- 1School of Nursing and Public Health, Yangzhou University, Yangzhou, Jiangsu, China
- 2Jiangsu Vocational College of Medicine, Yancheng, Jiangsu, China
Background: Statistics indicate that the morbidity of breast cancer is increasing globally, and its (overall figures) incidence has now surpassed that of lung cancer for the first time. The relation between a whole dietary pattern, rather than of a single food or nutrient, and breast cancer (BC) should be examined for findings to capture the complexities of diet and the potential for synergism between dietary components. Hence, the effects of dietary patterns on breast cancer have recently attracted increasing attention.
Objective: To systematically review the effects of dietary patterns on breast cancer risk, prognosis, and quality of life in survivors.
Methods: This systematic review was conducted following PRISMA guidelines and was registered in PROSPERO. Data from Ovid, China Biomedical Literature Database, Wanfang Data Knowledge Service Platform, CNKI, PubMed, Weipu, The Cochrane Library, Duxiu Data, ProQuest, Embase, Web of Science, and Scopus Database were retrieved and evaluated.
Results: A total of 47 studies that investigated the association between eating patterns and breast cancer were identified. Ten studies evaluated the effect of the model on treatment outcome and prognosis of breast cancer and two cross-sectional studies examined the influence of dietary patterns on quality of life. The resulting favorable dietary patterns were shown to regulate metabolic biomarkers, antioxidants, anti-inflammatory agents, and protective genes, and inhibit cell proliferation and invasion.
Conclusion: Numerous studies have examined the effects of healthy eating, plant-based, anti-inflammation, low-fat, and other favorable dietary patterns in relation to breast cancer. However, few studies reported significant associations and the studies had limitations, suggesting that the current findings should be interpreted with caution.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, CRD4202 2350171.
Introduction
The most recent estimates of the International Agency for Research on Cancer (IARC) indicated that breast cancer (BC) was the most prevalent cancer in women worldwide with 2.3 million diagnoses in 2020, thus surpassing lung cancer for the first time. BC is responsible for approximately 685,000 deaths per year, and it is the fifth leading cause of cancer-related deaths in women (1).
A previous study of the link between the gut and mammary glands found that diet could alter the gut microbiome and breast tumor microenvironment, thereby influencing tumorigenesis (2). Current research suggests that nutritional status affects cell invasion and lipid metabolism in BC (especially triple-negative breast cancer) (3), and can thus impact BC risk, treatment outcomes, and quality of life in survivors. Dietary research has shifted from studying single nutrients or foods to holistic dietary patterns (4), given that analysis of single nutrients and foods cannot address the effects of interactions between or changes in multiple nutrients and food components ingested together. In nutritional epidemiology, nutrients present in food are expressed based on their biological significance, and a new concept of food synergy has been established. The most reliable evidence for a link between diet and health outcomes is thus obtained by determining the overall effects of different eating patterns, considering the mutual effects of their nutrients (5, 6).
Breast cancer (BC) is the focus of extensive research, especially in countries with a high rate of the disease. Levels of consumption of animal products and all types of drinks are nearly twice as high and the consumption of plant- and grain-based foods is lower in countries with a high rate of BC. For example, in Mediterranean countries, where animal products are consumed at twice the rate of plant-based foods, the morbidity rate of BC is 51/100,000 (7). These findings highlight the need to explore the impact of dietary patterns on BC. However, most patients do not have sufficient understanding of the effects of dietary patterns and clinical factors on BC risk, disease outcomes, and quality of life in survivors, and a lack of understanding of relevant dietary patterns may lead to patients being diagnosed with advanced disease of BC (8).
A Mediterranean-style diet has been shown to reduce the risk of BC (9), while a low-fat diet reduced mortality in post-menopausal patients (10), and healthy eating patterns improved the quality of life of patients with BC (11). However, the role of dietary patterns in populations with specific BCs is inconclusive. We therefore systematically analyzed the effects of the components of different dietary patterns on BC, and determined which characteristics of the population were most affected by specific dietary patterns.
Materials and methods
Search process
The International System Review Registry Platform (PROSPERO) registration number for this project is CRD42022350171. The study is presented according to PRISMA guidelines for systematic reviews. Ovid, China Biomedical Literature Database, Wanfang Data Knowledge Service Platform, CNKI, PubMed, Weipu, The Cochrane Library, Duxiu Data, ProQuest, Embase, Web of Science, and the Scopus database were searched for relevant literature on BC and dietary patterns, using subject words and free words. The reference lists of the identified studies were also searched for additional studies. Dandamudi et al. published a systematic review of studies published up to January 2017 (12). The current search time was limited to studies published between 01 January 2017 and 30 July 2022, with no language restrictions.
The search identified articles with the following terms in the title or abstract: “Breast Neoplasms” OR “Breast Neoplasm” OR “Neoplasm, Breast” OR “Breast Tumors” OR “Breast Tumor” OR “Tumor, Breast” OR “Tumors, Breast” OR “Neoplasms, Breast” OR “Breast Cancer” OR “Cancer, Breast” OR “Mammary Cancer” OR “Cancer, Mammary” OR “Cancers, Mammary” OR “Mammary Cancers” OR “Malignant Neoplasm of Breast” OR “Breast Malignant Neoplasm” OR “Breast Malignant Neoplasms” OR “Malignant Tumor of Breast” OR “Breast Malignant Tumor” OR “Breast Malignant Tumors” OR “Cancer of Breast” OR “Cancer of the Breast” OR “Mammary Carcinoma, Human” OR “Carcinoma, Human Mammary” OR “Carcinomas, Human Mammary” OR “Human Mammary Carcinomas” OR “Mammary Carcinomas, Human” OR “Human Mammary Carcinoma” OR “Mammary Neoplasms, Human” OR “Human Mammary Neoplasm” OR “Human Mammary Neoplasms” OR “Neoplasm, Human Mammary” OR “Neoplasms, Human Mammary” OR “Mammary Neoplasm, Human” OR “Breast Carcinoma” OR “Breast Carcinomas” OR “Carcinoma, Breast” OR “Carcinomas, Breast” AND “Dietary pattern.”
Eligibility criteria and study selection
The inclusion criteria were: (1) cohort study, randomized controlled trial (RCT), cross-sectional research, or case-control study; (2) full text provided; and (3) study evaluated the effects of eating patterns or dietary interventions on BC risk, all-cause/specific mortality, recurrence, and quality of life. The exclusion criteria were: (1) dietary studies combined with physical activity; (2) studies without full text, results, and key data; (3) studies of any population not explicitly defined as cancer survivors; (4) cell and animal experiments, conference abstracts without full text, reviews, and meta-analyses; and (5) duplicate studies or several publications from the same study.
