
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 09 January 2023
Sec. Clinical Nutrition
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1017472
This article is part of the Research TopicNutritional Counseling for Lifestyle ModificationView all 9 articles
Aim: To evaluate the improvement of glycemic control and stress adaptation in patients with GDM by mobile phone WeChat management during novel coronavirus pneumonia.
Methods: In this study, 75 women with GDM were included, of whom 35 were included in mobile WeChat group management as the GDM-M group and 40 as the GDM group.
Results: After mobile WeChat group management for 4 weeks, E and NE were lower. MDA was lower, and SOD was higher. HOMA-IR was lower. E, NE, and cortisol were related to HOMA-IR positively, MDA was positively related to HOMA-IR, and SOD was negatively related to HOMA-IR. E and cortisol were positively related to MDA but negatively related to SOD.
Conclusion: The stress adaptation disorder and insulin resistance in patients with GDM who have completed mobile WeChat group management can be improved during novel coronavirus pneumonia. Mobile WeChat management played a positive role in improving the insulin resistance of women with GDM under special circumstances, which may reduce the risk of maternal and fetal complications.
Novel coronavirus pneumonia is a coronavirus disease that has increased rapidly since its first identification in Wuhan, China, in December 2019 (1). The novel coronavirus pneumonia has become a public health safety event. For public safety considerations, the experts suggest that everyone should reduce their outdoors, suspend public places, and wear masks when necessary (2). The novel coronavirus pneumonia has brought panic to the masses and is a psychological stress event for the public.
The prevalence of gestational diabetes mellitus (GDM) is increasing rapidly (3). GDM-complicated pregnancies can cause adverse effects on mothers [such as the increased risk of pregnancy-induced hypertension (PIH), preeclampsia, and type 2 diabetes] and neonates [such as macrosomia, large for gestational age (LGA), and adulthood type 2 diabetes mellitus] (4). For women with GDM, daily blood glucose monitoring, regular clinical visits, and healthy lifestyle program management help control the disease and its complications (5).
During the COVID-19 pandemic, most people attempted to reduce the number of times they went out and went to the hospital for treatment to reduce their exposure to the virus (6). In contrast, quarantine or control of patients with GDM leads to reduced activities, changes in eating habits, or increased eating opportunities. So, currently, the self-management of patients with GDM is significant, especially professional and accurate self-management (7).
Several studies showed that self-management in GDM is effective (8, 9), but most of them focused on lectures or group discussions (10–12). During the COVID-19 epidemic, the self-management ability of women with GDM was particularly important, but they had limited channels to obtain professional and detailed self-management knowledge. Therefore, during the COVID-19 epidemic, there were challenges between the insufficient self-management ability of women with GDM and the good control of blood glucose.
However, our previous study reported that stress hormones were increased in women with gestational diabetes mellitus, and women with GDM have stress adaptation disorder (13). Novel coronavirus pneumonia incidents also increased the chances of psychological stress in the public. Limited by the conditions, we attempted to teach women with GDM the self-management method of blood glucose control through a special way, WeChat group management, while investigating whether only relying on mobile WeChat group management can improve the stress adaptive disorder and blood glucose of women with GDM during the COVID-19 pandemic.
According to the American Diabetes Association criteria with a 75-g oral glucose tolerance test (OGTT) at 24–28 weeks of pregnancy, the diagnosis of GDM was made with the cutoff value being >5.1 mmol/L at fasting, >10.0 mmol/L at 1 h, and >8.5 mmol/L at 2 h (14). The exclusion criteria were as follows: (1) pregnant women with previously known medical complications during pregnancy such as hypothyroidism, polycystic ovary syndrome, DM 1 or 2, and hyperthyreosis; (2) multiple pregnancies; and (3) women who were treated with hormones or drugs that may affect glucose and hormone concentrations.
