- 1Department of Obstetrics and Gynecology, Affiliated Hospital of Jining Medical University, Zaozhuang Municipal Hospital, Zaozhuang, China
- 2Department of Obstetrics and Gynecology, The Second Affiliated Hospital of Shandong University, Jinan, China
- 3Department of Cardiology, Heart Center Leipzig at University Leipzig, Leipzig, Germany
- 4Department of Gynecology, Affiliated Hospital of Jining Medical University, Zaozhuang Municipal Hospital, Zaozhuang, China
Objective: Diet lifestyle can influence the risk of endometriosis. Therefore, we conducted a systematic meta-analysis to investigate the association between dairy products and the risk of endometriosis. Besides, we performed a dose-response meta-analysis to evaluate the amount of dairy intake affecting the risk of endometriosis.
Methods: Relevant studies were searched from Pubmed, Embase databases, Cochrane Library, and Web of Science from the inception to November 6th, 2020. Also, the dose-response meta-analysis was conducted. All the pooled results were performed by risk ratios (RRs).
Results: Finally, seven high-quality studies were included in the present meta-analysis. Total dairy intake was inversely associated with the risk of endometriosis, and the risk of endometriosis tended to decrease with a decrease in the risk of endometriosis when dairy products intake was over 21 servings/week (RR 0.87, 95% CI 0.76–1.00; pnon−linearity = 0.04). Similarly, people who consumed more than 18 servings of high-fat dairy products per week had a reduced risk of endometriosis (RR 0.86, 95% CI 0.76–0.96). When stratified-analyses were conducted based on specific dairy product categories, it indicated that people with high cheese intake might have a reduced risk of endometriosis (RR 0.86, 95% CI 0.74–1.00). Other specific dairy products such as whole milk (RR 0.90, 95% CI 0.72–1.12), reduced-fat/skim milk (RR 0.83, 95% CI 0.50–1.73), ice cream (RR 0.83, 95% CI 0.50–1.73), and yogurt (RR 0.83, 95% CI 0.62–1.11) have not shown significant evidence of an association with the risk of endometriosis. However, there is a higher risk of endometriosis in the females with high butter intake compared to females with low butter intake (1.27, 95% CI 1.03–1.55).
Conclusions: Overall, dairy products intake was associated with a reduction in endometriosis, with significant effects when the average daily intake ≥3 servings. When analyzed according to the specific type of dairy product, it was shown that females with higher high-fat dairy and cheese intake might have a reduced risk of endometriosis. However, high butter intake might be associated to the increased risk of endometriosis. More future studies are needed to validate and add to this finding.
Introduction
Endometriosis was defined as a growing infiltrate of endometrial tissue (glands and mesenchyme) outside the endometrium that bleeds repeatedly to form nodules and masses causing pain and may invade any part of the body, such as the bladder, kidneys, ureter, lungs, pleura, affecting the quality of life (1). Endometriosis was a devastating disease for reproductive women. It was reported that endometriosis affected 5–15% of women of reproductive age (2), of whom 30–50% are infertile (3). Although the occurrence of endometriosis is considered to be associated with risk factors such as immune, endocrine, genetic, and anatomical disorders (4, 5), the etiology of the disease is not fully clear (6).
Diet is a highly controllable risk factor for many chronic diseases, but its contributing role to endometriosis has not been extensively explored (7). A literature review from Parazzini et al. (8) suggested that women with endometriosis appear to consume fewer vegetables and omega-3 polyunsaturated fatty acids while consuming higher amounts of red meat, coffee, and trans fats. Dairy products as an important part of the diet are rich in a variety of amino acids and high in calcium, making them an ideal nutritious food. Studies have shown that dairy products and dietary calcium intake are negatively correlated with oxidative and inflammatory stress (9–12). Besides, a high intake of dairy products might reduce vascular inflammation (9). Retrograde menstruation is postulated to be a potential causal catalyst for endometriosis, and the high magnesium levels found in dairy products would relax smooth muscle and might reduce retrograde menstruation (13). Therefore, some researchers have hypothesized that dairy products intake might reduce the risk of endometriosis, while based on the currently limited studies this hypothesis has not been well-established. To address these gaps, we conducted a systematic meta-analysis to investigate the association between dairy products and the risk of endometriosis. Besides, we performed a dose-response meta-analysis to evaluate the amount of dairy intake affecting the risk of endometriosis.
Methods
Search Strategy
The protocol and report of this meta-analysis were based on a meta-analysis of observational studies from the Guidelines on Epidemiology (MOOSE) (14). Relevant studies were searched from Pubmed, Embase databases, Cochrane Library, and Web of Science from the inception to February 7th, 2021. Also, a manual library search was conducted. Two groups of medical subject headings (MeSH), including “dairy products” and “endometriosis” were used to ensure a comprehensive search. In addition, previous meta-analyses and systematic reviews were reviewed for full inclusion in the study, if applicable. A detailed search strategy is provided in Appendix 1.
Study Selection
The inclusion criteria for this study were as follows:
(1) Dairy intake as the exposure of interests.
(2) Control group was non-dairy intake or less frequent dairy intake.
(3) The endpoint of the study was the occurrence of endometriosis.
(4) Study type was restricted to case-control, cohort study or randomized controlled trial.
(5) There were available data on the maximum adjustment risk ratios (RRs), odds ratios (ORs), hazard ratios (HRs), together with corresponding 95% confidence intervals (CIs) in the study. Exclusion criteria:
(1) Studies on non-dairy intake.
(2) The endpoint of the study was non-occurrence of endometriosis.
