- 1Department of Geriatric Medicine, Center of Coronary Circulation, Xiangya Hospital, Central South University, Changsha, China
- 2National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Central South University, Changsha, China
- 3Department of Cardiovascular Medicine, Xiangya Hospital, Central South University, Changsha, China
- 4Department of Cardiovascular Medicine, The Third Xiangya Hospital, Central South University, Changsha, China
Aims: To assess the associations of vitamin and/or nutritional supplements (VNS) with falls among patients with diabetes.
Methods: 9,141 and 21,489 middle-aged participants with diabetes from Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial and UK Biobank were included. Use of VNS was collected at baseline, and fall events were recorded using annual questionnaires in ACCORD and electric records in UK Biobank during follow-up. The associations of VNS use with fall risk were analyzed using logistic regression models in ACCORD and Fine-Gray sub-distribution hazard models in UK Biobank. The role of specific supplements was also estimated in UK Biobank, adjusting for confounding factors and multiple comparisons.
Results: 45.9% (4,193/9,141, 5.5 median follow-up years) patients in ACCORD and 10.5% (2,251/21,489, 11.9 median follow-up years) in UK Biobank experienced fall and in-patient events during follow-up, respectively. In ACCORD, VNS using was associated with an increased risk of fall (full-adjusted odds ratio [OR]: 1.26, P < 0.05). In UK Biobank, despite no significant association between VNS overall and in-patient fall, vitamin B, calcium, and iron using increased the risk of falls significantly (full-adjusted hazard ratio range: 1.31–1.37, P < 0.05).
Conclusions: Use of specific VNS increased the risk of fall among patients with diabetes. The non-indicative use of nutritional supplements for patients with diabetes might be inadvisable.
1. Introduction
Fall is a primary burden to older people (1). According to the Global Burden of Diseases Study 2019, falls caused over 0.6 million deaths of all ages globally and were recognized as one of the top-ten-ranking causes of disability-adjusted life-years for older people aged ≥75 years old (2). And fall is tightly associated with poor health outcomes and adverse social effects (3). Nearly 70% of community-dwelling, older adults suffered from physical injuries from a fall, and over one-third reported impaired function after falls (4, 5). Additionally, the worldwide prevalence of diabetes was estimated to be 9.3% in 2019 (6). The prevalent chronic disease increases the risk of falling epidemiologically. According to a meta-analysis by Yang et al. (7), older patients with diabetes had a profoundly increased incidence of falls than diabetes-free people, and a similar tendency was observed among young patients with well-treated type 2 diabetes from the Maastricht Study (8).
The supplementation of vitamin D and calcium has been suggested in multifactorial strategies to prevent injurious falls (9). The preventive role of vitamin supplements, especially vitamin D, in falls has been studied in plenty of randomized, controlled trials (RCTs); however, the conclusions were conflicted. Although in a meta-analysis based on 5 RCTs, Heike et al. (10) found that vitamin D reduced the risk of fall among older people, independent of calcium supplementation, Mark et al. (11) suggested that vitamin D, when were applied as mono-supplement, exhibited no significant effect on falls, hip fractures, and total fractures, irrespective of the doses used. Another recent meta-analysis involving 47 RCTs showed that vitamin D supplementation prevented falls significantly when applied in combination with calcium (12). However, the result that high-dose vitamin D supplementation was associated with a higher risk of falls and fractures was observed (13, 14). Additionally, no other types of vitamin/mineral supplements have been reported to have significant effects on physical function and the risk of fall (15–18). Up till now, most studies about the role of vitamin supplements in falls are RCTs that concentrated on the potential effects of vitamin and/or nutrition treatment in specific types and doses. The settings of these intervention studies are different from the “real world” in which the use of multiple or multi-vitamin/mineral products are common (19). Although routine vitamin supplement is not recommended by current guidelines for patients with diabetes (20, 21), we noticed that nearly 33% of participants in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial used vitamin and/or nutritional supplements (VNS) at baseline, and the proportion was 47.0% among participants with diabetes in UK Biobank. These data provide an opportunity to evaluate the potential association between VNS and the risk of fall in patients with diabetes, which has not been addressed in any clinical trials.
Therefore, we performed a post-hoc analysis utilizing data from ACCORD trial to assess the association between VNS and fall incidence among patients with type 2 diabetes, verified their associations and specified the role of individual supplements in UK Biobank.
2. Materials and methods
2.1. Study design and population
Both ACCORD and UK Biobank have been described previously (22, 23). ACCORD trial is a multicenter RCT with a double factorial design that enrolled 10,251 participants aged 40–79 years with type 2 diabetes at a high risk for cardiovascular diseases (CVD) events from 77 clinical sites in the U.S. and Canada. Among 9,620 participants of ACCORD, 9,141 participants with available information in VNS, fall records, and covariates were enrolled in our primary analyses. UK Biobank is a large population-based, prospective cohort study, recruiting over 0.5 million participants aged between 40 and 69 years old from 2006 to 2010 across the U.K. We involved patients with diabetes at baseline (n = 27,736) and excluded those with hospital inpatient history of fall (n = 810) or missing information in the exposure, outcome, or covariates used (n = 5,437), leaving 21,489 participants involved in the second-step analyses. In UK Biobank, the status of diabetes at baseline was derived in aggregation of self-reported medical history, insulin use, and inpatient diagnoses recorded by International Classification of Diseases, 9th revision [ICD-9] and ICD-10 (details in Supplementary Table S1). Analyses based on ACCORD has been approved by the National Heart, Lung, and Blood Institute and the institutional review board of Xiangya Hospital, Central South University. UK Biobank has been approved by the National Health Service (NHS) National Research Ethics Service (approval letter dated 17th June 2011, Ref 11/NW/0382), and this study has been conducted using the UK Biobank resource under the project number 76118. Written informed consents have been provided by the participants in both databases.