In this study, 75 women with GDM were included, of whom 35 were included in the WeChat group management as the GDM-Management (GDM-M) group and 40 in the GDM group. In the WeChat group, we have professional dieticians who give professional diet suggestions and answer questions from patients on time every day. Women with GDM-M received information on the risks of GDM, detailed guidance on GDM diet, and some details in activities, blood glucose and weight tests, and a 3-day diet diary that was recorded for 1 week, and this study lasted for 4 weeks. Fasting blood glucose, 2 h blood glucose, daily diet, fasting weight, and time of exercise were included in the diary. Approval was obtained from the ethics committee of Yantai Yuhuangding Hospital, and informed consent was obtained from all participants.
Clinical features, including the gestational age at delivery, maternal age, and pre-gestational body mass index (BMI), were included for analysis. Blood glucose was determined using Roche Automatic Biochemical Analyzer (Roche Diagnostics, Mannheim, Germany). Malondialdehyde (MDA) and anti-OS enzyme superoxide dismutase (SOD) were detected according to the instructions of the kits (Jiancheng Bioengineering Institute, Nanjing, China). Fasting insulin was tested using an electrochemical luminescence immunoassay (Roche Diagnostics, Mannheim, Germany). Plasma epinephrine (E), noradrenaline (NE), and cortisol levels were measured using radioimmunoassay (RIA) (Roche Diagnostics, Mannheim, Germany). Homeostatic model assessment of insulin resistance (HOMA-IR) was used to evaluate insulin resistance in women with GDM (15): HOMA-IR = Fins (mU/L) × FPG (mmol/L)/22.5.
Data were evaluated using Student's t-test in SPSS 16.0 (SPSS, Inc., Chicago, IL, USA). Continuous variables of normal distribution data are presented as mean ± standard error. Data that were not normally distributed were log-transformed before analysis. A P-value of < 0.05 was considered statistically significant.
There was no significant difference in maternal age, gestational weeks, and BMI between the GDM group and the GDM-M group (Table 1).
The cortisol level was slightly higher in the GDM-M group than in the GDM group, but the difference was not statistically significant (P > 0.05, Figure 1A). E concentration (388 ± 96 ng/L; P < 0.01) was lower in the GDM-M group than in the GDM group (415 ± 102 ng/L) (Figure 1B); NE levels (130 ± 53 ng/L; P < 0.05) were also lower in the GDM-M group than in the GDM group (146 ± 40 ng/L; P < 0.01) (Figure 1C). MDA was lower and SOD was higher in the GDM-M group than in the GDM group (both P < 0.01) (Figures 1D, E). HOMA-IR was lower in the GDM-M group (2.2 ± 0.4; P < 0.01) than in the GDM group (1.7 ± 0.4) (Figure 1F).
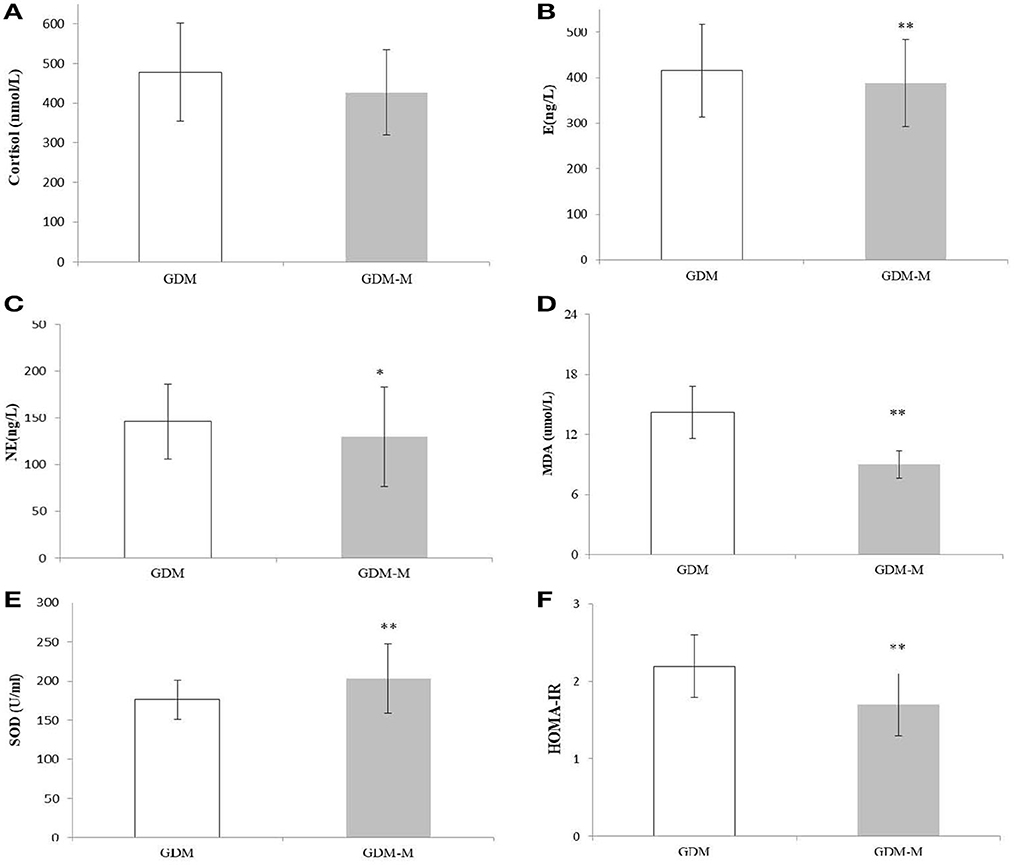
