- 1Department of Frigidzone Medicine, College of High Altitude Military Medicine, Army Medical University (Third Military Medical University), Chongqing, China
- 2Key Laboratory of Extreme Environmental Medicine, Ministry of Education of China, Chongqing, China
- 3Key Laboratory of High Altitude Medicine, People's Liberation Army (PLA), Chongqing, China
- 4Department of Hematology, Shengjing Hospital of China Medical University, Shenyang, China
- 5Department of Clinical Epidemiology, Shengjing Hospital of China Medical University, Shenyang, China
- 6Clinical Research Center, Shengjing Hospital of China Medical University, Shenyang, China
- 7Center of Reproductive Medicine, Shengjing Hospital of China Medical University, Shenyang, China
Objective: We aimed to examine associations of diet quality scores, including the dietary approaches to stop hypertension (DASH), alternate Healthy Eating Index (AHEI), and Chinese Healthy Eating Index (CHEI) with asthenoteratozoospermia risk in China.
Methods: Among 254 cases and 633 controls in a hospital-based case–control study in Shenyang, Liaoning Province, China, DASH, AHEI, and CHEI were calculated using a validated food frequency questionnaire. Asthenotetrazoospermia was evaluated according to World Health Organization guidelines. Unconditional multiple logistic regression was used to estimate odds ratios (ORs) with 95% confidence intervals (CIs) for the association between quality diet scores and asthenoteratozoospermia risk.
Results: We found that the CHEI score was inversely associated with asthenoteratozoospermia risk, with ORs of 0.59 (95% CI 0.39, 0.88) and 0.59 (95% CI 0.39, 0.88) for the 2nd and 3rd tertiles vs. the 1st tertile, respectively (P trend < 0.05). In addition, our data indicated that each standard deviation increase in CHEI, AHEI-2010, and DASH score was associated with 19, 13, and 17% decreased risk of asthenoteratozoospermia, respectively.
Conclusion: Our findings suggest that higher adherence to the CHEI, AHEI-2010, and DASH diet quality scores may reduce the risk of asthenoteratozoospermia, especially for younger participants.
Introduction
According to the WHO estimation, fertility problems have become an increasing medical problem affecting ~60–80 million couples, and male factors account for almost 50% of cases (1). As one of the principal types, asthenoteratozoospermia is defined as low sperm vitality or even malformation (2). In addition to genetic factors, environmental factors, lifestyle habits, and dietary factors may be relevant to sperm quality (3). Epidemiological studies have reported that sweetened beverages, red meat, and organ meat consumption are negative and that fish, egg, nut, and low-fat dairy consumption are positively correlated with sperm quality (4–7).
In reality, however, individuals eat combinations of food as meals instead of a single food, which makes it difficult to distinguish their individual effects (8). To overcome this challenge, dietary patterns were used to assess the effect of overall diet on sperm quality. A meta-analysis reported that individuals with the highest adherence to the healthy dietary pattern (highly related to fruit, vegetables, tomatoes, whole grain, legumes, and fish) had a significantly higher level of sperm concentration than those who had the lowest adherence to the healthy dietary pattern (9). Given that these dietary patterns (data-driven) do not apply to another population, the diet quality scores (priori-defined) are easier to calculate and compare across studies (10).
Dietary inflammatory index (DII) scores, as one of a priori-defined score, have been reported to not be associated with asthenozoospermia risk in our previous study (11). Other priori-defined diet scores have been reported to associate with overall sperm quality, such as the Healthy Eating Index-2005 (HEI-2005), the Alternate Healthy Eating Index-2010 (AHEI-2010), and dietary approaches to stop hypertension (DASH) (1, 12, 13). Studies have shown that HEI, AHEI, and DASH diet scores were associated with better overall sperm quality in Israel (1), and adherence to the DASH diet scores was related to a higher sperm count and concentration in southern Spain and Poland (12, 13). However, it is unknown whether this association can be extrapolated to Chinese populations. In addition, the relationships between the Chinese Healthy Eating Index (CHEI), which is used to assess overall diet quality among Chinese populations (14), and overall sperm quality have been unclear.
Therefore, to explore the diet quality scores appropriated for the Chinese population that can be used as a tool to improve sperm quality, we conducted a hospital–based case–control study to investigate the associations between DASH, AHEI-2010, and CHEI diet quality scores and asthenoteratozoospermia risk in China.