Data fetch and quality evaluation
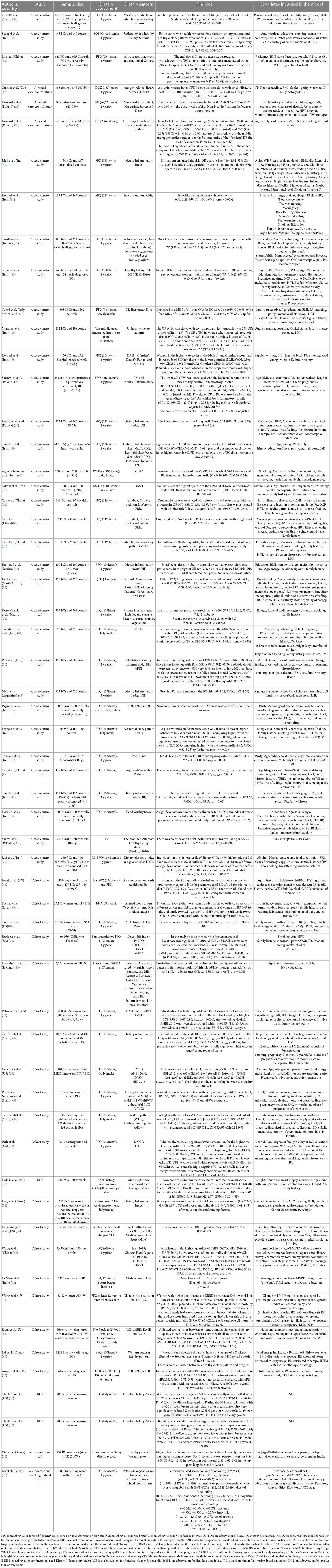
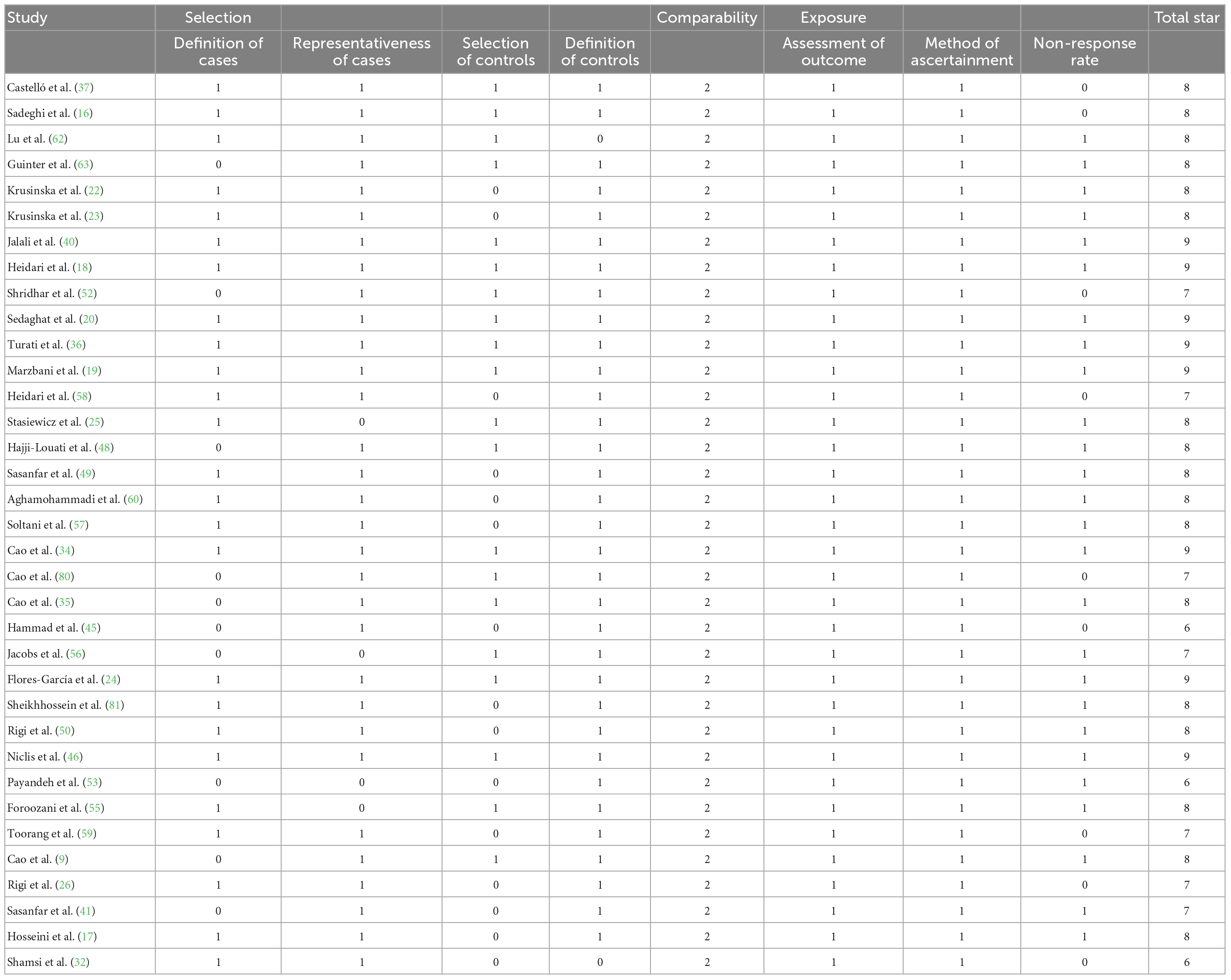
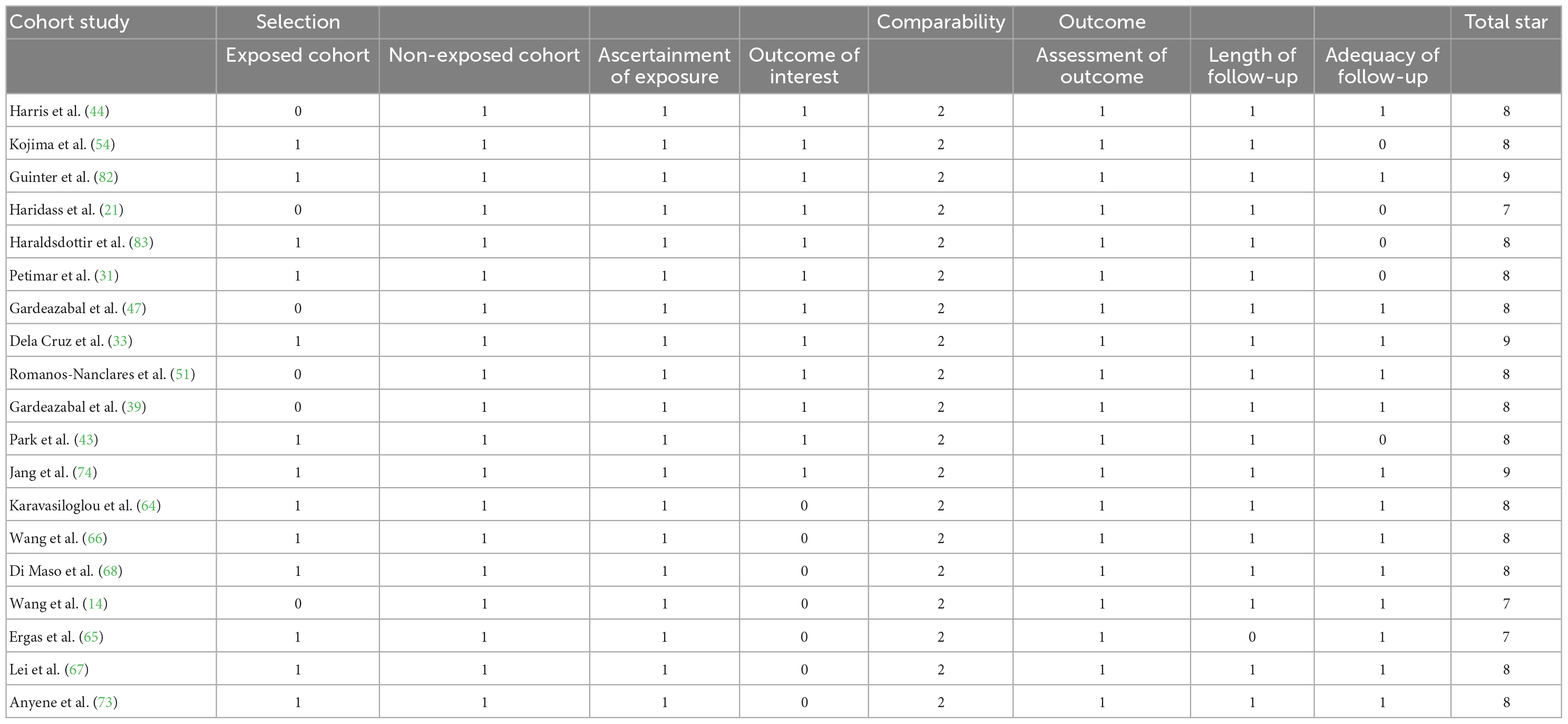
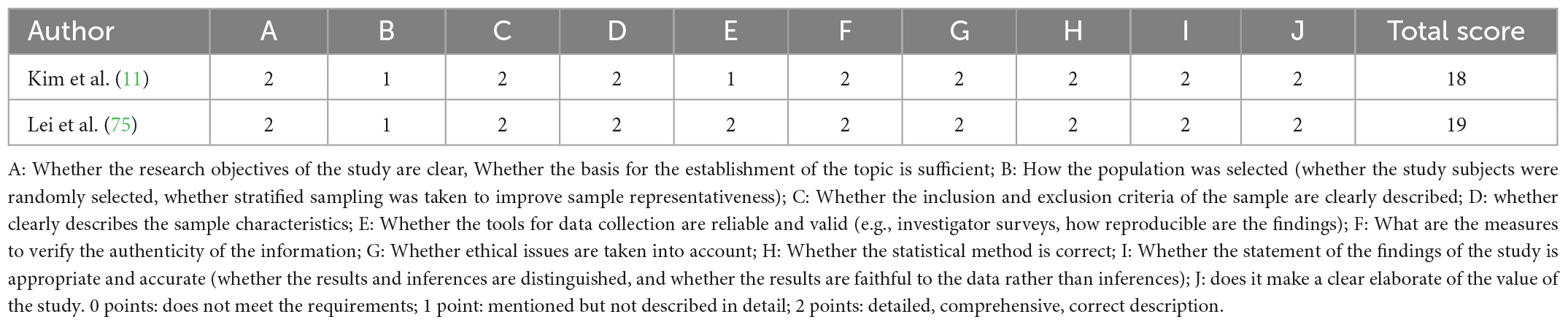
Articles were identified and the following data were retrieved by two researchers: general patient information, sample size, assessment of eating patterns, indicators of disease change, outcomes (relationship between dietary patterns and BC, 95% confidence intervals, odds ratios, correlation coefficients, hazard ratio, and p-values), and identification of confounding variables associated with BC (e.g., sex, smoking, tumor classification, estrogen, TNM staging, education, menarche, age, and menopausal age). The quality of case-control and cohort studies was assessed by the Newcastle-Ottawa scale (NOS), which includes selection of study population, comparability between groups, and outcome/exposure. The total score ranges from 0 to 9, with a score ≥ 6 indicating high-quality. Details of the NOS scale are provided in document S1. RCTs were assessed using Cochrane risk bias maps, with each aspect receiving a low, high, or unclear rating. The quality of the cross-sectional studies was based on the Joanna Briggs Institute (JBI) quality evaluation. This was a descriptive systematic review.
