
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr. , 31 October 2022
Sec. Clinical Nutrition
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1011002
 Phiwayinkosi V. Dludla1,2*
Phiwayinkosi V. Dludla1,2* Bongani B. Nkambule3
Bongani B. Nkambule3 Tawanda M. Nyambuya4
Tawanda M. Nyambuya4 Khanyisani Ziqubu5
Khanyisani Ziqubu5 Sihle E. Mabhida1
Sihle E. Mabhida1 Vuyolwethu Mxinwa3
Vuyolwethu Mxinwa3 Kabelo Mokgalaboni3,6
Kabelo Mokgalaboni3,6 Fransina Ndevahoma4
Fransina Ndevahoma4 Sidney Hanser7
Sidney Hanser7 Sithandiwe E. Mazibuko-Mbeje5
Sithandiwe E. Mazibuko-Mbeje5 Albertus K. Basson2
Albertus K. Basson2 Jacopo Sabbatinelli8
Jacopo Sabbatinelli8 Luca Tiano9
Luca Tiano9Background: Vitamin C is one of the most consumed dietary compounds and contains abundant antioxidant properties that could be essential in improving metabolic function. Thus, the current systematic review analyzed evidence on the beneficial effects of vitamin C intake on cardiovascular disease (CVD)-related outcomes in patients with diabetes or metabolic syndrome.
Methods: To identify relevant randomized control trials (RCTs), a systematic search was run using prominent search engines like PubMed and Google Scholar, from beginning up to March 2022. The modified Black and Downs checklist was used to assess the quality of evidence.
Results: Findings summarized in the current review favor the beneficial effects of vitamin C intake on improving basic metabolic parameters and lowering total cholesterol levels to reduce CVD-risk in subjects with type 2 diabetes or related metabolic diseases. Moreover, vitamin C intake could also reduce the predominant markers of inflammation and oxidative stress like C-reactive protein, interleukin-6, and malondialdehyde. Importantly, these positive outcomes were consistent with improved endothelial function or increased blood flow in these subjects. Predominantly effective doses were 1,000 mg/daily for 4 weeks up to 12 months. The included RCTs presented with the high quality of evidence.
Conclusion: Clinical evidence on the beneficial effects of vitamin C intake or its impact on improving prominent markers of inflammation and oxidative stress in patients with diabetes is still limited. Thus, more RCTs are required to solidify these findings, which is essential to better manage diabetic patients at increased risk of developing CVD.
Diabetes mellitus remains one of the leading causes of deaths worldwide (1). Although currently used antidiabetic therapies such as metformin and insulin can manage diabetes-associated complications (2, 3), their long-term therapeutic effects could be limited due to the rapid rise of diabetes-related deaths (4). Certainly, most diabetic patients (mainly due to pathological consequences of hyperglycemia) are known to be at increased risk for cardiovascular disease (CVD)-related deaths (Figure 1) (5, 6). Thus, in addition to understanding the precise pathological mechanisms implicated in diabetes-induced myocardial injury, there has been a growing need to discover novel pharmacological compounds, with strong cardioprotective properties to prolong the lives of diabetic patients.
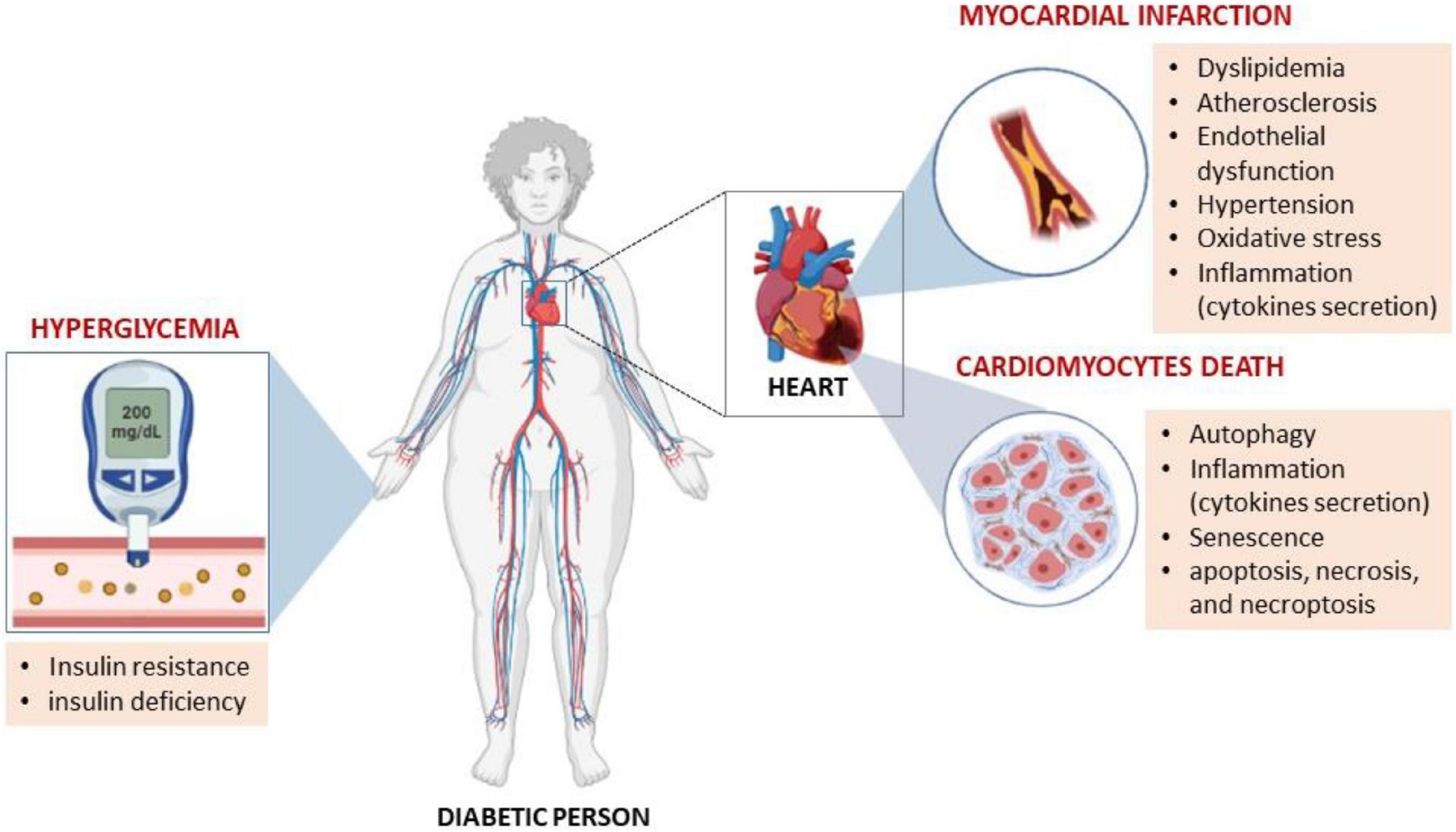
Figure 1. Hyperglycemia, as a major characteristic feature of diabetes mellitus, is known be responsible for prompting metabolic abnormalities that make an individual susceptible to increased cardiovascular disease (CVD)-risk. For example, abnormal levels of serum lipids (dyslipidemia) that may eventually cause atherosclerosis through endothelial dysfunction are all implicated in the development of CVDs. Similarly, preclinical studies have implicated pathological mechanisms such as abnormal autophagy and inflammation to be involved in this process.
