- 1Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
- 2Department of Public Health Management, School of Public Health, Kabul University of Medical Sciences, Kabul, Afghanistan
- 3Obesity and Eating Habits Research Center, Endocrinology and Metabolism Molecular-Cellular Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
- 4Food Security Research Center, Department of Community Nutrition, School of Nutrition and Food Science, Isfahan University of Medical Sciences, Isfahan, Iran
Background: Despite the adherence to the Mediterranean dietary pattern (MD) being associated with a reduced risk of several cancers, there is no report about the highly prevalent diet-disease associations in Afghanistan, particularly about gastric cancer (GC).
Objective: The aim of this study was to investigate the association between MD and GC in Afghanistan.
Methods: This hospital-based case-control study was carried out on a total number of 270 subjects (90 cases and 180 controls) aged between 20 and 75 years. Using the convenience-sampling method, cases and controls were selected. Cases were patients with GC whose condition was pathologically confirmed. The controls were apparently healthy people who were matched with cases in terms of age (±5 years) and sex. Assessment of dietary intake was done using a pre-tested food frequency questionnaire, designed specifically for Afghanistan. Adherence to the MD pattern was done based on the scores suggested in earlier studies.
Results: Out of 270 studied subjects, 73% were men. We found that subjects in the highest tertile of MD score had 52% decreased odds of GC (OR: 0.48; 95% CI: 0.24–0.98, P-trend = 0.05) compared with those in the lowest tertile. After considering potential environmental factors, age, and sex, the observed association disappeared (OR: 0.43; 95% CI: 0.13–1.38, P-trend = 0.41). After further adjustment for BMI in the last model, we found that participants with the highest MD score were 83% less likely to have GC than those in the lowest tertile (OR: 0.17; 95% CI: 0.03–0.80, P-trend = 0.14).
Conclusion: We found that greater adherence to MD might be associated with a lower odds of GC.
Introduction
Gastric cancer (GC) is one of the most common malignancies in the world; however, its prevalence has steadily declined over the past 50 years (1). Despite this reduction, GC is still the fifth most common cancer and the third most prevalent cause of cancer-related mortality (2). GC is highly prevalent in developing countries (3). Based on the recent WHO report, GC is the second most common cancer among Afghan men and the fourth in Afghan women (4).
Several lifestyle-related factors have been known to affect the risk of GC (4, 5). Among dietary factors, earlier studies have mostly focused on individual nutrients, while evaluating dietary patterns might be a more informative approach to clarify the link between nutrition and cancer (6). Mediterranean dietary pattern (MD) is characterized by high consumption of fruits, vegetables, whole grains, legumes, fish and seafood, nuts and seeds, olive oil as the main fat source, moderate alcohol consumption (particularly red wine), relatively low consumption of dairy products (mainly cheese and yogurt), and red and processed meat (7, 8). A recent systematic review and meta−analysis of observational studies provided evidence that greater adherence to the MD is associated with a lower risk of overall cancer-related deaths as well as lower incidence of colorectal, breast, prostate, liver, head and neck, and GC (9).
Most studies on the link between dietary factors and GC are limited to developed nations as limited information is available in developing countries, especially in Afghanistan. Given the particular nature of dietary intakes in Afghanistan along with the high prevalence of GC in this country (10, 11), it seems that investigating diet–GC relations in this country might move the field forward by providing additional information in this regard. Therefore, this study aimed to examine the association between adherence to the Mediterranean diet and the risk of GC in Afghanistan.
Materials and Methods
Study Participants
This hospital-based case-control study was carried out on a total number of 270 subjects aged between 20 and 75 years in Kabul, Afghanistan, in 2019. The sample size was calculated based on the formula for case–control studies (12). We hypothesized that almost 50% of Afghan adults are consuming unhealthy dietary patterns (high in fat and carbohydrate), so we assumed that such a dietary pattern might provide a 2.5 times greater risk of GC (13–15). Considering the type I error of 5%, study power of 80% (β = 0.2), and the ratio of cases to controls as 2, we reached 90 cases and 180 controls. A total of 90 new cases with GC who were pathologically diagnosed with cancer within the last month and 180 healthy controls who were matched with cases in terms of age (±5) and sex were selected. We excluded participants with a history of pathologically confirmed cancer (except for GC) or other types of cancer. Those with any type of other confirmed cancers (except GC) were excluded from the study. The study participants were matched in terms of age (±5 years) and sex. All study participants signed an informed written consent form before the initiation of data collection. The study was ethically approved by the medical bioethics committee of TUMS (Code: IR.TUMS.MEDICINE.REC.1399.184).
