
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Nutr., 03 November 2022
Sec. Nutrition and Food Science Technology
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1047827
This article is part of the Research TopicCurrent Trends in Food Processing and Nutrition to Mitigate Nutritional Health IssuesView all 11 articles
 Muhammad Faisal Manzoor1,2†
Muhammad Faisal Manzoor1,2† Tayyaba Tariq3†
Tayyaba Tariq3† Birjees Fatima3
Birjees Fatima3 Amna Sahar4
Amna Sahar4 Farwa Tariq3
Farwa Tariq3 Seemal Munir3
Seemal Munir3 Sipper Khan5
Sipper Khan5 Muhammad Modassar Ali Nawaz Ranjha6
Muhammad Modassar Ali Nawaz Ranjha6 Aysha Sameen7*
Aysha Sameen7* Xin-An Zeng1,2*
Xin-An Zeng1,2* Salam A. Ibrahim8*
Salam A. Ibrahim8*Bisphenol A (BPA) is a synthetic chemical widely employed to synthesize epoxy resins, polymer materials, and polycarbonate plastics. BPA is abundant in the environment, i.e., in food containers, water bottles, thermal papers, toys, medical devices, etc., and is incorporated into soil/water through leaching. Being a potent endocrine disrupter, and has the potential to alter several body mechanisms. Studies confirmed its anti-androgen action and estrogen-like effects, which impart many negative health impacts, especially on the immune system, neuroendocrine process, and reproductive mechanism. Moreover, it can also induce mutagenesis and carcinogenesis, as per recent scientific research. This review focuses on BPA’s presence and concentrations in different environments, food sources and the basic mechanisms of BPA-induced toxicity and health disruptions. It is a unique review of its type because it focuses on the association of cancer, hormonal disruption, immunosuppression, and infertility with BPA. These issues are widespread today, and BPA significantly contributes to their incidence because of its wide usage in daily life utensils and other accessories. The review also discusses researched-based measures to cope with the toxic chemical.
Xenoestrogens or endocrine disruptors are natural or synthetic compounds harmful to the endocrine system because they stop endogenous hormone production and normal functioning (1). Due to rapid advancement in human lifestyle, endocrine-disrupting chemicals are being introduced competently into the environment extensively, and living beings are directly or indirectly exposed to harmful chemicals such as Bisphenol A (BPA) (2–4).
Bisphenol A is among toxic chemicals, first highlighted by Aleksandr Dianin in 1891, then in 1905, they were made by Zincke using acetone condensation with two correspondents of phenol. In the mid-twentieth century (1940), a sudden rise in polymers (polycarbonates, polysulfone, polyacrylate, and epoxy resins) was observed with BPA. The polymers were also used as an antioxidant and endpoint for inhibiting polymerization in polyvinyl chloride plastics. Besides, flame retardant polymers, including tetrabromobisphenol-A were also prepared using the polymers (5). It makes different polymers, such as epoxy resins, polycarbonates, and other polymer materials (6, 7). Epoxy resins and polycarbonates were in high demand in 2015, 64 and 34%, respectively. Demand increases are expected with each passing year (8).
Additionally, in recent years, their uses have expanded to produce optical and electronic materials. Polymers also produce plastic food containers, drinking glasses, bowls, cups, and microwave-safe utensils (9, 10). Canned materials can be a significant source for food adulteration owing to direct contact since epoxy resins are utilized to protect the can from the inside (11, 12). They are used in other industries like the ink and paint industry, manufacturing of thermal papers, compact discs, electronics etc. (12, 13).
Since then, BPA has been abundantly used in food packaging materials, take-away water bottles, and lacquer coatings for tin cans causing human exposure to BPA via food and drinks (2–4). Furthermore, occupational workers get BPA exposure through direct contact with skin or inhalation, whereas the standard population is exposed to BPA by dust inhalation (14, 15). BPA has been linked to several serious health issues in animal model research. Numerous human-based epidemiological and observational studies on BPA exposure revealed similar results. BPA exposure is associated with the incidence of growth disruption, halting normal development, infertility, endocrine system disruption, immune system suppression, and carcinogenicity (16, 17).
By keeping in view the scenario mentioned above of BPA production and its utilization in different domains of life, the present review is aimed to elaborate on the different human BPA exposure routes and adverse health effects of toxicity with a special focus on basic mechanisms of endocrine disruption, infertility, carcinogenesis, and immunosuppression.
The estimated global volume of BPA utilization was 7.69 million metric tons in 2015 for different applications that were forecasted to increase to 7.7 million in 2016. Approximately 4.8% compound annual growth rate (CAGR) is observed from 2016 to 2022. The production is predicted to increase to 10.7 million metric tons in 2020 because of the broad applications of polycarbonate plastics and epoxy resins in every field. The global demand for BPA is estimated to reach USD 22.49 billion in 2022. It was recorded to be approximately USD 15.6 billion in 2015, with a forecast of 16.4 as of 2016, marking a faster CAGR of 5.4% in value. The largest market of BPA is located in the Asia Pacific, contributing to approximately 52% of the market share, while 36% is produced by the USA and Western Europe (18, 19). Due to these applications, its extensive scale application is observed in everyday life, such as in producing papers, toys, water pipes, electronic products, and other plastic materials (20, 21).
The molecular weight of BPA [4, 4-isopropylidenediphenol; 2, 2-bis (4-hydroxyphenyl)-propane] is 228.29 g/cm3, with a white crystal-like appearance and highly reactive due to the presence of hydroxyl group in the structure. The melting and boiling points of the toxic chemical are 156 and 220°C (at 5 hPa), respectively. The coefficient of BPA in water octanol is expressed in a logarithmic form value of 3.32 (log P = 3.32), indicating its high solubility in fats and less soluble in water (about 200 mg/dm3 at 25°C). Moreover, it can also be transformed into the ether, esters, and salts like other phenols. Additionally, the electrophilic substitution of BPA generally includes sulphonation, alkylation, and nitration (20, 22).
Bisphenol A is a well-known synthetic chemical globally used to manufacture different polymers, including epoxy resins, polycarbonates, and other polymer materials. Polycarbonates and epoxy resins are prominent polymers in significant bisphenol applications. Some other uses of bisphenol A include the production of different resins (unsaturated polyester, polysulfone, polyetherimide, and polyacrylate) (6, 7). In 2015, global demand for polycarbonates and epoxy resins was 64 and 34%, respectively. Moreover, the rise in demand for these two polymers will be observed with an average annual rate of 3 and 4% for the next 5 years (8). Furthermore, in recent years, their applications extended to manufacturing optical and electronic materials. Plastic cups, bottles, bowls, food containers, and utensils used for microwaves are also synthesized with polymers (9, 10).
Epoxy resins protect the can from the inside; therefore, they can be a considerable source for the adulteration of food items due to direct contact (11, 12). The storage bottles are also layered with epoxy resins for a similar purpose (23). Nonetheless, epoxy resins are also successfully applied in the paint and ink industry. Beyond this, epoxy resins also have a well-established reputation in manufacturing thermal paper, compact discs (CD), and digital video discs (12, 13). Whereas the derivate compounds from BPA are used in tickets and newspapers for antioxidants and stabilizers (15, 24) and, in the textiles industry, it is employed for infant socks preparation (25).
Bisphenol A is present almost everywhere in our surroundings and significantly affects our life. It can be part of the food and environment directly or indirectly, affecting living organisms.
Bisphenol A is an ‘omnipresent’ contaminant due to its presence in all possible resources that might be the source of its human exposure through air, water, and soil (26). There are three main routes for human exposure environmental, occupational, and contaminated food consumption (27). Workers synthesizing BPA and their related derivative compounds (i.e., polycarbonate, epoxy resins, and polyvinyl chloride) are easy targets for occupational exposure. The main reason for the environmental exposure is the contamination of the atmosphere, soil, and aquatic systems owing to the BPA entering the environment due to its use in thermal paper recycling and relevant industries (27, 28).
According to the findings of Zhang et al. (29), who assessed the BPA concentration in water of different areas of China, 19 out of 20 water treatment plants had 5–14 ng/L of BPA. A similar situation was reported in Canada, France and South Germany. The main reason behind the increased incidence of BPA is the increased occurrence of epoxy resins and polycarbonate plastics. According to the Global Bisphenol A (BPA) Market Report and Forecast 2021–2026 report, the worldwide BPA market was $10.92 billion in 2020. The expected Compound Annual Growth Rate (CAGR) is 7.8% between 2021 and 2026 (30). Manufacturing of BPA products, their utilization, aging, and disposal in the environment are the major reasons behind the addition of BPA in ecosystems (31). Point sources include effluents from sewage treatment facilities and landfill leachate, whereas non-point sources include epoxy resin and polycarbonate plastic shards that infiltrate aquatic bodies (32).
According to various studies, approximately 56 μg/L of BPA can be ingested from the aquatic environment, 1–150 μg/kg from soil (33, 34), while 2–208 ng/m3 of BPA can be inhaled from the surroundings and dust contributes 0.2–17.6 μg/g contamination (35). In addition, contaminated seafood ingestion, metallic food cans, and plastic bottles can contribute 13.3–213 μg/kg, 2–82 ng/g, and 0.234 μg/L, respectively (36), whereas landfill leachates (17.2 mg/L) (37), dermal route (7.1–71 μg/day) (38), and dental material (0.013–30 mg/day) also contaminate the environment (39).
Food exposure is the most important because fulfilling daily dietary needs is essential for survival (Table 1). Contamination of BPA through food exposure occurs due to the use of BPA for manufacturing different types of plastic containers [polycarbonate (PC) and polyvinylchloride (PVC) plastics] used for food serving and exposing their direct interaction with food. Epoxy resins are also used to manufacture food cans for inner coatings. Therefore, canned food products also play a significant role in adulterating food items. Residual monomers of these compounds migrate from the can to the food product, and food consumption causes safety issues in individuals (11, 12). Besides, food packaging materials are the primary cause of BPA accumulation in human beings. It is due to the penetration of BPA from packaging into foodstuff and beverages (40, 41). There are also secondary reasons which lead to exposure to BPA and hence the infected human population (25, 42, 43).
The migration of particles from the wrapping material to the food material is quite a complex phenomenon. It depends on different factors, including the composition of different food items, duration of contact time, the food temperature during contact, and packaging material type refs. Studies revealed that fat in foods also contributes to the migration of particles. Similarly, there is also a direct relationship between the square root of contact time and the concentration of molecules being migrated. Moreover, the high-temperature also leads to a rapid migration rate of residues (11, 12). BPA penetration into packaged products accelerates at higher temperatures (used for boiling water) than the lower temperature, around 20°C. It is also illustrated that the migration rate could be 55 folds more than the latter temperature (44). Food present in packaged products shows less absorption of BPA than the food preserved in canned materials with a standard concentration of 0.45 ng per 100 g (45).
Moreover, compounds like epoxy resins and PVC are used in manufacturing industries to protect the inner side of the can from corrosion and rust development due to direct contact with different food items (23). Bottles used for storage purposes also have such types of protective glaze. Monomers residues of BPA migrate into the food during high-temperature processing and storage in these bottles due to incomplete polymerization (23, 46).
Babies fed on mother milk or non-PC bottles had minimum BPA levels compared to babies using PC-free packaging. BPA levels were low compared to infants’ body mass using non-PC feeders and eating solid foods (6–36 months) (47). The research was conducted in two steps to check BPA levels in fresh, frozen, and canned foodstuff (using 204 samples). Firstly, they checked the BPA concentrations in canned products and then calculated BPA intake through diet. Results showed that the foods not packed in canned material had lower BPA levels (7%) than canned foods (73%), while dietary assessment of adults revealed canned coatings materials as the main BPA contributor. Altogether 12.6 ng/kg was calculated per day in the human body, out of which 12.4 ng/kg was penetrated from canned foods. Moreover, 3–12.95 ng/kg per day was the tendency of dietary consumption. In contrast, 30–70 ng/kg/day was determined in the urinary bladder, higher than the central capacity of dietary intake (48).