There has been a general interest in pharmacological compounds with strong antioxidant and anti-inflammatory properties for their protective effects against diabetes-associated cardiovascular complications (7–12). This is important since impaired glucose intolerance in a diabetic state has been associated with aggravated pro-inflammatory response and oxidative stress-induced vascular damage (13, 14). Consistently, due to their perceived ameliorative effects against inflammation and oxidative stress, there has been a great necessity to examine the protective effects of dietary compounds against diabetes-associated complications (15–17).
There is currently a considerable interest in understanding the therapeutic role of herbs and supplements against diabetes and CVD-related complications (18–20). This includes uncovering the therapeutic effects of vitamins, which are considered vital micronutrient that an organism requires for an adequate metabolic function. Indeed, various dietary compounds such as vitamin C are increasingly consumed for their envisaged benefits against metabolic complications (21–23). Vitamin C is considered an essential nutrient that functions as a vital antioxidant in protecting against oxidative stress and tissue damage (24, 25). Besides its availability as a dietary supplement, vitamin C can also be found in food sources including citrus fruits and vegetables. The beneficial effects of vitamin C are associated with their capacity to attenuate oxidative stress and inflammation (21). A previously published meta-analysis showed that vitamin C intake could improve glycemic control or blood pressure in adult participants (22, 26). More evidence is required to understand the health benefits of this dietary antioxidant, and to potentially curb the rising toll of CVD-related deaths in patients with diabetes or metabolic diseases. This is in support of recent reviews highlighting the gap in clinical evidence informing on the favorable outcomes of vitamin C in individuals at increased CVD-risk (27–29). Importantly, although other reviews have reported on the potential therapeutic effects of vitamin C on controlling basic metabolic function and CVD-related outcomes (26, 30, 31), very limited information exists on the implications or link with biomarkers of inflammation and oxidative stress such as C-reactive protein (CRP) and interleukin 6 (IL-6), and malondialdehyde (MDA) levels.
Supplementary file 1 contains the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines that were followed to prepare the manuscript. The current study does not have an approved protocol; however, the International prospective register of systematic reviews (PROSPERO) was cautiously surveyed to avoid duplicating systematic reviews or meta-analysis investigating a similar topic.
Briefly, a systematic search was run using prominent search engines like PubMed and Google Scholar, from beginning up to March 2022. This was done by two independent reviewers. To optimally cover relevant literature, a rather broad primary search strategy was applied where we explored all randomized controlled trials (RCTs) reporting on vitamin C intake in patients with diabetes or metabolic syndrome. Thereafter, the especial focus was placed on RCTs assessing the effect of vitamin C intake on outcomes related with CVD in diabetic individuals, and this was done in comparison to the placebo or comparative control. Medical Subject-Heading (MeSH) and text words “vitamin C,” “diabetes,” “metabolic syndrome,” “cardiovascular disease,” and their matching synonyms were used.
The study encompassed RCTs reporting on the therapeutic effects of vitamin C on outcomes related with CVD in adults (>18 years) with diabetes or metabolic syndrome. Notably, encompassed RCTs were those that assessed the use of vitamin C as an intervention, comprising the comparison group on placebo, reporting on any quantifiable outcome of CVD in patients with diabetes or metabolic syndrome. RCTs reporting on the use of vitamin C in conjunction with other therapies were excluded. Also, RCTs not describing the clear CVD-outcome or covered incomplete information were excluded. Relevant items, including participants, interventions, comparisons, and outcomes (PICO), are described below:
• Participants:
Adult patients with diabetes and at increased risk of developing CVD.
• Interventions:
Treatment intervention involved vitamin C intake in patients with diabetes or metabolic syndrome.
• Comparisons:
Patients receiving placebo were used a comparative control.
• Outcomes:
The primary outcomes for this systematic review included basic metabolic profiles such as blood glucose levels, and CVD-risk measurements like lipid profiles, endothelial function, and blood pressure. Whereas the secondary outcome were biomarkers of inflammation and oxidative stress.
Briefly, qualifying articles were carefully selected by at least two independent investigators. The main outcome of the study was to assess the effects of vitamin C intake on outcomes related with CVD in diabetes or condition of metabolic syndrome. It remained imperative to also assess correlation between duration of intervention and improvements in CVD-related outcomes in the study population. For accurate reporting, relevant data items extracted from each RCT included the name and year of publication, the country where the study was performed, sample and gender dissemination, as well as the dose and duration of intervention. The risk of bias was independently assessed by at least two investigators using of the adapted Downs and Black checklist, which is appropriate for both randomized and non-randomized studies (32, 33).
A total of 183 RCTs were inspected for eligibility, however, only 21 studies were selected, as shown in Figure 2. All encompassed studies were RCTs on the effects of vitamin C intake on outcomes related with CVD in patients with diabetes or metabolic syndrome. Disqualified studies were on the combination use of vitamin C with other pharmacological compounds, or for not having a well-defined control group. Other exclusions were related for not having a clear study design and not reporting on the effect of vitamin C on the predefined study population.
All contained RCTs were available from peer-reviewed journals, as shown in Table 1. Besides Australia (n = 3), Iran (n = 2), New Zealand (n = 1), Palestine (n = 1), most studies were from the United States (n = 4), United Kingdom (n = 5), and Europe (n = 5). Overall, the total of participants was 7,688, with an average age of 60 years, with at least 50% of them registered as males (Table 1). Furthermore, approximately 90% of RCTs evaluated type 2 diabetes (T2D), while the rest were focused on patients with type 1 diabetes and the metabolic syndrome (Table 1). In terms of dose selections, consistency was observed where most studies used vitamin C at 1,000 mg, taken once a day, or twice daily at doses of 500 mg (Table 1). The treatment duration was consistent at 4–6 weeks (Table 1), while other RCTs did evaluate short term effects of vitamin C intake in terms of hours a few days (34–36), whereas limited studies tested the long-term effects at 4 months (37–39), 1 year (40), 4 years (41), and 9.2 years (42).
