- Faculty of Medicine, Macau University of Science and Technology, Macau, China
The combined disease burden of diabetes mellitus (DM) and Alzheimer's disease (AD) is increasing, and the two diseases share some common pathological changes. However, the pharmacotherapeutic approach to this clinical complexity is limited to symptomatic rather than disease-arresting, with the possible exception of metformin. Whether nutritional intervention might extend or synergize with these effects of metformin is of interest. In particular, dietary patterns with an emphasis on dietary diversity shown to affect cognitive function are of growing interest in a range of food cultural settings. This paper presents the association between diabetes and AD. In addition, the cross-cultural nutritional intervention programs with the potential to mitigate both insulin resistance (IR) and hyperglycemia, together with cognitive impairment are also reviewed. Both dietary patterns and nutritional supplementation showed the effects of improving glycemic control and reducing cognitive decline in diabetes associated with AD, but the intervention specificity remained controversial. Multi-nutrient supplements combined with diverse diets may have preventive and therapeutic potential for DM combined with AD, at least as related to the B vitamin group and folate-dependent homocysteine (Hcy). The nutritional intervention has promise in the prevention and management of DM and AD comorbidities, and more clinical studies would be of nutritional scientific merit.
Introduction
Diabetes mellitus (DM) is a chronic disease with a metabolic disorder characterized by hyperglycemia, resulting from insufficient insulin secretion in the body or insulin resistance (IR) (1). According to published data, the global prevalence of diabetes was about 9.3% (463 million people) in 2019, and it is estimated that the prevalence will rise to 10.2% (578 million people) by 2030. More than 700 million individuals might be affected by diabetes worldwide by 2045 (2). At present, the treatment methods for DM mainly include five measures: dietary control, exercise, hypoglycemic medicine, health education, and self-monitoring.
Dementia is also a serious public health problem. Alzheimer's disease (AD), the most common type of dementia, is a chronic neurodegenerative disease characterized by impairment of memory and cognition, along with changes in behavior and personality (3). Pathological features of AD include amyloid plaques composed of fibrillar Aβ and neurofibrillary tangles composed of hyper-phosphorylated tau proteins that could induce oxidative stress, inflammatory damage, cerebrovascular damage, blood-brain barrier dysfunction, and neuronal death (4). The mechanism of AD development is not yet fully discovered and both genetic and environmental factors are involved (5). According to the reports in 2021, AD affected approximately 34 million people worldwide and approximately 5.8 million Americans aged 65 years and older currently have AD. From 2000 to 2019, the number of reported deaths related to AD increased by more than 145% (5, 6). Epidemiological studies have shown that n-3 long-chain polyunsaturated fatty acids (FAs) and docosahexaenoic acid could inhibit Aβ and tau protein production and help the neurons maintain normal function (7). Low intakes of n-3 FAs, B vitamins, and antioxidants have been linked to an increased risk of AD (8, 9). Currently, there is no effective drug that could reverse the symptoms of AD or stop neuronal damage and destruction, and the disease tends to progress gradually.
A substantial body of research indicates that nutrients and phytochemicals including vitamins, folic acid, and polyphenols may have therapeutic effects on DM combined with AD because they could regulate blood glucose concentration, slow the progress of cognitive decline, improve IR, and protect the nervous system from inflammation and/or oxidative damage (10–12). This review discusses and summarizes the effects and potential mechanisms of nutritional intervention of DM and AD, and provides suggestions for nutritional therapy to lower the risk of developing AD in DM individuals.
Methods
CiteSpace visual analysis software and the bibliometric analysis platform were used to analyze the status of the nutritional intervention that improves DM accompanied with AD. PubMed, EMBASE, Cochrane Library, and China National Knowledge Infrastructure (CNKI) databases were searched to identify the relevant and reliable literature up to June 2022. The following search terms were used: Alzheimer's disease, diabetes, dementia, food ingredients, nutrition, and diet. After screening the abstracts and titles, the relevant literature was analyzed and organized, focusing on the last 5 years. In total, 161 potentially relevant articles were included in this review.
Correlation between diabetes and Alzheimer's disease
Type 1 diabetes mellitus (T1DM) is a subtype of diabetes (13). Some links have been found between type 1 diabetes and cognitive impairment (14). A study on cerebral compromise and its underlying mechanisms in type 1 diabetes found altered levels of cerebrospinal fluid (CSF), a biomarker of AD, compared to controls. However, the observed profile does not match the full risk profile seen in pre-AD patients (15). The findings of a large retrospective cohort study of 343,062 hospitalized patients with type 1 diabetes indicate that type 1 diabetes is associated with an elevated risk of any dementia, AD, and vascular dementia, and is particularly pronounced in younger patients with diabetes (16). The mechanisms underlying the association between type 1 diabetes and the development of cognitive impairment are not yet fully understood. Further research is needed in the future.
Numerous epidemiological studies have linked diabetes to dementia caused by AD, especially type 2 diabetes mellitus (T2DM), and it is even considered that AD is likely to represent a brain-specific form of diabetes, namely type 3 diabetes. Some studies indicated that T2DM is a risk factor for AD (17), but there is no validation as to whether AD is a risk factor for T2DM. Type 2 diabetes mellitus accounts for one-tenth of people with dementia worldwide, and T2DM patients have a higher chance (>50%) to develop AD than those non-T2DM individuals (18–20). Alzheimer's disease and T2DM share common risk factors, such as obesity, aging, and IR (21–23). In addition, there are many common pathological mechanisms associated with IR between AD and T2DM, such as oxidative stress, impaired insulin signaling, mitochondrial dysfunction, neuro-inflammation, advanced glycation end products (AGEs), and metabolic syndrome, etc. (3, 24, 25). The insulin signaling pathway is initiated when insulin recognizes and binds to the transmembrane tyrosine kinase receptor (TKR). Activated TKR causes insulin receptor substrates (IRS) to be tyrosine phosphorylated by insulin receptor tyrosine kinase, followed by blocking downstream signaling pathways and impairing insulin signaling pathways, then working together with Aβ deposition and mitochondrial dysfunction to form a vicious circle (26).
Abnormalities of glucose metabolism may contribute to AD development in diabetic patients and the disorder of energy metabolism is directly associated with the pathological development of AD (27). Abnormal metabolism and transportation of glucose in DM could impair the cognitive performance of the patients (28). Therefore, adequate blood glucose control should be the main goal of therapeutic approaches to lower the risk of AD in diabetic individuals. Additionally, oxidative stress and mitochondrial dysfunction are linked to the onset and progression of AD in diabetic patients. It is postulated that the normal function of mitochondria is crucial for delaying aging and avoiding neurodegenerative illnesses (29). Mitochondrial dysfunction is a key factor in the pathogenesis of various diseases, such as diabetes and neurodegenerative diseases (30). The brain is very susceptible to mitochondrial dysfunction due to its high energy requirements (31). Many studies have shown that mitochondrial oxidative stress and the production of reactive oxygen species (ROS) are increased under hyperglycemic conditions, and a large amount of ROS could lead to a series of common AD pathological changes, such as the oxidative damage of proteins, carbohydrates, and lipids (32). A recent study found for the first time that adipose tissue-derived EVs from high-fat diet (HFD)-fed mice or patients with diabetes induce remarkable synaptic loss and cognitive impairment (33).
