- 1Department of Cardiology, College of Medicine, Sir Run Run Shaw Hospital, Zhejiang University, Hangzhou, China
- 2Key Laboratory of Cardiovascular Intervention and Regenerative Medicine of Zhejiang Province, Hangzhou, China
- 3Department of Cardiology, College of Medicine, The Fourth Affiliated Hospital, Zhejiang University, Yiwu, China
Backgrounds and Aims: Nutritional Risk Screening 2002 (NRS-2002) has been widely recommended for identifying the nutritional risk. However, the association between NRS-2002 and the prognosis of heart failure has not been fully addressed. This study aimed to explore the association of NRS-2002 with 1-year re-hospitalization and the length of initial hospital stay in heart failure patients.
Methods: This retrospective study included 2,830 heart failure patients. The primary endpoint was 1-year re-hospitalization for heart failure. The secondary endpoint was the length of initial hospital stay. The Log-binomial regression analysis was performed to determine the association between NRS-2002 and re-hospitalization. The Cox regression model was fitted to estimate hazard of discharge. The cumulative incidence curves of discharge were plotted using Kaplan–Meier method and log-rank test was performed. Exploratory analysis was also conducted according to the classification of heart failure and the level of N-terminal pro-B-type natriuretic peptide (NT-proBNP) fold-elevation.
Results: Among 2,830 heart failure patients, the mean age was 64.3 years and 66.4% were male. A total of 122 (4.3%) patients were considered at high nutritional risk. Log-binomial regression analysis demonstrated that higher NRS-2002 score was an independent risk factor of re-hospitalization ([1 vs. 0]: relative risks [RR] = 1.383, 95% CI = 1.152 to 1.660; [2 vs. 0]: RR = 1.425, 95% CI = 1.108 to 1.832; [3–7 vs. 0]: RR = 1.770, 95% CI = 1.310 to 2.393). Kaplan–Meier curve showed that the cumulative incidence of discharge was lower in high nutritional risk group (Log rank p < 0.001). Cox regression analysis also found that higher NRS-2002 score (2 or ≥3) was strongly associated with longer length of initial hospital stay ([2 vs. 0]: Hazard ratios [HR] = 0.854, 95% CI = 0.748 to 0.976; [3–7 vs. 0]: HR = 0.609, 95% CI = 0.503 to 0.737). Exploratory analysis showed that such association still remained irrespective of NT-proBNP fold-elevation, but only existed in patients with heart failure with preserved ejection fraction (HFpEF).
Conclusion: In patients with heart failure, high NRS-2002 score was strongly and independently associated with the incidence of 1-year re-hospitalization and the length of initial hospital stay.
Introduction
Heart failure is a major and growing public health problem, which results in high mortality and re-hospitalization rate (1). Heart failure can be caused by any structural or functional cardiac disorder that impairs the ability of the ventricle to fill or eject blood, and is considered as the terminal stage of various cardiovascular diseases (2). The progression of heart failure is associated with a variety of risk factors, most notably inflammation status, coronary artery disease, hypertension, diabetes, and obesity, and they are tightly related to impaired nutritional status (3, 4). It is well-established that high nutritional risk is widespread among heart failure patients and turns to be one of the most important determinants in the length of hospital stay, in-hospital mortality, and cardiovascular events, especially in the elderly (5–7). Accordingly, nutritional risk assessment in early stages plays a vital role not only in preventing the deterioration of heart failure, but also in predicting the prognosis of heart failure (8).
For decades, several nutritional assessment tools have been proposed and extensively used in clinical settings, such as Nutritional Risk Screening 2002 (NRS-2002), Controlling Nutritional Status (CONUT), Geriatric Nutritional Risk Index (GNRI), Mini Nutritional Assessment (MNA) (9–11). Among them, NRS-2002 has emerged as a simple nutritional assessment tool, which was first developed by Kondrup et al. and is composed of patient's nutritional status, severity of diseases, and age (12). Unlike other nutritional assessment tools that mainly focus on laboratory indicators such as albumin, lymphocyte, and so on; NRS-2002 additionally takes the effect of the changes in food intake and disease severity into consideration. Nowadays, NRS-2002 stands out as an effective, flexible, and comprehensive nutritional assessment tool and has been extensively used in the clinical nutrition assessment to provide nutritional information (13). Studies have shown that NRS-2002 performed well in predicting prognosis especially the mortality and length of hospital stay among patients with different types of cancers (14), chronic kidney disease (15), and cardiovascular disease (16). Recent research also found that the high nutritional risk assessed by NRS-2002 was significantly associated with the long-term mortality in hospitalized patients with chronic heart failure (CHF) (17). However, whether NRS-2002 is associated with 1-year re-hospitalization for heart failure and the length of initial hospital stay in heart failure patients has not been fully understood.
Therefore, this observational study was conducted to investigate the association between NRS-2002 and the clinical outcomes in heart failure patients, such as 1-year re-hospitalization for heart failure and the length of initial hospital stay.