2.2. Ascertainment of exposures and outcomes
In ACCORD, information on VNS use and fall outcomes were collected from annual questionnaires since 2001, in which participants were asked whether they used VNS or not and the occurrences of any falls in the previous 12 months. In the questionnaires, “Vitamins and/or nutritional supplements” was provided as an option in “Miscellaneous Non-prescribed Therapies,” and fall was defined as “fallen or landed on the floor or ground, or fallen and hit an object like a table or stair.” Participants were classified according to whether they received VNS or not (non-VNS) at baseline. And the occurrences of any falls reported during follow-up were recorded as the outcome.
In UK Biobank, information in VNS use was derived from touchscreen questionnaires finished at recruitment. For vitamin, mineral, and other supplements, participants were asked, “Do you regularly take any of the following? (You can select more than one answer),” with specific supplements including vitamin A, vitamin B, vitamin C, vitamin D, vitamin E, folate (Vit B9), fish oil, glucosamine, calcium, zinc, iron, selenium, and multivitamins ± minerals listed as options. Participants who selected ≥1 supplements were defined with VNS use. Regular use of specific supplements was also recorded according to corresponding options selected. The first occurrence and date of inpatient fall was derived from electric health-related records coded by ICD-9 (E880-E888) and ICD-10 (W00-W19).
2.3. Ascertainment of covariates
In ACCORD and UK Biobank, baseline information in demographic factors, lifestyles, and medical history was collected from standardized questionnaires, and anthropometric and biochemical parameters were also measured (details in Supplementary Table S2). In ACCORD, blood pressure, Michigan Neuropathy Screening Instrument (MNSI) score, and Health Utilities Index Mark3 (HUI3) score (an aggregate score of vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain) were measured by trained technicians. And type 2 diabetes was defined according to the 1997 American Diabetes Association criteria (22). Townsend Deprivation Index was calculated in UK Biobank and reflected the levels of deprivation (24). Body mass index (BMI, kg/m2) was calculated as the body weight (kg) divided by the square of height (m2). Diet was assessed by a healthy diet score (1 [more advisable]; 0 [less advisable]) adopted from the American Heart Association Guidelines (Supplementary Table S2) (25). For the assessment of frailty status, we used five frailty phenotype items defined by Fried et al. (26, 27): (1) Weight loss; (2) Exhaustion; (3) Physical activity; (4) Walking speed; and (5) Grip strength. The history of other cardiometabolic diseases, osteoporosis, and diabetic complications related to falls at baseline was also ascertained according to self-reported medical history and electrical health records (seen in Supplementary Table S1). In touchscreen questionnaires completed at recruitment, participants were asked, “In the last year have you had any falls?,” and people who answered “Only one fall” or “More than one fall” were thought to have recent fall history.
2.4. Statistical analysis
For both ACCORD and UK Biobank, we classified participants according to the use of VNS at baseline, and described the distribution of population characteristics respectively. Continuous variables with normal and abnormal distribution were expressed as mean (standard deviation [SD]) and median (interquartile range [IQR]), respectively, and categorical variables were expressed as number (percentage, %). Unpaired Student t-tests, Kruskal tests, and Chi-square tests were applied conditionally to compare the features of participants between the two groups.
In ACCORD trial, the association between VNS and fall outcome was assessed by logistic regression models, since the affirmatory timepoints of outcome were not available. 3 settings of models were fitted: model 1 was adjusted for age, sex, and race, model 2 was additionally adjusted for education, smoking status, and alcohol consumption, and model 3 was further adjusted for BMI, systolic, and diastolic blood pressure, MNSI score, HUI3 score, diabetes duration, level of hemoglobin A1c (HbA1c), history of foot ulcer requiring antibiotics, CVD, heart failure risk, and randomization arms.
Then we verified the association between VNS use and in-patient falls among patients with diabetes in UK Biobank, utilizing Fine-Gray sub-distribution hazard models, which accounted for the competing risk of death. The role of specific supplements including vitamins, mineral, and dietary supplements in the occurrences of in-patient fall was also studied in competing risk models, respectively. The models were fitted with 3 settings: model 1 (adjusted for age, sex, and race); model 2 (additionally adjusted for Townsend Deprivation Index, smoking status, alcohol consumption, diet, sleep duration, and five frailty phenotypes); model 3 (further adjusted for BMI, level of HbA1c, history of other cardiometabolic diseases, osteoporosis, and diabetic complications, and recent falls). To offset the imbalance in distribution of population characteristics in both databases, we calculated propensity scores for the use of VNS using logistic regression, matched the two groups using the nearest neighbor matching method (ratio 1:1), and reperformed the analyses in ACCORD and UK Biobank. In addition, we performed several sensitivity analyses to test the robustness of our results. Firstly, to reduce the potential effects of reverse causality, we excluded participants with self-reported ≥2 falls in the previous year at baseline, since they were at a higher risk of fall constitutionally. Secondly, we substituted the five frailty items with an aggregated variable frailty status. Patients who met no criteria were defined as non-frail, 1 or 2 criteria as pre-frail, and ≥3 criteria as frail. Thirdly, missing information in covariates involved was imputed with multiple imputation by chained equations. Fourthly, we excluded patients with diabetic complications at recruitment. Fifthly, we excluded patients who experienced inpatient fall during the first year of follow-up to account for reverse causality.
All analyses were conducted using R software, version 4.1.0. All P-values in our analyses were two-sided, and Benjamini and Hochberg (BH) method was used in analyses based on UK Biobank to account for multiple comparison. It was considered statistically significant when P-values < 0.05.
