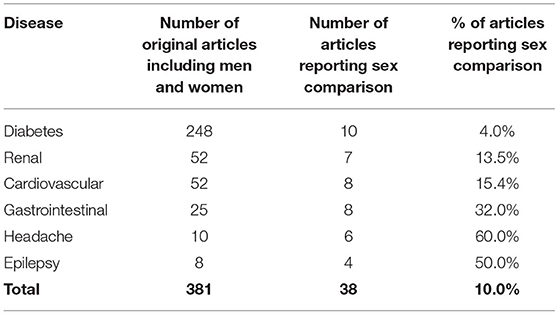
Table 2. Number and percentage of the studies reporting data for both men and women or reporting comparison between the two sexes during Ramadan fasting in the patients with diabetes, renal, cardiovascular, gastrointestinal diseases, headache, and epilepsy.
The total number of the patients was 25,023 of which 44.4% were female, and the mean age was 47.7 years. These studies reported general data from Ramadan and baseline time-points, i.e., before Ramadan. The sex effect was not always statistically analyzed. Only seven articles reported the odds ratio or relative risk for sex effect on observers of Ramadan, 18 articles reported a p-value for the comparison between men and women during Ramadan, eight articles reported the effect of RF in both sex separately, and five articles did not report a p-value.
The articles included in this review reported data for diabetes, renal diseases, GITDs, CVD, headaches, and epilepsy; and were conducted in 18 countries, mostly from Turkey (nine articles), Iran (five articles), Saudi Arabia (four articles), Egypt and Qatar (three articles), Morocco (two articles), Bahrain, Iraq, Israel, Jordan, Kuwait, Lebanon, Libya, Malaysia, Mali, Pakistan, Singapore, Tunisia (one article each). Most of these articles were published in the last 20 years, and were conducted in places where Ramadan fell in summer (27 articles, 71%) or autumn (10 articles, 26%); only one study was conducted in spring.
Sex Factor in Diabetes Diseases During Ramadan
A total of 10 observational studies including 3,936 patients, of which 46.3% women, with diabetes diseases, have reported data (28–37) for fasting men and women with type 2 diabetes or Type 1 Diabetes (Table 3). A large number of variables were reported in these studies, but we focused in this review on body mass index (BMI), blood glucose (BG), HbA1c, insulin resistance (IR), hypoglycaemia, hyperglycaemia, diabetic ketoacidosis, and emergency admission. No sex effect was reported in the baseline conditions before Ramadan except for BMI, which was higher in women (31, 32) (Figure 2).
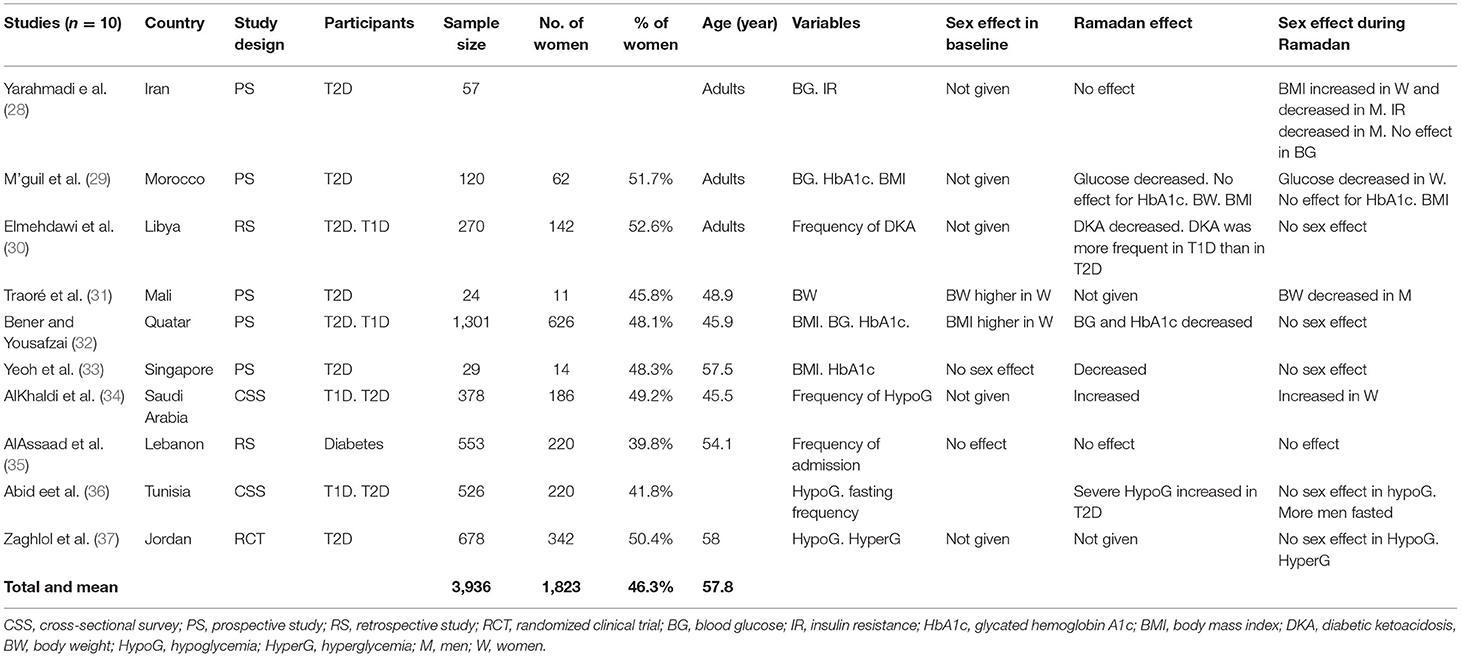
Table 3. Sex differences in outcomes related to diabetes in patients before and during Ramadan fasting.
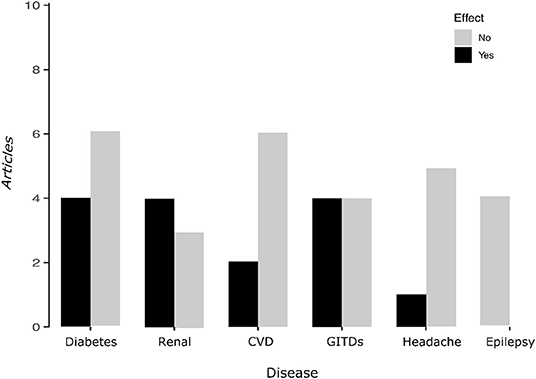
Figure 2. The Bar-plot summarizes the results obtained from studies analyzed and shows the articles that reported sex-related changes during Ramadan.  Number of articles reporting differences between men and women during Ramadan fasting
Number of articles reporting differences between men and women during Ramadan fasting  Number of articles reporting no differences.
Number of articles reporting no differences.
During Ramadan, a decrease in blood glucose BG (29, 32), HbA1c (32, 33), BMI (33), and diabetic ketoacidosis (30) was reported in four studies; while severe hypoglycaemia was reported to be increased in women (34, 36). RF effect was not significant for BG (28), Insulin resistance (28), HbA1c (29), BMI (29), and the frequency of emergency admission (35).
Sex effect during Ramadan was reported to be not significant in seven studies for BMI (32, 33), BG (28, 29, 32, 33), HbA1c (29, 32, 33), Hypoglycaemia (36, 37) the frequency of emergency admission (35). However, the sex effect during Ramadan was reported to be significant in four studies for BG (29), BMI (28, 31), IR (28), and hypoglycaemia (34). Thus, during Ramadan, BMI and body weight decreased in men and increase in women (28, 31), BG decreased and hypoglycaemia increased in women only (29, 34), and insulin resistance decreased in men only (28).