Bisphenol A is almost everywhere in our environment and is released from common consumer goods (Figure 1). It may enter our body through different routes like dermal and oral exposure or only through inhalation (49). The primary route of exposure is dietary exposure, including consumption of seafood or even freshwater fish polluted via BPA, fresh food commodities from polluted regions, ingestion of food packed in plastic and cans containers, and drinking polluted water (50). The second foremost route of absorption for BPA is dermal exposure (51). Direct paper contact (especially thermal paper), toys, and medical devices proportionally increase the BPA potential against the skin. Inhalation is the third most important route of exposure through BPA-containing vapors, mists, dust, and gases (50).
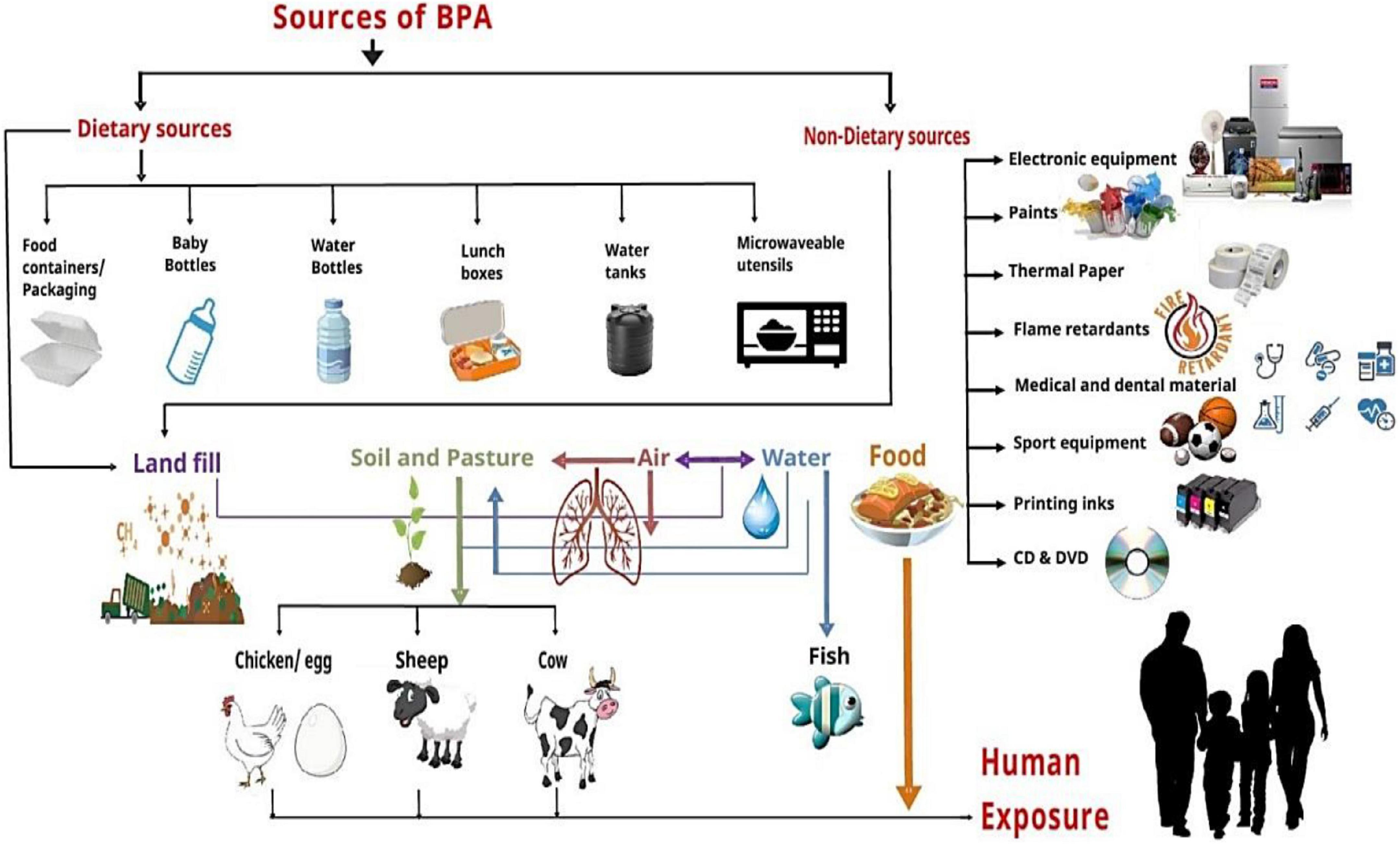
Figure 1. Humans exposure to BPA via different sources and exposed roots. Dietary sources (food containers/packaging, baby bottles, water bottles, lunch boxes, water tanks, and microwave utensils) and non-dietary sources (electronic equipment, paints, thermal paper, flame retardants, medical and dental materials, sports equipment, printing inks, and DVDs) contaminate landfill, soil, air, water, and food that directly or indirectly affect the human through different exposure routes.
Bisphenol A -human exposure’s primary source is canned food items. Therefore, this compound’s exposure mainly depends on the duration and amount of canned food usage in a person’s diet regimen. In kids older than 3 years, BPA exposure’s highest mean value was approximately 69.9 ng/kg body weight/day, with an utmost value of 189 ng/kg body weight/day. In adults, 139.9 ng/kg body weight/day was the highest mean value, with the maximum contact up to 419 ng/kg body weight/day (47). Wilson and colleagues estimated in a study that the exposure through inhalation for toddlers (1.5–5 years) was 0.23–0.42 ng/kg of body weight per day (52).
Generally, infants (0–6 months old) are the most affected through the alimentary canal all over the population with BPA exposure and its disruptions. The main reason for this exposure is the daily feeding of canned milk formulas in plastic feeder bottles containing PC. Hence, these plastic feeding bottles and canned milk powders make them most vulnerable to BPA’s side effects. Various research studies have been conducted to asses BPA levels and found that the BPA concentration is less than tolerable daily intake (TDI) (47).
Although, BPA exposure through inhalation and dermal routes accounts for less than 5% of all contact sources. The occupational population shares a more significant proportion (50). In a study, 154 composite samples were assessed for BPA analysis and 55 samples with BPA levels ranging from 0.19 to105.0 ng/g, respectively. The experimental results also indicated that canned foods had higher BPA concentrations than other food samples (23).
Bisphenol A is highly metabolized and secreted into urine, primarily as a glucuronide conjugate with a half-life of 2 h (53). BPA’s half-life also depends on the glucuronidase enzyme, which activates BPA through deconjugation in the bloodstream, and other organs (54). Furthermore, the valid biomarker of BPA exposure is total BPA (including free or conjugated) urinary concentration (55). The health aspect of free BPA (a weak estrogen) has been primarily observed in animal models. At the same time, limited neonatal human researches are available to check behavioral and executive functional effects, especially during critical child developmental stages and in the shortening of congenital space in male offspring (56, 57). However, several experiments revealed that BPA initially affects hepatic injury (53, 58). After ingestion, most BPA in the liver and gut is rapidly bound with glucuronic acid to release BPA glucuronide (BPA-G) by the glucuronidation process, facilitated by many enzymes (59).
Moreover, being fat-soluble, BPA has high adipose tissue affinity and is then released steadily to other histological structures in humans and mice (60, 61). An investigation to estimate the BPA division in humans highlighted that BPA is demonstrable in almost all human histological structures. In adipose tissues, it ranged from 1.13 to 12.27 ng/g, 0.78 to 3.34 ng/g in the liver, and 1 to 2.35 ng/g in the brain. In breast milk, total BPA was observed as 1.09 ng/mL, out of which 0.41 ng/mL content was identified as unconjugated BPA (6).
Furthermore, the conjugated BPA does not combine with the estrogen receptor (ER); therefore, they are biologically inactive and inert. However, another investigation revealed that BPA-conjugated forms could disturb cellular responsive action throughout membrane ERα contacts, which is responsible for quick signaling feedback (62). In contrast, in trace concentrations, unconjugated BPA (free BPA) can convert into other compounds such as BPA sulfate or BPA-S.
Bio-monitoring records reveal that BPA interaction with humans is prevalent (55, 63). However, there is still massive controversy on the legality of the reported measure of unconjugated BPA in whole blood, plasma, or serum. The discussion point is that adult human blood samples have up to 0.5–2 ng/mL (2.2–8.8 nM) unconjugated BPA. It is very high than the predicted levels of 0.51 μg/kg of body weight per day calculated based on adults’ estimated daily intake (48). Presumably, few of the even most substantial daily consumption records in this range (and lower) depend on the whole day urinary output, with back calculations of 596 German women and men (64).
According to the research conducted by Volkel et al., subjects were given a dose of 54–90 μg/kg of BW/day orally. The results showed that unconjugated BPA was not recognized in urine or serum in any human oral pharmacokinetic (PK) study. Though, the maximum value of finding in the study, 2.27 ng/ml (9.9 nM), is not as much susceptible as more current competencies of 0.05–0.3 ng/ml (0.25–1.76 nM) (65–67).
Another study, utilizing a LOD range of 0.01–0.95 ng/mL, was conducted in which 10 men were given a soup having an unconjugated d6-BPA of 0.097 ng/ml (0.42 nM) at 1.5 h, followed by administration of 29.9 μg/kg of body weight of BPA (68). The d6-BPA was 0.29% of the total BPA, leading researchers to conclude that the sublingual dietary exposure and absorption were reportedly different. Studies regarding the BPA’s pharmacokinetics in rats, mice, and rhesus monkeys using isotope compounds showed that oral consumption of 75 to over 1,000 μg/kg of body weight per day is essential concentrations of unconjugated BPA reported in humans (66, 69–71).
Overall, these changes led to the estimation that unconjugated BPA in the blood is linked with the preparation of the sample, storage, systematic procedure, and exposure conditions. For example, in hospitals where patients may be interacted with BPA from medical equipment or in professional settings (63, 72–78).
In animal model studies, BPA has reportedly caused many critical health conditions. Several human-based epidemiological and observational researches showed similar findings on exposure to BPA (47). Disrupted growth susceptibility is higher at certain phases of the life cycle on BPA exposure, halting normal development. Fetal or postnatal development stages are more critical as the body systems are not fully developed. BPA affected growth disruption due to its metabolism and elimination through enzyme systems amalgamation (16, 17). Because of the previous studies, this review will cover the effect of BPA on the human reproductive system, endocrine system, immune system, and carcinogenicity.
The endocrine system is one of the most synchronized and complex systems. BPA is an adverse endocrine-disrupting chemical (EDC) which suppresses or alters hormonal and enzyme synthesis, secretion, release, and transportation. BPA hinders the system’s activity by replacing endogenous hormones with transporter proteins (Figure 2). This alteration changes the free and bound hormonal concentrations present in plasma. This chemical also influences the neuroendocrine function, causing a physiological interruption in the organs. Studies have shown the increased serum level of estradiol in females and reduced testosterone in males due to BPA (79, 80).
