- 1Qods Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
- 2Department of Community Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
- 3Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
- 4Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
- 5School of Nutrition, Toronto Metropolitan University, Toronto, ON, Canada
- 6Diabetes Research Center, Endocrinology and Metabolism Clinical Sciences Institute, Tehran University of Medical Sciences, Tehran, Iran
Background: Food security is a fundamental human right that must be upheld to preserve excellent general welfare, and mental, physical, and social health. However, according to the United Nations Food and Agriculture Organization (FAO) report in 2020, the level of food insecurity in the world is increasing.
Objective: Determining the prevalence of food insecurity in Iran will be beneficial for Iran and other low-middle-income countries.
Methods: We searched both English and Persian (Iranian) databases including PubMed, Scopus, Web of Science, Google Scholar, SID, Irandoc, Magiran, Civilica, and Iranian Medical Sciences Theses System from 01 January 1990 to 01 February 2022. Observational studies that reported the prevalence of household food insecurity among a healthy Iranian population and assessed food insecurity at the individual or household level using validated questionnaires were included.
Results: One hundred six studies and/or theses with a total of 152, 300 participants met the review criteria. Our analyses demonstrated that the prevalence of food insecurity among the healthy Iranian population was 55.9% (95% CI: 52.6–59.2%) and the highest prevalence of food insecurity was in the western regions with 64.8% (95% CI: 57.7–72.0%). Subgroup analyses showed that food insecurity among women at 51.3% (95% CI: 45.1–57.6%) and rural inhabitants at 66.1% (95% CI: 58.8–73.4%) was significantly higher than men at 47.8% (95% CI: 41.8–53.8%) and urban residents at 47.1% (95% CI: 44.1–50.0%), respectively. Among the age groups, the highest prevalence of food insecurity was in adults at 56.5% (95% CI: 51.7–61.2%).
Conclusion: The prevalence of food insecurity in a healthy Iranian population was higher than the global average. Women, rural residents, and residents of the western regions of Iran had a higher prevalence of food insecurity. These groups should be prioritized in programs to reduce the prevalence of food insecurity in Iran.
Systematic review registration: www.crd.york.ac.uk/PROSPERO, identifier: CRD42022328473.
Introduction
Household food security has been defined as all members having adequate access to safe food through socially acceptable means for active and healthy life (1). Limited or uncertain sources of adequate and safe nutritional foods or the limited or uncertain ability to acquire food lead to food insecurity (FI). FI is a public health challenge around the world and millions of households are struggling to maintain or achieve food security, which includes availability, access, utilization, and ability (2, 3). It is not considered a static state and is on a spectrum (3). According to the United Nations in 2021, there is a higher prevalence of FI since the beginning of the COVID-19 pandemic compared to before the pandemic (4). The prevalence of household FI in north Iran has been estimated to be ~50.8% in total with 43.2% mild FI, 6.5% moderate FI, and 1.1% severe FI (5), which may have increased in recent years due to the COVID-19 pandemic and other economic and social issues.
Various methods are used to evaluate FI, two of which are used the most: (1) estimation of food consumption and (2) estimation of the cost of food preparation (6). These methods have limitations due to the cost, participant burden, and the need for an expert interviewer. Recently, “experiential” or “perception-based” methods have been used to measure FI (7). Under these methods, individual experience of FI (i.e., access) is measured through a survey and summarized in a scale. The Household Food Security Survey Module (HFSSM) has been consistently validated as a reliable and significant perception-based measure of FI in the United States (8). In Iran, FI is mainly investigated by measuring the adequacy of energy and nutrients using food questionnaires or by estimating the poverty line from income and expenditure surveys (6). FI is a threat to the health and survival of individuals within communities and can have both short- and long-term effects (9). Several factors influence the prevalence of FI including population growth, industrialization of communities, growing migration from rural to urban areas, inadequate levels of education, wars and economic sanctions by governments, pandemics or endemic diseases, and weather changes (10–12). In addition, FI can include a wide range of health-related conditions from undernutrition to overnutrition. Undernutrition includes wasting, underweight, stunting, anemia, and other diseases associated with nutritional deficiencies. Overnutrition can lead to chronic conditions such as obesity, diabetes, fatty liver, hypertension, poor mental health, and metabolic syndrome (13–17). As a result, a large burden is faced by the economy and society (5).
Several studies have been conducted to investigate the prevalence, causes, and types of FI around the world and in Iran. According to a meta-analysis from West Africa, the prevalence of FI in the rural population was ~60.91% and the highest prevalence was among large families, female-headed households, and low-income households with low education levels (10). Several systematic reviews and meta-analyses have been conducted in Iran (6, 11, 12). In a meta-analysis from 2017, the prevalence of FI was 49.2% based on studies that evaluated FI using questionnaires (12). Since the publication of the previous meta-analysis, many studies have been published evaluating the status of FI in Iran. Considering this, a new meta-analysis is warranted to provide updated results and summarize recent findings. Therefore, the objective of this systematic review and meta-analysis is to update the findings and conduct a more comprehensive review of the prevalence of FI with the consideration of multiple subgroups and other factors.
Method
This systematic review and meta-analysis were conducted based on the Preferred Reporting Items for Systematic Review and Meta-Analysis statement (PRISMA) guideline (18). The protocol of the present study was registered on the PROSPERO website (www.crd.york.ac.uk/PROSPERO) (PROSPERO registration number = CRD42022328473).
Search strategy and information sources
International scientific databases including Web of Science, PubMed, Scopus, Google Scholar, and Iranian databases (HYPERLINKs: “https://www.sid.ir/fa/journal/,” “https://ganj.irandoc.ac.ir/,” “https://www.magiran.com/paperadvancedsearch,” “http://thesis.research.ac.ir/faces/home.jspx,” and “https://civilica.com/”) were searched from 01 January 1990 to 01 February 2022 to identify relevant studies. The detailed search strategy is shown in Supplementary Table 1.
Inclusion and exclusion criteria
Inclusion criteria were (a) observational studies (cross-sectional and cohort studies), (b) studies published between 1990 and 2022, (c) studies with a healthy Iranian population, (d) studies that reported the prevalence and/or at least one associated factor with household FI, and (e) studies that assessed FI at the individual or household level using validated questionnaires. Gray literature from credible sources was included. Exclusion criteria were intervention studies, abstract studies, studies performed on pregnant women, and populations with evidence of specific diseases.
Quality assessment
The Joanna Briggs Institute (JBI) quality assessment checklist was used to perform the quality assessment of the published articles (19). Two independent researchers (HA and PS) conducted a quality assessment for each of the included studies. Studies that received scores of ≥5 were categorized as low risk or good quality and studies with scores of ≤4 were categorized as high risk or poor quality.
Study selection and data extraction
Two independent reviewers (HA and PS) screened the studies based on the eligibility criteria. The abstracts and titles of the studies were reviewed, and the included full-text studies were evaluated. Any disagreements were addressed by a third reviewer's decision.
The following data were extracted from the included studies: the name of the first author, publication year, study design, province, geographical zone, urban/rural, gender, sample size, and prevalence of household food insecurity and relevant FI factors.
Data synthesis and statistical analysis
Pooled estimates for the magnitude of household food insecurity were calculated using a random effects model and metaprop module in Stata 14.2. The reason for using a random effects model was to attempt to account for the methodological differences within the included articles. A binomial distribution formula was used to estimate standard errors for each sample (20). The Egger's test and Trim and Fill test were used to evaluate publication bias. A funnel plot of symmetry visualized publication bias graphically. Evidence of statistically significant publication bias was considered a p-value < 0.05. Sensitivity analyses were performed by removing the studies that showed evidence of potential publication bias (21). The heterogeneity between studies was assessed using the I2 test (22). Subgroup analyses were conducted based on geographic region, age groups, type of questionnaire, quality of studies, location, and gender. Using meta-regression analysis, we examined the presence of any linear relationship between observed effect size and time. Evidence of a significant difference within the subgroups by the test of group difference was considered P < 0.05.
Results
A total of 6,164 articles and theses were retrieved from the initial database search. After the removal of duplicates, 3,468 studies remained to be screened. Title and abstracts were screened yielding 195 studies for full-text review. One hundred six studies (96 cross-sectional articles and 10 theses) published between 2010 and 2021 including a total of 152,300 participants were included after a full-text review and for data extraction. Study selection is presented in the PRISMA flowchart (Figure 1).