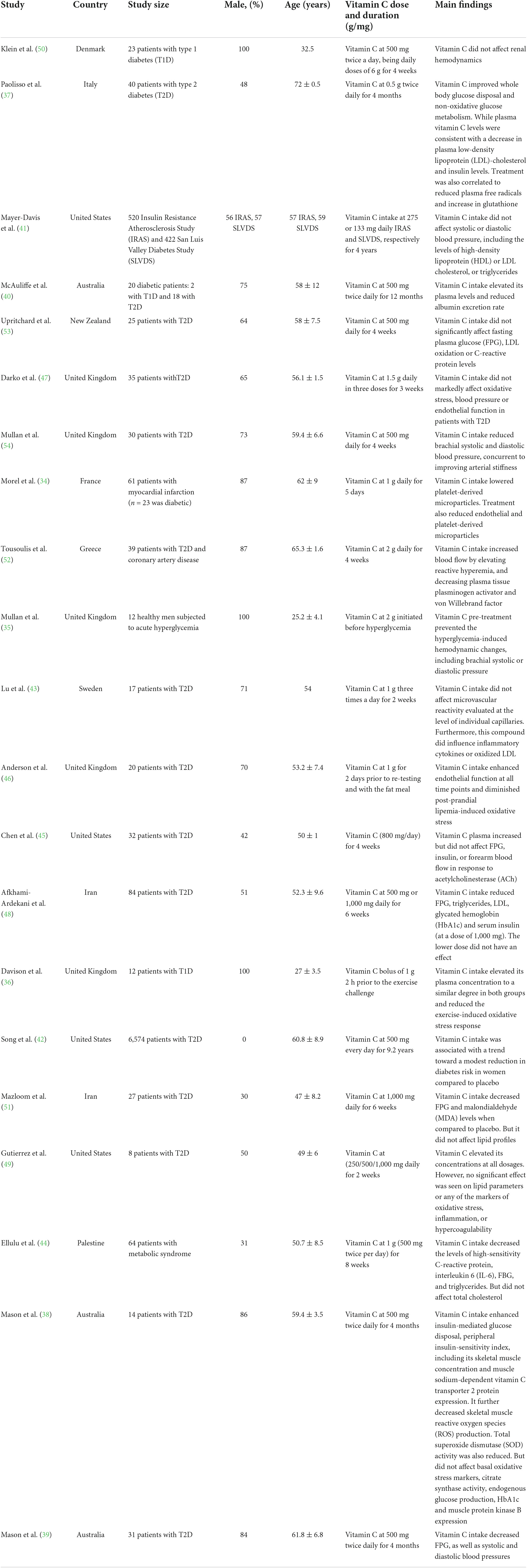
Table 1. An overview of studies reporting on the impact of vitamin C intake on cardiovascular disease (CVD)-related outcomes.
Briefly, the modified Back and Downs checklist with 26 questions and four domains, which are relevant for analyzing the quality of encompassed studies (32). Out of the 21 included studies six were excellent (38, 39, 42–45), 12 were scored as good (35, 37, 40, 46–54), and three were fair (34, 36, 41). Supplementary file 2 depicts that encompassed studies presented with low reporting bias with a median score of 8 out of a probable score of 10 (overall agreement 85.67%, kappa = 0.71), good external legitimacy with median score of 2 out of 3 (overall agreement 39.13%, kappa = 0.13), excellent internal validity with median score 7 out of 7 (overall agreement 65.22%, kappa = 0.34) and low risk assortment bias with median of 5 out of possible 6 (overall agreement 56.51%, kappa = 0.19). Therefore, interpretation of the findings can be trusted and applied outside the selected study population.
The overall included studies reported on vitamin C intake and its diverse effects on basic metabolic parameters such as glycated hemoglobin (HbA1c), fasting plasma glucose and insulin levels, as well as CVD related outcomes including lipid profiles and blood pressure (Table 1).
In relation to basic metabolic parameters, evidence available from as early as 1995 indicated that intake of vitamin C, at 500 mg twice daily for 4 months, could improve whole body glucose disposal and non-oxidative glucose metabolism in individuals with T2D (37). Interestingly, this was consistent with enhanced plasma vitamin C levels, a decline in plasma low-density lipoprotein (LDL)-cholesterol, as well as reduced free radicals and insulin levels. McAuliffe (40), confirmed some of these findings showing that vitamin C intake at a similar dose (500 mg) twice daily for 12 months could increase its plasma levels while resulting in reduced albumin excretion rate in diabetic patients. As new information became available, Mullan et al. (54) demonstrated that vitamin C intake at 500 mg daily for 4 weeks reduced brachial systolic and diastolic blood pressure concomitant to improving arterial stiffness in patients with T2D. Whereas Morel et al. (34) showed that vitamin C intake at 1,000 mg daily for 5 days reduced platelet-derived microparticles in diabetic patients with myocardial infarction.
Other beneficial effects linked with vitamin C intake in patients with diabetes or metabolic syndrome extended to improving blood flow or lowering blood pressure (35, 38, 39, 52); attenuating oxidative stress and endothelial dysfunction (36, 38, 39, 46). This was consistent with an effective control of fasting plasma glucose (FPG), triglycerides, LDL, HbA1c and serum insulin levels (38, 39, 48, 51); while also reducing the pro-inflammatory markers such as CRP and IL-6 (44). These positive effects with vitamin C intake were predominantly observed with the doses of 1,000 mg/daily, and intervention period of 4 weeks up to 12 months in patients with T2D. Alternatively, in patients with T1D, vitamin C intake could enhance its plasma levels and these effects were linked with reduced oxidative stress response (36, 40). However, very few studies have investigated the therapeutic effects of vitamin C in patients with T1D.
Opposing the advantages observed with vitamin C intake in controlling metabolic disease associated complications in diabetic patients, other studies did not report any positive effects with regular intake of this antioxidant. For example, Klein et al. (50) showed that vitamin C at 500 mg twice a day for 4 weeks could not normalize renal hemodynamics in normoalbuminuric in normotensive diabetic patients. Mayer-Davis et al. (41) revealed that vitamin C intake at 275 or 133 mg daily for 4 years did not impact systolic or diastolic blood pressure nor with HDL or LDL cholesterol, or triglycerides. Similarly, Upritchard et al. (53) and Darko et al. (47) showed that vitamin C intake between the doses of 500 and 1,500 mg daily for 3–4 weeks did not significantly improve endothelial function or affect FPG, LDL oxidation, or C-reactive protein levels in patients with T2D. Consistently, other studies showed that regular intake of vitamin C at 800–1,000 mg for 2–4 weeks did not significantly affect inflammatory cytokines, oxidized LDL, FPG or insulin levels, or forearm blood flow in patients with T2D (43, 45, 49). Notably, except for an RCT by Mayer-Davis et al. (41) which used approximately 520 participants, most of the studies that did not observe any significant results used a very low sample number, indicating this could have affected the power of the results. However, this is only a hypothesis, well-designed RCTs with adequate sample number are still required to give a better picture on the impact of vitamin C on outcomes related with CVD in patients with diabetes or metabolic syndrome.
