
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 08 December 2022
Sec. Nutritional Epidemiology
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1052340
This article is part of the Research TopicCare During Pregnancy and Early Childhood for Growth and Development in Low- and Middle- Income CountriesView all 20 articles
 Arti Maria1*
Arti Maria1* Ritika Mukherjee2
Ritika Mukherjee2 Swati Upadhyay1
Swati Upadhyay1 Kumari Pratima1
Kumari Pratima1 Tapas Bandyopadhyay1
Tapas Bandyopadhyay1 Rachita Gupta3
Rachita Gupta3 Bhawna Dubey1
Bhawna Dubey1 Abhinav Sharma1
Abhinav Sharma1 Pranaya Kumar Mall1
Pranaya Kumar Mall1 Manaswinee Sahoo1
Manaswinee Sahoo1 Keshav Kumar Pathak1
Keshav Kumar Pathak1 Priyanka Pawar2
Priyanka Pawar2 Archisman Mohapatra2*
Archisman Mohapatra2*Introduction: The COVID-19 pandemic disrupted newborn care and breastfeeding practices across most healthcare facilities. We undertook this study to explore the barriers and enablers for newborn care and breastfeeding practices in hospitals in Delhi, India for recently delivered mother (RDM)–newborn dyads during the first wave of the COVID-19 pandemic (2020) and inductively design a “pathway of impaction” for informing mitigatory initiatives during the current and future pandemics, at least in the initial months.
Materials and methods: We used an exploratory descriptive design (qualitative research method) and collected information from seven leading public health facilities in Delhi, India. We conducted separate interviews with the head and senior faculty from the Departments of Pediatrics/Neonatology (n = 12) and Obstetrics (n = 7), resident doctors (n = 14), nurses (labor room/maternity ward; n = 13), and RDMs (n = 45) across three profiles: (a) COVID-19-negative RDM with healthy newborn (n = 18), (b) COVID-19-positive RDM with healthy newborn (n = 19), and (c) COVID-19 positive RDM with sick newborn needing intensive care (n = 8) along with their care-giving family members (n = 39). We analyzed the data using grounded theory as the method and phenomenology as the philosophy of our research.
Results: Anxiety among clients and providers, evolving evidence and advisories, separation of the COVID-positive RDM from her newborn at birth, providers' tendency to minimize contact duration and frequency with COVID-positive mothers, compromised counseling on breastfeeding, logistic difficulties in expression and transportation of COVID-positive mother's milk to her baby in the nursery, COVID restrictions, staff shortage and unavailable family support in wards and nursery, and inadequate infrastructure were identified as major barriers. Keeping the RDM–newborn together, harmonization of standard operating procedures between professional associations and within and between departments, strategic mobilization of resources, optimization of human resources, strengthening client–provider interaction, risk triaging, leveraging technology, and leadership-in-crisis-situations were notable enablers.
Conclusion: The separation of the RDM and newborn led to a cascade of disruptions to newborn care and breastfeeding practices in the study institutions. Separating the newborn from the mother should be avoided during public health emergencies unless there is robust evidence favoring the same; routine institutional practices should be family centered.
Feeding mother's own milk (MOM) is advantageous for the recently delivered mother (RDM)–newborn dyad (1–6). Governments worldwide, care providers and breastfeeding support groups, the WHO, and several other stakeholders have been working toward its universalization. It is recommended that mothers should initiate breastfeeding immediately after birth, provide exclusive breastfeeding for up to 6 months, and continue breastfeeding along with complementary for at least up to 2 years. However, ensuring optimal breastfeeding practices among the population at large has been an uphill task for countries, especially low- and middle-income countries (LMICs). Institutional practices around birth and immediately thereafter, e.g., early-uninterrupted skin-to-skin contact, early initiation of breastfeeding, rooming-in, involving families in care of RDM–newborns, help in establishing and sustaining optimal newborn care, and breastfeeding practices (7–9). The increasing rate of institutional deliveries across the world provides an opportunity to ensure that optimal newborn care and breastfeeding practices are reinforced for mother–newborn dyads before their discharge. Unfortunately, the COVID-19 pandemic has challenged health systems worldwide leading to the disruption of routine healthcare services. Anticipating the pandemic's disruptive effect on RDM–newborn care services and optimal breastfeeding practices (10–13), the WHO released mitigatory advisories in early 2020 (14–16). Professional associations and institutional authorities also made efforts to mitigate the disruptions. Still, breastfeeding practices got compromised even in the most advanced healthcare setups (17, 18). Studies published later into the pandemic, i.e., in 2021 and 2022 indicate that breastfeeding practices got compromised in newborns during the pandemic due to a gamut of reasons including lack of high-quality professional services, peer-to-peer support, and social vulnerability and ignorance amidst challenges posed by the mass movement restrictions (19–21).
India has the world's largest annual birth cohort (~25 million) (22). Nevertheless, it continues to struggle in ensuring exclusive breastfeeding (EBF) in infants (as per the latest Demographic and Health Survey in India (NFHS-5), EBF rates were only about 63.7%) India promotes breastfeeding for improving newborn survival and development (23–25). Hence, India prioritizes institutional deliveries and baby-friendly hospital initiatives (BFHI) and has witnessed appreciable improvement in institutional practices for maternal and newborn care. In the initial months of the pandemic, India had to suspend non-essential healthcare services, e.g., out-patient consultations and elective procedures so that health care resources could be mobilized and redirected to pandemic combat (26). Teaching medical institutions (the front-leaders of optimal evidence-based practices) also had to reposition their resources to meet surge demands (27). During these initial months, India also witnessed a dip in institutional deliveries, duration of stay in the hospital post-delivery, and post-partum follow-up (both for the mother and the newborn) (28). To mitigate the potential disruption caused by the pandemic on institutional care of mother–newborn dyads and to standardize practices across India, the Federation of Obstetric and Gynecological Societies of India (FOGSI), National Neonatology Forum of India (NNF), and Indian Academy of Pediatrics released a joint statement in April 2020 (29). Nevertheless, newborn care and optimal breastfeeding practices likely got affected adversely during the pandemic. While there was an inadequate understanding of the “pathways” through which the COVID-19 pandemic impacted newborn care and optimal breastfeeding practices in institutional settings in India during the initial months of the pandemic, there was a gap in knowledge on how these could have been best salvaged. As with the guidance documents of WHO, even the joint statement needed contextual adaptation for implementation across healthcare facilities which most premier health care facilities would have likely undertaken. Thus, there was a need to explore, identify, and learn from experiences and practices across institutions. In the wake of the impediments caused by the COVID-19 pandemic, there was also a window of opportunity to examine institutional practices for newborn care and breastfeeding for critical learnings for building resilient “BFHI” systems. Consequently, we undertook this study to explore the barriers and enablers for newborn care and breastfeeding practices in hospitals in Delhi, India, for recently delivered mother (RDM)–newborn dyads during the first wave of the COVID-19 pandemic (2020) and inductively design a “pathway of impaction” for informing mitigatory initiatives during the current and future pandemics, at least in the initial months. Thus, in this study, we explored how newborn care and breastfeeding practices got impacted in institutionalized mother–newborn dyads in the major teaching medical institutions in Delhi, India in the initial months of the pandemic. We also explored what challenges these institutions faced in their effort to mitigate risk and sustain services and what innovations/enablers they identified in the process that could help inform ongoing practices and also develop standard protocols for future disasters. We believe that policy and program managers and healthcare providers engaged in mother-and-baby care and breastfeeding promotion efforts will find the findings useful for evidence-based action.
We used an exploratory descriptive qualitative design and conducted in-depth interviews (IDIs) with participants from seven medical institutions in Delhi; six of these were premier teaching medical schools in India. Two of the institutions were operating as ‘exclusive COVID-care facilities' at the time of data collection. Delhi had been one of the first and worst affected states and union territories in India during the COVID-19 pandemic (30). It also has some of the premier teaching medical institutions that not only provide state-of-the-art health services to a huge population but also actively engage in innovating and designing case management protocols that are adapted/followed by institutions nation-wide. Exploration of the impact of the COVID-19 pandemic on newborn care and breastfeeding practices in these institutions and how these managed mitigatory efforts held the promise of identifying not only the factors and pathways of impaction but also the potential nodes for intervention. These health facilities are spread across Delhi and cater to a diverse range of clientele across socio-economic strata from the Delhi National Capital Region as well as referral patients from across India with variegated newborn care and feeding practices.
In the study, we considered the “newborn” as the central focus (though it would have been ideal to center around mother–newborn dyads, it was operationally difficult at that point in time). We prepared a list of the stakeholders involved in newborn care and feeding in institutional settings by preparing a “pathway of care” schematic (described below in Study instruments). To start with, we decided to interview the head and the second-senior-most faculty in the departments of neonatology or pediatrics (if the institution did not have a department of neonatology) of the selected institutions. However, we also felt that we needed to get inputs from the head of the department of obstetrics at these institutions in order to triangulate information comprehensively and in line with our phenomenological philosophy. Consequently, we interacted with seven head obstetricians from the institutions studied. Neonatologists and obstetricians were responsible for the care of the newborn and the RDM, respectively, in maternity wards, isolation wards, nurseries, and newborn intensive care units. We considered these HCPs as a common group for triangulating information from “administrative leadership” perspective. Having three such HCPs from an institution added up to a total of 21 respondents in this category and were deemed adequate to saturate information. However, our team also appreciated that most of the maternal–newborn care, and especially that related to breastfeeding, in these institutions was delivered through resident doctors and nurses posted in the labor room and maternity wards. Hence, we requested the neonatology/pediatrics heads to nominate two residents and two nurses from their teams who had been posted in the care of RDM newborns for the longest duration and among the ones most actively involved in caregiving to this clientele among their colleagues. We requested to identify those residents and nurses who had been working in the institution before the pandemic hit, i.e., before February 2020. Thus, at each center, we selected these participants purposively. At that point, we assumed that with as many resident and nurse participants, we would most likely hit information saturation for each (31).