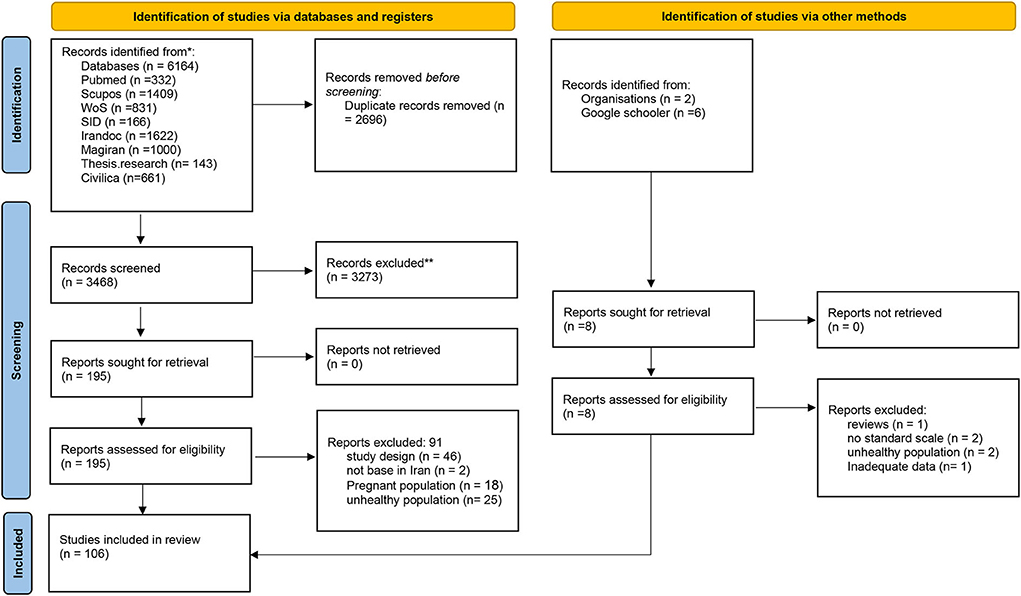
Figure 1. PRISMA flow diagram for study selection from: Page et al. (23). For more information, visit: http://www.prisma-statement.org/.
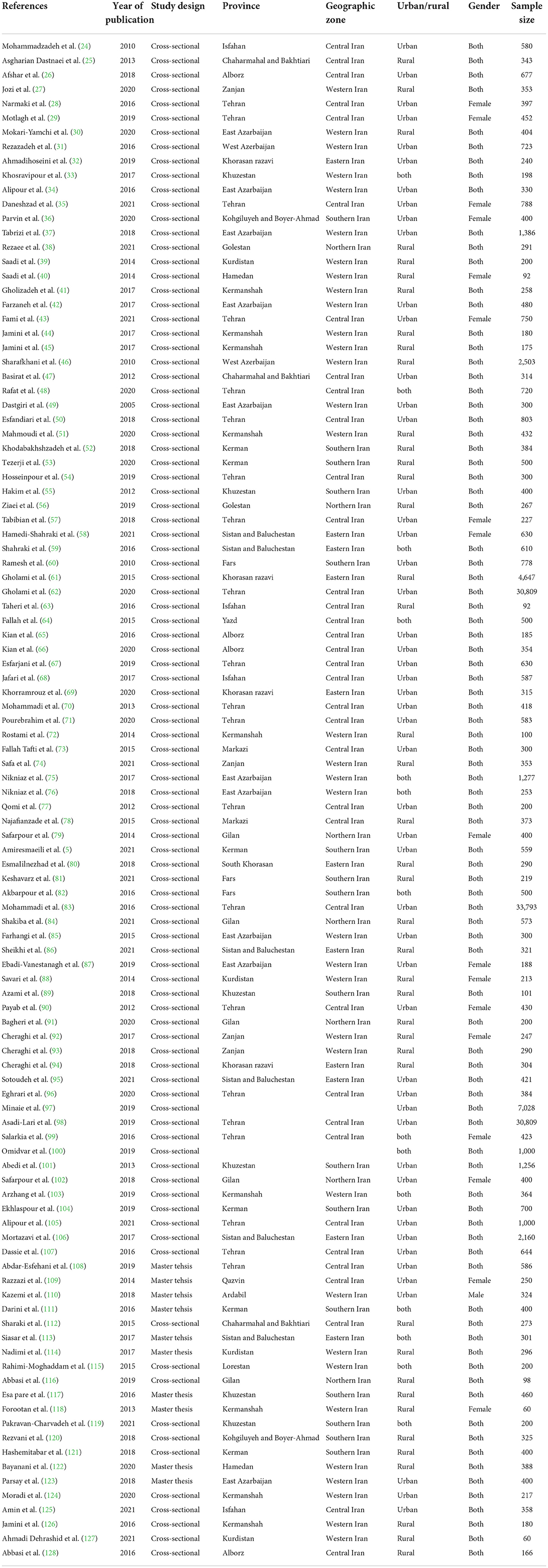
The characteristics of the included studies are shown in Table 1. Since some of the studies reported FI in different locations or genders, we considered them as separate studies. Of the included studies, 51 examined FI in urban areas, 41 in rural areas, and 14 in both areas. Included studies also investigated FI among men and women (n = 70), men (n= 20), and women (n= 35). In addition, studies were conducted on different age groups, including children (n = 14), adolescents (n = 6), adults (n = 45), and older adults (n = 9). Studies were conducted in several different locations including the central (n = 36), western (n = 34), southern (n = 16), northern (n = 7), and eastern (n = 11) parts of the country. Different questionnaires were used to assess FI including the United States Department of Agriculture 18-item Household Food Security Survey Module (USDA 18-item questionnaire) (n = 48), Household Food Insecurity Access Scale (HFIAS) (n = 32), US Department of Agriculture 6-item Household Food Security Survey Module (USDA 6-item) (n = 12), Radimer-Cornell (n = 6), Farsi Current Population Survey-Food Security Survey Module (FaCPS-FSSM) (n = 3), and the Coping Strategies Index (n = 3).
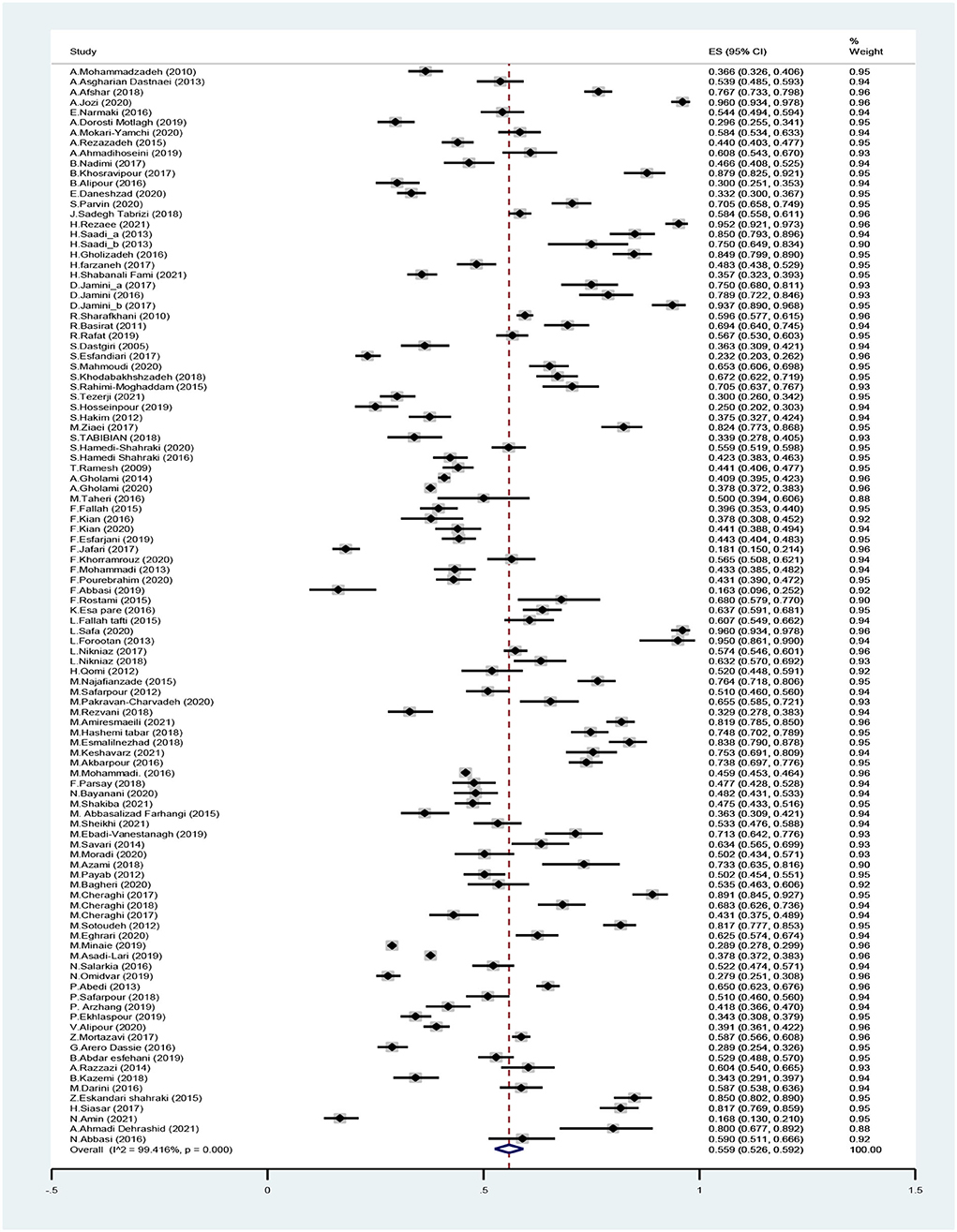
According to the meta-analysis, the total prevalence of FI in Iran was 55.9% (95% CI: 52.6–59.2%) (Figure 2). To determine heterogeneity, meta-regression and subgroup analyses were conducted.