Sex Factor in Renal Diseases During Ramadan
A total of seven studies including 4,193 patients of which 36.2% were women have reported sex-related effects in renal diseases (35, 38–43), especially in patients with the diagnosis of renal colic disease, chronic kidney disease (CKD), hemodialysis, and transplant recipients (Table 4). In the period before Ramadan, most of these studies showed sex-related effects in the frequency of renal diseases, with renal colic more frequent in men (35, 39, 41, 43). During Ramadan, hospital admissions for renal colic disease were higher in three studies (35, 38, 43) and mortality was higher in one study (40). The sex effect during Ramadan was significant in three studies which reported an increase in renal colic frequency in men only (35, 39, 43), and an increase in mortality in female hemodialysis patients (40). In patients admitted for CKD, the glomerular filtration rate increased during Ramadan but did not show sex effects during this month (38). Biochemical parameters did not show RF or sex effect (42).
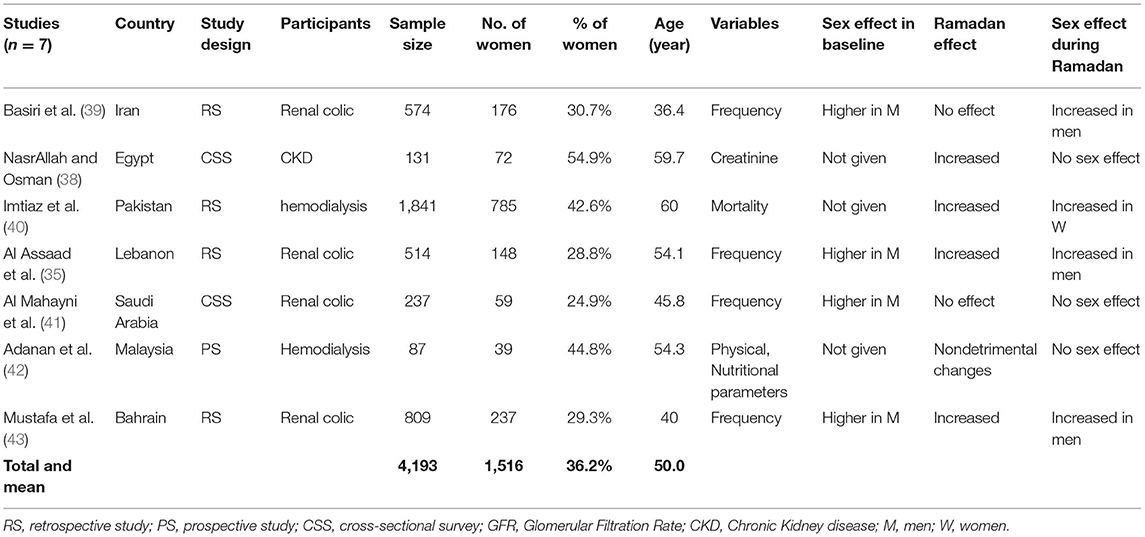
Table 4. Sex differences in outcomes related to renal diseases in patients during and outside the month of Ramadan.
Sex Factor in Cardiovascular Diseases During Ramadan
A total of eight observational studies including 6,111 patients, of which 42.9% were women, with CVD (Table 5) have reported data for fasting men and women (35, 44–50). In baseline conditions, the frequency of congestive heart failure (CHF), stroke, and the stroke scale was higher in men (35, 45, 50), while cerebral vein thrombosis (CVT) was higher in women (48, 49). During Ramadan, several studies showed no significant effect of fasting on the frequency of stroke (35, 44), congestive heart failure (45), Acute Myocardial Infarction (47); and biochemical parameters in stable patients with heart diseases (46). However, four studies reported a significant increase in CVT incidence, stroke score, and major adverse cardiac events (MACEs) (48–50).
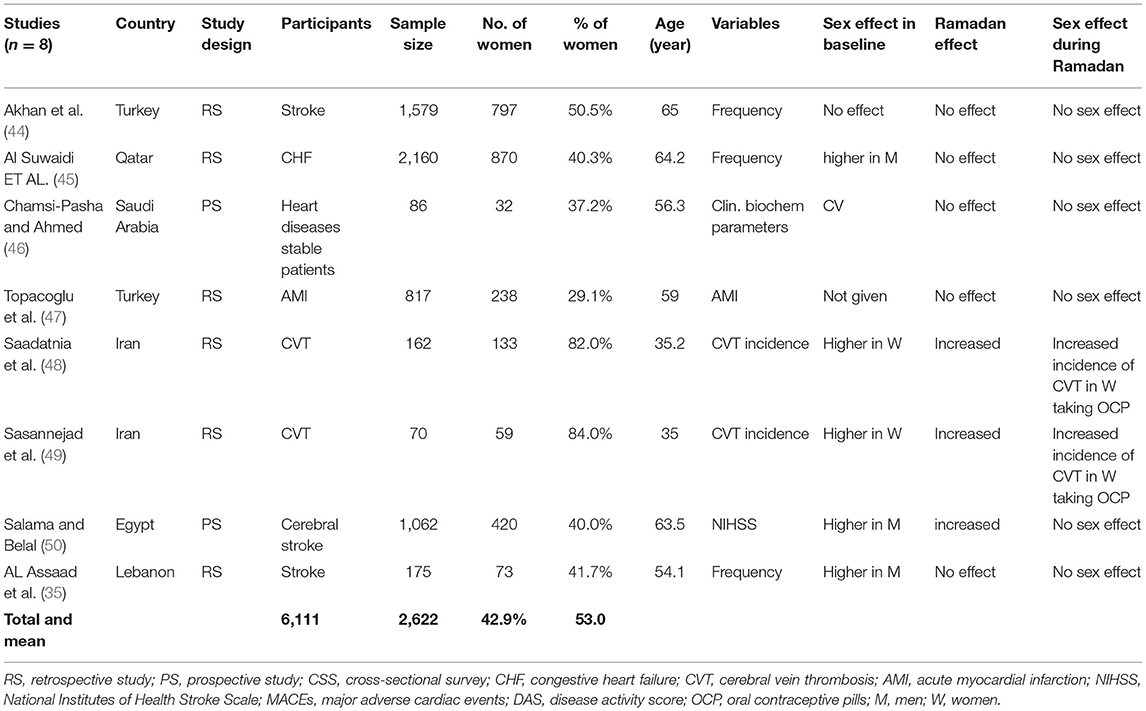
Table 5. Sex differences in outcomes related to cardiovascular diseases in patients during and outside the month of Ramadan.
No sex effect was reported during Ramadan for the incidence of stroke, CHF, Acute Myocardial Infarction, or MACEs, except the incidence of CVT which was reported to be significantly higher for fasting women, especially in women taking oral contraceptive pills (48, 49).
Sex Factor in Gastrointestinal Diseases During Ramadan
A total of eight papers with 5,409 patients of which 32.5% were women have reported statistical comparison between men and women on the frequency of GITDs (51–57). In the baseline period, sex effect was significant in most of these studies, since gastrointestinal diseases [Acute Upper Gastrointestinal Bleeding (AUGIB), Peptic Ulcer Perforation PUP, Appendicitis] were reported to be more frequent in men than women (51–58); except for acute cholecystitis disease which was higher in women (53).
During Ramadan the frequency of admission for AUGIB and PUP increased (51, 52, 54, 55, 57, 58). The sex effect during Ramadan was reported to be not significant in most of the included studies (53–56, 58). However, the study of Dönderici et al. (51), showed that female patients tended to develop more hemorrhage and perforations during Ramadan than male patients; and that of Gokakin et al. demonstrated that PUP increased in women only during Ramadan (55). On the others hand, surgery (52) and admission (57) for PUP increased in men only (Table 6).