At each center, we included RDMs across each of the three profiles: (a) COVID-19-negative RDM with a healthy newborn, (b) COVID-19-positive RDMs with healthy newborns, and (c) COVID-19-positive RDMs with sick newborns. We did not intend to stratify our results according to the RDM–newborn profile since we aimed at characterizing the “phenomenon” at the institutional level; having the three profiles of RDM–newborn dyads allowed for capturing nuanced experiences and insights. We aimed at interviewing as many participants in each profile till we hit information saturation. These participants were selected purposively with the help of the neonatology residents while balancing data saturation requirements, operational feasibility, participation from the seven healthcare institutions studied, and other socio-demographic characteristics (the socio-economic class, literacy, religion, parity of the RDM, and gender of the newborn). We chose RDMs who had delivered beyond 7 days preceding the date of the interview to a maximum of up to 10 days before. We kept this day-range in order to capture institutional experiences. We also undertook non-formal interactions (NFIs) with the RDMs' escorting family members (1 per RDM) at the hospital.
We interacted with all participants with prior informed consent and appointment. We did not have any refusal to participate.
The participant profiles are shown in Table 1.
For identifying the items of inquiry, we convened a meeting of the unit head and four faculty members (Neonatology), one lactation counselor, one obstetrics resident, and two extramural public health researchers with experience in qualitative methods. We prepared a “pathway of care” schematic for a pregnant woman reporting to a typical hospital in Delhi for delivery during the pandemic until her and her baby's discharge from the hospital. The pathway was reviewed with the three prototype RDM–newborn dyads (mentioned above) in mind. We anecdotally plotted the possible disruptions in pre-pandemic institutional practices at pre-delivery, at time of delivery, immediately post-delivery, during stay in the hospital, at discharge, and during follow-up. We reviewed relevant literature and designed interview guides for each participant category, pretested, and finalized them. We developed separate instruments for each participant category. Some of the items of inquiry were, however, retained across two or more tools. Supplementary Box 1 provides the tool development process. Box 1 illustrates the topics covered in the interviews and the number of items in each tool for the respective participant category. A checklist was prepared for NFI with the RDMs' escorts.
Box 1. Topics discussed in the interviews with Unit Heads, Resident Doctors, Lactation Counselors/Nurses, and Recently Delivered Mothers (RDMs).
Interviews with Unit Heads
• Overall effect of COVID-19 on breastfeeding promotive approaches
• Modifications made to accommodate IPC protocols in care of newborn
• Practices around testing of RDMs for COVID-19
• Challenges in implementing guidelines for breastfeeding and mitigating strategies
• Best practices for promoting optimal breastfeeding according to COVID-19 status
• Practices to reinforce optimal breastfeeding in RDMs after discharge
• Impact of COVID-19-related anxiety and stigma in care of RDM–newborn dyads
• Requirement for further skill building of staff
• Challenges in staff allocation for COVID duty
• Mitigation strategies for staff shortage
• Ways to ensure inter-departmental coordination while managing RDM–newborn dyads
• Suggestions for improving policies and practices
Interviews with Resident Doctors
• Adaptation of practices for newborn care immediately after delivering a baby
• Adaptation of routine in-patient services for RDM–newborn dyads
• Challenges experienced in advising for expression and feeding of breastmilk during COVID-19*
• Impact of COVID-19 on practices for optimal breastfeeding among RDMs*
• Challenges to breastfeeding during the pandemic and its impact on counseling strategies
• Receptivity of RDMs to breastfeeding advice during COVID-19 and its determining factors*
• Strategies adopted for managing babies born to COVID-19-positive mothers as compared to those COVID-19 negative and its effectiveness
• Challenges to decision-making with regard to breastfeeding practices
• Self-reflection on individual performance in ensuring optimal breastfeeding practices in RDMs*
Interviews with Lactation Counselors/Nurses
• Effect of COVID-19 in usual way of counseling of RDMs
• Challenges to effective lactational counseling during the pandemic and mitigating strategies
• Adaptation of newborn care practices for COVID-19 negative mothers
• Most effective strategies for reinforcing optimal newborn feeding practices
Interviews with Recently Delivered Mothers
• Experience regarding care and feeding of your newborn in the hospital
• Advice received on newborn feeding from hospital and family members during hospital stay and its impact
• Challenges experienced in feeding newborns during hospital stay and ways to address them
• Support received from the hospital that have helped her in feeding her newborn
• Support expected from hospital staff in feeding newborns during hospital stay
• Support expected for optimal feeding after discharge and in follow up
*Also discussed with Lactation Counselors/Nurses
IPC-Infection prevention and control; RDM- Recently delivered mother, COVID- Coronavirus disease
Six interviewers collected data—two qualitative researchers [AMo (male, MD) and RM (female, PhD)] and four neonatology faculty members [two females (SU and KP) and two males (SK and TB)], trained in interviewing techniques. The team interacted with participants over video meetings (Google Meet and WhatsApp) since physical meetings were restricted during the pandemic (32).
IDIs with the doctors were analyzed using English transcripts. Responses from nurses, RDMs, and their escorts were directly analyzed from the audio (“tape analysis”) to allow for the comprehension of responses that were in mixed language (Hindi and Indian English) and often emotional (33, 34). Analysis was done using NVIVO (35). Responses were free-listed and coded thematically using the grounded theory approach by RM, AMo, and PP (female, MPH), in consensus (36). We achieved data saturation for each participant category (31). The code frequencies were grouped as follows: “None” (0%); “Few” (below 25%); “Some” (25–49%); “Many” (50–74%); “Most” (75–99%); and “All” (100%) (37). “Quotable quotes” were identified from the responses.
We improvised the “pathway to care” schematic as an inductive framework enumerating the disruptions to breastfeeding practices in institutionalized RDM–newborn dyads. For this, we (RM, AMo, PP, AMa, SU, KP, and TB) triangulated narratives across stakeholder categories and incorporated feedback from the larger team of authors between November 2020 and February 2021 through an iterative process. The findings were deemed consistent with the data.
Quantitative information was summarized as frequency and proportion using MS Excel (MS Office 365).
The RDMs and their escorts were interviewed at the hospital/home between the 7th and 10th day of delivery as per their convenience. We conducted and audio-recorded each interaction with a prior appointment and informed verbal consent for participation in the interview and for audio-recording, which was also recorded prior to the initiation of the interview. Written consent was difficult to obtain due to the COVID-19 physical access restrictions in the isolation wards and healthcare facilities. The interactions were done in the participant's preferred language. The HCPs were interviewed in the office. The IDIs were limited to 45-to-75 min, while the NFIs were for about 10–15 min each to manage respondent burden and sustain engagement. Trained interviewers administered the interview items verbatim using structured interview guides. The responses were audio-recorded on multiple devices to protect against data loss. Transcripts were matched with the recordings for accuracy and completeness before analysis; we did tape analysis to capture the “sentiments” of the respondents. Findings were reported using the COnsolidated criteria for REporting Qualitative research (COREQ) checklist.
The age of the senior HCPs (neonatologists, pediatricians, and obstetricians) was 58.1 ± 3.4 years, the residents 29.3 ± 3.1 years, and nurses 43.2 ± 5.6 years. The age of the RDMs was 23.8 ± 3.2 years; 44.4% (n = 20) of these were first-time mothers, 82.2% (n = 37) were Hindus, 15.6% (n = 7) had 0–5 years of formal education, 8.9% (n = 4) were from economically weaker section, 51.1% (n = 23) had delivered through cesarean section. Of the newborns, 44.4% (n = 20) were female. We have provided the details of the RDMs' profiles and newborn care and feeding practices in Supplementary Table 1.
Here, we have narrated the key barriers across RDM–newborn profiles (Table 2); these were most prominent in the initial months of the pandemic.
