
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Nutr. , 18 October 2022
Sec. Nutrition, Psychology and Brain Health
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.1004953
This article is part of the Research Topic Impact of COVID-19 Pandemic on Eating Habits: 2-Year Legacy of Social Distancing Times View all 7 articles
The COVID19 pandemic has affected all aspects of people's lives. Eating habit plays a crucial role in children and adolescents' physical and mental development and the impacts might last until adulthood. This systematic review aimed to summarize a comprehensive and updated overview of eating habits changes due to COVID19 confinements among children and adolescents. A systematic literature search was performed in three databases for all the English studies published from the start of the confinements until April 2022. Two researchers screened articles independently and included observational studies which evaluated children's and adolescents' eating habits before and during confinements. The quality of the included studies was assessed by Newcastle-Ottawa Quality Assessment checklists for cross-sectional and cohort studies. Among 2,436 studies, 39 final full-text articles were included. The total participants of this systematic review consist of 157,900 children and adolescents. Seven categories were identified: daily eating patterns, junk food, beverage, fruits and vegetables, milk and dairy, protein-rich foods, and legumes and cereals. In summary, most of the included studies reported a significant increase in consumption of home-cooked meals, amount of food, snack, french fries, sweets, fruits, vegetables, legumes, bread, and bakery products. On the other hand, studies demonstrated significantly lower intake of fast food and soft drink. The studies reported controversial results about breakfast consumption, sugar-added drinks, caffeinated drinks, milk and dairy products, protein-rich foods (including meat, fish, egg and chicken, and poultry), rice, and cereal. Changes in children's and adolescents' eating habits during the COVID-19 era were both positive and negative, for example, a decrease in fast food, fruit, and vegetable consumption vs. an increase in snacking and sweet consumption. Both changes have significant short-term and long-term impacts on population health. This study could provide us with insight into the changes in eating habits in children and adolescents in the COVID-19 era which we can use to limit the negative consequences on health.
Due to the spread of the coronavirus disease, the imposed limitations to control the disease have led to many changes in millions of people's lives worldwide from the late 2019 until today (1). In addition to social distancing, lifestyle habits have changed during the COVID-19 era (2). Physical inactivity (3), increased screen time (4), psychological distress (5), and disruption of sleep patterns (6) have been reported during repeated confinements. As a result, these abrupt changes affected health behaviors, including eating habits, across all age groups (7). School closure, online teaching, and outdoor activity restriction were other dimensions that significantly impacted children and adolescents' lifestyles and eating behaviors (8).
Eating habit is “the habitual decisions of individuals or a group of people regarding what food they eat” (9) which was affected by COVID-19. Diet and eating habits play an important roles in children and adolescents' physical and mental development (10, 11). Any unhealthy eating habits in the growth period of life can lead to irreversible consequences such as the increased risk of obesity, non-communicable diseases, and decreased immune system function (12, 13).
Although some review studies showed that the pattern of consuming snacks, home-cooked food, junk foods, and fruits and vegetables increased significantly, on the other hand, some other studies showed controversial findings (1, 14–16).
Therefore, this systematic review was designed to assess the effect of the COVID-19 era on dietary habits in children and adolescents.
All research steps were conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statements in this systematic review (17).
A systematic literature search was performed to identify the impact of the COVID-19 epidemic on eating behaviors in children and adolescents. The electronic search was conducted in three international databases (Pubmed, Scopus, and Web of Science) for all the English studies published from the start of the confinements until April 2022. Moreover, Google scholar was also searched and reference checking was done. The following search terms were used in this systematic search, with the minimum restriction possible: (“eating habits”[Title/Abstract] OR “dietary intake”[Title/Abstract] OR “dietary pattern”[Title/Abstract] OR “food choices”[Title/Abstract] OR “diet quality”[Title/Abstract] OR “eating behaviors”[Title/Abstract] OR “food preferences*”[Title/Abstract]) AND (“covid-19”[Title/Abstract] OR “SARS-CoV-2”[Title/Abstract] OR “coronavirus”[Title/Abstract] OR “covid19”[Title/Abstract]).
All references were initially imported to End Note version 9.3.3, and duplicates were detected and removed. Two researchers FP and ME screened titles and abstracts in line with inclusion and exclusion criteria. The remaining studies that seemed potentially relevant were reviewed in their full text. Any conflicts at any stage of screening were discussed and resolved by two authors and senior authors.
• Papers investigated any changes (qualitative or quantitative) in eating behavior, including consumption of foods and beverages or following a specific diet.
• Exposure was lockdowns resulting from COVID-19, and studies compared eating habits with before lockdowns
• The population of interest was children and adolescents
• Observational studies, including cross-sectional, case-control, prospective, or retrospective cohort studies
• English-language studies.
• Eating habit changes were not compared before and during lockdowns
• Papers that evaluated eating habits only before OR during confinements
• Participants were not children or adolescents
• Clinical trials, reviews, books, and conferences.
The following items were extracted from eligible studies:
• General characteristics of the studies include the first author's name, year, and country.
• Methodological characteristics of the studies include study design, the population of the study, sample size, assessment tool, and target habit.
• Outcomes of the studies include changes in daily eating patterns (including the number of meals, eating breakfast, amount of foods and home-cooked foods) and different groups of foods and beverages and their subgroups, including Junk Foods (snack, fast food, French fries and chips, processed food and sweets), beverages (soft drink, sugar added drink, caffeinated drink), fruits & Vegetables, Milk and Dairy, Protein Sources (meat, egg, fish, chicken), Legumes & Cereals (rice, soybean, cereal, bread, and bakery).