(3) Cross-sectional studies were excluded.
(4) Conference abstracts, letters, and case reports were excluded.
Data Extraction and Quality Assessment
The following data were extracted using the Unified Data List, including first author, publication year, country, study design, sample, date of recruitment, age, dairy consumption, type of dairy, dairy consumption, and endometriosis ascertainment were also recorded. The maximum covariate-adjusted ORs, RRs, HRs were extracted. Any disagreements or disputes that arose during the data extraction process were resolved by mutual agreement. Besides, the study used the Newcastle-Ottawa Scale (NOS) (15) to assess the quality of the study, with an overall score of 9 points. Specifically, studies with a NOS score of more than 6 stars were considered high-quality studies, while studies with a NOS score of fewer than 6 stars were considered low-quality studies.
Statistical Analysis
The first primary endpoint of this study was a qualitative analysis of the relationship between dairy product intake and the risk of endometriosis. In general, HR is equal to RR, which can be roughly considered as RR (16). ORs were also converted to RRs, RR = OR/[(1-P0) + (P0 × OR)], where P0 indicates the incidence of the outcome in the unexposed group (17). The corresponding 95% CI is: SElog(RR) = SElog(OR) × log(RR)/log(OR) (18). When the P0 was low (<10%), the odds ratio is very similar to the risk ratio (16). Therefore, all the data are expressed as RRs. Inter-study heterogeneity between studies was evaluated using the I2 statistic, where I2 values of 25, 50, and 75% indicate low, moderate, and high inconsistency, respectively. Besides, we performed subgroup analysis and meta-regression to explore potential sources of heterogeneity and to compare different groups. Sensitivity analyses were performed by eliminating one study at a time to examine its impact on the combined results. To estimate the combined RRs more conservatively, we used a random-effects model, as it better explained the heterogeneity between studies. In addition, publication bias was assessed by Begg's and Egger's test (19, 20).