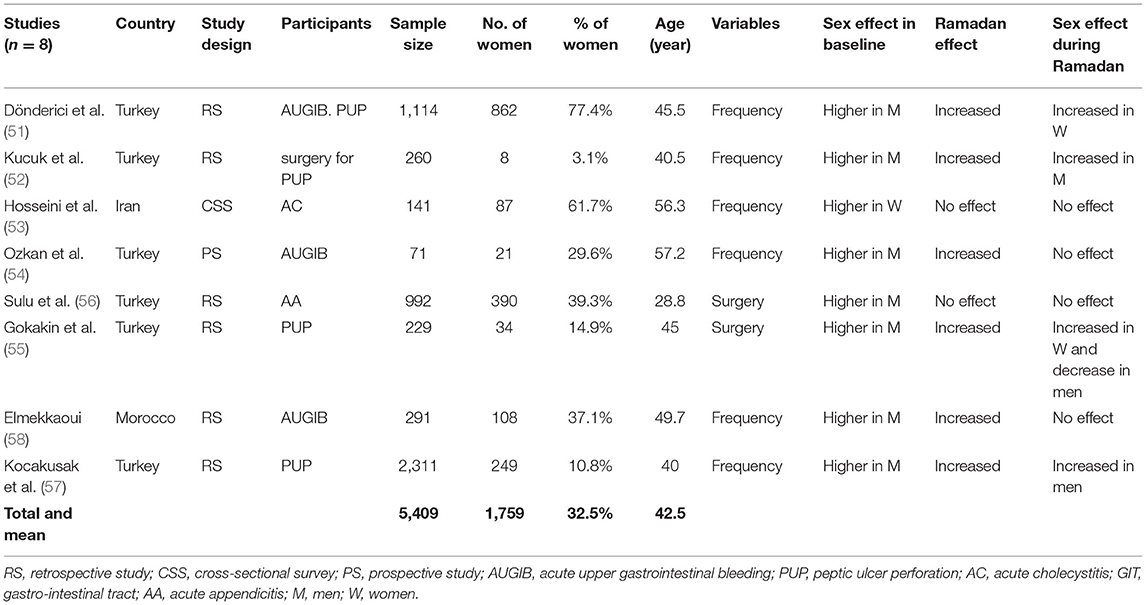
Table 6. Sex differences in outcomes related to gastrointestinal diseases in patients during and outside the month of Ramadan.
Sex Factor in Headache During Ramadan
A total of six studies with 4,688 patients of which 65.2% were women have reported statistical comparison between men and women on headache. Most of these studies reported that in the baseline condition, the headache was more frequent in women (35, 47, 59–61) and that RF was a triggering factor for headache (47, 59–61). The sex effect during Ramadan was reported to be not significant in most of these studies (35, 47, 59–61); except for one study realized in Qatar which reported an increase in headache in men during Ramadan (Table 7). Only one study showed that headaches increase during Ramadan in men only (62).
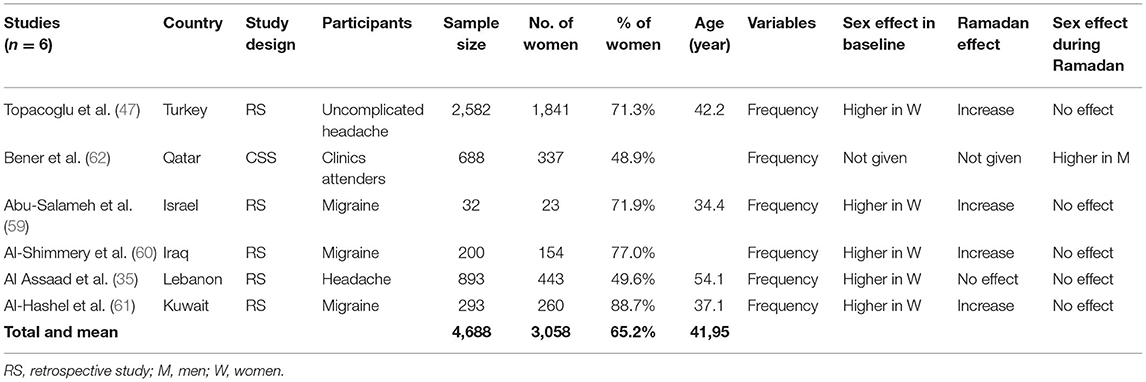
Table 7. Sex differences in the frequencies of Headache in patients during and outside the month of Ramadan.
Sex Factor in Epilepsy Frequency During Ramadan
Only four studies including 686 patients of which 47.7% were women have reported statistical comparison between men and women on epilepsy (35, 63–65). The comparison between men and women was not given in three studies epilepsy (35, 63–65), and only one study showed that the frequency of epilepsy was not different in men and women in the period outside Ramadan (35). During Ramadan, the four studies reported no significant differences between men and women in the risk of developing epileptic seizures or seizures frequencies during RF (Table 8).
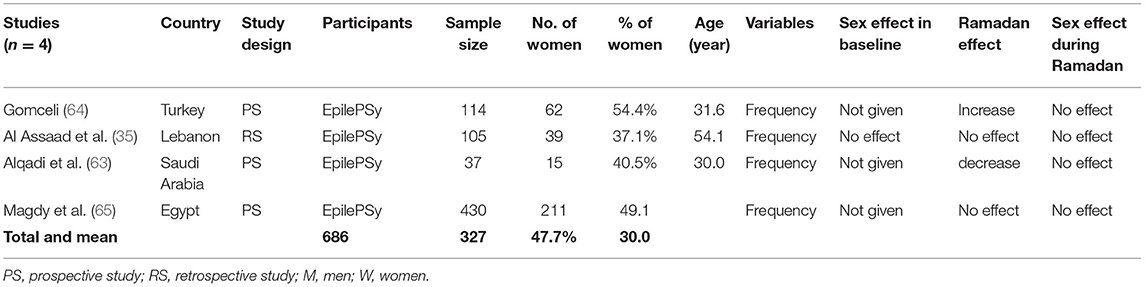
Table 8. Sex differences in the frequencies of epilepsy in patients during and outside the month of Ramadan.
Discussion
This systematic review included 38 studies reporting sex-based outcomes during Ramadan month, with primary data from 25,023 patients fasting and with one of these pathologies: diabetes, renal diseases, GITDs, CVD, headaches, and epilepsy, and of whom 44.4% were women. Of the total number of studies (n = 381), only 38 studies (10.0%) reported results in men and women separately or reported sex-based comparison during RF. This percentage was lower for the studies on Ramadan and diabetes (4%) (Figure 2).
Sex-based differences during Ramadan was reported by 18 studies for several variables such as BMI (28, 31), blood glucose (36) frequency of hypoglycemia (34), frequency of fasting (36), in patients with diabetes; renal colic (35, 39, 40, 43), mortality, thrombosis (48, 49), AUGIB and peptic ulcer perforation (51, 52, 57, 66). However, 21 studies reported that the sex factor was not associated with the effect of RF in diabetes (28–30, 32), renal diseases (38, 41, 42), CVD (44–46, 50, 67) GITDs (53–58), headache and epilepsy (59–61, 63–65, 67). Most of these differences between men and women were not specific to RF because they were also reported in the baseline period. Indeed, during the period outside Ramadan, the frequency of renal colic, CHF, stroke, GITDs diseases were higher in men; while BMI, CVT, and headache were higher in women.
Some methodological aspects must be considered when interpreting the results of these studies. First, we included studies that showed results in men and women separately, even though the sex effect was not analyzed directly for observers of RF. Only 25 studies reported direct sex-based comparison during Ramadan.