Materials and Methods
Design and Population
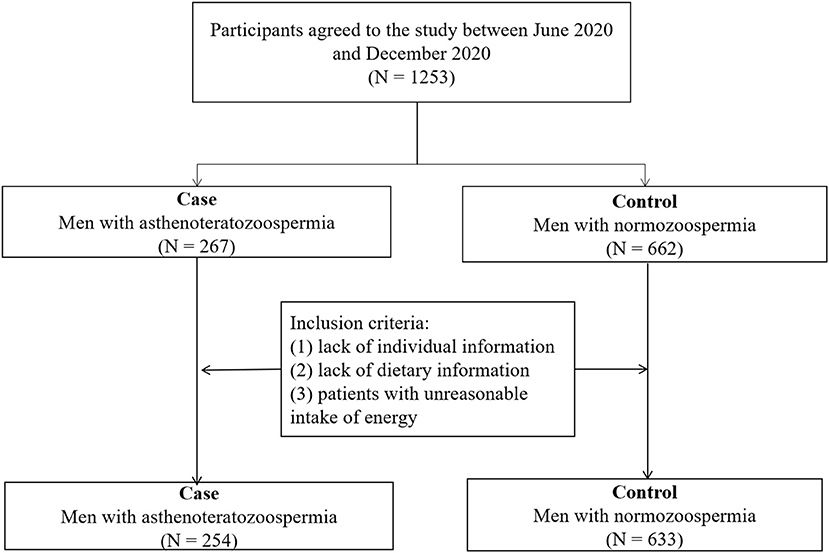
The present hospital-based case–control study was conducted to compare the diet quality scores of men with and without asthenoteratozoospermia. Study participants were men referred to the infertility clinic of Shengjing Hospital of China Medical University from June 2020 to December 2020. As shown in Figure 1, a reproductive medicine specialist diagnosed each man with asthenoteratozoospermia as a new patient (incident case) and was placed in the case group (n = 267) based on the World Health Organization (WHO) laboratory manual for the examination and processing of human semen (fifth edition, 2010) (1). Asthenoteratozoospermia is defined as the concentration and proportions of motile and morphologically normal spermatozoa below the reference values (<15 × 106 sperm/mL, <32% progressive motility, and <4% normal morphology) (1). Men with normozoospermia (n = 662) were selected as the control group and were companions of patients admitted to the same infertility clinic. Trained research interviewers administered a baseline questionnaire that included sociodemographic and dietary history for recruited men. Patients who had missing individual information or an invalid food frequency questionnaire (FFQ) were not eligible for recruitment, nor were patients with unreasonable intake of energy (<800 or >4,200 kcal/d). Two hundred fifty-four cases with asthenoteratozoospermia and 633 controls were included in the final analysis.
Ethical and research approvals were obtained from the ethics committee of Shengjing Hospital of China Medical University, with all participants providing written consent at study enrollment.
Semen Collection and Analysis
For 3–7 days of celibate, semen samples were collected without using condoms or lubricants through masturbation into a plastic tube in a dedicated room. Samples were liquefied for 60 min before analysis. Ejaculate volume, pH, sperm concentration, total count of sperm inspected, total motility, and the percentage of each motile grade of sperm were measured with WLJY9000. Flow cytometry was used to assess sperm DNA fragmentation and sperm DNA staining. After pasteurization, sperm smears were observed under an optical microscope and evaluated for morphology. The reference values of normal sperm were determined by the WHO criteria (15). External quality was controlled by experienced technicians.
Data Collection
All participants were asked to complete a self-administered, semiquantitative validated food frequency questionnaire (FFQ) that included 110 food items: they were asked how often, on average, during the previous year they had consumed each food. Estimations of energy and nutrient intakes were performed with the aid of the Chinese Food Composition Tables (16). In addition, demographic characteristics (age, education level, and household income), lifestyle (smoking, drinking, and physical activity), and other information were collected by a questionnaire. The heights and weights were collected by physical examination. After obtaining these measurements, the body mass index (BMI) was taken for each participant by dividing weight (kg) by height squared (m2).
Diet Quality Scores
We assessed 3 diet quality scores, and details are presented in Supplementary Table 1. The DASH score includes eight components: fruits, vegetables, nuts/legumes, dairy, whole grains, red meat, sugar-sweetened beverages, and sodium intake, which range from 8 to 40 (17). The AHEI-2010 score is based on vegetables (excluding potatoes), fruits, whole grains, nuts and legumes, long-chain n-3 fatty acids, polyunsaturated fatty acids, sweetened beverages and juice, red and processed meat, trans fat, sodium, and alcoholic drinks, which range from 1 to 110 (18). The CHEI score is calculated according to 12 adequacy components (total grains, whole grains and mixed beans, tubers, total vegetables, dark vegetables, fruits, dairy, soybeans, fish and seafood, seeds and nuts, poultry, and eggs) and 5 moderation components (red meat, cooking oils, sodium, added sugars, and alcohol), which range from 0 to 100 (14).