Assessment of Dietary Intakes
Participants’ usual dietary intakes during the past year were examined by a pre-tested Willett-format food frequency questionnaire (FFQ), that was designed specifically for the Afghan population. The questionnaire included 103 food items, with standard portion sizes according to Afghan common dietary intakes. The FFQ was completed through face-to-face interviews by a trained interviewer in the presence of individuals who were involved in the preparation and cooking of foods. All reported consumption frequencies were converted to grams per day by using household measures. Daily intakes of energy and nutrients were calculated for each person by using the USDA food consumption database. Almost all foods included in the questionnaire were available in the database, whereas for those foods not available in the database, similar ones were considered. Similar foods were chosen based on similarities in macronutrients (proteins, carbohydrate, and fats). For example, we put the information for meat for Pacha (leg meat).
Adherence to the Mediterranean Diet
We calculated MD score based on nine components [fruits, vegetables, fish, legumes, nuts, whole grains, the ratio of monounsaturated fatty acids (MUFAs) to saturated fatty acids (SFAs), meats (red meat, poultry, and proceed meats), and dairy products] as mentioned in earlier studies (16, 17). Participants received a score of 1 if they were above median intakes of fruits, fish, vegetables, legumes, nuts, whole grains, and the ratio of MUFA to SFA and below-median intakes of meats and dairy. They received 0 if their intake were more than the median of meats (red meat, poultry, and proceed meats) and dairy and less than the median intakes of fruits, fish, vegetables, legumes, nuts, whole grains, and the ratio of MUFA to SFA. The overall Mediterranean diet score was calculated by summing up the scores of each component. The range of MD scores was 0–9, with a higher score representing greater adherence to the MD.
Ascertainment of Gastric Cancer
The diagnosis of GC was confirmed based on the pathological test using the third edition of the International Classification of Diseases for Oncology (ICDO-3) and morphology codes 8490/3 (18, 19). We only enrolled GC patients who had been diagnosed for at most one year before the date of the interview.
Assessment of Other Variables
A pre-tested questionnaire was used to collect data on demographic characteristics including age, BMI, physical activity, sex, marital status, education level, occupation, smoking status, alcohol consumption, tooth brushing (times per week), and kebab food consumption. By using an International Physical Activity Questionnaire (IPAQ), we assessed the physical activity of participants through the face-to-face interviews. The results of the IPAQ were expressed as Metabolic Equivalents per week (METs/week). A trained dietitian completed all measurements. Weight was measured to the nearest 0.1 kg using a digital scale (Seca, Hamburg, Germany) with minimal clothes and without shoes. By the use of a tape measure, we measured the height of participants in a standing position without wearing shoes to the nearest 0.1 cm. BMI was calculated as weight (kg) divided by height in (m2).
Statistical Analysis
We categorized participants based on tertiles of the Mediterranean diet scores. The chi-square test was used to assess the distribution of categorical variables across tertiles of Mediterranean diet scores. We applied ANOVA for continuous variables to compare general characteristics of participants across tertiles of Mediterranean diet scores. For assessment of food and nutrients intakes of study participants across tertiles of MD score, we used analysis of covariance (ANCOVA) which was adjusted for age, sex, and total energy intake. To examine the association between Mediterranean diet scores and GC, we used binary logistic regression in three different models. First, we adjusted for age (continuous), and sex. Further adjustments were done for physical activity (continuous), marital status (married/not married), Kebab food consumption (yes/no), smoking (yes/no), tooth brushing (do not brush, brush), job status (former and worker, others), education (non-university graduate, university graduate), and alcohol use (yes/no) in the second model. To reach the obesity–independent relationships, further controlling was made for BMI in the final model. In all statistical analyses, the first tertile of Mediterranean diet score was used as the reference category. To obtain the overall trend of odds ratios across increasing tertiles of Mediterranean diet score, we considered tertiles as an ordinal variable in the logistic regression models. All statistical analyses were conducted using SPSS software version 25 (SPSS Inc., Chicago, IL, United States). P-values less than 0.05 were considered statistically significant.