Results
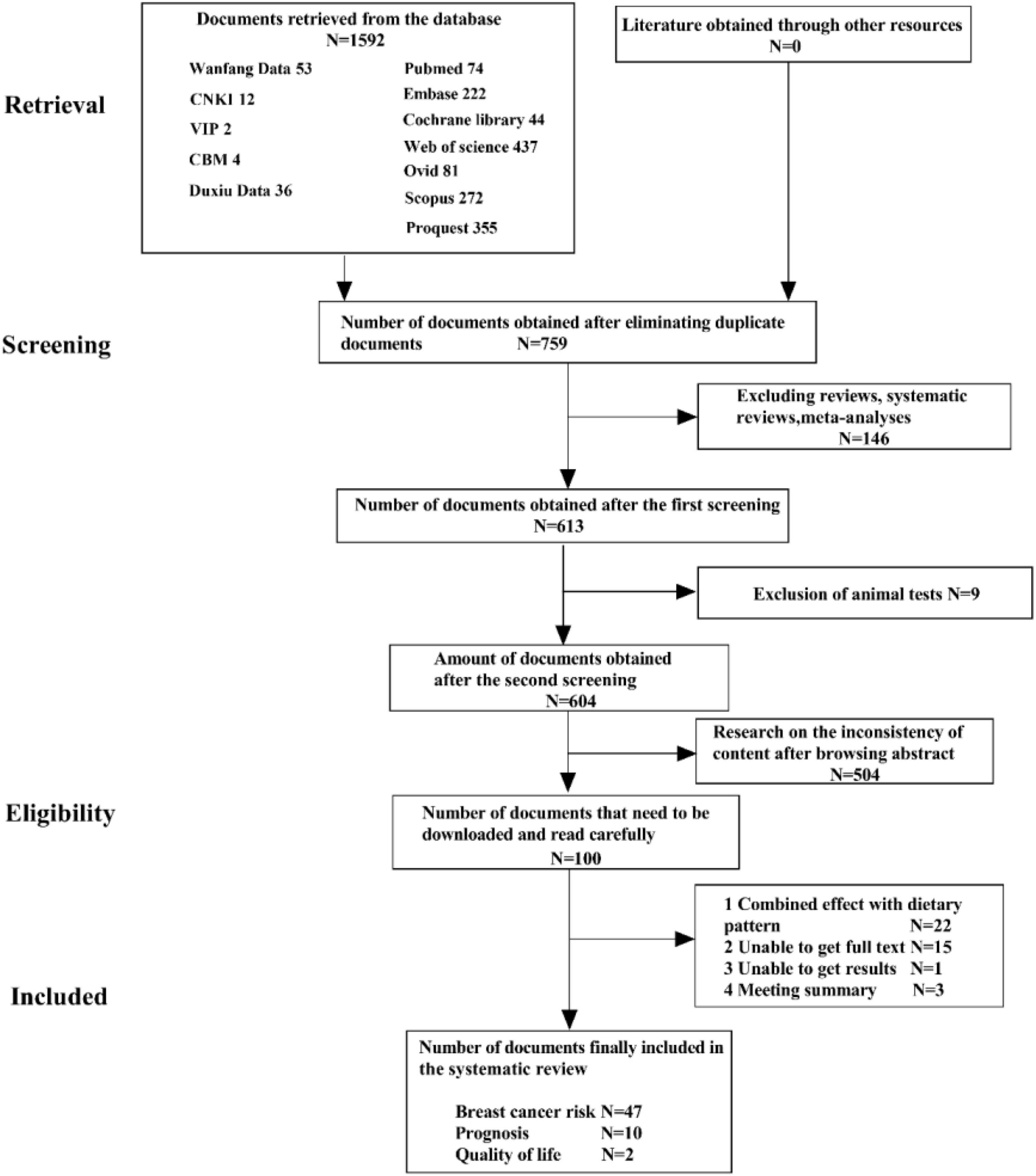
The PRISMA flowchart is shown in Figure 1. The preliminary search identified 1592 articles, of which 759 articles remained after excluding duplicate studies, and 107 articles remained after excluding systematic reviews, meta-analyses, animal experiments, and content discrepancies. The full texts of these articles were read, and the selected research findings, specific data, and comparator patterns are shown in Table 1. Forty-seven studies assessed the positive and negative effects of dietary patterns on cancer risk, 10 assessed the impact of eating patterns on treatment outcomes and prognosis, and two assessed the effects of eating patterns on quality of life in patients after a cancer diagnosis. This review included 35 case-control studies, 19 cohort studies, two cross-sectional studies, and three RCTs. The results of quality evaluations of the studies are presented in Tables 2–4 and Supplementary Figure 2. All previously conducted studies, except for three RCTs with a high risk of bias, were of high quality. In the three RCTs, random sequences were generated by using a permuted block algorithm and simple randomization, respectively. For allocation hiding, only Chlebowski et al. (13) described implementation points with hidden methods, while other two did not. It is difficult to blind the participants and researchers in dietary studies, and the three RCTs were therefore not blinded. However, the outcome evaluators were blinded in two of the studies (13, 14), but not in the third study (15). The mean and standard deviation were used to estimate the missing data in all three papers, and the reasonable effect size of the missing data did not affect the final observation results. There was no risk of selective reporting bias or other bias in any of the studies.
Dietary patterns and the risk of BC
The relationship between dietary patterns and the risk of BC has been studied by researchers in 16 different countries, particularly in relation to healthy, Mediterranean, inflammatory, plant-based, and Western dietary patterns (Supplementary material).