The quality of the included studies was assessed by Newcastle-Ottawa Quality Assessment Form for cross-sectional and cohort studies (18, 19). FP and ME independently appraised the studies' quality using Newcastle-Ottawa quality assessment checklists. The Newcastle-Ottawa scale evaluates the methodological quality of the studies in seven items for cross-sectional and eight items for cohort studies within three categories: (1) Selection of participants (maximum 4 scores), (2) Comparability of subjects (maximum 2 scores), (3) Assessment of outcome (maximum 3 scores). We classified the quality of each study as follows: for cross-sectional studies 9 and 10 points as “very good,” 7 and 8 points as “good,” 5 and 6 as “satisfactory,” and 0 to 4 as “unsatisfactory.” For cohort studies, if a study gets 3 or 4 points in the selection part AND 1 or 2 points in the comparability part, AND 2 or 3 points in the outcome part, it is considered “good quality.” If a study gets 2 scores in the selection part AND 1 or 2 scores in the comparability part AND 2 or 3 points in the outcome part, it is considered “fair quality,” and if a study scored 0 or 1 in the selection part OR 0 stars in comparability part OR 0 or 1 stars in outcome part, it is considered as “poor quality.”
The screening steps are shown in the PRISMA flow diagram (Figure 1). The initial electronic search of three databases retrieved 2,436 articles (Pubmed = 545, Scopus = 1,273, Web of science = 618). One thousand and twenty seven articles were detected as duplicates and removed. After reviewing titles and abstracts, 930 articles were excluded. Sixty four articles did not have an observational design, and 35 articles were excluded because of being book chapters and conferences. After that, 380 papers were reviewed for full text. Papers that did not specifically compare eating habits before and during COVID-19 lockdowns were deprived. Finally, 39 articles met the inclusion criteria for this systematic review (2, 5, 8, 20–55).
Characteristics of the included studies are presented in Table 1. Studies were conducted on all five continents. Nearly half of the studies (48%) were from Europe (Spain = 5, Poland = 4, Italy = 3, France = 2, Germany = 1, Netherland = 1, Greece = 1, Croatia = 1). Nine studies were conducted in America (United states = 5, Brazil = 3, Canada = 1), eight from Asia (Palestine = 2, China = 2, Saudi Arabia = 1, Japan = 1, South Korea = 1, Jordan = 1), and two from Africa (Egypt = 2), and one from Australia. One international study was performed in five countries (Spain, Italy, Brazil, Colombia, and Chile). Among 39 articles, 35 were cross-sectional studies, three cohorts, and one quasi-experimental. The total participants of this systematic review consist of 157,900 children and adolescents. Questionnaires were mostly employed as the assessment tool. Due to pandemic confinements and limitations, all studies had online or telephone interviews, except for three studies for which the interviews were held face-to-face, with health protocols being observed, following the cancelation of COVID-19 confinements. About 12 studies had prepared validated questionnaires that improved the study's quality.
Concerning the quality assessment of the studies, out of 39 studies, 15 were considered good or satisfactory quality, and 24 had low quality (Supplementary Table S1).
As shown in Table 2, data were categorized into seven groups, including daily eating patterns, junk food, beverages, fruits and vegetables, dairy and milk, protein-rich foods, legumes, and cereals. To have a simple outlook and rapid overview, changes in each item were illustrated with arrows. Generally, sweets, fruits, vegetables, and fast food were the most evaluated items by the studies. Any kind of dessert, chocolates, and cake was considered in the sweets category in this review. In summary, most of the included studies reported a significant increase in consumption of home-cooked meals, Amount of food, snack, french fries, sweets, fruits, vegetables, legumes, bread, and bakery products. On the other hand, most studies demonstrated significantly lower intake of fast food and soft drink. The studies reported controversial results about the consumption of breakfast, sugar-added drinks, caffeinated drinks, Milk and dairy products, protein-rich foods (including meat, fish, egg and chicken, and poultry), rice, and cereal (Figure 2).
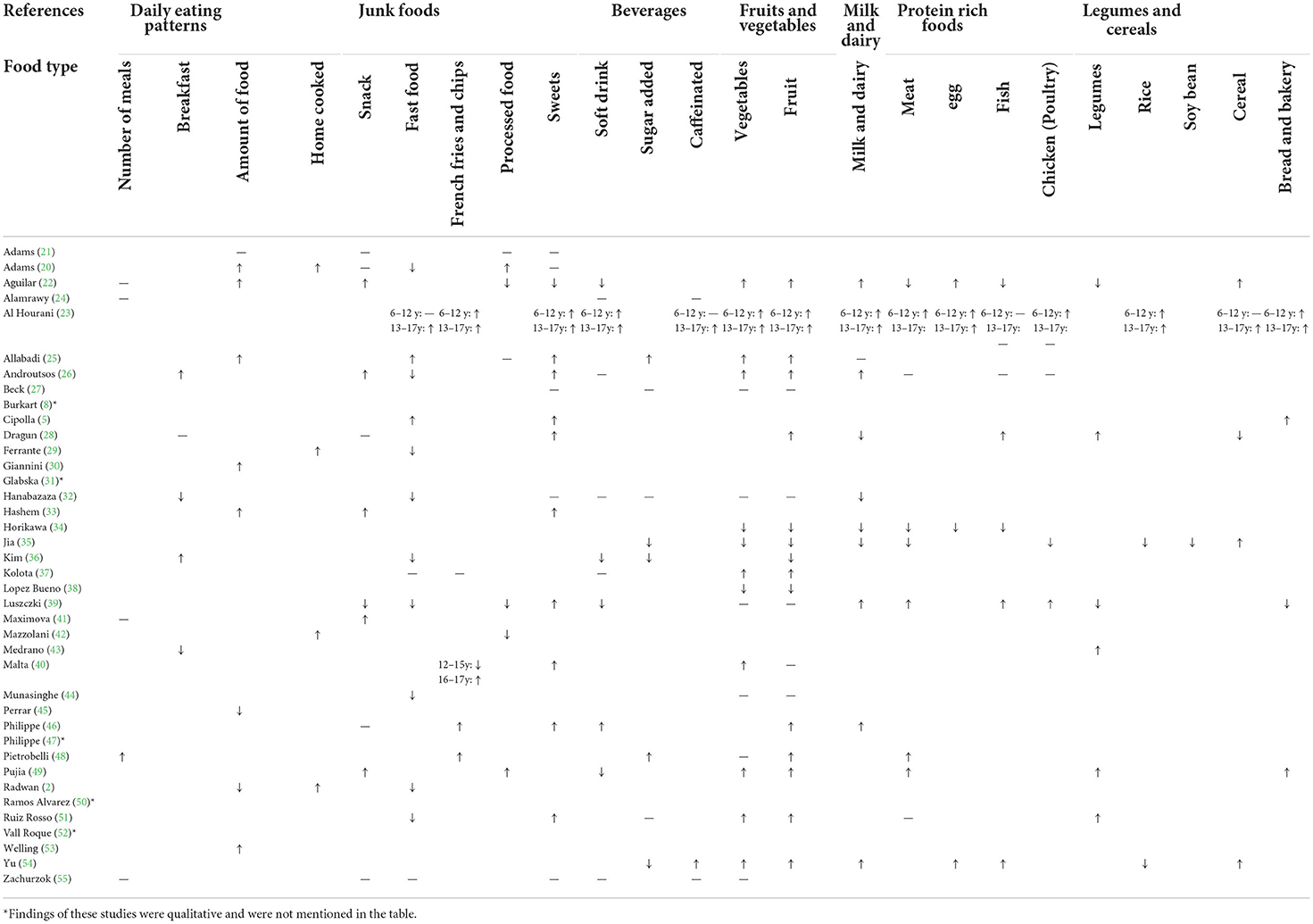
Table 2. Observed changes in eating habits in seven categories due to COVID-19 lockdowns in the 39 included studies.