Results
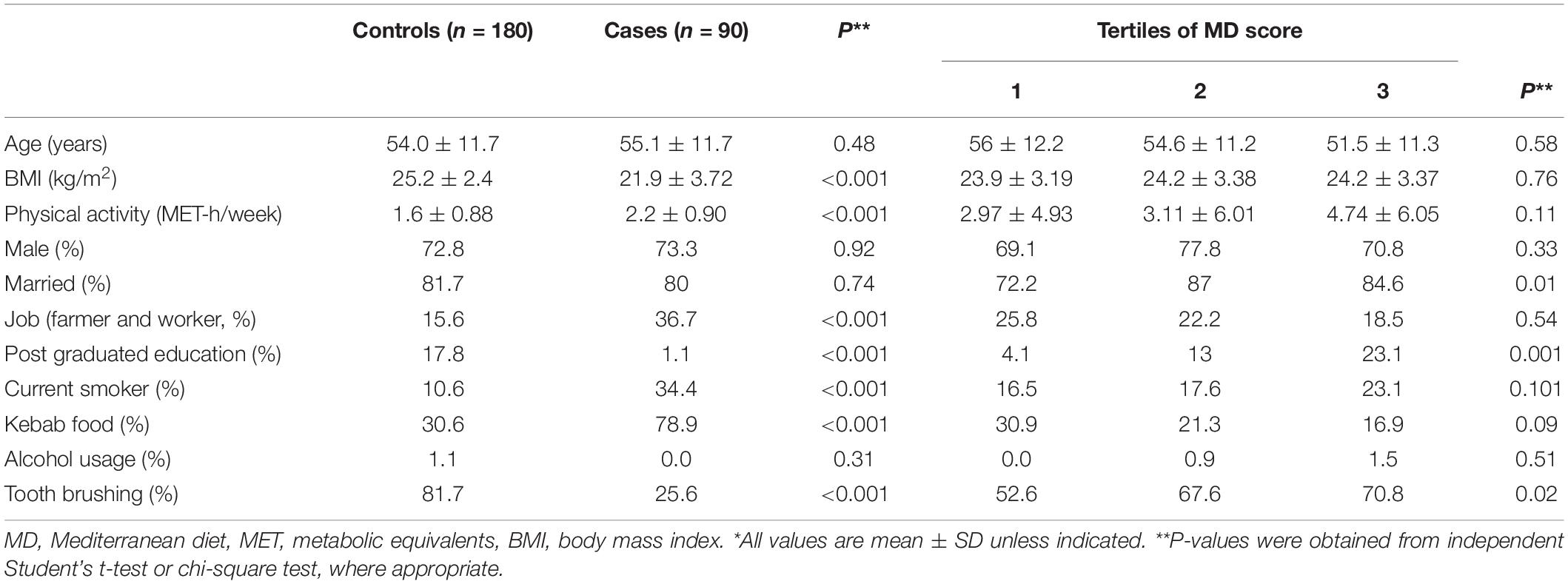
Compared to controls, cases were more physically active (METs) (2.2 ± 0.9 vs. 1.6 ± 0.88, P ≤ 0.001) and more likely to be farmer and worker (36.7 vs. 15.6%, P ≤ 0.001), be current smokers (34.4 vs. 10.6%, P ≤ 0.001), and consume kebab food (78.9 vs. 30.6%, P ≤ 0.001). Also, cases had a lower mean of BMI (21.9 ± 3.72 vs. 25.2 ± 2.4, P ≤ 0.001), less likely to be university post-graduated (1.1 vs. 17.8%, P ≤ 0.001), and do tooth brushing (25.6 vs. 81.7%, P ≤ 0.001). There were no other significant differences in other variables between cases and controls.
General characteristics of study subjects across tertiles of MD score are shown in Table 1. Compared with those with the lowest score, participants who had higher MD scores were more likely to have post-graduate education and brush their teeth. Those in the top tertile of MD score were more likely to be married than those in the bottom tertile. There were no other significant differences in terms of mean age, BMI, and participants’ distribution in terms of categorical variables across the MD score.