Subgroups and meta-regression analyses
The prevalence of FI in rural areas was 66.1% (95% CI: 58.8–73.4%) which was higher than the prevalence of FI in urban areas [47.1% (95% CI: 44.1–50.0%)] (Supplementary Figure 1). The prevalence of FI among women was higher [51.3% (95% CI: 45.1–57.6%) than the prevalence among men (47.8% (95% CI: 41.8–53.8%)] (Supplementary Figure 2). Pooled prevalence of FI was 44.7% (95% CI: 35.5–53.9%) in children, 40.6% (95% CI: 33.2–48.0%) in adolescents, 56.5% (95% CI: 51.7–61.2%) in adults, and 49.8 % (95% CI: 36.6–63.0%) in older adults.
Subgroup analyses by region revealed that the highest prevalence of FI was in the western part of the country [64.8% (95% CI: 57.7–72.0%)] and the lowest prevalence of FI was in the central part of the country [46.1% (95% CI: 43.1–49.2%)]. The prevalence of FI was also assessed according to questionnaires used in the studies. The prevalence of FI in studies that used USDA 18-item was 54.8% (95% CI: 49.0–60.6%), the HFIAS was 58.4% (95% CI: 49.8–67.1%), and the USDA 6-item was 48.2% (95% CI: 44.3–52.0 %). The highest prevalence of FI was 77.8 % (95% CI: 69.1–93.8%) in studies that used the Coping Strategies Index. Moreover, the prevalence was 53.4% (95% CI: 43.0–63.7%) in studies that used FaCPS-FSSM and 63.2% (95% CI: 38.2–88.1%) in studies that used Radimer-Cornell (Table 2). Meta-regression analyses using random effects models were conducted to analyze the change in the prevalence of FI over time; however, results indicated that there were no significant changes in FI over time (Figure 3).
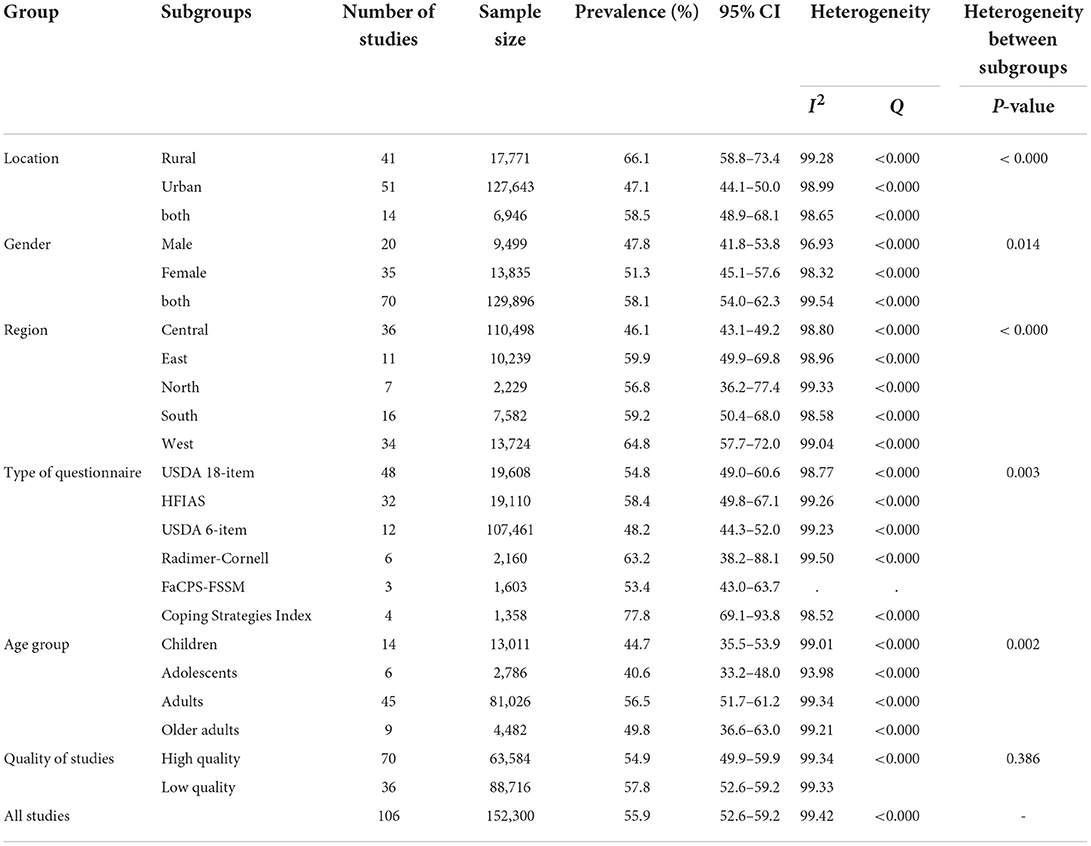
Table 2. Food insecurity prevalence data by location, sex, region, age group, quality of studies, and assessment tool.
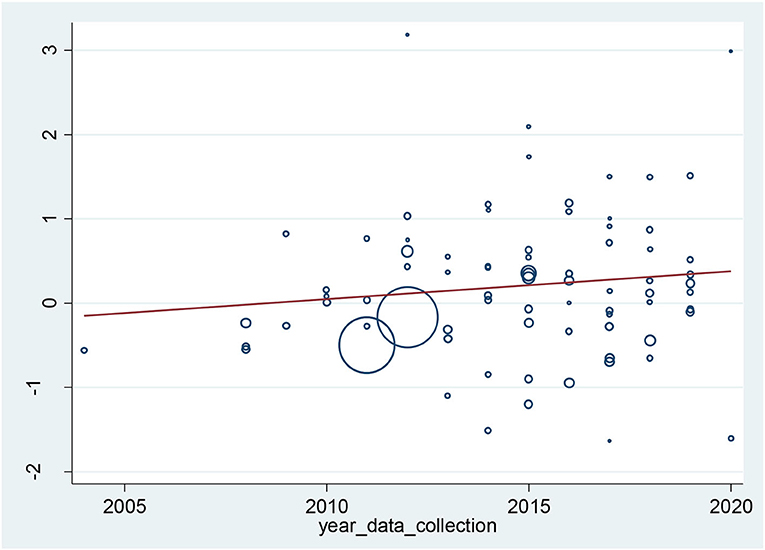
Figure 3. Association of the prevalence of food insecurity in households with years of data collection.
Quality assessment
The Joanna Briggs Institute (JBI) quality assessment checklist was used to assess the quality of the published articles (19). According to the checklist, 70 studies were categorized as high quality and 36 studies were categorized as low quality (Supplementary Table 2). Subgroup analysis revealed no evidence of a statistical difference between the two groups.