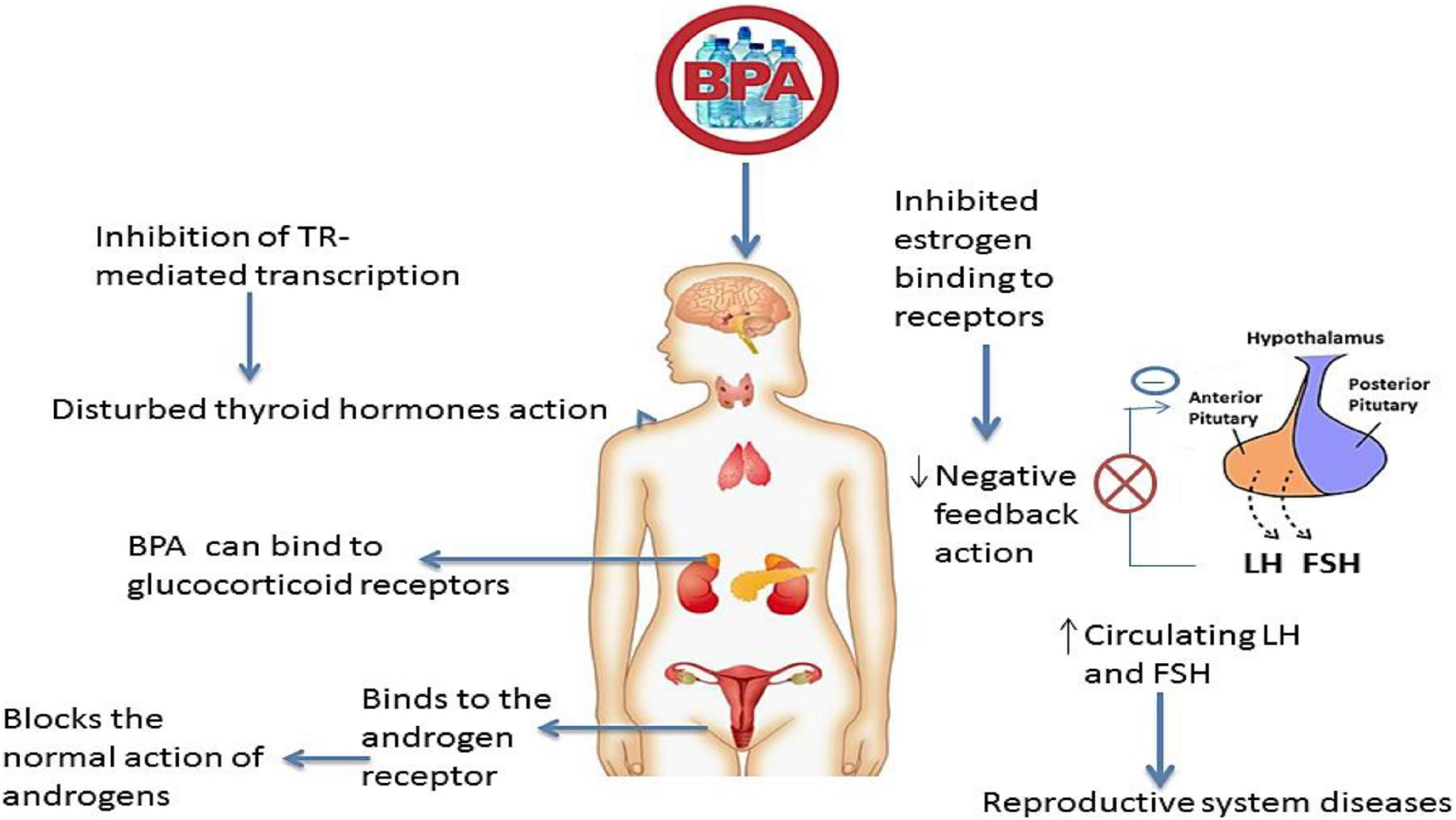
Figure 2. Bisphenol A as an endocrine disruptor. Estrogens negatively affect the release of follicle-stimulating hormone (FSH) and luteinizing hormones (LH). BPA can inhibit the estrogen binding to its receptors at the pituitary level, resulting in high levels of FSH and LH hormones in circulation. This can lead to reproductive system issues such as polycystic ovarian syndrome. BPA acts as anti-androgen by binding with androgen and glucocorticoid receptors and affecting their action. BPA can disturb the action of the thyroid hormone by inhibiting TR-mediated transcription of T3-response genes.
Mental health is highly influenced by the disrupter, which causes sex-specific mental impairment and behavioral changes. Disturbed and depressive tendencies rose because “Dehydroepiandrosterone (DHEA),” a neuroactive steroid in males, is decreased, resulting in a possible pathway of the depressive-like phenotype (81). Previous studies regarding the endocrine disruption of BPA are compiled to assess its potent role (Table 2).
Evidential studies have indicated that the reproductive system’s higher interruption susceptibility is observed due to this BPA (Table 3). Being an easy target, the reproductive system undergoes disturbing sex hormone activity and exertion. BPA also distracts the function and primary development of the reproductive system (Figure 3). Recent studies reported the BPA linkage with increased levels of serum luteinizing hormone (LH), estradiol (E2), progesterone, and testosterone (T) while decreased concentrations of serum cortisol (80). A significant association between BPA and higher total testosterone (TT) concentration in serum was also reported (82).
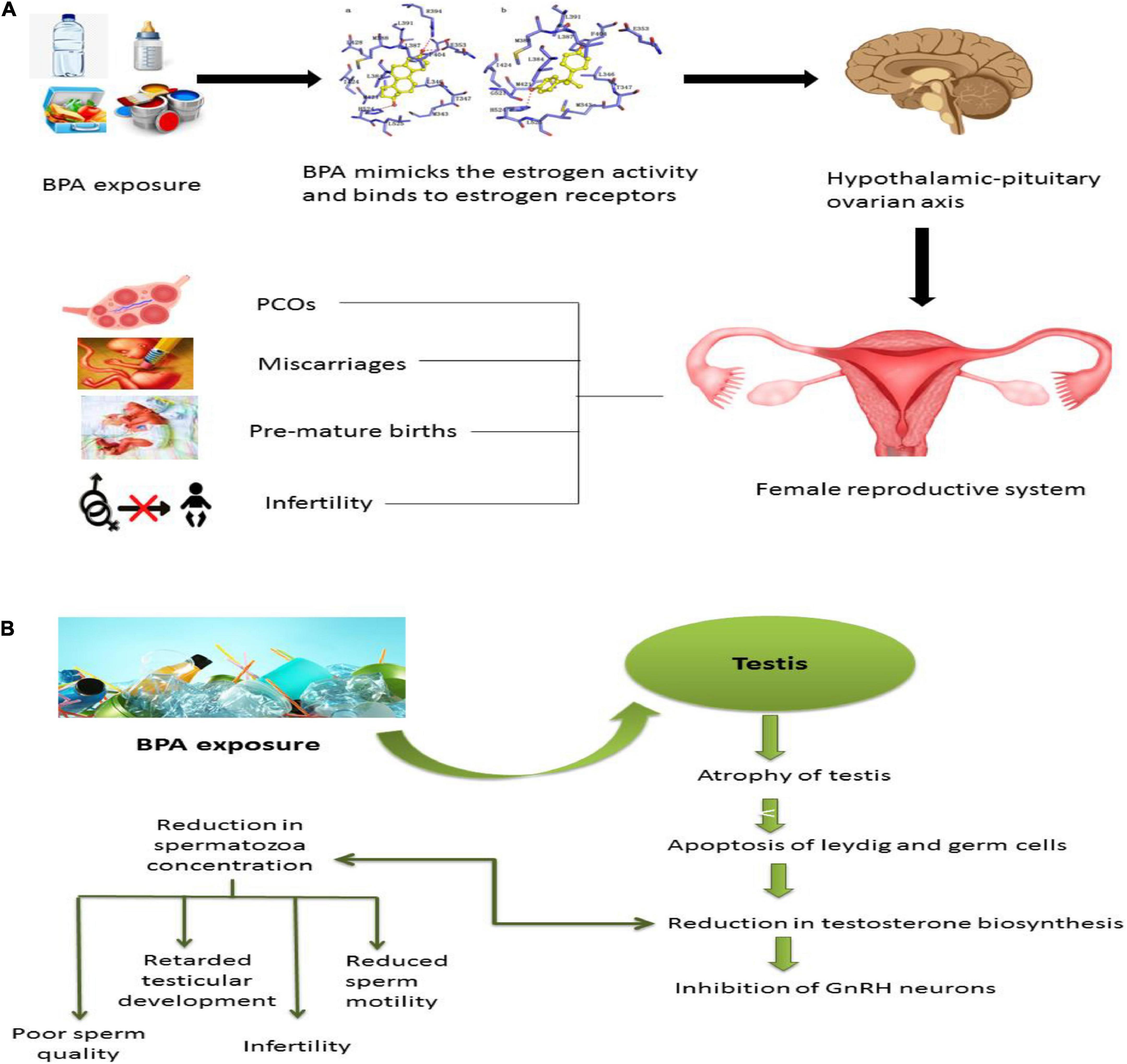
Figure 3. Effect of BPA on the reproductive system. (A) When exposed to BPA, females can develop fertility-related issues as it is very similar to estrogen structure and function. It binds to estrogen receptors and causes irreversible alteration to the hypothalamic-pituitary-ovarian axis. BPA will provoke estrogen and thus increase the chances of PCOs, delay puberty, miscarriages, endometriosis, premature births, and most of the time, BPA can cause infertility. (B) Exposure of males to bisphenol interferes with the reproductive system. BPA causes atrophy in the testis, apoptosis in Leydig cells and germ cells, and reduction in testosterone biosynthesis, which will either cause the reduction in spermatozoa reduction or inhibition of GnRH neurons. It causes sperm quality and quantity alterations, retardation of testicular development, infertility, and reduction in sperm motility.
The endometrial wall thickness and cycle of sex hormones associations are well studied. Scientists observed an age-based relationship between altered endometrial wall thickness and BPA levels (83). Moreover, polycystic ovary syndrome (PCOS) patients exhibited higher BPA serum concentrations than healthy women and patients (84, 85). The researchers also detected BPA’s potential role in PCOS and adverse pregnancy outcomes like premature delivery and miscarriage (86).
Males facing prolonged BPA exposure tend to have low sperm quality, sexual dysfunction, and impaired fertility. The amplitude of lateral head displacement (ALH), Wobble (WOB), Linearity (LIN), Mean Angular Displacement (MAD), sperm concentration, and association with BPA illustrated the fluctuated characteristics and velocity rate reduction. This array results in impaired reproductive function in males (87).
The incidence of numerous cancer types is rising exceptionally and appears to be linked with BPA (Table 4). It includes breast (88), ovarian, uterus, prostate (89–91), and testicular cancer (92). The findings of the various in vivo studies on animals (i.e., mice, rats, etc.) concluded that the raised estrogenic activity depicts the carcinogenic mechanistic action of BPA (93). BPA’s activation of tumorigenesis and cancerous cell development are still under experimentation (88). BPA stimulates cellular responses through binding to ER, although they reflect a weak affinity to each other (Figure 4).
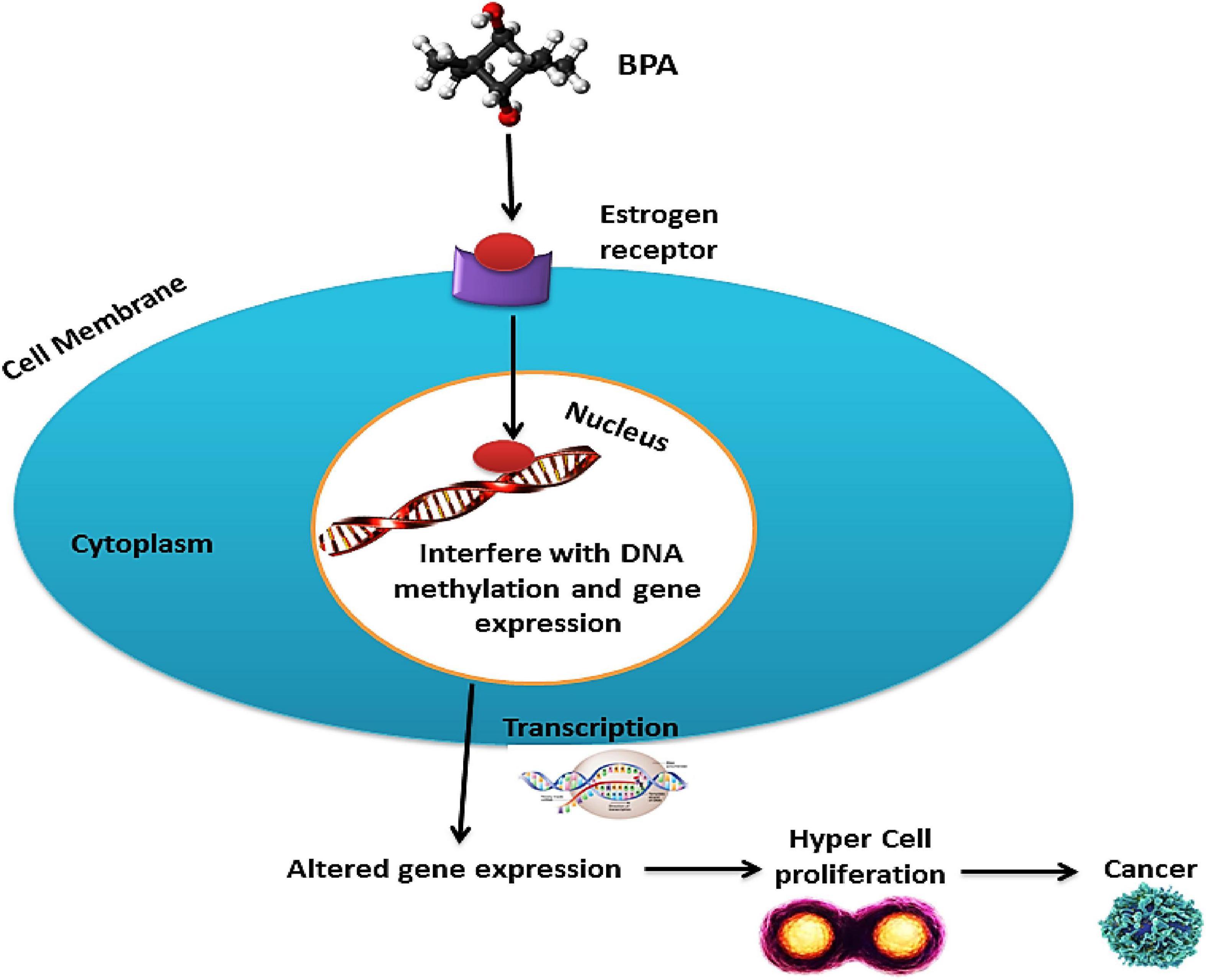
Figure 4. Carcinogenic activity of BPA; BPA interacts with the estrogen receptors and interferes with DNA methylation and gene expression after entering the nucleus. Thus altered gene expression leads to hypercell proliferation, which may lead to cancer.