The second endpoint of this study was to systematically assess the effect of dairy product intake on endometriosis. To this end, we conducted a quantitative dose-response meta-analysis. To maximize the available studies, we used the robust error meta-regression approach described by Xu and Doi (21) to establish a potential dose-response relationship between dairy product intake and the risk of endometriosis. In this “one-stage” framework approach, each included study was treated as a cluster across the whole population, which required that the studies include at least two categories. In this study, the restricted cubic spline was employed to fit the potential non-linear trend with three knots, and the non-linear P-value was calculated by testing the second spline coefficient of zero. The non-linear model was adopted when P for non-linear ≤ 0.05; otherwise, the linear model was adopted. In general, the included studies needed to take the category of lowest dose as the reference, and when the study of the non-lowest dose was taken as the reference, we converted it through the Excel macro file made by Hamling et al. (22) based on Greenland and Longnecker's theory (23). When the number of cases in a category was missing, the original authors were contacted. Besides, when studying open intervals, the amplitude was assumed to be the same as the adjacent category (24). Referring to the Food Frequency Questionnaire (FFQ) scale, it is generally considered that one serving is 250 ml. Also, all doses are expressed in the form of servings/week for the convenience of calculation. All data were analyzed using Stata 12.0.
Results
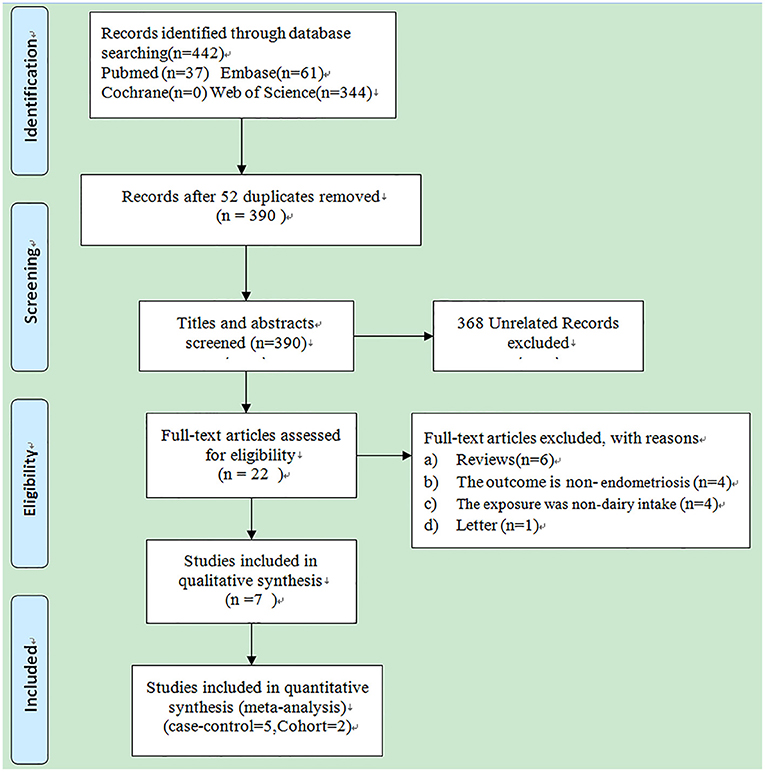
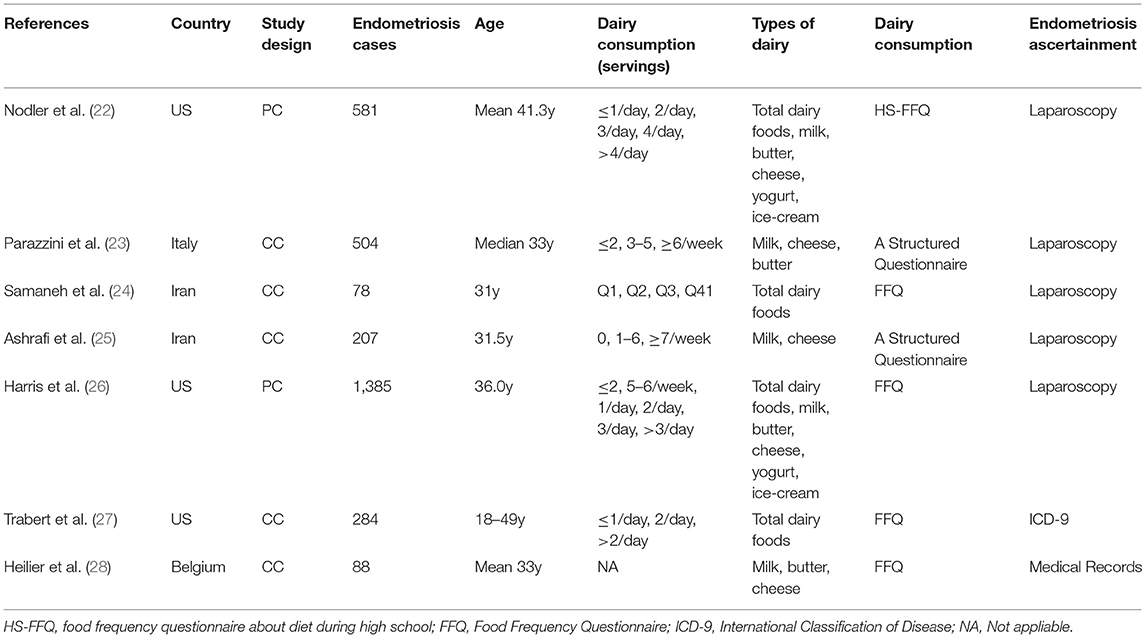
A total of 442 studies were searched from four electronic databases, PubMed, Embase, Cochrane library, and Web of science, as shown in Figure 1. Other additional studies were not revealed by manual search. Of these 442 studies, 52 were excluded because of duplication, whereas 368 unrelated studies were deleted after screening the titles and abstracts. The remaining 22 studies were carefully read in full, of which 15 were excluded for the following reasons: (a) review (n = 6); (b). The outcome is non-endometriosis (n = 4); (c). The exposure was non-dairy intake (n = 4); (d) Letter (n = 1). Finally, seven observational studies (25–31) were included in the present meta-analysis, including 5 case-control studies and 2 cohort studies. Baseline characteristics of