Anti-AD drugs, especially piracetam could significantly reduce some diabetic parameters, such as fasting plasma glucose (FPG), HbA1c, and serum insulin concentration in patients with diabetic AD (34). Similarly, epidemiological studies showed that some antidiabetic drugs such as metformin, applied in diabetic patients could reduce the risk of developing AD and all-cause dementia (4, 35). However, the protective effect of metformin on AD is controversial. One study found that metformin had a protective effect in diabetic patients accompanied by cognitive impairment or dementia, while the protective effect was not seen in non-diabetic individuals with cognitive impairment (36). The patients with mild cognitive impairment or mild AD showed little improvement after being treated with metformin in clinical trials (37, 38). In addition, the precise mechanism underlying the therapeutic activity of metformin in AD is unclear. Metformin may act through mechanisms involving glucose homeostasis, decreased amyloid plaque deposition, normalization of tau protein phosphorylation, and increased autophagy (39). More research is needed to confirm the potential role of metformin in DM accompanied by AD.
Nutritional intervention improves DM accompanied with AD
Due to the increasing prevalence, mortality, and complication rates, DM has a great impact on the quality of life in diabetic patients. The effect of pharmacology to cure AD is limited, as whether the nutritional intervention could reduce the risk and progression of AD in diabetic individuals is of significant interest. Changes in dietary intake and lifestyle are more important, and easier and safer to implement than medication. It is particularly important to explore scientific and effective nutritional interventions to improve the disease prognosis of DM patients with AD.
Management of dietary intake
For patients with diabetes and AD, it is common to have both declined cognition and unhealthy dietary intake, overconsumption of some foods makes it difficult to glucose control, while inappropriate strict limitation of food intake might induce hypoglycemia. Management of dietary intake is critical for blood glucose control in diabetic patients. Some studies found that improper dietary control, untimely drug adjustment, and the influence of exercise intensity contributed to poor glucose control in patients with AD accompanied by T2DM (40). Many studies also showed that a reasonable and healthy diet could provide appropriate nutrients and energy required by the patients without inducing significant fluctuation in blood glucose concentration (41–43). Well-planned dietary management could effectively control blood glucose and insulin concentrations and might help to delay further cognitive decline (44) in T2DM patients with AD.
Prevention of hypoglycemia
In cases of DM accompanied by dementia or AD, the patients might have a problem organizing their meals and even be insensitive to hungry, which could induce hypoglycemia (45). The caregiver should try his/her best to persuade him/her to eat, be patient with feeding, and if necessary, give a sugar-free liquid diet through tube feeding or provide intravenous nutrition as prescribed by the doctor to meet the needs of the body's energy (46). To prevent hypoglycemia, it is recommended that these patients should bring some candies and chocolates with them. For the in-patients who are not used to adapt the hospital diet, the dietitian should contact their family members to provide the patient's favorite, but low-sugar, low-fat, and fiber-rich foods (47). For those who have difficulty chewing or swallowing, the food with appropriate nutrients and energy should be ground into a paste and provided to the patients (48).
Reasonable control of the energy intake
According to the patient's physical activity level and eating habits, the dietitian could formulate a diet guide card, and calculate the daily intake of protein, fat, carbohydrate, vegetable, and fruit based on the total amount of food exchange portion. The dietitian could make an individual diet plan based on the daily calorie requirement of the patient. Coarse grains and pasta are the staple food with a low glycemic index (GI), certain types of dark green leafy vegetables are recommended for diabetic patients even at a relatively large amount, while foods rich in simple sugar, e.g., sucrose and honey should be limited. In general, three meals a day are allocated reasonably at the energy distribution of 2/5, 2/5, and 1/5 for breakfast, lunch, and dinner, respectively (49, 50).
Glycemic management
Good glycemic control is crucial for diabetic patients in suppressing disease progress, complications, and even the development of AD. Feeling hungry is a common symptom of DM patients. The quantity and quality of the food consumed should be cautious. Under the condition of enough energy and nutrients, the patients should choose foods that are low GI and rich in dietary fiber, such as coarse grains, potatoes, and miscellaneous beans. Dietary fiber could prevent postprandial hyperglycemia and be fermented by intestinal flora to produce short-chain FAs in the large bowel. Daily dietary fiber intake could reach up to 40 g for diabetic patients. At the same time, the patient's physical activity level and tolerance capacity should be monitored at the time of exercise to avoid hypoglycemia (49).
Dietary pattern
Improving effects of dietary patterns in DM-only patients
Changes in lifestyle and self-management skills are critical in the treatment of diabetes. A change in eating habits is one of the most important lifestyle changes and challenges for people with diabetes (51). Studies have shown that a low-carbohydrate diet (LCD) can improve glycemic control in people with T2DM, and the effects are even more pronounced with a ketogenic diet (KD) (52). However, there is currently no evidence that LCD or KD can delay or prevent the onset of T1DM (53). In addition, a meta-analysis found that Medi (Mediterranean diet) appears to be the most effective and efficient diet for better glycemic control in patients with T2DM (54). There is also evidence that Medi has beneficial effects on cardiometabolic health and reduces mortality in patients with T2DM (55).
Improving effects of dietary patterns in AD-only patients
For AD patients, observational studies suggested that the MIND (Mediterranean-DASH Diet Intervention for Neurodegenerative Delay) may be more protective against cognitive decline and AD than the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets, but more evidence on the MIND diet is required to make a firm judgment (56–58). Ketogenic diet has beneficial effects on enhancing mitochondrial function and cellular metabolism, which are associated with improved cognitive performance in older adults with AD. The level and duration of ketosis affect the improvement of cognitive outcomes (59).
Improving effects of dietary patterns in DM with AD patients
Medi, DASH, and MIND dietary patterns have been found to have a positive influence on DM with AD patients. Both the Medi and DASH dietary patterns emphasize the consumption of plant-based foods and low or limited consumption of red meat. Medi is a traditional diet originating from Mediterranean countries, that focuses on the consumption of abundant fruits, vegetables, legumes, unrefined grains, plenty of fish, and moderate dairy products (such as low-fat cheese and yogurt) and wine, taking olive oil as the cooking oil, while DASH emphasizes consumption of dairy products and low consumption of sodium, industrial sweets, and saturated fat (60). In middle-aged and older adults with T2DM, adherence to the Medi is related to better cognitive function and glycemic control (61, 62). The MIND diet is a combination of the Medi and DASH dietary patterns, emphasizing the consumption of natural plant foods, especially increasing the intake of berries and dark green leafy vegetables, which are rich in folic acid, lutein, lycopene, and alpha and beta carotene, which might play roles in anti-aging for the brain and help to maintain cognitive function (63–65). Adherence to any of the Medi, DASH, and MIND dietary patterns could improve insulin sensitivity, and reduce the likelihood of diabetes and inflammation, in turn reducing the risk of dementia and AD (66–69).
Ketogenic diet has also been found to have a positive influence on DM with AD patients. Ketogenic diets are low-carbohydrate, high-fat, moderate-protein diets that typically provide about 80% of calories from fat, 15% from protein, and 5% from carbohydrates (70). Medium-chain triglyceride (MCT) oil, a major lipid component in KD, may promote ketogenesis and maintain mitochondrial function, in conjunctive therapy for AD patients (71, 72). This dietary pattern could improve glycemic control in T2DM (73) and accompany cognitive impairment in AD (74). Long-term adherence to the KD is difficult with side effects attributable to the compromised dietary quality of micro-nutrient deficiency, along with poor appetite, nausea, constipation, fatigue, dyslipidemia, and unexpected weight loss (53, 75).
Supplements
Some studies have demonstrated that probiotic supplementation could improve T2DM and AD (76–79). For example, the probiotic Lactobacillus acidophilus attenuated the inflammatory response in T2DM by modulating hepatic gluconeogenesis, lipid metabolism, and gut microbiota in mice (80). Prebiotic inulin and dietary inulin may suppress inflammation and modulate gut macrobiotics during T2DM progression (81). In AD patients, cognitive function was improved after treatment with probiotics containing Lactobacillus and Bifidobacterium (82, 83).