Statistical Analysis
Descriptive statistics were examined for all variables. Continuous variables are reported as the mean ± standard deviation; categorical variables are presented as numbers of participants and percentages. We conducted Student's t-tests or chi-square-tests to compare differences between groups. We created tertiles of each diet score and used unconditional logistic regression analyses to estimate odds ratios (ORs) with 95% confidence intervals (CIs) to assess associations between quality scores and asthenoteratozoospermia risk. The lowest tertile of scores was considered the reference group. A linear trend was tested by treating the median value of each tertile as a continuous variable. In addition, we alternatively assessed the risk estimates associated with a continuous measure for a 1 standard deviation (SD) increase in scores. We used three models: model 1 (adjusted for energy and age) and model 2 (adjusted for energy, age, smoking status, drinking status, household income, education level, abstinence time, and physical activity). We conducted adjusted risk estimates for asthenoteratozoospermia by CHEI, AHEI-2010 and DASH scores in subgroup analyses stratified by age, BMI, and smoking status.
All statistical analyses were performed using SAS software, version 9.3, for Windows (SAS Institute Inc., Cary, NC, USA). All reported P-values are two-sided, and those that were <0.05 were defined as statistically significant.
Results
Characteristics of the Participants
As shown in Table 1, cases were more likely to have longer abstinence times and a higher proportion of current smokers than controls. In addition, the case with asthenoteratozoospermia tended to have a lower sperm concentration, total sperm count, progressive motility, total motility and normal sperm morphology than controls.
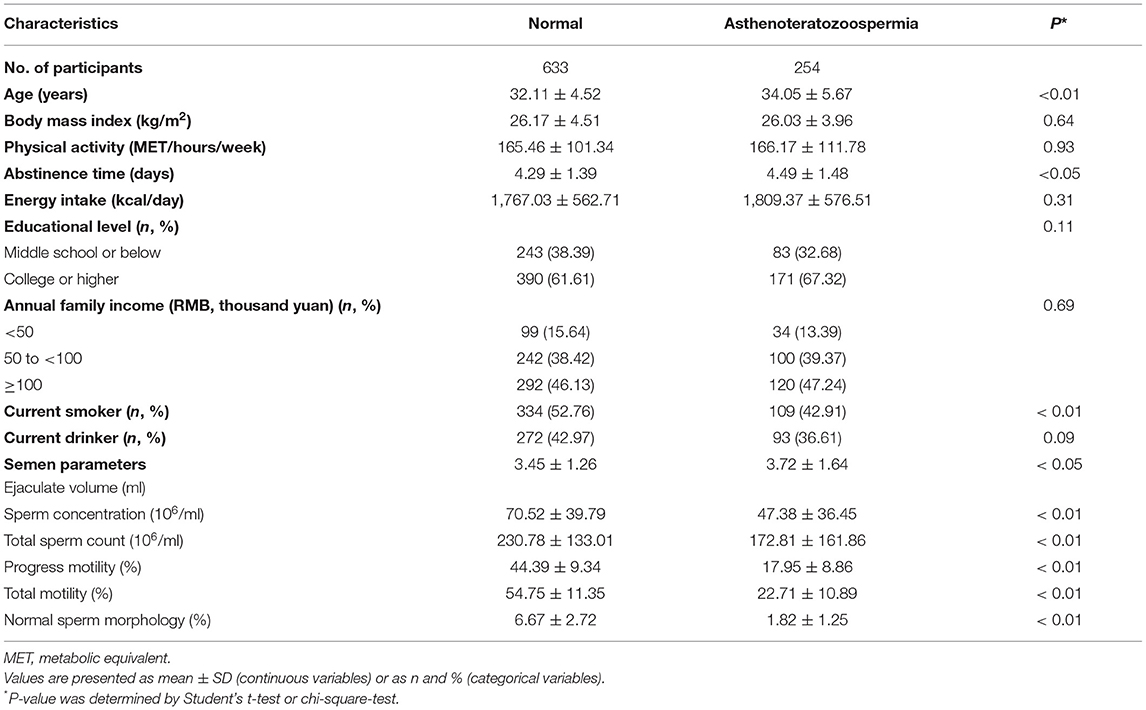
Table 1. General characteristics of participants in a case-control study of asthenoteratozoospermia.
General characteristics of participants according to tertiles of CHEI, DASH, and AHEI-2010 scores are presented in Supplementary Tables 2–4. Semen parameters, progress motility, and total motility were all increased across tertiles for CHEI, AHEI-2010, and DASH scores (P < 0.05). Participants with a high score of these three diet patterns were more likely to be younger, consume less energy and have a smoking and drinking history (P < 0.05).