Healthy eating patterns were investigated in populations from various geographical locations, including, Iran (n = 5), the United States (n = 3), Pakistan (n = 1), Poland (n = 2), and Mexico (n = 1). This pattern reduced the risk of BC, whereas unhealthy eating patterns increased the risk (16–24). An unhealthy diet was positively related to the occurrence of postmenopausal BC through its proinflammatory potential. In contrast, regular consumption of low-processed vegetable products and fish was negatively related to the occurrence of cancer (25). Another study in Iran found a significant positive correlation between dietary glycemic index and the incidence rate of BC (26), while high dietary fiber intake, such as beans and grains, was shown to reduce the risk of estrogen receptor negative (ER–) and progesterone receptor negative (PR–) BC in the United States (27). Meat and processed meat diets were associated with a higher risk of BC in a Chinese study (28), while the consumption of vegetables, fruit, and soybeans reduced the risk of postmenopausal BC, especially ER– and ER–/PR– subtypes (9). The consumption of fresh fruit and nuts was negatively correlated with the risk of menopausal BC, and foods with a high sodium content were positively correlated with the risk of menopausal BC in a South African study (29), and a multigrain diet reduced the risk of BC in a South Korean study (30). These findings were consistent with the results of the study on healthy eating patterns (16, 18). However, a study conducted by American researchers showed that the Alternative Healthy Eating Index–2010 (AHEI-2010) had a weak (but insignificant) correlation with the risk of BC, but after excluding alcohol, it was negatively correlated with the risk of ER–/PR– and ER–/PR–/human epidermal growth factor receptor 2 (HER2–) BC (31), and there was no relationship between this index and BC risk in another study conducted in Pakistan (18, 19, 32, 33).
Studies on the effects of a Mediterranean diet, characterized by high intakes of fish, vegetables, beans, boiled potatoes, fruit, olives and vegetable oils, and a low intake of fruit juice, were carried out in the United States (n = 3), China (n = 2), Spain (n = 1), and Italy and Switzerland (n = 1), while studies of ‘prudent’ dietary patterns similar to a Mediterranean-style diet (34) have been carried out in China (n = 1), Spain (n = 1), and Poland (n = 2). A higher score for a Mediterranean diet was negatively related to BC in some studies (21–23, 28, 35, 36), especially after the menopause (37–39), while the Spanish study and two studies in the United States showed only a weak or no correlation (31, 33, 39). Prudent dietary patterns were associated with a lower risk of BC in one study (34), but had no observable effect on BC in the Spanish study (37–39).
The effects of an inflammatory diet were investigated in Iran (n = 2), the United States (n = 2), Spain (n = 1), Poland (n = 1), Jordan (n = 1), France (n = 1), and Argentina (n = 1). Inflammatory dietary patterns, including high intakes of sugary soft drinks, refined grains, red and processed meat, margarine and other hydrogenated fats, and low intakes of green leafy vegetables, cruciferous vegetables, coffee, increased the risk of BC in premenopausal and overweight postmenopausal women (40–44). In addition, a low dietary inflammation index reduced the risk of BC in obese women (45, 46). However, there was no significant relationship between the dietary inflammation index and the incidence rate of BC in a Spanish study (47), while a French study found that an inflammatory diet only increased the risks of ER+, PR+, or HER2+ breast tumor subtypes, but found no relationship with triple-negative (ER–, PR–, and HER2–) BC (48).
Plant-based diets have been investigated in Iran (n = 3), China (n = 1), Spain (n = 1), and North India (n = 1). The plant diet index (PDI) and a healthy PDI were negatively correlated with the incidence rate of BC (28, 49–51), while an unhealthy PDI was associated with an increased risk (50). Lacto-ovo vegetarians (whose diet includes plants, dairy products, and eggs) had a lower risk of BC compared with meat eaters and lacto vegetarians (vegetarian diet and dairy products) according to a multicenter case-control study of women in northern India (52). However, there was no significant correlation between PDI and the incidence of BC in the Iranian study and another study in Japan (53, 54).
The effects of a Western dietary pattern were investigated in Iran (n = 1), Spain (n = 2), and Mexico (n = 1). This pattern (high intakes of fat, sugar products, and red and processed meat) increased women’s risk of BC in some studies (24, 29, 37–39). However, some studies found a positive correlation between a Western diet and the risk of invasive ductal carcinoma of the breast, but no significant correlation with the risk of invasive lobular carcinoma (55, 56).
Four beneficial dietary patterns are summarized: a healthy diet, Mediterranean diet, anti-inflammatory diet, and plant-based diet. Other dietary patterns negatively related to the risk of BC include dietary approaches to stop hypertension (DASH) (31, 57–59), Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) (60), a diet with a high intake of vitamins, trace elements, carbohydrates, fiber, and protein (61), and traditional diets (15, 56, 62). Dietary patterns positively related to the risk of BC include an estrogen-related dietary pattern (63) and a modern diet (15).
Dietary patterns and prognosis of BC
The relationship between dietary patterns and BC prognosis has been studied in four countries, particularly focusing on healthy, Mediterranean, and DASH diets. Two studies on healthy eating patterns conducted in the United States found that this pattern had the potential to reduce patient mortality (64, 65), while two studies in China found no such relationship (66, 67).
Two studies in the United States and one in Italy investigated the effects of a Mediterranean diet. The third national health and nutrition examination survey in the United States conducted in 2019 found no correlation (64), while the survey in 2021 showed that this diet was negatively related to BC mortality (65). In the Italian study, the 15-year overall survival rate among patients with high compliance to a Mediterranean diet was better than that among patients with low compliance, but there was no significant correlation with either increased or decreased mortality rates (68).
One study of the DASH diet in the United States showed that this diet reduced mortality in BC patients (65); however, a Chinese study found that adherence to the DASH diet was associated with higher mortality compared with adherence to the Chinese food pagoda CHFP-2007/2016 (66).
Dietary patterns shown to reduce mortality and improve overall survival among patients with BC include a low-fat diet (13, 69–72), diabetes risk-reduction diet (14), plant-based diet (73), and anti-inflammatory diet (74). However, different studies have shown different results in terms of all-cause mortality, specific mortality, total mortality, cancer recurrence, and non-BC-related deaths among BC patients, indicating the need for more research.
Dietary patterns and quality of life in BC
Two studies investigated the effects of dietary patterns on quality of life in patients with BC. A Korean study showed that healthy eating habits improved dyspnea but increased insomnia in specific populations (11). A Chinese study investigated the relationship between eating more grain and animal products and poorer functions, including respiratory function and constipation, and the effects of a high-fruit and vegetable diet in improving quality of life, including physical, emotional, and cognitive functions, as well as reducing common gastrointestinal reactions, breathing problems, and insomnia (75).
Discussion
A search was conducted to find and analyze recent studies examining the influence of dietary patterns on BC, to identify dietary patterns likely to prevent BC and improve its prognosis, and enhance the quality of life for BC survivors. The available data suggested that healthy dietary patterns had the most scientific evidence to support their beneficial effects compared with other dietary patterns. The different dietary patterns are discussed below in order of scientific evidence.
Adhering to a healthy diet pattern reduced the risk of BC, BC recurrence, all-cause mortality, and overall mortality, and improved the quality of life (especially in postmenopausal women and hormone receptor-negative women). This dietary pattern was characterized by low intakes of carbohydrates, red and processed meats, and sweet foods, and increased intakes of protein, folic acid, calcium, vitamin D, and fiber. Thus, even though physical activity decreased, the dietary fat energy percentage also decreased and body weight remained unchanged. This was consistent with a study of low-fat diet patterns (10). The results of the study on a prudent diet pattern (23), characterized by more frequent consumption of dairy products, fruit, vegetables, wholewheat bread, fish, and fruit juice, were similar, especially in premenopausal women, with significance for hormone receptor-positive and -negative tumors. This dietary pattern may reduce the risk of BC by regulating plasma lipid biomarkers, and improve the prognosis by reducing the overexpression of RhoA and Rho-associated protein kinase-related (8, 34).