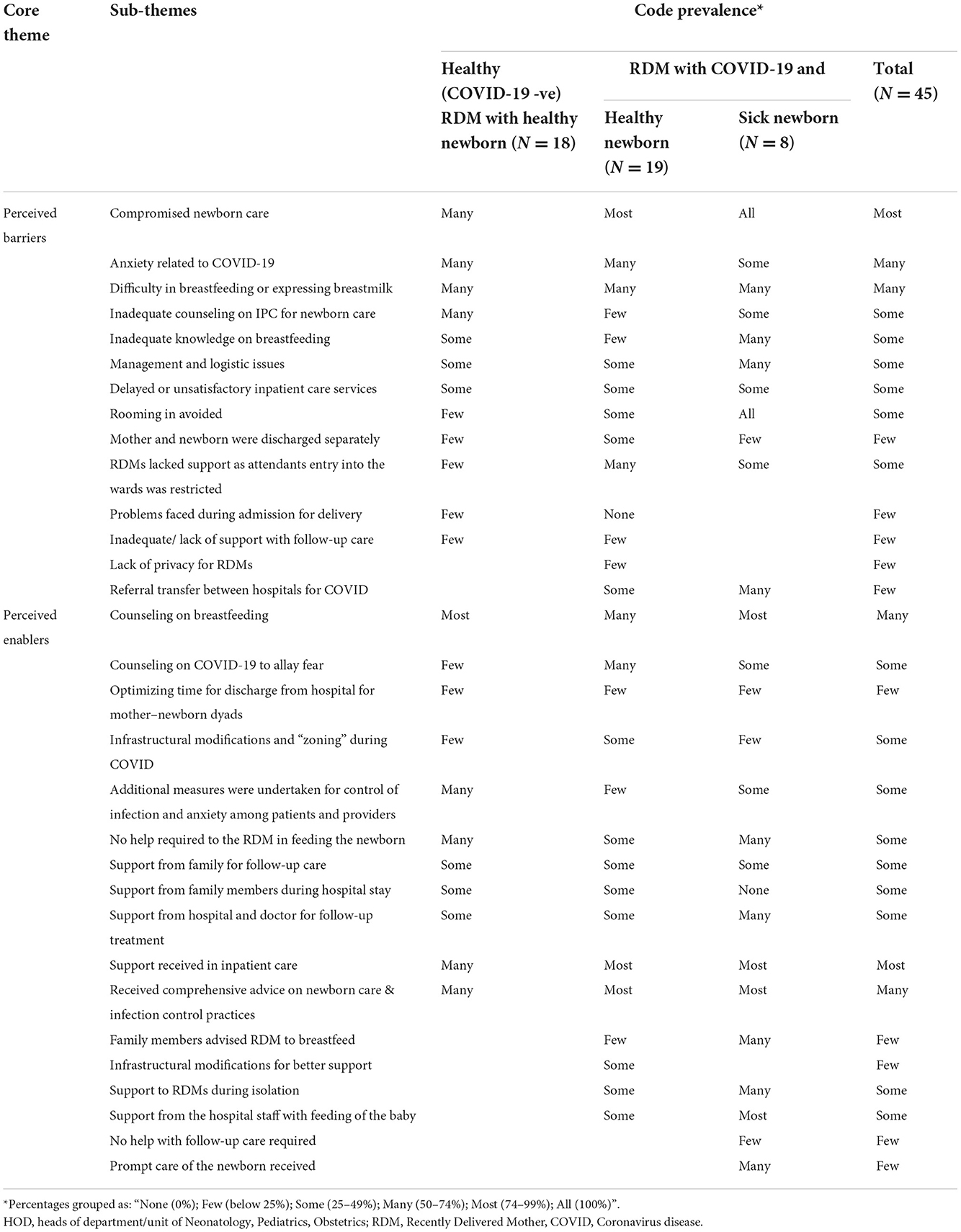
Table 2. List of core themes and sub-themes for optimal breastfeeding practices emerging from inductive data analysis and their code prevalence according to the different groups of recently delivered mothers.
Providers as well as clients were anxious that they might contract and/or transmit SARS-CoV-2 with fatal outcomes. Staff anxiety was attributable to inadequate availability and knowledge of using personal protective equipment (PPE), and unavoidable interactions with patients and escorts who often lacked COVID-appropriate behavior. Several staff members got exposed inadvertently, especially during posting in COVID-suspect wards, and had to undergo quarantine; this heightened anxiety and reluctance among colleagues.
“Reluctance was from seniors, including me. But residents and sisters were always prompt and discharged their duties sincerely, not putting senior people at risk of infection for work which may be handled (over phone) without going (physically).” (HOD, Neonatology)
During the initial months of the pandemic, institutional isolation had been made mandatory for all individuals testing positive for SARS-CoV-2. The RDMs, especially those asymptomatic, found such isolation extremely distressful. They were often not convinced that they were infected and did not want to co-isolate with those with symptomatic infection.
“I did not have fever or cold. I had no symptoms, not even breathlessness. I had absolutely no problems. Even then I was told that I am corona positive. This is my exact problem here. How can they do that? I still have no symptoms and no ailments. No cough, no cold, no fever. Yet, they say I am corona positive.” (-RDM, COVID-19 positive with healthy baby)
There were instances when RDMs, including those negative for COVID-19, resisted rooming-in and/or breastfeeding, fearing transmission of infection to their newborns. There were also instances when RDMs were more willing to breastfeed than to express and transport; they felt that storage may lead to an increased risk of infection. Clients feared that they and/or the newborn may get infected during the hospital stay. At times, family members did not want to accompany the RDM to the hospital for fear of getting infected. The RDMs and family members would often insist on discharge immediately after delivery. Family members also resisted rooming-in, breastfeeding, and transportation of expressed milk citing the risk of transmission of infection.
“I still feel that my baby became COVID positive because I breastfed. I hope I did not infect him, but I feel so because I breastfed him. So, I do not want to take any further risks. I do not want to breastfeed him again.” (-RDM, COVID-19 positive with sick baby)
As separate wards had to be created for risk stratification, resources often fell short. Procurement of new equipment had to be expedited and prudently distributed between the wards. PPEs, being in short supply, had to be used frugally. There was a lack of space for expansion. In most places, the isolation ward for the RDM was relatively far off from the nursery making transportation of expressed milk difficult. There were times when suspected COVID-19 patients and non-COVID-19 patients had to be kept in the same area, leading to increased anxiety among the RDMs and those accompanying them. Distancing between beds and rooming-in was challenging, and privacy could not be ensured for the RDMs to breastfeed or express milk.
As evidence was evolving fast, hospital and departmental protocols had to be updated frequently. The staff faced difficulty in adapting to the frequent change in the hospital protocols. Providers reported that obstetricians and neonatologists differed in respective departmental protocols for skin-to-skin contact, rooming-in, breastfeeding, and discharge. Initially, there was a lack of clarity on responsibilities and coordination between the departments.
“Problem is about the mindset and overcoming these resistances with our own [name of department] colleagues. I am strong minded, I get it implemented if these recommendations are strong, I still want to do it, but probably it's not all in my hands. I will definitely work on it, we as a team will try to do something and definitely, we will make it happen.” (- HOD, Department anonymized)
Given the surge in adult patients due to COVID-19, staff from the neonatology as well as obstetric departments was diverted toward adult wards, leading to acute staff shortage therein. The raging pandemic, quarantine protocols, and a few staff resignations accentuate the shortage. At times, to meet surge preparedness and/or meet gaps in staff strength, personnel from other specialties who had little/no experience in maternal–newborn care were posted in nurseries and maternity wards.
“Mother-baby dyads are being handled by health care providers who are usually not taking care of the newborn or mothers. So definitely we are trying to educate more and more.” (-HOD, Neonatologist)
Delays in test results for the RDMs led to prolonged stay of the newborn in the nursery, thus overburdening the inadequate staff therein. PPEs also reduced the staff's efficiency.
“Repeated counseling, getting expressed breast milk, looking at babies frequently, that all needs manpower, and time and manpower, get doubled when you are working with PPE.” (-HOD, Neonatologist)
Due to infection prevention and control (IPC) protocols, RDM's escorts were disallowed in delivery rooms and maternity wards. RDMs, especially those who were primiparous or had delivered by cesarean section, needed support for self-care and expression of breastmilk and faced many difficulties; escorts were anguished.
“Because of COVID, mother and baby were completely isolated. I or any other family member was not allowed inside. But this is not right, especially because she had C-section and someone should have been allowed to take care and help her.” (- Family member of RDM)
In the initial months of the pandemic, providers were unsure if breastfeeding was safe during COVID-19. If the RDM was COVID-19 positive or suspect, her newborn was separated immediately after the birth and started on artificial milk till the dyad tested negative for SARS-CoV-2. At times, a mother delivering at a non-COVID hospital was referred to a designated COVID hospital on being detected positive, while her baby was retained at the hospital of delivery. The separation was quite distressing for the RDMs and their families.
“I was not allowed to breastfeed or send expressed breastmilk to my baby. My baby was not given my milk. (-RDM, COVID-19 Positive with healthy baby)
“I did not even see my baby since birth, how could I have possibly breastfed her?”
(-RDM, COVID-19 Positive with healthy baby)
“I have to go to the other building to get the milk. I do it about 7-8 times a day. It is difficult as I have arthritis, but I have to do it because if I won't, who else (would do it)!” (- Mother-in-law of a COVID-19 positive RDM)
Interaction between the doctor, RDMs, and family members got compromised due to fear and limited visitations in face of staff shortage. The gap for counseling services was most glaring at places where these were most needed.
“When I had my first child, I was advised well about the breastfeeding. However, this time they explained nothing to me. They did not discuss or advised anything. Since delivery, the doctor has not even visited once to check on me.” (-RDM, COVID-19 negative)
Repeated donning and doffing of PPEs were inconvenient. Furthermore, conversations with masks on their face compromised both the duration and quality of interaction. Massages for newborn care and breastfeeding could not be provided consistently due to various reasons, e.g., reallocated staff often lacked standardized skills and motivation to counsel, specialties differed in their opinions, etc. All these factors adversely affected the opportunities for counseling in the early postnatal period for establishing optimal breastfeeding. Pandemic restrictions had separated the RDM from the family. Thus, the two had to be counseled separately. This not only increased the workload of the staff but was also deemed as less efficient than counseling both together.
Some of the RDMs and family members also reported being unaware of the newborn's care and wellbeing, indicating a gap in communication.
For instances where the RDM was COVID-positive, the family resisted rooming-in of the baby and rather preferred to take the baby home. In some cases when the mother was COVID-negative and the baby required nursery care, even obstetricians as well as families preferred that the mother be discharged to minimize risk exposure. Discharging the RDM and her newborn at different time points disrupted breastfeeding practices. Families also reported difficulty in managing the newborn at home without the mother.
“I am troubled that they are not discharging my wife. I am staying with the baby alone in the house. It's difficult for me to manage. Yesterday they asked me to come at 10 am today and they would discharge, now they are saying they will not” (- Family member of RDM)
Most hospitals had suspended post-partum as well as neonatal follow-up clinics and had moved on to patient-initiated telephonic follow-up. However, with frequently changing staff, it was difficult for an RDM to contact the staff that had tended to her and her newborn when in the hospital. Also, hospitals at times did not have phone numbers of the RDMs or their families to contact after discharge. The providers were unsure if optimal breastfeeding practices were sustained once discharged from the hospital.