Figure 1. Histograms of plasma stress, oxidative stress, and glucose-related indexes—cortisol (A), E (B), NE (C), MDA (D), SOD (E), and HOMA-IR (F) in two groups. Data are presented as mean ± SD. A two-sample t-test was used to determine whether the differences in the GDM-M group were statistically significant. *Indicates P < 0.05 vs. GDM group, and P < 0.01 is expressed by**. E, epinephrine; NE, noradrenaline; MDA, malondialdehyde; SOD, superoxide dismutase.
In the GDM group, E, NE, and cortisol were positively related to HOMA-IR (all P < 0.05), MDA was positively related to HOMA-IR while SOD was negatively related (both P < 0.05). Only cortisol was positively related to HOMA-IR in the GDM-M group (P < 0.05) (Table 2).
In the GDM group, E and cortisol were positively related to MDA (both P < 0.05), and E and cortisol were negatively related to SOD (both P < 0.05). In the GDM-M group, cortisol was positively related to MDA (P < 0.01) and E was negatively related to SOD (P < 0.01) (Table 3).
To the best of our knowledge, this is the first study on stress adaptation in patients with GDM by mobile phone management during novel coronavirus pneumonia. Pregnancy for women is stressful (16). Our previous study showed that stress hormones were significantly increased in women with GDM, indicating that stress adaptation disorder occurred (13).
During the novel coronavirus pneumonia, to reduce risks, people were asked to stay at home and avoid going out. Pregnant women with GDM have been protected by their families and advised to stay at home all the time. To control blood glucose, we chose to establish a mobile WeChat management group to manage diet, blood glucose monitoring, sports education, and management for patients with GDM.
Previous studies showed that, based on the mobile WeChat group to manage blood glucose, most of them can achieve relatively ideal results in terms of blood glucose indicators (17, 18). Our tertiary hospital has professional clinical nutrition experts, obstetricians, and nursing teams and has advanced GDM management and education experience. Patients with GDM have high compliance, and it is easy to achieve ideal management results. However, during the epidemic, the only method to manage the blood glucose of patients with GDM is by establishing a WeChat group using mobile phones.
Stress is a matter of debate (19, 20). It is defined as the nonspecific response of the body to any stressor (21–23). However, prolonged stress-related psychophysiological alterations may increase the risk of functional or mental disorders, induce cytological effects, and lead to diseases (16, 24).
Stress could activate the hypothalamic-pituitary-adrenal (HPA) axis, induce cytological effects, and lead to diseases (25). Cortisol is the most frequently used biomarker of the physiological stress responses of the HPA axis. Hosler's study showed that stress is a potentially chronic, long-term, and rarely detected risk factor for metabolic disturbances, and more studies on stress exposure and psychological stress as GDM risk factors are needed (26).