A few studies reported that eating habit changes qualitatively. Medrano et al. evaluated adherence to the Mediterranean diet using the Mediterranean Diet Quality Index for children and teenagers (KIDMED) questionnaire (43). They observed that the KIDMED score increased among participants during confinements (43). In another study, dietary intake increased, and the pattern changed to unhealthy foods (unhealthy:+1.2 foods, 95% CI = 1.0, 1.5) (8). A study in Spain demonstrated that eating habits for 44.6% of women aged 14–24 years deteriorated since the lockdowns started, while 24.8% reported no change and 30.5% reported their eating habits got better (52).
To our knowledge, this is the first comprehensive systematic review that evaluated the impacts of the confinements during the COVID-19 era on children's and adolescents' eating habits.
As mentioned, we divided findings into categories to simplify assessing the results and understanding how children's and adolescents eating habits changed. We could see different results among studies, even those from the same country. Many parameters influence the obtained results.
The findings of the studies, in this case, were equivocal. All of the studies reported no change in the number of meals per day except one study, which was a study in Italy that included 41 children and adolescents. The information in this study was collected before COVID-19 started and just 3 weeks after the mandatory national quarantine started (48). An important factor influencing the outcome is the time the study was done. Included articles were conducted at different quarantine periods, for example, beginning, middle, or after the confinement. A youth's psychiatric condition, such as depression, anxiety, or insomnia, is significantly associated with her/his eating habits, including the number of meals, increased consumption of caffeinated or energy drinks, etc., (24). As a result of stress, boredom, and increased screen time led to irregularity in meal distribution (22).
There are controversies among studies' reports about breakfast consumption change during confinements. Two studies have reported a decrease in breakfast consumption during confinement compared with pre-pandemic (32, 43). On the other hand, another two studies indicated an increase (26, 36). One study did not find a significant difference in the frequency of breakfast consumption in their participants (28). Sleep patterns have changed during the COVID-19 era, and inadequate sleep is related to unhealthy diets such as skipping breakfast (37). Skipping breakfast is related to a higher risk of overweight and obesity in children and adolescents (62). On the other hand, due to school closure, children had more time to have regular meals. It is worth considering that the quality of the four studies was unsatisfactory except for Kim et al.'s study, a survey with 105,600 participants conducted in South Korea (36).
Confinements and stay-home orders led to positive changes in daily lifestyle, one of which was the increased consumption of home-cooked meals (2, 20, 29, 42). Closure of shops, malls, and restaurants or limited open hours have made respondents shift to home-cooked meals (2). Consuming more home-cooked food provides spending more time with family by participating in cooking, eating together, and communicating (20, 42). Parents are generally responsible for providing food for their children, so they should be educated about preparing healthy foods and building healthy eating habits (20, 42).
The amount of food is one of the important factors that identifies the household food environment and food security (20, 21). Most of the included studies have indicated an increase in the amount of food children and adolescents consumed during COVID-19 confinements compared with pre-pandemic (21, 22, 25, 30, 33, 53). In the families who became food insecure or stayed insecure, the amount of consumed foods has decreased (21). Economic crisis and loss of the source of income during a pandemic might limit access to food in disadvantaged families (2).
In accordance with our findings, in a systematic review by Mignogna et al., conducted among all age groups, an increase in food intake and the number of daily meals were observed (56).
We considered the most frequently evaluated junk food items in the included studies: snacks, fast foods, French fries or chips, processed food, and sweets.
It was hypothesized that stress, boredom, and long screen time exposure during confinements are associated with frequent snacking. Among the included studies in this review, five studies showed increased snacking. TV watching, laptop, and mobile screen time were significantly associated with frequent snacking between meals and at night (21). Other five articles reported no change in consumption of snacks (20, 21, 28, 46, 55). In a cohort study by Adams et al., unhealthy snack intake increased in May 2020 compared to before COVID-19. A few months later, in September 2020, participants' calorie-dense snack intake decreased. We can see that families and children adapted to confinement conditions over time (21).