The binding ability of the receptor to hold co-repressors is lost. As the regulation of co-regulators by the BPA–ER complex is disproportionate to the affinity of BPA to ER, the type and expression levels of ER-regulated targets are determinants for the tissue and cellular specificity of the BPA response. BPA can induce genomic responses at concentrations lower than the levels at which it is expected to bind to nuclear ERs (94).
Studies have revealed that oxidative stress, immune function, and inflammation are directly related to BPA exposure. The correlation between BPA and the induction of mitochondrial damage and cellular apoptosis resulted in systematic degradation (95–97), causing an alternation in immune cell populations and functioning of the innate and adaptive immune system owing to developmental BPA exposure (Figure 5).
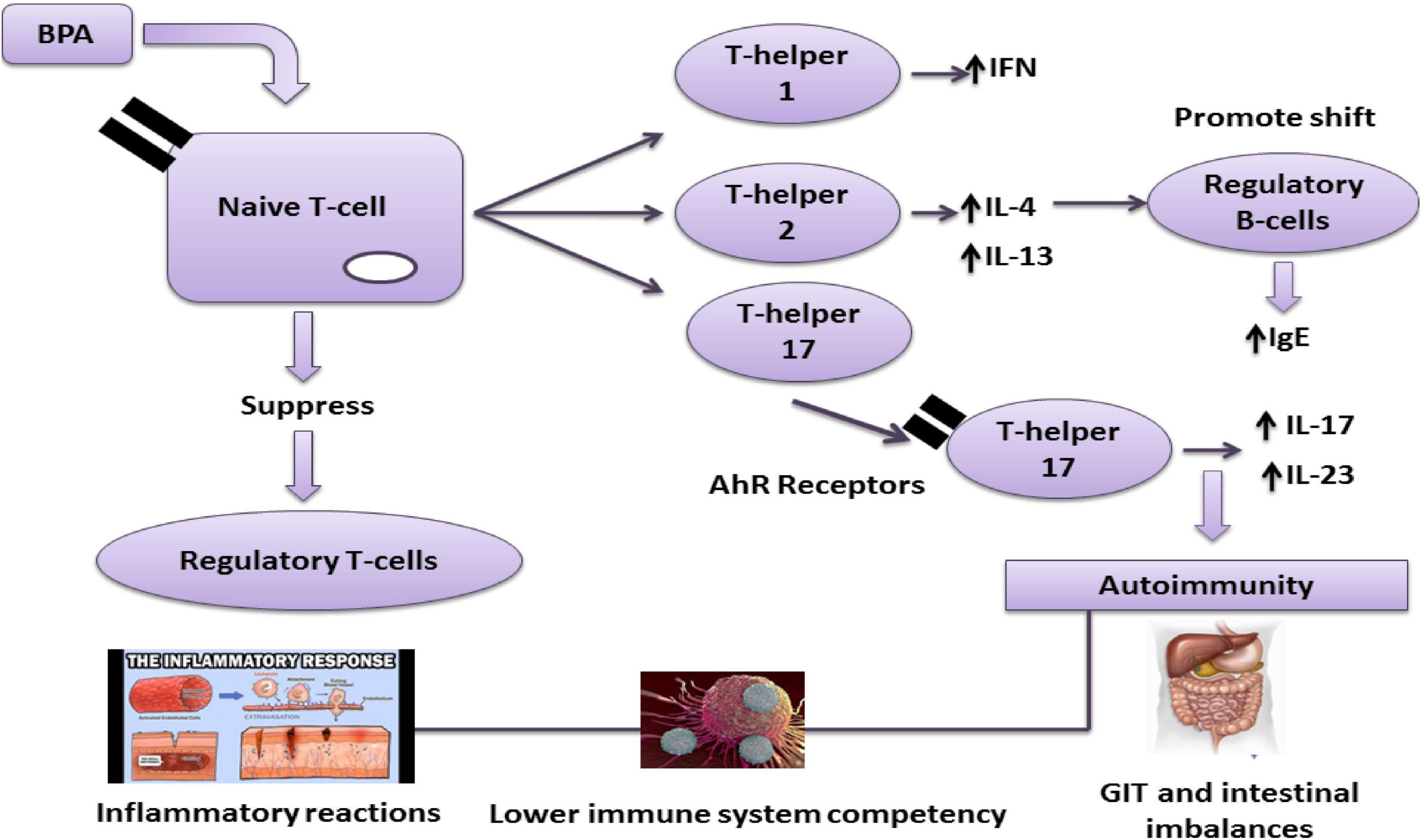
Figure 5. Effect of the BPA immune system BPA can promote autoimmunity via T-helpers 1, 2, and 17. Aryl hydrocarbon receptors (AhR) are involved in regulating immune responses, followed by the production of T-helper 17 a critical factor in T-cells in various autoimmune diseases.
Similarly, it also decreased T regulatory (Treg) cells and up-regulated pro-inflammatory and anti-inflammatory cytokines and chemokines. T1D development in females and males could be accelerated and decline on exposure to BPA (Table 5) (98).
The primary source of contact for BPA is food for the general population. According to the United States Environmental Protection Agency (EPA), BPA’s reference dose is 50 μg/kg BW/day. EFSA decreased this TDI dose from 50 μg/kg BW/day to 4 μg/kg BW/day in 2015 due to its harmful health effects (12).
A temporary TDI of BPA was set by the CEF panel that was 4 μg/kg BW per day. The board applied an uncertainty factor of 150 for this purpose for different body systems, including the reproductive system, metabolism, neurobehavioral, immune system, and mammary glands. It was done to assess the uncertainty along with inter and intraspecies differences. CEF declared no harmful health impacts by comparing this t-TDI with the estimates of exposure from the diet for any age group and common health concerns from the combined exposure. Therefore, this estimation of exposure to non-dietary sources showed considerable uncertainty compared to dietary sources’ estimates, imploring further research (99).
The rate of exposure from non-dietary sources, including thermal paper or medical devices based on current t-TDI derived by EFSA, was assessed by the SCENIHR or RAC, the Risk Assessment Committee. SCENIHR concluded that neonates in ICU, dialysis patients, and young children with prolonged medical treatment are at higher risk of getting adverse health effects from BPA as it may enter through systemic exposure after exposure to non-oral routes. But besides that, we cannot neglect the benefits of these devices (100). RAC also published and presented a restriction proposal for using BPA in the thermal paper under ECHA as an opinion of BPA’s hazards on human health. The consumers were satisfied by RAC, ensuring the risk of BPA exposure through the thermal paper was controlled. Simultaneously, the chance of getting BPA exposure from cashiers was not declared adequately in control. Severe effects can be faced by pregnant female workers working in a high-exposure environment (101).
Higher exposure rates of BPA are reported in Infants and children compared to adults. For breastfed infants, the average (95th percentile) BPA intake was 0.3 μg/kg body weight (BW) per day (1.3 μg/kg BW per day) for the age of 0 and 6 months. At the same time, 2.4 mg/kg BW per day (4.5 mg/kg BW per day) was reported for infants receiving formula from polycarbonate, according to WHO (47). European Union and Brazil have set the permissible limit of 600 μg/kg in infant foods. A study was conducted to assess the limit of BPA in infant formulas and reported the presence of BPA below the required level (0.2–10.2 μg/kg) (102). Another study estimated the BPA intake in different age groups and genders and concluded that their exposure was below the permissible limit (25 μg/kg of body weight/day) of Health Canada. However, dietary exposure to BPA for infants (0.22–0.33 μg/kg of body weight/day) was more than for adults (0.052–0.081 μg/kg of body weight/day). The increased intake was linked to the intake of canned and liquid milk-based infant formula (23).
Several restrictions on BPA use have been made after detecting its deteriorating health effects in different countries. The No Observed Adverse Effect Level (NOAEL) of BPA at a dose of 5,000 ng/kg body weight/day through the food intake was considered by the Food and Drug Administration in 2008 in the United States. Some EU Member States’ also banned it in food packaging and containers for children up to 3 years of age, while some have prolonged this ban for other products. Denmark also prohibited using BPA in packaging materials, including cups, or bottles related to food, especially for a breast milk substitute, in 2010. The use of BPA in baby bottles was also banned after 1st March 2011 by EU Commission Directive No. 8/2011 as a preventive measure (103).
Likewise, baby pacifiers containing BPA were also banned in Austria in 2011. All the materials containing BPA that had a chance to contact food were suspended in France by passing a law in 2012 except for industrial equipment, such as tanks and pipes. They also introduced the labeling requirements for food items prepared for children and pregnant women. In 2013, Sweden banned the BPA-containing materials in lacquers of packaging linings for food prepared for children aged 0–3 years (104).
FDA restricted baby bottles and Sippy cups having BPA in 2012 and BPA derivatives in cans on infant formula in 2013 (41, 105, 106). The Commission also conducted an evaluation (started in December 2017) focusing on existing legislation on food packaging; this evaluation ended in 2019. To support the Commission’s evaluation, the Joint Research Centre published a study (107) on the market condition of food packaging not coordinated in the EU. In December 2017, EFSA announced that a strategy was finalized to re-evaluate BPA toxicity with a working group for better results. BPA usage was restricted in thermal paper in January 2020, which would be through registration, evaluation, and authorization. Then restriction of chemicals regulation will decrease the use of BPA in all types of recycling packaging (108).
There is a need to find alternative solutions to BPA due to the health hazards of this compound’s use in packaging material. Several studies have been conducted in the previous few years to find the best suitable alternative to BPA having the same properties. Researchers have identified a few compounds that can be used as a replacement for BPA. The low estrogenic and endocrine potential of tetramethyl bisphenol F epoxy resin, bisguaiacol F, and tetramethyl bisphenol F diglycidyl ether is demonstrated in several studies. The researcher also suggested that further research is needed on this group of compounds to assess the potential possible effects of these compounds on human health.
Meanwhile, the authors suggested that they could be viable alternatives to BPA. These BPA substitute-based products are consumed under the label of “BPA-free.” This term gives the impression that the products are safe, but the substitutes’ safety is not fully verified (109, 110).