The rapid prevalence of diabetes (55), coupled with the lack of effective therapies for its management (56), has propelled research into establishing alternative approaches to prevent this calamity. Dietary supplements have become an attractive target to investigate for their health benefits, especially due to their envisaged safety profile and potential bioactive properties (16, 57, 58). Vitamin C is considered an essential nutrient, also forming part of the World’s Health Organizations List of Essential Medicine, with abundant antioxidant effects (59, 60). Although many factors such as absorption and bioavailability profiles can influence its physiologic concentrations (61), it has long estimated that adequate intake of vitamin C of either 200 mg/day from five servings of fruits and vegetables or 100 mg/day is necessary to prevent its deficiency with a margin of safety (62). Consistently, epidemiological data support the observed improvements in CVD-related outcomes with high consumption of fruits and vegetables rich in antioxidants like vitamin C and E (63–66). Alternatively, while experimental data suggest vitamin C and E can protect against oxidative stress-induced cellular damage by scavenging of reactive oxygen species or by neutralizing lipid hydroperoxyl radicals (60), convincing evidence on the effect of multiple dietary supplements on metabolic and cardiovascular health is scarce (67). In fact, although quantitative analysis supports the positive effects of vitamin C intake on improving blood glucose control or blood pressure in patients with T2D (22, 26), such evidence has not been linked with CVD-related outcomes in conditions of metabolic syndrome.
The current systematic review involved 21 RCTs, with 7,688 participants, evaluating the impact of vitamin C intake on basic metabolic parameters such as HbA1c, FPG, and insulin levels, as well as CVD-related outcomes including lipid profiles and blood pressure (Table 1). In fact, overwhelming studies supported the beneficial effects of vitamin C intake on improving metabolic function and reducing cholesterol levels in patients with diabetes or metabolic syndrome. In addition to reducing the pro-inflammatory markers such as CRP and IL-6 (44), vitamin C intake at an average dose of 1,000 mg daily between 3 weeks up to a period of 12 months showed consistent results lowering FPG, triglycerides, LDL, HbA1c, and serum insulin levels (38–40, 48, 51). Interestingly, these results were supported by significantly increased plasma levels of this antioxidant after its intake in these patients (Table 1). Notably, the reduction in total cholesterol was associated with attenuation of oxidative stress and amelioration of endothelial dysfunction in these patients (36, 38, 39, 46). Further suggesting that vitamin C may exerts its therapeutic effects by terminating oxidation of lipid products that are linked with exacerbation of inflammation and endothelial dysfunction, as demonstrated elsewhere (61, 68–70). This result could also translate to improve blood flow and reduced blood pressure, as demonstrated in some RCTs (35, 38, 39, 52). However, clinical evidence on the beneficial effects of vitamin C intake or its impact on improving prominent markers of inflammation and oxidative stress in patients with diabetes is still limited. Thus, more RCTs are required to solidify these findings, which is essential to better manage diabetic patients at increased risk of developing CVD.
Other studies included within the current systematic review reported that vitamin C intake did not influence markers of metabolic function or CVD. Notably, some studies showed that intake with vitamin C at an average dose of 1,000 mg daily for 2–4 weeks does not significantly affect blood pressure nor with HDL and LDL cholesterol, as well as triglycerides (41, 50). Even when taken at a lower dose of 275 or 133 mg daily for a prolonged period of 4 years (41), it was apparent this antioxidant does not affect systolic or diastolic blood pressure nor with HDL or LDL cholesterol, or triglycerides. Others showed that vitamin C intake at 800–1,000 mg for 2–4 weeks also does not impact inflammatory cytokines, oxidized LDL, FPG or insulin levels, or forearm blood flow in patients with T2D (43, 45, 49). These results are like others showing failure of vitamin C intake to improve metabolic disease-related complications or to protect against CVDs in various clinical settings (71, 72). However, this evidence is still limited, additional studies are required to confirm any of these findings. Preclinical studies can serve as the reference model to further explore other potential benefits of vitamin C. This is essential since various preclinical models have demonstrated that this antioxidant can ameliorate the pathological consequences of inflammation and oxidative stress to alleviate diabetes-associated complications (73–76).
Summarized evidence showed that vitamin C intake could potentially improve basic metabolic profile while markedly reducing the levels of total cholesterol in patients with T2D and the metabolic syndrome (Figure 3). This was consistent with improved endothelial function, which is consistent to previous reports (35, 38, 39, 52). The fact that most antioxidant therapies have been dismissal in diabetes in clinical trials (77), highlights the need for additional RCTs to confirm these effects, especially for patients with T1D. Indeed, by searching the PubMed engine, very few RCTs could be accessed/identified reporting on the effects of vitamin C intake in patients with diabetes (78). Thus, additional clinical trials should consider the use of larger sample sizes and lengthier intake periods that are driven to stratify effects on the basis of baseline glycemic control necessary to validate favorable outcomes of vitamin C intake. Future considerations should include making use of a qualitative approach “meta-analysis” to strengthen the presented evidence. Which is one of the limitations of the current review, since most included RCTs were too diverse and presented very substantial heterogeneity and this could have affected the interpretation of results.