Our results showed that cortisol was slightly lower in the GDM group, but the difference was not statistically significant. E and NE concentrations decreased, indicating that stress adaptation disorder decreased after mobile phone intervention, which means that, using WeChat group management, some of the stress hormones of patients with GDM decreased and the stress adaptation disorders of patients with GDM improved. E, NE, and cortisol were positively related to HOMA-IR, which indicates that, if the stress adaptation disorder of patients with GDM is improved, their insulin resistance will also decrease.
Throughout the experiment, all GDM-M participants considered choosing the right diet, adequate physical exercise, accurate blood glucose monitoring, and a standard diet diary. During the epidemic period, the level of psychological stress in the public increased (27, 28). We believe that the stress adaptation disorder of patients with GDM will further increase. This hypothesized pathway leads to the development of GDM, including psychological stress responses and stress adaptation disorder.
Pregnancy is considered a state of enhanced oxidative stress (29–31). A higher level of oxidative stress could lead to pathological pregnancies, including gestational diabetes mellitus (GDM) (32). It has been confirmed that oxidative stress plays an important role in the etiology of congenital malformations in animal models of diabetes (33).
Stress hormones including E and cortisol were positively correlated with MDA and negatively correlated with SOD, suggesting that the mechanism of stress adaptive disorder was positively related to oxidative stress injury, which was consistent with our previous research findings (13).
Our results showed that MDA was decreased and SOD was increased in the GDM-M group, and MDA and SOD were positively and negatively correlated with HOMA-IR, respectively. These findings indicate that oxidative stress impairment was lower after mobile phone management, suggesting that the decrease in oxidative stress injury in patients with GDM could improve the stress adaptive disorder, thus improving the insulin resistance of patients with GDM.
Our study has two limitations. First, there was a significant difference at baseline between the GDM-M and GDM groups. Patients with GDM who are willing to join the mobile WeChat management group may have a significant influence on compliance, providing more positive findings. Second, our study reports only the short-term effects and cannot conclude long-term mobile phone management.
Our previous interventional experimental study found that whey protein preloading can alleviate the stress adaptation disorder of patients with GDM and improve blood glucose (34). We pondered if WeChat group management plus whey protein preload will have a more surprising effect on these patients. In the future, we will continue to carry out a series of studies.
In summary, during novel coronavirus pneumonia, patients with GDM who have complete mobile phone management can improve their stress adaptation disorder and play a positive role in improving insulin resistance in women with GDM under special circumstances, especially during the epidemic, which may reduce the risk of maternal and fetal complications. Compared with some diabetes-related applications, a study on the long-term effects and cost-effectiveness of blood glucose management in patients with GDM based on mobile phone WeChat management group is warranted, especially during the novel coronavirus pneumonia or other infectious diseases.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Yantai Yuhuangding Hospital Committee. Informed consent was obtained from all participants.
YF and YW designed the study and wrote the manuscript. YL and QF performed the data analysis. XL and XS provided study oversight. All authors approved the final manuscript.