The increased restrictive rules for using BPA for human health and the environment have become a significant standard for substitution in research and industry (19, 111). Several “bisphenol analogs” have been produced to replace BPA in various applications (112). The most significant market shares are held by BPF (4, 4′-methylene diphenyl), BPS [bis (4-hydroxyphenyl) sulfone], and BPAF [2, 2-bis (4-hydroxyphenyl) hexafluoropropylene] (113–115). Reports and databases are available on the viability of these monomers as BPA substitutes. In Korea, BPS is used for thermal receipt papers and BPF as a water pipe coating agent instead of BPA (116). Although further research is needed to assess these compounds’ potential effects, the authors suggest they could be viable alternatives to BPA (117).
Bisphenol A can cause multiple organ toxicity after entering the body through the respiratory, dermal, and gastrointestinal tract. It disturbs different cellular mechanisms and hormonal functions by binding with the receptors and activating downstream pathways. The outcomes of BPA exposure are cancers, endocrine disruptions, immunosuppression and reproductive defects. However, there are still ambiguities and many unanswered questions about BPA’s metabolism and its toxic effects. There is a need to elaborate on the combined effects of BPA with other pollutants. Conclusively, BPA-free alternatives should be promoted to avoid these adverse consequences.
It is obvious from the current review that more basic non-human primate research and clinical studies are needed to understand the too-complex mechanisms behind BPA activity fully. Nevertheless, several variations across species have been identified, although rats and mice have been demonstrated to be ideal models for investigating the causes of chronic human diseases. Additionally, additional research is needed as a preventative and precautionary measure, especially for developing fetuses and young children, as they are more vulnerable to the harmful effects of this prevalent compound in both developed and developing countries, which requires more attention even through public awareness campaigns. However, because humans are exposed to various pollutants, it is important to consider that BPA may have additive and synergistic effects with other widely used compounds.
MM, TT, AyS, and SM: conceptualization. AmS, MN, and FT: methodology. TT, FT, and SK: software. MM, TT, FT, and SM: writing—original draft preparation. MM, AyS, and X-AZ: writing—review and editing. X-AZ: supervision. SI: supervision and funding acquisition. All authors have read and agreed to the published version of the manuscript.
This research was funded, in part, by grants (Project Nos. NC.X337-5-21-170-1 and NC.X341-5-21-170-1) in addition to the 1890 capacity building project from the National Institute of Food and Agriculture (NIFA). This research was funded by the Guangdong Provincial Key Laboratory of Intelligent Food Manufacturing, Foshan University, Foshan, China (Project ID: 2022B1212010015).
We would like to acknowledge the support of the Agricultural Research Station at North Carolina Agricultural and Technical State University (Greensboro, NC, United States).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The contents are solely the authors’ responsibility and do not necessarily represent the official views of NIFA.
BW, bodyweight; CAGR, compound annual growth rate; CEF, EFSA panel on food contact materials, enzymes, flavorings, and processing aids; EFSA, European food safety authority; EPA, environmental protection agency; FAO, food and agriculture organization; FDA, food and drug administration; FSH, follicle-stimulating hormone; GABAA, aminobutyric acid type A; IGF-1, insulin-like growth factor 1; PC, polycarbonate; PK, pharmacokinetic; PVC, polyvinylchloride; RAC, risk assessment committee; SCENIHR, EU scientific committee on emerging and newly identified health risks; TDI, tolerable daily intake; USD, United States dollar; WHO, World Health Organization.
1. Ma Y, Liu H, Wu J, Yuan L, Wang Y, Du X, et al. The adverse health effects of bisphenol A and related toxicity mechanisms. Environ Res. (2019) 176:108575. doi: 10.1016/j.envres.2019.108575
2. Khan MR, Ouladsmane M, Alammari AM, Azam M. Bisphenol A leaches from packaging to fruit juice commercially available in markets. Food Packaging Shelf Life. (2021) 28:100678. doi: 10.1016/j.fpsl.2021.100678
3. Wang R, Huang Y, Dong S, Wang P, Su X. The occurrence of bisphenol compounds in animal feed plastic packaging and migration into feed. Chemosphere. (2021) 265:129022. doi: 10.1016/j.chemosphere.2020.129022
4. Zhang Y, Yuan Z-L, Deng X-Y, Wei H-D, Wang W-L, Xu Z, et al. Metal-organic framework mixed-matrix membrane-based extraction combined HPLC for determination of bisphenol A in milk and milk packaging. Food Chem. (2022) 386:132753. doi: 10.1016/j.foodchem.2022.132753
5. Wang X, Nag R, Brunton NP, Siddique MAB, Harrison SM, Monahan FJ, et al. Human health risk assessment of bisphenol A (BPA) through meat products. Environ Res. (2022) 213:113734. doi: 10.1016/j.envres.2022.113734
6. Wang H, Liu Z-H, Zhang J, Huang R-P, Yin H, Dang Z, et al. Insights into removal mechanisms of bisphenol A and its analogues in municipal wastewater treatment plants. Sci Total Environ. (2019) 692:107–16. doi: 10.1016/j.scitotenv.2019.07.134
7. Tözüm MS, Alay Aksoy S, Alkan C. Manufacturing surface active shell and bisphenol A free thermochromic acrylic microcapsules for textile applications. Int J Energy Res. (2021) 45:7018–37. doi: 10.1002/er.6287
8. Markit, I. Bisphenol A. Chemical Economics Handbook. (2016). Available online at: https://www.ihs.com/products/bisphenol-chemical-economics-handbook.html
9. EFSA Panel on Food Contact Materials and Aids. Scientific opinion on the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs. EFSA J. (2015) 13:3978. doi: 10.2903/j.efsa.2015.3978
10. Hamed EM, Li SF. Molecularly imprinted polymers-based sensors for bisphenol-A: recent developments and applications in environmental, food and biomedical analysis. Trends Environ Anal Chem. (2022) 35:e00167. doi: 10.1016/j.teac.2022.e00167
11. Flint S, Markle T, Thompson S, Wallace E. Bisphenol A exposure, effects, and policy: a wildlife perspective. J Environ Manag. (2012) 104:19–34. doi: 10.1016/j.jenvman.2012.03.021
12. Neufeld K, Ezell K, Grow WA. Plastic additives decrease agrin-induced acetylcholine receptor clusters and myotube formation in C2C12 skeletal muscle cell culture. CellBio. (2015) 4:12. doi: 10.4236/cellbio.2015.41002
13. Brown MS, Somma L, Mendoza M, Noh Y, Mahler GJ, Koh A. Upcycling compact discs for flexible and stretchable bioelectronic applications. Nat Commun. (2022) 13:3727. doi: 10.1038/s41467-022-31338-9
14. Erren TC. Bisphenol A and cancer: a prelude to challenging epidemiology. Int Arch Occup Environ Health. (2022) 95:313–4. doi: 10.1007/s00420-021-01752-5
15. Hahladakis, JN, Iacovidou E, Gerassimidou S. An overview of the occurrence, fate, and human risks of the bisphenol-A present in plastic materials, components, and products. Integr Environ Assess Manag. (2022): doi: 10.1002/ieam.4611
16. Gerona RR, Woodruff TJ, Dickenson CA, Pan J, Schwartz JM, Sen S, et al. Bisphenol-A (BPA), BPA glucuronide, and BPA sulfate in midgestation umbilical cord serum in a northern and central California population. Environ Sci Technol. (2013) 47:12477–85. doi: 10.1021/es402764d
17. Divakaran K. Age-Related and Genetically-Determined Variation in Bisphenol A-Metabolizing Enzymes: Impact on Infant Bisphenol A Disposition. Milwaukee, WI: Medical College of Wisconsin (2014).
19. Almeida S, Raposo A, Almeida-González M, Carrascosa C. Bisphenol A: food exposure and impact on human health. Compr Rev Food Sci Food Saf. (2018) 17:1503–17. doi: 10.1111/1541-4337.12388
20. Vasiljevic T, Harner T. Bisphenol A and its analogues in outdoor and indoor air: properties, sources and global levels. Sci Total Environ. (2021) 789:148013. doi: 10.1016/j.scitotenv.2021.148013
21. Xing J, Zhang S, Zhang M, Hou J. A critical review of presence, removal and potential impacts of endocrine disruptors bisphenol A. Comp Biochem Physiol C Toxicol Pharmacol. (2022) 254:109275. doi: 10.1016/j.cbpc.2022.109275
22. Desai DP, Jagtap RN. Synthesis of ultraviolet curable bisphenol-based epoxy acrylates and comparative study on its physico-chemical properties. J Appl Polym Sci. (2022) 139:52022. doi: 10.1002/app.52022
23. Cao X-L, Perez-Locas C, Dufresne G, Clement G, Popovic S, Beraldin F, et al. Concentrations of bisphenol A in the composite food samples from the 2008 Canadian total diet study in Quebec City and dietary intake estimates. Food Addit Contam. (2011) 28:791–8. doi: 10.1080/19440049.2010.513015
24. Michałowicz J. Bisphenol A–sources, toxicity and biotransformation. Environ Toxicol Pharmacol. (2014) 37:738–58. doi: 10.1016/j.etap.2014.02.003
25. Freire C, Molina-Molina J-M, Iribarne-Durán LM, Jiménez-Díaz I, Vela-Soria F, Mustieles V, et al. Concentrations of bisphenol A and parabens in socks for infants and young children in Spain and their hormone-like activities. Environ Int. (2019) 127:592–600. doi: 10.1016/j.envint.2019.04.013
26. Huang Y, Wong C, Zheng J, Bouwman H, Barra R, Wahlström B, et al. Bisphenol A (BPA) in China: a review of sources, environmental levels, and potential human health impacts. Environ Int. (2012) 42:91–9. doi: 10.1016/j.envint.2011.04.010
27. Kang J-H, Kondo F, Katayama Y. Human exposure to bisphenol A. Toxicology. (2006) 226:79–89. doi: 10.1016/j.tox.2006.06.009
28. Rene ER, Kar S, Krishnan J, Pakshirajan K, López ME, Murthy D, et al. Start-up, performance and optimization of a compost biofilter treating gas-phase mixture of benzene and toluene. Bioresour Technol. (2015) 190:529–35. doi: 10.1016/j.biortech.2015.03.049
29. Zhang Y, Chen Z, Wu P, Duan Y, Zhou L, Lai Y, et al. Three-dimensional heterogeneous electro-fenton system with a novel catalytic particle electrode for bisphenol A removal. J Hazard Mater. (2020) 393:120448. doi: 10.1016/j.jhazmat.2019.03.067
30. Liang L, Zhang J, Feng P, Li C, Huang Y, Dong B, et al. Occurrence of bisphenol A in surface and drinking waters and its physicochemical removal technologies. Front Environ Sci Eng. (2015) 9:16–38. doi: 10.1007/s11783-014-0697-2
31. Radwan EK, Ibrahim M, Adel A, Farouk M. The occurrence and risk assessment of phenolic endocrine-disrupting chemicals in Egypt’s drinking and source water. Environ Sci Pollut Res. (2020) 27:1776–88. doi: 10.1007/s11356-019-06887-0
32. Makinwa T, Uadia P. Occurrence of bisphenol A (BPA) in ponds, rivers and Lagoons in South-Western Nigeria and uptake in Catfish evidence of environmental contamination. Food Public Health. (2017) 7:1–6.