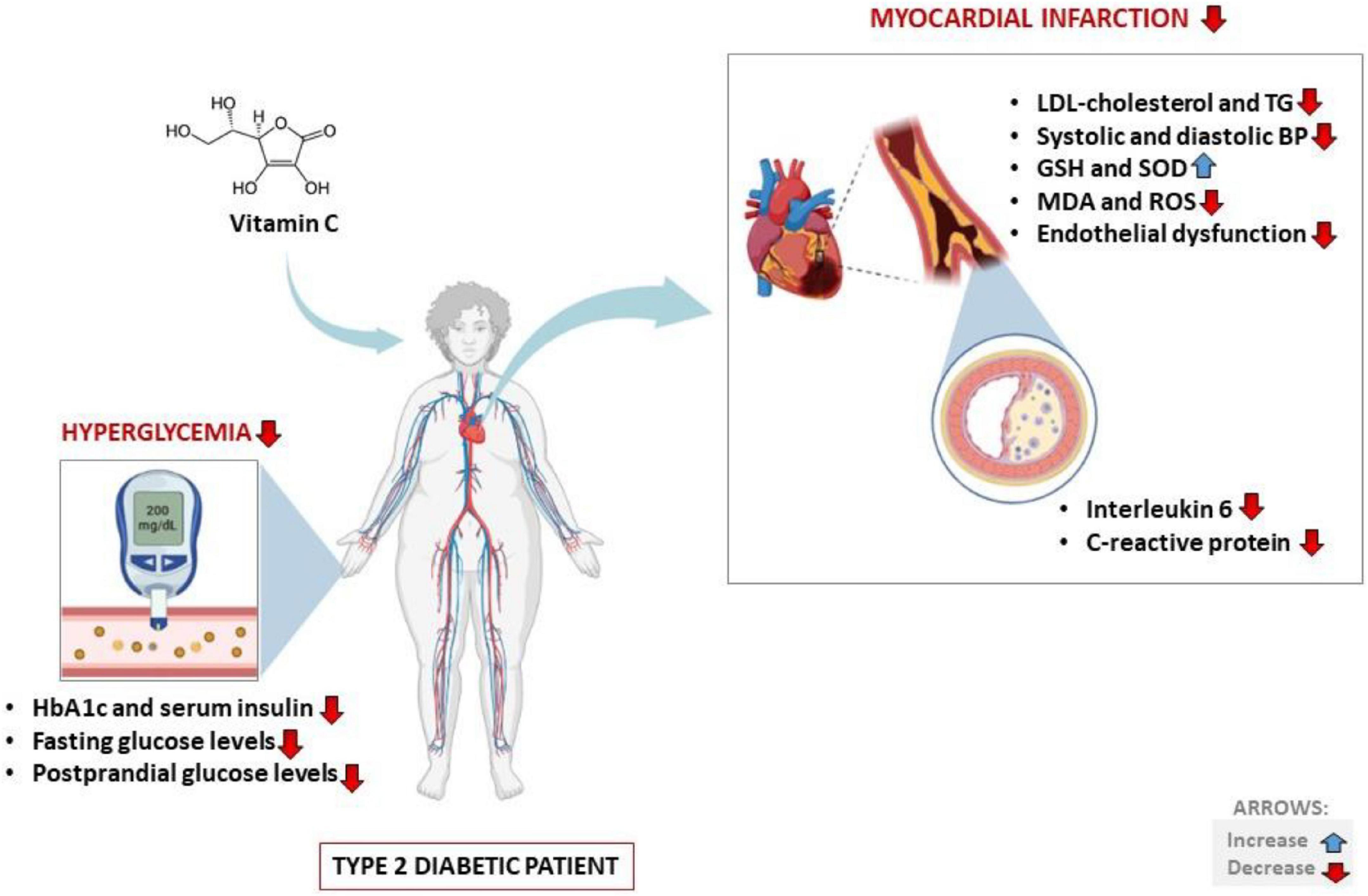
Figure 3. Potential health benefits of vitamin C intake on cardiovascular disease-related outcomes in type 2 diabetic patients. Briefly, besides improving basic metabolic parameters such as impaired glucose/insulin levels, vitamin C intake ca also lower total cholesterol concentrations to reduce blood pressure and positively affect blood circulation. HbA1c, glycated hemoglobin; LDL, low-density lipoprotein; TG, triglycerides; GSH, glutathione; SOD, superoxide dismutase; MDA, malondialdehyde; ROS, reactive oxygen species.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
PD, BN, and LT: concept and original draft. PD, BN, and TN: literature search and data extraction. VM, KM, and FN: assess quality of evidence. All authors: writing and final approval of the manuscript.
This work was supported in part by baseline funding from the Biomedical Research and Innovation Platform of the South African Medical Research Council (SAMRC) and the National Research Foundation (Grant numbers: 141929 and 117829).
BN is a University of KwaZulu-Natal Developing Research Innovation, Localisation and Leadership in South Africa (DRILL) fellow. DRILL is a NIH D43 grant (D43TW010131) awarded to UKZN in 2015 to support a research training and induction programme for early career academics. The work by KZ, reported herein was made possible through partial funding by the South African Medical Research Council through its Division of Research Capacity Development under the Researcher Development Award Programme.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The content hereof is the sole responsibility of the authors and do not necessarily represent the official views of the SAMRC or the funders.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1011002/full#supplementary-material
Supplementary file 1 | Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) checklist.
Supplementary file 2 | Downs and Black checklist.
CVD, cardiovascular disease; CRP, C reactive protein; DBP, diastolic blood pressure; FPG, fasting plasma glucose; IL, interleukin; GRADE, Grading of Recommendations Assessment Development and Evaluation; HbA1c, glycated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MDA, malondialdehyde; PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analysis; RCT, randomized controlled trials; SBP, systolic blood pressure; SMD, standard mean difference; T2D, type 2 diabetes.
1. World Health Organization [WHO]. The Top 10 Causes Of Death. Geneva: World Health Organization (2020).
2. Ng KW, Allen ML, Desai A, Macrae D, Pathan N. Cardioprotective effects of insulin: how intensive insulin therapy may benefit cardiac surgery patients. Circulation. (2012) 125:721–8. doi: 10.1161/CIRCULATIONAHA.111.063784
3. El Messaoudi S, Rongen GA, de Boer RA, Riksen NP. The cardioprotective effects of metformin. Curr Opin Lipidol. (2011) 22:445–53. doi: 10.1097/MOL.0b013e32834ae1a7
4. Chaudhury A, Duvoor C, Reddy Dendi VS, Kraleti S, Chada A, Ravilla R, et al. Clinical review of antidiabetic drugs: implications for type 2 diabetes mellitus management. Front Endocrinol. (2017) 8:6. doi: 10.3389/fendo.2017.00006