Second, we could not give a quantitative summary of evidence substantiating the association between the fasting effects and the sex factor, as there were limited available quantitative data based on sex comparison. Additionally, most of the included studies did not mention “sex” or “gender” as a factor in the title or the objective of the study. Only one article specified sex differences in the title (33) but the sex aspect was not mentioned in the introduction and as one of the study objectives. In one study, only “women” was mentioned in the title even though both men and women were included in the study (49). Finally, we excluded the studies that compared fasting patients with non-fasting patients during given days in Ramadan, because, in this protocol, patients in the two groups did not have the same characteristics in the period before Ramadan. For example, in four studies (68–71) the fasting group and the non-fasting group did not have the same age; and in one study they did not have the same comorbidity status (72) which could bias the RF effects. We also excluded the studies comparing data before and after Ramadan without providing outcomes during the month of Ramadan (22, 73) because changes recorded several weeks after Ramadan could be different than changes assessed during Ramadan.
Additional methodological challenging issue during Ramadan is related to the disparity in the number of fasting days for men and women. According to Muslim rules, menstruating women cannot fast during Ramadan and up to 40 days following childbirth. Also, women are allowed not to fast during pregnancy and lactation. This implies that women have fewer fasting days in comparison to men. The length of fasting is 23–25 days in women and 29–30 days in men (7). This disparity could represent a challenge for researchers since they have to take into consideration the number of fasting days during Ramadan to compare disease outcomes. Despite this challenge, sex-based research in Ramadan is needed.
Regarding the sex factor in diabetes outcome, several large studies and systematics reviews showed that many aspects of energy balance and glucose metabolism are regulated differently in males and females and influence their predisposition to type 2 diabetes (74). In the non-diabetic population, men had higher fasting plasma glucose and HbA1c levels than women (75). In patients with Type 2 diabetes, women had greater reductions in BG, and higher annual rates of severe hypoglycemia than men (76). Moreover, in a study using data from 751 studies including 4,372,000 adults from 146 countries, diabetes was reported to be more prevalent in men than in women, with higher prevalence in the Middle East and North Africa in comparison to western countries (77). In a recent review about metabolic health in the Middle East and North Africa, it was reported that Middle Eastern and North African women have the highest risk of metabolic diseases compared to women globally (78).
RF would be acceptable for patients with well-balanced diabetes who are conscious of their disease and compliant with their diet and drug intake, especially in patients who had received focused individualized diabetic education sessions and antidiabetic medications adjustment before and after Ramadan (9, 26, 79, 80). However, an increase in hypoglycemia attacks during Ramadan was reported (25, 34, 36).
During Ramadan, BMI and body weight decreased in men and increased in women, BG decreased and hypoglycaemia increased in women only. Differences between men and women in knowledge, attitude, and practice may explain part of these results during Ramadan. It has been shown that more women than men broke the fast in relation to diabetes concerns (81, 82). Additionally, women changed their medications during Ramadan (81) and have lower drug adherence than men, especially for high-cost drugs (83).
As in diabetes, kidney dysfunction was also shown to be influenced by the sex factor, and the female sex is shown to be reno-protective (84–86). Estrogen hormones could play a key role in this protective effect. A recent review reported that experimental and clinical studies have shown that targeting estrogen signaling pathways might have protective effects against certain renal disorders (87). Despite this protection of females against the initiation of kidney disease, the progression of multiple nephropathies displays the worst outcomes amongst female patients, in comparison to men (88). A large study that assessed dialysis outcomes in the Human Mortality Database with 206,374 patients receiving hemodialysis from 12 countries have demonstrated that fewer women than men were undergoing hemodialysis treatment and that the survival advantage that women have over men in the general population was markedly diminished in hemodialysis patients (89). In the present review, most of the studies also reported that renal diseases were more frequent in men before and during Ramadan. Two studies (40, 42) reported that fewer women (42.6 and 44.8%) received hemodialysis in the baseline period. The study by Imtiaz et al. (40) reported that the mortality rate increased in hemodialysis patients during Ramadan (10.5% during Ramadan vs. 6.9%−9.5% outside Ramadan), with more female patients undergoing hemodialysis that die (53%) during Ramadan. But, this study did not report a direct sex-based comparison of mortality during Ramadan. Additionally, data from different countries reported that the likelihood of women being registered on transplant waiting lists is less than men (90); and therefore, they are less likely to receive organ transplants. Still, the relationship between mortality in hemodialysis female patients and health service access needs to be more studied.
The prevalence of CVD was known to be higher in men (91). Recently, the sex-based differences in stroke have been questioned, as some controversial results were obtained in clinical and population studies. It was reported that women are more affected by stroke, exhibiting higher mortality and disability rates post-stroke than men. Also, the incidence of strokes rises in young women (92). In this review, the incidence and frequency of CVD did not change during Ramadan, except for CVT incidence, which increased. Jahrami et al. (12), reported in a recent meta-analysis that RF may confer short-term transient protection against CVD among healthy people. Another review concluded that studies on RF in patients with cardiac disease are sparse, observational, of small sample size, and have short follow-ups (93). No sex effect was reported during Ramadan for the incidence of stroke, CHF, Acute Myocardial Infarction, or MACEs. However, the incidence of CVT was higher for fasting women taking oral contraceptive pills. According to Ghiasian Jahrami et al. (94), women in Moslem countries use OCPs to delay their menstruation and postpone their period during Ramadan, which will allow them to observe the fasting during the entire month. This last study showed also that fasting in patients with CVT using OCPs causes a significant increase in the focal neurological deficit and hemorrhage (94). Dehydration during Ramadan dehydration was the most common risk factor for CVT among fasting women (95).
As in diabetes, renal, and CVD, sex-based differences in GITDs, such as gastro-esophageal reflux and peptic ulcer diseases are reported by several large studies and were more frequent in men (96, 97). It is important to mention that these differences were found mainly among young men and young women. In postmenopausal women, the prevalence of GITDs increases more rapidly in women than men so the prevalence in elderly patients is similar in both sexes or greater in women (97, 98). In the same way, Ye et al. (99) demonstrated that the integrity of the esophageal mucosa is more fragile in males than in females; and that the esophageal mucosal barrier attenuates more rapidly with increasing age in females than in males. These findings suggest that exposure to estrogen during the reproductive years in women protects them from the onset of several GITDs (98).
In this review, in the baseline condition, and as it was described in the literature, AUGIB and PUP were more frequent in men than women, except for acute cholecystitis which was higher in women. During Ramadan, GITDs increased. The study of Iraki et al. (100) suggested that the modifications of feeding and sleeping schedule during Ramadan induced a decrease in gastric pH, and could be a risk factor for the duodenal ulcer. The results related to the differences between men and women during Ramadan were controversial. The study of Dönderici et al., and that of Gokakin et al. showed that the AUGIB and the PUP increased more in fasting women while the finding of Kucuk and Kocakusak showed an increase in fasting men for the PUP. In these two studies, the mean age of the population was younger than in the studies by Dönderici et al., and Gokakin. Age was demonstrated to be an important factor in sex-based differences in several diseases. For this reason, it is important to take into consideration the age factor while comparing outcomes in men and women during Ramadan.
Regarding Headache, in the period outside Ramadan, the headache was more frequent in women. In a recent large study, migraine and severe headaches were considered by authors serious public health issues, In 2018, the prevalence was 15.9% across all adults, with women more affected than men (21% of women and 10.7% of men) (101). In a recent review, migraine over the life course occurs in women three to four times more often than in men (102). As in diabetes and renal diseases, estrogen fluctuation was thought to be involved in the explanation of the disparity in migraine between men and women (102).