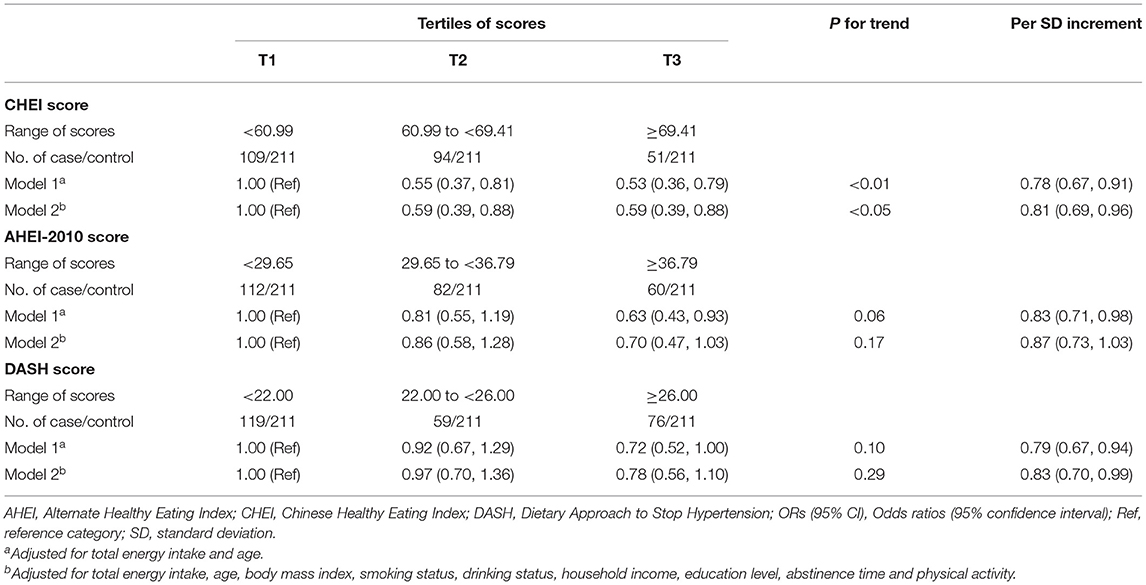
Table 2. Adjusted OR and 95 % CIs for asthenoteratozoospermia risk according to tertile of dietary quality scores.
Association of Diet Quality With Asthenoteratozoospermia Risk
The relationships between diet quality scores and asthenoteratozoospermia risk are presented in Table 2. The CHEI score was inversely associated with the risk of asthenoteratozoospermia in the age- and total energy-adjusted model (T3 vs. T1, OR = 0.53, 95% CI: 0.36–0.79, P trend < 0.01) as well as in the multivariate adjusted model (T3 vs. T1, OR = 0.59, 95% CI: 0.39–0.88, P trend < 0.05). In addition, we found no statistically significant associations between AHEI-2010 and DASH and asthenoteratozoospermia risk in the age- and total energy-adjusted models (T3 vs. T1, OR = 0.63, 95% CI: 0.43–0.93, P trend = 0.06 for AHEI-2010; OR = 0.72, 95% CI: 0.52–1.00, P trend = 0.10 for DASH) or multivariable-adjusted models (T3 vs. T1, OR = 0.70, 95% CI: 0.47–1.03, P trend = 0.17; OR = 0.78, 95% CI: 0.56–1.10, P trend = 0.29). We found that these diet quality scores were significantly associated with the decreased risk of asthenoteratozoospermia by 22% (95% CI, 9–33%) for per 1 SD increase in CHEI score, 17% (95% CI, 2–29%) for per 1 SD increase in AHEI score, and 21% (95% CI, 6–33%) for per 1 SD increase in DASH score.