3. Results
3.1. ACCORD
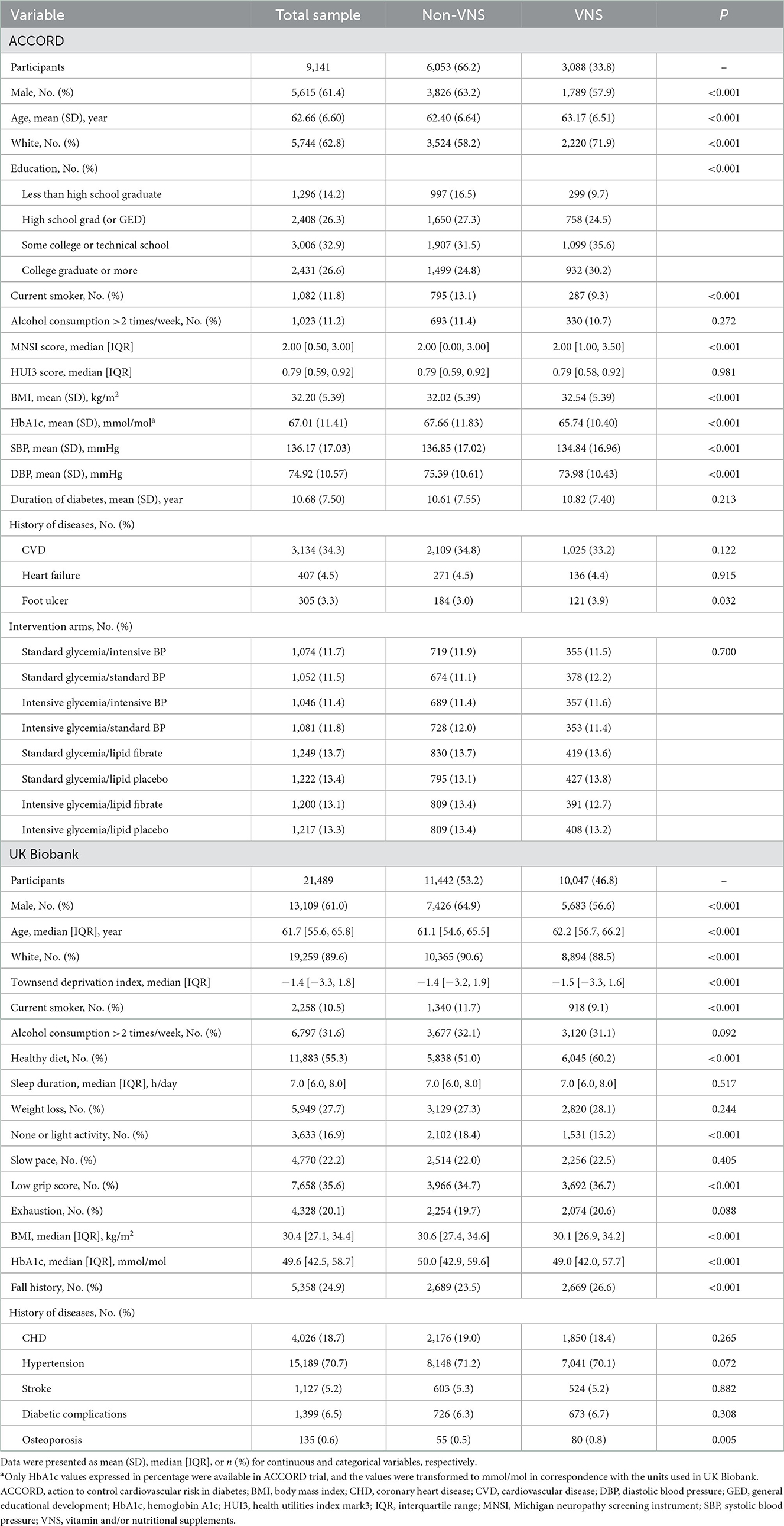
Of 9,141 enrolled patients, the mean (SD) age was 62.66 (6.60) years and 5,615 (61.4%) were male. Compared with those who did not receive VNS, participants who used VNS were more likely to be female, older, white race, and highly educated; more likely to have higher BMI, lower HbA1c and blood pressure levels (Table 1). A propensity matching was performed and 5,984 participants were identified, with 2,992 in each group (Supplementary Table S3).
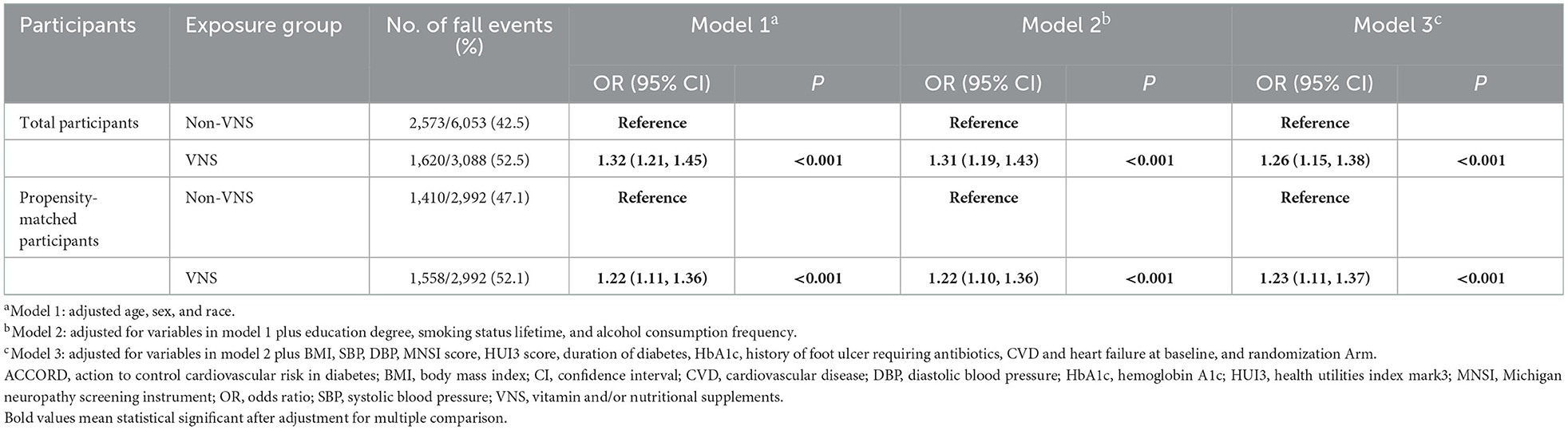
During the median 5.5 years of follow-up, 52.5% (1,620/3,088) and 42.5% (2,573/6,053) patients with and without VNS use occurred at least one fall, respectively. According to the results in total participants (Table 2), using VNS was related to an increased risk of fall among patients with diabetes in model 1 (odds ratio [OR]: 1.32, 95% confidence interval [CI] 1.21–1.45). The association was attenuated but remained significant after multivariable adjustments in model 2 and 3 (full-adjusted OR: 1.26, 95% CI 1.15–1.38). After propensity-matching, VNS using was also significantly associated with an increased risk of fall in patients with diabetes before and after multivariable adjustments (full-adjusted OR: 1.23, 95% CI 1.11–1.37).