During Ramadan, headaches and migraine increased in both men and women. The mechanisms triggering or worsening headaches during fasting are still hypothetical. One of the hypotheses is related to the change in the circadian rhythms of food intake and the oxidative state. Both fasting and eating a large meal could disturb the homeostatic state. Several studies reported that meal skipping might be one of the major causes of headaches and that minimizing daily blood glucose fluctuations might help prevent migraines and headaches (103–105). In the review of Torelli Jahrami et al., hypoglycemia and caffeine withdrawal have been especially implicated as causative factors in headache during fasting. The study of Bener et al. reported that the frequency of headaches increased only in men (62). The coffee and tobacco privation during Ramadan daytime may explain part of these specific increases in headache in fasting men since smoking is more frequent in men than in women in Moslem countries (106, 107).
During Ramadan, noting that little progress has been made in the reporting differences between men and women with diseases, it is hazardous to make any conclusion about the sex-related differences during fasting. It is important to emphasize that any sex based changes in health outcomes during RF may be confounded by other factors such as lifestyle, knowledge, attitude, practice, health access, etc.
Conclusion
Currently, small attention is paid to sex as a determinant factor in patients while fasting during Ramadan. There appeared to be differences in the frequency and incidence of diseases in men and women during Ramadan. The results should be interpreted with caution as only a few studies reported results for men and women separately. The authors suggest that closer attention to sex differences regarding the frequency and the progression of the diseases may help to improve the quality of the study and the patient care, especially to benefit those patients willing to fast during Ramadan.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
RR and MF jointly developed the research questions and the research methods for the review. RR, NA, and DA selected studies from the title and abstract and reviewed the full text of the relevant articles. RR and NA made the data extraction. RR was a major contributor to writing the manuscript and MF provides edits. All authors contributed to the final versions of the manuscript, read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We Thank Roky Meryem for her assistance in English editing on this manuscript.
Abbreviations
AUGIB, acute upper gastrointestinal bleeding; BG, blood glucose; BMI, body mass index; CHF, congestive heart failure; CKD, chronic kidney disease; CVD, cardiovascular diseases; CVT, cerebral vein thrombosis; GITDs, gastro-intestinal tract diseases; HbA1c, glycated hemoglobin A1c; MACEs, major adverse cardiac events; PUP, peptic ulcer perforation; RF, Ramadan fasting.
References
1. Shansky RM, Murphy AZ. Considering sex as a biological variable will require a global shift in science culture. Nat Neurosci. (2021) 24:457–64. doi: 10.1038/s41593-021-00806-8
2. Tannenbaum C, Schwarz JM, Clayton JA, de Vries GJ, Sullivan C. Evaluating sex as a biological variable in preclinical research: the devil in the details. Biol Sex Differ. (2016) 7:13. doi: 10.1186/s13293-016-0066-x
3. Arnegard ME, Whitten LA, Hunter C, Clayton JA. Sex as a biological variable: a 5-year progress report and call to action. J Womens Health. (2020) 29:858–64. doi: 10.1089/jwh.2019.8247
4. Geller SE, Koch A, Pellettieri B, Carnes M. Inclusion, analysis, and reporting of sex and race/ethnicity in clinical trials: have we made progress? J Womens Health. (2011) 20:315–20. doi: 10.1089/jwh.2010.2469
5. Heidari S, Babor TF, De Castro P, Tort S, Curno M. Sex and gender equity in research: rationale for the sager guidelines and recommended use. Res Integr Peer Rev. (2016) 1:2. doi: 10.1186/s41073-016-0007-6
6. Alahmad G, Al-Jumah M, Dierickx K. Review of national research ethics regulations and guidelines in Middle Eastern Arab countries. BMC Med Ethics. (2012) 13:34. doi: 10.1186/1472-6939-13-34
7. Faris ME, Hussein RN, Al-Kurd RA, Al-Fararjeh MA, Bustanji YK, Mohammad MK. Impact of ramadan intermittent fasting on oxidative stress measured by urinary 15-f(2t)-isoprostane. J Nutr Metab. (2012) 2012:802924. doi: 10.1155/2012/802924
8. Jahrami HA, Alsibai J, Clark CCT, Faris ME. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur J Nutr. (2020) 59:2291–316. doi: 10.1007/s00394-020-02216-1
9. Faris ME, Jahrami HA, Alsibai J, Obaideen AA. Impact of Ramadan diurnal intermittent fasting on the metabolic syndrome components in healthy, non-athletic Muslim people aged over 15 years: a systematic review and meta-analysis. Br J Nutr. (2020) 123:1–22. doi: 10.1017/S000711451900254X
10. Faris ME, Jahrami H, BaHammam A, Kalaji Z, Madkour M, Hassanein M, et al. systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res Clin Pract. (2020) 165:108226. doi: 10.1016/j.diabres.2020.108226
11. Faris ME, Jahrami H, Abdelrahim D, Bragazzi N, BaHammam A. The effects of Ramadan intermittent fasting on liver function in healthy adults: a systematic review, meta-analysis, and meta-regression. Diabetes Res Clin Pract. (2021) 178:108951. doi: 10.1016/j.diabres.2021.108951
12. Jahrami HA, Faris ME, I Janahi A, I Janahi M, Abdelrahim DN, Madkour MI, et al. Does four-week consecutive, dawn-to-sunset intermittent fasting during Ramadan affect cardiometabolic risk factors in healthy adults? A systematic review, meta-analysis, and meta-regression. Nutr Metab Cardiovasc Dis. (2021) 31:2273–301. doi: 10.1016/j.numecd.2021.05.002
13. Roky R, Houti I, Moussamih S, Qotbi S, Aadil N. Physiological and chronobiological changes during Ramadan intermittent fasting. Ann Nutr Metab. (2004) 48:296–303. doi: 10.1159/000081076
14. BaHammam AS, Almeneessier AS. Recent evidence on the impact of ramadan diurnal intermittent fasting, mealtime, and circadian rhythm on cardiometabolic risk: a review. Front Nutr. (2020) 7:28. doi: 10.3389/fnut.2020.00028
15. Adlouni A, Ghalim N, Saïle R, Hda N, Parra HJ, Benslimane A. Beneficial effect on serum apo AI, apo B and Lp AI levels of Ramadan fasting. Clin Chim Acta Int J Clin Chem. (1998) 271:179–89. doi: 10.1016/S0009-8981(97)00245-3
16. Mirmiran P, Bahadoran Z, Gaeini Z, Moslehi N, Azizi F. Effects of Ramadan intermittent fasting on lipid and lipoprotein parameters: An updated meta-analysis. Nutr Metab Cardiovasc Dis. (2019) 29:906–15. doi: 10.1016/j.numecd.2019.05.056
17. Prasetya G, Sapwarobol S. Intermittent fasting during Ramadan improves insulin sensitivity and anthropometric parameters in healthy young Muslim men. Am J Lifestyle Med. (2021) 15:200–6. doi: 10.1177/1559827618815430
18. Faris ME, Jahrami HA, Alhayki FA, Alkhawaja NA, Ali AM, Aljeeb SH, et al. Effect of diurnal fasting on sleep during Ramadan: a systematic review and meta-analysis. Sleep Breath Schlaf Atm. (2020) 24:771–82. doi: 10.1007/s11325-019-01986-1
19. Roky R, Iraki L, HajKhlifa R, Lakhdar Ghazal N, Hakkou F. Daytime alertness, mood, psychomotor performances, and oral temperature during Ramadan intermittent fasting. Ann Nutr Metab. (2000) 44:101–7. doi: 10.1159/000012830
20. Roky R, Chapotot F, Hakkou F, Benchekroun MT, Buguet A. Sleep during Ramadan intermittent fasting. J Sleep Res. (2001) 10:319–27. doi: 10.1046/j.1365-2869.2001.00269.x
21. Bahammam AS, Almushailhi K, Pandi-Perumal SR, Sharif MM. Intermittent fasting during Ramadan: does it affect sleep? J Sleep Res. (2014) 23:35–43. doi: 10.1111/jsr.12076
22. Dabbous Z, Bashir M, Elzouki A-N, Ahmed MS, Farouk S, Hassanien M, et al. Differential effects of gender and patient background diversity on the changes in metabolic and biophysical profiles in people with type-2 diabetes from different ethnicities who fast during Ramadan (H1439); a prospective study from Qatar. Diabetes Res Clin Pract. (2019) 152:171–6. doi: 10.1016/j.diabres.2019.03.032
23. Husain R, Duncan MT, Cheah SH, Ch'ng SL. Effects of fasting in Ramadan on tropical Asiatic Moslems. Br J Nutr. (1987) 58:41–8. doi: 10.1079/BJN19870067