While most patients were satisfied, some complained of inadequate communication during their hospital stay. Family members at times reported facing stigmatized behavior and inadequate help from the hospital support staff. The RDM in the isolation ward as well as family members felt under-informed; they reported a gap in communication with the nursery staff. As entry into the nursery was restricted, they questioned the quality of care for the newborn.
While most clients appreciated improved hygiene and IPC at the hospital, others expressed dissatisfaction. They complained about unclean wards, walkways, toilets, cumbersome administrative processes, uncomfortable beds (no backrest to support breastfeeding mothers), and lack of privacy and comfort. Family members accompanying RDMs reported overcrowding, lack of chairs in waiting areas, and lack of adequate, clean, and separate toilets for men and women.
“Hygiene was very bad. 2 maternity rooms 1 room had 12 – 15 beds while the other room had 3 beds. At one point 10 – 12 patients were there who were all using one common toilet. The toilet was being cleaned only once in 24 hrs. (There were) cockroaches in the room” (- Family member of RDM)
The clients complained that stringent IPC practices coupled with conflicting information from different health personnel led to avoidable delays in services. Family members had to arrange their own personal protective provisions adding to their out-of-pocket expenditures.
“We reached emergency at 2 am and then the report was not accepted, she was not given the private ward…These were not good. The Gynae doctor said we can do the test from outside but emergency doctor refused…Took too much of time in admission” (- Family member of RDM)
We noticed temporal trends in the providers' and participants' attitudes to COVID-19 after the initial months; practices and innovations emerged as enablers (Tables 3, 4) in response to disruptions caused by the pandemic.
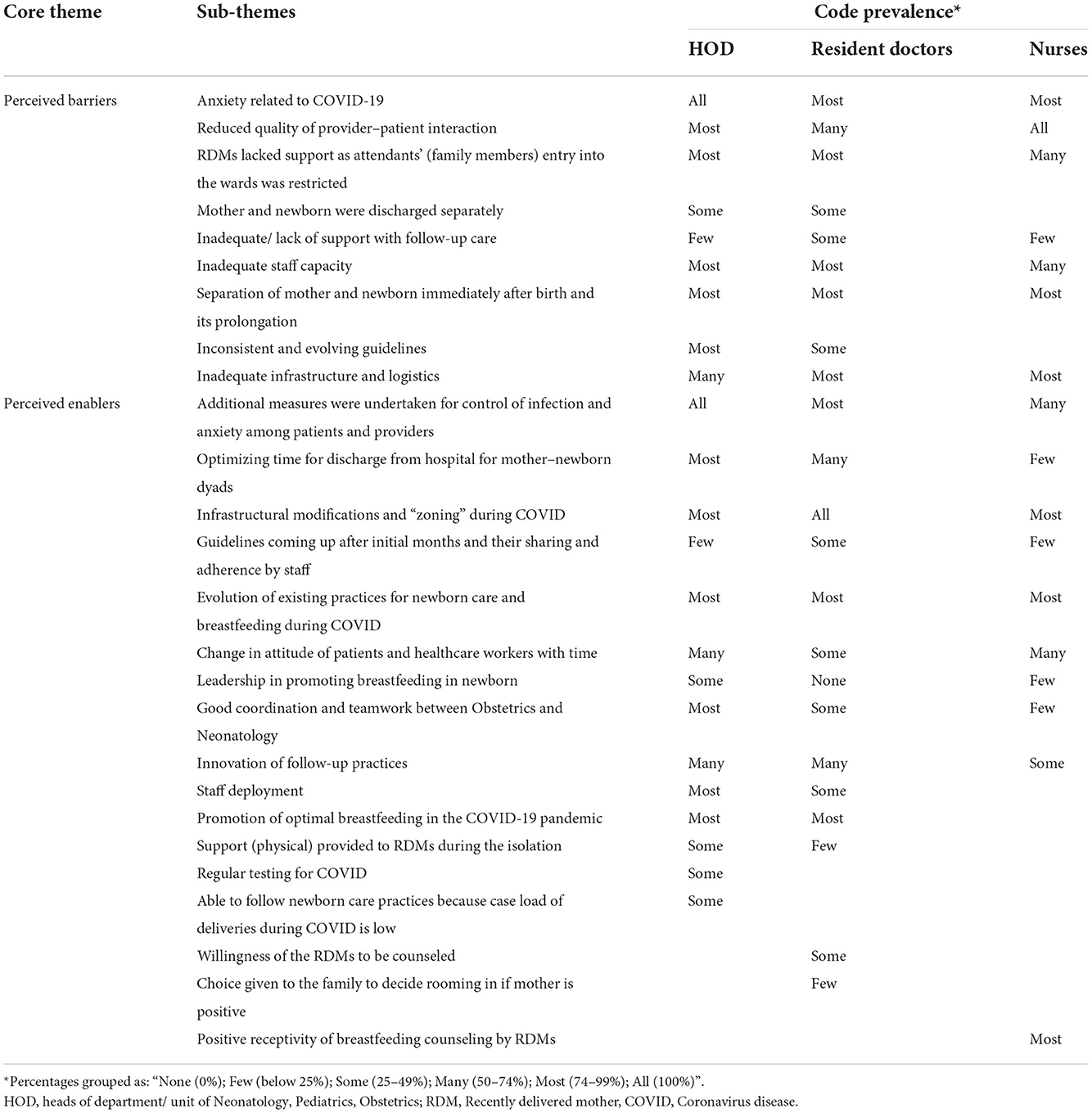
Table 3. List of core themes and sub-themes for optimal breastfeeding practices emerging from inductive data analysis and their code prevalence according to the healthcare providers.
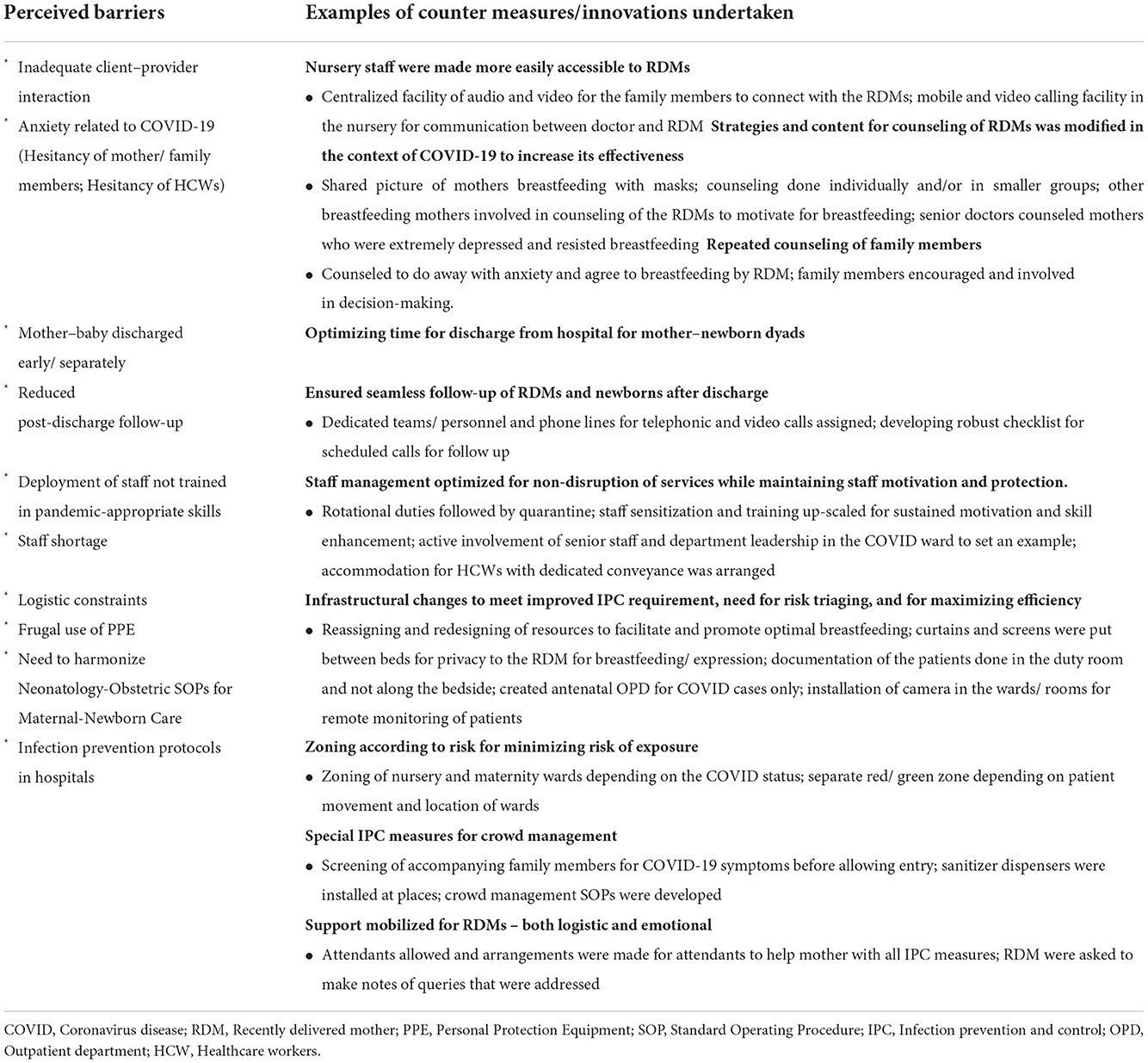
Table 4. Barriers experienced, and counter measures undertaken to ensure optimal breastfeeding among institutionalized mothers during COVID-19 pandemic.