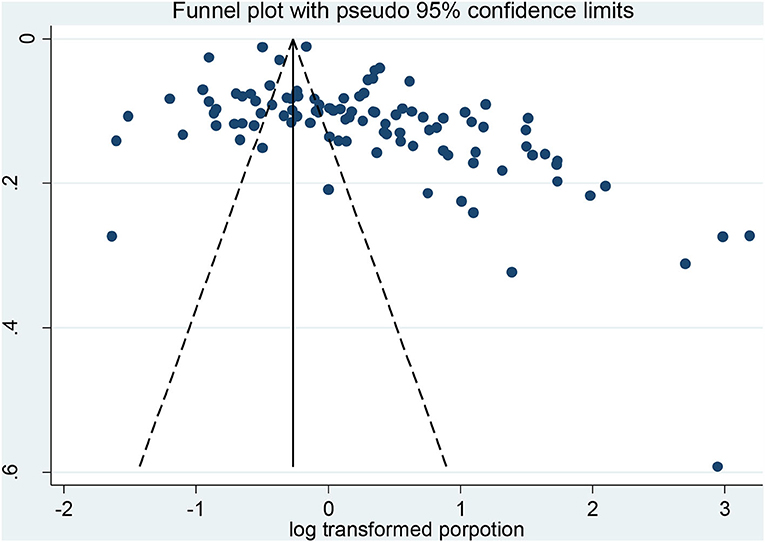
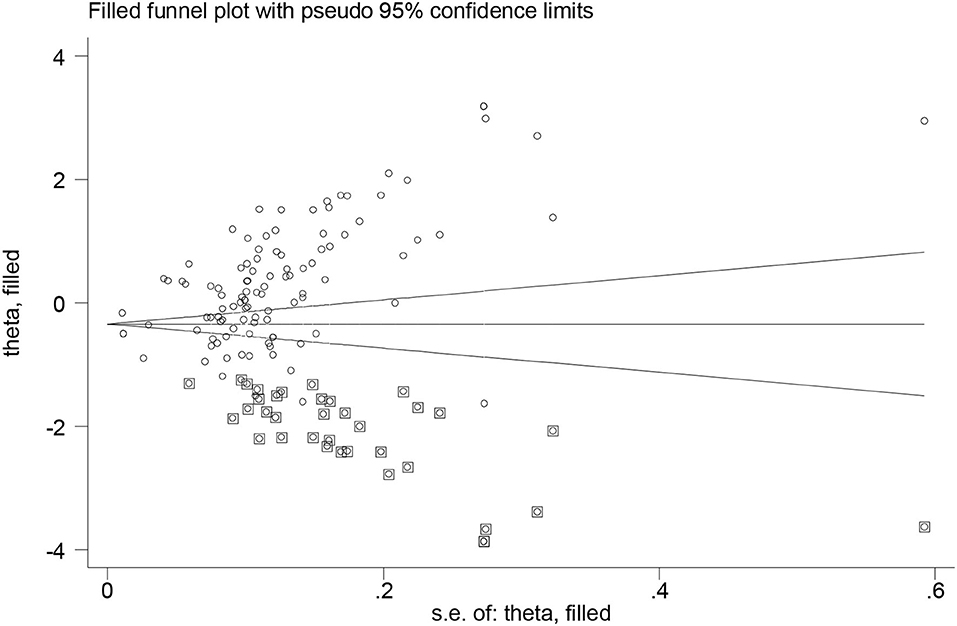
Publication bias
Despite searching several databases, searching gray literature, and not having language limitations, the results of the funnel plot (Figure 4) and Egger's test (P < 0.000) revealed evidence of publication bias. The trim and fill method using random effects was used to adjust the pooled prevalence estimates for publication bias. After imputing 36 studies below the mean, the result indicated an adjusted prevalence of 74.6% (95% CI: 67.3–82.7%) among participants (Figure 5). Furthermore, there was a significant heterogeneity between subgroups based on the region (P-value < 0.000), gender (P-value = 0.017), type of FI questionnaire (P-value = 0.004), and location (P-value < 0.000).
Sensitivity analysis
Sensitivity analysis suggested that there were no changes in the mean prevalence after the removal of individual studies (Supplementary Figure 3).
Discussion
The present systematic review and meta-analysis evaluated the prevalence of FI in Iran examining 106 articles and theses among 152,300 participants from 2010 to 2021 with the consideration of gender, geographical areas, age groups, location, and type of questionnaires. According to the United Nations International Children's Emergency Fund (UNICEF), about 375.8 million people in Asian countries including Iran and the Pacific faced hunger in 2020, which increased by nearly 54 million people compared to 2019. Moreover, more than 1.1 billion people did not have access to adequate food in 2020 (129). Based on the present meta-analysis, the total prevalence of FI in Iran was 55.9% (95% CI: 52.6–59.2%), which is considered high. A previous meta-analysis evaluating FI in Iran also revealed a high prevalence of FI among different age categories (6, 11, 12). Differences in inclusion and exclusion criteria could be considered a potential reason for the contrasting findings. Additionally, this present study evaluated a greater amount of studies over several databases using a comprehensive search strategy.
In this study, subgroup analyses were performed based on identified factors to evaluate FI prevalence comprehensively. Subgroup analyses revealed that FI prevalence was significantly higher in Iranian women compared to men (51.3 vs. 47.8%, p < 0.000). In line with our findings, Diab-El-Harake et al. found a higher prevalence of FI in women living in Arab countries (130). In addition, a meta-analysis conducted by Jung et al. found that female-headed households were 75% (95 % CI: 49–96%) more likely to experience FI compared to male-headed households (131). Another meta-analysis in Ethiopia also found a higher FI prevalence in female-headed households (132). Furthermore, based on the 2019 State of FI report, the prevalence of FI was higher among women compared to men in every continent from 2016 to 2019 (133). Broussard (134) suggested that a higher prevalence of FI may be explained by differences in household income, social networks, and educational attainment. Furthermore, that gender differences in income accounted for more than 70% of the gender gap in FI, and lower educational attainment accounted for 5–45% of the gap. In addition, women may express more positive emotions when they are not necessarily experiencing favorable conditions, suggesting that cultural factors may influence the status of FI in women (135).
According to Sinclair et al., rural women had a higher prevalence of FI, which is in accordance with our subgroup analyses based on the region that indicated that the prevalence of FI was higher in rural areas [66.1% (95% CI: 58.8–73.4%)] compared to urban areas [47.1% (95% CI: 58.8–73.4%)] (136). Another study conducted by Sims et al. found that there was FI and malnutrition among Indian rural women (137). In addition, Sansón-Rosas et al. found high rates of FI in Colombian rural households (138). It is accepted that poverty is significantly linked to FI (139) and it is often considered the most common determinant of FI across the globe (139). Economic constraints may explain a higher prevalence of FI in rural areas (140). Many people who are from low-income households and are vulnerable to FI reside in rural areas and depend on agricultural activities to produce food; and in case of limited access to agricultural facilities and lands, they will face inadequate food availability (141).
In the present study, the highest prevalence of FI was among adults (56.5% [95% CI: 51.7–61.2%]) compared to different age groups. Sinclair et al. also found a higher prevalence of FI among people between the ages of 25–49 across the globe (136). A possible explanation for these findings may be that adults are often the head of the household and in the case of inadequate access to food, they may prioritize other members of the household. It also should be considered that fewer studies have been conducted among adolescents and older adults compared to those conducted on the adult population in Iran.
Another factor in the present study that made a significant difference in the prevalence of FI was the location of the participants' habitation as it was found that FI was higher in the western part of the country (64.8% [95% CI: 57.7–72.0%]) compared to the eastern (59.9% [95% CI: 49.9–69.8%]) and southern (59.2% [95% CI: 50.4–68.0%]) parts of the country. Mortazavi et al. conducted a cross-sectional study evaluating FI in the southern parts of Iran and in accordance with results from the present study, found a high prevalence of FI (58.8 %) (142). The current study found that the prevalence of FI in the northern parts of Iran was 56.8% (95% CI: 36.2–77.4%). A cross-sectional study conducted by Shakiba et al. also found a high prevalence of FI (50.8%) in northern Iran (84). Studies have shown that there are many risk factors for FI, including demographic characteristics and financial resources including age, economic status, employment, savings, educational level of the head of the household, single parenthood, and ethnicity (84, 142, 143). The impact of these risk factors on food security varies across populations, which reveals the potential influence of regional practices, policies, and nutrition programs (144, 145). However, to our knowledge, no study to date has examined the impact of regional influences in Iran. Future research is needed to validate the types of conclusions that can be drawn from this study.
Subgroup analyses were also conducted based on the type of questionnaire used to evaluate FI. Despite the fact that the questionnaires used in all of the studies were validated, there was evidence of a statistically significant difference between subgroups (p-value for heterogeneity: 0.003). However, the results for the prevalence of FI from the USDA 18-item (54.8% [95% CI: 49.0–60.6%]) and HFIAS (58.4% [95% CI: 49.8–67.1%]) were relatively similar, which were the questionnaires used in most of the studies. Other questionnaires were only used in a small number of included studies, which may explain the significant differences that were found in this study in the subgroup analysis for the type of questionnaire. Finally, the subgroup analysis for the results of the quality assessment did not reveal any evidence of a significant difference between high-quality and low-quality studies.
Strengths and limitation
To the best of our knowledge, the current meta-analysis included the highest number of studies to evaluate the prevalence of FI in Iran. The previous meta-analysis conducted by Behzadifar et al. (129) included 31 studies until 2015; therefore, the prevalence estimates reported in the present study represent the current findings. In addition, we performed subgroup analyses based on previously identified factors that may influence FI and found significant associations between the named factors and the prevalence of FI, which provided a strong comprehensive review of the relationships. However, this study had limitations worth considering when evaluating the findings. There was evidence of high heterogeneity between included studies. Furthermore, we did not assess the different levels of FI that may exist among the participants. Future studies and reviews may consider evaluating varying levels of FI as it may provide more information about FI status.