24. Sajid KM, Akhtar M, Malik GQ. Ramadan fasting and thyroid hormone profile. J Pak Med Assoc. (1991) 41:213–6.
25. Salti I. Efficacy and safety of insulin glargine and glimepiride in subjects with Type 2 diabetes before, during and after the period of fasting in Ramadan. Diabet Med J Br Diabet Assoc. (2009) 26:1255–61. doi: 10.1111/j.1464-5491.2009.02836.x
26. Abdelrahim D, Faris ME, Hassanein M, Shakir AZ, Yusuf AM, Almeneessier AS, et al. Impact of Ramadan diurnal intermittent fasting on hypoglycemic events in patients with type 2 diabetes: a systematic review of randomized controlled trials and observational studies. Front Endocrinol. (2021) 12:624423. doi: 10.3389/fendo.2021.624423
27. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
28. Yarahmadi S, Larijani B, Bastanhagh MH, Pajouhi M, Baradar Jalili R, Zahedi F, et al. Metabolic and clinical effects of Ramadan fasting in patients with type II diabetes. J Coll Physicians Surg Pak. (2003) 13:329–32.
29. M'guil M, Ragala MA, El Guessabi L, Fellat S, Chraibi A, Chabraoui L, et al. Is Ramadan fasting safe in type 2 diabetic patients in view of the lack of significant effect of fasting on clinical and biochemical parameters, blood pressure, and glycemic control? Clin Exp Hypertens. (2008) 30:339–57. doi: 10.1080/10641960802272442
30. Elmehdawi R, Ehmida M, Elmagrehi H. Incidence of diabetic ketoacidosis during Ramadan fasting in Benghazi-Libya. Oman Med J. (2009) 24:99–102. doi: 10.5001/omj.2009.23
31. Traoré M, Galibois I, Lemieux S. Influence du jeûne du Ramadan sur les sensations d'appétit chez des musulmans diabétiques de type 2 au Mali. Appl Physiol Nutr Metab. (2013) 38:795–801. doi: 10.1139/apnm-2012-0337
32. Bener A, Yousafzai MT. Effect of Ramadan fasting on diabetes mellitus: a population-based study in Qatar. J Egypt Public Health Assoc. (2014) 89:47–52. doi: 10.1097/01.EPX.0000451852.92252.9b
33. Yeoh ECK, Zainudin SB, Loh WN, Chua CL, Fun S, Subramaniam T, et al. Fasting during Ramadan and associated changes in glycaemia, caloric intake and body composition with gender differences in Singapore. Ann Acad Med Singap. (2015) 44:202–6.
34. AlKhaldi YM, AlKhaldi AY, AlQahtani AS, Al-Shahrani BS, Meshawi EA, Albishri BM. Incidence of hypoglycemia and its risk factors among diabetics during Ramadan in Abha city, Aseer Region, KSA. J Fam Med Prim Care. (2019) 8:2793–8. doi: 10.4103/jfmpc.jfmpc_250_19
35. Al Assaad RG, Bachir R, El Sayed MJ. Impact of Ramadan on emergency department visits and on medical emergencies. Eur J Emerg Med. (2018) 25:440–4. doi: 10.1097/MEJ.0000000000000485
36. Abid M, Hsairi M, Elleuch M, Ben Aissa E. Survey on diabetic patients treated with insulin during the fasting month of Ramadan. Int J Gen Med. (2018) 11:33–40. doi: 10.2147/IJGM.S131308
37. Zaghlol LY, Beirat AF, Amarin JZ, Hassoun Al Najar AM, Hasan YY, Qtaishat A, et al. Effect of dosage reduction of hypoglycemic multidrug regimens on the incidences of acute glycemic complications in people with type 2 diabetes who fast during Rama?ān: a randomized controlled trial. Front Endocrinol. (2021) 12:613826. doi: 10.3389/fendo.2021.613826
38. NasrAllah MM, Osman NA. Fasting during the month of Ramadan among patients with chronic kidney disease: renal and cardiovascular outcomes. Clin Kidney J. (2014) 7:348–53. doi: 10.1093/ckj/sfu046
39. Basiri A, Moghaddam SMMH, Khoddam R, Nejad ST, Hakimi A. Monthly variations of urinary stone colic in Iran and its relationship to the fasting month of Ramadan. J Pak Med Assoc. (2004) 54:6–8.
40. Imtiaz S, Nasir K, Dhrolia MF, Hussain M, Abbas HN, Ahmad A. Mortality trend among hemodialysis patients during the Islamic month of Ramadan: a 24 years retrospective study. J Coll Physicians Surg Pak. (2015) 25:189–92.
41. Al Mahayni AO, Alkhateeb SS, Abusaq IH, Al Mufarrih AA, Jaafari MI, Bawazir AA. Does fasting in Ramadan increase the risk of developing urinary stones? Saudi Med J. (2018) 39:481–6. doi: 10.15537/smj.2018.5.22160
42. Adanan NIH, Md Ali MS, Lim JH, Zakaria NF, Lim CTS, Yahya R, et al. Investigating physical and nutritional changes during prolonged intermittent fasting in hemodialysis patients: a Prospective Cohort Study. J Ren Nutr. (2020) 30:e15–26. doi: 10.1053/j.jrn.2019.06.003
43. Mustafa MN, Al-Omran AJ, Raees AA. Frequency of renal colic during the month of Ramadan. Bahrain Med Bull. (2020) 42:3.
44. Akhan G, Kutluhan S, Koyuncuoglu HR. Is there any change of stroke incidence during Ramadan? Acta Neurol Scand. (2000) 101:259–61. doi: 10.1034/j.1600-0404.2000.101004259.x
45. Al Suwaidi J, Bener A, Hajar HA, Numan MT. Does hospitalization for congestive heart failure occur more frequently in Ramadan: a population-based study (1991-2001). Int J Cardiol. (2004) 96:217–21. doi: 10.1016/j.ijcard.2003.06.018
46. Chamsi-Pasha H, Ahmed WH. The effect of fasting in Ramadan on patients with heart disease. Saudi Med J. (2004) 25:47-51.
47. Topacoglu H, Karcioglu O, Yuruktumen A, Kiran S, Cimrin AH, Ozucelik DN, et al. Impact of Ramadan on demographics and frequencies of disease-related visits in the emergency department. Int J Clin Pract. (2005) 59:900–5. doi: 10.1111/j.1742-1241.2005.00460.x
48. Saadatnia M, Zare M, Fatehi F, Ahmadi A. The effect of fasting on cerebral venous and dural sinus thrombosis. Neurol Res. (2009) 31:794–8. doi: 10.1179/016164109X12445505689481
49. Sasannejad P, Mellat Ardekani A, Velayati A, Shoeibi A, Saeidi M, Foroughipour M, et al. Cerebral vein thrombosis in women using short course oral contraceptive consumption. Iran J Reprod Med. (2012) 10:537–42.
50. Salama H, Belal T. Is There any consequence of Ramadan fasting on acute cerebral stroke? Egypt J Neurol Psychiat Neurosurg. (2014) 51:333–6.