It remains debatable whether patients with T2DM and AD could benefit from vitamin supplementation. Vitamin A may be involved in nerve regeneration, neurodevelopment, and neurodegeneration, including AD (84, 85). Vitamin C and E have been touted for potentially favorable anti-oxidative effects in T2DM and AD (86, 87). Vitamin D deficiency might increase neurodegenerative risk, in part through ted development of IR and diabetes by reducing insulin signaling (88, 89). Experimental studies indicated that vitamin D had the potential to prevent and treat cognitive decline in dementia (90), and cohort studies suggested that higher concentrations of circulating vitamin D may lower the risk of all-cause dementia and AD in T2DM. Vitamin D supplementation in the elderly might slow cognitive decline and delay the onset of dementia, especially AD (91, 92).
Hyperhomocysteinemia (HHcy) is a risk factor for AD development, and once HHcy is corrected, the development of AD might be postponed (93–95). Homocysteine (Hcy) is a sulfur-containing non-proteinogenic amino acid that enhances excitotoxicity and causes DNA damage and death in neurons, impairing short-term memory and learning (96). Hyperhomocysteinemia is a state in which the body has an excess of Hcy (97). Vitamins B-6, B-12, and folic acid are essential dietary nutrients for maintaining normal physiological concentrations of Hcy (98). Folic acid (also known as the oxidized form of vitamin B-9) supplementation has positive effects on diabetes-related oxidative stress (99) and could improve cognitive function in AD patients (100). Folic acid supplementation alone or the use of multivitamin supplements containing vitamins B-6, and B-12 have been shown to be effective in reducing plasma Hcy concentrations in patients with AD and DM (101–103). Brain atrophy is accelerated in the elderly with cognitive impairment, particularly those who have AD (104). It has been demonstrated that HHcy is linked to brain atrophy. Supplementation with B vitamins to elderly with mild cognitive impairment may slow the acceleration of brain atrophy by lowering blood Hcy concentrations (105). Additionally, a high baseline of plasma n-3 FA was observed to improve the positive effects of high-dose B vitamin supplementation, which decreased the mean rate of brain shrinkage by 40% in participants with high plasma n-3 FA concentrations compared to those in the placebo group. In contrast, B vitamins had no effect on brain shrinkage in patients with low concentrations of plasma n-3 FA (106). Even though numerous studies explored the association between plasma Hcy and AD, it is not easy to tell the exact effects of Hcy, folate, or vitamin B-12 on cognition and/or AD pathogenesis (107). Understanding the underlying mechanisms of HHcy in AD may help to improve the treatment and bring immediate clinical advantages for the patients.
The antioxidant and anti-inflammatory effects of bioactive compounds, such as polyphenols and carotenoids in vegetables and fruits make them candidates for the prevention and control of DM and AD. Polyphenols such as resveratrol (108–112), gallic acid (11, 113, 114), curcumin (115–118), anthocyanins (119), luteolin (120), hesperetin (121), genistein (122), Boswellia serrata gum extract (123), mango leaf extract (124), and flavonoids (125), exist in a variety of plants. They have various functions, such as preventing oxidative stress damage, regulating blood glucose concentration, inhibiting inflammation, improving IR, and neuroprotection, which are all beneficial to DM and AD. A great body of research have confirmed that having foods rich in polyphenols could reduce the risk of DM and AD (12), improve insulin sensitivity in DM patients to inhibit the formation of AGEs, and promote cellular uptake of glucose (126). Polyphenols could also prevent the subsequent development of DM-related complications such as cardiovascular disease, neuropathy, etc., and improve neuronal metabolism and cognitive performance (127), Carotenoids, such as lycopene have been shown having beneficial effects on diabetes and its associated complications in many animal studies, and are potentially effective drug components for the treatment of AD (128, 129).
Supplementation of trace elements, such as magnesium and zinc in diabetic patients could promote glucose transport, maintain normal cell function and lipid metabolism, and enhance tyrosine kinase activity. There was a significant negative association between magnesium intake and all-cause dementia, but the same association was not observed in AD, whereas cognitive improvement was found after zinc therapy in a mouse model of AD, indicating that zinc may play an important role in the pathogenesis of AD (130, 131).
Intake of n-3 FAs (132), pentacyclic triterpenoids (133), Hedera nepalensis crude extract and lupin alcohol (134), marine phenolics (135), fig leaf extract (136), α-lipoic acid (137) has been shown to positively mediate inflammatory and immune responses, reduce the risk of IR and neurocognitive impairment, and ultimately decrease the risk of AD.
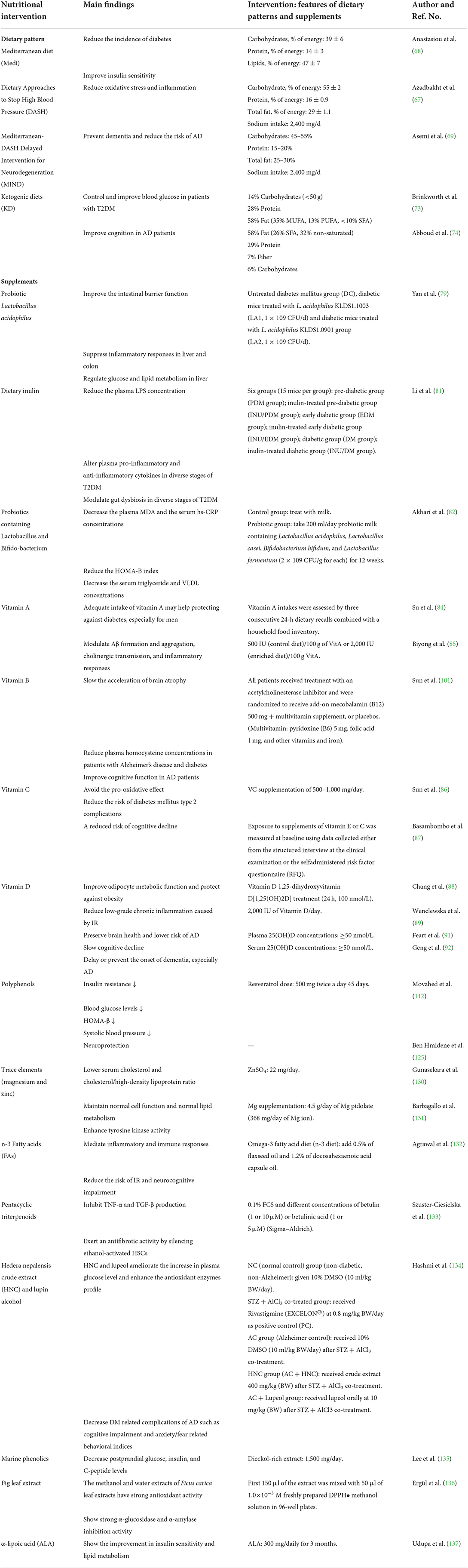
The effects of nutritional intervention for DM with AD mentioned above are summarized in Table 1.
Conclusion
The prevalence of DM and AD increases year by year. These two diseases share a common underlying pathological mechanism, and DM patients have a higher risk of developing AD. Therefore, a focus on how to prevent and treat DM accompanied by AD should underscore the potential relevance of nutritional intervention strategies in three respects: food intake management, dietary pattern, and nutrient supplementation. To date, various food factors and dietary components including probiotics, polyphenols, trace elements, and n-3 FAs, have been countenanced as candidates for cognitive maintenance or improvement in diabetic patients who are prone to brain dysfunction. Two dietary patterns, the KD, and the Mediterranean diet have been found to be therapeutically effective in DM and AD. Multi-nutrient supplements together with a healthy dietary pattern may enhance the therapeutic effectiveness. The key to the prevention of DM accompanied by AD is to identify the risk factors such as obesity, lack of exercise, and unhealthy eating habits before the disease is apparent, and to establish effective intervention strategies, especially nutritional measures.