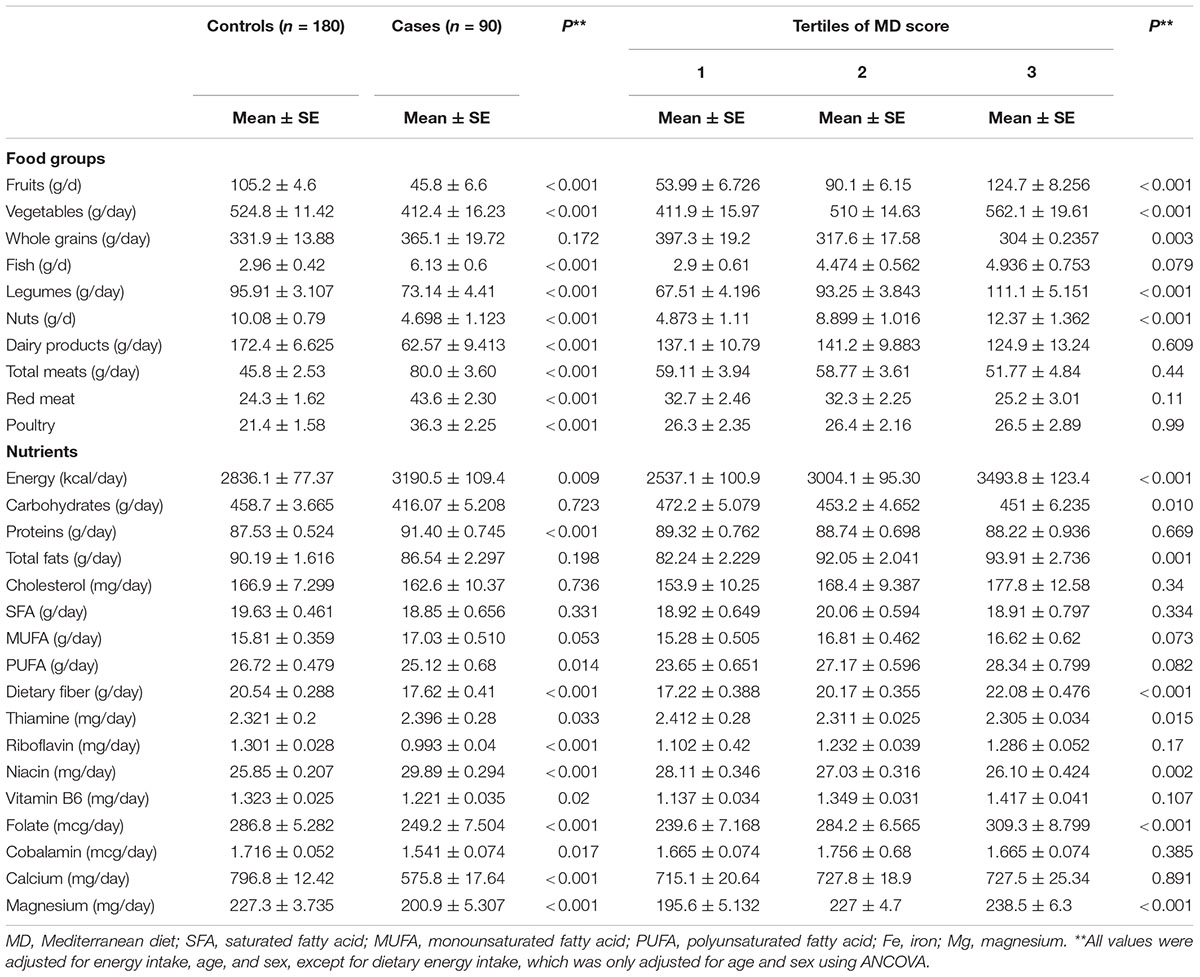
Compared to controls, patients with GC had higher consumption of fish (6.13 ± 0.6 vs. 2.96 ± 0.42, P ≤ 0.001), meat products (59.65 ± 2.955 vs. 31.23 ± 2.08, P ≤ 0.001), total energy (3190.5 ± 109.4 vs. 2836.1 ± 77.37, P = 0.009), protein (91.4 ± .745 vs. 87.53 ± 0.524, P ≤ 0.001), MUFA (17.03 ± 0.51 vs. 15.81 ± .359, P = 0.053), and vitamins B1 (2.396 ± .28 vs. 2.321 ± 0.2, P = 0.033), B3 (29.89 ± 0.294 vs. 25.85 ± 0.207, P ≤ 0.001) and the had lower intakes of fruit (45.8 ± 6.6 vs. 105.2 ± 4.6, P ≤ 0.001), vegetables (412.4 ± 16.23 vs. 524.8 ± 11.42, P ≤ 0.001), nuts (4.698 ± 1.123 vs. 10.08 ± .79, P ≤ 0.001), legumes (73.14 ± 4.41 vs. 95.91 ± 3.107, P ≤ 0.001), dairy products (62.57 ± 9.413 vs. 172.4 ± 6.625, P ≤ 0.001), PUFA (25.12 ± .68 vs. 26.72 ± 0.479, P = 0.014), dietary fiber (17.62 ± 0.41 vs. 20.54 ± 0.288, P ≤ 0.001), vitamin B2 (0.993 ± .04 vs. 1.301 ± 0.028 P ≤ 0.001), B6 (1.221 ± 0.035 vs. 1.323 ± 0.025, P = 0.02), B9 (249.2 ± 7.504 vs. 286.8 ± 5.282, P ≤ 0.001), B12 (1.541 ± 0.074 vs. 1.716 ± 0.052, P = 0.017), calcium (575.8 ± 17.64 vs. 796.8 ± 12.42, P ≤ 0.001), and magnesium (200.9 ± 5.307 vs. 227.3 ± 3.735, P ≤ 0.001). Food and nutrients intakes of study participants across tertiles of MD score are presented in Table 2. Individuals in the highest tertile of MD score had higher consumption of fruit, vegetables, fish, legumes, nuts, total energy, total fat, dietary fiber, folate, magnesium and lower intakes of whole grain, carbohydrates, and niacin compared to those in the lowest tertile.