5. American Heart Association [AHA]. Cardiovascular Disease And Diabetes. Dallas, TX: American Heart Association (2022).
6. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. (2018) 17:83. doi: 10.1186/s12933-018-0728-6
7. Dludla PV, Dias SC, Obonye N, Johnson R, Louw J, Nkambule BB. A systematic review on the protective effect of N-acetyl cysteine against diabetes-associated cardiovascular complications. Am J Cardiovasc Drugs. (2018) 18:283–98. doi: 10.1007/s40256-018-0275-2
8. Dludla PV, Joubert E, Muller CJF, Louw J, Johnson R. Hyperglycemia-induced oxidative stress and heart disease-cardioprotective effects of rooibos flavonoids and phenylpyruvic acid-2-O-β-D-glucoside. Nutr Metab. (2017) 14:45. doi: 10.1186/s12986-017-0200-8
9. Park EJ, Pezzuto JM. The pharmacology of resveratrol in animals and humans. Biochim Biophys Acta. (2015) 1852:1071–113. doi: 10.1016/j.bbadis.2015.01.014
10. Zheng J, Cheng J, Zheng S, Feng Q, Xiao X. Curcumin, a polyphenolic curcuminoid with Its protective effects and molecular mechanisms in diabetes and diabetic cardiomyopathy. Front Pharmacol. (2018) 9:472. doi: 10.3389/fphar.2018.00472
11. De Blasio MJ, Huynh K, Qin C, Rosli S, Kiriazis H, Ayer A, et al. Therapeutic targeting of oxidative stress with coenzyme Q10 counteracts exaggerated diabetic cardiomyopathy in a mouse model of diabetes with diminished PI3K(p110alpha) signaling. Free Radic Biol Med. (2015) 87:137–47. doi: 10.1016/j.freeradbiomed.2015.04.028
12. Kong M, Xie K, Lv M, Li J, Yao J, Yan K, et al. Anti-inflammatory phytochemicals for the treatment of diabetes and its complications: lessons learned and future promise. Biomed Pharmacother. (2021) 133:110975. doi: 10.1016/j.biopha.2020.110975
13. Ansley DM, Wang B. Oxidative stress and myocardial injury in the diabetic heart. J Pathol. (2013) 229:232–41. doi: 10.1002/path.4113
14. Boudina S, Abel ED. Diabetic cardiomyopathy, causes and effects. Rev Endocr Metab Disord. (2010) 11:31–9. doi: 10.1007/s11154-010-9131-7
15. Calvano A, Izuora K, Oh EC, Ebersole JL, Lyons TJ, Basu A. Dietary berries, insulin resistance and type 2 diabetes: an overview of human feeding trials. Food Funct. (2019) 10:6227–43. doi: 10.1039/c9fo01426h
16. Derosa G, Limas CP, Macías PC, Estrella A, Maffioli P. Dietary and nutraceutical approach to type 2 diabetes. Arch Med Sci. (2014) 10:336–44. doi: 10.5114/aoms.2014.42587
17. Kahal H, Halama A, Aburima A, Bhagwat AM, Butler AE, Graumann J, et al. Effect of induced hypoglycemia on inflammation and oxidative stress in type 2 diabetes and control subjects. Sci Rep. (2020) 10:4750. doi: 10.1038/s41598-020-61531-z
18. Tapsell LC, Hemphill I, Cobiac L, Patch CS, Sullivan DR, Fenech M, et al. Health benefits of herbs and spices: the past, the present, the future. Med J Aust. (2006) 185:S1–24. doi: 10.5694/j.1326-5377.2006.tb00548.x
19. Yeh GY, Eisenberg DM, Kaptchuk TJ, Phillips RS. Systematic review of herbs and dietary supplements for glycemic control in diabetes. Diabetes Care. (2003) 26:1277–94. doi: 10.2337/diacare.26.4.1277
20. Dludla PV, Nkambule BB, Mazibuko-Mbeje SE, Nyambuya TM, Orlando P, Silvestri S, et al. Tea consumption and its effects on primary and secondary prevention of coronary artery disease: qualitative synthesis of evidence from randomized controlled trials. Clin Nutr ESPEN. (2021) 41:77–87. doi: 10.1016/j.clnesp.2020.11.006
21. Mahmoud AM, Hernandez Bautista RJ, Sandhu MA, Hussein OE. Beneficial effects of citrus flavonoids on cardiovascular and metabolic health. Oxid Med Cell Longev. (2019) 2019:5484138. doi: 10.1155/2019/5484138
22. Ashor AW, Werner AD, Lara J, Willis ND, Mathers JC, Siervo M. Effects of vitamin C supplementation on glycaemic control: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr. (2017) 71:1371–80.
23. Gordon DS, Rudinsky AJ, Guillaumin J, Parker VJ, Creighton KJ. Vitamin C in health and disease: a companion animal focus. Top Companion Anim Med. (2020) 39:100432. doi: 10.1016/j.tcam.2020.100432
24. Kawashima A, Sekizawa A, Koide K, Hasegawa J, Satoh K, Arakaki T, et al. Vitamin C induces the reduction of oxidative stress and paradoxically stimulates the apoptotic gene expression in extravillous trophoblasts derived from first-trimester tissue. Reprod Sci. (2015) 22:783–90. doi: 10.1177/1933719114561561
25. Ryan MJ, Dudash HJ, Docherty M, Geronilla KB, Baker BA, Haff GG, et al. Vitamin E and C supplementation reduces oxidative stress, improves antioxidant enzymes and positive muscle work in chronically loaded muscles of aged rats. Exp Gerontol. (2010) 45:882–95. doi: 10.1016/j.exger.2010.08.002
26. Mason SA, Keske MA, Wadley GD. Effects of vitamin C supplementation on glycemic control and cardiovascular risk factors in people with type 2 diabetes: a GRADE-assessed systematic review and meta-analysis of randomized controlled trials. Diabetes Care. (2021) 44:618–30. doi: 10.2337/dc20-1893
27. Morelli MB, Gambardella J, Castellanos V, Trimarco V, Santulli G. Vitamin C and cardiovascular disease: an update. Antioxidants. (2020) 9:1227. doi: 10.3390/antiox9121227
28. Ashor AW, Brown R, Keenan PD, Willis ND, Siervo M, Mathers JC. Limited evidence for a beneficial effect of vitamin C supplementation on biomarkers of cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. Nutr Res. (2019) 61:1–12. doi: 10.1016/j.nutres.2018.08.005
29. Zhu N, Huang B, Jiang W. Targets of vitamin C with therapeutic potential for cardiovascular disease and underlying mechanisms: a study of network pharmacology. Front Pharmacol. (2020) 11:591337. doi: 10.3389/fphar.2020.591337
30. Tareke AA, Hadgu AA. The effect of vitamin C supplementation on lipid profile of type 2 diabetic patients: a systematic review and meta-analysis of clinical trials. Diabetol Metab Syndr. (2021) 13:24. doi: 10.1186/s13098-021-00640-9