Most studies indicated that fast food consumption decreased (2, 20, 26, 29, 32, 36, 39, 44, 51). As mentioned above, in the home-cooked category, fast food consumption decreased due to the closure and limited open hours of restaurants, malls, and cafes or the fear of becoming infected by the person delivering the food (2). In addition, parents and children tended to eat more healthy and homemade foods to enhance their health and immunity. The characteristic of the participants could be an important factor that has an impact on the obtained result. Clearly, children's eating habits differ from adolescents', or subjects with underlying diseases might have a specific diet compared with a healthy one (46). One study showed a significant increase in pizza consumption in those aged 13–17 compared with those aged 6–12 (23). Another study reported increased consumption of pizza, bread, and pasta to fill the time in children and adolescents who are overweight or suffering from obesity, and this study showed that the lockdowns worsened participants' eating habits (5).
“Convenience food” was considered processed food in this study. Three studies showed a decrease (22, 39, 42), and two showed no change in consumption of processed food (21, 25). The authors noted that the consumption of fast foods was reduced after “stay-home” orders. The decrease in processed and convenience food correlates with reduced fast food intake (22, 39). However, two studies reported an increase in processed food intake. Due to supply chain issues for healthy animal proteins, vegetables, and fruits during the pandemic, the costs increased. Therefore, Eating preferences were changed toward cheap and high-calorie foods like processed foods (24).
It is obvious that having lots of French fries is an unhealthy eating habit. Almost all the included articles pointed to increased consumption of French fries or potato chips (23, 46, 48).
In line with previous studies in children and adolescents or adults (56), most of the included studies (ten) indicated an increase in comfort unhealthy food consumption like sweets, desserts, pastries and cakes, candy, and chocolates in participants during confinements (5, 23, 25, 26, 28, 33, 39, 40, 46, 51). Eating is one of the coping mechanisms to reduce the intensity of negative stressors related to pandemics (63). Foods rich in sugar and fat are preferred as pleasant and instant rewards to distract a person from experiencing negative emotions (64). Only one study in Spain showed that intake of sweets and pastries decreased, especially in boys, and explained the lower social interactions during confinements could partly describe this change (22).
Generally, studies have shown discordant results in the consumption of different types of beverages and their changes during confinements. Most of the studies indicated no change in consumption of soft drinks, sugar-added drinks, and caffeinated drinks (24, 26, 27, 32, 37, 51, 55). Four studies reported a lower amount of soft drink consumption during COVID-19 than before confinement (22, 36, 39, 49). During Confinement eating out decreased, which could explain the lower consumption of soft drinks. By contrast, two studies showed a higher intake of soft drinks (23, 46). These controversies can be explained due to geographical differences and the time of studies. For example, one of the studies reported a higher intake of soft drinks conducted during the holy month of Ramadan in Jordanian adolescents (23).
Coffee is a good source of energy. Adolescents especially use coffee to improve their mood, depression, and cognitive function; these psychological changes were increased during the quarantine period (57–59); this view can explain the increased consumption of coffee in the adolescent age group in two studies (23, 54).
Three Good quality studies demonstrated a significant decrease in the intake of sugar-added drinks (35, 36, 54). Two other studies reported an increase in sugar-added beverages, but their questionnaire was invalid, and their population was not representative of all the nations' adolescents and children (25, 48).
Fresh fruits and vegetables are integral to a healthy lifestyle and diet; they are necessary for a healthy immune system. In this systematic review, twenty studies evaluated the intake of fruits, and eleven studies reported a significant increase in consumption of fruits (22, 23, 25, 26, 28, 37, 46, 48, 49, 51, 54), but four studies reported the opposite change (34–36, 38). Also, five studies did not show significant change during confinements compared to before the pandemic (27, 32, 39, 40, 44). Eighteen studies investigated the change in the consumption of vegetables. Nine articles demonstrated a significant increase (22, 23, 25, 26, 37, 40, 49, 51, 54), three articles showed a decrease (34, 35, 38), and six studies did not report significant change compared to before COVID-19 (27, 32, 39, 44, 48, 55). Finally, we can conclude that consumption of fruits and vegetables increased during the COVID-19 pandemic compared to before the pandemic. During confinement and COVID-19, People tended to change their diet to healthy foods such as fruits and vegetables. Low fruit and vegetable intake in some countries may be explained by lower availability and higher price. In some countries, COVID-19 tremendously affected farms and industries (60). For example, tight quarantine rules in China and the USA led to difficulties in going out of the house, and therefore, the availability of fruits and vegetables decreased (61). Thus, governments have to consider these problems in farming fruits and vegetables and look for solutions for same situation like COVID-19 pandemics may happen in future again.
Findings of studies about dairy and milk intake are disputed. Six studies reported an increase (22, 23, 26, 39, 46, 54). On the other hand, four of them showed a decrease in the consumption of milk and dairy products (28, 32, 34, 35). In some countries, dairy industries were influenced by the COVID-19 pandemic due to the closure of restaurants, worker shortage, difficulties in transportation, etc., (61), so lower intake of dairy products could be explained by this point of view. Generally, we can not find an exact answer to how dairy intake has changed during confinement.
Protein-rich foods play an important role in healthy human nutrition with their high protein, vitamin, and mineral contents. So, protein-rich foods are recommended for a healthy diet (62). In this systematic review, nine articles investigated intake of meat during COVID-19 (22, 23, 26, 34, 35, 39, 48, 49, 51).four studies reported increased intake (23, 39, 48, 49), and three other articles showed decreased intake (22, 34, 35). Also, two articles did not report a significant change in meat consumption during COVID-19 compared to before COVID-19 (26, 51). World disasters and pandemics throughout history have influenced the consumption of protein-rich foods. Therefore, During the COVID-19 pandemic confinements, people were confronted with difficulties. For example, meat producers have faced problems in meat harvesting and shipment of products, and all of these reasons adversely impacted meat production (63). Socioeconomic status (SES) is another factor that plays a crucial role in eating habits. People with disadvantaged SES were more prone to worsen their diet and eating habits (39). Due to the pandemic and restrictions, changes occurred in SES in most families, and pre-existing inequalities were exacerbated (45).