Current evidence shows that high adherence to a Mediterranean diet significantly reduces the incidence rate of BC, especially invasive ductal and lobular BC, it is more significant for ER- or ER+, has the best anti-tumor-metastasis effect, and reduces disease recurrence, overall mortality, and other complications such as cardiovascular disease, and has a greater beneficial impact than a prudent dietary pattern (37, 68). The mechanism involves reducing glucose, weight, and waist circumference, improving biochemical parameters, reducing the biological activities of insulin-like growth factor 1 (IGF-1), testosterone, and estradiol, increasing antioxidation, and repairing DNA (36, 65). A summary analysis of the individual components of the Mediterranean diet showed that the protective effect was mainly attributable to fruit, vegetables, and whole grains (21, 35). The protective effect of the Mediterranean diet, which contains fish, beans, nuts, seeds, whole grains, and vegetables, may be due to specific chemical components, such as lignans and polyphenols, or to its wider nutrient components, such as fatty acids, resveratrol, organic sulfur compounds, quercetin, kaempferol, and apigenin, as well as the common micronutrients zinc and selenium, and phytochemicals, such as flavonoids, carotenoids, vitamins C and E, vitamin A, natural retinoids, and omega-3 polyunsaturated fatty acids. An increase in circulating tumor cells in the body was shown to be delayed by low-fat components (76). These compounds have demonstrated anticancer properties including affecting the growth and progression of BC, cancer cell cycle growth arrest, apoptosis, inflammation, angiogenesis, and DNA methylation of the gene, which can prevent the progress of obesity-related BC, and has a positive impact on all-cause mortality (77, 78).
Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND), a Mediterranean diet, and DASH diet are all plant-based diets, emphasizing the consumption of fruits and green leafy vegetables, beans, whole grains, nuts, fish, and poultry, and low intakes of saturated fats and red meat. These diets are sources of carotenoids, flavonoids, folic acid, and vitamin E. The mechanisms of this type of diet reduce the risk and mortality of BC similar to the effects of a Mediterranean diet (21, 66).
Compliance with a plant-based diet reduces the risk of BC, especially those types of BC that are more likely to become invasive, and improves the overall survival rate, especially in patients with ER–, HER2 basal-like, and luminal A BC. This diet includes more fruit and vegetables, especially cruciferous and yellow/orange vegetables, beans, nuts, seeds, and whole grains (12). The mechanism involves the reduction of IGF-1, blood glucose, and total cholesterol, while phytochemicals (allicin, hesperidin, and astragalus polysaccharide) included in this diet significantly inhibit the growth of primary tumors and metastatic lesions by reducing the expression of genes (50). Although there is a negative correlation trend between soluble fiber and estradiol levels, serum estradiol and estrone levels are not related to dietary fiber. A plant-based diet can thus improve the prognosis of BC by affecting the intestinal microbiota and hormone levels (21, 66); however, further studies are needed to clarify this.
In addition, a low-glucose diet, characterized by the intake of glucose equal to or lower than the average fasting level, improved insulin resistance (HOMA-IR) and other cancer-related serum biomarkers in some studies, thereby favorably regulating postmenopausal obesity as a postmenopausal BC prevention strategy (79). Other dietary patterns that improve the prognosis and quality of life of BC patients, such as an anti-inflammatory diet, have been shown to improve the prognosis of BC patients by reducing cardiovascular mortality (25).
It is also important to understand the mechanisms of dietary patterns that are negatively associated with disease, such as a Western diet, which is characterized by higher intakes of red and processed meat, dairy products, and saturated fats. A Western diet can lead to BC via the production of several carcinogenic compounds associated with cooking and processing meat, including nitrates, nitrites, heterocyclic amines, and polycyclic aromatic hydrocarbons (55). In an inflammatory diet, inflammatory markers increase BC risk by stimulating angiogenesis, cell proliferation, and migration, and preventing apoptosis, while other inflammatory biomarkers may reduce quality of life. In addition, the key mediators of the inflammatory response promote tumor growth, angiogenesis, and invasion through the influence of insulin resistance and increased cytokines (25). However, results on this topic are currently lacking, and more correlation studies are needed.
This study showed that a balanced dietary pattern [large amounts of protein (mainly white meat), fruits, and vegetables (rich in vitamins and minerals), nuts, beans, low omega-3 fatty acid diet of fish and seafood, whole grains, vegetable oil, and low intake of spices] may prevent BC and improve BC prognosis. However, except for alcohol intake, no studies have yet demonstrated a consistent and significant correlation for any specific foods, and the study of dietary patterns is affected by regional and cultural backgrounds. The beneficial dietary patterns summarized in this review should thus be interpreted carefully in view of the exploratory nature of the analysis. The findings are inconsistent, indicating the need for further studies to explore this topic.
Niclis et al.’s case-control study of inflammatory dietary patterns showed an association with disease risk, whereas Gardeazabal et al.’s cohort study showed no such association, which may reflect recall bias rather than a true difference (46, 47). Some studies showed that inflammatory diets increased the risk of BC (ER+, PR+, HER2+), but few studies have examined hormone-negative or triple-negative BC, and the effect of diet on heterogeneous breast risk or prognosis remains unclear (25). Foroozani et al.’s study did not assess the role of dietary patterns based on the histological subtype of breast cancer (55). Finally, although most of the included studies adjusted for a large number of confounding factors (body mass index, family history, smoking, etc.) that may confuse the association between dietary patterns and BC, not all studies adjusted for all potential confounding factors, such as physical activity and smoking. Future research should thus pay attention to this aspect. In addition, more evidence is required regarding prior and posterior eating patterns, study area, menopausal status, and hormonal status, to produce more conclusive results.
Limitations
This study had some limitations. We only retrieved published literature, which may have led to publication bias due to incomplete literature collection. In addition, the reproducibility of dietary patterns was poor, due to differences in dietary research methods, evaluation methods (factor analysis, reduced rank regression), research populations, and regions. Because of the high heterogeneity among the included studies, the results were not analyzed by objective quantitative methods, and we were therefore unable to perform subgroup analyses due to the limited number of included studies.
Notably, despite the large number of studies, nutritional studies often produced inaccurate and/or contradictory results. In addition, BC is a multifactorial disease, and diet is only one of numerous risk factors associated with its pathology.
In addition, nutrition research has some problems. First, food surveys do not conform to reality, and different patients have different reactions to the same food as a result of interactions among genes, nutrients, and the intestinal microbiota. In addition, food nutritional profiles are affected by food practices and storage (e.g., fresh vegetables are chemically different from processed vegetables). Although clinical trials can be used to investigate simple and short-term problems, they are unsuitable for studying long-term diseases: it is difficult to randomly assign different diets to different populations and track them for many years to determine if a certain food is related to specific diseases. Furthermore the confounding factors in observational studies were not controlled, potentially leading to inaccurate results.
Conclusion
Despite these limitations, the results of different types of studies (with different environments, methods, and patients) suggested similar conclusions, indicating a link between dietary patterns and clear health outcomes. Based on these findings, it is better to propose a “healthy” diet model, rather than claim any impact of specific foods or food ingredients. BC patients should be encouraged to improve their dietary habits before, during, and after treatment, in order to improve their long-term survival and quality of life.
This study systematically reviewed the impact of dietary patterns on BC risk, treatment outcomes, prognosis, and quality of life. On one hand, most studied dietary patterns tended to prevent the occurrence of BC, while fewer studies examined their effects on the prognosis and quality of life of survivors. On the other hand, more RCTs are needed to demonstrate the effects of these dietary patterns on cancer-specific outcomes (event-free survival, recurrence), and more research is required to clarify the mechanisms underlying the correlation of dietary patterns with BC based on biological processes.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YB and JZ: conceptualization, methodology, formal analysis, and writing—original draft. HS and MX: investigation. JCQ and SJ: resources. YL and JLQ: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Su Jiao Ji Han (2019) No. 2, Jiangsu Province Elderly Education Learning Resource Library Sub library Project and Postgraduate Research and Practice Innovation Program of Jiangsu Province, China (Grant number: SJCX22_1829).
Acknowledgments
We thank YL for suggestions on the design and revision of the manuscript and JZ and HS for consulting the literature. We are grateful for the network equipment support policy of the School of Nursing, Yangzhou University, China. We also thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1057057/full#supplementary-material
References
1. WHO World Cancer Day 2021: Spotlight on IARC Research Related to Breast Cancer. (2021). Available online at: https://www.iarc.who.int/featured-news/world-cancer-day-2021/ (accessed May 02, 2021).