all included studies are shown in Table 1. Two of the seven included observational studies reported an association between whole milk, ice cream, yogurt, and reduced-fat/skim milk intake and the risk of endometriosis; three studies reported an association between low-fat dairy, high-fat dairy and butter intake and the development of endometriosis; four studies reported an association between total dairy intake and the risk of endometriosis; five studies reviewed an association between the intake of milk, cheese and the risk of endometriosis. For dose-response meta-analysis, four studies focused on the relationship between the consumption of milk, cheese and the occurrence of endometriosis; three studies focusing on the correlation between total dairy products intake and the development of endometriosis; two studies focusing on the association between high-fat dairy products consumption and the risk of endometriosis. The quality of the included studies is assessed in Supplementary Table 1. Of these 7 studies, 3 scored 8 stars; 4 scored 7 stars. All studies scored 6 stars or higher and were considered high-quality studies.
Meta-Analysis
Total Dairy Product (High vs. Low)
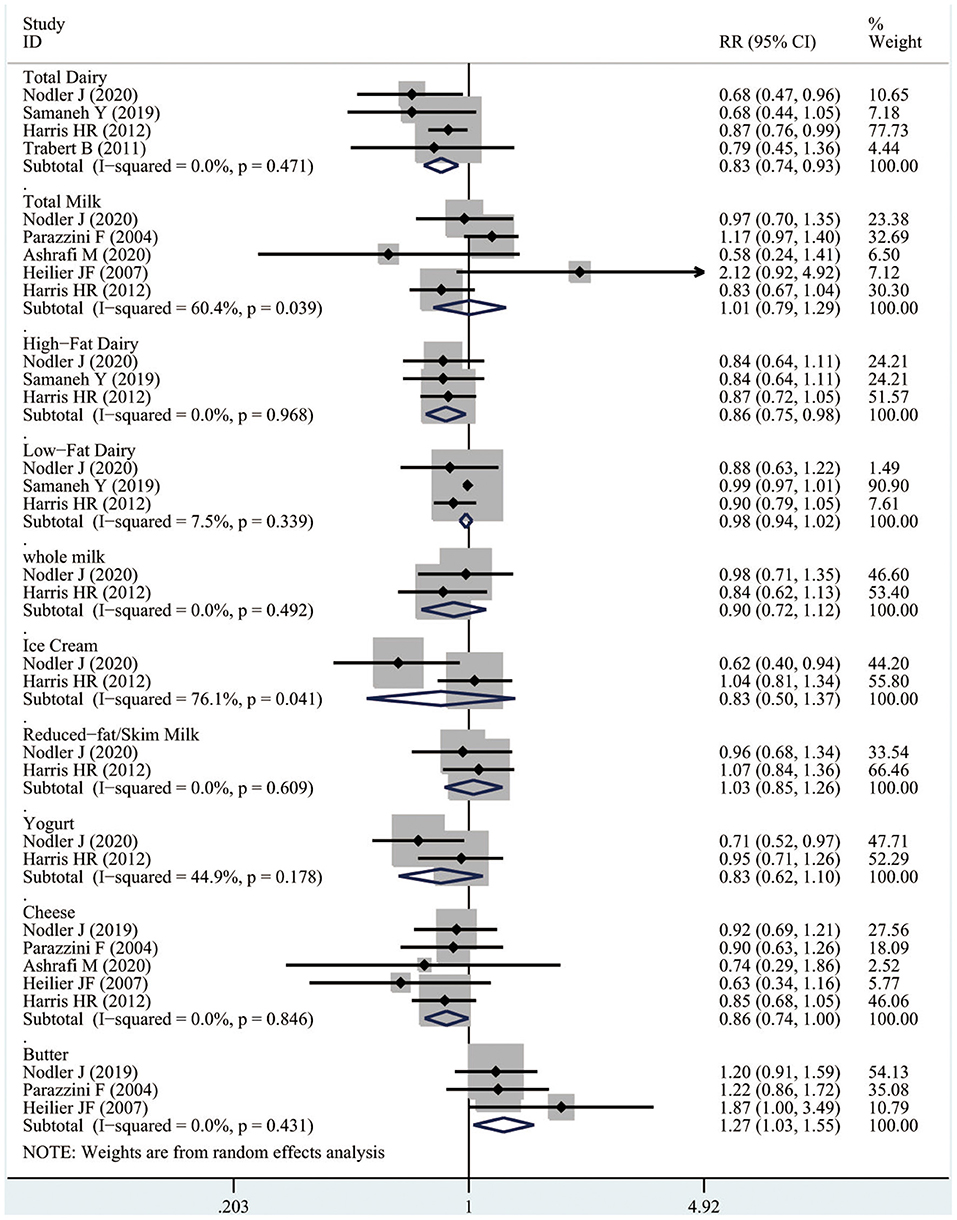
As shown in Figure 2, four studies involving 2,328 cases reported the association between total dairy products intake and the risk of endometriosis. Compared with the low dairy products intake, women with high dairy products would have a reduced risk of endometriosis (RR 0.83, 95% CI 0.74–0.93; I2 0%).
Three studies containing a total of 2,250 cases were included in the dose-response meta-analysis. As illustrated in Figure 3A, total dairy intake was inversely associated with the risk of endometriosis. Specifically, as total dairy intake increased, the risk of endometriosis tended to decrease, with a significant decrease in the risk of endometriosis when dairy products intake was ≥21 servings/week (RR 0.87, 95% CI 0.76–1.00; pnon−linearity = 0.04).
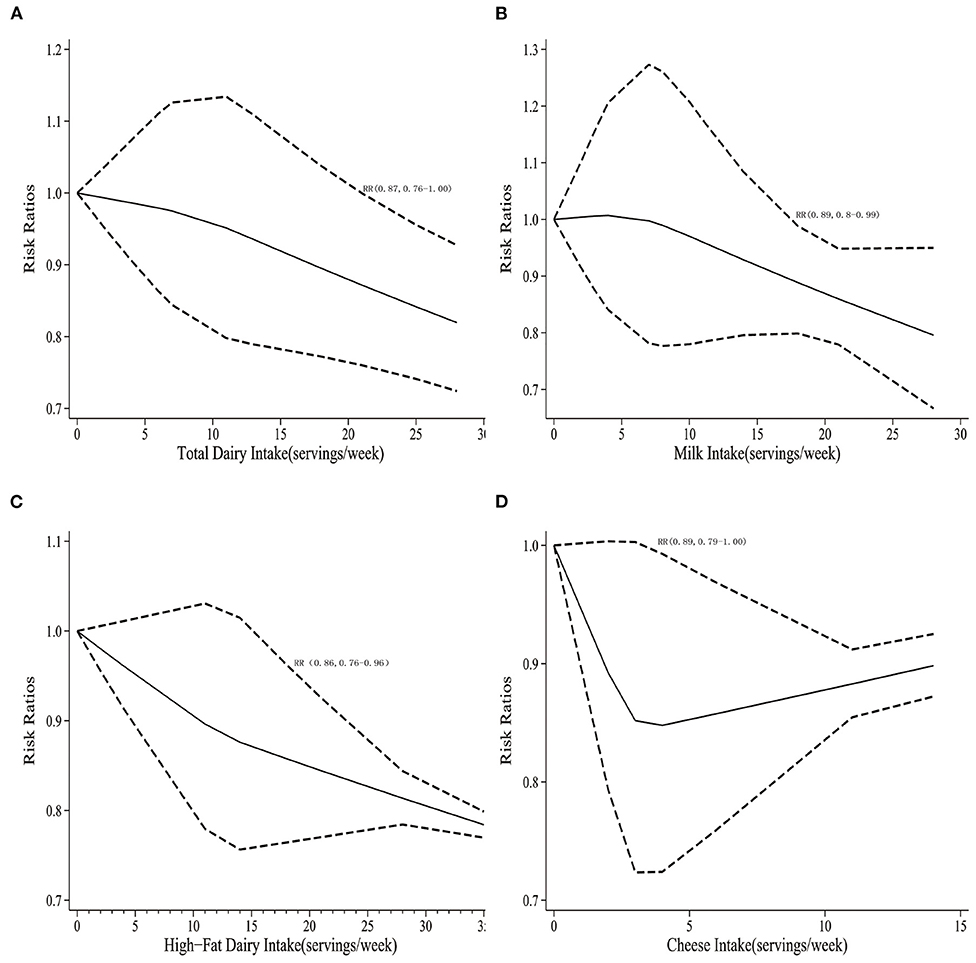
Figure 3. (A) Dose-response for total dairy products and the risk of endometriosis. (B) Dose-response for total milk products and the risk of endometriosis. (C) Dose-response for high-fat dairy products and the risk of endometriosis. (D) Dose-response for cheese and the risk of endometriosis.