31. Ashor AW, Lara J, Mathers JC, Siervo M. Effect of vitamin C on endothelial function in health and disease: a systematic review and meta-analysis of randomised controlled trials. Atherosclerosis. (2014) 235:9–20. doi: 10.1016/j.atherosclerosis.2014.04.004
32. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. (1998) 52:377–84. doi: 10.1136/jech.52.6.377
33. O’Connor SR, Tully MA, Ryan B, Bradley JM, Baxter GD, McDonough SM. Failure of a numerical quality assessment scale to identify potential risk of bias in a systematic review: a comparison study. BMC Res Notes. (2015) 8:224. doi: 10.1186/s13104-015-1181-1
34. Morel O, Jesel L, Hugel B, Douchet MP, Zupan M, Chauvin M, et al. Protective effects of vitamin C on endothelium damage and platelet activation during myocardial infarction in patients with sustained generation of circulating microparticles. J Thromb Haemost. (2003) 1:171–7. doi: 10.1046/j.1538-7836.2003.00010.x
35. Mullan BA, Ennis CN, Fee HJ, Young IS, McCance DR. Protective effects of ascorbic acid on arterial hemodynamics during acute hyperglycemia. Am J Physiol Heart Circ Physiol. (2004) 287:H1262–8. doi: 10.1152/ajpheart.00153.2003
36. Davison GW, Ashton T, George L, Young IS, McEneny J, Davies B, et al. Molecular detection of exercise-induced free radicals following ascorbate prophylaxis in type 1 diabetes mellitus: a randomised controlled trial. Diabetologia. (2008) 51:2049–59. doi: 10.1007/s00125-008-1101-1
37. Paolisso G, Balbi V, Volpe C, Varricchio G, Gambardella A, Saccomanno F, et al. Metabolic benefits deriving from chronic vitamin C supplementation in aged non-insulin dependent diabetics. J Am Coll Nutr. (1995) 14:387–92. doi: 10.1080/07315724.1995.10718526
38. Mason SA, Della Gatta PA, Snow RJ, Russell AP, Wadley GD. Ascorbic acid supplementation improves skeletal muscle oxidative stress and insulin sensitivity in people with type 2 diabetes: findings of a randomized controlled study. Free Radic Biol Med. (2016) 93:227–38. doi: 10.1016/j.freeradbiomed.2016.01.006
39. Mason SA, Rasmussen B, van Loon LJC, Salmon J, Wadley GD. Ascorbic acid supplementation improves postprandial glycaemic control and blood pressure in individuals with type 2 diabetes: findings of a randomized cross-over trial. Diabetes Obes Metab. (2019) 21:674–82. doi: 10.1111/dom.13571
40. McAuliffe AV, Brooks BA, Fisher EJ, Molyneaux LM, Yue DK. Administration of ascorbic acid and an aldose reductase inhibitor (tolrestat) in diabetes: effect on urinary albumin excretion. Nephron. (1998) 80:277–84. doi: 10.1159/000045187
41. Mayer-Davis EJ, Monaco JH, Marshall JA, Rushing J, Juhaeri. Vitamin C intake and cardiovascular disease risk factors in persons with non-insulin-dependent diabetes mellitus. from the insulin resistance atherosclerosis study and the san luis valley diabetes study. Prev Med. (1997) 26:277–83. doi: 10.1006/pmed.1997.0145
42. Song Y, Cook NR, Albert CM, Van Denburgh M, Manson JE. Effects of vitamins C and E and beta-carotene on the risk of type 2 diabetes in women at high risk of cardiovascular disease: a randomized controlled trial. Am J Clin Nutr. (2009) 90:429–37. doi: 10.3945/ajcn.2009.27491
43. Lu Q, Bjorkhem I, Wretlind B, Diczfalusy U, Henriksson P, Freyschuss A. Effect of ascorbic acid on microcirculation in patients with Type II diabetes: a randomized placebo-controlled cross-over study. Clin Sci. (2005) 108:507–13. doi: 10.1042/CS20040291
44. Ellulu MS, Rahmat A, Patimah I, Khaza’ai H, Abed Y. Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: a randomized controlled trial. Drug Des Devel Ther. (2015) 9:3405–12. doi: 10.2147/DDDT.S83144
45. Chen H, Karne RJ, Hall G, Campia U, Panza JA, Cannon RO, et al. High-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am J Physiol Heart Circ Physiol. (2006) 290:H137–45. doi: 10.1152/ajpheart.00768.2005
46. Anderson RA, Evans LM, Ellis GR, Khan N, Morris K, Jackson SK, et al. Prolonged deterioration of endothelial dysfunction in response to postprandial lipaemia is attenuated by vitamin C in Type 2 diabetes. Diabet Med. (2006) 23:258–64. doi: 10.1111/j.1464-5491.2005.01767.x
47. Darko D, Dornhorst A, Kelly FJ, Ritter JM, Chowienczyk PJ. Lack of effect of oral vitamin C on blood pressure, oxidative stress and endothelial function in Type II diabetes. Clin Sci. (2002) 103:339–44. doi: 10.1042/cs1030339
48. Afkhami-Ardekani M, Shojaoddiny-Ardekani A. Effect of vitamin C on blood glucose, serum lipids & serum insulin in type 2 diabetes patients. Indian J Med Res. (2007) 126:471–4.
49. Gutierrez AD, Duran-Valdez E, Robinson I, de Serna DG, Schade DS. Does short-term vitamin C reduce cardiovascular risk in type 2 diabetes? Endocr Pract. (2013) 19:785–91. doi: 10.4158/EP12431.OR
50. Klein F, Juhl B, Christiansen JS. Unchanged renal haemodynamics following high dose ascorbic acid administration in normoalbuminuric IDDM patients. Scand J Clin Lab Invest. (1995) 55:53–9. doi: 10.3109/00365519509075378
51. Mazloom Z, Hejazi N, Dabbaghmanesh MH, Tabatabaei HR, Ahmadi A, Ansar H. Effect of vitamin C supplementation on postprandial oxidative stress and lipid profile in type 2 diabetic patients. Pak J Biol Sci. (2011) 14:900–4. doi: 10.3923/pjbs.2011.900.904
52. Tousoulis D, Antoniades C, Tountas C, Bosinakou E, Kotsopoulou M, Toutouzas P. Vitamin C affects thrombosis/fibrinolysis system and reactive hyperemia in patients with type 2 diabetes and coronary artery disease. Diabetes Care. (2003) 26:2749–53. doi: 10.2337/diacare.26.10.2749
53. Upritchard JE, Sutherland WH, Mann JI. Effect of supplementation with tomato juice, vitamin E, and vitamin C on LDL oxidation and products of inflammatory activity in type 2 diabetes. Diabetes Care. (2000) 23:733–8. doi: 10.2337/diacare.23.6.733
54. Mullan BA, Young IS, Fee H, McCance DR. Ascorbic acid reduces blood pressure and arterial stiffness in type 2 diabetes. Hypertension. (2002) 40:804–9. doi: 10.1161/01.hyp.0000039961.13718.00
55. Internation Diabetes Federation [IDF]. IDF Diabetes Atlas. 10th ed. Brussels: Internation Diabetes Federation (2022).