Methods
Study Population
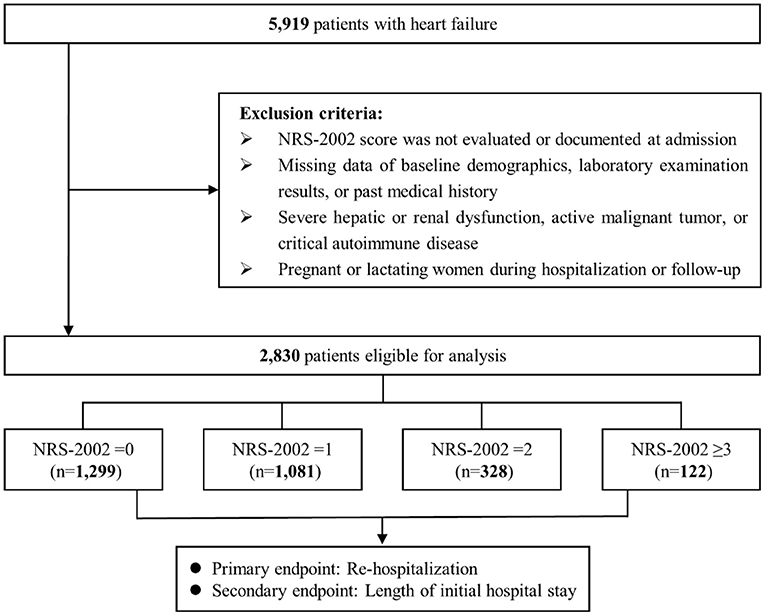
In this observational study, 5,919 heart failure patients, who were hospitalized in Sir Run Run Shaw Hospital and its medical consortium hospitals from January 2009 to April 2019, were recruited. Patients with the following criteria were excluded: (1) NRS-2002 score was not evaluated or documented at admission; (2) missing data on baseline characteristics, laboratory measurements, or past medical history; (3) severe hepatic or renal dysfunction, active malignant tumor, or critical autoimmune disease; (4) pregnant or lactating women during hospitalization or follow-up. Finally, a total of 2,830 patients were enrolled. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting standards were followed (18). Ethical approval was obtained from the ethics committee of Sir Run Run Shaw Hospital (NO.20201217-36).
Sample Size Estimation
The estimated number of participants was based on the incidence of re-hospitalization in the previous study and on the principle of 10 outcome events per variable (19). A previous study reported that ~20% patients with heart failure would be re-admitted within 1-year (1). Therefore, 20% was adopted as the estimated incidence of re-hospitalization in patients with heart failure. According to the estimated incidence of re-hospitalization and nine variables included in the log-binomial regression model, at least 450 heart failure patients were needed, which was far less than actual enrollment.
The Definitions of Heart Failure and NRS-2002
According to the 2016 European Society of Cardiology (ESC), heart failure is defined as an inability of the heart to meet the humans' metabolic demands, accompanied with typical symptoms and signs. The typical symptoms of heart failure mainly include dyspnea, weakness, chest tightness, and cardiogenic shock. The typical signs of heart failure involve lower limb edema, elevated jugular venous pressure, and pulmonary oedema (20). According to the level of left ventricular ejection fraction (LVEF), heart failure is classified into three types: heart failure with reduced ejection fraction (HFrEF) (<40%), heart failure with mid-range ejection fraction (HFmrEF) (40–49%), and heart failure with preserved ejection fraction (HFpEF) (≥50%).
Based on the European Society for Clinical Nutrition and Metabolism (ESPEN), the detailed calculation method of NRS-2002 was listed in Supplementary Table 1 (21). NRS-2002 score is calculated according to patients' impaired nutritional status, the severity of disease and age. The impaired nutritional status and severity of disease are scored between 0 and 3 points, respectively. Patients aged 70 years or older would receive an additional point based on the total score. Age-adjusted total NRS-2002 score ranges on a scale of 0 to 7. A total NRS-2002 score ≥3 points is considered at high nutritional risk, while those with a score below 3 points are considered at low nutritional risk (22).
Study Endpoints
Patients who were first hospitalized for heart failure were enrolled in this study and were followed up for 1-year, regardless of the classification of heart failure. The primary endpoint was re-hospitalization for heart failure during a 1-year follow-up after discharge. And the secondary endpoint was the length of initial hospital stay, which was defined as the length of stay in patients who were hospitalized for heart failure for the first time and was calculated by subtracting the date of admission from the date of discharge.
Data Collection
Baseline characteristics and clinical parameters related to this study were all derived from the Hospital Information System (HIS). Demographic data, laboratory data, comorbidities, and medication were collected. Fasting venous blood samples were collected on the morning after hospital admission day and then immediately sent to hematological and biochemical laboratory examinations. LVEF was assessed according to the classical Teichholz method. N-terminal pro-B-type natriuretic peptide (NT-proBNP) was analyzed using the NT-proBNP fold-elevation (actual value divided by the upper limit of normal value according to the age stratification). Nutritional status was assessed routinely within 24 h after hospital admission by the NRS-2002, which was applied by the trained nursing staff.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD) if normally distributed, and median (interquartile range) if not. Categorical variables were expressed as numbers and proportions. Comparisons between high and low nutritional risk group were made using Student t-test if normally distributed or Mann–Whitney U test if not. The chi-square test or Fisher's exact test were used to examine the comparability of baseline characteristics for categorical variables according to minimal expected cell value.
The association between nutritional status (low nutritional risk and high nutritional risk) and 1-year re-hospitalization was evaluated using log-binomial regression models. Relative risks (RRs) with 95% CI were calculated. Covariates with potential significance for the prognosis of heart failure were adjusted in adjusted model 1, such as age (<65 or ≥65 years) (23), sex (male or female) (23), diabetes (yes or no) (24), hypertension (yes or no) (25), and estimated glomerular filtration rate (eGFR) (<90 or ≥90 ml/min/1.73 m2) (26). Adjusted model 2 further adjusted LVEF (<40, 40–49, or ≥50%) (27), NT-proBNP fold-elevation (<2 or ≥2) (28) and admission of diuretics (yes or no) (29). The association of NRS-2002 with the length of initial hospital stay was first visualized by loess smooth curve. Kaplan–Meier curve was generated to show the cumulative incidence of discharge in patients stratified by high and low nutritional risk and log-rank test was performed. Cox regression analysis was performed to estimate the hazard of discharge, with the same adjustment mentioned above. Hazard ratios (HRs) >1.0 represented shorter length of hospital stay, while HRs < 1.0 represented longer length of hospital stay. To further explore whether NRS-2002 remained effective in patients at low nutritional risk, the total population was divided into four categories (NRS-2002 score = 0, 1, 2, and ≥3). Log-binomial and Cox regression analysis were performed again and the NRS-2002 score = 0 group was regarded as the reference category. Finally, exploratory analysis was conducted according to the classification of heart failure and the level of NT-proBNP fold-elevation.