Furthermore, four levels of multivariable-adjusted ORs for GC across tertiles of MD score are shown in Table 3. In the crude model, subjects in the highest tertile of MD score had 52% decreased odds of GC (OR: 0.48; 95% CI: 0.24–0.98, P-trend = 0.05) compared with those in the lowest tertile. After adjustment for age and sex in the first model, this protective association became slightly attenuated (OR: 0.49; 95% CI: 0.24–1.01, P-trend = 0.06). After further adjustment for potential environmental confounders, there was no significant association between adherence to MD score and GC (OR: 0.43; 95% CI: 0.13–1.38, P-trend = 0.41). When we included BMI in the last model, we found that participants with the highest MD score were 83% less likely to have GC than those in the lowest tertile (OR: 0.17; 95% CI: 0.03–0.8, P-trend = 0.14).
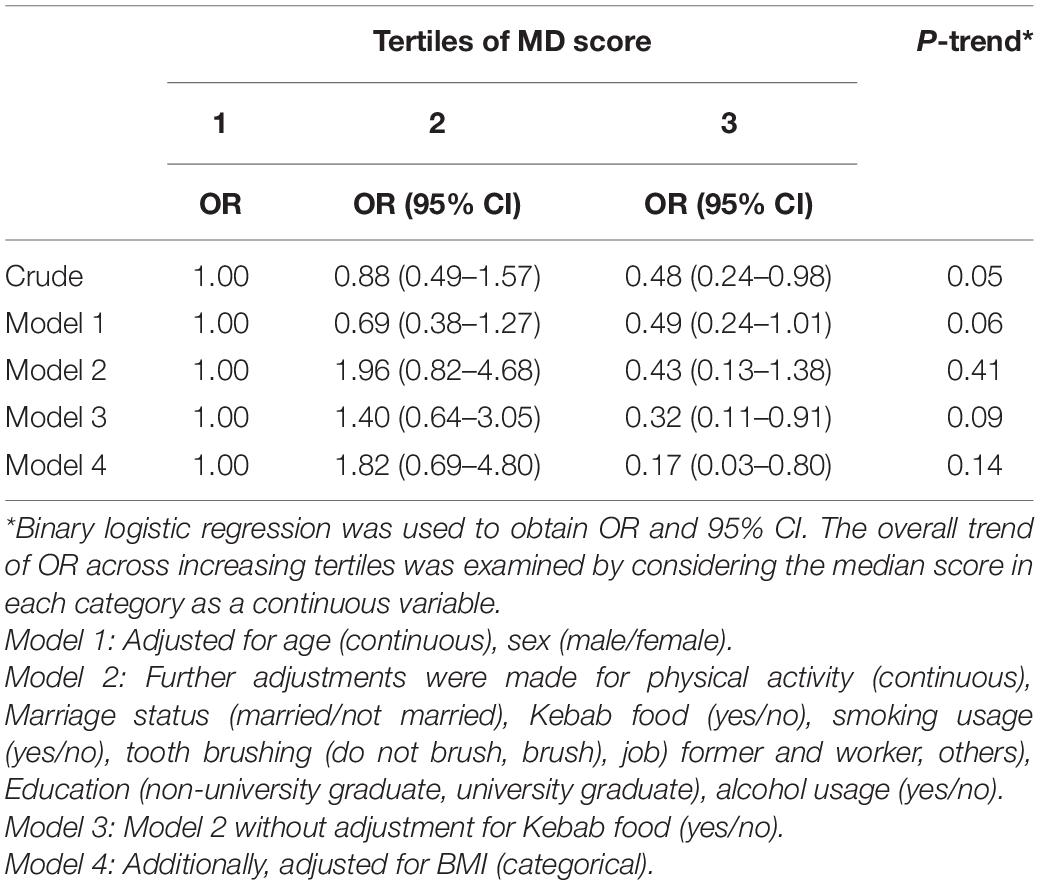
Table 3. Odds ratios (ORs) and 95% CIs of gastric cancer according to tertiles of the Mediterranean dietary score.