Additionally, included studies showed ambiguous results in consuming egg, fish, and chicken intake. Four studies investigated egg consumption in children and adolescents; three reported an increase, and one reported decreased intake of eggs (22, 23, 34, 54). Seven studies evaluated fish consumption in children and adolescents (22, 23, 26, 28, 34, 39, 54). Three articles showed increased fish intake. Two studies reported a decrease, and two did not report any significant change in fish intake. Only four studies evaluated chicken and poultry intake (23, 26, 35, 39). One study reported an increase, one showed a decrease, and one did not report a significant change. In conclusion, included studies showed various results among children and adolescents. We need further research with higher validity to improve our knowledge about protein-rich food intake change during COVID-19 compared to before the pandemic.
Six studies reported changes in the consumption of legumes. Children and adolescents significantly increased their consumption of legumes except for Spain and Poland children and adolescents (22, 28, 39, 43, 49, 51). Also, four studies reported changes in bread and bakery consumption during COVID-19 pandemic confinements, and all of them except a study performed in Poland reported a significant increase in consumption of bread and bakery compared to before the pandemic (5, 23, 39, 49). The study was conducted in Poland, used a validated questionnaire, and had a good quality assessment (39); however, the rest of the studies reported that increased bread and bakery consumption have poor qualities (5, 23, 49). Available data for consumption of rice, soybean, and cereal were limited. Just one article investigated soybean intake and reported a significant decrease in consumption before the pandemic (35). Also, just three studies evaluated rice consumption; one reported increased consumption (23), and two studies reported decreased consumption (35, 54). Due to limited data about these food types, we need further research investigating the intake of rice and soybean.
It has been shown that social well-functioning programs and food distribution systems can reduce the adverse effects of food insecurity induced by a different crisis. For example, Productive Safety Net Programme (PSNP) in Ethiopia during the pandemic showed a low risk of food insecurity (9.3%) in participants (64).
It is important to notice that this systematic review has some strengths and limitations. First, This is the first systematic review that summarizes the documents evaluating the Impact COVID-19 pandemic on children and adolescents' eating habits. Also, this study included many studies from all over the world. However, there were several limitations to this study. Firstly, most of the included studies are cross-sectional, and we recommend performing more longitudinal studies with longer follow up to evaluate longer consequences of dietary change during this period. Secondly, included studies had various designs and methodological aspects, which can make it difficult to reach exact conclusions about dietary changes; thirdly, most of the studies used online surveys for evaluating dietary change due to limitations of lockdowns, which can lead to recall bias in results because there were not any valid type of tool for dietary change assess. Recall bias decreases the value of reported changes because participants are likely to over or underestimate the answers in questionnaires. Included studies were conducted in several countries on the five continents with different cultures and specific eating habits which could be led to some inconsistency among observations.
Additionally, the availability of the internet is limited in lower-income countries and several groups of people. In most of the studies, dietary changes were evaluated in high and middle-income countries. In contrast, there is a greater probability of nutritional changes in low-income countries, especially during quarantine. For example, studies on adult populations in Nigeria, Mexico, and Bangladesh reported a significant worsening of food security status pre and post-pandemic periods based on earlier available data (65–67). The same results were reported for Uganda and Kenya (68).
The Impact of COVID-19 on children and adolescents' eating habits was both positive and negative, for example, a decrease in fast food, fruits, and vegetable consumption vs. an increase in snacking and sweet consumption. Both changes have significant short-term and long-term impacts on population health. This study could give us clues about changes in eating habits in children and adolescents during confinements. It is worth noting that eating habits established during the pandemic in children and adolescents could affect eating habits in future years and these changes could last until adulthood (20). Thus, we can use them to improve the negative changes during the COVID-19 era.
MQ and H-SE came with the idea of this article. FP, ME, and AE did the study search and evaluate the articles. FP and ME wrote the manuscript and the tables. MQ and H-SE did the final proof of the article. All authors contributed to the article and approved the submitted version.
This study was approved by the Alborz University of Medical Science.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.1004953/full#supplementary-material
COVID-19, Corona Virus Disease 2019; PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses; SES, Socioeconomic Status; PSNP, Productive Safety Net Programme; FP, Farzad Pourghazi; ME, Maysa Eslami.
1. Bakaloudi DR, Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Chourdakis M. Impact of the first COVID-19 lockdown on body weight: a combined systematic review and a meta-analysis. Clin Nutr. (2021) 1. doi: 10.1016/j.clnu.2021.04.015
2. Radwan H, Al Kitbi M, Hasan H, Al Hilali M, Abbas N, Hamadeh R, et al. Indirect health effects of covid-19: unhealthy lifestyle behaviors during the lockdown in the united arab emirates. Int J Environ Res Public Health. (2021) 18:1964. doi: 10.3390/ijerph18041964
3. Morres ID, Galanis E, Hatzigeorgiadis A, Androutsos O, Theodorakis Y. Physical activity, sedentariness, eating behaviour and well-being during a COVID-19 lockdown period in Greek adolescents. Nutrients. (2021) 13:1449. doi: 10.3390/nu13051449
4. Barr-Anderson DJ, Hazzard VM, Hahn SL, Folk AL, Wagner BE, Neumark-Sztainer D. Stay-at-home orders during COVID-19: the influence on physical activity and recreational screen time change among diverse emerging adults and future implications for health promotion and the prevention of widening health disparities. Int J Environ Res Public Health. (2021) 18:13228. doi: 10.3390/ijerph182413228
5. Cipolla C, Curatola A, Ferretti S, Giugno G, Condemi C, Delogu AB, et al. Eating habits and lifestyle in children with obesity during the COVID19 lockdown: A survey in an Italian center. Acta Biomed. (2021) 92:e2021196. doi: 10.23750/abm.v92i2.10912
6. Da Silva FR, Junior AHL, Brant VM, Lôbo ILB, Lancha LOP, Silva A, et al. The effects of COVID-19 quarantine on eating and sleeping behaviors. Nutrire. (2020) 45:1–4. doi: 10.1186/s41110-020-00128-y
7. González-Monroy C, Gómez-Gómez I, Olarte-Sánchez CM, Motrico E. Eating behaviour changes during the COVID-19 pandemic: a systematic review of longitudinal studies. Int J Environ Res Public Health. (2021) 18:11130. doi: 10.3390/ijerph182111130
8. Burkart S, Parker H, Weaver RG, Beets MW, Jones A, Adams EL, et al. impact of the COVID-19 pandemic on elementary schoolers' physical activity, sleep, screen time and diet: a quasi-experimental interrupted time series study. Pediatr Obes. (2022) 17:e12846. doi: 10.1111/ijpo.12846
