
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 08 December 2022
Sec. Nutrition and Sustainable Diets
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1023046
This article is part of the Research Topic Key nutrition and hydration insights for Public Health and Policy View all 26 articles
Background: In developing countries, including Ethiopia, maternal mortality is a major public health concern. The Ethiopian Demographic Health Survey (EDHS) reported that the maternal mortality ratio (MMR) was 420 per 100,000 live births in 2016. Iron-folic acid supplementation (IFAS) is a key intervention to reduce these deaths. Therefore, this study aimed to assess the magnitude of poor adherence to IFAS and associated factors among pregnant women who had at least four antenatal care in Ethiopia.
Methods: Secondary data analysis was used using 2016 Ethiopian Demographic and Health Survey (EDHS). We analyzed the data using Stata version 14. To identify factors associated with poor adherence to IFAS, a multilevel mixed-effect logistic regression model was fitted. Variables with a p < 0.05 in the multilevel mixed-effect logistic regression model were declared as significant factors associated with poor adherence to IFAS.
Result: The magnitude of poor adherence to IFAS was 82.87% (95% CI: 80.96–84.65). Women education; primary [adjusted odds ratio (AOR) = 0.48; 95% CI: 0.31–0.75] and secondary (AOR = 0.52; 95% CI: 0.29–0.96), husband education; primary (AOR = 0.56; 95% CI: 0.36–0.86) and secondary (AOR = 0.51; 95% CI: 0.29–0.95), and community media exposure (AOR = 0.47; 95% CI: 0.27–0.79) were significantly associated with poor adherence to IFAS.
Conclusion: In the current study, more than eight out of ten pregnant women who had at least four antenatal care had poor adherence to IFAS. Thus, promoting maternal and husband education and establishing community media with a priority on iron-folic acid supplementation and health-related programs are essential strategies to reduce poor adherence to IFAS.
The nutritional status of the mother during pregnancy has a significant impact on the health, development, and wellbeing of the child (1). Anemia is associated with maternal and infant morbidity and mortality during pregnancy since iron stores decrease and iron requirements increase (2). Anemia affects 38.2% of pregnant mothers worldwide, with Africa contributing 44.6%. Iron deficiency contributes to half of all anemia cases (3). Furthermore, more than one-fifth of maternal mortality in Sub-Saharan Africa (SSA) is indirectly attributable to anemia (4).
Iron deficiency is the major cause of anemia globally, particularly in SSA (5). Both the mother and the fetus can suffer from iron deficiency anemia during pregnancy (6). Preterm delivery, spontaneous abortion, low birth weight, and fetal distress are associated with anemia (6, 7).
Globally, anemia reduction is the second nutritional goal for 2025 and is a key component of achieving women's and children's health. The goal is to reduce anemia in women of reproductive age by 50% (8). Iron-folic acid supplementation (IFAS) is one of the most important interventions to reduce anemia among pregnant women (3, 8). A daily supplement containing 60 mg of elemental iron with 400 micrograms of folic acid is recommended for pregnant women by the World Health Organization (WHO) for 6 months (9). IFAS should be continued for three months postpartum in areas with high anemia prevalence (9). Furthermore, Ethiopia's national guideline for preventing and controlling micronutrient deficiency recommends taking IFAS daily for 6 months during pregnancy and 3 months after delivery (10). The Ethiopian national nutrition program (NNP II) also set a key target to increase the number of women receiving iron-folic acid supplements for more than 90 days during pregnancy to 50% by 2024 and 90% by 2029 (11, 12).
The poor adherence to IFAS varies across different settings, for instance, in urban and rural areas of Tigray, Ethiopia was 62.8 and 71.1%, respectively (13), Northeast, Ethiopia 52.4% (14), Shire refugee camps, Northern Ethiopia 35.3 (15), Tikur Anbessa Specialized Hospital, Ethiopia 36.4% (16), systematic review and meta-analysis in Ethiopia 58.6% (17), Tanzania 79.7% (18), and SSA 71.3% (19). Some of the identified factors that can affect poor adherence to IFAS include the age of the women, previous anemia, educational status, wealth index, knowledge about anemia, receiving counseling about nutrition, and husband support (13, 15, 17, 19–21).