All statistical tests were 2-sided and p-value <0.05 was considered significant. All statistical analysis were performed with the Statistical Package for Social Science software version 25.0 (SPSS Inc., Chicago, USA) and R software version 4.0.5 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Screening and Baseline Characteristics
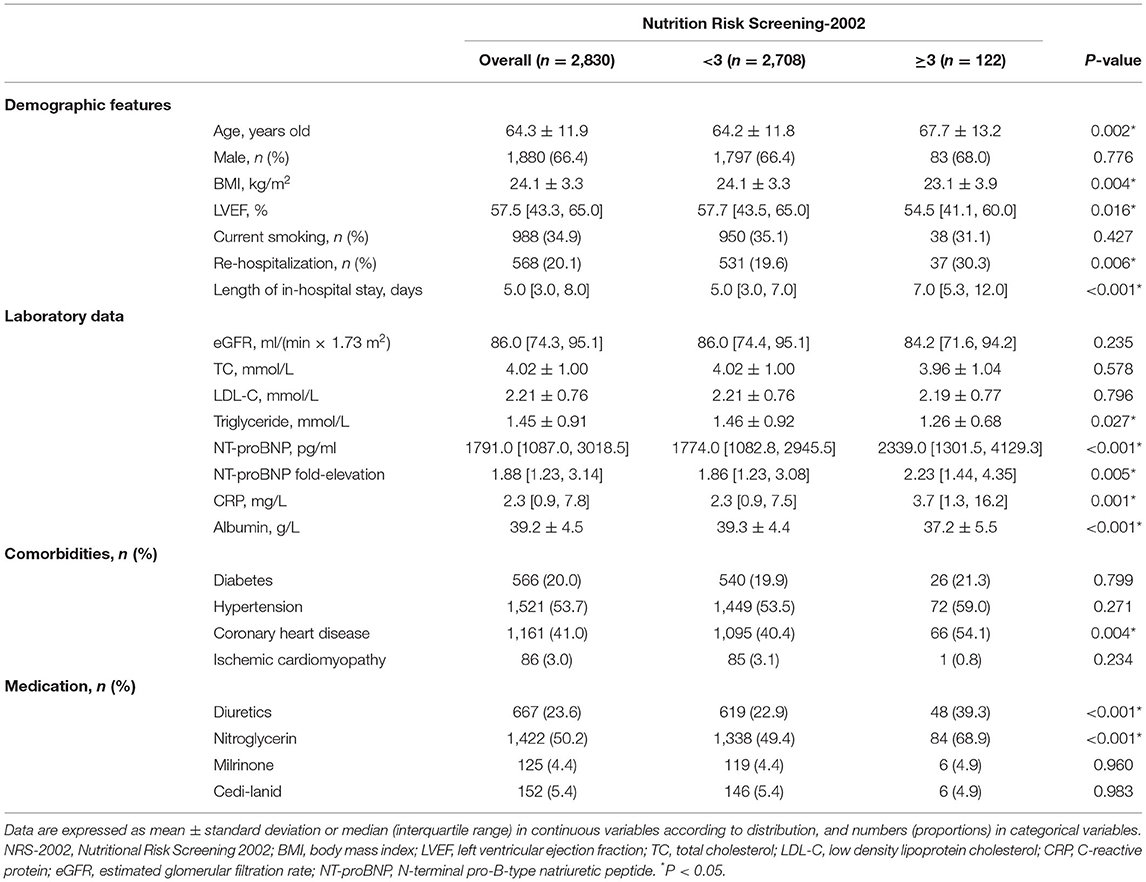
As shown in Figure 1, a total of 5,919 patients with heart failure were screened for eligibility and 2,830 patients were finally enrolled. Table 1 presents the baseline demographics and clinical features of enrolled patients. The average age was 64.3 ± 11.9 years and 1,880 (66.4%) were male. A total of 122 (4.3%) patients were at high nutritional risk (NRS-2002 score ≥3). A total of 568 (20.1%) patients were re-hospitalized for heart failure after discharge in 1-year follow-up. The median length of initial hospital stay was 5.0 [3.0, 8.0] days. Compared with low nutritional risk group, patients at high nutritional risk had a higher incidence of re-hospitalization (30.3 vs. 19.6%, p = 0.006), and longer length of initial hospital stay (7.0 [5.3, 12.0] days vs. 5.0 [3.0, 7.0] days, p < 0.001). Moreover, high nutritional risk patients had worse cardiac function with lower LVEF (54.5 [41.1, 60.0]% vs. 57.7 [43.5, 65.0]%, p = 0.016) and higher NT-proBNP fold-elevation (2.23 [1.44, 4.35] vs. 1.86 [1.23, 3.08], p = 0.005), and were more likely to be treated with diuretics (39.3 vs. 22.9%, p < 0.001) and nitroglycerin (68.9 vs. 49.4%, p < 0.001). However, there was no statistical difference in sex, smoking status, eGFR, total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), presence of diabetes, hypertension and ischemic cardiomyopathy, and medication with milrinone and cedi-lanid (all p-values >0.05).