9. Preedy VR, Watson RR. Handbook of Disease Burdens and Quality of Life Measures. New York, NY: Springer (2010).
10. O'Neil A, Quirk SE, Housden S, Brennan SL, Williams LJ, Pasco JA, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. (2014) 104:e31–42. doi: 10.2105/AJPH.2014.302110
11. Storz MA. The COVID-19 pandemic: an unprecedented tragedy in the battle against childhood obesity. Clin Exp Pediatr. (2020) 63:477. doi: 10.3345/cep.2020.01081
12. Zemrani B, Gehri M, Masserey E, Knob C, Pellaton R, A. hidden side of the COVID-19 pandemic in children: the double burden of undernutrition and overnutrition. Int J Equity Health. (2021) 20:1–4. doi: 10.1186/s12939-021-01390-w
13. Cena H, Fiechtner L, Vincenti A, Magenes VC, De Giuseppe R, Manuelli M, et al. COVID-19 pandemic as risk factors for excessive weight gain in pediatrics: the role of changes in nutrition behavior. a narrative review. Nutrients. (2021) 13:4255. doi: 10.3390/nu13124255
14. Bennett G, Young E, Butler I, Coe S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: a scoping review. Front Nutr. (2021) 8:53. doi: 10.3389/fnut.2021.626432
15. Neira C, Godinho R, Rincón F, Mardones R, Pedroso J. Consequences of the covid-19 syndemic for nutritional health: a systematic review. Nutrients. (2021) 13:1168. doi: 10.3390/nu13041168
16. Zupo R, Castellana F, Sardone R, Sila A, Giagulli VA, Triggiani V, et al. Preliminary trajectories in dietary behaviors during the COVID-19 pandemic: a public health call to action to face obesity. Int J Environ Res Public Health. (2020) 17:7073. doi: 10.3390/ijerph17197073
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:1–11. doi: 10.1186/s13643-021-01626-4
18. Moskalewicz A, Oremus M. No clear choice between Newcastle–Ottawa scale and appraisal tool for cross-sectional studies to assess methodological quality in cross-sectional studies of health-related quality of life and breast cancer. J Clin Epidemiol. (2020) 120:94–103. doi: 10.1016/j.jclinepi.2019.12.013
19. Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. Newcastle-Ottawa Quality Assessment Scale Cohort Studies. Ottawa, ON: University of Ottawa (2014).
20. Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity. (2020) 28:2056–63. doi: 10.1002/oby.22996
21. Adams EL, Caccavale LJ, Smith D, Bean MK. Longitudinal patterns of food insecurity, the home food environment, and parent feeding practices during COVID-19. Obes Sci Pract. (2021). doi: 10.1002/osp4.499
22. Aguilar-Martinez A, Bosque-Prous M, Gonzalez-Casals H, Colillas-Malet E, Puigcorbe S, Esquius L, et al. Social inequalities in changes in diet in adolescents during confinement due to COVID-19 in Spain: the DESKcohort project. Nutrients. (2021) 13:1577. doi: 10.3390/nu13051577
23. Al Hourani H, Alkhatib B, Abdullah M. Impact of COVID-19 lockdown on body weight, eating habits, and physical activity of jordanian children and adolescents. Disaster Medicine and Public Health Preparedness (Cambridge University Press) (2021) 1–9. doi: 10.1017/dmp.2021.48
24. Alamrawy RG, Fadl N, Khaled A. Psychiatric morbidity and dietary habits during COVID-19 pandemic: a cross-sectional study among Egyptian Youth (14–24 years). Middle East Current Psychiatry. (2021) 28. doi: 10.1186/s43045-021-00085-w
25. Allabadi H, Dabis J, Aghabekian V, Khader A, Khammash U. Impact of COVID-19 lockdown on dietary and lifestyle behaviours among adolescents in Palestine. Dynam Human Health. (2020) 7:2170.