The magnitude of anemia has persistently increased despite many efforts to fight it over the past three decades, including free provision of IFAS of mothers and the promotion of ANC. This can be supported by the evidence of EDHS, which found that the magnitude of anemia among reproductive-age women increased from 17% in 2011 to 24% in 2016. Only 5% of reproductive age women adhere to IFAS during their most recent pregnancy (22). Furthermore, various studies have been conducted in Ethiopia about IFAS (6, 7, 23–25). However, the majority of these focused on the effects of IFAS in newborns and pregnant women and only a limited number of studies assessed the adherence to IFAS and associated factors among pregnant women in Ethiopia. Nevertheless, there was no adequate literature that answered the reason why pregnant women who attended the recommended ANC had poor adherence to IFAS in the country. Therefore, this study aimed to determine the magnitude of poor IFAS and tried to explore factors determining adherence to IFAS among pregnant women who had at least four ANC.
This study used data from the most recent Ethiopia Demographic and Health Surveys (EDHS). EDHS is a nationally representative household survey conducted every 5 years in low- and middle-income countries (26). Using the women's recode (IR file) data set, we extracted independent and dependent variables. The dataset is freely available for download at: https://dhsprogram.com/data/available-datasets.cfm.
The EDHS employs two-stage stratified sampling technique. Which makes the data nationally representatives (7). A total weighted sample of 1,606 pregnant women within 5 years before the survey who had at least four antenatal care (ANC) were included in the study (Figure 1).
The outcome variable for this study was poor adherence to iron-folic acid supplementation. It was defined as not using iron-folic acid supplementation for ≥90 days during the pregnancy of the most recent birth. This was measured in the DHS data by the number of days when iron supplements (tablets) were taken as part of antenatal care. The poor adherence of <90 days threshold was chosen in accordance with previous studies (19, 27, 28).
In this study, individual and community-level factors that are associated with poor adherence to IFAS were considered. Individual level factors considered in the analysis were age (15–24, 25–34, and 35–49), women education (no formal education, primary education, and secondary and above), husband education (no formal education, primary education, and secondary and above), occupation of the respondents (employed, non-employed), wealth index (poor, middle, and rich), nutrition counseling (yes, no), and religion (Orthodox, Muslim, protestant, and catholic). Regarding media exposure (yes, no), we coded yes if the women read newspaper, listened radio, or watched television for at least once a week, and no for otherwise (7).
Of the community level variables, region (small peripheral, large central, and metropolitan) and place of residences (rural, urban) were directly accessed from DHS data sets. However, community media exposure (low, high) and community-level education (low, high) were constructed by aggregating individual-level characteristics at the cluster level. They were categorized as high or low based on the distribution of the proportion values computed for each community after checking the distribution by using the histogram. The aggregate variable was not normally distributed, and the median value was used as a cut-off point for the categorization (29, 30).
Data analysis was performed using Stata version 14. Before data analysis, all frequency distributions were weighted (v005/1000000) to ensure that the DHS sample was representative and to obtain accurate estimates and standard errors. In order to account for the hierarchical nature of the DHS data, a multi-level logistic regression analysis was conducted. First, bivariable multilevel logistic regression analysis was conducted and those variables with a p < 0.2 were considered for multivariable analysis.
After selecting variables for multivariable analysis, four models were fitted; null model (Model 0) which shows the variations in the poor adherence to IFAS in the absence of any independent variables. Model I adjusted for the individual-level variables, Model II adjusted for the community level variables and Model III adjusted for both individual and community level variables. Simultaneously, Model fitness was done using the deviance since these models were nested (20). In addition, Variance inflation factors (VIFs) were used to test for multicollinearity. Each independent variable had a VIF < 5, with a mean VIF of 1.84, indicating no significant multicollinearity. AORs were presented with a 95% confidence interval.
A total weighted sample of 1,606 pregnant women were included in this analysis. The median age of the study participants was 28 years (IQR: 24–33) and 73.49% of the women were rural dwellers. Nearly half (48.31%) of the pregnant women had no formal education. Of the study participants, 49.19% were employed and 50.81 % had media exposure. The majority (88.07%) of the pregnant women were from large central regions. More than half (52.87%) of the pregnant women were from households with rich wealth quantiles (Table 1).
The magnitude of poor adherence to IFAS in Ethiopia was 82.87% (95% CI: 80.96–84.65).