Toward August 2020, evidence was emerging that breastfeeding was safe during the pandemic. The COVID-19 wave in Delhi was also receding. HCPs were more confident and RDMs and family members were more receptive toward breastfeeding and rooming-in-related advice. The workload in hospitals was easing-off. The availability of PPEs had improved. Concurrently, COVID anxiety had also started waning. Provider–patient interactions improved.
Hospital processes had become more “COVID-adaptive” over time. Operational innovations minimized the risk of cross-infection and optimized IPC practices and the use of resources. For example, doctors scheduled clinical rounds of COVID wards after that in non-COVID wards and did the case notes documentation in the duty room instead of bedside, thus, minimizing the demand for PPEs. Staff allocation rosters were rationalized according to risk exposure and client load. Simultaneously, sensitization training and hand-holding support were also provided to the staff rotated from other specialties to the nursery and maternity wards. Crowd management practices became more efficient.
Suspension of elective services, mass movement restrictions (lock-down), and having designated COVID facilities helped in optimizing workload and improving institutional efficiency. As referral chains for transferring COVID-19 cases to designated facilities strengthened, case load on non-COVID facilities decreased. Institutional designations as exclusive COVID/non-COVID facilities made the implementation of SOPs easier, safer, and more efficient.
“Through these past 6 months, whole system has evolved so much! Initially we didn't know what to do. When we got COVID positive mother, the first question was, what to do with the baby if the baby is well. Now we have a separate step-down unit… we have COVID positive step-down nursery, we have COVID positive ward. So initially we did not have the whole setup and we used to lack on those aspects, and we have built ourselves around it.” (-Resident Doctor)
As testing capacity increased, all RDMs were tested for SARS-CoV-2. This increased confidence in the staff. The RDMs and families appreciated that the hospitals were strict with norms of social distancing and IPC and had made testing mandatory for all patients seeking admission. The RDMs, newborns, and HCPs were also monitored for COVID-19 symptoms. Symptomatic HCPs were tested and isolated, if positive. Hospitals had arranged separate accommodation, travel, and quarantine facilities for the staff on COVID-19 duty. This improved staff availability while minimizing the exposure of their families to SARS-CoV-2.
With time, the staff had adopted effective ways to counsel clients. HCPs had increased their availability and access for RDMs and family members. Departments now laid greater emphasis on counseling for skin-to-skin contact, breastfeeding, and rooming-in during pre-labor, labor, and at discharge to the RDMs and families. Providing detailed information on breastfeeding and newborn care as well as engagement of family members in the decision-making process led to better compliance with breastfeeding practices and overall satisfaction among the clients. Regular telephonic or video call–based updates about RDMs and their babies to the family members were initiated in two study hospitals. Reports were also shared with the family through WhatsApp messages. Several RDMs reported receiving prompt and timely treatment. The staff was also reported to be more patient, caring, and addressing their queries. Even the capacity of the support staff (e.g., guards and workers) for facilitating patients improved with experience.
“We get to talk to the doctor every day and get updates on the patient…they gave their number and they called twice in a day too! Once in the morning and once in the evening. They made two video clips and sent it to us, so that we can see the baby” (-Family member of a COVID-positive RDM)
“People say bad things about Government hospitals but my experience was very good. The doctors patiently heard and advised every patient, and we could ask them anything and they would always provide a solution for that.” (-Family member of a COVID-positive RDM)
Over the months, most facilities realized that if the RDM and her newborn were discharged on different days, it impeded breastfeeding. Consequently, they made efforts to align their discharge dates, i.e., only after both had completed mandatory days of institutional isolation or had tested negative for SARS-CoV-2. If rooming-in was possible, they were discharged after establishing breastfeeding.
One of the study hospitals had started allowing one family member per RDM to visit her in-hospital but with PPE on and within strict visiting hours. A few institutions had allowed family members into the nursery and involved them in the care of the newborn. This had improved care as well as feeding of expressed breastmilk.
As routine health services were impaired in the community, the institutions ensured that vaccination of the newborn was up to date and that the RDMs and family members had been adequately counseled for exclusive breastfeeding and after-care at home, at the time of discharge. They prioritized follow-up calls to RDM–newborn dyads that were in the high-risk category.
The use of video-calling services was a major technological innovation that one of the institutions had adopted. With funding from the Government, the institution had received hand-held electronic tablets with an internet connection—these were used by the staff in the nursery to interact with the RDMs under isolation. The RDMs in the said institution hailed this as a major enabler that allayed their anxiety as they could interact with the nursery staff as well as watch their babies being cared for in the nursery.
Gradually, the hospitals were able to install exhaust fans, cameras, and devices for remote monitoring and counseling of patients. Separate passages, lifts, and “red-green-yellow” zoning were done based on infection status for positive, negative, and suspected cases, respectively. Donning and doffing areas were separately ear-marked. Equipment was also procured for each zone to ensure IPC. Separate labor rooms and neonatal intensive care units (NICUs) were accordingly zoned and equipped expeditiously.
The Federation of Obstetric and Gynecological Societies of India (FOGSI), National Neonatology Forum of India (NNF), and Indian Academy of Pediatrics (IAP) had come up with a joint statement titled “clinical practice guidelines for perinatal-neonatal management of COVID-19 infection” on 26th March 2020 (38); an updated second version was released on 7th May 2020 (39). Simultaneously, the Indian Council of Medical Research (ICMR) also actively updated its advisories. Availability and wider dissemination of these guidelines facilitated the adoption and standardization of practices by providers who were now more confident in taking decisions and counseling the patients and their family members. Departmental standard operating protocols (SOPs) were revised in view of the guidelines after internal and interdepartmental meetings. Sharing literature on social media groups, e.g., closed WhatsApp groups, webinars, and training (physically provided in small groups or through virtual platforms) improved staff confidence for coordinated care.
The pandemic demanded efficient coordination and active engagement between Obstetric, Neonatology/Pediatric departments for optimal care of RDM–newborn dyads. As structured management protocols were evolving, coordination between these departments became dynamically adaptive. We noted that the departments that already had a smooth consensus-driven work culture could tide over the coordination challenges effectively. Day-to-day coordination was often through non-formal (not written down) understanding and accomplished over WhatsApp groups.
“…there are some coordinators in OBG team and neonatal team. Initiating breastfeeding is more of a joint effort.” (-HOD, Neonatology)
Departmental leadership played a very critical role as an enabler (“leadership in crisis”). Active engagement in surge preparedness for IPC and pandemic combat (“leading from front”) was deemed as a major leadership trait by the participants. These “leaders” advocated for the sustenance of pre-existing quality of maternal and newborn care practices even in the COVID wards, had active involvement in updating and contextual adaptation of the SOPs, and were at the forefront of patient care and administration. They kept abreast with the fast-evolving evidence and this instilled confidence among peers and staff. Alongside, they organized frequent sessions of counseling with staff and patients and motivated them constantly, exercised high levels of emotional intelligence, and demonstrated empathy for the overworked and often anxious staff and distressed patients.
“…our practices in terms of ensuring that the baby gets 1st drop of milk and every drop of her own mother's milk, is something that we ensure from the point that the lady is in the labor room…We have (a practice that) for the mother and her baby, breastfeeding has to be established… So, we ensure it happens here.” (-HOD, Neonatology).
Figure 1 shows the factors (in white and yellow boxes) influencing breastfeeding practices and their interactions (arrow heads) in institutionalized RDM–newborn dyads during the COVID-19 pandemic. The red colored boxes suggest the endpoints. Various barriers are depicted in the white and yellow boxes. The barriers highlighted in yellow are those that the institutions could intervene and overcome, at least partially.
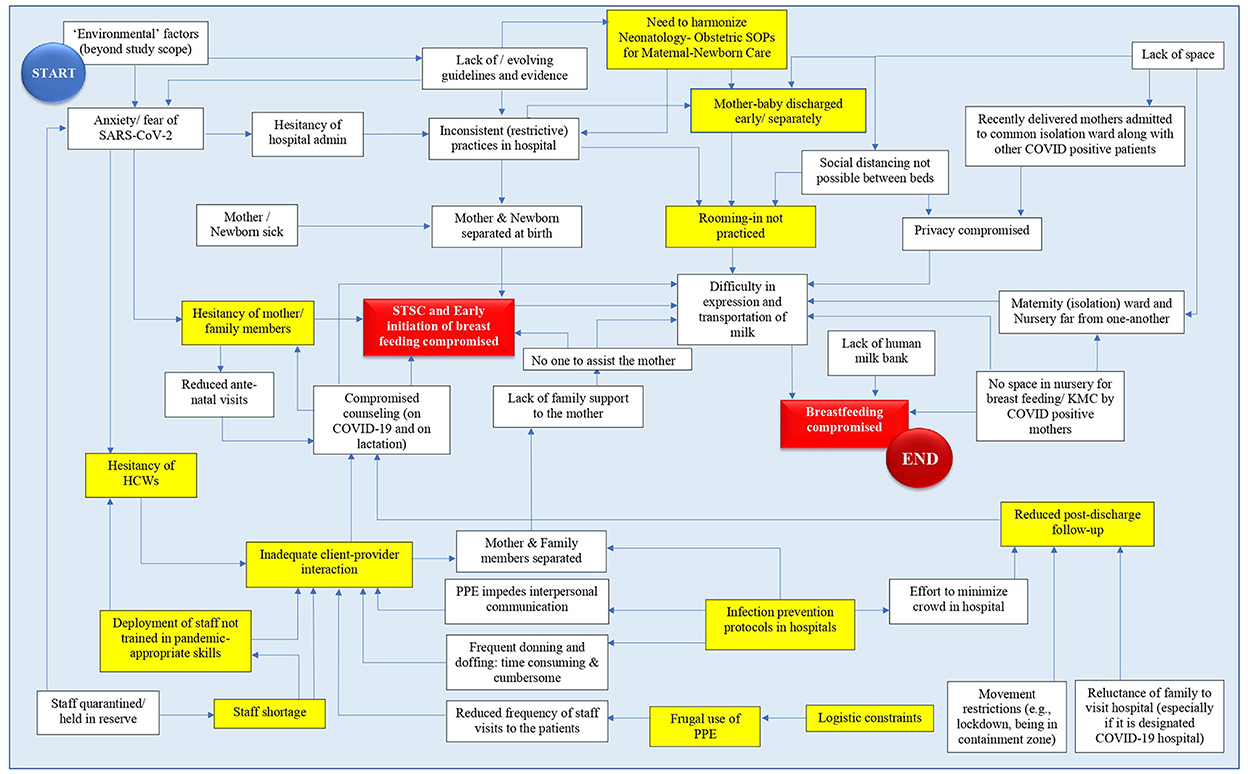
Figure 1. Analytic framework depicting the pathways of impaction of optimal breastfeeding practices in institutionalized mother-newborn dyads during the COVID-19 pandemic. The various barriers are depicted in the white boxes – the ones targeted by the study institution for mitigation have been highlighted in yellow. Boxes highlighted in red represent end-points; HCW, Health Care Worker; KMC, Kangaroo Mother Care; PPE, Personal Protection Equipment; STSC, Skin-To-Skin Contact; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; COVID, Coronavirus disease; SOP, Standard Operating Procedure.