Association of NRS-2002 With 1-Year Re-hospitalization
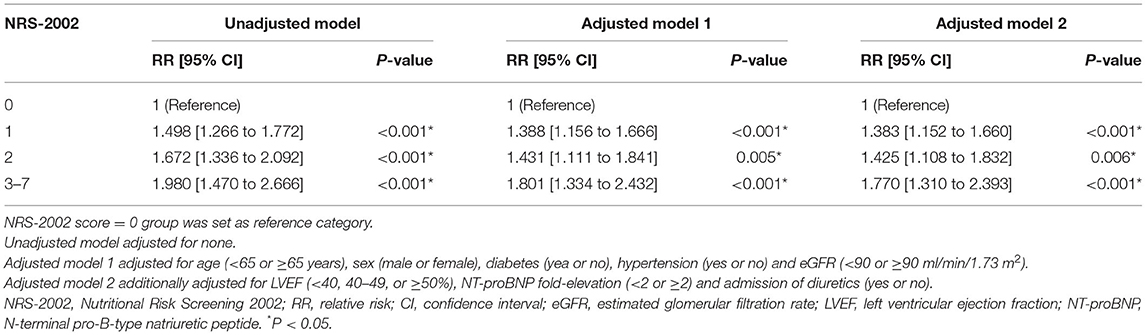
Figure 2A shows the population distribution stratified by nutritional categories (NRS-2002 score = 0, 1, 2, and ≥3), and the increasing trend of the incidence of re-hospitalization with the increase of NRS-2002 score. Log-binomial regression analysis was performed to reveal the association of nutritional risk assessed by NRS-2002 with 1-year re-hospitalization. Supplementary Table 2 shows that high nutritional risk (NRS-2002 score ≥3 vs. <3) was an independent risk factor of re-hospitalization (Adjusted model 2: RR = 1.424, 95% confidence interval (CI) = 1.083 to 1.871). Then, NRS-2002 was classified into four categories and the NRS-2002 = 0 group was considered as reference category. Higher NRS-2002 score was still found to be strongly and independently associated with higher incidence of re-hospitalization (Adjusted model 2: [1 vs. 0]: RR = 1.383, 95% confidence interval (CI) = 1.152 to 1.660; [2 vs. 0]: RR = 1.425, 95% CI = 1.108 to 1.832; [3–7 vs. 0]: RR = 1.770, 95% CI = 1.310 to 2.393) (Table 2).
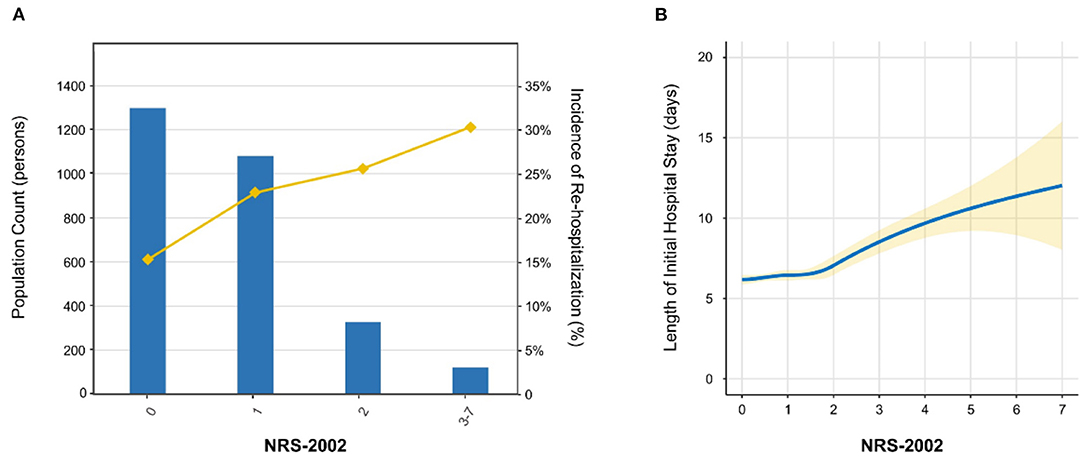
Figure 2. Population distribution and loess smooth curve. (A) The distribution of study population and the incidence of re-hospitalization. The histogram showed the population distribution of study subjects stratified by NRS-2002 categories, while the line chart showed the trend of incidence of re-hospitalization. (B) Loess smooth curve of NRS-2002 score with the length of initial hospital stay. The loess smooth curve was fitted for exploring the association between NRS-2002 score and the length of initial hospital stay. The yellow shadow around the solid line represents 95% confidence interval. NRS-2002 indicates Nutritional Risk Screening 2002.
Association of NRS-2002 With the Length of Initial Hospital Stay
Loess smooth curve was plotted, showing that with the increase of NRS-2002 score, the length of initial hospital stay increased correspondingly (Figure 2B). The cumulative incidence of discharge was also lower in the high nutritional risk group (Log rank p < 0.001) (Figure 3). Cox regression models verified that a high nutritional risk (NRS-2002 score ≥3 vs. <3) was associated with the increasing length of initial hospital stay (Adjusted model 2: HR = 0.636, 95% CI = 0.529 to 0.764) (Supplementary Table 2). Then, NRS-2002 was classified into four categories and the NRS-2002 = 0 group was regarded as a reference category. It was found that higher NRS-2002 score (2 or ≥3) was still tightly and independently associated with longer length of initial hospital stay (Adjusted model 2: [2 vs. 0]: HR = 0.854, 95% CI = 0.748 to 0.976; [3–7 vs. 0]: HR = 0.609, 95% CI = 0.503 to 0.737) (Table 3).
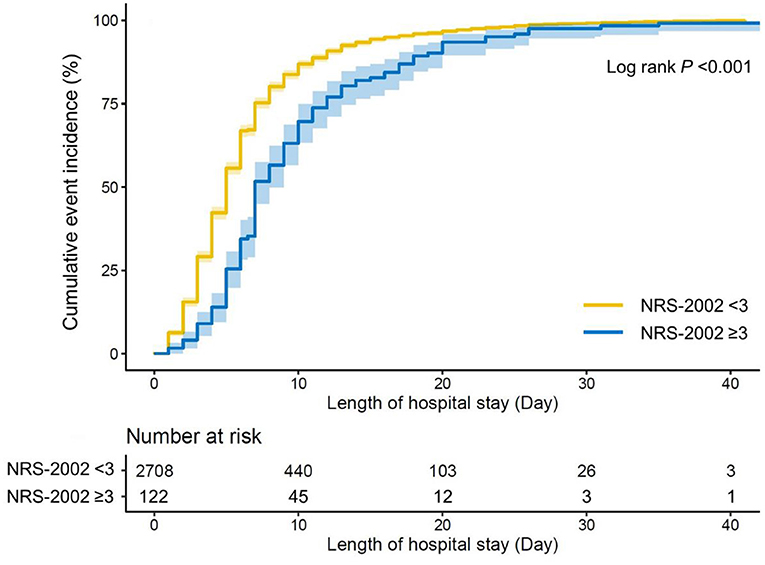
Figure 3. Cumulative incidence of discharge stratified by nutritional status. Kaplan–Meier curve was plotted to show the cumulative incidence of discharge in patients with low nutritional risk and high nutritional risk. Log rank p-value was also shown. NRS-2002 indicates Nutritional Risk Screening 2002.