The poor adherence to IFAS varied significantly across clusters. In the baseline model without an independent variable, 26.23 % of the variance in poor adherence to IFAS was explained by the variation in characteristics between clusters (ICC = 0.2623). In model 3, which included both individual and community level factors, the between-cluster variation, was reduced to 24.43%. Accordingly, the variance in IFAS adherence could be explained by differences in clusters. Model 3, which incorporated both individual and community-level factors, exhibited the best goodness of fit for predicting poor adherence to IFAS. The final model was selected because it has the lowest (1,250.90) deviance as compared with the other models (Table 2).
In the multilevel multivariable logistic regression model, both the individual and community level factors were fitted simultaneously. Thus, women education, husband education, and community media exposure were statistically associated with poor adherence to IFAS at 95% confidence level.
This study showed that pregnant women attended primary and secondary education and above were 52% (AOR = 0.48; 95% CI: 0.31–0.75) and 48% (AOR = 0.52; 95% CI: 0.29–0.96) less likely to have poor adherence to IFAS compared to women with no formal education, respectively. Women with husband education attended primary and secondary education and above were 44% (AOR = 0.56; 95% CI: 0.36–0.86) and 49% (AOR = 0.51; 95% CI: 0.29–0.95) less likely to have poor adherence to IFAS compared to their counterparts, respectively. The odds of poor adherence to IFAS in the community with high media exposure were 53% (AOR = 0.47; 95% CI: 0.27–0.79) low compared to their counterparts (Table 3).
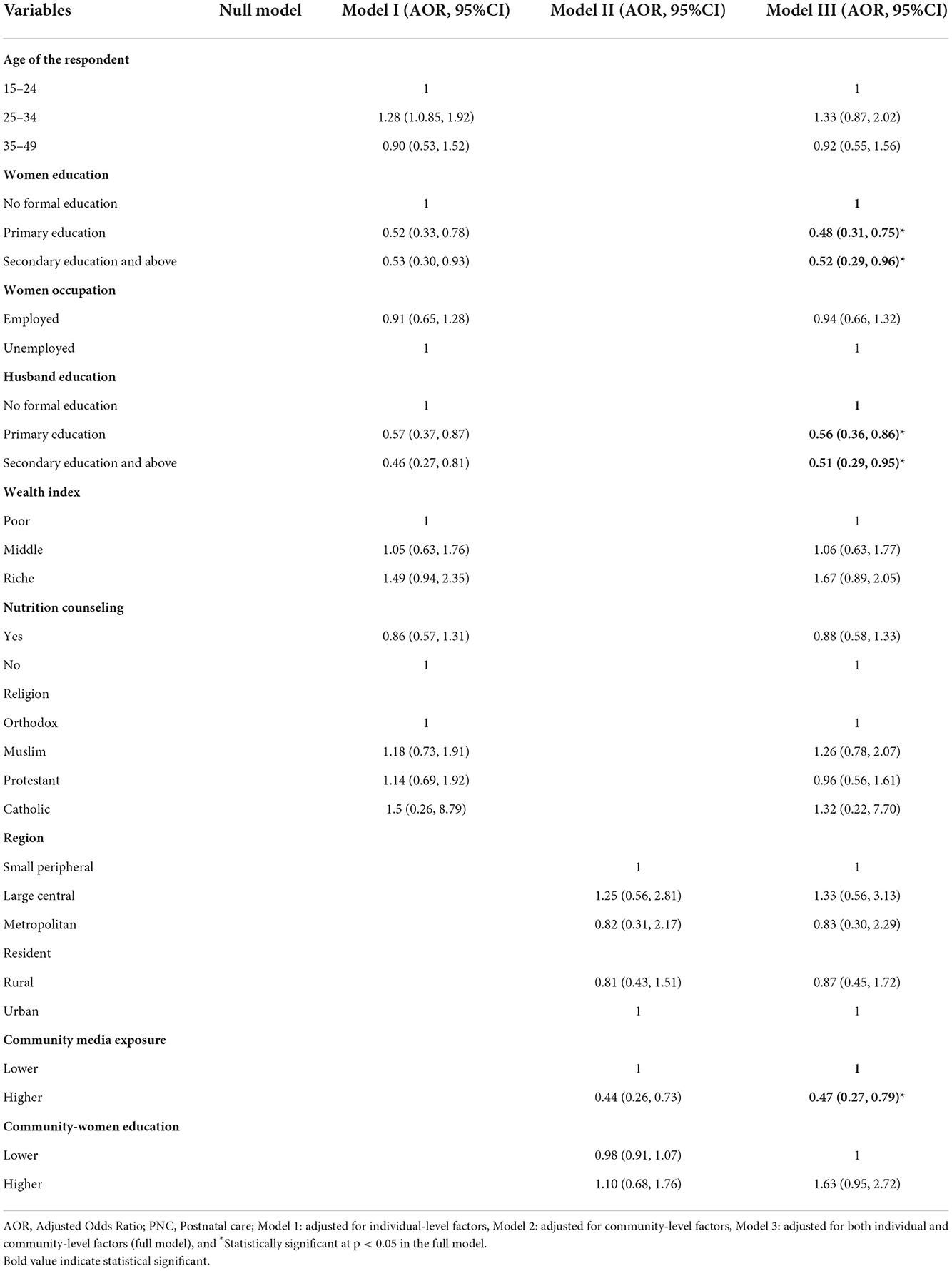
Table 3. Multivariable multilevel logistic regression model results of poor adherence to IFAS in Ethiopia.
The aim of this study was to determine poor adherence to IFAS and identify associated factors among pregnant women who had at least four ANC. This study found that 82.87% (95% CI: 80.96–84.65) of pregnant women who had at least four ANC had poor adherence to IFAS. The result of the study found that women's education, husband's education, and community-level media exposure were identified as the factors associated with poor adherence to IFAS.
The current study is lower than a study conducted in Ethiopia 87.6% (7). The possible explanation might be the difference in the study population. The current study exclusively included pregnant women who received the recommended ANC, whereas the previous study included pregnant women who were asked how many days they consumed IFA tablets regardless of the number of ANC visits (7). Women who received the recommended ANC visits had better knowledge about anemia compared to those who did not receive the recommended ANC visits (31). Previous studies have documented that ANC visits and knowledge of anemia have a negative relationship with poor adherence to IFAS (7, 23–25, 32). However, this finding is higher than that of