33. Langdon K, Warne MSJ, Smernik R, Shareef A, Kookana R. Field dissipation of 4-nonylphenol, 4-t-octylphenol, triclosan and bisphenol A following land application of biosolids. Chemosphere. (2012) 86:1050–8. doi: 10.1016/j.chemosphere.2011.11.057
34. Corrales J, Kristofco LA, Steele WB, Yates BS, Breed CS, Williams ES, et al. Global assessment of bisphenol A in the environment: review and analysis of its occurrence and bioaccumulation. Dose Resp. (2015) 13:1559325815598308. doi: 10.1177/1559325815598308
35. Rudel RA, Brody JG, Spengler JD, Vallarino J, Geno PW, Sun G, et al. Identification of selected hormonally active agents and animal mammary carcinogens in commercial and residential air and dust samples. J Air Waste Manag Assoc. (2001) 51:499–513. doi: 10.1080/10473289.2001.10464292
36. Basheer C, Lee HK, Tan KS. Endocrine disrupting alkylphenols and bisphenol-A in coastal waters and supermarket seafood from Singapore. Mar Pollut Bull. (2004) 48:1161–7. doi: 10.1016/j.marpolbul.2004.04.009
37. Yamamoto T, Yasuhara A, Shiraishi H, Nakasugi O. Bisphenol A in hazardous waste landfill leachates. Chemosphere. (2001) 42:415–8. doi: 10.1016/S0045-6535(00)00079-5
38. Biedermann S, Tschudin P, Grob K. Transfer of bisphenol A from thermal printer paper to the skin. Anal Bioanal Chem. (2010) 398:571–6. doi: 10.1007/s00216-010-3936-9
39. Van Landuyt K, Nawrot T, Geebelen B, De Munck J, Snauwaert J, Yoshihara K, et al. How much do resin-based dental materials release? A meta-analytical approach. Dental Mater. (2011) 27:723–47. doi: 10.1016/j.dental.2011.05.001
40. Vandenberg LN, Chahoud I, Heindel JJ, Padmanabhan V, Paumgartten FJ, Schoenfelder G. Urinary, circulating, and tissue biomonitoring studies indicate widespread exposure to bisphenol A. Environ Health Perspect. (2010) 118:1055–70. doi: 10.1289/ehp.0901716
41. Usman A, Ahmad M. From BPA to its analogues: is it a safe journey? Chemosphere. (2016) 158:131–42. doi: 10.1016/j.chemosphere.2016.05.070
42. Morgan MK, Nash M, Barr DB, Starr JM, Clifton MS, Sobus JR. Distribution, variability, and predictors of urinary bisphenol A levels in 50 North Carolina adults over a six-week monitoring period. Environ Int. (2018) 112:85–99. doi: 10.1016/j.envint.2017.12.014
43. Molina-Molina J, Jiménez-Díaz I, Fernández M, Rodriguez-Carrillo A, Peinado F, Mustieles V, et al. Determination of bisphenol A and bisphenol S concentrations and assessment of estrogen-and anti-androgen-like activities in thermal paper receipts from Brazil, France, and Spain. Environ Res. (2019) 170:406–15. doi: 10.1016/j.envres.2018.12.046
44. Le Corre L, Besnard P, Chagnon M-C. BPA, an energy balance disruptor. Crit Rev Food Sci Nutr. (2015) 55:769–77. doi: 10.1080/10408398.2012.678421
45. Geens T, Apelbaum TZ, Goeyens L, Neels H, Covaci A. Intake of bisphenol A from canned beverages and foods on the Belgian market. Food Addit Contam. (2010) 27:1627–37. doi: 10.1080/19440049.2010.508183
46. Noonan GO, Ackerman LK, Begley TH. Concentration of bisphenol A in highly consumed canned foods on the US market. J Agric Food Chem. (2011) 59:7178–85. doi: 10.1021/jf201076f
47. World Health Organization. Toxicological and Health Aspects of Bisphenol A. Report of Joint FAO/WHO Expert Meeting, 2-5 November 2010 and Report of Stakeholder Meeting on Bisphenol A, 1 November 2010. Ottawa, ON: World Health Organization (2011).
48. Lorber M, Schecter A, Paepke O, Shropshire W, Christensen K, Birnbaum L. Exposure assessment of adult intake of bisphenol A (BPA) with emphasis on canned food dietary exposures. Environ Int. (2015) 77:55–62. doi: 10.1016/j.envint.2015.01.008
49. Konieczna A, Rutkowska A, Rachon D. Health risk of exposure to bisphenol A (BPA). Rocz Państw Zakł Hig. (2015) 66:5–11.
50. Geens T, Aerts D, Berthot C, Bourguignon J-P, Goeyens L, Lecomte P, et al. A review of dietary and non-dietary exposure to bisphenol-A. Food Chem Toxicol. (2012) 50:3725–40. doi: 10.1016/j.fct.2012.07.059
51. Zalko D, Jacques C, Duplan H, Bruel S, Perdu E. Viable skin efficiently absorbs and metabolizes bisphenol A. Chemosphere. (2011) 82:424–30. doi: 10.1016/j.chemosphere.2010.09.058
52. Wilson NK, Chuang JC, Morgan MK, Lordo RA, Sheldon LS. An observational study of the potential exposures of preschool children to pentachlorophenol, bisphenol-A, and nonylphenol at home and daycare. Environ Res. (2007) 103:9–20. doi: 10.1016/j.envres.2006.04.006
53. Völkel W, Colnot T, Csanády GA, Filser JG, Dekant W. Metabolism and kinetics of bisphenol A in humans at low doses following oral administration. Chem Res Toxicol. (2002) 15:1281–7. doi: 10.1021/tx025548t
54. Ginsberg G, Rice DC. Does rapid metabolism ensure negligible risk from bisphenol A? Environ Health Perspect. (2009) 117:1639–43.
55. Calafat AM, Ye X, Wong L-Y, Reidy JA, Needham LL. Exposure of the US population to bisphenol A and 4-tertiary-octylphenol: 2003–2004. Environ Health Perspect. (2008) 116:39–44. doi: 10.1289/ehp.10753
56. Miao M, Yuan W, He Y, Zhou Z, Wang J, Li D. Parental exposure to bisphenol A during pregnancy and the anogenital distance of male offspring. Epidemiology. (2011) 22:S242. doi: 10.1097/01.ede.0000392434.72621.fb
57. Chevrier C, Petit C, Philippat C, Mortamais M, Slama R, Rouget F, et al. Maternal urinary phthalates and phenols and male genital anomalies. Epidemiology (Cambridge Mass.). (2012) 23:353. doi: 10.1097/EDE.0b013e318246073e
58. Tominaga T, Negishi T, Hirooka H, Miyachi A, Inoue A, Hayasaka I, et al. Toxicokinetics of bisphenol A in rats, monkeys and chimpanzees by the LC–MS/MS method. Toxicology. (2006) 226:208–17. doi: 10.1016/j.tox.2006.07.004
59. Shelby, MD. NTP-CERHR monograph on the potential human reproductive and developmental effects of bisphenol A. Ntp Cerhr Mon. (2008) 22:v,vii–ix,1–64assim.
60. Fernandez M, Arrebola J, Taoufiki J, Navalón A, Ballesteros O, Pulgar R, et al. Bisphenol-A and chlorinated derivatives in adipose tissue of women. Reprod Toxicol. (2007) 24:259–64. doi: 10.1016/j.reprotox.2007.06.007
61. Doerge DR, Twaddle NC, Vanlandingham M, Brown RP, Fisher JW. Distribution of bisphenol A into tissues of adult, neonatal, and fetal Sprague–Dawley rats. Toxicol Appl Pharmacol. (2011) 255:261–70. doi: 10.1016/j.taap.2011.07.009
62. Viñas R, Goldblum RM, Watson CS. Rapid estrogenic signaling activities of the modified (chlorinated, sulfonated, and glucuronidated) endocrine disruptor bisphenol A. Endocr Disrupt. (2013) 1:e25411. doi: 10.4161/endo.25411
63. Teeguarden JG, Hanson-Drury S. A systematic review of Bisphenol A “low dose” studies in the context of human exposure: a case for establishing standards for reporting “low-dose” effects of chemicals. Food Chem Toxicol. (2013) 62:935–48. doi: 10.1016/j.fct.2013.07.007
64. Koch HM, Kolossa-Gehring M, Schröter-Kermani C, Angerer J, Brüning T. Bisphenol A in 24 h urine and plasma samples of the German environmental specimen bank from 1995 to 2009: a retrospective exposure evaluation. J Expo Sci Environ Epidemiol. (2012) 22:610–6. doi: 10.1038/jes.2012.39
65. Mortensen ME, Calafat AM, Ye X, Wong L-Y, Wright DJ, Pirkle JL, et al. Urinary concentrations of environmental phenols in pregnant women in a pilot study of the National Children’s Study. Environ Res. (2014) 129:32–8. doi: 10.1016/j.envres.2013.12.004
66. Vom Saal FS, Welshons WV. Evidence that bisphenol A (BPA) can be accurately measured without contamination in human serum and urine, and that BPA causes numerous hazards from multiple routes of exposure. Mol Cell Endocrinol. (2014) 398:101–13. doi: 10.1016/j.mce.2014.09.028
67. Woudenberg F, Van Den Berg M, Erisman J, Van Den Hazel P, Lebret E, Leemans R, et al. Advisory letter the health risks of bisphenol A analogues. Gezondheidsraad. (2014):
68. Teeguarden JG, Twaddle NC, Churchwell MI, Yang X, Fisher JW, Seryak LM, et al. 24-hour human urine and serum profiles of bisphenol A: evidence against sublingual absorption following ingestion in soup. Toxicol Appl Pharmacol. (2015) 288:131–42. doi: 10.1016/j.taap.2015.01.009
69. Doerge DR, Twaddle NC, Vanlandingham M, Fisher JW. Pharmacokinetics of bisphenol A in neonatal and adult Sprague-Dawley rats. Toxicol Appl Pharmacol. (2010) 247:158–65. doi: 10.1016/j.taap.2010.06.008
70. Doerge DR, Twaddle NC, Woodling KA, Fisher JW. Pharmacokinetics of bisphenol A in neonatal and adult rhesus monkeys. Toxicol Appl Pharmacol. (2010) 248:1–11. doi: 10.1016/j.taap.2010.07.009
71. Taylor JA, Vom Saal FS, Welshons WV, Drury B, Rottinghaus G, Hunt PA, et al. Similarity of bisphenol A pharmacokinetics in rhesus monkeys and mice: relevance for human exposure. Environ Health Perspect. (2011) 119:422–30. doi: 10.1289/ehp.1002514
72. Chapin RE, Adams J, Boekelheide K, Gray LE Jr., Hayward SW, Lees PS, et al. NTP-CERHR expert panel report on the reproductive and developmental toxicity of bisphenol A. Birth Defects Res B Dev Reprod Toxicol. (2008) 83:157–395. doi: 10.1002/bdrb.20147
73. Dekant W, Völkel W. Human exposure to bisphenol A by biomonitoring: methods, results and assessment of environmental exposures. Toxicol Appl Pharmacol. (2008) 228:114–34. doi: 10.1016/j.taap.2007.12.008
74. Twaddle NC, Churchwell MI, Vanlandingham M, Doerge DR. Quantification of deuterated bisphenol A in serum, tissues, and excreta from adult Sprague-Dawley rats using liquid chromatography with tandem mass spectrometry. Rapid Commun Mass Spectrom. (2010) 24:3011–20. doi: 10.1002/rcm.4733
75. Mielke H, Partosch F, Gundert-Remy U. The contribution of dermal exposure to the internal exposure of bisphenol A in man. Toxicol Lett. (2011) 204:190–8. doi: 10.1016/j.toxlet.2011.04.032
76. Calafat AM, Koch HM, Swan SH, Hauser R, Goldman LR, Lanphear BP, et al. Misuse of blood serum to assess exposure to bisphenol A and phthalates. Breast Cancer Res. (2013) 15:403. doi: 10.1186/bcr3494
77. Longnecker M, Harbak K, Kissling G, Hoppin J, Eggesbo M, Jusko T, et al. The concentration of bisphenol A in urine is affected by specimen collection, a preservative, and handling. Environ Res. (2013) 126:211–4. doi: 10.1016/j.envres.2013.07.002