Total Milk (High vs. Low)
Five studies involving 2,765 cases reported the association between milk product intake and the risk of endometriosis. No significant evidence suggested that high milk intake was associated with the risk of endometriosis comparing with the low milk intake (RR 1.01, 95% CI 0.79–1.29; I2 0%).
Four studies containing a total of 2,677 cases were included in the dose-response meta-analysis. As shown in Figure 3B, milk intake tended to be inversely associated with the risk of endometriosis. Specifically, as milk intake increased, the risk of endometriosis would significantly decrease in the risk of endometriosis when milk consumption was ≥18 servings/week (RR 0.89, 95% CI 0.80–0.99; pnon−linearity = 0.022).
High-Fat Dairy (High vs. Low)
As illustrated in Figure 2, three studies including 2,044 cases suggested that females with high high-fat dairy intake might have a reduced risk of endometriosis compared to females with the low milk intake (RR 0.86, 95% CI 0.75–0.98; I2 0%). Similarly, two studies containing a total of 1,966 cases were included in the dose-response meta-analysis, and the risk of endometriosis would significantly reduce when high-fat dairy consumption was ≥18 servings/week (RR 0.86, 95% CI 0.76–0.96; pnon−linearity = 0.012), as shown in Figure 3C.
Low-Fat Dairy (High vs. Low)
Three studies including 2,044 cases indicated that women with high low-fat dairy intake might not be associated with the reduce the risk of endometriosis comparing with the low-fat dairy intake (RR 0.98, 95% CI 0.94–1.02; I2 0%), as illustrated in Figure 2. And yet due to the limited number of the current studies, the dose-response meta-analysis of low-fat dairy could not be conducted.
Whole Milk (High vs. Low)
Two studies including 1,966 cases indicated that no obvious positive evidence that high whole milk intake was associated with the risk of endometriosis comparing with the low whole milk intake (RR 0.90, 95% CI 0.72–1.12; I2 0%), as illustrated in Figure 2. However, the dose-response meta-analysis for whole milk could not be conducted based on the limited current studies.
Ice Cream (High vs. Low)
Two studies including 1,966 cases revealed that no obvious association was found between the high ice cream intake and the risk of endometriosis comparing with the low ice cream intake (RR 0.83,95% CI 0.50–1.73; I2 0%), as illustrated in Figure 2. However, the dose-response meta-analysis for whole milk could not be conducted based on the limited current studies.
Reduced-Fat/Skim Milk (High vs. Low)
Two studies including 1,966 cases indicated that there was no correlation was found between the high reduced fat/skim milk intake and the occurrence of endometriosis comparing with the low reduced fat/skim milk intake (RR 0.83, 95% CI 0.50–1.73; I2 0%), as illustrated in Figure 2. However, the dose-response meta-analysis for reduced-fat/skim milk could not be conducted based on the limited current studies.
Yogurt (High vs. Low)
Two studies including 1,966 cases suggested that women with high yogurt intake might not have a reduced risk of endometriosis compared with women with low yogurt intake (RR 0.83, 95% CI 0.62–1.11; I2 44.9%), as illustrated in Figure 2. However, the dose-response meta-analysis for yogurt could not be conducted based on the rare current studies.
Cheese (High vs. Low)
As shown in Figure 2, five studies involving 2,765 cases the association between cheese intake and the risk of endometriosis. Compared with the low cheese intake, females with high cheese intake might have a reduced risk of endometriosis (RR 0.86, 95% CI 0.74–1.00; I2 0%).
Four studies containing a total of 2,677 cases were included in the dose-response meta-analysis. As illustrated in Figure 3D, cheese intake was inversely associated with the risk of endometriosis. Specifically, as cheese intake increased, the risk of endometriosis tended to have a significant decrease the risk of endometriosis when cheese intake was ≥2 servings/week (RR 0.89, 95% CI 0.79–1.00; pnon−linearity = 0.033).
Butter (High vs. Low)
Three studies including 1,173 cases suggested that females with high butter intake might have an increased risk of endometriosis comparing with the low butter intake (RR 1.27, 95% CI 1.03–1.55; I2 0%), as illustrated in Figure 2. However, the dose-response meta-analysis for butter could not be performed due to the number of limited current studies.
The numbers of the studies that reported the association between specific dairy foods and the risk of endometriosis are so rare, therefore the subgroup analyses and the test and publication bias could not be conducted.
Discussion
The present meta-analysis involving 120,706 participants showed that total dairy products intake would reduce the risk of endometriosis and there was a dose-dependent relationship, with a significant reduction in the risk of endometriosis when dairy intake was ≥21 servings/week. Similarly, the risk of endometriosis would significantly reduce when the intake of high-fat dairy products was ≥18 servings/week. However, in the qualitative analysis, this association was not found for low-fat dairy intake, and the dose-response could not be carried further due to the limited number of studies. Stratified analyses for specific dairy product categories indicated that high cheese intake might reduce the risk of endometriosis and there was a dose-dependent relationship. In the qualitative analysis, milk intake might not reduce the risk of endometriosis, but a dose-dependent relationship was found. Other specific dairy products such as whole milk, skim milk, ice cream, and yogurts have not shown significant evidence of an association with the development of endometriosis. Also, high butter intake would tend to increase the risk of endometriosis; no further dose-response could be performed to verify this result due to the limited number of studies.