3.2. UK Biobank
Characteristics of the participants from UK Biobank are also presented in Table 1. Of 21,489 participants, the median [IQR] age was 61.7 [55.6, 65.8] years and 13,109 (61.0%) were male (Table 1). At baseline, 10,047 (46.8%) patients regularly used VNS, in which 6,071 habitually used vitamins (448 for vitamin A, 1,020 for vitamin B, 1,616 for vitamin C, 738 for vitamin D, 587 for vitamin E, and 617 for folate) and 8,387 habitually used mineral supplements. Compared with non-users, participants who used VNS were more likely to be female, older, non-white and less deprived. They were prone to have healthier lifestyles, fatigue phenotypes, lower BMI, lower HbA1c levels, and fall history. After propensity matching, 18,222 participants were identified, with 9,111 in each group (Supplementary Table S3).
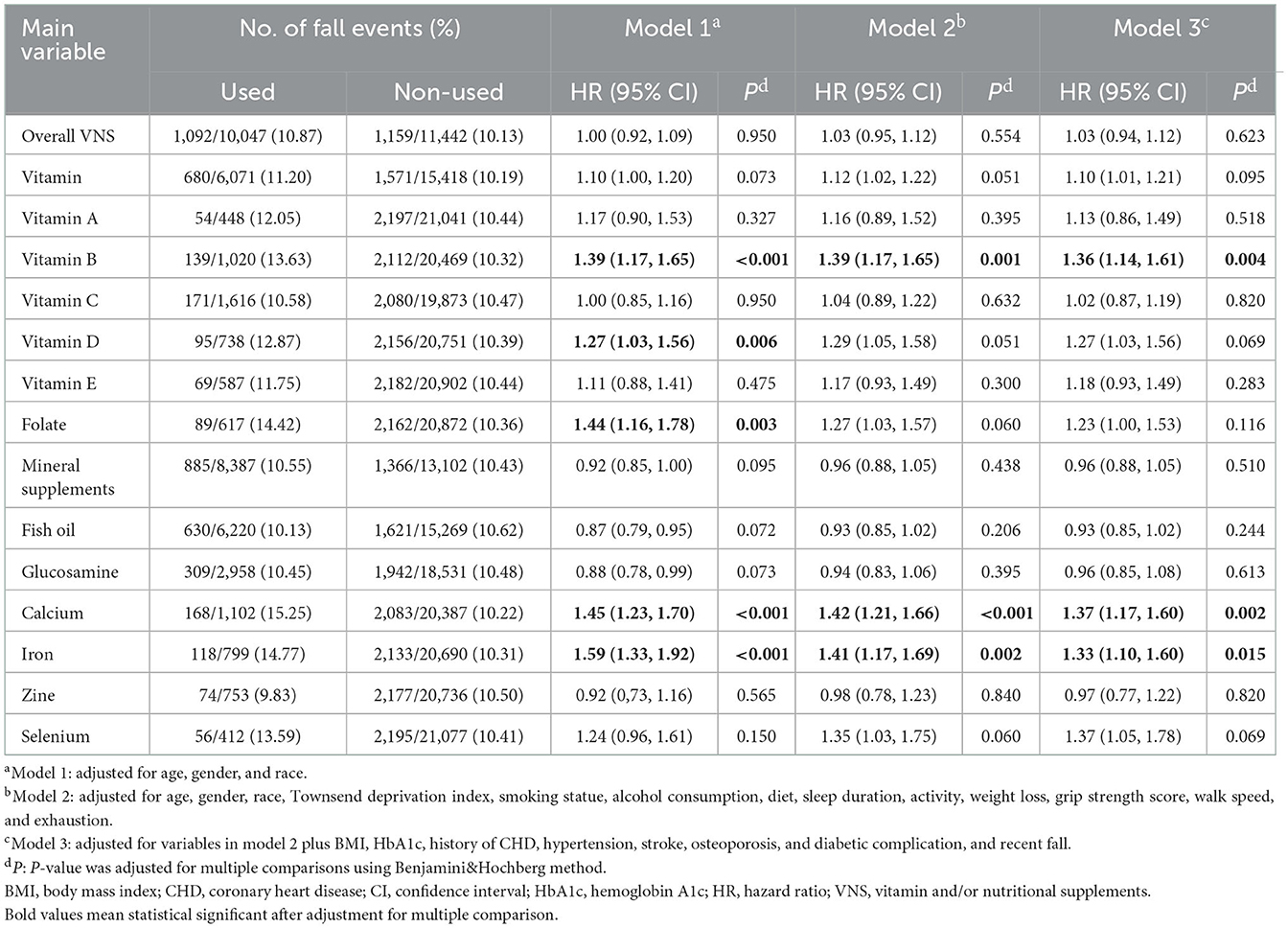
Overall, there were 2,251 participants experienced at least one inpatient fall during 11.9 median follow-up years. Table 3 shows the associations of overall VNS and specific supplements with the risk of inpatient fall in 3 models, respectively. The association between overall VNS and fall appeared not significate (full-adjusted HR: 1.03, 95% CI 0.94–1.12). When further analyzing the role of specific supplements, we observed heterogenicity in their effects on the risk of fall. For instance, after full adjustments, supplementation of total vitamin (HR: 1.10, 95% CI 1.01–1.21), vitamin B (HR: 1.36, 95% CI 1.14–1.61), vitamin D (HR: 1.27, 95% CI 1.03–1.56), folate (HR: 1.23, 95% CI 1.00–1.53), calcium (HR: 1.37, 95% CI 1.17–1.60), iron (HR: 1.33, 95% CI 1.10–1.60), and selenium (HR: 1.37, 95% CI 1.05–1.78) was associated with a higher risk of inpatient fall, respectively (Table 3). After further adjustment for multiple comparisons, the associations with fall risk remained significant for vitamin B (adjusted P = 0.004), calcium (adjusted P = 0.002), and iron (adjusted P = 0.015). No significant effect was observed for other specific supplements including vitamin A, vitamin C, vitamin D, vitamin E, folate, total mineral supplement, fish oil, glucosamine, zine, and selenium (adjusted P > 0.05). After propensity matching, the effects of vitamin B (full-adjusted HR: 1.35, adjusted P = 0.009) and calcium (full-adjusted HR: 1.36, adjusted P = 0.008) remained significant (Supplementary Table S4).
In sensitivity analyses, similar tendency was observed for the associations of overall VNS and specific supplements with the risk of inpatient falls, after excluding the participants who had a previous fall history, reported diabetic complications, occurred fall events during the first year of follow-up, modifying the assessment of frailty phenotype, or imputing the missing information in covariates (Supplementary Table S5).
4. Discussion
In this study, we assessed the associations of VNS use with the risk of fall among elderly patients with diabetes. Based on data from the ACCORD trial, we observed that VNS using was associated with an increased risk of fall events among patients with diabetes, and further tested our findings for specific supplements utilizing UK Biobank. We found that supplementation of vitamin B, iron, and calcium was independently associated with a higher risk of inpatient fall among patients with diabetes.
Existing studies in the effects of nutritional supplementation on falls mainly focused on vitamin D, generating mixed results. For instance, Bolland et al. (11) enrolled 37 RCTs, performed a trial sequential analysis, and found that vitamin D, when were applied as mono-supplement, exhibited no significant effect on falls, hip fractures, and total fractures, and the effects of vitamin D were independent of the doses used, while a recent meta-analysis indicated the protective role of vitamin D in fall prevention, especially when combined with calcium (12). Further analyses suggested that its effects might vary according to the supplementation doses and baseline nutritional status of participants (28, 29). Additionally, several RCTs have been conducted to evaluate the effects of vitamin B12 and folic acid supplementation (18) or vitamin K (16) on falls, and no significant effects on the risk of falls were observed. Although previous studies showed that most nutritional supplementation was associated with an increased muscle strength and alleviated frailty, there has been no studies that systematically evaluate the role of vitamins and dietary supplements on falls. And for patients with diabetes, who are at a higher risk of falls, no specific fall-preventive strategies have been developed yet. Therefore, utilizing data from the ACCORD trial and UK Biobank, we assessed the effects of total VNS, vitamins, and specific supplements on the risk of falls among patients with diabetes, and found the heterogenicity in their implications. Among the vitamins and dietary supplements involved in the baseline questionnaires of UK Biobank, vitamin B, calcium, and iron supplementation were associated with a significantly increased risk of inpatient fall, while the associations of other supplements with fall appeared insignificant, which appeared inconsistent with previous studies examining the associations of VNS with falls.
For fall-related clinical characteristics such as skeletal muscle mass, bone health, balance function, and frailty, the effects of nutritional supplementation observed in existing research also seemed to contradict our results (30). In a prospective study which enrolled 1,643 community-dwelling individuals aged ≥65 years, poor intake of vitamin B6, C, E, and folates was strongly and independently associated with frailty (31), and supplementation of whey protein, vitamin D, and E improved the muscle mass, strength, and life quality in older adults with sarcopenia (32). For elderly people, folate levels predict grip and leg strength (33), and low folate concentration is a risk factor for worse physical performance (34). Also, low levels of vitamin C and iron are also associated with age-related muscle loss and frailty syndrome (35–37). However, in reviewing the published literature, we also found that most studies that observed protective role of nutritional supplements in falls and related mechanisms were conducted among participants with nutritional deficiency. In developed countries such as U.K., U.S., and Canada, nutrient intake can usually be fulfilled by a high-quality diet, and people without increased demands might not benefit additionally via an extra nutritional supplementation (38–40). In addition, excessive nutritional supplementation might also have side effects or toxicity. For example, previous RCTs reported that supplementation of vitamin D in high doses daily (4,000 or 4,800 IU vitamin D3), monthly (60,000 IU vitamin D3 or 24,000 IU vitamin D3 plus 300 μg calcifediol), or annually (500,000 IU cholecalciferol) increased the risk of falls (13, 14, 41). High-dose vitamin B supplementation was associated with an increased risk for cataract (42). And in experimental studies, iron overload increased bone reabsorption and caused bone loss in mouse models (43). The evidence mentioned above supports our findings that specific vitamin and nutritional supplements were associated with an increased risk of inpatient fall among patients with diabetes. In addition, the information in the doses, duration, and brands for specific nutritional supplementation was not available in ACCORD and UK Biobank, and whether or not the enrolled participants had specific nutrient deficiencies was unknown in our analyses. Thus, it might be inapposite to compare our findings, which were derived from a “real-world” setting, with those of previous RCTs of specific supplements directly. And based on UK Biobank, we also conducted a series of sensitivity analyses and verified the reliability and robustness of our findings that vitamin B, iron, and calcium were independently associated with a higher risk of inpatient fall among patients with diabetes.