2. Soto-Pantoja D, Gaber M, Arnone A, Bronson S, Cruz-Diaz N, Wilson A, et al. Diet alters entero-mammary signaling to regulate the breast microbiome and tumorigenesis. Cancer Res. (2021) 81:3890–904. doi: 10.1158/0008-5472.CAN-20-2983
3. Corsetto P, Montorfano G, Zava S, Colombo I, Rizzo A. Nutrient deprivation induces lipid alterations and reduction of invasivity in triple negative breast cancer cells. Mol Living Syst. (2019) 9(Suppl. 1):362–3.
4. Kerr J, Anderson C, Lippman S. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. (2017) 18:e457–71. doi: 10.1016/s1470-204530411-4
5. Gleason P, Boushey C, Harris J, Zoellner J. Publishing nutrition research: a review of multivariate techniques–part 3: data reduction methods. J Acad Nutr Diet. (2015) 115:1072–82. doi: 10.1016/j.jand.2015.03.011
6. Castelló A, Buijsse B, Martín M, Ruiz A, Casas A, Baena-Cañada J, et al. Evaluating the applicability of data-driven dietary patterns to independent samples with a focus on measurement tools for pattern similarity. J Acad Nutr Diet. (2016) 116:1914–24.e6. doi: 10.1016/j.jand.2016.05.008
7. Radkevich L, Radkevich D. The dietary patterns are a modifying risk factor for breast cancer: an ecological study. Doklady Biol Sci. (2017) 472:21–7. doi: 10.1134/S0012496617010070
8. Shuvo S, Ahmad T, Paul D, Zahid M. Dietary patterns and knowledge perception of breast cancer risk patients: a case-control study in Bangladesh. Nutr Food Sci. (2017) 47:270–87. doi: 10.1108/NFS-05-2016-0060
9. Cao S, Liu L, Zhu Q, Zhu Z, Zhou J, Wei P, et al. Adherence to the vegetable-fruit-soy dietary pattern, a reference from Mediterranean diet, protects against postmenopausal breast cancer among Chinese women. Front Nutr. (2022) 9:800996. doi: 10.3389/fnut.2022.800996
10. Prentice R, Aragaki A, Howard B, Chlebowski R, Thomson C, Van Horn L, et al. Low-fat dietary pattern among postmenopausal women influences long-term cancer, cardiovascular disease, and diabetes outcomes. J Nutr. (2019) 149:1565–74. doi: 10.1093/jn/nxz107
11. Kim N, Song S, Jung S, Lee E, Kim Z, Moon H, et al. Dietary pattern and health-related quality of life among breast cancer survivors. BMC Womens Health. (2018) 18:65. doi: 10.1186/s12905-018-0555-7
12. Dandamudi A, Tommie J, Nommsen-Rivers L, Couch S. Dietary patterns and breast cancer risk: a systematic review. Anticancer Res. (2018) 38:3209–22. doi: 10.21873/anticanres.12586
13. Chlebowski R, Anderson G, Manson J, Prentice R, Aragaki A, Snetselaar L, et al. Low-fat dietary pattern and cancer mortality in the women’s health initiative (WHI) randomized controlled trial. JNCI Cancer Spectr. (2018) 2:ky065. doi: 10.1093/JNCICS/PKY065
14. Wang T, Farvid M, Kang J, Holmes M, Rosner B, Tamimi R, et al. Diabetes risk reduction diet and survival after breast cancer diagnosis. Cancer Res. (2021) 81:4155–62. doi: 10.1158/0008-5472.CAN-21-0256
15. Hidaka B, Kimler B, Fabian C, Carlson S. An empirically derived dietary pattern associated with breast cancer risk is validated in a nested case-control cohort from a randomized primary prevention trial [comparative study; journal article; randomized controlled trial; validation study]. Clin Nutr. (2017) 17:8–17. doi: 10.1016/j.clnesp.2016.10.008
16. Sadeghi M, Akbari M, Rashidkhani B, Ajami M, Jamshidi-Naeini Y, Davoodi S. Association between dietary patterns with breast cancer and pathobiological factor HER-2. J Mazandaran Univ Med Sci. (2017) 26:76–87.
17. Hosseini F, Shab-Bidar S, Ghanbari M, Majdi M, Sheikhhossein F, Imani H. Food quality score and risk of breast cancer among Iranian women: findings from a case control study. Nutr Cancer Int J. (2022) 74:1660–9. doi: 10.1080/01635581.2021.1957136
18. Heidari Z, Jalali S, Sedaghat F, Ehteshami M, Rashidkhani B. Dietary patterns and breast cancer risk among Iranian women: a case-control study. Eur J Obstetr Gynecol Reprod Biol. (2018) 230:73–8. doi: 10.1016/j.ejogrb.2018.09.018
19. Marzbani B, Nazari J, Najafi F, Marzbani B, Shahabadi S, Amini M, et al. Dietary patterns, nutrition, and risk of breast cancer: a case-control study in the west of Iran. Epidemiol Health. (2019) 41:e2019003. doi: 10.4178/epih.e2019003
20. Sedaghat F, Heidari Z, Jalali S, Doustmohammadian A, Ehteshami M, Rashidkhani B. Healthy eating index 2010 and breast cancer risk. Nutr Cancer Int J. (2018) 70:860–6. doi: 10.1080/01635581.2018.1490781
21. Haridass V, Ziogas A, Neuhausen S, Anton-Culver H, Odegaard A. Diet quality scores inversely associated with postmenopausal breast cancer risk are not associated with premenopausal breast cancer risk in the California teachers study. J Nutr. (2018) 148:1830–7. doi: 10.1093/jn/nxy187
22. Krusinska B, Wadolowska L, Slowinska M, Biernacki M. Associations of dietary patterns and metabolic-hormone profiles with breast cancer risk: a case-control study. Nutrients. (2018) 10:2013. doi: 10.3390/nu10122013
23. Krusinska B, Hawrysz I, Wadolowska L, Slowinska M, Biernacki M, Czerwinska A, et al. Associations of Mediterranean diet and a posteriori derived dietary patterns with breast and lung cancer risk: a case-control study. Nutrients. (2018) 10:470. doi: 10.3390/nu10040470
24. Flores-García M, Mérida-Ortega Á, Denova-Gutiérrez E, López-Carrillo L. Dietary patterns and breast cancer risk in women from Northern Mexico. Nutr Cancer. (2021) 73:2763–73. doi: 10.1080/01635581.2020.1860241
25. Stasiewicz B, Wadolowska L, Biernacki M, Slowinska M, Drozdowski M. Hybrid dietary-blood inflammatory profiles and postmenopausal breast cancer: a case-control study. Nutrients. (2020) 12:3503. doi: 10.3390/nu12113503
26. Rigi S, Salari-Moghaddam A, Benisi-Kohansal S, Azadbakht L, Esmaillzadeh A. Dietary glycaemic index and glycaemic load in relation to risk of breast cancer. Public Health Nutr. (2022) 25:1658–66. doi: 10.1017/S1368980021004018
27. Sangaramoorthy M, Koo J, John E. Intake of bean fiber, beans, and grains and reduced risk of hormone receptor-negative breast cancer: the San Francisco bay area breast cancer study. Cancer Med. (2018) 7:2131–44. doi: 10.1002/cam4.1423
28. Chang Y, Hou Y, Chen L, Wu J, Wu C, Chang Y, et al. Is vegetarian diet associated with a lower risk of breast cancer in Taiwanese women? BMC Public Health. (2017) 17:800. doi: 10.1186/s12889-017-4819-1
29. Jacobs I, Taljaard-Krugell C, Ricci C, Vorster H, Rinaldi S, Cubasch H, et al. Dietary intake and breast cancer risk in black South African women: the South African breast cancer study. Br J Nutr. (2019) 121:591–600. doi: 10.1017/S0007114518003744
30. Shin W, Lee H, Shin A, Lee J, Lee S, Lee J, et al. Multi-grain rice diet decreases risk of breast cancer in Korean women: results from the health examinees study. Nutrients. (2020) 12:2273. doi: 10.3390/nu12082273
31. Petimar J, Park Y, Smith-Warner S, Fung T, Sandler D. Dietary index scores and invasive breast cancer risk among women with a family history of breast cancer. Am J Clin Nutr. (2019) 109:1393–401. doi: 10.1093/ajcn/nqy392
32. Shamsi U, Gill T, Khan S, Azam I, Callen D, Iqbal R. The modified alternate healthy eating index-2010 and breast cancer risk among women from Karachi, Pakistan. J Pak Med Assoc. (2022) 72:1289–93. doi: 10.47391/JPMA.01276