26. Androutsos O, Perperidi M, Georgiou C, Chouliaras G. Lifestyle changes and determinants of children's and adolescents' body weight increase during the first COVID-19 lockdown in Greece: the COV-EAT study. Nutrients. (2021) 13:930. doi: 10.3390/nu13030930
27. Beck AL, Huang JC, Lendzion L, Fernandez A, Martinez S. Impact of the coronavirus disease 2019 pandemic on parents' perception of health behaviors in children with overweight and obesity. Acad Pediatr. (2021) 21:1434–40. doi: 10.1016/j.acap.2021.05.015
28. Dragun R, Vecek NN, Marendic M, Pribisalic A, Divic G, Cena H, et al. Have lifestyle habits and psychological well-being changed among adolescents and medical students due to COVID-19 lockdown in Croatia? Nutrients. (2020) 13:97. doi: 10.3390/nu13010097
29. Ferrante MJ, Goldsmith J, Tauriello S, Epstein LH, Leone LA, Anzman-Frasca S. Food acquisition and daily life for U.S. families with 4-to 8-year-old children during COVID-19: findings from a nationally representative survey. Int J Environ Res Public Health. (2021) 18:1734. doi: 10.3390/ijerph18041734
30. Giannini DT, Tavares CM, Takey M, Aloise MLR, da Costa AJ, de Carvalho DS, et al. Adolescents emotional state and behavioral and dietary habit changes during isolation due to the COVID-19 pandemic. J Am Nutr Assoc. (2022) 41:415–23. doi: 10.1080/07315724.2021.1897899
31. Glabska D, Skolmowska D, Guzek D. Population-based study of the changes in the food choice determinants of secondary school students: polish adolescents' COVID-19 experience (PLACE-19) study. Nutrients. (2020) 12:2640. doi: 10.3390/nu12092640
32. Hanbazaza M, Wazzan H. Changes in eating habits and lifestyle during COVID-19 curfew in children in Saudi Arabia. Nutr Res Pract. (2021) 15:S41–52. doi: 10.4162/nrp.2021.15.S1.S41
33. Hashem SA, El Refay AS, Mostafa HH, Kamel IH, Sherif LS. Impact of coronavirus disease-19 lockdown on Egyptian children and adolescents: dietary pattern changes health risk. Open Access Maced J Med Sci. (2020) 8:561–9. doi: 10.3889/oamjms.2020.5249
34. Horikawa C, Murayama N, Kojima Y, Tanaka H, Morisaki N. Changes in selected food groups consumption and quality of meals in japanese school children during the COVID-19 pandemic. Nutrients. (2021) 13:2743. doi: 10.3390/nu13082743
35. Jia P, Liu L, Xie X, Yuan C, Chen H, Guo B, et al. Changes in dietary patterns among youths in China during COVID-19 epidemic: the COVID-19 impact on lifestyle change survey (COINLICS). Appetite. (2021) 158:105015. doi: 10.1016/j.appet.2020.105015
36. Kim SY, Yoo DM, Min C, Choi HG. Changes in dietary habits and exercise pattern of Korean adolescents from prior to during the COVID-19 pandemic. Nutrients. (2021) 13:3314. doi: 10.3390/nu13103314
37. Kolota A, Glabska D. COVID-19 pandemic and remote education contributes to improved nutritional behaviors and increased screen time in a polish population-based sample of primary school adolescents: diet and activity of youth during COVID-19 (DAY-19) study. Nutrients. (2021) 13:1596. doi: 10.3390/nu13051596
38. Lopez-Bueno R, Lopez-Sanchez GF, Casajus JA, Calatayud J, Gil-Salmeron A, Grabovac I, et al. Health-related behaviors among school-aged children and adolescents during the Spanish Covid-19 confinement. Front Pediatr. (2020) 8:573. doi: 10.3389/fped.2020.00573
39. Luszczki E, Bartosiewicz A, Pezdan-Sliz I, Kuchciak M, Jagielski P, Oleksy L, et al. Children's eating habits, physical activity, sleep, and media usage before and during COVID-19 pandemic in Poland. Nutrients. (2021) 13:2447. doi: 10.3390/nu13072447
40. Malta DC, Gomes CS, Barros MBA, Lima MG, Silva AGD, Cardoso LSM, et al. The COVID-19 pandemic and changes in the lifestyles of Brazilian adolescents. Rev Bras Epidemiol. (2021) 24:e210012. doi: 10.1590/1980-549720210012
41. Maximova K, Khan MKA, Dabravolskaj J, Maunula L, Ohinmaa A, Veugelers PJ. Perceived changes in lifestyle behaviours and in mental health and wellbeing of elementary school children during the first COVID-19 lockdown in Canada. Public Health. (2022) 202:35–42. doi: 10.1016/j.puhe.2021.10.007
42. Mazzolani BC, Smaira FI, Astley C, Iraha AY, Pinto AJ, Marques IG, et al. Changes in eating habits and sedentary behavior during the COVID-19 pandemic in adolescents with chronic conditions. Front Pediatr. (2021) 9:714120. doi: 10.3389/fped.2021.714120
43. Medrano M, Cadenas-Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: a longitudinal analysis from the MUGI project. Pediatr Obes. (2021) 16:e12731. doi: 10.1111/ijpo.12731
44. Munasinghe S, Sperandei S, Freebairn L, Conroy E, Jani H, Marjanovic S, et al. The impact of physical distancing policies during the COVID-19 pandemic on health and well-being among Australian adolescents. J Adolesc Health. (2020) 67:653–61. doi: 10.1016/j.jadohealth.2020.08.008
45. Perrar I, Alexy U, Jankovic N. Changes in total energy, nutrients and food group intake among children and adolescents during the COVID-19 pandemic-results of the DONALD study. Nutrients. (2022) 14:297. doi: 10.3390/nu14020297
46. Philippe K, Chabanet C, Issanchou S, Monnery-Patris S. Child eating behaviors, parental feeding practices and food shopping motivations during the COVID-19 lockdown in France: (How) did they change? Appetite. (2021) 161:105132. doi: 10.1016/j.appet.2021.105132