56. Pandey A, Tripathi P, Pandey R, Srivatava R, Goswami S. Alternative therapies useful in the management of diabetes: a systematic review. J Pharm Bioallied Sci. (2011) 3:504–12. doi: 10.4103/0975-7406.90103
57. Lopez-Moreno J, Quintana-Navarro GM, Delgado-Lista J, Garcia-Rios A, Alcala-Diaz JF, Gomez-Delgado F, et al. Mediterranean diet supplemented with coenzyme Q10 modulates the postprandial metabolism of advanced glycation end products in elderly men and women. J Gerontol A Biol Sci Med Sci. (2018) 73:340–6. doi: 10.1093/gerona/glw214
58. Skeie G, Braaten T, Hjartaker A, Lentjes M, Amiano P, Jakszyn P, et al. Use of dietary supplements in the european prospective investigation into cancer and nutrition calibration study. Eur J Clin Nutr. (2009) 63(Suppl. 4):S226–38. doi: 10.1038/ejcn.2009.83
59. World Health Organization [WHO]. WHO Model Lists of Essential Medicines. Geneva: World Health Organization (2022).
60. Traber MG, Stevens JF. Vitamins C and E: beneficial effects from a mechanistic perspective. Free Radic Biol Med. (2011) 51:1000–13. doi: 10.1016/j.freeradbiomed.2011.05.017
61. Padayatty SJ, Levine M. Vitamin C: the known and the unknown and goldilocks. Oral Dis. (2016) 22:463–93. doi: 10.1111/odi.12446
62. Levine M, Rumsey SC, Daruwala R, Park JB, Wang Y. Criteria and recommendations for vitamin C intake. JAMA. (1999) 281:1415–23. doi: 10.1001/jama.281.15.1415
63. Pitsavos C, Panagiotakos D, Weinem M, Stefanadis C. Diet, exercise and the metabolic syndrome. Rev Diabet Stud. (2006) 3:118–26. doi: 10.1900/RDS.2006.3.118
64. Riccardi G, Giacco R, Rivellese AA. Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr. (2004) 23:447–56. doi: 10.1016/j.clnu.2004.02.006
65. Blekkenhorst LC, Sim M, Bondonno CP, Bondonno NP, Ward NC, Prince RL, et al. Cardiovascular health benefits of specific vegetable types: a narrative review. Nutrients. (2018) 10:595. doi: 10.3390/nu10050595
66. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. (2017) 46:1029–56. doi: 10.1093/ije/dyw319
67. Soare A, Weiss EP, Holloszy JO, Fontana L. Multiple dietary supplements do not affect metabolic and cardio-vascular health. Aging. (2014) 6:149–57. doi: 10.18632/aging.100597
68. Krajcovicová-Kudlácková M, Pauková V, Baceková M, Dusinská M. Lipid peroxidation in relation to vitamin C and vitamin E levels. Cent Eur J Public Health. (2004) 12:46–8.
69. Amini L, Chekini R, Nateghi MR, Haghani H, Jamialahmadi T, Sathyapalanet T. The effect of combined vitamin C and vitamin E supplementation on oxidative stress markers in women with endometriosis: a randomized, triple-blind placebo-controlled clinical trial. Pain Res Manag. (2021) 2021:5529741. doi: 10.1155/2021/5529741
70. Boonthongkaew C, Tong-Un T, Kanpetta Y, Chaungchot N, Leelayuwat C, Leelayuwat N. Vitamin C supplementation improves blood pressure and oxidative stress after acute exercise in patients with poorly controlled type 2 diabetes mellitus: a randomized, placebo-controlled, cross-over study. Chin J Physiol. (2021) 64:16–23. doi: 10.4103/cjp.cjp_95_20
71. Lee DH, Folsom AR, Harnack L, Halliwell B, Jacobs DR Jr. Does supplemental vitamin C increase cardiovascular disease risk in women with diabetes? Am J Clin Nutr. (2004) 80:1194–200. doi: 10.1093/ajcn/80.5.1194
72. Sesso HD, Buring JE, Christen WG, Kurth T, Belanger C, MacFadyen J, et al. Vitamins E and C in the prevention of cardiovascular disease in men: the Physicians’ Health Study II randomized controlled trial. JAMA. (2008) 300:2123–33. doi: 10.1001/jama.2008.600
73. Wold LE, Ren J. Streptozotocin directly impairs cardiac contractile function in isolated ventricular myocytes via a p38 map kinase-dependent oxidative stress mechanism. Biochem Biophys Res Commun. (2004) 318:1066–71. doi: 10.1016/j.bbrc.2004.04.138
74. Jiang Z, Li H, Schroer SA, Voisin V, Ju Y, Pacal M, et al. Hypophosphorylated pRb knock-in mice exhibit hallmarks of aging and vitamin C-preventable diabetes. EMBO J. (2022) 41:e106825. doi: 10.15252/embj.2020106825
75. Chen C, Han M, Zhang W, Cui J, Cui N, Cao L, et al. Identification of key genes and pathways in type 2 diabetes mellitus and vitamin C metabolism through bioinformatics analysis. Asia Pac J Clin Nutr. (2021) 30:715–29. doi: 10.6133/apjcn.202112_30(4).0018
76. Özerkan D, Özsoy N, Cebesoy S, Özer Ç. Distribution of spleen connective tissue fibers in diabetic and vitamin C treated diabetic rats. Biotech Histochem. (2021) 96:347–53. doi: 10.1080/10520295.2020.1795718
77. Johansen JS, Harris AK, Rychly DJ, Ergul A. Oxidative stress and the use of antioxidants in diabetes: linking basic science to clinical practice. Cardiovasc Diabetol. (2005) 4:5. doi: 10.1186/1475-2840-4-5
78. National Library of Medicine, through National Centre for Biotechnology Information. Vitamin C And Diabetes. (2022). Available online at: https://pubmed.ncbi.nlm.nih.gov/?term=vitamin+c+and+diabetes&filter=pubt.randomizedcontrolledtrial (accessed Sept 13, 2022).
Keywords: vitamin C, dietary supplements, antioxidants, diabetes mellitus, metabolic syndrome, cardiovascular diseases
Citation: Dludla PV, Nkambule BB, Nyambuya TM, Ziqubu K, Mabhida SE, Mxinwa V, Mokgalaboni K, Ndevahoma F, Hanser S, Mazibuko-Mbeje SE, Basson AK, Sabbatinelli J and Tiano L (2022) Vitamin C intake potentially lowers total cholesterol to improve endothelial function in diabetic patients at increased risk of cardiovascular disease: A systematic review of randomized controlled trials. Front. Nutr. 9:1011002. doi: 10.3389/fnut.2022.1011002
Received: 03 August 2022; Accepted: 29 September 2022;
Published: 31 October 2022.
Edited by:
Ming Yang, Sichuan University, ChinaReviewed by:
Mahesh Kumar Samota, Central Institute of Post-Harvest Engineering and Technology (ICAR), IndiaCopyright © 2022 Dludla, Nkambule, Nyambuya, Ziqubu, Mabhida, Mxinwa, Mokgalaboni, Ndevahoma, Hanser, Mazibuko-Mbeje, Basson, Sabbatinelli and Tiano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Phiwayinkosi V. Dludla, cGRsdWRsYUBtcmMuYWMuemE=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.