78. Ye X, Zhou X, Hennings R, Kramer J, Calafat AM. Potential external contamination with bisphenol A and other ubiquitous organic environmental chemicals during biomonitoring analysis: an elusive laboratory challenge. Environ Health Perspect. (2013) 121:283–6. doi: 10.1289/ehp.1206093
79. Xi W, Lee C, Yeung W, Giesy JP, Wong MH, Zhang X, et al. Effect of perinatal and postnatal bisphenol A exposure to the regulatory circuits at the hypothalamus–pituitary–gonadal axis of CD-1 mice. Reprod Toxicol. (2011) 31:409–17. doi: 10.1016/j.reprotox.2010.12.002
80. Wisniewski P, Romano RM, Kizys MM, Oliveira KC, Kasamatsu T, Giannocco G, et al. Adult exposure to bisphenol A (BPA) in Wistar rats reduces sperm quality with disruption of the hypothalamic–pituitary–testicular axis. Toxicology. (2015) 329:1–9. doi: 10.1016/j.tox.2015.01.002
81. Xin F, Fischer E, Krapp C, Krizman EN, Lan Y, Mesaros C, et al. Mice exposed to bisphenol A exhibit depressive-like behavior with neurotransmitter and neuroactive steroid dysfunction. Horm Behav. (2018) 102:93–104. doi: 10.1016/j.yhbeh.2018.05.010
82. Mustieles V, Ocón-Hernandez O, Mínguez-Alarcón L, Dávila-Arias C, Pérez-Lobato R, Calvente I, et al. Bisphenol A and reproductive hormones and cortisol in peripubertal boys: the INMA-Granada cohort. Sci Total Environ. (2018) 618:1046–53. doi: 10.1016/j.scitotenv.2017.09.093
83. Mínguez-Alarcón L, Gaskins AJ, Chiu Y-H, Williams PL, Ehrlich S, Chavarro JE, et al. Urinary bisphenol A concentrations and association with in vitro fertilization outcomes among women from a fertility clinic. Hum Reprod. (2015) 30:2120–8. doi: 10.1093/humrep/dev183
84. Akın L, Kendirci M, Narin F, Kurtoglu S, Saraymen R, Kondolot M, et al. The endocrine disruptor bisphenol A may play a role in the aetiopathogenesis of polycystic ovary syndrome in adolescent girls. Acta Paediatr. (2015) 104:e171–7. doi: 10.1111/apa.12885
85. Vahedi M, Saeedi A, Poorbaghi SL, Sepehrimanesh M, Fattahi M. Metabolic and endocrine effects of bisphenol A exposure in market seller women with polycystic ovary syndrome. Environ Sci Pollut Res. (2016) 23:23546–50. doi: 10.1007/s11356-016-7573-5
86. Shen Y, Zheng Y, Jiang J, Liu Y, Luo X, Shen Z, et al. Higher urinary bisphenol A concentration is associated with unexplained recurrent miscarriage risk: evidence from a case-control study in eastern China. PLoS One. (2015) 10:e0127886. doi: 10.1371/journal.pone.0127886
87. Ji M, Xia J, Di J, Liu Y, Chen R, Chen Z, et al. Graphene-like boron nitride induced accelerated charge transfer for boosting the photocatalytic behavior of Bi4O5I2 towards bisphenol a removal. Chem Eng J. (2018) 331:355–63. doi: 10.1016/j.cej.2017.08.100
88. Song H, Zhang T, Yang P, Li M, Yang Y, Wang Y, et al. Low doses of bisphenol A stimulate the proliferation of breast cancer cells via ERK1/2/ERRγ signals. Toxicol Vitro. (2015) 30:521–8. doi: 10.1016/j.tiv.2015.09.009
89. Maffini MV, Rubin BS, Sonnenschein C, Soto AM. Endocrine disruptors and reproductive health: the case of bisphenol-A. Mol Cell Endocrinol. (2006) 254:179–86. doi: 10.1016/j.mce.2006.04.033
90. Dolinoy DC, Huang D, Jirtle RL. Maternal nutrient supplementation counteracts bisphenol A-induced DNA hypomethylation in early development. Proc Natl Acad Sci USA. (2007) 104:13056–61. doi: 10.1073/pnas.0703739104
91. Doherty LF, Bromer JG, Zhou Y, Aldad TS, Taylor HS. In utero exposure to diethylstilbestrol (DES) or bisphenol-A (BPA) increases EZH2 expression in the mammary gland: an epigenetic mechanism linking endocrine disruptors to breast cancer. Horm Cancer. (2010) 1:146–55. doi: 10.1007/s12672-010-0015-9
92. Fenichel P, Chevalier N, Brucker-Davis F. Bisphenol A: an endocrine and metabolic disruptor. Ann Endocrinol. (2013) 74:211–20. doi: 10.1016/j.ando.2013.04.002
93. Rubin BS. Bisphenol A: an endocrine disruptor with widespread exposure and multiple effects. J Steroid Biochem Mol Biol. (2011) 127:27–34. doi: 10.1016/j.jsbmb.2011.05.002
94. Welshons WV, Nagel SC, Vom Saal FS. Large effects from small exposures. III. Endocrine mechanisms mediating effects of bisphenol A at levels of human exposure. Endocrinology. (2006) 147:s56–69. doi: 10.1210/en.2005-1159
95. Moon MK, Kim MJ, Jung IK, Koo YD, Ann HY, Lee KJ, et al. Bisphenol A impairs mitochondrial function in the liver at doses below the no observed adverse effect level. J Korean Med Sci. (2012) 27:644–52. doi: 10.3346/jkms.2012.27.6.644
96. Xu Y, Ai J, Zhang H. The mechanism of degradation of bisphenol A using the magnetically separable CuFe2O4/peroxymonosulfate heterogeneous oxidation process. J Hazard Mater. (2016) 309:87–96. doi: 10.1016/j.jhazmat.2016.01.023
97. Park JC, Lee M-C, Yoon D-S, Han J, Kim M, Hwang U-K, et al. Effects of bisphenol A and its analogs bisphenol F and S on life parameters, antioxidant system, and response of defensome in the marine rotifer Brachionus koreanus. Aqu Toxicol. (2018) 199:21–9. doi: 10.1016/j.aquatox.2018.03.024
98. Xu X, Zong S, Chen W, Liu D. Comparative study of bisphenol A degradation via heterogeneously catalyzed H2O2 and persulfate: reactivity, products, stability and mechanism. Chem Eng J. (2019) 369:470–9. doi: 10.1016/j.cej.2019.03.099
99. Bolognesi C, Castle L, Cravedi J-P, Engel K-H, Fowler PAF, Franz R, et al. Scientific opinion on the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs: executive summary. EFSA J. (2015) 13:3978.
100. Testai E, Hartemann P, Rodríguez-Farré E, Rastogi SC, De Jong W, Bustos J, et al. The Safety of the use of Bisphenol A in Medical Devices. Brussels: European Commission (2015). doi: 10.1016/j.yrtph.2016.01.014
102. Sun N, Guo Q, Ou J-B. Simultaneous determination of endogenous hormones and exogenous contaminants in infant formula powdered milk by salting-out assisted liquid–liquid extraction combined with solid-phase extraction purification and UPLC-MS/MS. Anal Methods. (2017) 9:6177–85. doi: 10.1039/C7AY02038D
103. Official Journal of the European Union. COMMISSION DIRECTIVE 2011/8/EU of 28 January 2011 amending Directive 2002/72/EC as regards the restriction of use of bisphenol A in plastic infant feeding bottles. OJ. (2011) 50:11–4.
104. Cwiek-Ludwicka K. Bisphenol A (BPA) in food contact materials-new scientific opinion from EFSA regarding public health risk. Rocz Państw Zakł Hig. (2015) 66:299–307.
105. Park H-S, Koduru JR, Choo K-H, Lee B. Activated carbons impregnated with iron oxide nanoparticles for enhanced removal of bisphenol A and natural organic matter. J Hazard Mater. (2015) 286:315–24. doi: 10.1016/j.jhazmat.2014.11.012
106. Qin F-X, Jia S-Y, Liu Y, Li H-Y, Wu S-H. Adsorptive removal of bisphenol A from aqueous solution using metal-organic frameworks. Desalination Water Treat. (2015) 54:93–102. doi: 10.1080/19443994.2014.883331
107. Catherine S, Barbara R, Simone G, Eddo H, Anja M, Filipe ALJ, et al. Non-Harmonised Food Contact Materials in the EU: Regulatory and Market Situation: BASELINE STUDY: Final Report. Brussels: European Commission (2016).
108. European Commission. COMMISSION REGULATION (EU) 2018/213 of 12 February 2018 on the use of Bisphenol A in Varnishes and Coatings Intended to come into Contact with Food and Amending Regulation (EU) No 10/2011 as Regards the use of that Substance in Plastic Food Contact Materials Official Journal of the European Union. Brussels: European Commission (2018).
109. Eladak S, Grisin T, Moison D, Guerquin M-J, N’tumba-Byn T, Pozzi-Gaudin S, et al. A new chapter in the bisphenol A story: bisphenol S and bisphenol F are not safe alternatives to this compound. Fertil Steril. (2015) 103:11–21. doi: 10.1016/j.fertnstert.2014.11.005
110. Rochester JR, Bolden AL. Bisphenol S and F: a systematic review and comparison of the hormonal activity of bisphenol A substitutes. Environ Health Perspect. (2015) 123:643–50. doi: 10.1289/ehp.1408989
111. Tickner J, Jacobs M. Improving the identification, evaluation, adoption and development of safer alternatives: needs and opportunities to enhance substitution efforts within the context of REACH. Environ Health Perspect. (2016) 124:265–80. doi: 10.1289/ehp.1409581
112. Chen D, Kannan K, Tan H, Zheng Z, Feng Y-L, Wu Y, et al. Bisphenol analogues other than BPA: environmental occurrence, human exposure, and toxicity ⋅ a review. Environ Sci Technol. (2016) 50:5438–53. doi: 10.1021/acs.est.5b05387
113. Andújar N, Gálvez-Ontiveros Y, Zafra-Gómez A, Rodrigo L, Álvarez-Cubero MJ, Aguilera M, et al. Bisphenol A analogues in food and their hormonal and obesogenic effects: a review. Nutrients. (2019) 11:2136. doi: 10.3390/nu11092136
114. Pelch K, Wignall JA, Goldstone AE, Ross PK, Blain RB, Shapiro AJ, et al. A scoping review of the health and toxicological activity of bisphenol A (BPA) structural analogues and functional alternatives. Toxicology. (2019) 424:152235. doi: 10.1016/j.tox.2019.06.006
115. Liguori F, Moreno-Marrodan C, Barbaro P. Biomass-derived chemical substitutes for bisphenol A: recent advancements in catalytic synthesis. Chem Soc Rev. (2020) 49:6329–63. doi: 10.1039/D0CS00179A
116. Song CY, Kim W, Gye MC. Current state of use and the risks of bisphenols: a minireview. Korean J Environ Biol. (2017) 35:581–94. doi: 10.11626/KJEB.2017.35.4.581
117. Szafran AT, Stossi F, Mancini MG, Walker CL, And Mancini MA. Characterizing properties of non-estrogenic substituted bisphenol analogs using high throughput microscopy and image analysis. PLoS One. (2017) 12:e0180141. doi: 10.1371/journal.pone.0180141
118. Niu Y, Zhang J, Wu Y, Shao B. Analysis of bisphenol A and alkylphenols in cereals by automated on-line solid-phase extraction and liquid chromatography tandem mass spectrometry. J Agric Food Chem. (2012) 60:6116–22. doi: 10.1021/jf301401k
119. Munguia-Lopez E, Gerardo-Lugo S, Peralta E, Bolumen S, Soto-Valdez H. Migration of bisphenol A (BPA) from can coatings into a fatty-food simulant and tuna fish. Food Addit Contam. (2005) 22:892–8. doi: 10.1080/02652030500163674
120. Yoshida T, Horie M, Hoshino Y, Nakazawa H, Horie M, Nakazawa H. Determination of bisphenol A in canned vegetables and fruit by high performance liquid chromatography. Food Addit Contam. (2001) 18:69–75. doi: 10.1080/026520301446412