Table 5 summarizes the suggestions for improvement coming from all participants of the study.
We observed that the pandemic disrupted newborn care and breastfeeding practices across RDM–newborn profiles at the study institutions through complex interrelated pathways. We identified RDM–newborn separation at birth as an important barrier that institutions largely failed to overcome in the initial months of the pandemic. In the initial months of the pandemic, there was considerable confusion and stress for healthcare providers (HCPs) and breastfeeding mothers regarding the safety of breastfeeding in RDMs with SARS-CoV-2 infection. Furthermore, the high delivery case load (~40–50 deliveries/day) at the participating facilities and lack of space precluded the possibility of rooming-in of so many suspect mothers and baby dyads in isolation wards. Institutions tried to stratify the laboring mothers by the status of SARS-CoV-2 test reports. The institutions kept the RDM baby separated until the test was reported negative. Since test results were invariably delayed, this resulted in the separation of the RDM and her newborn. Once separated, rooming-in and establishing breastfeeding became challenging. For a baby who was admitted to the nursery away from the mother, transportation of expressed breastmilk from the isolation ward to the nursery was another major barrier in our study. As a mother's visitation to the nursery to be involved in the care of her baby was limited for the fear of spreading COVID-19, there was considerable anxiety and stress among mothers that was counterproductive for their uninterrupted milk supply. We also noted that formula feeding and early discharge of the baby with alternative caregivers while the mother was still admitted in the COVID-ward became common practices.
Findings similar to ours have been reported from other countries too. In a global online survey involving 62 LMICs to provide insights on disruptions to coverage and quality of small and sick newborn care, it was found that preparedness for COVID-19 was suboptimal in terms of guidelines and availability of personal protective equipment and that the guidelines for testing of mother and newborn changed frequently. More than 85% of health personnel feared for their own health and 89% had increased stress (21). Newborn care practices were disrupted both due to reduced care-seeking and compromised and inexperienced staffing in the COVID wards. More than half reported that standard practices for small neonates such as kangaroo mother care were either discontinued or discouraged. Separation of the mother–baby dyad was reported for both COVID-positive mothers (50%) and those with unknown status (16%). Follow-up care was disrupted primarily due to families' fear of visiting hospitals (~73%). COVID-19 has also been reported to have also compromised the quality of counseling and the extent of social support to RDMs; we have also observed the same in this study (40).
Despite clear and comprehensive guidance from the WHO regarding exclusive breastfeeding, during the beginning of the pandemic (14), newborns were often separated from the mother at birth. Even professional associations, e.g., in the Philippines, Thailand, Malaysia, and the United States of America (USA) released guidelines supporting the separation (41). The separation affected breastfeeding (41–43). Some places allowed only screened donated breastmilk from COVID-19-negative mothers (44, 45). The disharmony between guidelines from the professional associations and that from the WHO was evident in the high-income countries as well. In a study (46) comparing the initial recommendations of the professional obstetrical and gynecological societies of five high-income countries, namely Australia, New Zealand (NZ), Canada, the United Kingdom (UK), and the USA, with that from the WHO (14, 16, 47), none of these aligned perfectly. Discordant guidelines impeded confident decision-making and the families received conflicting information. First-time mothers who were COVID-19 negative also reflected fear, anxiety, and doubts and often made a personal choice of not wanting to breastfeed their newborn for fear of unknowingly transmitting COVID-19 infection (test results were at times considered to be unreliable) (48). Inadequate provider–patient interaction both during hospital stay and during follow-up was another barrier to successful breastfeeding, during the COVID-19 pandemic. Nevertheless, mitigatory efforts were also responsive to the evolving evidence on the low risk of transmission of the virus through breastfeeding (49–55). For example, in April 2020, the American Association of Pediatrics recommended separating infected mothers from newborns but in July 2020, it retracted the advice (56, 57).
In the present study, the use of video-calling services was a major technological innovation that one of the institutions had adopted. This innovation was found to be a major enabler that allayed the anxiety of the mothers. Family-centered care (FCC) in the NICU focuses on building trust, reducing anxiety, partnering, and integrating families into the care of their infants. Many newborns in NICU have critical health issues causing anxiety and feelings of fear to parents and families. Separation, especially in life-threatening conditions, causes worry and apprehension among families. Providing a means for families to view live videos of their infants, any time of the day or night, and while away from the unit, can help alleviate this stress. Virtual visitation of caregivers has been used in a few NICUs in the USA and UK even before the COVID-19 pandemic (58–61). The NICVIEW is a web-based camera system (WBCS) that streams real-time video of the baby around the clock. In a questionnaire survey conducted in a Canadian hospital, following the implementation of NICVIEW for virtual visitation of caregivers during the COVID-19 pandemic due to the strict implementation of the policy of restricted entries found that 98.0% of parents felt very connected with their baby, and almost 90.0% of parents reported having the WBCS helped reduce their anxiety and stress levels to a great extent. An accepting attitude from HCPs, especially the nursing staff, is of paramount importance in improving the successful implementation of WBCS in the NICU.
While family centricity is important, HCP centricity was also critical during the early days of the pandemic, since it kept the HCPs confident and motivated. In a large hospital-based prospective cohort study from India with high patient load and resource limitations, a dynamic policy using a low-cost paperless communication system with mobile devices was reported to reduce the risk of HCP infection, improve their motivation, and re-deployment in the COVID wards (62). There are reports that leadership skills were useful during the pandemic for delivering essential facilities and services rapidly and with empathy during the pandemic (63–65). In the present study, we recorded leadership-in-crisis skills as helpful in mounting up a coherent response within the healthcare institutions, e.g., in motivating the staff, by rapidly delegating authority to organizational management, framing and updating standard operation procedures as per changing guidelines for the management of pregnant women and their neonates with suspected or proven COVID-19 infection, allaying anxiety of patients and providers, by innovating for improving neonatal and follow up care, and interdepartmental coordination, besides facilitating the mobilization of resources. This guiding coalition had an overriding vision to contain the infectious disease throughout the pandemic, while simultaneously catering to patients with and without COVID-19 infection. In the present study, other enablers which played a critical role in improving neonatal care and breastfeeding rates have conducive attitudes and neonatal care practices with the passage of time. Certain systemic interventions were also helpful e.g., designating some facilities exclusively for COVID-19 care, strengthening referral pathways, and release of joint statements by FOGSI-NNF-IAP. FOGSI-NNF-IAP Joint Statement greatly helped practitioners take confident decisions related to sustaining routine pre-pandemic practices for breastfeeding and newborn care (29). We infer that in case of a public health crisis, national health agencies and professional associations must ensure that coherent guidelines are released at the earliest and disseminated widely along with strategies to counter misinformation.
We pooled information from clients and providers across seven premier institutions in Delhi, which had pre-existing systems for evidence-based optimal newborn care practices. This gave us an opportunity to identify deviations from the “near-ideal.” However, we acknowledge that each institution had its own unique strengths and weaknesses, and our aggregated analysis does not delve deeper into these. To address the influence of temporal change, we requested the participants to respond with the initial 6 months of the pandemic (March-August 2020) as the reference period. We could not explore post-discharge breastfeeding practices.
We recommend against separating the mother and the newborn during public health emergencies without robust evidence favoring the same. We call for making routine RDM–newborn care practices family-centered at all times. We encourage the practice of early release of joint statements by professional associations and authorities during public health emergencies. Leveraging social media and video conferencing technology, having dedicated lactation teams, investing in improved hospital architecturalplanning, and having an in-campus human milk bank could provide an advantage against potential disruption and merit further research.
The learning of this study should help in building institution-based newborn care services more resilient against disruptions by public health emergencies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The Institutional Ethics Committee of ABVIMS and Dr. Ram Manohar Lohia Hospital, New Delhi reviewed and approved the study protocol. Administrative approval was provided by the Ministry of Health and Family Welfare. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AMa: concepts, design, definition of intellectual content, tool development, manuscript editing, manuscript review, and guarantor. RM: tool development, literature search, data acquisition, data analysis, manuscript preparation, and manuscript editing. SU, KPr, and TB: data acquisition, manuscript editing, and manuscript review. RG, BD, AS, PM, MS, and KPa: manuscript review. PP: tool development, literature search, data acquisition, and manuscript review. AMo: concepts, design, definition of intellectual content, tool development, data acquisition, data analysis, manuscript preparation, manuscript editing, and guarantor. All authors contributed to the article and approved the submitted version.