studies conducted in Ethiopia (23–25, 33–35), Tanzania 79.7% (18), and sub-Saharan African countries 71.3% (19). The possible explanation could be because of the difference in the study setting, the quality of service delivery in the health institutions, socio-demographic differences, and women's awareness of the importance of IFAS during pregnancy. For example, the previous studies done in Ethiopia were small-scale surveys compared to the EDHS survey, which was a national representative survey and included developing regions. Regarding socio-demographic variation, a previous study done in SSA reported that only 34.4% of the pregnant women had no formal education, which was lower than that of the current study (48.3%). Previous research has shown that women's education has a negative relationship with poor adherence to IFAS (21, 24, 36). Furthermore, the reason could also be the difference in access to health institutions and the availability of IFA in the nearby health facilities (7).
Pregnant women with primary education and secondary education and above were decreases poor adherence to IFAS by 52 and 48% as compared to those with no formal education, respectively. This result is in line with previous studies done in Ethiopia (24, 36), and Indonesia (37). Educated women are better informed about iron deficiency anemia and therapy, supplement benefits, and pregnancy in general. In addition, education may enhance awareness of micronutrient deficiency and ways to overcome it (7, 38).
Pregnant women with husband education who had formal education were less likely to have poor adherence to iron supplementation than those pregnant women with husbands who had no formal education. The finding is consistent with other study done in Ethiopia (39). This might be due to mothers with husband who were educated were autonomous on utilization of iron supplementation without the consent of their husbands.
Community media exposure is also negatively affected with poor adherence to IFAS. This study was supported by studies conducted in Ethiopia (40), and Asia (41). This is because different maternal and child health services including the importance of iron-folic acid supplementation during pregnancy are frequently given to the community through mass media. Therefore, pregnant women who are exposed to community media would have better understanding of the advantages of IFAS during pregnancy compared to those who do not have community media exposure (40).
This study used nationally representative data sets, which were collected with a standardized and validated data collection tools. A multilevel analysis was used in this study to account for the hierarchical nature of the data. The cross-sectional nature of the survey does not show the causal relationship between outcome and independent variables. Furthermore, due to the use of secondary data, essential factors like knowledge of anemia, and socio-cultural factors were not available in the EDHS data set, hence, they were not included in the analyzed.