Author contributions
ZL: conducted literature search in different search engines, contributed in preparation of first draft, and final version of the manuscript. SL: conducted literature search in different search engines and contributed in preparation of first draft of the manuscript. YX, TZ, and XY: provided guidance of the manuscript. LW: critically reviewed the manuscript, provided guidance, and approved the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The work is supported by Macau University of Science and Technology, Faculty Research Grant, FRG-21-036-FMD.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Athanasaki A, Melanis K, Tsantzali I, Stefanou MI, Ntymenou S, Paraskevas SG, et al. Type 2 diabetes mellitus as a risk factor for Alzheimer's disease: review and meta-analysis. Biomedicines. (2022) 10:778. doi: 10.3390/biomedicines10040778
2. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
3. Michailidis M, Moraitou D, Tata DA, Kalinderi K, Papamitsou T, Papaliagkas V. Alzheimer's disease as type 3 diabetes: common pathophysiological mechanisms between Alzheimer's disease and type 2 diabetes. Int J Mol Sci. (2022) 23:2687. doi: 10.3390/ijms23052687
4. Cummings J, Ortiz A, Castellino J, Kinney J. Diabetes: risk factor and translational therapeutic implications for Alzheimer's disease. Eur J Neurosci. (2022) 2022:10.1111/ejn.1561. doi: 10.1111/ejn.15619
5. Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. (2011) 10:819–28. doi: 10.1016/S1474-4422(11)70072-2
6. Alzheimer's disease facts and figures. Alzheimers Dement. (2021) 17:327–406. doi: 10.1002/alz.12328
7. Kamphuis PJ, Scheltens P. Can nutrients prevent or delay onset of Alzheimer's disease? J Alzheimers Dis. (2010) 20:765–75. doi: 10.3233/jad-2010-091558
8. Farkas M, Keskitalo S, Smith DE, Bain N, Semmler A, Ineichen B, et al. Hyper-homocysteinemia in Alzheimer's disease: the hen and the egg? J Alzheimers Dis. (2013) 33:1097–104. doi: 10.3233/jad-2012-121378
9. Faxén-Irving G, Freund-Levi Y, Eriksdotter-Jönhagen M, Basun H, Hjorth E, Palmblad J, et al. Effects on transthyretin in plasma and cerebrospinal fluid by DHA-rich n-3 fatty acid supplemen-tation in patients with Alzheimer's disease: the omegAD study. J Alzheimers Dis. (2013) 36:1–6. doi: 10.3233/jad-121828
10. Kaliś K. [Dual action of vitamin C versus degradation and supplementation]. Postepy Hig Med Dosw (Online). (2015) 69:1239–44. doi: 10.5604/17322693.1180642
11. Lupaescu AV, Iavorschi M, Covasa M. The use of bioactive compounds in hyperglycemia- and amyloid fibrils-induced toxicity in type 2 diabetes and Alzheimer's disease. Pharmaceutics. (2022) 14:235. doi: 10.3390/pharmaceutics14020235
12. Letenneur L, Proust-Lima C, Le Gouge A, Dartigues JF, Barberger-Gateau P. Flavonoid intake and cognitive decline over a 10-year period. Am J Epidemiol. (2007) 165:1364–71. doi: 10.1093/aje/kwm036
13. Li W, Huang E, Gao S. Type 1 diabetes mellitus and cognitive impairments: a systematic review. J Alzheimers Dis. (2017) 57:29–36. doi: 10.3233/jad-161250
14. Shalimova A, Graff B, Gasecki D, Wolf J, Sabisz A, Szurowska E, et al. Cognitive dysfunction in type 1 diabetes mellitus. J Clin Endocrinol Metab. (2019) 104:2239–49. doi: 10.1210/jc.2018-01315
15. Ouwens DM, van Duinkerken E, Schoonenboom SN, Herzfeld de Wiza D, Klein M, van Golen L, et al. Cerebrospinal fluid levels of Alzheimer's disease biomarkers in middle-aged patients with type 1 diabetes. Diabetologia. (2014) 57:2208–14. doi: 10.1007/s00125-014-3333-6
16. Smolina K, Wotton CJ, Goldacre MJ. Risk of dementia in patients hospitalised with type 1 and type 2 diabetes in England, 1998–2011: a retrospective national record linkage cohort study. Diabetologia. (2015) 58:942–50. doi: 10.1007/s00125-015-3515-x
17. Klimova B, Kuca K, Maresova P. Global view on Alzheimer's disease and diabetes mellitus: threats, risks and treatment Alzheimer's disease and diabetes mellitus. Curr Alzheimer Res. (2018) 15:1277–82. doi: 10.2174/1567205015666180925110222
18. Nam GE, Park YG, Han K, Kim MK, Koh ES, Kim ES, et al. BMI, weight change, and dementia risk in patients with new-onset type 2 diabetes: a nationwide cohort study. Diabetes Care. (2019) 42:1217–24. doi: 10.2337/dc18-1667
19. Leibson CL, Rocca WA, Hanson VA, Cha R, Kokmen E, O'Brien PC, et al. Risk of dementia among persons with diabetes mellitus: a population-based cohort study. Am J Epidemiol. (1997) 145:301–8. doi: 10.1093/oxfordjournals.aje.a009106
20. Li T, Cao HX, Ke D. Type 2 diabetes mellitus easily develops into alzheimer's disease via hyperglycemia and insulin resistance. Curr Med Sci. (2021) 41:1165–71. doi: 10.1007/s11596-021-2467-2
21. de la Monte SM. Contributions of brain insulin resistance and deficiency in amyloid-related neurodegeneration in Alzheimer's disease. Drugs. (2012) 72:49–66. doi: 10.2165/11597760-000000000-00000
22. Hu Z, Jiao R, Wang P, Zhu Y, Zhao J, De Jager P, et al. Shared causal paths underlying Alzheimer's dementia and type 2 diabetes. Sci Rep. (2020) 10:4107. doi: 10.1038/s41598-020-60682-3
23. Nisar O, Pervez H, Mandalia B, Waqas M, Sra HK. Type 3 diabetes mellitus: a link between Alzheimer's disease and type 2 diabetes mellitus. Cureus. (2020) 12:e11703. doi: 10.7759/cureus.11703
24. de la Monte SM, Wands JR. Alzheimer's disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol. (2008) 2:1101–13. doi: 10.1177/193229680800200619
25. Kandimalla R, Thirumala V, Reddy PH. Is Alzheimer's disease a type 3 diabetes? A critical appraisal. Biochim Biophys Acta Mol Basis Dis. (2017) 1863:1078–89. doi: 10.1016/j.bbadis.2016.08.018
26. Sun Y, Ma C, Sun H, Wang H, Peng W, Zhou Z, et al. Metabolism: a novel shared link between diabetes mellitus and Alzheimer's disease. J Diabetes Res. (2020) 2020:4981814. doi: 10.1155/2020/4981814
27. Banerjee K, Munshi S, Frank DE, Gibson GE. Abnormal glucose metabolism in Alzheimer's disease: relation to autophagy/mitophagy and therapeutic approaches. Neurochem Res. (2015) 40:2557–69. doi: 10.1007/s11064-015-1631-0
28. Butterfield DA, Halliwell B. Oxidative stress, dysfunctional glucose metabolism and Alzheimer disease. Nat Rev Neurosci. (2019) 20:148–60. doi: 10.1038/s41583-019-0132-6
29. Beal MF. Mitochondria take center stage in aging and neurodegeneration. Ann Neurol. (2005) 58:495–505. doi: 10.1002/ana.20624
30. Wijesekara N, Ahrens R, Sabale M, Wu L, Ha K, Verdile G, et al. Amyloid-β and islet amyloid pathologies link Alzheimer's disease and type 2 diabetes in a transgenic model. FASEB J. (2017) 31:5409–18. doi: 10.1096/fj.201700431R
31. Islam MT. Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol Res. (2017) 39:73–82. doi: 10.1080/01616412.2016.1251711