Discussion
In this case–control study, we found that individuals with the greatest adherence to the Mediterranean diet had lower odds of GC than those with the lowest adherence. To the best of our knowledge, this is the First study in Afghanistan that examined the association between MD patterns and GC.
Gastric cancer is the third leading cause of cancer-related death globally. According to the World Cancer Research Fund, the incidence of stomach cancer was 6.1% worldwide in 2018 (2, 20). MD is linked to a lower risk of different chronic conditions including overall cancer incidence (21). In the current study, we found that participants with the highest adherence of MD score were 83% less likely to have GC than those with the lowest adherence. In line with our findings, an updated systematic review and meta-analysis on adherence to Mediterranean diet and risk of different cancers indicated that higher adherence to the MD was related to a lower risk of cancer mortality in the general population, and all-cause mortality among cancer survivors as well as colorectal, head and neck, respiratory, gastric, liver and bladder cancer risks (22). The observed associations are mainly explained by higher intakes of fruits, vegetables, and whole grains (23, 24). An earlier cohort study in the Netherlands showed that higher adherence to MD pattern was associated with reduced risks of esophageal and GC (24). In another cohort study that included 485,044 subjects (144,577 men) aged 35–70 years old from 10 European countries, after 8.9 years of follow-up (HR: 0.67; 95% CI: 0.47–0.94), higher adherence to MD was associated with a significant lower risk of incident GC (13). Higher scores of MD were also associated with a significantly lower risk of overall cancer mortality (by approximately 13%) as well as the incidence of GC (by 27%) in a meta-analysis (23). In addition, findings of a hospital-based case-control study in Iran demonstrated that a high-quality diet, that assessed by Healthy Eating Index-2010 and Mediterranean Style Dietary Pattern, was inversely associated with the risk of colorectal cancer (25). Similar findings were also reported from Italy (26). Overall, adherence to MD pattern seems to have beneficial effects on human health in particular against the incidence of GC. As this dietary pattern is more usual in Mediterranean countries, conducting studies in other countries like developing countries such as Afghanistan might be a very valuable step for moving the nutrition field forward in this regard.
With regard to the mechanisms through which the Mediterranean diet might affect the risk of GC, there are several foods in the context of this dietary pattern that can help reduce the risk of cancer. Several mechanisms include reducing the growth of tumor cells (e.g., fish consumption), increasing the chemo-protective effects (i.e., olive oil), and inhibiting tumor development (i.e., dairy products), anti-oxidative and anti-inflammatory effects (fruit, vegetables, and olive oil consumption) (27) might be involved in this process. In addition, antioxidants from this dietary pattern can reduce oxidative DNA damages eliminating free radicals and taking part in many biological changes linked with all cancers (e.g., bioactivation of carcinogens, cell signaling, cell regulation circle, angiogenesis, and inflammation). In stomach neoplasia, a high intake of fresh fruit and vegetable in this dietary pattern may reduce the negative effects of Helicobacter pylori and its consequent damages (28). Red meat and its process methods have been reported to be associated with an increased risk of GC (29).
The strengths of our study are being the first study in Afghan adults as well as considering a wide range of confounders. Some potential limitations should also be taken into account while interpreting our findings. Given the case–control design of the study, having recall bias and selection bias is unavoidable. In addition, causality cannot be inferred based on our findings due to the case-control design of the study. Because of the use of FFQ to assess dietary intakes, misclassification of study participants might have occurred. We tried our best to consider lots of confounders in the study; however, residual confounding cannot be ignored. Although we determined the sample size based on the suggested formula for case–control studies, larger studies seem to be required to confirm our findings. Finally, we did not consider sodium intake as a confounding factor, even though previous studies showed that the Mediterranean diet patterns have a limited effect on restricting sodium intake (30).