Furthermore, diabetes is a non-negligible risk factor for falls (7), which is attributed to a series of pathophysiological decline (impaired postural control, gait patterns, and cognitive function), diabetic complications (polyneuropathy, dysfunction of visual and vestibular systems), and other co-morbidities such as hypertension, hyperlipemia, and CVDs that might appear along with the progression of diabetes (44). Considering that diabetes-related frailty, muscle strength reduction, retinopathy, peripheral neuropathy, and other pathophysiological mechanisms involved in the diabetes-related higher risk of falls, we excluded patients with fall-related diabetic complications at baseline in sensitivity analysis 4 to avoid the related reverse causality, and the results remained consistent. Although the European Society of Cardiology and the European Association for the Study of Diabetes do not recommend the general use of vitamin or micronutrient supplementation to prevent diabetes or CVDs for patients with diabetes, we observed that nutritional supplementation was common among patients with diabetes in both ACCORD trial (33.8%) and UK Biobank (46.8%). According to a recent research based on the National Health and Nutrition Examination Surveys, ~58% of U.S. adults with diabetes used dietary supplements during 2013–2014 (45). Based on this phenomenon, our results, although did not assess the dose-dependent effects of each supplement, are still important for patients, clinicians, and policymakers. For patients without malnutrition or special demands, the non-indicative use of dietary supplements needs to be carefully evaluated, since its side effects might lead to worse prognosis, despite its undefined clinical benefits. Utilizing the two prospective data with “real-world” settings, this study provides epidemiological evidence to warn the non-indicative use of nutritional supplements for patients with diabetes, considering its potentially higher risk of falls. And further clinical trials and genetically epidemiological research are necessary to prove our findings and provide higher-level evidence.
There were several limitations to our study. Firstly, the use of VNS was self-reported by participants at baseline in two cohorts. The detailed doses, duration, and brands of the supplements used were not available, making it impossible to analyze the potential dose-dependent effects of specific supplements. And during follow-up period, possible alterations in the exposure level might contribute to dilution bias in our analyses. However, according to the published studies, the reproducibility of nutritional supplementation in UK Biobank was stable and reliable (46, 47). Secondly, since the incidence of general fall events (e.g., any falls in the last year) during follow-up was only available for a subset of participants and the corresponding date of self-reported fall events was unavailable in UK Biobank, we defined the fall outcome as inpatient fall event using ICD-10 codes and corresponding date derived from electrical health records by UK Biobank, which might underestimate the incidence of fall events. Thirdly, the two cohorts used in this study, ACCORD and UK Biobank, were based on the developed countries, and most participants were white. Thus, it needs caution to generalize our findings to the population from other developing countries and races. Fourthly, reverse causality might remain in this observational research, although we have attempted to avoid its impacts by conducting several sensitivity analyses. For instance, in sensitivity analysis 1, after exclusion of participants who experienced ≥2 falls in the previous year, consistent results were also observed. Finally, even though we have adjusted for potential confounding factors including fall-related diabetic complications, frailty phenotype, previous fall history, and osteoporosis in the multivariable models, there were still residual confounding factors (e.g., balance measurements, not available in ACCORD and UK Biobank), which might cause deviations in our results.
In summary, our study revealed that specific nutritional supplementation of vitamin B, iron, and calcium were significantly associated with an increased risk of fall among patients with diabetes after adjustments for demographic, clinical, and laboratory factors, and further randomized, controlled trials designed specifically are in demand to validate our conclusion further.
Data availability statement
The datasets analyzed for this study can be found in the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository (https://biolincc.nhlbi.nih.gov/studies/accord/ for ACCORD trial) and UK Biobank (https://www.ukbiobank.ac.uk/) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository and UK Biobank.
Ethics statement
The studies involving human participants were reviewed and approved by the National Heart, Lung, and Blood Institute the Institutional Review Board of Xiangya Hospital, Central South University the National Health Service (NHS) National Research Ethics Service. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YB and XC are the guarantor of this work, had full access to all original data in the study, take responsibility for the integrity of the data, and the accuracy of the data analysis in the study. XC researched data. LH and TM researched data and wrote the manuscript. GZ, XC, and YB contributed to the discussion and reviewed/edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 81822004), the National Key Research and Development Program of China (grant number 2020YFC2008002), the Science and Technology Innovation Program of Hunan Province (grant numbers 2020RC4006 and 2021RC2014), and the Project of Innovation-driven Plan in Central South University (grant number 2020CX017).