121. Cunha S, Fernandes J. Assessment of bisphenol A and bisphenol B in canned vegetables and fruits by gas chromatography–mass spectrometry after QuEChERS and dispersive liquid–liquid microextraction. Food Control. (2013) 33:549–55. doi: 10.1016/j.foodcont.2013.03.028
122. Cao X-L, Corriveau J, Popovic S. Levels of bisphenol A in canned soft drink products in Canadian markets. J Agric Food Chem. (2009) 57:1307–11. doi: 10.1021/jf803213g
123. O’Mahony J, Moloney M, Mccormack M, Nicholls IA, Mizaikoff B, Danaher M. Design and implementation of an imprinted material for the extraction of the endocrine disruptor bisphenol A from milk. J Chromatogr B. (2013) 931:164–9. doi: 10.1016/j.jchromb.2013.05.025
124. Choi I-S, Cho J-H, Park E-J, Park J-W, Kim S-H, Lee M-G, et al. Multiple effects of bisphenol A, an endocrine disrupter, on GABAA receptors in acutely dissociated rat CA3 pyramidal neurons. Neurosci Res. (2007) 59:8–17. doi: 10.1016/j.neures.2007.05.003
125. Song K-H, Lee K, Choi H-S. Endocrine disrupter bisphenol a induces orphan nuclear receptor Nur77 gene expression and steroidogenesis in mouse testicular Leydig cells. Endocrinology. (2002) 143:2208–15. doi: 10.1210/endo.143.6.8847
126. Arase S, Ishii K, Igarashi K, Aisaki K, Yoshio Y, Matsushima A, et al. Endocrine disrupter bisphenol A increases in situ estrogen production in the mouse urogenital sinus. Biol Reprod. (2011) 84:734–42. doi: 10.1095/biolreprod.110.087502
127. Zhou J, Zhu X-S, Cai Z-H. The impacts of bisphenol A (BPA) on abalone (Haliotis diversicolor supertexta) embryonic development. Chemosphere. (2011) 82:443–50. doi: 10.1016/j.chemosphere.2010.09.056
128. Kunz N, Camm EJ, Somm E, Lodygensky G, Darbre S, Aubert ML, et al. Developmental and metabolic brain alterations in rats exposed to bisphenol A during gestation and lactation. Int J Dev Neurosci. (2011) 29:37–43. doi: 10.1016/j.ijdevneu.2010.09.009
129. Hamdy H, Yahia D, Afifi S, Salem DA. Endocrine disruption induced by bisphenol A in young and adult female Sprague Dawley rats. Comp Clin Pathol. (2018) 27:967–74. doi: 10.1007/s00580-018-2689-2
130. Kwintkiewicz J, Nishi Y, Yanase T, Giudice LC. Peroxisome proliferator–activated receptor-γ mediates bisphenol A inhibition of FSH-stimulated IGF-1, aromatase, and estradiol in human granulosa cells. Environ Health Perspect. (2010) 118:400–6. doi: 10.1289/ehp.0901161
131. Braun JM, Kalkbrenner AE, Calafat AM, Yolton K, Ye X, Dietrich KN, et al. Impact of early-life bisphenol A exposure on behavior and executive function in children. Pediatrics. (2011) 128:873–82. doi: 10.1542/peds.2011-1335
132. Meeker JD, Calafat AM, Hauser R. Urinary bisphenol A concentrations in relation to serum thyroid and reproductive hormone levels in men from an infertility clinic. Environ Sci Technol. (2010) 44:1458–63. doi: 10.1021/es9028292
133. Liu X, Miao M, Zhou Z, Gao E, Chen J, Wang J, et al. Exposure to bisphenol-A and reproductive hormones among male adults. Environ Toxicol Pharmacol. (2015) 39:934–41. doi: 10.1016/j.etap.2015.03.007
134. Feng M, Wu X, Li J, Ding L, Wang Z, Shen Y, et al. Relationship between daily exposure to bisphenol A and male sexual function-a study from the reproductive center. Zhonghua liu xing bing xue za zhi. (2018) 39:836–40.
135. Den Hond E, Tournaye H, De Sutter P, Ombelet W, Baeyens W, Covaci A, et al. Human exposure to endocrine disrupting chemicals and fertility: a case–control study in male subfertility patients. Environ Int. (2015) 84:154–60. doi: 10.1016/j.envint.2015.07.017
136. Hart RJ, Doherty DA, Keelan JA, Minaee NS, Thorstensen EB, Dickinson JE, et al. The impact of antenatal bisphenol A exposure on male reproductive function at 20–22 years of age. Reprod Biomed Online. (2018) 36:340–7. doi: 10.1016/j.rbmo.2017.11.009
137. Radwan M, Wielgomas B, Dziewirska E, Radwan P, Kałużny P, Klimowska A, et al. Urinary bisphenol A levels and male fertility. Am J Mens Health. (2018) 12:2144–51. doi: 10.1177/1557988318799163
138. Tian Y, Zhou X, Miao M, Li D-K, Wang Z, Li R, et al. Association of bisphenol A exposure with LINE-1 hydroxymethylation in human semen. Int J Environ Res Public Health. (2018) 15:1770. doi: 10.3390/ijerph15081770
139. Adoamnei E, Mendiola J, Vela-Soria F, Fernández MF, Olea N, Jørgensen N, et al. Urinary bisphenol A concentrations are associated with reproductive parameters in young men. Environ Res. (2018) 161:122–8. doi: 10.1016/j.envres.2017.11.002
140. Pollack AZ, Mumford SL, Krall JR, Carmichael AE, Sjaarda LA, Perkins NJ, et al. Exposure to bisphenol A, chlorophenols, benzophenones, and parabens in relation to reproductive hormones in healthy women: a chemical mixture approach. Environ Int. (2018) 120:137–44. doi: 10.1016/j.envint.2018.07.028
141. Nanjappa MK, Simon L, Akingbemi BT. The industrial chemical bisphenol A (BPA) interferes with proliferative activity and development of steroidogenic capacity in rat Leydig cells. Biol Reprod. (2012) 86:1–12. doi: 10.1095/biolreprod.111.095349
142. Acevedo N, Davis B, Schaeberle CM, Sonnenschein C, Soto AM. Perinatally administered bisphenol a as a potential mammary gland carcinogen in rats. Environ Health Perspect. (2013) 121:1040–6. doi: 10.1289/ehp.1306734
143. Fernández M, Bourguignon N, Lux-Lantos V, Libertun C. Neonatal exposure to bisphenol A and reproductive and endocrine alterations resembling the polycystic ovarian syndrome in adult rats. Environ Health Perspect. (2010) 118:1217–22. doi: 10.1289/ehp.0901257
144. Newbold RR, Jefferson WN, Padilla-Banks E. Long-term adverse effects of neonatal exposure to bisphenol A on the murine female reproductive tract. Reprod Toxicol. (2007) 24:253–8. doi: 10.1016/j.reprotox.2007.07.006
145. Prins GS, Hu W-Y, Shi G-B, Hu D-P, Majumdar S, Li G, et al. Bisphenol A promotes human prostate stem-progenitor cell self-renewal and increases in vivo carcinogenesis in human prostate epithelium. Endocrinology. (2014) 155:805–17. doi: 10.1210/en.2013-1955
146. Weinhouse C, Anderson OS, Bergin IL, Vandenbergh DJ, Gyekis JP, Dingman MA, et al. Dose-dependent incidence of hepatic tumors in adult mice following perinatal exposure to bisphenol A. Environ Health Perspect. (2014) 122:485–91. doi: 10.1289/ehp.1307449
147. Ayyanan A, Laribi O, Schuepbach-Mallepell S, Schrick C, Gutierrez M, Tanos T, et al. Perinatal exposure to bisphenol a increases adult mammary gland progesterone response and cell number. Mol Endocrinol. (2011) 25:1915–23. doi: 10.1210/me.2011-1129
148. Tharp AP, Maffini MV, Hunt PA, Vandevoort CA, Sonnenschein C, Soto AM. Bisphenol A alters the development of the rhesus monkey mammary gland. Proc Natl Acad Sci USA. (2012) 109:8190–5. doi: 10.1073/pnas.1120488109
149. Ashley-Martin J, Dodds L, Levy AR, Platt RW, Marshall JS, Arbuckle TE. Prenatal exposure to phthalates, bisphenol A and perfluoroalkyl substances and cord blood levels of IgE, TSLP and IL-33. Environ Res. (2015) 140:360–8. doi: 10.1016/j.envres.2015.04.010
150. Rees Clayton EM, Todd M, Dowd JB, Aiello AE. The impact of bisphenol A and triclosan on immune parameters in the US population, NHANES 2003–2006. Environ Health Perspect. (2011) 119:390–6. doi: 10.1289/ehp.1002883
151. Li J, Bach A, Crawford RB, Phadnis-Moghe AS, Chen W, D’ingillo S, et al. CLARITY-BPA: effects of chronic bisphenol A exposure on the immune system: part 2–characterization of lymphoproliferative and immune effector responses by splenic leukocytes. Toxicology. (2018) 396:54–67. doi: 10.1016/j.tox.2018.02.004
152. Roy A, Gaylo A, Cao W, Saubermann LJ, Lawrence BP. Neither direct nor developmental exposure to bisphenol A alters the severity of experimental inflammatory colitis in mice. J Immunotoxicol. (2013) 10:334–40. doi: 10.3109/1547691X.2012.747231
153. Malaisé Y, Menard S, Cartier C, Gaultier E, Lasserre F, Lencina C, et al. Gut dysbiosis and impairment of immune system homeostasis in perinatally-exposed mice to bisphenol A precede obese phenotype development. Sci Rep. (2017) 7:14472. doi: 10.1038/s41598-017-15196-w
154. Roy A, Bauer SM, Lawrence BP. Developmental exposure to bisphenol A modulates innate but not adaptive immune responses to influenza A virus infection. PLoS One. (2012) 7:e38448. doi: 10.1371/journal.pone.0038448
155. Nakajima Y, Goldblum RM, Midoro-Horiuti T. Fetal exposure to bisphenol A as a risk factor for the development of childhood asthma: an animal model study. Environ Health. (2012) 11:8. doi: 10.1186/1476-069X-11-8
156. Salahinejad A, Attaran A, Naderi M, Meuthen D, Niyogi S, Chivers DP. Chronic exposure to bisphenol S induces oxidative stress, abnormal anxiety, and fear responses in adult zebrafish (Danio rerio). Sci Total Environ. (2021) 750:141633. doi: 10.1016/j.scitotenv.2020.141633
157. Faheem M, Adeel M, Khaliq S, Lone KP. Bisphenol-A induced antioxidants imbalance and cytokines alteration leading to immune suppression during larval development of Labeo rohita. Environ Sci Pollut Res. (2020) 27:26800–9. doi: 10.1007/s11356-020-08959-y
158. Huang M, Liu S, Fu L, Jiang X, Yang M. Bisphenol A and its analogues bisphenol S, bisphenol F and bisphenol AF induce oxidative stress and biomacromolecular damage in human granulosa KGN cells. Chemosphere. (2020) 253:126707. doi: 10.1016/j.chemosphere.2020.126707
Keywords: bisphenol A, endocrine disruptor, synthetic chemical, polycarbonate plastics, epoxy resins, BPA toxicity
Citation: Manzoor MF, Tariq T, Fatima B, Sahar A, Tariq F, Munir S, Khan S, Nawaz Ranjha MMA, Sameen A, Zeng X-A and Ibrahim SA (2022) An insight into bisphenol A, food exposure and its adverse effects on health: A review. Front. Nutr. 9:1047827. doi: 10.3389/fnut.2022.1047827
Received: 18 September 2022; Accepted: 12 October 2022;
Published: 03 November 2022.
Edited by:
Seydi Yıkmış, Tekirdağ Namik Kemal Üniversitesi, TurkeyReviewed by:
Muhammad Tayyab Rashid, Henan University of Technology, ChinaCopyright © 2022 Manzoor, Tariq, Fatima, Sahar, Tariq, Munir, Khan, Nawaz Ranjha, Sameen, Zeng and Ibrahim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin-An Zeng, eGF6ZW5nQHNjdXQuZWR1LmNu; Aysha Sameen, ZHIuYXlzaGFzYW1lZW5AZ2N3dWYuZWR1LnBr; Salam A. Ibrahim, aWJyYWgwMDFAbmNhdC5lZHU=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.