This study was commissioned by the World Health Organization's India Country Office, New Delhi. The sponsors had no role in the conduct of the study and the analysis and interpretation of the findings. The researchers were independent of the funders throughout the study.
We convey our sincere thanks to the senior faculties in the Departments of Neonatology, Pediatrics, Obstetrics, and Gynecology of the participating institutions, i.e., All India Institute of Medical Sciences (AIIMS, New Delhi), Deep Chand Bandhu, Hospital (DCBH), Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital (ABVIMS and Dr. RML), University College of Medical Sciences and Guru Teg Bahadur Hospital (UCMS and GTB), and Lady Hardinge Medical College and Kalawati Sharan Hospital (LHMC and KSH), for their inputs and support to this study. We thank all the study participants. We also take the opportunity to convey thanks to our colleagues Dr. Kavita Rajesh, Dr. Shikha Nargotra, Dr. Chandra Prabha, Dr. Abhimanyu Singh Chauhan, and Dr. Ahmed Shammas Yoosuf at GRID Council for their support at various phases of the study and manuscript preparation. We thank our funder India Country Office of the World Health Organization and its representatives for making the study possible.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1052340/full#supplementary-material
HCP, Healthcare Provider; HOD, Head of Department; IPC, Infection prevention and control; PPE, Personal Protective Equipment; RDM, Recently delivered mothers.
1. Nguyen B, Jin K, Ding D. Breastfeeding and maternal cardiovascular risk factors and outcomes: A systematic review. PLoS ONE. (2017) 12:e0187923. doi: 10.1371/journal.pone.0187923
2. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. (2012) 8:CD003517. doi: 10.1002/14651858.CD003517.pub2
3. Binns C, Lee M, Low WY. The long-term public health benefits of breastfeeding. Asia Pac J Public Health. (2016) 28:7–14. doi: 10.1177/1010539515624964
4. Schwarz EB, Brown JS, Creasman JM, Stuebe A, McClure CK, Van Den Eeden SK, et al. Lactation and maternal risk of type 2 diabetes: a population-based study. Am J Med. (2010) 123:863.e1–6. doi: 10.1016/j.amjmed.2010.03.016
5. Figueiredo B, Canário C, Field T. Breastfeeding is negatively affected by prenatal depression and reduces postpartum depression. Psychol Med. (2014) 44:927–36. doi: 10.1017/S0033291713001530
6. Pimentel J, Ansari U, Omer K, Gidado Y, Baba MC, Andersson N, et al. Factors associated with short birth interval in low- and middle-income countries: a systematic review. BMC Pregnancy Childbirth. (2020) 20:156. doi: 10.1186/s12884-020-2852-z
7. Moore ER, Bergman N, Anderson GC, Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. (2016) 11:CD003519. doi: 10.1002/14651858.CD003519.pub4
8. Zhang Y, Yang J, Li W, Wang N, Ye Y, Yan S, et al. Effects of baby-friendly practices on breastfeeding duration in China: a case-control study. Int Breastfeed J. (2020)15:92. doi: 10.1186/s13006-020-00334-4
9. World Health Organization. Food and Agriculture Organization of the United Nations. In: Strengthening Nutrition Action: A Resource Guide for Countries Based on the Policy Recommendations of the Second International Conference on Nutrition (ICN2). Geneva (2018). Available online at: https://apps.who.int/iris/handle/10665/274739 (accessed November 6, 2022).
10. World Health Organization. Pulse Survey on Continuity of Essential Health Services During the COVID-19 Pandemic: Interim Report. (2020). Available online at: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS_continuity-survey-2020.1 (accessed 10 February 10, 2021).
11. Chetterje P. Gaps in India's preparedness for COVID-19 control. Lancet Infect Dis. (2020) 20:544. doi: 10.1016/S1473-3099(20)30300-5
12. Garg S, Basu S, Rustagi R, Borle A. Primary health care facility preparedness for outpatient service provision during the COVID-19 pandemic in India: cross-sectional study. JMIR Public Health Surveill. (2020) 6:e19927. doi: 10.2196/19927
13. Prinja S, Pandav CS. Economics of COVID-19: challenges and the way forward for health policy during and after the pandemic. Indian J Public Health. (2020) 64:231. doi: 10.4103/ijph.IJPH_524_20
14. World Health Organization. Breastfeeding and COVID-19. (2020). Available online at: https://www.who.int/news-room/commentaries/detail/breastfeeding-and-covid-19 (accessed November 5, 2022).
15. World Health Organization. Frequently Asked Questions: Breastfeeding and COVID-19 For Health Care Workers. (2020). Available online at: https://www.who.int/docs/default-source/reproductive-health/maternal-health/faqs-breastfeeding-and-covid-19.pdf?sfvrsn=d839e6c0_5 (accessed March 18, 2021).
16. World Health Organization. Clinical Management of COVID-19: Interim Guidance. (2020). Available online at: https://apps.who.int/iris/handle/10665/332196 (accessed November 5, 2022).
17. Marín Gabriel MA, Reyne Vergeli M, Caserío Carbonero S, Sole L, Molina TC, Calle IR, et al. Maternal, perinatal and neonatal outcomes with COVID-19: a multicenter study of 242 pregnancies and their 248 infant newborns during their first month of life. Pediatr Infect Dis J. (2020) 39:e393. doi: 10.1097/INF.0000000000002902
18. Ashish KC, Gurung R, Kinney MV, Sunny AK, Moinuddin Md, Basnet O, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. (2020) 8:e1273–81. doi: 10.1016/S2214-109X(20)30345-4
19. Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr. (2021) 17:e13088. doi: 10.1111/mcn.13088
20. Vazquez-Vazquez A, Dib S, Rougeaux E, Wells JC, Fewtrell MS. The impact of the COVID-19 lockdown on the experiences and feeding practices of new mothers in the UK: preliminary data from the COVID-19 New Mum Study. Appetite. (2021) 156:104985. doi: 10.1016/j.appet.2020.104985
21. Rao SPN, Minckas N, Medvedev MM, Gathara D, Prashantha YN, Seifu A, et al. Small and sick newborn care during the COVID-19 pandemic: global survey and thematic analysis of healthcare providers' voices and experiences. BMJ Glob Health. (2021) 6:e004347. doi: 10.1136/bmjgh-2020-004347
22. UNICEF India. Newborn and Child Health. Available online at: https://www.unicef.org/india/what-we-do/newborn-and-child-health (accessed November 6, 2022).
23. Gupta A, Thakur N. Infant and young feeding practices in India: current status and progress towards SDG targets. Proc Indian Natl Sci Acad. (2018) 84:853–65. doi: 10.16943/ptinsa/2018/49440
24. Gupta A, Dadhich J, Faridi M. Breastfeeding and complementary feeding as a public health intervention for child survival in India. Indian J Pediatr. (2010) 77:413–8. doi: 10.1007/s12098-010-0049-6
25. Holla-Bhar R, Iellamo A, Gupta A, Smith JP, Dadhich JP. Investing in breastfeeding – the world breastfeeding costing initiative. Int Breastfeed J. (2015) 10:8. doi: 10.1186/s13006-015-0032-y
26. Ministry of Health and Family Welfare. Government of India. Advisory for Hospitals and Medical Institutions. (2020). Available online at: https://www.mohfw.gov.in/pdf/AdvisoryforHospitalsandMedicalInstitutions.pdf (accessed November 6, 2022).
27. Business Today. AIIMS Shuts Down OPD Services Due to Coronavirus Pandemic. (2020). Available online at: https://www.businesstoday.in/latest/trends/story/aiims-shuts-down-opd-services-due-to-coronavirus-pandemic-252783-2020-03-23 (accessed November 6, 2022).
28. Express Healthcare. How the Pandemic Has Led to a Steady Decline in Institutional Deliveries Access to Maternal Healthcare. (2020). Available online at: https://www.expresshealthcare.in/blogs/how-the-pandemic-has-led-to-a-steady-decline-in-institutional-deliveries-and-access-to-maternal-healthcare/422862/ (accessed November 6, 2022).
29. Chawla D, Chirla D, Dalwai S, Deorari AK, Ganatra A, Gandhi A, et al. Perinatal-neonatal management of COVID-19 infection - guidelines of the federation of obstetric and gynaecological societies of India (FOGSI), national neonatology forum of India (NNF), and Indian academy of pediatrics (IAP). Indian Pediatr. (2020) 57:536–48. doi: 10.1007/s13312-020-1852-4
30. Hindustan Times. COVID-19 Cases Surge: Top 10 Cities in India Worst Hit by the Pandemic. (2020). Available online at: https://www.hindustantimes.com/india-news/covid-19-cases-surge-top-10-cities-in-india-worst-hit-by-the-pandemic/story-LKwTBNm1skXADUzapHQLLJ.html (accessed February 11, 2021).
31. Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. (2017) 27:591–608. doi: 10.1177/1049732316665344
32. Redlich-Amirav D, Higginbottom G. New emerging technologies in qualitative research. Qual Rep. (2014) 19:26. doi: 10.46743/2160-3715/2014.1212
33. Parameswaran UD, Ozawa-Kirk JL, Latendresse G. To live (code) or to not: a new method for coding in qualitative research. Qual Soc Work. (2020) 19:630–44. doi: 10.1177/1473325019840394
34. Markle DT, West RE, Rich PJ. Beyond transcription: technology, change, and refinement of method. Forum Qual Soc Res. (2011) 12:3. doi: 10.17169/fqs-12.3.1564
35. Qualitative Data Analysis Software | NVivo. Available online at: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed March 18, 2021).