The typical symptoms of endometriosis are pelvic pain, dysmenorrhea, dyspareunia, dysuria, malnutrition, and/or infertility (32). Women with endometriosis are often discovered because of dysmenorrhea, and the incidence of which is estimated to be between 45 and 90% in the developing countries (33, 34). Therefore, further improvement or treatment of the occurrence and progression of endometriosis remains an urgent challenge to be addressed. Current scientific evidence has pointed to the possibility that diet and lifestyle might affect inflammation, estrogen activity, the menstrual cycle, and prostaglandin metabolism in the body (35). As a result, diet and lifestyle can also affect the risk of endometriosis (36).
The pathogenesis of endometriosis remains inconclusive. Recently, a review by Rolla (37) systematically summarized the potential pathogenesis, diagnosis and treatment of endometriosis. Specifically, the current pathogenesis of endometriosis is mainly clustered on implantation theory, celomic theory, inflammatory disease, endometriomas, and hormonal receptors, with inflammatory receiving more attention from researchers. Scholl et al. (38) found increased expression of TNF-α in tissues from patients with endometriosis. Also, in vitro, TNF-α production by cultured endometrial cells were regulated by urocortin-2 and urocortin-3, neuropeptides expressed in human endometrium (39). Thus, TNF-α might be a key cytokine involved in the inflammatory aspects of endometriosis. In addition, IL-16, IL-8 in the peritoneal fluid may be involved in the pathogenesis of endometriosis by initiating or maintaining the inflammatory response in the peritoneal cavity (40). Cousins et al. suggested that human endometrium regenerates monthly in a cycle mediated by endometrial stem/progenitor cells such as CD140b+, CD146+, or SUSD2+ endometrial mesenchymal stem cells (eMSCs). N-cadherin+ endometrial epithelial progenitor cells and borderline population cells might be involved in the progression of the disease (41). Besides, it has been shown that Vitamin D receptor (VDR) and 1α-hydroxylase were overexpressed in the endometrium of patients with endometriosis, and thus Vitamin D might mediate the immune mechanism of endometriosis pathogenesis; however, this findings lacked evidence to support the relationship between VDR gene polymorphisms and endometriosis (42, 43). In a study by Zemel et al. (9) it was shown that in a mouse model, dairy diet reduced markers of oxidative and inflammatory stress, including TNF-αinhibitor and IL-6, which might laterally explain the possibility of dairy products reducing the risk of endometriosis (44). Besides, dairy products are high in magnesium, which not only reduces levels of inflammatory markers such as IL-6 and TNFα-R2 but also relaxes smooth muscle and might reduce retrograde menstruation (9). Our study showed that a total dairy products intake of more than 21 servings/week, or an average of >3 servings/day, significantly reduced the risk of endometriosis by 13% compared to women with no or low dairy intake, which is similar to the findings of Harris et al. (29). Simultaneously, the study by Harris et al. showed that milk intake reduced the risk of endometriosis, but only in the group with more than 2 servings/day. Likewise, our meta-analysis was conducted through High vs. Low showing that no support for the conclusion that milk reduces endometriosis, as this generalized between-group comparison could potentially attenuate the benefit of milk, whereas the dose-response analyses showed a reduced risk of endometriosis when milk intake was more than 18 servings/week, which is similar to the findings of Harris et al. (29). High-fat dairy products rich in calcium and vitamin D reduces oxidative stress and inflammatory stress, thereby reducing the risk of endometriosis (45). Dietary structure is a very complex lifestyle, and the underlying mechanisms of diet and the risk of endometriosis still need further research. Importantly, current guidelines for the diagnosis and management of endometriosis vary greatly in terms of recommendations and methodological quality from different countries to institutions, and more high-quality studies are needed to further refine them in the future (46).
Notably, our meta-analysis has the following advantages. First, to the best of our knowledge, this is the first study to systematically perform a qualitative meta-analysis of the relationship between dairy product intake and endometriosis. Furthermore, the qualitative results of the meta-analysis are further validated by the presentation of a dose-response meta-analysis. Second, some of the results of this study are contradictory to what is currently known, which will provide direction for future studies. Third, inter-study heterogeneity was low to moderate, and the quality of the included studies is high and the results are reliable.
Inevitably, this study also has some limitations. Firstly, due to the limited number of existing studies, subgroup analysis, and publication bias cannot be carried out. Second, although the results of most studies were adjusted for maximum covariates, the effects of residual confounding variables were not excluded. Third, due to the limited number of studies available, some specific types of dairy products, such as low-fat dairy, ice cream, and yogurt were not available for dose-response analyses.
Conclusion
Overall, dairy products intake is associated with a reduction in endometriosis, with significant effects when the average daily intake ≥3 servings. When analyzed according to the specific type of dairy product, it was shown that females with higher high-fat dairy and cheese intake might have a reduced risk of endometriosis. However, high butter intake might be associated to the increased risk of endometriosis. More future studies are needed to validate and add to this finding.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
XQ, MG, and QS designed the study. XL, LP, and WC did the literature searches and designed the data extraction form. XL, XQ, WC, MG, and QS collected the data. LP, WC, and WZ did the statistical analyses. XL, LP, WC, and WZ supervised the entire project. All authors critically revised subsequent drafts, read, and approved the submitted manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2021.701860/full#supplementary-material
References
1. Facchin F, Barbara G, Saita E, Mosconi P, Roberto A, Fedele L, et al. Impact of endometriosis on quality of life and mental health: pelvic pain makes the difference. J Psychosom Obstet Gynecol. (2015) 36:135–41. doi: 10.3109/0167482X.2015.1074173
2. Vinatier D, Orazi G, Cosson M, Dufour P. Theories of endometriosis. Eur J Obstet Gynecol Reprod Biol. (2001) 96:21–34. doi: 10.1016/S0301-2115(00)00405-X
3. Basta A, Brucka A, Górski J, Kotarski J, Kulig B, Oszukowski P, et al. The statement of Polish Society's Experts Group concerning diagnostics and methods of endometriosis treatment. Ginekol Pol. (2012) 83:871–6.
4. Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet. (2010) 27:441–7. doi: 10.1007/s10815-010-9436-1
5. Bianconi L, Hummelshoj L, Coccia ME, Vigano P, Vittori G, Veit J, et al. Recognizing endometriosis as a social disease: the European Union-encouraged Italian Senate approach. Fertil Steril. (2007) 88:1285–7. doi: 10.1016/j.fertnstert.2007.07.1324
6. Missmer SA, Chavarro JE, Malspeis S, Bertone-Johnson ER, Hornstein MD, Spiegelman D, et al. A prospective study of dietary fat consumption and endometriosis risk. Hum Reprod. (2010) 25:1528–35. doi: 10.1093/humrep/deq044
7. Heard ME, Melnyk SB, Simmen FA, Yang Y, Pabona JM, Simmen RC. High-fat diet promotion of endometriosis in an immunocompetent mouse model is associated with altered peripheral and ectopic lesion redox and inflammatory status. Endocrinology. (2016) 157:2870–82. doi: 10.1210/en.2016-1092
8. Parazzini F, Viganò P, Candiani M, Fedele L. Diet and endometriosis risk: a literature review. Reprod Biomed Online. (2013) 26:323–36. doi: 10.1016/j.rbmo.2012.12.011
9. Zemel MB, Sun X. Dietary calcium and dairy products modulate oxidative and inflammatory stress in mice and humans. J Nutr. (2008) 138:1047–52. doi: 10.1093/jn/138.6.1047
10. Stancliffe RA, Thorpe T, Zemel MB. Dairy attentuates oxidative and inflammatory stress in metabolic syndrome. Am J Clin Nutr. (2011) 94:422–30. doi: 10.3945/ajcn.111.013342
11. Zemel MB, Sun X, Sobhani T, Wilson B. Effects of dairy compared with soy on oxidative and inflammatory stress in overweight and obese subjects. Am J Clin Nutr. (2010) 91:16–22. doi: 10.3945/ajcn.2009.28468
12. Pei R, DiMarco DM, Putt KK, Martin DA, Gu Q, Chitchumroonchokchai C, et al. Low-fat yogurt consumption reduces biomarkers of chronic inflammation and inhibits markers of endotoxin exposure in healthy premenopausal women: a randomised controlled trial. Br J Nutr. (2017) 118:1043–51. doi: 10.1017/S0007114517003038
13. Altura BT, Altura BM. Endothelium-dependent relaxation in coronary arteries requires magnesium ions. Br J Pharmacol. (1987) 91:449–51. doi: 10.1111/j.1476-5381.1987.tb11235.x
14. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
15. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
16. Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. (1998) 280:1690–1. doi: 10.1001/jama.280.19.1690
17. Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. (2011) 342:d671. doi: 10.1136/bmj.d671
18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
19. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
21. Xu C, Doi SAR. The robust error meta-regression method for dose-response meta-analysis. Int J Evid Based Healthc. (2018) 16:138–44. doi: 10.1097/XEB.0000000000000132
22. Hamling J, Lee P, Weitkunat R, Ambuhl M. Facilitating meta-analyses by deriving relative effect and precision estimates for alternative comparisons from a set of estimates presented by exposure level or disease category. Stat Med. (2008) 27:954–70. doi: 10.1002/sim.3013
23. Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. (1992) 135:1301–9. doi: 10.1093/oxfordjournals.aje.a116237
24. Cheng W, Zhang Z, Cheng W, Yang C, Diao L, Liu W. Associations of leisure-time physical activity with cardiovascular mortality: a systematic review and meta-analysis of 44 prospective cohort studies. Euro J Prev Cardiol. (2018) 25:1864–72. doi: 10.1177/2047487318795194
25. Nodler JL, Harris HR, Chavarro JE, Frazier AL, Missmer SA. Dairy consumption during adolescence and endometriosis risk. Am J Obstet Gynecol. (2020) 222:257. doi: 10.1016/j.ajog.2019.09.010
26. Parazzini F, Chiaffarino F, Surace M, Chatenoud L, Cipriani S, Chiantera V, et al. Selected food intake and risk of endometriosis. Hum Reprod. (2004) 19:1755–9. doi: 10.1093/humrep/deh395
27. Samaneh Y, ShahidehJahanian S, Azadeh M, Anoshirvan K. The association of food consumption and nutrient intake with endometriosis risk in Iranian women: a case-control study. Int J Reprod Biomed. (2019) 17:661–70. doi: 10.18502/ijrm.v17i9.5102
28. Ashrafi M, Jahangiri N, Jahanian Sadatmahalleh SH, Aliani F, Akhoond MR. Diet and the risk of endometriosis in Iranian women: a case-control study. Int J Fertil Steril. (2020) 14:193–200. doi: 10.22074/ijfs.2020.44378
29. Harris HR, Chavarro JE, Malspeis S, Willett WC, Missmer SA. Dairy-food, calcium, magnesium, and vitamin D intake and endometriosis: a prospective cohort study. Am J Epidemiol. (2013) 177:420–30. doi: 10.1093/aje/kws247