Stratified Analyses
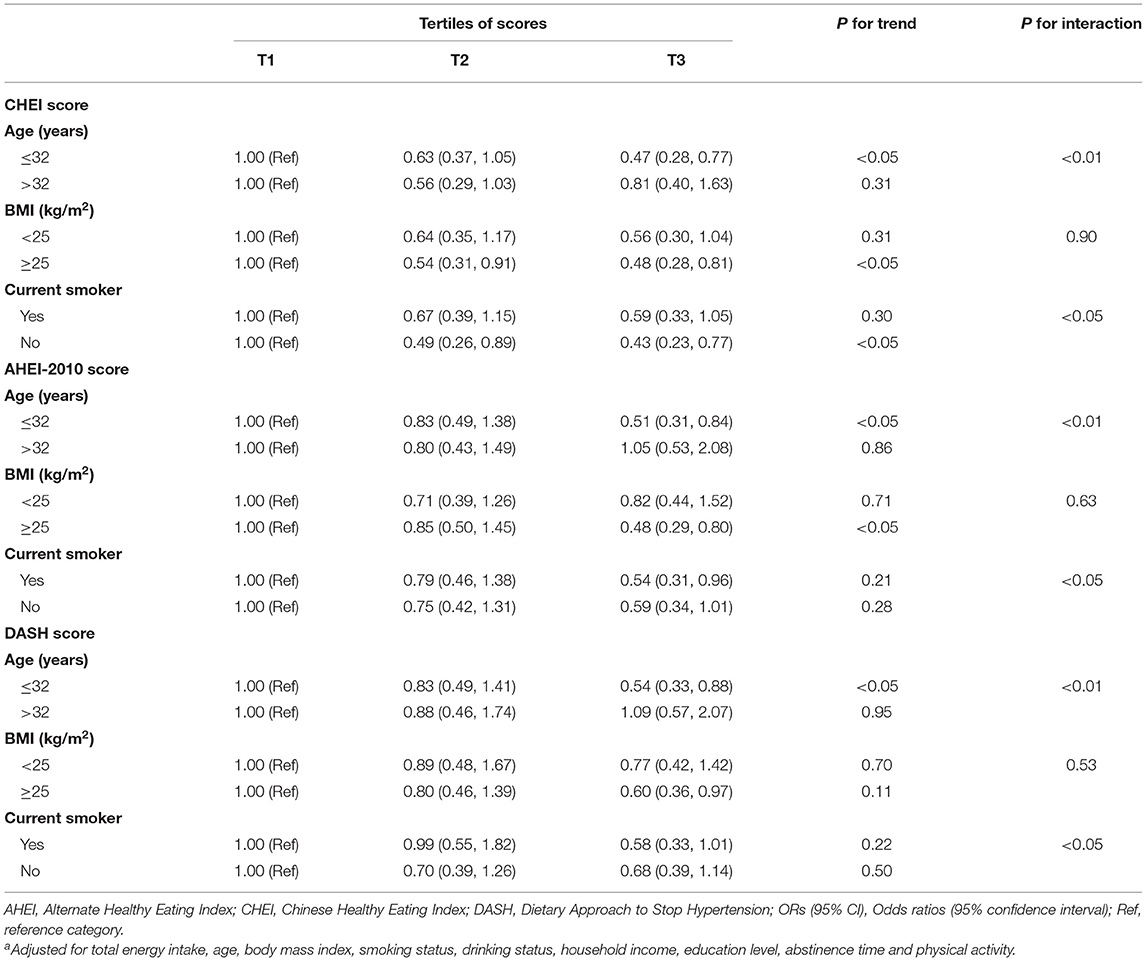
As shown in Table 3, we found that there were significant interactive effects of age and smoking status on the associations (all P for interaction < 0.05). For these scores, significant reverse associations were only witnessed in younger patients (T3 vs. T1, OR = 0.47, 95% CI: 0.28–0.77 for CHEI; OR = 0.51, 95% CI: 0.31–0.84, P trend < 0.05 for AHEI-2010; OR = 0.54, 95% CI: 0.33–0.88, P trend < 0.05 for DASH). When conducting subgroup analysis by smoking status, we found that CHEI was negatively related to asthenoteratozoospermia risk only in non-smokers (T3 vs. T1, OR = 0.43, 95% CI: 0.23–0.77).
Discussion
In the current study, we found that the inverse association between diet quality scores and asthenoteratozoospermia risk was evident for CHEI, AHEI-2010 and DASH scores overall, when the SD of diet quality scores was considered a continuous variable. In the stratified analyses, significant inverse associations for these three diet scores only appeared for individuals at a younger age.
There has been no study investigating the association between multiple diet quality scores and asthenoteratozoospermia risk. We found that higher adherence to the AHEI-2010 and DASH scores was inversely associated with asthenoteratozoospermia risk. Our results are partially consistent with a cross-sectional study conducted in Poland that reported that adherence to AHEI-2010 and DASH scores may have higher sperm concentration, normal sperm morphology, and total sperm count (12). Some similarities may also be found with observations conducted in Israel reporting that men in the highest quartiles of AHEI-2010 and DASH scores had significantly higher sperm concentrations and normal sperm morphology (1).
The AHEI-2010 and DASH scores were characterized by high intakes of fruit, vegetables, whole grains, and legumes and low intakes of sugar-sweetened, red/processed meat, and sodium. These high intake food groups were found to be positively associated with sperm count (3, 19), concentration (19), sperm motility (20, 21), and morphology (3, 19). These food groups serve as major sources of vitamins, minerals, and polyphenols, which are be considered antioxidant and anti-inflammatory. The antioxidants in male reproductive health may be positively associated with semen parameters (22–24), as these oxidants may reduce oxidative damage to sperm (25, 26), DNA maintenance, transfer RNA, and protein synthesis (27), and reduce the negative effects of inflammation (26, 28). Moreover, these two dietary scores recommend reduction in sugar-sweetened beverage, red/processed meat, and fat consumption. The relatively high content of sugars, saturated/trans fatty acids, and sodium may adversely affect sperm count (19), concentration (29, 30), sperm motility (3, 20), and morphology (3, 31).