Exploratory Analysis
To further explore the effect of NRS-2002 in different subgroups, an exploratory analysis was carried out according to heart failure classification (HFrEF, HFmrEF, or HFpEF) and the level of NT-proBNP fold-elevation (<2 or ≥2). Results of the association between NRS-2002 categories and 1-year re-hospitalization or the length of initial hospital stay were presented in Figure 4, respectively. Figure 4A shows that the positive association of a high NRS-2002 score with 1-year re-hospitalization still remained regardless of NT-proBNP fold-elevation level, but remained only in patients with HFpEF (all p-values <0.05). The results in Figure 4B showed that a high NRS-2002 score (NRS-2002 = 2 or ≥3) was tightly associated with a longer length of initial hospital stay in HFpEF patients or patients whose NT-proBNP fold-elevation <2, while in patients whose NT-proBNP more than 2, such positive association could only be observed when NRS-2002 ≥3.
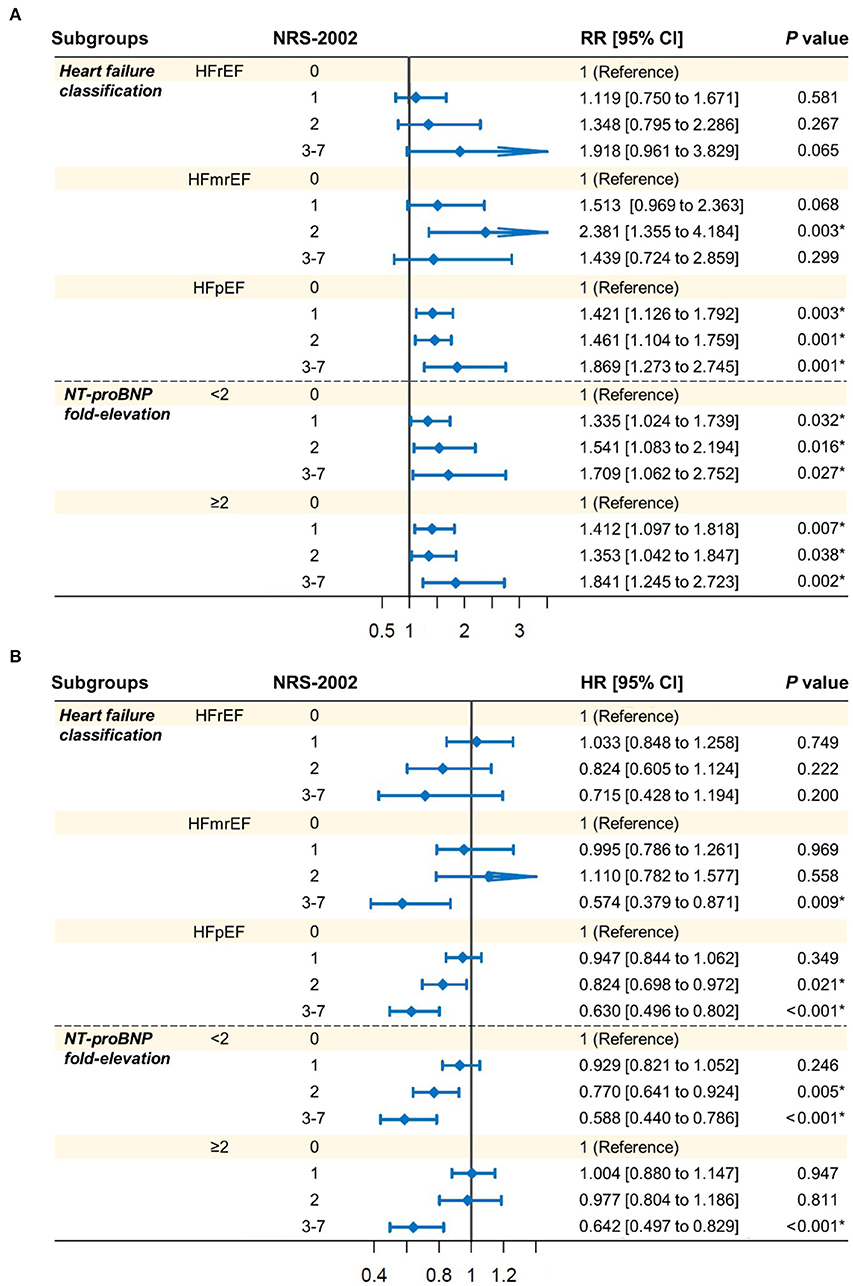
Figure 4. Exploratory analysis in the association of NRS-2002 categories with (A) 1-year re-hospitalization and (B) the length of initial hospital stay. Patients were classified according to heart failure classification (HFrEF, EFmrEF, or HFpEF) and the level of NT-proBNP fold-elevation (<2 or ≥2). Log-binomial regression analysis (A) and Cox regression analysis (B) were performed for different endpoints with the same covariates as in adjusted model 2 in Table 2, respectively. NRS-2002, Nutritional Risk Screening 2002; RR, relative risk; HR, hazard ratio; CI, confidence interval; HFrEF, heart failure with reduced ejection fraction; HFmrEF, heart failure with mid-range ejection fraction; HFpEF, heart failure with preserved ejection fraction; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
Discussion
In this observational study, nutritional risk assessed by NRS-2002 at admission was strongly and independently associated with re-hospitalization and the length of initial hospital stay in patients with heart failure. Specifically, high NRS-2002 score was an independent risk factor for 1-year re-hospitalization and the length of initial hospital stay. More importantly, exploratory analysis indicated that such association of NRS-2002 with re-hospitalization or the length of initial hospital stay generally existed irrespective of NT-proBNP fold-elevation, but only remained in patients with HFpEF.