Acknowledgments
We thank the staff and participants of the ACCORD trail and UK Biobank, and we acknowledge Dr. Jinchen Li for data application assistance. This research has been conducted using the UK Biobank resource under the project number 76118.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1082282/full#supplementary-material
References
1. Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb Mortal Wkly Rep. (2016) 65:993–8. doi: 10.15585/mmwr.mm6537a2
2. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
3. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. (2013) 75:51–61. doi: 10.1016/j.maturitas.2013.02.009
4. Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing. (2004) 33:58–65. doi: 10.1093/ageing/afh028
5. Alamgir H, Muazzam S, Nasrullah M. Unintentional falls mortality among elderly in the United States: time for action. Injury. (2012) 43:2065–71. doi: 10.1016/j.injury.2011.12.001
6. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes Atlas, 9(Th) edition. Diabetes Res Clin Pract. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
7. Yang Y, Hu X, Zhang Q, Zou R. Diabetes mellitus and risk of falls in older adults: a systematic review and meta-analysis. Age Ageing. (2016) 45:761–7. doi: 10.1093/ageing/afw140
8. de Waard EAC, Koster A, Melai T, van Geel TA, Henry RMA, Schram MT, et al. The association between glucose metabolism status, diabetes severity and a history of fractures and recent falls in participants of 50 years and older-the Maastricht study. Osteoporos Int. (2016) 27:3207–16. doi: 10.1007/s00198-016-3645-0
9. Tricco AC, Thomas SM, Veroniki AA, Hamid JS, Cogo E, Strifler L, et al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA. (2017) 318:1687–99. doi: 10.1001/jama.2017.15006
10. Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of vitamin D on falls: a meta-analysis. JAMA. (2004) 291:1999–2006. doi: 10.1001/jama.291.16.1999
11. Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. (2018) 6:847–58. doi: 10.1016/S2213-8587(18)30265-1
12. Thanapluetiwong S, Chewcharat A, Takkavatakarn K, Praditpornsilpa K, Eiam-Ong S, Susantitaphong P. Vitamin D supplement on prevention of fall and fracture: a meta-analysis of randomized controlled trials. Medicine. (2020) 99:e21506. doi: 10.1097/MD.0000000000021506
13. Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, et al. Annual high-dose oral vitamin d and falls and fractures in older women: a randomized controlled trial. JAMA. (2010) 303:1815–22. doi: 10.1001/jama.2010.594
14. Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, Staehelin HB, Meyer OW, Theiler R, et al. Monthly high-dose vitamin d treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med. (2016) 176:175–83. doi: 10.1001/jamainternmed.2015.7148
15. Dangour AD, Albala C, Allen E, Grundy E, Walker DG, Aedo C, et al. Effect of a nutrition supplement and physical activity program on pneumonia and walking capacity in Chilean older people: a factorial cluster randomized trial. PLoS Med. (2011) 8:e1001023. doi: 10.1371/journal.pmed.1001023
16. Witham MD, Price RJG, Band MM, Hannah MS, Fulton RL, Clarke CL, et al. Effect of vitamin K2 on postural sway in older people who fall: a randomized controlled trial. J Am Geriatr Soc. (2019) 67:2102–7. doi: 10.1111/jgs.16024
17. Ng TP, Feng L, Nyunt MS, Feng L, Niti M, Tan BY, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med. (2015) 128:1225–36.e1. doi: 10.1016/j.amjmed.2015.06.017
18. Swart KM, Ham AC, van Wijngaarden JP, Enneman AW, van Dijk SC, Sohl E, et al. A randomized controlled trial to examine the effect of 2-year vitamin B12 and folic acid supplementation on physical performance, strength, and falling: additional findings from the B-proof study. Calcif Tissue Int. (2016) 98:18–27. doi: 10.1007/s00223-015-0059-5
19. Ford KL, Jorgenson DJ, Landry EJL, Whiting SJ. Vitamin and mineral supplement use in medically complex, community-living, older adults. Appl Physiol Nutr Metab. (2019) 44:450–3. doi: 10.1139/apnm-2018-0515
20. American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: standards of medical care in diabetes-2020. Diabetes Care. (2020) 43(Suppl 1):S48–65. doi: 10.2337/dc20-S005
21. Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 Esc guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the Easd. Eur Heart J. (2020) 41:255–323. doi: 10.1093/eurheartj/ehz486
22. Group AS, Buse JB, Bigger JT, Byington RP, Cooper LS, Cushman WC, et al. Action to control cardiovascular risk in diabetes (Accord) trial: design and methods. Am J Cardiol. (2007) 99:21i−33i. doi: 10.1016/j.amjcard.2007.03.003
23. Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. (2015) 12:e1001779. doi: 10.1371/journal.pmed.1001779
24. Ye J, Wen Y, Sun X, Chu X, Li P, Cheng B, et al. Socioeconomic deprivation index is associated with psychiatric disorders: an observational and genome-wide gene-by-environment interaction analysis in the UK Biobank cohort. Biol Psychiatry. (2021) 89:888–95. doi: 10.1016/j.biopsych.2020.11.019
25. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American heart association. Circulation. (2017) 135:e146–603. doi: 10.1161/CIR.0000000000000491
26. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–56. doi: 10.1093/gerona/56.3.M146
27. Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493,737 UK Biobank participants. Lancet Public Health. (2018) 3:e323–e32. doi: 10.1016/S2468-2667(18)30091-4