In addition, we found that CHEI scores were inversely associated with asthenoteratozoospermia risk. As the instrument in China to assess diet quality overall, the CHEI score was developed according to the updated Dietary Guidelines for Chinese (14). The main components recommended by the CHEI score are higher intakes of total grains, whole grains, and mixed beans, tubers, total vegetables, dark vegetables, fruits, dairy, soybeans, fish and seafood, poultry, eggs, seeds, and nuts and limitation of red meat, cooking oils, sodium, added sugars and alcohol (14). Evidence from epidemiological studies has reported that high intakes of dairy (4), fruits and vegetables (19, 32), cereals (32), fish (5, 6), nuts (6), and eggs (6) were related to higher sperm quality. In addition, high consumption of red meat (6, 32), processed meat (5), habitual alcohol consumption (33), sugar-sweetened beverages (34), and fish was found to be associated with low semen quality. The apparent benefit of CHEI may be attributable to a high intake of foods containing antioxidants and carotenoids. Reactive oxygen species production has been associated with increased cellular damage and the rate of sperm ATP depletion, which leads to insufficient axonemal phosphorylation, lipid peroxidation, and loss of motility and viability (35). In addition, the CHEI pattern also contains a high amount of nutrients with good anti-inflammatory properties, such as omega-3 fatty acids, fruit, and vegetables, and a low amount of proinflammatory nutrients, such as red meat and unhealthy fat. Inflammation may affect reproduction through anatomical or functional changes in the male accessory gland and/or direct negative impacts on spermatozoa (28).
In the stratified analyses, we found that the favorable associations between the three diet quality scores and asthenoteratozoospermia risk persisted across participants whose age was below 32 years, which indicated that adhering to the latest dietary guidelines for Americans or Chinese individuals is more likely to decrease asthenoteratozoospermia risk for young participants. The reason may be that young participants often show less healthy eating habits than general participants (36, 37). In addition, smoking can have a harmful effect on semen quality through a variety of toxic substances and chemical substances (38). However, the beneficial substances produced by diet cannot compensate for the harm to semen quality caused by smoking, which may explain the negative correlations between the CHEI score and asthenoteratozoospermia risk in non-smokers.
Our study has several strengths. To our knowledge, this is the first study to investigate the association between CHEI, AHEI-2010, and DASH and the risk of asthenoteratozoospermia in a Chinese population. Furthermore, we not only adjusted for several confounding factors but also carried out numerous subgroup analyses, which ensured the authenticity and reliability of our research results. However, some limitations occurred in our study. First, we cannot exclude the possibility of reverse causality with a case–control design. However, we provided strong evidence of a positive association by eliminating the effect of potential confounders. Second, dietary information collected by the FFQ may induce recall bias. To reduce this bias, we used the FFQ, which has acceptable reproducibility and validity, to collect dietary information in a face-to-face manner. Third, there are some dietary components that are not included in the diet score, such as oil and salt, which may affect our results. In the future, we need to consider these factors to improve these studies.
Our findings suggested that higher adherence to the CHEI, AHEI-2010, and DASH diet quality scores may reduce the risk of asthenoteratozoospermia, especially for younger participants. Well-designed prospective cohort studies and randomized clinical trials are required to confirm these results.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Shengjing Hospital of China Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
QC, H-HW, Q-JW, QD, and B-CP conceived the study. B-CP contributed to the design. QD, X-BW, R-HG, XL, and B-CP collected the data. QC and Q-JW cleaned the data, checked the discrepancy, and analyzed the data. QC, H-HW, Q-JW, X-BW, R-HG, XL, X-LT, and B-CP interpreted the data. All authors read the manuscript and approved the final vision.