32. Kiritoshi S, Nishikawa T, Sonoda K, Kukidome D, Senokuchi T, Matsuo T, et al. Reactive oxygen species from mitochondria induce cyclooxygenase-2 gene expression in human mesangial cells: potential role in diabetic nephropathy. Diabetes. (2003) 52:2570–7. doi: 10.2337/diabetes.52.10.2570
33. Wang J, Li L, Zhang Z, Zhang X, Zhu Y, Zhang C, et al. Extracellular vesicles mediate the communication of adipose tissue with brain and promote cognitive impairment associated with insulin resistance. Cell Metab. (2022) 34:1264.e8–79.e8. doi: 10.1016/j.cmet.2022.08.004
34. Ahmed AS, Elgharabawy RM, Al-Najjar AH. Ameliorating effect of anti-Alzheimer's drugs on the bidirectional association between type 2 diabetes mellitus and Alzheimer's disease. Exp Biol Med (Maywood). (2017) 242:1335–44. doi: 10.1177/1535370217711440
35. Ahn KC, Learman CR, Baker GB, Weaver CL, Chung PS, Kim HG, et al. Regulation of diabetes: a therapeutic strategy for Alzheimer's disease? J Korean Med Sci. (2019) 34:e297. doi: 10.3346/jkms.2019.34.e297
36. Campbell JM, Stephenson MD, de Courten B, Chapman I, Bellman SM, Aromataris E. Metformin use associated with reduced risk of dementia in patients with diabetes: a systematic review and meta-analysis. J Alzheimers Dis. (2018) 65:1225–36. doi: 10.3233/jad-180263
37. Koenig AM, Mechanic-Hamilton D, Xie SX, Combs MF, Cappola AR, Xie L, et al. Effects of the insulin sensitizer metformin in Alzheimer disease: pilot data from a randomized placebo-controlled crossover study. Alzheimer Dis Assoc Disord. (2017) 31:107–13. doi: 10.1097/wad.0000000000000202
38. Luchsinger JA, Perez T, Chang H, Mehta P, Steffener J, Pradabhan G, et al. Metformin in amnestic mild cognitive impairment: results of a pilot randomized placebo controlled clinical trial. J Alzheimers Dis. (2016) 51:501–14. doi: 10.3233/jad-150493
39. Ning P, Luo A, Mu X, Xu Y, Li T. Exploring the dual character of metformin in Alzheimer's disease. Neuropharmacology. (2022) 207:108966. doi: 10.1016/j.neuropharm.2022.108966
40. Li YW. Analysis and nursing experience of poor blood sugar control in patients with senile dementia complicated by type 2 diabetes mellitus. Diabetes New World. (2019) 22:136–8. doi: 10.16658/j.cnki.1672-4062.2019.15.136
41. Wu XY, Lin XR, Zhang SX, Tu WZ. Effects of energy intake management on cognitive function in patients with Alzheimer's disease and diabetes mellitus. Gen Pract Clin Educ. (2019) 17:734–6. doi: 10.13558/j.cnki.issn1672-3686.2019.08.020
42. Tang X, Cardoso MA, Yang J, Zhou JB, Simó R. Impact of intensive glucose control on brain health: meta-analysis of cumulative data from 16,584 patients with type 2 diabetes mellitus. Diabetes Ther. (2021) 12:765–79. doi: 10.1007/s13300-021-01009-x
43. Xie L, Pu M, Liu Y. The effect of individual nursing on improving the living ability and blood sugar control of alzheimer disease patients with diabetes mellitus. Am J Translat Res. (2021) 13:9324–31.
44. Chen Y, Wang J, Wang LJ, Lin H, Huang PJ. Effect of different blood glucose intervention plans on elderly people with type 2 diabetes mellitus combined with dementia. Eur Rev Med Pharmacol Sci. (2017) 21:2702–7.
45. Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R, Katabi A, McCoy RG. Hypo-glycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Curr Diab Rep. (2018) 18:53. doi: 10.1007/s11892-018-1018-0
46. Cruz P. Inpatient hypoglycemia: the challenge remains. J Diabetes Sci Technol. (2020) 14:560–6. doi: 10.1177/1932296820918540
48. Cruz P, Blackburn MC, Tobin GS. A systematic approach for the prevention and reduction of hypoglycemia in hospitalized patients. Curr Diab Rep. (2017) 17:117. doi: 10.1007/s11892-017-0934-8
49. Zhong AH. Influence of comprehensive nursing on diabetic patients with Alzheimer's disease. Chin Health Std Manag. (2015) 6:256–8. doi: 10.3969/j.issn.1674-9316.2015.28.193
50. Jin JJ, Cui YJ. Observation on dietary care of type 2 diabetes mellitus by dietary guidance card. Mod Prevent Med. (2007) 45:94–6. doi: 10.3969/j.issn.1003-8507.2007.23.096
51. Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the academy of nutrition and dietetics. Clin Diabetes. (2016) 34:70–80. doi: 10.2337/diaclin.34.2.70
52. Chester B, Babu JR, Greene MW, Geetha T. The effects of popular diets on type 2 diabetes management. Diabetes Metab Res Rev. (2019) 35:e3188. doi: 10.1002/dmrr.3188
53. Bolla AM, Caretto A, Laurenzi A, Scavini M, Piemonti L. Low-carb and ketogenic diets in type 1 and type 2 diabetes. Nutrients. (2019) 11:962. doi: 10.3390/nu11050962
54. Schwingshackl L, Chaimani A, Hoffmann G, Schwedhelm C, Boeing H. A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus. Eur J Epidemiol. (2018) 33:157–70. doi: 10.1007/s10654-017-0352-x
55. Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, Khan T, Kendall CWC, Kahleova H, et al. Mediterranean diet, cardiovascular disease and mortality in diabetes: a systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. (2020) 60:1207–27. doi: 10.1080/10408398.2019.1565281
56. Morris MC, Tangney CC, Wang Y, Sacks FM, Bennett DA, Aggarwal NT. MIND diet associated with reduced incidence of Alzheimer's disease. Alzheimers Dement. (2015) 11:1007–14. doi: 10.1016/j.jalz.2014.11.009
57. van den Brink AC, Brouwer-Brolsma EM, Berendsen AAM, van de Rest O. The mediterranean, dietary approaches to stop hypertension (DASH), and mediterranean-dash intervention for neurodegenerative delay (MIND) diets are associated with less cognitive decline and a lower risk of Alzheimer's disease-a review. Adv Nutr. (2019) 10:1040–65. doi: 10.1093/advances/nmz054
58. Scarmeas N, Anastasiou CA, Yannakoulia M. Nutrition and prevention of cognitive impairment. Lancet Neurol. (2018) 17:1006–15. doi: 10.1016/s1474-4422(18)30338-7
59. Rusek M, Pluta R, Ułamek-Kozioł M, Czuczwar SJ. Ketogenic diet in Alzheimer's disease. Int J Mol Sci. (2019) 20:3892. doi: 10.3390/ijms20163892
60. Morris MC. Nutrition and risk of dementia: overview and methodological issues. Ann N Y Acad Sci. (2016) 1367:31–7. doi: 10.1111/nyas.13047
61. Lotan R, Ravona-Springer R, Shakked J, Lin HM, Ouyang Y, Shahar DR, et al. Greater intake of the medi diet is associated with better cognitive trajectory in older adults with type 2 diabetes. Diabetes Res Clin Pract. (2022) 190:109989. doi: 10.1016/j.diabres.2022.109989
62. Mattei J, Bigornia SJ, Sotos-Prieto M, Scott T, Gao X, Tucker KL. The mediterranean diet and 2-year change in cognitive function by status of type 2 diabetes and glycemic control. Diabetes Care. (2019) 42:1372–9. doi: 10.2337/dc19-0130
63. Martinis I, Vrca A, Bevanda M, Botić-Štefanec S, Badak J, Kušter D, et al. Nutritional assessment of patients with primary progressive dementia at the time of diagnosis. Psychiatr Danub. (2021) 33:226–35.