51. Dönderici O, Temizhan A, Küçükbaş T, Eskioglu E. Effect of Ramadan on peptic ulcer complications. Scand J Gastroenterol. (1994) 29:603–6. doi: 10.3109/00365529409092479
52. Kucuk HF, Censur Z, Kurt N, Ozkan Z, Kement M, Kaptanoglu L, et al. The effect of Ramadan fasting on duodenal ulcer perforation: a retrospective analysis - ProQuest. Indian J Surg. (2005) 67:195–8.
53. Hosseini SV, Torabijahromi M, Mosallaei M, Sabet B, Pourahmad S. The effect of season and Ramadan fasting on the onset of acute cholecystitis. Saudi Med J. (2006) 27:503–6.
54. Ozkan S, Durukan P, Akdur O, Vardar A, Torun E, Ikizceli I. Does Ramadan fasting increase acute upper gastrointestinal haemorrhage? J Int Med Res. (2009) 37:1988–93. doi: 10.1177/147323000903700637
55. Gökakin AK, Kurt A, Atabey M, Koyuncu A, Topçu O, Aydin C, et al. The impact of Ramadan on peptic ulcer perforation. Ulus Travma Ve Acil Cerrahi Derg. (2012) 18:339–43. doi: 10.5505/tjtes.2012.61257
56. Sulu B, Gunerhan Y, Ozturk B, Arslan H. Is long-term hunger (Ramadan model) a risk factor for acute appendicitis? Saudi Med J. (2010) 31:59–63.
57. Kocakusak A. Does Ramadan fasting contribute to the increase of peptic ulcer perforations? Eur Rev Med Pharmacol Sci. (2017) 21:150–4.
58. Amine EM, Kaoutar S, Ihssane M, Adil I, Dafr-Allah B. Effect of Ramadan fasting on acute upper gastrointestinal bleeding. J Res Med Sci. (2013) 18:230–3.
59. Abu-Salameh I, Plakht Y, Ifergane G. Migraine exacerbation during Ramadan fasting. J Headache Pain. (2010) 11:513–7. doi: 10.1007/s10194-010-0242-z
60. Al-Shimmery EK. Precipitating and relieving factors of migraine headache in 200 Iraqi Kurdish patients. Oman Med J. (2010) 25:212–7. doi: 10.5001/omj.2010.59
61. Al-Hashel JY, Abokalawa F, Toma R, Algubari A, Ahmed SF. Worsening of migraine headache with fasting Ramadan. Clin Neurol Neurosurg. (2021) 209:106899. doi: 10.1016/j.clineuro.2021.106899
62. Bener Abdulbari, Azhar A, Bessisso M. Do fasting and life style eating habits in Ramadan affect headache? Nutr Food Sci. (2007) 37:427–3. doi: 10.1108/00346650710838081
63. Alqadi K, Alghamdi O, Babtain F., Ba'arma H, Bajammal S, Albalawi M, et al. Effects of fasting during Ramadan on seizure control and quality of life in patients with epilepsy. Epilepsy Behav. (2020) 112:107440. doi: 10.1016/j.yebeh.2020.107440
64. Gomceli YB, Kutlu G, Cavdar L, Inan LE. Does the seizure frequency increase in Ramadan? Seizure. (2008) 17:671–6. doi: 10.1016/j.seizure.2008.03.008
65. Magdy R, Kishk NA, Abokrysha NT, Ramzy GM, Rizk HI, Hussein M. Predictors of successful Ramadan fasting in Muslim patients with epilepsy: a prospective study. Seizure. (2020) 80:67–70. doi: 10.1016/j.seizure.2020.04.012
66. Gokakin AK, Kurt A, Akgol G, Karakus BC, Atabey M, Koyuncu A, et al. Effects of Ramadan fasting on peptic ulcer disease as diagnosed by upper gastrointestinal endoscopy. Arab J Gastroenterol. (2012) 13:180–3. doi: 10.1016/j.ajg.2012.12.002
67. Assaad Khalil S, Gaber Amin N, Mohamed Ibrahim A, Zakaria Zaky D, Mounir Bishay M. Glycemic indices of dates “Ramadan Symbolic Food” in patients with type 2 diabetes using continuous glucose monitoring system. Diabetes Res Clin Pract. (2021) 172:108563. doi: 10.1016/j.diabres.2020.108563
68. Emami MH, Rahimi H. Effects of Ramadan fasting on acute upper gastrointestinal bleeding due to peptic ulcer. J Res Med Sci. (2006) 11:6.
69. Rahman MdO, Islam M. Association between fasting of Ramadan and risk factors of diabetes: a study from Rajshahi City in Bangladesh. Adv J Food Sci Technol. (2011) 3:360–5.
70. Alshamsi S, Binsaleh F, Hejaili F, Karkar A, Moussa D, Raza H, et al. Changes in biochemical, hemodynamic, and dialysis adherence parameters in hemodialysis patients during Ramadan. Hemodial Int. (2016) 20:270–6. doi: 10.1111/hdi.12369
71. Siddique S, Imran Y, Afzal MN, Malik U. Effect of Ramadan fasting on disease activity in patients with rheumatoid arthritis presenting in tertiary care hospital. Pak J Med Sci. (2020) 36:1032–5. doi: 10.12669/pjms.36.5.2099
72. Khazneh E, Qaddumi J, Hamdan Z, Qudaimat F, Sbitany A, Jebrin K, et al. The effects of Ramadan fasting on clinical and biochemical markers among hemodialysis patients: a prospective cohort study. PLoS ONE. (2019) 14:e0218745. doi: 10.1371/journal.pone.0218745
73. Elhadd T, Dabbous Z, Bashir M, Elzouki A, Ghadban W, Baagar K, et al. Incidence of hypoglycaemia in patients with type-2 diabetes taking multiple glucose lowering therapies during Ramadan: the PROFAST Ramadan Study. J Diabetes Metab Disord. (2018) 17:309–14. doi: 10.1007/s40200-018-0374-2
74. Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal J-F, Montagner A, et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. (2020) 63:453–61. doi: 10.1007/s00125-019-05040-3
75. Faerch K, Borch-Johnsen K, Vaag A, Jørgensen T, Witte DR. Sex differences in glucose levels: a consequence of physiology or methodological convenience? The Inter99 study. Diabetologia. (2010) 53:858–65. doi: 10.1007/s00125-010-1673-4
76. McGill JB, Vlajnic A, Knutsen PG, Recklein C, Rimler M, Fisher SJ. Effect of gender on treatment outcomes in type 2 diabetes mellitus. Diabetes Res Clin Pract. (2013) 102:167–74. doi: 10.1016/j.diabres.2013.10.001
77. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. Lancet. (2016) 387:1513–30. doi: 10.1016/S0140-6736(16)00618-8
78. Azizi F, Hadaegh F, Hosseinpanah F, Mirmiran P, Amouzegar A, Abdi H, et al. Metabolic health in the Middle East and North Africa. Lancet Diabetes Endocrinol. (2019) 7:866-79. doi: 10.1016/S2213-8587(19)30179-2
79. Tourkmani AM, Alharbi TJ, Bin Rsheed AM, AlRasheed AN, AlBattal SM, Abdelhay O, et al. Impact of Ramadan focused education program on medications adjustment for patients with type 2 diabetes in a primary health care institution in Saudi Arabia. Diabetes Metab Syndr. (2019) 13:161–5. doi: 10.1016/j.dsx.2018.07.012
80. Benaji B, Mounib N, Roky R, Aadil N, Houti IE, Moussamih S, et al. Diabetes and Ramadan: review of the literature. Diabetes Res Clin Pract. (2006) 73:117–25. doi: 10.1016/j.diabres.2005.10.028