30. Trabert B, Peters U, De Roos AJ, Scholes D, Holt VL. Diet and risk of endometriosis in a population-based case-control study. Br J Nutr. (2011) 105:459–67. doi: 10.1017/S0007114510003661
31. Heilier JF, Donnez J, Nackers F, Rousseau R, Verougstraete V, Rosenkranz K, et al. Environmental and host-associated risk factors in endometriosis and deep endometriotic nodules: a matched case-control study. Environ Res. (2007) 103:121–9. doi: 10.1016/j.envres.2006.04.004
32. Soave I, Occhiali T, Wenger J-M, Pluchino N, Caserta D, Marci R. Endometriosis and food habits: can diet make the difference? J Endometriosis Pelvic Pain Disord. (2018) 10:59–71. doi: 10.1177/2284026518773212
33. Chang SF, Chuang Mh. Factors that affect self-care behaviour of female high school students with dysmenorrhoea: a cluster sampling study. Int J Nurs Pract. (2012) 18:117–24. doi: 10.1111/j.1440-172X.2012.02007.x
34. Ozerdogan N, Sayiner D, Ayranci U, Unsal A, Giray S. Prevalence and predictors of dysmenorrhea among students at a university in Turkey. Int J Gynaecol Obstet. (2009) 107:39–43. doi: 10.1016/j.ijgo.2009.05.010
35. Jurkiewicz-Przondziono J, Lemm M, Kwiatkowska-Pamuła A, Ziółko E, Wójtowicz MK. Influence of diet on the risk of developing endometriosis. Ginekol Pol. (2017) 88:96–102. doi: 10.5603/GP.a2017.0017
36. Darling AM, Chavarro JE, Malspeis S, Harris HR, Missmer SA. A prospective cohort study of Vitamins B, C, E, and multivitamin intake and endometriosis. J Endometr. (2013) 5:17–26. doi: 10.5301/JE.5000151
37. Rolla E. Endometriosis: advances and controversies in classification, pathogenesis, diagnosis, and treatment. F1000Res. (2019) 8:F1000 Faculty Rev-529. doi: 10.12688/f1000research.14817.1
38. Scholl B, Bersinger NA, Kuhn A, Mueller MD. Correlation between symptoms of pain and peritoneal fluid inflammatory cytokine concentrations in endometriosis. Gynecol Endocrinol. (2009) 25:701–6. doi: 10.3109/09513590903159680
39. Novembri R, Carrarelli P, Toti P, Rocha AL, Borges LE, Reis FM, et al. Urocortin 2 and urocortin 3 in endometriosis: evidence for a possible role in inflammatory response. Mol Hum Reprod. (2011) 17:587–93. doi: 10.1093/molehr/gar020
40. Koga K, Osuga Y, Yoshino O, Hirota Y, Yano T, Tsutsumi O, et al. Elevated interleukin-16 levels in the peritoneal fluid of women with endometriosis may be a mechanism for inflammatory reactions associated with endometriosis. Fertil Steril. (2005) 83:878–82. doi: 10.1016/j.fertnstert.2004.12.004
41. Cousins FL, O DF, Gargett CE. Endometrial stem/progenitor cells and their role in the pathogenesis of endometriosis. Best Pract Res Clin Obstet Gynaecol. (2018) 50:27–38. doi: 10.1016/j.bpobgyn.2018.01.011
42. Lerchbaum E, Obermayer-Pietsch B. Vitamin D and fertility: a systematic review. Eur J Endocrinol. (2012) 166:765–78. doi: 10.1530/EJE-11-0984
43. Muscogiuri G, Altieri B, Annweiler C, Balercia G, Pal HB, Boucher BJ, et al. Vitamin D and chronic diseases: the current state of the art. Arch Toxicol. (2017) 91:97–107. doi: 10.1007/s00204-016-1804-x
44. Iwabe T, Harada T, Tsudo T, Tanikawa M, Onohara Y, Terakawa N. Pathogenetic significance of increased levels of interleukin-8 in the peritoneal fluid of patients with endometriosis. Fertil Steril. (1998) 69:924–30. doi: 10.1016/S0015-0282(98)00049-1
45. Zondervan KT, Becker CM, Koga K, Missmer SA, Taylor RN, Vigano P. Endometriosis. Nat Rev Dis Primers. (2018) 4:9. doi: 10.1038/s41572-018-0008-5
Keywords: dairy products, endometriosis, dose-response, milk, meta-analyses
Citation: Qi X, Zhang W, Ge M, Sun Q, Peng L, Cheng W and Li X (2021) Relationship Between Dairy Products Intake and Risk of Endometriosis: A Systematic Review and Dose-Response Meta-Analysis. Front. Nutr. 8:701860. doi: 10.3389/fnut.2021.701860
Received: 29 April 2021; Accepted: 24 June 2021;
Published: 22 July 2021.
Edited by:
Donato Angelino, University of Teramo, ItalyReviewed by:
Cinzia Ferraris, University of Pavia, ItalyHoda Elkafas, University of Illinois at Chicago, United States
Copyright © 2021 Qi, Zhang, Ge, Sun, Peng, Cheng and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuepeng Li, enpzbHl5bHhwQDE2My5jb20=
 Xiangying Qi1
Xiangying Qi1 Wenyan Zhang
Wenyan Zhang Wenke Cheng
Wenke Cheng