64. Pistollato F, Iglesias RC, Ruiz R, Aparicio S, Crespo J, Lopez LD, et al. Nutritional patterns associated with the maintenance of neurocognitive functions and the risk of dementia and Alzheimer's disease: a focus on human studies. Pharmacol Res. (2018) 131:32–43. doi: 10.1016/j.phrs.2018.03.012
65. Marcason W. What are the components to the MIND diet? J Acad Nutr Diet. (2015) 115:1744. doi: 10.1016/j.jand.2015.08.002
66. Jannasch F, Kröger J, Schulze MB. Dietary patterns and type 2 diabetes: a systematic literature review and meta-analysis of prospective studies. J Nutr. (2017) 147:1174–82. doi: 10.3945/jn.116.242552
67. Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC. The dietary approaches to stop hypertension eating plan affects c-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr. (2011) 141:1083–8. doi: 10.3945/jn.110.136739
68. Anastasiou CA, Yannakoulia M, Kosmidis MH, Dardiotis E, Hadjigeorgiou GM, Sakka P, et al. Mediterranean diet and cognitive health: initial results from the hellenic longitudinal investigation of ageing and diet. PLoS ONE. (2017) 12:e0182048. doi: 10.1371/journal.pone.0182048
69. Asemi Z, Tabassi Z, Samimi M, Fahiminejad T, Esmaillzadeh A. Favourable effects of the dietary approaches to stop hypertension diet on glucose tolerance and lipid profiles in gestational diabetes: a randomised clinical trial. Br J Nutr. (2013) 109:2024–30. doi: 10.1017/s0007114512004242
70. Veech RL. The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot Essent Fatty Acids. (2004) 70:309–19. doi: 10.1016/j.plefa.2003.09.007
71. Takeishi J, Tatewaki Y, Nakase T, Takano Y, Tomita N, Yamamoto S, et al. Alzheimer's disease and type 2 diabetes mellitus: the use of mct oil and a ketogenic diet. Int J Mol Sci. (2021) 22:12310. doi: 10.3390/ijms222212310
72. Hu Yang I, De la Rubia Ortí JE, Selvi Sabater P, Sancho Castillo S, Rochina MJ, Manresa Ramón N, et al. [Coconut oil: non-alternative drug treatment against Alzheimer's disease]. Nutr Hosp. (2015) 32:2822–7. doi: 10.3305/nh.2015.32.6.9707
73. Brinkworth GD, Luscombe-Marsh ND, Thompson CH, Noakes M, Buckley JD, Wittert G, et al. Long-term effects of very low-carbohydrate and high-carbohydrate weight-loss diets on psychological health in obese adults with type 2 diabetes: randomized controlled trial. J Intern Med. (2016) 280:388–97. doi: 10.1111/joim.12501
74. Abboud M, AlAnouti F, Georgaki E, Papandreou D. Effect of ketogenic diet on quality of life in adults with chronic disease: a systematic review of randomized controlled trials. Nutrients. (2021) 13:4463. doi: 10.3390/nu13124463
75. Lilamand M, Porte B, Cognat E, Hugon J, Mouton-Liger F, Paquet C. Are ketogenic diets promising for Alzheimer's disease? A translational review. Alzheimers Res Ther. (2020) 12:42. doi: 10.1186/s13195-020-00615-4
76. Carranza-Naval MJ, Vargas-Soria M, Hierro-Bujalance C, Baena-Nieto G, Garcia-Alloza M, Infante-Garcia C, et al. Alzheimer's disease and diabetes: role of diet, microbiota and inflammation in preclinical models. Biomolecules. (2021) 11:262. doi: 10.3390/biom11020262
77. Zhong SR, Kuang Q, Zhang F, Chen B, Zhong ZG. Functional roles of the microbiota-gut-brain axis in Alzheimer's disease: implications of gut microbiota-targeted therapy. Transl Neurosci. (2021) 12:581–600. doi: 10.1515/tnsci-2020-0206
78. Sánchez B, Delgado S, Blanco-Míguez A, Lourenço A, Gueimonde M, Margolles A. Probiotics, gut microbiota, and their influence on host health and disease. Mol Nutr Food Res. (2017) 61:201600240. doi: 10.1002/mnfr.201600240
79. Luca M, Di Mauro M, Di Mauro M, Luca A. Gut microbiota in Alzheimer's disease, depression, and type 2 diabetes mellitus: the role of oxidative stress. Oxid Med Cell Longev. (2019) 2019:4730539. doi: 10.1155/2019/4730539
80. Yan F, Li N, Shi J, Li H, Yue Y, Jiao W, et al. Lactobacillus acidophilus alleviates type 2 diabetes by regulating hepatic glucose, lipid metabolism and gut microbiota in mice. Food Funct. (2019) 10:5804–15. doi: 10.1039/c9fo01062a
81. Li K, Zhang L, Xue J, Yang X, Dong X, Sha L, et al. Dietary inulin alleviates diverse stages of type 2 diabetes mellitus via anti-inflammation and modulating gut microbiota in db/db mice. Food Funct. (2019) 10:1915–27. doi: 10.1039/c8fo02265h
82. Akbari E, Asemi Z, Daneshvar Kakhaki R, Bahmani F, Kouchaki E, Tamtaji OR, et al. Effect of probiotic supplementation on cognitive function and metabolic status in Alzheimer's disease: a randomized, double-blind and controlled trial. Front Aging Neurosci. (2016) 8:256. doi: 10.3389/fnagi.2016.00256
83. Téglás T, Ábrahám D, Jókai M, Kondo S, Mohammadi R, Fehér J, et al. Exercise combined with a probiotics treatment alters the microbiome, but moderately affects signalling pathways in the liver of male APP/PS1 transgenic mice. Biogerontology. (2020) 21:807–15. doi: 10.1007/s10522-020-09895-7
84. Biyong EF, Tremblay C, Leclerc M, Caron V, Alfos S, Helbling JC, et al. Role of retinoid x receptors (RXRS) and dietary vitamin A in Alzheimer's disease: evidence from clinicopathological and preclinical studies. Neurobiol Dis. (2021) 161:105542. doi: 10.1016/j.nbd.2021.105542
85. Su L, He J, Liu Z, Wu S, Chen P, Li K, et al. Dietary total vitamin A, β-carotene, and retinol intake and the risk of diabetes in chinese adults with plant-based diets. J Clin Endocrinol Metab. (2022) 107:e4106–14. doi: 10.1210/clinem/dgac439
86. Sun H, Karp J, Sun KM, Weaver CM. Decreasing vitamin C intake, low serum vitamin C level and risk for us adults with diabetes. Nutrients. (2022) 14:3902. doi: 10.3390/nu14193902
87. Basambombo LL, Carmichael PH, Côté S, Laurin D. Use of vitamin E and C supplements for the prevention of cognitive decline. Ann Pharmacother. (2017) 51:118–24. doi: 10.1177/1060028016673072
88. Chang E, Kim Y. Vitamin D decreases adipocyte lipid storage and increases nad-SIRT1 pathway in 3T3-L1 adipocytes. Nutrition. (2016) 32:702–8. doi: 10.1016/j.nut.2015.12.032
89. Wenclewska S, Szymczak-Pajor I, Drzewoski J, Bunk M, Sliwińska A. Vitamin D supplementation reduces both oxidative DNA damage and insulin resistance in the elderly with metabolic disorders. Int J Mol Sci. (2019) 20:2891. doi: 10.3390/ijms20122891