81. Gelhorn HL, Boye KS, Shalhoub H, Matza LS, Jordan JB, Alhammad A, et al. Patient-reported outcomes and impact of type 2 diabetes: a cross-sectional study in the Kingdom of Saudi Arabia. Patient Prefer Adherence. (2020) 14:2231–42. doi: 10.2147/PPA.S265126
82. Tan C, Yong AML, Haji Mohamad MA, Abdul Rahman H, Naing L. Fasting in Ramadan of Muslim patients with diabetes Mellitus, and knowledge and practice in relation to diabetes control in Brunei. Diabetes Res Clin Pract. (2018) 144:171–6. doi: 10.1016/j.diabres.2018.09.004
83. AlQarni K, AlQarni EA, Naqvi AA, AlShayban DM, Ghori SA, Haseeb A, et al. Assessment of medication adherence in saudi patients with type ii diabetes Mellitus in Khobar City, Saudi Arabia. Front Pharmacol. (2019) 10:1306. doi: 10.3389/fphar.2019.01306
84. Chauhan V, Eskin B, Allegra JR, Cochrane DG. Effect of season, age, and gender on renal colic incidence. Am J Emerg Med. (2004) 22:560–3. doi: 10.1016/j.ajem.2004.08.016
85. Neugarten J, Golestaneh L. Female sex reduces the risk of hospital-associated acute kidney injury: a meta-analysis. BMC Nephrol. (2018) 19:314. doi: 10.1186/s12882-018-1122-z
86. O'Brien Z, Cass A, Cole L, Finfer S, Gallagher M, McArthur C, et al. Sex and mortality in septic severe acute kidney injury. J Crit Care. (2019) 49:70–6. doi: 10.1016/j.jcrc.2018.10.017
87. Ma H-Y, Chen S, Du Y. Estrogen and estrogen receptors in kidney diseases. Ren Fail. (2021) 43:619–42. doi: 10.1080/0886022X.2021.1901739
88. Mitchell T, De Miguel C, Gohar EY. Sex differences in redox homeostasis in renal disease. Redox Biol. (2020) 31:101489. doi: 10.1016/j.redox.2020.101489
89. Hecking M, Bieber BA, Ethier J, Kautzky-Willer A, Sunder-Plassmann G, Säemann MD, et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the Dialysis Outcomes and Practice Patterns Study (DOPPS). PLoS Med. (2014) 11:e1001750. doi: 10.1371/journal.pmed.1001750
90. Piccoli GB, Alrukhaimi M, Liu Z-H, Zakharova E, Levin A, World Kidney Day Steering Committee. Women and kidney disease: reflections on world kidney day 2018. J Ren Care. (2018) 44:3–11. doi: 10.1111/jorc.12232
91. Appelros P, Åsberg S. Sex differences in stroke. Handb Clin Neurol. (2020) 175:299-312. doi: 10.1016/B978-0-444-64123-6.00021-7
92. Thomas SA, Bashir K, Jenkins DW, Pathan SA, Thomas SH. Ramadan-associated circadian census variation in a busy middle eastern emergency department. J Ayub Med Coll Abbottabad. (2019) 31:586–92.
93. Akhtar AM, Ghouri N, Chahal CAA, Patel R, Ricci F, Sattar N, et al. Ramadan fasting: recommendations for patients with cardiovascular disease. Heart. (2021) 108:258–65. doi: 10.1136/heartjnl-2021-319273
94. Ghiasian M, Mansour M, Moradian N. Prognosis of fasting in patients with cerebral venous thrombosis using oral contraceptives. Iran J Neurol. (2019) 18:82–4. doi: 10.18502/ijnl.v18i2.1293
95. AlSheef M, Alotaibi M, Zaidi ARZ, Alshamrani A, Alhamidi A, Zaidi SZA, et al. Prevalence of cerebral venous thrombosis with the use of oral contraceptive pills during the Holy month of Ramadan. Saudi Med J. (2020) 41:1063–9. doi: 10.15537/smj.2020.10.25397
96. Menon S, Prew S, Parkes G, Evans S, Smith L, Nightingale P, et al. Do differences in female sex hormone levels contribute to gastro-oesophageal reflux disease? Eur J Gastroenterol Hepatol. (2013) 25:772–7. doi: 10.1097/MEG.0b013e32835fbaab
97. Kim YS, Lee J, Shin A, Lee JM, Park JH, Jung H-Y. A Nationwide Cohort Study shows a sex-dependent change in the trend of peptic ulcer bleeding incidence in Korea between 2006 and 2015. Gut Liver. (2021) 15:537–45. doi: 10.5009/gnl20079
98. Asanuma K, Iijima K, Shimosegawa T. Gender difference in gastro-esophageal reflux diseases. World J Gastroenterol. (2016) 22:1800–10. doi: 10.3748/wjg.v22.i5.1800
99. Ye B, Wang Y, Lin L, Jiang L, Wang M. Sex-based differences in pH Parameters and esophageal impedance of patients with gastroesophageal reflux disease. Front Med. (2021) 8:629302. doi: 10.3389/fmed.2021.629302
100. Iraki L, Bogdan A, Hakkou F, Amrani N, Abkari A, Touitou Y. Ramadan diet restrictions modify the circadian time structure in humans. A study on plasma gastrin, insulin, glucose, and calcium and on gastric pH. J Clin Endocrinol Metab. (1997) 82:1261–73. doi: 10.1210/jc.82.4.1261
101. Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: UPDATED age, sex, and socioeconomic-specific estimates from government health surveys. Headache. (2021) 61:60–8. doi: 10.1111/head.14024
102. Al-Hassany L, Haas J, Piccininni M, Kurth T, Maassen Van Den Brink A, Rohmann JL. Giving researchers a headache - sex and gender differences in Migraine. Front Neurol. (2020) 11:549038. doi: 10.3389/fneur.2020.549038
103. Hufnagl KN, Peroutka SJ. Glucose regulation in headache: implications for dietary management. Expert Rev Neurother. (2002) 2:311–7. doi: 10.1586/14737175.2.3.311
104. Peroutka SJ. Serum glucose regulation and headache. Headache. (2002) 42:303–8. doi: 10.1046/j.1526-4610.2002.02083.x
105. Torelli P, Evangelista A, Bini A, Castellini P, Lambru G, Manzoni GC. Fasting headache: a review of the literature and new hypotheses. Headache. (2009) 49:744–52. doi: 10.1111/j.1526-4610.2009.01390.x
106. Masud H, Oyebode O. Inequalities in smoking prevalence: a missed opportunity for tobacco control in Pakistan. J Public Health. (2018) 40:271–8. doi: 10.1093/pubmed/fdx044
Keywords: diabetes, renal, cardiovascular, gastrointestinal, FAST, gender, Islam
Citation: Roky R, Aadil N, Krami AM, Benaji B, Errabih I, Abdelrahim DN and Faris ME (2022) Sex as a Biological Factor in the Changes in Disease Patients During Ramadan Intermittent Fasting: A Systematic Review. Front. Nutr. 9:908674. doi: 10.3389/fnut.2022.908674
Received: 30 March 2022; Accepted: 26 May 2022;
Published: 01 July 2022.
Edited by:
Domenico Sergi, University of Ferrara, ItalyReviewed by:
Greggory Davis, University of Louisiana at Lafayette, United StatesNazim Ghouri, University of Glasgow, United Kingdom
Copyright © 2022 Roky, Aadil, Krami, Benaji, Errabih, Abdelrahim and Faris. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rachida Roky, cm9reXJhY2hpZGFAZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
 Rachida Roky
Rachida Roky Nadia Aadil2
Nadia Aadil2 Dana N. Abdelrahim
Dana N. Abdelrahim MoezAlIslam Ezzat Faris
MoezAlIslam Ezzat Faris