Poor nutritional status and heart failure have a close association and commonly co-occur (30). Impaired nutritional status has been considered as one of the most critical risk factors of poor clinical outcomes in heart failure patients, especially in the elderly patients (6, 31). Therefore, it is of great interest to early evaluate the nutritional status of heart failure patients. A variety of nutritional assessment tools have been proposed and used in issued studies (32). Honda et al. and Joaquín et al. reported that both GNRI and MNA were useful tools to identify the nutritional risk in heart failure patients (33, 34). Kato et al. found that a high CONUT score was associated with a higher risk for in-hospital mortality and infection in patients with acute heart failure (AHF) (35). NRS-2002 was one of the accurate and flexible tools for nutritional status assessment, recommended by the Global Leadership Initiative on Malnutrition (GLIM) (36). Therefore, the current study chose NRS-2002 to assess heart failure patients' nutritional risk status and demonstrated that a high NRS-2002 score was a significant predictor of re-hospitalization and the length of initial hospital stay for patients with heart failure.
As a simple and convenient tool, NRS-2002 aims to identify nutritional at-risk individuals so that extra intervention can be initiated before the signs of malnutrition become obvious (37). The potential pathological mechanisms between NRS-2002 and the prognosis of heart failure are complex. All of the components of NRS-2002 can lead to an imbalance in energy synthesis and breakdown, which further induces oxidative stress, causes myocardial cell injury and ultimately leads to adverse cardiovascular events (38–41). Tevik et al. reported that NRS-2002 was significantly related to long-term mortality in hospitalized patients with CHF (16). Going further, the current study demonstrated that NRS-2002 was not only associated with the incidence of 1-year re-hospitalization, but also with the length of initial hospital stay. Therefore, it was crucial for heart failure patients' management and prognosis to early assess their nutritional status by NRS-2002.
Clinically, heart failure is a complex syndrome and is classified into three major types based on LVEF: HFrEF, HFmrEF, and HFpEF (20). HFpEF has become the major form of heart failure and researchers have found that the prognosis of HFpEF was not better than HFrEF patients, deserving more attention (42). To this end, the current study incorporated all types of heart failure populations involving HFrEF, HFmrEF, and HFpEF to better determine the effect of NRS-2002 in different types of heart failure. The results in Figure 4 showed that a high NRS-2002 score had a significant association with the incidence of re-hospitalization and the length of initial hospital stay only in HFpEF patients. It might indicate that there existed a limitation of NRS-2002 in predicting the re-hospitalization and the length of initial hospital stay in HFrEF and HFmrEF patients.
It was reported that NT-proBNP was a strong predictor of outcomes in heart failure patients (43). To eliminate the effects of NT-proBNP, in this study, log-binomial regression analysis and Cox regression analysis were conducted after the adjustment for covariates involving NT-proBNP fold-elevation. Besides, the exploratory analysis found that the positive association of high NRS-2002 score with re-hospitalization and the length of initial hospital stay still remained significant in heart failure patients with different NT-proBNP fold-elevation levels (<2 or ≥2), suggesting the validity of NRS-2002 in clinical practice.
The proportion of the high nutritional risk population among patients with heart failure differed significantly in previous studies (4.23–57%) (44–46). In the present study, the proportion of the high nutritional risk population (about 4.31%) was relatively low. In Tevik's research, only patients with LVEF ≤ 50% were included, which might result in the proportion of the high nutritional risk population higher (up to 57%) (44). The current study included patients with all types of heart failure, and the proportion of HFpEF was 66.8%. The nutritional status of HFpEF patients was relatively better than HFrEF patients, resulting in a lower proportion of high nutritional risk in the overall population of this study. The study by Czapla et al. also included patients with HFrEF, HFmrEF, and HFpEF, and the proportion of high nutritional risk (about 4.23%) was close to the proportion in this study (45).
This study also had some limitations that needed to be noticed. First, as a retrospective and observational study, the selection bias was unavoidable. Therefore, large prospective research should be conducted to support our findings. Second, in clinical practice, some patients at severe nutritional risk might receive relevant intervention by physicians or nutritionists during hospitalization or follow-up, such as nutritional supplementation, which might influence our results. Third, nutritional intake during hospitalization and follow-up, which is highly associated with not only nutritional status but also heart failure prognosis, was not available and needed to be considered as an important confounder in further research. Fourth, owing to the lack of the gold standard tool for nutritional assessment, the current study only investigated the role of NRS-2002 in the prognosis of patients with heart failure. Further studies need to focus on other nutritional assessment tools and compare the predictive performance in different tools.
Conclusion
High NRS-2002 score was strongly and independently associated with the incidence of 1-year re-hospitalization and the length of initial hospital stay in heart failure patients.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Sir Run Run Shaw Hospital of Zhejiang University (20200803-34). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
WZ and MS conceived and designed the study. ZC organized these data and drafted the manuscript with the help of HJ, WH, DL, ML, and MW. ZC and HJ analyzed the data. WH drew the pictures. WZ, MS, and MW detected any errors in the whole process. All authors have read and approved the manuscript for submission.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82070408), the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (2021RC014), and the Traditional Chinese Medicine Science and Technology Project of Zhejiang Province (2021ZB172).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.849034/full#supplementary-material
Abbreviations
NRS-2002, nutritional risk screening-2002; CONUT, controlling nutritional status; GNRI, geriatric nutritional risk index; MNA, mini nutritional assessment; CHF, chronic heart failure; STROBE, Strengthening the Reporting of Observational Studies in Epidemiology; ESC, European Society of Cardiology; LVEF, left ventricular ejection fraction; HFrEF, heart failure with reduced ejection fraction; HFmrEF, heart failure with mid-range ejection fraction; HFpEF, heart failure with preserved ejection fraction; ESPEN, European Society for Clinical Nutrition and Metabolism; HIS, Hospital Information System; SD, standard deviation; RRs, relative risks; HRs, hazard ratios; CI, confidence interval; eGFR, estimated glomerular filtration rate; NT-proBNP, N-terminal pro-B-type natriuretic peptide; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; AHF, acute heart failure; GLIM, Global Leadership Initiative on Malnutrition.