In conclusion, in this hospital-based case-control study we found that higher adherence to MD might be associated with a lower odds of GC. Further studies are needed to confirm this association.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, on reasonable request to the corresponding author.
Ethics Statement
This study was ethically approved by medical bioethics committee of TUMS (Code: IR.TUMS.MEDICINE.REC. 1399.184). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AE and SM were involved in the study’s conception, design, statistical analysis, and interpretation of the data. FA and AB were involved in data collection, data cleaning, statistical analysis, and manuscript drafting. AE supervised the study. All authors approved the final manuscript for submission.
Funding
The financial support for this study was provided by TUMS.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Balakrishnan M, George R, Sharma A, Graham DY. Changing Trends in stomach cancer throughout the world. Curr Gastroenterol Rep. (2017) 19:36. doi: 10.1007/s11894-017-0575-8
2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. (2018) 68:394–424.
3. Sipponen P, Correa P. Delayed rise in incidence of gastric cancer in females results in unique sex ratio (M/F) pattern: etiologic hypothesis. Gastr Cancer. (2002) 5:213–9. doi: 10.1007/s101200200037
4. Praud D, Bertuccio P, Bosetti C, Turati F, Ferraroni M, La Vecchia C. Adherence to the Mediterranean diet and gastric cancer risk in Italy. Int J Cancer. (2014) 134:2935–41.
5. Bertuccio P, Rosato V, Andreano A, Ferraroni M, Decarli A, Edefonti V, et al. Dietary patterns and gastric cancer risk: a systematic review and meta-analysis. Ann Oncol Off J Eur Soc Med Oncol. (2013) 24:1450–8.
6. Mousavi SM, Shayanfar M, Rigi S, Mohammad-Shirazi M, Sharifi G, Esmaillzadeh A. Adherence to the Mediterranean dietary pattern in relation to glioma: a case–control study. Clin Nutr. (2021) 40:313–9. doi: 10.1016/j.clnu.2020.05.022
7. Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, et al. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr. (1995) 61:1402s–6s. doi: 10.1093/ajcn/61.6.1402S
8. Trichopoulou A, Lagiou P. Healthy traditional Mediterranean diet: an expression of culture, history, and lifestyle. Nutr Rev. (1997) 55:383–9. doi: 10.1111/j.1753-4887.1997.tb01578.x
9. Schwingshackl L, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: an updated systematic review and meta-analysis of observational studies. Cancer Med. (2015) 4:1933–47. doi: 10.1002/cam4.539
11. Nagini S. Carcinoma of the stomach: a review of epidemiology, pathogenesis, molecular genetics and chemoprevention. World J Gastroint Oncol. (2012) 4:156. doi: 10.4251/wjgo.v4.i7.156
12. Edwardes MD. Sample size requirements for case-control study designs. BMC Med Res Methodol. (2001) 1:11. doi: 10.1186/1471-2288-1-11
13. Buckland G, Agudo A, Luján L, Jakszyn P, Bueno-de-Mesquita HB, Palli D, et al. Adherence to a Mediterranean diet and risk of gastric adenocarcinoma within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. Am J Clin Nutr. (2010) 91:381–90. doi: 10.3945/ajcn.2009.28209
14. Ye Y, Wu Y, Xu J, Ding K, Shan X, Xia D. Association between dietary carbohydrate intake, glycemic index and glycemic load, and risk of gastric cancer. Eur J Nutr. (2017) 56:1169–77. doi: 10.1007/s00394-016-1166-4
15. Hu J, La Vecchia C, Negri E, de Groh M, Morrison H, Mery L, et al. Macronutrient intake and stomach cancer. Cancer Caus Control. (2015) 26:839–47. doi: 10.1007/s10552-015-0557-9
16. deKoning L, Anand SS. Adherence to a Mediterranean diet and survival in a Greek population. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. N Engl J Med 2003; 348: 2599-608. Vasc Med (Lond Engl). (2004) 9:145–6. doi: 10.1191/1358863x04vm552xx
17. Sadeghi O, Keshteli AH, Afshar H, Esmaillzadeh A, Adibi P. Adherence to Mediterranean dietary pattern is inversely associated with depression, anxiety and psychological distress. Nutr Neurosci. (2019) 348:1–12.