33. Dela Cruz R, Park S, Shvetsov Y, Boushey C, Monroe K, Le Marchand L, et al. Diet quality and breast cancer incidence in the multiethnic cohort. Eur J Clin Nutr. (2020) 74:1743–7. doi: 10.1038/s41430-020-0627-2
34. Cao S, Liu L, Zhu Q, Zhu Z, Zhou J, Wei P, et al. Association between dietary patterns and plasma lipid biomarker and female breast cancer risk: comparison of latent class analysis (LCA) and factor analysis (FA). Front Nutr. (2021) 8:645398. doi: 10.3389/fnut.2021.645398
35. Cao S, Zhu Z, Zhou J, Li W, Dong Y, Qian Y, et al. Associations of one-carbon metabolism-related gene polymorphisms with breast cancer risk are modulated by diet, being higher when adherence to the Mediterranean dietary pattern is low. Breast Cancer Res Treat. (2021) 187:793–804. doi: 10.1007/s10549-021-06108-8
36. Turati F, Carioli G, Bravi F, Ferraroni M, Serraino D, Montella M, et al. Mediterranean diet and breast cancer risk. Nutrients. (2018) 10:326. doi: 10.3390/nu10030326
37. Castelló A, Boldo E, Pérez-Gómez B, Lope V, Altzibar J, Martín V, et al. Adherence to the Western, Prudent and Mediterranean dietary patterns and breast cancer risk: MCC-Spain study. Maturitas. (2017) 103:8–15. doi: 10.1016/j.maturitas.2017.06.020
38. Li Y, Hu B, Wu X, Qi X, Jiang J, Cui X, et al. Adherence to Mediterranean diet and the risk of breast cancer: a meta-analysis. Transl Cancer Res. (2018) 7:1290–7. doi: 10.21037/tcr.2018.10.13
39. Gardeazabal I, Romanos-Nanclares A, Martínez-González M, Castelló A, Sánchez-Bayona R, Pérez-Gómez B, et al. Mediterranean dietary pattern is associated with lower incidence of premenopausal breast cancer in the Seguimiento Universidad de Navarra (SUN) project. Public Health Nutr. (2020) 23:3148–59. doi: 10.1017/s1368980019003835
40. Jalali S, Shivappa N, Hebert J, Heidari Z, Hekmatdoost A, Rashidkhani B. Dietary inflammatory index and odds of breast cancer in a case-control study from Iran. Nutr Cancer Int J. (2018) 70:1034–42. doi: 10.1080/01635581.2018.1494843
41. Sasanfar B, Toorang F, Mozafari Nia M, Salehi-Abargouei A, Zendehdel K. Dietary inflammatory index and breast cancer: report from a large-scale case-control study. Nutr Cancer Int J. (2022) 74:1692–700. doi: 10.1080/01635581.2021.1957489
42. Ghanbari M, Shahinfar H, Imani H, Safabakhsh M, Shab-Bidar S. Association of empirically derived food-based inflammatory potential of the diet and breast cancer: a hospital-based case-control study. Clin Breast Cancer. (2022) 22:E567–75. doi: 10.1016/j.clbc.2021.12.010
43. Park Y, Shivappa N, Petimar J, Hodgson M, Nichols H, Steck S, et al. Dietary inflammatory potential, oxidative balance score, and risk of breast cancer: findings from the sister study. Int J Cancer. (2021) 149:615–26. doi: 10.1002/ijc.33581
44. Harris H, Willett W, Vaidya R, Michels K. An adolescent and early adulthood dietary pattern associated with inflammation and the incidence of breast cancer. Cancer Res. (2017) 77:1179–87. doi: 10.1158/0008-5472.CAN-16-2273
45. Hammad S, Mahmoud R, Shivappa N, Hebert J, Marie L, Tayyem R. Dietary inflammatory index and odds of breast cancer: a case-control study. Food Sci Nutr. (2021) 9:5211–9. doi: 10.1002/fsn3.2493
46. Niclis C, Shivappa N, Hebert J, Tumas N, del Pilar Diaz M. The inflammatory potential of diet is associated with breast cancer risk in urban Argentina: a multilevel analysis. Nutr Cancer Int J. (2021) 73:1898–907. doi: 10.1080/01635581.2020.1817953
47. Gardeazabal I, Ruiz-Canela M, Sanchez-Bayona R, Romanos-Nanclares A, Aramendia-Beitia J, Shivappa N, et al. Dietary inflammatory index and incidence of breast cancer in the SUN project. Clin Nutr. (2019) 38:2259–68. doi: 10.1016/j.clnu.2018.09.030
48. Hajji-Louati M, Cordina-Duverger E, Laouali N, Mancini F, Guenel P. A case-control study in France showing that a pro-inflammatory diet is associated with a higher risk of breast cancer. Sci Rep. (2021) 11:17019. doi: 10.1038/s41598-021-95955-y
49. Sasanfar B, Toorang F, Booyani Z, Vassalami F, Mohebbi E, Azadbakht L, et al. Adherence to plant-based dietary pattern and risk of breast cancer among Iranian women. Eur J Clin Nutr. (2021) 75:1578–87. doi: 10.1038/s41430-021-00869-7
50. Rigi S, Mousavi S, Benisi-Kohansal S, Azadbakht L, Esmaillzadeh A. The association between plant-based dietary patterns and risk of breast cancer: a case–control study. Sci Rep. (2021) 11:3391. doi: 10.1038/s41598-021-82659-6
51. Romanos-Nanclares A, Toledo E, Sánchez-Bayona R, Sánchez-Quesada C, Martínez-González M, Gea A. Healthful and unhealthful provegetarian food patterns and the incidence of breast cancer: results from a Mediterranean cohort. Nutrition. (2020) 79–80:110884. doi: 10.1016/j.nut.2020.110884
52. Shridhar K, Singh G, Dey S, Singh Dhatt S, Paul Singh Gill J, Goodman M, et al. Dietary patterns and breast cancer risk: a multi-centre case control study among north Indian women. Int J Environ Res Public Health. (2018) 15:1946. doi: 10.3390/ijerph15091946
53. Payandeh N, Shahinfar H, Amini M, Jafari A, Safabakhsh M, Imani H, et al. The lack of association between plant-based dietary pattern and breast cancer: a hospital-based case-control study. Clin Nutr Res. (2021) 10:115–26. doi: 10.7762/cnr.2021.10.2.115
54. Kojima R, Okada E, Ukawa S, Mori M, Wakai K, Date C, et al. Dietary patterns and breast cancer risk in a prospective Japanese study. Breast Cancer. (2017) 24:152–60. doi: 10.1007/s12282-016-0689-0
55. Foroozani E, Akbari A, Amanat S, Rashidi N, Bastam D, Ataee S, et al. Adherence to a Western dietary pattern and risk of invasive ductal and lobular breast carcinomas: a case-control study. Sci Rep. (2022) 12:5859. doi: 10.1038/s41598-022-09725-5
56. Jacobs I, Taljaard-Krugell C, Wicks M, Cubasch H, Joffe M, Laubscher R, et al. Dietary patterns and breast cancer risk in Black Urban South African women: the SABC study. Nutrients. (2021) 13:4106. doi: 10.3390/nu13114106
57. Soltani S, Benisi-Kohansal S, Azadbakht L, Esmaillzadeh A. Association between adherence to “dietary approaches to stop hypertension” eating plan and breast cancer. Nutr Cancer. (2021) 73:433–41. doi: 10.1080/01635581.2020.1756354
58. Heidari Z, Mohammadi E, Aghamohammadi V, Jalali S, Rezazadeh A, Sedaghat F, et al. Dietary approaches to stop hypertension (DASH) diets and breast cancer among women: a case control study. BMC Cancer. (2020) 20:708. doi: 10.1186/s12885-020-07209-1
59. Toorang F, Sasanfar B, Esmaillzadeh A, Zendehdel K. Adherence to the DASH Diet and risk of breast cancer. Clin Breast Cancer. (2022) 22:244–51. doi: 10.1016/j.clbc.2021.07.010
60. Aghamohammadi V, Salari-Moghaddam A, Benisi-Kohansal S, Taghavi M, Azadbakht L, Esmaillzadeh A. Adherence to the MIND diet and risk of breast cancer: a case-control study. Clin Breast Cancer. (2021) 21:E158–64. doi: 10.1016/j.clbc.2020.09.009
61. Fereidani S, Eini-Zinab H, Heidari Z, Jalali S, Sedaghat F, Rashidkhani B. Nutrient patterns and risk of breast cancer among Iranian women: a case- control study. Asian Pac J Cancer Prev. (2018) 19:2619–24.