90. Dickens AP, Lang IA, Langa KM, Kos K, Llewellyn DJ. Vitamin D, cognitive dysfunction and dementia in older adults. CNS Drugs. (2011) 25:629–39. doi: 10.2165/11593080-000000000-00000
91. Feart C, Helmer C, Merle B, Herrmann FR, Annweiler C, Dartigues JF, et al. Associations of lower vitamin d concentrations with cognitive decline and long-term risk of dementia and Alzheimer's disease in older adults. Alzheimers Dement. (2017) 13:1207–16. doi: 10.1016/j.jalz.2017.03.003
92. Geng T, Lu Q, Wan Z, Guo J, Liu L, Pan A, et al. Association of serum 25-hydroxyvitamin D concentrations with risk of dementia among individuals with type 2 diabetes: a cohort study in the UK BioBank. PLoS Med. (2022) 19:e1003906. doi: 10.1371/journal.pmed.1003906
93. Quadri P, Fragiacomo C, Pezzati R, Zanda E, Forloni G, Tettamanti M, et al. Homocysteine, folate, and vitamin B-12 in mild cognitive impairment, Alzheimer disease, and vascular dementia. Am J Clin Nutr. (2004) 80:114–22. doi: 10.1093/ajcn/80.1.114
94. Smith AD. The worldwide challenge of the dementias: a role for B vitamins and homocysteine? Food Nutr Bull. (2008) 29:S143–72. doi: 10.1177/15648265080292s119
95. Van Dam F, Van Gool WA. Hyperhomocysteinemia and Alzheimer's disease: a systematic review. Arch Gerontol Geriatr. (2009) 48:425–30. doi: 10.1016/j.archger.2008.03.009
96. Škovierová H, Vidomanová E, Mahmood S, Sopková J, Drgová A, Cervenová T, et al. The molecular and cellular effect of homocysteine metabolism imbalance on human health. Int J Mol Sci. (2016) 17:1733. doi: 10.3390/ijms17101733
97. Kim J, Kim H, Roh H, Kwon Y. Causes of hyperhomocysteinemia and its pathological significance. Arch Pharm Res. (2018) 41:372–83. doi: 10.1007/s12272-018-1016-4
98. Cacciapuoti F. Lowering homocysteine levels with folic acid and B-vitamins do not reduce early atherosclerosis, but could interfere with cognitive decline and Alzheimer's disease. J Thromb Thrombolysis. (2013) 36:258–62. doi: 10.1007/s11239-012-0856-x
99. Mutavdzin S, Gopcevic K, Stankovic S, Jakovljevic Uzelac J, Labudovic Borovic M, Djuric D. The effects of folic acid administration on cardiac oxidative stress and cardiovascular biomarkers in diabetic rats. Oxid Med Cell Longev. (2019) 2019:1342549. doi: 10.1155/2019/1342549
100. Chen H, Liu S, Ji L, Wu T, Ji Y, Zhou Y, et al. Folic acid supplementation mitigates Alzheimer's disease by reducing inflammation: a randomized controlled trial. Mediators Inflamm. (2016) 2016:5912146. doi: 10.1155/2016/5912146
101. Malouf M, Grimley EJ, Areosa SA. Folic acid with or without vitamin B12 for cognition and dementia. Cochrane Database Syst Rev. (2003) 4:Cd004514. doi: 10.1002/14651858.Cd004514
102. Sun Y, Lu CJ, Chien KL, Chen ST, Chen RC. Efficacy of multivitamin supplementation containing vitamins B6 and B12 and folic acid as adjunctive treatment with a cholinesterase inhibitor in Alzheimer's disease: a 26-week, randomized, double-blind, placebo-controlled study in Taiwanese patients. Clin Ther. (2007) 29:2204–14. doi: 10.1016/j.clinthera.2007.10.012
103. Gargari BP, Aghamohammadi V, Aliasgharzadeh A. Effect of folic acid supplementation on biochemical indices in overweight and obese men with type 2 diabetes. Diabetes Res Clin Pract. (2011) 94:33–8. doi: 10.1016/j.diabres.2011.07.003
104. Jack CR Jr, Shiung MM, Gunter JL, O'Brien PC, Weigand SD, Knopman DS, et al. Comparison of different MRI brain atrophy rate measures with clinical disease progression in AD. Neurology. (2004) 62:591–600. doi: 10.1212/01.wnl.0000110315.26026.ef
105. Smith AD, Smith SM, de Jager CA, Whitbread P, Johnston C, Agacinski G, et al. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PLoS ONE. (2010) 5:e12244. doi: 10.1371/journal.pone.0012244
106. Jernerén F, Elshorbagy AK, Oulhaj A, Smith SM, Refsum H, Smith AD. Brain atrophy in cognitively impaired elderly: the importance of long-chain ω-3 fatty acids and B vitamin status in a randomized controlled trial. Am J Clin Nutr. (2015) 102:215–21. doi: 10.3945/ajcn.114.103283
107. Farina N, Jernerén F, Turner C, Hart K, Tabet N. Homocysteine concentrations in the cognitive progression of Alzheimer's disease. Exp Gerontol. (2017) 99:146–50. doi: 10.1016/j.exger.2017.10.008
108. Szkudelski T, Szkudelska K. Resveratrol and diabetes: from animal to human studies. Biochim Biophys Acta. (2015) 1852:1145–54. doi: 10.1016/j.bbadis.2014.10.013
109. Kulashekar M, Stom SM, Peuler JD. Resveratrol's potential in the adjunctive management of cardiovascular disease, obesity, diabetes, Alzheimer disease, and cancer. J Am Osteopath Assoc. (2018) 118:596–605. doi: 10.7556/jaoa.2018.133
110. Zhang W, Yu H, Lin Q, Liu X, Cheng Y, Deng B. Anti-inflammatory effect of resveratrol attenuates the severity of diabetic neuropathy by activating the Nrf2 pathway. Aging (Albany NY). (2021) 13:10659–71. doi: 10.18632/aging.202830
111. Ma X, Sun Z, Han X, Li S, Jiang X, Chen S, et al. Neuroprotective effect of resveratrol via activation of SIRT1 signaling in a rat model of combined diabetes and Alzheimer's disease. Front Neurosci. (2019) 13:1400. doi: 10.3389/fnins.2019.01400
112. Movahed A, Nabipour I, Lieben Louis X, Thandapilly SJ Yu L, Kalantarhormozi M, et al. Antihyperglycemic effects of short term resveratrol supplementation in type 2 diabetic patients. Evid Based Complement Alternat Med. (2013) 2013:851267. doi: 10.1155/2013/851267
113. Jia JJ, Zeng XS, Song XQ, Zhang PP, Chen L. Diabetes mellitus and Alzheimer's disease: the protection of epigallocatechin-3-gallate in streptozotocin injection-induced models. Front Pharmacol. (2017) 8:834. doi: 10.3389/fphar.2017.00834
114. Bassiony HS, Zickri MB, Metwally HG, Elsherif HA, Alghandour SM, Sakr W. Comparative histological study on the therapeutic effect of green tea and stem cells in Alzheimer's disease complicating experimentally induced diabetes. Int J Stem Cells. (2015) 8:181–90. doi: 10.15283/ijsc.2015.8.2.181
115. Qin B, Panickar KS, Anderson RA. Cinnamon: potential role in the prevention of insulin resistance, metabolic syndrome, and type 2 diabetes. J Diabetes Sci Technol. (2010) 4:685–93. doi: 10.1177/193229681000400324
116. Lee MS, Wahlqvist ML, Chou YC, Fang WH, Lee JT, Kuan JC, et al. Turmeric improves post-prandial working memory in pre-diabetes independent of insulin. Asia Pac J Clin Nutr. (2014) 23:581–91. doi: 10.6133/apjcn.2014.23.4.24