Funding
This work was supported by the Shengjing Hospital Clinical Research Project (No. M0071 to B-CP).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.859143/full#supplementary-material
References
1. Efrat M, Stein A, Pinkas H, Unger R, Birk R. Dietary patterns are positively associated with semen quality. Fertil Steril. (2018) 109:809–16. doi: 10.1016/j.fertnstert.2018.01.010
2. Jaroszynski L, Dev A, Li M, Meinhardt A, Nayernia K. Asthenoteratozoospermia in mice lacking testis expressed gene 18 (Tex18). Mol Hum Reprod. (2007) 13:155–63. doi: 10.1093/molehr/gal107
3. Wang XB, Wu QJ, Liu FH, Zhang S, Wang HY, Guo RH, et al. The association between dairy product consumption and asthenozoospermia risk: a hospital-based case-control study. Front Nutr. (2021) 8:714291. doi: 10.3389/fnut.2021.714291
4. Afeiche MC, Bridges ND, Williams PL, Gaskins AJ, Tanrikut C, Petrozza JC, et al. Dairy intake and semen quality among men attending a fertility clinic. Fertil Steril. (2014) 101:1280–7. doi: 10.1016/j.fertnstert.2014.02.003
5. Afeiche MC, Gaskins AJ, Williams PL, Toth TL, Wright DL, Tanrikut C, et al. Processed meat intake is unfavorably and fish intake favorably associated with semen quality indicators among men attending a fertility clinic. J Nutr. (2014) 144:1091–8. doi: 10.3945/jn.113.190173
6. Yörüsün T, Akdevelioglu Y, Karabacak RO, Bozkurt N, Sanlier N, Yeşil S, et al. Nutritional factors related to male fertility: Turkish sample. Afr J Reprod Health. (2020) 24:85–95. doi: 10.29063/ajrh2020/v24i2.8
7. Soubry A, Murphy SK, Vansant G, He Y, Price TM, Hoyo C. Opposing epigenetic signatures in human sperm by intake of fast food versus healthy food. Front Endocrinol. (2021) 12:625204. doi: 10.3389/fendo.2021.625204
8. Hu FB, Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. (2002) 13:3–9. doi: 10.1097/00041433-200202000-00002
9. Arab A, Rafie N. Dietary patterns and semen quality: a systematic review and meta-analysis of observational studies. Andrology. (2018) 6:20–8. doi: 10.1111/andr.12430
10. Trichopoulos D, Lagiou P. Dietary patterns and mortality. Br J Nutr. (2007) 85:133–4. doi: 10.1079/BJN2000282
11. Liu FH, Wang XB, Wen ZY, Wang HY, Zhang M, Zhang S, et al. Dietary inflammatory index and risk of asthenozoospermia: a hospital-based case-controlled study in China. Front Nutr. (2021) 8:706869. doi: 10.3389/fnut.2021.706869
12. Danielewicz A, Morze J. Association of the dietary approaches to stop hypertension, physical activity, and their combination with semen quality: a cross-sectional study. Nutrients. (2019) 12:39. doi: 10.3390/nu12010039
13. Cutillas-Tolín A, Adoamnei E, Navarrete-Muñoz EM, Vioque J, Moñino-García M, Jørgensen N, et al. Adherence to diet quality indices in relation to semen quality and reproductive hormones in young men. Hum Reprod. (2019) 34:1866–75. doi: 10.1093/humrep/dez157
14. Yuan Y-Q, Li F, Dong R-H, Chen J-S, He G-S, Li S-G, et al. The development of a chinese healthy eating index and its application in the general population. Nutrients. (2017) 9:977. doi: 10.3390/nu9090977
15. World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen. Geneva: World Health Organization (2021).
17. Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. (2008) 168:713–20. doi: 10.1001/archinte.168.7.713
18. Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. (2012) 142:1009–18. doi: 10.3945/jn.111.157222
19. Mendiola J, Torres-Cantero AM, Moreno-Grau JM, Ten J, Roca M, Moreno-Grau S, et al. Food intake and its relationship with semen quality: a case-control study. Fertil Steril. (2009) 91:812–8. doi: 10.1016/j.fertnstert.2008.01.020
20. Eslamian G, Amirjannati N, Rashidkhani B, Sadeghi MR, Hekmatdoost A. Intake of food groups and idiopathic asthenozoospermia: a case-control study. Hum Reprod. (2012) 27:3328–36. doi: 10.1093/humrep/des311
21. Gaskins AJ, Colaci DS, Mendiola J, Swan SH, Chavarro JE. Dietary patterns and semen quality in young men. Hum Reprod. (2012) 27:2899–907. doi: 10.1093/humrep/des298
22. Mínguez-Alarcón L, Mendiola J, López-Espín JJ, Sarabia-Cos L, Vivero-Salmerón G, Vioque J, et al. Dietary intake of antioxidant nutrients is associated with semen quality in young university students. Hum Reprod. (2012) 27:2807–14. doi: 10.1093/humrep/des247