62. Lu S, Qian Y, Huang X, Yu H, Yang J, Han R, et al. The association of dietary pattern and breast cancer in Jiangsu, China: a population-based case-control study. PLoS One. (2017) 12:e0184453. doi: 10.1371/journal.pone.0184453
63. Guinter M, McLain A, Merchant A, Sandler D, Steck S. A dietary pattern based on estrogen metabolism is associated with breast cancer risk in a prospective cohort of postmenopausal women. Int J Cancer. (2018) 143:580–90. doi: 10.1002/ijc.31387
64. Karavasiloglou N, Pestoni G, Faeh D, Rohrmann S. Post-diagnostic diet quality and mortality in females with self-reported history of breast or gynecological cancers: results from the third national health and nutrition examination survey (NHANES III). Nutrients. (2019) 11:2558. doi: 10.3390/nu11112558
65. Ergas I, Cespedes Feliciano E, Bradshaw P, Roh J, Kwan M, Cadenhead J, et al. Diet quality and breast cancer recurrence and survival: the pathways study. JNCI Cancer Spectr. (2021) 5:kab019. doi: 10.1093/jncics/pkab019
66. Wang F, Cai H, Gu K, Shi L, Yu D, Zhang M, et al. Adherence to dietary recommendations among long-term breast cancer survivors and cancer outcome associations. Cancer Epidemiol Biomark Prev. (2020) 29:386–95. doi: 10.1158/1055-9965.EPI-19-0872
67. Lei Y, Ho S, Kwok C, Cheng A, Cheung K, Lee R, et al. Dietary pattern at 18-month post-diagnosis and outcomes of breast cancer among Chinese women with early-stage breast cancer. Cancer Manag Res. (2021) 13:4553–65. doi: 10.2147/cmar.S298619
68. Di Maso M, Dal Maso L, Augustin L, Puppo A, Falcini F, Stocco C, et al. Adherence to the Mediterranean diet and mortality after breast cancer. Nutrients. (2020) 12:3649. doi: 10.3390/nu12123649
69. Chlebowski R, Aragaki A, Anderson G, Thomson C, Manson J, Simon M, et al. Low-fat dietary pattern and breast cancer mortality in the women’s health initiative randomized controlled trial. J Clin Oncol. (2017) 35:2919–26. doi: 10.1200/jco.2016.72.0326
70. Pan K, Luo J, Aragaki A, Chlebowski R. Weight loss, diet composition and breast cancer incidence and outcome in postmenopausal women. Oncotarget. (2019) 10:3088–92. doi: 10.18632/oncotarget.26864
71. Xu L, Peterson L. The impact of diet on breast cancer outcomes [review]. Curr Nutr Rep. (2019) 8:212–21. doi: 10.1007/s13668-019-00278-0
72. Chlebowski R, Aragaki A, Anderson G, Simon M, Manson J, Neuhouser M, et al. Association of low-fat dietary pattern with breast cancer overall survival: a secondary analysis of the women’s health initiative randomized clinical trial. JAMA Oncol. (2018) 4:e181212. doi: 10.1001/jamaoncol.2018.1212
73. Anyene I, Ergas I, Kwan M, Roh J, Ambrosone C, Kushi L, et al. Plant-based dietary patterns and breast cancer recurrence and survival in the pathways study. Nutrients. (2021) 13:3374. doi: 10.3390/nu13103374
74. Jang H, Chung M, Kang S, Park Y. Association between the dietary inflammatory index and risk for cancer recurrence and mortality among patients with breast cancer. Nutrients. (2018) 10:1095. doi: 10.3390/nu10081095
75. Lei Y, Ho S, Kwok C, Cheng A, Cheung K, Lee R, et al. Association of high adherence to vegetables and fruits dietary pattern with quality of life among Chinese women with early-stage breast cancer. Qual Life Res. (2022) 31:1371–84. doi: 10.1007/s11136-021-02985-0
76. Liu X. Evaluation of the Effect of Dietary Pattern on Metastasis of Breast Cancer Based on in Vivo Capture of Circulating Tumor Cells. Jinan: Shandong Normal University (2020).
77. Lorenzo P, Izquierdo A, Diaz Lagares A, Carreira M, Macias Gonzalez M, Cueva J, et al. An epigenetic signature of obesityrelated breast cancer is reflected in leucocytes and associated with Mediterranean dietary pattern [conference abstract]. Obes Rev. (2020) 21(Suppl. 1):e13118. doi: 10.1111/obr.13118
78. Lorenzo P, Izquierdo A, Diaz-Lagares A, Carreira M, Macias-Gonzalez M, Sandoval J, et al. ZNF577 methylation levels in leukocytes from women with breast cancer is modulated by adiposity, menopausal state, and the Mediterranean diet. Front Endocrinol. (2020) 11:245. doi: 10.3389/fendo.2020.00245
79. Schembre S, Jospe M, Giles E, Sears D, Liao Y, Basen-Engquist K, et al. A low-glucose eating pattern improves biomarkers of postmenopausal breast cancer risk: an exploratory secondary analysis of a randomized feasibility trial. Nutrients. (2021) 13:4508. doi: 10.3390/nu13124508
80. Cao S, Lu S, Zhou J, Zhu Z, Li W, Su J, et al. Association between dietary patterns and risk of breast cancer in Chinese female population: a latent class analysis. Public Health Nutr. (2021) 24:4918–28. doi: 10.1017/s1368980020004826
81. Sheikhhossein F, Imani H, Amini M, Hosseini F, Shab-Bidar S. The association between adherence to MIND diet and risk of breast cancer: a case-control study. Int J Clin Pract. (2021) 75:e14780. doi: 10.1111/ijcp.14780
82. Guinter M, Sandler D, McLain A, Merchant A, Steck S. An estrogen-related dietary pattern and postmenopausal breast cancer risk in a cohort of women with a family history of breast cancer. Cancer Epidemiol Biomark Prev. (2018) 27:1223–6. doi: 10.1158/1055-9965.Epi-18-0514
Keywords: dietary patterns, breast cancer, breast cancer risk, prognosis, quality of life
Citation: Bu Y, Qu J, Ji S, Zhou J, Xue M, Qu J, Sun H and Liu Y (2023) Dietary patterns and breast cancer risk, prognosis, and quality of life: A systematic review. Front. Nutr. 9:1057057. doi: 10.3389/fnut.2022.1057057
Received: 29 September 2022; Accepted: 09 December 2022;
Published: 20 January 2023.
Edited by:
Kalliopi-Anna Poulia, Agricultural University of Athens, GreeceReviewed by:
Gianluca Rizzo, Independent Researcher, Messina, ItalyMostafa Dianatinasab, Maastricht University, Netherlands
Copyright © 2023 Bu, Qu, Ji, Zhou, Xue, Qu, Sun and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongbing Liu,  YmluZ2JpbmcxOTk1MDgwNkAxNjMuY29t
YmluZ2JpbmcxOTk1MDgwNkAxNjMuY29t
†ORCID: Yuan Bu, orcid.org/0000-0002-8575-7189
 Yuan Bu
Yuan Bu Junchao Qu
Junchao Qu Siqi Ji
Siqi Ji Jingxin Zhou
Jingxin Zhou Mengxin Xue
Mengxin Xue Jiling Qu
Jiling Qu Huiping Sun
Huiping Sun Yongbing Liu
Yongbing Liu