In the current study, more than eight out of ten pregnant women who had at least four antenatal care had poor adherence to iron-folic supplementation. Thus, promoting maternal and husband education and establishing community media with a priority on iron-folic acid supplementation and health-related programs are essential strategies to reduce poor adherence to iron-folic acid supplementation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements.
DA conceived the idea, extract the data, data analysis, and draft the manuscript. WD, TB, and DB participant in the data analysis, interpretation, and revising of the manuscript. The final manuscript has been read and approved by all authors.
Our gratitude is extended to the DHS programs for allowing us to use all of the relevant DHS data in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Christian P, Mullany LC, Hurley K, Katz J, Black R. Erratum to “Nutrition and maternal, neonatal, and child health” [Semin Perinatol (2015) 39:361–372]. Semin Perinatol. (2015) 2015:505. doi: 10.1053/j.semperi.2015.09.001
2. Harvey T, Zkik A, Auges M, Clavel T. Assessment of iron deficiency and anemia in pregnant women: an observational French study. Women's Health. (2016) 12:95–102. doi: 10.2217/whe.15.91
3. World Health Organization. WHO Global Anaemia Estimates, 2021 Edition. Anaemia in Women and Children. (2021). Available online at: https://www.who.int/data/gho/data/themes/topics/anaemia_in_women_and_children (accessed February 18, 2022).
5. Zegeye B, Anyiam FE, Ahinkorah BO, Ameyaw EK, Budu E, Seidu A-A, et al. Prevalence of anemia and its associated factors among married women in 19 sub-Saharan African countries. Arch Public Health. (2021) 79:1–12. doi: 10.1186/s13690-021-00733-x
6. Solomon Y, Sema A, Menberu T. Adherence and associated factors to iron and folic acid supplementation among pregnant women attending antenatal care in public hospitals of Dire Dawa, Eastern Ethiopia. Eur J Midwifery. (2021) 5:138595. doi: 10.18332/ejm/138595
7. Tadesse AW, Aychiluhm SB, Mare KU. Individual and community-level determinants of iron-folic acid intake for the recommended period among pregnant women in Ethiopia: a multilevel analysis. Heliyon. (2021) 7:e07521. doi: 10.1016/j.heliyon.2021.e07521
8. World Health Organization. Global Nutrition Targets 2025: Childhood Overweight Policy Brief. Geneva: World Health Organization (2014).
9. World Health Organization. Global Targets 2025 to Improve Maternal, Infant and Young Children Nutrition. Geneva: World Health Organization (2017).
10. Ethiopia TFDRo. Guidelines for the Prevention and Control of Micronutrient Deficiencies in Ethiopia Federal Ministry of Health. (2016). Ethiopia TFDRo.
11. Kennedy E, Mersha GA, Biadgilign S, Tessema M, Zerfu D, Gizaw R, et al. Nutrition policy and governance in Ethiopia: what difference does 5 years make? Food Nutr Bull. (2020) 41:494–502. doi: 10.1177/0379572120957218
13. Gebre A, Mulugeta A, Etana B. Assessment of factors associated with adherence to iron-folic acid supplementation among urban and rural pregnant women in North Western Zone of Tigray, Ethiopia: comparative study. Int J Nutr Food Sci. (2015) 4:161–8. doi: 10.11648/j.ijnfs.20150402.16
14. Assefa H, Abebe SM, Sisay M. Magnitude and factors associated with adherence to iron and folic acid supplementation among pregnant women in Aykel town, Northwest Ethiopia. BMC Preg Childbirth. (2019) 19:1–8. doi: 10.1186/s12884-019-2422-4
15. Getachew M, Abay M, Zelalem H, Gebremedhin T, Grum T, Bayray A. Magnitude and factors associated with adherence to iron-folic acid supplementation among pregnant women in Eritrean refugee camps, northern Ethiopia. BMC Preg Childbirth. (2018) 18:1–8. doi: 10.1186/s12884-018-1716-2
16. Nasir BB, Fentie AM, Adisu MK. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at Tikur Anbessa Specialized Hospital, Ethiopia. PLoS ONE. (2020) 15:e0232625. doi: 10.1371/journal.pone.0232625