23. Ross C, Morriss A, Khairy M, Khalaf Y, Braude P, Coomarasamy A, et al. A systematic review of the effect of oral antioxidants on male infertility. Reprod Biomed Online. (2010) 20:711–23. doi: 10.1016/j.rbmo.2010.03.008
24. Zareba P, Colaci DS, Afeiche M, Gaskins AJ, Jørgensen N, Mendiola J, et al. Semen quality in relation to antioxidant intake in a healthy male population. Fertil Steril. (2013) 100:1572–9. doi: 10.1016/j.fertnstert.2013.08.032
25. Smits RM, Mackenzie-Proctor R, Yazdani A, Stankiewicz MT, Jordan V, Showell MG. Antioxidants for male subfertility. Cochrane Database Syst Revi. (2019) 3:Cd007411. doi: 10.1002/14651858.CD007411.pub4
26. Moretti E, Cosci I, Spreafico A, Serchi T, Cuppone AM, Collodel G. Semen characteristics and inflammatory mediators in infertile men with different clinical diagnoses. Int J Androl. (2009) 32:637–46. doi: 10.1111/j.1365-2605.2008.00911.x
27. Molloy AM. Genetic aspects of folate metabolism. Sub-cell Biochem. (2012) 56:105–30. doi: 10.1007/978-94-007-2199-9_7
28. La Vignera S, Condorelli RA, Vicari E, Tumino D, Morgia G, Favilla V, et al. Markers of semen inflammation: supplementary semen analysis? J Reprod Immunol. (2013) 100:2–10. doi: 10.1016/j.jri.2013.05.001
29. Attaman JA, Toth TL, Furtado J, Campos H, Hauser R, Chavarro JE. Dietary fat and semen quality among men attending a fertility clinic. Hum Reprod. (2012) 27:1466–74. doi: 10.1093/humrep/des065
30. Liu CY, Chou YC, Chao JC, Hsu CY, Cha TL, Tsao CW. The association between dietary patterns and semen quality in a general Asian population of 7282 males. PLoS ONE. (2015) 10:e0134224. doi: 10.1371/journal.pone.0134224
31. Chiu YH, Afeiche MC, Gaskins AJ, Williams PL, Mendiola J, Jørgensen N, et al. Sugar-sweetened beverage intake in relation to semen quality and reproductive hormone levels in young men. Hum Reprod. (2014) 29:1575–84. doi: 10.1093/humrep/deu102
32. Braga DP, Halpern G, Figueira Rde C, Setti AS, Iaconelli A Jr., Borges E Jr. Food intake and social habits in male patients and its relationship to intracytoplasmic sperm injection outcomes. Fertil Steril. (2012) 97:53–9. doi: 10.1016/j.fertnstert.2011.10.011
33. Jensen TK, Gottschau M, Madsen JO, Andersson AM, Lassen TH, Skakkebæk NE, et al. Habitual alcohol consumption associated with reduced semen quality and changes in reproductive hormones; a cross-sectional study among 1221 young Danish men. BMJ Open. (2014) 4:e005462. doi: 10.1136/bmjopen-2014-005462
34. Nassan FL, Priskorn L. Association between intake of soft drinks and testicular function in young men. Hum Reprod. (2021) 18:3036–48. doi: 10.1093/humrep/deab179
35. Peña ST Jr., Gummow B, Parker AJ, Paris DBBP. Antioxidant supplementation mitigates DNA damage in boar (Sus scrofa domesticus) spermatozoa induced by tropical summer. PLoS ONE. (2019) 14 e0216143. doi: 10.1371/journal.pone.0216143
36. Gouda M, Matsukawa M, Iijima H. Associations between eating habits and glycemic control and obesity in Japanese workers with type 2 diabetes mellitus. Diab Metab Syndrome Obes Targets Ther. (2018) 11:647–58. doi: 10.2147/DMSO.S176749
37. Lee DH, Jung KY, Park KS, Kim KM, Moon JH, Lim S, et al. Characterization of patients with type 2 diabetes according to body mass index: Korea National Health and Nutrition Examination Survey from 2007 to 2011. Endocrinol Metab. (2015) 30:514–21. doi: 10.3803/EnM.2015.30.4.514
Keywords: DASH, AHEI-2010, CHEI, asthenoteratozoospermia, case–control study
Citation: Cui Q, Wang H-H, Wu Q-J, Wang X-B, Guo R-H, Leng X, Tan X-L, Du Q and Pan B-C (2022) Diet Quality Scores and Asthenoteratozoospermia Risk: Finding From a Hospital-Based Case–Control Study in China. Front. Nutr. 9:859143. doi: 10.3389/fnut.2022.859143
Received: 21 January 2022; Accepted: 21 March 2022;
Published: 11 April 2022.
Edited by:
Wei Bao, University of Science and Technology of China, ChinaReviewed by:
Tommaso Filippini, University of Modena and Reggio Emilia, ItalySilvia Y. Moya-Camarena, Consejo Nacional de Ciencia y Tecnología (CONACYT), Mexico
Copyright © 2022 Cui, Wang, Wu, Wang, Guo, Leng, Tan, Du and Pan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiang Du, ZHVxaWFuZzkxMkAxMzkuY29t; Bo-Chen Pan, cGFuYmNAc2otaG9zcGl0YWwub3Jn
†These authors have contributed equally to this work
 Qi Cui
Qi Cui Hui-Han Wang4†
Hui-Han Wang4† Qi-Jun Wu
Qi-Jun Wu Xiao-Bin Wang
Xiao-Bin Wang