28. Ling Y, Xu F, Xia X, Dai D, Xiong A, Sun R, et al. Vitamin D supplementation reduces the risk of fall in the vitamin D deficient elderly: an updated meta-analysis. Clin Nutr. (2021) 40:5531–7. doi: 10.1016/j.clnu.2021.09.031
29. Kong SH, Jang HN, Kim JH, Kim SW, Shin CS. Effect of vitamin D supplementation on risk of fractures and falls according to dosage and interval: a meta-analysis. Endocrinol Metab. (2022) 37:344–58. doi: 10.3803/EnM.2021.1374
30. Gana W, De Luca A, Debacq C, Poitau F, Poupin P, Aidoud A, et al. Analysis of the impact of selected vitamins deficiencies on the risk of disability in older people. Nutrients. (2021) 13:163. doi: 10.3390/nu13093163
31. Balboa-Castillo T, Struijk EA, Lopez-Garcia E, Banegas JR, Rodriguez-Artalejo F, Guallar-Castillon P. Low vitamin intake is associated with risk of frailty in older adults. Age Ageing. (2018) 47:872–9. doi: 10.1093/ageing/afy105
32. Bo Y, Liu C, Ji Z, Yang R, An Q, Zhang X, et al. A high whey protein, vitamin D and E supplement preserves muscle mass, strength, and quality of life in sarcopenic older adults: a double-blind randomized controlled trial. Clin Nutr. (2019) 38:159–64. doi: 10.1016/j.clnu.2017.12.020
33. Wee AK. Serum folate predicts muscle strength: a pilot cross-sectional study of the association between serum vitamin levels and muscle strength and gait measures in patients >65 years old with diabetes mellitus in a primary care setting. Nutr J. (2016) 15:89. doi: 10.1186/s12937-016-0208-3
34. Ao M, Inuiya N, Ohta J, Kurose S, Takaoka H, Abe Y, et al. Relationship between homocysteine, folate, vitamin B12 and physical performance in the institutionalized elderly. J Nutr Sci Vitaminol. (2019) 65:1–7. doi: 10.3177/jnsv.65.1
35. Lewis LN, Hayhoe RPG, Mulligan AA, Luben RN, Khaw KT, Welch AA. Lower dietary and circulating vitamin c in middle- and older-aged men and women are associated with lower estimated skeletal muscle mass. J Nutr. (2020) 150:2789–98. doi: 10.1093/jn/nxaa221
36. Johnston CS, Barkyoumb GM, Schumacher SS. Vitamin C supplementation slightly improves physical activity levels and reduces cold incidence in men with marginal vitamin C status: a randomized controlled trial. Nutrients. (2014) 6:2572–83. doi: 10.3390/nu6072572
37. Zawadzki B, Mazur G, Butrym A. Iron dysregulation and frailty syndrome. J Clin Med. (2021) 10:5596. doi: 10.3390/jcm10235596
38. Rautiainen S, Manson JE, Lichtenstein AH, Sesso HD. Dietary supplements and disease prevention: a global overview. Nat Rev Endocrinol. (2016) 12:407–20. doi: 10.1038/nrendo.2016.54
39. Bischoff-Ferrari HA, Freystatter G, Vellas B, Dawson-Hughes B, Kressig RW, Kanis JA, et al. Effects of vitamin D, omega-3 fatty acids, and a simple home strength exercise program on fall prevention: the do-health randomized clinical trial. Am J Clin Nutr. (2022) 115:1311–21. doi: 10.1093/ajcn/nqac022
40. Fingeret M, Vollenweider P, Marques-Vidal P. No association between vitamin C and E supplementation and grip strength over 5 years: the Colaus study. Eur J Nutr. (2019) 58:609–17. doi: 10.1007/s00394-018-1646-9
41. Smith LM, Gallagher JC, Suiter C. Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: a randomized clinical trial. J Steroid Biochem Mol Biol. (2017) 173:317–22. doi: 10.1016/j.jsbmb.2017.03.015
42. Selin JZ, Lindblad BE, Bottai M, Morgenstern R, Wolk A. High-dose B-vitamin supplements and risk for age-related cataract: a population-based prospective study of men and women. Br J Nutr. (2017) 118:154–60. doi: 10.1017/S0007114517001994
43. Tsay J, Yang Z, Ross FP, Cunningham-Rundles S, Lin H, Coleman R, et al. Bone loss caused by iron overload in a murine model: importance of oxidative stress. Blood. (2010) 116:2582–9. doi: 10.1182/blood-2009-12-260083
44. Rasmussen NH, Dal J. Falls and fractures in diabetes-more than bone fragility. Curr Osteoporos Rep. (2019) 17:147–56. doi: 10.1007/s11914-019-00513-1
45. Li J, Li X, Gathirua-Mwangi W, Song Y. Prevalence and trends in dietary supplement use among us adults with diabetes: the national health and nutrition examination surveys, 1999–2014. BMJ Open Diabetes Res Care. (2020) 8:925. doi: 10.1136/bmjdrc-2019-000925
46. Liu X, Zhuang P, Li Y, Wu F, Wan X, Zhang Y, et al. Association of fish oil supplementation with risk of incident dementia: a prospective study of 215,083 older adults. Clin Nutr. (2022) 41:589–98. doi: 10.1016/j.clnu.2022.01.002
Keywords: ACCORD, diabetes, fall, nutritional supplements, UK Biobank
Citation: He L, Ma T, Zhang G, Cheng X and Bai Y (2023) Association of vitamin and/or nutritional supplements with fall among patients with diabetes: A prospective study based on ACCORD and UK Biobank. Front. Nutr. 9:1082282. doi: 10.3389/fnut.2022.1082282
Received: 28 October 2022; Accepted: 28 December 2022;
Published: 13 January 2023.
Edited by:
Sandra M. Colorado-Yohar, Murcia Regional Health Council, SpainReviewed by:
Xianwen Shang, The University of Melbourne, AustraliaXikang Fan, Jiangsu Provincial Center for Disease Control and Prevention, China
Copyright © 2023 He, Ma, Zhang, Cheng and Bai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xunjie Cheng,  Y2hlbmdjc3UzMTlAY3N1LmVkdS5jbg==; Yongping Bai,
Y2hlbmdjc3UzMTlAY3N1LmVkdS5jbg==; Yongping Bai,  YmFpeW9uZ3BpbmdAY3N1LmVkdS5jbg==
YmFpeW9uZ3BpbmdAY3N1LmVkdS5jbg==
 Lingfang He1,2
Lingfang He1,2 Guogang Zhang
Guogang Zhang Yongping Bai
Yongping Bai