Conclusion
The findings of this systematic review and meta-analysis revealed that the prevalence of FI is high in Iran. The prevalence was higher among women, adults (aged), in rural areas and the western part of the country. It is an important finding that the prevalence of FI in Iran is influenced by age, gender, socioeconomic status, and habitation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LA and PA contributed to the study design, registered the study protocol, manuscript revision, and final version approval. NB edited the manuscript. SA, PS, MM, and MN-S contributed to the literature searches, title/abstract and full-text screening, extracted data, quality assessment, and manuscript drafting. PA contributed to the statistical analysis, ran the meta-analyses, and did data charting. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Tehran University of Medical Sciences (Grant Number: IR.TUMS.MEDICINE.REC.1400.1423).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1006543/full#supplementary-material
References
2. Motbainor A, Worku A, Kumie A. Level and determinants of food insecurity in East and West Gojjam zones of Amhara Region, Ethiopia: a community based comparative cross-sectional study. BMC Public Health. (2016) 16:1–13. doi: 10.1186/s12889-016-3186-7
3. Gross R, Schoeneberger H, Pfeifer H, Preuss H-J. The four dimensions of food and nutrition security: definitions and concepts. Scn news. (2000) 20:20–5.
4. Niles MT, Beavers AW, Clay LA, Dougan MM, Pignotti GA, Rogus S, et al. A multi-site analysis of the prevalence of food insecurity in the United States, before and during the COVID-19 Pandemic. Curr Dev Nutr. (2021) 5:nzab135. doi: 10.1093/cdn/nzab135
5. Amiresmaeili M, Yazdi-Feyzabadi V, Heidarijamebozorgi M. Prevalence of food insecurity and related factors among slum households in Kerman, south of Iran. Int J Health Plann Manage. (2021) 36:1589–99. doi: 10.1002/hpm.3242
6. Mohammadi Nasrabadi F, Omidvar N, Khoshfetrat M, Kolahdooz F. Household food insecurity in the Islamic Republic of Iran: a systematic review and meta-analysis. EMHJ. (2014) 20:698–706. doi: 10.26719/2014.20.11.698
7. Radimer KL, Olson CM, Campbell CC. Development of indicators to assess hunger. J Nutr. (1990) 120:1544–8. doi: 10.1093/jn/120.suppl_11.1544
8. Nord M. Household Food Security in the United States 2009. Collingdale,PA: DIANE publishing (2010).
9. Szabo S. Urbanisation and food insecurity risks: assessing the role of human development. Oxf Dev Stud. (2016) 44:28–48. doi: 10.1080/13600818.2015.1067292
10. Gebremichael B, Beletew B, Bimerew M, Haile D, Biadgilign S, Baye K. Magnitude of urban household food insecurity in East Africa: a systematic review and meta-analysis. Public Health Nutr. (2021) 1–27. doi: 10.1017/S1368980021003529
11. Behzadifar M, Behzadifar M, Abdi S, Arab Salmani M, Ghoreishinia G, Falahi E, et al. Prevalence of food insecurity in iran: a systematic review and meta-analysis. Prev Food Insecur Iran. (2016) 19:288–94. doi: 10.15171/mejdd.2016.31
12. Daneshi-Maskooni M, Sakineh S-B, Badri-Fariman M, Erfan A, Mohammadi Y, Jafarnejad S, et al. Questionnaire-based prevalence of food insecurity in Iran: a review article. Iran J Public Health. (2017) 46:1454.
13. Saaka M, Osman SM. Does household food insecurity affect the nutritional status of preschool children aged 6-36 months? Int J Popul Res. (2013) 2013. doi: 10.1155/2013/304169
14. COMMON IAMO. The Debilitating Cycle of HIV, Food Insecurity, and Malnutrition. Burlington Junction, MO: IAMO (2012).
15. Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff. (2015) 34:1830–9. doi: 10.1377/hlthaff.2015.0645
16. Morales ME, Berkowitz SA. The relationship between food insecurity, dietary patterns, and obesity. Curr Nutr Rep. (2016) 5:54–60. doi: 10.1007/s13668-016-0153-y
17. Pourmotabbed A, Moradi S, Babaei A, Ghavami A, Mohammadi H, Jalili C, et al. Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutr. (2020) 23:1778–90. doi: 10.1017/S136898001900435X
18. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
19. Peters M, Godfrey C, McInerney P, Soares C, Khalil H, Parker D. The Joanna Briggs Institute Reviewers' Manual 2015: Methodology for JBI Scoping Reviews (2015).
20. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
21. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
22. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
24. Mohammadzadeh A, Dorosty A, Eshraghian M. Household food security status and associated factors among high-school students in Esfahan, Iran. Public Health Nutr. (2010) 13:1609–13. doi: 10.1017/S1368980010000467
25. Asgharian Dastnaei A, Karami E, Keshavarz M. Determinants of Rural Households' Food Security. Agric Econ. (2013) 7:85–107.
26. Afshar A, Pourghaderi M, Hakim S, Safari A, Barati H. Rapid assessment of food insecurity in the urban households in Karaj. J Inflamm Dis. (2018) 22:74–82. doi: 10.29252/qums.22.2.74
27. Jozi A, Safa L, Salali Moghadam N. A study on the effects of nutritional awareness and attitude on rural households' food security level (The Case of Zanjan County). Iran J Agric Econ Dev Res. (2020) 51:715–30.
28. Narmaki E, Shirasb F, Qorbani M, Sotoudeh gassociation between food security and anthropometric measurements body composition blood blood pressure in women attending municipality sports clubs in west of Tehran. Iran J Diabet Lipid Disord. (2017) 16:103–10.
29. Motlagh ARD, Azadbakht L, Kaboli NE. Food insecurity in obese adolescent females in tehran schools: an examination of anthropometric and socio-economic factors. Curr Res Nutr Food Sci J. (2019) 7:280–6. doi: 10.12944/CRNFSJ.7.1.28
30. Mokari-Yamchi A, Faramarzi A, Salehi-Sahlabadi A, Barati M, Ghodsi D, Jabbari M, et al. Food security and its association with social support in the rural households: a cross-sectional study. Prev Nutr Food Sci. (2020) 25:146. doi: 10.3746/pnf.2020.25.2.146
31. Rezazadeh A, Omidvar N, Eini-Zinab H, Ghazi-Tabatabaie M, Majdzadeh R, Ghavamzadeh S, et al. Food insecurity, socio-economic factors and weight status in two Iranian ethnic groups. Ethn Health. (2016) 21:233–50. doi: 10.1080/13557858.2015.1061102
32. Ahmadihoseini A, Omidvar N, Nematy M, Safarian M, Salehi M. The relationship between food insecurity and anthropometric measures at birth in low income households. Iran J Pediatr. (2019) 29. doi: 10.5812/ijp.88410
33. Khosravipour B, Dorani M, Mehrab Ghoochani O. Investigating the Household's Food Insecurity of the Bawi Township. J Rural Dev Strategies. (2017) 4:231–46.
34. Alipour B, Abbasalizad Farhangi M, Asghari S, Amirkhizi F, Dahri M, Abedimanesh N, et al. Child-specific food insecurity and its sociodemographic and nutritional determinants among Iranian schoolchildren. Ecol Food Nutr. (2016) 55:231–40. doi: 10.1080/03670244.2015.1129324
35. Daneshzad E, Dorosty-Motlagh A, Bellissimo N, Suitor K, Azadbakht L. Food insecurity, dietary acid load, dietary energy density and anthropometric indices among Iranian children. Eating Weight Disord Stud Anorexia Bulimia Obes. (2021) 26:839–46. doi: 10.1007/s40519-020-00921-8
36. Parvin S, Salehi S, Joshan M, Akbar Tabar Tori M, Malekzadeh J, Pirooz R, et al. The situation of food security and related factors in female teachers of Yasuj Education School Board. Armaghane danesh. (2020) 25:515–28. doi: 10.52547/armaghanj.25.4.515
37. Tabrizi JS, Nikniaz L, Sadeghi-Bazargani H, Farahbakhsh M, Nikniaz Z. Socio-demographic determinants of household food insecurity among Iranian: a population-based study from northwest of Iran. Iran J Public Health. (2018) 47:893.
38. Rezaei H, Shirani Beid Abadi F. rezaee a, Joolaie R, abedi sarvestani a. Assessing the relationship between food insecurity and agricultural sustainability (case study: rural areas of Gorgan County). Agric Econ. (2021) 15:135–62.