47. Philippe K, Issanchou S, Monnery-Patris S. Contrasts and ambivalences in French parents' experiences regarding changes in eating and cooking behaviours during the COVID-19 lockdown. Food Qual Prefer. (2022) 96:104386. doi: 10.1016/j.foodqual.2021.104386
48. Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in verona, Italy: a longitudinal study. Obesity. (2020) 28:1382–5. doi: 10.1002/oby.22861
49. Pujia R, Ferro Y, Maurotti S, Khoory J, Gazzaruso C, Pujia A, et al. The effects of COVID-19 on the eating habits of children and adolescents in Italy: a pilot survey study. Nutrients. (2021) 13:2641. doi: 10.3390/nu13082641
50. Ramos Alvarez O, Arufe Giraldez V, Cantarero Prieto D, Ibanez Garcia A. Changes in physical fitness, dietary habits and family habits for Spanish children during SARS-CoV-2 lockdown. Int J Environ Res Public Health. (2021) 18:13293. doi: 10.3390/ijerph182413293
51. Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, Ulloa N, Brun P, Acevedo-Correa D, et al. Covid-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. (2020) 12:1807. doi: 10.3390/nu12061807
52. Vall-Roqué H, Andrés A, Saldaña C. The impact of COVID-19 pandemic and lockdown measures on eating disorder risk and emotional distress among adolescents and young people in Spain. Behav Psychol. (2021) 29:345–64. doi: 10.51668/bp.8321208n
53. Welling MS, Abawi O, van den Eynde E, van Rossum EFC, Halberstadt J, Brandsma AE, et al. Impact of the COVID-19 pandemic and related lockdown measures on lifestyle behaviors and well-being in children and adolescents with severe obesity. Obes Facts. (2022) 15:186–96. doi: 10.1159/000520718
54. Yu B, Zhang D, Yu W, Luo M, Yang S, Jia P. Impacts of lockdown on dietary patterns among youths in China: the COVID-19 Impact on Lifestyle Change Survey. Public Health Nutr. (2021) 24:3221–32. doi: 10.1017/S1368980020005170
55. Zachurzok A, Wojcik M, Gawlik A, Starzyk JB, Mazur A. An attempt to assess the impact of pandemic restrictions on the lifestyle, diet, and body mass index of children with endocrine diseases-preliminary results. Nutrients. (2021) 14:156. doi: 10.3390/nu14010156
56. Mignogna C, Costanzo S, Ghulam A, Cerletti C, Donati MB, de Gaetano G, et al. Impact of nationwide lockdowns resulting from the first wave of the COVID-19 pandemic on food intake, eating behaviors, and diet quality: a systematic review. Adv Nutr. (2022) 13:388–423. doi: 10.1093/advances/nmab130
57. Abalo R. Coffee and Caffeine Consumption for Human Health. Basel: Multidisciplinary Digital Publishing Institute (2021). p. 2918.
58. Haskell-Ramsay CF, Jackson PA, Forster JS, Dodd FL, Bowerbank SL, Kennedy DO. The acute effects of caffeinated black coffee on cognition and mood in healthy young and older adults. Nutrients. (2018) 10:1386. doi: 10.3390/nu10101386
59. Nehlig A. Effects of coffee/caffeine on brain health and disease: what should I tell my patients? Pract Neurol. (2016) 16:89–95. doi: 10.1136/practneurol-2015-001162
60. Filip R, Anchidin-Norocel L, Gheorghita R, Savage WK, Dimian M. Changes in dietary patterns and clinical health outcomes in different countries during the SARS-CoV-2 pandemic. Nutrients. (2021) 13:3612. doi: 10.3390/nu13103612
61. Qingbin W, Liu C-q, Zhao Y-f, Kitsos A, Cannella M, Wang S-k, et al. Impacts of the COVID-19 pandemic on the dairy industry: lessons from China and the United States and policy implications. J Integr Agric. (2020) 19:2903–15. doi: 10.1016/S2095-3119(20)63443-8
62. Haskaraca G, Bostanci E, Arslan Y. Effects of the COVID-19 pandemic on eating and meat consumption habits of Turkish adults. Turkish J Agric Food Sci Technol. (2021) 9:63–9. doi: 10.24925/turjaf.v9i1.63-69.3704
63. Ijaz M, Yar MK, Badar IH, Ali S, Islam MS, Jaspal MH, et al. Meat production and supply chain under COVID-19 scenario: current trends and future prospects. Front Vet Sci. (2021) 8:660736. doi: 10.3389/fvets.2021.660736
64. Abay K, Berhane G, Hoddinott J, Tafere K. COVID-19 and Food Security in Ethiopia: Do Social Protection Programs Protect? Chicago, IL: University of Chicago Press (2020). doi: 10.1086/715831
65. Gaitán-Rossi P, Vilar-Compte M, Teruel G, Pérez-Escamilla R. Food insecurity measurement and prevalence estimates during the COVID-19 pandemic in a repeated cross-sectional survey in Mexico. Public Health Nutr. (2021) 24:412–21. doi: 10.1017/S1368980020004000
66. Amare M, Abay KA, Tiberti L, Chamberlin J. Impacts of COVID-19 on food security: panel data evidence from Nigeria. IFPRI Discussion Paper 1956. Washington, DC: International Food Policy Research Institute (IFPRI). doi: 10.2499/p15738coll2.133866
67. Hamadani JD, Hasan MI, Baldi AJ, Hossain SJ, Shiraji S, Bhuiyan MSA, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health. (2020) 8:e1380–e9. doi: 10.1016/S2214-109X(20)30366-1
Keywords: COVID-19, children, adolescence, eating habits, pandemic
Citation: Pourghazi F, Eslami M, Ehsani A, Ejtahed H-S and Qorbani M (2022) Eating habits of children and adolescents during the COVID-19 era: A systematic review. Front. Nutr. 9:1004953. doi: 10.3389/fnut.2022.1004953
Received: 27 July 2022; Accepted: 04 October 2022;
Published: 18 October 2022.
Edited by:
William Tebar, University of São Paulo, BrazilReviewed by:
Yvelise Ferro, Magna Græcia University, ItalyCopyright © 2022 Pourghazi, Eslami, Ehsani, Ejtahed and Qorbani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hanieh-Sadat Ejtahed, aGFuaWVqdGFoZWRAeWFob28uY29t; Mostafa Qorbani, bXFvcmJhbmkxMzc5QHlhaG9vLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.