References
1. Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. (2020) 22:1342–56. doi: 10.1002/ejhf.1858
2. Hunt SA. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. (2005) 46:e1–82. doi: 10.1016/j.jacc.2005.08.022
3. Rahman A, Jafry S, Jeejeebhoy K, Nagpal AD, Pisani B, Agarwala R. Malnutrition and cachexia in heart failure. JPEN J Parenter Enteral Nutr. (2016) 40:475–86. doi: 10.1177/0148607114566854
4. Vest AR, Chan M, Deswal A, Givertz MM, Lekavich C, Lennie T, et al. Nutrition, obesity, and cachexia in patients with heart failure: a consensus statement from the heart failure society of America Scientific Statements Committee. J Card Fail. (2019) 25:380–400. doi: 10.1016/j.cardfail.2019.03.007
5. Kinugasa Y, Kato M, Sugihara S, Hirai M, Yamada K, Yanagihara K, et al. Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ J. (2013) 77:705–11. doi: 10.1253/circj.CJ-12-1091
6. Narumi T, Arimoto T, Funayama A, Kadowaki S, Otaki Y, Nishiyama S, et al. Prognostic importance of objective nutritional indexes in patients with chronic heart failure. J Cardiol. (2013) 62:307–13. doi: 10.1016/j.jjcc.2013.05.007
7. Sze S, Zhang J, Pellicori P, Morgan D, Hoye A, Clark AL. Prognostic value of simple frailty and malnutrition screening tools in patients with acute heart failure due to left ventricular systolic dysfunction. Clin Res Cardiol. (2017) 106:533–41. doi: 10.1007/s00392-017-1082-5
8. Tsuchihashi-Makaya M, Kinugawa S. Nutrition as a new treatment target in chronic heart failure. Circ J. (2013) 77:604–5. doi: 10.1253/circj.CJ-13-0028
9. Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. (2005) 20:38–45.
10. Cereda E, Pedrolli C. The use of the Geriatric Nutritional Risk Index (GNRI) as a simplified nutritional screening tool. Am J Clin Nutr. (2008) 87:1966–7. doi: 10.1093/ajcn/87.6.1966
11. Christner S, Ritt M, Volkert D, Wirth R, Sieber CC, Gaßmann KG. Evaluation of the nutritional status of older hospitalised geriatric patients: a comparative analysis of a Mini Nutritional Assessment (MNA) version and the Nutritional Risk Screening (NRS 2002). J Hum Nutr Diet. (2016) 29:704–13. doi: 10.1111/jhn.12376
12. Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. (2003) 22:321–36. doi: 10.1016/S0261-5614(02)00214-5
13. Raslan M, Gonzalez MC, Dias MC, Nascimento M, Castro M, Marques P, et al. Comparison of nutritional risk screening tools for predicting clinical outcomes in hospitalized patients. Nutrition. (2010) 26:721–6. doi: 10.1016/j.nut.2009.07.010
14. Bargetzi L, Brack C, Herrmann J, Bargetzi A, Hersberger L, Bargetzi M, et al. Nutritional support during the hospital stay reduces mortality in patients with different types of cancers: secondary analysis of a prospective randomized trial. Ann Oncol. (2021) 32:1025–33. doi: 10.1016/j.annonc.2021.05.793
15. Borek P, Chmielewski M, Małgorzewicz S, Debska Slizień A. Analysis of outcomes of the NRS 2002 in patients hospitalized in nephrology wards. Nutrients. (2017) 9:287. doi: 10.3390/nu9030287
16. Tevik K, Thürmer H, Husby MI, de Soysa AK, Helvik AS. Nutritional risk is associated with long term mortality in hospitalized patients with chronic heart failure. Clin Nutr ESPEN. (2016) 12:e20–29. doi: 10.1016/j.clnesp.2016.02.095
17. Hersberger L, Dietz A, Bürgler H, Bargetzi A, Bargetzi L, Kägi-Braun N, et al. Individualized nutritional support for hospitalized patients with chronic heart failure. J Am Coll Cardiol. (2021) 77:2307–19. doi: 10.1016/j.jacc.2021.03.232
18. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. (2007) 147:W163–94. doi: 10.7326/0003-4819-147-8-200710160-00010-w1
19. Moons KG, de Groot JA, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. (2014) 11:e1001744. doi: 10.1371/journal.pmed.1001744
20. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. (2016) 37:2129–200. doi: 10.1093/eurheartj/ehw128
21. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. (2003) 22:415–21. doi: 10.1016/S0261-5614(03)00098-0
22. da Silva Fink J, Marcadenti A, Rabito EI, Silva FM. The New European Society for clinical nutrition and metabolism definition of malnutrition: application for nutrition assessment and prediction of morbimortality in an emergency service. JPEN J Parenter Enteral Nutr. (2018) 42:550–6. doi: 10.1177/0148607117695248
23. Sciomer S, Moscucci F, Salvioni E, Marchese G, Bussotti M, Corrà U, et al. Role of gender, age and BMI in prognosis of heart failure. Eur J Prev Cardiol. (2020) 27:46–51. doi: 10.1177/2047487320961980
24. Lehrke M, Marx N. Diabetes mellitus and heart failure. Am J Med. (2017) 130:S40–50. doi: 10.1016/j.amjmed.2017.04.010
25. Slivnick J, Lampert BC. Hypertension and heart failure. Heart Fail Clin. (2019) 15:531–41. doi: 10.1016/j.hfc.2019.06.007
26. Smith DH, Thorp ML, Gurwitz JH, McManus DD, Goldberg RJ, Allen LA, et al. Chronic kidney disease and outcomes in heart failure with preserved versus reduced ejection fraction: the Cardiovascular Research Network PRESERVE Study. Circ Cardiovasc Qual Outcomes. (2013) 6:333–42. doi: 10.1161/CIRCOUTCOMES.113.000221
27. Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. (2017) 70:2476–86. doi: 10.1016/j.jacc.2017.08.074
28. Ndumele CE, Matsushita K, Sang Y, Lazo M, Agarwal SK, Nambi V, et al. N-Terminal pro-brain natriuretic peptide and heart failure risk among individuals with and without obesity: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. (2016) 133:631–8. doi: 10.1161/CIRCULATIONAHA.115.017298
29. Felker GM, Ellison DH, Mullens W, Cox ZL, Testani JM. Diuretic therapy for patients with heart failure: JACC state-of-the-art review. J Am Coll Cardiol. (2020) 75:1178–95. doi: 10.1016/j.jacc.2019.12.059
30. Wleklik M, Uchmanowicz I, Jankowska-Polańska B, Andreae C, Regulska-Ilow B. The role of nutritional status in elderly patients with heart failure. J Nutr Health Aging. (2018) 22:581–8. doi: 10.1007/s12603-017-0985-1
31. Nishi I, Seo Y, Hamada-Harimura Y, Sato K, Sai S, Yamamoto M, et al. Utility of nutritional screening in predicting short-term prognosis of heart failure patients. Int Heart J. (2018) 59:354–60. doi: 10.1536/ihj.17-073
32. Dent E, Hoogendijk EO, Visvanathan R, Wright ORL. Malnutrition screening and assessment in hospitalised older people: a review. J Nutr Health Aging. (2019) 23:431–41. doi: 10.1007/s12603-019-1176-z
33. Honda Y, Nagai T, Iwakami N, Sugano Y, Honda S, Okada A, et al. Usefulness of geriatric nutritional risk index for assessing nutritional status and its prognostic impact in patients aged ≥65 years with acute heart failure. Am J Cardiol. (2016) 118:550–5. doi: 10.1016/j.amjcard.2016.05.045
34. Joaquín C, Puig R, Gastelurrutia P, Lupón J, de Antonio M, Domingo M, et al. Mini nutritional assessment is a better predictor of mortality than subjective global assessment in heart failure out-patients. Clin Nutr. (2019) 38:2740–6. doi: 10.1016/j.clnu.2018.12.001
35. Kato T, Yaku H, Morimoto T, Inuzuka Y, Tamaki Y, Yamamoto E, et al. Association with Controlling Nutritional Status (CONUT) score and in-hospital mortality and infection in acute heart failure. Sci Rep. (2020) 10:3320. doi: 10.1038/s41598-020-60404-9
36. Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr. (2019) 38:1–9. doi: 10.1016/j.clnu.2018.08.002
37. Velasco C, García E, Rodríguez V, Frias L, Garriga R, Alvarez J, et al. Comparison of four nutritional screening tools to detect nutritional risk in hospitalized patients: a multicentre study. Eur J Clin Nutr. (2011) 65:269–74. doi: 10.1038/ejcn.2010.243
38. Luo H, Chiang HH, Louw M, Susanto A, Chen D. Nutrient sensing and the oxidative stress response. Trends Endocrinol Metab. (2017) 28:449–60. doi: 10.1016/j.tem.2017.02.008
39. Münzel T, Camici GG, Maack C, Bonetti NR, Fuster V, Kovacic JC. Impact of oxidative stress on the heart and vasculature: part 2 of a 3-part series. J Am Coll Cardiol. (2017) 70:212–29. doi: 10.1016/j.jacc.2017.05.035
40. Tan BL, Norhaizan ME, Liew WP. Nutrients and oxidative stress: friend or foe? Oxid Med Cell Longev. (2018) 2018:9719584. doi: 10.1155/2018/9719584
41. van der Pol A, van Gilst WH, Voors AA, van der Meer P. Treating oxidative stress in heart failure: past, present and future. Eur J Heart Fail. (2019) 21:425–35. doi: 10.1002/ejhf.1320
42. Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. (2017) 14:591–602. doi: 10.1038/nrcardio.2017.65
43. Zile MR, Claggett BL, Prescott MF, McMurray JJ, Packer M, Rouleau JL, et al. Prognostic implications of changes in N-terminal pro-B-type natriuretic peptide in patients with heart failure. J Am Coll Cardiol. (2016) 68:2425–36. doi: 10.1016/j.jacc.2016.09.931
44. Tevik K, Thürmer H, Husby MI, de Soysa AK, Helvik AS. Nutritional risk screening in hospitalized patients with heart failure. Clin Nutr. (2015) 34:257–64. doi: 10.1016/j.clnu.2014.03.014
45. Czapla M, Juárez-Vela R, Łokieć K, Karniej P. The association between nutritional status and in-hospital mortality among patients with heart failure-a result of the retrospective Nutritional Status Heart Study 2 (NSHS2). Nutrients. (2021) 13:1669. doi: 10.3390/nu13051669
Keywords: heart failure, Nutritional Risk Screening 2002, 1-year re-hospitalization, length of initial hospital stay, nutritional risk
Citation: Chen Z, Jiang H, He W, Li D, Lin M, Wang M, Shang M and Zhang W (2022) The Association of Nutritional Risk Screening 2002 With 1-Year Re-hospitalization and the Length of Initial Hospital Stay in Patients With Heart Failure. Front. Nutr. 9:849034. doi: 10.3389/fnut.2022.849034
Received: 05 January 2022; Accepted: 30 March 2022;
Published: 29 April 2022.
Edited by:
Maurizio Marra, University of Naples Federico II, ItalyReviewed by:
Javier Ena, Hospital Marina Baixa, SpainEmmanouella Magriplis, Agricultural University of Athens, Greece
Rita Guerra, Fernando Pessoa University, Portugal
Copyright © 2022 Chen, Jiang, He, Li, Lin, Wang, Shang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenbin Zhang, MzMxMzAxMUB6anUuZWR1LmNu; Min Shang, bWluc2hhbmdAemp1LmVkdS5jbg==
†These authors have contributed equally to this work
 Zhezhe Chen
Zhezhe Chen Hangpan Jiang3†
Hangpan Jiang3† Duanbin Li
Duanbin Li Min Wang
Min Wang Min Shang
Min Shang Wenbin Zhang
Wenbin Zhang