36. Glaser BG, Strauss AL, Strutzel E. The discovery of grounded theory; strategies for qualitative research. Nurs Res. (1968) 17:364. doi: 10.1097/00006199-196807000-00014
37. Saxena M, Srivastava A, Dwivedi P, Bhattacharyya S. Is quality of care during childbirth consistent from admission to discharge? A qualitative study of delivery care in Uttar Pradesh, India. PLoS ONE. (2018) 13:e0204607. doi: 10.1371/journal.pone.0204607
38. Federation of Obstetric and Gynecological Societies of India, National Neonatology Forum, India, Indian Academy of Pediatrics. Clinical Practice Guideline. Perinatal Neonatal management of COVID 19 infection Ver.1.0. (2020). Available online at: https://perinatalcovid19.files.wordpress.com/2020/03/fogsi-nnf-iap-covid19-perinatal-neonatal-guideline-ver-1.0-march-26-2020.pdf.pdf?fbclid=IwAR1vtAWoR0Ap7PczFvStZhzRtRWIaWfElSKstkSpfemjfgmNTEUqdGvF2AY (accessed March 8, 2021).
39. Federation of Obstetric and Gynecological Societies of India, National Neonatology Forum, India, Indian Academy of Pediatrics. Clinical Practice Guideline. Perinatal Neonatal Management of COVID 19 Ver.2.0. (2020). Available online at: https://iapindia.org/pdf/1465-Summary-FOGSI-NNF-IAP-Perinatal-Covid19-ver-2-0-May-11.pdf (accessed March 8, 2021).
40. Ceulemans M, Verbakel JY, Van Calsteren K, Eerdekens A, Allegaert K, Foulon V. SARS-CoV-2 infections and impact of the COVID-19 pandemic in pregnancy and breastfeeding: results from an observational study in primary care in Belgium. Int J Environ Res Public Health. (2020) 17:6766. doi: 10.3390/ijerph17186766
41. Tomori C, Gribble K, Palmquist AEL, Ververs MT, Gross MS. When separation is not the answer: breastfeeding mothers and infants affected by COVID-19. Matern Child Nutr. (2020) 16:e13033. doi: 10.1111/mcn.13033
42. Del Río R, Pérez ED, Gabriel MÁM. Multi-centre study showed reduced compliance with the World Health Organization recommendations on exclusive breastfeeding during COVID-19. Acta Paediatr. (2020) 110:3. doi: 10.1111/apa.15642
43. Popofsky S, Noor A, Leavens-Maurer J, Quintos-Alagheband ML, Mock A, Vinci A, et al. Impact of maternal severe acute respiratory syndrome Coronavirus 2 detection on breastfeeding due to infant separation at birth. J Pediatr. (2020) 226:64–70. doi: 10.1016/j.jpeds.2020.08.004
44. Ashokka B, Loh M-H, Tan CH, Su LL, Young BE, Lye DC, et al. Care of the pregnant woman with coronavirus disease 2019 in labor and delivery: anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am J Obstet Gynecol. (2020) 223:66–74.e3. doi: 10.1016/j.ajog.2020.04.005
45. Singh MV, Shrivastava A, Maurya M, Tripathi A, Sachan R, Monica, et al. Vertical transmission of SARS-CoV-2 from an asymptomatic pregnant woman in India. J Trop Pediatr. (2020) 25:fmaa048. doi: 10.1093/tropej/fmaa048
46. Turner S, McGann B, Brockway M. 'Merilee' a review of the disruption of breastfeeding supports in response to the COVID-19 pandemic in five Western countries and applications for clinical practice. Int Breastfeed J. (2022) 17:38. doi: 10.1186/s13006-022-00478-5
47. World Health Organization. Clinical Management of Severe Acute Respiratory Infection When Novel Coronavirus (2019-nCoV) Infection is Suspected: Interim Guidance. (2020). Available online at: https://apps.who.int/iris/handle/10665/330893 (accessed November 5, 2022).
48. Spatz DL, Froh EB. Birth and breastfeeding in the hospital setting during the COVID-19 Pandemic. Am J Matern Child Nurs. (2021) 46:30–5. doi: 10.1097/NMC.0000000000000672
49. Furman L, Noble L. Bench research, human milk, and SARS-CoV-2. Pediatrics. (2021) 147:e2020033852. doi: 10.1542/peds.2020-033852
50. Bandyopadhyay T, Sharma A, Kumari P, Maria A, Choudhary R. Possible early vertical transmission of COVID-19 from an infected pregnant female to her neonate: a case report. J Trop Pediatr. (2021) 67:1. doi: 10.1093/tropej/fmaa094
51. Neef V, Buxmann H, Rabenau HF, Zacharowski K, Raimann FJ. Characterization of neonates born to mothers with SARS-CoV-2 infection: review and meta-analysis. Pediatr Neonatol. (2021) 62:11–20. doi: 10.1016/j.pedneo.2020.10.001
52. Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet Lond Engl. (2020) 395:809–15. doi: 10.1016/S0140-6736(20)30360-3
53. Krupa A, Schmidt M, Zborowska K, Jorg D, Czajkowsha M, Skrzypulec-Plinta V. Impact of COVID-19 on pregnancy and delivery - current knowledge. Ginekol Pol. (2020) 91:564–8. doi: 10.5603/GP.a2020.0127
54. Lubbe W, Botha E, Niela-Vilen H, Reimers P. Breastfeeding during the COVID-19 pandemic – a literature review for clinical practice. Int Breastfeed J. (2020) 15:82. doi: 10.1186/s13006-020-00319-3
55. Goh XL, Low YF, Ng CH, Amin Z, Ng YPM. Incidence of SARS-CoV-2 vertical transmission: a meta-analysis. Arch Dis Child Fetal Neonatal Ed. (2021) 106:112–3. doi: 10.1136/archdischild-2020-319791
56. Wyckoff AS. AAP Issues Guidance on Infants Born to Mothers with Suspected or Confirmed COVID-19. (2020). Available online at: https://publications.aap.org/aapnews/news/6713/AAP-issues-guidance-on-infants-born-to-mothers (accessed November 5, 2022).
57. Downey K. AAP No Longer Recommends Separating Newborns From Mothers With COVID-19. (2020). Available online at: https://www.healio.com/news/pediatrics/20200728/aap-no-longer-recommends-separating-newborns-from-mothers-with-covid19 (accessed November 5, 2022).
58. Rhoads SJ, Green A, Gauss CH, Mitchell A, Pate B. Web camera use of mothers and fathers when viewing their hospitalized neonate. Adv Neonatal Care. (2015) 15:440–6. doi: 10.1097/ANC.0000000000000235
59. Escobedo MB, Shah BA, Song C, Mitchell A, Pate B. Recent recommendations and emerging science in neonatal resuscitation. Pediatr Clin North Am. (2019) 66:309–20. doi: 10.1016/j.pcl.2018.12.002
60. Minton S, Allan M, Valdes W. Teleneonatology: a major tool for the future. Pediatr Ann. (2014) 43:e50–55. doi: 10.3928/00904481-20140127-11
61. Huckabay LM. Impact of a research study a decade later: the use of pictures in a neonatal intensive care unit as a mode of nursing intervention to enhance maternal-infant bonding. Sch Inq Nurs Pract. (1999)13:367–73.
62. Dutta U, Sachan A, Premkumar M, Gupta T, Sahoo S, Grover S, et al. Multidimensional dynamic healthcare personnel (HCP)-centric model from a low-income and middle-income country to support and protect COVID-19 warriors: a large prospective cohort study. BMJ Open. (2021) 11:e043837. doi: 10.1136/bmjopen-2020-043837
63. Crain MA, Bush AL, Hayanga H, Boyle A, Unger M, Ellison M, et al. Healthcare leadership in the COVID-19 pandemic: from innovative preparation to evolutionary transformation. J Healthc Leadersh. (2021) 13:199–207. doi: 10.2147/JHL.S319829
64. Allameh SF, Khajavirad N, Labaf A, Mirzazadeh A, Sadeghniiat-Haghighi K, Mortazavi SJ, et al. Twelve lessons on hospital leadership during COVID-19 pandemic. Arch Bone Jt Surg. (2020) 8:277–80. doi: 10.22038/abjs.2020.47829.2363
Keywords: breastfeeding, newborn care, India, COVID-19, hospital, isolation, baby friendly hospital initiative, family centered care
Citation: Maria A, Mukherjee R, Upadhyay S, Pratima K, Bandyopadhyay T, Gupta R, Dubey B, Sharma A, Mall PK, Sahoo M, Pathak KK, Pawar P and Mohapatra A (2022) Barriers and enablers of breastfeeding in mother–newborn dyads in institutional settings during the COVID-19 pandemic: A qualitative study across seven government hospitals of Delhi, India. Front. Nutr. 9:1052340. doi: 10.3389/fnut.2022.1052340
Received: 23 September 2022; Accepted: 10 November 2022;
Published: 08 December 2022.
Edited by:
Nita Bhandari, Center for Health Research and Development, Society for Applied Studies, IndiaReviewed by:
Jeanette Mary Andrade, University of Florida, United StatesCopyright © 2022 Maria, Mukherjee, Upadhyay, Pratima, Bandyopadhyay, Gupta, Dubey, Sharma, Mall, Sahoo, Pathak, Pawar and Mohapatra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arti Maria, YXJ0aW1hcmlhQGdtYWlsLmNvbQ==; Archisman Mohapatra, YXJjaGlzbWFuLm1AdGhlZ3JpZGNvdW5jaWwub3Jn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.