This study was supported by grants from the Yantai Science and Technology Innovation Development Plan Project (2020YD028).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-perso n transmission: a study of a family cluster. Lancet. (2020) 395:514–23. doi: 10.1016/S0140-6736(20)30154-9
2. Carlos WG, Dela Cruz CS, Cao B, Pasnick S, Jamil S. Novel Wuhan (2019-nCoV) Coronavirus. Am J Respir Crit Care Med, (2020) 201:P7–p8. doi: 10.1164/rccm.2014P7
3. Khan T, Macaulay S, Norris SA, Micklesfield LK, Watson ED. Physical activity and the risk for gestational diabetes mellitus amongst pregnant women living in Soweto: a study protocol. BMC Womens Health. (2016) 16:66. doi: 10.1186/s12905-016-0345-z
4. Nguyen CL, Pham NM, Binns CW, Duong DV, Lee AH. Prevalence of gestational diabetes mellitus in eastern and southeastern Asia: a systematic review and meta-analysis. J Diabet Res. (2018) 2018:6536974. doi: 10.1155/2018/6536974
5. Moradi F, Ghadiri-Anari A, Enjezab B. COVID-19 and self-care strategies for women with gestational diabetes mellitus. Diabetes Metab Synd. (2020) 14:1535–9. doi: 10.1016/j.dsx.2020.08.004
6. Jethwani P, Saboo B, Jethwani L, Kesavadev J, Kalra S, Sahay R, et al. Management of children and adolescents having type 1 diabetes during COVID-19 pandemic in India: challenges and solutions. Int j diabetes dev c. (2020) 40:335–9. doi: 10.1007/s13410-020-00865-w
7. Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Synd. (2020) 14:273–6. doi: 10.1016/j.dsx.2020.04.001
8. Johnson QB, Berry DC. Impacting diabetes self-management in women with gestational diabetes mellitus using short messaging reminders. J am assoc nurse pra. (2018) 30:320–6. doi: 10.1097/JXX.0000000000000059
9. Sushko K, Menezes HT, Wang QR, Nerenberg K, Fitzpatrick-Lewis D, Sherifali D. Patient-reported Benefits and Limitations of Mobile Health Technologies for Diabetes in Pregnancy: A Scoping Review. Can J Diabet. (2022). doi: 10.1016/j.jcjd.2022.08.001 [Epub a head of print].
10. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. (2013) 12:14. doi: 10.1186/2251-6581-12-14
11. Carolan M. Diabetes nurse educators' experiences of providing care for women, with gestational diabetes mellitus, from disadvantaged backgrounds. J Clin Nurs. (2014) 23:1374–84. doi: 10.1111/jocn.12421
12. Homko CJ, Sivan E, Reece EA. The impact of self-monitoring of blood glucose on self-efficacy and pregnancy outcomes in women with diet-controlled gestational diabetes. Diabetes Educat. (2002) 28:435–43. doi: 10.1177/014572170202800313
13. Feng Y, Feng Q, Yin S, Xu X, Song X, Qu H, et al. Stress adaptation disorders play a role in rat gestational diabetes with oxidative stress and glucose transporter-4 expression. Gynecol Endocrinol. (2020) 36:786–90. doi: 10.1080/09513590.2019.1707797
14. He Z, Xie H, Liang S, Tang Y, Ding W, Wu Y, et al. Influence of different diagnostic criteria on gestational diabetes mellitus incidence and medical exp enditures in China. J Diabetes Investig. (2019) 10:1347–57. doi: 10.1111/jdi.13008
15. Abbasi F, Okeke Q, Reaven GM. Evaluation of fasting plasma insulin concentration as an estimate of insulin action in nondiabetic individuals: comparison with the homeostasis model assessment of insulin resistance (HOMA-IR). Acta Diabetol. (2014) 51:193–7. doi: 10.1007/s00592-013-0461-2
16. Radaelli T, Varastehpour A, Catalano P, Hauguel-de Mouzon S. Gestational diabetes induces placental genes for chronic stress and inflammatory pathways. Diabetes. (2003) 52:2951–8. doi: 10.2337/diabetes.52.12.2951
17. Jones EJ, Peercy M, Woods JC, Parker SP, Jackson T, Mata SA, et al. Identifying postpartum intervention approaches to reduce cardiometabolic risk among American Indian w omen with prior gestational diabetes, Oklahoma, 2012-2013. Prev Chronic Dis. (2015) 12:E45. doi: 10.5888/pcd12.140566