117. Thota RN, Rosato JI, Dias CB, Burrows TL, Martins RN, Garg ML. Dietary supplementation with curcumin reduce circulating levels of glycogen synthase kinase-3β and islet amyloid polypeptide in adults with high risk of type 2 diabetes and Alzheimer's disease. Nutrients. (2020) 12:1032. doi: 10.3390/nu12041032
118. Abdulmalek S, Nasef M, Awad D, Balbaa M. Protective effect of natural antioxidant, curcumin nanoparticles, and zinc oxide nanoparticles against type 2 diabetes-promoted hippocampal neurotoxicity in rats. Pharmaceutics. (2021) 13:1937. doi: 10.3390/pharmaceutics13111937
119. Khan MS, Ikram M, Park TJ, Kim MO. Pathology, risk factors, and oxidative damage related to type 2 diabetes-mediated Alzheimer's disease and the rescuing effects of the potent antioxidant anthocyanin. Oxid Med Cell Longev. (2021) 2021:4051207. doi: 10.1155/2021/4051207
120. Wagle A, Seong SH, Shrestha S, Jung HA, Choi JS. Korean thistle (Cirsium japonicum var. maackii (Maxim.) Matsum.): a potential dietary supplement against diabetes and Alzheimer's disease. Molecules. (2019) 24:649. doi: 10.3390/molecules24030649
121. Lai MC, Liu WY, Liou SS, Liu IM. The citrus flavonoid hesperetin encounters diabetes-mediated Alzheimer-type neuropathologic changes through relieving advanced glycation end-products inducing endoplasmic reticulum stress. Nutrients. (2022) 14:745. doi: 10.3390/nu14040745
122. Li RZ, Ding XW, Geetha T, Al-Nakkash L, Broderick TL, Babu JR. Beneficial effect of genistein on diabetes-induced brain damage in the ob/ob mouse model. Drug Des Devel Ther. (2020) 14:3325–36. doi: 10.2147/dddt.S249608
123. Gomaa AA, Makboul RM, Al-Mokhtar MA, Nicola MA. Polyphenol-rich Boswellia serrata gum prevents cognitive impairment and insulin resistance of diabetic rats through inhibition of GSK3β activity, oxidative stress and pro-inflammatory cytokines. Biomed Pharmacother. (2019) 109:281–92. doi: 10.1016/j.biopha.2018.10.056
124. Infante-Garcia C, Jose Ramos-Rodriguez J, Marin-Zambrana Y, Teresa Fernandez-Ponce M, Casas L, Mantell C, et al. Mango leaf extract improves central pathology and cognitive impairment in a type 2 diabetes mouse model. Brain Pathol. (2017) 27:499–507. doi: 10.1111/bpa.12433
125. Ben Hmidene A, Hanaki M, Murakami K, Irie K, Isoda H, Shigemori H. Inhibitory activities of antioxidant flavonoids from tamarix gallica on amyloid aggregation related to Alzheimer's and type 2 diabetes diseases. Biol Pharm Bull. (2017) 40:238–41. doi: 10.1248/bpb.b16-00801
126. de Bock M, Derraik JG, Brennan CM, Biggs JB, Morgan PE, Hodgkinson SC, et al. Olive (Olea europaea L) leaf polyphenols improve insulin sensitivity in middle-aged overweight men: a randomized, placebo-controlled, crossover trial. PLoS ONE. (2013) 8:e57622. doi: 10.1371/journal.pone.0057622
127. Silveira AC, Dias JP, Santos VM, Oliveira PF, Alves MG, Rato L, et al. The action of polyphenols in diabetes mellitus and Alzheimer's disease: a common agent for overlapping pathologies. Curr Neuropharmacol. (2019) 17:590–613. doi: 10.2174/1570159x16666180803162059
128. Li W, Wang G, Lu X, Jiang Y, Xu L, Zhao X. Lycopene ameliorates renal function in rats with streptozotocin-induced diabetes. Int J Clin Exp Pathol. (2014) 7:5008–15.
129. Yu L, Wang W, Pang W, Xiao Z, Jiang Y, Hong Y. Dietary lycopene supplementation improves cognitive performances in tau transgenic mice expressing P301L mutation via inhibiting oxidative stress and tau hyperphosphorylation. J Alzheimers Dis. (2017) 57:475–82. doi: 10.3233/jad-161216
130. Gunasekara P, Hettiarachchi M, Liyanage C, Lekamwasam S. Effects of zinc and multimineral vitamin supplementation on glycemic and lipid control in adult diabetes. Diabetes Metab Syndr Obes. (2011) 4:53–60. doi: 10.2147/dmso.S16691
131. Barbagallo M, Dominguez LJ, Galioto A, Pineo A, Belvedere M. Oral magnesium supplementation improves vascular function in elderly diabetic patients. Magnes Res. (2010) 23:131–7. doi: 10.1684/mrh.2010.0214
132. Agrawal R, Gomez-Pinilla F. ‘Metabolic syndrome' in the brain: deficiency in omega-3 fatty acid exacerbates dysfunctions in insulin receptor signalling and cognition. J Physiol. (2012) 590:2485–99. doi: 10.1113/jphysiol.2012.230078
133. Szuster-Ciesielska A, Plewka K, Daniluk J, Kandefer-Szerszeń M. Betulin and betulinic acid attenuate ethanol-induced liver stellate cell activation by inhibiting reactive oxygen species (ROS), cytokine (TNF-α, TGF-β) production and by influencing intracellular signaling. Toxicology. (2011) 280:152–63. doi: 10.1016/j.tox.2010.12.006
134. Hashmi WJ, Ismail H, Mehmood F, Mirza B. Neuroprotective, antidiabetic and antioxidant effect of hedera nepalensis and lupeol against STZ + ALCL(3) induced rats model. Daru. (2018) 26:179–90. doi: 10.1007/s40199-018-0223-3
135. Lee SH, Jeon YJ. Efficacy and safety of a dieckol-rich extract (ag-dieckol) of brown algae, ecklonia cava, in pre-diabetic individuals: a double-blind, randomized, placebo-controlled clinical trial. Food Funct. (2015) 6:853–8. doi: 10.1039/c4fo00940a
136. Ergül M, Ergül M, Eruygur N, Ataş M, Uçar E. In vitro evaluation of the chemical composition and various biological activities of Ficus carica leaf extracts. Turk J Pharm Sci. (2019) 16:401–9. doi: 10.4274/tjps.galenos.2018.70037
Keywords: nutritional intervention, dietary patterns, diabetes mellitus, Alzheimer's disease, review
Citation: Li Z, Li S, Xiao Y, Zhong T, Yu X and Wang L (2022) Nutritional intervention for diabetes mellitus with Alzheimer's disease. Front. Nutr. 9:1046726. doi: 10.3389/fnut.2022.1046726
Received: 17 September 2022; Accepted: 31 October 2022;
Published: 15 November 2022.
Edited by:
Zhiping Yu, University of North Florida, United StatesReviewed by:
Gonzalo Emiliano Aranda-Abreu, Universidad Veracruzana, MexicoMin Chen, Icahn School of Medicine at Mount Sinai, United States
Yuxia Ouyang, Icahn School of Medicine at Mount Sinai, United States
Copyright © 2022 Li, Li, Xiao, Zhong, Yu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Wang, bGluZ3dhbmdAbXVzdC5lZHUubW8=
 Zhi Li
Zhi Li Simian Li
Simian Li Xi Yu
Xi Yu Ling Wang
Ling Wang