39. Saadi H, Azizi M, Azami M. Extension education and food security of farmer households (Case study: Qorveh county, Kurdistan Province). Iran J Agric Econ Dev Res. (2014) 45:483–99.
40. Saadi H, Moaddab HV. Assessment of female-headed household's food security and the affecting factors; case study: women in Razan City. Women Dev Pol. (2014) 11:411–26. doi: 10.22059/jwdp.2013.36536
41. Gholizadeh H, Rostamian Motlagh Z, Badsar M, Shams A. Culture and nutrition knowledge, and their relationship with food insecurity among rural households in Kermanshah County, Iran. J Rural Res. (2017) 8:54–67. doi: 10.21859/jjr-08014
42. Farzaneh H, Gargari BP, Jafarabadi MA, Farzaneh A, Arzhang P. Household food insecurity and its related socioeconomic and nutritional factors among northwest Iranian high-school students. Rawal Med J. (2017) 42:239–45.
43. Fami HS, Aramyan LH, Sijtsema SJ, Alambaigi A. The relationship between household food waste and food security in Tehran city: the role of urban women in household management. Indus Market Manage. (2021) 97:71–83. doi: 10.1016/j.indmarman.2021.06.016
44. Jamini D. Food security and its implications on rural areas. Geogr Plann Space. (2017) 7:113–30.
45. Jamini D, Amini A, Ghadermarzi H, Tavakoli J. Measurement of food security and investigation of its challenges in rural areas (case study: Badr District From Ravansar County). J Reg Plann. (2017) 7.
46. Sharafkhani R, Dastgiri S, Gharaaghaji R, Ghavamzadeh S, Didarloo A. The role of household structure on the prevalence of food insecurity. Eur J Gen Med. (2010) 7:385–8. doi: 10.29333/ejgm/82890
47. Basirat R, Salehi Abargouei A, Esmaillzadeh A. The association between household food insecurity and childhood obesity among Iranian school-aged children in Farokhshahr. Koomesh J. (2012) 13:254–63.
48. Rafat R, Rezazadeh A, Arzhang P, Alipourr A. The association of food insecurity with sociodemographic factors and depression in the elderly population of Qarchak city–Iran. Nutr Food Sci. (2020). doi: 10.1108/NFS-06-2019-0191
49. Dastgiri S, Mahboob S, Tutunchi H, Ostadrahimi A. Determinants of Food Insecurity: A Cross– Sectional Study in Tabriz. J Ardabil Univ Med Sci. (2006) 6:233–9.
50. Esfandiari S, Omidvar N, Eini-Zinab H, Doustmohammadian A, Amirhamidi Z. Associations among food insecurity, academic performance, and weight status in primary schoolchildren in Tehran, Iran: a cross-sectional study. J Nutr Educ Behav. (2018) 50:109–17.e1. doi: 10.1016/j.jneb.2017.05.365
51. Mahmoudi S, Khoramivafa M, Hadidi M, Ahmadi M, Jalali A. Food Security Status among Rural Households in Sarpolzahab and its Association with Socio-Economic and Agricultural Factors. J Res Rural Plann. (2020) 9:35–47.
52. Khodabakhshzadeh S, Moradabadi SA, Khodabakhshzadeh S, Baniasadi M, Khalilabad TH. Food security and its related factors in the rural households of Bam city in Iran: a logistic regression model approach. Arch Iran Med. (2018) 21:26–8.
53. Tezerji S, Nazari Robati F. Status of food security in Kerman, Iran During the COVID-19 pandemic. J Arak Univ Med Sci. (2020) 23:774–85. doi: 10.32598/JAMS.23.COV.6254.2
54. Hosseinpour S, Dorosty AR, Djazayery A. Association of food insecurity with nutrition status, food diversity and anthropometric status in Iranian elderlies: a cross-sectional study. J Nutr Sci Diet. (2019) 5. doi: 10.18502/jnsd.v5i1.5232
55. Sara Hakim A. Mohammad Reza E. Prevalence of food insecurity and its correlates health monitor. J Iran Inst Health Sci Res. (2012) 11:791–7.
56. Ziaei SM, Shirani Bidabadi F, Eshraghi F, Keramatzadeh A. Identification of coping strategies on food insecurity and its effective factors in rural areas of Gorgan. Agric Econ Dev. (2019) 26:47–69.
57. Tabibian S, Daneshzad E, Bellissimo N, Brett NR, Dorosty-Motlagh AR, Azadbakht L. Association between adherence to the dietary approaches to stop hypertension diet with food security and weight status in adult women. Nutr Diet. (2018) 75:481–7. doi: 10.1111/1747-0080.12440
58. Hamedi-Shahraki S, Mir F, Amirkhizi F. Food insecurity and cardiovascular risk factors among Iranian Women. Ecol Food Nutr. (2021) 60:163–81. doi: 10.1080/03670244.2020.1812596
59. Shahraki SH, Amirkhizi F, Amirkhizi B, Hamedi S. Household food insecurity is associated with nutritional status among Iranian children. Ecol Food Nutr. (2016) 55:473–90. doi: 10.1080/03670244.2016.1212710
60. Ramesh T, Dorosty Motlagh A, Abdollahi M. Prevalence of household food insecurity in the City of Shiraz and its association with socio-economic and demographic factors, 2008. Iran J Nutr Sci Food Technol. (2010) 4:53–64.
61. Gholami A, Foroozanfar Z. Household food security status in the Northeast of Iran: a cross-sectional study. Med J Islam Repub Iran. (2015) 29:227.
62. Gholami A, Jahromi LM, Shams-Beyranvand M, Khazaee-Pool M, Naderimagham S, Mehrizi AA, et al. Household food insecurity and health-related quality of life in an urban adult population in Iran. Curr Nutr Food Sci. (2020) 16:381–90. doi: 10.2174/1573401315666191114142121
63. Taheri F, Shafi EH, Dorosty AR. Assessment of food insecurity prevalence and associated factors in village of Qehi, Isfahan in 2016. Res Bull Med Sci. (2016) 21:138–45.
64. Madvari FF, Yeganeh HS, Siasi F, Sotoudeh G, Hosseini SM, Rad SVM. Food security and factors related to it in households under coverage of urban health centers and health houses in Mehriz, Iran. Sci J School Public Health Inst Public Health Res. (2015) 12:79–93.
65. Kian F, Farhadian H, Chobchian S. Food insecurity assess of urban household of Alborz province. Food Sci Technol. (2016) 13:167–79.
66. Kian F, Farhadian H, Choobchian S. Do Iranian households benefit from food according to their health characteristics? A case study from Alborz Province, Iran. J Public Health. (2021) 1–7. doi: 10.1007/s10389-021-01631-w
67. Esfarjani F, Hosseini H, Khaksar R, Roustaee R, Alikhanian H, Khalafi M, et al. Home food safety practice and household food insecurity: a structural equation modeling approach. Iran J Public Health. (2019) 48:1870. doi: 10.18502/ijph.v48i10.3495
68. Jafari F, Ehsani S, Nadjarzadeh A, Esmaillzadeh A, Noori-Shadkam M, Salehi-Abargouei A. Household food insecurity is associated with abdominal but not general obesity among Iranian children. BMC Public Health. (2017) 17:1–8. doi: 10.1186/s12889-017-4262-3
69. Khorramrouz F, Doustmohammadian A, Eslami O, Khadem-Rezaiyan M, Pourmohammadi P, Amini M, et al. Relationship between household food insecurity and food and nutrition literacy among children of 9–12 years of age: a cross-sectional study in a city of Iran. BMC Res Notes. (2020) 13:1–6. doi: 10.1186/s13104-020-05280-2
70. Mohammadi F, Omidvar N, Harrison GG, Ghazi-Tabatabaei M, Abdollahi M, Houshiar-Rad A, et al. Is household food insecurity associated with overweight/obesity in women? Iran J Public Health. (2013) 42:380.
71. Pourebrahim F, Omidvar N, Rezazadeh A, Eini-Zinab H, Shirani P. Food security and its association with socioeconomic status and diet diversity in free living elderly in Tehran, Iran. 2020. doi: 10.21203/rs.3.rs-28947/v1
72. Rostami F, Shahmoradi M, Baghaei S. Factors affecting on rural households food security (Case study: Karnachy Village in Kermanshah County). Iran J Agric Econ Dev Res. (2014) 45:725–37.
73. Fallah Tafti L, Mozafari Khosravi H, Najarzadeh A, Falahzadeh H. Food security status of elders and its related factors in Arak in 2012. Tolooebehdasht. (2016) 14:64–78.
74. Safa L, Jozi A. Investigating the villagers' food security situation and determining its relationship with their demographic characteristics (the case of Zanjan County). Iran Agric Exten Educ J. (2021) 17:185–94.