18. Tsirou E, Grammatikopoulou MG, Theodoridis X, Gkiouras K, Petalidou A, Taousani E, et al. Guidelines for medical nutrition therapy in?gestational diabetes mellitus: systematic review and critical appraisal. J Acad Nutr Diet. (2019) 119:1320–39. doi: 10.1016/j.jand.2019.04.002
19. Rolińska A, Aftyka A, Samardakiewicz M. Coping with stress in complicated pregnancy and gestational weight gain. Int J Environ Res Public Health. (2021) 18:10493. doi: 10.3390/ijerph181910493
20. Solis Paredes JM, Perichart Perera O, Montoya Estrada A, Reyes Muñoz E, Espino Y, Sosa S, et al. Gestational Weight Gain Influences the Adipokine-Oxidative Stress Association during Pregnancy. Obesity facts. (2021) 14:604–12. doi: 10.1159/000518639
22. Huang H, Yang K, Wang R, Han WH, Kuny S, Zelmanovitz PH, et al. β-Cell compensation concomitant with adaptive endoplasmic reticulum stress and β-cell neogenesis in a diet-induced type 2 diabetes model. Appl physiol nutr me. (2019) 44:1355–66. doi: 10.1139/apnm-2019-0144
23. Biobaku F, Ghanim H, Batra M, Dandona P. Macronutrient-mediated inflammation and oxidative stress: relevance to insulin resistance, obesity, and atherogenesis. J Clin Endocr Metab. (2019) 104:6118–28. doi: 10.1210/jc.2018-01833
24. Horsch A, Kang J S, Vial Y, Ehlert U, Borghini A, Marques-Vidal P, et al. Stress exposure and psychological stress responses are related to glucose concentrations during pregn ancy. Br J Health Psychol. (2016) 21:712–29. doi: 10.1111/bjhp.12197
25. Berger I, Werdermann M, Bornstein SR, Steenblock C. The adrenal gland in stress - Adaptation on a cellular level. J Steroid Biochem Mol Biol. (2019) 190:198–206. doi: 10.1016/j.jsbmb.2019.04.006
26. Hosler AS, Nayak SG, Radigan AM. Stressful events, smoking exposure and other maternal risk factors associated with gestational diabetes mellitus. Paediatr Perinat Epidemiol. (2011) 25:566–74. doi: 10.1111/j.1365-3016.2011.01221.x
27. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
28. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
29. Jelly P, Chadha L, Kaur N, Sharma S, Sharma R, Stephen S, et al. Impact of COVID-19 pandemic on the psychological status of pregnant women. Cureus. (2021) 13:e12875. doi: 10.7759/cureus.12875
30. Kara P, Nazik E, Nazik H, Özer D. Post-traumatic stress disorder and affecting factors in pregnant women in the COVID-19 pandemic. Psychiat danub. (2021) 33:231–9. doi: 10.24869/psyd.2021.231
31. Davoudian T, Gibbins K, Cirino NH. Perinatal loss: the impact on maternal mental health. Obstet Gynecol Surv. (2021) 76:223. doi: 10.1097/OGX.0000000000000874
32. Ma Y, Xu S, Meng J, Li L. Protective effect of nimbolide against streptozotocin induced gestational diabetes mellitus in rats via alteration of inflammatory reaction, oxidative stress, and gut microbiota. Environ Toxicol. (2022) 37:1382–93. doi: 10.1002/tox.23491
33. Lappas M, Hiden U, Desoye G, Froehlich J, Hauguel-de Mouzon S, Jawerbaum A. The role of oxidative stress in the pathophysiology of gestational diabetes mellitus. Antioxid Redox Signal. (2011) 15:3061–100. doi: 10.1089/ars.2010.3765
Keywords: novel coronavirus pneumonia (COVID-19), GDM, stress adaptation, mobile phone management, insulin resistance
Citation: Feng Y, Lv Y, Feng Q, Song X, Li X and Wang Y (2023) Improvement of stress adaptation and insulin resistance in women with GDM by WeChat group management during novel coronavirus pneumonia. Front. Nutr. 9:1017472. doi: 10.3389/fnut.2022.1017472
Received: 12 August 2022; Accepted: 12 December 2022;
Published: 09 January 2023.
Edited by:
Ramona De Amicis, University of Milan, ItalyReviewed by:
Dharma Lindarto, Department of Internal Medicine, IndonesiaCopyright © 2023 Feng, Lv, Feng, Song, Li and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Feng,  fenghanxiao1985@163.com; Yongjun Wang,
fenghanxiao1985@163.com; Yongjun Wang,  wangyongjun519@163.com
wangyongjun519@163.com
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.