18. Yang D, Hendifar A, Lenz C, Togawa K, Lenz F, Lurje G, et al. Survival of metastatic gastric cancer: significance of age, sex and race/ethnicity. J Gastroint Oncol. (2011) 2:77. doi: 10.3978/j.issn.2078-6891.2010.025
19. Fritz AG. International Classification of Diseases for Oncology: ICD-O. Geneva: World Health Organization (2013).
20. Chan DSM, Abar L, Cariolou M, Nanu N, Greenwood DC, Bandera EV, et al. World Cancer research fund international: continuous update project-systematic literature review and meta-analysis of observational cohort studies on physical activity, sedentary behavior, adiposity, and weight change and breast cancer risk. Cancer Causes Control. (2019) 30:1183–200. doi: 10.1007/s10552-019-01223-w
21. Benetou V, Trichopoulou A, Orfanos P, Naska A, Lagiou P, Boffetta P, et al. Conformity to traditional Mediterranean diet and cancer incidence: the Greek EPIC cohort. Br J Cancer. (2008) 99:191–5. doi: 10.1038/sj.bjc.6604418
22. Morze J, Danielewicz A, Przybyłowicz K, Zeng H, Hoffmann G, Schwingshackl L. An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer. Eur J Nutr. (2020) 2:1–26.
23. Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. (2017) 9:1063.
24. Schulpen M, Peeters PH, van den Brandt PA. Mediterranean diet adherence and risk of esophageal and gastric cancer subtypes in the Netherlands Cohort Study. Gastr Cancer Off J Int Gastr Cancer Associat Jpn Gastr Cancer Associat. (2019) 22:663–74. doi: 10.1007/s10120-019-00927-x
25. Jafari Nasab S, Bahrami A, Rafiee P, Hekmatdoust A, Ghanavati M, Rashidkhani B, et al. Healthy eating index-2010 and Mediterranean-style dietary pattern score and the risk of colorectal cancer and adenoma: a case-control study. Nutr Cancer. (2020) 72:1326–35. doi: 10.1080/01635581.2019.1683212
26. Stojanovic J, Giraldi L, Arzani D, Pastorino R, Biondi A, Persiani R, et al. Adherence to Mediterranean diet and risk of gastric cancer: results of a case-control study in Italy. Eur J Cancer Prevent Off J Eur Cancer Prevent Organ (ECP). (2017) 26:491–6. doi: 10.1097/CEJ.0000000000000371
27. Grosso G, Buscemi S, Galvano F, Mistretta A, Marventano S, La Vela V, et al. Mediterranean diet and cancer: epidemiological evidence and mechanism of selected aspects. BMC Surg. (2013) 13, (Suppl. 2):S14. doi: 10.1186/1471-2482-13-S2-S14
28. Castelló A, Boldo E, érez-Gómez BP, Lope V, Altzibar JM, Martín V, et al. Adherence to the Western, Prudent and Mediterranean dietary patterns and breast cancer risk: MCC-Spain study. Maturitas. (2017) 103:8–15. doi: 10.1016/j.maturitas.2017.06.020
29. Hernández-Ramírez RU, ópez-Carrillo LL. [Diet and gastric cancer in Mexico and in the world]. Salud Pub Mexico. (2014) 56:555–60.
Keywords: diet, gastric cancer, Mediterranean diet (MD), case-control, Afghanistan
Citation: Amiry F, Mousavi SM, Barekzai AM and Esmaillzadeh A (2022) Adherence to the Mediterranean Diet in Relation to Gastric Cancer in Afghanistan. Front. Nutr. 9:830646. doi: 10.3389/fnut.2022.830646
Received: 07 December 2021; Accepted: 09 February 2022;
Published: 28 March 2022.
Edited by:
Maria Hassapidou, International Hellenic University, GreeceReviewed by:
Meghit Boumediene Khaled, University of Sidi-Bel-Abbès, AlgeriaTommaso Filippini, University of Modena and Reggio Emilia, Italy
Copyright © 2022 Amiry, Mousavi, Barekzai and Esmaillzadeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad Esmaillzadeh, YS1lc21haWxsemFkZWhAdHVtcy5hYy5pcg==
 Freshta Amiry
Freshta Amiry Seyed Mohammad Mousavi
Seyed Mohammad Mousavi Ahmad Mujtaba Barekzai1
Ahmad Mujtaba Barekzai1 Ahmad Esmaillzadeh
Ahmad Esmaillzadeh