75. Nikniaz L, Tabrizi JS, Sadeghi-Bazargani H, Farahbakhsh M, Nikniaz Z. Food insecurity increases the odds of obesity among Iranian women: a population-based study of northwestern Iran. Nutr Diet. (2017) 74:454–9. doi: 10.1111/1747-0080.12356
76. Nikniaz L, Tabrizi JS, Sadeghi-Bazargani H, Farahbakhsh M, Nikniaz Z. Is Food Insecurity Associated With Lipid Profile and Atherogenic Indices in Iranian Adults? A population-based study. Topics Clin Nutr. (2018) 33:23–30. doi: 10.1097/TIN.0000000000000124
77. Hasan-Ghomi M, Mirmiran P, Amiri Z, Asghari G, Sadeghian S, Sarbazi N, et al. The association of food security and dietary variety in subjects aged over 40 in district 13 of Tehran. Iran J Endocrinol Metab. (2012) 14:360–7.
78. Najafianzadeh M, Mobarak-Abadi A, Ranjbaran M, Nakhaei M. Relationship between the prevalence of food insecurity and some socioeconomic and demographic factors in the rural households of Arak, 2014. Iran J Nutr Sci Food Technol. (2015) 9:35–44.
79. Safarpour M, Dorosty Motlagh A, Hosseini SM, Ranjbar Noshari F, Safarpour M, Daneshi Maskooni M, et al. Prevalence and outcomes of food insecurity and its relationship with some socioeconomic factors. Knowl Health. (2014) 8.
80. Esmailnejad M, Akbarpour M, Mikaniki J, Falsoleiman M. Assessing the implications of climate change on food security and rural livelihoods case study: rural farmers in Migan Nehbandan. Geography. (2018) 16:5–18.
81. Keshavarz M. Investigating food security and food waste control of farm families under drought (A case of Kherameh County). Space Econ Rural Dev. (2021) 9:83–106.
82. Akbarpoor M, Mahdavi Damghani A, Deihimfard R, Veisi H. Assessment of the food security status in Marvdasht County. J Agroecol ( ) (2016) 6.
) (2016) 6. 
83. Mohammadi M, Eshraghian M, Dorosti A, Asadi Lari M, Mansournia M, Ahsani-Nasab S. Identification of the determinaints of food insecurity in tehran using a multilevel model. Iran J Nutr Sci Food Technol. (2016) 10:13–20.
84. Shakiba M, Salari A, Mahdavi-Roshan M. Food insecurity status and associated factors among rural households in the north of Iran. Nutr Health. (2021) 27:301–7. doi: 10.1177/0260106021996840
85. Farhangi MA, Alipour B, Rezazadeh K, Ghaffary A, Eidi F, SaberGharamaleki A, et al. Food insecurity and its related socioeconomic and nutritional factors: evidence from a sample of population in the northwest of Iran. Qual Assur Safety Crops Foods. (2015) 7:109–13. doi: 10.3920/QAS2013.0317
86. Sheikhi M, Omidvar N, Tabatabaei SM, Eini-Zinab H. Is nutritional functional diversity in the rural food and nutrition system associated with food security and nutrient adequacy? A Case Study of Rural Areas of Zahedan City, Iran. BMC Public Health. (2021) 22:751. doi: 10.21203/rs.3.rs-525134/v1
87. Ebadi-Vanestanagh M, Azizi-Lalabadi M, Jahangiry L, Alizadeh M. Challenges of food insecurity indicators, diet quality and weight outcomes in women: a cross-sectional study. Prevent Nutr Food Sci. (2019) 24:393. doi: 10.3746/pnf.2019.24.4.393
88. Savari M, Shabanali Fami H, Daneshvar Ameri Z. Analysis situation food security and factors affecting thereon in the rural society city of Divandarreh. J Rural Res. (2014) 5:311–32. doi: 10.22059/JRUR.2014.52473
89. Aazami M, Hashemiamin N, Soroushmehr H. A survey on food insecurity of rural households and factors affecting it in Khuzestan Province of Iran: a case study of Bostan Sub-district. Village Dev. (2018) 20.
90. Payab M, DorostyMotlagh A, Eshraghian M, Rostami R, Siassi F, Ahmadi M. The relationship between household food insecurity status and depression in mothers with school children living in Ray in 2010. Iran J Epidemiol. (2012) 8:37–44.
91. Bagheri M, Hadad H, Shirvanian AR. Study of relationship between food security and income poverty in rural areas of Guilan Province in Iran: a case study of Amlash County. Village Dev. (2020) 22. doi: 10.30490/RVT.2020.293733.1076
92. Cheraghi M, Kazemi N. Food security and related economic factors in rural elderly women. Koomesh. (2018) 20:203–9.
93. Mehdi Cheraghi BM-Y, Zahra E-S. Analysis of geographical factors affecting food security of rural households(Case study: Zanjan township) (JGET) Geographical Engineering of Territory (2018).
94. Charaghi M, Mohammadi Yeganeh B, Musavi Zare SS. The role of non-farm activities on the food security of rural households case study: Fazl Rural district, Nishabour city. J Rural Dev Strat. (2018) 5:51–66. doi: 10.22048/rdsj.2018.53551.1541
95. Sotoudeh M, Amaniyan S, Jonoush M, Vaismoradi M. A community-based survey of household food insecurity and associated sociodemographic factors among 2–6 years old children in the Southeast of Iran. Nutrients. (2021) 13:574. doi: 10.3390/nu13020574
96. Eghrari M, Sharifian Sani M, Mohaqeqi Kamal SH, Ghaedamini Harouni G, Zanjari N, Ahmadi S. Food insecurity among elderly in Tehran: prevalence, risk and protective factors. J Mazandaran Univ Med Sci. (2020) 30:107–16.
97. Minaie M, Movahedi A, Motlagh AD, Abdollahi Z, Djazayery A. Association of socioeconomic status and food security with anthropometric indices among 2–5-year-old urban children in eight different cities in Iran. Int J Prev Med. (2019) 10. doi: 10.4103/ijpvm.IJPVM_143_18
98. Asadi-Lari M, Jahromi LM, Montazeri A, Rezaee N, Mehrizi AAH, Shams-Beyranvand M, et al. Socio-economic risk factors of household food insecurity and their population attributable risk: a population-based study. Med J Islam Repub Iran. (2019) 33:119. doi: 10.47176/mjiri.33.119
99. Salarkia N, Omidvar N, Zaeri F, Zeinab HE, Neyestani TR. Mother's self-efficacy mediates the relationship between household food insecurity and maternal infant feeding styles. Matern Child Health J. (2016) 20:602–12. doi: 10.1007/s10995-015-1859-y
100. Omidvar N, Ahmadi D, Sinclair K, Melgar-Quiñonez H. Food security in selected Middle East and North Africa (MENA) countries: an inter-country comparison. Food Security. (2019) 11:531–40. doi: 10.1007/s12571-019-00935-w
101. Abedi P, Abbaspor Z, Montazeri S, Vakili M, Haghigheizadeh M. Food insecurity prevalence and its related factors in households in Ahvaz, Iran. Malaysian J Nutr. (2013) 19.
102. Safarpour P, Motlagh ARD, Sadeghi H. Relationship Between Food Insecurity and Depression in Elementary School Students' Mothers (2018).
103. Arzhang P, Gargari BP, Sarbakhsh P, Farzaneh H. Household food insecurity and associated factors among rural and urban high school students in Kurdish population of Iran. Progr Nutr. (2019) 21:56–64.
104. Ekhlaspour P, Foroumandi E, Ebrahimi-Mameghani M, Jafari-Koshki T, Arefhosseini SR. Household food security status and its associated factors in Baft-Kerman, IRAN: a cross-sectional study. Ecol Food Nutr. (2019) 58:608–19. doi: 10.1080/03670244.2019.1652818
105. Alipour V, Rezapour A, Shali M, Harati Khalilabad T. Elderly's food security and its associated socioeconomic determinants in Tehran: a cross-sectional study. Health Science Reports. (2021) 4:e240. doi: 10.1002/hsr2.240
106. Mortazavi Z, Dorosty AR, Eshraghian MR, Ghaffari M, Ansari-Moghaddam A. Household food insecurity and its association with self-reported infectious and parasitic diseases among household mothers in Southeast of Iran. Health Scope. (2017) 6. doi: 10.5812/jhealthscope.15125
107. Dassie GA, Motlagh AD, Chamari M, Mohammadreza E. Prevalence of food insecurity and its association with muscle mass, hand grip strength and gait speed among elderly in tehran. Int J Pharm Sci Res. (2016) 7:2889. doi: 10.13040/IJPSR.09758232.7(7).2889-95
108. Abdar-Esfehani B. The relationship between household food security and food intake quality, nutritional adequacy and food diversity of final year high school students in Tehran in the academic year 2017 (Master thesis) (2017).