17. Sendeku FW, Azeze GG, Fenta SL. Adherence to iron-folic acid supplementation among pregnant women in Ethiopia: a systematic review and meta-analysis. BMC Preg Childbirth. (2020) 20:1–9. doi: 10.1186/s12884-020-2835-0
18. Lyoba WB, Mwakatoga JD, Festo C, Mrema J, Elisaria E. Adherence to iron-folic acid supplementation and associated factors among pregnant women in Kasulu communities in north-western Tanzania. Int J Reprod Med. (2020) 2020:3127245. doi: 10.1155/2020/3127245
19. Ba DM, Ssentongo P, Kjerulff KH, Na M, Liu G, Gao X, Du P. Adherence to iron supplementation in 22 sub-Saharan African countries and associated factors among pregnant women: a large population-based study. Curr Dev Nutr. (2019) 3:nzz120. doi: 10.1093/cdn/nzz120
20. Asmamaw DB, Eshetu HB, Negash WD. Individual and community-level factors associated with intention to use contraceptives among reproductive age women in sub-Saharan Africa. Int J Public Health. (2022) 107:1604905. doi: 10.3389/ijph.2022.1604905
21. Felipe-Dimog EB Yu C-H, Ho C-H, Liang F-W. Factors influencing the compliance of pregnant women with iron and folic acid supplementation in the Philippines: 2017 Philippine demographic and health survey analysis. Nutrients. (2021) 13:3060. doi: 10.3390/nu13093060
22. Ethiopia CSA, Macro O. Ethiopia demographic and health survey. Addis Ababa: Central Statistical Agency (2016).
23. Workineh Y, Semachew A, Ayalew E, Temesgen WA. Compliance to Iron-folic acid supplementation and its association with the number of ANC visits in Ethiopia: systematic review and meta-analysis. Adv Prevent Med. (2019) 2019:3602585. doi: 10.1155/2019/3602585
24. Boti N, Bekele T, Godana W, Getahun E, Gebremeskel F, Tsegaye B, et al. Adherence to Iron-Folate supplementation and associated factors among Pastoralist's pregnant women in Burji districts, Segen area People's zone, southern Ethiopia: community-based cross-sectional study. Int J Reprod Med. (2018) 2018:2365362. doi: 10.1155/2018/2365362
25. Gebremariam AD, Tiruneh SA, Abate BA, Engidaw MT, Asnakew DT. Adherence to iron with folic acid supplementation and its associated factors among pregnant women attending antenatal care follow up at Debre Tabor General Hospital, Ethiopia, 2017. PLoS ONE. (2019) 14:e0210086. doi: 10.1371/journal.pone.0210086
26. Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and health surveys: a profile. Int J Epidemiol. (2012) 41:1602–13. doi: 10.1093/ije/dys184
27. Titilayo A, Palamuleni M, Omisakin O. Sociodemographic factors influencing adherence to antenatal iron supplementation recommendations among pregnant women in Malawi: analysis of data from the 2010 Malawi Demographic and Health Survey. Malawi Med J. (2016) 28:1–5. doi: 10.4314/mmj.v28i1.1
28. Kassa ZY, Awraris T, Daba AK, Tenaw Z. Compliance with iron folic acid and associated factors among pregnant women through pill count in Hawassa city, South Ethiopia: a community based cross-sectional study. Reprod Health. (2019) 16:1–8. doi: 10.1186/s12978-019-0679-8
29. Liyew AM, Teshale AB. Individual and community level factors associated with anemia among lactating mothers in Ethiopia using data from Ethiopian demographic and health survey, 2016 a multilevel analysis. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-08934-9
30. Getaneh T, Negesse A, Dessie G, Desta M, Moltot T. Predictors of unmet need for family planning in Ethiopia 2019: a systematic review and meta-analysis. Arch Public Health. (2020) 78:1–11. doi: 10.1186/s13690-020-00483-2
31. Zekarias B, Meleko A, Hayder A, Nigatu A, Yetagessu T. Prevalence of anemia and its associated factors among pregnant women attending antenatal care (ANC) in Mizan Tepi University Teaching Hospital, South West Ethiopia. Health Sci J. (2017) 11:0–0. doi: 10.21767/1791-809X.1000529
32. Asmamaw DB, Habitu YA, Negash WD, Desta DZ, Mekonnen EG. Effective breastfeeding technique and associated factors among lactating mothers in Gidan District, North-East, Ethiopia: a community-based cross-sectional study. BMJ Open. (2022) 12:e059518. doi: 10.1136/bmjopen-2021-059518
33. Jikamo B, Samuel M. Non-adherence to iron/folate supplementation and associated factors among pregnant women who attending antenatal care visit in selected Public Health Institutions at Hosanna Town, Southern Ethiopia, 2016. J Nutr Disord Ther. (2018) 8:2161-0509.1000230. doi: 10.4172/2161-0509.1000230
34. Demisse B, Temesgen H, Dessie B, Kassa GM. Adherence status to iron with folic acid supplementation and associated factors among pregnant women receiving antenatal care at public health facilities in Northwest Ethiopia. SAGE Open Med. (2021) 9:20503121211049934. doi: 10.1177/20503121211049934
35. Gebremichael TG, Welesamuel TG. Adherence to iron-folic acid supplement and associated factors among antenatal care attending pregnant mothers in governmental health institutions of Adwa town, Tigray, Ethiopia: cross-sectional study. PLoS ONE. (2020) 15:e0227090. doi: 10.1371/journal.pone.0227090
36. Arega Sadore A, Abebe Gebretsadik L, Aman Hussen M. Compliance with iron-folate supplement and associated factors among antenatal care attendant mothers in Misha District, South Ethiopia: community based cross-sectional study. J Environ Public Health. (2015) 2015:781973. doi: 10.1155/2015/781973
37. Titaley CR, Dibley MJ. Factors associated with not using antenatal iron/folic acid supplements in Indonesia: the 2002/2003 and 2007 Indonesia Demographic and Health Survey. Asia Pac J Clin Nutr. (2015) 24:162–76. doi: 10.6133/apjcn.2015.24.1.10
38. Madestria NPO, Moedjiono AI, Tahir M, Suarayasa K, Nur R, Syam A. Effect of education through video and packaging modifications of iron tablets on female adolescent behavior in the iron supplementation intake in SMPN 2 and SMPN 1 Parigi. Gaceta Sanitaria. (2021) 35:S127–30. doi: 10.1016/j.gaceta.2021.10.011
39. Agegnehu G, Atenafu A, Dagne H, Dagnew B. Adherence to iron and folic acid supplement and its associated factors among antenatal care attendant mothers in Lay Armachiho health centers, Northwest, Ethiopia, 2017. Int J Reprod Med. (2019) 2019:5863737. doi: 10.1155/2019/5863737
40. Agegenehu CD, Tesema GA, Teshale AB, Alem AZ, Yeshaw Y, Kebede SA, et al. Spatial distribution and determinants of iron supplementation among pregnant women in Ethiopia: a spatial and multilevel analysis. Arch Public Health. (2021) 79:1–14. doi: 10.1186/s13690-021-00669-2
41. Warvadekar K, Reddy J, Sharma S, Dearden KA, Raut MK. Socio-demographic and economic determinants of adherence to iron intake among pregnant women in selected low and lower middle income countries in Asia: insights from a cross-country analyses of global demographic and health surveys. Intl J Comm Med Public Health. (2018) 5:1552–69. doi: 10.18203/2394-6040.ijcmph20181234
Keywords: adherence, associated factors, iron-folic acid, EDHS, Ethiopia
Citation: Asmamaw DB, Debebe Negash W, Bitew DA and Belachew TB (2022) Poor adherence to iron-folic acid supplementation and associated factors among pregnant women who had at least four antenatal care in Ethiopia. A community-based cross-sectional study. Front. Nutr. 9:1023046. doi: 10.3389/fnut.2022.1023046
Received: 19 August 2022; Accepted: 28 November 2022;
Published: 08 December 2022.
Edited by:
Sumantra Ray, RNutr, NNEdPro Global Centre for Nutrition and Health, United KingdomReviewed by:
Emyr Reisha Isaura, Airlangga University, IndonesiaCopyright © 2022 Asmamaw, Debebe Negash, Bitew and Belachew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Desale Bihonegn Asmamaw, ZGVzYWxlYmlob25lZ24xOTg4QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.