109. Razzazi A. Determining the relationship between menopausal age and security and dietary pattern in women in Qazvin in 2014 (Master thesis).
110. Kazemi B. Relationship Between Physical Fitness and Body Composition with Food Security Among Male Students of Khalkhal City in Different Weight Categories (2018).
111. Darini M. Investigating the Factors Affecting Food Security Using Food Diversity Indicators and Coping Strategies (Case Study: Jabalbarz Region) (Master thesis) (2014).
112. Sharaki ZE. Analysis of the Role of Food Security in the Sustainable Development of Rural Areas; Case Study: Taqanak Village (Masters thesis) (2015).
113. Siasar H. Assessing the Food Security Situation of Urban and Rural Families in Zabol (Master thesis) (2017).
114. Nadimi B. Analysis of Effective Factors on the Selection of Strategies to Combat Food Insecurity Rural Households, A Case Study: Awalan village (Kamyaran City) (2017).
115. Rahimi-Moghadam S, Mahdavi-Damghani A, Akbarpoor M, Sajjadian M, N R-S. Investigating the food security situation of Poldakhtar city. Ecol Agric (2015).
116. Abbasi F, Kavoosi M. “Investigating the food security situation in the plain villages of eastern Guilan province (Case study: Machian village, Rudsar city),” in Fifth National Conference on Applied Research in Management and Accounting (2019).
117. Esapare K. Assessing the Food Insecurity of Households in Rural Areas Dezful City, Khouzestan (2016).
118. Forootan L. Investigating The Food Security Situation and the Factors Affecting it in Rural Households Baladarband, Razi.
119. Pakravan-Charvadeh M, Hoseini S, Noori-Naeeni S. Identifying socio-economic factors related to food security of households in urban and rural areas of Khuzestan province. J Clean Prod. (2021) 25:113–36.
120. Rezvani M, Sanaee-Moghadam S. Role of Rural-Urban Links in Food Security of Rural Households Case: Dehdasht East, Dehdash (2018).
121. Hashemitabar M, Akbari A, Dorini M. Analysis of Factors Affecting Food Security in Rural Areas in the South of Kerman Province (2018).
122. Bayanani N. Assessing the Food Security Situation at the Household Level in the Villages of Bahar City and the Factors Affecting It (2020).
124. Shabanali-Fami H, Moradi M, Asadi A. The effect of agricultural water consumption management on food security of farmers' households in the family exploitation system: A case study of Kermanshah city. Islamic Azad Univ Sci Res Branch J. (2020) 12:51–64.
125. Amin N, Akbari H, Jafarnejad S. Food security, mental health, and socioeconomic status: a cross-sectional study among medical college students in central part of Iran, Kashan. Health Sci Rep. (2022) 5:e476. doi: 10.1002/hsr2.476
126. Jamini D, Amini A, Ghadermarzi H, Tavakkoli J. Measuring food security and its determinants in rural areas: a case study of the farmers in the Central District of Ravansar, Kermanshah. J Geogr Reg Dev. (2017) 14:225–46. doi: 10.22067/GEOGRAPHY.V14I2.63833
127. Ahmadi Dehrashid A, Bijani M, Valizadeh N, Ahmadi Dehrashid H, Nasrollahizadeh B, Mohammadi A. Food security assessment in rural areas: evidence from Iran. Agric Food Secur. (2021) 10:1–18. doi: 10.1186/s40066-021-00291-z
128. Abbasi N, Ghoochani O, Ghanian M, Kitterlin M. Assessment of Households' Food Insecurity through use of a USDA Questionnaire. Adv Plants Agric Res. (2016) 4:1–8. doi: 10.15406/apar.2016.04.00155
129. UNICEF. The State of Food Security and Nutr in the World 2021. New York City, New York: UNICEF (2021).
130. Marwa Diab-El-Harake, Samer Kharroubi, Jumanah Zabaneh, Joma L. Gender-based differentials in food insecurity and wellbeing in Arab countries. Global Food Secur. (2022) 32:100609. doi: 10.1016/j.gfs.2021.100609
131. Jung NM, de Bairros FS, Pattussi MP, Pauli S, Neutzling MB. Gender differences in the prevalence of household food insecurity: a systematic review and meta-analysis. Public Health Nutr. (2017) 20:902–16. doi: 10.1017/S1368980016002925
132. Negesse A, Jara D, Habtamu T, Dessie G, Getaneh T, Mulugeta H, et al. The impact of being of the female gender for household head on the prevalence of food insecurity in Ethiopia: a systematic-review and meta-analysis. Public Health Rev. (2020) 41:15. doi: 10.1186/s40985-020-00131-8
133. World Health Organization. The State of Food Security and Nutr in the World 2019: Safeguarding Against Economic Slowdowns and Downturns. Mount Vernon, Virginia: Food & Agriculture Org. (2019).
134. Broussard NH. What explains gender differences in food insecurity? Food Policy. (2019) 83, 180–194. doi: 10.1016/j.foodpol.2019.01.003
135. Asfahani F, Kadiyala S, Ghattas H. Food insecurity and subjective wellbeing among arab youth living in varying contexts of political instability. J Adolesc Health. (2019) 64:70–8. doi: 10.1016/j.jadohealth.2018.08.010
136. Kate Sinclair, Davod Ahmadigheidari, Diana Dallmann, Meghan Miller, Melgar-Quiñonez H. Rural women: Most likely to experience food insecurity and poor health in low- and middle-income countries. Global Food Secur. (2019) 23:104–15. doi: 10.1016/j.gfs.2019.04.006
137. Sims A, van der Pligt P, John P, Kaushal J, Kaur G, McKay FH. Food insecurity and dietary intake among rural indian women: an exploratory study. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18094851
138. Sansón-Rosas AM, Bernal-Rivas J, Kubow S, Suarez-Molina A, Melgar-Quiñonez H. Food insecurity and the double burden of malnutrition in Colombian rural households. Public Health Nutr. (2021) 24:4417–29. doi: 10.1017/S1368980021002895
139. ADB, -AR,. Cooperation and Integration in Asia and the Pacific. Asian Development Bank Annual Report 2012. Retrieved from https://wwwadborg/sites/default/files/institutional-document/33806/adb-annual-report-2012pdf
140. Duflo E. Women empowerment and economic development. J Econ Lit. (2012) 50:1051–79. doi: 10.1257/jel.50.4.1051
141. Koren O, Bagozzi BE. From global to local, food insecurity is associated with contemporary armed conflicts. Food Secur. (2016) 8:999–1010. doi: 10.1007/s12571-016-0610-x
142. Mortazavi Z, Dorosty AR, Eshraghian MR, Ghaffari M, Ansari-Moghaddam A, Mohammadi M. Household food insecurity in Southeastern Iran: severity and related factors. Int J Food Sci. (2017) 2017:7536024. doi: 10.1155/2017/7536024
143. Behzadifar M, Behzadifar M, Abdi S, Malekzadeh R, Arab Salmani M, Ghoreishinia G, et al. Prevalence of food insecurity in Iran: a systematic review and meta-analysis. Arch Iran Med. (2016) 19:288–94.
144. Costa NS, Santos MO, Carvalho CPO, Assunção ML, Ferreira HS. Prevalence and factors associated with food insecurity in the context of the economic crisis in Brazil. Curr Dev Nutr. (2017) 1:e000869. doi: 10.3945/cdn.117.000869
Keywords: food insecurity, food security, Iran, prevalence, food supply
Citation: Arzhang P, Abbasi SH, Sarsangi P, Malekahmadi M, Nikbaf-Shandiz M, Bellissimo N and Azadbakht L (2022) Prevalence of household food insecurity among a healthy Iranian population: A systematic review and meta-analysis. Front. Nutr. 9:1006543. doi: 10.3389/fnut.2022.1006543
Received: 07 August 2022; Accepted: 05 October 2022;
Published: 15 November 2022.
Edited by:
Harsharn Gill, RMIT University, AustraliaReviewed by:
Huaqing Liu, Bengbu Medical College, ChinaHaiquan Xu, Institute of Food and Nutrition Development (CAAS), China
Copyright © 2022 Arzhang, Abbasi, Sarsangi, Malekahmadi, Nikbaf-Shandiz, Bellissimo and Azadbakht. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leila Azadbakht, QXphZGJha2h0bGVpbGFAZ21haWwuY29t
†ORCID: Leila Azadbakht orcid.org/0000-0002-5955-6818
 Pishva Arzhang
Pishva Arzhang S. Haniye Abbasi2
S. Haniye Abbasi2 Leila Azadbakht
Leila Azadbakht